A PEER-REVIEWED FORUM FOR NURSE PRACTITIONERS
NEWSLINE
■■ Substituting MDs With APPs in Nursing Homes ■■ Hawaii Repeals Physician Chart Reviews for PAs LEGAL ADVISOR
Medical Errors and Negligence
|
SEPTEMBER 2019
| www.ClinicalAdvisor.com
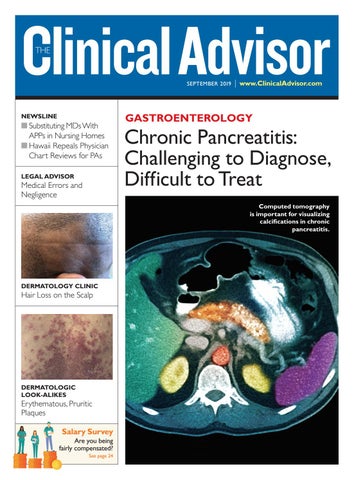
GASTROENTEROLOGY
Chronic Pancreatitis: Challenging to Diagnose, Difficult to Treat Computed tomography is important for visualizing calcifications in chronic pancreatitis.
DERMATOLOGY CLINIC
Hair Loss on the Scalp
DERMATOLOGIC LOOK-ALIKES
Erythematous, Pruritic Plaques Salary Survey Are you being fairly compensated? See page 24