Retiring FMOLHS head reflects on 40 years in health care practice, leadership
By JULIE MINDA
When Dr. Richard Vath retires this summer as president and CEO of Franciscan Missionaries of Our Lady Health System in Baton Rouge, Louisiana, he will cap off a career spanning 40 years.

Vath had practiced in Baton Rouge for 23 years as a pulmonary critical care physician before joining the leadership team of FMOLHS’ Our Lady of the Lake Regional Medical Center in 2006 as quality and patient safety medical director. In 2019, Vath was named president and CEO of FMOLHS, which has five hospital campuses and a network of outpatient sites in Louisiana and Mississippi. Beginning May 1, E.J. Kuiper transitions to system president and CEO.
During his tenure as CEO, Vath helped set a long-term vision for FMOLHS and spearheaded its expansion in Mississippi
Despite backlash, DEI leaders say Catholic health systems remain committed
By LISA EISENHAUER
Leaders of diversity, equity and inclusion initiatives across the Catholic health care ministry say a conservative backlash against such efforts isn’t shaking their systems’ resolve.
“I am proud that, in the face of external pressure, in the face of DEI being hijacked and sort of redefined as something negative and harmful, we have not been moved,” says LaRonda Chastang, senior vice president of diversity, equity and inclusion at Trinity Health.
At Bon Secours Mercy Health, Odesa Stapleton, chief diversity and inclusion officer, says the system is unwavering in its “culture of inclusion” that, as at other systems, extends into training and education, recruitment and retention, equity in care, community partnerships and supplier diversity.
Marcos Pesquera, system vice president for community health and chief diversity officer, says of CHRISTUS Health’s DEI
“Ten years ago, a hospital was a safe space, a sacred space, better yet, like a school or church and you didn’t have to think about security to the level that we do today. Unfortunately, societal violence has changed.” — Todd Miller

How to reduce violence in the workplace?
By VALERIE SCHREMP HAHN BRIDGETON, Missouri
Before SSM Health behavioral health nurse April Reitz joined her colleagues on a training mat to practice self-defense techniques, she smoothed a piece of red-orange painter’s tape onto her right jawline. The tape signaled to her group to avoid touching her there. Last year, a patient punched her in the face, dislocating her jaw, and she was still recovering.
Before the attack, Reitz said, “I never dreaded going to work.” Now she does.
“But yet, I still feel a calling in my life, and I feel like God equips you to what he calls you to,” she said. “And this is
Mercy Cedar Rapids partners on hub for dementia

care innovation
By JULIE MINDA
CEDAR RAPIDS, Iowa — Four years ago, Susie Winkowski and her husband, Walt, left the resort they’d owned on the West Coast because his dementia was making it too difficult to keep up with the business. They moved to Cedar Rapids to be closer to family. Susie Winkowski felt overwhelmed and under-equipped for her caregiving role, until she learned about the Family Caregivers Center here. Since connecting with the center, she’s been taking part in caregiver support groups, building deep friendships with other caregivers and their spouses and learning how she and her husband can achieve the best quality of life even given his diagnosis.
The Winkowskis are among the dozens of people with dementia or caregivers who are benefiting from the offerings of the Family Caregivers Center and its new sister
First 1,000 Days program 3 Executive changes 16 Nurse honor guards 2 PERIODICAL RATE PUBLICATION MAY 2024 VOLUME 40, NUMBER 5 Continued on 8 Continued on 10 Continued on 15 Continued on 12 SSM Health opens security academies to teach employees
Security officer Eric Visor shows nurse Brittany Drummond a self-defense technique at the SSM Health Security Academy in suburban St. Louis.
Facilitators and participants in a support group for people living with dementia gather in the vestibule of the Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia in Cedar Rapids, Iowa. The center offers numerous support groups for people with dementia, their caregivers and older adults.
Josh Booth /Diamond Label Films
Jerry Naunheim/@CHA
Vath




common good in their local communities.
As members of honor guard, CHRISTUS Health nurses pay tribute to nurses who have died
By JULIE MINDA
Some nurses have found a unique way of honoring the legacy of their nurse colleagues who have died. They’ve established honor guard units that perform ceremonies at funerals or memorial services. Nurses at three CHRISTUS Health hospitals have established or are in the process of establishing such units.

“It is very emotional for the families and nurses who attend the service,” says Anitha Sanderson, chief nursing officer at CHRISTUS Mother Frances Hospital — Sulphur Springs in Texas, and one of the “founding mothers” who helped establish the Northeast Texas Nurse Honor Guard in February 2023. “To get to know these nurses and their experiences and contributions to the profession has been amazing — and an honor.”
Sanderson and five other CHRISTUS Health Mother Frances nurses started the unit after learning of the concept from CHRISTUS Southeast Texas — St. Elizabeth in Beaumont. CHRISTUS St. Michael Health System in Texarkana, Texas, is developing its program now. The three CHRISTUS facilities are sharing information and resources about how to establish and maintain an honor guard.
A lamp, a rose, a card
The honor guard can pay tribute to any deceased nurse, not just those who had worked at CHRISTUS.
When the honor guard is enlisted to hold a ceremony at a nurse’s funeral, three or more members participate. One member carries a lit lamp, another carries a white rose and sympathy card and a third carries a triangle musical instrument. The nurse with the lamp leads the procession. Then all honor guard members read the Florence Nightingale tribute, which is a poem titled “She Was There.” Nightingale is regarded as the founder of modern nursing.
After the recitation, a unit member reads aloud a description of the nursing career of the deceased. Afterward, one nurse extinguishes the lamp and another gives the card
“To get to know these nurses and their experiences and contributions to the profession has been amazing — and an honor.”
Anitha Sanderson
—

New Mercy site
The Missouri-based system will build a $650 million, 75-bed hospital and outpatient care center in Wentzville in Eastern Missouri.

PeaceHealth hub
An expansion at the PeaceHealth Southwest Medical Center Emergency Department in Vancouver, Washington, will house a Community Health Hub.



American Hospital AssociationInstitute for Diversity and Health Equity (IFDHE) ApolloMD
Aquinas Institute of Theology Care Continuity
EWTN Global Catholic Network Health Trust Performance Group
Huron Institute of Reproductive Grief Care
Key Green Solutions
Loyola University Chicago Bioethics Institute
SafePoint by SoundThinking ShiftMed
to one of the deceased’s loved ones and places the rose atop the deceased’s coffin or by the person’s urn. Then another honor guard member rings the triangle and says the name of the deceased nurse three times.
Sanderson says this final roll call “is similar to the final roll call done at a military service and does not leave a dry eye in the house.”
She says the unit has conducted more than a half dozen ceremonies. Loved ones of the honored nurses have expressed much gratitude and given donations to the honor guard so that other nurses can be celebrated.
Growing presence
The CHRISTUS honor guard units are among the 250-plus groups nationwide that have launched with the help of the National Nurse Honor Guard. That group was inspired by the efforts of an honor guard established by the Kansas State Nurses Association as well as by honor guard ceremonies conducted by nurses in Detroit. The National Nurse Honor Guard began in 2011. Some nurses have set up state bodies. The three CHRISTUS-initiated units are part of the Texas State Nurse Honor Guard.
To set up and recruit members for the Northeast Texas unit, the six Mother Frances Hospital nurses who volunteered to be founding mothers used resources from St. Elizabeth to create a private Facebook group. Then they spread the word to nurses throughout Northeast Texas.
So far, the founding mothers have welcomed nearly three dozen nurses into the Northeast Texas unit. Active and retired nurses can be members. They do not have to be employed by CHRISTUS to join the honor guard. Those who join do so on a voluntary and unpaid basis.
The unit provides resources to the members so that they may learn how to perform the ceremony. Members purchase their own all-white nursing uniforms, which include scrubs, caps, shoes and socks. The state honor guard supplies blue capes for each ceremony. Mother Frances provides the other supplies.
Sacrificial service
The Northeast Texas group’s founding mothers have built awareness of their group with funeral homes and nursing homes and similar providers in an 11-county area in northeast Texas. When those providers become aware that a nurse has died, they tell the surviving family members about the honor guard and the ceremonial services they can provide. They connect interested families with the unit.
The unit members meet periodically to practice the ceremonies, and then once they are called upon to perform a tribute at a nurse’s funeral, they meet just before the service to establish their roles and prepare.
Sanderson says as participants in these memorial services, the unit’s members have learned about the legacies of those they are honoring. One of the nurses they celebrated had to temporarily abandon her dream to be nurse and instead build planes in California during World War II. After the war, she was able to resume her education and then pursue her nursing career. Another nurse the unit honored had been head nurse at Parkland Memorial Hospital in Dallas on Nov. 22, 1963, when John F. Kennedy was brought in after being shot.

Kari Froneberger is director of quality/ infection prevention, risk management, safety and accreditation for Mother Frances in Sulphur Springs and for CHRISTUS Mother Frances Hospital — Winnsboro. She is an honor guard founding mother. She says even though she and the other guard members may never have met the nurses they honor, they are able to connect with them.
“These nurses have spent their entire life devoted to the service of others — to making others comfortable, happy and healthy,” she says. “It’s very meaningful for us … and touching to be able to honor their selflessness and sacrifice.”
To read the poem “She Was There,” visit chausa.org/chw. jminda@chausa.org
Contact Madeline Hantak at mhantak@chausa.org for information about underwriting.
POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@ chausa.org. Periodicals postage rate is paid at St. Louis and additional mailing offices. Annual subscription rates: CHA members free, others $29 and foreign $29.
Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA. Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
Vice President Communications and Marketing Brian P. Reardon
Editor Lisa Eisenhauer leisenhauer@chausa.org 314-253-3437
Associate Editor Julie Minda jminda@chausa.org 314-253-3412
We Will
© Catholic Health Association of the United States, May 2024 Catholic Health World (ISSN 87564068) is published monthly and copyrighted © by the Catholic Health Association of the United States.
Associate Editor Valerie Schremp Hahn vhahn@chausa.org 314-253-3410
Graphic Design Norma Klingsick
Advertising ads@chausa.org 314-253-3477
Empower Bold Change
SM FIND MORE CHA RESOURCES ONLINE chausa.org Our ministry is an enduring sign of health care rooted in the belief that every person is a treasure, every life a sacred gift, every human being a unity of body, mind and spirit. This vibrant video series shines a spotlight on the contributions of CHA member ministries in promoting human dignity and the common good. CHAUSA.ORG/CATHOLICHEALTH
to Elevate Human Flourishing.
the work of CHA members in advancing human dignity and the
Video series This is Catholic Health Care celebrates
Members of the Northeast Texas Nurse Honor Guard conduct a tribute ceremony for nurse Amanda Turley, who had worked in the nursery at CHRISTUS St. Michael Hospital in Texarkana, Texas. The honor guard members are, from left, Cassidy Cameron, Sarah Mills, Kari Froneberger and Anitha Sanderson. The ceremony took place in January at St. Michael.
Sanderson
Froneberger
2 CATHOLIC HEALTH WORLD May 2024
Intermountain Health’s First 1,000 Days helps families, babies navigate first years
By VALERIE SCHREMP HAHN
Lacey Starcevich was 19 years old when she showed up at the emergency room at St. James Hospital in Butte, Montana, with a bladder infection. She didn’t have a home, she was addicted to drugs, she was severely underweight, and, as she eventually found out, she was 11 weeks pregnant.

She felt like her world was crashing down around her. At her first appointment with an obstetrician, social worker Joslin Hubbard came in to talk to her.
“She was very caring and sweet and she made me feel not judged,” said Starcevich. “Not one ounce of me wanted to be in that room. And she just made me feel like I was welcomed, like I needed to be there.”
Hubbard explained to her the importance of the first 1,000 days of a mother and baby’s life, and that there was hope and help for her and her baby.
Hubbard helped start the First 1,000 Days program at St. James in southwestern Montana, part of Intermountain Health. The program seeks to screen pregnant patients and connect them to the help they may need and follow them through their pregnancy and the first two years of their child’s life. The program name comes from the length of a typical pregnancy (270 days) plus the first two years of the baby’s life (365 days plus 365 days).
“This first 1,000 days is a critical and crucial time in human development,” said Hubbard in an interview with Catholic Health World. “It’s a great time for you to be able to set up your child for success later in life. We tried to come at it as a positive — which it is. It’s an opportunity in positivity, or a positive chance to impact life.”
The program started in 2018 when the hospital got a grant from the Montana Healthcare Foundation to provide care coordination to help support social determinants of health, specifically ones around

substance use and mental health needs.
Intermountain Health runs a similar program out of the midwifery clinic at St. Vincent Regional Hospital in Billings, Montana, and is working to get a program off the ground at Holy Rosary Hospital in Miles City, Montana.
Hubbard, who now works as an ER navigator for St. James, helped get First 1,000 Days rolling while she was an OB care coordinator.
In February, Hubbard and Starcevich joined April Ennis Keippel, Intermountain Health director of community health, and Jana Distefano, director of community health for Professional Research Consultants, in describing the First 1,000 Days program on a panel. The panel was at the American Hospital Association’s Rural


“ This first
1,000 days is a critical and crucial time in human development.
It’s
a great time for you to be able to set up your child for success later
in life.”
— Joslin Hubbard
Lacey Starcevich, her husband Jim, and their sons Raiden, 4, and Parker, 2, live in Butte, Montana. Lacey Starcevich credits the First 1,000 Days program at St. James Hospital with saving her life and helping her start her family.
Health Care Leadership Conference in Orlando.
Fighting against adversity
Butte is a mining community. In its heyday, it was the largest city between Chicago and San Francisco. “People from all over the world came to work in the copper mines,” said Keippel. “It was known as the richest hill on earth.”

But it was dangerous work, and a “live for today” attitude has prevailed through the generations, she said.
In a 2023 community health survey, more than 42% of women in Butte-Silver Bow County, where most residents are white, reported symptoms of chronic depression. Nearly half of all surveyed were low income. Nearly half of women reported their life has been negatively affected by substance abuse, either their own or somebody else’s. Many of the women in crisis were of childbearing age.
Compared to other states, Montana has the third highest percentage of children who have experienced two or more adverse childhood experiences, such as living with someone with an alcohol or drug problem and being a victim or witness of neighborhood violence.
patient, addressing and discussing issues behind the answers.
If a woman misses prenatal appointments, it may not be because she doesn’t care, it may simply be because she doesn’t have a way to get there, said Hubbard.
If a woman pregnant with her second child reports she experienced postpartum depression after her first, care coordinators with the program may be in touch with her more often after she has her second baby to look for signs of trouble.
It isn’t always obvious who needs help.
“We would have labor and delivery nurses that we would screen, and they would say, ‘You know, I think I had postpartum depression with my first baby. This is my second, but I was too scared to say anything. I wasn’t sure,’” said Hubbard.
Expectant mothers who had previous miscarriages or infertility issues also might need help because if they do experience depression and anxiety, they might be afraid to tell anyone because they worked hard to achieve this pregnancy, said Hubbard.
How often the care coordinator or care providers follow up with the women depends on the need.
Tools for success
Starcevich didn’t have insurance when she found out she was pregnant, so Hubbard helped her enroll in Medicaid, an outpatient drug treatment program, and a nurse-family partnership so that she could get regular care. She got clean within a week and moved into her boyfriend’s parents’ home.
She said Hubbard “gave me all the tools to set me up for success.”
Her son, Raiden, is now 4 years old. She and her boyfriend, Jim, got married, and they have a second son, Parker, who is 2. They both have jobs and a home, and life is good. They are teaching Raiden how to snowboard. And, as she told the attendees at the panel at the conference in Orlando, she still texts Hubbard for support.
The First 1,000 Days program, Starcevich said, saved her life.
“It not only saved me and Raiden, it helped me create the family I have today,” she said.
MEDICATION ASSISTED TREATMENT PROVIDERS
“If you don’t have a way to intervene, that cycle continues multiple generations over,” said Keippel. “I think that’s what we’ve seen in the Butte community. So the First 1,000 Days project is really a way to intervene, where you can kind of break that cycle, and be able to provide the change or resources to change. For some people, I think, if you’ve never known anything else, how would you envision a different world for yourself?”
How the program works
The idea of the First 1,000 Days program is to connect pregnant patients with resources that they didn’t know were available and that caregivers might not have known the patients needed. Care coordinators work directly with the patients, and others with the hospital work with community partners to coordinate care and try to address issues.
When patients are in the waiting room, they are given a questionnaire that asks about their home life, whether they have adequate housing and transportation, are feeling symptoms of prenatal depression, or if they are experiencing domestic violence. A nurse collects the questionnaire when the patient comes into the exam room, and the care coordinator goes through it with the
There are other successes: St. James Hospital has seen fewer babies born with a positive neonatal drug screen, a large increase in mothers who have received adequate prenatal care, and a smaller percentage of newborns removed by child protective services. In some cases where a newborn cannot live with the mother, the outcome may not be as traumatic when the mother gets help from the First 1,000 Days program because the care coordinators have discussed the options with the mother during her pregnancy. The mother may have arranged for an open adoption or otherwise been more involved in making the decisions, said Hubbard.
Keippel said the program’s focus on helping the poor and vulnerable aligns with the system’s mission.
“Intermountain’s mission is really about helping people to live their healthiest lives possible,” she said. “But for Catholic care sites, ours is really about revealing and fostering God’s healing love. I just think this is a great example.”
Hubbard urges any system that would like to start a similar program to start small, even by screening a small category of patients and families. And she said providers should remember that these women want to do well and want to love their babies in a way they may have never been loved themselves.
“As an organization, we can’t solve everyone’s issues, but we can give them compassion and empathy and understanding and love,” she said. “And those are sometimes the greatest gifts that we can give individuals.”
vhahn@chausa.org
Source: Montana Healthcare Foundation How
PRENATAL CARE PROVIDERS PEER RECOVERY COACHES CHILD AND FAMILY SERVICES CARE COORDINATOR SOCIAL SERVICE PROVIDERS HOUSING AND OTHER AGENCIES PUBLIC HEALTH DEPARTMENTS CARE COORDINATOR
HOME
the First 1,000 Days program works
BEHAVIORAL HEALTH PROVIDERS
VISITING PROGRAMS
Hubbard
May 2024 CATHOLIC HEALTH WORLD 3
Keippel
SSM Health looks to the sun as it works toward climate goals
By KATHLEEN NELSON
The most recent example of SSM Health’s commitment to environmental sustainability can be found in a field in Centralia, Illinois. The field contains an array of solar panels, which will supply energy to SSM Health St. Mary’s Hospital.
The collection of solar panels went online in November and is the first of several that SSM Health envisions in the four states it serves. The system plans to bring an array online at SSM Health Good Samaritan Hospital in Mount Vernon, Illinois, this year.
The solar projects are one facet of SSM Health’s commitment to the White House’s climate pledge for health care organizations to become carbon-neutral by 2050. Other projects focused on environmental sustainability include reducing the use of plastic water bottles, diverting hundreds of tons of surgical waste from landfills, and investing in solar energy financing funds and water infrastructure funds that are focused on environmental sustainability.

To learn more about the solar projects and SSM Health’s plans to fulfill the climate pledge, Catholic Health World talked to Gerry Kaiser, SSM Health’s vice president of facilities and real estate.
Why take the health care pledge to be carbon neutral by 2050?
We wanted to show our commitment to joining others in addressing the carbon footprint issue. It helps bring awareness both in and outside the system as we’re tracking and looking at our progress in reducing our footprint. And, reducing our carbon footprint and the impact on the environment aligns with the mission and values of SSM. It’s part of who we are.
Why are solar arrays part of the first phase of your strategy?
Solar arrays help reduce Scope 2 emissions, which is energy you purchase. The primary purchases for most systems are natural gas and electricity. We also have to look at how that electricity is produced: Is it produced by nuclear energy, coal fire, natural gas? So, we can reduce emissions if we can get as much energy as possible from clean sources, like solar.
Why start the initiative in Illinois?
Of the four states we operate in, Illinois is most favorable for solar because of incen-

So it was a natural place to start.
How much of the electricity that the hospital uses does the solar array provide?
It’s about 20%. We try to size it for what we call the baseload for what the hospital needs. The load varies day to day and season to season. You’re limited based on how much ground you’ve got, but we have a second phase at Centralia that we’re looking at. We’ve got some more land that we could put to use.
Can you provide an update on the array at SSM Health Good Samaritan Hospital in Mount Vernon?
We have materials on-site for the first phase at Mount Vernon. We expect Mount Vernon to be online later this year, probably in the fall.
What is the strategy and timetable in your other states: Missouri, Oklahoma and Wisconsin?
In Missouri, the electric utility, Ameren, is developing solar arrays themselves. Ameren approached a number of larger users and asked them to subscribe to the solar farm they are building. We’ve subscribed to their first phase farm, which is expected to go online in 2025, and is expected to pick up 17% of our usage in the St. Louis area. They also are planning a phase two. We’ll subscribe and take more power from them.
One of the other things we’re exploring is participating in the Inflation Reduction Act, which allows nonprofits to receive direct payments in lieu of tax credits for renewable energy. We’re in the development process of projects in Oklahoma and Wisconsin that we hope to have reimbursed by IRA.
Taken as a group, how much could solar energy eventually reduce the sys-
tem’s carbon footprint?
Under current technology, we’d hope to get 40% to 50%. If Ameren keeps building, we’ll keep buying. There are other opportunities that could be on the table, such as community-produced solar. At this point, I’d say 10 years is a good time frame for reaching that goal.
Can you give details on other projects that can help meet the goal of being carbon-neutral by 2050?
We’ve adopted guidelines to design new facilities to meet WELL building certification, in lieu of LEED (Leadership in Energy and Environmental Design). The standards are similar, but WELL building emphasizes ongoing operation and the interior design, and how they affect people working inside the building, more than how you build it, which LEED does. As we design new projects, we’re looking to incorporate ways to convert out of fossil fuel consumption to electric, in the belief that we can get more clean electric power in the future.
We’ve been involved in a number of tree planting efforts over the years. CEO Laura Kaiser asked that we plant thousands of trees across our system over the last few years. And we’re involved in a community effort called Forest ReLeaf to plant trees in St. Louis. We’re looking for similar organizations in the other regions.
What are the pie-in-the-sky goals or benchmarks along the way that you want to hit every 10 or 15 years?
We brought on Adam Walker as a sustainability manager for the system last year. He’s working to establish the strategy: what we want to achieve, when we want to achieve it and most importantly, how we’re going to achieve it.
St. Luke’s in Houston joins call for collaborative response to climate change
St. Luke’s Health is among the funders of a new report that warns about the health impacts of climate change on the system’s home turf of Houston. The report offers a series of recommendations to address the threat.
“Houston’s Future: The Intersection of Climate Change and Health Care” was released April 10 by the nonprofit Center for Houston’s Future, which St. Luke’s co-sponsors. The report notes that south Texas faces significant risks as the planet warms from extreme heat, floods and hurricanes. It points to escalating related-health effects, such as more incidences of heatstroke, respiratory illnesses and mosquito-borne illnesses.
The report points out that the health care sector has a dual role in climate change as a major source of the greenhouse gas emissions linked to global warming and the provider of treatment for climate change’s health impacts.
“Urgent action to mitigate climate change and address the disparate economic impact of climate change on historically underserved communities is crucial to safeguard Houston’s residents and build a healthier future for all,” the report says.
The report’s recommendations for Houston’s health care providers include partnering to share strategies, developing protocols to identify and address climate-related health concerns, and leadership in calling for climate action.
“As part of CommonSpirit Health, the nation’s largest nonprofit health care system, St. Luke’s Health recognizes that we play a large role in creating and investing in healthier, more equitable communities where we live, work, learn and pray,” Doug Lawson, St. Luke’s CEO and president of CommonSpirit Health’s South Region, said in a release about the report. “We are pleased to fund the center’s report that highlights the vital role of collaboration as we work toward sustainable, resilient, climate-smart health care.”
Avera to invest $245 million in construction at two Sioux Falls, South Dakota, campuses
Avera Health plans to undertake $245 million in construction at two campuses in Sioux Falls, South Dakota, in order to expand women’s, children’s, digestive health, orthopedic, surgery, cancer care and other services. This is the largest building project in the health system’s history and the largest expansion of hospital space in Sioux Falls’ history.
By early 2027, Avera plans to erect a sixstory tower at its flagship medical center, Avera McKennan Hospital & University Health Center. This tower will create a new main entrance for the facility and will establish a focused area for women’s and children’s services. The building project will add 158 beds, bringing the medical center’s capacity to 802 beds.
In a press release, Avera McKennan Hospital & University Health Center Regional President and CEO Dr. Ronald Place notes that Avera has been steadily expanding its pediatric program over the past 20 years. He says the new tower will allow for Avera to have the “modern and expanded facili-

a department of Avera McKennan, offering specialty care and other clinical services. At that campus, Avera will add a threestory building for digestive health services. When those clinicians move to the new building, Avera will use the vacated space for an expansion of orthopedic services. That campus construction is expected to be complete in 2026.
According to the release, the projects will help accommodate increased demand for health services as Sioux Falls’ population has grown. That growth is projected to continue.
It is estimated the population of the Sioux Falls metropolitan statistical area will increase by more than 100,000 people in the next 15 years. The current population is more than 200,000.
Avera expects to begin construction at both campuses this summer.
Avera has 37 hospitals and a network of additional sites serving South Dakota and surrounding areas of Minnesota, Iowa, Nebraska and North Dakota.
A field of solar panels next to SSM Health St. Mary’s Hospital in Centralia, Illinois, is expected to produce 327,641 kilowatts of energy in its first year. That’s enough to power about 31 homes for a year. tives.
Kaiser
ties to complement the compassionate and excellent care our
women
The
4 CATHOLIC HEALTH WORLD May 2024
At an event announcing Avera Health construction plans, Avera McKennan Hospital & University Health Center Regional President and CEO Dr. Ronald Place explains the building project to employees. The project, which will take place on two Sioux Falls, South Dakota, campuses, is to cost about $245 million.
teams provide” for
and children.
Avera on Louise Health Campus is
A new STAR: Essentia Health joins clinical research network
By KARI WILLIAMS
Patients at Essentia Health now have a say in what the health system’s researchers study.
Earlier this year, the Minnesota-based system became part of the Stakeholders, Technology and Research (STAR) Clinical Research Network alongside Stanford University. It’s one of 10 health systems in the partnership.
STAR CRN, a member of the National Patient-Centered Clinical Research Network, has data on more than 15 million patients and involves patients in the research process.
“Through this network, we have access to a broad array of clinical data, informatics tools, patients, providers, and systems to address an array of research questions,” the STAR CRN website notes. “The objective of our CRN is to robustly support comparative effectiveness studies, pragmatic clinical trials, health system innovation, and the other research needs of our stakeholders and partners.”
Dr. Catherine Benziger, a cardiologist at Essentia, said an important aspect of the network’s research is that it is patientdriven and patient-focused.

“Rather than research just being done in ivory towers and urban areas, (STAR CRN is) linking researchers in those settings with large health systems and then also really prioritizing research that patients want to do,” she said. “And it’s doing research differently in that in every stage of every research application, a patient or patient partner … has to be involved in that process of designing the research. It’s not just a bunch of Ph.D.s and M.D.s designing the research.”








Stakeholders, Technology, and Research CRN


specialty groups, as well as our population health and our nursing informatics.”
Waring said what makes Essentia’s inclusion special is that the network is the “star consortium” of clinical research networks and Essentia is the only partner that is not an academic medical center.
Essentia competed against other large health systems such as the University of Minnesota to join the network. Part of the reason for Essentia’s inclusion was its clinical research program.
Waring said Essentia strengthens the network in part because the system serves a large rural area that spans northern Minnesota, northwestern Wisconsin and North Dakota.
In each project, patients act as experts because they’re the ones Benziger said researchers want to recruit and enroll.
“I’ve learned so much from the patient partners, and I think it’s really important that we include patients in all of our other studies as well because of the experience that’s been so positive as part of doing research with this network,” Benziger said.
Mike Sylvester, Essentia’s patient partner, was treated at the hospital system’s heart and vascular center. He has had six heart and vascular surgeries since 2016. He has suffered a stroke that initially left him blind, paralyzed and unable to speak; has battled a heart valve disease; and undergoes care for epilepsy.

Equal player
When a health system and health providers participate in research, Benziger said patients, by default, receive a better level of care.
“We know people, even in placebo groups, do better than people in usual care,” Benziger said. “And so I think it’s really important that we continue to offer research in order to be able to provide our patients with the highest level of care. Furthermore, as an investigator who does a lot of research, I am constantly going to meetings and getting updates on what’s kind of the latest and greatest in terms of medical treatments for cardiac conditions.”

Essentia has a co-principal investigator model with Benziger and Dr. Stephen Waring, principal scientist at the Essentia Institute of Rural Health, at the helm. The institute is Essentia’s research center. It offers patients participation in dozens of studies. Essentia includes 14 Catholic hospitals, which take part in the research.
Also part of Essentia’s STAR CRN team are two research evaluation specialists, a patient partner and a stakeholder engagement lead.
“That is our core team,” Benziger said. “But then we are reaching out to a lot of our clinical groups, like primary care and sub-
“That alone is certainly challenging, but it also brings a different population, a rural population, where we know our Wisconsin rural is different than our North Dakota rural in some places,” Waring said, “and not just in terms of the health care access issues, but also just in terms of culture, which are really big factors in health care.”
Importance of the patient partner
The concept of including patients in the planning of research, according to Benziger, is novel and allows patients to bring topics to the medical professionals. “It totally flipped the research process on its head,” Benziger said.
She added that patient partners “are a critical and equal member of the research team. Every site has a patient partner on the leadership board, and then also patients who sit on the steering committee, and they have equal voting rights.”
“I was told on many occasions I probably shouldn’t even be alive,” Sylvester said.
Before becoming Essentia’s patient partner for STAR CRN, he already was serving on Essentia’s patient and family advisory council.
Because of his health history, Sylvester has a lot of experience with health care delivery. He uses his insights to help others, including through patient advocacy work. Some of that work is with the Alliance for Aging and Rock the Heart, a nonprofit that supports people who have aortic and heart valve disease.
Through Essentia’s involvement in the STAR CRN, Sylvester said he hopes people will be able to learn more about their health conditions so they can make better decisions about their care. “The whole idea of this is to, again, pay it forward for other people so they’ll have more information,” Sylvester said.
Every problem Essentia research looks at includes a patient perspective. No effort moves forward unless the patient partners “have signed off on this as being an important thing to do and an important approach to take,” Waring said.
The patient-focused approach, according to Waring, can uncover gaps in health care and better ways to address issues such as diabetes, depression, heart/vascular disease and mental health.
Benziger said she believes the collaboration with the STAR CRN puts Essentia on the map as an equal player in research.
“We have a lot of very skilled investigators as well as research scientists in our health system that are really bringing top care to our patients,” Benziger said. “And so I think it just is that seal of approval. I knew we were doing really good work, but it just really validates that the Essentia Institute of Rural Health is really a leader in clinical research nationally.”
Tornado damages, temporarily closes Mercy hospital in southern Oklahoma
By VALERIE SCHREMP HAHN
A tornado heavily damaged the 25-bed Mercy Health Love County hospital and clinic in Marietta, Oklahoma, just north of the Texas border.
The tornado hit the hospital late on April 27, a Saturday. Nobody in the building was hurt. Before the tornado hit, about 10 workers were able to move two patients from the emergency room and eight inpatients to storm shelters on the property. Within hours, the patients were transferred to other facilities.
“We are so grateful for our heroic coworkers who moved patients and visitors to safety before the storm hit,” Scott Callender, administrator of Mercy Health Love County, said in a statement. “We regularly train for severe weather, so our co-workers were ready and knew what to do.”
The hospital’s administrative section was “just decimated. Large parts of
the roof are gone,” said Mercy spokeswoman Meredith Huggins. She noted that nobody was in the administrative offices on that Saturday night.
The emergency room and the suite that houses the CT scanner also were heavily damaged, Huggins said, while many of the patient rooms were unscathed.
“We’re so thankful everybody was safe,” she said. “We had minimal people inside the facilities.”
The hospital and the clinic are closed for the foreseeable future. About 150 people work there, and Mercy administrators have offered assurance that the staffers will have employment in other facilities.
The nearest Mercy hospital is in Ardmore, Oklahoma, about 20 miles away. The hospitals are part of Chesterfield, Missouribased Mercy.
Mercy is working to establish a fund to help employees whose homes were destroyed or damaged. vhahn@chausa.org
 Benziger
Waring
Benziger
Waring
Vanderbilt University Medical Center Vanderbilt Health Affiliated Network Meharry Medical College Essentia Health Duke University School of Medicine University of North Carolina Health Care Wake Forest University School of Medicine Stanford University School of Medicine Mayo Clinic Health Sciences South Carolina STAR CRN sites
A tornado slammed Mercy Health Love County hospital and clinic in Marietta, Oklahoma, the night of April 27. Ten patients and about 10 workers inside the building were uninjured.
May 2024 CATHOLIC HEALTH WORLD 5

FROM THE MAIN STAGE
Keynote speakers:

AMY FINKELSTEIN
John and Jennie S.
MacDonald Professor of Economics at MIT
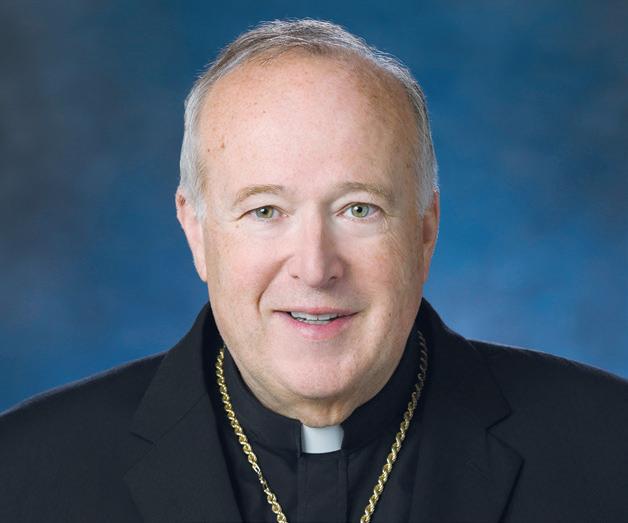
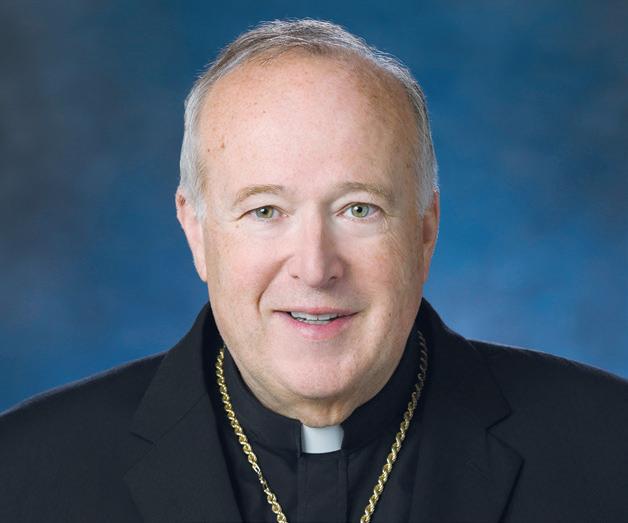
CARDINAL
ROBERT M C ELROY
Bishop of the Diocese of San Diego

TOM KOULOPOULOS
Author, Futurist and Leader
Catholic Health Care and American Culture Panel:

CATHLEEN
KAVENY, JD, PH.D.
Darald and Juliet Libby
Millennium Professor at Boston College

DR. CLAUDIA
RUIZ SOTOMAYOR, DBE, HEC - C
Chief, Ethics Consultation Service, and Clinical Ethicist, Pellegrino Center for Clinical Bioethics

MICHAEL SEAN WINTERS
Columnist, National Catholic Reporter, and Fellow, Center for Catholic Studies, Sacred Heart University
6 CATHOLIC HEALTH WORLD May 2024
JOIN THE CELEBRATION
Be sure to join us for the heartwarming ceremonies that spotlight our remarkable award winners and the amazing work happening in Catholic health care.
LIFETIME ACHIEVEMENT AWARD
For a lifetime of contributions
RON HAMEL, PH.D.
Past Member
SSM Health Ministries, St Louis, Missouri
Board of Directors
SSM Health, St Louis, Missouri
SISTER CAROL KEEHAN AWARD
For boldly championing society’s most vulnerable
DORI LESLIE
President
CHI Friendship, Fargo, North Dakota
2024’S ACHIEVEMENT CITATION AWARD WINNER
will be revealed at Assembly!
TOMORROW’S LEADERS
Honoring young people who will guide our ministry in the future
RACHELLE BARINA
Chief Mission Officer
Hospital Sisters Health System, Springfield, Illinois
CARRIE MEYER MCGRATH
System Director, Formation Design and Delivery
CommonSpirit Health, Chicago, Illinois
BRIDGET FITZPATRICK
Chief Operating Officer
Richmond Community Hospital, Bon Secours Mercy Health, Richmond, Virginia
CALEB TOWNES
Director of Consumer Patient Experience
Ascension Alabama, Birmingham, Alabama
SAM PROKOPEC
Executive Director
St. Joseph’s Elder Services, West Point, Nebraska
THOMAS KLEIN, FACHE
Chief Operating Officer
Ascension Medical Group Michigan, Warren, Michigan
SHEKINAH SINGLETERY
Director of Community Health & Well-Being
Trinity Health Ann Arbor and Livingston Hospitals, Livonia, Michigan
DAN WOODS, MSN, RN
Senior Director of Emergency Services and Hospital Throughput
St. Dominic-Jackson Memorial Hospital, Jackson, Mississippi
FAITH HALFORD
Systems Manager Materials Management St. Joseph’s/Candler Health System Savannah, Georgia
ZACH ZIRKELBACH
Chief Financial Officer
Ascension St. Vincent, Evansville, Indiana
MEGAN TIMM
Regional Director of Community Health
SSM Health St. Mary’s Hospital, Janesville, Wisconsin
HALEY BUSCH, PHARMD, BCPS
Quality Manager, Opioid Stewardship Program Coordinator
CHI Saint Joseph Health, Lexington, Kentucky
register today

CATHOLIC HEALTH CARE AND AMERICAN CULTURE SESSIONS
Our pre-Assembly materials include podcast recordings, articles, videos and more. Access the materials and join us for the virtual dialogue sessions on Thursdays in May from 1 to 1:45 p.m. ET.
March 1, 2022 CATHOLIC HEALTH WORLD 7 May

Clinicians and support staff stand in a circle to listen to live instructors and watch
self-defense and positioning techniques.
Security academy
From page 1
just a season I am working through — like, there’s a lot to be learned.”
Reitz and her colleagues gathered in March at the SSM Health Security Academy, part of a systemwide effort to improve security and reduce workplace violence in SSM Health facilities. The academy, housed in an office building near SSM Health DePaul Hospital in suburban St. Louis, opened in December 2022.
SSM Health, which has 23 hospitals in Missouri, Illinois, Wisconsin and Oklahoma, opened a similar academy in Madison, Wisconsin, in January. It plans to open another in late spring in Oklahoma City. Clinicians and security officers in Southern Illinois attend classes at the DePaul location.
An ongoing concern
Violence at health care sites is an ongo-


ing concern. A 2023 National Nurses United survey of 914 nurses said more than eight in 10 saw or experienced violence in the last year. More than 37% of the nurses said they have considered leaving their job due to violence, and nearly 25% had changed jobs or left the profession.
Earlier this year, CHA and other professional groups wrote a letter in support of national legislation, the Safety from Violence for Healthcare Employees (SAVE) Act, which would provide federal protections for health care workers who are victims of violence in the workplace.
Just four months before the security academy near DePaul Hospital opened in 2022, a patient at the hospital stabbed and seriously wounded a nurse and a paramedic.
“Ten years ago, a hospital was a safe space, a sacred space, better yet, like a school or church and you didn’t have to think about security to the level that we do today,” said Todd Miller, SSM Health’s system vice president of security. “Unfortunately, societal violence has changed. The expectations of people coming in have changed. And so we’re having to adjust to that.”

The academy is just one tool the system is using in response to workplace violence. Over the last two years, the system has added more weapon detection units, hired about 100 more security officers for nearly 500 total, and redesigned physical spaces to make them safer.
SSM Health says the efforts have been effective. Worker compensation cases related to workplace violence events dropped from 105 totaling $4 million in 2021 to 64 totaling $1.2 million through October 2023. In 2021, there were 413 reported “struck by patient” events across the system, 418 in 2022, and 326 in 2023.
The number of employee days away due to workplace violence has also decreased. They totaled 105 in 2021, 89 in 2022 and 82 in 2023.
Seeking the best outcome
Housing academies in a fixed large space allows leaders to bring in clinical and security team members to train together, which
instructional videos at the SSM Health Security Academy in suburban St. Louis. The padded mat was used to practice physical
April Reitz practices a chokehold on fellow nurse Jessica Wampler at a class at the SSM Health Security Academy. Reitz has a piece of painter’s tape on her jaw to signal where she was punched by a patient last year. She is still recovering.
Clinical partner Bria Burns, center, practices a self-defense technique with clinical partner Chaya Thomas as instructor Melisa Dare looks on at the SSM Health Security Academy in suburban St. Louis.
8 CATHOLIC HEALTH WORLD May 2024
Miller


is unique, said Aimee Anderer, director of the security academy near St. Louis.

“It was always clinical did their training and security did ours, but yet we go into a scene in a hospital room and we’re all working together,” she said. “Now, the right hand knows what the left hand is doing. We’re one unit.”
The academies include classroom space, a mock hospital room, a simulator where officers can train with actors on a screen, areas to practice with a Taser, a computer lab for report writing, and a large mat where security officers and clinicians can practice hands-on techniques.
The training varies depending on role and position. There are classes in report writing, trauma-informed care, selfdefense and team defensive tactics. All the security officers carry Tasers. They need extra training to carry firearms. When the academy opened, 18 officers in the St. Louis area were licensed to carry firearms. Now, 42 are.
The focus of the training is on everything that can be done before having to touch someone who is posing a threat, Miller said. “If we can verbally de-escalate, that’s the best outcome,” he said.
Security leaders with SSM Health teach security staff and clinicians and that helps build rapport, Miller said. “The more you train with somebody, the more comfortable you are when you’re in the real environment to work together successfully,” he said.
SSM Health uses curriculum from AVADE Workplace Violence Prevention, which its website says is “designed to educate, prevent and mitigate the risk of violence to workers in health care and private corporations.” The training covers proactive strategies to de-escalate and avoid issues to reduce risk of injury and prepares staff to be “ready, responsible and capable.” In addition to seeking to prevent harm to all parties in any interaction, SSM Health uses “trauma-informed response” to be alert to any previous incidents that may be contributing to the actions of a patient or visitor.
Training at the academy
On a recent visit to the academy, Crystal Campbell, a security officer at SSM Health Cardinal Glennon Children’s Hospital in St. Louis, ran through several scenarios on the simulator while Anderer watched. She attended to get certified to carry a weapon.
Campbell responded to scenarios projected on a wall. In one in the hallway of a back office, two men opened fire. In another, she encountered a disgruntled, suicidal employee who had been fired and refused to leave. In a third, a man upset with a high hospital bill stood in the lobby and threatened to hurt himself with a knife.

“
It was always clinical did their training and security did ours, but yet we go into a scene in a hospital room and we’re all working together. Now, the right hand knows what the left hand is doing. We’re one unit.”
— Aimee Anderer
She and Anderer then talked about how she handled each situation.
“I really appreciate you calling him ‘sir’ even though he’s trying to kill you,” Anderer said of the back-office scenario, in which Campbell shot the men who fired at her.
Campbell also ran through a scenario in the academy’s mock hospital room, where trainer Tom Whyte, a security supervisor at SSM Health St. Joseph Hospital in St. Charles, Missouri, played the role of a patient who refused to leave. He was hungry and didn’t have anywhere to go, he told Campbell.
“You can’t stay here, Mr. Johnson,” she said. “I can get some numbers for you. We can go back downstairs, and we can talk to the social worker. I can get you something to eat. But you have to get out of bed, and we have to go downstairs together.”
He refused, and after a couple minutes of discussion, he put a knife to his own neck. She asked him repeatedly to put the knife down, and then deployed a training Taser. He dropped the knife, and the scenario ended.
Anderer debriefed Campbell afterward on her techniques and Campbell passed.
Campbell has a background in corrections and has worked with SSM Health for two years. She has visited the academy several times for training. The staff is warm and welcoming, she said, and she feels supported as an employee.
“They teach you what to do, what to expect,” she said.
During another recent day at the academy, eight clinicians getting training on self-defense techniques first talked about defensive verbalization. Melisa Dare, an instructor who also works as a central intake assessor at DePaul Behavioral Health Urgent Care, had the group repeat “No!” “Stop!” “Get back!” and other phrases after her.
“Now, why do we do defensive verbalization?” she asked the group. “It creates witnesses. It establishes our authority. It keeps you breathing. When we get into fight, flight or freeze, that is where you are very apt to get tunnel vision. But by defensive verbalization you do keep yourself breathing and it fights off that tunnel vision. It may be used as a distraction. It alerts others of a confrontation. It provides direction to the aggressor. And it mitigates liability risks to both you and SSM.”
Over on the mats, Dare and security officer instructors Eric Visor and Marlos Woods used videos and hands-on instruction to show the group physical techniques: how to stand at a 45-degree angle to maintain balance and stability, how to move forward and backward, how to use distraction techniques, and how to push someone away.
Rhonda Childs, a regional ICU float nurse, said she appreciates that SSM Health provides the classes. “I think it’s pretty good that we are getting to take a class that shows us how to properly not only defend and protect ourselves, but also remain aware,” she said. “After 17 years, thank God I’ve never had to come in contact with anything like this, but this is still always good because you never know when it’s going to happen.” vhahn@chausa.org
IN BRIEF
HSHS hospitals receive Illinois grant for dialogue around equity Hospital Sisters Health System has received a Healing Illinois grant to foster discussion between central Illinois community members and health care professionals around equity in health care. Healing Illinois is an initiative from the Illinois Department of Human Services and the Field Foundation of Illinois. Statewide, 184 recipients will receive $4.5 million in funding for communitybased activities to advance racial healing. In Central Illinois, this grant is awarded by the United Way of Central Illinois. Earlier this year, HSHS received a Healing Illinois grant to support a speaker series in Southern Illinois.
The HSHS grant project is called “Revealing and Embodying Racial Healing for All People: Healing Central Illinois.” The goal is to foster in-person dialogue between community members and HSHS colleagues to advance racial healing.
The Healing Illinois grant project in Central Illinois will remember the 1908 Springfield Race Riots and the role of the Hospital Sisters at St. John’s Hospital in offering care for all people regardless of race. Invited HSHS colleagues and community members will participate in two daylong programs in the weeks leading up to Juneteenth.
Participating hospitals will include HSHS St. John’s Hospital in Springfield, HSHS St. Mary’s Hospital in Decatur, HSHS St. Anthony’s Memorial Hospital in Effingham, HSHS St. Francis Hospital in Litchfield and HSHS Good Shepherd Hospital in Shelbyville.
Ascension report outlines commitment to advancing maternal health St. Louis-based Ascension has published a report that provides an in-depth look at the health system’s role in delivering care to newborns and their mothers and at the social determinants of health that often lead to disparities in care.
The report is titled “1 in 50: Ascension’s Maternal Health Report,” a nod toward Ascension’s delivery of one of every 50 babies born in the United States. The system’s birthing units nationwide have delivered between 72,000 and 78,000 infants every year for the past five years, which represents about 2% of the 3.6 million babies born in the U.S. every year.
The report notes that in 2023 about 41.5% of Ascension’s maternal patients had Medicaid coverage and 1.65% were self-pay. It also says Ascension’s maternal health outcomes “strongly outperform” national averages. The system’s maternal mortality rates for 2021 were 21% lower than nationwide rates for all patients and 41% lower for Black/African American patients. Ascension points to key maternal health initiatives. This includes its Postpartum Nudge Program that addresses the link between hypertension, heart issues and maternal mortality; a social determinants of health screening tool; and food-related initiatives such as a program that delivers fresh foods and meals to women who identify as food insecure. It makes the food deliveries for eight weeks postpartum.
PeaceHealth to partner in rehabilitation hospital in Oregon
PeaceHealth and Lifepoint Rehabilitation have received regulatory approval to build a 67,000-square-foot inpatient rehabilitation hospital in Springfield, Oregon. The standalone building will have 42 inpatient beds with additional space for future expansion. It will be next to a PeaceHealth urgent care facility called the PeaceHealth RiverBend Annex.
PeaceHealth and Lifepoint Rehabilitation will break ground on the facility in October and open it in January 2026.
Melisa Dare, an instructor at the SSM Health Security Academy, yells words and phrases like, “No!” “Stop!” and “Get back!” for a class of clinicians and support staff to repeat after her.
SSM Health Security Academy instructor Melisa Dare and security officer Eric Visor demonstrate a defensive move at the academy.
Anderer
Photos by Jerry Naunheim/@CHA
May 2024 CATHOLIC HEALTH WORLD 9
and Louisiana. He also led the system through the pandemic as well as through the clinical and financial challenges that have followed.
He spoke to Catholic Health World about what drew him to medicine and to ministry system leadership. His responses have been edited for length and clarity:
How did you become interested in a career in medicine?
The easiest answer is that it was serendipity. There are no physicians in our family — we are a very right-brained family. I was interested in science and in life sciences and had planned to be a marine biologist. On a lark, my cousin had applied to med school and enjoyed it and I decided to do the same.
Once I was in my residency, I realized I enjoyed the blend of art and science in internal medicine. I enjoy the process of gleaning symptoms, building a story of the illness. I love interacting with the patient to build the story of the illness and then applying the blend of art and science to help the patient.
What were some of the main challenges you faced as a physician?
The biggest challenge was when I was part of a small group of just three pulmonary care physicians managing patient care at four different hospitals in Baton Rouge. We were on call on a rotating basis. It took a psychological and emotional toll because we were taking care of the very sick. Many died. We learned to really face challenges. We had to squash our emotions to perform. Critical care physicians tended to do better in COVID because we are used to compartmentalizing our emotions.
What we learned then and what hospitals are learning now is we had to work as teams and it’s important to recognize the need to develop the team — the scrub techs, the nurses, the physicians. As more physicians moved to hospital-based environments, they suddenly needed that skill, of developing teams. And I’d had to develop that skill already, and that served me well in leadership roles.
What are some of the main changes you’ve witnessed in medicine over your career?
There have been changes in the pressures as medicine has evolved into more subsegments of specialized units. That requires specialized training. So you require physicians to have more experience over time, and medicine becomes more compartmentalized. And this amplifies the staffing issues. This was seen, for example, during COVID when pulmonary care physicians were burning out. Hospitals couldn’t find their expertise with other clinicians. Given the physicians’ compensation and the facilities’ revenues, hospitals couldn’t keep up with the cost of care. It became an insurmountable task.
It’s hard as a leader not to use traditional thinking. We had to transform six different areas of the hospital just to keep up with the volumes of patients coming in during COVID. It was a little easier for me as a

“
The biggest joy, and I’m going to miss this most, is working with the people here. It’s been a joy watching them develop their talents and rise to the occasion and for all of us to learn together.”
system leader with my clinical background — I understood the disease clinically. And coming from Louisiana we were used to setting up incident command centers because of hurricanes. It was clear to me as COVID started we had to set up incident command, because we do that every year during hurricane season.
It actually was post-COVID that was more difficult.
Why was the aftermath of the COVID peak more difficult?
The real issues for all of us go back to the super-specialization of hospital care. The real challenge was the burnout and people not being interested in doing this hard work in these circumstances anymore. And we all are dealing with this in different ways. We doubled down on engaging our workforce partners, including Louisiana State University. We are working to attract new workers, build relationships as a team, and support them. Our mission team has worked with HR to continue to support our staff, and that’s been a huge effort.
What has improved most in medicine over the course of your career?
The team efforts towards quality have improved most. In 1983 when I started practicing medicine, we did not have the quality standards we have today except for the regulations and compliance guidelines that we had. In 1999, the Institute of Medicine published To Err Is Human, and two years later it published Crossing the Quality Chasm, and this asked: ‘What should quality look like?’ and ‘How do we define and execute on quality?’ And we saw change. This started a passion of mine, and I came in to Our Lady of the Lake to set up this quality-related work. I had studied teams of physicians and how to influence behavior to promote quality.
Then, we started to look at population health, the need to look at quality outcomes outside of the hospital. We looked at: How do we get everyone on the same page? This is a huge focus for us, and we are in the top 5% of the country when it comes to quality. Our work with accountable care organizations has enabled us to define and clarify what our mission is and how that relates to quality outcomes.
What attracted you to leadership in Catholic health care?
I’ve always been interested in leadership and raising people’s performance. I realized that there were lots of patients cared for by providers who didn’t have the proper training. I asked myself, how can we raise everyone up? And I became interested in raising standards, including by working through the electronic medical record. I saw that I could make a bigger impact and on a larger scale through leadership. And so I led quality and safety efforts at Our Lady of the Lake. I used my background to learn how to motivate change in physicians.
What has it been like to be a leader in Catholic health care in particular?
I had practiced at Our Lady of the Lake as
a physician, but as a leader I learned more about the mission and was impressed at how this small group of introverted women had created these facilities that are part of our system, and I saw how these nuns were so effective in inculcating their mission. When I became CEO I said I needed to understand this better. I took CHA’s sponsor formation course and figured out it’s not just about how we relate to each other as a team but also with the church.
What are some of the joys you’ve had as CEO of this system?
The biggest joy, and I’m going to miss this most, is working with the people here. It’s been a joy watching them develop their talents and rise to the occasion and for all of us to learn together. As a Franciscan system, we are a relationally driven organization, and I’ve worked on marrying that relational and the performance-driven aspects of our work together.
What insights would you share with other Catholic health care leaders?
I’ve never had a more fulfilling role as this, and it’s humbling to realize that there is still much work to do. A big focus for the next generation of health care leaders in the ministry is that not only do we really need to build and strengthen Catholic health care, we also need to drive the triple aim. We need to continue to demonstrate quality outcomes. We need to change the quality of care and focus on the health of populations. We have to figure all this out, and also figure out how to lower the total cost of care — or I’m not sure what will happen in the long haul.
To do this work, we have to make sure we continue to take seriously the formation of leaders in the Catholic health care ministry, or we won’t be able to continue to pursue our mission and vision.
jminda@chausa.org
Sr. Mack held leadership roles in Bon Secours congregation, health system
Sr. Anne Marie Mack, CBS, died March 31 at age 76. During more than four decades as a Bon Secours sister, she held numerous top leadership roles in the congregation and in many of its health ministries.

Sr. Elaine Davia, CBS, Bon Secours congregation area leader, said in an announcement that Sr. Mack “was a guiding light for
many, and the impact of her leadership throughout the years will be felt well into the future.”
Sr. Mack entered the Congregation of Sisters of Bon Secours in 1965 and professed her final vows in 1978. She earned her bachelor’s of nursing degree from the University of Delaware in Newark and her master’s in nursing from Wayne State University in Detroit.
She was a nurse at what was then Bon Secours Hospital in Grosse Pointe, Michigan.
In the congregation, she served in multiple, progressive leadership roles. Among the posts she held was chair of the provincial general assembly, assistant provincial, provincial secretary, associate liaison sister and — from 1997 to 2005 — president of the congregation in the U.S. Beginning in 2005, she held leadership roles in what was then Bon Secours Health System, including as vice president of mission for two hospitals in Richmond, Virginia. She retired in September 2021 as senior vice president of sponsorship for the
Bon Secours Richmond Health System. She served on the boards of multiple Bon Secours Health subsystems and facilities, including as board president at facilities in Michigan and Virginia.
From 2008 to 2011, she chaired the board of UNANIMA International, a nongovernmental organization of women religious advocating at the United Nations on behalf of vulnerable populations.
Sr. Mack played a key role in founding the Cristo Rey Richmond school for vulnerable children.
Vath From page 1
Sr. Mack
Dr. Richard Vath chats with Jennifer DeCuir at the headquarters of Franciscan Missionaries of Our Lady Health System in Baton Rouge, Louisiana. Vath is retiring as president and CEO of the system. DeCuir is executive vice president and general counsel.
10 CATHOLIC HEALTH WORLD May 2024
Providence reaches out to those of diverse religions with ‘Faith-full Fridays’
By LORI ROSE
When patients enter a Catholic hospital such as Providence Little Company of Mary Medical Center in Torrance, California, they are greeted with religious symbols that may not be part of their own faith tradition.

people of other faiths are not afraid to walk in the front door?”
Bringing positive energy to healing
and their caregivers, is just such a gift.”
Levin said chaplains also provide special resources for Buddhist and Hindu patients.
we are upholding the Providence promise to ‘know me, care for me, ease my way.’”
Finding unity across faiths

But Lead Chaplain Aviva Levin, who works with Spiritual Care Manager Paul White to oversee an interfaith team of chaplains at Little Company of Mary, is working to ensure that every patient — regardless of faith — feels cared for and welcomed with open arms. As part of that mission, Levin created a program called “Faith-full Fridays” to make sure she and her colleagues are meeting the unique needs of nonCatholic patients, including those who identify as Jewish, Muslim, Hindu, agnostic and atheist.
“When I got here, I heard conversations from leadership about their desire to articulate to faith communities outside of the Catholic Church that this is a hospital, first and foremost,” said Levin, who is Jewish. “Yes, we have crucifixes, but that doesn’t get in the way of first-class medical treatment. But how do we communicate that so that
Levin joined Little Company of Mary, part of Providence St. Joseph Health, in 2021 after completing her training in clinical pastoral education. During her training at a hospital that is not faith-based, she had witnessed a program in which Jewish patients were provided a prayer sheet and challah bread. Knowing that Fridays are uniquely sacred to those who identify as Jewish and Muslim, she proposed Faithfull Fridays at Little Company of Mary as a way to help those patients observe certain rituals that might bring peace and positive energy to their healing.
On Faith-full Fridays, chaplains deliver special bags to new patients who identify as Jewish or Muslim: Shabbat bags for Jewish patients that include battery-operated tea lights, kosher grape juice and a bread roll to help them observe the Sabbath; and prayer beads for Muslim patients along with a booklet with blessings and prayers from the Quran for health and healing.
“It’s such an amazing gift to be able to do this work,” Levin said. “The fact that a Catholic health ministry has a female Jewish lead chaplain and embraces my kooky ideas and my desires to go in and make this the best experience possible for patients
If a patient identifies as nonreligious, the chaplains offer support through guided meditations, music, art, nature — whatever might help that person find meaning and connection and feel cared for without judgment. A Catholic priest chaplain attends to the sacramental needs of Catholic patients and their loved ones.
“Wherever you are on the spectrum, we’re here to support you,” Levin said. “We’re saying: ‘Hey, we really see you,’ and
“It’s such an amazing gift to be able to do this work. The fact that a Catholic health ministry has a female Jewish lead chaplain and embraces my kooky ideas and my desires to go in and make this the best experience possible for patients and their caregivers, is just such a gift.”
— Aviva Levin
ENRICHING THEIR SOULS WHILE THEIR BODY HEALS.
The Faith-full Fridays program has been adopted at Little Company of Mary Medical Center in San Pedro, California, as well. White, manager of spiritual care at both Little Company of Mary hospitals, said the response at each medical center has been overwhelmingly positive.
“In a Catholic health care system such as Providence it is the norm to have Catholic and Protestant chaplains,” he said. “It is more unusual to have a chaplain who is Jewish. And even more unusual to have chaplains who are Jewish and Muslim, which we do.”
White said that while society in general has become less religious and the faith tradition of the chaplain seems to matter less to patients, there is a genuine appreciation from Jewish and Muslim patients. “They express feeling seen in a place where they may have anticipated they would not be accepted,” he said.
For Levin, coming to work every day in a place where crucifixes adorn each patient room has helped deepen her understanding of how different faiths can find unity.
“When we first initiated the Faith-full Friday program, I knocked on a Muslim gentleman’s door and offered him his prayer beads. He froze,” Levin recalled. “He looked at me, placed his right hand to his heart and said, ‘I am a Muslim in a Catholic hospital receiving ritual support from a Jewish chaplain. Can you imagine such a thing?’
“And I said, ‘I dream of the day when our faith is what brings us closer to one another as opposed to distant.’ It just warmed my heart.”

We have a lot in common. Like you, our mission is to provide care and healing to those most in need. As the world’s largest Catholic media network, EWTN offers free faith-based programs and podcasts, live and On Demand news, TV and radio to all who are suffering in mind, body or soul. Discover the healing power of God’s love and compassion. Contact Christine Schicker, cschicker@ewtn.com, to learn how to add EWTN and EWTN Español to your system free of all license fees.
Be sure to stop by EWTN’s Booth at
TELEVISION • RADIO • NEWS • ONLINE • PUBLISHING • EWTN.COM
Catholic Health Assembly in San Diego, June 9-11, 2024. Developing a Roadmap to Responsible Donations — Global Health Learning and Sharing Network May 7 | 1 p.m. ET Webinar: Catalysts for Compassion: A Conversation with the American Hospital Association on Person-Centered Language May 14 | 1 – 2 p.m. ET Mission in Long-Term Care Networking Call May 16 | 11 a.m. – Noon ET Assembly 2024 June 9 –11 Upcoming Events from The Catholic Health Association chausa.org/calendar
the
Levin
May 2024 CATHOLIC HEALTH WORLD 11
White
Founder-director of dementia center draws on personal experience, passion to serve
CEDAR RAPIDS, Iowa — About a decade ago, when Tim Charles, then-president and CEO of Mercy Cedar Rapids, wanted to explore the possibility of starting a facility for caregivers of people with dementia and other chronic illnesses, he knew just who to ask.
An acquaintance, Kathy Good, had been a social worker who served for more than a decade as caregiver for her husband, Dave Good. The retired judge had been diagnosed with Alzheimer’s disease and was living at HallMar, a residential care center at Mercy Medical Center. (HallMar moved to an off-campus location last year.)
Charles had witnessed Good’s dogged determination to learn about and understand her husband’s condition and to advocate on his behalf so he could live life as fully as possible.
As she recounts in her 2023 book, My World Wore a Bow Tie, Good left no stone unturned seeking information about her husband’s condition. She located experts who could help plot out a course for him, obtained — often through convoluted methods — the medications he needed, ensured his access to the care he required, and even worked with HallMar to improve the decor in the facility so he and his fellow residents could enjoy beautiful surroundings.
It turns out that Charles’ instincts were on target — Good has applied the wisdom gained as a caregiver to build out a full range of services and resources. Over the last 10 years, she has led the establishment of a Family Caregivers Center on Mercy
Dementia care
From page 1
facility, the Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia. Mercy Cedar Rapids opened the Innovation Center in June to greatly expand dementia programming and services and to spur innovation regarding older adults and those living with dementia.
The Innovation Center, which is connected to HallMar Village, is a joint venture of Mercy Cedar Rapids and Presbyterian Homes & Services. HallMar Village is a 237-resident senior living community that opened in the fall.
Personal connection
Mercy took on dementia and caregiver services in a big way around 2014. ThenMercy President and CEO Tim Charles had seen a caregivers’ center in a hospital in New York and wanted to explore whether Mercy could open a similar site. He was aware — and extensive subsequent research confirmed — that there was a critical lack of services and support in Cedar Rapids for the growing population of people serving as caregivers for people with dementia.
Charles recruited an acquaintance, Kathy Good, to lead efforts to start such a center. Good, formerly a social worker, was also a caregiver for her husband, Dave Good, who had dementia. First as a volunteer and then as paid Mercy staff, Kathy Good, along with Charles and other Mercy staff and donors, visited caregiver centers elsewhere in the country. Good researched how Mercy might establish such a center. She engaged with Mercy executives, dementia experts, community leaders and a panel of caregivers to develop ideas and build out some plans. She also took part in a business innovation incubator of sorts to refine the plans and worked with Mercy to create the site.
In December 2015, Good and a team of Mercy leaders opened the Family Caregivers Center on the campus of Mercy Medical Center in Cedar Rapids. The caregivers’ center has offices for its four staff members

Good addresses staff and volunteers of the
Medical’s campus and the Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia, which is connected to the new HallMar senior living community in suburban Cedar Rapids. She has overseen the creation at the centers of an expansive and growing menu of programs for caregivers and people with dementia and other
chronic illnesses.
Good’s book is partly a recounting of what it was like to be the wife of an accomplished, outgoing, healthy man blindsided by an Alzheimer’s diagnosis and how the two Goods navigated life as Dave’s condition worsened until his death. He died on May 17, 2015, at age 68. The book also serves
6.9 MILLION
Americans age 65 and older are living with Alzheimer’s dementia. Of this group, 73% are age 75 or older.
By 2050, this number is projected to rise to nearly 13 million.
as a comprehensive guide to how Good and others developed the Family Caregivers Center and Innovation Center.
The book is available from the Family Caregivers Center. For more information, visit mercycare.org/services/ family-caregivers-center/.
—JULIE MINDA
A SLOW, UNCERTAIN PROGRESSION 1 IN 3 SENIORS dies with Alzheimer’s or another dementia. It kills more than breast cancer and prostate cancer combined.
People age 65 and older survive an average of four to eight years after a diagnosis of Alzheimer’s, yet some live as long as 20 years with Alzheimer’s.
PREVALENCE BY GENDER AND RACE
ALMOST TWO-THIRDS of Americans with Alzheimer's are women.
Older Black Americans are about twice as likely to have Alzheimer's or other dementias as older whites.
Older Hispanics are about one and one-half times as likely to have Alzheimer's or other dementias as older whites.
An Alzheimer’s Association report on Iowa says about 11% of Iowans aged 65 plus have Alzheimer’s dementia. That is about 62,200 people. That report estimates that about 4,100 people who are aged 65 plus in Linn County, Iowa, have Alzheimer’s dementia. This is about 10% of the population that is in that age group. Cedar Rapids is in Linn County.

THE COST Health and long-term care costs for people living with dementia are projected to reach $360 BILLION in 2024 and nearly $1 trillion in 2050.
and working space for its dozens of volunteers. It also has a few small meeting rooms and a library of books and other materials on dementia, caregiving and related topics. At the center, caregivers can access resources, support groups, educational experiences and other programming. Good is the center’s director.
Several years after the caregivers’ center opened, Good and her team and executives at Mercy identified a need to expand programming to better serve not only caregivers but also people with dementia as well as older adults. She and the team recognized they needed more space. When they learned that there was a shuttered church available for development on the property where Mercy and Presbyterian were building the HallMar senior living community, Good and her team jumped at the chance to transform that church into a hub serving
Source: Alzheimer’s Association
Cedar Rapids
Kathy
Family Caregivers Center. Good is director of the center, which is run by Mercy Cedar Rapids.
12 CATHOLIC HEALTH WORLD May 2024
Kathy Good with her husband, Dave Good, a retired judge who was diagnosed with Alzheimer’s disease and who she provided care to for more than a decade.

people with dementia and older adults.
Customer discovery
The church has been totally revamped. What was the vestibule now is the Innovation Center welcome area, staff offices and meeting rooms; the former sanctuary serves as a multipurpose conference area, event space, auditorium and exercise room. The center also has a secondary gathering area equipped with a commercial kitchen. There also is a Center for Memory Health where clinicians can evaluate people to determine if they have dementia. The clinical team works with clients to develop care plans and then provide needed services. The Innovation Center connects to HallMar Village. Walking trails around the center link to surrounding neighborhoods to encourage integration into the broader community.
Good says she and her colleagues who have developed the center and its programming have relied heavily not only on research but also on a process they call customer discovery, to ensure that what they develop is in line with what people want and need. Through that approach, staff who are developing plans and programming conduct extensive engagement with the people they’ll be serving and with experts in the field.
The Innovation Center is meant to serve as a “living classroom.” Its staff and volunteers are constantly evolving the center’s offerings in line with people’s stated needs and preferences. Current offerings include the Center for Memory Health’s assessment and follow-up services, educational and informational presentations, caregiver respite programs, social and support groups for people with dementia and their caregivers, exercise classes, a singing group,
Susie Winkowski says the Family Caregivers Center and now the Innovation Center are helping her and her husband fully grasp that “even though he has dementia, he can still do what he did before,” such as traveling, socializing and even country western dancing.
and entertainment such as musical performances. Coming soon is a “connection club” that will provide engaging activities for people living with earlier-stage dementia and respite for their caregivers. The center also has a showroom featuring appliances that could be helpful for people with dementia and displays of everyday items — ranging from can openers to chairs — that could be useful to them in their homes.
The Innovation Center also plans to expand its involvement in research projects and to engage in advocacy on behalf of people with dementia and their caregivers.
The Family Caregivers Center has an annual budget of around $450,000, and the Innovation Center has a budget that is around $400,000. (These figures exclude the budget for the Center for Memory Health.) Both the caregivers’ center and Innovation Center are funded in part by philanthropy through the Mercy Medical Center Foundation. Mercy Medical Center also supplies a significant amount of funding.
Innovation Center showcases household items that can benefit people with dementia

CEDAR RAPIDS, Iowa — At the innovation hub that Mercy Cedar Rapids and a partner opened last summer, there is a showroom and kiosk area to help people with dementia and their caregivers learn about household items and how to use them.
The Chris & Suzy DeWolf Family Innovation Center for Aging & Dementia in suburban Cedar Rapids, which is run by Mercy Cedar Rapids, has two areas where people can inspect the household items. In the appliance showroom, several Samsung smart appliances are set up for use in a model kitchen. Small household tools, like can openers, are set up in kiosks elsewhere in the center.
Cedar Rapids’ Grand Appliance store donated the appliances and has provided its staff’s expertise to the Innovation Center. The center is training volunteers to be able to demonstrate the appliances to the center’s clients.
There is a smart refrigerator, induction stove, dishwasher and microwave on display in the center’s showroom. These appliances have safety features that can prevent tragedy. For instance, the induc-
Focus on strengths, capabilities
Good says a thrust of the Innovation Center is to reframe people’s perspectives on aging and dementia.
She says there is a pervasive view in society — and often among people with dementia and their caregivers — that those with dementia can’t contribute much to those around them, and that they can’t have

tion stove’s surface does not get hot anywhere except under a pan placed on it.
All the appliances can be monitored and operated remotely. If a caregiver is at work, they will know if their loved one with dementia has turned on a stove at home. The caregiver also could view the contents of the refrigerator from anywhere through video technology. This could help save time driving home to view the contents before going grocery shopping.
Also in the showroom is a furniture display. Innovation Center visitors can test out different chairs and tables for sturdiness and stability and ease of use for older adults and people with dementia.
In another area, the Innovation Center has multiple kiosks with a rotating display of assistive devices such as specially designed silverware and thermostats. Innovation Center staff and volunteers can explain to clients how the items can benefit older adults and people with dementia.
—JULIE MINDA
much quality of life. To the contrary, Good says, there is much that people with cognitive impairment can do and enjoy.
The Innovation Center’s staff and volunteers have a mantra: people should focus on their strengths and capabilities, rather than having a singular focus on what they’ve lost and the negative aspects of life with dementia. Staff and volunteers help people with dementia, and their caregivers, to identify and build upon their capabilities and adapt to deficiencies.
Winkowski says the Family Caregivers Center and now the Innovation Center are helping her and her husband fully grasp that “even though he has dementia, he can still do what he did before,” such as traveling, socializing and even country western dancing.
Barb Snively and Cindi McKee volunteer with a Family Caregivers and Innovation Center program that is a partnership with a church. They provide companionship to people with dementia while the caregivers get respite.
McKee says, “No matter what they are dealing with physically or mentally, they are still a valuable person.”
Snively says her volunteer work has reaffirmed her belief that people living with dementia still have a lot to contribute to their world. “They make us volunteers smile,” she says. “They are still capable of giving and receiving joy.”
jminda@chausa.org
Kenneth Royar, left, and Steve Nurre chat with other members of the Together in Song chorus at the Innovation Center. Royar is a participant and Nurre is the director of the musical group assembled by Mercy Cedar Rapids’ caregiver and innovation centers. Made up of people with dementia and other chronic conditions as well as other community members, the group presents spring and fall concerts of songs that resonate with them and their audiences.
A patio offers expansive views of the grasslands behind the Innovation Center. The center is connected to HallMar Village, a senior living community. Walking paths go through both properties and connect with those in adjacent neighborhoods.
The Innovation Center staff and volunteers have set up several kiosks like this one around the center. The kiosks display everyday tools and small appliances that could make life easier for people with dementia and for older adults. This kiosk displays easy-grip silverware and a jar opener.
Josh Booth /Diamond Label Films
May 2024 CATHOLIC HEALTH WORLD 13
Josh Booth /Diamond Label Films
Josh
Booth /Diamond Label Films
‘God has been in this story.’
Couple with Parkinson’s undergo brain surgery on same day, by same surgeon at Baylor St. Luke’s in Houston
By VALERIE SCHREMP HAHN
Allison Toepperwein and Steven Eury can hardly believe the twists and turns their lives have taken over the last several years.
Faith and science play a big role. Parkinson’s disease plays another.
Toepperwein, 46, and Eury, 43, who live outside Charlotte, North Carolina, both have had early-onset Parkinson’s disease since 2010. Back then, the two didn’t know one another and lived in different parts of the country. Each had noticed hand tremors, a symptom of the disease.
In December, the couple underwent deep brain stimulation surgery at Baylor St. Luke’s Medical Center in Houston on the same day, in the same operating suite, by the same doctor. In late January, the couple had their implanted electrical stimulation devices activated. They have experienced minimal symptoms since.
“We want to shout from the rooftops that God has been in this story,” said Toepperwein. “As far as this surgery goes, it’s just right in line with our story. God allowed two people with Parkinson’s — who got married, who had symptoms at the same time, now married with combined families — (to have) this surgery, agreed to both do on the same day by the same surgeon.”

That neurosurgeon, Dr. Sameer Anil Sheth, said while the couple’s story is unique, the operation they underwent is a routine one known to produce good outcomes. It’s even common to do two such surgeries a day at the hospital. To have it on the same day was the couple’s choice.
“Primarily, I’m very happy for the two of them,” Sheth said. “Secondarily, I’m hopeful that their storylines resonate with other people, and it will encourage someone who maybe doesn’t know about (the surgery) to find out about it.”
Living with Parkinson’s disease
Parkinson’s disease is a neurologic disorder affecting the brain and causing difficulty with movements or motor functions, according to the American Parkinson Disease Association. About 1 million people live with Parkinson’s in the United States and about 10 million worldwide, according to the association. When someone ages 21-50 is diagnosed, about 10% of cases, it is considered early-onset or young-onset Parkinson’s.
The cause is unknown. It’s more common in older men. Research suggests it’s tied to genetic predispositions or environmental exposures to things like pesticides and solvents.
Toepperwein was 32 in April 2010, a new mother to a baby daughter, and living in Austin, Texas, when she held up a coffee pot with her left hand and it began to shake. She could only stop the shaking by pressing her left hand with her right one.
Eury was 29 in December 2010, living in North Carolina, visiting the hospital for his son’s birth. He noticed a tremor in his hand when he held up a camera to film. The next year, he was diagnosed with early-onset Parkinson’s.
Both of their marriages fell apart. Toepperwein and her daughter moved in with her father outside Houston. Stress exacerbates symptoms, and Toepperwein’s symptoms had become undeniable: She lost use of her left arm, she dragged her right foot, and she began slurring her words and choking on food. She was diagnosed with Parkinson’s on New Year’s Eve 2014, five months after leaving her husband.
“I was just at the lowest of my life,” she said.


She got a job in communications at the Baylor College of Medicine in Houston and connected with doctors within that system for treatment.
She began blogging, taking medication, and exercising. In 2016, she became the first person with Parkinson’s to compete on the television show “American Ninja Warrior.”
She had several frustrating dating experiences. In May 2020 she wrote a heartfelt prayer on a piece of paper, surrendering her search for a soulmate, trusting that God would find the right person for her.
Just four days later, Eury bought some property on a street outside of Charlotte.
The street was named Allison. He wanted to build a new home there for himself, his son and daughter and his dog Allie.
In August 2020, a friend texted Eury a blog post that Toepperwein had written about dating with Parkinson’s. He asked if Eury had looked at any dating sites for people with the disease and sent a link to Toepperwein’s profile. “Not yet,” Eury texted back. “But the blonde may change my mind.”
They met in person in October 2020, and within a few months, they had fallen in love. Toepperwein helped Eury build his home in North Carolina. In October 2022, they got married.

“Primarily, I’m very happy for the two of them.
Secondarily, I’m hopeful that their storylines resonate with other people, and it will encourage someone who maybe doesn’t know about (the surgery) to find out about it.”
— Dr. Sameer Anil Sheth
Game-changing surgery
Both Eury and Toepperwein had limited results managing their symptoms with medication, which they had to constantly adjust.
“But it also started going downhill as far as how much medicine it took just to give me a few moments or few minutes a day of
Steven Eury leads wife Allison Toepperwein through the hall at Baylor St. Luke’s Medical Center in Houston. In December, they underwent deep brain stimulation surgery on the same day.
Allison Toepperwein and her husband Steven Eury have early-onset Parkinson’s disease. They connected online before meeting in person.
Dr. Sameer Anil Sheth performs deep brain stimulation surgery, which involves having electrodes probed into different locations of the brain to help alleviate symptoms of Parkinson’s disease.
Continued on 15
Sheth
14 CATHOLIC HEALTH WORLD May 2024
DEI backlash
From page 1
commitment, “We have remained steadfast.”
Their comments come amid a wave of blows against diversity efforts on the grounds that the initiatives give unfair advantages to some groups.
In several states, including Texas, where CHRISTUS is based, lawmakers have passed measures to halt DEI initiatives at universities. Those measures follow a Supreme Court decision last summer that struck down affirmative action in college admissions. Meanwhile, a conservative nonprofit called The American Alliance for Equal Rights has sued various private and public organizations over race-based programs, such as internships offered exclusively to minority groups.
Doubling down
Chastang says the backlash might in some conversations prompt her to change her language when she discusses Trinity Health’s push for diversity, equity and inclusion. Sometimes, she will instead reference terms from Catholic social teaching such as justice and solidarity to explain that the system’s DEI efforts are extensions of its mission to respect and provide quality care to everyone, especially the poor and vulnerable.
“If those three letters — ‘D’ period, ‘E’ period, ‘I’ period — are causing people to trip up and I need to talk about it differently, I’ll update my language so that I can bring people along,” she says.
Whatever the terminology, Chastang says Trinity Health has put DEI in motion systemwide. It produces an annual DEI report that spotlights its efforts and shares the related successes. The report for fiscal year 2023, for example, points out that of the Livonia, Michigan-based system’s workforce of about 150,000 across 27 states, 30,000 employees this year voluntarily acknowledged the system’s DEI commitment statement. The statement includes: “DEI is a central part of living our mission, core values and achieving our vision.”
Meanwhile, the system’s Colleague Resource Groups, set up to foster an inclusive and welcoming environment for staff members by helping them network with others with common interests or experi-
Parkinson’s surgery
From page 14
relief,” said Eury.
Toepperwein struggled with back muscle contractions, something that the medication, Botox injections or massages barely alleviated.
The surgery they each underwent involves having electrodes probed into different target locations of the brain, depending on the patient’s symptoms. A generator/ stimulator is then implanted just under the collarbone. Thin wires run from the electrodes beneath the skin under the scalp, behind the ear and down the patient’s neck to the stimulator. The stimulator can be charged and programmed remotely.
The couple traveled to Houston to have their surgery on Dec. 18; Eury first, then Toepperwein.
“We feel like we could not have had better surgeons, a better team — everybody was such an incredible blessing,” Toepperwein said.
Eury calls the surgery “a game-changer.” “Not of our own works,” he said, pointing upwards. “This was His gift to us.”
The couple took some time to physically recover from the surgery before the devices were activated in late January.
The programming sessions took hours, with a nurse practitioner adjusting the frequency and strength of the electrical pulses the device sends to their brains. Afterward,


ence, have grown from a few to more than 10 groups and membership spiked 66% last year. The separate groups include those for women, African Americans, veterans and the LGBTQ+ community.
Chastang says while other organizations might be pulling back, Trinity Health has “consistently doubled down on our commitment to diversity, equity and inclusion. It’s not a program, it’s not an activity. It is our identity. It is how we want to and choose to show up in the world.”
Setting goals
Stapleton says DEI was a priority for Bon Secours Mercy Health well before tragic events such as the deaths at the hands of police of George Floyd in Minneapolis and Breonna Taylor in Louisville, Kentucky, made diversity initiatives trendy.
In the last few years, however, Stapleton says the Cincinnati-based system has been intentional about setting goals for its efforts and tracking progress.
In 2019 Bon Secours Mercy Health committed, within five years, to contract at least $50 million — a year-over-year 5% increase in its diverse business spend — in its supplies or services from minority businesses. It reached that goal in less than four years. “We’ve exceeded that $50 million just by being more inclusive in the bidding process, and we’re trying to do even more,” Stapleton says.
The system recently signed an “impact workforce commitment” as part of its participation in the Healthcare Anchor Network. The system pledged over the next five years to hire 10% of its associates from ZIP codes with high percentages of marginalized people within communities in its seven-state footprint.

Hiring, growing diverse leaders
Stapleton says Bon Secours Mercy Health encourages leaders to recruit and interview qualified job candidates from minority groups that reflect the communities served. The percentage of people from such groups hired for positions at director level or above across the system hit 19% in 2020 and 21% last year.
The system also is working to develop leaders from within, including efforts to ensure that women and people of color who are on executive tracks have mentors.
The system’s goal, Stapleton says, is for its leadership to reflect the racial and ethnic makeup of the communities it serves. “We’re not lowering the qualifications,” she notes. “They have to be equally or better qualified than any other candidate for executive talent acquisition to include them on the slate.”
Stapleton says she sees DEI initiatives as a manifestation of Bon Secours Mercy Health’s commitment to honoring and elevating the human dignity of all people, but also as vital to its survival. “If we don’t have providers of multiple ethnicities, multiple generations, different races, different backgrounds, are people going to want to come to us for care?” she asks.
Mirroring the community
Pesquera says CHRISTUS Health is steeped in a commitment to diversity that is reflected in the makeup of its board of
directors. The board is almost equally split by gender and one-third of its 15 members are people of color. The current chair, Maricela Breedlove, is Hispanic.
“Our goal is not to see how everyone else is doing and then we perform accordingly,” Pesquera says. “Our goal is to look at our patient population and our communities and the diversity that exists within the folks that we’re able to serve. And that’s how we want to mirror and that’s how we want to look.”
Part of Pesquera’s job is to monitor CHRISTUS’ metrics around diversity at its hospitals, which are in Texas, Louisiana, New Mexico, Chile, Mexico and Colombia, and report on the system’s progress to the board every six months. A goal that the system set in 2020 is to increase what was then 24% representation of minority groups in executive levels to 32% by 2025. Pesquera says the system is already near 30% as it replaces people moving or retiring from those jobs through promotions and new hires.
To help develop a diverse pool of candidates for its top posts, CHRISTUS has a sponsorship program for minority associates who show promise as future leaders. Those associates are paired with executives who can give them high-visibility projects, invite them to showcase their knowledge at board meetings and otherwise open doors that can put them on a path to C-suite offices.
“Basically, the goal is to bring highperforming associates to rooms they normally do not have access to,” Pesquera says.
As intentional as CHRISTUS is in its efforts to diversify its executive ranks, Pesquera says in the end hiring decisions are based on whoever is the best fit.
“We’re going to hire always the best person for the job that has the right qualifications, but we are going to look and make sure that we have reached out to organizations and individuals that are diverse, that are minorities, and consider them in the process,” he says.
leisenhauer@chausa.org

they were able to stand up, turn and walk without shaking and make fine motor movements with their hands. For the first time in a long time, Eury’s parents could hear him speak: the Parkinson’s disease had affected his voice, and he had only been able to whisper.
Sheth had explained to them that the deep brain stimulator acts as a traffic cop for the brain: It disrupts the abnormal electrical signals that affect movement for
patients, stopping the bad traffic and allowing the healthy traffic to flow more easily. The couple has since had more sessions to program and adjust the devices and are scheduled for more. In the meantime, they report they’re doing great. They’ve joined a rock-climbing gym and go bike riding together. Eury started running. They also speak to groups to tell their story.
They continue to live on Allison Street with their combined family of three teenag-
ers and their dog Allie.
“It truly is a quality-of-life procedure, and our quality of life is just incredible” compared to before, said Toepperwein. “You know, we walk in somewhere and we forget that we have Parkinson’s. We walk into somewhere and see people that we haven’t seen in six months to a year and they’re just blown away and dumbfounded.”
Faith and the future
Toepperwein and Eury know the surgery isn’t a cure. It’s meant to help alleviate their symptoms, giving them another 10 to 15 years of quality life, and they wait for a cure or a way to better manage symptoms by then. They continue to grapple with that uncertainty and are grateful for the here and now.
Sheth, the surgeon, points out that he’s not working alone. He credits his surgical team.
“From a faith point of view,” he said, “I’m just here to kind of humbly serve and do my part in a big, intricate web of people who are doing their part with excellence.”
Toepperwein said her faith has allowed her to face the uncertainties of her life, especially when she moved 1,100 miles to be with Eury. “I was just going with it. God was opening all these doors,” she said. Eury agrees. “This is a battle that is not easy,” he said, “but we see the Lord’s hand in all this. There’s no denying it.” vhahn@chausa.org
Delving into DEI • A Health Progress Diversity, Equity and Inclusion Discussion Guide offers a means to move toward greater understanding of one another and patients. chausa.org/DEIguide
Chastang Stapleton Pesquera
Allison Toepperwein, pictured with her daughter Emma, competed on the TV show “American Ninja Warrior” in 2016 and 2017.
May 2024 CATHOLIC HEALTH WORLD 15

Furry blessings
Tails were wagging in April as canine therapists made the rounds and got special attention
Top: Alli Wilson, left, and Maegan Stone, nurse externs at CHRISTUS Good Shepherd Medical Center — Longview in Texas, get some face time with Zoey on April 30, National Therapy Animal Day. The hospital celebrated the day with a blessing of its four therapy dogs.
Top right: Lily Grace sports a colorful bandana and tutu for the gathering in the healing garden at CHRISTUS Good Shepherd — Longview. The event marked her introduction as a therapy dog. Right: On the eve of National Therapy Animal Day, therapy dogs and their handlers are blessed at CHRISTUS Cancer Center at Highland Medical Center in Shreveport, Louisiana. National Therapy Animal Day honors animals that, with their handlers, bring comfort and healing to those in need.
Far right: Resident Margie Frandsen pets Henry during a visit in mid-April by the therapy group Love on a Leash to Benedictine Living Community — Bismarck in North Dakota. Residents of the community gifted their visitors with “doggie bags” of treats to take home. Love on a Leash’s therapy pets and their handlers visit the community monthly to provide emotional support and spread cheer.
KEEPING UP



PRESIDENTS/CEOS
Trinity Health regions have announced these changes:
Shelleye Yaklin has retired as president of Trinity Health Grand Haven, a hospital that joined Trinity Health in 2022. Gary Allore succeeds Yaklin as president. Allore also will remain president of Trinity Health Muskegon and Shelby hospitals. John Foss, who is senior vice president of operations for Shelby Hospital, will lead day-to-day operations for both the Grand Haven and Shelby hospitals.
In the Trinity Health Mid-Atlantic region, James Woodward plans to retire as president and CEO, effective Jan. 3.
Robert J. Erickson to Hospital Sisters Health System Wisconsin market president and CEO. Most recently, he was president and CEO of UnityPoint Health Trinity Regional Health System, which has a presence in Illinois and Iowa. He succeeds Brian Charlier, who retired. In addition to his market role, Erickson is president and CEO of HSHS St. Vincent Hospital and HSHS St. Mary’s Hospital Medical Center in Green






Bay, Wisconsin. He also will oversee HSHS’s two other Wisconsin hospitals, HSHS St. Nicholas Hospital in Sheboygan and HSHS St. Clare Memorial Hospital in Oconto Falls.
Facilities within CommonSpirit Health have made these changes:
Dr. Christina “Tina” Johnson to Dignity Health Sacramento, California, market president, from president and CEO of Sacramento’s Mercy General Hospital. In her new role, she will oversee five Dignity Health hospitals in the Greater Sacramento area. The market leadership role comes as part of a statewide restructuring to better align with organizational goals of CommonSpirit Health, says a release. A search for a new Mercy General Hospital president and CEO is underway. Michael Korpiel, the prior Sacramento market president, will be president and CEO of Dignity Health Mercy San Juan Medical Center in Carmichael, California. Katherine Vergos to Dignity Health Las Vegas market president as well as Siena Hospital campus president and CEO, effective May 12. Most recently, she was presi-



dent of SSM Health’s Fond du Lac, Wisconsin, market and president of St. Agnes Hospital in Fond du Lac. At Dignity Health, Vergos succeeds Jon Van Boening, who is retiring.
Andrea Burch to president of Intermountain Health’s Lutheran Medical Center in Wheat Ridge, Colorado, from interim president. She succeeds Scott Peek. He departed the role to become president of Intermountain Health’s front range market as well as president of Saint Joseph Hospital in Denver. Burch will lead Lutheran Medical Center’s move to its replacement location this summer.
ADMINISTRATIVE CHANGES
St. Louis-based Ascension has made these changes: Michelle H. Kohler to executive vice president and chief human resources officer, effective June 1; and Amber Sims to executive vice president, chief strategy and growth officer.
Jan M. Barrett to executive director of Duluth Benedictine Ministries, the ministerial public juridic person for the Benedictine
Sisters of St. Scholastica Monastery in Duluth, Minnesota.
Jill Hackenmueller to senior vice president, people development, for Benedictine in Minneapolis.
Dr. Kim Ruscher to chief medical officer for the PeaceHealth Oregon network.
Margaret M. Horvath to executive director of Providence Alaska Children’s Hospital in Anchorage, Alaska.
Jason Demke to chief operating officer for Mercy Hospital Fort Smith in Arkansas, part of Chesterfield, Missouri-based Mercy.
Marilyn Alejandro-Rodriguez to community health director for Mercy Health — Lorain in Ohio, part of Bon Secours Mercy Health.
GRANT
Ascension Saint Thomas River Park in McMinnville, Tennessee, received a $7.6 million grant from the state of Tennessee. Ascension Saint Thomas will match that amount, bringing the total investment to $15.2 million. The hospital will use the funds to enhance various departments. Improvements will include relocating and expanding the emergency department and intensive care unit. Separately, Ascension Saint Thomas River Park will use a $138,000 donation from the Ascension Saint Thomas Foundation for additional upgrades.
ANNIVERSARY
Mercy College of Health Sciences Des Moines, Iowa, 125 years.
Erickson
Horvath
Barrett Vergos
Demke
Hackenmueller
Burch
AlejandroRodriguez
Ruscher
16 CATHOLIC HEALTH WORLD May 2024

































 Benziger
Waring
Benziger
Waring