Leaving no one behind: DePaul clinics widen reach in New Orleans
By LISA EISENHAUER
NEW ORLEANS — The groundbreaking in August on an expanded replacement clinic in the Algiers neighborhood of New Orleans is just the latest example of the growth of DePaul Community Health Centers.
The new clinic is being built at an estimated cost of $14.4 million and is planned to open in September 2024. It will have 20,000 square feet of space, five times as much as the current site. The new facility will offer more on-site services, including optometry and urgent care.
The groundbreaking came four months after the opening of a DePaul clinic in Harvey, another economically challenged
Trinity Health grant fuels mentoring program at Student
Advocacy Center
PROVIDING SPACE TO SERVE THE COMMUNITY
Cedar Rapids nonprofits pay nearly nothing as tenants of Mercy center
By KARI WILLIAMS
Anell Eccleston remembers a conversation early in his relationship with a boy he was mentoring in which the boy mentioned that he expected to end up in jail.
“He didn’t know how he was going to end up there, he just knew he would,” recalls Eccleston, director of care and sustainability for the Student Advocacy Center of Michigan.
The boy was one of nine siblings in a family that had been touched by incarceration and poverty. The boy’s mother was unemployed most of the roughly three years Eccleston worked with the boy through the center, a nonprofit focused on keeping
The Kids First Law Center and YPN (formerly, Young Parents Network) are among the nonprofits that get nearly free office space from Mercy Cedar Rapids. Above, Kids First Executive Director Jenny Schulz is at the office of that organization for kids navigating their parents’ conflicted relationships. Below, YPN volunteer Rebecca Hein provides child care. It is common for the nonprofit’s volunteers to tend to children while parents and guardians attend prenatal and parenting education activities.
 By JULIE MINDA
By JULIE MINDA
CEDAR RAPIDS, Iowa
When a disastrous flood in 2008 displaced numerous nonprofits and simultaneously hyperinflated the cost of office space here, Mercy Cedar Rapids came up with a creative idea that has since benefited multiple nonprofits, their clients, the community and the health system.
The health system transformed a somewhat dilapidated 100-year-old building it owned near its campus from an underutilized storage site into a vital hub for nonprofits. The building houses five mission-based organizations, at negligible cost to those tenants.
The arrangement has allowed Mercy Cedar Rapids to serve the community in a distinct way and the center’s tenants
Continued on 4
Avera mobile lab brings researchers to rural communities
 By VALERIE SCHREMP HAHN
By VALERIE SCHREMP HAHN
The Avera Research Institute is on the move — literally.
The institute, part of Avera Health, recently acquired a 25-foot mobile research unit, a 2023 Turtle Top Terra Transit vehicle, that travels around the state. It is mostly based in Pierre, South Dakota, which is centrally located and gives easier access to partnering with tribal nations and rural communities.
At its “bricks and mortar” site in Sioux Falls, the Avera Research Institute also is involved in studies on cancer among American Indians, substance use and

Community benefit briefing 3 Executive changes 6 Denver hospital celebrates 150 years 2
Continued on 7 Continued on 6 Continued on 8 The Avera Research Institute is using its new mobile unit to reach people in remote parts of Avera Health’s service area, allowing them to participate in the institute’s studies.
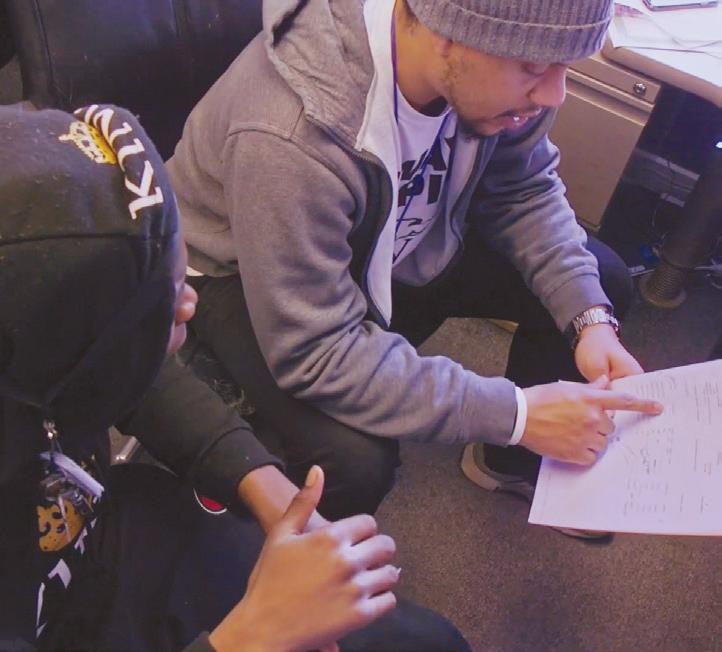
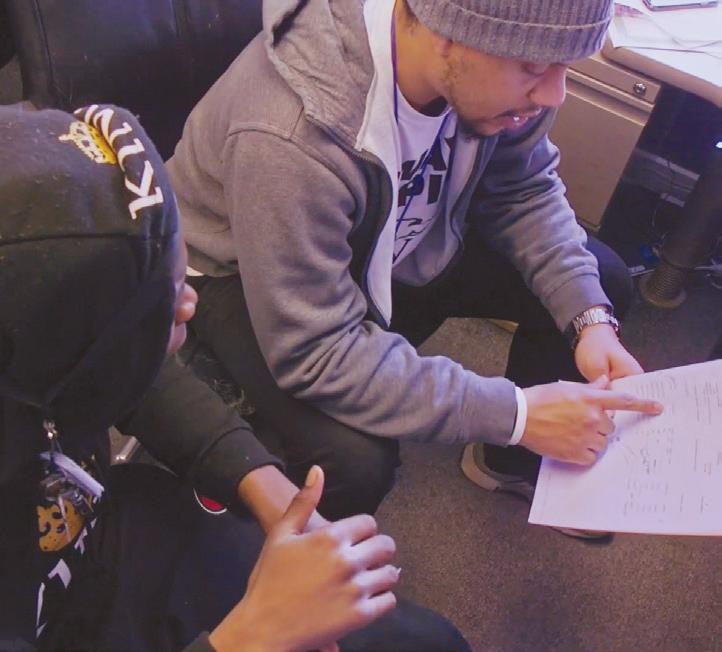
Anell Eccleston talks with a student he was mentoring as part of the Check & Connect program run by the Student Advocacy Center of Michigan. The program recently got a grant from Trinity Health Ann Arbor Hospital.
PERIODICAL RATE PUBLICATION
Josh Booth /Diamond Label Films
OCTOBER 2023 VOLUME 39, NUMBER 16
2 CATHOLIC HEALTH WORLD October 2023
Mercy Health — Youngstown partners to build rehab hospital
Denver’s Saint Joseph Hospital is the city’s largest teaching hospital. It was founded in 1873 by the Sisters of Charity of Leavenworth.
Saint Joseph marks 150 years in Denver
Saint Joseph Hospital is celebrating its 150th anniversary with a series of events, including a gala, blessing of caregivers’ hands and a “Mega Cookie Monday,” carrying on a tradition of the hospital’s foundresses, the Sisters of Charity of Leavenworth, to deliver freshly baked cookies to caregivers throughout the facility.
Saint Joseph traces its roots to 1873, when Mother Xavier Ross of the Sisters of Charity of Leavenworth, Kansas, sent four sisters west with $9 to start a hospital. In Denver, they solicited funds from miners, cowboys and others to begin providing health care services out of a cottage.

Soon after, the sisters moved the hospital into a brick building in an area that some community members called out as questionable since it was known to have prostitutes. “We’ll take the question out of the neighborhood,” one of the sisters said.
In 1876, the sisters began construc-
We’ve Got a New Look
have a
❖
Easier to share content across social media
Improved display on your mobile device
Health Progress
chausa.org/hp
tion of a new facility on land donated by the territorial governor. A flour baron led a fund-raising campaign for that campus’ construction. According to information from the hospital, through a citywide bazaar and a monster euchre party organized by “the unsinkable” Molly Brown, the campaign raised $10,000. The site was the first private teaching hospital in Denver and remains the city’s largest such facility.
The hospital relocated to a replacement facility in 1961 and then to another replacement facility — at its current location — in 2014.
Today Saint Joseph is a 400-bed hospital with more than 2,600 staff and nearly 1,600 physicians. It provides emergency care, heart and vascular care, labor and delivery services, oncology services, orthopedics, respiratory therapy, surgery and other services. It has clinical partnerships with Kaiser Permanente and National Jewish Health.
Saint Joseph became part of Intermountain Health when Saint Joseph’s parent company SCL Health merged with Intermountain in April 2022.
Catholic Health World (ISSN 87564068) is published semimonthly, except monthly in January, April, July and October and copyrighted © by the Catholic Health Association of the United States. POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@chausa.org. Periodicals postage rate is paid at St. Louis and additional mailing offices. Annual subscription rates: CHA members free, others $29 and foreign $29. Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA. Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
Vice President Communications and Marketing
Brian P. Reardon
Editor Lisa Eisenhauer leisenhauer@chausa.org
314-253-3437
Associate Editor Julie Minda jminda@chausa.org
314-253-3412
The 66,000-square-foot, two-story facility will be called Mercy Health Rehabilitation Hospital. It is expected to cost about $43.8 million to build. The projected opening is in late 2024. The hospital will have 60 private rooms, multidisciplinary therapy gymnasiums, outdoor courtyards and other spaces designed to help patients return to activities of daily living, according to a release from Mercy Health.
The new hospital will include a 12-bed brain injury unit with private dining and a therapy gym. All units will be structurally designed for the needs of patients receiving acute inpatient rehabilitation care for stroke, traumatic brain injury, amputation and other injuries and disorders.
Mercy Health, part of Bon Secours Mercy Health, has 22 hospitals across Ohio and Kentucky. Lifepoint Rehabilitation is a unit of Lifepoint Health, based in Brentwood, Tennessee. Lifepoint Health has acute care hospitals and rehabilitation and behavioral health facilities in 31 states.

Earlier this year, Mercy Health — Youngstown and Lifepoint Behavioral Health, another business unit of Lifepoint Health, announced they had formed a separate partnership to construct and operate a 72-bed inpatient behavioral health hospital. That facility will cost about $44 million to build.
Assumption Community to become part of Benedictine
The effective date of the change is dependent on the review and approval of the Minnesota Department of Health, Benedictine said, but is not expected before Nov. 1.
Associate Editor Valerie Schremp Hahn vhahn@chausa.org
314-253-3410
Graphic Design Norma Klingsick
Fr. LeRoy Scheierl, pastor of Saint Boniface, said in a release that because of the increasing complexity of the health care sector, “no single parish is able to adequately oversee the important health care of our senior citizens.”
He added, “By transferring membership from the Church of Saint Boniface to Benedictine, we want to ensure not only the long-term care and well-being of our valuable seniors who need our special attention, but also ensure the long-term existence of our wonderful facility along with our employees.”
We Will Empower Bold Change to Elevate Human
Assumption Community includes Assumption Home, a 76-bed skilled nursing facility; Assumption Court, a 59-unit assisted living campus; Asher Haus, a 28-unit assisted living memory care building; the John Paul Apartments, a 61-unit subsidized senior apartment building; and Assumption Community Services, a Medicare-certified home health agency. The campus currently employs 153 people.
Deans of Catholic Colleges of Nursing Networking Call Oct. 3 | 1 – 2 p.m. ET United Against Human Trafficking Networking Call Oct. 4 | Noon – 1 p.m. ET Community Benefit 101: The Nuts and Bolts of Planning and Reporting Community Benefits Virtual Program Oct. 24 – 26 | 2 – 5 p.m. ET each day Global Health Networking Call Nov. 1 | 1 – 2:30 p.m. ET Mission Leader Seminar Virtual Program Tuesdays Nov. 7 – 28 | 1 – 2:30 p.m. ET Upcoming Events from The Catholic Health Association chausa.org/calendar © Catholic Health Association of the United States, October 2023
Advertising ads@chausa.org 314-253-3477 Updated graphics and visuals
Flourishing. SM
❖
❖
design.
The websites for CHA’s publications
fresh
chausa.org/chw
Health World
Catholic
Three Sisters of Charity of Leavenworth look over blueprints for a $7.5 million building and expansion for Saint Joseph Hospital. From left are Sr. Mary Pierre, SCL, head of the pediatrics department; Sr. Mary Asella, SCL; and Sr. Mary Kieran, SCL, head of the surgical department. This image appeared in the Denver Catholic Register on May 28, 1959.
Mercy Health — Youngstown in Ohio broke ground Aug. 31 on an inpatient rehabilitation hospital it is building in partnership with Lifepoint Rehabilitation.
Photo provided by Archdiocese of Denver Archives
Assumption Community in Cold Spring, Minnesota, is becoming part of Benedictine. The senior living community will move from oversight by the Church of Saint Boniface, Cold Spring, and the Saint Cloud Diocese.
CHA briefing explains community benefit standards to congressional staffers
 By VALERIE SCHREMP HAHN
By VALERIE SCHREMP HAHN
Community benefit, a driving force behind the Catholic health ministry’s current mission, may have its roots in the 1700s when a congregation of women religious came from Europe to America to visit and aid the sick and the poor.
“They looked around and saw what needed to be done. ... You could say they were doing the first community health needs assessments,” Julie Trocchio, CHA’s senior director of community benefit and continuing care, said during an online briefing for congressional staffers on community benefit requirements for notfor-profit hospitals hosted by CHA Sept. 7.
Lucas W. Swanepoel, senior director of government relations, in explaining why CHA offered the briefing, noted that the association has been a leader in establishing community benefit best practices. “At a time when there is increasing scrutiny around hospital community benefit programs, we hope to use this expertise, and work of the Catholic health ministry, to break through the noise and confusion about the tax requirements that not-forprofit hospitals must abide by,” Swanepoel said.
He added that the briefing provided an opportunity to remind congressional staff of the current legal requirements and demonstrate the many ways not-for-profit hospitals take these requirements seriously in their work to serve those in need in their community.
Picking and choosing
A tax expert from Ernst & Young LLP and representatives from Franciscan Missionaries of Our Lady Health System and CHRISTUS Health spoke during the briefing.
The presenters explained that community benefit is a well-defined set of activities that tax-exempt hospitals must do to
Catholic health care’s investments into community benefit

$2.8 billion
Financial assistance at cost (charity care)
$6.51 billion
Unreimbursed Medicaid and costs of other means-tested programs

$1.87 billion
Community health improvement, subsidized health services and cash and in-kind contributions for community benefit
$1.8 billion
Health professions education
$547 billion
Health research
Based on an analysis of available data from 353 FY2019 IRS Form 990, Schedule-H filings representing approximately 650 Catholic hospitals
Source: CHA
maintain their status as tax-exempt entities under federal law.
Stephen Clarke, managing director of the exempt organization tax services division of Ernst & Young, noted the community benefit standard was established by the IRS in 1969. The Affordable Care Act in 2010 added more requirements, such as having hospitals adopt and promote a financial assistance policy and do a community health needs assessment every three years. It also limited certain charges and collections actions.

Clarke detailed the eight types of
reportable community benefits, including research, health professions education, and financial assistance or at-cost charity care. He noted that nonprofit hospitals and their community benefit standards have received increased media attention over the past year.
“Interestingly, most of these press outlets or research groups don’t report on all eight types of community benefit, but they pick and choose categories that they think are community benefit or charitable,” he said. “Oftentimes, only a couple or a few of those categories are highlighted by the press.”
Top 10 needs
Coletta Barrett, vice president of mission at Our Lady of the Lake Regional Medical Center in Baton Rouge, Louisiana, talked about her hospital system’s affiliation with Healthy BR, a mayoral initiative to address the health of the community. Our Lady of the Lake is part of FMOLHS.
All five of the major hospitals that serve the Baton Rouge region are part of the initiative and collaborated to create a community health needs assessment. “We may have individual implementation strategies, but we all report into the same implementation plan,” she said. “Therefore, we can focus our efforts on those key priorities and move the needle on some of these community strategies.”
The hospitals analyzed data and talked to people in the community to identify the top 10 needs of the community, which included access to care and prevention of cancer, diabetes and sexually transmitted diseases. “By focusing on areas of improvement and collectively working in our own ways, we’re able to address significant population health issues in Baton Rouge,” Barrett said.
From surveys to programs
Marcos Pesquera, system vice president of community health and health equity and chief diversity officer at CHRISTUS Health, talked about his health system’s work in underserved communities and focused on the Corpus Christi region in Texas.

CHRISTUS made surveys about community needs available in both printed and online formats. The system got about 500 responses in at least seven languages from the Corpus Christi region alone, Pesquera said.
One of the many programs the system implemented in response is a food prescription program, in which medical providers refer patients and eligible community members to a food bank or to get monthly food boxes. They are then asked to schedule a follow-up medical visit after they are enrolled. “It’s been quite a success,” Pesquera said.
The hospital system also uses AmeriCorps workers as community health program coordinators to maintain data on resources to help community partners. Those workers are based at the partner organizations, “which is great because they can deal with the public, with the community and with their peers,” Pesquera said. “That’s how we’re able to integrate all of our programs throughout the community.”
Resources related to community benefit requirements are available at chausa. org/communitybenefit. In addition, CHA is offering the three-day program Community Benefit 101 Oct. 24-26. Information is at chausa.org/events. vhahn@chausa.org
Colorado hospital co-sponsors ‘Mugs for Rugs’

Last month and this month in the greater Lafayette, Colorado, community, Good
Samaritan
Medical
Loose throw rugs are a common trip-
ping hazard in homes. “More than 70% of patients who are admitted to Good Samaritan Medical Center with traumatic injuries suffered those injuries due to a fall,” said Grace Dobbertin, Good Samaritan trauma outreach education coordinator. “Common injuries resulting from falls include broken bones and traumatic brain injuries.” Swaps were to be made on a first-come, first-served basis at several locations. The rugs that were collected were set to be donated to local animal shelters, Good Samaritan said in a release.
“We hope to use this expertise, and work of the Catholic health ministry, to break through the noise and confusion about the tax requirements that not-for-profit hospitals must abide by.”
— Lucas W. Swanepoel
Trocchio
Swanepoel
Barrett U.S. Postal Service STATEMENT OF OWNERSHIP, MANAGEMENT, AND CIRCULATION (Required by 39 U.S.C. 3685) 1. Publication title: Catholic Health World 2. Publication number: 8756-4068 3. Filing date: Oct. 1, 2023 4. Issue frequency: Semimonthly except monthly in January, April, July and October. 5. No. of issues published annually: 20 6. Annual subscription price: members — Free; Nonmembers (Domestic & Foreign) — $29 7. Complete mailing address of known office of publication: 4455 Woodson Rd., St. Louis, MO 63134-3797 8. Complete mailing address of headquarters or general business office of publisher: The Catholic Health Association of the United States, 4455 Woodson Rd., St. Louis, MO 63134-3797 9. Full names and complete addresses of publisher,
Pesquera editor, and associate editors: Catholic Health Association, publisher; Lisa Eisenhauer, editor; Julie Minda and Valerie Schremp Hahn, associate editors; 4455 Woodson Rd., St. Louis, MO 63134-3797 10. Owner: The Catholic Health Association of the United States, 4455 Woodson Rd., St. Louis, MO 63134-3797 11. Known bondholders, mortgagees, and other security holders: None. 12. The purpose, function, and nonprofit status of this organization and the exem pt status for federal income tax purposes have not changed during the preceding 12 months. 13. Publication name: Catholic Health World 14. Issue date for circulation data below: Sept. 15, 2023 15. Extent and nature of circulation: a. Total number of copies printed (net press run) b. Paid and/or requested circulation (1) Paid/requested outside-county mail subscriptions stated on Form 3541. (2) Paid in-county subscriptions (3) Sales through dealers and carriers, street vendors, counter sales, and other USPS paid distribution (4) Other classes mailed through the USPS c. Total paid and/or requested circulation [Sum of 15b(1), (2), (3), and (4) ] d. Free distribution by mail (Samples, complimentary, and other free) (1) Outside-county as stated on Form 3541 (2) In-county as stated on Form 3541 (3) Other classes mailed through the USPS (4) Free distribution outside the mail (Carriers or other means) e. Total free distribution [Sum of 15d(1), (2), (3), and (4)] f. Total distribution (Sum of 15c and 15e) g. Copies not distributed h. Total (Sum of 15f and g) i. Percent paid and/or requested circulation (15c/15f x 100) 17. This statement of ownership will be printed in the October 2023 issue of this publication.
Average No. Copies Each Issue During Preceding 12 Months
No. Copies of Single Issue Published Nearest to Filing Date 13,919 12,247 381 24 12,652 989 39 1,028 13,680 239 13,919 92.48%
13,625 12,093 362 26 12,481 880 27 907 13,388 237 13,625 93.23% I certify that all information furnished on this form is true and complete. I understand that anyone who furnishes false or misleading information on this form or who omits material or information requested on the form may be subject to criminal sanctions and/or civil sanctions. Lisa Eisenhauer editor
October 2023 CATHOLIC HEALTH WORLD 3
Good Samaritan Medical Center in Lafayette, Colorado, and three partners sponsored a “Mugs for Rugs” exchange with dates in September and October to help people reduce their risk of falling by trading in their throw rugs for a drinking mug.
Good Samaritan, now a part of Intermountain Health, joined Boulder County Area Agency on Aging, Colorado Trauma Network and Foothills Regional Emergency Medical and Trauma Advisory Council to make the trades.
Center and partners are inviting people to trade in their throw rugs, which present a fall risk, for these mugs. From left, Stephanie Coppom, trauma nurse coordinator; Dr. Travis Guthrie, emergency physician; and Mary Ann Ronfeldt, emergency charge nurse, show off the mugs.
Office space for nonprofits
From page 1
to direct funds that normally would go toward leasing or renting office space to programming, services and material aid to vulnerable people.
The Sisters of Mercy established Mercy Cedar Rapids with a mission to serve people in need, says Melissa Dean, director of health equity and community partnerships at the 424-bed Mercy Medical Center, part of Mercy Cedar Rapids. She says with the nonprofits hub, “we are continuing to address needs in a way that the founding sisters would wholeheartedly support. There’s a spirit in this building — the people here love what they do, they have a passion for serving others. The work they’re doing is really hard, but they have that spirit.”
Alejandro Pino is executive director of the nonprofit YPN (formerly, Young Parents Network), which is a center tenant. He says, “Mercy’s presence is seen and felt throughout the community. Our mission aligns with their focus of service.”
A building with a purpose
On June 13, 2008, the Cedar River that runs through Cedar Rapids crested at 31.12 feet, more than 11 feet higher than the prior record. The waters flooded 10 square miles, or 14%, of the city. An estimated 1,300 damaged properties had to be demolished. Nonprofits were among the 486 tax-exempt
Center’s tenants serve Cedar Rapids’ most vulnerable populations
Boys & Girls Clubs of the Corridor
Founded in 1993, the nonprofit has six centers in east-central Iowa, providing underserved kids with access to sports and recreation, the arts, leadership opportunities, wellness activities, workforce preparation and education. The clubs serve about 300 kids per day. The organization is funded in large part through philanthropy.
Catholic Charities of the Archdiocese of Dubuque’s Immigration Legal Services

This arm of Catholic Charities provides immigrants across the 30 counties of the Dubuque archdiocese with advice and representation in legal matters involving immigration status. This includes free legal consultations and very low-cost access to help for achieving status related to green cards, asylum, naturalization, deferred action for childhood arrivals, and fiance visas. The office also assists with refugee petitions, travel documents and other services.
Kids First Law Center
This nonprofit provides support to kids whose parents have divorced, are divorcing or are experiencing other severe conflict. This includes legal representation and workshops for kids, joint parenting sessions and neutral exchange assistance for when kids move between parents.
Metro Catholic Outreach
This charity is a collaborative project of the 11 Catholic parishes of the Cedar Rapids, Iowa, metropolitan area. It provides a food pantry, referrals to social services, and financial aid for housing and utilities for people in need throughout Cedar Rapids.

YPN, formerly Young Parents Network
facilities hit.
In the wake of the disaster, many nonprofits had nowhere to go. Their spaces were unsalvageable. But they couldn’t afford to relocate, since undamaged office space in Cedar Rapids was at a premium. For Boys & Girls Clubs of the Corridor, for instance, the $250,000 insurance reimbursement would not cover the rebuilding cost, and the city declared eminent domain on the club’s old site.
Sr. Susan O’Connor, RSM, then Mercy Cedar Rapids vice president of mission integration, became aware of the nonprofits’ office space problem and remembered that the one-hospital health system already had allowed nonprofit organizations to


have free office space in a building owned by the hospital before. She wondered: Could Mercy Cedar Rapids again house nonprofits?
Then-Mercy President and CEO Tim Charles joined Sr. O’Connor as the driving forces behind an effort to transform a underused building that it owned into a hub for nonprofits.
This nonprofit offers free prenatal, parenting and child and family development programming to vulnerable families. It also offers peer support groups and a home visitation program. Clients also get transportation, food and child care access.

Include your organization’s Christmas message in the Dec. 15 issue of Catholic Health World invites you to extend a seasonal greeting to your employees and to colleagues in the Catholic health ministry. Visit chausa.org/Christmas for more details. Send an email to ads@chausa.org to reserve your ad space. Share the joy of the season with a Christmas message to the ministry ADS DUE BY NOV. 20.
Shoppers browse for clothing, toys and other items at the We Care Shop at YPN. YPN participants earn incentive points to purchase baby care items in the store. Ways to earn points include meeting with an accredited YPN parent educator and documenting healthy behaviors. The shop is fully stocked by community donations and run by YPN staff and volunteers.
Each tenant of the Sister Mary Lawrence Community Center gets access to locked storage space in the basement of the center. Metro Catholic Outreach uses its space as a makeshift food pantry. Clients can drive up to the loading dock of the facility for free food on specified food pantry days.
John Tursi, executive director of Boys & Girls Clubs of the Corridor, in his office at the Sister Mary Lawrence Community Center. Tursi says that having the headquarters at the center means that less space is used at the Boys & Girls Club locations for administration, opening more space for programming for kids.
Dean
Josh Booth /Diamond Label Films
Josh Booth /Diamond Label Films
4 CATHOLIC HEALTH WORLD October 2023
Josh Booth /Diamond Label Films
John Tursi, executive director at Boys & Girls Clubs of the Corridor, recalls that Sr. O’Connor said, “We want this to be a community space for likeminded organizations.”
Up to code
When some prospective tenant organizations had an architect assess the suitability of the facility that Mercy leadership had chosen to be an office hub, that expert said it would cost millions of dollars to bring it up to code, recalls Tursi, head of one of those organizations. He says Charles told the nonprofits that Mercy would figure out how to make it work.
Mercy narrowed its tenant list to four nonprofits and partnered with them to develop the space. Those original tenants were Kids First Law Center, Young Parents Network, Gems of Hope and the Boys & Girls Clubs.
To renovate, Mercy invested some of its own capital, and the nonprofits raised over $600,000 to assist.
The two-story building, which had been used at various times as a laundry facility, a Penny Saver publication office and for hospital storage, required a near-total overhaul. This included gutting the interior; subdividing the space for offices; adding some square footage; creating new stairwells and windows; installing an elevator; building restrooms; installing water systems, heating and air conditioning and electrical; and adding interior design elements.
The grand opening was in September 2011. The health system dubbed the hub the Sister Mary Lawrence Community Center. Sr. Mary Lawrence Hallagan, RSM, was a Mercy administrator and Sisters of Mercy congregation head who was affectionately known as “the builder” for spurring great expansion at Mercy, especially during the 1950s and 1960s. She died in 1999.
Two nonprofits became center tenants after the original four: Metro Catholic Outreach and an office of the Catholic Charities of the Archdiocese of Dubuque. The Gems of Hope cancer charity is to move out later this year. Its space needs have changed.
Cost avoidance
The tenant organizations pay $1 per year to lease their space.
Jenny Schulz, attorney and executive director of Kids First, says conservative estimates are that office space would cost well over $1,500 per month, so the nonprofits are saving more than $18,000 annually in rent. But, she says, the tenants get much
IN BRIEF
Mercy signs agreement to operate rural Missouri hospital
Perry County Memorial Hospital in Perryville, Missouri, and Perry County Health System will integrate with Mercy under a lease agreement effective Oct. 1. Mercy will operate and manage the county-owned hospital under its new name, Mercy Hospital Perry.
Mercy Hospital Perry will be the 17th critical access hospital Mercy owns or operates through lease agreements.
“This hospital is an essential part of our ability to care for Southeast Missouri, and we’re looking forward to being a vital part of this community for decades to come,” Mercy President and CEO Steve Mackin said in a release.
more than practically free space. They get access to the building’s shared conference rooms, bathrooms, break room and an internet and telephone system. They also have access to locked storage in the building’s basement — an essentiality for Metro Catholic Outreach’s food pantry and for YPN’s large cache of diapers.
Mercy handles janitorial services, maintenance, grass mowing, snow removal and security for the common spaces of the building. The tenants just pay the costs for their own spaces — utilities, cleaning, upkeep and decor.
Kate Leonard-Getty, Metro Catholic Outreach executive director, says without the cost avoidance inherent in being a center tenant, “we couldn’t exist.”
Yer Vang, director of Immigration Legal Services for Catholic Charities of Dubuque, says with costs rising for staffing and other business expenses, it is a godsend not to have to budget for expensive office space as well.


The nonprofit directors
— Getty, Pino, Schulz, Tursi and Vang — all say that their organizations absolutely are able to deliver many more services and other aid to vulnerable populations of Cedar Rapids because they are in the hub.
Fringe benefits
Being co-located has many benefits, say the nonprofits’ directors.

It is common for the organizations to refer their clients to the other organizations at the center. Vang says many of the immigration service’s clients have low incomes and language and transportation barriers, — so it’s an added benefit that those indi-
viduals can get many other services in the building.
Schulz adds that she likes that her office can do “warm handoffs,” walking clients to the other organizations. Pino says just giving people a phone number for a recommended service provider “is not entirely helpful or compassionate” for people who struggle to access services.
A strong sense of community has emerged among the nonprofits. Schulz says she has relied upon other directors in the building for advice, and they upon her. For instance, they compared notes on how to handle COVID-19 protocols and vaccinations. They’ve also shared ideas with one another on how to partner on advocacy efforts on behalf of their clients.
Payoff
Dean says Mercy gets many benefits from the hub. For one, the organizations are meeting crucial social needs, and addressing social determinants of health is a priority for Mercy. Supporting these nonprofits means strengthening a social safety net for the community, including Mercy patients and staff who are in need. In fact, Mercy staff commonly refer patients to the organizations in the hub.
Additionally, by hosting these nonprofits, Mercy can become involved and connected with them in a more integral way, Dean says — Mercy can watch their work in action.
“This is a way we can be a small part of this incredible work that they are doing, and to support their expertise,” Dean says. “And it’s a really unique way to understand on a deeper level what is happening at nonprofits in our community.”
jminda@chausa.org
Mercy already has hosted community roundtable events to hear how Mercy can best serve Perry County as well as to learn what residents envision for the future of health care in the area.
The transition includes installing a new electronic health record system through Epic. This system offers one medical record to all Mercy health care providers. It also offers patients online appointment scheduling, access to their records, contact with their physicians, online bill payment and more.
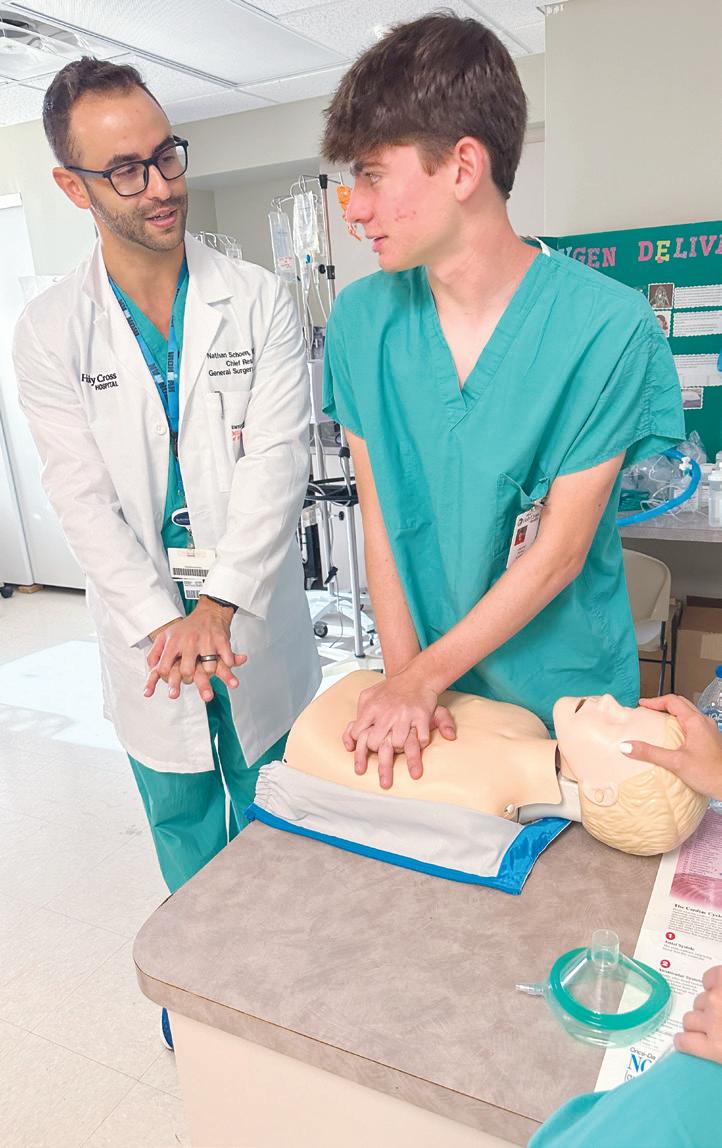
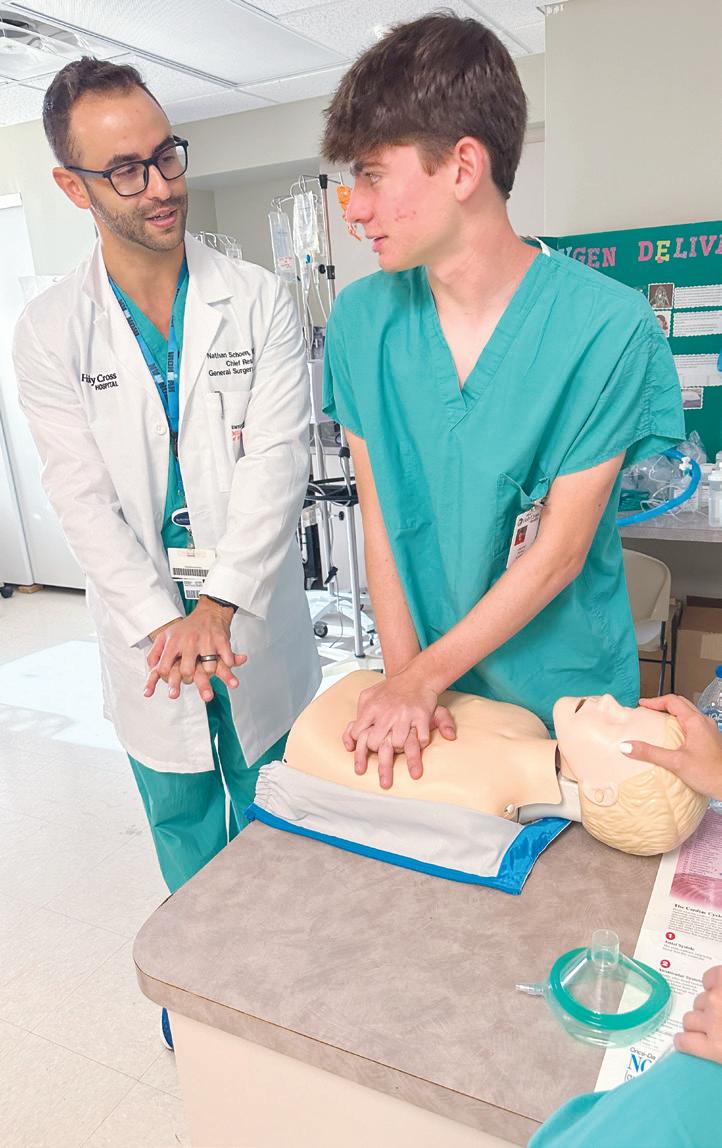
Dr. Nathan Schoen, co-founder of the Summer Surgical Scholars Program and chief surgery resident at University of Miami at Holy Cross, teaches Vincent Perez how to perform CPR. Perez was one of five high school students who participated in the program’s inaugural session.
Summer program immerses teens in surgeons’ world

Five aspiring doctors enrolled this summer in the University of Miami/Holy Cross Health Summer Surgical Scholars Program, a new immersive program for high school students interested in medicine and surgery.
A member of Trinity Health, Holy Cross Health is a Catholic teaching hospital in Fort Lauderdale, Florida.
Over the course of four days, participants in the scholars program shadowed general surgery residents and attending physicians in the operating room, clinic and emergency room, attended academic lectures and participated in additional hands-on experiences.
Dr. Nathan Schoen, chief surgery resident of University of Miami at Holy Cross, said the program he co-founded “provides high school students a truly unique opportunity to develop early medical interests and gain insight into surgical specialties.”
The program was available free to students ages 16 and older who are relatives of Holy Cross Health employees. The general surgery residents and attending physicians who participated volunteered their time.
Tursi
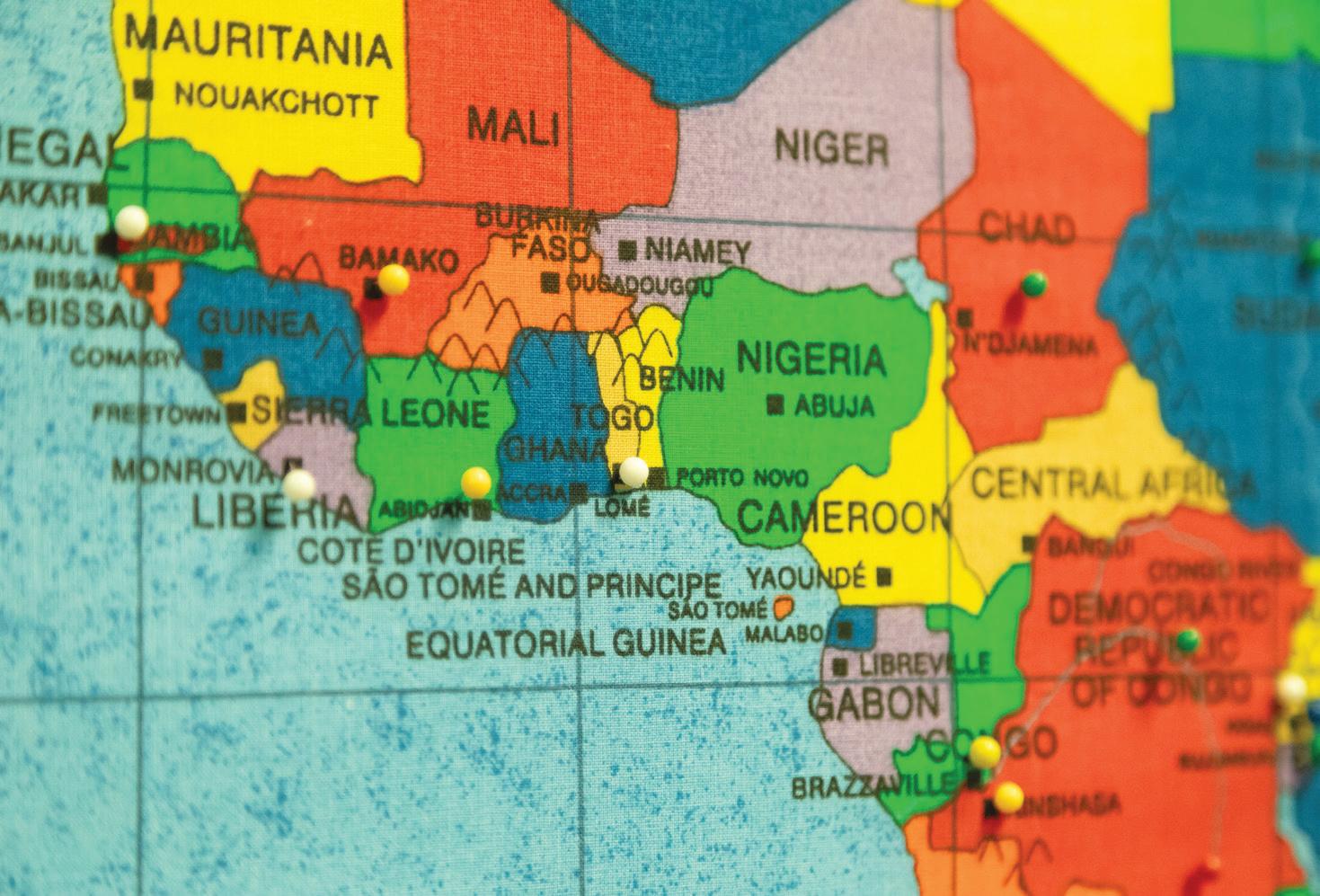
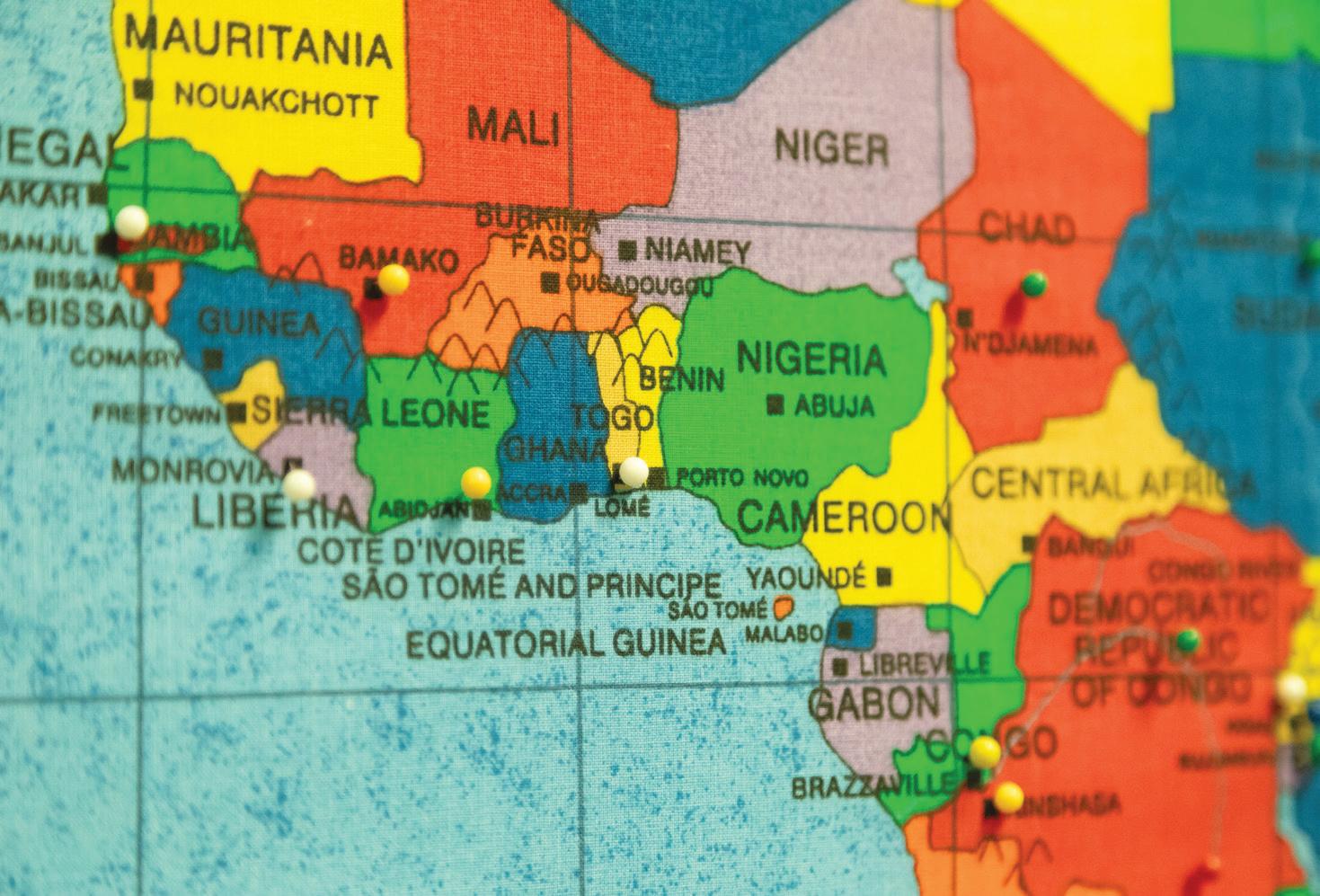
Pins on a map at Catholic Charities of Dubuque Immigration Legal Services indicates the countries from which its clients have immigrated to the U.S. There are about four dozen pins on the full world map.
YPN Program Specialist Nicole Humpal guides children through the halls of Kirkwood Community College in Cedar Rapids, Iowa. YPN provides free child care during many of its prenatal and parenting education events. Here, the kids pretend to be unicorns marching in a parade.
Schulz
Vang
October 2023 CATHOLIC HEALTH WORLD 5
Josh Booth /Diamond Label Films
PRESIDENTS/CEOS
James Dover to president and CEO of Avera Health starting Oct. 23. He was most recently in the same position at Sparrow Health, based in Lansing, Michigan.

Bo Beaudry to Ascension senior vice president and ministry market executive for Ascension Oklahoma. He was CEO for Cedar Park Regional Medical Center in Cedar Park, Texas, which is a joint venture involving Ascension Seton in Texas.
Shannon Striebich to president and CEO of the Trinity Health Michigan Market, from senior vice president of operations of that market and president of Trinity Health Oakland and Trinity Health Livonia hospitals.
Kevin Cullinan to CEO for St. Anthony Hospital, Lakewood, Colorado. He was vice president and chief ambulatory officer for CommonSpirit Health’s Colorado/Kansas/ Utah Division. Cullinan was a CHA Tomorrow’s Leader honoree in 2017. St. Anthony is part of CommonSpirit.


Steven Jorgensen is retiring as president of St. Mary’s Health System and senior

Mobile research unit
From page 1
reproductive health, and food as medicine.
vice president for Covenant Health but will remain in an advisory capacity through Dec. 31. Cindy Segar-Miller will be interim president of St. Mary’s Health System while a search for Jorgensen’s successor is conducted. St. Mary’s is part of Covenant Health of Tewksbury, Massachusetts.
Lydia Parkey to president of St. Bernards Foundation, part of St. Bernards Healthcare in Jonesboro, Arkansas. She was director of physician marketing and executive director for St. Bernards Medical Group.


ADMINISTRATIVE CHANGES
Dr. Nandita Gupta to chief medical officer of PeaceHealth St. John Medical Center in Longview, Washington.
Lesley Tilley to regional vice president of operations for Our Lady of the Lake Health, a subsidiary of Franciscan Missionaries of Our Lady Health System of Baton Rouge, Louisiana. Tilley will oversee the strategic direction and day-to-day operations of four FMOLHS critical access hospitals, a mental and behavioral health service line and ambulatory sites.
What’s inside the unit?
GRANTS AND GIFTS
Trinity Health has received $12.5 million from the Centers for Disease Control and Prevention to start a hub to provide diabetes prevention programming to adults over 65 and Black and Latino/Hispanic adults 18 or older who are at risk for type 2 diabetes. The Trinity Health hub will be one of four in the nation. It will offer a 12-month lifestyle change program designed to help participants achieve moderate weight loss through healthy eating habits and increased physical activity. The hub’s overall goals are to improve access to its programming, reduce disparities in outcomes, increase the use of existing coverage benefits, and work to expand payer coverage of this evidencebased intervention.
PeaceHealth has pledged to donate $2.8 million to Lane Community College in Eugene, Oregon. Over the past nearly 20 years, PeaceHealth has been investing in the growth of the college’s nursing program. This new commitment provides four years of funding, which will allow for an increase in the number of nursing students, which in time is to result in an expansion of the local nursing workforce, according to a press release. The funds also will enable the nursing program to reestablish and expand a respiratory therapy program.
ANNIVERSARY
HSHS St. Joseph’s Hospital Breese in Illinois, 125 years.
Sr. Maya joining CHA as senior director for theology, sponsorship

Sr. Teresa Maya, CCVI, will be CHA’s senior director for theology and sponsorship, beginning Oct. 23.
She was congregational leader for the Sisters of Charity of the Incarnate Word in San Antonio from 2014 to 2022 and had served on the congregation’s leadership team since 2008.

She served as president of the Leadership Conference of Women Religious from 2016 to 2019. Diarmuid Rooney, CHA vice president of sponsorship and mission services, said Sr. Maya “played a pivotal role in guiding multiple congregations as they restructured their ministries to meet the challenges of the future.”
Sr. Maya also has served on leadership boards for CHRISTUS Health, where she advocated for fruitful relationships between sponsors and governance leaders.
Born and raised in Mexico, Sr. Maya entered the Sisters of Charity in that country and professed her vows in 2002. She was a principal in the congregation’s Mexican schools prior to serving in congregational leadership.
Sr. Maya has a doctor of philosophy in history from El Colegio de Mexico; a master of arts in systematic theology from the Graduate Theological Union; and a bachelor of arts from Yale University.
easily incorporate rural populations in health research.
It’s got two clinic rooms inside with two entrances, so we can see two families in separate spaces. We’re able to do physical exams and developmental assessments, and it’s got a blood collection chair to help make things as comfortable as possible for everyone. We have an awning over the front as well, so if we have it at a health fair, we can set up a table easily and have people going in and out.
Did you all look at other mobile labs to inform how you developed yours?
We consulted with a few colleagues that use mobile units to see how they have theirs designed and lessons learned. We ended up modeling our unit after one used by Dr. Johnnye Lewis’ group at the University of New Mexico. They do many projects in collaboration with the Navajo Nation and have many remote and poor road conditions, so we have much in common with them.
Tell me about your footprint.
Elliott
Amy Elliott, the institute’s chief clinical research officer, came to Avera five years ago. At that time, the institute had 15 people. It now has close to 80. She recently spoke with Catholic Health World from her office in Sioux Falls about the institute and the new mobile unit. Responses have been edited for length and clarity.
What sets your research institute apart?
A lot of health systems have a research and innovation arm to them that will do, for example, industry clinical trials, especially in the oncology space. What’s not as common is having an infrastructure that also includes a lot of investigator-initiated research and involvement, especially from a community-based health system, and involvement in national networks at the level in which we are involved. And also our size — we have close to 80 full-time individuals now. We’re quite large, actually, in terms of a research institute.
How did you get the mobile unit?
Our mobile unit came through a supplement on a large National Institutes of Health grant that we’ve been part of for the past seven years called ECHO.
I’ve always wanted to take research out to people who otherwise may not be able to participate. We kind of have a mantra of bringing cutting-edge research to the prairie. One of the things COVID really taught us is the importance of being able to be nimble and inclusive. Another important lesson learned is that while most people have pretty good internet connectivity, there are still huge pockets, particularly in rural areas, that don’t. And connectivity also differs by socioeconomic status. By bringing things out to people, we can help make sure that we’re being more equitable and not limiting who has access to research studies, which can include interventions not available in other settings.
It’s been fun to watch kids engage and be excited about the unit. We really try to help promote that to kids when they’re participating in a research study — you’re doing science, you’re helping others.
Pictures on social media show the kids wearing little lab coats and a buffalo mascot named Boom Boom. It looks like you have some creative researchers.
Our community engagement team is very creative. We do many activities to get people excited about research and, more importantly, to get them excited about what they’re part of. They’re part of contributing to something that can help influence health for kids for generations to come. We really try to embrace everyone and make everyone feel a part of that vision. Research can be intimidating and finding ways to connect with children and families helps everyone feel part of the larger team that is trying to answer important questions.
How will including people in rural areas into research benefit the people of your service area?
Oftentimes, rural areas are overlooked when it comes to health research. Given that health research helps determine what becomes standard of care — for instance, which drugs proven effective move on to general use — if populations aren’t included in the formative studies, then the results may or may not be applicable.
We also have nonintervention studies that are looking at childhood development and what early exposures can influence that development. There is sometimes an assumption that “rural” is just a change in geography. However, we know there are many unique aspects to rural living and lifestyles that are important to include.
Two large grants (from the NIH) and our mobile unit make it possible for us to more
Grant funding enables Avera institute to expand participant population for research
In September, the Avera Research Institute announced it will receive $58 million in funding from the National Institutes of Health over seven years for research to benefit the health of mothers and children, especially those in American Indian and rural communities.
Of the funding, $47 million is for a second cycle of the Environmental Influences on Child Health Outcomes, or ECHO, study. This builds on seven years of work the Avera institute has done looking at environmental influences on
children. Such influences can include sleep, nutrition and allergens.
The rest of the funding will go toward establishing a maternal health research center of excellence, one of 10 planned around the country. Avera’s center will be based at the Avera McKennan Hospital & University Health Center in Sioux Falls, South Dakota.
A portion of the grant dollars is going toward the establishment of the mobile unit.
— VALERIE SCHREMP HAHN
The research institute actually goes beyond the Avera medical and clinical service footprint. We have offices in Sioux Falls, which is on the east side of the state, and also in Rapid City, which is on the western side of the state. We also have an office in Pine Ridge, which is the largest American Indian reservation in our region.
We are a largely rural state with a significant percent of American Indian residents. The western part of the state has more of the larger reservation lands. On Pine Ridge, there is a high unemployment rate and basic resources, such as housing, are difficult for families. There are many tribal members that work every day to improve life and conditions in that area. I think the tremendous strength and sense of community is often overlooked. What is often highlighted is the problems and challenges.
So many people are working to try to help improve unhealthy conditions. But it really is the work that’s happening within the people themselves that is, I think, where the true power of change lies. We are very honored to have been invited and approved to use research to help answer important questions to these communities. We are very cognizant of our role and that the power lies within the people and sense of community.
Some of these studies involve asking personal questions about drug addiction or mental health issues. That has to be a challenge.
This is a challenge and can be difficult on both the participants and staff. This is another reason why it’s important to be able to have options for people to participate. Being able to bring a vehicle to them also just lets people know they’re important and lets them answer difficult questions in person or remotely. Our participants are very generous in telling their life stories and truly are looking for ways to help others. We’re able to hold research within a very confidential space. Research is able to happen in a cocoon of sorts, to help protect participants’ privacy and confidentiality. vhahn@chausa.org
KEEPING UP
6 CATHOLIC HEALTH WORLD October 2023
Beaudry Dover Parkey Striebich Cullinan Jorgensen
Sr. Maya
CommonSpirit names CEOs for its newly acquired Utah hospitals
CommonSpirit Health has named the CEOs for the five Utah hospitals it acquired in May. The facilities previously had been part of Steward Health Care. CommonSpirit’s Centura Health subsystem is managing the hospitals.
The newly named leaders:
Kevin Jenkins to market CEO in Utah and CEO, Holy Cross Hospital — Salt Lake. He was CEO of St. Anthony Hospital in Lakewood, Colorado, which is part of Centura.

Advocacy center
From page 1
students in school, supported and engaged.
One day, the boy told Eccleston that most of his brothers and sisters could not read at grade level. “From that point on, we ended up working on reading,” Eccleston says, especially with materials that aligned with the boy’s interest in cars.
The boy started to do better in math, science and reading. He went on to graduate from high school and is now an automotive mechanic.
The boy also got involved in the center’s youth-organizing program. “He was able to advocate for equitable policy,” Eccleston says. “He was also able to take what we learned from that moment and extend that to support so many more.”
Distributing dollars
Success stories like that and the nonprofit’s history of serving the Ypsilanti community led Trinity Health Ann Arbor Hospital and Trinity Health Livingston Hospital to give the center a $50,000 Community Impact Grant, one of eight of varying amounts awarded by the hospitals this year. Both are part of the nine-hospital Trinity Health Michigan regional system.
Trinity Health Ann Arbor President Alonzo Lewis says the grants went to community groups or agencies focused on issues identified in the hospitals’ community health needs assessments. For Trinity Health Ann Arbor, the priorities of the grants were: mental health and substance-use disorders; obesity and related illnesses; and preconceptual and perinatal health.
The goal of the grants is to strengthen successful community organizations and to seed or support unique programs, Lewis says. The Student Advocacy Center, he says, has a “meaningful impact on breaking the cycle of poverty.”
“They’re improving mental health, social support and the life trajectories of our youth … who are struggling most with school,” he adds.
Check & Connect
The Student Advocacy Center was founded in 1975. It is based in Ypsilanti, a city a few miles east of Ann Arbor with a population of about 20,000. Although 93% of the city’s adult residents are high school graduates, about 30% of the population lives in poverty, according to the U.S. Census Bureau.
Part of the Student Advocacy Center’s mission statement is: “A robust public education is a human right and essential to a thriving democracy.” In addition to mentoring students, it assists those who are suspended, expelled, denied special education support or challenged by other barriers. The center offers a helpline for families whose kids are struggling in school and educational activities for kids. The center, which has 19 staff, also does community organizing to advocate for educational justice. Many of the students the center assists are from low-income and minority families.
Michael Jensen to CEO of Holy Cross Hospital — Davis. He is continuing in the role he held at the facility when it was under Steward’s ownership.
Christine McSweeney to CEO of Holy Cross Hospital — Jordan Valley. She was chief operating officer of St. Anthony Hospital in Lakewood.
Angie Simonson to CEO of Holy Cross Hospital — Jordan Valley West, from CEO at St. Thomas More Hospital in Cañon City, Colorado.
Chris Stines to CEO of Holy Cross Hospital — Mountain Point, from vice president, service lines for the Colorado/ Kansas/Utah Division.
The five Holy Cross hospitals in Utah are among the 20 hospitals and 240 physician practices and clinics that make up CommonSpirit’s Colorado/Kansas/Utah Division, as of Aug. 1. Facilities within that division are transitioning from the Centura to the CommonSpirit name and brand.
CHA, representing more than 600 hospitals and 1,600 long-term care and other health facilities in all 50 states, advances the ministry of the Catholic Church in caring for people and communities. Grounded by our core values of respect, integrity, stewardship and excellence, CHA team members work collaboratively to bring hope and healing to those we serve as we advocate for health equity and access to care for all. CHA and our members promote a culture of inclusion and belonging that brings together people of diverse faiths and backgrounds in our belief that every person is a treasure; every life a sacred gift; and every human being a unity of body, mind and spirit. Through our mission and values, we will empower bold change to elevate human flourishing.
Students take part in Telling Tales Out of School, an annual storytelling and awards event that raises funds for the Student Advocacy Center of Michigan. The center’s mentoring program, Check & Connect, is part of its effort to work collaboratively with underserved students, and their families, to keep them in school, realize their rights to a quality public education and experience success.

Eccleston says the grant from Trinity Health will help the center “create sustainability in our programming.” Specifically, he says the grant will be used for the center’s Check & Connect program. One of his previous positions with the center was as a mentor in the program.
Established around 2012, Check & Connect aims to keep students in classrooms, with a focus on mental health and making connections to other therapeutic organizations. Students who are struggling with behavior in school, absenteeism or poor grades — all warning signs that they may disengage and drop out — get referred to the program by one of the center’s several community partners and paired with a mentor. Mentors and students connect weekly for at least two years.
With the COVID-19 pandemic and its restrictions over, Eccleston considers the biggest issue for youth to be social connectedness. The pandemic, he says, “really took everything a step back” for many students, including in how to engage with authority
figures and be part of a team.
“It’s almost like they had to relearn how to be a student again,” Eccleston says.
Eccleston notes that while educators see keeping students in classrooms as vital to their long-term well-being, some schools have made that harder through a resurgence of so-called zero-tolerance policy practices. According to a Brookings Institution survey, most public schools had such policies, or “mandatory penalties for students who break certain rules,” in place during the 2021-22 school year.
Eccleston says Check & Connect follows an “evidence-based education mentorship model” geared toward school completion by looking at the whole child. He estimates that 75-100 students are working with mentors through the program at any given time. The mentors are on the center’s staff and get special training. “It’s a very intentional and intensive program,” Eccleston notes.
Full circle
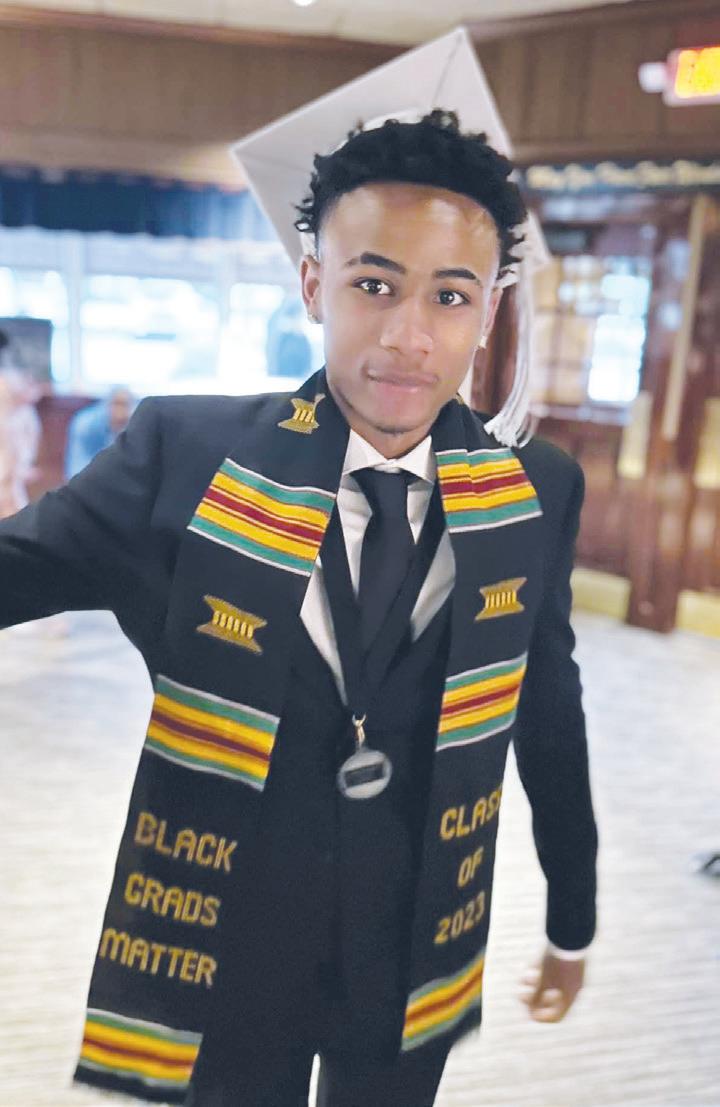
Ky’Andre Vaughn, a 2023 high school graduate, is a recent participant in Check & Connect. Vaughn says he went through a rough patch his freshman year and his father, who was involved with a different mentoring program, connected him with the Student Advocacy Center.
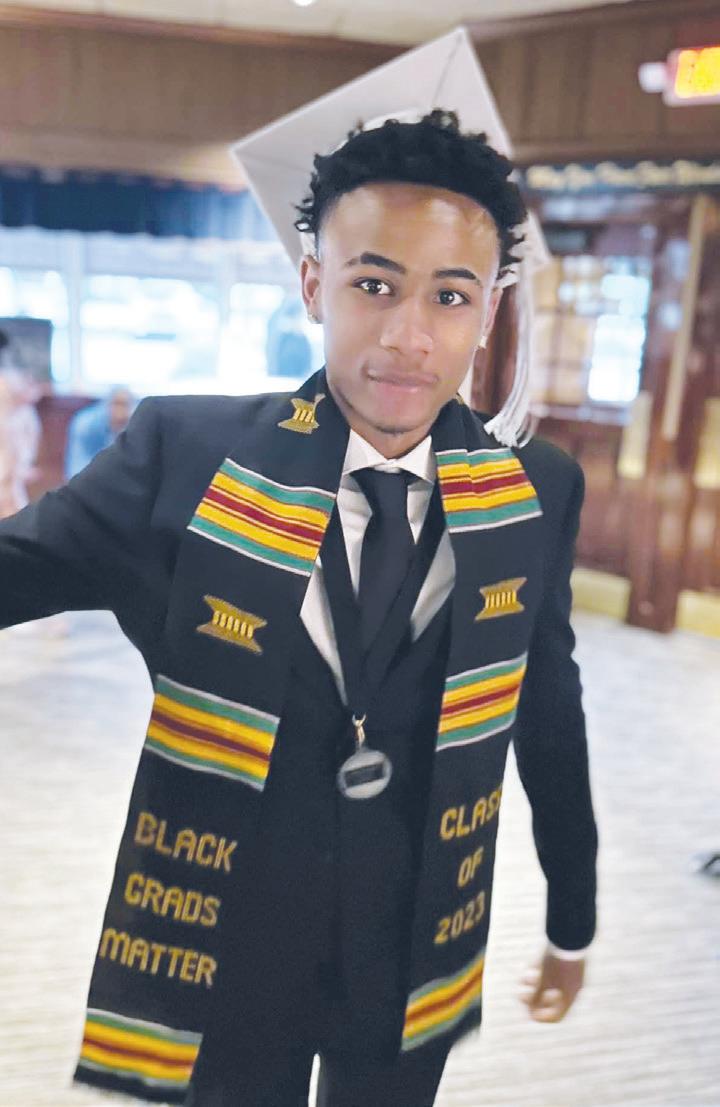
“At first I wasn’t too fond of it,” Vaughn recalls. “It kind of seemed like, from my perspective at a young age, it was where kids go when they’re in trouble or need guidance, or just don’t have enough help. I didn’t think of it in a positive way.”
Once he got into the program, he learned it could be tailored to his own interests — basketball, in his case. The life lessons he got from his mentor were framed around the game, such as that it’s OK to miss a shot and to stick with his pursuits.
“Now I think it’s an awesome, amazing program,” he says. “I think a lot of kids should definitely look into it.”
CHA is excited to announce the development of a new Theology and Ethics Center. The mission of this center is to help health care ministries of the Catholic Church address complex issues so that they may more effectively fulfill their missions. It does this through intentional and honest dialogue, faithful and creative scholarship, and practical consultations. Through the center’s work, the U.S. church and its ministries may more effectively witness to the dignity of human life and more compellingly communicate its vision for a just, equitable and compassionate society. The vision of this center is to be the most comprehensive resource for faithfully exploring how Catholic health care ministries can best serve in today’s world.
The executive director will be responsible for implementing the overall vision of the center and overseeing all related administrative duties; ensuring that the center has developed robust resources and expertise regarding culture and ecclesiology, justice and health equity, governance and identity, organizational ethics, vocation and diversity, and clinical bioethics. The executive director will ensure that the center is committed to transparent inquiry, dialogue over debate, theological rigor, and practical applicability. The executive director will assist in promoting a vision and understanding of the Catholic health ministry as an essential ministry of the Catholic Church, and duties will include serving as a spokesperson on theological and ethical issues facing Catholic health and maintaining effective relationships with other national organizations and CHA members.
To view a more detailed posting for this position, including a list of position requirements, visit the careers page on chausa.org.
Interested parties should direct inquiries to:
Cara Brouder
Sr. Director, Human Resources
Catholic Health Association
Phone: 314-253-3498
For consideration, please email your resume to HR@chausa.org.
Ky’Andre Vaughn got mentoring through Check & Connect. He graduated from high school this spring. He says the program taught him about the many opportunities and paths available to him.
From his experience, Vaughn says mentors at the Student Advocacy Center were there to listen along with providing guidance. “The biggest thing I learned was just to say yes,” Vaughn says. “There are a lot of different opportunities and paths.”
JOB
POSTING: EXECUTIVE DIRECTOR, THEOLOGY AND ETHICS CENTER
Lewis
March 1, 2022 CATHOLIC HEALTH WORLD 7 October 2023
DePaul clinics
From page 1 neighborhood that is just across the Mississippi River from New Orleans’ famous French Quarter. The Harvey clinic has more than double the space of the one it replaced that was next door in Gretna, Louisiana.
Meanwhile, a clinic that will be part of a 192-unit affordable housing development that is under construction is set to open in January in the Central City neighborhood. With that clinic’s opening, DePaul is closing a smaller nearby one.
Since the first clinic of what would become DePaul Community Health Centers opened in 1997, the network has grown to 11 standing clinics plus two mobile ones that it sets up across the city.
President and CEO Michael Griffin sees the expansion of space and access to services as evidence that DePaul is succeeding in its mission. “Our goal is to improve the health status of the entire community,” Griffin says.
From acute to community care
DePaul is part of St. Louis-based Ascension. DePaul’s roots go back to the Daughters of Charity congregation that began providing health care in New Orleans in 1834. When the congregation sold its Hotel Dieu Hospital in New Orleans in 1992, it shifted its focus from acute care to community care. Five years later, the congregation opened its first community clinic under the Daughters of Charity Services of New Orleans brand, later renamed to Ascension DePaul Services of New Orleans.
DePaul Community Health Centers, which is under the umbrella of Ascension DePaul Services, is a federally qualified health center. As such, it operates under specific guidelines, including taking direction from a board with a majority of members who are users of its services. Like all FQHCs, DePaul gets enhanced reimbursements for its services from Medicaid and Medicare. That extra funding is meant to offset the cost of a requirement that the clinics serve all patients, including those who are uninsured.
“We have a sliding fee scale for all of our clinics on all our services,” Griffin explains. “Individuals who don’t have any coverage or insurance can have a discount on services based on their household income.”
Jennifer Frizzell, vice president of population health and quality management, says DePaul counted about 50,000 unique patients — including 13,000 children — in 2022, about double the number from 2012. Of its patient population, 97% meet federal guidelines for low income and 87% identify as part of a racial or ethnic minority. Most of the patients qualify for Medicaid, Medicare or one of the low- or no-cost insurance programs on the federal marketplace.
Centralization improves DePaul’s care delivery
DePaul Community Health Centers continues to innovate to improve its care delivery process.
One change made in recent years was to go to centralized care coordination to handle all referrals to specialists.
Jennifer Frizzell, vice president of population health and quality management, says an example would be if a primary care physician orders a cardiology appointment. “We hand hold the patient through the entire process, making the appointments for them, making sure they get the necessary authorizations for any specialty care or testing, and then ultimately, making sure that the providers get a consultation or report back from the specialist closing that referral loop,” she explains.
Before the change to the centralized system, Frizzell says closing the loop took on average 71 days. That’s now down to about 22 days.
DePaul also centralized its call center to handle patient inquiries for appointments, prescription refills and such. Last year, it handled 287,000 inbound calls. When there is a letup on inbound calls, the call center’s workers reverse the process and phone patients to check on their health status and see if they are following care plans.
— LISA EISENHAUER
Paul Bryant is among DePaul’s patients. Bryant, 57, drives about an hour from his home in Donaldsonville, Louisiana, to a clinic to see his primary care doctor. He credits that doctor for helping to move him from a lethargic state in 2020 that left him weighing in at 350 pounds and dealing with hypertension and diabetes.
He since has begun to focus keenly on his health, including switching to a nosugar, plant-based diet and upping his exercise regimen. The changes have brought the weight on his 6-foot-2 frame down to 270. He’s also able to control his diabetes without medication.
Of the medical care he gets from DePaul, Bryant says: “I’m very comfortable and pleased with it.”
Team empowerment
DePaul offers a medical home to all its patients. In addition to primary care, its services include pediatrics, podiatry, dental, eye care and pharmacy services. The clinics have integrated behavioral health into primary care. New patients are screened for behavioral and mental health issues such as substance misuse and depression. All of the clinics have therapists on staff who can address mental and behavioral needs.
Dr. Robert Post, DePaul’s chief medical officer, has been with Daughters of Charity’s health ministry since the days of Hotel Dieu Hospital. He says that after Hurricane Katrina devastated New Orleans in 2005, the ministry rethought its care model and adopted one based on the Nuka System of Care developed in Alaska.

The model allows the various members of the care team — nurse care managers, community health navigators, behavioral health specialists and others — to use their unique roles and skill sets to meet patient needs without a direct order from someone else.
“It’s basically empowering every member of the care team to serve the patients directly without having to go through specific providers,” Post explains. “It’s made a huge difference, I think, in our outcomes.”
Needs beyond medical care
In addition to medical and behavioral health care, DePaul providers screen patients for social determinants of health needs, such as food insecurity and housing. Frizzell says the findings show the breadth of need in the New Orleans neighborhoods the clinics serve.

“The average patient here at DePaul Community Health Centers doesn’t have just one social determinant they’re trying to overcome,” she notes. “The average is actually seven, seven things in their life that are preventing them from putting themselves and or their health care as a priority.”
Patrice Paisley is part of the team of community health navigators that DePaul

employs to help patients meet those social needs. When care providers identify a need for nonmedical help, they flag Paisley’s team through the patient’s electronic medical record.
The team uses the Findhelp platform, formerly Aunt Bertha, to directly link patients to partner organizations that can assist with a myriad of services, including transportation, child care, utility assistance and access to healthy food. She has helped domestic violence victims find emergency shelter, a cancer patient get rental assistance and a teenage mother find a stroller for her newborn.
“We message the provider back and say ‘Hey, we got the flag. We provided this, this and this to the patient. Need anything else, let us know,’” Paisley says.
Paisley assists at the food giveaway that DePaul hosts the second Friday of every month in conjunction with the Second Harvest Community Food Bank. Anyone can come and get a box with fresh and shelfstable foods. The line for the giveaway typically stretches around the block. “I think we started with about 500 people and at our last pantry it was like 2,432 people,” Paisley says.
Caring for newcomers
To reach new patient populations, DePaul does continual community outreach. It sets up information tables about its services at health fairs and other community events.
Sr. Irma Vargas, DC, is one of DePaul’s patient and community engagement specialists. She keeps an office at the Society of St. Vincent de Paul New Orleans, which offers social services to those in need in the community, including newly arrived immigrants. Sr. Vargas informs St. Vincent’s clients of the health services available at DePaul and helps them enroll in insurance programs.
Often the immigrants are traumatized from their journey and in need of mental health care, Sr. Vargas says. It also is not uncommon for newcomers to be pregnant, infected with a sexually transmitted disease or in severe need of dental care.
Many of those she assists have come from Mexico and other Spanish-speaking countries. Spanish is her second language. But she also has assisted immigrants from Haiti, Korea, Vietnam and elsewhere. Among these newcomers, she says, are “the poorest of the poor,” or people with no resources or family support.
Sr. Vargas coordinates culturally informed care from DePaul Community Health Centers for anyone in need. “Jesus did not leave anybody behind and that’s our thing, too,” she says.
Training providers
Griffin says DePaul considers as part of its mission to train the next generation of community health care providers. It long has had relationships with medical, nursing and pharmacy schools in New Orleans to bring students into its clinics as part of their training. In more recent years, it has started its own residency program for physician assistants. It is in the process of adding family medicine and dental residencies.
Griffin is hopeful that the exposure to a community health care setting will convince some of the practitioners to stay. “There’s only a small percentage that do, because the bigger money in medicine is in cardiology and in all of these other types of specialties,” he notes.
Post says his support for the Daughters of Charity’s mission to improve the health of underserved communities has kept him in community health care. In his more than three decades with DePaul and its predecessor organizations, he’s been heartened by the dramatic expansion in services and patient population he has helped oversee.

“There’s a lot of people, a lot of communities that really depend on us to help manage their care,” he says.
leisenhauer@chausa.org
Residents line up for the weekly food giveaway at DePaul Community Health Centers’ headquarters in the Gert Town neighborhood in New Orleans. The giveaway is operated in conjunction with the Second Harvest Community Food Bank. Anyone who comes gets a box of fresh and shelf-stable foods.
Frizzell
Post
“The average patient here at DePaul Community Health Centers doesn’t have just one social determinant they’re trying to overcome. The average is actually seven.”
— Jennifer Frizzell
8 CATHOLIC HEALTH WORLD October 2023
Michael Griffin, president and CEO of DePaul Community Health Centers, leads a tour through a hallway lined with pictures related to the community health centers’ history. DePaul’s roots are in the ministry of the Daughters of Charity, a congregation that arrived in the city in the 1800s to provide health care.

 By JULIE MINDA
By JULIE MINDA
 By VALERIE SCHREMP HAHN
By VALERIE SCHREMP HAHN



 By VALERIE SCHREMP HAHN
By VALERIE SCHREMP HAHN