HEALTH PROGRESS

www.chausa.org
JOURNAL OF THE CATHOLIC HEALTH ASSOCIATION OF THE UNITED STATES
OUR
WINTER 2023 LIVING
CATHOLIC IDENTITY

➲ Beginning this January, join us as we renew our rhythms of well-being — intentionally, mindfully, prayerfully and communally. chausa.org/renewyear YEAR R E NEW START THE YEAR WITH A FOCUS ON WELL-BEING MISSION MONDAY • TIME TO THINK TUESDAY WONDER WEDNESDAY • THANKFUL THURSDAY • REFOCUS FRIDAY 20 23 I came
they might have life and have it more abundantly. — JOHN 10:10
so
DEPARTMENTS

WINTER 2023
2 EDITOR’S
BETSY
54
Survey Reveals Encouraging Trends — and Concerns —
Mission Leaders
58
BENEFIT CHA Guide Incorporates Equity Into All Aspects of Community Benefit JULIE
BSN, MS 61 ETHICS What Is Abortion?
PhD 65 AGING Mapping
Diversity, Equity and
in Aging Services JULIE
MS 68
Transforming Health in
Changing World
31 POPE FRANCIS — FINDING GOD IN DAILY LIFE 72 PRAYER SERVICE 4 MAINTAINING IDENTITY AND INCLUSIVITY IN CATHOLIC HEALTH CARE John O. Mudd, JD, JSD, and John Shea, STD 10 HARNESSING OUR POWER THROUGH CHARISM Fr. Joseph J. Driscoll, DMin 15 ENSURING QUALITY CARE MEANS PRIORITIZING THE MOST VULNERABLE: A Q&A WITH DR. ALISAHAH JACKSON Kelly Bilodeau 19 A GUIDE TO MAINTAINING CLINICAL TRIAL INTEGRITY IN CATHOLIC HEALTH CARE Pukar Ratti, CIM, CCRP, FACMPE, and Steven J. Squires, PhD, MEd 25 UNPRECEDENTED TIMES CALL FOR REVAMPED LEADERSHIP SKILLS Martin Schreiber, EdD 32 FLOURISHING THROUGH FORMATION: CATHOLIC IDENTITY IS REINFORCED WITH THOUGHTFUL APPROACHES Sarah Reddin, D.HCML 38 THE EVOLUTION OF SPONSORSHIP MODELS: A PROGRESS REPORT Fr. Charles Bouchard, OP, STD 45 WHY LISTENING MATTERS FOR BETTER UNDERSTANDING IN A DIVIDED CHURCH Bishop John Stowe, OFM Conv. LIVING OUR CATHOLIC IDENTITY HEALTH PROGRESS www.chausa.org WINTER 2023 1 HEALTH PROGRESS®
48 FINDING HEALTH: MAYBE WE NEED TO LOOK ELSEWHERE?
IN YOUR NEXT ISSUE THINKING STRATEGICALLY
NOTE
TAYLOR
MISSION
for Future of
DENNIS GONZALES, PhD, and JILL FISK, MATM
COMMUNITY
TROCCHIO,
BRIAN M. KANE,
the Road to
Inclusion
TROCCHIO, BSN,
THINKING GLOBALLY
a
BRUCE COMPTON
FEATURE
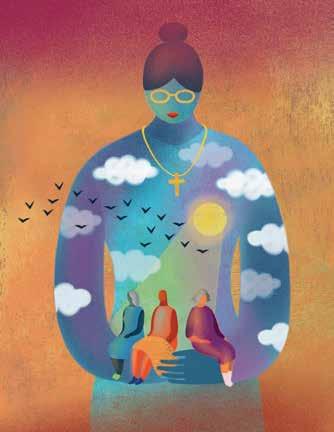
Alexander Garza, MD Illustrations
by Anna Godeassi
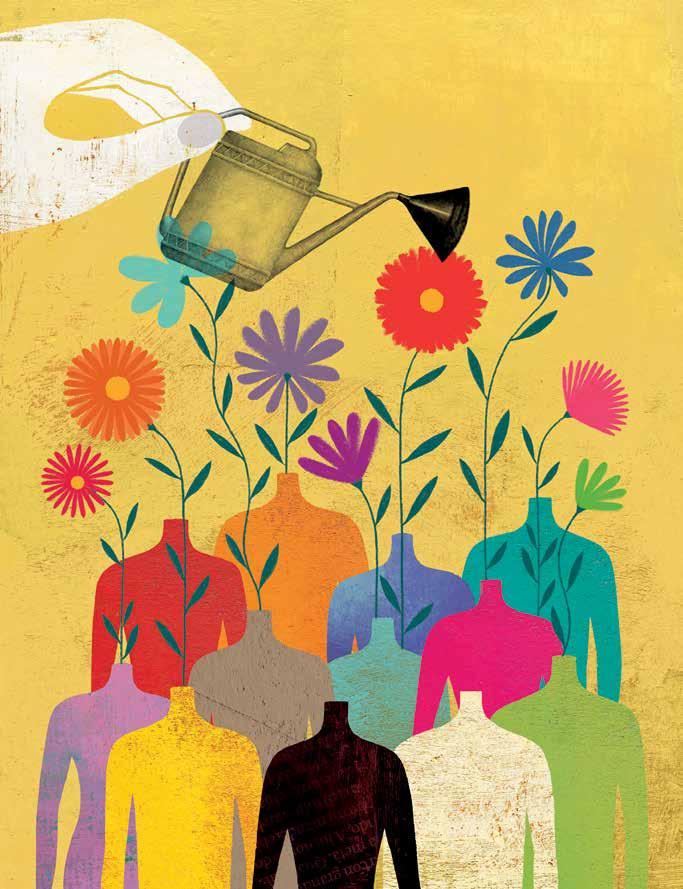
People long to connect with community, to believe their work is meaningful and to feel spiritually whole. At CHA, we’ve certainly been asked by the membership to focus on well-being and caring for the whole person.
because from the 1970s to the 2010s, Catholic Mass attendance in the United States dropped by roughly half, according to a survey highlighted in a recent National Catholic Register article. The less populated pews have become even more pronounced after the height of the COVID pandemic, as parishioners have not returned to prepandemic numbers.1
BETSY TAYLOR
And this issue of Health Progress, along with previous ones, reinforces that shared identity can make a difference in Catholic health care systems. In the opening article of this issue, two authors with longtime ties to Catholic health care, John Shea, STD, and John Mudd, JD, JSD, explain that they’ve found one of the best ways to allow Catholic identity to thrive is to not water it down. This includes not only using language and examples that others understand, and finding connections that resonate with people who have diverse backgrounds and experiences, but also knowing that the faith’s central messages resonate broadly and remain timeless and powerful.
Health Progress has included a few articles in recent issues where health care executives in human resources, mission and formation are increasingly collecting data, while from relatively small sample sizes, showing that the Catholic identity of the ministry work can be a recruitment and retention factor for some employees. Ascension’s Vice President of Ministry Formation and Mission Integration Sarah Reddin, D.HCML, makes that point in this issue as well, noting that one of Ascension’s leadership programs has found participants much more likely to stay with the system for at least two years than those who do not take part.
This resonates as being all the more striking
If we know the central, beautiful truths of Catholicism have lifted believers across millennia, and we know that people are actively seeking ways to feel connected and whole, is it possible that Catholicism needs to improve its invitation and approach, perhaps to focus less on what divides us, and more on what we share in common? That is, maybe not further refine the message itself, but instead its delivery?
While it is not a Catholic concept, one that I return to is tikkun olam from Judaism, the concept of engaging in acts of kindness to repair the world. As we embark on a new year, I am always filled with hope — hope that I may bring my best self both to my work and my life outside of it. And I also hold hope that as people search for meaning and healing, we may offer the hand of hope or healing they seek.
NOTE
1. Joan Frawley Desmond, “The Catholic Church Battles to Fill the Pews,” National Catholic Register, Dec. 1, 2022, https://www.ncregister.com/news/ the-catholic-church-battles-to-fill-the-pews.

EDITOR’S NOTE
2 WINTER 2023 www.chausa.org HEALTH PROGRESS
®
VICE PRESIDENT, COMMUNICATIONS AND MARKETING BRIAN P. REARDON EDITOR BETSY TAYLOR btaylor@chausa.org
MANAGING EDITOR CHARLOTTE KELLEY ckelley@chausa.org
GRAPHIC DESIGNER NORMA KLINGSICK
ADVERTISING Contact: Anna Weston, 4455 Woodson Rd., St. Louis, MO 63134-3797, 314-253-3477; fax 314-427-0029; email ads@chausa.org.
SUBSCRIPTIONS/CIRCULATION Address all subscription orders, inquiries, address changes, etc., to Service Center, 4455 Woodson Rd., St. Louis, MO 63134-3797; phone 800-230-7823; email servicecenter@chausa.org. Annual subscription rates are: free to CHA members; $29 for nonmembers (domestic and foreign).
ARTICLES AND BACK ISSUES Health Progress articles are available in their entirety in PDF format on the internet at www.chausa.org. Photocopies may be ordered through Copyright Clearance Center, Inc., 222 Rosewood Dr., Danvers, MA 01923. For back issues of the magazine, please contact the CHA Service Center at servicecenter@chausa.org or 800-230-7823.
REPRODUCTION No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission from CHA. For information, please contact Betty Crosby, bcrosby@ chausa.org or call 314-253-3490.
OPINIONS expressed by authors published in Health Progress do not necessarily reflect those of CHA. CHA assumes no responsibility for opinions or statements expressed by contributors to Health Progress.
2022 AWARDS FOR 2021 COVERAGE
Catholic Press Awards: Magazine of the Year — Professional and Special Interest Magazine, Second Place; Best Special Issue, Second Place; Best Layout of Article/Column, Second and Third Place; Best Color Cover, Honorable Mention; Best Guest Column/Commentary, First Place; Best Regular Column — General Commentary, Second Place; Best Regular Column — Pandemic, Second Place; Best Coverage — Pandemic, Second Place; Best Essay, First and Third Place, Honorable Mention; Best Feature Article, First Place and Honorable Mention; Best Reporting on a Special Age Group, Second Place; Best Writing Analysis, Third Place; Best Writing — In-Depth, Third Place.
Produced in USA. Health Progress ISSN 0882-1577. Winter 2023 (Vol. 104, No. 1).
Copyright © by The Catholic Health Association of the United States. Published quarterly by The Catholic Health Association of the United States, 4455 Woodson Road, St. Louis, MO 63134-3797. Periodicals postage paid at St. Louis, MO, and additional mailing offices. Subscription prices per year: CHA members, free; nonmembers, $29 (domestic and foreign); single copies, $10.
POSTMASTER: Send address changes to Health Progress, The Catholic Health Association of the United States, 4455 Woodson Road, St. Louis, MO 63134-3797.
Follow CHA: chausa.org/social
EDITORIAL ADVISORY COUNCIL
Trevor Bonat, MA, MS, chief mission integration officer, Ascension Saint Agnes, Baltimore
Sr. Rosemary Donley, SC, PhD, APRN-BC, professor of nursing, Duquesne University, Pittsburgh
Fr. Joseph J. Driscoll, DMin, director of ministry formation and organizational spirituality, Redeemer Health, Meadowbrook, Pennsylvania
Tracy Neary, regional vice president, mission integration, St. Vincent Healthcare, Billings, Montana
Gabriela Robles, MBA, MAHCM, vice president, community partnerships, Providence St. Joseph Health, Irvine, California
Jennifer Stanley, MD, physician formation leader and regional medical director, Ascension St. Vincent, North Vernon, Indiana
Rachelle Reyes Wenger, MPA, system vice president, public policy and advocacy engagement, CommonSpirit Health, Los Angeles
Nathan Ziegler, PhD, system vice president, diversity, leadership and performance excellence, CommonSpirit Health, Chicago
CHA EDITORIAL CONTRIBUTORS
ADVOCACY AND PUBLIC POLICY: Lisa Smith, MPA
COMMUNITY BENEFIT: Julie Trocchio, BSN, MS
CONTINUUM OF CARE AND AGING SERVICES: Julie Trocchio, BSN, MS
ETHICS: Nathaniel Blanton Hibner, PhD; Brian Kane, PhD
FINANCE: Loren Chandler, CPA, MBA, FACHE
INTERNATIONAL OUTREACH: Bruce Compton
LEGAL: Catherine A. Hurley, JD
MINISTRY FORMATION: Diarmuid Rooney, MSPsych, MTS, DSocAdmin
MISSION INTEGRATION: Dennis Gonzales, PhD
THEOLOGY AND SPONSORSHIP: Fr. Charles Bouchard, OP, STD
HEALTH PROGRESS www.chausa.org WINTER 2023 3

Maintaining Identity and Inclusivity in Catholic Health Care
JOHN O. MUDD, JD, JSD, and JOHN SHEA, STD Consultants on Catholic Leadership Formation Programs
In Catholic health care, an ever-changing workforce can present new opportunities to enhance and preserve its identity and culture. This endeavor — to tie one’s calling with the ministry’s mission — can, however, invite new challenges, especially when welcoming staff with increasingly diverse backgrounds that are both religious and nonreligious. Those who regularly encounter this dynamic know it has no easy resolution.
For the last 20 years, we have grappled with this issue in formation and administrative settings, working with hundreds of Catholic health care leaders. From our experiences, we offer lessons learned on some areas of concern. It is our hope that by continuing this vital conversation, Catholic health care can find new ways to carry on the healing ministry of Jesus.
TWO WRONG APPROACHES
Before offering our suggestions on how to respond to a changing workforce and its beliefs, while still remaining faithful to Catholic health care’s mission and identity, we first want to rule out two approaches that have been proven not to work — based on our time in Catholic health care. The first is trying not to offend those with different beliefs by avoiding language or engaging in practices that might be considered “religious” or “spiritual.” For example, recently a mission leader was asked to give a short reflection to a gathering of donors, but to not say “Jesus.”
The goal of this strategy — what might be called a “watered-down” approach — is to be sensitive. However, this tactic can result in excluding
conversations on topics and traditional practices that are central to the Catholic ministry’s identity.
A second approach is trying to blend the ministry’s mission and values with the dominant secular culture, perhaps even implying that the Catholic and secular cultures are virtually the same.
History is filled with examples of health care and educational organizations that are secular today but were founded within a religious tradition. Their transition from religious to secular was usually not the result of an intentional decision to drop their religious heritage, but rather the cumulative effect of small decisions and shifts in practice that eroded that tradition over time. Ultimately, the decision to become secular became merely a recognition of what had already occurred.
The result of either watering down the Catholic heritage or trying to blend it with secular culture is inevitably the loss of Catholic identity. Over time, the ministry becomes Catholic in name only — an organization that may still deliver quality health care, but is no longer connected with or defined by the Catholic tradition.
Instead of these fruitless approaches, we offer
HEALTH PROGRESS www.chausa.org WINTER 2023 5 LIVING OUR CATHOLIC IDENTITY
three principles to guide how the ministry can be faithful to its Catholic identity while still welcoming into the ministry people from diverse backgrounds.
Principle One: Values Alignment
Everyone who chooses to serve in a Catholic ministry must demonstrate their commitment to the ministry’s values. This is not optional. Only when the ministry holds staff accountable for living up to its values is the ministry itself being faithful to its identity. If a staff member fails to show respect for patients and colleagues, for example, that person does not belong in a ministry that professes the value of respect. Demonstrating a commitment to the ministry’s values does not mean being perfect, but it does mean that the everyday speech and behavior of those who work in the ministry must be in line with the values the ministry professes.
The source of the Catholic ministry’s values is its theological understanding of God, Jesus and the human person. Those with different religious or philosophical backgrounds are free to ground the values in their own traditions. For example, while everyone in the ministry must demonstrate respect for others and excellence in their work, they may base those values on their own philosophical or religious understanding. A Buddhist and a secular humanist will ground the values of compassion and respect differently. What is essential is that they demonstrate the values in their words and actions.
and experience? Similarly, the ministry’s performance evaluation process should assess whether employees’ words and actions are consistent with its values, and, if they fall short, it should have effective improvement plans and respectful ways to separate those who fail to improve.
It can be challenging to deal with a person who is failing to uphold the ministry’s values but who otherwise has valuable skills. The temptation is to overlook where the person exhibits deficits in the values of the ministry to retain their other contributions. Yet, if some staff get away with unacceptable behavior, that tells others the ministry doesn’t really care, and a “staff infection” spreads. On the other hand, when the ministry makes clear that everyone, even high-profile people, must demonstrate the values, the message also spreads that this ministry walks its talk and is faithful to its identity.
Principle Two: Respect
To ensure that all are committed to the ministry’s values, its hiring processes should include a focus on them and help those who are hiring determine if candidates have demonstrated values like respect, integrity, compassion and excellence. They should ask themselves: Is there evidence of those values shown in the person’s life
Those who choose to work in the Catholic ministry must show respect for its Catholic tradition and heritage, regardless of their own beliefs. When a person with different beliefs accepts the invitation to work in a Catholic ministry, it is like visiting the home of someone from a different culture. If the invitation is accepted, the guest is expected to respect the host’s culture. The same would be expected of Catholics who choose to work in a Jewish or Adventist hospital. For those working in a Catholic ministry, respect for its tradition includes participating in practices like reflections before meetings, celebrations of milestones in the ministry’s history, and orientation and educational programs that explain its heritage. Respect extends in a special way to the ministry’s organizational and ethical principles. One does not need to personally agree with the ministry’s principles and positions, but must show respect for them, and, consistent with their responsibilities, must follow them.1
Principle Three: Welcoming Diverse Traditions
The third principle is the reciprocal of the first two — the ministry must demonstrate respect for the diverse backgrounds of its staff. The model is Jesus welcoming everyone, including outsiders.
6 WINTER 2023 www.chausa.org HEALTH PROGRESS
Demonstrating a commitment to the ministry’s values does not mean being perfect, but it does mean that the everyday speech and behavior of those who work in the ministry must be in line with the values the ministry professes.
LIVING OUR CATHOLIC IDENTITY
Welcoming all who work in the ministry means at the outset not suggesting any effort to convert them. While it is essential to explain the tradition and heritage of the ministry in which they work, it must also be made clear that the ministry respects their beliefs and does not intend to proselytize or indoctrinate them.
In a formation program for senior executives, a question was asked of every group: “What do you not want to happen in this program?” The number one response in every cohort was, “No proselytizing.” The deep-seated fear was that the Catholic faith-based organization would try, in one way or another, to make converts. The prevalence of this suspicion suggests it has to be explicitly rejected.
A welcoming attitude can be demonstrated in many ways. One way is to show how the Catholic tradition, its stories, language and practices share elements with other traditions. When describing the value of compassion, for example, the ministry’s stories of compassion may be complemented with stories from other traditions. Jewish, Sufi and Buddhist traditions — to name a few — are rich with spiritual teachings and stories. Incorporating them shows a welcoming attitude and how the Catholic tradition shares values with others.
emphasis and why it is central to the ministry’s work.
Another way to show respect for those with different backgrounds is to avoid using “insider” language. Like others in the health care world — for example, clinicians, information technology specialists and accountants — Catholics have their own specialized terms. But using insider terms leaves some outside of the conversation and can generate confusion and misunderstanding. In explaining the Catholic tradition, it is essential to use language that is understandable and tailored to the role of the listener. A floor nurse may need to understand only a few Catholic terms, whereas an executive will need to understand and be able to use many.2
While it is essential to explain the tradition and heritage of the ministry in which they work, it must also be made clear that the ministry respects their beliefs and does not intend to proselytize or indoctrinate them.
A similar approach can be used in explaining the centrality of the Catholic social tradition. The newcomer may never have heard of any “social tradition,” much less one that is Catholic. It can help to start the explanation with what is familiar: all clinical professions share the humanitarian tradition of providing excellent, compassionate care and respecting patients, regardless of their personal or economic status. This humanitarian tradition includes working for the common good, or, as expressed in the U.S. Constitution, promoting “the general Welfare.” Religious traditions of the East and West also foster respect and care for others, especially those who are vulnerable. When explained in the context of humanitarian or other religious traditions, the Catholic social tradition becomes less mysterious and more like the Catholic dialect of a language newcomers have already heard. Starting with what is familiar also makes it easier to highlight the Catholic social tradition’s areas of
A number of words Catholics commonly use need explaining to those new to the ministry. Some examples include: What is a sister? (Few entering Catholic health care today have known, much less worked with, a Catholic sister.) What is a congregation, religious order, superior, province, provincial council or a charism? What is a layperson, bishop, archbishop, diocese or a hierarchy? What is a ministry, sponsorship or sponsor? What is canon law, the Vatican, a dicastery, a public juridic person, an ecumenical council or Vatican II? What are encyclicals or the ERDs, and what does preferential option for the poor, subsidiarity, and, more recently, synodality mean?
Words like these can be translated into more familiar terms. For example, an order of sisters’ “province” or a church “diocese” might be translated as a “region” or “geographic territory”; “canon law” as “church law”; a “public juridic person” as a “church corporation”; or a “dicastery” as a “Vatican department.” As with any translation, nuances from the original may be lost, but the listener will better understand the concept and will appreciate being welcomed into the conversation,
HEALTH PROGRESS www.chausa.org WINTER 2023 7
not left wondering what is being said.
Some of the ministry’s practices will also be unfamiliar to a newcomer. The practice of starting meetings with a reflection may be seen at first as a formality, something like singing the national anthem before a ballgame. Explaining that the reflection is a time to pause, be fully present, and connect the meeting with the mission and values can overcome the misinterpretation. The newcomer can learn to appreciate that the reflection should not be simply listening to a few pious words or a management quotation, but a time to consider the “why” of the work before diving into the “who, what, where and when.”
Catholic ministries have found creative ways to welcome those with different traditions. For example, when a Catholic system assumed ownership of a hospital serving a predominantly Jewish community, the hospital’s dedication ceremony included local rabbis placing mezuzahs at the entrances to patient rooms along with chaplains placing the traditional crosses. Another Catholic hospital set aside a special room where its Muslim staff and visitors could pray. Catholic hospitals have found ways to connect regularly with local religious leaders by inviting them to engage with the ministry and to teach hospital staff about cultural sensitivities of patients and ways to honor their healing and end-of-life customs. These are all ways the ministry maintains the interfaith openness of its Catholic identity.
The challenge of maintaining Catholic identity while being welcoming also arises when a Catholic ministry enters a close relationship with an organization that is not Catholic. While this complex topic is beyond the scope here, there is a parallel challenge of ensuring that the partner organization is committed to the values of the Catholic ministry and, if the Catholic identity is intended
to remain, that the ministry’s practices are not diluted or lost because of the relationship.
CONCLUSION
When the founding communities of sisters began to transfer the leadership of their ministries to laypersons more than a generation ago, some doubted that the ministries could remain Catholic without sisters at the helm. The widespread development of orientation and formation programs, along with maintaining cultural practices, have proven effective in keeping Catholic identity and heritage alive. An ongoing challenge is to engage Catholic health care’s increasingly diverse leaders and staff so they feel ownership of their ministry’s Catholic heritage and share the commitment to pass it on.
JOHN O. MUDD served as system mission leader for Providence Health & Services (now Providence St. Joseph Health) before retiring in 2016 and continued to assist with Providence St. Joseph Health’s formation programs.
JOHN SHEA is a consultant to faith-based organizations, dioceses and parishes, and provides theological, mission and formation services. He is working with Providence St. Joseph Health on Forming Formation Leaders and the Community of Formation Practice.
NOTES
1. Chad Raith, “How to Strengthen Catholic Identity in a Diverse Workforce,” Health Progress 102, no. 2 (Spring 2021): 63-68, https://www.chausa.org/publications/ health-progress/archives/issues/spring-2021/how-tostrengthen-catholic-identity-in-a-diverse-workforce.
2. Framework for Ministry Formation (St. Louis: Catholic Health Association, 2020), https://www.chausa.org/ store/products/product?id=4363.
8 WINTER 2023 www.chausa.org HEALTH PROGRESS
MINISTRY
FOR THE CATHOLIC HEALTH
INSPIRED BY THE SAINTS CONTEMPLATIONS
A series of huddle cards depicting the lives of seven saints who represent the core commitments of CHA’s Shared Statement of Identity. Featuring original artwork from Lydia Wood, St. Louis-based artist and activist. Visit chausa.org/saints to order your cards and accompanying audio files.
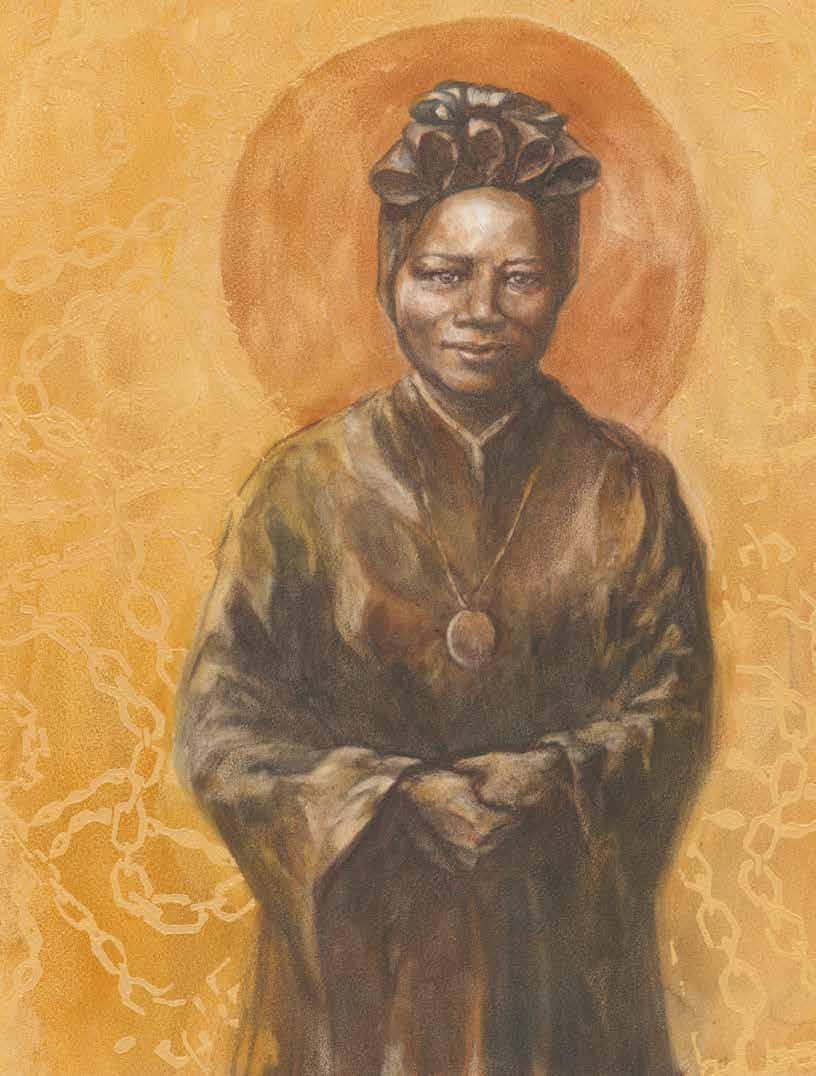 ST. JOSEPHINE BAKHITA
ST. JOSEPHINE BAKHITA
 LIVING OUR CATHOLIC IDENTITY
LIVING OUR CATHOLIC IDENTITY
Harnessing Our Power Through Charism
FR. JOSEPH J. DRISCOLL, DMin
He’s 50 years old. It’s the 1960s. A white Catholic priest is sent as pastor to St. JohnSt. Hugh’s Church in Roxbury, a small Black Catholic community in Boston’s inner city. He remembers well the hot summer day when his Baptist neighbors across the street invited him to their porch for a tall glass of cold lemonade.
Smiling in the retelling of the story years later, the priest, Fr. John Philbin, says, “I knew that with that invitation, I was no longer an outsider, but had been now accepted by my neighbors.”
Rocking back and forth in the porch chairs during the leisurely conversation that day, his neighbor suddenly turned to Fr. John and said, “You know, I know where you get your power from.”
Smiling, curious and somewhat amused, the priest replied, “You do?”
settings ever venture such a statement?
Even more telling, have we ever in the Catholic health ministry asked ourselves the question: Do we know where we get our power from?
Our powerhouse is the “real presence” of the Holy Spirit and a unique gift to a founder of a ministry that meets a need in specific times and circumstances that attracts others.
“Yes,” his neighbor said, pointing to the rectory across the street and the chapel’s bay windows. “From that box over there.”
His neighbor explained that he could see Fr. John sitting in the chapel every morning with his eyes closed, saying his prayers before he went out to do his day’s work.
The box, the “powerhouse,” was the tabernacle where the Blessed Sacrament was reserved. In the Catholic tradition, we believe that the real presence of Christ is in the consecrated hosts. Not just symbolically, but Christ truly present sacramentally in his body and blood.
CHARISM AS SOURCE AND POWER
“I know where you get your power from.”
Would the people coming into our ministry
Let’s be clear. We do not get this from our mission, values or vision. Those are all after the fact. Those statements are our reflection upon, discernment about, and articulation of an experience with the Divine power. A Divine power initiates a particular ministry and mission from a time past, sustains both in the present, and promises that ministry and mission in a future, yet unknown, time.
Our “box” is instead the “charism.” Our powerhouse is the “real presence” of the Holy Spirit and a unique gift to a founder of a ministry that meets a need in specific times and circumstances that attracts others.
And this presence still attracts others — and continues to do so in specific times and circumstances.
HEALTH PROGRESS www.chausa.org WINTER 2023 11
Charism, in the biblical and ecclesial tradition, is not generic. Charism is unique and specific to a story. No more than the Christ, the promised Anointed One of Israel, was generic, but rather born — and given the name Jesus in historical and narrative accounts — in a Jewish family in Palestine and in a specific time and circumstances.
This is an important point because presently, from Rome to some of our ministries here in the U.S., there are conversations about the possible emergence of a new charism generalized as “Catholic health care.” This use of the notion of charism is not supported by the tradition.
All our ministries share in common this healing ministry of Jesus Christ. Charism, however, is the coming of the promised Spirit, the impetus or power to establish these healing ministries of Jesus Christ with specificity, to the time and circumstances, and with particularity, to a spirituality emerging from a founder’s story and faith.
For the Sisters of the Redeemer, for example, this healing power of Jesus is viewed from, and experienced in, the cross. Essentially, the suffering before us in our ministries is united with the suffering of Christ, and the promise of “redemption,” something of worth is going to come out of this suffering, that the founder saw as bringing “life in fullness.”
From Paul’s letter to the Corinthians through to, and culminating with the rediscovery and renewal of charisms at, and following, the Second Vatican Council, these gifts are the real presence of the Spirit initiating, sustaining and promising our ministry and mission. Different perhaps; changed and changing, yes; but as Pope St. John Paul II asserts, even “in this newness, however, the Spirit does not contradict him[her]self.”1
CHARISM AS COMMUNITY SENT ON MISSION
At the end of Vatican II, the bishops writing in Perfectae Caritatis recognized the “wonderful variety of religious communities” and the way the gifts “differ according to the grace which is allotted to them.”2, 3 This diversity of gifts is represented in all the ways the Spirit initiates, sustains and promises a ministry and mission that meets the needs of God’s people, and in our case — in Catholic health care — those who are sick, suffering and dying.
Unique and particular to each institution’s founding and emerging story, charism, a particular gift, is of the one Spirit, and is the power and source of our ministry and mission. Charism is the real presence of the Spirit and the gift — then, now and always.
A charism is invisible, real, alive, active, moving and mysterious. It creates the ministry and discovers and discerns its mission.
Not only in our history, but now, every day, in every way, in every place, where we proclaim and live this ministry as a community sent by the Spirit in mission to the world, charism is present.
The irony in this is that we may have inadvertently undermined the power of charism present in our daily operations by creating our legacy walls and celebrating annually our founder’s feasts memorialized in time past. Charism is not past or passive.
Charism is invisible. Like the wind, it “blows where it wills, and you can hear the sound it makes, but you do not know where it comes from or where it goes; so it is with everyone who is born of the Spirit.” (John 3:8) We experience the charism even as we struggle to articulate this gift we cannot actually see, but true to the Gospel metaphor, we feel it like the wind.
Charism is real, active and moving. Like the Pentecostal experience of that first outpouring of the Spirit, “suddenly there came from the sky a noise like a strong driving wind,” and then there “appeared to them tongues as of fire, which parted and came to rest on each one of them.” (Acts 2:2-3)
This power felt from above was real, and experienced by individuals and the community. It is further described as active power, as they were “all filled with the Holy Spirit and began to speak in different tongues.” This power was then recounted as moving out to others, “devout Jews from every nation under heaven staying in Jerusalem,” for “at this sound, they gathered in a large crowd.” (Acts 2:4-6)
12 WINTER 2023 www.chausa.org HEALTH PROGRESS
Unique and particular to each institution’s founding and emerging story, charism, a particular gift, is of the one Spirit, and is the power and source of our ministry and mission.
LIVING OUR CATHOLIC IDENTITY
And finally, charism is mysterious. We cannot define it, but we can and must describe it.
The founders themselves did not define the ministry. They did not have a strategic plan and map for what would become their ministry and mission. It was first “an experience of the Spirit” that needed time “to be lived, safeguarded, deepened and constantly developed by them in harmony with the Body of Christ continually in the process of growth.”4
Even today, hundreds of years later, some of our present-day leaders of these founding religious communities still work to describe anew the “genuine originality”5 of their charism, while at the same time “scrutinizing the signs of the times and of interpreting them in the light of the Gospel. Thus, in language intelligible to each generation.”6
Mystery is the nature of the Holy Spirit. Ultimately, we cannot define either the Divine or the Divine’s actions in a word-limited sentence. Yet, we can and must describe with human words as best we can while approaching this mystery, and seek to uncover its meaning anew.
To notice, understand and appreciate charism makes more conscious the source of the ministry and the movement in mission. The sharper the awareness, the better the understanding; and the deeper the appreciation, the more it prepares each of us to recognize that this is ultimately God’s work through us. It is God calling us in vocation to this work.
brought forth by a creative and free Spirit. This Spirit brings unity in diversity and creates order out of chaos. These fruits of the charism are core to who we are (ministry) and what we do (mission) in the practical day-to-day.
CHARISM AS DAY-TO-DAY PRACTICALITY
The challenge is for our present-day ministry leaders and frontline staff to notice, understand and appreciate that there “is” an invisible power that moves above, underneath, inside and through the ministry community, and then outside as mission into the world.
This invisible power moves in every aspect of our ministry community, whether in direct care of patients and residents, or institutional structures such as our boards in deliberation, or strategies decided and acted upon at our management meetings. This invisible power is in our care delivery places, in our hallways and parking lots, as well as in our chapels and spiritual practices, everywhere, in every way, every day.
At Redeemer Health in Meadowbrook, Pennsylvania, we have been on a two-year initiative to help all our ministry partners become more aware of the charism in the ordinary, better understand the charism as a real presence in the now, and more deeply appreciate and watch for the charism in the day-to-day work of ministry and mission.
This invisible power is in our care delivery places, in our hallways and parking lots, as well as in our chapels and spiritual practices, everywhere, in every way, every day.
If charism is in fact that which distinguishes us from all other health care, nonprofit and forprofit alike, then it seems the focus on charism is critical for maintaining, enriching and renewing our Catholic identity. We need to consciously and actively go back to the source of our power. This charism is what moves us in our good works through a ministry community in a mission to the world.
We need to point back to God through Jesus’ revelation to us of a powerful love, one that is
Redeemer Health provides health care in Pennsylvania and New Jersey, including an acute care hospital, home health and hospice services, three skilled nursing facilities, personal care, a retirement community, low-income housing, an independent living community, a transitional housing program for homeless families, and multiple homes for intellectually and developmentally disabled adults.
Inspired by, and in response to, the 2019 general chapter of international congregation of the Sisters of the Redeemer — headquartered in Würzburg, Germany — we prioritized this formation initiative on charism. Their resolution mandated “the continued deepening and educating of Sisters and our partners in mission in Redeemer Charism and Spirituality.”7
With the support of the Redeemer leadership, a Redeemer charism and spirituality work group was formed in the fall of 2020 in order to oversee — even guarantee — the integration of charism
HEALTH PROGRESS www.chausa.org WINTER 2023 13
and spirituality in all we do. Assuring maximum buy-in from leadership, our CEO recommended the oversight group consist of two sisters, two sponsor board members, two board of trustee members and two executive leaders (the CEO and mission leader).
Through the group’s work, a program called “Charism Animators of Redeeming Love” has emerged, scheduled to begin in early 2023. It is a one-year program that will consist of 25 participants and begin with an initial retreat, gatherings every other month and a closing integrative retreat. The program’s impact will be measured through qualitative preprogram and postprogram surveys on charism.
The program’s two retreats are core to its effectiveness, as strengthening awareness of the invisible power of charism is a spiritual exercise that needs time and space. Quieting the outside noise allows people to become more sensitive to the inner movements and to the subtle, mysterious ways that we can become more aware of the Divine in and around us, especially in our day-today work in ministry.
Unlike other ministry formation programs, the attempt here is more akin to group spiritual direction, not so much the individual’s path, but the organization’s spiritual journey.
We hope that by heightening spiritual skills such as observation, listening, discernment and deliberation that our leaders will develop a curiosity, and take those skills back into their day-today work: to “sense” the invisible, name the experience and to help others appreciate this is the charism at work.
As these cohorts grow in number, we envision making these opportunities available to frontline staff through 15-minute reflection modules developed to increase this awareness, understanding and appreciation through the entire organization and the communities we serve.
CONCLUSION
As invisible and mysterious as our charisms may be, people who encounter us — staff, patients and residents — have an almost intuitive sense of this power and source in charism. How often do we hear people in our institutions say, “There is something different about coming here,” or, “I
have worked at many facilities, but this one just has a feeling that is unlike the others in which I have worked.”
Wouldn’t it be something to move from intuitive ambiguity of this “difference” to a more conscious and concrete affirmation of who and what it is that is moving through our ministry and mission everywhere, every day and in every way?
One of our sisters recently shared a powerful story that summarizes the power of charism.
During a lunch she had with a 95-year-old resident in assisted living — a long-time benefactor and friend of the ministry — her friend tearfully said to the sister, “I don’t know what it is with your people, but it seems they all have ‘it.’” She went on to ask, “Do they come in with ‘it’? Or do they absorb ‘it’ here? For me, it’s really profound.”
We know the ‘it’ is our invisible, real, alive, active, moving and mysterious charism at work as it was in past times, is now, and always will be.
FR. JOSEPH J. DRISCOLL is director of ministry formation and organizational spirituality for Redeemer Health in Meadowbrook, Pennsylvania.
NOTES
1. Pope John Paul II, Vita Consecrata, section 12, https://www.vatican.va/content/john-paul-ii/en/apost_ exhortations/documents/hf_jp-ii_exh_25031996_ vita-consecrata.html.
2. Second Vatican Council, Perfectae Caritatis, section 1, https://www.vatican.va/archive/ hist_councils/ii_vatican_council/documents/ vat-ii_decree_19651028_perfectae-caritatis_en.html.
3. Second Vatican Council, Perfectae Caritatis, section 8.
4. Sacred Congregation for Religious and Secular Institutes, “Directives for the Mutual Relations Between Bishops and Religious in the Church,” section 11, https:// www.vatican.va/roman_curia/congregations/ccscrlife/ documents/rc_con_ccscrlife_doc_14051978_ mutuae-relationes_en.html.
5. Sacred Congregation, “Directives for the Mutual Relations,” section 12.
6. Second Vatican Council, Gaudium et Spes, section 4, https://www.vatican.va/archive/ hist_councils/ii_vatican_council/documents/ vat-ii_const_19651207_gaudium-et-spes_en.html.
7. “Sisters of the Redeemer General Chapter Resolutions 2019,” Sisters of the Redeemer.
14 WINTER 2023 www.chausa.org HEALTH PROGRESS
Ensuring Quality Care Means Prioritizing the Most Vulnerable
A Q&A WITH DR. ALISAHAH JACKSON
KELLY BILODEAU Contributor to Health Progress
Alisahah Jackson, MD, is the first president of the new Lloyd H. Dean Institute for Humankindness & Health Justice at CommonSpirit Health. She stepped into this role in November 2022 after serving as CommonSpirit’s vice president of population health innovation and policy. As part of her mission to improve health equity, she helped to establish the system’s Vulnerable Populations Council. This interdisciplinary executive leadership group is improving care by creating initiatives to address social determinants of health and to support vulnerable patients across the organization. The 25-member group coordinates with the Vulnerable Populations Care Collaborative, an assemblage of clinical leaders who put these strategic plans into use across the organization, which includes more than 1,000 care sites and 140 hospitals in 21 states. Health Progress recently spoke with Jackson about the council and its goal of promoting quality care.
Can you tell me about the origins of the Vulnerable Populations Council and how CommonSpirit Health addressed vulnerable populations prior to its formation?
One of my responsibilities was to help our system think through how we care for our vulnerable populations. What I found when I got here was that there were so many departments and providers doing great work and taking care of what we may consider vulnerable populations. But it was very siloed. As I learned more and more, I said we really need to have some sort of infrastructure that can bring all these people together: 1) to acknowledge, recognize and celebrate the great work that they are doing; 2) to identify where there are opportunities to align work; 3) to leverage some of those best practices; and then ulti-
mately, 4) to start thinking about how to measure our work, so that we can speak to the outcomes that it is having. That’s how the Vulnerable Populations Council came about.
What was the council’s first initiative?
We realized pretty early on, as the conversations were happening nationally around COVID, that communities of color were disproportionately affected. We were seeing that in our facilities as well as in the national data. So, we educated our communities on that information and other risk factors. People with chronic medical conditions like diabetes and asthma were at higher risk, and we presented that information in a way that was culturally sensitive to those communities that were disproportionately affected.
HEALTH PROGRESS www.chausa.org WINTER 2023 15 LIVING OUR CATHOLIC IDENTITY
We realized that we needed a process to do that. So, we worked with our marketing and communications teams to create material. They vetted it through the Vulnerable Populations Council, making sure that from a health literacy standpoint, it was at a basic reading level, using a lot of graphics and pictures to try to get the information out there.
We also had to create educational materials for our providers as well — that was an ongoing process. We were updating the information as more was coming out from the CDC and other studies. We were updating our providers on that new information.
And then, as the vaccine became available, we recognized that communities that were disproportionately affected were also hesitant to get the vaccine. So, we created a whole vaccineawareness campaign. We went into those communities in a lot of our markets, partnering with trusted community providers and organizations, like churches, universities, and of course, public health departments. It required multiple organizations coming to the table, but getting out of this mindset of always expecting the patient to come to us, the care provider, and instead for us to really get out into the community. We had multiple vaccination events, including drive-through clinics, at community locations, like schools and churches, and at farms with migrant workers. That was extremely powerful, and we were able to serve so many more patients.
How did you track your outcomes?
For COVID, we had a COVID dashboard created by our organization’s quality and data analytics teams and patient-safety leader. We were able to look at everything from hospitalizations to vaccine administration. We could leverage heat maps [graphs that show the values of data represented by a color scale] — actually even look at the zip code level — to see how we were doing. I can’t stress enough the need for collaboration, and having the data to support and validate the work that we were doing.
Are there other council-driven changes that have made a difference in patient health?
Health literacy — clearly that was a big focus as it related to COVID. But we started to realize that we had that same issue across a lot of our different patient-education materials and information. We formed a committee to specifically focus on health literacy across our organization that also includes language services. So, making sure that we have the appropriate resources for language services in the communities we serve, and recognizing that those needs are different for each community.
There are also some things that we focused on standardizing; for example, how we collect information around someone’s preferred language. With the work on COVID, we recognized that we weren’t consistently capturing that information in all of our markets but that it was something we needed to do.
CommonSpirit Health uses a broad definition when defining vulnerable populations, noting that all are vulnerable at times. For the council’s work, Dr. Alisahah Jackson explains they prioritize populations that are systematically excluded, face significant health disparities and are often invisible. These groups include, but are not limited to, communities of color, LGBTQ+ people and those with low health literacy.
 Dr. Alisahah Jackson
Dr. Alisahah Jackson
16 WINTER 2023 www.chausa.org HEALTH PROGRESS
How do you collect information about your patient populations?
Information collection is done as a part of the registration process. Our Office of Diversity, Inclusion, Equity and Belonging, which participates in the Vulnerable Populations Council, really took that on. They expanded the work around how we’re collecting race, ethnicity and language data in a consistent, standardized way. One example includes working with our vendors, like those who support our electronic health records, to make sure that those fields are standardized throughout our different systems. And then training our staff on the best practice for allowing the patient to self-identify [or allowing them to choose not to disclose] those characteristics, but also recognizing that we needed to actually train our staff to feel comfortable having that conversation with the patient. We also train them to explain to the patient why we are now being much more intentional about collecting that data.
How has obtaining that type of detailed information helped your organization?
This year we are really leveraging that information to look at some of our quality measures. I think this is what hospitals and health systems should be doing, even though it’s not necessarily a requirement, just yet. I think that will likely be changing as well, given some of the guidelines that you’re seeing from the Centers for Medicare & Medicaid Services and other payers. It allows us to do a deeper dive into how we’re doing on quality.
I think that’s important because often when we aggregate data, we may get a false sense of our performance. Without the ability to start to disaggregate that data to look at specific populations, we may not realize that there’s a certain population that, for example, doesn’t have good diabetes control. Or maybe there’s a specific clinic where patients don’t have good diabetes control. Often, I would say it’s more due to process or resource issues versus it being that the doctor is treating that patient with bias. Nine times out of 10, that is not the case. It usually does go back to a system that is perpetuating disparities. So, we have to get to the root cause of what’s happening in that system, in that process, that’s contributing to the problem. That’s how we’re now able to leverage the data around race, ethnicity and language.
LIVING OUR CATHOLIC IDENTITY
Have you learned anything surprising from your data?
I do think that for some of my colleagues, there have been eye-opening moments. One has been assuming that processes are working as designed. If you actually go and do the deep dive or an audit, you often find that the process isn’t necessarily working as designed. One example I can give is around blood pressure control. In some offices, we saw a discrepancy around blood pressure control for a certain patient population. So, we dove deeper into what was going on. There’s a best practice around taking blood pressure. If a patient comes into an office and their blood pressure is elevated, you let them sit in the office for about 10 minutes in the exam room and let them kind of calm down. Then, you go back in and recheck it. And what we found is that the medical assistants saw significant turnover. Even though they had received training on this, they weren’t consistently doing that blood pressure recheck. That’s a process issue. We had to retrain them and make sure that providers knew to look for the documentation of a second blood pressure if it was noted as elevated, and if not, rechecking it themselves. And that actually improved some of the numbers that we were seeing. So, I think that’s just an example of what you can do from a quality improvement standpoint if you’re looking at the data in a different way.
Do you think that the council will help your organization to improve outcomes among vulnerable patients?
I definitely do because this council is specifically focused on caring for the vulnerable and making sure that we keep that front and center as we do our work. For us, it’s a part of our mission and remaining true to it. I think having this space, where people feel comfortable and safe in bringing up some of their concerns, has been really helpful. I want to emphasize that, because I think sometimes those spaces aren’t created for these types of conversations. I do think that’s been a huge driver for some of the initiatives and programs, and, quite frankly, the outcomes that we’ve now been able to look at on the organizational level.
KELLY BILODEAU is a freelance writer who specializes in health care and the pharmaceutical industry. She is the former executive editor of Harvard Women’s Health Watch. Her work has also appeared in The Washington Post, Boston magazine and numerous health care publications.
HEALTH PROGRESS www.chausa.org WINTER 2023 17
Earn
your advanced degree in Healthcare Ethics
Duquesne University offers an exciting graduate program in Healthcare Ethics to engage today’s complex issues.
Courses are taught face-to-face on campus or through online learning for busy professionals.
The curriculum provides expertise in clinical ethics, organizational ethics, public health ethics and research ethics, with clinical rotations in ethics consultation.
Doctoral students research pivotal topics in healthcare ethics and are mentored toward academic publishing and conference presentation.
MA in Healthcare Ethics (Tuition award of 25%)
This program requires 30 credits (10 courses). These credits may roll over into the Doctoral Degree that requires another 18 credits (6 courses) plus the dissertation.
Doctor of Philosophy (PhD) and Doctor of Healthcare Ethics (DHCE)
These research (PhD) and professional (DHCE) degrees prepare students for leadership roles in academia and clinical ethics.
MA Entrance – 12 courses
BA Entrance – 16 courses

Graduate Certificate in Healthcare Ethics
This flexible program requires 15 credits (5 courses). All courses may be taken from a distance. The credits may roll over into the MA or Doctoral Degree (PhD or DHCE).
Questions?
or chce@duq.edu
412.396.4504
duq.edu/globalhealthethics
LIVING OUR CATHOLIC IDENTITY
A Guide to Maintaining Clinical Trial Integrity in Catholic Health Care
PUKAR RATTI, CIM, CCRP, FACMPE System Director, Research and Academics, CHRISTUS Health STEVEN J. SQUIRES, PhD, MEd Vice President of Ethics, CHRISTUS Health
Those who don’t do clinical research in Catholic health care settings may hope a program can grow “despite” its faith-based setting. Those of us who do this work in faith-based organizations realize these settings can be truly beneficial and structured to allow ethical and significant research programs to grow and thrive. At the CHRISTUS Institute for Innovation and Advanced Clinical Care, we infuse Catholic identity, Church teaching and mission — along with federal regulations and clinical research operations — into all of the institute’s operational processes. The impact of this integration goes far beyond regulatory compliance for those involved in CHRISTUS Health’s nearly 700 active clinical studies and more than 10,000 participants.
This standardization and incorporation of mission and ethics into the program’s operations fuels the growth of CHRISTUS Health’s clinical research programs. The health care system has developed informational resources and makes subject matter experts available to sponsors and scientific investigators to ensure research protocols and practices are appropriate to a faithbased setting. In fact, the average time from a new study’s submission to the research central office until its launch at CHRISTUS Health is less than 75 days, compared to the industry’s average of 90 days. We believe that our approach would be useful to others in Catholic health care, and to mission- and values-driven secular health care. Our hope is that others find insights from this model and replicate its components for their clinical research programs. Throughout the COVID-19
pandemic, those working in health care so often saw how clinical research advances life-saving treatments.
ABOUT THE INSTITUTE
Driven by the mission to extend the healing ministry of Jesus throughout its work, CHRISTUS Health offers coordinated and organized advanced clinical care and research for patients through its Institute for Innovation and Advanced Clinical Care. The institute is an integrated, multidisciplinary enterprise that provides strategic planning, expert consultation and catalyst support services for clinical research growth across the health system. It includes a system office that delivers essential services to conduct and support research, such as an institutional review board, compliance, research education,
HEALTH PROGRESS www.chausa.org WINTER 2023 19
finance and reporting, and pre- and post-award services for clinical research studies.
The participating ministries of CHRISTUS Institute for Innovation and Advanced Clinical Care are organized across the United States into five geographic regions: 1) Louisiana, 2) Southeast Texas, 3) South Texas, 4) Northeast Texas and 5) New Mexico. Each of these five research hubs is led by a research leader — who reports to one system research executive. This forms a hub-and-spoke organizational chart, where one major location serves as a central point for coordinating clinical research initiatives to and from other locations. Some of the major clinical research focus areas at CHRISTUS Health include oncology, cardiology, electrophysiology, pediatrics, neurology, COVID19 and wound care.
ENSURING ERD INTEGRATION INTO CLINICAL RESEARCH
To affirm integration of the Ethical and Religious Directives for Catholic Health Care Services (ERDs) into relevant clinical research matters, the institute created and deployed a multi-integrated operating model. (See graphic on page 21). To ensure its success, relevant stakeholders were involved during each step. Internally, we refer to these stages through the acronym “FIRE CONTROL.”
1. Feasibility Review
The first step in the process is the feasibility review, which is an internal review that involves research leaders, local mission leaders, senior leadership team members and other department leaders who use a feasibility analysis tool to assess together if the clinical research project is an operational fit for the ministry. The tool captures and documents responses to a series of questions in six major categories: mission alignment; patient population and recruitment; study design; local operations and support; contract and research coverage analysis; and budget.
The review’s mission alignment section allows each evaluator an early opportunity to assess whether the clinical research project abides by the ERDs by reviewing elements that may conflict with Catholic teaching. Examples include sterilization, some types of gene therapy or genetic modification of human tissue, or use and/ or distribution of contraception. This section also
checks if the project plans to exclude research participants with limited English proficiency, unless clinically justifiable. If any aspects of research are identified as not aligning with the ERDs or Catholic teaching, identity or mission during feasibility assessment, it is either immediately rejected or returned for appropriate revisions. For instance, a sponsor requested CHRISTUS Health participation in a clinical trial for a medicine used to treat infertility. The research protocol required sites to keep and distribute contraceptives. CHRISTUS’ clinical research institute deemed the study ‘not feasible’ after failing to find an appropriate alternative.
2. Informed Consent Form Review
For some medium- to high-risk clinical research projects, a pregnancy prevention clause may be necessary within the research informed consent form for those initiatives that require disclosure per policies set forth by the Office for Human Research Protections and/or the Food and Drug Administration (FDA).1, 2 A research informed consent form is typically a description of clinical investigation, risks, benefits, participation fees, confidentiality, compensation and/or medical treatment for injury, voluntary participation and more. CHRISTUS Health’s institutional review board requires that the standard language for pregnancy prevention be used in all applicable research-informed consents, in addition to all parental permission and participant agreement forms for subjects aged 13-17 years.
As a Catholic ministry, CHRISTUS Health provides standard clauses that avoid unethical actions within CHRISTUS Health (moral agency) or associated with CHRISTUS Health (moral cooperation) by emphasizing appropriate birth regulation means and not specifying certain pregnancy prevention means via inclusion of approved template language. In 2016, we developed a series of seven standard clauses — ordered from most preferred to least preferred — to allow flexibility for our clinical research sponsors and investigators. After review in 2021, our mission and ethics leaders developed two standard clauses in English and Spanish in lieu of the prior seven standard clauses to capture pregnancy precautions during and after study. If any adaptations of the standard clause result, they require reapproval by mission and ethics leaders before the clinical
20 WINTER 2023 www.chausa.org HEALTH PROGRESS
research project can be submitted for ethical and board review.
3. Institutional Review Board/Ethics Review
Under FDA and Department of Health & Human Services regulations, all human subject research must be reviewed by an institutional review board prior to its start. Furthermore, the board should consist of reviewers with both scientific and nonscientific backgrounds, and not affiliated with the institution to ensure a balanced scientific and ethical review that protects participants’ rights, integrity and welfare.3, 4
CHRISTUS Health’s institutional review board consists of additional reviewers, such as ethicists and mission leaders, to ensure alignment with Catholic teaching, the ERDs and protection of the most vulnerable populations (such as children, elderly, those who are poor and racial minorities). Additionally, to better serve our communities, CHRISTUS Health has established several academic partnerships — both Catholic and nonCatholic. By combining our strengths on research, these academic partnerships enable our communities more access to research participation without compromising our identity or integrity.
4. Contract Review
As part of launching a clinical research project, CHRISTUS Health enters into contractual agreements with all legal parties involved. These agreements allow for the legal exchange of clinical research funding, materials and data between the two parties, and memorializes the rights and obligations of each party. In each clinical research agreement at CHRISTUS Health, the parties are required to acknowledge that 1) CHRISTUS Health is a faith-based organization, 2) all operations at CHRISTUS Health are in accordance with the ERDs, as interpreted by a local bishop, and 3) CHRISTUS Health’s operations — in accordance with the ERDs — and its principles and beliefs of the Roman Catholic Church are a matter of conscience. If CHRISTUS Health were to determine that any aspect of an arrangement would violate the ERDs, the options are to work together in good faith to resolve or terminate participation. Secondly, our health system ensures that each clinical research agreement is accompanied with a fair reimbursement and payment schedule for services rendered to remain
Research Review for Mission Alignment A look at the stakeholders responsible for each aspect of CHRISTUS Health’s “FIRE CONTROL” operating model. FEASIBILITY REVIEW • Regional Research Leaders • Research Executive • Ethics Executive • Mission Leaders FIRE CONTROL OPERATING MODEL COMPONENTS • Stakeholders INFORMED CONSENT FORM REVIEW • Regional Research Leaders • Research Coordinators and Nurses • Institutional Review Board • Ethics Executive • Research Sponsor INSTITUTIONAL REVIEW BOARD/ ETHICS REVIEW • Institutional Review Board CONTRACT REVIEW • Legal Counsel • Contracts Analyst • Research Sponsor POLICIES AND STANDARD OPERATING PROCEDURES • Research Executive • Institutional Review Board Staff INITIAL AND ONGOING EDUCATION • Research Executive • Institutional Review Board Staff LANGUAGE ACCESS SERVICES • Research Coordinators and Nurses • Language Access Service Vendors • Health Equity, Diversity and Inclusion Department Source: CHRISTUS Health HEALTH PROGRESS www.chausa.org WINTER 2023 21 LIVING OUR CATHOLIC IDENTITY
responsible stewards of health care resources. Thirdly, we aim for favorable language in clinical research agreements for our patients (especially those in vulnerable situations) to ensure that there is a clear arrangement on how patients will be compensated in the rare event of a clinical research-related injury.
5. Policies and Standard Operating Procedures
Clearly written policies and standard operating procedures eliminate uncertainty, ambiguity and/ or misinterpretation about how to apply the ERDs in clinical research. These allow CHRISTUS Institute for Innovation and Advanced Clinical Care to follow standardized processes and reduce errors. Some of the clinical research policies in effect cover topics such as research-informed consents, language access services and institutional review board, to name a few.
6. Initial and Ongoing Education
CHRISTUS’ clinical research institute is committed to providing comprehensive initial and ongoing education opportunities to its clinical research workforce, medical residents and fellows, institutional review board members and physician investigators involved in its clinical research. As part of this effort, the institute rolls out an annual lecture series program on good clinical practices. Subject matter experts give bimonthly presentations on relevant and timely topics, including lectures specific to Catholic teaching, such as the “ERDs and Clinical Research” and “Ethical Research.”
7. Language Access Services
Access to language services is not only about potential research participants, but also for all those impacted by the study’s clinical research results and validity. Excluding groups with limited English proficiency from studies leads to biased and exclusionary results, not only with medications and treatments, but clinical protocols and algorithms.5 As noted by specific directives in the ERDs, duties to the community and vulnerable persons compel Catholic health care to minimize any communication barriers to prevent further exclusion (beyond those of the study) and the growth of any existing vulnerabilities.6
Secular rules are in unison with faith-based commitments. Since 1964, the United States has
passed a series of acts, laws, executive orders and regulations to enhance language access services to all in health care. Provisions in federal government and FDA regulations require investigators to obtain informed consents in a language that is understandable to the clinical research participant or their legally authorized representative.7, 8
The CHRISTUS Institute for Innovation and Advanced Clinical Care ensures fair and equitable selection of volunteer research subjects for its clinical trials and research projects and therefore promotes health equity, diversity and inclusion. This commitment encourages potential clinical research subjects who altruistically volunteer despite any English-speaking barriers, including non- or limited-English proficiency, deafness and hearing difficulties.
We have set the tone for reliable and consistent language access services at the system level for all our patients by establishing a system policy, adopting standardized processes and retaining credible vendors. We provide our clinicians and other team members with the tools necessary to deliver language access services through: 1) live/ onsite professional interpretation, 2) qualified bilingual staff, 3) document translation, 4) video remote interpretation and 5) over-the-phone interpretation.
In addition to these day-to-day steps related to clinical care, CHRISTUS Health requires the fulllength informed-consent document to be translated into the subject’s language. We also use a CHRISTUS-approved bilingual witness for clinical research studies with linguistic distribution of more than 1,000 study subjects, or more than 5% of the study’s subject population (whichever is greater). In addition, we use a translated shortform consent with a CHRISTUS-approved bilingual witness for clinical research studies with linguistic distribution of less than 1,000 study subjects or lower than 5% of the study subject’s population (whichever is smaller). These services are available at no cost to clinical research subjects and their legally authorized representatives. Per our policy, we do not allow minors or family members of patients to serve as interpreters during the informed-consent process.
As a result of the use of professional interpreters and translators in clinical research, many benefits emerge, including the assurance of clinical research participants’ understanding,
22 WINTER 2023 www.chausa.org HEALTH PROGRESS
LIVING OUR CATHOLIC IDENTITY
upholding the quality and efficiency of interpretation services, and reducing or eliminating clinical research participant safety risks to study participants due to misinterpretation.
MODEL’S IMPACT ON CLINICAL RESEARCH
Having mission- and ethics-based standards that go beyond federal regulations and expanding clinical research programs are not mutually exclusive. Faith-based or not, it is imperative that all clinical research institutions follow applicable federal regulations. Sometimes these regulations may conflict with the Church’s teachings. Examples include pregnancy prevention methods, gene therapy research and selection of subjects. However, our FIRE CONTROL operating model helps to maintain the delicate balance between the ERDs, federal regulations and clinical research operations.
CHRISTUS Health’s clinical research institute has expanded significantly while hardwiring mission, identity and teachings rooted in sources such as the ERDs. Since the application of our innovative operating model, the total number of active clinical research studies has more than doubled in the last five years, including a growth of 28% in fiscal year 2021 (compared to the previous fiscal year) — despite the period’s height of COVID-19 cases — and a continued growth of 12% in FY2022, so that the system is involved in almost 700 studies a fiscal year. Furthermore, the number of our research participants per fiscal year has consistently been between 10,000 and 15,000 since FY2017, and we continue to recruit from diverse populations.
CONCLUSION
By sharing our FIRE CONTROL operating model, we hope others may draw from it to find new ways to advance the care provided through clinical research. By using clinical research that is innovative, ethical and financially responsible, not only can we improve the experience of research participants and the potential study outcomes, we can help to ensure the human dignity of every patient.
PUKAR RATTI is system director of research and academics at CHRISTUS Health in Irving, Texas. STEVEN J. SQUIRES is vice president of ethics at CHRISTUS Health in Irving, Texas. He was recognized as a member of the CHA 2016 class of Tomorrow’s Leaders.
NOTES
1. “2018 Requirements (2018 Common Rule): 45CFR46.116,” U.S. Department of Health & Human Services, January 2019, https://www.hhs.gov/ohrp/ regulations-and-policy/regulations/45-cfr-46/ revised-common-rule-regulatory-text/index.html.
2. “CFR–Code of Federal Regulations Title 21: 21CFR50 Subpart B,” U.S. Food and Drug Administration, July 2022, https://www.accessdata.fda.gov/scripts/cdrh/ cfdocs/cfcfr/CFRSearch.cfm?CFRPart=50.
3. “Title 45: Part 46 — Protection of Human Subjects,” Electronic Code of Federal Regulations, July 2018, https://www.ecfr.gov/on/2018-07-19/title-45/ subtitle-A/subchapter-A/part-46.
4. “CFR–Code of Federal Regulations Title 21,” U.S. Food & Drug Administration, July 2022, https:// www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/ CFRSearch.cfm?CFRPart=56.
5. Gau Bugeja, Ajay Kumar, and Arup Banerjee, “Exclusion of Elderly People from Clinical Research: A Descriptive Study of Published Reports,” British Medical Journal 315, no. 7115 (October 1997): 1059, https:// doi.org/10.1136/bmj.315.7115.1059; Susan Reverby, “Inclusion and Exclusion: The Politics of History, Difference, and Medical Research,” Journal of the History of Medicine and Allied Sciences 63, no. 1 (January 2008): 103-13, https://doi.org/10.1093/jhmas/jrm030; Darshali Vyas, Leo G. Eisenstein, and David S. Jones, “Hidden in Plain Sight — Reconsidering the Use of Race Correction in Clinical Algorithms,” The New England Journal of Medicine 383, no. 9 (August 2020): 874-882, https:// doi.org/10.1056/NEJMms2004740.
6. United States Conference of Catholic Bishops, “Directive 3” and “Directive 8” in The Ethical and Religious Directives for Catholic Health Care Services: Sixth Edition (Washington, DC: United States Conference of Catholic Bishops, 2018).
7. “Title 45,” Electronic Code of Federal Regulations. 8. “Title 21,” U.S. Food & Drug Administration.
HEALTH PROGRESS www.chausa.org WINTER 2023 23










CONTENTS INCLUDE: Complete searchable version of the Ethical and Religious Directives for Catholic Health Care Services Glossary of important ethics terms Collection of relevant articles and resources addressing important clinical issues in Catholic health care
Info at Your Fingertips! FOR CHA MEMBERS CHA’S ETHICS APP is a valuable collection of ethics information for clinicians who provide patient care and for the ongoing education of ethicists, mission leaders, ethics committees and clinicians in Catholic health care. To download the app, visit www.chausa.org/EthicsApp (member login required)
Ethics
Unprecedented Times Call for Revamped Leadership Skills
MARTIN SCHREIBER, EdD Vice
“A health care organization that is efficient and capable of addressing inequalities cannot forget that its raison d’être … is compassion ... .” 1
— Pope Francis
The COVID-19 pandemic accelerated a reimagination of our current models of health care and intensified the focus on health equity for those who are poor and vulnerable, while bringing with it a cadre of additional and complex leadership challenges. Successful leadership in this age of health care requires a renewed leadership focus on mission, purpose and vision, along with updated strengths and skills to best advance the healing ministry of Jesus.
In response to these challenges, Providence is preparing leaders in new ways, beginning with a commitment to individual self-discovery, compassion and whole-person leadership. As noted by author and psychiatrist Elisabeth Kübler-Ross, “People are like stained-glass windows. They sparkle and shine when the sun is out, but when the darkness sets in, their true beauty is revealed only if there is a light from within.”2 Advancing Catholic health care’s mission will require us to think differently. At Providence’s Mission Leadership Institute, we think of individuals on a pilgrimage with caregivers walking a path to selfdiscovery. To support leaders’ introspection, this work toward personal growth takes some nontraditional approaches to break down the walls that protect our weaknesses and fears, to recognize our own biases and to confront our vulner-
abilities. This extraordinary time in health care has made us realize that an honest examination by leaders of their internal inventory can help build their personal resilience. We believe in aiding them as they develop a wealth of resources. By drawing upon these helpful tools, our leaders can be better equipped to support and motivate others.
SHAPING LEADERS FOR HEALTH CARE’S FUTURE
During the volatile period triggered by the pandemic, Catholic health care systems experienced a variety of unprecedented events: the need to rapidly and skillfully care for unusually high volumes of patients; to adapt to immediate technological changes; and to coordinate rapid responses to urgent health inequities. A level of “mission fragility,” a genuine concern about being
 President, Providence Mission Leadership Institute, Providence St. Joseph Health
President, Providence Mission Leadership Institute, Providence St. Joseph Health
HEALTH PROGRESS www.chausa.org WINTER 2023 25
LIVING OUR CATHOLIC IDENTITY

LIVING OUR CATHOLIC IDENTITY
able to meet needs and to respond to patients and other care providers in the way we are called to do, was introduced. It warranted an urgent redesign of leader preparedness. Leadership success demanded quicker responses, broader communication skills, engagement of an entire campus and a whole-person sensory awareness. This work included approaches developed as a result of the ongoing overstimulation and burnout experienced by health care professionals during the pandemic. One way to protect against that overstimulation was to bring back the necessary focus on one’s five basic senses and intuition like never before (what we call “5S + leadership”).
Based on the changing circumstances of health care, we began to reimagine how we train leaders, pivotal to securing the future of Catholic health care. A new style of leadership became necessary: one that is more agile, more connected and responsive to constant fluctuations in health care environments, and better facilitated by reimagined strategy and leadership training centered on the mission.
TRANSFORMING LEADERSHIP TRAINING AT PROVIDENCE
human life. This includes respecting the principle of subsidiarity — which calls us to empower decision-making to those most directly impacted — and meeting the needs of those who are poor or uninsured, especially children, pregnant women, immigrants and other vulnerable populations.3 In addition, the Catholic tradition of health care connects social justice with the delivery of care. Carolyn Woo, PhD, who holds the role of Distinguished President’s Fellow for Global Development at Purdue University, was one of the institute’s keynote speakers on the topic of the whole
Leadership success demanded quicker responses, broader communication skills, engagement of an entire campus and a whole-person sensory awareness.
person. She said: “What I say and what I do must align.”4 She motivated us to look beyond our current crisis and rise toward a new dawning.
The leadership training redesign at Providence was initiated in June 2020, drawing from the vision of Dougal Hewitt, chief mission and sponsorship officer, and Rod Hochman, MD, president and CEO. The Providence Mission Leadership Institute launched in November 2021 as an accredited program in mission-centered leadership. It guides individuals through accelerated leadership development in three main areas: immersive learning, mindfulness in practice and activating one’s purpose.
After reviewing several global leadership approaches, it became clear to fulfill the mission, purpose and vision, created by the Providence legacy congregations, that this curriculum focus — supplemented with renowned speakers from across the U.S. — was the best option.
Much of our institute’s curriculum is based on CHA’s Shared Statement of Identity for the Catholic Health Ministry. Of utmost importance today for the nation’s health care system are the values that respect human dignity and protect
The institute is using a hybrid learning format that connects caregivers virtually and in person with graduate-level academic rigor. A distinct feature of the institute is the mission-centered leader platform that offers curated modules for education and inspiration: embracing art; specifically crafted music playlists for each of the seven core commitments of Catholic health care; LinkedIn learning posts; podcasts; and a library of session videos. The modules explain the principles and language of Catholic health care as it relates to the pandemic and the intensifying need to care for the poor and vulnerable with a health equity lens.
The first cohort of the Mission Leadership Institute offered whole-person development to 300 caregivers, all receiving an advanced certificate of 12 graduate credits from the University of Providence for completing the program. The cohort has its final session in March 2023. A Catholic university and the academic ministry of Providence, the University of Providence is located in Great Falls, Montana, and is accredited by the Northwest Commission on Colleges and Universities.
In one of the sessions, Hochman summarizes how the Mission Leadership Institute prepares
HEALTH PROGRESS www.chausa.org WINTER 2023 27
FORMATION AND MISSION LEADERSHIP INSTITUTE
The Mission Leadership Institute is designed to facilitate development across several diverse health care campus disciplines and leaders.
leaders to sustain Providence’s mission. “If you think about the three words ‘Mission Leadership Institute,’ what is more core to any organization? We know that if your compass isn’t right on your mission, nothing else is going to happen. And then it is all about leadership. …. It’s not about who is the CEO, it is leadership all the way through. ... The concept of institute codifies that it is part of who you are. To me, when you hear the word institute, I think about learning … In the Mission Leadership Institute, while we don’t have all the answers, we do know that our common commitment is that we are going to learn how to do this the right way.”5
The Mission Leadership Institute was designed so caregivers throughout the campus can take part in varying levels of education and skill building to enhance their leadership career development. Three pathways feed into the framework of the Mission Leadership Institute: 1) Discerning Mission Leaders, 2) Mission Leadership Academy
and the 3) Mission Leader Platform (as previously described), which includes a course called Mission Integration Masterclass.
In the initial Discerning Mission Leaders program, which started in November 2021, about 30 caregivers from various disciplines were selected to take part in a graduate certificate program. It focuses on needed skills for new and aspiring mission leaders who want to explore a calling in mission integration.

The Mission Leadership Academy is an advanced certificate program that involves mission-centered leadership development for those early in their careers. In addition to Providence’s formation opportunities, the academy fosters mission development at many different points in a person’s career and encourages the entry of candidates who do not fit the traditional formation profile.
We also offer a special reorientation series called Mission Integration Masterclass. Targeted
MISSION LEADERSHIP INSTITUTE PROGRAM FORMATION PROGRAM
All Caregiver Formation
Mission Leadership Academy
Core Leader Formation
Discerning Mission Leaders Mission Leader Platform 28 WINTER 2023 www.chausa.org HEALTH PROGRESS
Ministry Leadership Formation MissionCentered Caregivers
to our current and aspiring mission leaders, the class uses a case study method for ongoing learning based on Providence’s CARES (counsel, advocate, renew, ethically discern and spiritually support) model.
COMPETENCIES IN LEADERSHIP FOR FUTURE TRANSFORMATION
In one of the institute’s recent sessions on the poor and vulnerable, keynote speaker Maureen Bisognano, president emerita and senior fellow of the Institute for Healthcare Improvement, discussed the importance of curiosity as an essential skill for leaders in Catholic health care. During her presentation, she asked participants a simple yet pivotal self-discovery question: What matters to you?6
LIVING OUR CATHOLIC IDENTITY
The capacity for renewal — continued learning and reenergizing — is an important trait for today’s leaders. Individuals need strategies for how to replenish their inner resources, and their organizations need structures to support them in this area. Woo, in laying the groundwork for mission-centered leaders, spoke on how those who are resilient have the capacity to reflect and to appreciate beauty. Fostering renewal needs to be one of the skills ingrained in all future leaders, and part of that relates to an understanding of the culture of encounter in Catholic health care. As Pope Francis noted, a culture of encounter involves “not just seeing, but looking; not just hearing, but listening; not just passing people by, but stopping with them … allowing yourself to be moved with compassion … .” 7
Effective leaders take a personal interest in the long-term development of their employees, and they use tact and other social skills to encourage them to achieve their best. It is not about being “nice” or “understanding”— it is about tapping into individual motivations in the interest of
allowing a person to flourish and further an organization’s goal. A great leader’s unique achievement is a human and social one that stems from one’s understanding of their fellow workers.
At the institute, we have released the leadership models that Catholic health care has relied on in the past. While our values remain, we need leaders responsive to greater diversity, equity and inclusion. We need thoughtful ways to preserve Catholic identity while also respecting the beliefs of others. The new curriculum of leadership development programs within Catholic health care at Providence focuses on skills in addition to religiosity. These include the curiosity and capacity for renewal previously explained, and further aptitudes needed for future health care leaders, including empowerment and flexibility.
In addition to fully developing all skills needed for current and future health care leaders, program evaluation plays an important role in understanding how leadership development takes place and how it contributes to improving health outcomes. 8 While the Mission Leadership Institute has developed 300 leaders across the Providence health system, ongoing evaluations have demonstrated the impact of this development through pre- and post-course surveys, course completion tracking, podcast listener metrics and e-portfolio assessments.
The training of mission-centered leaders for tomorrow will no doubt undergo frequent adjustment as we respond to ongoing health care delivery changes. Through this ongoing work, we will continue to stay focused on the core mission of Catholic health care, which encompasses health equity and an awareness of all people’s needs.
CONCLUSION
In the future, every health care system should be asking: Are we ready for what’s new today and what lies ahead? Are our leaders prepared for the future, and how can we continually ensure that they have the right tools for success?
As we continue to focus on flexibility, empowerment, renewal and curiosity, the capacity for hope still remains as the sometimes flickering light that illuminates the path ahead. We are
HEALTH PROGRESS www.chausa.org WINTER 2023 29
While our values remain, we need leaders responsive to greater diversity, equity and inclusion. We need thoughtful ways to preserve Catholic identity while also respecting the beliefs of others.
light bearers for those we encounter in our work, particularly those on the margins.
MARTIN SCHREIBER is vice president of Providence’s Mission Leadership Institute in Irvine, California. He hosts the “Providence Walk With Me” podcast. He authored two chapters on resilience and storytelling in the book Physician Well-Being During Sustained Crisis
NOTES
1. Pope Francis, “Message of His Holiness Pope Francis to the Participants in the 32nd International Conference on the Theme: ‘Addressing Global Health Inequalities,’” Vatican, November 2017, https://www. vatican.va/content/francesco/en/ messages/pont-messages/2017/ documents/papa-francesco_20171118_ conferenza-disparita-salute.html.
2. Jim Clemmer, The Leader’s Digest: Timeless Principles for Team and Organization Success (Toronto, Canada: ECW Press, 2003).
3. United States Conference of Catholic
Bishops, Forming Consciences for Faithful Citizenship: A Call to Political Responsibility from the Catholic Bishops of the United States (Washington, DC: 2007).
4. Carolyn Woo, “Whole Person” (Providence Mission Leadership Institute Whole-Person Session, Sonoma, California, March 17, 2022).
5. Dr. Rod Hochman, “Welcome and Introduction to the Mission Leadership Institute” (Providence Mission Leadership Institute Whole-Person Session, Sonoma, California, March 17, 2022).
6. Maureen Bisognano, “Leading with Compassion and Kindness” (Mission Leadership Institute Justice Session, Portland, Oregon, July 14, 2022).
7. Pope Francis, “For a Culture of Encounter,” The Holy See, September 13, 2016, https:// www.vatican.va/content/francesco/en/ cotidie/2016/documents/papa-francescocotidie_20160913_for-a-culture-ofencounter.html.
8. Joel Njah et al., “Measuring for Success: Evaluating Leadership Training Programs for Sustainable Impact,” Annals of Global Health 87, no. 1 (July 2021): 63, http://doi.org/10.5334/aogh.3221.
Upcoming Events
from
The Catholic Health Association
Virtual Series: Ministry Formation Workshop
Tuesdays | From Jan. 24 to June 20 | 1 – 3 p.m. ET
Virtual Dialogue: Honoring the Religious Diversity of Our Staff — Leveraging the Expertise of Chaplains
Jan. 26 | 1 – 2:15 p.m. ET
Virtual Program: Foundations of Catholic Leadership Orientation: Jan. 31 | 1 – 2 p.m. ET Sessions: Thursdays | From Feb. 2 to March 23 | 1 – 3:30 p.m. ET
United Against Human Trafficking Networking Zoom Call
Feb. 7 | Noon – 1 p.m. ET
Faith Community Nurse Networking Zoom Call
Feb. 27 | 1 – 2 p.m. ET
chausa.org/calendar
30 WINTER 2023 www.chausa.org HEALTH PROGRESS
Finding God in Daily Life
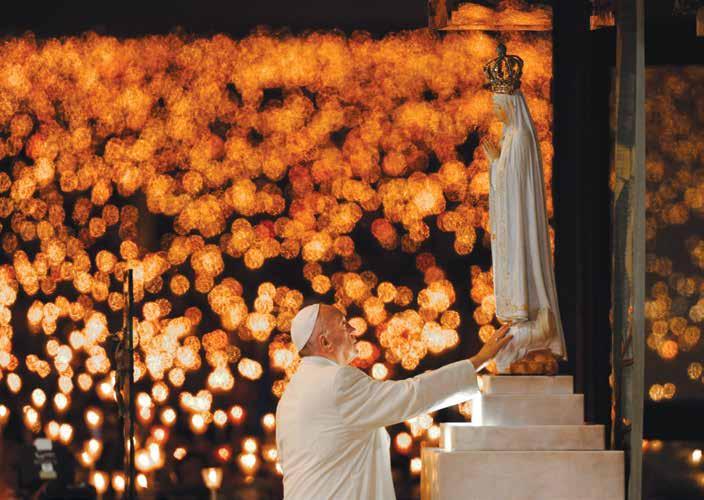
— Pope Francis’ address to staff and clients of Catholic Charities at St. Patrick Catholic Church in Washington, D.C., on September 24, 2015

“Faith makes us open to the quiet presence of God at every moment of our lives, in every person and in every situation.”
Paulo Duarte/Associated Press
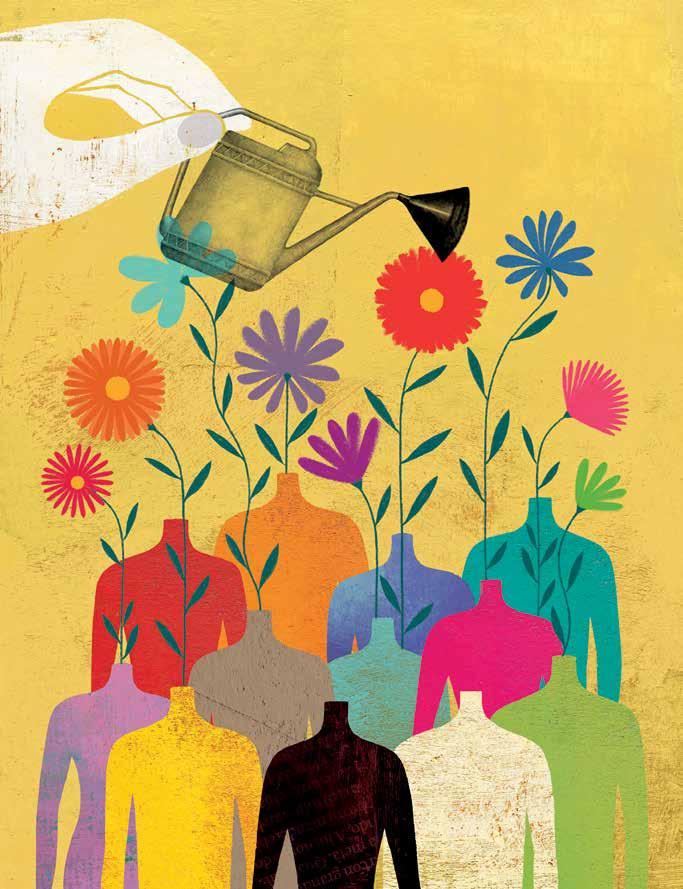
Flourishing Through Formation:
Catholic Identity Is Reinforced With Thoughtful Approaches
 SARAH REDDIN, D.HCML Vice President, Ministry Formation–Mission Integration, Ascension
SARAH REDDIN, D.HCML Vice President, Ministry Formation–Mission Integration, Ascension
Health care’s internal pressures and external headwinds are numerous and complex. Certainly, patient care remains at the core, but in various roles leaders and team members must consider factors as broad as employee engagement and retention, health equity, pandemic trauma and fatigue, and much more.
In addition, Catholic health care specifically is experiencing affronts to identity, the very core of our ministry. Where will our ministries find the resources necessary to carry out a preferential option for those experiencing poverty? How do we reconcile the disconnect that some employees feel between their sense of purpose and the challenges we face to live the ministry’s mission, vision and values? What legislation can we rely on to navigate governmental reimbursement models, and what supports can we turn to in order to resist systemic pressures on Catholic health care’s principles and commitments? How do we live our Catholic identity amidst today’s changing needs? And, even more, what does it mean to be Catholic health care?
Our mission-inspired communities of health care professionals can find answers through communal reflection on the links among personal, professional and organizational identities, and the ways they intersect and support each other. This is the essence of ministry formation. Through
the discipline of formation, health ministries can ensure human flourishing and the integrity of ministry identity in consistent and inclusive ways.
UNDERSTANDING OF SELF AND MINISTRY’S IDENTITY
In many Catholic health systems, the work of ministry formation is most clearly identified through its leadership programs. At Ascension, these include the ministry-wide 18-month Executive Ministry Leadership and 12-month Foundations of Ministry Leadership programs, undertakings that have been going strong since 2004 and 2009. At Bon Secours Mercy Health, leaders are provided ministry formation through its Stories of Grace program. And Intermountain Healthcare provides Living Our Values Everyday for managers and direct caregivers.
While these are just some examples of formation programs, there are also innovations occurring in CHRISTUS Health’s Core Focus program and Ascension’s newest cohort-based Roots of Ministry Leadership program. Introduced in
HEALTH PROGRESS www.chausa.org WINTER 2023 33
LIVING OUR CATHOLIC IDENTITY
2021, Roots — as it is informally known across the system — provides a series of six local retreats that teach and explore the principles of Catholic ministry identity in a case study format via hybrid delivery, alternating in-person and live virtual retreats. The retreats provide supervisors, managers and directors the opportunity to develop distinctive ministry competencies in an applied setting.
Formation experiences are provided in other ways, including organizational spirituality initiatives (for example, prayer and reflection practices, employee spiritual well-being resources, annual feast day celebrations and resources for organizational milestones and transitions), team-based sessions on various themes (for example, theological virtues and writings from the foundresses) and small-group departmental integrations that bring formation into teams’ daily operations. This combination of programs provides the organization with multiple pathways to advance human flourishing and sustain the ministry’s identity with integrity.
To embody Catholic health care in our work requires a strong understanding of self, the ministry and the organization. This awareness is nurtured by tradition, faith, sacramentality and a sense of community; it also means responding to evolving needs. Catholic health care’s self-identity is curated by exploring — through methods that source shared values, beliefs and connections — Jesus’ healing ministry, the stories of the religious founders and coworkers’ present-day narratives. Through the practice of self-understanding and the rigorous cultivation of our strengths, wisdom and innovation facilitated by ministry formation, Catholic health care can find the answers needed to address today’s challenges.
THE IMPACT OF FORMATION
Why is formation essential to Catholic health care? What is the organizational impact? Recent results from Ascension’s formation programs highlight some of the reasons:
Formation is a retention strategy. Research on Ascension’s Foundations of Ministry Leader-
ship program reveals that participants are 10.5 times more likely to stay with the organization for at least two years than those who did not participate.
Formation is a well-being strategy. Participants in the Cultivating Reverence for Living program, provided virtually through sequential modules, reported a 15% reduction in perceived stress
over the six-week engagement.
Formation is an employee engagement strategy. Employees describe formation’s smallgroup model as a way to find meaning in their work. One participant described it as fulfilling “my need to be grounded back into why I chose this [work] … an amazing refresher, inspirational and rewarding.”
Without formation, the nurturing of connection to one’s purpose and community is left unattended. Thus, the real “why” of formation can be best understood as a demonstration of the Catholic health ministry’s anthropological and theological foundation, rooted in the image of God, or the imago Dei. It is from this belief that a deep reverence for all human persons to be seen in the fullness of who they are — deserving of respect, dignity, justice and belonging — flows. Thus, formation’s core outcome is articulated: Who one is shows up in what they do, and what they do influences who they are. With the same holding true for teams, groups and ministries as a whole, the distinctive contributions of formation toward growing a culture of ministry are revealed.
MEASURING SUCCESS
Methods for assessing formation’s impact are an essential component to ensure a thorough portfolio of resources for all health care professionals
34 WINTER 2023 www.chausa.org HEALTH PROGRESS
To embody Catholic health care in our work requires a strong understanding of self, the ministry and the organization. This awareness is nurtured by tradition, faith, sacramentality and a sense of community; it also means being able to respond to evolving needs.
LIVING OUR CATHOLIC IDENTITY
Personal Techniques to Aid in Leading Formation
Over the years of serving in a formation role, I have developed a set of key strategies that continue to guide and expand my approach. They are offered here as a resource to other leaders to further refine and grow their formation practices across the ministry:
REFLECT
The primary text of formation is our own lives and relationship with God.
PLAN
Be intentional, purposeful and resonant with how you collect, design and know material. Facilitate without attachment.
PREPARE
Pray, reflect and meditate before, during and after every formation experience.
INTEGRATE
Extend formation facilitation into the ministry’s daily life through strategic, intentional partnerships and collaborations.
INCLUDE
Choose diverse narratives, authors, artists and musicians in curriculum design to represent voices from across the fabric of humanity.
and partners. To determine formation’s personal impact on participants, the use of a net promoter score survey question — commonly used throughout health care and other settings to determine customer satisfaction and loyalty — offers a valid and defined method. For example, when applied to a formation program, feedback on the survey question “How likely are you to recommend this offering to a colleague?” provides insight into the offering’s facilitation, content and overall participant experience.
Recently, Ascension’s formation team pushed deeper to measure the effectiveness of its efforts and developed a set of personal impact survey questions. Participants respond to a set of 12 statements and prompts, such as “Because of this formation experience, I have a better understanding of Ascension as a ministry.” The use of a common participant survey across a variety of programs, modules, materials and experiences provides a consistent data set essential to report the formation offering’s ongoing impact, its planning and its collaborative design.
EXPANDING FORMATION’S REACH
The ministry’s commitment to human dignity and maintaining the integrity of its identity brings to light the questions of where, how, by and for whom should formation be provided. Increasingly, Ascension’s formation programs have
opened new pathways to integrate this discipline.
As one example, as a component of Ascension’s well-being strategies for nurses, formation modules and materials help to nourish spirituality and belonging and move participants beyond resilience to flourishing. Other departments and teams across Ascension engage in annual formation as part of their learning plans through offerings themed around vocation, community and ministry. Additionally, our boards, executive teams and sponsors are active participants in quarterly formation sessions centered on our values, theological virtues and principles of Catholic social teaching. Diversity and inclusion are an important part of this work. Ascension’s mission and ministry councils provide annual celebrations and rituals, cultural events, volunteer opportunities and well-being sessions for employees in our hospital, clinical and administrative sites. Weekly prayer and meditation groups meet in-person and online to explore faith and spirituality in communal settings. Furthermore, spiritual direction sessions are offered for free to any Ascension employee as part of the ministry’s support for their holistic health.
These integrations can serve as a leading approach for mission integration to pave new trajectories for formation curricula, resources and services to be experienced in more equitable ways than ever before, resulting in expanded
HEALTH PROGRESS www.chausa.org WINTER 2023 35
access for associates.
Formation is a core obligation to our sponsors as an essential, ongoing mechanism for nurturing and growing the integrity of ministry identity. Human beings are constantly in the process of being formed. Through engagement with the Divine, our personal sense of self and our experiences — including those we encounter at an individual, organizational and ministerial level — shape who we are becoming. Specifically in health systems with staff from increasingly diverse backgrounds, formation is critical to shaping the health ministry’s self-understanding. By meeting participants where they are on their continuous path of formation, leaders and facilitators can — if for a few minutes, months or years — create opportunities for reflection on identity in community over time that strengthen the ministry itself.
CONCLUSION
formation’s significant contributions to employee engagement, well-being and retention and partner with mission integration colleagues to open avenues to formation opportunities. Through formation, individuals, teams and communities encounter their own and others’ humanity shaped and held by the ministry’s
Formation is a core obligation to our sponsors as an essential, ongoing mechanism for nurturing and growing the integrity of ministry identity. Human beings are constantly in the process of being formed.
Everyone in Catholic health care can play a part in formation. Leaders of formation programs can advance the conversation by participating in CHA’s virtual gatherings to learn, build community and share best practices. Mission integration leaders with some or no formal formation responsibilities can commit to bringing reflection on identity into collaborations with colleagues across the ministry. Clinical, operational or administrative leaders can understand
QUESTIONS FOR DISCUSSION
Catholic identity. These encounters nourish the seeds of identity that can provide solutions to the challenges Catholic health care faces today and tomorrow. Investing in ministry formation is living our Catholic identity. The ministry’s future depends on it.
SARAH REDDIN serves as vice president of ministry formation–mission integration at Ascension. Reddin and her team are committed to delivering increasingly equitable access to formation programs, resources and services for the health system’s associates and affiliated partners. She also is a member of CHA’s 2022 class of Tomorrow’s Leaders.
Sarah Reddin, vice president of Ministry Formation-Mission Integration for Ascension, asks questions within this article that may prompt additional discussion as well as some follow-up questions.
1. An abiding commitment to human dignity and to ministry identity integrity leads to this question: Where, how, by whom and for whom ought formation be provided?
2. How often does your workplace or system consider its formation offerings? When evaluating opportunities presented in your work environment, what have you found most helpful spiritually or for growth? Did this experience help you better understand the Catholic mission of your work and your role in it?
3. Have you found short formation experiences to be helpful to you, or to better connect your personal skills to the organization’s mission? What about virtual experiences?
36 WINTER 2023 www.chausa.org HEALTH PROGRESS
CHA Career Center
Maximized visibility — See the diverse career opportunities and job openings in Catholic health systems, hospitals and long-term care facilities across the country.


Focused on highly specialized positions — Ethics, mission and pastoral care.













Priced right — CHA members can list basic job postings free for 30, 60 or 90 days.


Connected — Post to the CHA Career Center with the option to also post on the National Healthcare Career Network (NHCN).
































































CHECK IT OUT TODAY! CAREERS.CHAUSA.ORG VALUE-ADDED
FOR
BENEFITS
CHA MEMBERS ✦
✦
✦
✦
A consolidated JOB BOARD with value for job seekers and employers alike!
The Evolution of Sponsorship Models: A Progress Report
FR. CHARLES BOUCHARD, OP, STD
Despite significant progress in our understanding, we are still asking some of the same questions about identity, authority and competence related to sponsorship — the structured relationships through which the sponsor, in the name of the Church, directs and influences the Catholic health care ministry.1 I would like to sketch the history of sponsorship in recent decades and pose some questions for the ministry to consider regarding these relationships moving forward.
The first significant change in sponsorship occurred in 1980, when eight groups of sisters agreed to create the Catholic Health Corporation, a civil entity based in Omaha that combined their separately sponsored hospitals into one Catholic system.2 Eventually, the system became Catholic Health Initiatives, which is now part of CommonSpirit Health.
In 1985, the sisters went a step further and petitioned for establishment of a new juridic person, a type of church corporation that would replace the sisters’ collaborative arrangement with a single sponsor. Because this had never been done before, there were a lot of questions. For instance, it was not clear which canonically competent church authority was the most appropriate to establish such an entity.
The system went first to the Congregation for Institutes of Consecrated Life and Societies of Apostolic Life (now a dicastery) in 1985; CICLSAL referred them back to the NCCB (the National Conference of Catholic Bishops, precursor of the USCCB) since a national bishops’ conference may establish a PJP. When the NCCB
failed to act on the petition, the group considered establishing a PJP in each diocese where they had a ministry. That seemed too complicated, so they settled on a single PJP that would be established in the Archdiocese of Omaha. After further consultation between the Archbishop of Omaha and CICLSAL, CHC was referred back to CICLSAL, which in June of 1991 established Catholic Health Care Federation as the new sponsoring entity for CHC.3
The term “sponsorship” is relatively new and does not appear in canon law. The late Fr. John J. McGrath appears to be the first to use the term in 1968.4 Sr. Melanie DiPietro, SC, JCD, JD, said that she, Father (later Cardinal) Adam Maida and Nicholas Cafardi used the term around 1975 as they were completing a book and needed a title. They wanted to be clear that sponsorship describes a relationship distinct from ownership. At the last minute, they inserted “sponsorship” into the original title and published Ownership, Control and Sponsorship of Catholic Institutions 5
The late Sr. Mary Concilia Moran, RSM, probably knew about the early use of the term, but
38 WINTER 2023 www.chausa.org HEALTH PROGRESS
LIVING OUR CATHOLIC IDENTITY
she was the first to examine it systematically and bring it into common usage. In 1978, she said sponsorship “consists of the support of, influence on and responsibility for a project, program or institution which furthers the goals of the sponsoring group.” She also provided a detailed list of criteria for sponsorship.6
Today, we often define sponsorship as a “link” or a relationship between a good work in health care, education or social services and the Church; this link makes it Catholic. Until the 1980s, sponsorship was highly visible because of the sisters and brothers who literally embodied it, but we didn’t talk about it much. Today, sponsorship is invisible to most Catholics, but there is a great deal of theological ferment about what it is, what it means and whether it is effective.7 (See sidebar on pages 40 and 41 for descriptions.)
SPONSOR CHALLENGES
Each model of sponsorship faces certain challenges. Let me articulate a few of them.
What is the unique role of the sponsor?
One of the most frequent questions about Catholic health care sponsorship is “What does the sponsor do that is distinct from board governance?” or “Is there anything that is unique to the sponsor’s role?”
The sponsor must influence the organization, but it has no operational or managerial role. Its influence is limited to a short but important list of things that are described as reserved powers in its statutes and bylaws. These powers differ from one system to another, but they may include appointing or confirming board members and the CEO; changing the mission; presenting regular reports to the Holy See, and maintaining a good relationship with the local church. Maintaining Catholic identity and a functional relationship with the local and universal Church and initiating and ensuring spiritual formation at all levels seem to be the most important.
Systems that have mirror boards, where the sponsor and board are the same group of people, may find it difficult to clarify the unique responsibilities of each. There is a danger that the role of
one will just collapse into the other.
Systems that have a separate board and sponsor, on the other hand, need to ensure that the sponsor understands its distinct role to avoid disempowering or interfering with the board. Likewise, the board needs a clear understanding of sponsorship, or it may view input as interference.
The fact that the sponsor’s distinct role defined by its reserved powers means its members must have different competencies.8 Boards have to be diverse and representative of the ministry’s service area. They must have financial, legal, medical and other kinds of specialized expertise. Religious and cultural diversity is also important.
The sponsor, on the other hand, may have some of these competencies, but they must have theological competence and ecclesial prudence so that they can mandate and assess formation for the ministry and navigate the sometimes murky waters of ecclesial relationships.9 In systems where the board and the sponsor are the same group, we must ask whether it is possible or reasonable to expect board members who are not Catholic or even Christian to exercise sponsor authority in the name of the Church.
Geography and Mission
The Church is divided up into dioceses, which are geographical areas governed by a bishop. The bishop is responsible for the life of the church in his geographical area. Religious communities do a particular specialized work (such as education or health care) and they usually serve in many different dioceses. Our founders responded to bishops’ invitations and went where they were called. There was no strategic plan.
Managing such an organization requires a market strategy, which is primarily the board’s responsibility. But it also requires a ministry strategy that is focused on the following question: “What is the most effective way to preach the Gospel through
HEALTH PROGRESS www.chausa.org WINTER 2023 39
Today, we often define sponsorship as a “link” or a relationship between a good work in health care, education or social services and the Church; this link makes it Catholic.
the ministry of health care?” Board and sponsor must work together to assure that they address both areas.
Diversity and Identity: Can we have it both ways?
Our health care and educational institutions were shaped by generations of European immigrants and the sisters who accompanied them. They planted Catholicism in the United States, and started schools and hospitals to serve others, even though as immigrants and as Catholics they faced discrimination and, in some cases, exclusion. Today we are serving even more diverse racial
and ethnic populations and LGBTQ persons. We intentionally cultivate diversity in our leadership, providers and staff. We are keenly aware of cultural, racial and economic differences that lead to disparities in access and quality of care. CHA’s “We Are Called” initiative is just one example of many efforts we are proud of, designed to identify and eliminate socio-economic disparities.
Paradoxically, as we are cultivating diversity, we are also trying to be more Catholic (or more explicitly Catholic). CHA and all of its members have formation programs geared toward deepening identity and mission, but this can sometimes
REVIEW OF PUBLIC MODELS OF SPONSORSHIP
There are two broad categories of juridic persons in canon law: private (in which tangible assets are privately owned but at the service of the Church) and public in which assets are church property or stable patrimony. We will focus on those that are public.1 Described in the following are four and a half major kinds of public juridic persons, starting first with “traditional.” (You may be wondering how there can be a half of a sponsorship model. I’ll get to that shortly.)
1. Traditional Sponsorship: There are two kinds of traditional sponsors, namely, religious institutes (mostly women’s communities, but some men’s communities, like the Alexian Brothers and the Camillians) and dioceses, where the bishop is the official sponsor. Both have existed for centuries, but today there are only a few of each of these sponsor models.
Religious sponsorship relies on the presence of a religious institute, usually the founding community.
CHRISTUS Health (Sisters of Charity of the Incarnate Word) and Franciscan Sisters of Christian Charity Sponsored Ministries in Manitowoc, Wisconsin, are examples. In each case, the sisters
themselves are a juridic person, so they are the link between the ministry and the rest of the Church.
Diocesan sponsorship includes systems that were founded or acquired by a diocese. Catholic Health in Buffalo, New York (Diocese of Buffalo), and St. Elizabeth Healthcare (Diocese of Covington, Kentucky) are examples of diocesan-sponsored health care. There are also some diocesan senior care systems, such as ArchCare in the Archdiocese of New York. Institutions under diocesan sponsorship do not need a further link because they are part of the local church.
The next three models do not rely on a traditional religious sponsor but on a new canonical entity — a church corporation called a public juridic person. Dioceses, religious orders, parishes and lay groups like Sant’Egidio are all types of juridic persons. The particular kind we are talking about in health care is often referred to as a “ministerial juridic person” (MJP) to distinguish it from religious orders and other groups that were founded primarily to nurture personal spirituality and prayer rather than to sponsor institutional ministries.
2. Distinct or separate sponsorship exists where a new MJP has been established to succeed the traditional religious sponsor (or sponsors in the case of a merger or collaborative partnership). It meets separately from the board but collaborates with it through regular communication. It may meet jointly with the board for relationship building and common understanding of issues of importance to the ministry, but does not vote on governance matters. Ascension, Bon Secours Mercy and Hospital Sisters Health System are examples of a distinct or separate sponsorship arrangement. SCL Health is a somewhat different case. It recently merged with Intermountain Healthcare but retains its Catholic identity under the sponsorship of Leaven Ministries.
3. Hybrid models are so called because the sponsor is a distinct group of people, but they are all also voting members of the board. In this model, all sponsors are board members, but not all board members are sponsors. The sponsor members are always present when the board meets, but they also meet separately. Calais Ministries (sponsor of
40 WINTER 2023 www.chausa.org HEALTH PROGRESS
LIVING OUR CATHOLIC IDENTITY
appear to be in tension with our efforts to foster diversity. We are accused of discriminating against women, people of color and sexual minorities. Some say we mislead patients about services we provide.10 Can we counter this negative perception and also promote our Catholic identity? I think we can.
To accomplish this, our formation programs must be inclusive but focused. Our institutions act in the name of the Church, and we are concerned with passing on a particular theological and spiritual heritage through our ministries. We are not out to convert anyone to Catholicism, but we must
make a special effort to explain Catholicism: what our fundamental theological convictions are, why we do what we do, and how we view the world, political life, economics and the human person. Our view of the person as essentially communal, for example, is not popular in a culture obsessed with individual rights and freedom and which tends to see the culmination of Christian faith in an individual commitment to choose Jesus Christ as a personal savior. Our commitment to the common good is suspect at best in American society, and the notion of sacramentality — that God’s grace is mediated through human actions, rituals
Franciscan Missionaries of Our Lady Health in Louisiana) and SSM Health Ministries (sponsor of SSM Health in Missouri) are hybrid sponsorship structures.
4. A “mirror” board is a third model. Many of Catholic health care’s biggest systems, including CommonSpirit Health, Mercy and Trinity Health have what we call mirror boards. In a mirror arrangement, the MJP and the board are the same group of people and function as both the civil board and the canonical sponsor. This group usually includes representatives of some of the founding communities. In some cases, a certain number or percentage of sister members of founding communities are required; in others, it is not.2
4 1/2. “Catholic by contract.” I call this half of a sponsorship model because it is not sponsorship in the sense that there is an official canonical link to the Church. Instead, these are situations in which an outside, other-than-Catholic entity buys a hospital or other facility from a Catholic system. The buyer may be another faith-based entity, a nonprofit secular
entity, a university-based medical center or an investor-owned entity.
In an attempt to maintain Catholic values, these arrangements use a Catholic identity agreement or covenant in which the buyer agrees to preserve some aspects of Catholic identity as a condition of the sale. These conditions vary from one agreement to another, but usually include adherence to the Ethical and Religious Directives for Catholic Health Care Services, leadership formation, a priest chaplain, hiring of a senior mission leader, one or more seats on the governance board, maintenance of Catholic symbols, chapel and sacramental services and ways of honoring the founding community. These arrangements lack permanence and in some cases may only be an attempt to lessen the pain of the need to sell.3
Examples of this model are Mercy Hospital in Miami, owned by HCA Healthcare; Saint Vincent Hospital in Worcester, Massachusetts, owned by Tenet Healthcare in partnership with the Diocese of Worcester; and Mercy Hospital of Pittsburgh, which merged with the University of Pittsburgh Medical Center as UPMC Mercy.
NOTES
1. Fr. Frank Morrisey, “Canon Law–Ownership Defined Differently in Civil, Canon Law,” Health Progress 90, no. 1 (January/February 2009): 14-15. PeaceHealth is the only private juridic person in the United States. This means that while it is a Catholic work, the material goods are held by a civil corporation and are not considered church goods.
2. Some charters require that the sponsor have a certain number of religious; some require a majority of Catholics, while some do not stipulate that religious are required, but allow the original sponsors to appoint and remove members of the PJP.
3. Sr. Sharon Holland, “Sponsorship and the Vatican,” Health Progress 82, no. 4 (July/August 2001): 35; Kathleen Boozang, ed., “Is a For-Profit Structure a Viable Alternative for Catholic Health Care Ministry?” Proceedings of a Symposium, Seton Hall Law School in Collaboration with the University of St. Thomas (Seton Hall University, 2012).
HEALTH PROGRESS www.chausa.org WINTER 2023 41
and relationships — was largely rejected by many of the Reformers in favor of unmediated grace and reliance on Scripture alone.11
How do pontifical Ministerial Juridic Persons (MJPs) relate to the local Church?
The sponsor has a canonical obligation to the universal Church. It is the Holy See that grants approval to new pontifical MJPs, and these MJPs must report regularly to Rome.12 Accountability on a local level is more complicated because most Catholic health systems in the U.S. are large and may operate in five, 10 or even 20 different dioceses. This is not so much of an issue in traditional sponsor models because religious orders have years or even centuries of experience working with local bishops. Bishops and religious superiors understood each other’s roles and knew how to make it all work.
It is a bigger concern for new MJPs whose lay members do not have that history and who may be operating from an “obedience” model rather than a kind of collaborative one that is necessary for a sponsor and a bishop who both report to the Holy See. Most lay people know nothing about MJPs, and there are even some bishops who do not fully understand the reality of new MJPs and how to relate to them. The ministry’s formation programs for sponsors must help lay members acquire the ecclesial prudence that enables them to fulfill their mission and do so in particular diocesan churches.
which a sponsor body has no religious members at all yet the dicastery says its competence does not extend to such entities. It has rejected at least one petition from a group that could not guarantee the presence of sisters for the long term.
What happens if the founding community has no more sisters who can serve on the sponsor body? Do they just find any religious who happens to be available? If we do that, how do we preserve the charism of the founding community?
Can a MJP consisting entirely of lay people be created? If so, who would be the competent authority to approve it? DICLSAL with a modified charter? Another existing dicastery? An entirely new dicastery? These questions echo those that arose in the creation of the Catholic Health Care Federation.
We are keenly aware of cultural, racial and economic differences that lead to disparities in access and quality of care.
CHA’s “We Are Called” initiative is just one example of many efforts we are proud of designed to identify and eliminate socio-economic disparities.
Who is competent to establish and oversee new ministerial juridic persons?
I already noted the early confusion that began in 1985 about who would establish the Catholic Health Care Federation. This remains an issue today. 13 DICLSAL continues to consider petitions for new MJPs, but it has made it clear that new MJPs will be approved only if the petitioner can assure that there will be religious who serve as members of the MJP into the foreseeable future. Today, however, we can see that many founding communities are diminished and some will complete their mission and cease to exist. There will be cases in
The creation of an entirely lay MJP would be the most important development in the role of the laity since Vatican II.14 Lay people always “helped the sisters” with their ministries, but soon they may be fully in charge and directly accountable to the Holy See. Do we have confidence that we can now identify and form lay members of MJPs to lead their institutions as ministries of the Church? Are we prepared to provide the kind of adult ecclesial formation they need? Are these lay persons able to grasp, preserve and transmit the charism they have inherited and keep our institutions as vital and effective in the Church and for the world as they were in the past?15 If we are unable to do so, Catholic health care (and education) will cease to exist as ministries of the Church in any meaningful way.
CONCLUSION
There is no assurance that Catholic health care as we know it today will survive into the future.
42 WINTER 2023 www.chausa.org HEALTH PROGRESS
However, the fact that we have retained our identity and values — despite continued mergers and acquisitions and partnerships, political intrigue, concerns over government funding and pressure to conform to secular expectations — is very encouraging. I believe that Catholicism’s institutional presence in the world is essential. Our institutions provide essential services, and they are a counterbalance to secular institutions that do not serve the common good or promote human flourishing in the same way. They are also a sacramental presence to the world. They exist in time and space but reveal the transcendent. With continued development of sponsorship by Catholic laity and formation of leaders and associates, the Catholic health care ministry can remain an important Gospel presence in the American context.
FR. CHARLES E. BOUCHARD, OP, is senior director, theology and sponsorship, for the Catholic Health Association, St. Louis.
NOTES
1. Anne Asselin, “The Ministry of Sponsorship and Its Duty of Accountability,” Studia Canonica 55, no. 1-2 (2021): 75-102; Sr. Doris Gottemoeller, “Challenges for Sponsorship Today,” Health Progress 103, no. 3 (Summer 2022): 12-16.
2. This effort was preceded by the Sisters of Mercy, who in 1976 brought their hospitals in the Midwest into the Sisters of Mercy Health Corporation which is now part of Trinity Health. See historical note at https://www.
LIVING OUR CATHOLIC IDENTITY
mercyone.org/about-us/history.
3. The history of this process is described in detail by Fr. Jordan Hite and Jane E. Poe, “An Innovative Way to Continue the Ministry” Health Progress 73, no. 7 (September 1992): 56-58.
4. John Joseph McGrath, Catholic Institutions in the United States: Canonical and Civil Law Status (Washington, DC: Catholic University of America Press, 1968). This was early in the debate about whether hospital properties remained church goods when they were owned by a civil corporation.
5. Fr. Adam Maida and Nicholas P. Cafardi, Pennsylvania Catholic Conference (Harrisburg, Pennsylvania, 1975). See Sr. Melanie DiPietro, SC, “An Examination of the Universitas Rerum and the Universitas Personarum of New Public Juridic Persons Succeeding to the Healthcare Apostolates of Religious Institutes in the United States” (JCD diss., Pontifical University of St. Thomas Aquinas, 2004), 37-39, note #47. The term sponsorship suggested “under the auspices of,” and was meant to highlight influence rather than title to property and to allow some flexibility for the future. It did not have all the technical nuance it has today.
6. Sr. Mary Concilia Moran, RSM, “Sponsorship: The Uneasy Question,” Hospital Progress 59, no. 10 (October 1978): 52.
7. Karen Sue Smith, Overview of Sponsorship (St. Louis: Catholic Health Association, 2014), https://www. chausa.org/docs/default-source/sponsorship/ overviewofsponsorship-karensuesmith.pdf?sfvrsn=0. CHA uses this definition of sponsorship: “Sponsorship of a health care ministry is a formal relationship between an authorized Catholic organization and a legally formed system, hospital, clinic, nursing home (or other institution) entered into for the sake of promoting and sustaining Christ’s healing ministry to people in need.” Patrick Shea provides several definitions of sponsorship, in “Transitioning Sponsorship with Regard to Religious Institutes,” Proceedings of the Catholic Theological Society of America Annual Meeting 77 (2015): 328-351.
8. Guide for Sponsors in Catholic Health Care: An Explanation of Purpose, Qualifications, Structures and Competencies (St. Louis and Washington, DC: Catholic Health Association, 2021).
9. Anne Asselin makes a similar point: “Members who sit on sponsorship boards, although fulfilling the usual responsibilities of other corporate boards, must realize that far more is required of them.” (“The Ministry of Sponsorship,” 90.)
10. Katherine Stewart, “Why Was a Catholic
HEALTH PROGRESS www.chausa.org WINTER 2023 43
I believe that Catholicism’s institutional presence in the world is essential. Our institutions provide essential services, and they are a counterbalance to secular institutions that do not serve the common good or promote human flourishing in the same way.
Hospital Willing to Gamble with My Life?,” The New York Times, February 25, 2022, https://www.nytimes. com/2022/02/25/opinion/sunday/roe-dobbsmiscarriage-abortion.html; Frances Stead Sellers and Meena Venkataramanan, “Spread of Catholic Hospitals Limits Reproductive Care Across the U.S.,” The Washington Post, October 10, 2022, https://www. washingtonpost.com/health/2022/10/10/abortioncatholic-hospitals-birth-control/. Groups like MergerWatch monitor expansions by Catholic hospitals with the assumption that such agreements limit women’s care.
11. Clarke E. Cochran, “Renewing the Sacramental,” Health Progress 84, no. 6 (November/December 2003): 12-15.
12. Today there are about 35 pontifical ministerial juridic persons. There are 18 in the United States, 13 in Australia and three in Canada. Those in Australia belong to an umbrella membership organization called the Association of Ministerial PJPs Juridic Persons.
13. Sr. Sharon Holland, IHM, JCD, discusses the basis for CICLSAL’S competency on page 34 in “Sponsorship and the Vatican,” Health Progress 82, no. 4 (July/August 2001). In a later article she notes that national bishops’ conferences have the competency to establish juridic persons and suggests that the Pontifical Council for the Laity and the Pontifical Council for the Pastoral Care of Catholic Health Care Workers as entities that could pos-
QUESTIONS FOR DISCUSSION
sibly erect new PJPs. “Vatican Expert Unpacks Canonical PJP Process,” Health Progress 92, no. 5 (September/ October 2011): 54.
14. A 2014 article written at the request of a number of CEOs described the development of these new canonical entities. Catholic Health Association, “Ministerial Juridic Persons: The Growing Role for Laity in Canonical Sponsorship of Catholic Health Care,” Health Progress 95, no. 5 (September/October 2014): 60-63.
15. Sr. Sharon Holland raises the question of formation twice. In 2001 she asks, “Is there adequate formation for a ‘Catholic culture’ led by laypersons, especially for those more accustomed to working in the public sector?” in “Sponsorship and the Vatican,” 37; in 2011 she asks whether the laity are prepared: “From the beginning … there was a sense that the PJP might be a provisional, or even an immediate, step toward total lay responsibility for the apostolates long in the hands of religious. Congregations neither affirmed nor denied the possibility of an eventual lay responsibility for the ministry. However, most intended to retain qualified religious in the governing group for the immediate future. The goal was to preserve the future of the apostolic works in the church, and to do so while the religious still had choices about how to proceed and while there were still active and expert members who could mentor a new beginning.” (“Vatican Expert,” 59.)
In this article on sponsorship, CHA’s Senior Director of Theology and Sponsorship, Fr. Charles Bouchard, OP, STD, explains the complexities of forming early public juridic persons before highlighting the evolution of different sponsorship models and posing some key questions to consider about sponsorship’s future.
1. Who do you think needs to understand what a sponsor is and their role in your Catholic health care ministry? Is it church leadership, executive leadership, frontline care providers or the public? Why?
2. Does your system or facility effectively explain sponsors and their roles? Why is this important to advance the healing ministry of Jesus?
3. If you are on a sponsor board, what are your thoughts about the best ways to prepare for the future? How do you communicate the values of your organization to others? If a tension arises between secular and Catholic understandings on an issue, how do you proceed to maintain the integrity of the ministry?
4. Leadership roles in Catholic health care require a variety of intellectual abilities and skills related to theology, ethics, health care, medicine and business, among others. What does your system do to support these needs? Is more education or formation needed? Or possibly a greater ability to build teams where people’s diverse skills can be joined together?
44 WINTER 2023 www.chausa.org HEALTH PROGRESS
LIVING OUR CATHOLIC IDENTITY
Why Listening Matters for Better Understanding in a Divided Church
BISHOP JOHN STOWE, OFM Conv. Bishop of Catholic Diocese of Lexington
The U.S. Conference of Catholic Bishop’s fall release of the culmination of synodal listening sessions held in dioceses across the country, titled National Synthesis of the People of God in the United States of America for the Diocesan Phase of the 2021-2023 Synod, reveals a common set of themes that are on the hearts and minds of American Catholics.1 People everywhere — including myself as experienced during our sessions held in the Diocese of Lexington — were surprised by the vast agreement discovered when they actually listened and heard from each other. They learned not only about their common love for the Church, but also a similar desire to see it flourish and to be an effective sacrament of God’s presence in the world.
FINDING COMMON GROUND OPENLY AND HONESTLY
The impetus for this effort began in the fall of 2021, when Pope Francis invited the global Catholic Church to employ prayerful and careful listening as an intentional first step of a two-year process called “Synod on Synodality.” This synod, a gathering, is focused on how the Church should move forward in unity. At the first Synod of Bishops to launch the process, Francis presided over the assembly at the Vatican, where he instructed the bishops to speak boldly and to listen charitably. This is a difficult challenge for many, if not all of us. To really promote the unity of the Church — a lack that was poignantly mentioned in the U.S. synthesis, especially when some bishops seem to flaunt their defiance of the pope — it is important that we address issues openly and honestly and not suppress our differences. In the setting of the Church, it is a fundamental requirement that this should be done in charity, even in the age of social media. Pope Francis told some of us during our time with him at the last ad limina visit
in Rome for U.S. bishops in November 2019 that it was acceptable for those gathered to criticize him because he learns a lot from such criticism; yet, he instructed that the place to do it was at the gathering, where it could be talked through, not in the press.
Pope Francis also teaches us that our differences, even our conflicts, are not to be feared. People argue and “fight”— hopefully nonviolently — about what is important to them. Most often, a healthy disagreement is much more productive than a polite withdrawal or indifference to an issue. The pope suggests that unresolved conflicts are the opening for the Holy Spirit to point to a new way. When we have reached the limits of our arguments and reasoning, we can seek the guidance of the Spirit to do what is humanly impossible. But this requires seeing the other not so much as an opponent — and especially not as an enemy — but as a fellow traveler on this path of faith who sees and understands things differently than ourselves.
HEALTH PROGRESS www.chausa.org WINTER 2023 45

LIVING OUR CATHOLIC IDENTITY
We cannot really be one church if we are not able to have disagreements in a civil and constructive manner. Furthermore, we certainly cannot be one church if decisions that affect everyone are put to a majority vote and we ignore the misgivings of the minority. We also cannot be one church if we sweep our differences and difficulties under the rug — as we did with reports of sexual abuse, and as we continue to do with systemic racism and our exclusive policies so painfully felt by women, LGBTQ persons, people of color and others. Careful listening, prayer, reflection on the Word of God, consultation of the sources of our Catholic tradition and silence all contribute to
points and those who have not always been welcome to the table. Although some views are now more acceptable in public discourse, they are still incompatible with the Gospel of Jesus. The insensitivity and lack of civility promoted in the media has become common in too many settings. But it is also not helpful when we say things like “that is too political” or argue that politics are unrelated to our faith. First, we have to distinguish between “partisan” and “political,” a distinction too often omitted in public discourse. We can and must avoid partisanship, but to avoid all political issues would render our faith irrelevant in the world and would surrender a valuable voice in the discourse. Remember that “politics” doesn’t have to be a dirty word. Pope Francis calls it not only a noble vocation, but insists that it should also occasionally serve as an exercise of charity. But this requires that politics be in the service of the common good for all, not just for our own party or for people like ourselves.
an atmosphere where dialogue can help us discover common ground, and the Spirit can lead us “toward” unifying solutions, but not magically creating them.
In my parish and diocesan experience, I see what happens when people sit down and break bread with people whose life and experiences differ from their own. I see crusaders against gay rights break down in tears when they witness the sacrificial love of same-sex partners as one companion deals with a life-threatening illness. I also see anti-immigrant spokespersons become speechless when they hear of the gruesome experiences that migrants tell them with the help of an interpreter. When people are reduced to labels, causes and statistics, they are easy to characterize and even dismiss; but when they are seen as a sister and brother, one who struggles with many of the same issues that they themselves do, it is much harder to do so.
RESPECTING AND HONORING OUR DIFFERENCES
Of course, we should not underestimate the effort and good will that is required to bring together people who have diametrically opposed view-
The unity we desire in the Church should not be confused with uniformity. Diversity is a blessing and is part of what makes us genuinely Catholic. How we create a true community — that is, come together as one with all of the gifts of that diversity — is the challenge that lies before us. From what I have read and heard from the Synod, this is what we all want.2
BISHOP JOHN STOWE is bishop of the Roman Catholic Diocese of Lexington in Kentucky. He was previously vicar provincial of the Province of Our Lady of Consolation in Mount Saint Francis, Indiana, and pastor and rector of the Basilica and National Shrine of Our Lady of Consolation in Carey, Ohio.
NOTES
1. United States Conference of Catholic Bishops, National Synthesis of the People of God in the United States of America for the Diocesan Phase of the 2021-2023 Synod (Washington, DC: 2022).
2. The remarks in this article were originally made by Bishop John Stowe at the Leadership Roundtable at the Catholic Partnership Summit in Washington, DC, on September 22, 2022.
HEALTH PROGRESS www.chausa.org WINTER 2023 47
We cannot really be one church if we are not able to have disagreements in a civil and constructive manner. Furthermore, we certainly cannot be one church if decisions that affect everyone are put to a majority vote and we ignore the misgivings of the minority.

Finding Health: Maybe We Need To Look Elsewhere?
ALEXANDER GARZA, MD
SSM Health Chief Community Health Officer and COVID-19 Incident Commander of St. Louis Metropolitan Pandemic Task Force
As the story goes, a businessman was walking home from work one evening. He noticed another man on his hands and knees under a streetlight, searching frantically for something. Feeling pity for the man, the businessman put his briefcase down and joined the searcher, asking him, “Can I help you? What are you looking for?”
The man replied, “Oh, thank you; I have lost my keys, and I won’t be able to get into my home unless I find them. Could you help me?”
“Of course,” said the businessman, thinking the search would not take long, and he got to work scouring the asphalt underneath the light. After a couple of unsuccessful minutes, the businessman sat up and watched the searcher combing the same ground again.
He then asked, “Where do you believe you were when you lost your keys?” Without looking up, the searcher blindly pointed to a dark field a few dozen yards away. “I am pretty sure I dropped them over there.”
The businessman looked at him incredulously and then at the darkened field, remembering he was now late getting home. He pointed to the ground and said, “If you lost them over there, why are you looking here?”
“Because,” the searcher explained, “this is where the light is.”
I use this story as an analogy in attempting to explain the approach to “health” in the United States. It illustrates the concern that we will forever be looking under the lamppost of health care delivery — searching incessantly and without success — for the answers to what ails us without looking in the areas where health is lost.
The statistics and correlations regarding the
“health” of the U.S. seem redundant now. They are so accepted that the magnitude of their shock value has become background noise, or an expectation that this is just how things are. The political talking points about what is right or wrong with health care and health — amongst other social issues — are as predictable as the sun rising in the east and setting in the west.
Importantly, we must be clear with what we mean when we discuss the “health” of our country. “Health” is distinctly different — yet connected — to “health care,” or the act of addressing medical problems in the country. In the U.S., health and health care are paradoxically related. For much of our history, we have falsely equated the health “of our communities” with the delivery of health care “to the community.” The premise of this mindset is that if we only delivered “more” health care — or similarly, better access to it — then our communities would be “more” healthy. If only we looked harder under the lamppost, we might find our keys. Unfortunately, most evidence does not support this cause and effect.
DETERMINING IMPACT ON HEALTH WHERE IT MATTERS
Year after year, as a country, we spend more and more on health care with little gain in overall health. In fact, we seem to be getting worse. In 2020, according to the Centers for Medicare
HEALTH PROGRESS www.chausa.org WINTER 2023 49
& Medicaid Services’ (CMS) National Health Expenditure Account, the U.S. spent $4.1 trillion on health care, $12,530 per person and a staggering 19.7% of our GDP.1 This spending far outweighs any of the other countries in the Organization for Economic Co-operation and Development.2 For this vast amount of money, we receive little in return at the population level. In 2020, the average lifespan of a U.S. citizen was one of the lowest of any of the Organization for Economic Co-operation and Development countries, at 77 years.3 Life expectancy has decreased from 2019 to 2021 to 76.1 years, the largest drop over a two-year period since 1921.4
Buried beneath these summary statistics lie the hard facts that make these rankings attainable. The U.S. has one of the highest suicide, maternal mortality, infant mortality, obesity and chronic disease burden rates of any of the Organization for Economic Co-operation and Development countries, which, of course, translates to more and younger deaths.5, 6 This burden is not equally distributed in our society, with the poor and vulnerable much more likely to fall in these categories.
There is no doubt that tremendous advances have been made in the delivery of health care, medical devices and therapeutics, all of which are impactful at the individual level with some — such as the COVID vaccines — affecting entire populations. However, there is limited evidence to suggest that many of these technical advances have had a significant impact on the health of the community in general, or on the overall health of our country.
Instead, great advances in health are more generally correlated with improved standards of living and other measures outside of health care delivery. In his groundbreaking study, British physician Thomas McKeown found that advances in lifespan in England and Wales from the mid19th century to the 1960s were more attributable to things such as improved nutrition and sanitation, and not as much from medical discoveries, such as antibiotics.7, 8 This was supported by the work of American physician and epidemiologist J. Michael McGinnis, who famously estimated that health care delivery was responsible for 10%-15% of preventable mortality in the U.S.9 Numerous studies have concluded that being able to afford nutritious food, housing, clothing, transportation and education have all contributed to the improvement in health throughout history. Indeed, this was recognized in the World Health Organization’s Constitution in 1948, which
acknowledged how health was impacted by political and social issues as well as the importance of working across other domains — such as education, agriculture, housing and economics — if we were to improve health globally.10, 11 Despite this, the world shifted to the belief that “health” was equal to medical care, and that if we just focused on health care delivery, that this would somehow solve the problem.
FACTORS OUTSIDE OUR HOSPITAL WALLS
With improved living standards and their resultant increases in life expectancy came the rise of chronic diseases, such as hypertension, diabetes and heart disease, along with a medical model to describe their causes. Health care delivery became increasingly focused on the “proximate causes” for disease, such as poor diet, lack of exercise, smoking and others. But what has not changed is that there are populations with higher risk for the proximate causes than others, begging the question: What makes someone at risk for a risk?12
The “risk for being at risk” is tied to “social determinants of health,” which the Centers for Disease Control and Prevention defines as “… conditions in the environments where people are born, live, learn, work, play, worship and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.” 13 Following this, the CMS has recently advanced rules instructing hospitals to screen for “social determinants of health” and to provide resources to those in need.14
Although these are good measures, are they enough, and will they appreciably help solve the complex issue of health? One could argue that it only continues to drive the narrative that health care will improve health, which, when objectively viewed, is not addressing the problem where it lies. It is continuing to search under the lamppost while the keys are in the darkened field. If addressing the social determinants of health is the goal, because we accept that they contribute to poor health outcomes and disparities, then we should also understand why someone is at risk for negative social determinants of health. This is important to understand, especially since prolonged exposure to negative social determinants is cumulative on disease outcomes, just like toxins or other more proximate causes.
HEALTH AND STRUCTURAL ISSUES
Unfortunately, the U.S. is also an outlier when
50 WINTER 2023 www.chausa.org HEALTH PROGRESS
it comes to spending on the very things that impact social determinants, such as social services. The majority of Organization for Economic Co-operation and Development countries fund social services at much higher ratios to total health care spending — and as a percentage of GDP — than the U.S.15 In 2019, the U.S. spent 18.7% of GDP on social services and 16.9% of GDP on health services — a nearly 1:1 ratio. In contrast, Organization for Economic Co-operation and Development countries, on average, spent 20% of GDP on social services and 8.8% of GDP on health services — an over 2:1 ratio. To think of it another way, the U.S. spends $1.11 on social services for every $1.00 on health care, compared to the average of $2.27 on social services for every $1.00 on health care in other Organization for Economic Co-operation and Development countries, these nations experiencing better outcomes.16, 17
Related but apart from this, there is an increasing body of research that correlates poverty to poor health outcomes with social determinants serving as intermediaries.18 The data has shown that across the board, as one improves their socioeconomic position, they improve their lifespan, even when controlling for race and ethnicity, suggesting the strong link between poverty and health.19 Poverty, for all intents and purposes, helps establish and perpetuate the environments where people live, work and play — the social determinants. The U.S. is experiencing very troubling macroeconomic issues with high inflation, making those who are poor even more so. In addition, income inequity has increased significantly and, similar to the high cost of health care, the U.S. is again an outlier.
To describe this disparity, we can look at the Gini coefficient, which is a commonly used metric to represent income inequality within a nation or social group. It has a range from 0–1 where 0 equals complete equality in distribution of wealth and 1 equals complete inequality. According to data from the Organization for Economic Co-operation and Development, in 2021, the U.S. had the highest inequality of all the G-7 [informal
grouping of advanced democracies] countries with a coefficient of 0.38.20 People in the lowest tiers of income struggle to get out of poverty, thus the cycle perpetuates and continues the ecosystem that drives poor health.
If these are all true, then health is much more a product of structural issues set into motion from the time of someone’s birth, depending on their social station in the community rather than an event solely due to proximate causes. It is difficult to then rationalize that health care, which treats disease, can impact health in any appreciable way when its foundations and origins are so far removed.
SECURING THE PEACE
Exclusively addressing proximate causes has rarely produced long-lasting solutions in health or really any other issue that plagues our society. Perhaps it is the simplicity of the answer, a direct action — more health care — that makes us feel better, or, for that matter, focusing nominally on social determinants of health. But complex problems rarely have simple solutions, and health is the definition of complexity. Trying to understand how this all fits together can be maddening. However, there are a couple of instances during my career that have helped me when thinking these issues through.
Twenty years ago, when I was serving in the U.S. Army in Iraq as part of a civil affairs team to help rebuild hospitals and clinics, we understood that as a strategy, we could not shoot our way to victory, and that the key to victory was not just the sole responsibility of the infantry. Winning the war meant making the country stable enough for us to leave. This wasn’t just about combat; it was about the citizenry, the society and its population. When people feel safe and secure, assured they can work and provide for their families, and are free to live their best lives, then you have stability — a real victory. “Securing the peace,” the motto of my civil affairs unit, is hard, complex and engaging work. But it was the only way to bring about our end-state, a lesson that we forgot
“… great advances in health are generally correlated with improved standards of living and other measures outside of health care delivery.”
HEALTH PROGRESS www.chausa.org WINTER 2023 51
repeatedly to our detriment.
Likewise, in approaching community health, I think about when I was SSM Health’s chief quality officer and the tools we used in patient safety — the “five whys.” As any safety professional understands, you keep asking the question “Why?” until you arrive at the root cause. Though we are very good at doing this for errors in the delivery of health care, we are very poor in doing this for health overall, which would eventually lead us outside of the four walls of the health care system.
So, although we will address social determinants of health within the health care system, there is only so much we can do to address issues that are much bigger — and really outside — of health care delivery. True health rests with us as a nation and as a society. Without the collective efforts to improve those things that drive the social determinants, we will forever be looking under the lamppost and wondering why we can never find the keys.
ALEXANDER GARZA is chief community health officer for St. Louis-based SSM Health and COVID-19 incident commander for the St. Louis Metropolitan Pandemic Task Force. He is the winner of CHA’s 2022 Sister Carol Keehan Award.
NOTES
1. “NHE Fact Sheet,” Centers for Medicare & Medicaid Services, August 2022, https://www.cms. gov/Research-Statistics-Data-and-Systems/StatisticsTrends-and-Reports/NationalHealthExpendData/ NHE-Fact-Sheet.
2. “Health at a Glance 2019,” Organization for Economic Co-operation and Development, https://www.oecd.org/ unitedstates/health-at-a-glance-united-states-EN.pdf.
3. “Life Expectancy at Birth,” OECD iLibrary, https://doi. org/10.1787/27e0fc9d-en.
4. “Life Expectancy in the U.S. Dropped for the Second Year in a Row in 2021,” Centers for Disease Control and Prevention, August 31, 2022, https://www.cdc.gov/ nchs/pressroom/nchs_press_releases/ 2022/20220831.htm#.
5. Roosa Tikkanen and Melinda K. Abrams, “U.S. Health Care from a Global Perspective, 2019: Higher Spending, Worse Outcomes?,” The Commonwealth Fund, January 30, 2020, https://doi.org/10.26099/7avy-fc29.
6. Eric C. Schneider et al., “Mirror, Mirror 2021 — Reflecting Poorly: Health Care in the U.S. Compared to Other High-Income Countries,” Commonwealth Fund, August 4, 2021, https://doi.org/10.26099/01DV-H208.
7. Thomas McKeown and R.G. Record, “Reasons for the Decline of Mortality in England and Wales during the Nineteenth Century,” Population Studies 16, no. 2 (1962): 94-122.
8. James Colgrove, “The McKeown Thesis: A Historical Controversy and Its Enduring Influence,” American Journal of Public Health 92, no. 5 (2002): 725-29.
9. J. Michael McGinnis, Pamela Williams-Russo, and James R. Knickman, “The Case for More Active Policy Attention to Health Promotion,” Health Affairs 21, no. 2 (March/April 2002): 78-93.
10. “Constitution of the World Health Organization,” in Basic Documents: Forty-Ninth Edition 2020 (Geneva: World Health Organization, 2020).
11. Theodore M. Brown, Marcos Cueto and Elizabeth Fee, “The World Health Organization and the Transition from ‘International’ to ‘Global’ Public Health,” American Journal of Public Health 96, no. 1 (January 1, 2006): 62-72, https://doi.org/10.2105/AJPH.2004.050831.
12. Bruce G. Link and Jo Phelan, “Social Conditions as Fundamental Causes of Disease,” Journal of Health and Social Behavior (1995): 80-94.
13. “Social Determinants of Health,” Centers for Disease Control and Prevention, https:// health.gov/healthypeople/priority-areas/ social-determinants-health.
14. “CMS Proposes Policies to Advance Health Equity and Maternal Health, Support Hospitals,” Centers for Medicare & Medicaid Services, April 18, 2022, https:// www.cms.gov/newsroom/press-releases/cmsproposes-policies-advance-health-equity-andmaternal-health-support-hospitals.
15. “Social Expenditure Database (SOCX),” Organization for Economic Co-operation and Development, https://www.oecd.org/social/expenditure.htm.
16. “Social Spending,” Organization for Economic Co-operation and Development, https://doi. org/10.1787/7497563b-en.
17. “Health at a Glance 2021,” OECD iLibrary, https://doi. org/10.1787/ae3016b9-en.
18. Raj Chetty et al., “The Association Between Income and Life Expectancy in the United States, 2001-2014,” Journal of the American Medical Association 315, no. 16 (April 2016): 1750-66, https://doi.org/10.1001/ jama.2016.4226.
19. Paula A. Braveman et al., “Socioeconomic Status in Health Research: One Size Does Not Fit All,” Journal of the American Medical Association 294, no. 22 (December 2005): 2879-88, https://doi.org/10.1001/ jama.294.22.2879.
20. “Income Inequality,” Organization for Economic Co-operation and Development, https://data.oecd.org/ inequality/income-inequality.htm.
52 WINTER 2023 www.chausa.org HEALTH PROGRESS








Calls Bringing together thought leaders to discuss a more just and healthy society Subscribe to the podcast on your device store or visit chausa.org/podcast. Health Calls Catholic Health Association of the United States Health Calls The Future of Global Health SUBSCRIBE TO CHA’S OFFICIAL PODCAST
Health
SURVEY REVEALS ENCOURAGING TRENDS — AND CONCERNS — FOR FUTURE OF MISSION LEADERS


Since the early 1970s, the Catholic Health Association has been committed to promoting the role and function of mission leaders in Catholic health care. Our Mission Leader Survey (conducted in 1993, 2006 and 2013) has helped to create a standardized and professional set of competencies and requirements for mission leaders. Additionally, the results helped guide the curriculum for certificate and graduate degrees in mission integration.
Since the last survey was completed in 2013, much has happened in our world and in health care. This transformation is apparent in the results of the 2022 Mission Leader Survey, which highlights changes that continue to occur in the Catholic church and in Catholic health care, especially as it relates to staff burnout, increasing financial stress and political and racial unrest. Its feedback also reflects the continued evolution of this role and points to some specific areas of interest, concern and hope, further acknowledging the importance of the ministry’s continued work to cultivate and inspire mission leaders.
SURVEY BACKGROUND
Similar to the 2013 questionnaire, the 2022 Mission Leader Survey was designed by members of CHA’s Mission Services Department and Mission Leader Advisory Council, in collaboration with The REID Group, a consulting firm headquartered in Seattle. Results were shared at CHA’s Assembly last summer, and shortly after a virtual webinar was held to provide a more thorough overview of the findings, as well as an opportunity for mission leaders to discuss their thoughts.1
SURVEY RESULTS: KEY DEMOGRAPHICS
Sent to nearly 600 mission leaders across the United States, the 2022 survey received a response rate of 45%. Its 35 questions captured information on key demographics, roles in the organization, use of time in mission responsibilities, critical relationships, a self-evaluation on mission leader competencies and ongoing formational and educational needs. More than 50% of respondents were ages 50 to 65, with almost 20% over 65. The largest single age range for respondents was those in the 40 to 49 category, with 30% under age 49.
Operationally, 40% of respondents work in a local ministry or facility; nearly 30% serve at the regional or market level; and more than 25% operate at the system level. Fifty percent work in an acute care setting, 29% serve in a regional/market/system role; and 11% work in long-term care.
Reflecting the new reality of the uptick of virtual work during the pandemic, 60% of mission leaders work onsite, 11% are virtual and the remaining 29% work in a hybrid situation. The largest single category of job title is director/manager at 47%; followed by vice president at various health system levels at 40%; and, notably, more than 12% choosing “other” as a job title, this segment preferring to self-describe their titles. This latter group possibly suggests mission leaders are being asked to undertake an increasingly diverse set of roles and responsibilities.
Overall, the 2022 data shows a definite decrease in vice president and executive-level mission leader roles and a substantial increase in director/manager roles. Finally, 74% of mission
MISSION
DENNIS GONZALES
54 WINTER 2023 www.chausa.org HEALTH PROGRESS
JILL FISK
leaders consider themselves a member of the senior leadership team, with 43% reporting to the CEO/president, 25% to another mission executive and 6% to another senior leader. It is worth noting that due to the dominance of the vice president role in previous years, the 2022 survey included the following question: Are you a member of the senior leadership team?
Diversity
In terms of diversity, respondents were overwhelmingly white/non-Hispanic at 86%, with the next largest ethnicity being Hispanic/Latino at 5% and Black at 4%. It appears that little progress has been made in the diversity of mission leaders over the past 10 years. This result is particularly disappointing, especially in light of the ministry-wide We Are Called pledge launched by CHA in 2021 and signed by almost 90% of Catholic health care ministries.2 One of the four pillars of the pledge, called “Putting Our Own House in Order,” states that “we will examine all aspects of our organizations, including how we provide
Gender and Faith
Women were the predominant workers in the field at almost 56%, with men at 44%. However, compared with CHA’s 2013 survey, the gender gap seems to be narrowing: previously, almost 70% of respondents were women and only 30% men. When looking at a correlation of gender and title, the results are split evenly, with 50% of those in a VP role at any level being women. However, when looking specifically at regional and system VP positions, males outnumber females by 9%. Also worth noting, and not surprisingly, the vast majority identify as Catholic at 80%, down from 87% in 2013 and 93% in 2006. Most of the remaining 20% describe themselves as Christian.
Succession
clinical care; how we recruit, hire, promote and retain employees; how we conduct our business operations including visible diversity and inclusivity at the decision, leadership and governance levels; and how we incentivize and hold our leaders accountable to ensure we are truly dismantling and not perpetuating racism and inequity.” This is clearly an area where much work needs to be done, one that will require a deliberate effort to recruit and develop more diverse candidates into mission leadership.
Consistent with previous trends, in less than five years, almost 33% of respondents plan to leave their work as a mission leader. This percentage grows to 57% for those planning to leave their role in less than 10 years. From this data, it appears there is a significant gap between the large number of those mission leaders who plan to retire relatively soon and the similarly large percentage of those who are newer to the field, leaving a small percentage of those in the middle. If this trend continues and boomers do in fact retire at the implied rate, we will need to discern how to fill that leadership gap. As such, identifying and developing potential mission leaders, succession planning, mentoring, coaching, sponsorship and focused recruitment efforts will become increasingly important. Whether because of retirement or a desire to find a different line of work, these responses indicate a significant amount of turnover in the field in the next decade.
Competency
Interestingly, while current mission leaders may have health care experience overall, respondents indicate much less experience in mission leadership specifically. Thirty-seven percent of respondents report only one to five years in their mission
HEALTH PROGRESS www.chausa.org WINTER 2023 55
It appears that little progress has been made in the diversity of mission leaders over the past 10 years. This result is particularly disappointing, especially in light of the ministry-wide We Are Called pledge launched by CHA in 2021 and signed by almost 90% of Catholic health care ministries.
leader role, with 22% having more than 15 years of experience. This result indicates that Catholic health care is having some success in recruiting candidates from other health care disciplines. It also dramatically highlights the approaching leadership and experience gap. What remains unclear is how these candidates are being equipped and prepared for the role. To that end, mission leaders were asked, “Given the many challenges facing Catholic health care today, what are the top three CHA mission leader core competencies required of mission leaders?” The responses included: incorporating the mission and values into all operations of the organization; ensuring the centrality of mission in strategy; and advocating for persons who are marginalized and affected by poverty.
RESPONDING TO TODAY’S CHALLENGES
When asked about the main institutional challenges mission leaders are facing, the top responses include caregiver well-being, maintaining organizational culture in a changing work environment, promoting our Catholic identity and creating formative experiences to deepen personal and organizational meaning. Based on the related survey data, these challenges certainly ring true, and CHA remains focused on providing resources for the ministry that address these needs.
Looking ahead, mission leaders were asked what they considered to be the top three factors regarding the future of mission leadership. The top responses included integrating mission in an increasingly diverse culture, recruiting the next
generation of mission leaders and being a member of the senior leadership team.
Based on these results, as a ministry, we must ask ourselves: Are we up to the challenge to ensure the future of mission leadership? What are the implications in terms of our Catholic identity, mission, values and founding charism? These are vital questions, indeed, that must be asked, answered and acted upon. When asked about a vision of effective, integrated and thriving mission leadership, a respondent replied, “Empower[ing] teams to empower individuals to foster and reveal the love of Jesus in the name of the Church. Teamwork is characterized by and for our seven core commitments. It would look like an apostolic community built on a life of prayer … .” As mission leaders, this is our invitation and our call.
DENNIS GONZALES, PhD, is senior director, mission innovation and integration, for the Catholic Health Association, St. Louis. JILL FISK, MATM, is director, mission services, for the Catholic Health Association, St. Louis.
NOTES
1. The full recording of the “Future of Mission Leadership: 2022 Mission Leader Survey” webinar is available on the following CHA website: https://www.chausa.org/ online-learning/detail/the-future-of-mission-leadership2022-mission-leader-survey.
2. “We Are Called,” Catholic Health Association, https:// www.chausa.org/cha-we-are-called.
56 WINTER 2023 www.chausa.org HEALTH PROGRESS





Would you like to have Health Progress and Catholic Health World delivered to your home? A Passionate Voice for Compassionate Care® CONTACT THE SERVICE CENTER AT SERVICECENTER@CHAUSA.ORG
CHA GUIDE INCORPORATES EQUITY INTO ALL ASPECTS OF COMMUNITY BENEFIT

Agrowing body of research shows that centuries of racism in this country has had a profound and negative impact on communities of color. Data shows that racial and ethnic minority groups in the United States experience higher rates of illness and death across a range of health conditions, including diabetes, hypertension, obesity, asthma and heart disease, than the white population. Additionally, the life expectancy of non-Hispanic/Black Americans is four years lower than that of white Americans.1
involves continually monitoring health, economic and social factors and demonstrating that the organization is acting on these conditions and community concerns.
JULIE TROCCHIO
To meet today’s challenges to identify and address these and other health disparities and to form more authentic, effective community partnerships, this past fall, CHA released the 2022 edition of its Guide for Planning and Reporting Community Benefit 2 The resource has been updated to incorporate what we have learned about health equity, disparities, and the social and environmental determinants of health. The guide incorporates how to use these learnings throughout community benefit and community health improvement programming.
While addressing the complexities of health inequities is beyond the scope of any one organization or entity, community benefit programs can make a difference when we work with community members whose voices have not been heard and who experience disparities. The Guide for Planning and Reporting Community Benefit calls on community benefit leaders and their colleagues to fully engage with communities, to be present, to listen intently, to effectively partner with community members, and to be accountable for addressing inequities.
Being present involves developing long-term community relationships and encountering community members where they work and live. Listening means going beyond focus groups and surveys in required assessments every three years. It
The new guide describes how we can work with diverse populations in all aspects of our community benefit programs to promote equity and address disparities, as demonstrated in the following examples.
Build a Sustainable Infrastructure
Establish commitment to equity in critical documents, including mission and value statements, as well as strategic and organizational plans and policies.
Work toward building diversity among community benefit staff, consultants and advisory bodies.
Participate in coalitions with community organizations that work with persons who experience disparities and discrimination.
Allocate resources to address social determinants of health and disparities.
Community Engagement
Understand the history of the community regarding discrimination and structural racism by hearing the stories of community members.
Assess current partnerships for diversity and ensure they include cross-sector organizations and people who experience disparities and discrimination.
Assess and address any barriers to commu-
COMMUNITY
BENEFIT
58 WINTER 2023 www.chausa.org HEALTH PROGRESS
nity engagement, such as past experiences with the organization and other trust issues.
Hold meetings and conduct activities at times and places convenient to the community. Provide transportation and child care, if needed.
Accounting and Finance
In community benefit reporting, acknowledge programs that address disparities and promote equity.
Reach out to racial and ethnic minority community members with information about financial assistance policies.
Align community benefit budget decisions with equity goals.
As part of the organization’s investment strategy, include investments in community organizations that will improve social determinants of health and advance equity.
Assessment
Gather data using culturally appropriate tools and methodologies that consider factors such as the population’s language needs and literacy levels.
Collect and analyze data on health outcomes and risk behaviors and other factors that impact health by income, disability status, geography and race/ethnicity.
Involve community members in collecting and analyzing assessment information.
Make assessment findings available to community members and groups who experience disparities and request their feedback.
Planning
Build on community strengths and assets and value community expertise.
Look at existing programs, and evaluate whether they are addressing racial and ethnic disparities identified in the community.
Develop implementation strategies collaboratively with community members who experience disparities, and get feedback from community members to ensure services are culturally appropriate and convenient.
Address factors that contribute to diverse populations’ higher health risks and poorer outcomes, and revise implementation strategies with changing community demographics.
Implementation
Focus the implementation strategy on health disparities in the community and ensure that programs and activities address health inequities.

Collaborate with diverse community organizations to manage implementation of programs that address issues that might prevent programs from achieving desired impacts.
Maximize the use of community health workers in assessment and program planning, implementation and evaluation.
Use advocacy to address laws and regulations that enable structural racism in the community.
Evaluation
Engage stakeholders who reflect the diversity of the community and ensure that many of
HEALTH PROGRESS www.chausa.org WINTER 2023 59
While addressing the complexities of health inequities is beyond the scope of any one organization or entity, community benefit programs can make a difference when we work with community members whose voices have not been heard and who experience disparities.
their voices are heard when making judgments on how to improve programs or whether to continue offering them.
Incorporate health equity into evaluation goals, questions and design.
Gather data using culturally appropriate tools and methodologies that consider factors such as the population’s language needs, literacy levels and facilitator preferences.
Identify and analyze variables that can assess different effects of interventions across population groups.
Communications
Use language that is accessible and meaningful to your audience, and tailor communications based on the unique circumstances of different populations.
Consider ways to improve the accessibility of content, and offer materials in languages spoken in the community.
Avoid jargon and use straightforward, easyto-understand language.
Publicly emphasize the value of ensuring that everyone has an equal opportunity for health and that reducing disparities contributes to the common good and benefits all.
A core objective of the CDC’s Healthy People 2030 — the 10-year plan to address the nation’s most critical public health priorities and challenges — is to “eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all.”3 For community benefit leaders, this is the essence of our work,
the reason we work within our organizations and with community partners in pursuit of health equity. Our communities are healthier when all community members are healthy. Health equity is necessary for this to happen.
The “We” in CHA’s We Are Called initiative means all of us: all Catholic health organizations, all of our departments and programs, and all who work in Catholic health care. 4 We are called to use our experience and expertise to address and correct past injustices and inequalities and to make our communities healthier and more just. Community benefit leaders are in an excellent position to do this when we use an equity lens in our work.
JULIE TROCCHIO, BSN, MS, is senior director of community benefit and continuing care for the Catholic Health Association, Washington, D.C.
NOTES
1. “Racism and Health,” Centers for Disease Control and Prevention, https://www.cdc.gov/minorityhealth/ racism-disparities/index.html.
2. “A Guide for Planning and Reporting Community Benefit,” Catholic Health Association, https://www. chausa.org/communitybenefit/a-guide-for-planningand-reporting-community-benefit.
3. “Healthy People 2030 Questions & Answers,” Office of Disease Prevention and Health Promotion, https://health.gov/our-work/national-healthinitiatives/healthy-people/healthy-people-2030/ questions-answers.
4. “We Are Called,” Catholic Health Association, https://www.chausa.org/cha-we-are-called.
60 WINTER 2023 www.chausa.org HEALTH PROGRESS ››› To order the updated
Community
Guide for Planning and Reporting
Benefit, visit www.chausa.org/guide
ETHICS
WHAT IS ABORTION?
The memorial Mass for my cousin John took place last summer at St. Patrick’s Church in Newburgh, New York. My ancestors came to this region as Irish immigrants during the 19th century, and although many of my family today have moved to other states and countries, we continue to have a connection to this area, gathering here during times like this.
BRIAN KANE
As an extended family, our time together was spent sharing with each other. Our conversations were a mixture of the promises of the future lives of our children, the accomplishments of those who were poised to be adults, and the experiences of the lives of those who had shaped us.
In the midst of our conversations, one issue came up more than a few times: the recent Dobbs v. Jackson Women’s Health Organization decision and abortion in the United States. For many amongst us, this topic was personal. The discussions never became too heated, but it was clear that there were differences on how to address this issue moving forward.
However, we do know that Catholic social tradition argues that there are two essential truths: the dignity of the person and the common good. Every person deserves to be recognized for their intrinsic worth, and we, as a community, should work to create the conditions where every person flourishes.
A MISSION TO CARE, NOT CONTROL

Some of the disagreements surrounding abortion during my family’s exchanges arose from personal experiences that involved navigating emotionally challenging circumstances, ranging from encountering the unexpected to managing difficult pregnancies. Some of our differences were also because, as a family raised in the theology and
culture of Catholicism, we share deeply rooted values about life and abortion.
Some of my family’s fringes echoed extremities of the national political debates. But most did not, as the majority were compassionate about how to best address the needs of others. The middle still exists for most Americans, if not now, perhaps in American politics.
It is important to remember that the discussion that we, as a national community, should be having now is about how to respect and nurture the lives of those whom we love. Sound bites are destructive when they insist on imposing control over the life of a woman or child. The same is true about enacting control on Catholic health care when it works to meet the needs of women and children. Instead of control, we need to care, together.
How is it possible that we have a society where a mother’s love for her child has instead been turned into a battle of survival between the two? Abortion is accepted by some as a “medical” answer to a social problem, one where women may be in crisis and do not have the means or resources to support a pregnancy. Pregnancy and parenthood come with physical, emotional, financial and personal responsibilities; some of these only women can shoulder.1 Men and our communities
Sound bites are destructive when they insist on imposing control over the life of a woman or child. The same is true about enacting control on Catholic health care when it works to meet the needs of women and children. Instead of control, we need to care, together.
HEALTH PROGRESS www.chausa.org WINTER 2023 61
should share many of these responsibilities with women. But that does not always happen. When women do not receive support, some seek other ways.
The intention of “the right to choose” is to solve that problem by asserting one’s autonomy, a stance sometimes voiced in the statement “It’s my choice.” Whether alone, or feeling pressured or that they don’t have options, the choice for some becomes “my child or me.” And, in Catholicism, we view that as a tragic decision, one that diminishes both a mother and her child.
We, as an American community, accept and ignore abortion’s consequences when we do not create the solutions necessary to alleviate the pain of pregnant women who need help, or those who become mothers and need additional support and resources. The conflict between mother and child persists, despite efforts to address this conflict.
Abortion currently remains an option in some states for women. Making abortion illegal, however, doesn’t change the circumstances for women who still think abortion is their only choice. Abortion is fundamentally a care issue. How can we provide the social support for pregnant women so that abortion doesn’t appear to them to be the best choice for their situation?
I find it hard to believe that abortion is the first choice for most women who are unexpectedly pregnant. But I don’t find it difficult to understand that abortion seems to be an option when alternatives for the care of that mother and her child are not available, and abortion is legal.
It is common wisdom that Catholics believe that abortion is immoral. The sentiment is more than 20 centuries old. In the Didache, one of the earliest existing Christian texts, it is stated that “thou shalt not murder a child by abortion nor kill them when born.”2 That declaration was followed by care. For the Christian community, it was never enough to state a moral ideal without actions to back it up. The early Christian community cared by reaching out to those who were discarded by Roman society. At the time, this was countercultural.
MEDICAL INTERVENTION
Another issue in this broad social conversation about abortion today is the accusation that Catholic health care, in the pursuit of safeguarding both maternal and prenatal life, restricts clinical care
for mothers. 3 Proponents of elective abortion rights conflate the voluntary choice to abort a viable pregnancy with complications in pregnancy, like ectopic pregnancy and premature rupture of membranes. These are not the same.
Ectopic pregnancies and premature deliveries are medical situations that require intervention. Therefore, terminations of pregnancy, per Catholic moral thought, are not all abortions.4 There are clinical situations where it is medically necessary — and ethically consistent with Catholic ethics — to assist a woman in discontinuing a problem pregnancy.
So, what is considered abortion? There are disparate theological, medical and political answers to this question, which contradict each other. Those differences contribute to misunderstandings and harm for women.
Theologically, the Catholic answer is that abortion is the intentional termination of a pregnancy that could be, or is, viable. If the intention is to make certain that the embryo or fetus is terminated, then we would describe that act as an abortion. It is immoral because the intention is the deliberate act of ending the life of an innocent person in utero.5
Medical interventions that address harmful consequences of nonviable pregnancies are not abortions because they are not meant to cause the death of the embryo or fetus. If the pregnancy can never be viable, and symptoms point toward increasingly dangerous conditions for the mother — like sepsis — then it would be moral to address these medical situations, even if we can foresee that the embryo or fetus will die. The standard is whether the pregnancy would be able to reach viability, not whether the pregnancy is before the time of viability.
It is important for some nuance here, for example, when there is an ectopic pregnancy. We may not directly terminate an embryo, which is a human person. If, however, that embryonic person is implanted in a fallopian tube, and that implantation is a threat to the mother, what should be done? The answer is that we should treat the medical problem since this is a nonviable pregnancy. The continued growth of the embryo will result in a rupture of the fallopian tube and the death of the embryo and possibly the mother. It would be moral to either excise the potentially rupturing fallopian tube, or to use a pharmacological response,
62 WINTER 2023 www.chausa.org HEALTH PROGRESS
to resolve this clinical situation if it is clear that using medication (in this case, methotrexate) will not directly lead to ending the embryo’s life.6
Similarly, if a woman experiences a premature rupture of her uterine membranes or a preterm premature rupture of membranes, the primary questions are whether the embryo — or more likely, the fetus — is viable, and whether the mother is in medical danger. In some well-known cases, clinicians have interpreted Catholic ethics incorrectly.7 In those cases, septic pregnancies were allowed to continue and threaten the life of the mother because clinicians believed that Catholic ethics required the established death of the embryo or fetus before intervention. That is not correct. In these cases, if the clinical determination is that the pregnancy is not viable, it is moral to assist in managing the medical circumstances of the pregnancy, even if the embryo or fetus will die as an indirect consequence.
of abortion. Dobbs has left the regulation of abortion to the states, but they disagree on what it actually is. The state definitions are inconsistent.9 Some state legislatures — in a drastic effort to protect prenatal life — have passed laws that are harsh and misinformed in their understanding of medicine.10
It is important to understand that Catholic moral thought does not align completely with the descriptions of “pro-life” or “pro-choice.” Instead, we are both “pro-mother” and “pro-child.” The line is drawn for us when a woman wants to abort her healthy, nascent child. That choice is not medical, it is personal, and it immorally ends the life of someone who has the right to exist. No child should die because of that choice. Conversely, no mother should die because her pregnancy is not viable.
Medically, the term “abortion” is confusing. In the Merck Manual, abortion is described as a consequence, rather than an act or a choice. It is the “death of the fetus, sometimes with passage of products of conception (fetus and placenta), before 20 weeks gestation.” This definition makes no distinction between elective abortion and miscarriage. Thus, it confuses the consequence of a choice with an intention. The fact that an embryo or a fetus dies as the result of a natural circumstance of a nonviable pregnancy — or, alternatively, as the result of an intentional medical procedure to end a pregnancy — is not significant, according to Merck. What matters is that the pregnancy has ended and the embryo or fetus is dead.8
A DUTY TO CARE FOR ALL BEINGS
What about law and politics? In the aftermath of Dobbs, and the patchwork of state laws that will now regulate abortion, it is important to note that there is no common legal and political definition
What about the “right to life”? As a theologian and bioethicist, my personal judgment is that early human life (at chromosomal transfer, or syngamy, and on) is a human person and has rights because of their existence. Every person, once conceived, has a claim to be born and the ability to live as God intended them to be. To deliberately take this right away from them in their vulnerable state is immoral.
The “right to life” is intellectually consistent. But saying this doesn’t solve the conflict of how to respect the life of the woman who helped to create and nurture this person. This new person doesn’t erase the rights of their mother, nor, as already stated, do the mother’s rights eliminate those of her child.
Perhaps the problem is that too often we emphasize rights without corresponding duties. A right to choose a goal that is self-beneficial includes the duty to not choose an act that is wrong, and also to choose in favor of the disadvantaged. To end the life of an innocent person is immoral, regardless of whether it benefits us personally. We cannot claim a moral right of autonomy that disregards the duty to care for others.
The same obligation exists for those who advance a right to life. It includes the duty to care for all persons in need, not just unborn children. Persons need care after birth, not just during pregnancy. Choosing life means to create
HEALTH PROGRESS www.chausa.org WINTER 2023 63
It is important to understand that Catholic moral thought does not align completely with the descriptions of “pro-life” or “pro-choice.”
structures that minimize, and eliminate, tragic choices. And, that is what Catholic health care and social services are about.
CONCLUSION
In a recent address, Pope Francis stated that “We were put in this world to love him (God) and our neighbors. Everything else passes away, only this remains. The tragedy … summons us to take seriously the things that are serious, and not to be caught up in those that matter less; to rediscover that life is of no use if not used to serve others. For life is measured by love.”11
Abortion is a tragedy because it demonstrates our failure to care for women who make this choice, and also our inadequacy to care for those unborn children whose lives are ended by this act. If our lives are measured by love, what is abortion?
BRIAN M. KANE, PhD, is senior director, ethics, for the Catholic Health Association, St. Louis.
NOTES
1. Ross Douthat, “What Do the Physical Costs of Pregnancy Mean for the Abortion Debate?,” New York Times, October 5, 2022, https://www.nytimes. com/2022/10/05/opinion/pregnancy-abortion-dobbs. html.
2. The Didache or the Teachings of the Twelve Apostles, trans. by J.B. Lightfoot (London: MacMillan & Co., 1891), § 2.2.
3. Francis Stead Sellers and Meena Venkataramanan, “Spread of Catholic Hospitals Limits Reproductive Care Across the U.S.,” The Washington Post, October 10, 2002, https://www. washingtonpost.com/health/2022/10/10/ abortion-catholic-hospitals-birth-control/.
4. Kate Cohen, “Chrissy Tiegen Has Shown What Abortion Is. Some Refuse to Accept It.”, The Washington Post, September 20, 2022, https://www. washingtonpost.com/opinions/2022/09/20/ chrissy-teigen-abortion-lost-pregnancy/.
In this article, the reporter states that “An abortion is the deliberate termination of a human pregnancy.” The statement lacks nuance with regard to different medical conditions.
5. The principle of double effect guides Catholic decision-making in complex cases. In short, the principle helps to distinguish the three parts of a human act: the object, the intention and the circumstances. Within the
context of this column, it will not be possible to do a complete analysis of each individual situation.
6. Peter A. Clark, SJ, “Methotrexate and Tubal Pregnancies: Direct or Indirect Abortion?” The Linacre Quarterly 67, no. 1 (February 2000): 7–24; Ron Hamel, “Catholic Hospitals and Ectopic Pregnancies,” Health Care Ethics USA 19, no. 1 (Winter 2011): https://www.chausa. org/publications/health-care-ethics-usa/archives/ issues/winter-2011/catholic-hospitals-and-ectopicpregnancies; William May, “Methotrexate and Ectopic Pregnancy,” Ethics & Medics 23, no. 3 (March 1998): 1-3, https://doi.org/10.5840/em19982335; Albert S. Moraczewski, “Ectopic Pregnancy Revisited,” Ethics & Medics 23, no. 3 (March 1998): 3-4; Moraczewski, “Tubal Pregnancies: Part I,” Ethics & Medics 21, no. 6 (June 1996): 3-4; Moraczewski, “Tubal Pregnancies: Part II,” Ethics & Medics 21, no. 8 (August 1996): 3-4.
7. The seminal case here is the death of Savita Halappanavar in Ireland in 2012 due to a septic miscarriage that was not treated properly. While she was not treated at a Catholic hospital, her death became a mandate for changing abortion laws in Ireland.
8. Antonette T. Dulay, “Spontaneous Abortion,” Merck Manual, October 2022, https://www.merckmanuals. com/professional/gynecology-and-obstetrics/ abnormalities-of-pregnancy/spontaneous-abortion.
9. “California Health & Safety Code, Section 123464 (2020),” Justia, 2020, https://law.justia.com/codes/ california/2020/code-hsc/division-106/part-2/ chapter-2/article-2-5/section-123464/; “Alabama Code, Section 26-21-2 (2021),” Justia, 2021, https://law. justia.com/codes/alabama/2021/title-26/chapter-21/ section-26-21-2/.
10. Paradoxically, those states that seem to be most intent on restricting abortion access also have the highest rates of maternal mortality due to inadequate systems available for prenatal and post-partum care for women, particularly in minority communities. See below for more on this topic: “Health of Women and Children Report 2019,” America’s Health Rankings/United Health Foundation, September 2019, https://assets.americashealthrankings.org/app/ uploads/health-of-women-and-children-2019.pdf; David Albert Jones, “The End of Roe Doesn’t Need to Bring an Increase in Maternal Morality,” The New York Times, July 9, 2022, https://www.nytimes.com/2022/07/09/ opinion/roe-abortion-women-death.html.
11. Pope Francis, “Homily of His Holiness Pope Francis,” April 5, 2020, https://www.vatican.va/content/ francesco/en/homilies/2020/documents/papafrancesco_20200405_omelia-palme.html.
64 WINTER 2023 www.chausa.org HEALTH PROGRESS
MAPPING THE ROAD TO DIVERSITY, EQUITY AND INCLUSION IN AGING SERVICES

There is a new roadmap for aging service providers who want to begin, refine or sustain a program for promoting diversity, equity and inclusion ( DEI ) in their settings. LeadingAge California has developed a helpful toolkit, called “Diversity, Equity and Inclusion Roadmap,” to provide long-term care facilities, senior housing programs and other aging services with step-by-step guidance for setting and achieving DEI goals.1 As the toolkit notes, when organizations commit to being informed by America’s diversity, “the field can make bold strides toward an equitable workforce.”
WHY INCORPORATE DEI NOW?
We have always been called to correct past injustices, and equal employment protection under the law has been with us since passage of the Civil Rights Act in 1964. Yet, the LeadingAge California roadmap states that “major employers across the nation have been successful in maintaining a homogenous executive workforce.” Today, the rise of public consciousness of DEI in American society — resulting from a combination of the COVID-19 pandemic and the police killings of George Floyd and Breonna Taylor — has led to a national (and often local) introspection on its importance.
Committing to DEI values can assist aging service providers in many aspects of their operations, according to the toolkit. It cites that “DEI in the workplace will dramatically impact workforce culture, quality of care, community outreach, corporate policy, hiring practices, promotion strategies, and strategic partnerships.” It can increase employee satisfaction and retention, and build new connections to pipelines of diverse talent.
The roadmap describes five phases in the DEI process: preparation, planning, implementation, progress evaluation and maintenance of initiatives.
Phase 1: DEI Preparation
The roadmap’s preparation begins with introspection, including an evaluation of social demographics at all levels of employment and an organization’s board of directors, as well as a review of current and past hiring practices.
An important part of preparation is visibility. The organization’s executives and board should be visible and outspoken leaders of the initiative by attending meetings, supporting the initiative with space and funding, and acknowledging that this is important — if challenging — and sometimes anxiety-generating work.
The roadmap suggests that preparation involved to build a DEI infrastructure includes establishing a budget, forming a DEI committee and providing its members with basic training. Some organizations should consider hiring or contracting with a diversity expert to lead discussions. Other preparatory steps entail establishing a DEI calendar for regular meetings, events and deliverables; developing short and long-term goals; and instituting cultural holidays — such as celebrating Juneteenth — to more comprehensively teach the organization and its community about DEI.
Phase 2: DEI Planning
After the preparation phase, the roadmap suggests taking three to six months to plan a robust DEI initiative. This includes establishing “safe
AGING
JULIE TROCCHIO
“DEI is an emerging corporate strategy to enhance the workforce and morale of existing staff.”
HEALTH PROGRESS www.chausa.org WINTER 2023 65
— LeadingAge California’s Diversity, Equity and Inclusion Roadmap
space guidelines” for the DEI committee. Members should be encouraged to share honestly and speak up if another participant shares an opinion that makes anyone uncomfortable. The committee should agree that each participant is trusted to act in the group’s best interest. As the roadmap notes, “A single person should not be expected to speak on behalf of an entire demographic that they represent. They will, however, be expected to provide insight on best practices by providing cultural insight.”
Planning also should include establishing a DEI corporate framework with the creation of a DEI statement. The statement should express the organization’s commitment to diversity, equity and inclusion. It should also be short — no more than three sentences — and easy for the reader to understand and repeat.
Phase 3: DEI Implementation
After all the preparation and planning is complete, aging service organizations should release their DEI statement and promote the initiative throughout the institution. An important step is reviewing organizational policies, especially hiring. The DEI statement can be included in job postings, new staff onboarding and in employee interviews. The roadmap also suggests looking at promotion polices and being creative in using wages or benefits to recognize expertise and to show staff members they are valued.
DEI training is another critical step in implementing the initiative. Current and new staff should participate in initial training and have annual updates — all of which can be incorporated into existing training modules.
Implementation, the roadmap notes, should also include establishing clear measurable outcomes with specific dates, for example: “By three months from the start of the initiative: Establish diversity metrics and target outcomes for diversity of staff, board and committees.” Or, another example can state: “By the end of year three after the start of the initiative: The diversity of employees [and board] will match that of county or state demographics.”
Phase
4: DEI Progress Evaluation
Evaluation means looking at qualitative and quantitative data. One step could be an annual employ-
ee satisfaction and workplace culture survey that incorporates the organization’s DEI goals, and measures results against the goals. If goals are not met, find out why: Is it lack of executive or board leadership support? Are policies (such as hair discrimination) presenting barriers? Is funding for the initiative insufficient? Has communication not been successful?
Once barriers have been identified, the initiative can get back on track by reevaluating its plan and considering the hire of a DEI expert for guidance. The organization may need to refocus the initiative or reprioritize certain aspects. Also, review suggestions from your expert and the work of the DEI committee.
Phase 5: Maintenance of Effort
The roadmap offers six action steps for maintaining the DEI initiative: 1) conduct and report on metrics about staff and resident social demographics, employee satisfaction and initiative events and activities; 2) communicate progress to board, employees, residents and the local community; 3) subscribe to DEI newsletters and keep up with other resources; 4) consider hiring an executive team member to oversee the initiative; 5) establish a DEI critical response team to address DEI-related complaints and concerns; and 6) identify staff to attend conferences and education on DEI Catholic-sponsored aging service providers who want to be part of CHA’s We Are Called initiative should take a look at this new and valuable resource.2 It includes the previously described step-by-step guidelines and can help aging organizations, whether they are beginning or fine-tuning their DEI efforts. It also offers examples from the field and resources for more information. It is truly a one-stop resource for aging service providers.
JULIE TROCCHIO, BSN, MS, is senior director of community benefit and continuing care for the Catholic Health Association, Washington, D.C.
NOTES
1. “Diversity, Equity and Inclusion Roadmap,” LeadingAge California, 2022, https://indd.adobe.com/ view/77191b23-20fe-4e1b-b0ec-d3b2d7934506.
2. “We Are Called,” Catholic Health Association, https://www.chausa.org/cha-we-are-called.
66 WINTER 2023 www.chausa.org HEALTH PROGRESS
Global Health Meditative Reflections
In partnership with The Carter Center and Center for Compassionate Leadership meditative experts, this series of reflections will help you build resiliency, focus on global health topics and increase well-being.

Go to chausa.org/globalreflections to access these resources!

THINKING GLOBALLY TRANSFORMING HEALTH IN A CHANGING WORLD

Rapid and transformative change has profoundly affected nearly every aspect of our lives these last few years. Health care workers around the world have endured high stress levels and enormous tolls on their well-being, leading to burnout and staffing shortages. The confrontation between science and politics around COVID-19 showed how easily trust could be eroded, exacerbating challenging pandemic circumstances for those in health care. The pandemic also significantly magnified long-existing health inequities, including the disproportionate toll of COVID on under-resourced communities early on and at the height of the pandemic. These and many other challenges are realities both at home and abroad. As a ministry of the universal Church, we must think globally, even as we attend to urgent local matters, recognizing the potential impact of our actions on people worldwide.
years in these areas: the health sector; significant shifts in the global health agenda; and technological changes that will revolutionize the future of health care. Findings and recommendations from the study will support the Catholic health ministry’s future thought leadership and advocacy agendas.
BRUCE COMPTON
To examine changing global health and technology trends and their impact on the future of global health partnerships, CHA enlisted the support of Accenture’s social impact business, Accenture Development Partnerships, to address social, economic and environmental issues globally. Their findings reveal close alignment of global and domestic health trends and challenges brought by either the pandemic or other recent factors, highlighting the critical importance of strategic global health partnerships.
FUTURE OF GLOBAL HEALTH PARTNERSHIP MODELS
COVID served as a reality check for countries worldwide, raising questions about the overall state of global health security. Global health security is the existence of strong and resilient public health systems that can prevent, detect and respond to infectious disease threats wherever they occur in the world.1 CHA and Accenture Development Partnerships explored the immediate impacts of the pandemic over the past several
Even with all we have recently experienced, most countries are still unprepared for future pandemic threats. The push to build more resilient health systems has never been more significant. As the world seeks to increase global health security and preparedness for future pandemics, the importance of working together and rebuilding trust cannot be underestimated.
CHA’s study with Accenture points to four critical elements — in addition to top trends to consider (see sidebar on page 70 for further details) — to create successful future global health partnership models.
68 WINTER 2023 www.chausa.org HEALTH PROGRESS
Even with all we have recently experienced, most countries are still unprepared for future pandemic threats. The push to build more resilient health systems has never been more significant.
1. Creating More Horizontal and Equitable Relationships: Growth of relationships between donors and grantees and high-income and lowincome countries.
2. Building Strategic Partnerships: Fewer, bigger and better partnerships to address health challenges at scale.
3. Using Untapped Collaborators: Emergent and underutilized health partners, such as community health workers and others, are valued as part of mainstream and integrated health strategies.
4. Partnership Growth Through Digital Technologies: Expansion of partnerships through digital technologies, enabling accessibility, ease of collaboration and real-time communication.
MOST SIGNIFICANT TRENDS IN GLOBAL HEALTH Health Equity
In the U.S., nearly 90% of all health care executives have health equity initiatives as part of their core business strategies. As a Catholic health ministry, a similar percentage of systems have pledged to confront racism by achieving health equity in CHA’s We Are Called pledge.2 Those on the margins often struggle to navigate the complexities of traditional health paradigms, leaving people lost or altogether excluded. We cannot deny the reality that COVID’s impacts were experienced unequally across the world, with already vulnerable groups enduring far more significant disease burden. Again, Catholic health care’s work in this area is substantial at home and abroad. If we do not put our own houses in order, we cannot influence the world stage.
Workforce Shortage
The World Health Organization estimates a global shortage of 10 million health care workers by 2030, with nurses representing a majority of this gap.3, 4 Globally, 90% of national nurse associations reported concerns that the pandemic is driving increasing numbers of people to leave the profession.5 The ongoing workforce shortage crisis, fueled by decades of underinvestment, was intensified by COVID, leading to an acceleration
of staffing shortages and increased burnout.
In “From Competition to Collaboration,” a policy brief on global workforce developed by the UK Tropical Health Education Trust, partners are offered guidance by suggesting an ethical route through workforce shortage challenges, focusing on the fate and well-being of each country’s national health service and strengthening the health care of low- and middle-income countries.6
Many health care professionals from low- and middle-income countries migrate to other nations to find employment, as their home countries are unable to allocate enough resources to health. These workers are a precious resource to these nation’s communities, something that their vulnerable populations so desperately need. As we continue to struggle with our workforce issues, the effects of recruitment from low- and middleincome countries is an important factor to consider.
Climate Change
Recognized by many as the most significant global health threat of the 21st century, climate change is identified as a global health emergency by leading health institutions worldwide. Human health is affected by climate change’s direct and indirect
impacts as a significant determinant of our health outcomes. The pandemic exposed the weak public health systems and disaster preparedness strategies currently in place in many countries. Many voices call for a renewed and integrated approach to global health to prepare for future international health threats.
Established by the Centers for Disease Control and Prevention, the One Health initiative is a collaborative strategy uniting experts from multiple disciplines and sectors.7 The initiative works at local, regional, national and global levels to achieve optimal health outcomes. One Health recognizes
HEALTH PROGRESS www.chausa.org WINTER 2023 69
We cannot deny the reality that COVID’s impacts were experienced unequally across the world, with already vulnerable groups enduring far more significant disease burden.
GROWING TRENDS IMPACTING GLOBAL HEALTH PARTNERSHIPS
Since 2020, global health has endured rapid and transformative change due to the COVID-19 pandemic and other factors. Through CHA’s collaborative exploration with Accenture Development Partnerships — which involved both secondary research and a series of consultations with global and digital health experts — discoveries revealed changing global health and technology trends and their impact on future global health partnership opportunities.
Immediate Impacts of COVID on the Health Sector
1. Delayed, Deferred and Disrupted Health Care: More than two years into the pandemic, health systems are still facing significant challenges in providing and restoring health services. Due to limitations imposed by COVID-19, millions of individuals have delayed or avoided medical care for fear of their own safety or social and economic risks. The result is a dramatically altered disease burden and a population of patients dealing with its harmful health consequences.
2. Rebuilding Trust: The highly charged disagreements between science and politics in recent years has exposed the weakened trust in vaccines, medicine and science. This deterioration is due to uncertainty, political divisiveness, the erosion of public health information and the rise of misinformation, particularly in social media.
3. Pandemic Preparedness: Most countries remain vastly unprepared for future pandemic threats, potentially even more socially and economically devastating than COVID-19. With the impacts of the pandemic still ongoing, the need for building more resilient health systems is greater now than ever.
Largest Shifts in the Global Health Agenda Over the Past Two Years
4. Achieving Health Equity for All: Though health equity has been a buzzword in the global health sphere for years, since 2020 the sector has seen it evolve in new and important ways. The COVID-19 pandemic has brought many of these inequities, and the market dynamics that have caused them, to the forefront of public discourse and the global health agenda.
5. Future Health Workforce: Decades of underinvestment have diminished our global health workforce, as the world struggles to deal with shrinking numbers, insufficient capacity and increased pressure being placed on our health systems. This crisis has only been intensified through COVID-19, leading to significant staffing shortages, increased burnout and other challenges that will continue to persist beyond the pandemic.
6. The Human Cost of Climate: Climate change has been recognized as a global health emergency by leading health institutions around the world and has even been dubbed “the greatest global health threat of the 21st century.” Human health is currently, and will even further be, affected by both the direct and indirect impacts of climate change as a major determinant of our health outcomes.
7. Population Dynamics: The UN estimates that the world’s population is expected to increase by nearly 2 billion people, from 8 billion at present to 9.7 billion in 2050, before reaching a peak of nearly 11 billion by the end of the century as fertility rates continue to decline.1 The changing demographics of our global population are shifting health care needs and creating new demand for health services that support evolving population dynamics.
Technology Trends From the Past Two Years That Will Revolutionize the Future of Health Care
8. Patients in Power: Patients today have new expectations for health care and have redefined what it means to put patients in charge. As a result, health care will need to consider future advancements such as increasing its accessibility to patients and further enabling them to be equal decision-making partners in their course of treatment.
9. Acceleration of Virtual Health: Physical limitations to access health care imposed by the pandemic have rampantly driven the delivery of health services through digital technologies to overcome these barriers.
10. Data Collaboratives: Cross-industry and multi-sectoral collaborations are becoming the future state of health care due to global challenges becoming increasingly multi-faceted, thus requiring a diverse set of parties to adequately address them. Though health data is still largely unshared globally, the last few years have emphasized the greater need for international cooperation and collaborative data efforts to discover insights into health and wellness.
NOTE
1. “Our Growing Population,” United Nations, https://www.un.org/en/global-issues/population.
70 WINTER 2023 www.chausa.org HEALTH PROGRESS
the interconnectedness of all living creatures and their shared environment. As a Catholic health ministry, we share in this initiative as a vital partner in Pope Francis’ Laudato Si’ Action Platform, which calls us to sustainability and a spirit of integral ecology.8
CONCLUSION
With changing population dynamics and the use of virtual technology for better access to care, opportunities exist for transformation in global health, including the possible expansion of more Catholic health care outside of the U.S. As we think about the trends and issues identified through this recent research, we should continue to discern how we are called to continue the healing ministry of Jesus in a changing world.
To see the full findings of this report, “View From 2022: A Look at the Changing Global Health Landscape and Future of Partnerships,” visit chausa.org/ globalhealth.
BRUCE COMPTON is senior director, global health, for the Catholic Health Association, St. Louis.
NOTES
1. “What is Global Health Security?,” Centers for Disease Control and Prevention, May 2022, https:// www.cdc.gov/globalhealth/security/what.htm.
2. “We Are Called,” Catholic Health Association, https://www.chausa.org/cha-we-are-called.
3. “Health Workforce,” World Health Organization, https://www.who.int/health-topics/health-workforce #tab=tab_1.
4. “Nursing and Midwifery,” World Health Organization, March 2022, https://www.who.int/news-room/ fact-sheets/detail/nursing-and-midwifery.
5. “COVID-19 Pandemic One Year On: ICN Warns of Exodus of Experienced Nurses Compounding Current Shortages,” International Council of Nurses, March 11, 2021, https://www.icn.ch/news/covid-19-pandemicone-year-icn-warns-exodus-experienced-nursescompounding-current-shortages.
6. Graeme Chisholm, “From Competition to Collaboration,” Tropical Health and Education Trust, https://www. thet.org/wp-content/uploads/2019/07/FromCompetition-to-Collaboration_THETPolicyReport-1.pdf.
7. “One Health,” Centers for Disease Control and Prevention, https://www.cdc.gov/onehealth/index.html.
8. Laudato Si’ Action Platform, https://laudatosi actionplatform.org/.
HEALTH PROGRESS www.chausa.org WINTER 2023 71
Prayer for Tomorrow’s Promise
JENNIFER COBB, MDiv, MBA, BCC MISSION LEADER
NOTE: For this prayer service, it is helpful to have notecards and pens so that participants can write their thoughts during the pauses.
INTRODUCTION
We often like to think of the new year as a new beginning. Its story hasn’t yet been written, and the year ahead is full of hope and possibilities. We make resolutions, promising ourselves that we will do — and be — better than last year.
The late Sr. Mary Roch Rocklage, a Sister of Mercy and an iconic health care leader, was well-known for saying, “God made you who you are because he thought you’d enjoy it.”
As we enter into this space together, you are invited to bring all your hopes and dreams to the year ahead and carry along your experiences of the past year. It has helped to form and lead you to who you are today.
FIRST READING
“You formed my inmost being; You knit me in my mother’s womb. I praise You, because I am wonderfully made; wonderful are Your works! My very self You know.
My bones are not hidden from You, when I was being made in secret, fashioned in the depths of the earth.
Your eyes saw me unformed; in Your book all are written down; my days were shaped, before one came to be.”
(Psalms: 139:13-16)
FIRST REFLECTION
How incredible is it to consider that God, who created the world, delights in each of us, and specifically, in you. Take a moment to imagine God relishing that you exist — not because of your accomplishments or what you contribute to the world — but exulting in you because God is simply overjoyed that you are you.
(Pause)
Consider the year that has just passed. You are not the same person as you were then. There have been moments of incredible joy and deep sorrow. The experiences of this past year have helped to form you, and God was present through every moment. Take a few minutes to remember, examine and observe within yourself what the year has been. As you do, write on one side of your notecard how it has shaped you.
SECOND READING
“For I know well the plans I have in mind for you — oracle of the Lord — plans for your welfare and not for woe, so as to give you a future of hope.”
(Jeremiah 29:11)
SECOND REFLECTION
As we look to the year ahead, we bring all that has shaped us today. We look with joy and excitement, anxiety and uncertainty, and with steadfast faith that God has never left our side and will remain our guide and strength.
Although this year’s story is still unwritten, its outline may be clear in our imagination. We already possess our expectations for what “will be,” and we are planning how to bring it forth. On your notecard, write your hope and expectations for the year ahead.
On your notecard, you have a story of the past that has formed you and your future dreams. Let us take this moment to lift our pasts and our intentions for the year ahead to God.
CLOSING PRAYER
God, You are ever present with us. You held us this past year — cheering when we were filled with joy and lifting us when our strength was not enough. We ask that You guide and direct our steps in the year ahead. Teach us to be more fully the people You created us to be, the people in whom You delight. Help us to serve with our complete selves, joyfully, humbly and eagerly. With each step, unfold for us a future that brings us closer to You. Amen.
WINTER 2023 www.chausa.org HEALTH PROGRESS 72 PRAYER SERVICE
“Prayer Service,” a regular department in Health Progress, may be copied without prior permission.
FOUNDATIONS of CATHOLIC HEALTH CARE LEADERSHIP
JOIN US FOR FOUNDATIONS LIVE 2023
Leaders in Catholic health care have come to recognize the crucial importance of formation in ensuring the Catholic identity of our ministries. CHA’s Foundations of Catholic Health Care Leadership program provides executives, board members, directors, managers, clinicians and other leaders in Catholic health care with a foundation in core theological and ethical principles that are at the heart of the Catholic health ministry.
Foundations Live is a series of eight consecutive weekly virtual sessions on Thursdays from February 2 to March 23, 2023, from 1-3:30 p.m. ET. An orientation session to familiarize participants with the overall program agenda and online format is scheduled for Tuesday, January 31, 2023, from 1-2 p.m. ET.
Contact Diarmuid Rooney, CHA interim vice president of sponsorship and mission services, at drooney@chausa.org or 314-253-3465.
REGISTER TODAY AT CHAUSA.ORG/EVENTS
QUESTIONS?
A Passionate Voice for Compassionate Care® Designed for Leaders Like You!

MEDICAID COVERAGE TOOLKIT AVAILABLE NOW. PROTECT WHAT’S PRECIOUS. DOWNLOAD AT TALKING POINTS Crafted for staff to guide patients through the process, including how to update their information CLEAR MESSAGING Featuring direct paths to helpful information and state Medicaid agencies READY TO USE Designed to cobrand or rebrand to align with your system’s guidelines CHAUSA.ORG/MEDICAID



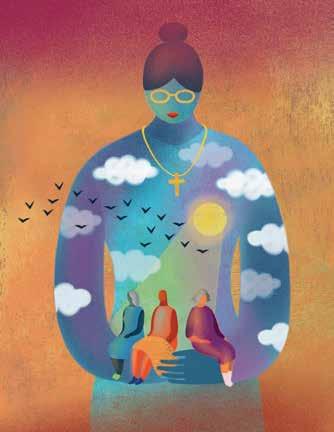



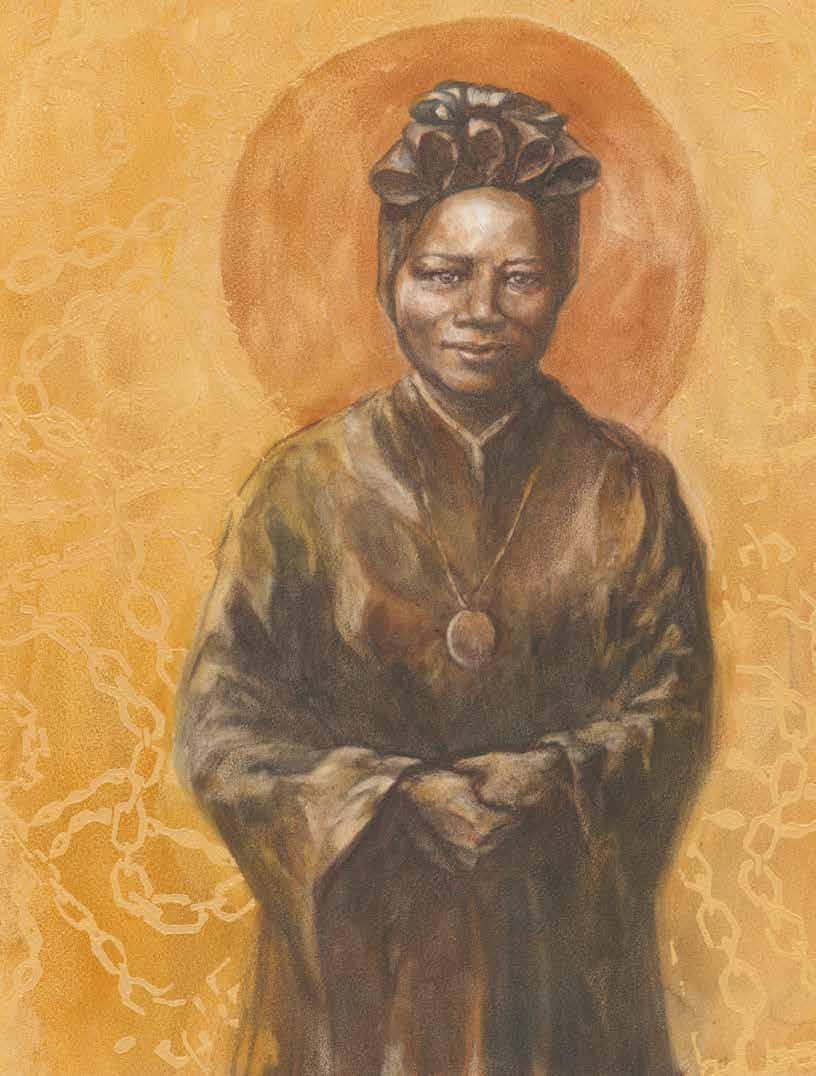 ST. JOSEPHINE BAKHITA
ST. JOSEPHINE BAKHITA
 LIVING OUR CATHOLIC IDENTITY
LIVING OUR CATHOLIC IDENTITY
 Dr. Alisahah Jackson
Dr. Alisahah Jackson