By JULIE MINDA
By JULIE MINDA
Holy Name Medical Center President and CEO
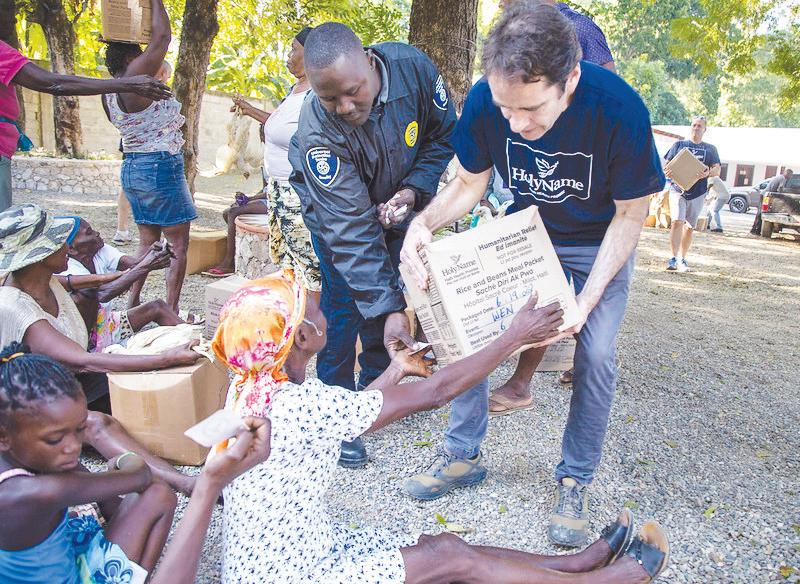
Michael Maron clearly recalls the pivotal meeting he had about a dozen years ago with the leadership of Hôpital Sacré Coeur in Milot, Haiti, to launch the New Jersey medical center’s partnership with that North Haiti hospital. Holy Name’s foundation had just taken over sponsorship of the struggling Haitian hospital, and Maron was telling the leaders there about Holy Name’s vision for how the transition would take place.
His speech was met with blank stares.
When he asked why everyone was so disengaged from this fresh start, a surgeon spoke up, noting that Maron was just the latest in a long procession of “blancs” — or foreigners — who had swooped in from the U.S. to tell the Haitians how to do things. They were sure Maron would disappear just as quickly as so many of the other













Staffing mandates spark deep concern for long-term care providers
By LISA EISENHAUER
Executives at Catholic health systems that provide long-term care say while they support the goals of new federal staffing mandates for nursing homes, they see a disconnect between the goals and the rules.
Scott LaRue, president and CEO of New York-based ArchCare, noted that the mandates finalized April 22 by the Biden administration largely ignore the ongoing funding and workforce challenges vexing long-term care providers.
“They’re not part of the solution to solve those problems,” LaRue said. “I find the whole thing very problematic and superficial in the approach.”
In its announcement, the White House said the rules fulfill the president’s commitments to give Americans access to safe long-term care and to promote quality in caregiving jobs.
“Medicare and Medicaid pay billions


How to address physician burnout?
Ascension’s on the case
By VALERIE SCHREMP HAHN
It would take a nearly 27-hour day for physicians to follow all nationally recommended guidelines to care for an average number of patients, according to a 2022 study. When he was starting work addressing clinician burnout around 2015, Dr. Aaron Shoemaker remembers another study that said it would take “only” 22 hours.
“That’s a long day,” he quipped. “There’s not a lot of sleep in there.”
Shoemaker is a co-lead with Dr. Jennifer Stanley of the Ascension National Clinician Engagement and Well-Being Council,
unpaid caregivers 12 When Healthcare Really Cares campaign 13 Project Compassion 2 PERIODICAL RATE PUBLICATION JUNE 2024 VOLUME 40, NUMBER 6
on 10
Supporting
Continued
Name’s support stabilizes hospital amid unrelenting turmoil in Haiti ASSEMBLY 2024 AWARDS ACHIEVEMENT CITATION
Holy
MEET TOMORROW’S LEADERS PAGES 3-5 LIFETIME ACHIEVEMENT AWARD RON HAMEL PAGES 6-7 SISTER CAROL KEEHAN AWARD DORI LESLIE PAGES 8-9
Cedar Wang, Holy Name vice president for nursing, left, provides training to Nirva Fils-Aime, director of community services at Hôpital Sacré Coeur in Haiti. The two are at the Russell Berrie Institute for Simulation Learning at Holy Name Medical Center in Teaneck, New Jersey. Some Milot, Haiti, providers travel to the U.S. for training.
Continued on 15
Jennifer Nochez, a certified nurse aide at Benedictine Living Community — New Brighton, Minnesota, talks with a resident. The system has found nurse aides challenging to recruit in some places. Continued on 14

Clinical ethics
The field of study gets the Commission on Accreditation of Allied Health Education Programs’ approval as a health science discipline.

Equity conference
Check out eight takeaways from the speakers and sessions at the American Hospital Association’s Accelerating Health Equity Conference.

Ethical AI use
Providence St. Joseph Health joins the Rome Call for AI Ethics, an international endorsement of ethical artificial intelligence use.
Project Compassion website offers guidance through end-of-life care
By NANCY FOWLER
What is an advance directive? When is it time for palliative care? What do Catholic teachings have to say about these topics? Some of the most difficult questions people ever face concern how to care for loved ones in the final stages of life.

Last November, a priest and a doctor in Syracuse, New York, launched Project Compassion, a website designed primarily for Catholics struggling with these issues. The idea was born during ongoing conversations over coffee. The more Fr. Charles Vavonese and Dr. Paul Fiacco talked about endof-life topics, the more they wanted to find a way to offer spiritual and medical guidance on a large scale.
Years before the website was rolled out, the pair wrote 13 articles on end-of-life topics for the Catholic Sun, the official newspaper of the Roman Catholic Diocese of Syracuse. They made presentations on the subjects they’d written about, including grieving, the role of hope at the end of life and legal issues related to end-of-life care.
The response was overwhelming. But as successful as their efforts were, they still weren’t reaching enough people. “People kept saying, ‘You’ve got to do more,’” says Fr. Vavonese, director of Project Compassion.
A different experience
Fr. Vavonese and Fiacco began planning an ambitious website. They wanted to provide resources for patients diagnosed with serious illness, their families and caregivers, as well as lay ministers, health care providers and the general public. They envisioned explanatory videos, a pastoral care training program and a polished, professional look. But all that would cost money.
At the time, both men worked for Syracuse’s St. Joseph’s Health, a member of Trinity Health. They collaborated with St. Joseph’s Health Foundation to apply for a grant from the Mother Cabrini Health Foundation, a nonprofit that supports health and well-being initiatives in New York state. The application was approved for $500,000.
“We were lucky,” Fr. Vavonese says. “With a half million, you can do a lot.”
They selected a web-hosting company and hired a retired local newscaster and a videographer who once worked for the diocese. The team shot and produced 19 videos on subjects that range from pain management to spiritual questions about the ubiquitous experience of death.
“It’s going to happen to you; it’s going to happen to me,” says Fiacco, Project Compassion’s medical director.
But as inevitable as death is, much about the way Americans die has changed over the past century, Fiacco says. People once died quickly from infectious diseases such as pneumonia, polio and tetanus. Even then, when little could be done medically, holis-

tic care was the norm in Catholic hospitals.
Thanks to antibiotics and immunizations, many people now survive once-fatal conditions. The causes of death today are more likely to be heart disease, cancer or diabetes — diseases people can live with for months or years. During this time, health care providers can give primary palliative care, which eases the symptoms of the disease but cannot cure it. This care is multidisciplinary and includes emotional and spiritual social care.
“Doctors are trained very well to attend to the physical needs,” Fiacco says. “But what about the emotional and spiritual journey?”
Doctors who want to delve deeply into end-of-life issues and palliative care options with patients and their families often don’t have the time.
“The website is an attempt to say to the patients, ‘OK, I can’t have all these conversations with you, but I want to provide this holistic kind of care,’” Fiacco says.
Primary palliative care
It’s imperative to begin talking about primary palliative care as soon as possible, Fiacco says. For example, a diagnosis of pancreatic cancer should immediately be paired with a conversation about palliative measures. The website videos provide a way for families to talk about it.
While many of the videos hold value for non-Catholics, Catholicism is at the heart of the project. For instance, since many Catholics worry about the sanctity of life versus the need for medications like morphine, the website addresses the ethics behind such decisions, according to Fr. Vavonese.
“Administering the pain medication at the end of life might shorten a life, but using the moral principle of double effect, we as Catholics are permitted to do that — after meeting certain criteria,” Fr. Vavonese says.
This kind of guidance can be lifechanging for caregivers and family members. Fr. Vavonese remembers one man who cried when he learned the decisions he’d made for his dying wife were consistent with Catholic teachings.
“He said, ‘Now that you’ve told me I did
the right thing, I’m not worried anymore,’” Fr. Vavonese says.
The future
Given the reality that there are fewer clergy, the website includes pastoral care training for lay ministers to meet the need to provide spiritual support to those receiving primary palliative care. Since the training is continually available online, people no longer have to wait to enroll in in-person training that might not start for several months.
“Now if somebody walks into the parish and says, ‘I’d like to become a Eucharistic minister,’ it’s very easy for the pastor to say, ‘Here’s some training for you,’” Fr. Vavonese says, referencing a video on Project Compassion that trains lay ministers who visit the sick and homebound.
Fr. Vavonese and Fiacco are working to let more people know about the pastoral care training. One initiative would promote the series to those involved in prison ministries. Another idea in the works would make Project Compassion a resource in the Community Division of Trinity Health, which includes visits with providers in the medical group and care managers outside the hospital.
Sheila Johnson, vice president of population health clinical operations at Trinity Health, was among those who reviewed the grant application for Project Compassion for Mother Cabrini Health Foundation.

“I was struck by how it would help more laypersons become involved in pastoral care, as well as help our patients who are suffering,” Johnson says.
Johnson is excited about what Trinity Health — with 101 hospitals in 27 states — could do to boost a site she considers invaluable.
“When I went on it, I was able to find everything; it’s organized, the content is very professionally developed and it’s easy to understand,” Johnson says. “Having all of this in one place is just a wonderful idea.”
Reading the Signs of Our Times: A CHA Book Club for Leaders
Catholic Health World (ISSN 87564068) is published monthly and copyrighted © by the Catholic Health Association of the United States.
POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@ chausa.org. Periodicals postage rate is paid at St. Louis and additional mailing offices. Annual subscription rates: CHA members free, others $29 and foreign $29.
Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA. Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
Vice President Communications and Marketing Brian P. Reardon
Editor Lisa Eisenhauer leisenhauer@chausa.org 314-253-3437
Associate Editor Julie Minda jminda@chausa.org 314-253-3412
Associate Editor Valerie Schremp Hahn vhahn@chausa.org 314-253-3410
Graphic Design Norma Klingsick
Advertising ads@chausa.org 314-253-3477
We Will Empower Bold Change to Elevate Human Flourishing. SM
© Catholic Health Association of the United States, June 2024
FIND MORE CHA RESOURCES ONLINE chausa.org/chw
in Catholic Health Care — Bimonthly Series June 18, Aug. 20, Oct. 22 | 1 – 2 p.m. ET Faith Community Nurses Networking Call July 9 | 1 – 2 p.m. ET United Against Human Trafficking Networking Call Oct. 2 | Noon — 1 p.m. ET Deans of Catholic Colleges of Nursing Networking Call Oct. 8 | 1 – 2 p.m. ET Community Benefit 101 Oct. 15 — 17 | 2 – 5 p.m. ET each day Upcoming Events from The Catholic Health Association chausa.org/calendar
Fr. Charles Vavonese offers guidance on end-of-life moral-medical issues in a video that is part of the collection of Project Compassion resources. Fr. Vavonese was a co-creator of the site — compassionandcope.org.
Fiacco
2 CATHOLIC HEALTH WORLD June 2024
Johnson
TOMORROW’S
Up-and-comers find innovative ways to advance health care ministry’s mission
By KATHLEEN NELSON
With respect for the past, passion for the present and vision for the future, Tomorrow’s Leaders show a commitment to Catholic health care that inspires confidence. This year, a dozen leaders age 40 or younger received recognition for their significant contributions to the ministry. Catholic Health World posed questions about their achievements and inspiration to these young leaders.
 Rachelle Barina, 36 Chief mission officer, Hospital Sisters
Rachelle Barina, 36 Chief mission officer, Hospital Sisters
Health System, Springfield, Illinois
Achievements
Guided creation of HSHS’s first strategic plan specific to mission.
Standardized the HSHS ethics program with oversight through one unified ethics council. Launched colleague and executive formation programs. Who inspired your career? My mom was a physical therapist in public schools. When our school calendars misaligned, I would go to work with her. I met kids my age who were living with disabilities. Watching my mom’s care and encountering these kids taught me what a precious and fragile gift each person is. What previous experiences helped shape your career? I spent several years working part time in a jail. I learned the complexities of health, social and economic factors. I learned the power of listening, as well as the limits of helping another person. Probably most importantly, I learned that folks who were incarcerated were generally relatable, good people.
Why is Catholic health care a good fit for you? I love Catholic theology, and I also want to serve in the church in a way that directly impacts people and communities. Catholic health care seeks to live the Catholic tradition amidst the messy, beautiful, and challenging realities of our lives and institutions — a perfect fit. Which of your achievements will be most impactful? One of the things I’m excited about is the ethics program that we’ve built during the last two years at HSHS. We are finding ways to use the strengths that each person brings, gain efficiencies and

“promote wide-reaching learning opportunities and consultation support.
Endorsement
“Rachelle always sees the dignity of the person before her. She genuinely enjoys listening to the story of others and helping the person articulate the beauty of that story in a way that inspires others.” — Damond W. Boatwright, president and CEO, Hospital Sisters Health System
Haley Busch, 30 Quality manager, opioid stewardship program coordinator, CHI Saint Joseph Health, Lexington, Kentucky, part of CommonSpirit Health

Achievements
Established a pharmacistdriven pain management and addiction medicine consult
Rachelle always sees the dignity of the person before her. She genuinely enjoys listening to the story of others and helping the person articulate the beauty of that story in a way that inspires others.”
— Damond W. Boatwright
service.
Headed the hospital’s sepsis committee, which led to a top-decile ranking among CommonSpirit hospitals in reducing incidents.
Developed an opioid stewardship program that led to a 17% reduction in daily use of opioids by patients and a 37% reduction in concurrent prescriptions of opioids and benzodiazepine.
What do you like best about your job? Our company does a great job of hiring good folks, giving them the resources to do good things, then not putting guardrails on them. Being part of a culture that puts patients first, and bringing the healing presence of God to our patients, means so much to me.
Why is Catholic health care a good fit for you? From conversations with leaders, patients and staff, it’s become clear that healing goes beyond the physical ailments and beyond evidencebased guidelines. It’s about healing mind, body, spirit and soul, and I think we do that best within a faith-based organization with faith-based resources.
Which of your achievements will be most impactful? The pharmacist-driven addiction medicine consult service. Historically, we did a great job of treating a patient with IV drug use for an infectious complication, but we didn’t address the real reason they were in our hospital. I was able to build a program that bridged those gaps, seeing patients bedside and having conversations about what they needed holistically: not just medication but psychosocial treatment for long-term recovery.
Patients and their families said we were the first system to treat them like a patient and not a drug user.
Now, every member of our clinical pharmacy team is empowered to complete those consults. Our team owns it.
Endorsement
“Haley’s integrity, commitment to excellence, self-awareness, and utilization of data and evidence-based practices is a modest representation of the characteristics that qualify her as a health care leader of the future.”
— April Jennings, director of quality, Lexington market, CHI Saint Joseph Health
Bridget Fitzpatrick, 40 Chief operating officer, Bon Secours Richmond Community Hospital, Richmond, Virginia
Achievements
Drove construction of a freestanding emergency center in an underserved area.
Led expansion and redesign of the main hospital in Richmond.
Helped develop safety procedures that celebrate “Good Catches,” resulting in a 52% increase in safety reporting in 2022.

Who is your role model? My dad, Daniel Fitzpatrick, is a physician in our Youngstown, Ohio, market. He encouraged me to find a career that adds value to people’s lives. After finishing undergrad work, I volunteered at St. Francis Medical Center in Midlothian, Virginia. It opened my eyes to what it is like to be with patients at the most vulnerable time in their lives and the fact that health care offers careers to more than
nurses and doctors.
What do you like best about your job? Our team is faced with unique challenges every day: a new process or regulation, a new engagement with community or a new technology or ways to improve patient care. We may not know the answer right away, but we’re going to come together as a multidisciplinary team, find evidence-based best practices, and work to ensure our patients and community get the best care. Why is Catholic health care a good fit for you? We have to see people from the holistic perspective of mind, body and spirit. Catholic health care allows us to do that while being respectful of their own spiritual perspective. It attracts people who want to be compassionate and empathetic, who do the things you can’t put into a job description.
What is your next big goal? I switched jobs with one of my colleagues in January. Before that, I was the COO at St. Francis Medical Center in Richmond. So, my next big goal is mastering this role and understanding the hospital. I want to continue and expand on the work of my predecessor to be a connector with local governments, other nonprofits, small businesses and faith-based leaders to enhance spaces, create workforce opportunities, and build trust with the community.
Endorsement
“Her ability to execute and innovate with positive energy and enthusiasm is unparalleled. She does so by leading with vulnerability and encouraging others to do the same.” — Chris Accashian, chief operating officer, Bon Secours Richmond market
Faith Halford, 24 Systems manager, materials management, St. Joseph’s Candler Health System, Savannah, Georgia
Achievements
Deployed digital tablets to central supply, allowing the department to place orders in real time, improve order accuracy and turnaround time, and ensure that floors remained well-stocked. Developed a “ship-to dictionary,” to ensure that vendors supplied the system’s 26 off-site locations faster and more accurately. Gathered more than 50,000 items that were delivered to Poland to aid the Ukrainian people.
What previous experiences helped shape your career? I’ve wanted to work in health care since I was 13 and visited a family member in the hospital. The death of my father from COVID reinforced my desire. He was here and received remarkable care from every nurse. I still speak to some of them and wanted to support them. That’s what I like about supply chain. You can reach out and touch everyone,
Haley Busch, right, dons a Harry Potter-esque robe for a skit with colleagues during leadership development meetings at CHI Saint Joseph Health in Lexington, Kentucky.
ASSEMBLY 2024 AWARDS Continued on 4 June 2024 CATHOLIC HEALTH WORLD 3
LEADERS

and get the staff what they need to provide excellent care.
What do you like best about your job? I love our team. I enjoy problem solving, and I know every day there will be a problem that we have to solve. There’s a lot of variation, so that’s exciting.
Why is Catholic health care a good fit for you? I grew up in a Catholic household and attended Catholic schools since kindergarten. I feel that in a Catholic health system, I can honor that upbringing and carry on the mission of the founders.
What is your next big goal?
Continuing to seek improvement in workflow. We want to expand using digital tablets in settings other than ORs and receiving, which will streamline and optimize our ability to get the staff what they need to help our patients.
Endorsement
“Faith is a forward thinker and is passionate about continuous quality improvement, always seeking a more efficient and effective way to produce desirable outcomes.” — John Albright, director, home health and Georgia Infirmary (past Tomorrow’s Leader honoree)

Tom Klein, 35
Chief operating officer, Ascension Medical Group — Ascension Michigan, Warren, Michigan
Achievements
Directed field operations for four emergency mass tuberculosis testing centers that served 15,000 patients.
Led successful plan to improve associate turnover rate.
Developed a business plan to add four additional 3D mammography machines, improving mammography access by 15% from pre-pandemic levels. Who is your role model or inspiration? My father had the biggest influence on my leadership.
I went into my undergrad studies thinking I would be a doctor, but I also helped run a small family construction business. When you’re leading people double or triple your age, you learn a lot of skills really quickly. At the University of Michigan, I learned there was a business and
entrepreneurial side of health care as well as a clinical side. Why is Catholic health care a good fit for you? I was born and raised Catholic, but it’s more than just the word Catholic. It’s about the mission and values you commit to, treating everyone the same regardless of race, creed or color.
Which of your achievements will be most impactful? In the last year, we’ve improved by 13% the number of patients who received Medicare annual wellness visits.
In doing more of these, we saw mammography and colonoscopy rates go up. We’ve seen the number of patients with controlled diabetes management go up, too. We’re making people healthier and keeping people out of the hospital.
“ I was born and raised Catholic, but it’s more than just the word Catholic. It’s about the mission and values you commit to, treating everyone the same regardless of race, creed or color.”
— Tom Klein
What is your next big goal? The large business goal is increasing access for our patients. In addition, Ascension Michigan is awaiting formal legal and ecclesial approvals for its plan to form a joint venture with Henry Ford Health. I’m super excited about the future of health care in Michigan.
Endorsement
“He has the rare combination of courage, curiosity, and humility to drive the organization past familiar boundaries despite his colleagues’ strong bias for the status quo.” — Dr. Douglas J. Apple, chief clinical officer, Ascension Michigan, interim president and CEO, Ascension Genesys Hospital, in Grand Blanc, Michigan
Carrie Meyer McGrath, 40 System director, formation design and delivery, CommonSpirit Health, Chicago
Achievements
Led creation of Called to Lead, CommonSpirit’s formation experience for new leaders.
Contributed to CHA’s Ministry


Identity Assessment tool, cowriting the initial draft, training facilitators and coaching mission leaders.
Champions virtual formation as a tool to innovate, create community and steward resources.
What previous experiences helped shape your career?
I studied theology, learning what makes people tick and what they are passionate about, what affirms a meaningful life. As I finished my studies and learned about formation in Catholic health care, I thought I could take that conviction and make it real and make those connections. Why is Catholic health care a good fit for you? I care about the confluence of practical and spiritual and the traditions of our founders and the communities we serve. One of the reasons I wanted to come to CommonSpirit is the name and the com-
mitment that name requires. It’s inspiring to explore how we commit to the common good guided by the Holy Spirit.
Which of your achievements has been most impactful? What was really impactful about building Called to Lead is we pulled together our mission leaders for feedback. We heard from the Pacific Northwest, Southern California, Tennessee, Ohio and the Dakotas. We tried to incorporate what can resonate across the mission but reflect the local heritage. What is your next big goal? We are working on an executive formation experience called Leading Together. Over 14 months, leaders will grapple with the essential questions in Catholic health care while upholding the traditions of our founders.
Endorsement
“She possesses an innate ability to translate and apply theological and spiritual content. She has high personal standards and respectfully challenges those with whom she works to give their best to the ministry.” — Kyle Klosterman, CommonSpirit system vice president, mission and formation (past Tomorrow’s Leaders honoree)
Sam Prokopec, 35 Executive director, St. Joseph’s Elder Services, West Point, Nebraska, a member of Franciscan Sisters of Christian Charity Sponsored Ministries

Achievements Increased census in assisted living from 25 in 2021 to 38 this year, and in skilled nursing from 38 to its capacity of 52.
Achieved five-star rating in the last two years from the Centers for Medicare and Medicaid Services.
Incorporated mission as part of the orientation process. Takes on all responsibilities, including driving residents to appointments and clearing tables.

Who are your inspirations?
My mom was a career RN, so I knew from an early age that I would somehow be in health care. While I was in college, majoring in exercise therapy, my grandma lived in a nursing home. She hated every minute of it. It wasn’t where she wanted to be. I took her grievances and hoped to make a better life for others. What do you like best about your job? I like that I can impact the residents’ day in multiple ways, especially helping out with activities. This week, for example, we grilled steak and chicken for the residents. I also enjoy having the sisters around us, visiting our residents. We’re blessed to have them in our community. Which of your achievements has been most impactful? When I arrived, there was a very good team in place, but they needed direction. To lay the groundwork for stability and provide continuity are what I’m most proud of. What is your next big goal? We are kicking off a complete remodel of our assisted living facility. We’ve been planning it for more than 12 months, and it will take 15-22 months to complete. Even though the process will be a
Sam Prokopec is known for bringing a smile to the faces of residents at St. Joseph's Retirement Community in West Point, Nebraska, whether serving as an alternative target at table bowling or dressing as a hotdog.
Hundreds of clothing items were donated through the Colleague Clothing Swap sponsored by Trinity Health WorkParent Colleague Resource Group for both colleagues and patients. Shekinah Singletery, second from right, co-founded the group.
4 CATHOLIC HEALTH WORLD June 2024 TOMORROW’S LEADERS
challenge, I’m excited to get that started.
Endorsement
“His zealousness for life and involvement in all aspects of the organization are felt. There’s not a week that goes by that I don’t see Sam having a drink and talking about the military with our veterans, or playing games, or just making people smile.” — Tyler Toline, president and CEO, Franciscan Healthcare
Shekinah Singletery, 32
Director of community health and well-being, Trinity Health Ann Arbor in Ypsilanti, Michigan, and Trinity Health Livingston in Howell, Michigan
Achievements
Guided a partnership with Michigan Community Health Worker Alliance to develop a local community health worker coalition.
Set up user-friendly methods for local ministries to report the community health work that could be aggregated at the system level.

Co-founded and co-leads the Trinity Health WorkParent Colleague Resource Group (CRG) to support employees who are working parents and caregivers. Who are your inspirations? My parents are both pastors. I went along when they visited shut-ins and provided communion at hospitals. I saw the differences among government-funded hospitals, for-profits and not-forprofits. That opened my eyes to the disparities in health care.
At the University of Michigan, Professor Richard Lichtenstein introduced me to the concepts of social determinants of health and health equity. He helped me give a name to what I witnessed and experienced in my youth. His passion and advocacy made me want to champion the work. Which achievement in your current job are you most proud of and why? I’m leading the community health workers statewide initiative, which integrated eight distinct programs in seven counties into one program. It’s helping to generate revenue for more community health workers.
Having the WorkParent CRG across all of Trinity Health is another achievement I am proud of, since I have a 5-year-old and a 1-year-old. We have more than 200 members — new and returning parents, as well as caregivers.
We provide a supportive environment to share experiences, obtain resources and foster business innovation where they can thrive and impact internal policies and procedures in a variety of departments.
What is your next big goal?
My next big goal is for Trinity Health Michigan to be a model of excellence in community health, specifically in health equity and integration of clinical and social care.
Endorsement
“What truly sets Shekinah apart is her exceptional ability to inspire and galvanize those around her. Her enthusiasm is infectious, and her motivation is relentless.” —
Dr. Chiquita Berg, vice president, community health and wellbeing, Trinity Health Michigan
Megan Timm, 37
Regional director of community health, SSM Health of Wisconsin
Achievements
Implemented ConnectRx in the Madison area to coordinate housing, nutrition and support services to pregnant women of color.
Expanded diversity in the supplier network, providing $4 million for often overlooked community vendors.
Teaches in-school smoking and vaping education programs.

Who is your role model or inspiration? I grew up with a family of teachers, and I thought I’d follow that path. When I speak to groups, I’m very teacher-like, and I love working with large groups. I also have an aunt who is a dietitian in rural Wisconsin. I combined those to educate the community in health and food. What do you like best about your job? I work with the best people. It’s a small community health team, but it is mighty. Building connections with our partners to sustain change is the best magic in the world.
Why is Catholic health care a good fit for you? It’s a really beautiful marriage of finding a career at a place that doesn’t just talk it, but really wants to be part of the change and support partners that make the change. Which of your achievements will be most impactful? ConnectRx is so innovative in that it’s not just consulting those who are impacted. It’s partnering and bringing them into decisionmaking. So often in public health,
we educate the public or consult, or we extract information and move on. But with ConnectRx, we learn from the people we serve and follow their lead in the effort to make change.
The work around vaping prevention is a treat for me, because direct care isn’t normally part of my work. So, I love to connect with students in areas that don’t have a lot of extra services, to learn from them and work on solutions with them.
Endorsement
“During difficult conversations or in the midst of working on complex issues, Megan’s openhearted listening brings people together to find common ground and best possible solutions.” — Sue Anderson, regional president, SSM Health of Wisconsin
Caleb Townes, 26
Director of consumer & patient experience, Ascension St. Vincent’s, Birmingham, Alabama
Achievements
Redesigned in-person orientation after years of virtual presentations.
Developed consumer experience commitment groups in each of Ascension Alabama’s five hospitals and 24 clinics.
Improved from fourth to first in market patient experience scores. Who are your inspirations? My mother was a dental hygienist. She didn’t inspire me because I like brushing my teeth. But I was with her when she worked, and I saw that her personal relationships were often more important than the clinical care she gave. What previous experience helped shape your career? I was a youth minister. I taught kindergarten through fifth grade. The most success I’ve had in this role is when I’m replicating what I did with them. What a kindergartner needs is the same as what an adult needs in terms of support, encouragement and belief in themselves. It’s the same whether you’re 6 or 60.
What do you like best about your job? Day 1 of orientation: I’m dealing with new colleagues when their belief in themselves is at its maximum. I can affirm their belief in themselves. We put the focus on who you are, as opposed to what you do. If we can get people to remember why they chose this job, we’re going to have a lot of fun.

His energy is contagious, and his youth allows us to reach new staff and leaders in a way that many of us simply cannot.”
— James Epperson on Caleb Townes
Endorsement
“ “What truly sets Shekinah apart is her exceptional ability to inspire and galvanize those around her. Her enthusiasm is infectious, and her motivation is relentless.”
— Dr. Chiquita Berg
“His energy is contagious, and his youth allows us to reach new staff and leaders in a way that many of us simply cannot.” — James Epperson, chief nursing officer, Ascension St. Vincent’s East in Birmingham, Alabama
Dan Woods, 37 Senior director, emergency services and hospital throughput, St. Dominic Hospital, Jackson, Mississippi, a member of Franciscan Missionaries of Our Lady Health System
Achievements Helped guide renovation and expansion of emergency services. Assisted in leading establishment of PACE, the system’s throughput/transfer center to more timely and efficiently place patients.

Helped reduce emergency medical service “wall times,” reducing downtime by 73% for EMS staff before returning to answer calls.
largest vulnerable populations in the country. My next big goal is to tackle that head-on by bringing technological and operational innovation that Mississippi health care has had a limited exposure to.
Endorsement
“Dan understands the importance of defending human dignity. He promotes this by voicing its importance to his staff during onboarding processes and quarterly staff meetings.” — Dr. Bradley Burns, medical director, St. Dominic Hospital emergency department
Zach Zirkelbach, 38 Chief financial officer, Ascension St. Vincent, Evansville, Indiana

Achievements
Converted all financial documents in the transition to a national platform and rebranding of Ascension St. Vincent. Guided changes leading to a 2% increase in profit margin at Ascension St. Vincent Evansville. Participated in the Homeless Experience, a two-day immersion in homelessness.
Who is your role model? I try to emulate my parents. My dad worked for the Daughters of Charity before they became part of Ascension, which is why I feel like working for Ascension is part of a family. My mom was a pediatric nurse.
What do you like best about your job? Being from Evansville, I have a lot of pride in our mission and hospital. I very much enjoy the team I work with, the staff and the physicians. We challenge each other, and we pick each other up.
What is your next big goal? Our ABIDE (Appreciation, Belongingness, Inclusivity, Diversity and Equity) council has been invigorated since the start of 2024. My goal isn’t just to pump out content and share it, but to invite our 5,000 associates to be an active part of the council. If we can help people understand what we’re trying to do with the culture, they will realize that they have a role to play in it.
Who is your role model? My dad is a nuclear engineer. My mom is very active in the church. A lot of my foundation was built in math and science, and a firm foundation in your faith is essential to answer most of life’s problems. What do you like best about your job? I’m a nerd at heart. I love taking difficult problems and complex projects and applying systems thinking. I love taking someone from food service and getting them to think about how what they do affects nursing, finance or IT. Being the engineer on that train is fun for me, challenging the mental model and evolving to a unified approach. Why did you feel that Catholic health care was a good fit for you? I never imagined five years ago that I would show up to a place that starts every meeting with a prayer and always questions whether what we’re doing really matches the mission of caring for people. Those are nice reminders of why I belong here. What is your next big goal? We’re one of the handful of faith-based hospitals and the only Catholic hospital in the state. We shoulder a burden that’s challenging but wonderful, serving one of the
How did the homeless immersion experience impact your job? I don’t have direct contact with the people we serve, but I can’t think of a better way of living our mission than to get a better understanding of what the poor and vulnerable deal with on a day-to-day basis. When you walk a mile in their shoes, you pick up on a lot of mental health issues and what it feels like to start off on the wrong foot. It’s not that they’ve done this to themselves; it’s more that they don’t know how to pick themselves up. I wanted to humble myself and try to understand.
What is your next big goal? I’m really excited to get back to work on our five- and 10-year strategic plans. We just had our 150th anniversary. It feels like we’re setting up for the next 150.
Endorsement
“He genuinely wants to learn from other leaders to better understand how their departments work. This empowers others to want to work side-by-side with him in an effort for improvement and stronger financial performance.” — Shelby Collins, vice president, southern region, Ascension Medical Group
June 2024 CATHOLIC HEALTH WORLD 5 TOMORROW’S LEADERS
LIFETIME ACHIEVEMENT AWARD
Hamel calls on leaders to carry out ministry of healing, make ethical decisions
 By VALERIE SCHREMP HAHN
By VALERIE SCHREMP HAHN
Theologian and ethicist Ron Hamel frequently turns to Jesus’ parable of the good Samaritan, in which a man is attacked by robbers who strip and beat him.
A priest and a Levite pass by and don’t help. A Samaritan, considered an outcast of Jewish society, does help. He stops, cleans the man’s wounds and takes him to an inn to recover.
The parable is an important lesson for those in Catholic health care, says Hamel. He challenges them to answer the questions: Who are the people on the margins of our society? And what do they need from us?
“The key thing we need to focus on is carrying out a ministry of healing,” said Hamel. “And the question always is: How do we best do that in the current circumstances, for the people we serve?”
For 40 years of asking and answering such questions and offering guidance to those within the ministry who must decide how to respond, Hamel is this year’s recipient of CHA’s Lifetime Achievement Award.
Hamel, 78, is considered a mainstay in the field of Catholic health care ethics. He’s written or edited eight books, penned dozens of articles and book chapters, served as a college instructor and professor, and mentored or guided many younger ethicists.
Laura Kaiser, president and CEO of SSM Health, said in a statement that Hamel’s “passion and dedication to Catholic health care are inspiring.
“Ron has a remarkable way of providing clarity around complex issues through the lens of Catholic moral teaching and ethics,” she added.
Kaiser said Hamel provided “wise counsel and valuable insight” as a board member and president from 2015-2022 of SSM Health Ministries, the sponsor of the St. Louis-based system. He was also a member of the SSM Health Board of Directors from 2015-2021.
Patrick McCruden, chief mission integration officer for SSM Health, said Hamel is not only knowledgeable, easygoing and approachable, but also effective.
“There’s a lot of people who think that just by being right, that’s what makes you good at this,” he said. “But it really doesn’t. You have to be effective. It’s not enough to say ‘Oh, this is what the church teaches.’ You have to be able to articulate that and get them to a place of acceptance.”
In retirement, Hamel continues to serve. He is on the CHRISTUS Health Board Mission Integration and Human Resources Committee and the Quality Committee. He is resource ethicist for the American Association of Nurse Anesthesiology and consults with Catholic health care systems.
Continuing challenges
Changes in technology and culture continue to present new challenges for ethicists. That’s something that attracted Hamel to the field more than 40 years ago.
“That’s a large part of the fun of it,” he said. “Knowing that the way we think about these issues can have some very practical applications and implications for people.”
Hamel grew up in a blue-collar family in Waterbury, Connecticut, and has a younger brother and sister. He entered the seminary in high school, earned his bachelor’s degree in philosophy, and left the seminary when he was around 30. To support himself, he taught ethics and theology at colleges in New York while going to graduate school. He received his master’s degree in contemporary/systematic theology and his Ph.D. in Christian theological ethics from Fordham University in New York.
Around this time, in the late 1960s and early 1970s, large debates emerged around the topics of health, bioethics and birth control.
“I just thought those issues were so intriguing,” Hamel said. “And I’ve always been curious about why people do what they do.”
He saw teaching as an expression of the ministry he did not pursue in the priesthood, but after about 15 years, he began to burn out. He got a new opportunity when he was asked to join the Park Ridge Center for the Study of Health, Faith and Ethics, a now-defunct think tank in Chicago, as a senior associate. That led to a job as the

head of clinical ethics at Lutheran General Hospital in Park Ridge, Illinois, which was associated with the center.
Hamel called those years some of the best of his career. “I was dealing with patients and families and doctors and nurses, and every single case was different and challenging,” he said. “I knew that I had made a difference in a family’s life or a patient’s life or helped the patient to die a better death by the decisions that we made or helped the physician deal with a family.”
During Hamel’s time at the hospital, he made connections at CHA and joined the organization in 1998 as its senior ethicist. By the time of his retirement in 2014, he had written about 60 articles and columns for CHA’s journal, Health Progress
Shaping thought, future ethicists
“There was a time when health care ethics was simply ‘ethics at the bedside.’ Ron played a key role in expanding and transforming that definition,” Fr. Thomas A. Nairn, OFM, who worked alongside Hamel at CHA as senior director of ethics, said in Hamel’s award nomination. “He was very strong in encouraging us to consider how we respond to the poor in our midst, for example. Health care ethics and ethics itself used to be seen as restrictive — things you can’t do. Ron allowed leaders in health systems to see ethics is a help, not a hindrance. It lets people see we are what we claim to be.”
When Hamel retired, Fr. Nairn wrote an article in Health Progress summarizing Hamel’s contributions to Catholic health care ethics during his tenure at CHA. He divided Hamel’s work into three realms: individual, societal and institutional.
Fr. Nairn wrote that Hamel challenged Catholic health care to see how developments in genomics could serve humanity, addressed the topic of emergency contraception after sexual assault, and emphasized that justice should be “at the heart of the healing ministry.” Hamel encouraged
ASSEMBLY 2024 AWARDS
Hamel spent decades writing about and offering counsel on Catholic health care ethics. “The key thing we need to focus on is carrying out a ministry of healing,” he says.
Ron Hamel shares a laugh with his former colleague Patrick McCruden, chief mission integration officer for SSM Health. As a theologian and ethicist, Hamel has focused on asking and answering complex and difficult questions related to the Catholic health ministry.
6 CATHOLIC HEALTH WORLD June 2024
Once Films Once Films
organizations to practice “organizational integrity”— the idea of talking the talk and walking the walk — and discussed the theological principle of cooperation and the future of Catholic health care ethics, Fr. Nairn wrote.
“He’s observing, but what I also like about him is there’s not this kind of like, ‘Hey, I’m older. I’m more experienced. I don’t have anything to learn from you.’ It’s a mutual relationship in that regard where he’s learning and growing as much as we are.”
— Michael Panicola
During his time at CHA, Hamel realized many of his mentors in the field had either retired or passed away. He performed two surveys to get an idea of the average age and experience of Catholic health care ethicists in the field. As he suspected, there were gaps. He recruited and influenced younger ethicists by inviting them to colloquiums and being available to answer questions.
Michael Panicola considers Hamel a mentor. Panicola met Hamel at the CHA assembly in New Orleans in 1998. At the time, he was pursuing his Ph.D. and in his first week as an ethicist at SSM Health.
Panicola remembers feeling a little awestruck meeting Hamel and other ethics leaders.
“We hit it off professionally, and then we became friends pretty quickly,” said Panicola. “He’s an amazing listener. He’s observing, but what I also like about him is there’s not this kind of like, ‘Hey, I’m older. I’m more experienced. I don’t have anything to learn from you.’ It’s a mutual relationship in that regard where he’s learning and growing as much as we are.”
Panicola eventually became a vice president of ethics at SSM Health, and the two collaborated on several articles. They celebrate holidays together, and Panicola’s three grown children consider Hamel, who never married, as a third grandfather.
Panicola noted that the soft-spoken Hamel can get “fiery,” especially if he suspects a ministry is being disingenuous.
Speaking with courage
Rachelle Barina, chief mission officer for Springfield, Illinois-based Hospital Sisters Health System, also considers Hamel a mentor. “He’s not always challenging every issue. But when it’s necessary to care for people who are in vulnerable spots, he’s willing to speak with courage,” said Barina, a 2024 Tomorrow’s Leaders honoree. She cited, for example, that Hamel and Panicola took on the topic of emergency contraception after sexual assault and came to the conclusion that it was ethically justifiable and that victims of sexual assault should have access to emergency contraceptive medications. Their position was not without considerable debate in some sectors.
To stay grounded, Hamel meditates daily and enjoys nature, hiking and traveling. He volunteers at a food pantry and is looking for other ways to serve.
He thinks the future challenges of Catholic health care are surmountable. The needs that the founding congregations saw still exist, he said, but the way they’re addressed is evolving. He thinks people shouldn’t only come to hospitals to be healed or cured; hospitals need to go into the community.
“It’s a question of seeing need, stopping, appreciating the need, and doing what needs to be done to address the need,” said Hamel.
“That’s what the good Samaritan did.” vhahn@chausa.org
FROM THE MAIN STAGE
Keynote speakers:

AMY FINKELSTEIN
John and Jennie S. MacDonald Professor of Economics at MIT
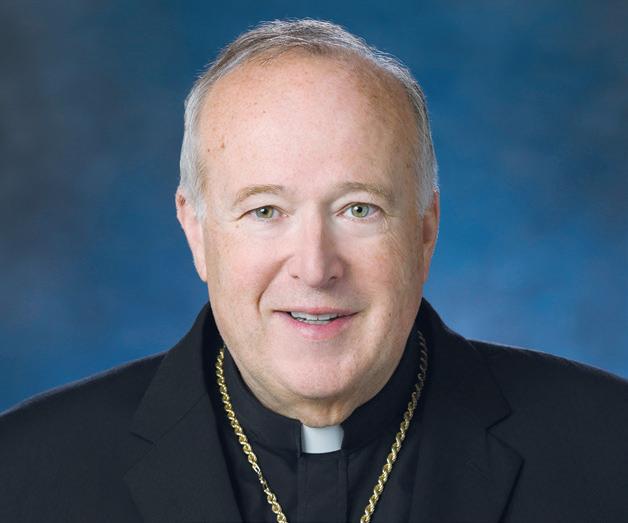
CARDINAL ROBERT M C ELROY
Bishop of the Diocese of San Diego

TOM KOULOPOULOS
Author, Futurist and Leader
Catholic Health Care and American Culture Panel:

CATHLEEN KAVENY, JD, PH.D.
Darald and Juliet Libby Millennium Professor at Boston College

DR. CLAUDIA RUIZ SOTOMAYOR, DBE, HEC - C
Chief, Ethics Consultation Service, and Clinical Ethicist, Pellegrino Center for Clinical Bioethics

MICHAEL SEAN WINTERS
Columnist, National Catholic Reporter, and Fellow, Center for Catholic Studies, Sacred Heart University
March 1, 2022 CATHOLIC HEALTH WORLD 7 June
SISTER CAROL KEEHAN AWARD
CHI Friendship president strives to give people ‘a life that they choose to live’
 By LORI ROSE
By LORI ROSE
For Dori Leslie, president of CHI Friendship, success in serving people with developmental and intellectual disabilities isn’t always measured in major milestones. Often it’s the little things that are cause for celebration.
When a person supported by CHI Friendship joins a bowling league, adopts a cat, clocks out at a new job without help, or chooses their own dining table — these are stories of growth, independence and bud-
ding passions that may seem ordinary to some, but to Leslie carry deep meaning and satisfaction.
The stories illustrate how Fargo, North Dakota-based CHI Friendship nurtures the abilities, talents and interests of each person it serves and helps them reach their goals and realize their dreams. And the stories demonstrate to the wider world that people with disabilities are just like everyone else.
“My passion is to make the people we support feel loved and cared for every

day,” Leslie said. “Unfortunately, there are still a lot of boundaries for acceptance of people who have a different kind of ability. We’ve come so far, but we have a long way to go. Yet, that’s our fuel for our passion to continue.”
In recognition of her leadership in championing those who are among society’s most vulnerable, and for her unwavering advocacy for increased freedom and opportunities for people with disabilities, Leslie is the recipient of CHA’s 2024 Sister Carol Keehan Award. CHA created the award in honor of the former CHA president and CEO, a longtime defender of social justice and health care access for all.
The award is given each year to someone who advocates for a more equitable and compassionate health system, exhibits a commitment to social justice, defends society’s most poor and vulnerable, demonstrates the ability to shape public opinion, is steadfast in the face of adversity, and works to further the common good.
“Dori has the deepest servant leadership heart of any not-for-profit leader that I have seen,” said North Dakota state Sen. Kathy Hogan, who is chair of the CHI Friendship board. “I’ve worked in human leadership for almost 50 years. Dori exemplifies servant leadership. She always remembers that the primary purpose is to ensure that the people who are supported are valued as human beings.”
Christ in the face of all people
Leslie, who earned a bachelor’s degree in physical and special education and a master’s in leadership from the University of Jamestown in North Dakota, started working with vulnerable populations while still
in college. She fell in love with the industry and the people she served. After graduation, she joined CHI Friendship, now part of CommonSpirit Health, as a direct support professional — the person who helps individuals served with their day-to-day activities. Over the next two decades, she took on numerous roles within the organization. CHI Friendship named her president in 2017.
CHI Friendship serves 275 people through residential and vocational programs and employs about 400. Through Leslie’s leadership, it has become an industry leader, embracing new ideas, promoting community-integrated employment, and advocating for all people to regain and maintain their legal rights. Leslie has worked with local, state and national leaders to make sure that people with disabilities are not marginalized and that the standards set for the lives they lead are the same standards she and her colleagues have for themselves.
“We help people have a life that they choose to live, a life that is filled with their decisions, if they want to go to church, if they want to go shopping, if they want to go to a park and just hang out,” Leslie said. “We help them have a life of purpose and a life of meaning.”
Her conviction that Christ is in the face of each person she meets is at the core of everything she does. “To me, serving others is the right thing to do,” she said. “It’s who I am as a person. Helping others is part of my personal spirituality, and it brings me life.”
Retired CHI Friendship CEO Jeff Pederson worked with Leslie for 20 years and saw her living out her values every day.
“People with intellectual and develop-
Dori Leslie, right, chats with Secera Beciraj at the second annual Friendship Formal, an event for those CHI Friendship serves. Leslie has been president of the Fargo, North Dakota-based organization since 2017. CHI Friendship develops residential and vocational programs to assist people with developmental disabilities to live and function to the best of their ability in the community.
ASSEMBLY 2024 AWARDS 8 CATHOLIC HEALTH WORLD June 2024
Dori Leslie greets Jay Sorum, a CHI Friendship board member, at the organization’s 50th anniversary gala. Sorum is among the many people supported by CHI Friendship. Under Leslie’s leadership, the organization embraces new ideas, promotes community-integrated employment and advocates for legal rights for everyone.
mental disabilities are oftentimes seen as the least of my brethren,” he said. “Dori has been a champion for their right to participate in all aspects of their lives and for them to be seen and accepted as part of society. She is a wonderful role model.”
Challenging norms
Recently, Leslie led an initiative to take a closer look at the restrictions affecting people served, whether those people live in one of CHI Friendship’s seven group homes or receive other services. Her goal was to remove as many restrictions as possible to encourage those served to take charge of their own care and their own lives.
She started with a role-playing exercise with staff members that was designed to create feelings of discomfort. Afterward, she said, there was “a newfound empathy involving rights restrictions and people were ready to roll up their sleeves and get to work” removing those barriers.
Rights restrictions are meant to ensure safety for people with disabilities and are agreed upon by the person’s guardian and reviewed annually. But Leslie believed many were unnecessary, overreaching or outdated. Working with case managers and others, she set out to challenge the norm. So far, more than 300 rights restrictions have been removed from those CHI Friendship serves. Leslie said this has increased selfesteem, empowerment and independence.
“ We
really try to advocate and educate that people who have a disability are no different than anybody else. Because guess what? We all have different abilities. We all excel at some things and we all need more help at some things.”
— Dori Leslie
“In the field of developmental disabilities, it is quite often the norm to have people with a disability not have the same rights as every other American citizen,” Leslie said. “We have given people their rights back regarding voting, where they go to eat or what they eat, or how much pop they can have a day, or the right to marry, or the right to who they live with.
“It’s not the popular thing to do, but it’s the right thing to do,” she said. “It’s hard, but hard things yield great results. And by making sure that we give every person that we serve the ability to live a life, just like
you and I want to, we’re making change happen.”
Leslie cited the example of a resident who did not like living in a traditional group home and wanted his own apartment in the community.
“He sat right at the end of my desk and said, ‘I’m moving, please help me. I don’t want to live with anybody else,’” she recalled. “We all wrapped our arms around him and said, ‘You’re right. You’re in charge.’ Today, he’s successfully living in his own apartment, happy, makes his own decisions, and we’re there to support him when he needs us to.”
A pioneer
Leslie said CHI Friendship has long been a trailblazer in the industry and she is dedicated to continuing that leadership.
“People often call us pioneers who try new things, who are bold and not afraid to make a difference,” she said. “I have seen, over my past 26 years, a paradigm shift within our services. Twenty-plus years ago, people were all living in group homes, large institutions. And Friendship was one of the North Dakota facilities that said, ‘What if people lived in their own apartments by themselves? Yes, let’s make it happen.’”
Today, CHI Friendship supports 41 individuals in its group homes and provides services to 71 others who rent apartments across the community.

Similarly, CHI Friendship is an industry leader in ensuring that people who want to work can work. The organization has 150 people in its vocational program. Leslie is committed to making connections in the community that might lead to new employment opportunities for those served.
She also works to educate others about the value of an inclusive community. The more ways in which CHI Friendship and the people it serves are involved in the community — through employment and volunteer opportunities, through churches and schools, and even media appearances — the healthier the community is, in her view. During her tenure, CHI Friendship has increased community outreach activities that help shape public opinion and illustrate that people are all more alike than different.
“It is important to me personally, but also our industry, to continue to educate others that people who have all kinds of abilities are included in all aspects of life,” she said. “We really try to advocate and educate that people who have a disability are no different than anybody else. Because guess what? We all have different abilities. We all excel at some things and we all need more help at some things.”
A culture of respect
Staff members and colleagues say Leslie nurtures a culture of respect, compassion and camaraderie that makes Friendship a great place to work. David Jones, regional market president for CommonSpirit Health, sees it in action.
Community Benefit 101
The Nuts and Bolts of Planning and Reporting Community Benefit
OCTOBER 15, 16 & 17, 2024
Each day from 2 to 5 p.m. ET
CHA’s highly regarded Community Benefit 101 provides new community benefit professionals, and others who want to learn more, with the foundational knowledge and tools of community benefit programming.
LEARN MORE AND REGISTER NOW AT WWW.CHAUSA.ORG/CB101
This virtual program is taught by experienced community benefit leaders. Topics covered include the importance of the organization’s community benefit mission, public policy, what counts as community benefit, community health needs assessment and implementation strategies, program planning and evaluation, accounting principles and communicating the organization’s community benefit story.
ATTENDEES WILL RECEIVE A COPY OF CHA’S A GUIDE FOR PLANNING AND REPORTING COMMUNITY BENEFIT.
Thank you to our sponsor, the American Hospital Association.

“When she talks about the people she works with, whether the employees or the communities she serves, she really does get excited,” Jones said. “Her eyes light up. She definitely lives what she is getting honored for. Dori ties everything back to the mission. It makes her a very consistent and honest leader.”


Bold Change
Elevate
We Will Empower
to
Human Flourishing. SM
Contact Madeline Hantak at mhantak@chausa.org for information about underwriting. American Hospital Association — Institute for Diversity and Health Equity (IFDHE) ApolloMD Aquinas Institute of Theology Care Continuity EWTN Global Catholic Network Health Trust Performance Group Huron Institute of Reproductive Grief Care Key Green Solutions Loyola University Chicago Bioethics Institute SafePoint by SoundThinking ShiftMed June 2024 CATHOLIC HEALTH WORLD 9
Achievement Citation
From page 1 interlopers had.

Maron assured the group he was a man of his word, and he promised them that Holy Name would be different. He said Holy Name would be a true partner to Hôpital Sacré Coeur, continually seeking the staff’s perspective, respecting their input and working closely with them to improve health care access in North Haiti.
For its success in keeping this promise, Teaneck, New Jersey-based Holy Name has earned CHA’s 2024 Achievement Citation, the association’s recognition of innovative programming that changes lives.
Surging volumes
The Montreal province of the Brothers of the Sacred Heart founded the 10-bed Hôpital Sacré Coeur in 1968 on land that the Catholic Archdiocese of Cap Haitien owned in Milot. In 1986, at the Cap Haitien archbishop’s request, the Brothers’ Center for the Rural Development of Milot, or CRUDEM Foundation, assumed financial and supervisory control of Sacré Coeur.
When a 7.0-magnitude earthquake ravaged Haiti’s capital and most populous city, Port-au-Prince, in January 2010 and when cholera broke out about 10 months after the quake, Sacré Coeur experienced large surges of patients. Milot is about 120 miles north of Port-au-Prince.

Holy Name obstetrician Dr. David Butler already had been traveling to Sacré Coeur as a medical missionary for about a dozen years when he journeyed there in 2010 to provide medical aid to quake victims. He was so distressed at the conditions he witnessed that upon his return to New Jersey he pleaded with Maron to help solve one of the Milot hospital’s greatest concerns: regularly running out of oxygen. Without oxygen, doctors could not perform lifesaving surgeries.
Maron coordinated the purchase and transport of an oxygen generator then traveled to Milot to ensure its safe delivery and installation. That 2010 visit inspired Maron to engage Holy Name leadership and clinicians in increasing involvement in the Haiti hospital. This included Holy Name providing bridge loans to shore up Sacré Coeur’s finances as it strained to respond to ongoing patient surges.
By 2012 it had become clear that the hospital was in such dire financial straits that without even more help, it would close, leaving the approximately 250,000 people
HAITI
DEMOGRAPHICS
More than 60% of the population of 11 million lives below the poverty line.
Three-quarters of Haitians live on approximately $2.41 per day.
More than 4 million face crisis- or emergency-level food insecurity.
Life expectancy at birth is 63 years, compared with 76 years in the U.S.

Haiti has as few as 10 health professionals per 10,000 inhabitants. The World Health Organization’s recommended ratio is 45 per 10,000.
More than 80% of funding for health services comes from the international donor community.
The country is facing numerous crises, including high unemployment and inflation; a volatile national currency; and severe recurring fuel shortages.

in the region around Milot with no hospital. Holy Name agreed that year to sponsor Sacré Coeur.
Evolution
As sole sponsor of Sacré Coeur, which now has about 230 inpatient beds, the New Jersey hospital foundation has provided tens of millions of dollars in funding since 2012 as well as administrative, technological, operational and clinical support. Holy Name also has coordinated dozens of meal packaging events in the U.S. over the past five years. The medical center has shipped more than 1 million of those packaged meals per year to Haiti for distribution to malnourished people in the Milot region.
Butler says under the Holy Name–Sacré Coeur partnership, the Milot hospital has become a smoothly functioning facility with a healthy supply chain, a growing capacity to offer health and social services, and a strategic plan for additional growth. All these feats are extremely difficult to accomplish in a country plagued by natural disasters, poverty, civil unrest and gang violence. Sacré Coeur has become an economic powerhouse and lifeblood of northern Haiti, Butler says. He is chair of the board of Haiti Health Promise — the Holy Name affiliate that fundraises for Sacré Coeur.
Holy Name Executive Vice President of Operations Steve Mosser has coordinated many of the capital projects, construction
The focus over the decade of Holy Name’s sponsorship has been on having the U.S. clinicians educate and train Haitian clinicians so that the Milot team can increasingly take over the medical procedures. The goal is to continually build capacity and eventually hand off all the work to the Haitian staff.
Sources: U.S.
Cap Haitien Milot Port-au-Prince
Department of State, World Bank and U.S. Agency for International Development
HEALTH CARE AND SOCIOECONOMIC OUTLOOK
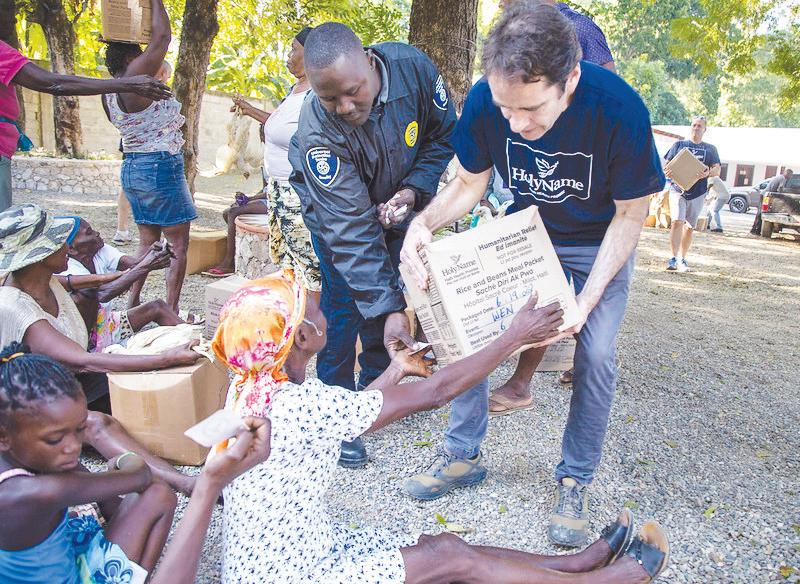
Dr. James Morgan, right, assists in the distribution of food to community members in Milot, Haiti, in May 2023. The food was packed and assembled at one of the “packathons” sponsored by Holy Name Medical Center and its foundation.
Dr. Harold Prévil, left, and Dr. David Butler, center, perform a surgery in 2020 at Hôpital Sacré Coeur. Butler, a Holy Name obstetrician, has completed many mission trips to Haiti over the past 32 years.
ASSEMBLY 2024 AWARDS
Maron
10 CATHOLIC HEALTH WORLD June 2024
Butler
Despite challenges, Holy Name and Hôpital Sacré Coeur plan for growth
Even though civil unrest and other major challenges in Haiti have threatened to disrupt the advancement of Milot’s Hôpital Sacré Coeur, the hospital has succeeded in partnering with its sponsor — Teaneck, New Jersey-based Holy Name Medical Center’s foundation — to make continual improvements over the past dozen years. And Sacré Coeur has plans to grow even more in the years ahead.
Under Holy Name’s sponsorship, Sacré Coeur has installed a critically needed oxygen generator and power plant, added
a cafeteria that the staff had been pleading for, renovated or added emergency department and clinic space, and added four operating rooms. It now has plans to add a much-needed Women’s and Children’s Hospital.
Holy Name has purchased land near Sacré Coeur for future development. Holy Name is seeking U.S. funding — both philanthropic and governmental — for growth in that geographic area.
Holy Name President and CEO Mike Maron says construction of any kind is
difficult in Haiti because there is little to no infrastructure to tap into. Builders need to dig their own wells and generate their own power, for instance.
Also, supply chains can be so unreliable that Holy Name has found it beneficial to invest in Milot-area supply. For instance, Holy Name is investing in Milot-area agriculture for food staples and it plans to expand upon these efforts as it helps grow Sacré Coeur’s recently secured 95-acre farm.
Additionally, acute lack of housing and
HÔPITAL SACRÉ COEUR 2023 STATISTICS
Beds: 230 Outpatient visits: 57,057
Hospital admissions: 6,557
Emergency room visits: 4,963
Surgeries: 2,491 Newborn deliveries: 2,340 Diagnostic tests: 17,377 Prescriptions filled: 136,303

work and operational work at Sacré Coeur under Holy Name’s sponsorship. He attributes the Haiti hospital’s success to Holy Name and Sacré Coeur’s commitment to the spirit of partnership that Maron established in 2012.


Mosser says Holy Name and Sacré Coeur have continually evolved their relationship. Before Holy Name became sponsor, he says, the usual way of doing things was to have a different team of medical missionaries from all across the U.S. come to the Milot hospital about every week to perform surgeries and other skilled procedures, with those clinicians often bringing family members along. The visiting clinical teams normally would bring medical and other supplies with them. Dr. James Morgan, medical director of Haiti Health Promise, says under this approach, it was nearly impossible for the Haiti staff to have continuity and to systematically address root causes of hospital issues. Plus, with the “drop-in” medicine, there was very little preventive or follow-up care or social services available to patients, so it was difficult to promote healthy outcomes over the long term.
Over time, Holy Name has been cutting back on the use of drop-in medical missionaries, and clinicians who do come must have multiple medical skill sets. They no longer can bring family members who essentially had been like missionary tourists. The focus over the decade of Holy
Name’s sponsorship has been on having the U.S. clinicians educate and train Haitian clinicians so that the Milot team can increasingly take over the medical procedures. The goal is to continually build capacity and eventually hand off all the work to the Haitian staff.

Cedar Wang, Holy Name vice president of nursing operations, has supported the Milot staff’s professional development by building up a comprehensive training and education program that includes simulations and role-play scenarios in the Sacré Coeur staff’s native languages, Haitian Creole and French.
Community building
Just as Holy Name has been seeking to hand as much clinical control as possible over to the staff, it also has been seeking to “localize” the hospital’s supply chain and operations.
For the past decade, the Holy Name–Sacré Coeur team has been aiming to use Haitian laborers working with Haitian raw materials to the extent possible when constructing new facilities, or to at least have the on-site workers train Milot-area workers in their trades.
As much as possible, Holy Name also has been aiming to use local food suppliers for staff and patient nutrition. Through these efforts, Sacré Coeur has increased its capacity over the last decade-plus to provide emergency, maternity, pediatric, dental, prosthetic, laboratory, pathology, HIV/AIDS and a
quality education has made it difficult to attract and retain clinical and other staff in Milot. The broader local population also has suffered because of the housing shortage and lack of access to quality education. So Holy Name plans to continually invest in Milot-area housing and education.
Maron says Holy Name expects this community-building to pay off in the long term by stabilizing Milot.
— JULIE MINDA
variety of other services, plus it has built up a strong community health outreach team. It also has strengthened nutrition, housing and education in the surrounding community.
Pervasive threats
Despite all that has been achieved, further progress at Sacré Coeur is under constant threat, say the Holy Name leaders. Southern Haiti — and in particular Port-auPrince — is experiencing great upheaval, extreme civil unrest, poverty and gang takeovers. Northern Haiti is not immune from the reverberations. Sacré Coeur staffing, supply lines, hospital safety and resources are continually at risk.
The Holy Name leaders say they and their colleagues remain committed to Northern Haiti and they have hope the momentum that Holy Name and Sacré Coeur have built up is not in vain.
Butler says the Haitian people have a persistence that is remarkable — and that bodes well for the long-term success of Sacré Coeur.
Wang says the camaraderie that has grown among the Holy Name and Sacré Coeur staffs has made them all feel like one big team, pursuing one mission, and that puts them in a strong position to take on the challenges.
“This relationship has grown and deepened,” says Morgan.
Mosser says: “It feels like the Hôpital Sacré Coeur staff are extended family.”
For more on Holy Name’s support for Haiti, visit chausa.org/chw. jminda@chausa.org


















 Hôpital Sacré Coeur was founded in 1968 on land that the Archdiocese of Cap Haitien owned in Milot in Northern Haiti. At its start, it had 10 beds. It now has 230 beds and last year had 6,557 admissions.
Mosser
Morgan
Hôpital Sacré Coeur was founded in 1968 on land that the Archdiocese of Cap Haitien owned in Milot in Northern Haiti. At its start, it had 10 beds. It now has 230 beds and last year had 6,557 admissions.
Mosser
Morgan
GLOBAL HEALTH Developing a Roadmap for Sharing Network for Leaders in Catholic Health Care FIND RESOURCES CHAUSA.ORG/ GLOBAL-HEALTH FOR MORE INFORMATION: Contact Bruce Compton Senior Director,
Global Health bcompton@chausa.org
June 2024 CATHOLIC HEALTH WORLD 11
Wang
Caregivers of people with chronic conditions get support at Iowa center
By JULIE MINDA
CEDAR RAPIDS, Iowa — When Bob Kazimour and his wife, Jan, were honorary chairs of a fundraising effort about a decade ago to raise capital to start the Family Caregivers Center on the Mercy Medical Center campus in Cedar Rapids, little did he know that center would become a vital resource for him.
When Jan developed Alzheimer’s years later and in time became nonmobile and nonverbal, he found his caregiving role to be increasingly difficult. He turned to the Family Caregivers Center and got access to a wide range of resources and joined a men’s coffee group. Those men who are caregivers to spouses with dementia have been meeting since 2016 to talk about what they are experiencing and to share insights on how to better care for themselves and their wives.

“This group has been wonderful for me — we’ve helped each other a lot,” Kazimour says. With the support of the other men in the group, “I don’t feel like a lone ranger,” he says. Kazimour’s wife died Sept. 7. Kazimour is among the thousands of Cedar Rapids-area caregivers who have received resources, services, programming and support from the Family Caregivers Center since its 2015 opening. According to founder and Director Kathy Good, the center seeks to ease caregivers’ stress and equip them to nurture themselves and their loved ones.
Around-the-clock role
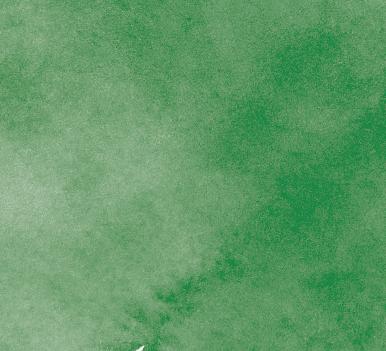
A 2020 report from the National Alliance for Caregiving says about 53 million people in the U.S. are unpaid caregivers.
This role can be highly stressful and emotionally and physically taxing; and for some it is a 24-hour, seven-days-a-week role. It can be so strenuous and difficult that the caregivers themselves can pay a price in terms of their own mental and physical well-being. An estimated 40% of caregivers die before the person they are tending to. Mary Ann Grobstich, a community facilitator with the Family Caregivers Center, says these caregivers are at great risk, especially since in many communities there is not much support available.
To address such gaps that were evident in Cedar Rapids a decade ago, Good

CAREGIVING IN THE U.S. 2020
The number of Americans providing unpaid care has increased.*
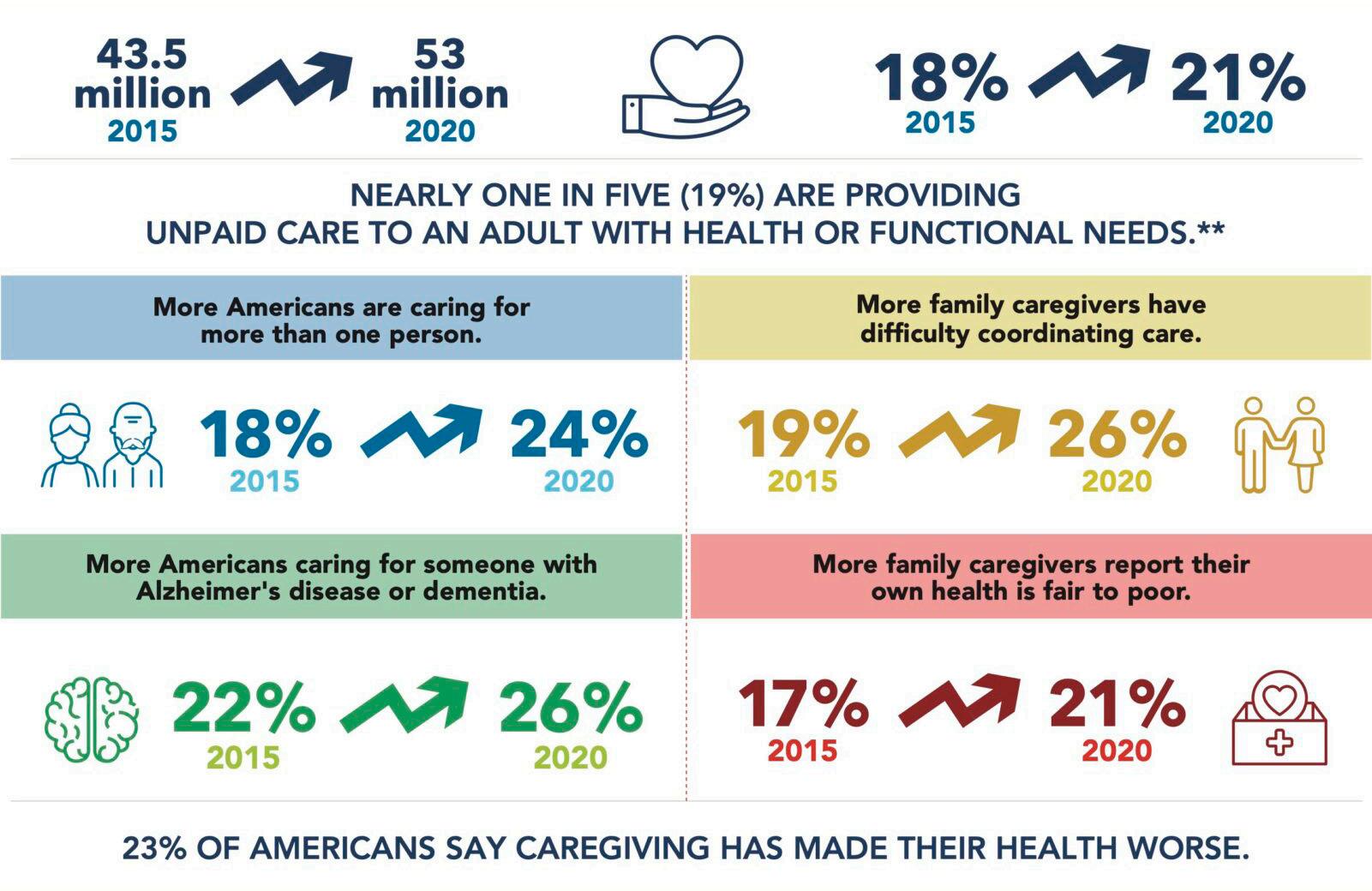
* Provided care to an adult or child with special needs.
** The remainder of this data is based on the 19% or 48 million caregivers caring for an adult.
Sources: Caregiving in the U.S. 2020, National Alliance for Caregiving and AARP
accepted the challenge of Tim Charles, who was Mercy Cedar Rapids president and CEO

at the time, to see whether Mercy could replicate the idea of a family caregiver center he’d seen in New York. Good, who had a social work background, was an acquaintance of Charles. At the time he approached her, she was a caregiver for her husband, Dave, who had Alzheimer’s and was a resident of Mercy’s HallMar care center.
From concept to reality
Good embarked on an extensive effort to create a center that would aid caregivers and the people they were supporting. She worked with Mercy leadership and a committee of community leaders with caregiving experience to study the gaps in services for caregivers locally, consult numerous caregivers and experts in caregiving, build plans for the center, fundraise for it and coordinate its development and eventual completion.
The Family Caregivers Center opened on the Mercy campus in 2015. Mercy since has opened another center in suburban Cedar Rapids — Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia — to spur innovation in programming for people living with chronic conditions, including changing cognitive abilities.
The two centers share a staff of less than a dozen, with most of them having a social work background and many of them with lived experience as caregivers. Dozens of volunteers support the centers’ work. The Family Caregivers Center has an annual budget of about $450,000, and the Innova-
tion Center, about $400,000 (excluding the Center for Memory Health that is on the premises). Since partnering recently, Mercy Cedar Rapids and Presbyterian Homes & Services jointly own the buildings. The centers are funded by Mercy and through philanthropy.
Ever-growing list of offerings
Good, her team, volunteers and a committee of community members with caregiving experience are continually evolving and expanding the resources that the Family Caregivers Center and the Innovation Center provide. Many of the centers’ offerings are free, though clinical services provided at the Center for Memory Health at the Innovation Center are paid by insurance.
Caregiver resources are available at both the Family Caregivers Center and the Innovation Center. Staff meet one-on-one with every family who seeks services and talk to them about their situation and needs then connect them with services. The centers’ staff — in many cases along with trained volunteers — offer emotional support and help accessing community resources, respite services, educational presentations, and referrals to legal services such as on wills and advance directives. The centers have a lending library of materials that offer caregivers relevant information. The centers are getting ready to debut an online networking tool for caregivers.
But the bread and butter of the centers’ caregiver offerings are the numerous support and social groups that caregivers can access. Many are available as hybrid in-person and virtual gatherings. There are groups available for women caregivers, men caregivers, couples in which one person is living with dementia, and people transitioning out of caregiving after their loved one’s death. There are exercise, gardening, journaling and spirituality workshops, all geared to caregivers. Sometimes the workshops are open to people living with chronic conditions. There also are group series on the legal aspects of caregiving, sexuality between caregivers and their spouses with dementia, and loss and grieving. More groups and sessions are being added continually.
The centers offer companions for people with dementia while spouses attend sessions.
Hunger for services
Sue Rowbotham is a volunteer who cofacilitates a support group for people with early-stage dementia. She says “people are
Good
In Cedar Rapids, Iowa, the Family Caregivers Center and the Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia host numerous group sessions for family caregivers and people with dementia. Mary and Gary Crandall participate in a discussion as part of the Living My Best Self group session for people with early-stage dementia and their caregivers. The centers are a department of Mercy Medical Center in Cedar Rapids.
A group of people who are caregivers to individuals with dementia take part in a journaling group at the Family Caregivers Center on the campus of Mercy Medical Center in Cedar Rapids, Iowa. They learned to use journaling to reduce their stress by processing their feelings.
Continued on 13
12 CATHOLIC HEALTH WORLD June 2024
Josh Booth /Diamond Label Films
Sweet treats and sharing:
Men’s coffee group is lifeline for members
By JULIE MINDA
CEDAR RAPIDS, Iowa — Each week more than 20 men meet at the Family Caregivers Center on the campus of Mercy Medical Center here, with some of them gathered around one of the center’s meeting room tables and others joining on the big screen in the room by Zoom.
While the assortment of baked goods on the counter in the corner is a magnet for many of the in-person attendees, the camaraderie, resources and sharing are what draw all the members back to this group each week to delve into what they are experiencing as caregivers or former caregivers of wives or partners living with chronic conditions including dementia.
One of numerous support groups that the Family Caregivers Center and its sister facility, the Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia, offer, the men’s coffee group started around 2016. A Family Caregivers Center volunteer had lamented to the center’s founderdirector, Kathy Good, about society’s lack of attention to the needs of men caring for loved ones with dementia. And Good worked with volunteers to start the group.
The group’s popularity has led to the need to offer two weekly sessions to accommodate the growing numbers. And sessions now are held at the Innovation Center that opened last summer rather than the Family Caregivers Center.
No forbidden topic
Rob Cook is one of several men who volunteer as facilitators of the group and attend as participants. He says everything discussed during the weekly sessions is kept confidential by all attendees, and “no topic is forbidden.” He says the men share their experiences, their hopes, their goals, their spirituality, the practical issues they are facing and potential solutions, and the basics of medical concerns they and their spouses are encountering. A retired physician, Dr. William Gallbraith, helps the group talk through those medical topics — everything from fall risks to incontinence.
Group members learn about the numerous resources offered by the Family Caregivers Center and Innovation Center, and they often share with one another interesting books and articles they’ve found helpful on dementia or caregiving or similar topics. They point each other to community providers and services they’ve used, such as a dentist at a local community college who essentially makes house calls.
Many of the men knew each other socially and/or professionally before joining the group. Many have become friends through the group. Some men continue

Practical solutions
CHA launches ad campaign to tell story of Catholic health care
By VALERIE SCHREMP HAHN
CHA has launched a digital media ad campaign to introduce Catholic health care and communicate its unique value to patients and the community.
The campaign, When Healthcare Really Cares, is framed around three messaging pillars: whole person, community, and access, and tells the national story of Catholic health care. Its tagline is “We care. You flourish.”
hungry for” what the centers are providing. Some people participate in multiple support groups and classes and also sign on as volunteers.
Staff member Grobstich says a key reason people choose to become so invested and involved in the centers has to do with the culture the centers have created. She says the focus is on building trusting relationships and on engagement. “We have this commonness in caregiving, and that is humbling,” Grobstich says. “This creates an openness to learn and to have real connections with one another.”
to attend the coffee gatherings even after their spouses die. The group began with five attendees; the count has ebbed and flowed over time. There now are about two dozen men attending between the two meeting times.
New role
Bob Kazimour is a men’s coffee group member who was a caregiver for his wife, Jan, until her death. He says the support sessions are vital for men because, for most of them, caregiving is a new role. Kazimour was the youngest — and the only boy — in a family of five. Between his sisters, wife and two daughters, he was always taken care of. “We men usually didn’t do the caregiving,” he says. “We weren’t exposed to it. We cut down trees and dug holes. We didn’t take on the caregiving roles.”
Group member Paul Swearingen agrees. He says when he married his wife nine years ago, she already had Parkinson’s and later was diagnosed with dementia. He says with 60% of family caregivers being women, society doesn’t always see men as caregivers and men don’t always anticipate that someday they will become caregivers. But he says husbands generally are the best caregivers for their wives because they know them best and can serve as their advocates.
Swearingen says he recognized that he was trying to do too much on his own and so he has learned, in large part through the coffee group, that he needs to accept help from others and to delegate some tasks to people who can assist him.
He says the group also has helped him understand the importance of caring for his own health. He says he had put his own well-being on hold for the nine years of his marriage as he focused on caring for his wife. He’s now been convinced to see a physician and has learned that his own health is at risk due to neglect. He is now making some healthy lifestyle changes.
Kathy Krapfl, the Family Caregivers Center office coordinator, says, “You can see the relief of caregivers when they are in the groups, when they are in the network (of caregivers). They find joy. There is laughter.”
It is usual for caregivers in the support groups and other activities to build deep and lasting friendships with one another. They commonly socialize outside of classes and sessions.
Lisa Hawk, a center social worker and counselor, says in this environment, “caregivers feel safe to process what they are going through. They feel they have permission to focus on their own needs,” which
Many of the men’s discussions are focused on problem-solving for concerns that have arisen as they care for their wives. They share cooking tips — some of them are the primary cook of their household for the first time now. They talk through how they’ve learned to safely get their wives in and out of the shower to prevent falls.
One group member, Larry Doehrmann, came up with a fidget blanket that he shared with the group. Each blanket has items attached that people can manipulate to keep their hands busy. The blanket kept his wife occupied in her restlessness. She had dementia. She died in 2022, but Doehrmann remains active with the group.
Swearingen developed a gait belt, or a sturdy belt that a companion can use to safely steady their loved one. He offered the belts, which are used for fall prevention, to group members. He now is looking to patent them.
The group has spurred this creativity not just around practical concerns but also when it comes to how the men come together to process the emotions they are feeling. So many share similar experiences and perspectives that they are able to empathize, encourage and cheer one another on.
Cook says, “Men are not supposed to be good at expressing our needs and fears, but we’ve found that we are better at it than we thought we would be.”
Group member Tom Brennom says he has been like a sponge, absorbing all the learnings and experiences of the group. He sees the group as helping him live his life to the fullest. “I’m passionate about this group,” he says.
Swearingen credits the coffee group members with convincing him to see to his own health and prevent a personal health crisis. “I probably wouldn’t be here if it weren’t for this group,” he says. jminda@chausa.org
can be very difficult for them to do.
The centers have found that meeting the multidimensional needs of caregivers can greatly enhance the caregivers’ health and well-being, which can in turn improve mental health and clinical outcomes. This can be true for both the caregivers and those they are caring for.
“It takes a whole team to ensure caregivers are healthy and well,” says Abby Weirather, manager of the Family Caregivers Center.
Hawk adds: “Caregiving is never going to be easy, but we are trying to make it easier.” jminda@chausa.org
“Our members do an amazing job telling the story of Catholic health care in their local communities,” said Sr. Mary Haddad, RSM, president and CEO of CHA. “At a national level, the narrative around our ministry too often is misrepresented or tied to hot-button issues. This campaign is designed to provide examples of how our mission and commitment to human dignity and the common good are reflected in the care we provide.”
While the campaign’s social media posts will be shared nationally, paid ads initially will be directed toward a general population with Catholic health systems in Oklahoma City, Milwaukee and Philadelphia. The campaign later will move to St. Louis; Portland, Oregon; and Detroit. In addition, outdoor digital ads will appear in Washington.
“We are using paid digital ads to amplify the stories that our members share with CHA through our publications and other programming,” said Brian Reardon, CHA’s vice president of communications and marketing. “This campaign will also support the advocacy work of CHA and provide examples of what it means to embrace bold change to elevate human flourishing, which is what our vision statement calls us to do.”
The campaign, developed by St. Louisbased marketing services firm Brado, employs a tone that shows Catholic health care is trusting, accessible and accomplished. The goal of the campaign is to create and build respect for Catholic health care in the face of ongoing misunderstandings and criticisms.
Its ads include messages like, “When healthcare really cares, mental health is just as important as physical health.” Other ads say “When healthcare really cares, zip codes don’t define treatment” or “When healthcare really cares, insurance companies don’t play doctor.”
Other messages revolve around preventive care, neighborhood health, health beyond the exam room, treating patients with respect, seeking out the vulnerable to meet their needs, and treating anyone regardless of ability to pay.
Ads will appear on Facebook, Instagram, iHeart Radio and YouTube, at bus stops, and on streaming television platforms. CHA members will have the opportunity to leverage the campaign with their own brand identity.
In November, CHA and its partners in the Alliance for Access to Care launched the Healthcare Here media campaign, which calls out commercial insurance companies that are posting record profits while making it hard for people to get care.
The website for the When Healthcare Really Cares campaign is wecareyou flourish.com.
vhahn@chausa.org
A coffee group for men meets at the Family Caregivers Center and the Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia. Most of the men are caring for spouses with dementia, or have had the experience of doing so. The centers are a department of Mercy Medical Center in Cedar Rapids.
Continued from 12
June 2024 CATHOLIC HEALTH WORLD 13
Long-term care staffing
From page 1
of dollars per year to ensure that 1.2 million Americans that receive care in nursing homes are cared for, yet too many nursing homes chronically understaff their facilities, leading to substandard or unsafe care,” the announcement said. “Understaffing can also have a disproportionate impact on women and people of color who make up a large proportion of the nursing home workforce because, without sufficient support, these dedicated workers can’t provide the care they know the residents deserve.”
The mandates, which begin to phase in in August, are documented in a 125-page post by the Centers for Medicare & Medicaid Services. The agency said the mandates are based on evidence collected since 2016 and lessons learned during the COVID-19 pandemic. Along with many other specific requirements, long-term care facilities that receive Medicare and Medicaid funding must:
Have registered nurses on-site around the clock.
Have 3.48 hours per resident per day of total staffing, of which 0.55 hours per day must be from registered nurses and 2.45 must be from nurse aides. The remaining 0.48 hours can be from any combination of nurse or aide staff.
LaRue pointed out that the federal mandates are similar to rules passed in 2021 in New York state, where ArchCare has seven nursing homes with a total of 2,100 beds. He said industry associations have estimated that 75% of the state’s about 600 nursing homes are not meeting mandates.

“The legislators were very proud of the work that they did, and they had committed to funding them,” LaRue said. “Of course, they have not funded it. In order for (ArchCare) to meet the staffing mandate, I would need another $22 million in revenue.”
LaRue and others who have reviewed the federal staffing mandates noted that the rules do not come with the promise of any enhanced funding to recruit, train or pay staff.
From problem to crisis

Allison Q. Salopeck, president and CEO at Jennings, said she understands the desire to crack down on the “bad players” who run nursing homes with inadequate staff. But she said the staffing mandates have the potential to be devastating across the board for longterm care providers.
“You look across the country, and we’re not talking about a workforce crisis and lack of nurses and lack of nursing home workers as a result of trying to stop this staffing mandate,” said Salopeck, whose system is based in suburban Cleveland. “We’ve been talking about this because it’s a real problem that
FROM 2020 TO JUNE 2023 31% were nonprofit 62% of residents relied on Medicaid 70% of the homes were in urban settings
579 NURSING HOMES CLOSED
21,508 residents were displaced
45,217 beds were lost
AMONG ALL NURSING HOMES AS OF JUNE 2023: 55% were turning away prospective residents/patients
24% closed spaces due to labor shortages
Source: Access to Care Report by the American Health Care Association, August 2023
30
U.S. counties became “nursing home deserts”

started before the pandemic and got to crisis level during the pandemic.”
Salopeck is particularly concerned about the specific breakdown of the staffing requirements. She said while the mandates set specific requirements for registered nurses, they lump the care of licensed practical nurses in with that of nurse aides. The rules, she said, fail to acknowledge that LPNs are the backbone of long-term care in the United States.
“What this does is it really flips us from staffing with mainly LPNs to needing to staff with mainly RNs,” she said. “And they’re just not out there.”
Salopeck also pointed out that the rules are singularly focused on the medical needs of people in long-term care. The mandates make no mention of or allowances for staffing to meet the other aspects of the holistic care that Jennings and other Catholic providers offer, such as pastoral care and social services. “I think it’s a real mistake to have ignored all of those,” she said.

‘Ill-advised’ mandate
In its statement on the staffing regulations, CHA expressed disappointment that the final version “establishes an ill-advised staffing mandate” and sets hours requirements at a time when nurses are scarce.
“We are deeply concerned that the new staffing mandate could actually harm residents and nursing facilities, which will have to leave beds empty or even close if there are not enough nurses to meet the mandate,” CHA said. “Vulnerable seniors will have even less access to the quality care they need.”
The American Health Care Association and the National Center for Assisted Living estimate that more than 1,000 nursing homes have closed since 2015. Of those, 579 closed during the pandemic and displaced 21,508 residents. Meanwhile, the U.S. Census Bureau says the senior population that long-term care facilities largely serve saw its fastest growth in more than a century from 2010 to 2020, to 16.8% of the population, and that growth is continuing.
LeadingAge, the association of nonprofit, mission-driven providers of aging services, also has taken issue with the mandates. Katie Smith Sloan, LeadingAge president and CEO, sent a letter to President Joe Biden expressing dismay over how, in the rollout of the rules, the administration disparaged nursing homes, depicting them as neglectful of patients and their management as indifferent to direct care workers. She also warned of the mandates’ potential effects.
“These new minimum staffing requirements, which come with no additional funds for recruitment, training, or support for increases in Medicaid reimbursement (the main source of nursing homes’ funding), will likely result in unintended consequences,” Sloan wrote. “Older adults’ and families’ existing difficulties in accessing
care will worsen. Already, staffing shortages have resulted in nursing homes placing holds on beds, closing wings, limiting admissions or — worse yet — shuttering entirely.”
Costs and penalties
CMS estimates the average annual increase in costs from the staffing mandates at $4.3 billion over the next 10 years. However, Janine Finck-Boyle, vice president of health policy and regulatory affairs at LeadingAge, said the organization calculated that meeting the mandates will require nursing homes to add about 27,000 registered nurses and 78,000 nurse aides. Its estimated annual cost to pay those workers is about $7 billion.

Meanwhile, Finck-Boyle pointed out that various factors such as immigration restrictions, lack of nurse educators and competition from others in the health care sector have resulted in a “dried up pipeline” for nursing home staff.
The CMS announcement of the mandates proposes a $75 million federal incentive program to bolster nursing home staff, money that Finck-Boyle said would come from monetary penalties on facilities for deficient practices, including failing to meet the staffing mandates. She noted the irony of turning the proceeds of fines for staffing deficiencies into incentives to address a workforce crisis that is itself making the staffing mandates unworkable.
Another quirk in the mandates that Finck-Boyle noted is that while facilities can file for waivers to give them more time to come into compliance, applications for the waivers can only be made after a facility has been cited for being out of compliance.
Finck-Boyle spent two decades in nursing home administration in the District of Columbia, which instituted staffing mandates in 2005. She said those mandates were challenging but manageable. She doesn’t believe the federal rules are, given the dearth of available workers and the lack of increased financial support.
“It’s an unfunded mandate, and I will say that all the time, an unfunded mandate without a pipeline of workforce,” she said.
Viability in doubt
Jerry Carley, president and CEO of Benedictine, said almost all of the 33 long-term care communities his system operates in five Midwestern states already meet or exceed the overall staffing standard. But as with other systems, the specific requirement for RNs and nurse aides is the challenge.

“In some of our rural communities, for example, we haven’t had an RN applicant for two years,” Carley said.
The shortage of nurse aides also is acute, he said, with Benedictine relying on highcost agency staffing to fill positions. He said the worker shortages are worst in rural areas, where the Census Bureau says populations are disproportionately older compared to the rest of the nation.
“Now you throw the staffing mandate on top of it, and there’s just a concern over what’s the future viability of these small rural locations, as well as others,” Carley said. “That’s the piece that worries me the most.”
Carley said the toll of the mandates could be especially harsh on Catholic facilities because of their vow to care for people regardless of means. Like other nonprofit care providers, Benedictine gets much of its funding for those residents from Medicaid.
“The federal government’s going to have to step up and fund these mandates,” Carley said. “They have to, because if they don’t, there is a risk and a high probability that we’ll see what we have seen over the last 10 or 20 years with the number of nursing homes closing.”
leisenhauer@chausa.org
A Jennings resident dances with Deb Tables, a state trained nurse aide who is the life enrichment coordinator. They were taking part in a Mardi Gras celebration at the community in Garfield Heights, Ohio, near Cleveland.
Registered nurse Angelique Robles checks on resident Jodi Stoner at Mary Manning Walsh Nursing Home & Rehabilitation Center, one of seven ArchCare facilities in New York. The system’s head says federal staffing mandates that begin to phase in later this year will be “very problematic.”
LaRue
Salopeck
Carley
14 CATHOLIC HEALTH WORLD June 2024
Finck-Boyle
Hochman to retire as Providence president and CEO at year’s end
Dr. Rod Hochman plans to retire as president and CEO of Providence St. Joseph Health, effective Jan. 1. He has worked in health care for 45 years, 17 of them at Providence.

Hochman had been president and CEO of Swedish Health Services when Swedish merged with Providence Health & Services in 2012. He then joined Providence Health & Services as a group president that year, before becoming the system’s president and CEO in 2013. When Providence Health & Services merged with St. Joseph Health in 2016 to become Providence St. Joseph Health, Hochman assumed leadership of that system.
Under Hochman, Providence has invested heavily in advanced technology, including virtual care, data-driven sys-
Physician burnout
From page 1
which works with advanced practice providers and leaders systemwide to address clinician burnout.
St. Louis-based Ascension is one of the nation’s largest health systems, with about 5,200 physicians and 2,300 advanced practice providers. It has been honored three times by the American Medical Association’s Joy in Medicine Health System Recognition Program, most recently last year, for its efforts to reduce burnout and improve well-being among physicians.
Widespread concern
In 2023, for the third year in a row, a survey of doctors by The Physicians Foundation found that six in 10 often experience feelings of burnout.

“Lots and lots of physicians left during the pandemic,” said Shoemaker. “And I think burnout is a real thing. A lot of physicians are leaving medicine because they’re going to work for an insurance company. Or they’re retiring at 55 instead of 65.”
As the leads of the well-being council, Stanley, a family medicine doctor with Ascension Medical Group in North Vernon, Indiana, and Shoemaker, who specializes in internal medicine and pediatrics with Ascension Medical Group in Fishers, Indiana, are in charge of a council of about 40 physicians who meet regularly to discuss how to best help clinicians.
Wellness tools
To start its work, the well-being council looked to the Stanford Model of Professional Fulfillment to focus on three domains of well-being: a culture of wellness, efficiency of clinical practice, and personal resilience. Following that model and on the council’s advice, Ascension has rolled out several efforts to help.
It has developed a clinical well-being and engagement “playbook” to get everyone on the same page to develop things like a clinical symposium, a networking event, and a refill protocol.

Stanley helped write the playbook, which has been updated several times. “It’s all of those best practices we have collected from across the country, all tucked into one book,” she said.
Ascension also adopted the Mayo Clinic’s Well-Being Index, an online assessment tool for health care workers that measures distress and is accessible via an app. Clinicians can use the app to answer a few questions about how they’re doing and feeling.
tems and initial forays into artificial intelligence applications. Hochman helped to form Truveta, a consortium of health systems aggregating medical data for use in research on disease prevention and treatment.
Under Hochman, Providence increased its investment in community benefit work. The system also established the Well Being Trust to address behavioral health and substance misuse and has made sizable investments in health equity work.
The system also has boosted its environmental stewardship work during Hochman’s tenure, including by making a pledge to be carbon neutral and by signing on to the White House Health Care Sector Climate Pledge.
During his time as Providence president and CEO, Hochman has served as board chair of CHA and of the American Hospital Association. Under his chairmanship, AHA
helped coordinate a unified response to the onset of the COVID pandemic.
In a Providence press release, AHA President and CEO Rick Pollack said Hochman’s “leadership in the health care sector has been nothing short of visionary.” CHA President and CEO Sr. Mary Haddad, RSM, said in the release that Hochman “has led the way in a changing world while always keeping the focus on the mission.” Last year, Hochman received CHA’s Sister Carol Keehan Award, which goes to individuals who excel in boldly championing society’s most vulnerable.
Separately, Truveta announced in May that Hochman is its new board of directors’ chair. Providence was a founding member of the health data collaborative, whose members also include CommonSpirit Health, Bon Secours Mercy Health and Trinity Health.
ADDRESSING PHYSICIANS’ WELL-BEING 78%

TRAGIC OUTCOMES
60% of physicians report for the third year in a row often having feelings of burnout, compared with 40% before the pandemic.
of physicians said there is stigma surrounding mental health and seeking mental health care among physicians.



PRESIDENTS/CEOS
Chicago-based CommonSpirit Health and CommonSpirit subsidiaries have made these changes:
48% of physicians said they know a physician/ colleague/ peer who said they would not seek mental health care.
More than half of physicians know of a physician who has ever considered, attempted or died by suicide, increasing in comparison to 2022 and 2021.
Only 31% of physicians agree that their workplace culture prioritizes physician well-being, declining from 36% a year ago.
Source: The Physicians Foundation’s 2023 Survey of America’s Current and Future Physicians
The app can show their results over time and connect them with resources.
Spotting issues
Shoemaker said data shows that if clinicians develop mental health issues, medical mistakes that result in harm can follow, and, at the extreme end, so can physician suicide. Tools like the Mayo Clinic’s wellbeing app can help leaders spot issues as they develop.
“If we want to live our mission and impact the health of our individuals in the communities we live in, we have to do it with a well clinician workforce,” Shoemaker said.
While individual answers remain anonymous, Ascension leaders can see overall results from the app and address concerns.
“For example, we identified that our newest clinicians were struggling, and so that really was the impetus for us to make an improved onboarding program,” said Stanley. “We take that feedback and can use it to direct things.”
In 2021, Ascension launched a peer support program to help clinicians after they’ve gone through a critical event, loss or another stressful situation like treating a mother who had gone into cardiac arrest after having a baby.
“Those sorts of things that happen really are emotionally difficult to process,” said Stanley. “This is an opportunity for those folks to connect with a peer, not to provide therapy or counseling, but to simply say, How are you? It’s really to just give them a space, it might be five minutes, it might be 30 minutes, it might be a phone call on Monday, and then another phone call on Thursday to check up. So it’s relatively informal.”
Ascension also looks for ways to help doctors work more efficiently and to reduce “pajama time” completing paperwork outside regular daytime hours. The health system has seen a correlation between increased pajama time hours and turnover, Shoemaker said.
“Can we go out and find those people, and then give them special education, and say, Hey, we’re noticing that you can do this, or you’re having trouble with this, let’s help,” he said.
Help can come in many forms, such as a template to document all the components of a well child exam or by showing physicians how to reduce keystrokes while typing in the electronic medical record.
Fostering growth
Providing professional growth opportunities, such as coaching, mentoring, and symposiums for women and clinicians from underrepresented groups, is also part of Ascension’s overall well-being efforts.
A program called Elevate helps clinicians become better leaders by sharpening their emotional intelligence and communication skills. Stanley helped plan that program, which consists of a yearlong session with monthly remote meetings. Senior leaders participate in the calls and rising leaders ask questions, letting everyone get to know one another, she said. The rising leaders end Elevate with a capstone project, which they present to senior leadership.
Stanley said several of the projects have led to systemwide programs. “And so the rest of the organization benefitted,” she said.
As Stanley explains to clinicians from all religious backgrounds, the well-being council’s efforts align with the mission of Ascension as a Catholic ministry “rooted in the loving ministry of Jesus as healer.”
“It doesn’t say as Jesus our savior. No one can deny that Jesus touched one person at a time and healed them, and that’s what we’re called to do,” said Stanley. “Whether I sit in an exam room with someone and simply be present while they tell me how difficult it is since her husband has passed away, whether I sit with a physician who’s struggling because she’s drowning in charting and can’t get home to her kids, I see how I can help. That’s what we do.” vhahn@chausa.org
Jeremy Bradshaw to market president for the Greater Salt Lake market, effective June 17. He will lead the five CommonSpirit Holy Cross hospitals in northern Utah and oversee CommonSpirit’s growth in that state. Previously he was CEO at St. Mark’s Hospital in Salt Lake, part of HCA’s MountainStar Healthcare. Andrew Gaasch to region president for the Mountain Region. He was CommonSpirit executive vice president and chief financial officer.
Anthony Houston to president of CommonSpirit’s Arizona market. He was market president of CommonSpirit’s CHI Saint Joseph Health in Lexington, Kentucky. Rodger Page to president of the north state market of Dignity Health, which is part of CommonSpirit. He also will continue as president of Dignity’s Mercy Medical Center–Mount Shasta and St. Elizabeth Community Hospital–Red Bluff. CommonSpirit created this new market leadership role as part of a statewide restructuring to better advance CommonSpirit’s organizational goals.
St. Louis-based Ascension and Ascension subsidiaries have made these changes:
Roddex “Rodd” Barlow to president, Via Christi St. Francis in Wichita, Kansas. He was senior vice president of operations for WellMed Networks’ El Paso and Southern New Mexico facilities. Barlow succeeds Joy Scott, who Ascension has promoted to market administrator for Wichita.
Don Damron, to president, Ascension St. Vincent Kokomo in Indiana, from regional chief operating officer for the Ascension St. Vincent North Region.
Marion Teixeira to president, Ascension St. Vincent Anderson in Indiana, from regional director of behavioral health for the Ascension St. Vincent North Region.
Jennifer Burrows to CEO of Providence Oregon, from CEO of Providence St. Vincent Medical Center in Portland, Oregon. She replaces William Olson, who is retiring. Robert “Bob” Honeycutt to president of CHRISTUS Santa Rosa Hospital — San Marcos in Texas. He was CEO of Saint Mary’s Regional Health System in Russellville, Arkansas.
Tauana McDonald to president and CEO of Mount Carmel Health System in Columbus, Ohio, effective July 1. She was president and chief operating officer of Mount Carmel Grove City in Ohio. She succeeds Lorraine Lutton, who is retiring.
PeaceHealth of Vancouver, Washington, and two of its facilities have made these changes: Cherelle Montanye to chief hospital executive at PeaceHealth Southwest Medical Center in Vancouver, from chief administrative officer of PeaceHealth St. John Medical Center in Longview, Washington. And Kendall Sawa to chief hospital executive of PeaceHealth St. John, from chief operating officer of Providence Portland Medical Center in Oregon. Valerie L. Powell-Stafford to president of Saint Francis Hospital of Hartford, Connecticut, part of Trinity Health. She was president and CEO of HCA Northside Hospital in St. Petersburg, Florida. In her new role, Powell-Stafford also will oversee Mount Sinai Rehabilitation Hospital in Hartford.
UP
KEEPING
Shoemaker
Stanley
Hochman
Houston McDonald Page
June 2024 CATHOLIC HEALTH WORLD 15

Honoring the fallen
A participant in Pittsburgh Mercy Intellectual & Developmental Disabilities Services programs holds flags as he assists staff member Stacy Fitzgerald with decorating veterans’ graves in the Civil War plot at Allegheny Cemetery in Pittsburgh. A group affiliated with Pittsburgh Mercy has volunteered for this community service for nearly a decade.
See more photos and social media posts from Catholic health systems and hospitals marking Memorial Day. chausa.org/chw
Chaplain relishes her healing vocation and invigorating avocations
By JULIE MINDA
Rosana Slezeviciute knew the moment she interviewed to become the chaplain of Mercy Medical Center Mount Shasta in Northern California that she’d found a place she could really call home.
As the sole chaplain at the rural mountain town’s only hospital since 2016, Slezeviciute has found a warm, interconnected community and a chance to engage with others intimately through her healing profession — all against the backdrop of one of the tallest peaks of California’s Cascade mountain range.
She’s also found plenty of outlets for her love of nature — and adventure. She’s a regular on the hiking and climbing routes around Mount Shasta and is a member of the community’s volunteer search and rescue team.
She says immersing herself in the small community and helping people through both her chaplain and mountain rescue roles have been rewarding. “I fell in love with Mount Shasta,” she says of the community.
Personal connection
Originally from a small village in Lithuania in Eastern Europe, Slezeviciute first lived in Boston and San Francisco after arriving in the U.S. in 1999. In both, she’d longed to live in a smaller community, where she could really feel a connection with others.
“I chose Mount Shasta because of the people,” says Slezeviciute. “When I interviewed here, I saw that everyone was so friendly. And then once I accepted the job and moved here, I’ve really enjoyed getting to know people at the hospital and at my church.”
And, she says serving at a small hospital, “I get to spend more time with patients (as compared to a big facility). I get to know the other people who work here. There is time to listen. I become part of their lives, and we get to know each other.”
The other main boon of living in this rural mountain town is the surroundings, she says. “It is like being in heaven here, it is so beautiful. We have the mountains, the lakes, the forest. Around here we love hiking, and skiing and climbing.”
The great outdoors
Seven years ago, she accepted an invitation to give back to the mountain community by joining the search and rescue team, a voluntary role. In monthly trainings, she’s learned how to assist with cave, river, mountain, lake and forest rescues. She’s learned to use snowmobiles and other rescue vehicles. She’s been trained in administering first aid, in navigating the vast Mount Shasta wilderness, and in survival techniques. She’s on a search and rescue team pager around the clock.
There are all kinds of situations that


she and her fellow search and rescue team members encounter, such as adventurers lost or injured in the back country, elderly people who have become disorientated and off course, people stuck in the snow. She knows how to dig a hole in the snow for shelter, to use ropes to immobilize a person during a rescue, to cross a mountain crevice with a ladder and to ration food for survival.
She’s aided in both rescues and recoveries. She’s joined in some families’ joy upon a loved one’s rescue. And she’s comforted families whose loved ones have not survived.
Slezeviciute says her most difficult search and rescue mission was to respond to California’s deadliest wildfire, the 2018 blaze in Paradise, which is about 150 miles south of Mount Shasta. That fire killed at least 85 people, covered 153,336 acres and destroyed more than 18,000 structures, including homes.
Slezeviciute’s team was among the numerous groups from around the region called in to help Paradise responders. Slezeviciute says it was devastating to search that ravaged community for survivors. “It was really hard emotionally,” she said. “There was so much sadness, grief and pain.”
For difficult rescue missions and for the many emotionally taxing days as a chaplain, she’s learned to draw on the strength of her circle of supporters, including friends and colleagues in Mount Shasta’s faith community.
Catholic renaissance
Even Mount Shasta, with its population of 3,000, is large compared with the Eastern European farming village where Slezeviciute was born and raised. Betygala, in central Lithuania, has a population of just several hundred people. Slezeviciute and her twin sister were the oldest of nine children on a family farm. Growing up in the 1970s and 1980s, Slezeviciute shouldered much of the work of tending animals — and her siblings — while her parents cared for her twin. That sister had medical conditions that kept her hospitalized much of her youth.
For much of Slezeviciute’s childhood, Lithuania was part of the Soviet Union, whose leadership was intent on squelching Lithuanian pride and Catholic practice. But she witnessed a passionate defense of Christianity among members of her community. Some risked imprisonment and death erecting mass displays of crosses, for instance. She gravitated to her grandparents’ own furtive practice of Catholicism, internally embracing the faith. So, when the Soviet Union dissolved in 1990, and Lithuania became the first Soviet republic to declare its independence, Slezeviciute was eager to take part in the Catholic renaissance that followed.
Initially interested in becoming a religion teacher, she took a leap of faith and accepted a scholarship in 1999 to study at Boston College. Slezeviciute says life in the huge U.S. city was a culture shock with throngs of people everywhere, grocery and retail stores packed with limitless options, and restaurants of every type close by.
New calling
Returning to Lithuania after her studies, Slezeviciute found herself consumed with learning how to use spiritual practices to comfort her ailing twin, who had carcinoma. On the advice of a priest she knew, Slezeviciute decided to pursue clinical pastoral education in the U.S. She earned a graduate degree in San Francisco and in 2008, during her second year of studies, she accepted a chaplain position at Seton Med-
ical Center in Daly City, California, outside San Francisco.
While she knew she’d found the career she was meant to have, the setting of that first position was not ideal for her. At the large urban medical center, it was hard to get to know staff and patients individually.
The facility where Slezeviciute served was part of the Daughters of Charity Health System of Los Altos Hills, which was bought by a private investment firm in 2016. Her position was eliminated in 2015 in the leadup to the divestiture.
During her interview for the chaplain position at Mercy Medical Center Mount Shasta, a CommonSpirit Health facility, she was enamored by the welcoming community. And during the eight years she’s worked there, she’s built a close circle of friends at the critical access hospital, at her church and in the community.
Slezeviciute says the Mount Shasta community feels like a family. In her role as chaplain, she says she greatly appreciates that she knows most of her colleagues and patients by name. She knows their families. She knows their struggles.
Lasting impact
Slezeviciute laughs that one of the few downsides of being a chaplain in such a small community is that everyone knows you, and so you must be on your best behavior. There’s no cutting people off in traffic and no driving on snow-covered mountain roads without the legally mandated snow tire chains.
She says her favorite aspect of her role is to comfort the many people who turn to the hospital for care, whatever their faith background. She says that even for people who have no faith or who are angry with the church, she hopes that the kindness and love she shows them opens their minds to faith.
“I am so proud to be in Catholic health care because I’ve always stuck to the phrase that the best way to live your faith is to practice it,” she says. jminda@chausa.org
Rosana Slezeviciute, the chaplain at Mercy Medical Center Mount Shasta in Northern California, summits Mount Shasta.
Slezeviciute rides in a helicopter. She was with fellow search and rescue team members.
16 CATHOLIC HEALTH WORLD June 2024
 By JULIE MINDA
By JULIE MINDA






















 Rachelle Barina, 36 Chief mission officer, Hospital Sisters
Rachelle Barina, 36 Chief mission officer, Hospital Sisters














 By VALERIE SCHREMP HAHN
By VALERIE SCHREMP HAHN


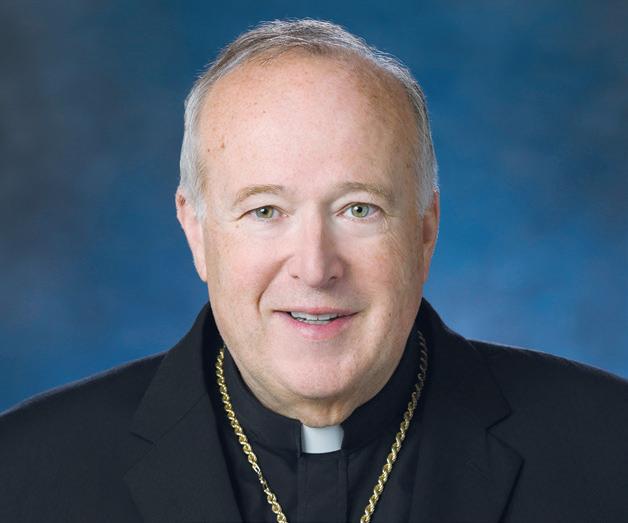




 By LORI ROSE
By LORI ROSE