Biases impact care of opioid-dependent patients 2



With the end of a congressional provision that had extended Medicaid coverage during the COVID-19 public health emergency, states are set to begin on April 1 what some Catholic health care leaders and Medicaid experts expect to be a chaotic and cumbersome process to redetermine the
eligibility of the more than 90 million people currently enrolled in Medicaid or the Children’s Health Insurance Program.
A sweeping budget measure passed by Congress and signed by President Joe Biden in the final days of 2022 ended the continuous Medicaid coverage requirement for states that had been in effect since March 2020. It allows the recertification of eligi-
bility — a process dubbed the Medicaid unwinding — to start April 1. The end result of the unwinding will be that 5.3 million to 14.2 million people will lose their coverage, according to Kaiser Family Foundation estimates.
The Office of the Assistant Secretary for Planning and Evaluation within the Department of Health and Human Services pre-

dicts about half of those disenrollments will be of people who are eligible for coverage but stymied in providing proof by procedural hurdles, such as not being able to get through to the appropriate state agency because of overwhelmed phone lines.
Mike Slubowski, president and chief executive of Trinity Health, says the Continued on 4

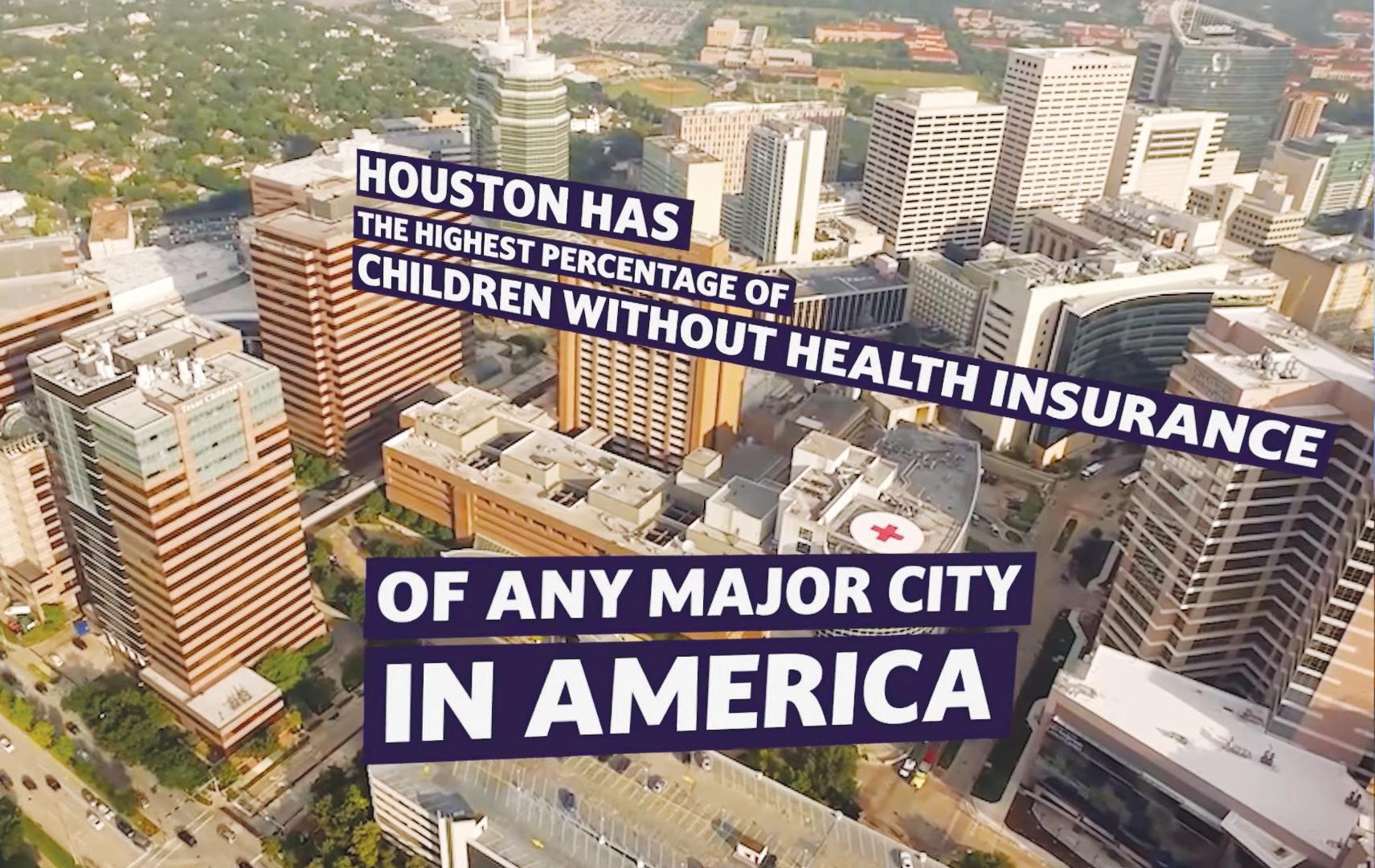
A video series being produced by St. Luke’s Health is spotlighting the paradox faced by people who live near the Texas Medical Center in Houston but are unable to access most of its world-class services because they are uninsured or underinsured.
St. Luke’s Health, based in Houston, is part of CommonSpirit Health. St. Luke’s and the Baylor College of Medicine are joint owners of Baylor St. Luke’s Medical Center, an academic and research hospital that is part of the 1,345-acre Texas Medical Center complex. The complex calls itself “the largest medical city in the world.”
The complex is a partnership of several member institutions, including hospitals, health systems, public health agencies, colleges and hospices. Facilities on the


 By JULIE MINDA
By JULIE MINDA
Feller concedes that people who are accustomed to how things are usually done in memory care facilities may find the approaches used in the newest unit at ArchCare at Ferncliff Nursing Home and Rehabilitation Center to be rather unorthodox.
With some guidance, residents of the Center for Advanced Memory Care that Ferncliff opened in January 2022 plan their own recreation calendar, prepare the dining room for mealtimes, maintain Ferncliff gardens and greet visitors, among countless other activities, says Feller. She is assistant
In mid-February CHA will launch an online Ministry Identity Assessment platform that will streamline some of the processes of conducting a comprehensive evaluation of how well ministry systems and facilities manifest the Catholic health mission.
Ministry leaders will be able to use the tool to organize teams to assess how effectively their organizations are living out each of seven areas of responsibility, as set out in the core commitments of Catholic health care. The online tool guides the teams through the assessments, the analysis of the results and the development of performance improvement action plans based on the findings.
Dennis Gonzales, CHA senior director of mission innovation and integration, says by participating in the thorough, stepby-step self-assessment process, Catholic health systems and facilities will identify
strengths and reasons to celebrate as well as areas for growth and continuous quality improvement. The tool offers a blueprint for such improvements and a way of keeping track of progress toward those goals. Gonzales says the tool will help the ministry to build a repository of best practices from across Catholic health care to serve as inspiration for ministry organizations looking to expand their work.
The portal incorporates an updated version of the comprehensive Ministry Identity Assessment tool that CHA first made available to its representative members in 2019. Developed by a task force of mission and ethics experts convened by CHA, the assessment tool is in line with Gospel and theological values and foundational elements of Catholic social teaching.
As doctors weigh treatment approaches for patients who are addicted to opioids, Mark Kuczewski thinks it is important that these clinicians acknowledge how their own biases influence care plans.
Kuczewski directs the Neiswanger Institute for Bioethics and is a professor of medical ethics for the Stritch School of Medicine at Loyola University Chicago.
During a CHA webinar titled “Clinical Ethics and Opioid Use Disorders,” he said health care providers’ views on addiction can have a profound impact on the patients they treat. Misconceptions can lead to poorer outcomes for patients.
Some providers might place great weight on a patient’s prognosis for recovering from addiction when making clinical decisions. “Unfortunately, there’s no particularly good way to make such a prognostication,” Kuczewski explained in an emailed response to follow-up questions. “All a physician can do is assess the patient’s expressed willingness to seek treatment and help to arrange the conditions that make recovery more likely, e.g., direct discharge to a treatment facility.”
Kuczewski told the webinar audience that it is essential for providers to understand the biological underpinnings of addiction and the implications for treatment of comorbidities. He said that a medical judgment should not be based on whether the clinician concludes a person with late-stage substance dependency has a quality of life worth extending.
Kuczewski told Catholic Health World that as a bioethicist he believes “a clinician should undertake extensive treatments that improve a patient’s quality of life and potentially prolong a patient’s life, regardless of whether the patient’s health ultimately will continue to deteriorate because of an active addiction to alcohol or other drugs.

“That is, medicine does not usually judge treatments as effective only if they are permanently successful and the outcomes for patients with substance use disorders should not be judged differently,” he explained.
Opioid misuse and dependency have risen sharply in the U.S. for three decades, spurred on by pharmaceutical companies and pharmacies’ malicious marketing of addictive substances to increase sales. The U.S. Department of Health and Human Services estimated 10.1 million people aged 12 or older misused opioids in 2018, with most of them using prescription pain relievers. The agency said emergency department visits for opioid overdoses rose 30% between July 2016 and September 2017.
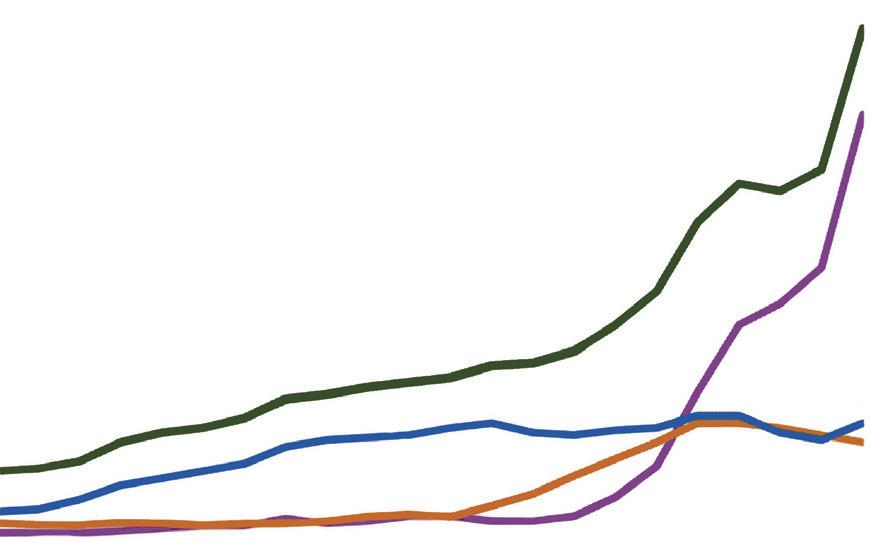
Overdose deaths involving opioids have increased by more than eight times since 1999, according to the Centers for Disease Control and Prevention. Kuczewski said 75% of the nearly 92,000 drug overdose deaths in the U.S. in 2020 involved an opioid.
Over about the last 10 years, criminals who have been illicitly manufacturing and trafficking drugs have been lacing heroin and other street drugs with synthetic fentanyl, a highly concentrated, powerful opioid. Fentanyl has led to an “explosion” of overdose deaths, said Kuczewski.
The use of medication-assisted therapies to quell drug cravings and access to safe injection facilities are potentially lifesaving options for people who are addicted and using street drugs, he said.
Clinicians and ethicists in health care facilities are increasingly deliberating clinical and ethical quandaries related to patients and opioids.
For patients in pain, clinicians must
UNITED STATES, 1999-2020
Source: CDC/NCHS, National Vital Statistics System, Mortality. CDC WONDER, Atlanta, GA: US Department of Health and Human Services, CDC; 2020. http://wonder.cdc.gov/.
determine to what extent prescription opioid use is appropriate, for what types of pain, in what dose and for how long, given the heightened potential for developing dependency and other harms. Addiction risks are not necessarily relevant when it comes to palliating severe pain in patients at the end of life, Kuczewski said.
He noted that it can be difficult for a clinician to tell the difference between patients who are legitimately seeking prescription opioids to mitigate unresolved physical pain and those who suffer from a substance use disorder and “can easily come to believe they are in pain.”
Kuczewski told Catholic Health World that it is essential for prescribing physicians to have a plan for “how the end of the use of the opioids will occur or (for) engaging in alternative modalities of managing the pain.”
He said a particular challenge is when providers struggle to keep safe patients who arrive at a hospital seriously ill and actively drug seeking. Patients may try to smuggle in drugs and even attempt to inject their own illicit drugs into a central or peripheral catheter.
Kuczewski said an important backdrop to decision-making around patients’ safe use of opioids has to do with all patient-facing health care professionals’ understanding of the roots of substance use disorders, including opioid addiction.
He said some clinicians believe opioid addiction is the result of people’s choices and they bear full responsibility. Others believe opioid addiction is primarily related to genetic predisposition to addiction or untreated underlying mental illness, such as depression.
Kuczewski said research shows that opioid use — especially over time — permanently alters the brain’s circuitry, so that the brain is in a continual state of deprivation.
This is the root of drug craving and can lead to drug-seeking behavior, said Kuczewski.
According to the CDC, “evidence-based approaches to treating opioid addiction include medications and combining medications with behavioral therapy. ... Medications used in the treatment of opioid addiction support a person’s recovery by helping to normalize brain chemistry, relieving cravings, and in some cases preventing withdrawal symptoms.”
Kuczewski used a patient case study during the webinar to illustrate how a nuanced consideration of opioid addiction can influence treatment decisions: A 30-year-old man was admitted to a health care facility with severe pain, concentrated on his side, and a fever. He reported he’d recently relapsed and was in opioid withdrawal. The hospital had twice before treated him for endocarditis. The attending physician sought an ethics consult to determine, among other concerns, whether mitral valve replacement was appropriate, given the likelihood that the patient would continue to use opioids and that would render the risky and invasive procedure futile.
Medical providers want to bring about the patient’s good, and in questioning the ethics of heart valve surgery the physician is saying that if the procedure has a high risk of failure owing to the use of opioids, perhaps it really isn’t something a surgeon should be doing, Kuczewski explained.
In the actual case that is the basis of the case study, the clinician-ethicist team decided that a heart surgeon should replace the heart valve. After surgery, the hospital discharged the patient to inpatient rehab. The patient went two years before again relapsing and seeking care at the hospital for endocarditis that was likely precipitated by the use of injectable drugs.
Kuczewski told Catholic Health World that, generally, physicians decide what pro-
cedures or other treatments or medications to offer based on their judgment of what has a reasonable chance of bringing medical benefit.
He explained that patients’ and surrogates’ rights to make decisions are mostly negative — that is, they can refuse any treatment. But they can’t make a physician offer something he or she believes will be ineffective. Kuczewski said in the case examined during the webinar, “two years of recovery and freedom from the endocarditis should probably be seen as a win.” If the likelihood of permanent recovery is the benchmark for care decisions, the patient with substance dependence may not be offered lifesaving procedures like valve replacement.
Kuczewski said in treating patients with an opioid addiction, clinicians and patients should work together to realistically define goals. Perhaps, he said, there is success in simply reducing harm to the patient, paving a way for potential addiction recovery and giving the patient better quality of life — even if the person continues using.
“We’re saying we don’t want you to die,” Kuczewski said of approaches that treat the symptoms regardless of the resolution of the addiction.
jminda@chausa.org
Virtual Program: Using Inflation Reduction Act Incentives to Meet Environmental Sustainability Goals Jan. 18 | 1 – 2 p.m. ET
Virtual Series: Ministry Formation Workshop Tuesdays | From Jan. 24 to June 20 | 1 – 3 p.m. ET
CHA’s Protect What’s Precious Toolkit Introduction Call Jan. 25 | 1 – 1:45 p.m. ET
Virtual Dialogue: Honoring the Religious Diversity of Our Staff — Leveraging the Expertise of Chaplains Jan. 26 | 1 – 2:15 p.m. ET
Catholic Health World (ISSN 8756-4068) is published semimonthly, except monthly in January, April, July and October and copyrighted © by the Catholic Health Association of the United States. POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@ chausa.org. Periodicals postage rate is paid at St. Louis and additional mailing offices. Annual subscription rates: CHA members free, others $29 and foreign $29.
Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA. Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
Virtual Program: Foundations of Catholic Leadership Orientation: Jan. 31 | 1 – 2 p.m. ET
Sessions: Thursdays | From Feb. 2 to March 23 | 1 – 3:30 p.m. ET
United Against Human Trafficking Networking Zoom Call Feb. 7 | Noon – 1 p.m. ET

CHA is offering resources to help its members start off the year by focusing on well-being.
Jill Fisk, director of mission services at CHA, says the ReNew Year framework that CHA began rolling out this month is loosely based on the concepts that underpin the U.S. Department of Veterans Affairs’ Whole Health approach to care.

The approach puts the person at the center of a circle with mindful awareness surrounding the core and influencers such as “spirit and soul,” “moving the body,” and “friends, family and co-workers” in the next layer. The VA says Whole Health “centers around what matters to you, not what is the matter with you.”
Fisk says CHA’s modified approach aligns with the ministry’s Catholic and Christian identity to help users reconnect with themselves, with others and with the ministry’s mission, vision and values. She says the approach is based on what members of CHA’s well-being task force indicated was needed to help staff improve their well-being.
The task force’s recommendation was “to call people back into re-envisioning and reimagining their purpose, their vocation, to be reinspired,” she adds.
ReNew Year has a theme for each weekday — Mission Monday, Time to Think Tuesday, Wonder Wednesday, Thankful Thursday and Refocus Friday. Saturday and Sunday share the theme of Worthy Weekend.
The ReNew Year resources are posted on a page of CHA’s website. For each day of the week, the webpage includes an explanation of “the why” behind the theme and links to various resources curated by CHA. Those resources include questions for reflection, prayers and videos. Additional resources will be added later.
Josh Matejka, director of creative services at CHA, says ReNew Year was designed to be simple in hopes of helping users develop a rhythm of well-being in their lives. “The idea is that this will be the first step in a more foundational approach to well-being,” he says.
The ReNew Year resources are available at chausa.org/renewyear.
CHA’s mission “to advance the Catholic health ministry of the United States in caring for people and communities” is tightly connected to the association’s core values of integrity, respect, excellence and stewardship.
Beyond a mission statement and core values, CHA in recent years created a shared statement of identity, outlined health care principles and priorities in the document “Our Vision for U.S. Health Care,” and developed and updated successive threeyear strategic plans that guide the work of the association.
These documents provide clarity to CHA’s purpose and priorities and frame the principles the association and its members use to advocate for health policy that leaves no one behind.
With the fiscal year 2021–2023 strategic plan set to be updated, the CHA Board of Trustees determined that an important first step would be to develop a clearly articulated vision statement that aligns with the mission and values of CHA and informs CHA’s strategic priorities going forward. The board believes adopting a vision statement that captures the ministry’s aspirations for CHA and Catholic health care in the U.S. is of great importance in a time of serious challenges, immense unmet needs,
and increasing opportunities to serve in dynamic new ways.
The board appointed a Vision Committee in the fall to craft the statement. “Given the continuous change and need for transformation in the health care industry, the board felt it was the right time to review and update the strategic plan for CHA and to do so in the context of its vision statement, mission and values,” said Laura Kaiser, board chair.
chausa.org/renewyear
Kaiser, president and chief executive of SSM Health, and Damond Boatwright, vice chair of the CHA board and president and chief executive of Hospital Sisters Health System, co-chair the Vision Committee.
CHA board members who fill out the committee are Cynthia Bentzen-Mercer, executive vice president/chief administrative officer, Mercy; Dougal Hewitt, executive vice president/chief mission and sponsorship officer, Providence St. Joseph Health; Fahad Tahir, chief strategy officer, Ascension Saint Thomas; and Tina M. Weatherwax-Grant, senior vice president, public policy and advocacy, Trinity Health.
Kaiser said that in order to achieve desired outcomes, an organization’s vision statement, mission statement, values and strategy must work in harmony. “A vision statement offers an aspirational view of the desired future, a direction to work toward. A mission statement describes why an organization and the people who comprise it are pursuing the vision and endeavoring to complete the work necessary to deliver on the mission. Our values describe desired behaviors we will embrace as together we pursue our vision, mission and strategy,” she said.
Tenfold Health, a consultancy providing services to CHA and the board on the vision statement development, is reaching out to CHA members and external stakeholders this month to seek their participation in interviews or virtual focus groups. Those information gathering sessions are intended to gain insight into what the evolution of Catholic health care might look like and what opportunities might exist for the ministry to positively impact the direction of health care in the U.S. During a meeting in November, members of the Vision Committee agreed that the vision statement needs to be bold and serve as a healing and unifying call to action.
This month CHA members who have been active in the association through service on committees, advisory councils, work groups or affinity groups are being asked to complete a short survey. Other members will be invited to participate in small group Zoom meetings with Tenfold to provide additional input.
Information gathered from the survey and conversations with members will be shared with the Vision Committee and used to shape the vision statement that will be approved by the CHA board and shared with the CHA membership in June.
For more information about the visioning process, contact Brian Reardon, CHA vice president of communications and marketing, at breardon@chausa.org.
“A vision statement offers an aspirational view of the desired future, a direction to work toward.”
— Laura Kaiser
unwinding is certain to be a “real disruptor” for providers of care to the low-income Americans who rely on Medicaid.
The process will be complicated in part because each state will have its own methods and timelines of up to 12 months for the redeterminations of eligibility, Slubowski says. He points out that many states aren’t planning for “an easy, warm handoff” of those who no longer quality for Medicaid to other coverage options such as the federally subsidized insurance marketplace. “We are worried about that.”
Trinity Health, based in Livonia, Michigan, operates in 26 states and cares for 1.5 million patients who rely on Medicaid or states’ CHIP coverage. CHIP provides lowcost insurance for children whose family income is too high for Medicaid but too low to purchase private insurance.
If just 5% of Trinity’s Medicaid and CHIP insured patients lose coverage and have no other means to pay for treatment, Slubowski says the system stands to take an annual $80 million hit on revenue.
Compounding that financial blow, he says, could be that many of those patients, once uninsured, would no longer have access to a regular source of primary care to prevent or manage chronic conditions. Instead, acutely ill patients likely would turn to emergency rooms, where the cost of providing care is high, and urgent care facilities, where patients get only episodic treatment.
Tricia Brooks, a research professor at the Georgetown University McCourt School of Public Policy’s Center for Children and Families, urges all health care providers to be proactive in informing patients about the unwinding. Brooks took part in a CHA webinar in November on the unwinding and discussed it during a later interview with Catholic Health World She notes that Medicaid and CHIP cover about half of the nation’s children. “Medicaid is also the predominant source of coverage for pregnancy, people of color and rural communities,” she adds.
Brooks says the redetermination requirement will affect all of the children enrolled in Medicaid and most of the children enrolled in CHIP because of how some of those state programs are connected to Medicaid.
She notes that researchers say 6 million children stand to lose Medicaid or CHIP coverage in the unwinding. For some of them, the coverage loss will be because they no longer qualify due to changes in their family income or situation. For others, the coverage will end because their families fail to successfully complete the reenrollment process.
However, the deal struck on Medicaid redeterminations in the end-of-the-year spending bill requires that states continue coverage for children for at least a year, even if a family’s income makes them ineligible for government health insurance. The measure also makes permanent what had been a temporary rule letting states provide Medicaid coverage for a year postpartum.
Congress put the continuous coverage requirement in place as one of several requirements for states to qualify for enhanced funding during the pandemic. Since then, the Medicaid and CHIP rolls have grown by more than 19 million, according to the Kaiser Family Foundation.
Brooks says some states might be under political pressure to finish the redetermi-

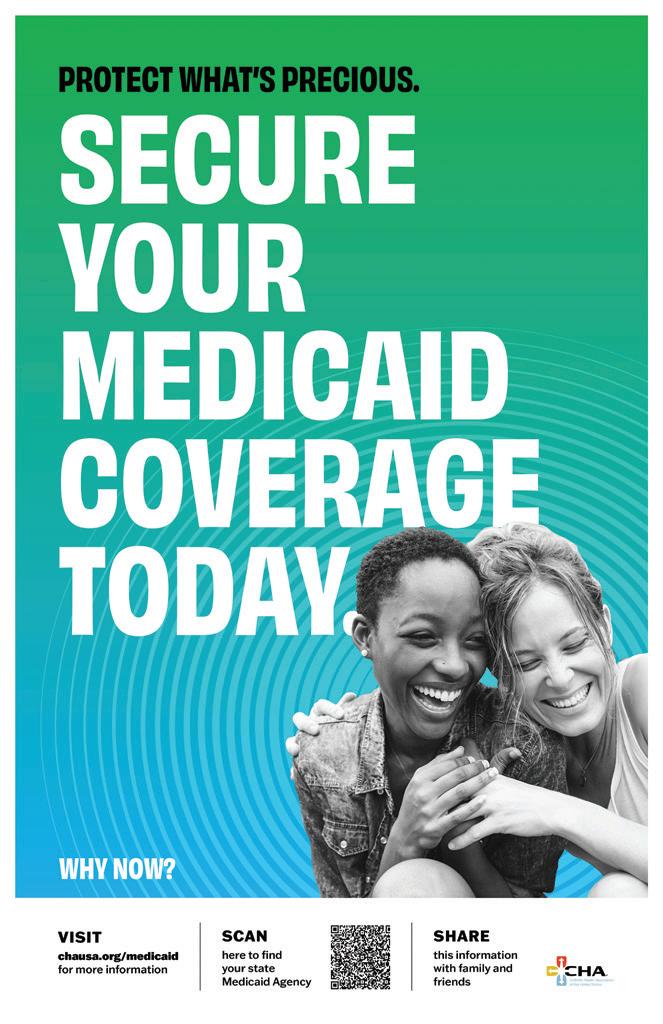
CHA is expanding the resources in its Medicaid Makes It Possible campaign to add free downloadable tools that member organizations can rebrand or cobrand and use to guide patients through the Medicaid eligibility redetermination process. That process has been on pause nationwide since the start of the pandemic but is set to restart April 1.
Josh Matejka, director of creative services at CHA, says the Protect What’s Precious resources are designed to be patient-facing, with clear, concise messages.
One of the tools is a set of posters that have the address for the Medicaidfocused page on CHA’s website and a QR code that, when scanned by a smartphone camera, links to Medicaid.gov, where users can access the websites of state agencies that are handing the reenrollment process. Postcard-size versions of the posters that can be used as handouts are also available. The posters
nations on eligibility quickly and cull their rolls, especially given that the enhanced federal funding begins to phase out in the quarter after the provision ends.
The unwinding, Brooks says, “is a really big deal because of the unprecedented volume of work required for states to return to their routine eligibility and enrollment operations.” She adds that it is coming at a time when states, like private employers, face challenges in recruiting and retaining workers.
Brooks and her colleagues at Georgetown have created an extensive set of “unwinding resources” to assist various stakeholders throughout the process.

CHA also has created tools for systems to use and to customize to help in guiding Medicaid patients through the unwinding.
Paulo Pontemayor, senior director of governmental relations at CHA, notes that the organization’s members provide care at more than 2,200 sites, putting them in direct contact with many patients who rely on Medicaid.

“CHA is committed to Medicaid and strengthening Medicaid but also to protecting beneficiaries as part of our commitment to ensuring access and affordability for all,” Pontemayor says. “This is linked to our strategic advocacy goals and also really to the essence of what CHA’s work is since the passing of the Affordable Care Act.”
Another organization offering advice and assistance to health care providers on the Medicaid redeterminations is Catholic Charities USA. Ben Wortham, the group’s vice president of behavioral health integration, and Susan Loughery, associate executive director of Catholic Charities Trenton in New Jersey, also took part in the CHA webinar in November.
Wortham notes that a majority of the billing that Catholic Charities does nationwide for behavioral and mental health care are Medicaid claims. The organization’s revenue for that care falls far short of its expenses, he says.
“For someone to lose their insurance and Catholic Charities not be able to bill that insurance, it would really add to that deficit,” Wortham says.

He says the organization is proactively working with clients who are reliant on
are available in English and Spanish.
Ministry members can broadcast on their closed-circuit TV systems a CHA video with information about how patients can reenroll in Medicaid.
The toolkit also includes talking points on how to discuss the reenrollment process with patients. CHA will introduce the toolkit in a call from 1-1:45 p.m. ET, Jan. 25. For details visit chausa.org.
Medicaid to ensure that they maintain their eligibility for the coverage.
Wortham says Catholic Charities partners with many Catholic hospitals and systems on programs. He welcomes any providers that overlap the organization’s vast footprint to reach out for collaborations related to the Medicaid unwinding.
Providence St. Joseph Health set up a steering team in fall 2021 to plan for the unwinding. Tue Nguyen, the system’s director of patient outreach and financial sponsorship, says team members are from many disciplines, including financial counseling, population health, communications and marketing, government relations, com-
munity health investment and physician enterprise. They have set up policies and best practices in advance of the unwinding in hopes of minimizing its financial impact on patients and the system.
One of the team’s strategies has been to build partnerships between the system’s financial counselors, who are well-versed in Medicaid enrollment and qualifications, and its community health workers, who are on the frontlines in the rural and communities of color that are often most reliant on the public health insurance program.
At Providence ministries, the two groups are meeting virtually every other week to educate each other — the counselors discussing their resources and the community health workers sharing their outreach efforts.
The team is working on a variety of communications that will be deployed to reach patients before the unwinding begins. Some communications will be customized for enrollees by language and to point them to websites with information specific to the state in which they reside.
Nguyen says that because of the team’s prep work, Providence is “very ready” for the start of the redeterminations.
Slubowski says Trinity Health’s preparations for the unwinding include identifying programs that can assist patients who might fall through the cracks. It is also readying an “education center” with resources for staff, especially those at its safety net health centers, to understand and explain to patients the specifics of the redetermination process in their state.
Slubowski says the system’s advocacy, well-being, community health, marketing and communication and revenue excellence teams are all playing a role in preparing care providers and patients for the unwinding.


“Our folks are nimble and they’re doing their very best to keep the spinning plates going,” he says. “But it’s a challenge.”
leisenhauer@chausa.orgFrom page 1
campus tally more than 9,200 beds, 10 million patient visits, and 180,000 surgeries per year.
Despite the complex’s vast health care offerings, Doug Lawson, chief executive of St. Luke’s Health and senior vice president of operations for the Texas Division of CommonSpirit Health, says many residents of Houston and surrounding communities can only access its care in its emergency departments because they lack health insurance for primary and specialty care.
“That is the most expensive and inefficient and, ultimately, ineffective way to project care,” Lawson says.
To shine a light on the situation, St. Luke’s is tapping the insight of health care executives and providers and civic leaders for its eight-part video series called “ExamiNATION.”
The first episode, “The Challenge,” came out in September. The five-minute video focuses on social justice issues within Houston’s health care system. One of the initial statements made is that the city has the highest percentage of uninsured children of any major American city. The speaker, Stephen L. Klineberg, the director of the Kinder Institute for Urban Research at Rice University in Houston, says that fact is central to the challenge of “building a viable society in the 21st century.”
Another featured speaker in the episode is Houston Mayor Sylvester Turner. He notes that in some of the city’s ZIP codes life expectancies are as much as 25 years less than in others.
“Recognizing where these health disparities are, that’s important,” Turner says in the video. “But then, once you recognize them, the question is: What type of investment, what type of resources are going to be put into these communities not just to touch on them but to be transformational in terms of people’s health care to remove the unjust disparities, the inequities, and bring these communities up?”
The second episode, “Managing Chronic Conditions & Cancer,” came out in October. It underscores the importance of regular screenings and maintenance exams to detect disease early and how lifestyle decisions and environmental factors affect health.
that care is delivered consistently and uniformly,” Wells says. “The reality is, it is not.”
He’s hopeful that the video series will open the eyes of the leaders across the city and state to the need for access to and funding for medical care for all residents.
“I’m old enough to know better than to think that it’s going to revolutionize things,”
Wells says of the video series. “But I think maybe it will move the ball farther down the road in terms of allowing people to think about these things, perhaps differently, and to realize we’re all in this together.”
Released in December, the third episode in the series focuses on the need for access to mental health care. One of the speakers is Cardinal Daniel DiNardo of the Archdiocese of Galveston-Houston. “One of the things the church can do is to encourage our own people and people everywhere to not see mental distress or mental health distress as something that is shameful,” Cardinal DiNardo says.
He adds that mental, psychological and spiritual health “is important if we’re going to make sure that our bodily health is sound.”
Other topics that the series will explore in future episodes include heart health, human trafficking, health care affordability, and diversifying the caregiver workforce.
One of the roadblocks to access that the speakers in the videos mention is Texas’ refusal to expand Medicaid under the Affordable Care Act, as most states have done. A study by Texas A&M University estimates that if the state were to expand Medicaid under the ACA, 1.5 million more Texans would be eligible to enroll. The U.S.
Census Bureau says Texas, at 18%, has the highest percentage of uninsured people in the nation.
Lawson says St. Luke’s has been among the voices in the health care sector strongly urging the state legislature to expand the public insurance program under the ACA, so far to no avail. “People are suffering as a result of our lack of expansion,” he says. “It’s very disappointing and frustrating for all of us that are in health care in Texas.”
St. Luke’s is using its social media channels to get the “ExamiNATION” videos seen. Lawson says he knows the videos are getting views based on the number of shares, likes and comments on the posts and on the feedback he gets, which he says is overwhelmingly positive. The first episode in the series had more than 2,600 views on YouTube by early January.
Lawson says St. Luke’s is using the series as a sort of pilot to see how best to get its messages out. He hopes that the videos are sparking discussions at dining room tables, in corporate board rooms and among policymakers about the need for wider access to health care.
“Ultimately, more than anything, I’m hopeful that we create a positive and productive conversation that puts us in a position to improve health and wellness across the communities that we serve,” he says.

leisenhauer@chausa.org
One of the speakers in the eight-minute episode is Dr. Kenneth Wells, a physician who is president of Alken Health Resources, a firm that designs, implements and manages corporate health care and wellness services. Wells is a past member of the board of directors of St. Luke’s and of Irving, Texasbased CHRISTUS Health.


He notes in the video that early detection is a key to thwarting the progression of cancer and other diseases. “You may not stop the disease from occurring in totality, but you can certainly flatten the curve as it relates to it and ideally prevent it from extending on and requiring more invasive-type therapy,” he says.
In an interview with Catholic Health World Wells adds that the inability of some people to get screenings and checkups puts them at greater risk of getting diagnosed later in the disease process and having a bad medical outcome. “We like to think
“We like to think that care is delivered consistently and uniformly. The reality is, it is not.”
— Dr. Kenneth Wells
Novice drivers are experiencing the perils of distracted and impaired driving — in a controlled setting — through a community benefit program of St. James Healthcare in Butte, Montana.
The Butte School District mandates participation in the Distracted Driver training for students taking the district’s driver education class. About 160 students took part in last year’s training on June 30. About 1,100 students have completed the training since St. James started it.
During the three-hour session, participants learn that driving while distracted or impaired can be deadly, why it’s important to give big rigs a lot of space and how to safely yield the right-of-way to emergency vehicles.
They navigate an obstacle course in a golf cart. On the first pass, the driver focuses on the course, the second time around the student taps out a text while driving, and on the final go-around, the driver peers through vision-distorting goggles that mimic the effects of inebriation. Staff clock students during each spin to show how distractions and inebriation slow response times.
Amber Henson is the trauma and disas-

ter planning assistant at the hospital, which is part of Intermountain Healthcare’s SCL Health. She says the course is a “great way to not only talk about the dangers of distracted driving,” but also to demonstrate those hazards firsthand on a controlled course.
She says motor vehicle accidents are one of the leading causes of trauma and death in Montana, and Butte has a high number of alcoholrelated vehicular accidents.
St. James replicated the program from one offered by another SCL hospital,
St. Vincent Healthcare in Billings, Montana. St. James has offered it around midyear each year since 2015, except for two years due to COVID-19 disruption.
Members of St. James’ trauma and patient registration teams as well as nurses from the intensive care unit and other associates volunteer to staff the sessions and present much of the training’s content.
The driving course is set up on Butte High School’s parking lot, with the golf carts, 500 traffic cones and other supplies loaned by local businesses. Henson says that the portion of the training when the students

1
Completing a ministry identity assessment is formative for ministry executives and staff, says Fr. Joseph Cardone, chief mission officer for Bon Secours Mercy Health. That system has been piloting the online tool.

Gonzales says the updated web-based Ministry Identity Assessment retains the original emphasis on the seven core commitments of Catholic health care. Those commitments represent a consensus of the Catholic health ministry. The second edition of the assessment tool also retains components drawn from the Baldrige Health Care Criteria for Performance Excellence.
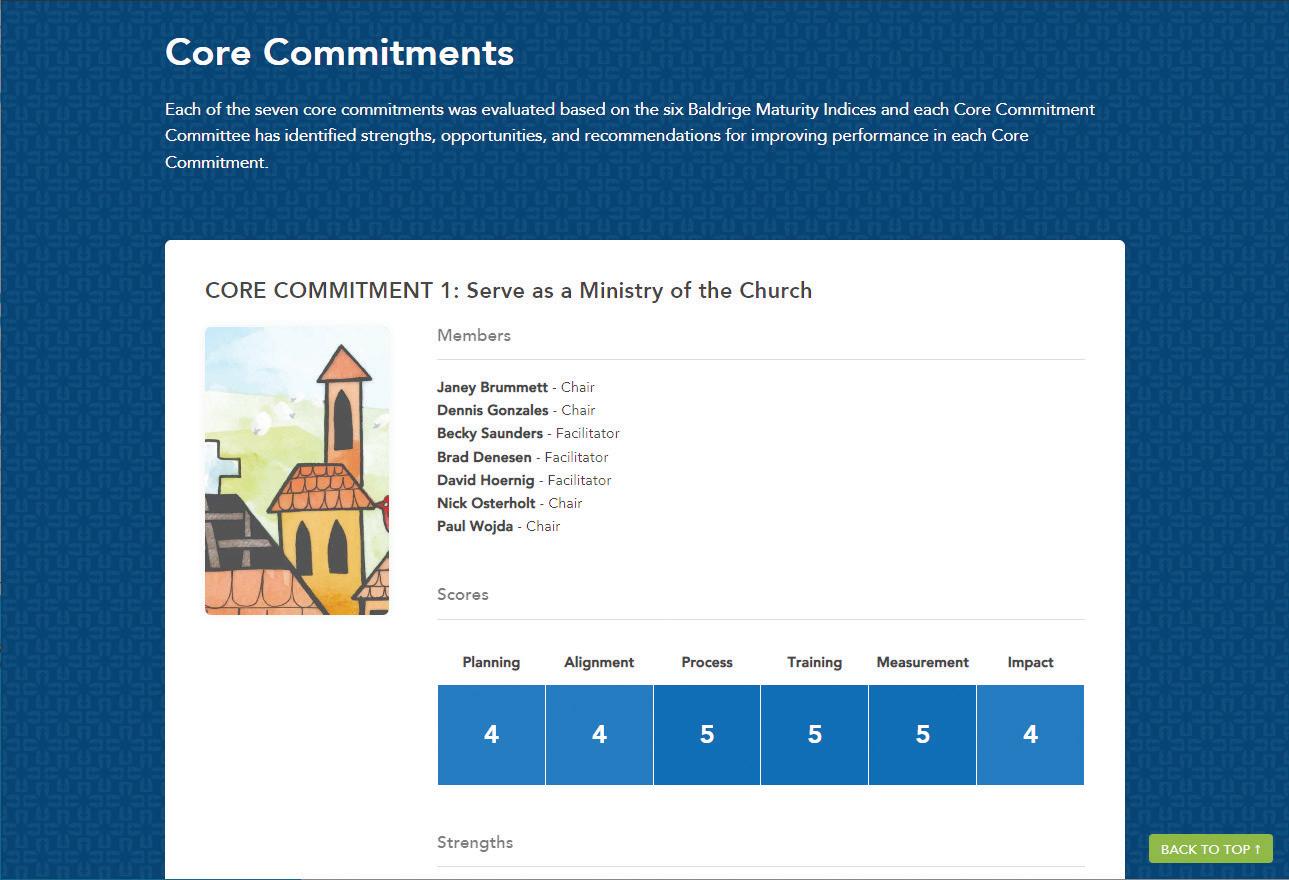
The updated tool also incorporates scoring methods from the Catholic Identity Matrix developed by Ascension and the University of St. Thomas. Gonzales says Mark Repenshek, Ascension vice president of ethics and church relations, made extensive contributions to the revisions and updates of the CHA Ministry Identity Assessment. “The best of CHA’s and Ascension’s and the university’s ministry identity assessments are incorporated in the new edition of the tool,” Gonzales says.
Repenshek adds: “Ascension's involvement helped to further the rigor of the assessment through a more explicit and in-depth integration of the Baldrige Performance Excellence Program framework and the development of a methodology to perform analyses of clinical procedures relative to the Ethical and Religious Directives for Catholic Health Care Services.”
The original Ministry Identity Assessment was published as a book with illustrations based on Gospel texts. The complete contents of that book have been available for download by CHA members since the book first went into print in 2019. The updated, online iteration of the assessment replaces the original version. Like the original assessment, it is a members-only
resource.
Nick Osterholt, CHA editor of digital communications, says the association has been working with a vendor since last year to build “from scratch” the web-based tool that members have been asking for. A committee of CHA and ministry staff have been developing the ideas for the tool, incorporating input from association members. The result is a customizable and adaptable tool that provides ministry members with a site where they can convene staff contributing to the Ministry Identity Assessment work. The member can add their own collateral documents for their assessment teams.
On the portal, staff will be prompted to methodically assess their organization’s policies, practices, community partnerships, culture and other aspects of their work. Other content and resources relate to the seven core commitments of Catholic health providers: serving as a ministry of the church, promoting and defending human dignity, promoting the common good, attending to the whole person, caring for poor and vulnerable people, acting on behalf of justice and stewarding resources.
The assessment process involves a steering committee overseeing the effort at each participating system and subcommittees working on each core commitment assessment. The systems determine who is on their teams — participants can include sponsors, board members, staff, patients and community members.
As part of the assessment process, the subcommittee members enter scores into forms on the portal to indicate how effectively they think the organization is completing specific activities related to particular commitments. After individuals have entered their scores, the subcommittee discusses those scores and their meanings. They then enter into forms on the portal new scores arrived at through consensus. Committee chairs and the steering team then enter final scores for each area evaluated. The tool organizes and provides a report on these scores, as well as the strengths and opportunities for improvement for each core commitment. The tool also provides the platform for developing action plans based on the results.
The entire process takes about three to four months. CHA makes a seasoned ministry leader available as an external reviewer

to provide input on the effort. CHA encourages organizations to repeat the assessment process every three years and gauge how well they are doing against their prior assessments.
It is expected that the use of the tool will lead to consistent points of comparison and increased sharing of best practices around the ministry, since numerous Catholic health systems will be assessing their work against the same criteria, says Gonzales.
Ascension’s Texas market and three markets within Bon Secours Mercy Health — Lorain, Toledo and Youngstown in Ohio — have been piloting the platform since late summer. This year, both systems are planning to expand the tool’s use to more of their markets.
Fr. Cardone and Amy Marcum, Bon Secours Mercy Health’s chief mission operations officer, have been leading that system’s work during the pilot.
Fr. Cardone says this is the first time the 48-hospital system has had a single tool and approach that all of its markets will use to evaluate how they are living out Catholic identity. When Bon Secours Health System and Mercy Health merged in 2018 to form the larger system, leadership began discussing the need to have a unified approach to assessing identity. The new platform meets that goal, Fr. Cardone says.
He notes that the Ministry Identity Assessment aligns with Bon Secours Mercy Health’s emphasis on Catholic moral and

drive the golf carts wearing the Fatal Vision Alcohol Goggles is meant to show them how alcohol impairs acuity and presents a danger to drivers, passengers and others on the road.
Henson says when students are instructed to text a friend while driving the golf cart, they learn that cell phones draw their eyes and attention from the road.
Butte-area first responders staff stations near the driving course. Montana Highway Patrol officers take participants through the steps of sobriety testing. Members of the Butte Fire Department explain what to do when an emergency vehicle is approaching. An ambulance crew instructs the students on hands-on CPR. Representatives from the Montana Trucking Association invite students to sit in the cab of a big rig and describe to them what it’s like to be on the road in these large vehicles. The students get an appreciation for the limited sightlines from the cab and the stopping speeds and distances required by semitrucks and trailers.
This year, Pat Goldhahn spoke to the participants about the 2016 death of his 15-year-old daughter Lauryn. She died in a car accident in Fairfield, Montana. She was not wearing a seatbelt. He described the pain and shock of her death. He also talked about the importance of organ donation.
The Ministry Identity Assessment online platform that CHA is launching in February has a section that explains the seven core commitments of Catholic health care. The platform includes resources to guide Catholic health care providers in assessing their fidelity to the Catholic health mission.
social teaching, and the biblical tradition of Catholic health care. Fr. Cardone says that this alignment helped secure the executive buy-in that was critical to the individual markets making the commitment to conduct the ministry assessment using the online platform.
Marcum says the assessments completed during the pilot phase were extremely informative for Bon Secours Mercy Health. “We have been doing great things, but we have not been benchmarking all of those things. It became apparent as we used the platform where benchmarking was really needed.” She says the measurement taking place through the assessments has led to action plans that will have a profound impact on the work Bon Secours Mercy Health does.
In addition to taking steps to improve how it is living out its identity and mission as a ministry of the church, Bon Secours Mercy Health will be celebrating all the good work that has been confirmed and documented through the evaluations, Marcum says.

More information on the Ministry Identity Assessment platform is available at chausa.org/MinistryIdentity. At the time of the platform’s launch, the fee for using the tool will be posted on the web page.
Brian Smith, CHA’s vice president of sponsorship and mission services, led much of the work to create and implement the first version of the Ministry Identity Assessment and he led the process to create the online platform. Smith died Nov. 8. Gonzales says the resource is an important part of Smith’s legacy of service to the Catholic health ministry.
jminda@chausa.org
From page Fr. Cardone Repenshek Osterholt Marcum A driver navigates the Distracted Driver obstacle course, part of Distracted Driver training that is mandatory for students enrolled in driver’s education in the Butte, Montana, school district. St. James Healthcare offers the Distracted Driver training as a community benefit.Pope Emeritus Benedict XVI, who died Dec. 31 at the age of 95, is being remembered within the Roman Catholic Church and its health care ministry and among world leaders as a humble intellectual devoted to tradition.
The former German Cardinal Joseph Ratzinger was pontiff from April 2005 until resigning in February 2013. Announcing his decision to step down as pope, and citing his advanced age, he said that his strength “of mind and body has deteriorated in me to the extent that I have had to recognize my incapacity to adequately fulfill the ministry entrusted to me.”
After becoming the first pope in 600 years to resign, he resided at a monastery on the Vatican grounds. The emeritus pope’s final words, according to an aide, were: “Lord, I love you.”
Pope Francis paid tribute to Pope Benedict at a New Year’s Eve prayer service, referring to him as “such a noble, such a gentle person.”
“Only God knows the value and strength of his intercession and his sacrifices offered for the good of the church,” Pope Francis said.
Pope Benedict was a close collaborator and the theological expert behind many of the major teachings of his predecessor, Pope John Paul II, Catholic News Service reported. Before he became pontiff, he led the work of the Vatican’s Congregation for the Doctrine of the Faith for 24 years. In that role, he was in charge of safeguarding Catholic teaching on faith and morals, correcting the work of some Catholic theologians and ensuring the theological solidity of the documents issued by other Vatican offices.
When he became pope at age 78, he was the oldest man to ascend to the highest rank of the church since 1730. During his papacy, Pope Benedict worked to rekindle faith in God. Speaking during World Youth Day in his first year as pontiff, he said: “In vast areas of the world today, there is a strange forgetfulness of God.”
His final testament, released after his death by the Vatican, urged the faithful to stand firm. “I have seen, and see, how, out of the tangle of hypotheses, the reasonableness of faith has emerged and is emerging anew,” he said. “Jesus Christ is truly the Way,
the Truth, and the Life — and the church, in all her shortcomings, is truly His Body.”
Sr. Mary Haddad, RSM, president and chief executive officer of CHA, said of Pope Benedict: “After a long and rich life of service to the church marked by a sharp, theological intellect, I believe his lasting gift to us will be as one who humbly embraced his humanity.”
In a 2009 article for CHA’s journal Health Progress, Clarke E. Cochran, then vice president for mission integration at Covenant Health System in Lubbock, Texas, discussed how Pope Benedict’s third encyclical, “Caritas in Veritate,” which translates to “Charity in Truth,” applied to Catholic health care without specifically addressing it.
The encyclical, Cochran said, “expresses teachings that support the organization and mission of Catholic health care in the United States. Yet, it contains both overt and subtle challenges to the practices of Catholic health care in our time.” Those challenges included providing mind, body and spiritual care for patients as well as fair working conditions and wages for staff.
Sr. Patricia Talone, RSM, who retired in 2016 as vice president of mission services at CHA, said that while Pope Benedict’s experience leaned more toward theological study than pastoral care, his writings and pronouncements, such as those he issued

on the World Day of the Sick, showed a strong allegiance to the church’s mission to care for the sick.
His missives and teachings, she said, brought a focus to the importance of providing compassionate and spiritual care and recognizing the vulnerability of people who are sick. “Benedict, while he was an academic, expressed gratitude and thanks to the people who were doing that work,” Sr. Talone said.
The Religious Formation Conference, a national organization serving Catholic women’s and men’s religious institutes, called Pope Benedict a committed scholar and prolific theologian who contributed significantly to the Catholic intellectual tradition.
In a statement issued by the White House, President Joe Biden said the retired pontiff “will be remembered as a renowned theologian, with a lifetime of devotion to the church, guided by his principles and faith.” He added: “May his focus on the ministry of charity continue to be an inspiration to us all.”
In his tribute to the late pontiff, U.N. Secretary-General António Guterres said Pope Benedict was “principled in his faith, tireless in his pursuit of peace, and determined in his defense of human rights.”
leisenhauer@chausa.org
Sr. Juliana Casey, IHM, died Dec. 29 under hospice care at the Monroe, Michigan, motherhouse of the Sisters, Servants of the Immaculate Heart of Mary. She was 82.

An acclaimed theologian, Sr. Casey was a thought leader in Catholic health care for nearly three decades. She began her health care career in the late 1980s at CHA where her knowledge of theology, and her teaching and writing skills dovetailed.
As CHA’s vice president of mission services, Sr. Casey pioneered a program to prepare people to be mission leaders in health care facilities. In 1991, she wrote CHA’s Food for the Journey: Theological Foundations of Catholic Healthcare. Considered an essential formation resource to this day, the book explains theological concepts including how Catholic health care is a visible form of Christ’s healing mercy and how Catholic health care functions as an essential ministry of the Catholic Church. The book also delves into the social justice teachings of Jesus and how they are reflected in the health ministry’s special attention to the needs of the poor and vulnerable.
In 1994, Sr. Casey moved from CHA to a post as vice president for mission services at the Sisters of Mercy Health System in St. Louis, now Mercy. In 1999, she joined
Catholic Health East, where she was executive vice president of mission integration and led the formation of the system’s sponsors, trustees and executives. At CHE, she influenced many health care and hospital administrators with her theological acumen, says an obituary from her congregation. (Trinity Health and Catholic Health East merged in 2013.)
After Sr. Casey’s 2010 retirement, she was a consultant and served as a member of the sponsor board of Providence St. Joseph Health.
Dr. Rod Hochman, president and chief executive of Providence, said, “Juliana was a tireless advocate for serving the poor and vulnerable. She was truly a force for good. I was blessed to witness her commitment and compassion up close many times during her service as a Providence sponsor. Her guidance was incredibly helpful to Providence as we steered our mission toward the future. Her influence on leaders in health care cannot be overstated. Juliana will be deeply missed, but there is comfort in knowing that she leaves behind a deep legacy that will continue to guide and inspire us well into the future.”
In 2015, CHA published Sr. Casey’s Voices from the Journey, a book that celebrates the people of Catholic health care. In it, Sr. Casey shared the perspectives of a
housekeeper, a sponsor, a physician, a family member, a patient and others in Catholic health care facilities.

Sr. Mary Haddad, RSM, CHA president and chief executive officer, said of Sr. Casey: “Over the years, she inspired so many in Catholic health care to embrace their call to serve the healing ministry of Jesus. Her ability to provide a solid theological foundation with creativity and practicality set the standard for formation.”
Born in Detroit on Oct. 19, 1940, Juliana Casey earned a bachelor’s degree from Detroit’s Marygrove College and a master’s degree from the University of Michigan. She entered the Sisters, Servants of the Immaculate Heart of Mary in 1964.
She taught at every level of education from elementary school through graduate school.

She earned an ecclesial doctorate from the Universite Catholique de Louvain in Belgium in 1977. From 1979 to 1985 she was provincial of the Northeast Province of the IHM congregation.
She was a prolific author, lecturer and scripture scholar, concentrating on biblical theology, spirituality and women’s studies. She represented women religious on a committee of the United States Conference of Catholic Bishops that focused on peace, an experience that led her to write and lecture on the subject in subsequent years.
From page 1
administrator of the Rhinebeck, New York, nursing home that is part of the New York City-based ArchCare. ArchCare is the health care ministry of the Archdiocese of New York.
She says the Montessori learning and development principles employed in the memory care unit give greater independence and control to 37 residents, all of whom have mild to moderate dementia.
Dr. Maria Montessori, one of Italy’s first female doctors, in the early 1900s pioneered the student-led, self-paced but guided educational approach that bears her name. There are about 5,000 Montessori schools educating over 1 million children from infancy through adolescence in the U.S., and thousands more Montessori schools worldwide, according to the American Montessori Society.
Ferncliff and Jennings, another Catholic continuum of care organization, are finding that applying Montessori principles in memory care facilities has boosted resident engagement, and produces positive clinical outcomes and a strong sense of community among residents.

Ferncliff and Jennings both work with the Center for Applied Research in Dementia to apply core Montessori principles in the care of residents with dementia. The private, for-profit company based in Solon, Ohio, says that since its launch in 2011, it has helped eldercare organizations in 25 states and in Asia, Australia and Europe incorporate Montessori principles in patient care.
Cameron Camp cofounded the company and directs research and development there. In graduate school in the late 1970s, earning a doctorate in psychology, he studied cognition and aging. In the 1980s, he was on the faculty of the psychology department of the University of New Orleans, working in a doctoral program in applied developmental psychology. In connection with that position, he worked at an adult day center in Kenner, Louisiana, that exclusively served clients with dementia. His work there included research activity and training students on working with people with dementia.

Around the same time, Camp and his wife sent their two youngest children to a Montessori school. The couple’s son attended from age 3 to 10, and their daughter from age 3 to 8.
At one point Camp taught child development at the university level. Camp would later write that his wife became a Montessori preschool teacher, and he taught child development at a Montessori training center. He began to see how Montessori practices and principles might align with neuroscientific concepts related to beneficial care for people with dementia. Since the 1990s he has been developing and testing practical applications of Montessori principles in the care of people with dementia. And, for more than a decade he and other
members of the center’s staff have trained staff of memory care facilities to use those applications.
The center’s standard programming includes an eight-hour, in-person didactic training session for facilities’ staff then monthly in-person brush-up sessions and ongoing remote support for them. Organizations pay roughly $20,000 for 18 months of this type of programming.
Allison Q. Salopeck is president and chief executive of Jennings, which has four campuses in Northeast Ohio. She met Camp during an internship when she was a graduate student — he was conducting a research project on reducing the use of restraints in nursing homes, and she was completing her thesis on the same concept — and the two shared information.
In about 2004 when Salopeck was chief operating officer of Jennings, she gave the OK for a Jennings campus in Garfield Heights to take part in one of Camp’s research projects, which involved residents

using a Montessori activity cart. The cart contained materials for various activities the residents could choose to do to improve their physical or mental dexterity. For instance, there was a tub filled with beans and coins — residents could separate the beans from the coins, classify the coins by type and/or count the change.
Around 2018, Jennings opened its Jennings at Notre Dame Village campus in Chardon, Ohio, which includes assisted living with memory support in a small house environment. Salopeck accepted Camp’s invitation for Jennings and the Center for Applied Research in Dementia to partner to use Montessori concepts in the small houses.
The relationship has evolved — Jennings provides office space for center researchers at its Garfield Heights campus, Jennings’ largest campus. In exchange those researchers provide dementia training, consultation and support for staff of Jennings campuses, particularly staffers working in the small houses for residents with dementia.
Vivian Springer, executive director of Jennings at Notre Dame Village, says the researchers’ ongoing training and consultation for staff emphasizes that residents can and should do as much for themselves as possible. “What you do for me, you take from me” is a Montessori credo.
Springer says, “Whether planning life enrichment activities or the menu, residents are very much driving these decisions. Residents are very active in participating in their household.” For example, she said, some residents do their own laundry, help one another, garden and perform household duties around meals.
Staff demonstrate in small steps how to complete a given task. Springer says the approach is “giving residents purpose to their day and the sense of accomplishment for themselves, leading to improved or continued self-esteem, pride and dignity. And joy — the sense of doing something they want to do and can do well.
“We really shouldn’t underestimate the importance of this feeling.”
At Ferncliff, Feller says the residents’ dining committee is responsible for setting and clearing tables and filling water cups. Hydration committee members choose and prepare fresh fruit. Welcoming committee members meet and greet new residents. Gardening committee members plant seeds and tend to the flowers and vegetables.
Residents enthusiastically participate in programs they shape, Feller says. This includes music therapy, art therapy, daily exercise sessions, special events and charitable giving.

Last year residents baked dog biscuits for the Ulster County Society for the Prevention of Cruelty to Animals. And two residents won awards for artwork they submitted to a Leading Age New York contest.
There is a waiting list for entry to Ferncliff’s memory unit. And, the Montessori approach has been so successful there that ArchCare is planning to implement it at at least one of its five other nursing homes.
Research that Camp and co-investigators published in 2016 found that Montessori-based dementia training of staff at 16 facilities resulted in use of fewer drugs including antipsychotics, antianxiety medications and antidepressants with residents. After staff training, researchers found there were fewer reactive behaviors among residents and an improvement in employee retention.
Springer says the use of the Montessori concepts in the small house environment at Jennings at Notre Dame Village has improved the overall physical status of residents. For instance, residents generally have not had the unhealthy weight loss or extensive physical decline that is often seen in memory care.
While Feller says the Ferncliff memory care unit’s use of the Montessori approach is so new that leaders have not yet been able to document outcomes, she likes what she sees. “It has surprised me how well residents have come together as a community. They care about each other.”
Use visual hints, cues or templates
Go from the simple to the more complex
Give the person something to hold
Break a task down into steps
When there is a mistake, think engagement rather than failure
To end, ask “Did you enjoy this?” and “Would you want to do this again?”
“
The approach is “giving residents purpose to their day and the sense of accomplishment for themselves, leading to improved or continued selfesteem, pride and dignity. And joy — the sense of doing something they want to do and can do well.”
— Vivian Springer