Research Report 2018-20
A selection of published research by CMCC faculty
Featured articles include:
9 Effect of Cervical Manipulation on Vertebral Artery and Cerebral Haemodynamics in Patients with Chronic Neck Pain: A Crossover Randomised Controlled Trial
Moser N, Mior S, Noseworthy M, Côté P, Wells G, Behr M, Triano J
20 NTG-101: A Novel Molecular Therapy that Halts the Progression of Degenerative Disc Disease

Matta A, Karim MZ, Gerami H, Jun P, Funabashi M, Kawchuk G, Goldstein A, Foltz W, Sussman M, Eek BC, Erwin WM
40 SafetyNET Community-Based Patient Safety Initiatives: Development and Application of a Patient Safety and Quality Improvement Survey
Funabashi M, Pohlman KA, Mior S, O'Beirne M, Westaway M, De Carvalho D, El-Bayoumi M, et al.
51 Spinal Manipulation Therapy Improves Tactile Allodynia and Peripheral Nerve Functionality and Modulates Blood Oxidative Stress Markers in Rats Exposed to KneeJoint Immobilization
Duarte FCK, Kolberg C, Riffel AP, Souza JA, Bello-Klein A, Partata WA
78 The Passive Voice and Comprehensibility of Biomedical Texts: An Experimental Study with 2 Cohorts of Chiropractic Students
Millar N, Budgell B
87 “I Stay in Bed, Sometimes All Day.” A Qualitative Study Exploring Lived Experiences of Persons with Disabling Low Back Pain
Esson SA, Côté P, Weaver R, Aartun E, Mior S
104 Exploring Chiropractic Services in the Canadian Forces Health Services – Perceptions of Facilitators and Barriers Among Key Informants
Mior SA , Vogel E, Sutton D, French S, Côté P, Nordin M, Loisel P, Laporte A
Our Mission
Deliver world class chiropractic education, research and patient care
Our Vision
An academic institution recognized for creating leaders in spinal health
CMCC is dedicated to pursuing innovation in education, research and patient care. In this way, the institution effectively prepares its students to become tomorrow’s leaders in spinal health.
CMCC’s achievements in these academic years demonstrate the success of this approach in paving the way toward increased collaboration with other health care professions, and helping to define the profession within the changing Canadian health care landscape.
CMCC Research Report 2018–20
A selection of published research by CMCC faculty
6 Welcome
9 Effect of Cervical Manipulation on Vertebral Artery and Cerebral Haemodynamics in Patients with Chronic Neck Pain: A Crossover Randomised Controlled Trial Moser N, Mior S, Noseworthy M, Côté P, Wells G, Behr M, Triano J
20 NTG-101: A Novel Molecular Therapy that Halts the Progression of Degenerative Disc Disease
Matta A, Karim MZ, Gerami H, Jun P, Funabashi M, Kawchuk G, Goldstein A, Foltz W, Sussman M, Eek BC, Erwin WM
34 Does Manual Therapy Affect Functional and Biomechanical Outcomes of a Sit-to-Stand Task in a Population with Low Back Pain? A Preliminary Analysis
Carpino G, Tran S, Currie S, Enebo B, Davidson BS, Howarth SJ
35 Force Transmission Between Thoracic and Cervical Segments of the Spine During Prone-Lying High-Velocity Low-Amplitude Spinal Manipulation: A Proof of Principle for the Concept of Regional Interdependence Engell S, Triano JJ, Howarth SJ
36 Lower-Limb Factors Associated with Balance and Falls in Older Adults: A Systematic Review and Clinical Synthesis
Neville C, Nguyen H, Ross K, Wingood M, Peterson EW, Dewitt JE, Moore J, King MJ, Atanelov L, White J, Najafi B
37 Correlations Between Individuals’ Characteristics and Spinal Stiffness in Individuals With and Without Back Pain: A Combined Analysis of Multiple Data Sets Pagé I, Swain M, Wong A, Breen A, De Carvalho D, Descarreaux M, Funabashi M, Kawchuk G
38 A Descriptive Analysis of Shoulder Muscle Activities During Individual Stages of the Turkish Get-Up Exercise St-Onge E, Robb A, Beach TAC, Howarth SJ
39 Nonspecific Low Back Pain: Inflammatory Profiles of Patients With Acute and Chronic Pain
Teodorczyk-Injeyan JA, Triano JJ, Injeyan HS
40 SafetyNET Community-Based Patient Safety Initiatives: Development and Application of a Patient Safety and Quality Improvement Survey
Funabashi M, Pohlman KA, Mior S, O'Beirne M, Westaway M, De Carvalho D, El-Bayoumi M, et al.
51 Spinal Manipulation Therapy Improves Tactile Allodynia and Peripheral Nerve Functionality and Modulates Blood Oxidative Stress Markers in Rats Exposed to Knee-Joint Immobilization
Duarte FCK, Kolberg C, Riffel AP, Souza JA, Bello-Klein A, Partata WA
65 Comprehensive Nonsurgical Treatment Versus Self-directed Care to Improve Lumbar Spinal Stenosis: A Randomized Trial
Ammendolia C, Côté P, Southerst D, Schneider M, Budgell B, Bombardier C, Hawker G, Rampersaud YR
66 The Association Between Psychological and Social Factors and Spinal Pain in Adolescents Batley S, Aartun E, Boyle E, Hartvigsen J, Stern PJ, Hestbæk L
67 Development and Validation of a Model Predicting Post-Traumatic Headache Six Months After a Motor Vehicle Collision in Adults
Cancelliere C , Boyle E3, Côté P, Holm LW, Salmi LR, Cassidy JD
68 Clinical Outcomes in Neurogenic Claudication Using a Multimodal Program for Lumbar Spinal Stenosis: A Study of 49 Patients With Prospective Long-term Follow-up Chow NW, Southerst D, Wong JJ, Kopansky-Giles D, Ammendolia A
69 The Safety of Spinal Manipulative Therapy in Children Under 10 Years: A Rapid Review Corso M, Cancelliere C, Mior S, TaylorVaisey A, Côté P
70 Symptoms Patients Receiving Manual Therapy Experienced and Perceived as Adverse: A Secondary Analysis of a Survey of Patients’ Perceptions of What Constitutes an Adverse Response Funabashi M, Carlesso LC
71 Clinical Scenarios for Which Cervical Mobilization and Manipulation Are Considered by an Expert Panel to be Appropriate (and Inappropriate) for Patients with Chronic Neck Pain
Herman PM, Vernon H, Hurwitz EL, Shekelle PG, Whitley MD, Coulter ID
72 Trajectories of Pain Intensity Over 1 Year in Adults With Disabling Subacute or Chronic Neck Pain
Pico-Espinosa OJ, Côté P, Hogg-Johnson S, Jensen I, Axén I, Holm LW, Skillgate E
73 Perioperative Pain Management and Chronic Postsurgical Pain After Elective Foot and Ankle Surgery: A Scoping Review Stiegelmar C, Li Y, Beaupre LA, Pedersen MA, Dillane D, Funabashi M
74 A Pilot Study Assessing Patient-Centred Care in Patients with Chronic Health Conditions Attending Chiropractic Practice
Stuber KJ, Langweiler M, Mior S, McCarthy PW
75 Biomechanical Matching of Low Back External Demands During the Open- and Closed-Chain Side Bridge
Tuff T, Beach TAC, Howarth SJ
76 Prevalence of Low Back Pain, Pelvic Girdle Pain, and Combination Pain in a Pregnant Ontario Population
Weis CA , Barrett J, Tavares P, Draper C , Ngo K, Leung J, Huynh T, Landsman V
77 The Influence of Hip Joint Angle on the Ratio Between Adduction and Abduction Torque in Experienced, Recreational Male Ice Hockey Players Welsh P, Howitt S, Howarth SJ
78 The Passive Voice and Comprehensibility of Biomedical Texts: An Experimental Study with 2 Cohorts of Chiropractic Students Millar N, Budgell B
83 Promoting the Use of Self-Management in Patients with Spine Pain Managed by Chiropractors and Chiropractic Interns: Barriers and Design of a Theory-Based Knowledge Translation Intervention
Eilayyan O, Thomas A, Hallé MC, Ahmed S, Tibbles A, Jacobs C, Mior SA , et al.
84 Promoting the Use of Self-Management in Novice Chiropractors Treating Individuals with Spine Pain: The Design of a TheoryBased Knowledge Translation Intervention Eilayyan O, Thomas A, Hallé MC, Ahmed S, Tibbles A, Jacobs C, Mior SA et al.
85 The Development of a Global Chiropractic Rehabilitation Competency Framework by the World Federation of Chiropractic Côté P, Sutton D, Nicol R, Brown R and Mior S
86 Comparison of Chiropractic Student Lexicon at Two Educational Institutions: A CrossSectional Survey Gleberzon BJ, Pohlman KA, Russell E
87 “I Stay in Bed, Sometimes All Day.” A Qualitative Study Exploring Lived Experiences of Persons with Disabling Low Back Pain Esson SA, Côté P, Weaver R, Aartun E, Mior S
99 The Prevalence of Anxiety, Stress and Depressive Symptoms in Undergraduate Students at the Canadian Memorial Chiropractic College Meckamalil C, Brodie B, Hogg-Johnson S, Carroll LJ, Jacobs C, Côté P
100 Ontario Chiropractors' Knowledge of Exercise Guidelines for Pregnant Patients Weis CA , Baas E, Ciesla K, Kimpinski C, Landsman V
101 Health-Related Quality of Life and Balance Confidence Among Participants in a Senior Community-Based Exercise (SWIFT) Program Compared to Age Matched Controls: A Cross-Sectional Study
Cougle E, Black M, Hogg-Johnson S, Decina P, Tibbles A, Mior S
102 The Association Between Psychological and Social Factors and Spinal Pain in Adolescents Batley S, Aartun E, Boyle E, Hartvigsen J, Stern PJ, Hestbæk L
103 Clinicians’ Views About the Experience of Disability Due to Low Back Pain. Results From a Focus Group Study
Cedraschi C, Campello M, Salmi LR, Côté P
104 Exploring Chiropractic Services in the Canadian Forces Health Services –Perceptions of Facilitators and Barriers
Among Key Informants
Mior SA , Vogel E, Sutton D, French S, Côté P, Nordin M, Loisel P, Laporte A
113 System Dynamics to Investigate Opioid Use and Chiropractic Care for Chronic Musculoskeletal Pain
McGregor M, Nielsen A, Chung C, Fillery MD, Wakeland W, Mior S
114 Examining the Effects of Low Back Pain and Mental Health Symptoms on Healthcare Utilisation and Costs: A Protocol for a Population-Based Cohort Study
Wong JJ, Côté P, C Tricco, Rosella LC
115 The Global Spine Care Initiative: World Spine Care Executive Summary on Reducing SpineRelated Disability in Low- and Middle-Income Communities
Haldeman S, Nordin M, Chou R, Côté P, Hurwitz EL, Johnson CD, Randhawa K et al.
116 Reliability and Validity of Clinical Tests to Assess Posture, Pain Location, and Cervical Spine Mobility in Adults with Neck Pain and its Associated Disorders: Part 4. A Systematic Review from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration
Lemeunier N, Jeoun EB, M Suri, T Tuff, Shearer H, Mior S, Wong JJ, da Silva-Oolup S, Torres P, D'Silva C, Stern P, Yu H, Millan M, Sutton D, Murnaghan K , Côté P
117 Brain Drain: Psychosocial Factors Influence Recovery Following Mild Traumatic Brain Injury - 3 Recommendations for Clinicians Assessing Psychosocial Factors
Cancelliere C , Mohammed RJ
118 Relationship Between Early Prescription Dispensing Patterns and Work Disability in a Cohort of Low Back Pain Workers' Compensation Claimants: A Historical Cohort Study
Carnide N, Hogg-Johnson S, Koehoorn M, Furlan AD, Côté P
119 Non-Pharmacological Management of Persistent Headaches Associated with Neck Pain: A Clinical Practice Guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration
Côté P, Yu H, Shearer HM, Randhawa K, Wong JJ, Mior S, Ameis A, et al.
120 Manipulation and Mobilization for Treating Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis for an Appropriateness Panel
Coulter ID, Crawford C, Vernon H, Hurwitz EL, Khorsan R, Suttorp Booth M, Herman PM
121 Understanding Patient Profiles and Characteristics of Current Chiropractic Practice: A Cross-Sectional Ontario Chiropractic Observation and Analysis STudy (O-COAST)
Mior S, Wong JJ, Sutton D, Beliveau PJH, Bussières A, Hogg-Johnson S, French S
122 Opioid Overdose Hospitalization Trajectories in States with and without Opioid-Dosing Guidelines
SearsJM, Fulton-Kehoe D, Schulman BA, Hogg-Johnson S, and Franklin GM
123 Faculty Presentations: 2018-19
Academic Year
126 Faculty Presentations: 2019-2020
Academic Year
127 Accepted Presentations at Cancelled Venues
Welcome
In its 75 year history, CMCC has earned an outstanding reputation for the strength and rigour of its evidence-based curriculum and for its innovative and highly productive research program, one of the largest at a chiropractic institution in North America.

Research is one of the vital parts of the institutional mission: To deliver world class chiropractic education, research and patient care, and is a key pillar of our strategic plan. CMCC scientists, clinicians and educators play an essential role in probing, challenging and expanding the chiropractic knowledge base for the care and safety of patients suffering from musculoskeletal disorders and to contribute to the improvement of tomorrow’s chiropractors.
To that end, CMCC maintains a long term commitment to support impactful research through an active and diverse portfolio. Our group of full-time researchers and staff, a high percentage of our clinical and teaching faculty, along with our adjunct faculty and CMCC’s endowed Research Chair, all undertake to publish premier research on spinal manipulation and the chiropractic adjustment. They seek to answer the vital questions about the adjustment from a micro and macro level - how to increase its efficacy, understand its clinical relevance, and how best to apply it and integrate it within the health and performance spectrum.
It is our pleasure to provide you with the 2018-2020 Research Report – a report that speaks to the quality and diversity of research that has emerged from the collaborations and dedication of CMCC’s educators and scientists. It contains a selection of abstracts and seven feature articles from CMCC’s academic community published over these two academic years. It is the culmination of efforts from our dedicated scientists and collaborators in the five CMCC research streams:
1. Biological basis of manual therapies
2. Clinical and health services research



3. Education in health care
4. Health and wellness
5. Knowledge translation and health policy
The generous contributions from CMCC members and donors, as well as our funding agencies, national and provincial, have provided critical support to CMCC’s research efforts. Grantsmanship continues to yield strong returns and research productivity remains high in spite of the new challenges the pandemic introduced in 2020. With the emergence of COVID-19 around the globe, researchers who submitted and were approved to present their excellent work internationally were unfortunately not able to do so

CMCC Research Report 2018–2020 6
Dr. David Wickes President
Dr. Christine Bradaric-Baus Vice President, Academic
Dr. Silvano Mior Director, Research Partnerships and Health Policy
Dr. Samuel Howarth Director, Human Performance Research and McMorland Family Research Chair in Mechanobiology
Dr. Brian Budgell Director, Life Sciences Research
with the cancellation of essentially all external conferences and symposia. However the work that they have contributed and published is nonetheless of great significance and value to our health care community.
Reflecting on these two years of research, it is clear that the collaboration and integration of knowledge in each of these research streams has contributed to advancing the knowledge and understanding of chiropractic education and patient care and continues to empower knowledge translation between the research domains.
Please enjoy this sample of our scientists’ recent work as we look together toward the future.
Research Activity
Note:withtheemergenceoftheCOVID-19pandemicandsubsequentcancellationofalltravelandconferencesinandafterMarch2020, presentationsacceptedandscheduledcouldnotbedelivered.
A selection of published research by CMCC faculty 7
80 70 60 50 40 30 20 10 0 2014-15 2015-16 2016-17 2017-18 Publications Presentations 2018-19 2019-20 Lorem ipsu m Publications and Presentations
CMCC Research Report 2018–20
Grant Submissions by Funder
Grant Success
CMCC Research Report 2018–2020 8
38% Federal Government 4% Provincial Government 54% Foundation
14 12 10 8 6 4 2 0 2018-19 2014-15 2015-16 2016-17 2017-18 Declined Awarded 2019-20
Biological Basis of Musculoskeletal Injury and Manual Therapies
Effect of Cervical Manipulation on Vertebral Artery and Cerebral Haemodynamics in Patients with Chronic Neck
Pain: A Crossover Randomised Controlled Trial
Moser N1 , Mior S1,2 , Noseworthy M 3 , Côté P1,2 , Wells G 4 , Behr M 4 , Triano J1 1CanadianMemorialChiropracticCollege, 2UniversityofOntarioInstituteofTechnology, 3Queen'sUniversity, 4MacquarieUniversity, 5New York University, 6UniversityofToronto, 7Canadian Centre for Health Economics
Abstract
Objective:
It is hypothesised that cervical manipulation may increase the risk of cerebrovascular accidents. We aimed to determine whether cervical spine manipulation is associated with changes in vertebral artery and cerebrovascular haemodynamics measured with MRI compared with neutral neck position and maximum neck rotation in patients with chronic neck pain.
Setting:
The Imaging Research Centre at St. Joseph’s Hospital in Hamilton, Ontario, Canada.
Participants:
Twenty patients were included. The mean age was 32 years (SD ±12.5), mean neck pain duration was 5.3 years (SD ±5.7) and mean neck disability index score was 13/50 (SD ±6.4).
Interventions:
Following baseline measurement of cerebrovascular haemodynamics, we randomised participants to: (1) maximal neck rotation followed by cervical manipulation or (2) cervical manipulation followed by maximal neck rotation. The primary outcome, vertebral arteries and cerebral haemodynamics, was measured after each intervention and was obtained by measuring three-dimensional T1-weighted high-resolution anatomical images, arterial spin labelling and phase-contrast flow encoded MRI. Our secondary outcome was functional connectivity within the default mode network measured with resting state functional MRI.
Results:
Compared with neutral neck position, we found a significant change in contralateral blood flow following maximal neck rotation. There was also a significant change in contralateral vertebral artery blood velocity following maximal neck rotation and cervical manipulation. We found no significant
changes within the cerebral haemodynamics following cervical manipulation or maximal neck rotation. However, we observed significant increases in functional connectivity in the posterior cerebrum and cerebellum (resting state MRI) after manipulation and maximum rotation.
Conclusion
Our results are in accordance with previous work, which has shown a decrease in blood flow and velocity in the contralateral vertebral artery with head rotation. This may explain why we also observed a decrease in blood velocity with manipulation because it involves neck rotation. Our work is the first to show that cervical manipulation does not result in brain perfusion changes compared with a neutral neck position or maximal neck rotation. The changes observed were found to not be clinically meaningful and suggests that cervical manipulation may not increase the risk of cerebrovascular events through a haemodynamic mechanism.
Trial registration number NCT02667821
Introduction
Anecdotal evidence from case reports and case series suggest that neck manipulation increases the risk of vertebrobasilar artery stroke.1–3 However, the epidemiological evidence does not support this hypothesis.4 5 In their case-crossover study, Cassidy et al found that the risk of vertebrobasilar artery stroke was similar for patients with neck pain or headaches who consult physicians and those who consult chiropractors.4 This suggests that the hypothesised association is due to protopathic bias.
Understanding whether neck manipulation increases the risk of stroke is important because patients with neck pain frequently consult chiropractors and manipulation of the cervical spine is commonly performed for symptomatic relief.6–10 Dissection of the vertebral artery is involved in most cases that implicate cervical manipulation.11 However, when damage to the vertebral artery is absent, vasospasm12–15 and ‘subclinical’ endothelial injury have also been hypothesised to be causes of stroke.
A selection of published research by CMCC faculty 9
According to the vasospasm hypothesis, placing the head in rotation and hyperextension during a manipulation leads to considerable stress and stretch forces in the vertebral artery, specifically at the C2/C1 and cephalad/distal portion of the vertebral artery.16–18 This mechanical compression or stretching of the vertebral artery may lead to changes in blood flow and the subclinical injury to the vertebral artery can lead to thrombosis.19
Several studies have investigated changes in blood flow during cervical spine motion.20–28 Most studies report a decrease in vertebral artery flow contralateral to the side of rotation.20–23, 25–28 Less is understood about blood flow during and after a cervical manipulation, but two studies found no significant changes in vertebral artery blood flow or blood velocity following cervical manipulation in healthy individuals.29, 30 However, the impact of cervical manipulation on vertebral artery blood flow in the population likely to undergo this manoeuvre for therapeutic purposes is unknown. Neck pain patients may differ from that of healthy populations because moderate to severe perceived neck disability, as measured with the Neck Disability Index (NDI) is correlated with cortical hypoperfusion.31
Therefore, our primary aim was to determine whether cervical manipulation leads to a meaningful change in vertebral and cerebral haemodynamics compared with neutral neck position or neck rotation in adult patients with chronic neck pain. Our secondary aim was to compare the functional connectivity within the default mode network (DMN) between neutral neck position, neck rotation and cervical manipulation. We hypothesised that cervical manipulation or maximal neck rotation is associated with significant change in vertebral and cerebral haemodynamics compared with neutral neck position in adult patients with chronic neck pain.
Methods
Study design
We conducted a crossover randomised controlled study. In each subject, we randomised the sequence of cervical manipulation and maximal neck rotation and compared their effects on cerebrovascular haemodynamics. No washout period was used between each intervention. It was assumed that the time needed to measure the blood haemodynamics allowed enough time to return to their baseline status.32
Participants
Patients who were eligible for the study were attending a teaching clinic of the Canadian Memorial Chiropractic College, Toronto, Canada between September 2016 and April 2017. We recruited participants via poster advertising displayed at the teaching clinic, word of mouth and referrals from the supervising clinicians at the clinic. To be included, patients had to meet the following criteria:
(1) at least 18 years old; (2) chronic neck pain (≥3 months’ duration) defined as either neck pain-associated disorder or whiplashassociated disorder; (3) grade I–II neck pain,33 defined as neck pain
with no signs or symptoms of major structural pathology, which may or may not interfere with activities of daily living; (4) prescribed cervical manipulation by the clinician at the teaching clinic supervising their care and (5) provide written informed consent. Exclusion criteria were a history of neck pain with associated arm pain within the last 6 months; any current or history of neurological symptoms including facial or extremity weakness, abnormal sensation to the face, body, or extremities, uncontrolled movements, abnormal gait, dizziness, unexplained nausea/ vomiting, difficulty with speaking or swallowing; history of new or severe (Visual Analogue Scale >6/10) headaches in the last 3 months; any contraindications to MRI; or any history of using drugs that affect blood flow such as warfarin, or anticoagulants. In addition, all participants refrained from vigorous physical activity and ingesting alcohol and caffeine 1 day before their scheduled participation.
Randomisation and masking
We used simple randomisation to allocate participants to one of two sequences of interventions: (1) maximal neck rotation followed by upper cervical manipulation or (2) upper cervical manipulation followed by maximal neck rotation. The study coordinator (NM) conducted the randomisation using a randomised table generator (GraphPad Software, La Jolla, California, USA). The random allocation was communicated verbally to the study clinician (SM) on the day of the study protocol. Randomisation was concealed, no other study personnel or participants were aware of the intervention assignments.
Procedures
Prior to commencement of the study protocol, participants underwent a cervical spine examination by the clinician (SM) performing the test manoeuvres to identify the site of manipulation. Baseline information on each participant was collected and included: age, gender, height, weight, NDI score, neck pain intensity, duration of neck complaint and headache pain intensity (table 1).
Baseline MRI of the upper cervical spine and brain with the neck in the neutral position was conducted before randomisation. Neutral neck position was defined by alignment of the Frankfort plane in a vertical orientation. For continuity of neutral alignment during imaging between test conditions, the MRI laser land-marking tool was used to triangulate between three oil-based markers (vitamin E capsules) taped to the nasion (bridge of the nose) and immediately in front of the tragus of the ears, bilaterally.
CMCC Research Report 2018–2020 10
Table 1 Baseline participant characteristics

Following random allocation, either maximal neck rotation or cervical manipulation was first performed, followed by the other procedure. Maximal neck rotation was achieved by instructing participants to rotate their head as far as comfortably possible in the direction opposite to the side of clinical symptoms as elicited during the cervical spine examination. The clinician performing the interventions assisted the rotation via a soft hand contact on the patient’s head. The degree of maximal neck rotation was measured by an inclinometer and the position was held for 1 min before returning to neutral neck position for MRI sequencing. The cervical manipulation procedure was a high velocity, low amplitude impulse, with targeted contact at C1–C2 on the side of most discomfort as elicited on palpation, with the participant’s head in combined axial rotation, flexion and lateral flexion postures. Variations of head positions between operators for this procedure have been demonstrated to be relatively small.34 35 A practitioner with >30 years of practice experience conducted the cervical manipulation (SM).36–38 The manipulation procedure was performed on the adjustable and pivotal MRI bed in the MRI room with the participant in the supine position. The clinician performed the procedure by first establishing the end range of motion to determine appropriate preload position for the manipulation before applying a clinical force impulse in the coronal plane with minimal traction component.
Before each manoeuvre, the participants were queried on their comfort, condition and willingness to continue. The participant’s head was repositioned to neutral immediately after each manoeuvre, and then retracted into the MRI bore. Each manoeuvre was carried out on the scanner bed in the MRI room.
Outcomes
The primary outcome measure was cerebrovascular haemodynamics within the vertebral arteries and posterior cerebrum measured with MRI. The MRI data were acquired using a 3Telsa MR750 scanner and 20-channel neurovascular array radiofrequency coil (GE Healthcare, Milwaukee, Wisconsin, USA).
The primary outcome was measured following a standardised protocol. First, the baseline MRI was performed. The head was immobilised with sponges in a neutral neck position and a localiser scan was completed. Next, high-resolution anatomical images were collected using a three-dimensional (3D) inversion recovery prepped fast-spoiled gradient recalled echo T1weighted scan (repetition time [TR]/echo time [TE]=11.4/4.3 ms, TI=450 ms, flip angle=12°, 512×256 matrix, 140 slices, 24 cm field of view [FOV], reconstructed to 1 mm3 isotropic voxels). Following the anatomical scan, microvascular perfusion was assessed using a 3D spiral-based fast-spin echo pseudocontinuous arterial spin labelling (TE/TR/TI=10.5/4629/1525 ms, FOV=24 cm, 512×8 spiral interleaves, 3NEX, reconstructed to give an in-plane resolution of 1.875×1.875 [128×128] with 4 mm thick slices, scan time=30 s). Following arterial spin labelling (ASL), a phase-contrast scan for vertebral artery flow quantification was performed. At the upper cervical level C1–C2, the contralateral and ipsilateral vertebral arteries, defined to the direction of head motion, were assessed and anatomical images were established to localise the vertebral artery circulation. As previously published by Ho et al,39 the method for obtaining flow quantification of the vertebral artery was a two-dimensional phase-contrast pulse sequence. To capture accurate vertebral artery flow, the imaging plane is ideally perpendicular to the central axis of the blood vessel. This imaging plane was selected on the vessel of interest at the C1–C2 intervertebral level based on arterial visualisation on a maximum intensity projection of a 3D time-of-flight MRI angiogram. Acquisition parameters were as follows: fast gradient-recalled echo; echo time/repeat time=3.9/8.9 ms, flip angle=20o, 20 cm FOV; 512×512 matrix; 244 Hz/pixel receiver bandwidth; 1 average; 4 mm thick; and velocity encoding of 50 cm/s encoded over 30 phases per cardiac cycle. All image measurements were obtained by manually selecting the optimal anatomical site between the base of the odontoid process and ~1 cm above the tip of the dens. Data acquisition was triggered by peripheral gating using a pulse oximeter, with sequence acquisition time for each flow measurement being ~1.5 min, depending on heart rate.39 According to Lotz et al, vessel obliquity is tolerable to ±15°, above which will cause a significant deviation from true flow.40
The secondary outcome measure was functional connectivity within the DMN. For baseline measurement, this was performed immediately following the phase-contrast MRI, but prior to manipulation. Resting state functional MRI data (ie, blood oxygen level dependent, BOLD signal) was acquired using a gradient echo, echo planar imaging sequence (64×64 matrix, 28 axial slices [5 mm thick, no skip], 24 cm FOV, TE/TR/flip angle=35 ms/2000 ms/90o, 180 temporal points, total scan time=6 min). During the resting state scan, participants were asked to keep their eyes open, stay awake and not think of anything in particular.
A selection of published research by CMCC faculty 11 Moser et al
Following the baseline MRI scan, the image sequence to obtain the primary and secondary outcomes changed to the following: 3-plane localiser, ASL, phase-contrast, resting state MRI and 3D anatomical scan. The latter three were always performed with the 3D anatomical last seeing as microvascular changes (ie, blood flow) were more likely to be detected early after the cervical manipulation and maximal neck rotation, while structural changes (ie, 3D scan) would not be expected to occur. Participants were scanned a total of three times for each session: baseline, and two procedures in random order.
After testing, each participant was observed for 1 hour and contacted by a study coordinator (NM) within 24 hours of release for follow-up on status. Adverse events, defined as side effects that are harmful, were assessed via open-ended questions.41 These included local soreness and pain in the area of the applied test manoeuvres (minor adverse events), as well as signs of stroke or transient ischaemic attack (major adverse events).
Statistical analysis
Previous research examining reproducibility of cerebral perfusion measurements using ASL suggested that the mean per cent perfusion difference was 7.1 (SD ±12).42 To date, no study has provided information on cerebral blood flow and perfusion after mechanical challenges to the cervical spine.43 Since minimal clinically important differences have not yet been established, we chose to calculate the study sample size by assuming an effect size. We assumed that a change of at least 2 SD from the normal mean flow would indicate a significant variability of the haemodynamics to the mechanical challenges performed to the cervical spine. Based on this effect size, a power of 80%, a significance level at p<0.05 and two-sided t-test, we calculated that a sample size of 16 participants was necessary.43 We increased our sample size by 20% (n=20 participants) to account for possible dropouts.
An experienced analyst (MB), who remained blinded to the sequence of test manoeuvres, performed the data quantification of the primary and secondary outcomes. Microvascular perfusion and resting state MRI data were analysed using analysis of functional neuroimaging (AFNI).44 For each participant, all ASL and resting state MRI data were spatially registered to the initial (neutral condition) position. Anatomical, blood flow and functional data were transformed automatically to the Colin27 atlas, using the AFNI command @ auto_tlrc, with functional data resampled to a 2 mm isometric grid.45 Temporal band-pass filtering with cut-offs of 0.009 Hz < f < 0.08 Hz was performed in order to suppress unwanted physiological signals and some hardware noise.46 Functional connectivity within the DMN was assessed using the AFNI plugin InstaCorr, a seed-based approach, which uses the Pearson method of correlation to compare time signals.47 The DMN is the most dominant temporally correlated resting network in the awake brain, defined as regions positively correlated in time with the posterior cingulate cortex (PCC) seed voxel. The PCC
was defined automatically using the AFNI Talairach method ‘Talairach to’ and selecting a single voxel from each the left and right PCC for one analysis (ColinN27 coordinates: 10, 54, 14 and − 10 , 54, 14). These were both subsequently fused in the post processing. A 5 mm with full width at half maximum (FWHM) Gaussian spatial smoothing filter was applied for maximise likelihood of overlap with interparticipant group analysis. Also, temporal outliers determined with the AFNI function 3dToutcount were censored out. Finally, the AFNI plugin 3dClustSim was used to threshold any clusters with fewer than 20 voxels. The ASL cerebral blood flow data were analysed similar to resting state MRI in that following spatial coregistration to the neutral condition and spatial blurring with a 5 mm FWHM Gaussian convolution kernel, ASL data were warped to the N27 atlas. Group analysis was accomplished using a repeat one-way within-participant 3D-analysis of variance (ANOVA), with the one factor being neck position. Post hoc testing included contrasts between neutral, maximum voluntary rotation and cervical manipulation, and also a contrast between maximum voluntary rotation and cervical manipulation. Statistical significance was defined as anything lower than an alpha value of 0.05, with prior cluster thresholding dealing with multiple comparisons.
Flow analysis was performed using Segment V.1.9 software 47 (Medviso, Lund, Sweden). Dynamic regions of interest were drawn on the left and right vertebral arteries to quantify the mean, as well as peak velocity and flow. Data in the trigger window portion of the cardiac cycle were derived by spline interpolation using Matlab (Mathworks, Natick, Massachusetts, USA). Mean and SDs were calculated for vertebral artery blood velocity, flow, peak velocity and peak flow for each of the head conditions and vertebral artery side. Differences between task manoeuvres and vertebral artery flow and velocity were evaluated using a two-way ANOVA with factors for participants and head position. The level of significance was set at 0.05. Analyses were conducted using R-project V.2.12.1 (R Development Core Team, 2010. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http:// www. R- project. org/) and SAS software. Vertebral artery blood flow variability was calculated over the 30 phases per cardiac cycle by examining the flow errors in the left and right vertebral arteries for each of the conditions. Additionally, we analysed the impact of order of procedures by examining the interaction between order and head position in the two-way ANOVA.48
Results
Between September 2016 and April 2017, a total of 936 participants were screened for the study; 916 failed prescreening (figure 1). Most did not meet the inclusion criteria (n=890); 446 participants were found to have acute neck pain (<3 months of duration); 119 participants had pain in the upper extremity and/or were identified to have radicular symptoms;
CMCC Research Report 2018–2020 12
216 participants were not receiving spinal manipulative therapy to the cervical spine as part of their ongoing treatment; 68 participants reported >6/10 headache intensity on average; 15 participants were using anticoagulants; 3 participants declined to participate; 23 participants were either unable to acquire transportation to the study location or unable to attend the scheduled time. Twenty participants (14 female, 6 male) aged 23–66 years (mean [SD], 32 [±12.5] years) were enrolled in the study. The average NDI score was 13/50 (SD ±6.4) with an average neck pain intensity of 5/10 (SD ±2.1) and a mean duration of neck pain of 5.3 years (SD ±5.7) (table 1).
The total time elapsed for each participant testing protocol was 60 min. The total time elapsed for each test manoeuvre was ~20 min. This included applying the test manoeuvre (maximum of 1 min), replacing the participant back into the MRI bore (~1 min) and image sequencing as noted above (~18 min).
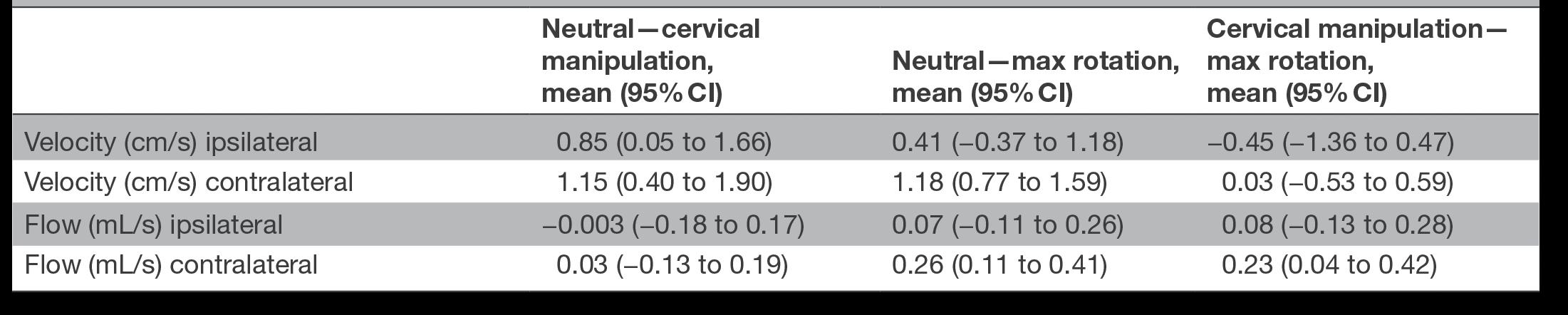
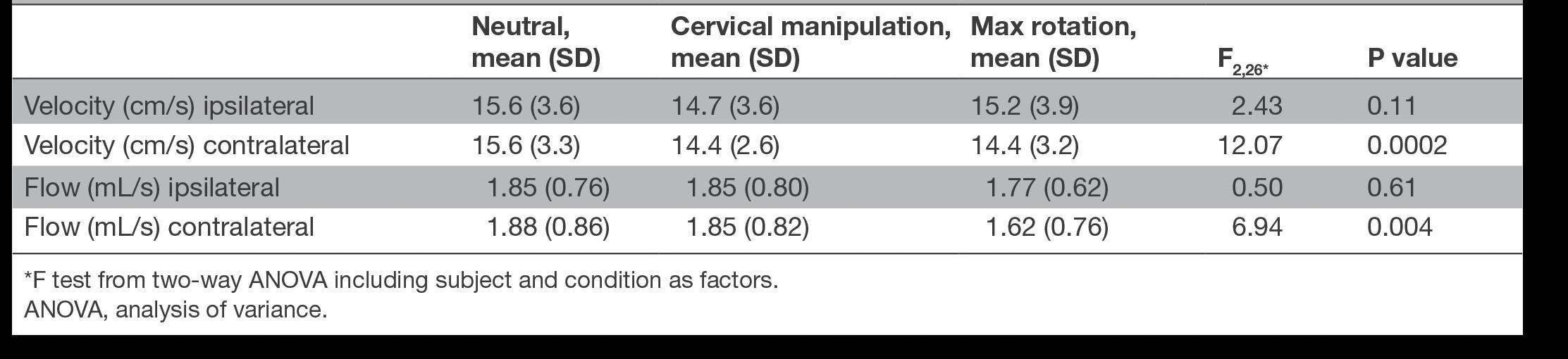
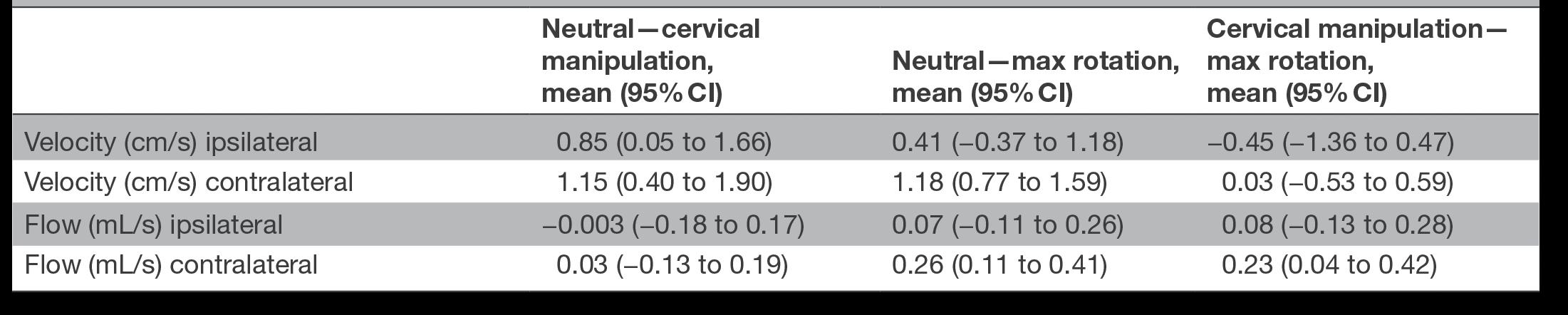
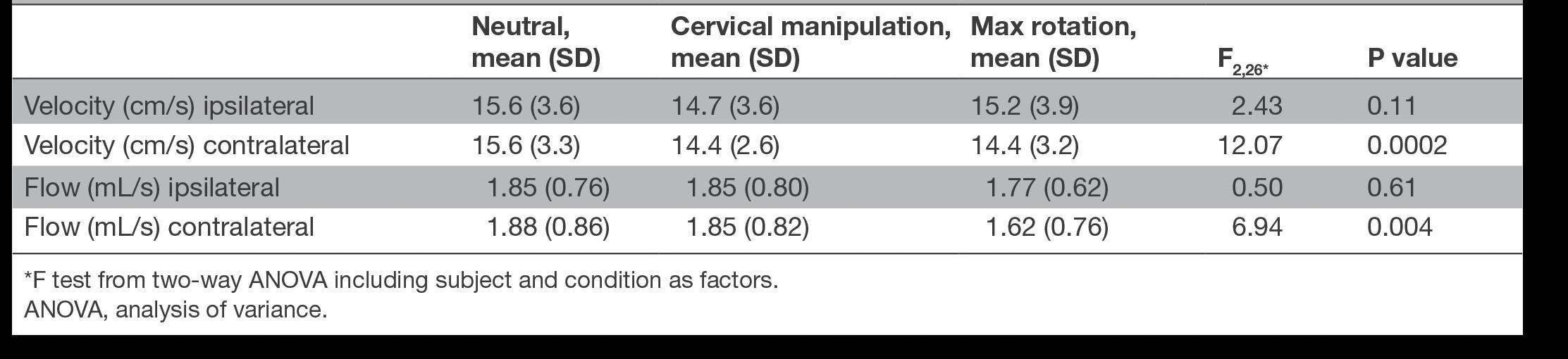
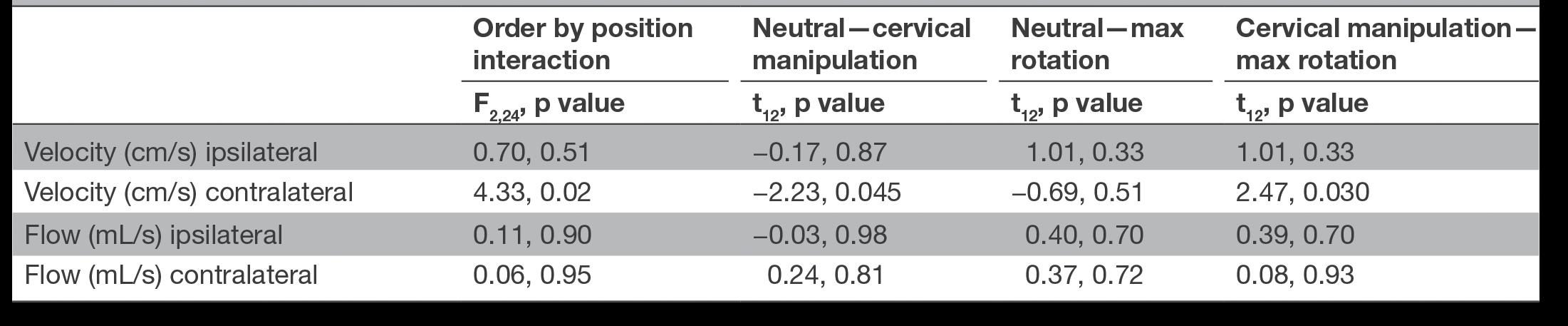
When compared with neutral neck position, maximal neck rotation and cervical manipulation did not significantly alter cerebral perfusion within the posterior cerebrum or cerebellum (table 2). A significant change was found in both contralateral vertebral artery blood flow and blood velocity between the three procedures (table 3). When comparing interventions to discern

A selection of published research by CMCC faculty 13
Moser et al Fig1Protocolflowandmethodprocess.
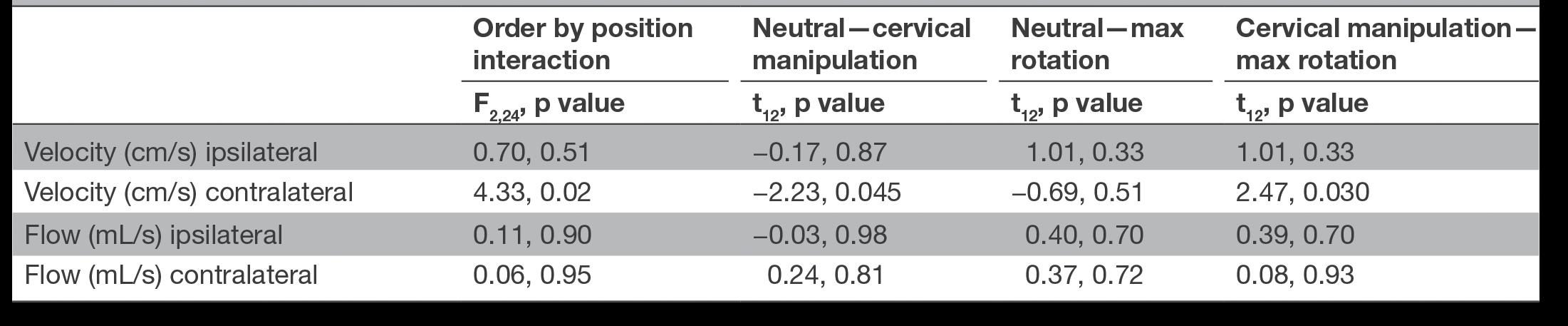
which interventions were different, we found a significant difference in the contralateral vertebral artery blood flow between neutral and maximal neck rotation (0.26 mL/min, 95% CI 0.11 to 0.41) as well as between cervical manipulation and maximal neck rotation (0.23, 95% CI 0.04 to 0.42). We also found a significant difference in contralateral vertebral artery blood velocity between neutral and cervical manipulation (1.15, 95% CI 0.4 to 1.9) and between neutral and maximal neck rotation (1.18, 95% CI 0.77 to 1.59) (table 4). Finally, we found no significant differences in flow variability within the vertebral arteries between the interventions (online supplementary figures I and II).
We measured a significant increased functional connectivity post manipulation (p<0.05). More specifically, when compared with the resting position, the following areas showed significantly increased functional connectivity: uvula, cerebellar tonsils, left fusiform gyrus and left middle temporal gyrus, right middle temporal gyrus, right middle occipital gyrus, bilateral cuneus, left precuneus and left middle occipital gyrus (online supplementary table I).
When examining for an order effect of experimental procedures on outcomes, we found a significant order effect only for contralateral vertebral artery blood velocity (table 5, p=0.02). For subjects receiving the manipulation first, the difference in contralateral velocity between manipulation and maximal rotation conditions is on average 0.50 cm/s (95% CI −0.15 to 1.16), whereas it is on average −0.60 cm/s (95% CI −1.54 to 0.34) if they received the manipulation second. That is, velocity is higher for which ever condition comes first.

No major adverse events were reported. One minor adverse event, mild neck soreness, was reported immediately post procedure by one participant. The participant attributed the soreness to having to lay motionless on the hard scanner bed during study protocol.
Discussion
Our primary objective was to assess the cerebrovascular and vertebral artery blood flow and velocity changes between various head positions including cervical manipulation in patients with chronic neck pain. We found no significant cerebral perfusion changes within the posterior cerebrum or cerebellum. There was, however, a significant change in the contralateral vertebral artery blood flow following maximal neck rotation. We found similar changes in the contralateral vertebral artery blood velocity following both cervical manipulation and maximal neck rotation. We found no significant change in blood flow variability between the vertebral arteries, nor between the various head positions. The decrease in contralateral blood flow to the side of maximal rotation supports previous studies.16 The finding of nonsignificant change in blood flow ipsilateral and contralateral to the side of cervical manipulation is also consistent with previous works.29 30 Unlike previous work, our results suggest a significant change in contralateral blood velocity following cervical manipulation and maximal head rotation. Given the changes in vertebral artery haemodynamics are more pronounced following maximal head rotation compared with cervical manipulation, specifically in contralateral flow, the changes may be the result of the head turning rather than the effect of the thrust associated with cervical manipulation. This assumption is supported by Herzog et al who suggest that cervical manipulation imposes less stretch to the vertebral artery than the turning of the head.18
No reference values for minimally clinically important differences in the vertebral artery blood flow and velocities have been established. However, haemodynamic stenosis has been long considered as a diameter reduction of >50%, which in the vertebral artery has been associated with a peak and enddiastolic flow >108 and 36 cm/s, respectively.49 As suggested by Licht et al, 21 a change in peak velocity of >25% from baseline would be necessary for clinically relevant decrease in the vertebral artery. We observed no such reductions in our study. Furthermore, an arbitrary threshold of 200 mL/min net vertebral
CMCC Research Report 2018–2020 14
Table 2 Mean cerebral and cerebellar perfusion (in millilitres per 100 grams of tissue per minute) for each condition as determined by arterial spin labelling technique
artery flow volume was originally proposed and below this value patients were said to be at risk of becoming symptomatic with vertebrobasilar ischaemia.50 Seidel et al, however, reported that net vertebral artery blood flow volume of less than ~100 mL/ min can be considered as an indicator of low blood volume.51 In our study, the net vertebral artery blood flow volume showed that in both experimental procedures, values remained >200 mL/min (222 mL/min for cervical manipulation and 203 mL/min for maximal neck rotation). When examining flow changes, the largest change was 14%, which occurred in the contralateral vertebral artery following maximal rotation. When we examined the vertebral artery blood velocities, we found a 7% change for both cervical manipulation and maximal rotation compared with neutral. Therefore, the relative blood flow and velocity changes observed are small and not considered clinically relevant. Continuing, none of the participants during any of the experimental procedures reported, or were observed by the investigators, to have any signs or symptoms of neurological compromise. Although vertebral artery blood flow and velocity reductions can occur with head positional changes, the individual typically remains asymptomatic due to several factors, including the presence of collateral circulation.52 53 In the present work, this was illustrated by the preservation of cerebral perfusion despite the changes in contralateral vertebral artery haemodynamics.
Vertebrobasilar artery stroke secondary to vertebral artery dissection is a rare but devastating occurrence.54 A unique
characteristic of these strokes is that they can develop in healthy adults and they frequently occur in close temporal relationship to benign neck movements,55 56 cervical manipulation57 or trivial trauma.58 59 Due to the rarity of the condition, very little is known about the risk factors for vertebrobasilar artery stroke. Our study extends the understanding on the effects of cervical manipulation on vertebral artery and cerebrovascular haemodynamics. It is also the first study to directly measure the impact of cervical spinal manipulation on intracranial and extracranial blood flow in a chronic neck pain population. Together with previous work,29 30 our results support the position that the association between cervical manipulation and stroke is due to protopathic bias.4
When compared with a neutral neck position, both maximum voluntary neck rotation and cervical manipulation resulted in significantly increased functional connectivity throughout the DMN as seen on the BOLD signal. Changes in the BOLD signal arise from complex interactive modulation of blood flow, blood volume and local metabolic rate, all leading to change in the local ratio of oxyhaemoglobin to deoxyhaemoglobin. This ratio drives the change in BOLD signal through magnetic susceptibility differences that exist between oxidation states of the haemoglobin complex. The areas affected within the DMN have been identified as being involved with functions of visually guided eye movements,60 facial and word recognition,61 visuospatial processing,62 episodic memory, reflection on self and consciousness.63 The observed increase in functional
A selection of published research by CMCC faculty 15 Moser et al
Table 3 ANOVA statistics comparing mean flow and velocity across head positions for ipsilateral and contralateral side, controlling for subject
Table 4 Mean paired differences between baseline and interventions
connectivity may be a consequence of sensory stimulation and patient self-awareness from handling of a body region such as the neck. When examining the aforementioned areas specifically for changes in blood flow using ASL, no significant changes were observed between any of the test head conditions. This strongly suggests that the observed increased functional connectivity were not a result of altered blood flow but secondary to changes in either blood volume or metabolic activity.
Our study had strengths. First, our design ensured control of confounders and provided statistical efficiency. Second, we used phase-contrast MRI blood flow measurement because of its greater sensitivity compared with ultrasonography (which would not have been able to adequately penetrate through bone to probe the vessels we wanted to measure), and because it is considered the criterion standard for both diagnosis of vertebrobasilar artery stroke and quantifying blood flow.39, 64–67 Estimates of repeatability of flow measures were made in preliminary work by quantifying vertebral artery flow in a single healthy participant twice over a 2-month interval.29
A limitation of the study was the restriction of analysis to a time (average 115 s) following the test manoeuvres. Realtime measures currently are technically not feasible and transient effects of various neck positions on vertebral artery and cerebrovascular haemodynamics may have been missed. Post manoeuvre analysis makes comparisons with other realtime studies challenging. Thus, the results only describe post procedural effects and cannot be generalised to the possible effects occurring during the test manoeuvres. However, it is notable that to be clinically relevant, sustained changes would likely be required that would extend into the sampled time interval of this study. Moreover, the possibility that neck pain participants exist who exhibit idiosyncratic responses cannot be excluded. To date, no such mechanisms have been measured and reported in the literature.
In conclusion, we found no significant change in blood flow in the posterior cerebrum or cerebellum in chronic neck pain participants after maximum head rotation and cervical manipulation. In addition, we found no clinically meaningful changes in the blood flow or velocity in the vertebral arteries before–after head positional change and spinal manipulation.
Our study adds to a growing body of knowledge regarding the impact of head position and cervical manipulation on vascular and neural activity in patients with neck pain. It is the first study to measure cerebral blood flow, vertebral artery blood flow and velocity in patients undergoing neck manipulation for neck pain. Our study does not support the hypothesis that neck manipulation or neck rotation are associated with vasospasm of the vertebral artery.
Patient and public involvement
Patients and public were not involved in the development, design, recruitment and randomisation of this study.
Author affiliations
1Graduate Studies, Canadian Memorial Chiropractic College, Toronto, Ontario, Canada
2Faculty of Health Sciences, University of Ontario Institute of Technology, Oshawa, Ontario, Canada
3Radiology, McMaster University Faculty of Engineering, Hamilton, Ontario, Canada
4Faculty of Health Sciences, University of Ontario Institute of Technology, Oshawa, Ontario, Canada
5Faculty of Kinesiology and Physical Education, University of Toronto, Toronto, Ontario, Canada
6Department of Medicine, Division of Physical Medicine and Rehabilitation, University of Toronto, Toronto, Ontario, Canada
Acknowledgements
Appreciation is extended to MRI technologists at the Imaging Research Centre for their assistance in data capture and for all of their support and effort with this study. Similarly, thanks are due to the Imaging Research Centre at St Joseph’s Healthcare and Dr Shanker Nesathurai and the Department of Physical Medicine and Rehabilitation at St Joseph’s Hospital for their ongoing support in this project. Special thanks are given to Dr Sheilah Hogg-Johnson for her timely help with this work’s statistical analysis.
Contributors
Concept development (provided idea for the research): NM, JT, GW and SM. Design (planned the methods to generate the results): NM, JT, MN and GW. Supervision (provided oversight,
CMCC Research Report 2018–2020 16
Table 5 Order effect on vertebral artery haemodynamics
responsible for organisation and implementation, writing of the manuscript): NM, SM, JT, GW and PC. Data collection/ processing (responsible for experiments, patient management, organisation or reporting data): NM, SM, MB and MN. Analysis/ interpretation (responsible for statistical analysis, evaluation and presentation of the results): NM, MB, SM, JT, GW and MN. Literature search (performed the literature search): NM. Writing (responsible for writing a substantive part of the manuscript): NM and SM. Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): NM, SM, PC, MN, GW and JT. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding
Partial financial support was provided by the Canadian Chiropractic Protective Association and NCMIC Research Foundation and Canadian Memorial Chiropractic College.
Disclaimer
The funders of the study had no role in the study design, data collection, data analysis, data interpretation or writing of the report.
Competing interests
Conflicts of interest were reported for this study include the following: JT is an occasional lecturer on behalf of NCMIC and CCPA, and MN received an honorarium for lecture on behalf of Bayer.
Patient consent for publication
Not required.
Ethics approval
The McMaster University Hamilton Integrated Research Ethics Board (HiREB) (REB#1303) and Canadian Memorial Chiropractic College Research Ethics Board approved the study (REB# 1604×01).
Provenance and peer review
Not commissioned; externally peer reviewed.
Data sharing statement
No additional data are available.
Open access
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http:// creativecommons. org/licenses/by-nc/4.0/.
References
1. Albuquerque FC, Hu YC, Dashti SR, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg 2011;115:1197–205.
2. Ernst E. Manipulation of the cervical spine: a systematic review of case reports of serious adverse events, 19952001. Med J Aust 2002;176:376–80.
3. Norris JW, Beletsky V, Nadareishvili ZG. Sudden neck movement and cervical artery dissection. The Canadian Stroke Consortium. CMAJ 2000;163:38–40.
4. Cassidy JD, Boyle E, Côté P, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine 2008;33(4 Suppl):S176–83.
5. Boyle E, Côté P, Grier AR, et al. Examining vertebrobasilar artery stroke in two Canadian provinces. Spine 2008;33(4 Suppl):S170–5.
6. Côté P, Wong JJ, Sutton D, et al. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J 2016;25:2000–22.
7. Kjaer P, Kongsted A, Hartvigsen J, et al. National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy. Eur Spine J 2017;26:2242–57.
8. Hurwitz EL, Coulter ID, Adams AH, et al. Use of chiropractic services from 1985 through 1991 in the United States and Canada. Am J Public Health 1998;88:771–6.
9. Hurwitz EL, Chiang LM. A comparative analysis of chiropractic and general practitioner patients in North America: findings from the joint Canada/United States Survey of Health, 2002-03. BMC Health Serv Res 2006;6:49.
10. Haldeman S, Carey P, Townsend M, et al. Arterial dissections following cervical manipulation: the chiropractic experience. CMAJ 2001;165:905–6.
11. Patijn J. Complications in manual medicine: A review of the literature. J Manual Med 1991;6:89–92.
12. Smith RA, Estridge MN. Neurological complications of head and neck manipulations: A report of two cases. JAMA 1962;182:528–31.
13. Frisoni GB, Anzola GP. Vertebrobasilar ischemia after neck motion. Stroke 1991;22:1452–60.
14. Mann T, Refshauge KM. Causes of complications from cervical spine manipulation. Aust J Physiother 2001;47:255–66.
15. Schmitt HP. Anatomical structure of the cervical spine with reference to pathology of manipulation complications. Man Med 1991;6:93–101.
16. Mitchell J. Vertebral Artery Blood flow Velocity Changes Associated with Cervical Spine rotation: A Meta-Analysis of the Evidence with implications for Professional Practice. J Man Manip Ther 2009;17:46–57.
17. Kawchuk GN, Jhangri GS, Hurwitz EL, et al. The relation between the spatial distribution of vertebral artery
A selection of published research by CMCC faculty 17
Moser et al
compromise and exposure to cervical manipulation. J Neurol 2008;255:371–7.
18. Herzog W, Leonard TR, Symons B, et al. Vertebral artery strains during high-speed, low amplitude cervical spinal manipulation. J Electromyogr Kinesiol 2012;22:740–6.
19. Dunne JW, Conacher GN, Khangure M, et al. Dissecting aneurysms of the vertebral arteries following cervical manipulation: a case report. J Neurol Neurosurg Psychiatry 1987;50:349–53.
20. Arnold C, Bourassa R, Langer T, et al. Doppler studies evaluating the effect of a physical therapy screening protocol on vertebral artery blood flow. Man Ther 2004;9:13–21.
21. Licht PB, Christensen HW, Højgaard P, et al. Vertebral artery flow and spinal manipulation: a randomized, controlled and observer-blinded study. J Manipulative Physiol Ther 1998;21:141–4.
22. Mitchell JA. Changes in vertebral artery blood flow following normal rotation of the cervical spine. J Manipulative Physiol Ther 2003;26:347–51.
23. Mitchell J, Keene D, Dyson C, et al. Is cervical spine rotation, as used in the standard vertebrobasilar insufficiency test, associated with a measureable change in intracranial vertebral artery blood flow? Man Ther 2004;9:220–7.
24. Mitchell J, Kramschuster K. Real-time ultrasound measurements of changes in suboccipital vertebral artery diameter and blood flow velocity associated with cervical spine rotation. Physiother Res Int 2008;13:241–54.
25. Rivett DA, Sharples KJ, Milburn PD. Effect of premanipulative tests on vertebral artery and internal carotid artery blood flow: a pilot study. J Manipulative Physiol Ther 1999;22:368–75.
26. Rivett DA, Sharples KJ, Milburn PD. Reliability of ultrasonograpahic measurement of vertebral artery blood flow. NZ J Physiother 2003;31:119–28.
27. Rossitti S, Volkmann R, Lofgren J. Changes of blood flow velocity in the vertebro-basilar circulation during rotation of the head in the normal human. Biomech Sem 1992;6:92–9.
28. Stevens A. Functional Doppler sonography of the vertebral artery and some considerations about manual techniques. Man Med 1991;6:102–5.
29. Quesnele JJ, Triano JJ, Noseworthy MD, et al. Changes in vertebral artery blood flow following various head positions and cervical spine manipulation. J Manipulative Physiol Ther 2014;37:22–31.
30. Erhardt JW, Windsor BA, Kerry R, et al. The immediate effect of atlanto-axial high velocity thrust techniques on blood flow in the vertebral artery: A randomized controlled trial. Man Ther 2015;20:614–22.
31. Bakhtadze MA, Vernon H, Karalkin AV, et al. Cerebral perfusion in patients with chronic neck and upper back pain: preliminary observations. J Manipulative Physiol Ther 2012;35:76–85.
32. Barrett KE, Ganong WF. Ganong’s Review of Medical
Physiology. 25th ed. New York, NY: McGraw-Hill Medical, 2015.
33. Guzman J, Haldeman S, Carroll LJ, et al. Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Clinical practice implications of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. Spine 2008;33(4 Suppl):S199–213.
34. Cambridge ED, Triano JJ, Ross JK, et al. Comparison of force development strategies of spinal manipulation used for thoracic pain. Man Ther 2012;17:241–5.
35. Descarreaux M, Dugas C, Raymond J, et al. Kinetic analysis of expertise in spinal manipulative therapy using an instrumented manikin. J Chiropr Med 2005;4:53–60.
36. Cohen E, Triano JJ, McGregor M, et al. Biomechanical performance of spinal manipulation therapy by newly trained vs. practicing providers: does experience transfer to unfamiliar procedures? J Manipulative Physiol Ther 1995;18:347–52.
37. Triano JJ, Rogers CM, Combs S, et al. Developing skilled performance of lumbar spine manipulation. J Manipulative Physiol Ther 2002;25:353–61.
38. Triano JJ, Rogers CM, Combs S, et al. Quantitative feedback versus standard training for cervical and thoracic manipulation. J Manipulative Physiol Ther 2003;26:131–8.
39. Ho SS, Chan YL, Yeung DK, et al. Blood flow volume quantification of cerebral ischemia: comparison of three noninvasive imaging techniques of carotid and vertebral arteries. AJR Am J Roentgenol 2002;178:551–6.
40. Lotz J, Meier C, Leppert A, et al. Cardiovascular flow measurement with phase-contrast MR imaging: basic facts and implementation. Radiographics 2002;22:651–71.
41. Ioannidis JP, Evans SJ, Gøtzsche PC, et al. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Ann Intern Med 2004;141:781–8.
42. Parkes LM, Rashid W, Chard DT, et al. Normal cerebral perfusion measurements using arterial spin labeling: reproducibility, stability, and age and gender effects. Magn Reson Med 2004;51:736–43.
43. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Erlbaum Associates, Publishers, 1988.
44. Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res 996;29:162–73.
45. Holmes CJ, Hoge R, Collins L, et al. Enhancement of MR images using registration for signal averaging. J Comput Assist Tomogr 1998;22:324–33.
46. Jang JH, Kim JH, Jung WH, et al. Functional connectivity in fronto-subcortical circuitry during the resting state in obsessive-compulsive disorder. Neurosci Lett 2010;474:158–62.
47. Wang J, Wang L, Zang Y, et al. Parcellation-dependent small-world brain functional networks: a resting-state fMRI study. Hum Brain Mapp 2009;30:1511–23.
CMCC Research Report 2018–2020 18
48. Fleiss JL. The Design and Analysis of Clinical Experiments. Toronto: Wiley, 1986.
49. Yurdakul M, Tola M. Doppler criteria for identifying proximal vertebral artery stenosis of 50% or more. J Ultrasound Med 2011;30:163–8.
50. Bendick PJ, Glover JL. Vertebrobasilar insufficiency: evaluation by quantitative duplex flow measurements. A preliminary report. J Vasc Surg 1987;5:594–600.
51. Seidel E, Eicke BM, Tettenborn B, et al. Reference values for vertebral artery flow volume by duplex sonography in young and elderly adults. Stroke 1999;30:2692–6.
52. Arnetoli G, Amadori A, Stefani P, et al. Sonography of vertebral arteries in De Kleyn’s position in subjects and in patients with vertebrobasilar transient ischemic attacks. Angiology 1989;40:716–20.
53. Sakaguchi M, Kitagawa K, Hougaku H, et al. Mechanical compression of the extracranial vertebral artery during neck rotation. Neurology 2003;61:845–7.
54. Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol 2009;8:668–78.
55. Senter HJ, Sarwar M. Nontraumatic dissecting aneurysm of the vertebral artery. Case report. J Neurosurg 1982;56:128–30.
56. Sherman DG, Hart RG, Easton JD. Abrupt change in head position and cerebral infarction. Stroke 1981;12:2–6.
57. Haldeman S, Kohlbeck FJ, McGregor M. Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation therapy: a review of sixty-four cases after cervical spine manipulation. Spine 2002;27:49–55.
58. Josien E. Extracranial vertebral artery dissection: nine cases. J Neurol 1992;239:327–30.
59. Okawara S, Nibbelink D. Vertebral artery occlusion following hyperextension and rotation of the head. Stroke 1974;5:640–2.
60. Heinen SJ, Keller EL. The function of the cerebellar uvula in monkey during optokinetic and pursuit eye movements: single-unit responses and lesion effects. Exp Brain Res 1996;110:1–14.
61. Kanwisher N, Yovel G. The fusiform face area: a cortical region specialized for the perception of faces. Philos Trans R Soc Lond B Biol Sci 2006;361:2109–28.
62. Lamm C, Windischberger C, Leodolter U, et al. Evidence for premotor cortex activity during dynamic visuospatial imagery from single-trial functional magnetic resonance imaging and event-related slow cortical potentials.
Neuroimage 2001;14:268–83.
63. Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain 2006;129:564–83.
64. Sengelhoff C, Nebelsieck J, Nassenstein I, et al. Neurosonographical follow-up in patients with spontaneous cervical artery dissection. Neurol Res 2008;30:687–9.
65. Dittrich R, Dziewas R, Ritter MA, et al. Negative ultrasound findings in patients with cervical artery dissection. Negative
ultrasound in CAD. J Neurol 2006;253:424–33.
66. Nebelsieck J, Sengelhoff C, Nassenstein I, et al. Sensitivity of neurovascular ultrasound for the detection of spontaneous cervical artery dissection. J Clin Neurosci 2009;16:79–82.
67. Oktar SO, Yücel C, Karaosmanoglu D, et al. Blood-flow volume quantification in internal carotid and vertebral arteries: comparison of 3 different ultrasound techniques with phase-contrast MR imaging. AJNR Am J Neuroradiol 2006;27:363–9.
OriginallypublishedinBMJOpen,2019May28;9(5):e025219. ReproducedwithpermissionunderCCBY-NC.
AccessOnline:https://doi.org/10.1136/bmjopen-2018-025219
A selection of published research by CMCC faculty 19 Moser et al
Biological Basis of Musculoskeletal Injury and Manual Therapies
NTG-101: A Novel Molecular Therapy that Halts the Progression of Degenerative Disc Disease
Matta A1, Karim MZ1, Gerami H1, Jun P 2 , Funabashi M2,6 , Kawchuk G 2 , Goldstein A
, Foltz W 3 , Sussman M 3 , Eek BC 4 , Erwin WM 1,5,6
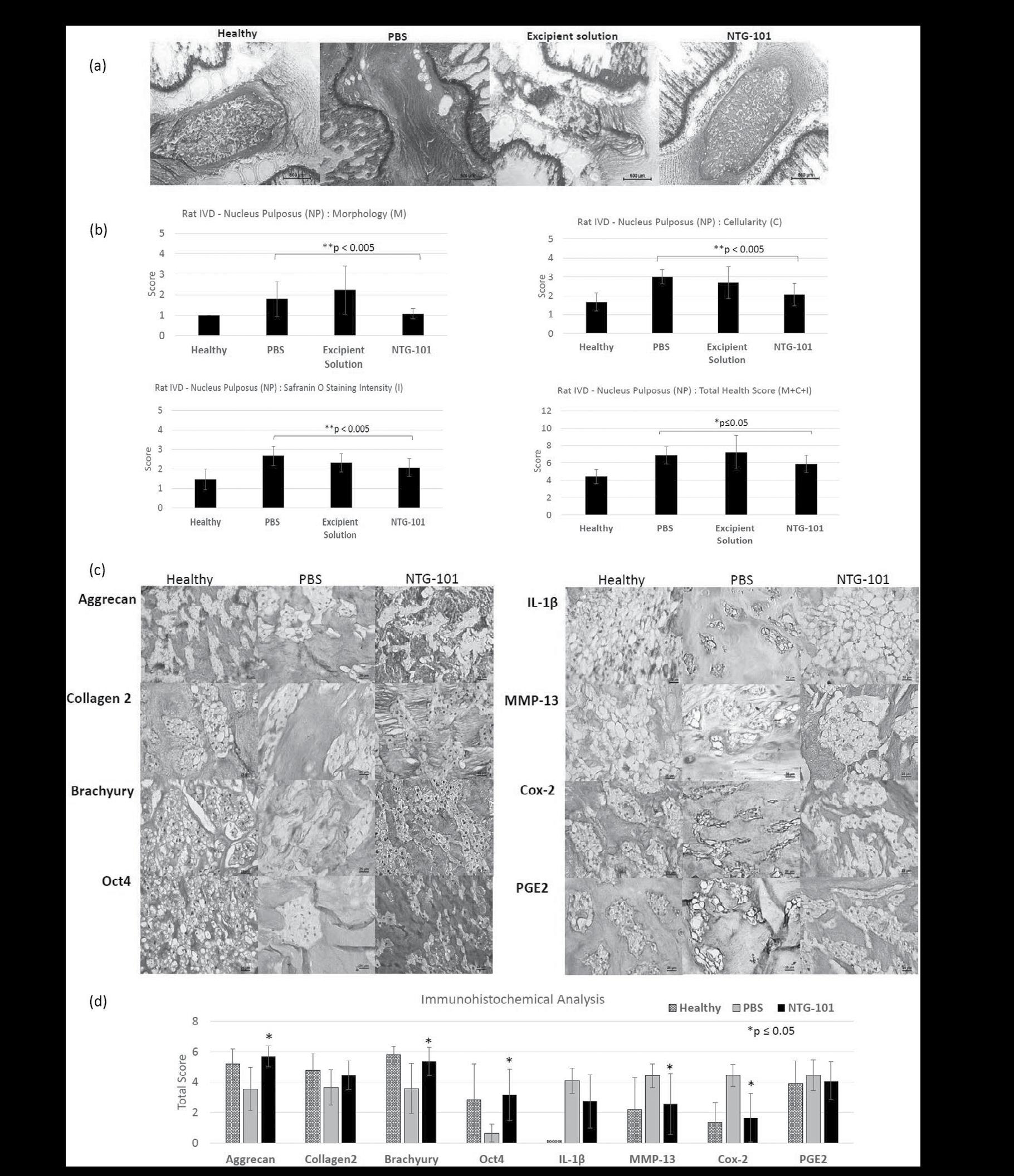
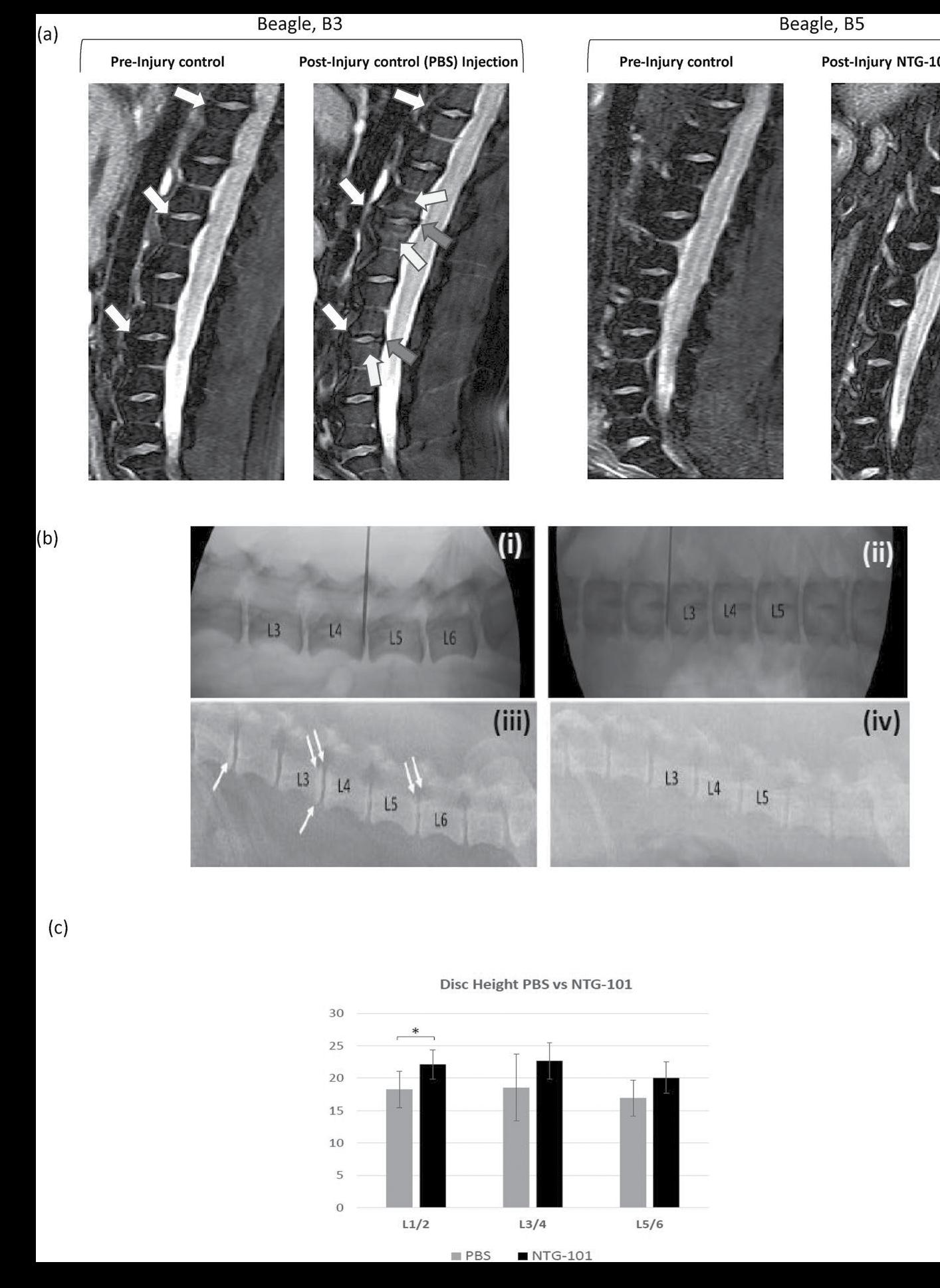
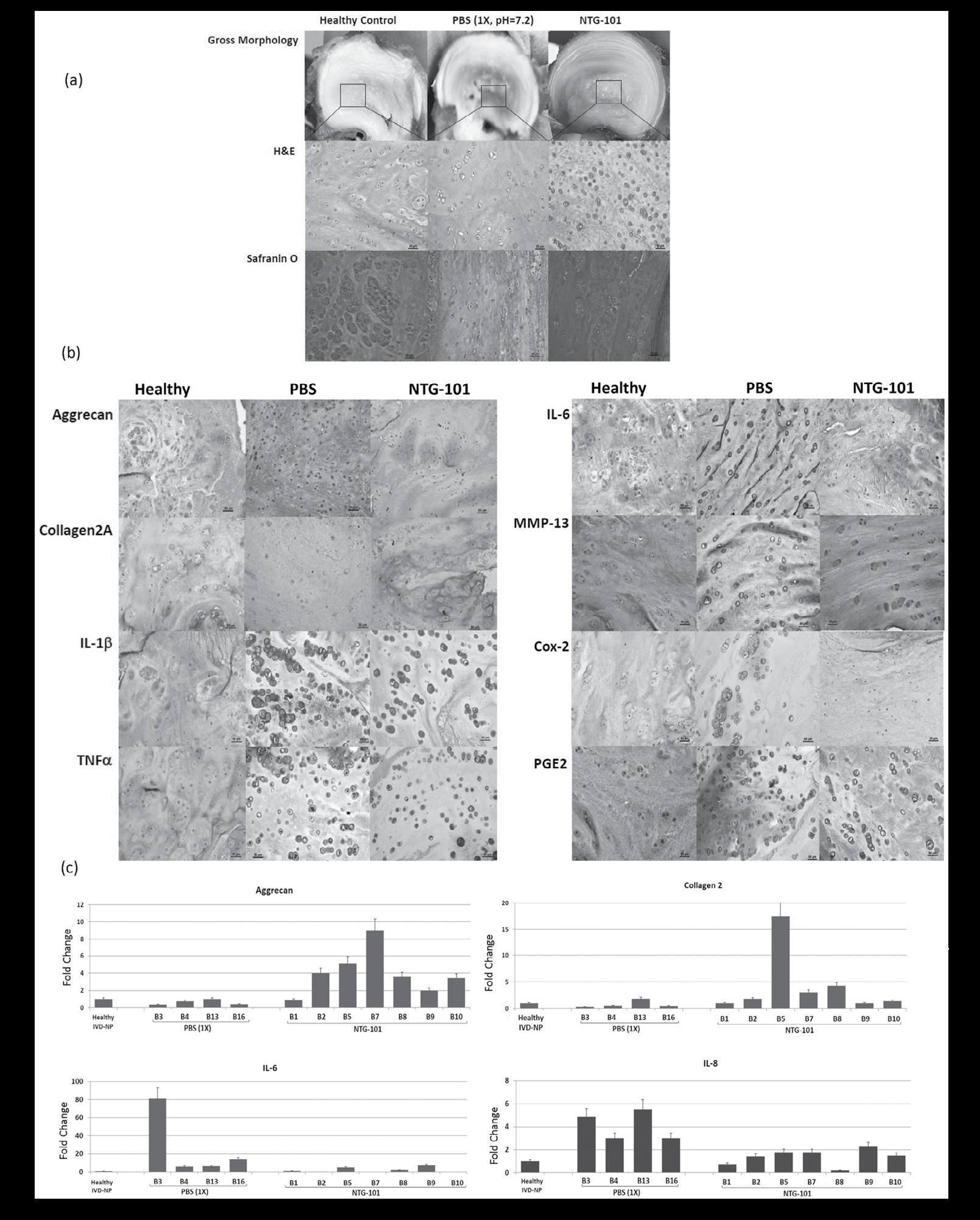
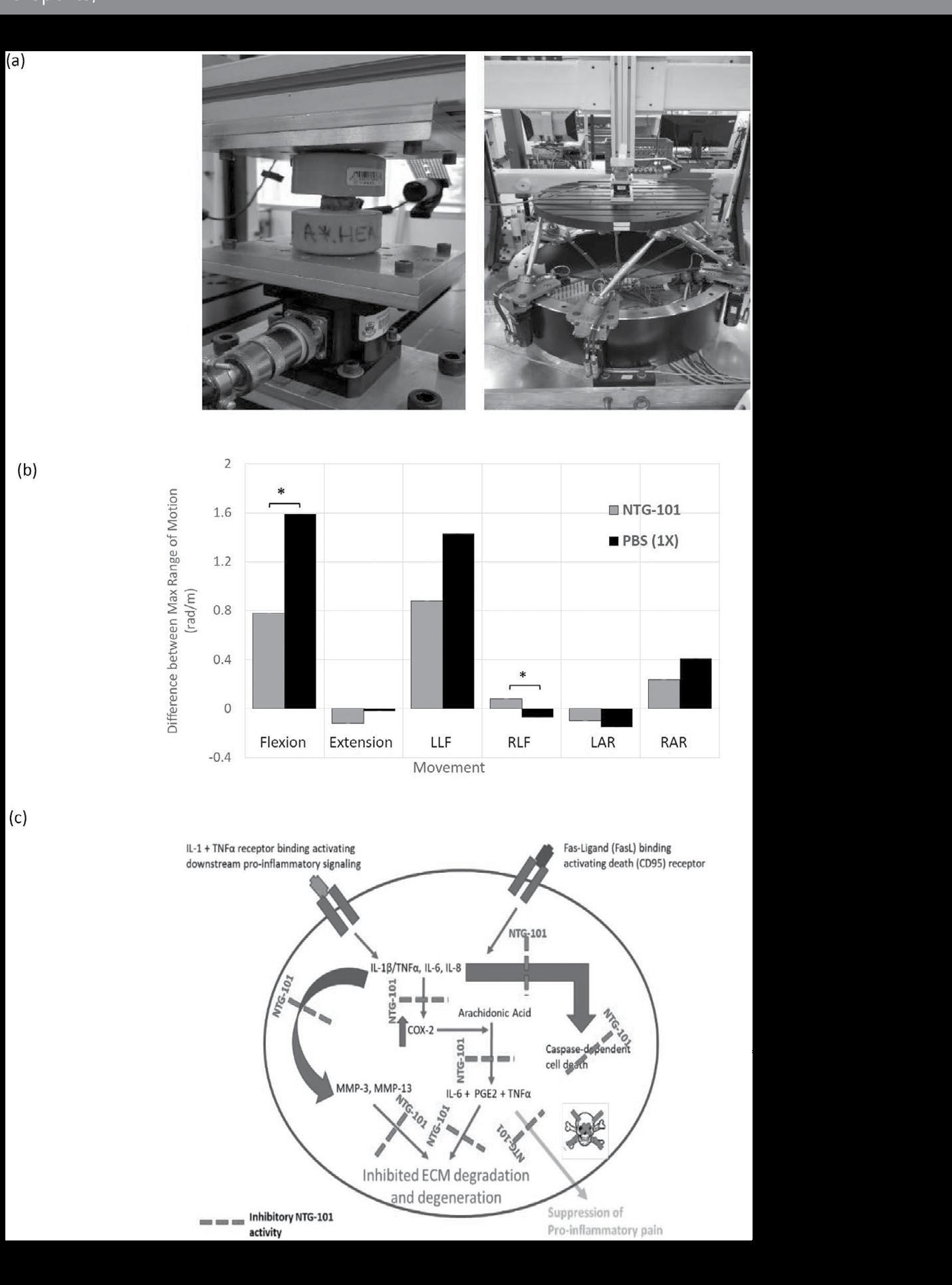
The tremendous cost, pain and disability associated with degenerative disc disease (DDD) makes the development of a biological agent that can mitigate the course of DDD, a critical unmet need. We have identified and reported that a single injection of a combination of recombinant human (rh) Transforming growth factor beta 1 (TGF-β1) and Connective tissue growth factor (CTGF) proteins into the injured intervertebral disc (IVD) nucleus pulposus (NP) can mediate DDD in a pre-clinical rodent model. In this study, we developed and evaluated the efficacy of a novel molecular therapy (NTG101) containing rhTGF-β1 and rhCTGF proteins suspended in an excipient solution using in vivo models of DDD including rat-tail and chondrodystrophic (CD) canines. Needle puncture injury in CD-canine NPs resulted in loss of hydration, disc height and showed radiographic evidence of DDD like humans. However, NTG- 101-injected IVDs maintained disc height and demonstrated retention of viscoelastic properties as compared to IVDs injected with phosphate buffer saline (PBS, 1X, pH = 7.2). In addition, a single intra-discal injection of NTG-101 into the injured IVD-NPs resulted in sustained expression of healthy extra-cellular matrix (ECM) proteins (aggrecan, collagen 2A1) and reduced expression of inflammation associated proteins and molecules (IL-1β, IL-6, IL-8, MMP-13, Cox-2 and PGE2) as compared to vehicle controls. In conclusion, we demonstrated that a single intra-discal injection of the novel formulation, NTG101 confers a robust anti-inflammatory, anti-catabolic and proanabolic effects in pre-clinical models of DDD thereby restoring homeostasis. These findings suggest the therapeutic potential of NTG-101 for clinical use.
Degenerative disc disease (DDD) results in significant disability, tremendous expense and the highest number of disabilityadjusted life years globally1–3. Costs to the healthcare system associated with DDD-related disability have remained fairly consistent for a number of years (1991–2007) with estimates that range between USD 50–100 billion/annum3–5. In fact, a direct correlation with the severity of DDD on MRI and back pain has been reported in a large population based study of 1043 individuals6. Numerous attempts to treat DDD with biological therapy have not yet achieved the desired result7–10. Given the tremendous costs, pain and disability associated with DDD and the current lack of any disease modifying treatment, a biological therapy that could mediate the progression of DDD or even confer a regenerative effect would revolutionize the approach to
DDD. With respect to the development of an effective molecular therapeutic, chondrodystrophic (CD) canines that have a propensity to develop DDD, and the non-chondrodystrophic (NCD) canines that are protected from developing DDD, offer a unique platform for investigation. We and others have extensively reported on the anti-degenerative effects of Notochordal Cell Conditioned Medium (NCCM) obtained from the notochordal cell-rich intervertebral disc nucleus pulposus (IVD-NP) of the NCD-canine11–20. Recently, we injected NCCM into the needle puncture injury induced degenerative rat tail IVD-NP and demonstrated that soluble factors present in NCCM can mitigate the progression of DDD18. Amongst the thousands of soluble proteins contained within NCCM, we identified and showed that a single injection containing rhTGF-β1 and rhCTGF recapitulated the anti-degenerative and pro-anabolic effects of a single injection of NCCM in rat-tail needle puncture model of DDD18
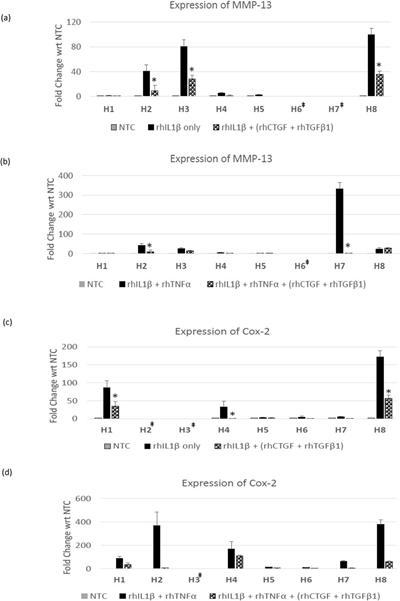
In the current study, we evaluated the efficacy of a novel, molecular therapeutic ‘NTG-101’ containing a combination of rhTGF-β1 and rhCTGF proteins suspended in an excipient solution in in vivo models of DDD including rat-tail NP and CD-canine NPs. Our results demonstrated a single intra-discal injection of NTG-101 confers anti-degenerative effects leading to reduction in expression of pro-inflammatory cytokines including interleukin-1 beta (IL-1β), interleukin–6 (IL-6), interleukin–8 (IL-8), ECM degrading enzymes (MMP-13), cyclooxygenase-2 (Cox-2) while inducing pro-anabolic effects upon the IVDNP restoring expression of healthy ECM proteins (aggrecan, collagen 2A1). In addition, we also observed the maintenance of disc height and biomechanical characteristics in IVDs injected with NTG-101 as compared to vehicle controls in CD-canines. These findings suggested the therapeutic potential of NTG-101 for clinical use in future.
Materials and Methods
Animals and Ethics Statement
All animals (rats/CD-canines) were obtained in collaboration with a licensed animal facility and all experiments were conducted in Canadian Council on Animal Care (CCAC) accredited facilities (University Health Network, Toronto). All experimental protocols were carried out in accordance with CCAC policies and guidelines and approved by the Institutional Animal Care Committee of University Health Network (UHN), Toronto, Ontario, Canada.
CMCC Research Report 2018–2020 20
3
1NotogenInc, 2UniversityofAlberta, 3UniversityHealthNetwork, 4Private Practice, 5UniversityofToronto, 6CanadianMemorialChiropracticCollege
Cell Viability, Cell Proliferation Assay and Gene Expression Analysis.
Human degenerative disc nucleus pulposus tissues were obtained from patients (n = 8) undergoing discectomy or fusion surgery at Toronto Western Hospital, University Health Network (UHN), Toronto with all cases obtained in accordance with the guidelines approved by the Research Ethics Board, Toronto Western Hospital, UHN, Toronto. Nucleus pulposus (NP) tissue was enzymatically digested and cells were cultured within a hypoxic incubator (NuAire, MN, USA) as described earlier17,18. Thereafter the cells were either cultured in serum free ADMEM (no treatment controls) or treated with rhIL-1β (10 ng/ml), tumor necrosis factor alpha (rhTNFβ, 50 ng/ml), or a combination of rhCTGF (100 ng/ml) + rhTGF-β1 (10 ng/ml) proteins for 24–72 hrs under hypoxic conditions to determine the effect of the treatment on cell viability, proliferation and ECM synthesis17,18. For details, see Supplementary data.
Intra-Discal Injection of NTG-101 in Pre-Clinical Rodent Model of DDD
We used our established rat-tail needle puncture injury model of DDD using 12-week old female Wistar rats (n = 27, Charles River Laboratories Inc.) as described earlier18. IVD needle puncture injury was performed in 5-caudal discs per animal using fluoroscopic image guidance as described earlier18. Four weeks post injury, animals were randomized into 3 groups (including 9 animals per group), and the injured discs were injected with 8.0 µl of vehicle (i.e. phosphate buffer saline, PBS, 1X, pH = 7.2) or excipient solution (ES) or NTG-101 using a 32 G needle under fluoroscopic guidance. At the end of the experiment (10 weeks post-injury), the animals were humanely euthanized. At least one caudal IVD per animal was fixed in formalin as a representative for histological analysis. Agematched (22-week-old) healthy IVDs were obtained from rat tail IVDs that served as uninjured, healthy controls.
Intra-Discal Injection of NTG-101 or Vehicle (PBS, 1X) in PreClinical CD-Canine Model of DDD
All animals (n = 16) were obtained from a licensed animal testing facility (Kingfisher International Inc., Stouffville, Ontario, Canada). Briefly, the disruptive needle puncture injury was performed in 3-non-contiguous lumbar IVD-NPs at levels (L1/2, L3/4 and L5/6) by a clinical Veterinarian in 3-year old chondrodystrophic (CD) canines (age matched) using fluoroscopic guidance. Four weeks post-injury animals were randomized and were administered with a single intra-discal injection of 350.0 µl of either vehicle (Group 1, n = 6) or NTG101 (Group 2, n = 10) under fluoroscopic guidance in injured IVDs. The remaining discs i.e. adjacent healthy IVDs (L2/3, L4/5 and L6/7) served as no treatment controls (NTCs) in both the groups. At the end of experiment (i.e.14 weeks post injection) the animals were humanely euthanized, and each lumbar vertebral motion segment was dissected aseptically.
Magnetic Resonance Imaging (MRI)
MR Imaging (MRI) was performed using a 3 Tesla Verio MRI system (IMRIS, Minnetonka, MN), with dogs (n = 5) in prone position and feet - first orientation. A 24-element spine matrix radiofrequency (RF) coil was posterior to the animal, and a 4-element small flexible RF coil was positioned anterior to the lumbar region. The RF coils were purchased via IMRIS Inc., Winnipeg, Manitoba, Canada. The lumbar discs were first visualized using a stack of at least 3 sagittal-oriented 2D fatsuppressed T2-weighted images (echo time 83 ms, repetition time 4000 ms, 320 × 240 matrix over a 15 × 15 cm field-ofview providing 0.6 × 0.5 mm in-plane resolution, 3 mm slice thickness, 230 Hz/pixel readout bandwidth, 2 averages, 4 min 10 sec acquisition time).
Disc Height Analysis in Chondrodystrophic (CD) Canines. Disc height analysis in CD canines (n = 16) was performed using fluoroscopic images obtained using Sedecal Dragon SPSLW digital X-ray system at baseline and the endpoint (i.e. 14 weeks post-intradiscal injection). Acquired radiographs were saved as DICOM images and using MicroDicom software (microdicom. com) and disc height was calculated from the superior to the inferior vertebral endplate. For details, see Supplementary Data.
Histology, Immunohistochemistry (IHC) and Gene Expression Analysis.
Hematoxylin and eosin (H&E) and Safranin-O staining was performed on paraffin-embedded sections (5 µm) to assess general morphology and proteoglycan content18. Histological grading of IVD-NP (injury followed by treatment) was carried out based on IVD – NP morphology, cellularity and Safranin O staining intensity in paraffin embedded sections following criterion described for rat21,22 and canine IVDs23 (Supplementary Tables 1–3). The histological scoring was done by 3 observers (ME, AM and HG), and scores were recorded independently. In the case of inter-observer variability of scores, all 3 observers reviewed scores and arrived at a final consensus score. Immunohistochemistry for ECM proteins (Aggrecan, Collagen 2A1), notochordal cell marker (Brachyury), stem cell marker (Oct4), pro-inflammatory cytokine (IL-1β and IL-6), ECM degrading enzyme (Matrix metalloproteinases-13, MMP13) and inflammation association and pain related enzymes (Cyclooxygenase-2, Cox-2 and Prostaglandin E2, PGE2) was performed using the Vectastain Rabbit kit with Diaminobenzidine (DAB) as the chromogen18. Immunohistochemistry sections were analyzed semi-quantitatively using total of scores obtained based on % positivity and staining intensity for respective proteins24 (Supplementary Table 4). We performed quantitative Real Time - Polymerase Chain Reaction (qRT - PCR) to determine the effect of treatment on healthy ECM genes (Aggrecan, Collagen 2A1, hyaluronan and proteoglycan link protein 1, HAPLN1), inflammation and pain associated cytokines (IL-6 and IL-8) using species and gene specific primers with SYBR Green reagent. For details, see Supplementary Data.
A selection of published research by CMCC faculty 21 Matta et al
Biomechanical Analysis
We evaluated PBS (n = 4) or NTG-101 (n = 6) injected canine IVDs (L5/6) and adjacent lumbar spine segments, L6/7 serving as healthy no-treatment controls (n = 10). Custom software (LabVIEW, National Instruments) was used to test the specimens using an unconstrained force-control system. Force and moment targets were achieved by adjusting the velocity on each axis in proportion to force or moment errors while limiting the maximum velocity of the system. Flexion, extension, lateral bending and axial rotation were performed with three cycles each. Testing velocity was 0.1 degree per second with a maximal moment of 2.0 Nm. The resulting angle vs. moment data were then determined25. For details, see Supplementary Data. Statistical Analysis. Histograms representing mean ± standard deviation (S.D.) were plotted for all outcomes reported in this study. Statistical analysis was performed using Student’s t-test (paired/unpaired), Analysis of variance (ANOVA), Wilcoxon Signed Rank test and Mann-Whitney U test using SPSS 16.0 software (Chicago, IL, USA). P-value ≤ 0.05 was defined as statistically significant for all tests.
Results
Evaluation of the Anabolic Effects of the Combination of rhCTGF (100 ng/ml) and rhTGF-β1 (10 ng/ml) Proteins on Human NP Cells
Treatment with a combination of rhCTGF (100 ng/ml) and rhTGF-β1 (10 ng/ml) significantly increased the viability of human NP cells derived from all the donors within 48 hrs – 72 hrs as compared to their respective no treatment controls for specific time points (Fig. 1a, Supplementary Figure 1a). The increase in cell viability of human NP cells was further supported by increased cell proliferation in these cells on treatment with a combination of rhCTGF and rhTGF-β1 over 72 hrs as shown by increased bromodeoxyuridine (BrdU) incorporation (Fig. 1b, Supplementary Figure 1b). In addition, treatment with this combination induced a significant increase in expression of healthy ECM proteins including aggrecan, Col2A1 and HAPLN1 in human degenerative disc NP cells within 24 hrs (Fig. 1c–e, Supplementary Figure 1c). We observed a significant increase in aggrecan mRNA levels in human NP cells in at least 50% of the donors (H1, H4, H5 and H8, Fig. 1c), while increased Col2A1 expression was observed in all the donors (Fig. 1d). Treatment with combination of rhCTGF (100 ng/ml) and rhTGF-β1 (10 ng/ml) proteins increased HAPLN1 mRNA levels in human degenerative disc NP cells derived from 4 of the 8 (H2, H5, H6 and H7) donor patients (Fig. 1e).
Evaluation of Anti-Catabolic Effects of Combination Treatment
[rhCTGF (100 ng/ml) + rhTGF-β1 (10 ng/ml)] on Human NP Cells.
Human NP cells derived from patients (n = 8, H1- H8) undergoing spinal surgery were treated with pro-inflammatory cytokines, rhIL-1β (10 ng/ml) alone or in combination with rhTNFβ (50 ng/ml) for 24 hrs. Treatment with rhIL-1β alone or a combination of rhIL-1β + rhTNFa induced expression of MMP-
13 and Cox-2 in human NP cells (Fig. 2a–d). Notably, addition of a combination of rhCTGF (100 ng/ml) and rhTGF-β1 (10 ng/ml) proteins in the culture medium, reduced expression of MMP13 and Cox-2 mRNA in degenerative disc NP cells treated with rhIL-1β alone or in combination with rhTNFa within 24 hrs (Fig. 2a–d).
Histological Evaluation of Rat-Tail IVD - NP Tissue Sections (Healthy/PBS/Excipient Solution (ES)/NTG-101).
We evaluated the scores for morphology (M), cellularity (C) and Safranin-O staining intensity (I) in tissue sections (n = 15, done in duplicates per group) obtained from rodent injured IVD – NPs that received an intra-discal injection of PBS, excipient solution or NTG-101 and untreated, non-injured age-matched healthy control IVD-NPs. The IVD-NPs that received an intra-discal injection of vehicle or excipient solution, showed distinguished features of disc degeneration with small, low cellularity or acellular IVD-NP with metaplasia of annulus fibrosus showing intense Safranin O staining. We observed the significant loss of cellularity and a strong Safranin O staining in PBS injected IVDs in comparison to healthy controls demonstrating the development of a degenerative phenotype (Fig. 3a and b). However, rat injured IVDs injected with NTG-101 showed no significant difference in scores for morphology, cellularity, Safranin-O staining intensity and total score for histology as compared to healthy controls (Fig. 3a and b).
Immunohistochemical Analysis of Rat IVD - NP Tissue Sections (Healthy/PBS/NTG-101).
Immunohistochemical analysis was performed on serial tissue sections used for Safranin O staining to determine the expression of important proteins in rat-tail IVDs that received an intra-discal injection of NTG-101, PBS and healthy age-matched (22-week-old) rat IVD-NP tissues. We observed moderate/ intense aggrecan and Col2A1 immunostaining in ECM and nuclear Brachyury, Oct4 expression in notochordal cell rich IVD-NPs injected with NTG-101, similar to healthy controls IVDs. However, injured IVDs injected with vehicle showed loss or reduced levels of these proteins (Fig. 3c and d). In fact, we observed a significant increase in inflammation and associated proteins including IL-1β, MMP-13 and Cox-2 levels in rat-tail IVDs injected with PBS (1X, pH = 7.2) following needle puncture injury (Fig. 3c and d). However, NTG-101 injected IVD - NPs demonstrated no or low levels of IL-1β, MMP-13 and Cox-2 suggesting that NTG-101 suppresses inflammation within IVD - NPs following injury (Fig. 3c and d). No significant alterations in PGE2 levels were observed 10 weeks post-injection of either PBS or NTG-101 in rat tail IVD-NP tissue sections (Fig. 3c and d).
CMCC Research Report 2018–2020 22
Fig1Pro-anaboliceffectsofcombinationtreatmentonhumanNPcells.(a)Panel showshistogramsrepresentingaveragecellviability(%)ofhumanNPcells(H1H8)treatedwiththecombinationofrhCTGFandrhTGF-β1proteinsfor48hrs and72hrsincomparisontoNotreatmentcontrols(NTC,shownbysinglebaras arepresentativefor%cellviability48hrsand72hrs)asdeterminedusingcell viabilityassays(*p ≤ 0.05,**p<0.005).(b)Panelshowshistogramsrepresenting averagecellproliferation(%)ofhumanNPcells(H1-H8)treatedwiththe combinationofrhCTGFandrhTGF-β1proteinsfor72hrsascomparedtoNo treatmentcontrols(NTC)determinedusingBrdUenzymelinkedimmunosorbent assay(ELISA)assay(*p ≤ 0.05).TotalRNAwasextractedhumanNPcells(H1-H8) treatedwithcombinationtreatmentorleftuntreatedingrowthmediumfor24 hrstodeterminetheeffectoftreatmentonexpressionofhealthyECMgenes.

qRT-PCRanalysisshowingmRNAexpressionlevelsof(c)aggrecan,(d)Col2A1and (e)HAPLN1inhumanNPcells(H1-H8)treatedwiththecombinationofrhCTGF andrhTGF-β1proteinsfor24hrsincomparisontotheirrespectiveNotreatment controls(NTC,*p ≤ 0.05).
MRI Assessment of CD-Canine IVDs
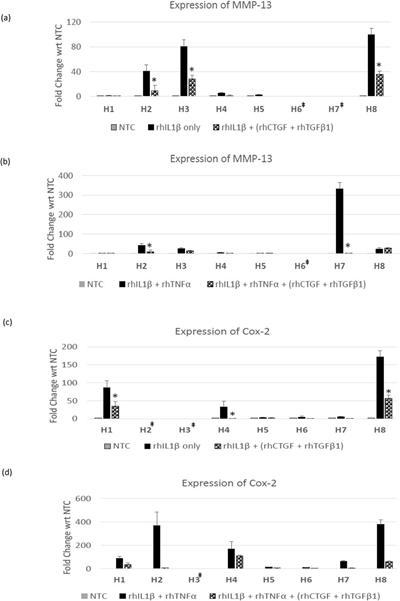
Among the CD-canines (n = 2) injected with PBS (1X, pH = 7.2), animal (B3) developed robust degenerative changes at the L3/4 and L5/6-disc spaces. These degenerative changes included extensive type 1 modic changes affecting L3/4 and to a lesser extent L5/6 with a loss in disc height and the development of marginal osteophytes at the posterior superior and inferior
aspect of the vertebral body (Fig. 4a). It is noteworthy that the lumbar spine of this canine (B3) was normal at baseline and these phenotypic changes representing DDD occurred after disruptive needle puncture injur y only (Fig. 4a). Among the CD-canines (n = 3) that received an intra-discal injection of NTG-101, post-injury, no evidence of DDD was observed 14 weeks post injection and all IVDs appeared identical to baseline (Fig. 4a, Supplementary Figure 2). No change was observed in adjacent, uninjured IVDs irrespective of the intervention given to animals (Fig. 4a, Supplementary Figure 2).
Fig2Anti-inflammatoryeffectsofcombinationtreatmentonhumanNPcells. Panelshowshistogramsrepresentingexpressionof(a,b)MMP-13or(c,d)Cox-2 mRNAlevelsinhumandegenerativeIVD-NPcells(H1–H8)treatedwith(a andc)rhIL-1βalone;(bandd)rhIL-1β + rhTNFa onlyorinthepresenceofa combinationofrhCTGF(100ng/ml)+rhTGFβ1(10ng/ml)asrevealedbyqRTPCRanalysis.p-valuesforcombinationofrhIL-1β/rhIL-1β+rhTNFa+rhCTGF+ rhTGF-β1arewithrespecttorhIL-1βaloneorrhIL-1β+rhTNFaalonerespectively (*p ≤ 0.05).‡ThesesamplesdidnotshowexpressionofMMP-13orCox-2on treatment with rhIL-1βalone or combination of rhIL-1β + rhTNFa.
Disc Height of CD-Canine IVDs.
At baseline, no statistically significant difference was observed in the disc heights for all animals (n = 16, Supplementary Figure
A selection of published research by CMCC faculty 23
Matta et al
3). However, IVDs injected with PBS (1X, pH = 7.2) post injury, demonstrated clear radiographic evidence of DDD with the development of marginal osteophytes at the vertebral endplate/ vertebral interface (in a representative image of specimen B3) at the L3/4 and L5/6-disc spaces (Fig. 4b). There was clear evidence at the L1/2 spinal level that discs injected with PBS (1X, pH = 7.2) showed a significant reduction in disc height as compared to NTG-101 injected IVDs (p ≤ 0.05, Fig. 4c).
Morphological and Histological Evaluation of CD-Canine IVD –NPs.
We evaluated the gross morphology and histology (cellularity and proteoglycan content) of canine IVDs injected with either NTG-101 or PBS (1X, pH = 7.2) following needle puncture injury at spinal level L3/4 and compared it to adjacent uninjured, healthy IVD – NPs (spinal level, L4/5). Gross morphology of the IVD – NPs revealed reduced size and fibro-cartilaginous appearance of the NP in 4 of the 6 beagle IVDs that received an intra-discal injection of PBS (1X, pH = 7.2) as compared to adjacent, uninjured IVDs (Fig. 5a). Among the CD-canine IVDs that received an intra-discal injection of NTG-101, gross morphology was like adjacent uninjured, control IVDs (Fig. 5a). Histological evaluation demonstrated moderate cellularity with clusters of chondrocyte like-cells (CLCs) in uninjured, control or NTG-101 injected IVD – NPs as revealed by H&E and Safranin O staining (Fig. 5a, Supplementary Figure 4). In contrast, the IVD - NPs injected with PBS (1X, pH = 7.2) displayed a lack of chondrocyte like cells (CLC) - clusters in H&E and decrease in Safranin O staining (Fig. 5a, Supplementary Figure 4).
Immunohistochemical Analysis of Canine IVD – NPs. Our IHC analysis revealed low or no detectable levels of ECM proteins including aggrecan and Col2A1 in CD-canine injured IVDs injected with PBS (1X, pH = 7.2). On the other hand, NTG-101 injected IVDs demonstrated moderate or intense aggrecan and Col2A1 immunostaining within the ECM surrounding NP cells, similar to that observed in uninjured, control IVDs demonstrating the pro-anabolic effects of NTG101 (Fig. 5b). However, PBS (1 × , pH = 7.2) injected IVD - NP tissues demonstrated a moderate to strong immunostaining for pro-inflammatory cytokines (IL-1β, TNFa and IL-6) and inflammation induced MMP-13, Cox-2 and PGE2 levels (Fig. 5b). Whereas NTG-101 injected IVD - NPs revealed cellular clusters that were devoid of IL-1β, TNFa, IL-6, MMP-13, Cox-2 and PGE2 immunostaining like control IVD-NP tissues (Fig. 5b) clearly supporting the anti-inflammatory role of NTG-101 (Fig. 5b).
Gene Expression Analysis of CD-Canine IVD – NPs.
Fourteen weeks post - treatment, total RNA was extracted from CD-canine IVDs that received an intra-discal injection of PBS (1X, pH = 7.2) or NTG-101 at spinal levels (L1/2) and from adjacent, uninjured control IVDs at spinal level (L2/3). Gene expression of aggrecan, Col2A1, IL-6 and IL-8 was determined in injured IVD – NP tissues injected with NTG-101, PBS (1X, pH = 7.2) and control IVDs using qPCR with canine gene specific
primers. Quantitative real time PCR results revealed an increase in aggrecan and Col2A1 gene expression in NTG-101 injected IVD-NPs in comparison to PBS – injected IVD-NP tissues and significant reduction in gene expression levels of both the proinflammatory cytokines, IL-6 and IL-8 as compared to PBSinjected IVD – NPs (Fig. 5c, Supplementary Figure 4).
Biomechanical Analysis of Canine – IVDs.
We performed repeated measures of the maximum rotational angle (a measure of how much the sample changes over time which is a measure of the viscoelastic properties of the sample) achieved using the NTG-101 or PBS-injected IVDs (L5/6) and compared these changes to the adjacent, uninjured IVD (L6/7) that served as a no treatment control (Fig. 6a). The absolute and normalized values (range, mean ± SD) for flexion, extension, left lateral flexion (LLF), right lateral flexion (RLF), left axial rotation (LAR) and right axial rotation (RAR) for CD-canine IVDs injected with either NTG-101 or PBS (1X) (Tables 1, 2 and Fig. 6b). For normalization, absolute values were normalized with respect to IVD height for each specimen. We observed significant differences in normalized values for flexion and right lateral flexion (RLF) in the PBS-injected IVDs in comparison to the IVDs injected with NTG-101 (p ≤ 0.05, Tables 1, 2 and Fig. 6b).
CMCC Research Report 2018–2020 24
(uninjured,healthyage-matchedcontrol),injuredIVDsinjectedwitheitherPBS(1X,pH=7.2),excipientsolutionorNTG-101(Scalebar:500µm).Panel(b)showsthehistogram analysisshowingmeanscore±S.D.ofthemorphology(M),cellularity(C),SafraninOstainingintensity(I)andtotalhealthscore(M+C+I).***p-valueforNTG-101injected groupofanimalsiswithrespecttothegroupofinjuredIVDsinjectedwithPBSonly.Panel(c)representsimagesofimmunohistochemistryforAggrecan,Col2A1,Brachyury, Oct4,IL-1β,MMP-13,Cox-2andPGE2inage-matched,uninjured,healthyrattailIVDsaswellasinjuredIVDsinjectedwithPBS(1X)orNTG-101(Scalebar:25µm).Panel (d)representhistogramsshowingaveragevaluesofIHCtotalscoreobtainedforaggrecan,Col2A1,Brachyury,Oct4,IL1-β,MMP-13,Cox-2andPGE2.Eachhistogramshows mean±SD,*p≤ 0.05.
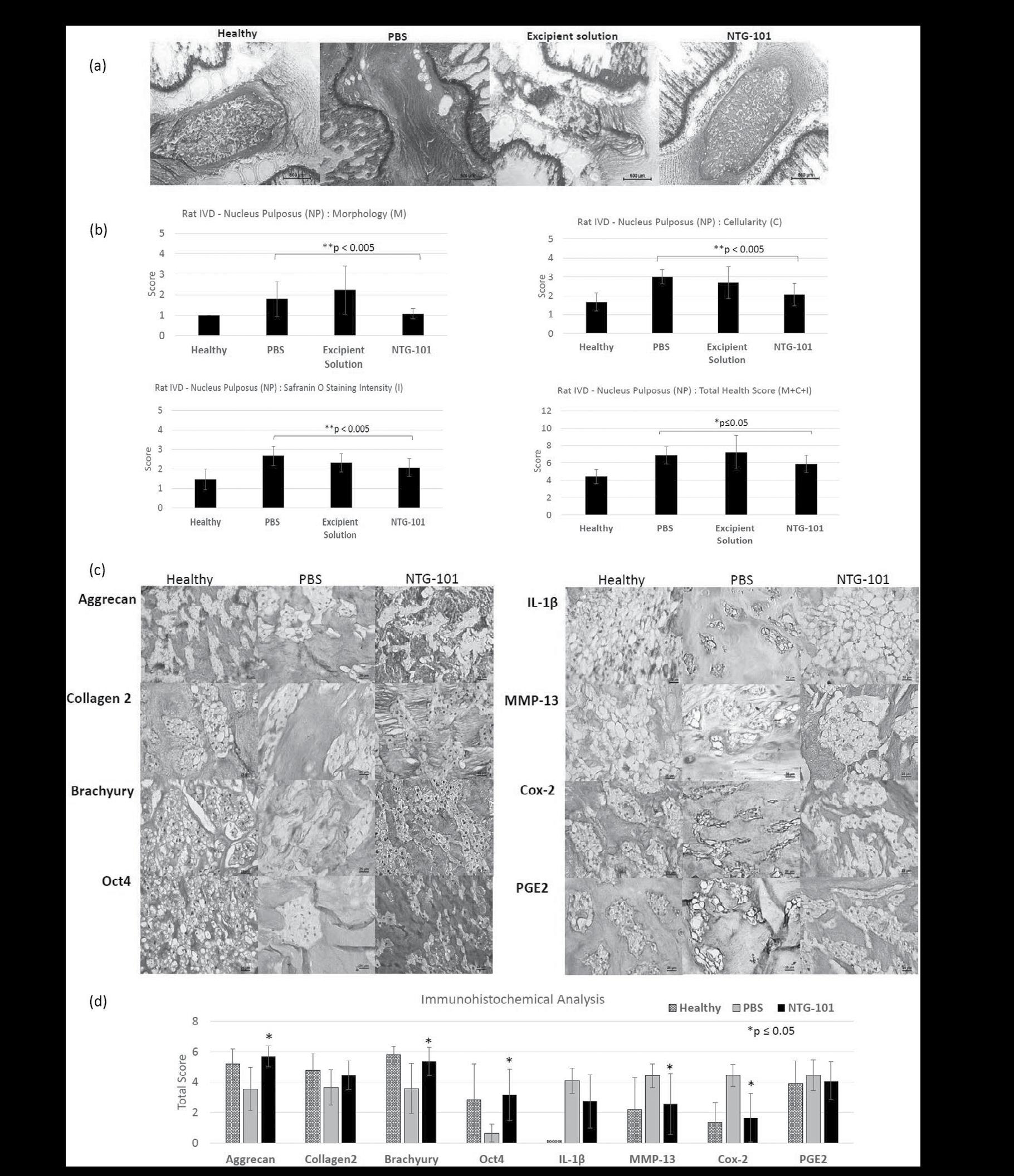
A selection of published research by CMCC faculty 25 Matta et al
Fig3Effectofintra-discalinjectionofNTG-101inrodentneedlepuncturediscinjurymodel.(a)RepresentativeimagesshowingSafranin-OstainedrodentIVDtissuesections
Fig4(a)Representativeimageshowing3TMRIofCD-canine(B3andB5)lumbarspinewithwell-hydrateddiscspriortoinjury(baselineMRI).Inthisimage,whitearrows showthetargetedIVDsforneedlepunctureinjury.Nextimageshows3TMRIofCD-canine(B3)lumbarspine18weekspost-injury(i.e.14weekspost-treatment).Theyellow arrowsdepictrobust“modic”changeswithinbonemarrowabuttingthevertebralendplatethatwerecompletelyabsentpriortoinjury.Osteophyteswereobservedatspinal levels(L3/4andL5/6)18weekspost-injuryindicatingthedevelopmentofDDDinvehiclecontrols(redarrows).WhileCD-canine(B5)thatreceivedanintra-discalinjectionof NTG-101representedMRIscansshowingnosignificantdifferencefrombaselineimagesi.e.priortoinjury.(b)Representativeradiographicimagesofbeagle,B3(PBSinjected) andbeagle,B5(NTG-101injected)atbaseline(iandii)and14weekspostinjections(iiiandiv).Atbaseline,thereisnodemonstrableDDDbetweenanimalsthatreceivedPBS orNTG-101(iandiii).However,attheendpointthereisevidenceofDDDatL1/2,L3/4andL5/6intheB3beagle(lossofdischeight,endplatesclerosis)(iii)whereasin(iv)the B5beagleshowsnodetectableDDD.Whitearrowsdepictsub-chondralsclerosisanddoublewhitearrowsdepictthedevelopmentofmarginalosteophytesatthevertebral endplates.(Note,needlevisibleinaandcwasforplacementpurposesonlyanddoesnotrepresentinjectionorneedleinjury).(c)Panelrepresentshistogramsshowing changeinmeanvaluesofthedischeightatrespectivespinallevels(L1/2,L3/4andL5/6)injectedwithNTG-101orPBS(1X,pH=7.2)wheretheL1/2levelshowsasignificant preservationofdischeightindiscsinjectedwithNTG-101(*p ≤ 0.05).
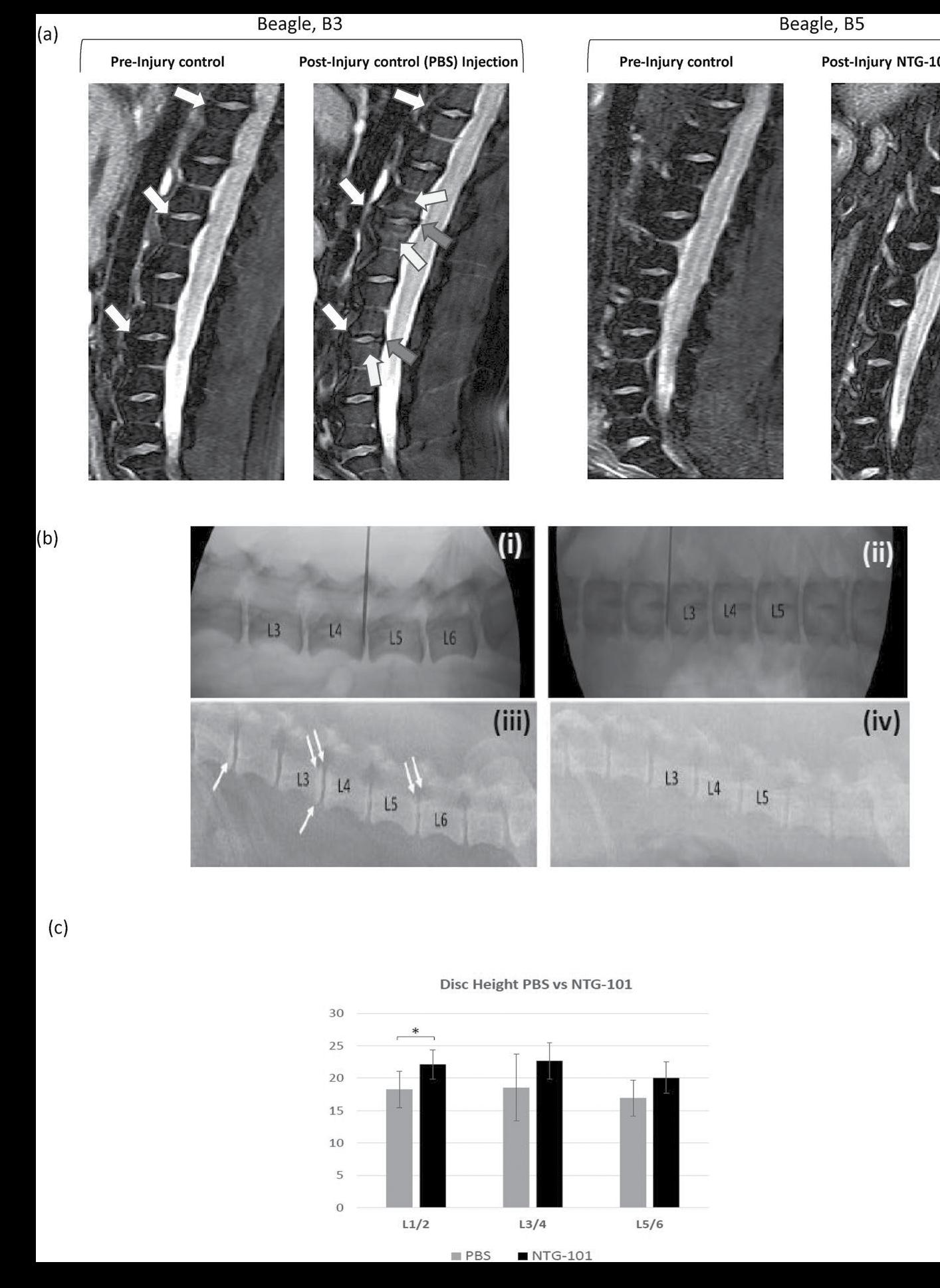
CMCC Research Report 2018–2020 26
Fig5(a)RepresentativeimagesshowinggrossmorphologyoftheCD-canineIVDsatspinallevel(L3/4)thatreceivedanintra-discalinjectionofPBSorNTG-101andadjacent IVDatspinallevel(L4/5)representinguninjuredIVD.HematoxylinandEosin(H&E)stainedsectionsrevealedcellularitywhileSafraninOstainingrepresentedproteoglycan content.Healthy(notreatment)controlsrevealnormalIVD-NPmorphologywithgoodcellularityandintactECM.IVDsinjectedwithPBS(1X,pH=7.2)displayedmarkedly disturbedcellularityandECMwhereasNTG-101injectedIVDswerecomparabletoadjacent,uninjuredIVD-NPs(Scalebar:50µmforH&E,SafraninOstainedsections).(b) Immunohistochemicalanalysisofaggrecan,collagentype2A1,IL-1β,TNFβ,IL-6,MMP-13,Cox-2andPGE2levelsinuninjuredcontrols,PBSandNTG-101injectedIVD–NPs (Scalebar:50µm).(c)PanelsshowshistogramsrepresentingrelativefoldchangeinmRNAlevelsofhealthyECMgenes(aggrecan,Col2A1)andinflammation,painassociated genes(IL-6andIL-8)expressioninCD-canineIVD-NPtissuesthatreceivedasingleintra-discalinjectionofNTG-101orPBS(1X,pH=7.2)withrespecttoadjacenthealthy, uninjuredIVD-NPsobtainedfromthesameanimal.AllgeneexpressionfoldchangesfortheinjectedIVD-NPswerenormalizedtoexpressionlevelsintheindividualadjacent, healthycaninediscusingHPRTusedashousekeepinggene.InFig.5,datafromadjacent,healthycanineIVD-NPsisshownasarepresentativesinglebar.
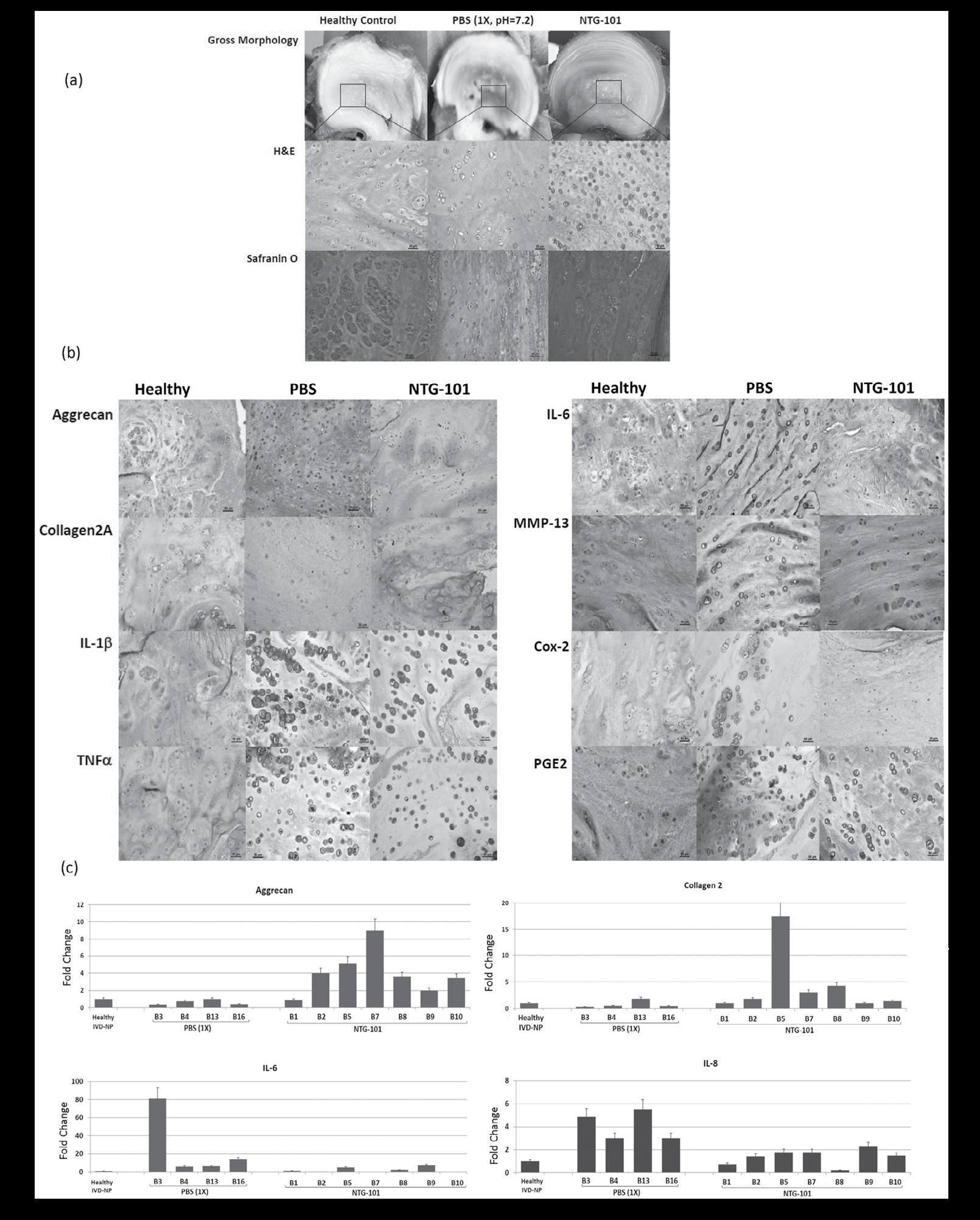
A selection of published research by CMCC faculty 27 Matta et al
Discussion
Both CTGF and TGF-β1 are vital elements during embryological development of the IVD and cartilage, as well as the postnatal stage26,27. Further, CTGF and TGF-β1 are vital to the homeostatic regulation of the IVD-NP18. Ageing, inflammation and other degenerative conditions along with lack of CTGF and TGF-β1 lead to dysregulated signaling pathways leading to progression of DDD18,28. However, the notochordal cell rich IVD-NP in NCD-canines that secrete CTGF and TGF-β1 resist the development and progression of DDD18. We have previously demonstrated that a single injection of NCCM into the injured/degenerative rat-tail IVD-NPs conferred a robust anti-degenerative and pro-anabolic effect that was recapitulated by a single injection of a combination of rhCTGF + rhTGF-β1 proteins18. In the current study, we evaluated the effect of this combination treatment on cell viability, proliferation, gene expression of healthy ECM proteins (aggrecan, col2A1, HAPLN1) and inflammation induced expression of MMP-13 and Cox-2 in human degenerative IVD-NP cells. Our results demonstrated pro-anabolic and anti-inflammatory effects of the combination of rhCTGF and rhTGF-β1 in human NP cells. Treatment with the combination of these growth factors induced cell viability and proliferation as well as exhibited robust ECM protein synthesis while suppressing inflammation. Further, our in vivo results revealed no significant difference in total histological scores for rat-tail injured IVD-NPs that received an intra-discal injection of higher doses of rhCTGF (200 ng/ml) or rhTGF-β1 (20 ng/ ml) in comparison to rhCTGF (100 ng/ml) or rhTGF-β1 (10 ng/ ml) respectively (data not shown). Considering the therapeutic potential of this combination both in in vitro (human and rodent) and in vivo rodent disc injury model, we formulated NTG-101 containing rhCTGF (100 ng/ml) and rhTGF-β1 (10 ng/ml) in an excipient solution and tested its efficacy in two independent in vivo models of DDD following needle puncture injury (i.e. rodent and CD-canines). The CD-canine has been validated as an appropriate model of human disease by our group and others further supporting the use of this large animal model to investigate the progression of DDD and evaluate the biological therapy25,29
Interestingly, we found that a single injection of NTG-101 conferred a robust pro-anabolic and anti-catabolic effects in the CD-canine model indicating that our intervention can restore homeostatic regulation within degenerative IVD-NPs. On the other hand, we found that the injured canine IVDs that were injected with vehicle degenerated in a fashion akin to the human IVDs. These signs of degeneration include modic changes, and loss of disc height as well as other molecular, histological and biomechanical changes consistent with DDD30,31. Among animals that received an intradiscal injection of the vehicle post-injury, we observed loss of disc height, sub-chondral sclerosis and formation of marginal osteophytes as revealed by radiographic analysis. These IVD-NPs also showed low cellularity, decreased expression of aggrecan and Col2A1 while over expressing the pro-inflammatory cytokines (IL-1β, IL-6,
IL-8, TNFα) suggesting the development of an inflammatory microenvironment in the IVD-NP. These observations are also supported by prior studies emphasizing the possible role of proinflammatory cytokines and pain of disc origin32. Interestingly, Burke et al 33, reported that disc tissues obtained from back pain patients undergoing surgery displayed significantly elevated levels of IL-6, IL-8, and PGE2 than did patients with sciatica or as compared to normal. In contrast, the IVDs of the NTG-101 injected animals demonstrated no significant changes on MRI imaging and radiographs as compared to the adjacent, healthy IVDs at the endpoint. In addition, these IVD-NPs maintained a healthy disc phenotype showing cellular IVD-NPs with expression of aggrecan, Col2A1 like adjacent healthy IVDs. We also observed reduced expression of inflammation and associated proteins (IL-1β, IL-6, IL-8, TNFα, Cox-2 and MMP13) clearly suggesting the pro-anabolic and anti-inflammatory role of NTG-101 in degenerative IVD-NPs. These results strongly suggest that a single injection of NTG-101 into the degenerative disc can overcome the injury and pro-inflammatory effects conferred by needle puncture injury and induce repair. However, the degenerative disc derived human NP cells showed a heterogenous response on treatment with the combination of rhCTGF + rhTGF-β1 proteins within 24 hrs – 72 hrs in this study. These human IVD-NP primary cell cultures containing mixed populations of NP and likely AF and endplate - cells were derived from patients undergoing discectomy and pose a major challenge in in vitro studies34. Further, the lack of cellular and molecular markers for NP cells adds to this complexity35 Nevertheless, our study established the proof of principle and large-scale studies including safety and toxicity as well as efficacy of NTG-101 in patient derived NP - cells and clinical trials are underway to determine the clinical utility of NTG-101.
The progression of DDD is marked by the development of a progressively pro-inflammatory milieu within the NP leading to degradation of healthy ECM molecules including aggrecan and collagen type 2 (Fig. 6c). This results in loss of hydration, disc height and impaired biomechanical properties driven by inflammation demonstrating homeostatic dysregulation in the degenerative IVD-NP31,36. There are myriad events involved with these pathological changes but increased IL-1β and TNFα levels are fundamental to driving inflammation-related progressive degeneration18,37. We have previously demonstrated increased levels of IL-1β and TNFα in IVD-NPs following needle puncture injury in our rodent model of DDD18. The net result of sustained exposure to these pro-inflammatory cytokines within the degenerative IVD-NP results in degradation of the ECM, loss of viable cells and diminished structural and biomechanical properties of the IVD32,38,39. IL-1β is one of the major players involved with the progression of DDD due to its pro-inflammatory effects within the IVD-NP33,37,38. Overexpression followed by binding of IL-1β and TNFα results in increased transcription of pro-inflammatory cytokines including IL-1β, IL-6, IL-8 and TNFα, the ECM degrading enzymes MMP-3, MMP-13, A disintegrin and metalloproteinase with
CMCC Research Report 2018–2020 28
Fig6Close-upofvertebralsegmentwithintestingframe.(a)Fullviewofhexapod (6-axisloadcell)testingrobot.(b)BiomechanicalassessmentofdegenerativeL5/6 IVDmotionsegmentsinjectedwithNTG-101orPBS.Thespecimens’properties (underflexionandrightlateralflexionloading)oftheNTG-101injecteddiscs arestatisticallysignificantlypreservedcomparedtothoseinjectedwithPBS(*p ≤ 0.05).(c)Modelrepresentingmechanismofaction(MoA)ofNTG-101showing itsanti-inflammatory,anti-catabolicandpro-anaboliceffectsinadegenerative IVD-NP.TreatmentwithNTG-101suppressesinflammationinducedexpression ofmatrixdegradingenzymes(MMP-3,MMP-13),celldeathandpainassociated molecules(Cox-2,PGE2).
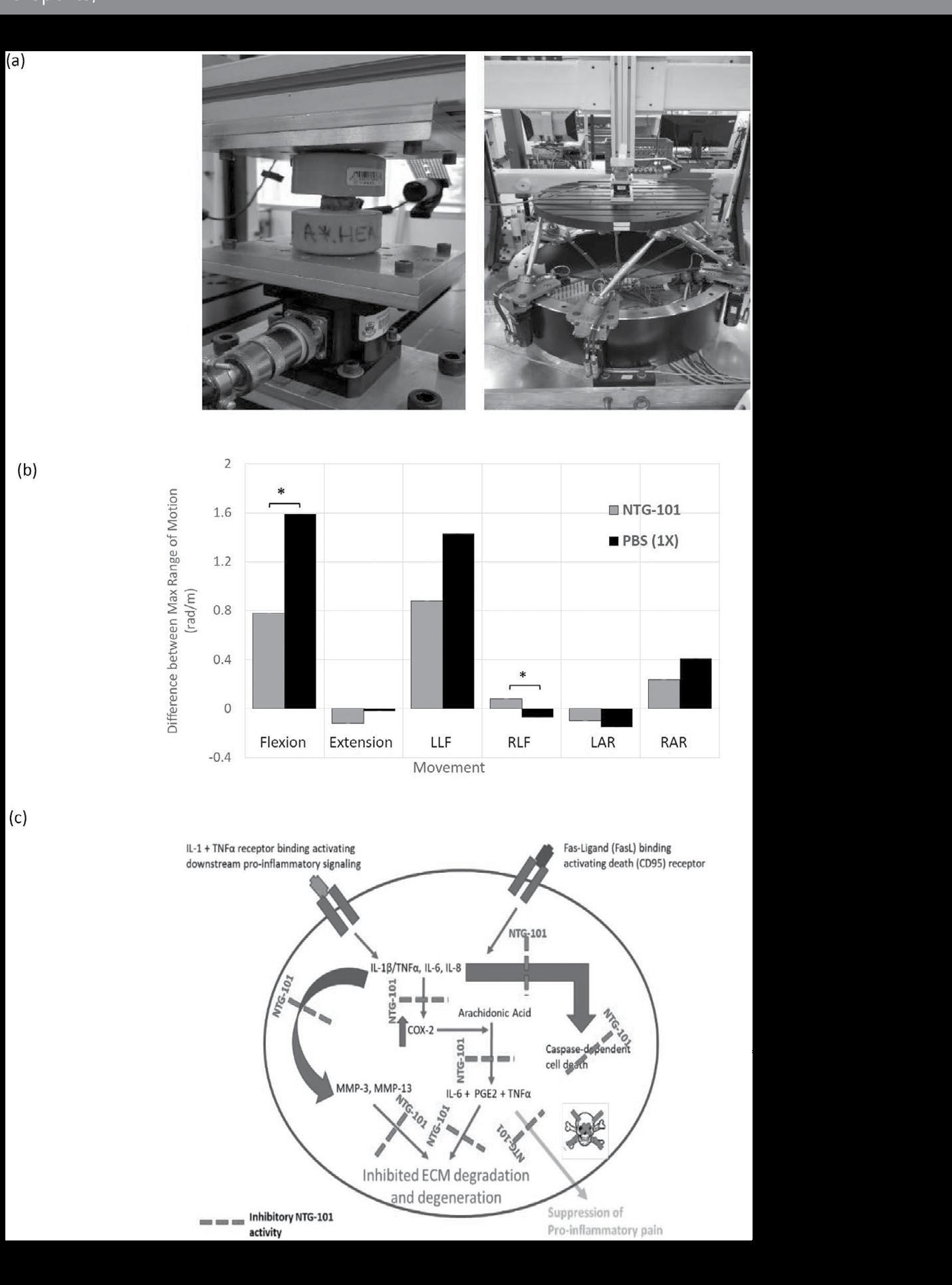
thrombospondin motifs −4/5 (ADAMTS-4/5) and inflammation/ pain associated protein (Cox-2). Both IL-6 and IL-8 further promote inflammation resulting in a positive feedback loop that in turn increases expression of TNFα, MMP-3 and Cox232. The net result is the development of the pro-catabolic microenvironment within IVD-NP enriched in ECM degrading enzymes, inhibition of de novo ECM protein synthesis leading to impaired water binding within the NP, and the production of pain related molecules1,32
Our data suggest that NTG-101 plays an important role in the suppression of inflammation and the restoration of ECM proteins (aggrecan, Col2A1, and HAPLN1) both in vitro and in in vivo (Fig. 6c). Among the components of NTG-101, both CTGF and TGF-β1 are known for their anti-inflammatory and cell growth promoting functions. The CTGF protein comprises insulin-like growth factor binding protein (IGFBP), von Willebrand factor C (VWC), thrombospondin (TSP) and Cystine knot (CT) domains that confer CTGF the ability to modulate growth factor signaling. The IGFBP domain is capable of binding to aggrecan and promote its production from chondrocytes40, while the VWC domain interferes bone morphogenetic protein-4 (BMP-4) dependent signaling but enhances the receptor binding to TGF-β141. On the other hand, the TSP domain is important for adhesion, collagen deposition and the regulation of angiogenesis by CCN2/CTGF42,43. The CT domain that binds to heparan sulfate proteoglycans (HSPGs) and integrins (αVβ3 1) is critical for adhesion, mitogenic effects and extracellular matrix production44–46. In addition to its anabolic role, CTGF can also suppress IL-1β-induced mRNA levels of MMP-3 and ADAMTS5 through cell surface integrin receptors 3 and α5β1) in IVD-NP cells28. Of note, co-transduction of lentiviral vectors containing TGFβ3, CTGF and tissue inhibitor of metalloproteinsases-1 (TIMP1) genes induced significant expression of type II collagen and aggrecan, delaying IVD - degeneration in rabbit annular puncture model of DDD47 Further, Cai et al 48, reported the addition of rhTGF-β1 partially reversed the catabolic effects of conditioned medium obtained from degenerative human IVD-NP cells (dCM) but increased expression of tissue inhibitor of metalloproteinsases-1/2/3 (TIMP-1/2/3), aggrecan and Col248. Recently, Bian et al 49 , showed increased expression of CCN2/CTGF and aggrecan in response to TGF-β signaling activation, supporting our results. Another report by Tran et al 28, also suggested that TGF-β regulates CTGF expression via activation of transcription factor, activator protein 1 (AP1) representing an attempt at repair following injury in a murine model28. Within the context of these observations, it is noteworthy that both CTGF and TGF-β1 proteins are capable of activating Smad-2/3 dependent signaling to increase the transcription of proteoglycans such as aggrecan, collagen type 2 and HAPLN128,50,51. CTGF can signal via complex interplay with Src and MAPKs to activate Smad-2/3 signaling28. Further using TGFβ-RII knock-out and lumbar spine instability mouse models, Bian et al 49, reported activation of TGF-β signaling following mechano-signaling
A selection of published research by CMCC faculty 29
Matta et al
Table 1 Absolute values of flexion, extension, lateral bending and axial rotation in CD-canine treated IVD segments.
Table 1. Absolute values of flexion, extension, lateral bending and axial rotation in CD-canine treated IVD segments.
Table
Table 2 Normalized values of flexion, extension, lateral bending and axial rotation in CD-canine treated IVD segments.
flexion, extension, lateral bending and axial rotation in CD-canine treated IVD segments.
Table 2. Normalized values of flexion, extension, lateral bending and axial rotation in CD-canine treated IVD segments.
demonstrating homeostatic dysregulation in the degenerative IVD-NP31,36. There are myriad events involved with these pathological changes but increased IL-1β and TNFα levels are fundamental to driving inflammation-related progressive degeneration18,37. We have previously demonstrated increased levels of IL-1β and TNFα in IVD-NPs following needle puncture injury in our rodent model of DDD18. The net result of sustained exposure to these pro-inflammatory cytokines within the degenerative IVD-NP results in degradation of the ECM, loss of viable cells and diminished structural and biomechanical properties of the IVD32 38 39. IL-1β is one of the major players involved with the progression of DDD due to its pro-inflammatory effects within the IVD-NP33,37,38
transduction via integrins (αvβ6) plays an important role in maintaining homeostasis and cellular functions in IVD. However, this effect could be dose dependent as demonstrated by Bian et al 52, wherein authors showed supraphysiological levels of TGFβ can lead to end plate degeneration and be detrimental to IVD. In contrast to our findings, both CTGF and TGF-β1 have been reported to promote fibrosis in some connective tissue disorders53. However, within the hypoxic, ischemic, avascular and immune privileged IVD-NP, we did not observe development of fibrosis within the NP following injection of NTG-101. In fact, in our study this combination of proteins served to increase cell survival, synthesis of vital ECM molecules, and suppressed the pro-inflammatory/catabolic environment within the degenerative IVD-NPs.
demonstrating homeostatic dysregulation in the degenerative IVD-NP31,36. There are myriad events involved with these pathological changes but increased IL-1β and TNFα levels are fundamental to driving inflammation-related progressive degeneration18,37. We have previously demonstrated increased levels of IL-1β and TNFα in IVD-NPs following needle puncture injury in our rodent model of DDD18. The net result of sustained exposure to these pro-inflammatory cytokines within the degenerative IVD-NP results in degradation of the ECM, loss of viable cells and diminished structural and biomechanical properties of the IVD32 38 39. IL-1β is one of the major players involved with the progression of DDD due to its pro-inflammatory effects within the IVD-NP33,37,38
Management. Advances in Orthopedics 2012, https://doi. org/10.1155/2012/970752 (2012).
3. Global burden of disease study 2013 collaborators. Global, regional, and national incidence, prevalance, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386, 743–800, https://doi.org/10.1016/S0140-6736(15)60692-4 (2015).
Over-expression followed by binding of IL-1β and TNFα results in increased transcription of pro-inflammatory cytokines including IL-1β, IL-6, IL-8 and TNFα, the ECM degrading enzymes MMP-3, MMP-13, A disintegrin and metalloproteinase with thrombospondin motifs 4/5 (ADAMTS-4/5) and inflammation/pain associated protein (Cox-2). Both IL-6 and IL-8 further promote inflammation resulting in a positive feedback loop that in turn increases expression of TNFα, MMP-3 and Cox-232. The net result is the development of the pro-catabolic microenvironment within IVD-NP enriched in ECM degrading enzymes, inhibition of de novo ECM protein synthesis leading to impaired water binding within the NP, and the production of pain related molecules1 32 .
Over-expression followed by binding of IL-1β and TNFα results in increased transcription of pro-inflammatory cytokines including IL-1β, IL-6, IL-8 and TNFα, the ECM degrading enzymes MMP-3, MMP-13, A disintegrin and metalloproteinase with thrombospondin motifs 4/5 (ADAMTS-4/5) and inflammation/pain associated protein (Cox-2). Both IL-6 and IL-8 further promote inflammation resulting in a positive feedback loop that in turn increases expression of TNFα, MMP-3 and Cox-232. The net result is the development of the pro-catabolic microenvironment within IVD-NP enriched in ECM degrading enzymes, inhibition of de novo ECM protein synthesis leading to impaired water binding within the NP, and the production of pain related molecules1 32 .
4. Simon, D., Jaime, C. & Scott, H. A systemic review of low back pain cost of illness studies in the United States and Internationally. The Spine Journal 8, 8–20 (2008).
Based on our results using in vivo models as reported here, it is tantalizing to hypothesize that an injection of NTG-101 may have similar effects on human degenerative IVD-NPs. In conclusion we provide a strong rationale for the use of NTG-101 as a novel, molecular therapy to treat DDD.
References
1. Adams, M. A. & Roughley, P. J. What is intervertebral disc degeneration and what causes it? Spine 31, 2151–2161 (2006).
2. Fadi, T. et al. Lumbar Degenerative Disc Disease: Current and Future Concepts of Diagnosis and
Our data suggest that NTG-101 plays an important role in the suppression of inflammation and the restoration of ECM proteins (aggrecan, Col2A1, and HAPLN1) both in vitro and in in vivo (Fig. 6c). Among the components of NTG-101, both CTGF and TGF-β1 are known for their anti-inflammatory and cell growth promoting functions. The CTGF protein comprises insulin-like growth factor binding protein (IGFBP), von Willebrand factor C (VWC), thrombospondin (TSP) and Cystine knot (CT) domains that confer CTGF the ability to modulate growth factor signaling. The IGFBP domain is capable of binding to aggrecan and promote its production from chondrocytes40, while the VWC domain interferes bone morphogenetic protein-4 (BMP-4) dependent signaling but enhances the receptor binding to TGF-β141. On the other hand, the TSP domain is important for adhesion, collagen deposition and the regulation of angiogenesis by CCN2/CTGF42,43. The CT domain that binds to heparan sulfate proteoglycans (HSPGs) and integrins (αVβ3 and α5β1) is critical for adhesion, mitogenic effects and extracellular matrix production44–46. In addition to its anabolic role, CTGF can also suppress IL-1β-induced mRNA levels of MMP-3 and ADAMTS5 through cell surface integrin receptors (αvβ3 and α5β1) in IVD-NP cells28. Of note, co-transduction of lentiviral vectors containing TGFβ3, CTGF and tissue inhibitor of metalloproteinsases-1 (TIMP1) genes induced significant expression of type II collagen and aggrecan, delaying IVD - degeneration in rabbit annular puncture model of DDD47. Further, Cai et al 48, reported the addition of rhTGF-β1 partially reversed the catabolic effects of conditioned medium obtained from degenerative human IVD-NP cells (dCM) but increased expression of tissue inhibitor of metalloproteinsases-1/2/3 (TIMP-1/2/3), aggrecan and Col248. Recently, Bian et al 49, showed increased expression of CCN2/CTGF and aggrecan in response to TGF-β signaling activation, supporting our results. Another report by Tran et al 28, also suggested that TGF-β regulates CTGF expression via activation of transcription factor, activator protein 1 (AP1) representing an attempt at repair following injury in a murine model28. Within the context of these observations, it is noteworthy that both CTGF and TGF-β1 proteins are capable of activating Smad-2/3 dependent signaling to increase the transcription of proteoglycans such as aggrecan,
5. Tom, A. et al. Paid expenditures and productivity costs associated with permanent disability pensions in patients with spinal disorders: Nationwide Finnish register-based study, 1990–2010. Eur Spine Journal 25, 275–281 (2016).
Our data suggest that NTG-101 plays an important role in the suppression of inflammation and the restoration of ECM proteins (aggrecan, Col2A1, and HAPLN1) both in vitro and in in vivo (Fig. 6c). Among the components of NTG-101, both CTGF and TGF-β1 are known for their anti-inflammatory and cell growth promoting functions. The CTGF protein comprises insulin-like growth factor binding protein (IGFBP), von Willebrand factor C (VWC), thrombospondin (TSP) and Cystine knot (CT) domains that confer CTGF the ability to modulate growth factor signaling. The IGFBP domain is capable of binding to aggrecan and promote its production from chondrocytes40, while the VWC domain interferes bone morphogenetic protein-4 (BMP-4) dependent signaling but enhances the receptor binding to TGF-β141. On the other hand, the TSP domain is important for adhesion, collagen deposition and the regulation of angiogenesis by CCN2/CTGF42,43. The CT domain that binds to heparan sulfate proteoglycans (HSPGs) and integrins (αVβ3 and α5β1) is critical for adhesion, mitogenic effects and extracellular matrix production44–46. In addition to its anabolic role, CTGF can also suppress IL-1β-induced mRNA levels of MMP-3 and ADAMTS5 through cell surface integrin receptors (αvβ3 and α5β1) in IVD-NP cells28. Of note, co-transduction of lentiviral vectors containing TGFβ3, CTGF and tissue inhibitor of metalloproteinsases-1 (TIMP1) genes induced significant expression of type II collagen and aggrecan, delaying IVD - degeneration in rabbit annular puncture model of DDD47. Further, Cai et al 48, reported the addition of rhTGF-β1 partially reversed the catabolic effects of conditioned medium obtained from degenerative human IVD-NP cells (dCM) but increased expression of tissue inhibitor of metalloproteinsases-1/2/3 (TIMP-1/2/3), aggrecan and Col248. Recently, Bian et al 49, showed increased expression of CCN2/CTGF and aggrecan in response to TGF-β signaling activation, supporting our results. Another report by Tran et al 28, also suggested that TGF-β regulates CTGF expression via activation of transcription factor, activator protein 1 (AP1) representing an attempt at repair following injury in a murine model28. Within the context of these observations, it is noteworthy that both CTGF and TGF-β1 proteins are capable of activating Smad-2/3 dependent signaling to increase the transcription of proteoglycans such as aggrecan,
6. Cheung Kennetch, M. C. et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population of one thousand forty-three individuals. Spine 34, 934–940 (2009).
7. Goupille, P., Mulleman, D. & Chevalier, X. Is interleukin-1 a good target for therapeutic intervention in intervertebral disc degeneration: lessons from the osteoarthritic experience. Arthritis Res Ther 9, 110 (2007).
8. Sinclair, S. M. et al. Attenuation of inflammatory events in human intervertebral disc cells with a tumor necrosis factor antagonist. Spine 36, 1190–1196 (2011).
CMCC Research Report 2018–2020 30
www.nature.com/scientificreports/
Biomechanical Characteristics NTG-101 Range (Mean ± SD) (rad) PBS (1X) Range (Mean ± SD) (rad) Flexion 0.01–0.02 (0.02 ± 0.00) 0.02–0.03 (0.02 ± 0.01) Extension 0.01–0.00 (0.00 ± 0.01) 0.01–0.00 (0.00 ± 0.00) Lateral bending Left 0.01–0.03 (0.02 ± 0.01) 0.01–0.03 (0.02 ± 0.01) Right 0.00–0.00 (0.00 ± 0.01) 0.00–0.00 (0.00 ± 0.01) Axial Rotation Left 0.00–0.00 (0.00 ± 0.00) 0.00–0.00 (0.00 ± 0.00) Right 0.00–0.02 (0.01 ± 0.00) 0.00–0.01 (0.01 ± 0.00)
Biomechanical Characteristics NTG-101 Range (Mean ± SD) (rad) PBS (1X) Range (Mean ± SD) (rad) Flexion 0.50–0.88 (0.78 ± 0.19) 1.21–1.99 (1.59 ± 0.39) Extension 0.49–0.22 ( 0.12 ± 0.3) 0.061–0.01 ( 0.02 ± 0.04) Lateral bending Left 0.35–1.14 (0.88 ± 0.36) 0.81–1.91 (1.43 ± 0.56) Right 0.00–0.24 (0.08 ± 0.11) 0.12– 0.04 ( 0.07 ± 0.04) Axial Rotation Left 0.14– 0.05 ( 0.01 ± 0.04) 0.20– 0.07 ( 0.15 ± 0.07) Right 0.12–0.39 (0.24 ± 0.11) 0.21–0.53 (0.41 ± 0.17)
1. Absolute values of
www.nature.com/scientificreports/ 11 R tS | (2018) 8:16809 | DOI:10.1038/s41598-018-35011-4
Table 2. Normalized values of flexion, extension, lateral bending and axial rotation in CD-canine treated IVD segments.
Biomechanical Characteristics NTG-101 Range (Mean ± SD) (rad) PBS (1X) Range (Mean ± SD) (rad) Flexion 0.01–0.02 (0.02 ± 0.00) 0.02–0.03 (0.02 ± 0.01) Extension 0.01–0.00 (0.00 ± 0.01) 0.01–0.00 (0.00 ± 0.00) Lateral bending Left 0.01–0.03 (0.02 ± 0.01) 0.01–0.03 (0.02 ± 0.01) Right 0.00–0.00 (0.00 ± 0.01) 0.00–0.00 (0.00 ± 0.01) Axial Rotation Left 0.00–0.00 (0.00 ± 0.00) 0.00–0.00 (0.00 ± 0.00) Right 0.00–0.02 (0.01 ± 0.00) 0.00–0.01 (0.01 ± 0.00)
Biomechanical Characteristics NTG-101 Range (Mean ± SD) (rad) PBS (1X) Range (Mean ± SD) (rad) Flexion 0.50–0.88 (0.78 ± 0.19) 1.21–1.99 (1.59 ± 0.39) Extension 0.49–0.22 ( 0.12 ± 0.3) 0.061–0.01 ( 0.02 ± 0.04) Lateral bending Left 0.35–1.14 (0.88 ± 0.36) 0.81–1.91 (1.43 ± 0.56) Right 0.00–0.24 (0.08 ± 0.11) 0.12– 0.04 ( 0.07 ± 0.04) Axial Rotation Left 0.14– 0.05 ( 0.01 ± 0.04) 0.20– 0.07 ( 0.15 ± 0.07) Right 0.12–0.39 (0.24 ± 0.11) 0.21–0.53 (0.41 ± 0.17)
9. Masuda, K. Biological repair of the degenerated intervertebral disc by the injection of growth factors. European Spine Journal 17, S441–S451 (2008).
10. Woods, B. I., Vo, N., Sowa, G. & Kang, J. D. Gene Therapy for Intervertebral Disc Degeneration. Orthopaedic Clinics of North America 42, 563–574 (2011).
11. Aguiar, D. J., Johnson, S. L. & Oegema, T. R. Notochordal cells interact with nucleus pulposus cells: regulation of proteoglycan synthesis. Experimental Cell Research 246, 129–137 (1999).
12. Erwin, W. M. & Inman, R. D. Notochord cells regulate intervertebral disc chondrocyte proteoglycan production and cell proliferation. Spine 31, 1094–1099 (2006).
13. Erwin, W. M., Ashman, K., O’Donnell, P. & Inman, R. D. Nucleus pulposus notochord cells secrete connective tissue growth factor and upregulate proteoglycan expression by intervertebral disc chondrocytes. Arthritis and Rheumatism 54, 3859–3867 (2006).
14. Erwin, W. M., Las Heras, F., Islam, D., Fehlings, M. G. & Inman, R. D. The Regenerative Capacity of the Notochordal Cell: Tissue Constructs Generated in Vitro under Hypoxic Conditions. The Journal of Neurosurgery-Spine 10, 513–522 (2009).
15. Erwin, W. M., Islam, D., Inman, R. D., Fehlings, M. G. & Tsui, F. W. Notochordal cells protect nucleus pulposus cells from degradation and apoptosis: implications for the mechanisms of intervertebral disc degeneration. Arthritis Res Ther 13, R215, https:// doi.org/10.1186/ar3548 (2011).
16. Arne, M. et al. Notochordal cell-derived conditioned medium protects human nucleus pulposus cells from stress-induced apoptosis. The Spine Journal 4, https://doi.org/10.1016/j. spinee.2017.01.003 (2017).
17. Matta, A., Karim, M. Z., Isenman, D. & Erwin, W. M. In Lumbar Spine Research Society (Chicago, 2016).
18. Matta, A, K M., Zia, Isenman, D. E. & Erwin, W. M. Molecular therapy for degenerative disc disease: Clues from secretome analysis of the notochordal cell-rich nucleus pulposus. Scientific Reports 7, https://doi.org/10.1038/srep45623 (2017).
19. Bach, F. C. et al. Soluble and pelletable factors in porcine, canine and human notochordal cell-conditioned medium: implications for IVD regeneration. European Cells and Materials 32, 163–180 (2016).
20. de Vries, S. A. et al. Conditioned medium derived from notochordal cell-rich nucleus pulposus tissue stimulates matrix production by canine nucleus pulposus cells and bone marrow-derived stromal cells. Tissue Engineering Part A 21, 1077–84 (2015).
21. Rutges, J. P. et al. A validated new histological classification for intervertebral disc degeneration. Osteoarthritis and Cartilage 21, 2039–2047 (2013).
22. Shu, C. C. et al. A Histopathological Scheme for the Quantitative Scoring of Intervertebral Disc Degeneration and the Therapeutic Utility of Adult Mesenchymal Stem Cells for Intervertebral Disc Regeneration. Int J Mol Sci 18, E1049 (2017).
23. Bergknut, N. et al. Intervertebral disc disease in dogs-Part 1: A new histological grading scheme for classification of interevertebral disc degeneration in dogs. The Veterinary Journal 195, 156–163 (2013).
24. Matta, A. et al. Prognostic significance of head-and-neck cancer biomarkers previously discovered and identified using iTRAQ - labeling and multidimensional liquid chromatography - tandem mass spectrometry. Journal of Proteome Research 7, 2078–87 (2008).
25. Erwin, W. M. et al. The biological basis of degenerative disc disease: proteomic and biomechanical analysis of the canine intervertebral disc. Arthritis Res Ther 17, https://doi. org/10.1186/s13075-015-0733-z (2015).
26. Hongting, J. et al. TGF-B signaling plays an essential role in the growth and maintenance of intervertebral disc tissue. FEBS Letters 585, 1209–1215 (2011).
27. Jake, B. et al. Impaired intervertebral disc development and premature disc degeneration in mice with notochord-specific deletion of CCN2. Arthritis and Rheumatism 65, 2634–2644 (2013).
28. Tran Cassie, M. et al. Regulation of CCN2/Connective Tissue Growth Factor expression in the nucleus pulposus of the intervertebral disc. Arthritis and Rheumatism 62, 1983–1992 (2010).
29. Niklas, B. et al. The Dog as an Animal Model for Intervertebral Disc Degeneration? Spine 37, 351–358 (2012).
30. Margaux, B., Marie-Martine, L.-C., Rannou, F. & Christelle, N. Active discopathy: a clinical reality. Rheumatic and Musculoskeletal Diseases 4, https://doi.org/10.1136/ rmdopen-2018-000660 (2018).
31. Adams, M. A. & Dolan, P. Intervertebral disc degeneration: evidence for two distinct phenotypes. Journal of Anatomy 221, 497–506 (2012).
32. Risbud, M. V. & Shapiro, I. M. Role of cytokines in intervertebral disc degeneration: pain and disc content. Nature Reviews Rheumatology 10, 44–56 (2014).
33. Burke, J. G. et al. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. Journal of Bone and Joint Surgery 84-B, 196–201 (2002).
34. Schubert, A. K. et al. Quality assessment of surgical disc samples discriminates human annulus fibrosus and nucleus pulposus on tissue and molecular level. Int J Mol Sci 13, 19 (2018).
35. Pattappa, G. et al. Diversity of intervertebral disc cells: phenotype and function. Journal of Anatomy 221, 480–496 (2012).
36. Inoue, N. & Espinoza, A. A. Biomechanics of Intervertebral Disc Degeneration. Orthopaedic Clinics of North America 42, 487–499 (2011).
37. Johnson Zariel, I., Schoepflin Zacharay, R., Hyowon, C., Shapiro, I. M. & Risbud, M. V. Disc in Flames: Roles of TNF-a and IL-1B in Intervertebral Disc Degeneration. European Cells and Materials 30, 104–16 (2015).
38. Le Maitre, C. L., Hoyland, J. A. & Freemont, A. J. Catabolic cytokine expression in degenerate and herniated human
A selection of published research by CMCC faculty 31
Matta et al
intervertebral discs: IL-1beta and TNFalpha expression profile. Arthritis Research and Therapy 9, R77 (2007).
39. Cui, L. Y. et al. IL-1beta sensitizes rat intervertebral disc cells to Fas ligand mediated apoptosis in vitro. Acta Pharmacologica Sinica 28, 1671–1676 (2007).
40. Aoyama, E. et al. N-terminal domains of CCN family 2/connective tissue growth factor bind to aggrecan. Biochemical Journal 420, 413–420 (2009).
41. Abreu, J. G., Ketpura, N. I., Reversade, B. & De Robertis, E. M. Connective-tissue growth factor (CTGF) modulates cell signalling by BMP and TGF-B. Nature Cell Biology 4, 599–604 (2002).
42. Tong, Z. Y. & Brigstock, D. R. Intrinsic biological activity of the thrombospondin structural homology repeat in connective tissue growth factor. Journal of Endorinolgy 188, R1–R8 (2006).
43. Inokai, I. et al. Connective tissue growth factor binds vascular endothelial growth factor (VEGF) and inhibits VEGF-induced angiogenesis. FEBS Letters 16, 219–221 (2002).
44. Gao, R. & Brigstock, D. R. Connective tissue growth factor (CCN2) induces adhesion of rat activated hepatic stellate cells by binding of its C-terminal domain to integrin alpha(v) beta(3) and heparan sulfate proteoglycan. Journal of Biochemistry 279, 8848–8855 (2004).
45. Gao, R. & Brigstock, D. R. A novel integrin alpha5beta1 binding domain in module 4 of connective tissue growth factor (CCN2/ CTGF) promotes adhesion and migration of activated pancreatic stellate cells. Gut 55, 856–862 (2006).
46. Hoshijima, M. et al. CT domain of CCN2/CTGF directly interacts with fibronectin and enhances cell adhesion of chondrocytes through integrin alpha5beta1. FEBS Letters 580, 1376–1382 (2006).
47. Liu, Y. et al. Lentivirus-mediated TGF-β3, CTGF and TIMP1 gene transduction as a gene therapy for intervertebral disc degeneration in an in vivo rabbit model. Exp Ther Med 11, 1399–1404 (2016).
48. Feng, C. et al. The paracrine effect of degenerated disc cells on healthy human nucleus pulposus cells is mediated by MAPK and NF- kB pathways and can be reduced by TGF-B1. DNA and Cell Biology 36, 143–158 (2017).
49. Bian, Q. et al. Mechanosignaling activation of TGFβ maintains intervertebral disc homeostasis. Bone Research 5, 17008, https://doi. org/10.1038/boneres.2017.8 (2017).
50. Schmierer, B. & Hill, C. S. TGFβ–SMAD signal transduction: molecular specificity and functional flexibility. Nature Reviews Molecular Cell Biology 8, 970, https://doi. org/10.1038/nrm2297 (2007).
51. Rik, D. & Zhang Ying, E. Smad-dependent and Smadindependent pathways in TGF-B family signalling. Nature 425, 577–584 (2003).
52. Bian, Q. et al. Excessive Activation of TGFβ by Spinal Instability Causes Vertebral Endplate Sclerosis. Scientific Reports 6, 27093, https://doi.org/10.1038/srep27093 (2016).
53. Ihn, H. Pathogenesis of fibrosis: role of TGF-B and CTGF. Current Opinion in Rheumatology 14, 681–685 (2002
Acknowledgements
The authors gratefully acknowledge funding support from Mr. Jeff Skoll.
Author Contributions
A.M. and W.M.E. designed all in vivo and in vitro experiments, wrote and edited manuscript. W.F. and M.S. designed and performed all MRI-related experiments reviewed all relevant data and wrote relevant sections of the manuscript. P.J., G.K. and M.F. designed, performed interpreted, wrote and reviewed all experimental aspects of the biomechanics-related work. A.G. performed and supervised all canine in vivo injuries and injections. A.M., M.Z.K. and W.M.E. performed all other experiments and analyzed data. H.G. performed histological and immunohistochemical experiments. B.E. reviewed the final manuscript and provided clinically-related commentary. W.M.E. provided all the reagents, financial support and infrastructure for performing the experiments.
Additional Information
Supplementary information accompanies this paper at https:// doi.org/10.1038/s41598-018-35011-4.
Competing Interests:
Dr. A.M., M.K. and W.M.E. has stock ownership and receive salary support from Notogen Inc. Dr. W.M.E. has partial salary support via Canadian Chiropractic Research Foundation/ Canadian Memorial Chiropractic College. H.G. has stock ownership and receive salary support from Notogen Inc. Dr. B.E. has stock ownership in Notogen Inc. Dr. P.J., M.F., G.K., A.G., W.F. and M.S. declare no potential conflict of interest.
Publisher’s note:
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
© The Author(s) 2018
CMCC Research Report 2018–2020 32
OriginallypublishedinScienceReportsbySpringerNature 2018Nov14;8(1):16809.
ReproducedunderthetermsoftheCreativeCommonsCCBY license.
AccessOnline:https://doi.org/10.1038/s41598-018-35011-4.
A selection of published research by CMCC faculty
33
et al
Matta
Biological Basis of Musculoskeletal Injury and Manual Therapies
Does Manual Therapy Affect Functional and Biomechanical Outcomes of a Sit-to-Stand Task in a Population with Low Back Pain? A Preliminary Analysis
Carpino G1, Tran S1 , Currie S2 , Enebo B2 , Davidson BS2 , Howarth SJ1 1CanadianMemorialChiropracticCollege, 2UniversityofDenver
Abstract
Introduction:
Manual therapy (MT) hypothetically affects discrepant neuromuscular control and movement observed in populations with low back pain (LBP). Previous studies have demonstrated the limited influence of MT on movement, predominately during range of motion (ROM) testing. It remains unclear if MT affects neuromuscular control in mobility-based activities of daily living (ADLs). The sit-to-stand (STS) task represents a commonly performed ADL that is used in a variety of clinical settings to assess functional and biomechanical performance.
Objective:
To determine whether MT affects functional performance and biomechanical performance during a STS task in a population with LBP.
Methods:
Kinematic data were recorded from the pelvis and thorax of participants with LBP, using an optoelectronic motion capture system as they performed a STS task before and after MT from November 2011 to August 2014. MT for each participant consisted of two high-velocity low-amplitude spinal manipulations, as well as two grade IV mobilizations of the lumbar spine and pelvis targeted toward the third lumbar vertebra and sacroiliac joint in a side-lying position; the order of these treatments was randomized. Pelvis and thorax kinematic data were used to derive the time-varying lumbar angle in the sagittal plane for each STS trial. The difference between the maximum and minimum lumbar angles during the STS trial determined the sagittal ROM that was used as the
biomechanical outcome. Time to complete each STS trial was used as a functional measure of performance. Pre-MT and postMT values for the lumbar sagittal ROM and time to completion were statistically analysed using paired samples t-tests.
Results:
Data were obtained from 40 participants with 35 useful datasets (NRS = 3.3 ± 1.2; 32.4 ± 9.8 years; 16 females, 19 males). After MT, lumbar sagittal ROM increased by 2.7 ± 5.5 degrees (p = 0.007). Time to complete the STS test decreased by 0.4 ± 0.4 s (p < 0.001).
Discussion:
These findings provide preliminary evidence that MT might influence the biomechanical and functional performance of an STS task in populations with LBP. The MT intervention in this study involved a combination of spinal manipulations and mobilizations. Future work will expand upon these data as a basis for targeted investigations on the effects of either spinal manipulation and mobilization on neuromuscular control and movement in populations with LBP.
OriginallypublishedinChiropractic&ManualTherapies(2020) 28:5
OpenAccessarticle.Thisarticleisreproducedundertheterms of the Creative Commons Attribution 4.0 International License http://creativecommons.org/licenses/by/4.0/)
AccessOnline:https://doi.org/10.1186/s12998-019-0290-7
CMCC Research Report 2018–2020 34
Force Transmission Between Thoracic and Cervical Segments of the Spine During Prone-Lying High-Velocity Low-Amplitude Spinal Manipulation: A Proof of Principle for the Concept of Regional Interdependence
Engell S, Triano JJ, Howarth SJ CanadianMemorialChiropracticCollege
Abstract
Background
Regional interdependence is conceptually based on observations that applying manual therapy to a remote anatomical region has an effect in the area of the patient’s primary complaint. The current model for regional interdependence depends on force transmissibility within the body. This investigation sought to determine transmissibility between forces applied to the thoracic spine during prone-lying high-velocity low-amplitude spinal manipulative therapy and the cervical spine.
Methods
A chiropractic treatment table was modified to allow (or disallow) translation of the headrest in the caudal-cephalad direction when unlocked (or locked). Prone-lying high-velocity low-amplitude spinal manipulative therapy was applied to the thoracic region of 9 healthy participants with the headrest in both configurations. Head and thorax kinematics and kinetics were measured at interfaces between participant and the external environment, which included the clinician’s hands. Compressive forces at the cervicothoracic junction and angular kinematics of the cervical spine were derived. Ratios between the clinician-applied forces (input) and the cervical compressive force (output) were also determined.
Findings
The cervical spine extended during all high-velocity lowamplitude spinal manipulative therapy trials. Force input-tooutput ratios exceeded 1 for high-velocity low-amplitude spinal manipulative therapy trials performed with the headrest in the locked configuration, which was greater than ratios for the unlocked configuration.
Interpretation
Forces imparted to thoracic spine during high-velocity lowamplitude spinal manipulative therapy were transmitted to the cervical spine, which provided a precursor for the regional interdependence model for manual therapy. Friction between the participant’s face and the treatment table’s head rest likely amplified cervical compressive forces.
OriginallypublishedinClinicalBiomechanics,2019Oct;69:5863.
ReproducedwithpermissionfromElsevier.
Access Online:https://doi.org/10.1016/j.clinbiomech.2019.07.006
A selection of published research by CMCC faculty 35
Lower-Limb Factors Associated with Balance and Falls in Older Adults: A Systematic Review and Clinical Synthesis
Neville C1, Nguyen H2 , Ross K3 , Wingood M 4 , Peterson EW 5 , Dewitt JE6 , Moore J7, King MJ 8 , Atanelov L9, White J10 , Najafi B2
Abstract
Background:
Despite sufficient evidence to suggest that lower-limb–related factors may contribute to fall risk in older adults, lower-limb and footwear influences on fall risk have not been systematically summarized for readers and clinicians. The purpose of this study was to systematically review and synethesize the literature related to lower-limb, foot, and footwear factors that may increase the risk of falling among community-dwelling older adults.
Methods:
We searched PubMed, Embase, PsycINFO, CINAHL, Web of Science, Cochrane Library, and AgeLine. To describe the trajectory toward increasing risk of falls, we examined those articles that linked age-related changes in the lower limb or footwear to prospective falls or linked them to evidence-based fall risk factors, such as gait and balance impairment.
Results:
This systematic review consisted of 81 articles that met the review criteria, and the results reflect a narrative review of the appraised literature for eight pathways of lower-limb–related influences on fall risk in older adults. Six of the eight pathways support a direct link to fall risk. Two other pathways link to the intermediate factors but lack studies that provide evidence of a direct link.
Conclusions:
This review provides strong guidance to advance understanding and assist with managing the link between lower-limb factors and falls in older adults. Due to the lack of literature in specific areas, some recommendations were based on observational studies and should be applied with caution until further research can be completed. (J Am Podiatr Med Assoc 110(5): 1-29, 2020)
OriginallyappearedintheJournaloftheAmericanPodiatric MedicalAssociation,2020Sep1;110(5):Article_4.
ReproducedwithpermissionfromtheAmericanPodiatric Medical Association.
AccessOnline:https://doi.org/10.7547/19-143
CMCC Research Report 2018–2020 36
1UpstateMedicalUniversity, 2BaylorCollegeofMedicine, 3CanadianMemorialChiropracticCollege, 4UniversityofVermont, 5UniversityofIllinois, 6Advanced Foot and Ankle Associates, 7CumberlandFootandAnkleCentersofKentucky, 8UpperlineHealthcare,Nashville, 9SteadyStrides:Johns HopkinsPhysicalMedicineandRehabilitation, 10SafeStep,OrthoticHoldingsInc.
Correlations Between Individuals’ Characteristics and Spinal Stiffness in Individuals With and Without Back Pain: A Combined Analysis of Multiple Data Sets
Abstract
Objectives:
The purpose of this study was to describe the correlations between individual characteristics and spinal stiffness as measured with different spinal stiffness measurement devices in individuals with and without back pain.
Methods:
A secondary analysis of 3 adult data sets obtained using 3 different devices, in 2 spinal regions, from a total of 5 separate cross-sectional studies was conducted. Differences in spinal stiffness between men and women and in the strength of correlations among spinal stiffness and age and anthropometric characteristics were evaluated using either the t test for independent samples, Pearson’s correlation coefficient, or Kendall’s τ rank correlation coefficient.
Results:
As expected, results varied between data sets; however, few factors had consistent correlations. Specifically, spinal stiffness was significantly lower in women than men in all 3 data sets. Height was positively correlated with spinal stiffness across all data sets. Although weight was correlated with thoracic stiffness, its correlation with lumbar stiffness varied. In 2 data sets, body mass index was inversely associated with lumbar spinal stiffness, whereas results from the thoracic spine region revealed a positive correlation. The results for 1 data
set suggest that physiological measurement evaluating body weight distribution may also affect spinal stiffness; however, the specific correlation remains unclear.
Conclusion:
Despite data set differences, significant correlations were observed, indicating that participants’ characteristics appear to affect spinal stiffness measurement. (J Manipulative Physiol Ther 2018;41:734-752)
Key Indexing Terms: Back Pain; Association; Spine; Complementary Therapies
OriginallypublishedintheJournalofManipulative PhysiologicalTherapeutics,Nov-Dec2018;41(9):734-752.
ReproducedwithpermissionfromElsevier.
AccessOnline:https://doi.org/10.1016/j.jmpt.2018.04.006
A selection of published research by CMCC faculty 37
Pagé I1, Swain M2 , Wong A 3 , Breen A 4 , De Carvalho D5 , Descarreaux M5 , Funabashi M6 , Kawchuk G7 1Université du Québec à Trois-Rivières, 2MacquarieUniversity, 3HongKongPolytechnicUniversity, 4AECCUniversityCollege, 5MemorialUniversityof Newfoundland, 6CanadianMemorialChiropracticCollege, 7UniversityofAlberta
A Descriptive Analysis of Shoulder Muscle Activities During Individual Stages of the Turkish Get-Up Exercise
St-Onge E1, Robb A 2 , Beach TAC 3 , Howarth SJ1 1CanadianMemorialChiropracticCollege, 2Private Practice, 3UniversityofToronto
Abstract
The Turkish Get-Up (TGU) is a complex and multi-planar exercise; the performer begins in a supine lying position, progresses toward upright standing through a series of 7 stages while holding a mass overhead in one hand, and returns to the original supine lying position through a reversal of the same 7 stages. A descriptive analysis of shoulder muscle activity during the TGU may provide insight toward its use in training and rehabilitation contexts. Our objectives were to: (1) describe the activity patterns from a subset of muscles that span the glenohumeral joint during individual stages of the TGU, and (2) interpret these patterns through comparisons between left- and right-side muscles, and between the up and down phases of the TGU. Twelve individuals with at least one-year experience performing the TGU were included in this study. Surface electromyographic (EMG) recordings were bilaterally obtained from 8 glenohumeral muscle groups while participants performed ten trials of the TGU with a kettlebell in their right hand. Instants representing the start and end of each TGU stage were identified from a synchronized video for each trial, and EMG activities for each muscle were integrated over the duration of each stage. Average integrated EMG and withinparticipant coefficients of variation were calculated. Overall, the greatest muscular demand occurred during the second (press
to elbow support) and fifth (leg sweep) stages. Activities from muscles on the ipsilateral side to the kettlebell (right-side) were greater during stages when the contralateral upper limb did not contribute to supporting the body; however, contralateral (left-side) muscles were invoked during stages when the nonkettlebell-bearing forearm or hand contributed to supporting the body. The results suggest the importance of training both phases of the TGU to gain the most benefit from the exercise and highlights the asymmetric nature of the exercise, which may be particularly relevant for athletes engaged in activities with rotational demands.
OriginallypublishedintheJournalofBodywork&Movement Therapies23(2019)Jan;23(1):23-31.
ReproducedwithpermissionfromElsevier.
AccessOnline:https://doi.org/10.1016/j.jbmt.2018.01.013
CMCC Research Report 2018–2020 38
Nonspecific Low Back Pain: Inflammatory Profiles of Patients With Acute and Chronic Pain
Teodorczyk-Injeyan JA, Triano JJ, Injeyan HS CanadianMemorialChiropracticCollege
Abstract
Background:
The pathogenesis of low back pain (LBP) remains unclear. However, recent studies suggest that the inflammatory response may be inherent in spinal pain. The purpose of this study was to discern inflammatory profiles in patients with nonspecific acute and chronic LBP in relation to those in asymptomatic individuals.
Materials and methods:
Peripheral blood samples were obtained from asymptomatic controls and patients with nonspecific acute and chronic LBP reporting a minimum pain score of 3 on a 10-point Visual Analogue Scale (VAS). The levels of in vitro production of proinflammatory (tumor necrosis factor α [TNFα], interleukin [IL] 1β, IL-6, IL-2, interferon γ) and anti-inflammatory (IL-1 receptor antagonist, soluble receptors of TNF2, and IL-10) mediators were determined by specific immunoassays.
Results:
The mean VAS scores were comparable between the acute and chronic LBP patient groups. Compared with asymptomatic group, the production of TNFα, IL-1β, IL-6 and their ratios to IL-10 levels were significantly elevated in both patient groups (P=0.0001 to 0.003). In acute LBP group, the ratio of IL-2:IL-10 was also significantly increased (P=0.02). In contrast, the production of interferon γ was significantly reduced compared
with the other study groups (P=0.005 to 0.01), nevertheless, it was positively correlated (P=0.006) with pain scores. In chronic LBP patients, the production of TNFα, IL-1 receptor antagonist, and soluble receptors of TNF2 was significantly increased (P=0.001 to 0.03) in comparison with the control and acute LBP groups, and TNFα and IL-1β levels were positively correlated (P<0.001) with VAS scores.
Conclusions:
The inflammatory profiles of patients with acute and chronic LBP are distinct. Nonetheless, in both patient groups, an imbalance between proinflammatory and anti-inflammatory mediator levels favors the production of proinflammatory components.
OriginallypublishedinTheClinicalJournalofPain2019 Oct;35(10):818-825.
ReproducedwithpermissionfromWoltersKluwerHealth,Inc.
AccessOnline:https://doi.org/10.1097/AJP.0000000000000745
A selection of published research by CMCC faculty 39
SafetyNET Community-Based Patient Safety Initiatives: Development and Application of a Patient Safety and Quality Improvement Survey
Abstract
Objectives:
To: 1) develop/adapt and validate an instrument to measure patient safety attitudes and opinions of community-based spinal manipulative therapy (SMT) providers; 2) implement the instrument; and 3) compare results among healthcare professions.
Methods:
A review of the literature and content validation were used for the survey development. Community-based chiropractors and physiotherapists in 4 Canadian provinces were invited.
Results:
The Agency for Healthcare Research and Quality’s (AHRQ) Medical Office Survey on Patient Safety Culture was the preferred instrument. The survey was modified and validated, measuring 14 patient safety dimensions. 276 SMT providers volunteered to respond to the survey. Generally, SMT providers had similar or better patient safety dimension scores compared to the AHRQ 2016 medical offices database.
Discussion:
We developed the first instrument measuring patient safety attitudes and opinions of community-based SMT providers. This instrument provides understanding of SMT providers’ opinions and attitudes on patient safety and identifies potential areas for improvement.
Introduction
Patient safety is a leading healthcare challenge.1 In 1999, the U.S. Institute of Medicine’s To Err is Human: Building a Safer Health System2 report advised the development and sustainability of an open and constructive patient safety culture. In 2002, the Canadian government’s Building a Safer System: A National Integrated Strategy for Improving Patient Safety in Canadian Health Care3 supported and emphasized the need for leadership with this challenge. These reports laid out comprehensive strategies to reduce preventable medical errors, which did not focus on individuals making the error, but rather
on how the systems, processes and conditions fail to prevent the error.4
One strategy to promote and understand a healthcare organization’s existing patient safety culture is by assessing its current attitudes and opinions toward safety.4 Although several surveys currently exist to assess attitudes and opinions, most are designed for large, acute care settings rather than communitybased health care environments. As the majority of people receive care in community-based settings, further information about community-based health care providers’ behaviors, attitudes, and opinions about patient safety is needed.5
Spinal manipulative therapy (SMT) is a therapeutic intervention commonly used by chiropractors and physio-therapists and perceived to carry added risks to patients with varying evidence regarding the incidence of associated adverse events (AEs).6 It is estimated that 4.5 million Canadians and over 50% of Americans receive SMT per year.7,8 Despite SMT’s popularity, few formal patient safety and reporting mechanisms are available5, increasing the need for specific SMT-related patient safety initiatives. As most SMT is provided in community-based offices/ clinics9, having a patient safety survey specifically for these settings is essential.
SafetyNET is an international and multidisciplinary research team, whose primary goal is to support strategies that promote a patient safety culture among SMT providers.10 Although AEs following SMT intervention have been described to vary widely in severity and frequency, no robust causal inferences have been made.6,11,12 Thus, systematic reviews investigating SMT-related AEs have called for more research.13,14
To date, only a few patient safety mechanisms, such as reporting and learning systems, exist to systematically monitor and reduce SMT-related harms.15 With the call for more research and few patient safety measurement options, there is a need to measure and assess current patient safety attitudes and opinions. Therefore, our study aimed to: 1) develop or adapt an assessment tool to measure patient safety attitudes and opinions of community-based SMT providers, specifically chiropractors
CMCC Research Report 2018–2020 40 Clinical and Health Services Research
Funabashi M1,2 , Pohlman KA 3,4 , Mior S1 , O'Beirne M 4 , Westaway M5,6 , De Carvalho D7, El-Bayoumi M8 , et al. 1CanadianMemorialChiropracticCollege, 2UniversityofAlberta, 3ParkerUniversity, 4UniversityofCalgary, 5Privatepractice, 6McMasterUniversity, 7MemorialUniversityofNewfoundland, 8NewBrunswickChiropractors'Association
and physiotherapists; 2) validate this assessment tool; 3) implement this tool with community-based chiropractors and physiotherapists who apply SMT; and 4) compare the resultant scores against other healthcare professions.
Methods
Survey Development
We conducted a literature review with assistance of a health sciences librarian who is expert in scoping reviews to identify available patient safety surveys and their applicability to the SMT setting. Searches were conducted in Google, Google Scholar, and PubMed. Search terms included: ‘patient safety survey’, ‘patient safety culture’, and ‘patient safety climate’; in conjunction with ‘community-based’, ‘ambulatory’, ‘medical offices’, and ‘general practice’. Based on consultation with subject matter experts on our research team, surveys specific for SMT professions were not expected and, therefore, terms related to ‘chiropractic’, ‘physiotherapy’, ‘manual therapy’ or ‘spinal manipulative therapy’ were not included in the search. In addition to the electronic databases, content experts on the research team were also queried for suggested relevant surveys. All citation abstracts were screened and assessed by the SafetyNET team members to evaluate their relevance to the following criteria: 1) addressed the research question; 2) measurement properties established (i.e., with reported validity and reliability); 3) ease of use (i.e., lack of patient safety jargon, manageable number of sections, each section was not too long); and 4) estimated number of necessary modifications (although this was not a determinant factor).
Relevant surveys (Table 1) were independently assessed by eight SafetyNET multidisciplinary team members with expertise in SMT, epidemiology, patient safety and/or survey development. Feedback was summarized and presented to all 22 expert SafetyNET team members. The preferred survey was identified by consensus and modifications were made to meet our study needs using an iterative consensus-based process.
The final stage involved content validation adhering to the COnsensus-based Standards for the selection of health status Measurement INstruments (COSMIN) checklist.16 A face-toface qualitative focus group was conducted to evaluate the relevance and comprehensiveness of the modified survey with a convenience sample of volunteers attending a chiropractic educational conference in Edmonton, Alberta. Then, a feasibility assessment of the survey was conducted by circulating it amongst SMT providers to further evaluate the content and face validity, the functionality and time to complete the survey.
Survey Application
The final survey was created using a standardized Research Electronic Data Capture (REDCap) database. REDCap is a secure, web-based application designed to support data capture for research providing an intuitive interface for validated
data entry, audit trails for data manipulation, and export procedures.17 Invitation to participate in survey completion was distributed via email to Canadian community-based chiropractors and physiotherapists from four different Canadian provinces through their respective provincial associations.
Survey Data Analysis
Data on patient safety culture dimensions were analyzed in two ways using Stata13 Software (StataCorp. 2013) and Excel 2013. First, a positive percentage composite score was calculated for each dimension by averaging the percent positive responses on the questions within each dimension. For negatively worded questions, disagreeing was considered a positive response. Second, survey dimensions’ scores were calculated based on the mean response to the five-point scale and its 95% confidence interval (CI). Pearson chi-square test was used to compare the scores from SMT providers with the AHRQ medical offices comparative database, with level of significance at p=0.05. Each dimension required that all questions be answered to be included. Frequencies of responses were calculated for factors inhibiting participation in a reporting and learning system, patient safety items and quality issues, information exchange with other settings, and overall clinic self-ratings.
Comparative Database
The Medical Office Survey on Patient Safety Culture is an expansion of AHRQ’s Hospital Survey on Patient Safety Culture to the medical office setting. Its content has been extensively tested for validity and reliability, and it has been in use since 2004.18 It was designed to measure the culture of patient safety in medical offices from the perspective of providers and staff. The Medical Office Survey on Patient Safety Culture 2016 User Comparative Database has been previously described.19 Briefly, it consists of data from 1,528 medical offices located across the United States and 25,127 medical office respondents from varied specialties who completed the survey between 2013 and 2015. This comparative database report was developed as a tool for comparison of survey results, internal assessment, and to provide supplemental information to help offices/clinics identify their strengths and areas with potential for improvement.
Results Survey Development
The literature review identified four commonly used surveys that assessed patient safety attitudes and opinions in communitybased settings (Table 1).18,20–22 The AHRQ Medical Office Survey on Patient Safety Culture was identified as the team’s preferred instrument.18
Based on feedback from the SafetyNET team, the following modifications were made to the AHRQ medical office survey: 1) the word ‘medical’ was removed, and, replaced with ‘clinical’ or ‘office’; 2) for ‘Organizational Learning’ and ‘Overall Perceptions of Patient Safety and Quality’ each question was asked regarding its clinical and administrative perspective; 3) in the ‘Overall
A selection of published research by CMCC faculty 41
Funabashi et al
Surveys identified during the literature review that evaluate patient safety attitudes and opinions in ambulatory settings.
Author / Year Manuscript Title
de Wet et al., 2010 22
Purpose
Hoffman et al., 2011 21
The development and psychometric evaluation of a safety climate measure for primary care
The Frankfurt Patient Safety Climate Questionnaire for General Practices (FraSiK): analysis of psychometric properties
To measure perceptions of safety climate among primary care teams outside of North America.
To measure patient safety climate in practices with only 1-2 doctors, who are owners with 2-4 other professional employees (small offices).
Primary care teams in National Health Service, Scotland
General practice in Germany
563 primary care team members from 49 general practices
332 healthcare professionals working in 60 general practices
Modak et al., 2007 20
Measuring safety culture in the ambulatory setting: the Safety Attitudes Questionnaire (SAQ)– Ambulatory Version (SAQ-A)
To measure safety attitudes of outpatient settings.
Sorra et al., 2016 18
Medical Office Survey on Patient Safety Culture- User Guide
Modification of the AHRQ Hospital Survey on Patient Safety Culture. Emphasized safety and quality issues that are known to affect patient safety in medical offices.
Academic, urban, outpatient practice in Texas, United States
Medical Offices in the United States
30 items, measuring 5 safety climate factors:
1) Leadership,
2) Teamwork,
3) Communication,
4) Workload,
5) Safety Systems.
72 items, measuring 9 dimensions:
1) Teamwork climate,
2) Error management,
3) Safety of clinical processes,
4) Perception of causes of errors,
5) Job satisfaction,
6) Safety of office structure,
7) Receptiveness to healthcare assistants,
8) Patient safety of medical care.
{Adapted from the SAQ-A}
251 outpatients providers (physicians, nurses, managers, medical assistants and support staff)
Pilot tested in 2007 with 200 offices, > 4,100 surveys. First released in 2009, with comparable databases released approximately every 2 years.
62 item survey, measuring 6 factors:
1) Teamwork climate,
2) Safety climate,
3) Perceptions of management,
4) Job satisfaction,
5) Working conditions,
6) Stress recognition.
51 item survey, measuring 13 dimensions:
1) Teamwork,
2) Work pressure and pace,
3) Staff Training,
4) Office processes and standardization,
5) Communication openness,
6) Patient Care Tracking / Follow-up,
7) Communication about error,
8) Owner / Managing Partner / Leadership support for patient safety,
9) Organizational learning,
10) Overall perceptions of patient safety and quality,
11) List of patient safety and quality issues,
12) Information exchange with other settings,
13) Overall ratings on quality and patient safety
interface for validated data entry, audit trails for data manipulation, and export procedures.17 Invitation to participate in survey completion was distributed via email to Canadian community-based chiropractors and physiotherapists from four different Canadian provinces through their respective provincial associations.
Survey Data Analysis
Rating’ section, socioeconomic status was removed from ‘Equitable’ as the team felt it should not be grouped with the other qualities listed (i.e., gender, race, ethnicity, language) considering SMT is a non-insured service in Canada and access may be affected differently than these other qualities. Socioeconomic status was therefore developed into a separate question looking at ‘To what degree do the following affect your care plan’ with the addition of: ‘Insurance coverage’; ‘Patient accessibility to the office’; and ‘Other (specify)’; and 4) a section on ‘Reporting and Learning System Barriers’, based on questions adapted from Benn et al. (2009)23 was added. A brief description of the dimensions of the survey as well as the modifications made to the AHRQ medical office survey can be found in Table 2. The full modified survey is available from the authors upon request.
Data on patient safety culture dimensions were analyzed in two ways using Stata13 Software (StataCorp. 2013)
and Excel 2013. First, a positive percentage composite score was calculated for each dimension by averaging the percent positive responses on the questions within each dimension. For negatively worded questions, disagreeing was considered a positive response. Second, survey dimensions’ scores were calculated based on the mean response to the five-point scale and its 95% confidence interval (CI). Pearson chi-square test was used to compare the scores from SMT providers with the AHRQ medical offices comparative database, with level of significance
Chiropractors who participated in the focus group (n=24 of 63) stated that the survey was lengthy, but the information obtained would be valuable. They also felt that some questions would be better in different locations to promote response, and that some required additional clarification. Consequently, the following survey items were further modified: 1) the more sensitive section (i.e., List of Patient Safety and Quality Issues) was moved towards the end of the survey; 2) definitions were added to help clarify terminology differences amongst SMT professions (e.g., manual therapy, manipulation, adjustments); 3) modifications were made for each profession, reflecting the language/culture of each responding group (e.g., “office” versus “clinic”); and 4) the title of the survey was changed to ‘Survey to Support Quality Improvement’, to add clarity for the survey’s purpose.
CMCC Research Report 2018–2020 42 J Can Chiropr Assoc 2018; 62(3) 133
Table 1.
Setting / Location Population Studied (sample size) Survey Items and Dimensions / Factors
Table 1 Surveys identified during the literature review that evaluate patient safety attitudes and opinions in ambulatory settings.
These actions resulted in two versions of the ‘Survey to Support Quality Improvement’, one for chiropractors and one for physiotherapists. Both surveys have 14 dimensions with seven derived directly from the AHRQ Medical Office Survey on Patient Safety Culture, six from the AHRQ Medical Office Survey with some modified questions, and one dimension unique for this survey added by the SafetyNET team (Table 2).
Survey Application and Comparison Participant Response
A total of 417 SMT providers volunteered to respond to the survey: 356 chiropractors and 61 physiotherapists. Surveys from 120 chiropractors and 21 physiotherapists were excluded due to missing responses to questions (no complete section). We included 276 surveys, with complete data from 236 chiropractors (85.5%) and 40 physiotherapists (14.5%).
Respondent and Patient Characteristics
Table 3 provides a summary of demographic characteristics of respondents. Respondents were predominantly male (72.1%), providing treatment for an average of 31.6 hours per week, and treating less than 100 patients per week.
Patient Safety Culture Dimensions
In Figure 1, composite scores are contrasted with the AHRQ 2016 comparative database. With the exception of Patient Care Tracking/Follow-up scores, all other scores were greater than the AHRQ database. Specifically, Work Pressure and Pace, Office Processes and Standardization, and Overall Perception of Patient Safety – Clinical scored statistically significantly higher than the AHRQ database.
Factors Inhibiting Participation in a Reporting and Learning System
Perceived barriers to participation in a patient safety reporting and learning system are summarized in Table 4. Time pressure was identified as the biggest limitation, with patient concerns (i.e., perceived inconvenience for the patients and potential to create negative perception in patients) being the next most frequently reported limitation. A modest level of concern was reported regarding potential regulatory and legal implications. Most (57%) reported the fear of blame was not a barrier to reporting potential AEs.
Patient Safety Items and Quality Issues/Information Exchange with Other Settings
In comparison to the AHRQ database, SMT providers who responded to the survey had higher scores in most other items (Table 5). The SMT providers scored statistically significantly lower than medical offices in items related to medication list being updated and abnormal lab or imaging test not being followed up within one business day. Scores related to the use of the wrong patient chart, a chart not being available, clinical information filed into the wrong chart, and equipment not
working properly were similar to scores in the AHRQ medical office 2016 database (< 5% difference).
Respondents described the greatest difficulty in exchanging information with other healthcare clinics. While information exchange with outside labs/imaging centers was comparable, information exchange difficulty with other physician clinics was statistically significantly higher than the AHRQ medical office 2016.
Overall Clinic Self-Ratings
In Table 6, overall clinic self-ratings dimensions for respondents were found to be statistically significantly higher than the AHRQ medical office 2016 database; however, the overall clinic rating was comparable. Items that affect a patient’s care plan were found to be equally distributed for items measured. Other items that were described as affecting the patient’s specifically designed care plan were: patient’s desire to follow care plan, patient’s expectations, and patient’s level of discomfort.
Discussion Survey Development
As expected, our literature review did not retrieve a specific instrument developed for SMT providers, but it identified an existing validated survey used for other healthcare professions did meet our criteria. The selected survey tool, AHRQ’s Medical Office Survey on Patient Safety Culture was adapted and minimally modified for SMT providers, allowing comparison of 14 patient safety dimensions with AHRQ medical office 2016 database.
A previous review of several patient safety surveys, including the AHRQ Medical Office Survey on Patient Safety, concluded that survey results should be interpreted with caution as there was no established link with improved patient outcomes.24 However, another recent systematic review reported a trend demonstrating a positive relationship between patient safety culture and patient outcomes in hospital settings but this was not statistically significant.25 In high-risk industries, an open constructive safety environment was found to lead to high employee safety compliance and better organizational performance.26 The need to understand patient safety attitudes and opinions through the use of cross-sectional surveys may help researchers, patient safety personnel, and administrators identify areas of strengths and those in need of improvement with an aim to increasing positive patient outcomes and reducing medical error, despite the lack of current evidence for this result.
Survey Application
We present the first study to measure community-based SMT providers’ patient safety attitudes and opinions. The patient safety dimension of ‘work pressure & pace’ scored greater than the AHRQ comparative data base, indicating
A selection of published research by CMCC faculty 43 Funabashi et al
Table 2 AHRQ’s survey dimensions and description, reliability measures, and modifications made for the SafetyNET survey.
Table 2. AHRQ’s survey dimensions and description, reliability measures, and modifications made for the SafetyNET survey.
Information Exchange with Other settings
Teamwork
Work Pressure and Pace
Staff Training
Office Processes and Standardization
How often the office had problems exchanging accurate, complete, and timely information with other entities.
The extent to which the office has a culture of teamwork, mutual respect, and close working relationships among staff and providers.
The extent to which there are enough staff and providers to handle the patient load, and the office work pace is not hectic. 40.76No
30.80No
Communication About Error
Owner / Managing Partner / Leadership Support for Patient Safety
Organizational Learning
Overall Perceptions of Patient Safety and Quality
Overall Ratings on Quality and Patient Safety
Factors inhibiting participation in a reporting and learning system
The extent to which the office is organized, has an effective workflow, has standardized processes for completing tasks, and has good procedures for checking the accuracy of work performed.
The extent to which providers in the office are open to staff ideas about how to improve office processes, and staff are encouraged to express alternative viewpoints and do not find it difficult to voice disagreement.
The extent to which the office reminds patients about appointments, documents how well patients follow treatment plans, follows up with patients who need monitoring, and follows up when reports from an outside provider are not received.
The extent to which providers and staff are: 1) willing to report mistakes they observe and do not feel like their mistakes are held against them, and 2) talk openly about office problems and how to prevent errors from happening.
The extent to which office leadership actively supports quality and patient safety, places a high priority on improving patient care processes, does not overlook mistakes, and makes decisions based on what is best for patients.
The extent to which the office has a learning culture that facilitates making changes in office processes to improve the quality of patient care and evaluates changes for effectiveness.
The extent to which the quality of patient care is more important than getting more work done, office processes are good at preventing mistakes, and mistakes do not happen more than they should.
Overall rating of care, systems and clinical processes the office has in place to prevent, catch, and correct problems that have the potential to affect patients.
Not part of AHRQ.
{Adapted from Benn et al.24}
AHRQ – Agency for Healthcare Research and Quality
40.77No Changes
40.81No Changes
40.78No Changes
40.75No Changes
40.76No Changes
60.82Separated each question into administrative / clinical parts.
80.79Separated each question into administrative / clinical parts.
90.87 Separated ‘patient’s socioeconomic status’, ‘insurance coverage’, ‘patient accessibility to the office’, and ‘other’ into individual categories.
9NANot part of AHRQ.
{Adapted from Benn et al.24}
CMCC Research Report 2018–2020 44 J Can Chiropr Assoc 2018; 62(3) 135
18 # of items AHRQ Cronbach’s alpha SafetyNet modifications List of Patient Safety and Quality Issues
in clinical
that affect patient safety and quality of care. 80.86Removed ‘A pharmacy contracted our office to clarify or correct a prescription.’
Dimensions Dimension brief description
Issues that can happen
offices
Removed ‘Pharmacies’ and ‘Hospitals’. Added ‘Other healthcare offices’ and ‘Insurance / Third Party Payers?’
40.90
40.83No Changes
Changes
The extent to which the office gives providers and staff effective onthe-job training, trains them on new processes, and does not assign tasks they have not been trained to perform. Changes
Communication Openness
Patient Care Tracking / Follow-up
Respondent and Patient Characteristics
that respondents often felt rushed and that they may have too many patients for the amount of time available. This was also observed in medical offices regardless of the job position27, indicating the need for processes and systems to accommodate the busy work-load and to reduce potential staff burnout27
Table 3 provides a summary of demographic characteristics of respondents. Respondents were predominantly male (72.1%), providing treatment for an average of 31.6 hours per week, and treating less than 100 patients per week.
Patient Safety Culture Dimensions
Similar to other healthcare professions, this survey found that ‘time pressure and lack of clear reportable incident definitions’ were the largest concern of SMT providers in participating in a reporting system.23,28 Time pressure was an expected finding, as healthcare providers often have competing demands for their time and perceive themselves as “too busy” to report incidents5,28,29, emphasizing the importance of ‘ease of use’ when developing an evaluation system. Although “busyness” is a socially acceptable excuse for non-participation in incident
In Figure 1, composite scores are contrasted with the AHRQ 2016 comparative database. With the exception of Patient Care Tracking/Follow-up scores, all other scores were greater than the AHRQ database. Specifically, Work
Providers opinions on factors that may inhibit participation in a reporting and learning system.
Pressure and Pace, Office Processes and Standardization, and Overall Perception of Patient Safety – Clinical scored statistically significantly higher than the AHRQ database.
reporting systems, patient safety is one of the most prominent healthcare challenges and improving health care is a shared responsibility that must include health care providers, researchers and patients to be successful.1
Factors Inhibiting Participation in a Reporting and Learning System
‘Lack of a clear definition for reportable incident’ has been identified in previous studies among chiropractors and other professionals utilizing SMT.5,28,30 More specifically, a qualitative study with SMT providers observed that not only was defining AEs following SMT challenging, but also that the perceived difficulty of tracking these events would exceed the benefits of having the reported information.31 Similar to our survey findings, a systematic review focusing on clinical incident reporting suggested having a standardized definition of an AE, along with clearly described reporting methods, including mechanism, anonymity, accessibility, and ease of input.32 To address these
Perceived barriers to participation in a patient safety reporting and learning system are summarized in Table 4. Time pressure was identified as the biggest limitation, with patient concerns (i.e., perceived inconvenience for the patients and potential to create negative perception in patients) being the next most frequently reported limita-
A selection of published research by CMCC faculty 45 136 J Can Chiropr Assoc 2018; 62(3)
Demographic and background characteristics of responding SMT providers. (n=276) Provider Characteristics SMT Providers Gender, Female, n (%) 77 (27.9%) Years in practice, Mean (range) 19.4 (1-53) Hours worked in a typical week, Mean (range)31.6 (4-55) Average number (range) of personnel working in the clinic Other health care provider 3.1 (1-10) Therapy Assistant 2.7 (1-10) Other employee/ staff 2.4 (1-6) Patient visits per week, n (%) < 50 45 (16%) 50-99 74 (26.8%) 100-149 44 (15.9%) 150-199 25 (9%) Highest level of non-physiotherapy / non-chiropractic degree, n (%) Bachelor ’s degree 148 (53.6%) Master ’s degree 13 ( 4.7%) Academic Doctoral degree 8 ( 2.9%) Other 14 ( 5 %) Province of practice, n (%) Newfoundland and Labrador 31 (11.2%) New Brunswick 15 ( 5.4%) Ontario 190 (68.8%) Alberta 40 (14.5%)
Table 3.
Table 4.
Factors inhibiting RLS participation Not at all Yes, a little Yes, a lot Patient Concerns Perceived inconvenience for the patients 22%51%27% Potential to create negative perception in patients 26%49%25% Office Concerns Time pressure 11% 42%46% Lack of clear definitions as to what constitutes a reportable incident 32%55%14% Resource constraints 65%28% 7% Big Picture Concerns Regulatory implications 41%42%17% Legal implications 36%47%17% Fear of blame 57%38% 5% Believe reporting is unnecessary 65%32% 3% RLS – Reporting and Learning System
Table 3 Demographic and background characteristics of responding SMT providers. (n=276)
Funabashi et al
Table 4 Providers opinions on factors that may inhibit participation in a reporting and learning system.
Fig1ThepositivecompositescoresfromthepatientsafetydimensionsarepresentedforSMTproviderswhorespondedtothesurveyandthe2016AHRQcomparative database.Asterisksindicatedimensionsthatthepercentageofpositivecompositescoresfor“stronglyagree/agree”responsesfromSMTprovidersweresignificantlydifferent thantheonesfromthe2016AHRQmedicalofficescomparativedatabase.
The positive composite scores from the patient safety dimensions are presented for SMT providers who responded to the survey and the 2016 AHRQ comparative database. Asterisks indicate dimensions that the percentage of positive composite scores for “strongly agree/agree” responses from SMT providers were significantly different than the ones from the 2016 AHRQ medical offices comparative database.
tion. A modest level of concern was reported regarding potential regulatory and legal implications. Most (57%) reported the fear of blame was not a barrier to reporting potential AEs.
perceived challenges, the SafetyNET team adapted an AE definition based on the patient safety scientific literature and their content team experts to “any unfavorable sign, symptom, or disease temporally associated with the treatment, whether or not caused by the treatment”33. Regarding the incident reporting mechanism, the SafetyNET team has also developed and validated profession-specific instruments to track and evaluate potential AEs related to SMT in a systematic yet in a timeefficient manner.34 Provider feedback from a larger study using these instruments (personal communication) suggest that both providers and patients find these instruments easy and quick to use .34
Patient Safety Items and Quality Issues/Information Exchange with Other Settings
In comparison to the AHRQ database, SMT providers who responded to the survey had higher scores in most
other items (Table 5). The SMT providers scored statistically significantly lower than medical offices in items related to medication list being updated and abnormal lab or imaging test not being followed up within one business day. Scores related to the use of the wrong patient chart, a chart not being available, clinical information filed into the wrong chart, and equipment not working properly were similar to scores in the AHRQ medical office 2016 database (< 5% difference).
We found that providers perceived that ‘potential patient concerns’ were an important barrier to participation in a reporting system. Previous studies, however, suggest this concern is not shared by patients.10,34 Patients who have participated in a SafetyNET’s pilot reporting system stated that they were pleased their provider was participating in a study directly assessing patient safety.34 Additionally, Huerta and colleagues (2016)35 observed that not only can patients provide unique input on safety and care, but by reporting events related to safety, they are more engaged in their care.
Regarding direct patient safety items, our study found that respondents scored the item ‘updating a patient’s medication
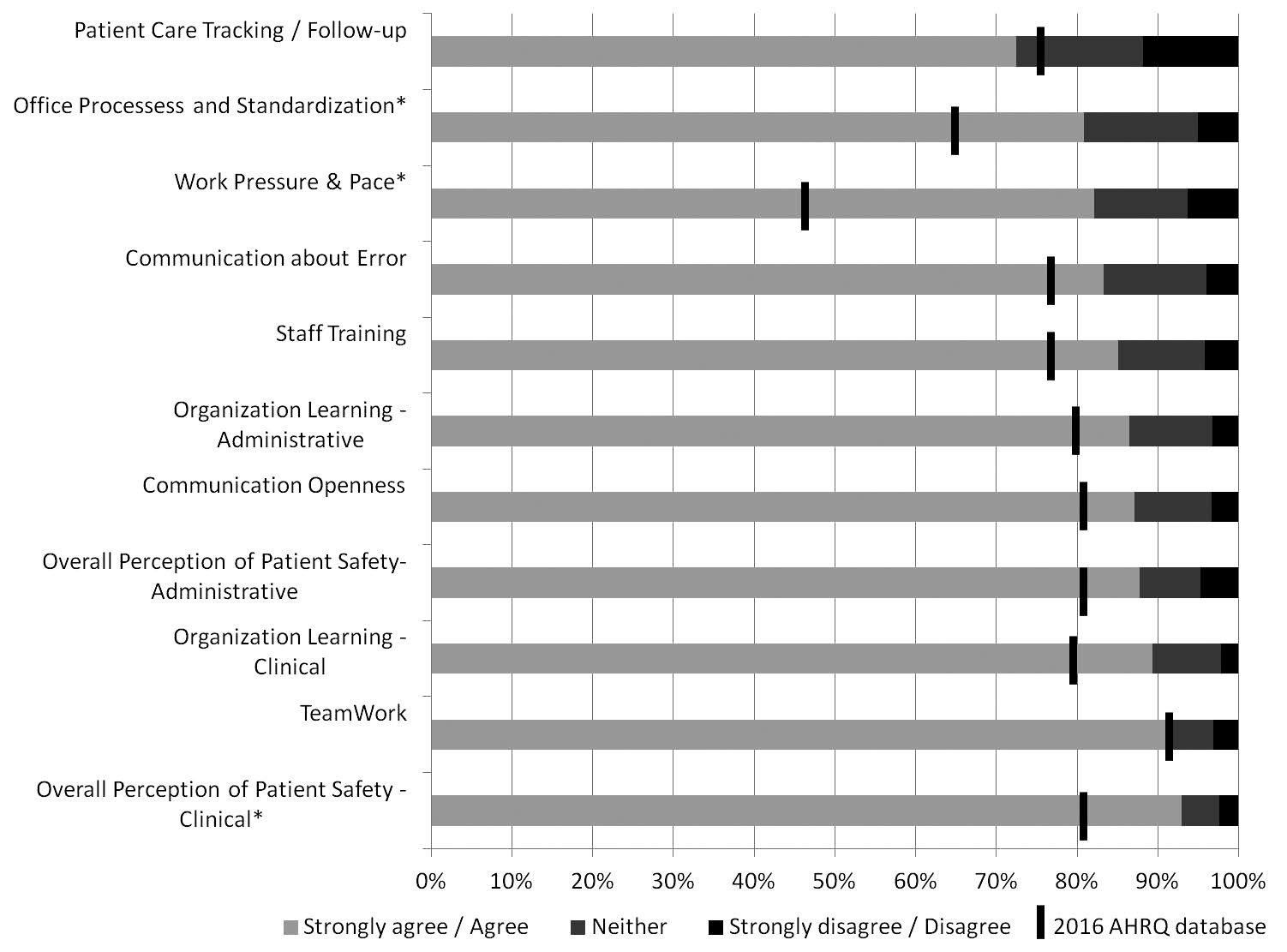
CMCC Research Report 2018–2020 46 J Can Chiropr Assoc 2018; 62(3) 137
Figure 1.
average percent positive response by number of providers. A desirable outcome corresponds to a high percentage value, which represented less frequency of occurrence.
list’ lower than medical offices.19 Although prescribing medications is typically not within the scope of the SMT providers, seeking information about a patient’s medication list provides healthcare professionals with important information regarding the patient’s current health status.36,37 Thus, not only do changes in a patient’s medication list indicate a change in the patient’s health condition38, but some medications may pose specific risks for SMT treatment, such as increased risk of bleeding39. Therefore, adequate pharmacological training and continued professional development to recognize the importance of asking about patient medication use at every visit could potentially increase patient safety within health care providers’ clinics/offices.
Respondents described the greatest difficulty in exchanging information with other healthcare clinics. While information exchange with outside labs/imaging centers was comparable, information exchange difficulty with other physician clinics was statistically significantly higher than the AHRQ medical office 2016.
Overall Clinic Self-Ratings
In Table 6, overall clinic self-ratings dimensions for respondents were found to be statistically significantly higher than the AHRQ medical office 2016 database; however, the overall clinic rating was comparable. Items that affect a patient’s care plan were found to be equally distributed for items measured. Other items that were described as affecting the patient’s specifically designed care plan were: patient’s desire to follow care plan, patient’s expectations, and patient’s level of discomfort.
The development and application of the survey described in this study is an important step towards creating a paradigm-shift in SMT providers regarding patient safety research and initiatives. Understanding the opinions and attitudes of SMT providers towards patient safety and identifying potential areas for improvement can lead to specific strategies and interventions to promote a constructive patient safety culture and support the development of effective systems for continuous learning and quality improvement. Although patient safety strategies and initiatives are currently being developed to promote a safety culture and address specific areas, future investigations are
Discussion
needed to assess the feasibility of these strategies’ and their impact on patient outcomes.
Survey Development
Limitations
Survey Development
Results from the pilot study conducted with the developed Survey to Support Quality Improvement suggest that a limitation of this instrument is its length. A lengthy survey is likely to lower the response rate, especially for items positioned at the end of the survey, and may lead to an increased chance for nonresponse bias.40
Survey Application
Given that the results presented in this study include responses from 276 SMT providers, the results from this study should be interpreted with caution as it only reflects the attitudes and opinions of SMT providers who responded to our survey.
As expected, our literature review did not retrieve a specific instrument developed for SMT providers, but it identified an existing validated survey used for other healthcare professions did meet our criteria. The selected survey tool, AHRQ’s Medical Office Survey on Patient Safety Culture was adapted and minimally modified for SMT providers, allowing comparison of 14 patient safety dimensions with AHRQ medical office 2016 database. A previous review of several patient safety surveys, including the AHRQ Medical Office Survey on Patient Safety, concluded that survey results should be interpreted with caution as there was no established link with improved patient outcomes.24 However, another recent systematic review reported a trend demonstrating a positive relationship between patient safety culture and patient
Another limitation of our work is the comparator group. Although Canadian SMT providers’ patient safety attitudes and opinions were investigated in the current study, an American database from medical offices (from AHRQ) was used for comparison as a Canadian patient safety database is not available. Therefore, potential cultural differences should also be considered as a potential limitation when interpreting our results.
A selection of published research by CMCC faculty 47 Funabashi et al 138 J Can Chiropr Assoc 2018; 62(3)
Composite-level
Dimension Composite Mean % AHRQ –2016 Patient safety items and quality issue Access to care:
89%90% Patient identification: The wrong
95%97% Charts/Records: A patient’s chart/record was not available when needed 91%90% Charts/Records: Clinical information was filed, scanned, or entered into the wrong patient’s chart/record 94%89% Equipment: Equipment was not working properly or was in need of repair or replacement 95%92% Medication: A patient’s medication list was not updated during his or her visit. 56%* 80% Diagnostics Test: Results from a lab or imaging test were not available when needed 82%* 70% Diagnostics Test: Critical abnormal result from a lab or imaging test was not followed up within 1 business day 66%* 94% Difficulty with Information Exchange with Other Setting Outside labs / imaging centers 91%82% Other physician clinics (AHRQ: Other medical offices / outside physicians) 89%* 77% Other healthcare clinic 92%NA Insurance / Third Party Payers 70%NA Other (i.e. Worker’s Compensation Board, employers of patients, schools) 76%NA AHRQ 2016 – 2016 Agency for Healthcare Research and Quality medical offices comparative database * – Significantly different than 2016 AHRQ database scores
Table 5.
A patient was unable to get an appointment within 48 hours for an acute/serious problem.
chart/record was used for a patient.
Table 5 Composite-level average percent positive response by number of providers. A desirable outcome corresponds to a high percentage value, which represented less frequency of occurrence.
Table 6 Providers’ perception of overall clinic self-rating.
*– Significantly different than 2016 AHRQ database for the same scores How
AHRQ – Agency for Healthcare Research and Quality
AHRQ 2016 – 2016 AHRQ medical offices comparative database
Conclusions
outcomes in hospital settings but this was not statistically significant.25 In high-risk industries, an open constructive safety environment was found to lead to high employee safety compliance and better organizational performance.26 The need to understand patient safety attitudes and opinions through the use of cross-sectional surveys may help researchers, patient safety personnel, and administrators identify areas of strengths and those in need of improvement with an aim to increasing positive patient outcomes and reducing medical error, despite the lack of current evidence for this result.
Survey Application
This study identified, adapted, and conducted content validation for the SafetyNET’s Survey to Support Quality Improvement to measure the patient safety culture of SMT providers, specifically chiropractors and physiotherapists. The survey measures the perceptions of their attitudes and opinions toward patient safety and quality improvement items and is the first study of its kind conducted in Canada. Generally, SMT providers had similar or better patient safety dimension scores compared to the AHRQ 2016 medical offices database. By understanding SMT providers’ opinions and attitudes towards patient safety and identifying areas for improvement, organization-specific strategies can be developed to support a culture of patient safety and promote quality improvement.
Acknowledgements
We present the first study to measure community-based SMT providers’ patient safety attitudes and opinions. The patient safety dimension of ‘work pressure & pace’ scored greater than the AHRQ comparative data base, indicating that respondents often felt rushed and that they may have
The work was done as part of a team grant; the authors would like to thank their team members, Dr. Michael D. Hill and Dr. Jerome Yager for their insightful comments and suggestions to improve the work. This study was supported by funding from the Canadian Institutes of Health Research (CIHR # TIR-112758), Alberta References Innovates—Health Solutions (AIHS # 20111389), and the generosity of the Stollery Children’s Hospital
too many patients for the amount of time available. This was also observed in medical offices regardless of the job position27, indicating the need for processes and systems to accommodate the busy work-load and to reduce potential staff burnout27.
Foundation and supporters of the Lois Hole Hospital for Women through the Women and Children’s Health Research Institute (WCHRI # RES0013182).
References
1. Brasaite I, Lecturer RNP, Kaunonen M, Suominen T. Healthcare professionals ’ knowledge, attitudes and skills regarding patient safety: a systematic literature review. Scand J Caring Sci. 2015;29(1):30–51.
2. Kohn L, Corrigan J, Donaldson M. To err is human: building a safer health system. Washington DC: National Academy Press; 2000.
Similar to other healthcare professions, this survey found that ‘time pressure and lack of clear reportable incident definitions’ were the largest concern of SMT providers in participating in a reporting system.23,28 Time pressure was an expected finding, as healthcare providers often have competing demands for their time and perceive themselves as “too busy” to report incidents5,28,29 , emphasizing the importance of ‘ease of use’ when developing an evaluation system. Although “busyness” is a socially acceptable excuse for non-participation in incident reporting systems, patient safety is one of the most prominent healthcare challenges and improving health care is a shared responsibility that must include health
3. Wade J (Chair). Building a Safer System: A National Integrated Strategy for Improving Patient Safety in Canadian Health Care. The National Steering Committee on Patient Safety 2002;59.
4. Patankar M, Brown J, Sabin E, Bigda-Peyton T. Safety
CMCC Research Report 2018–2020 48 J Can Chiropr Assoc 2018; 62(3) 139
Dimension PoorFairGoodVery Good Excellent Patient centered 0%2%12% 34%* 52%* AHRQ 2016 0%7%27%36%30% Timely 1%3%20% 41%* 35%* AHRQ 2016 7%13%31%35%15% Efficient 0%1%20% 43%* 36%* AHRQ 2016 3%9%26%45%18% Equitable Patient: gender, race, ethnicity, language, etc 0%0%5%34%*61%* AHRQ 2016: gender, race, ethnicity, socioeconomic status, language etc.1%5%15%27%52% Overall clinic rating to prevent, catch, and correct problems that have the potential to affect patients 1%5%27%46%21% AHRQ 2016 1%7%26%49%18%
Table 6. Providers’ perception of overall clinic self-rating.
do the following dimension affect patient’s specifically designed care plan? Never Rarely Sometimes Most of the time Always Socioeconomic status 22%22%40%10%5% Insurance coverage 32%20%33% 11% 4% Patient’s accessibility to clinic 26%28%34%9%3% Other 9% 9% 55%18%9%
Culture: building and sustaining a cultural change in aviation and healthcare. VT, USA: Ashgate Publisingh Limitied; 2012
5. Rozmovits L, Mior S, Boon H. Exploring approaches to patient safety: the case of spinal manipulation therapy. BMC Complement Altern Med. 2016;161–169.
6. Hebert JJ, Stomski NJ, French SD, Rubinstein SM. Serious adverse events and spinal manipulative therapy of the low back region: a systematic review of cases. J Manipulative Physiol Ther. 2015;38(9):677–691.
7. Canadian Chiropractic Association. https://www. chiropractic.ca/media-centre/quick-facts/.
8. Weeks WB, Goertz CM, Meeker WC, Marchiori DM. Public perceptions of doctors of chiropractic: results of a national survey and examination of variation according to respondents’ likelihood to use chiropractic, experience with chiropractic, and chiropractic supply in local health care markets. J Manipulative Physiol Ther. 2015;38(8):533–544.
9. Christensen M, Hyland J, Goertz C, Kollasch M. Practice Analysis of Chiropractic 2015: A project report, survey analysis, and summary of chiropractic practice in the United States.
10. Vohra S, Kawchuk GN, Boon H, Caulfield T, Pohlman KA, Beirne MO. SafetyNET: An interdisciplinary research program to support a safety culture for spinal manipulation therapy. Eur J Integr Med. 2014;6(4):473–477.
11. Rubinstein SM. Adverse events following chiropractic care for subjects with neck or low-back pain: do the benefits outweigh the risks? J Manipulative Physiol Ther. 2008;31(6):461–464.
12. Assendelft WJJ, Bouter L, Knipschild P. Complications of spinal manipulation. J Fam Pract. 1996;42(5):475–80.
13. Vohra S, Johnston BC, Cramer K, Humphreys K. Adverse events associated with pediatric spinal manipulation: a systematic review. Pediatrics. 2007;119(1):e275–e283.
14. Tuchin P. A replication of the study ‘Adverse effects of spinal manipulation: a systematic review.’ Chiropr Man Therap. 2012;20(1):30.
15. Thiel H. Incident reporting and learning systems for chiropractors – Developments in Europe. J Can Chiropr Assoc. 2011;55(3):155–158.
16. Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, Bouter LM, de Vet HC. The COSMIN checklist
for evaluating the methodological quality of studies on measurement properties: A clarification of its content. BMC Med Res Methodol. 2010;10(1):22.
17. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) –A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
18. Sorra J, Gray L, Famolaro T, Al E. AHRQ Medical Office Survey on Patient Safety Culture: User’s Guide. 2016.
19. Famolaro T, Yount N, Hare R, Thornton S, Sorra J. Medical Office Survey on Patient Safety Culture 2016 User Comparative Database Report. (Prepared by Westat, Rockville, MD, under Contract No. HHSA 290201300003C). Rockville, MD: Agency for Healthcare Research and Quality, AHRQ Publication No. 16-0028-EF.;
20. Modak I, Sexton JB, Lux TR, Helmreich RL, Thomas EJ. Measuring safety culture in the ambulatory setting: The safety attitudes questionnaire – Ambulatory version. J Gen Intern Med. 2007;22(1):1–5.
21. Hoffmann B, Domanska OM, Albay Z, Mueller V, Guethlin C, Thomas EJ, Gerlach FM. The Frankfurt Patient Safety Climate Questionnaire for General Practices (FraSiK): analysis of psychometric properties. BMJ Qual Saf. 2011;20(9):797–805.
22. de Wet C, Spence W, Mash R, Johnson P, Bowie P. The development and psychometric evaluation of a safety climate measure for primary care. BMJ Qual Saf. 2010;19(6):578–584.
23. Benn J, Koutantji M, Wallace L, Spurgeon P, Rejman M, Healey A, Vincent C. Feedback from incident reporting: information and action to improve patient safety. Qual Saf Heal Care. 2009;18(1):11–21.
24. Colla J, Bracken A, Kinney L, Weeks W. Measuring patient safety climate: a review of surveys. BMJ Qual Saf. 2005;14364–366.
25. DiCuccio MH. The relationship between patient safety culture and patient outcomes: a systematic review. J Patient Saf. 2015;11(3):135–142.
26. Clarke S. The relationship between safety climate and safety performance: a meta-analytic review. J Occup Health Psychol. 2006;11(4):315–327.
27. Hickner J, Smith SA, Yount N, Sorra J. Differing perceptions of safety culture across job roles in the ambulatory setting:
A selection of published research by CMCC faculty 49 Funabashi et al
analysis of the AHRQ Medical Office Survey on Patient Safety Culture. BMJ Qual Saf. 2016;25(8):588–594.
28. Gunn SJ, Thiel HW, Bolton JE. British Chiropractic Association members ’ attitudes towards the Chiropractic Reporting and Learning System: a qualitative study. Clin Chiropr. 2008;1163–69.
29. Cvijovic K, Boon H, Jaeger W, Vohra S. Pharmacists’ participation in research: A case of trying to find the time. Int J Pharm Pract. 2010;18(6):377–383.
30. Thiel H, Bolton J. The reporting of patient safety incidents –first experiences with the chiropractic reporting and learning system (CRLS): A pilot study. Clin Chiropr. 2006;9(3):139–149.
31. Winterbottom M, Boon H, Mior S, Facey M. Informed consent for chiropractic care: Comparing patients’ perceptions to the legal perspective. Man Ther. 2015;20(3):463–468.
32. Parmelli E, Flodgren G, Fraser SG, Williams N, Rubin G, Eccles MP. Interventions to increase clinical incident reporting in health care. Cochrane Database Syst Rev. 2012;(8):1–23.
33. World HO. WHO Draft Guidelines for Adverse Event Reporting and Learning Systems. World Alliance for Patient Safety 2005;1–75.
34. Pohlman KA, Beirne MO, Thiel H, Cassidy JD, Mior S, Hurwitz EL, Westaway M, Ishaque S, Yager J, Vohra S. Development and validation of providers’ and patients’ measurement instruments to evaluate adverse events after spinal manipulation therapy. Eur J Integr Med. 2014;6(4):451–466.
35. Huerta TR, Walker C, Murray KR, Hefner JL, Mcalearney AS, Moffatt-bruce S. Patient safety errors: leveraging health information technology to facilitate patient reporting. J Healthc Qual. 2016;38(1):17–23.
36. Marek K, Antle L. Medication Management of the Community-Dwelling Older Adult. In: Hughes R, Ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008.
37. Sullivan G, Lansbury G. Physiotherapists’ knowledge of their clients’ medications: A survey of practising physiotherapists in New South Wales, Australia. Physiother Theory Pract. 1999;15(3):191–198.
38. Wright A, Pang J, Feblowitz JC, Maloney FL, Wilcox AR, Ramelson HZ, Schneider LI, Bates DW, Wright A. A method
and knowledge base for automated inference of patient problems from structured data in an electronic medical record. J Am Med Informatics Assoc. 2011;18859–18867.
39. Spyropoulos AC, Bauersachs RM, Omran H, Cohen M. Periprocedural bridging therapy in patients receiving chronic oral anticoagulation therapy. Curr Med Res Opin. 2006;22(6):1109–1122.
40. K B. The effect of questionnaire length on response rate – A review of the literature. In: ASSOCIATION PSOSRMAS, Ed. American Statistical Association: 1996 proceedings of the Section on Survey Research Methods. Salt Lake City, UT: ASA, 1996; 1996. p 1020–1025.
OriginallypublishedintheJournaloftheCanadianChiropractic Association2018Dec;62(3):130-142.
Reproducedwithpermission.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6319430/
CMCC Research Report 2018–2020 50
Spinal Manipulation Therapy Improves Tactile Allodynia and Peripheral Nerve Functionality and Modulates Blood
Oxidative Stress Markers in Rats Exposed to Knee-Joint Immobilization
Abstract
Objectives:
The purpose of our study was to evaluate the effect of manually assisted lumbar spinal manipulation therapy on tactile allodynia, peripheral nerve functional recovery, and oxidative markers in rats exposed to knee immobilization-inducing hypersensitivity.
Methods:
Tactile allodynia and sciatic, tibial, and peroneal functional indices were assessed before the knee joint immobilization, 24 hours after the knee cast removal, and 24 hours after 3 weeks of lumbar therapy with the Activator Adjusting Instrument, model 4 (AAI 4). Subsequently, the blood was collected from each rat, and oxidative markers such as lipid hydroperoxide levels; nitric oxide metabolites; and superoxide dismutase, catalase, and glutathione peroxidase activities were assessed.
Results:
The AAI 4 improved the immobilization-induced allodynia and recovered the peripheral nerve functional indices impaired after knee immobilization. Immobilized rats treated with AAI 4 therapy presented a lack of significant changes in lipid hydroperoxides and nitric oxide metabolites in the plasma contrasting with rats that were kept freely in their cages, with no therapy applied, which presented elevated lipid hydroperoxides levels. Also, the antioxidant catalase enzymatic activity decreased in the blood of rats immobilized and treated with AAI 4. Conclusion: These results suggest that manually assisted lumbar spinal manipulation therapy modulates systemic oxidative stress, which possibly contributes to the analgesia and recovery of peripheral nerve functionality.
(J Manipulative Physiol Ther 2019;42:385-398)
Key Indexing Terms: Manipulation, Spinal; Immobilization; Oxidative Stress; Hyperalgesia; Central Nervous System Sensitization
Introduction
Spinal manipulative therapy (SMT) is widely used to
manage and treat painful musculoskeletal conditions.1,2 Among nonpharmacologic treatments, SMT has shown good effectiveness to treat pain.2-4 However, the biological mechanisms associated with SMT remain unclear, and further studies are necessary to better understand the analgesic effect of SMT.
Chiropractors and other manual therapists who apply SMT commonly use high-velocity and low-amplitude SMT in their clinical routine. However, techniques involving the use of instruments (manually assisted spinal manipulation therapy [MASMT]) are also employed, such as the Activator Adjusting Instrument (AAI).3-5 This tool is a hand-operated and springloaded device designed for clinical practice that applies a high-speed thrust force in a specific line of drive.3-5 Importantly, it has determined analgesic effects comparable to SMT6,7 in patients with different painful etiologies during clinical practice and in experimentally pain-induced animal studies.8-10 Although investigation using AAI has risen in the last decade,8 the mechanisms behind its analgesic effects are still poorly understood, and further investigation in this field is demanded.
Previous studies have demonstrated that SMT modifies the activity of antioxidant enzymes such as catalase,2 superoxide dismutase (SOD), and glutathione peroxidase (GPx) in human blood.11 According to Poljsak et al,12 oxidative stress may be defined as an excessive amount of reactive oxygen species (ROS), which is the net result of an imbalance between production and destruction of these species. The ROS include singlet oxygen, superoxide radicals, hydroxyl radicals, and hydrogen peroxide (H2O2). There is also reactive nitrogen (nitric oxide [NO]–derived molecules), iron, copper, and sulfur species, which could contribute to increased ROS formation and oxidative stress and impair the redox balance.12 Diverse physiological enzymes such as SOD, catalase, and GPx are used to counterattack the ROS. The SOD converts the superoxide anion to H2O2, and catalase and GPx decompose H2O2 to water and oxygen.12-14 The ROS and NO play an essential role in the pathogenesis of pain, and the scavenging of these species appears to present an opportunity to normalize the oxidative status altered by pain.13-17
A selection of published research by CMCC faculty 51 Clinical and Health Services Research
Duarte FCK1,2,KolbergC2, Riffel AP2, Souza JA2, Bello-Klein A2, Partata WA2 1CanadianMemorialChiropracticCollege, 2FederalUniversityofRioGrandedoSul/UFRGS
Immobilization-inducing hypersensitivity has been used to study abnormal nociception and pain mediated by enhanced production of ROS and spinal sensitization.18 In addition, spinal motor neuron degeneration and electrophys-iological changes in the sciatic nerve have also been reported, suggesting that gait performance variability may occur after hind limb immobilization.19-24 Although the antinociceptive effect of the Activator Adjusting Instrument, model 4 (AAI 4), has successfully been reported when it was applied on the immobilization site in rats with hind limb immobilization,10 no studies have explored whether intervention with the AAI 4 on the lumbar spine leads to similar antinociceptive effects. Also, the mechanism of the AAI 4 leading to antinociceptive benefits in addition to its potential effect of improving walking gait performance have not been explored so far.
Thus, the primary purpose of this study was to investigate the causal relationship between the AAI 4 modulating mechanical nociception and free walking gait patterns in animals exposed to knee immobilization. To reveal the potential mechanism of the AAI 4, the secondary aim was to evaluate the effects of AAI 4 on pro-oxidative stress parameters such as lipid hydroperoxide levels and NO metabolites and on antioxidant enzyme SOD, catalase, and GPx activities.
We set out the hypothesis that the AAI 4 on segments L4L5 induces antinociceptive effect and better performance on free walking pattern in rats exposed to 4 weeks of knee immobilization. We also tested the hypothesis that the AAI 4 on segments L4-L5 modulates the ROS and activity of antioxidant enzymes in the blood of rats exposed to 4 weeks of knee immobilization.
These findings will have important implications to enhancing our understanding of the underlying mechanisms responsible for the clinical manifestation of analgesia and benefits on motor functionality seen during chiropractic therapy.
Methods
Experimental Procedures
Animals. All animal procedures were approved by the ethics committee of the Universidade Federal do Rio Grande do Sul (#21462). Thirty adult male Wistar rats, weighing 200 to 300 g, were provided by the Center for Reproduction and Experimentation of Laboratory Animals of the Universidade Federal do Rio Grande do Sul, and were divided into experimental groups described later. All rats were housed in the room with a stable temperature of 23oC±1oC and fed a regular pellet diet ad libitum
• Naive: Rats that did not undergo right knee joint immobilization for 4 weeks (n = 6).
• Naive-AAI 4: Rats that did not undergo right knee joint immobilization for 4 weeks and had the AAI 4 with adapter applied to the spinous process of L4-L5 for 3 weeks, 3 times/wk, used in force setting “1” (n = 6).
• Immobilization-AAI 4 (I-AAI 4): Rats that had their right knee joint immobilized for 4 weeks and had the AAI 4 with adapter applied to the spinous process of L4-L5 for 3 weeks, 3 times/wk, used in force setting “1” (n = 6).
• Immobilization-sham (I-sham): Rats that had their right knee joint immobilized for 4 weeks and had a lighter and gentler AAI 4 with adapter applied when compared with the I-AAI 4 group, to the spinous process of L4-L5 for 3 weeks, 3 times/wk (n = 6).
• Immobilization-remobilization free: Immobilizationremobilization free (I-RF) rats that had their right knee joint immobilized for 4 weeks and were kept freely in their cages for 3 weeks (n = 6) without application of the AAI 4.
For more details of the experimental groups, see Figure 1. The AAI 4 with the adapter was used as described by Duarte et al.25 Lumbar spinal segments were chosen as a therapeutic site to prevent the manipulation of the hind limb that had been immobilized. In addition, the lumbar spine is the location where most afferent fibers from neurosegmentally linked joints such as the hip, knee, and ankle enter.22
The AAI 4 was used in force setting “1,” because the adapter practically determines the maximum peak force value at force setting 1 of the AAI 4.25 The I-sham group aimed to discard any effects of the touch and audible “click” sound when the AAI 4 is triggered. Contrasting the naive-AAI4 and IIA4, the sham group had the AAI4 lightly touching the L4-L5 spinous processes. Since a preload is required to properly deliver the force of the AAI4 and consequently elicit its effects4 we intentionally did not perform preadjustment compression onto the target prior to firing the instrument in the sham group which substantially decreased the force delivered by AAI4.11
Immobilization Procedure
The knee joint immobilization procedure was performed as described by He and Dishman.24 After anesthesia (90 mg/kg of ketamine and 10 mg/kg of xylazine), the right knee joint was shaved, and 2 plastic glass splints (Fig 2A) were placed on the medial and lateral sides of the knee joint and then gently wrapped with adhesive plaster around the limb to restrain the movement of the joint. The right knee joint was immobilized in the extended position (150°). A plastic glass belt was attached surrounding the abdomen area to ensure rats would keep their hind paw apparatus (Fig 2B). After the knee immobilization, the foot skin color and movements of the foot, knee, and hip joints were checked daily by the same researcher. No immobilization casts were placed on the contralateral hind limb. After regaining consciousness, the rats returned to their cages and were maintained in the same conditions described earlier.
Mechanical Threshold
The mechanical threshold was assessed by electronic von Frey apparatus (Insight Equipamentos LTDA, Ribeirão Preto, SP,
CMCC Research Report 2018–2020 52
Fig1Aschematicdiagramshowstheexperimentalgroupsdesignatedinthisstudy.ThirtyadultmaleWistarrats,weighing200to300g,weredividedinto2maingroups,the naivegroupcontaining12Wistarratsandtheimmobilizationgroupcontaining18Wistarrats.Thenaivegrouporiginated2differentsubsets:naive,containing6Wistarrats, composedofratsthatdidnotundergotheimmobilizationandhadnoAAI4therapy;naive-AAI4,containing6Wistarrats,composedofratsthatdidnotundergoimmobilization buthadAAI4therapycarriedoutontheL4-L5spinousprocessfor3weeks3timesperweek,usedintheforcesetting“1.”Inaddition,theimmobilizationgrouporiginated3 differentsubsets:immobilization-AAI4(I-AAI4),containing6Wistarrats,composedofratsthatunderwentrightkneejointimmobilizationfor4weeksand,afteritsremoval, hadtheAAI4therapycarriedoutontheL4-L5spinousprocessfor3weeks,3timesperweek,usedintheforcesetting“1”;immobilization-sham(I-sham),containing6Wistar rats,composedofratsthatunderwentrightkneejointimmobilizationfor4weeksand,afteritsremoval,hadalighterandgentlerAAI-4therapyappliedontheL4-L5spinous processfor3weeks3timesperweek;andimmobilization-remobilizationfree(I-RF),containing6Wistarrats,composedofratsthatunderwentrightkneejointimmobilization for4weeksandaftercastremoval,werekeptfreelywithintheircagesfor3weeks.AAI4,ActivatorAdjustingInstrument,model4.
Fig1. Aschematicdiagramshowstheexperimentalgroupsdesignatedinthisstudy.ThirtyadultmaleWistarrats,weighing200to 300g,weredividedinto2maingroups,thenaivegroupcontaining12Wistarratsandtheimmobilizationgroupcontaining18Wistar rats.Thenaivegrouporiginated2differentsubsets:naive,containing6Wistarrats,composedofratsthatdidnotundergothe immobilizationandhadnoAAI4therapy;naive-AAI4,containing6Wistarrats,composedofratsthatdidnotundergoimmobilization buthadAAI4therapycarriedoutontheL4-L5spinousprocessfor3weeks3timesperweek,usedintheforcesetting “1.” Inaddition, theimmobilizationgrouporiginated3differentsubsets:immobilization-AAI4(I-AAI4),containing6Wistarrats,composedofratsthat underwentrightkneejointimmobilizationfor4weeksand,afteritsremoval,hadtheAAI4therapycarriedoutontheL4-L5spinous processfor3weeks,3timesperweek,usedintheforcesetting “1”;immobilization-sham(I-sham),containing6Wistarrats,composed ofratsthatunderwentrightkneejointimmobilizationfor4weeksand,afteritsremoval,hadalighterandgentlerAAI-4therapyapplied ontheL4-L5spinousprocessfor3weeks3timesperweek;andimmobilization-remobilizationfree(I-RF),containing6Wistarrats, composedofratsthatunderwentrightkneejointimmobilizationfor4weeksandaftercastremoval,werekeptfreelywithintheircages for3weeks. AAI4,ActivatorAdjustingInstrument,model4.
aimedtodiscardanyeffectsofthetouchandaudible “click” soundwhentheAAI4istriggered.ContrastingthenaiveAAI4andIIA4,theshamgrouphadtheAAI4lightlytouching theL4-L5spinousprocesses.Sinceapreloadisrequiredto properlydelivertheforceoftheAAI4andconsequentlyelicit itseffects 4 weintentionallydidnotperformpreadjustment compressionontothetargetpriortofiringtheinstrumentinthe shamgroupwhichsubstantiallydecreasedtheforcedelivered byAAI4. 11
Brazil) to evaluate nociceptive changes after immobilization or after the therapy. A positive response was indicated by an abrupt withdrawal of the paw, and the intensity of the stimuli that provoked the withdrawal response was automatically recorded (in grams). Only the ipsilateral hind paw was subjected to the von Frey test. A single trial consisted of 5 applications of the plastic tip, once every 0 to 30 seconds. The mean of 5 readings was taken as the threshold for a particular timing trial to each rat. This mean indicated the value of mechanical allodynia in that point.14
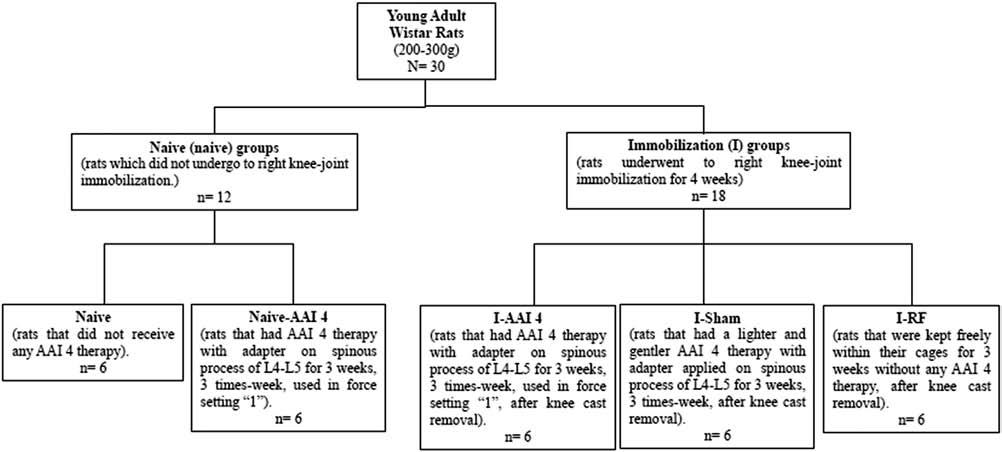
immobilizationcastswereplacedonthecontralateralhind limb.Afterregainingconsciousness,theratsreturnedtotheir cagesandweremaintainedinthesameconditionsdescribed earlier.
MechanicalThreshold
The mechanical threshold was assessed before the knee joint immobilization procedure (pre-immobilization value). After immobilization, the mechanical threshold was evaluated 24 hours after knee-joint cast removal and 24 hours after 3 weeks with AAI 4 application. This test was conducted at the same time of day (7:00 AM), by the same researcher, and in a room with a stable temperature of 23°C ± 1°C.
ImmobilizationProcedure
Sciatic, Peroneal, and Tibial Functional Indices
hind limb locomotor activity was monitored by analysis of the footprints after free walking gait analysis.27,28 Rat footprints were used to determine the following measurements: (1) distance from the heel to the third toe, the print length (PL); (2) distance from the first to the fifth toe, the toe spread (TS); and (3) distance from the second to the fourth toe, the intermediate toe spread (ITS). The 3 measurements were obtained from the experimental (E) and normal (N) sides. Several prints of each foot have been achieved on each track, but only 3 prints of each foot were used to determine the mean measurements on the experimental and normal sides. These means were included in the functional indices formulas.
Thekneejointimmobilizationprocedurewasperformedas describedbyHeandDishman. 24 Afteranesthesia(90mg/kgof ketamineand10mg/kgofxylazine),therightkneejointwas shaved,and2plasticglasssplints(Fig2A)wereplacedonthe medialandlateralsidesofthekneejointandthengently wrappedwithadhesiveplasteraroundthelimbtorestrainthe movementofthejoint.Therightkneejointwasimmobilizedin theextendedposition(150°).Aplasticglassbeltwasattached surroundingtheabdomenareatoensureratswouldkeeptheir hindpawapparatus(Fig2B).Afterthekneeimmobilization, thefootskincolorandmovementsofthefoot,knee,andhip jointswerecheckeddailybythesameresearcher.No
To estimate the functional sciatic, peroneal, and tibial nerve indices, a largely accepted method that determines nerve function abnormalities of innervated target organs postnerve injury was employed.26-28 Thus, the recovery of the right
Sciatic Functional Index = −38.3 (EPL–NPL)/NPL
+109.5 (ETS–NTS)/NTS
+13.3 (EIT–NIT)/NIT–8.8
Tibial Functional Index = −37.2(EPL–NPL)/NPL
Themechanicalthresholdwasassessedbyelectronicvon Freyapparatus(InsightEquipamentosLTDA,RibeirãoPreto, SP,Brazil)toevaluatenociceptivechangesafterimmobilizationorafterthetherapy.Apositiveresponsewasindicatedby anabruptwithdrawalofthepaw,andtheintensityofthestimuli thatprovokedthewithdrawalresponsewasautomatically recorded(ingrams).Onlytheipsilateralhindpawwas subjectedtothevonFreytest.Asingletrialconsistedof5 applicationsoftheplastictip,onceevery0to30seconds.The meanof5readingswastakenasthethresholdforaparticular timingtrialtoeachrat.Thismeanindicatedthevalueof mechanicalallodyniainthatpoint. 14
+104.4 (ETS–NTS)/NTS
+45.6 (EIT–NIT)/NIT–8.8
Peroneal Functional Index = −174.9 (EPL–NPL)/NPL
+80.3 (ETS–NTS)/NTS
Themechanicalthresholdwasassessedbeforetheknee jointimmobilizationprocedure(pre-immobilizationvalue). Afterimmobilization,themechanicalthresholdwasevaluated 24hoursafterknee-jointcastremovaland24hoursafter3 weekswithAAI4application.Thistestwasconductedatthe
+13.4
A selection of published research by CMCC faculty 53 Duarte et al
387 Duarteetal JournalofManipulativeandPhysiologicalTherapeutics MASMTImprovesAllodynia,NerveFunction,andROS Volume 42,Number6
sametimeofday(7:00 AM),bythesameresearcher,andina roomwithastabletemperatureof23°C±1°C.
Sciatic,Peroneal,andTibialFunctionalIndices
The resulting functional index was considered to be the index of the functional condition of the nerve, where 0 (±11) represents the normal function and -100 represents the complete loss of functionality.23,24,26 The functional indices were assessed before the knee joint immobilization procedure (pre-immobilization value), 24 hours after knee joint cast removal, and 24 hours after 3 weeks with AAI 4 application. The tests were conducted at the same time of the day (8:00 AM), by the same researcher, and in a room with a stable temperature of 23oC±1oC.
Blood Sample Preparation
Toestimatethefunctionalsciatic,peroneal,andtibialnerve indices,alargelyacceptedmethodthatdeterminesnerve functionabnormalitiesofinnervatedtargetorganspost-nerve injurywasemployed. 26-28 Thus,therecoveryoftherighthind limblocomotoractivitywasmonitoredbyanalysisofthe footprintsafterfreewalkinggaitanalysis. 27,28 Ratfootprints wereusedtodeterminethefollowingmeasurements:(1) distancefromtheheeltothethirdtoe,theprintlength(PL);(2) distancefromthefirsttothefifthtoe,thetoespread(TS);and (3)distancefromthesecondtothefourthtoe,theintermediate toespread(ITS).The3measurementswereobtainedfromthe experimental(E)andnormal(N)sides.Severalprintsofeach foothavebeenachievedoneachtrack,butonly3printsofeach footwereusedtodeterminethemeanmeasurementsonthe experimentalandnormalsides.Thesemeanswereincludedin thefunctionalindicesformulas.
thecompletelossoffunctionality. 23,24,26 Thefunctional indiceswereassessedbeforethekneejointimmobilization procedure(pre-immobilizationvalue),24hoursafterknee jointcastremoval,and24hoursafter3weekswithAAI4 application.Thetestswereconductedatthesametimeof theday(8:00 AM),bythesameresearcher,andinaroom withastabletemperatureof23 o C±1 o C.
BloodSamplePreparation
81% (vol/vol) of 90% methanol, 2 mmol/L of xylenol orange (o-Cresolsulfonphthalein-3’-3”-bis [methyliminodiacetic acid sodium salt]) to a final concentration of 100 µmol/L, 1 mol/L of sulfuric acid to a final concentration of 25 mmol/L, 40 mmol/L of 2,6-di-tert-butyl-4-methylphenol to a final concentration of 4 mmol/L, and 10 mmol/L of ferrous sulfate to a final concentration of 250 µmol. Samples were prediluted 1:10 in Milli-Q (Direct-Q3, Millipore SAS, Molsheim, France) water before the test. Then, they were divided into 2 tubes with 90 µL of the sample in each. The samples were incubated for 30 minutes with 10 µL of 90% methanol or 10 µL of 1 mmol/L TPP. After incubation, the samples were pipetted in duplicate in the microplate and incubated with working reagent (1:9) with stirring for 1 hour at room temperature. Absorbance at 560 nm was obtained with a Zenyth 200 spectrophotometer (Anthos, Salzburg, Austria), and the absorbance values of the duplicates obtained with TPP were subtracted from the values for the duplicates without TPP. Results are expressed in nanomoles of lipid hydroperoxides per milligram of protein.
SciaticFunctionalIndex ¼ 38 3EPL–NPL ðÞ=NPL
þ 109 5ETS–NTS ðÞ=NTS
þ 13 3EIT–NIT ðÞ=NIT–8 8
All rats were euthanized by decapitation and blood was promptly collected. For oxidative stress parameters analysis, the blood samples were centrifuged at 1000 g for 20 minutes in a refrigerated centrifuge (Sorvall RC-5B, Rotor SM-24, DuPont Instruments, Wilmington, Delaware). Plasma samples were aliquoted for later analysis of lipid hydroperoxides and NO metabolites and stored at -70°C. For analysis of lipid hydroperoxides, the plasma was diluted 1:1 (v/v) in butylated hydroxytoluene (90% in methanol) before being stored.29 Red blood cells (RBCs) were washed 3 times with cold 0.9-N phosphate-buffered saline. Aliquots of RBCs were stored at -70° C in 1 mM HCl and 4mM MgSO4 buffer diluted 50:500 (v/v) for later analyses of enzymatic antioxidant activity.29
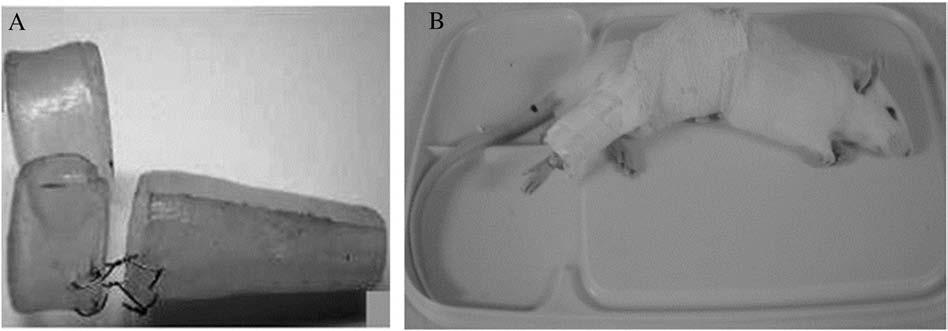
TibialFunctionalIndex ¼ 37:2EPL–NPL ðÞ=NPL
þ 104 4ETS–NTS ðÞ=NTS
Determination of Lipid Hydroperoxides
þ 45 6EIT–NIT ðÞ=NIT–8 8
PeronealFunctionalIndex ¼ 174 9EPL–NPL ðÞ=NPL
þ 80 3ETS–NTS ðÞ=NTS
þ 13:4
The method is based on oxidation of Fe2+ to Fe3+ in the presence of lipid hydroperoxides and formation of complexes of Fe3+ with xylenol orange.30 According to the technique adapted from Sodergren et al31 for each sample, a blank reduced with 10 mmol/L of triphenylphosphine (TPP) in absolute methanol was used.
At the time of the test, a working reagent was prepared with
Theresultingfunctionalindexwasconsideredtobe theindexofthefunctionalconditionofthenerve,where0 (±11)representsthenormalfunctionand-100represents
Determination of NO Metabolites
Allratswere euthanized bydecapitationandbloodwas promptlycollected.Foroxidativestressparametersanalysis,thebloodsampleswerecentrifugedat1000gfor20 minutesinarefrigeratedcentrifuge(SorvallRC-5B,Rotor SM-24,DuPontInstruments,Wilmington,Delaware). Plasmasampleswerealiquotedforlateranalysisoflipid hydroperoxidesandNOmetabolitesandstoredat-70°C. Foranalysisoflipidhydroperoxides,theplasmawas diluted1:1(v/v)inbutylatedhydroxytoluene(90%in methanol)beforebeingstored. 29 Redbloodcells(RBCs) werewashed3timeswithcold0.9-Nphosphate-buffered saline.AliquotsofRBCswerestoredat-70°Cin1mM HCland4mMMgSO4 bufferdiluted50:500(v/v)forlater analysesofenzymaticantioxidantactivity. 29
DeterminationofLipidHydroperoxides
ThemethodisbasedonoxidationofFe 2+ toFe 3+ inthe presenceoflipidhydroperoxidesandformationofcomplexesofFe 3+ withxylenolorange. 30 Accordingtothe techniqueadaptedfromSodergrenetal 31 foreachsample,a blankreducedwith10mmol/Loftriphenylphosphine (TPP)inabsolutemethanolwasused.
Atthetimeofthetest,aworkingreagentwasprepared with81%(vol/vol)of90%methanol,2mmol/Lofxylenol orange(o-Cresolsulfonphthalein-3′-3″-bis[methyliminodiaceticacidsodiumsalt])toafinalconcentrationof
Pure plasma samples without previous preparation or dilution were analyzed for NO metabolites.29 Nitrites were determined using the Griess reagent, to measure NO metabolites, in which a chromophore with a strong absorbance at 540 nm is formed by reaction of nitrite with a mixture of 0.1% naphthyl-ethylenediamine and 1%sulfanilamide. Nitrates were determined as total nitrites (initial nitrite plus nitrite reduced from nitrate) after their reduction using nitrate reductase from Aspergillus species in the presence of nicotinamide adenine dinucleotide phosphate. A standard curve was established with a set of serial dilutions (10-8 – 10-3 mol/L) of sodium nitrite. Absorbance at 540 nm was obtained with a Zenyth 200 spectrophotometer (Anthos). Results were expressed as millimoles of NO metabolites per liter.29
CMCC Research Report 2018–2020 54
388 JournalofManipulativeandPhysiologicalTherapeutics Duarteetal July/August2019 MASMTImprovesAllodynia,NerveFunction,andROS
Fig2. (A)Theplasticglasssplintsusedforthekneeimmobilization,and(B)aratwithkneejointimmobilizedandwrappedwith adhesiveplasteraroundtherighthindlimb.
Fig2(A)Theplasticglasssplintsusedforthekneeimmobilization,and(B)aratwithkneejointimmobilizedandwrappedwithadhesiveplasteraroundtherighthindlimb.
Determination of Antioxidant Enzyme Activities
In this study, Cu-Zn SOD activity was determined. The activity of SOD expressed as units per milligram of protein (U/mg protein) was measured based on its action to neutralize the superoxide radicals to prevent oxidation of adrenaline to adrenochrome, a colorful byproduct that can be measured at 480 nm (SP22 spectrophotometer, Bioespectro, Curitiba, PR, Brazil).32 The SOD activity was determined by measuring the velocity of inhibition of adrenaline oxidation. The reaction medium contained glycine buffer (50 mmol/L, pH 11.3) and adrenaline (60 mmol/L, pH 2.0).33
The GPx activity was measured by following nicotinamide adenine dinucleotide phosphate oxidation at 340 nm (T60U spectrophotometer, PG Instruments Ltd, Leicestershire, United Kingdom) as described by Flohé and Gunzler.33 The GPx results were expressed as nanomoles of peroxide/hydroperoxide reduced per minute per milligram of protein.
Catalase activity was determined by following the decrease in absorption at 240 nm (T60U spectrophotometer, PG Instruments Ltd) in a reaction medium containing 50 mmol/L phosphate buffer (pH 7.2) and 10 mmol/L hydrogen peroxide (H2O2) and expressed as picomoles of H2O2 reduced per minute per milligram protein.33-35
Protein Measurement
Protein was measured by the method of Lowry using bovine serum albumin as standard.36
Statistical Analysis
The sample size for the present study was established based on previous studies using WINPEPI software version 9.1. A significant α level of .05 and 95% power resulted in a sample size of 6 rats per group. Data were analyzed by 2 independent researchers. All data are reported as means ± standard error of the values of 6 rats per group. Normal Gaussian distribution of the data was analyzed by the Shapiro-Wilk test. Levene’s test analyzed constant variance. Biochemical results were analyzed using 1-way analysis of variance (factor: treatment) followed by the Tukey post hoc test. Mechanical threshold and functional indices were compared by repeated-measures 2-way analysis of variance (factors: treatment and time) followed by the Tukey post hoc test. Differences were considered statistically significant when P was b.05. All statistical analyses were carried out with Sigma State package version 3.1 (Systat Software Inc, Chicago, Illinois) for Windows.
Results
Mechanical Threshold
The mechanical threshold did not change significantly in naive and naive-AAI 4 groups (P > .05). Twenty-four hours after the end of the immobilization period, the mechanical threshold reduced in I-AAI 4 (mean difference [MD] = 30.45; 95% confidence interval [CI] (12.68-48.22); P < .0001), I-sham
(MD = 36.9; 95% CI [19.13-54.67]; P < .0001), and I-RF rats (MD = 22.77; 95% CI [5.004-40.54]; P = .0030) (Fig 3). The reduction was around 38% in all groups when compared with preimmobilization levels. A decrease of 38% in the mechanical threshold suggests the presence of hyperalgesia in these rats. In addition, 3 weeks of the AAI 4 therapy improved the mechanical threshold, returning the mechanical threshold to pre-immobilization levels. This was implied because no significant difference was found when compared with preimmobilization values within group (MD = -1.465; 95% CI [-19.23 to 16.3]; P >.9999), compared with post-24 hours cast removal (MD = -31.92; 95% CI [-49.68 to -14.15]; P < .001), or when compared with naive and naive-AAI 4 (MD = [9.601],[0.1403]; 95% CI [-8.167 to 27.37], [-17.63 to 17.91]; P > .999), indicating total recovery of the mechanical threshold. Interestingly, 3 weeks post-sham therapy did not show significant improvement of the mechanical threshold compared with post-24 hours cast removal (MD = -14.33; 95% CI [-32.1 to 3.435]; P = .2340). The mechanical threshold did not return to pre-immobilization levels within group (MD = 22.57; 95% CI [4.799-40.33]; P = .0034). After 3 weeks with sham therapy, the mechanical threshold was significantly decreased in these rats compared with naive (MD = 23.66; 95% CI [5.893-41.43]; P = .0018) and naive AAI 4 (MD = 18.54; 95% CI [0.7765-36.31]; P =.0335) groups. This result indicates that the value of force developed by the instrument appears to influence the recovery of mechanical threshold in immobilized rats. Similarly to I-sham, the mechanical threshold of the I-RF rats did not show significant recovery compared with post-24 hours cast removal (MD = -9.272; 95% CI [-27.04 to 8.496]; P = .8471), indicating that the recovery of mechanical threshold was small. In addition, the mechanical threshold was significantly different compared with the pre-immobilization threshold (MD =13.5; 95% CI [2.61-24.39]; P = .0117). After 3 weeks with free remobilization, the mechanical threshold was significantly decreased in these rats compared with naive (MD = 24.66; 95% CI [6.888-42.42] P =.0010)andnaive AAI 4 (MD = 18.54; 95% CI [0.7765-36.31]; P =.0335) groups.
Sciatic, Peroneal, and Tibial Functional Indices
The functional indices did not differ significantly in naive and naive-AAI 4 groups (P > .05). The indices values were between -12 and -4 in these rats through all nerve indices assessed. The walking gait analysis values significantly decreased after 24 hours, ranging between -25 and -20 in the immobilized rats in the sciatic, peroneal, and tibial functional indices, respectively, within each group compared with pre-immobilization levels on the I-AAI 4 (MD = 12.92, 17, 14.12; 95% CI [10.71-15.13], [14.98-19.02], [12.11-16.14]; P b .0001), I-sham (MD = 8.541, 15, 16.07; 95% CI [6.333-10.75], [12.98-17.02], [14.06-18.09]; P < .0001), and I-RF (MD = 6.542, 14, 11.91; 95% CI [4.334-8.75], [11.98-16.02], [9.895-13.93]; P b .0001) as well as when I-AAI 4, I-sham, and I-RF were compared to naive (I-AAI 4: MD = 14.79, 19, 15.79; 95% CI [11.55-18.03], [16.04-21.96], [12.83-18.75]; P < .0001) (I-sham: MD = 9.674, 17, 17.51; 95% CI [6.435-12.91], [14.04-19.96], [14.55-20.46]; P < .0001) (I-RF: MD = 9.724, 17,
A selection of published research by CMCC faculty 55 Duarte et al
Fig3Assessmentofmechanicalthresholdinratsthatunderwentkneejointimmobilizationfor4weeksand,aftercastremoval,hadtheAAI4therapyappliedonthelumbar spinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean±standarderrorofthemean.*Indicatessignificantdifferencecomparedtopre-immobilization values.#Indicatessignificantdifferencecomparedwithnaivegroups.“a”representssignificantdifferencecomparedtopost-castremoval(repeated-measures2-wayanalysis ofvariancefollowedbyTukeyposthoctest,Pb.05).ExperimentalgroupsareasdescribedinFigure1.AAI4,ActivatorAdjustingInstrument,model4;I,immobilization;RL, rightleg.
Fig3. Assessmentofmechanicalthresholdinratsthatunderwentkneejointimmobilizationfor4weeksand,aftercastremoval,hadthe AAI4therapyappliedonthelumbarspinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean±standarderrorofthe mean.*Indicatessignificantdifferencecomparedtopre-immobilizationvalues. # Indicatessignificantdifferencecomparedwithnaive groups. “ a ” representssignificantdifferencecomparedtopost-castremoval(repeated-measures2-wayanalysisofvariancefollowedby Tukeyposthoctest, P b .05).Experimentalgroupsareasdescribedin Figure1 AAI4,ActivatorAdjustingInstrument,model4; I, immobilization; RL,rightleg.
P N .999),indicatingtotalrecoveryofthemechanical threshold.Interestingly,3weekspost-shamtherapydidnot showsignificantimprovementofthemechanicalthreshold comparedwithpost-24hourscastremoval(MD=-14.33; 95%CI[-32.1to3.435]; P =.2340).Themechanical thresholddidnotreturntopre-immobilizationlevelswithin group(MD=22.57;95%CI[4.799-40.33]; P =.0034).After 3weekswithshamtherapy,themechanicalthresholdwas significantlydecreasedintheseratscomparedwithnaive (MD=23.66;95%CI[5.893-41.43]; P =.0018)andnaive AAI4(MD=18.54;95%CI[0.7765-36.31]; P =.0335) groups.Thisresultindicatesthatthevalueofforcedeveloped bytheinstrumentappearstoinfluencetherecoveryof mechanicalthresholdinimmobilizedrats.SimilarlytoI-sham, themechanicalthresholdoftheI-RFratsdidnotshow significantrecoverycomparedwithpost-24hourscast removal(MD=-9.272;95%CI[-27.04to8.496]; P = .8471),indicatingthattherecoveryofmechanicalthreshold wassmall.Inaddition,themechanicalthresholdwas significantlydifferentcomparedwiththepre-immobilization threshold(MD=13.5;95%CI[2.61-24.39]; P =.0117).After 3weekswithfreeremobilization,themechanicalthreshold wassignificantlydecreasedintheseratscomparedwithnaive (MD=24.66;95%CI[6.888-42.42] P =.0010)andnaive AAI4(MD=18.54;95%CI[0.7765-36.31]; P =.0335) groups.
Sciatic,Peroneal,andTibialFunctionalIndices
14.58; 95% CI [6.485-12.96], [14.04-19.96], [11.62-17.53]; P < .0001 ) and naive-AAI 4 (I-AAI 4: MD = 11.57, 16, 14.12; 95% CI [8.327-14.8], [13.04-18.96], [11.17-17.08]; P < .0001) (I-sham: MD = 6.453, 14, 15.84; 95% CI [3.214-9.692], [11.04-16.96], [12.88-18.8]; P < .0001) (I-RF: MD = 6.503, 14, 12.91; 95% CI [3.264-9.742], [11.04-16.96], [9.954-15.87]; P < .0001) (Figs 4A, 4B, and 4C). The indices of these nerves showed recovery in I-AAI 4 rats. At the end of 3 weeks of therapy, the sciatic functional index was similar to the pre-immobilization (MD = 1.1912; 95% CI [-0.2963 to 4.12]; P > .05) and to the naive-AAI 4 groups (MD = 0.557; 95% CI [-2.682 to 3.796]; P > .9999), which shows a full recovery of this nerve after AAI 4 therapy. We found an important improvement after 3 weeks of AAI 4 therapy in the sciatic (post-cast removal: -18.566; post-3 weeks AAI therapy: -7.557; MD = 3.726; 95% CI [0.4872-6.965]; P = .01), peroneal (post-cast removal: -23; post-3 weeks AAI 4: -10; MD = 6; 95% CI [3.039-8.961]; P< .0001), and tibial nerve indices (post-cast removal: -20; post-3 weeks AAI 4: -9; MD = 5.405; 95% CI [2.448-8.362]; P < .0001), reaching indices values close to naive animals; however, neither the peroneal indices (MD = 4; 95%CI [1.981-6.019]; P < .0001) nor the tibial indices (MD = 3.515; 95% CI[1.499-5.531]; P = .0002) fully returned to pre-immobilization values. In addition, although a robust reduction post-3 weeks AAI 4 therapy was found, it still presented a significant difference compared with the peroneal naive and naive-AAI 4 indices (MD = 6, 3; 95% CI [3.039-8.961], [0.03926-5.961]; P < .0001, P = .0439 ) and tibial naive and naive AAI 4 indices (MD = 5.182, 3.515; 95% CI [2.225-8.139], [0.5582-6.472]; P < .01).
The sciatic, peroneal, and tibial indices of these 3 nerves did not show recovery 3 weeks post-I-sham therapy when compared
Thefunctionalindicesdidnotdiffersignificantlyin naiveandnaive-AAI4groups(P N .05).Theindicesvalues werebetween-12and-4intheseratsthroughallnerve indicesassessed.Thewalkinggaitanalysisvaluessignificantlydecreasedafter24hours,rangingbetween-25and
-20intheimmobilizedratsinthesciatic,peroneal,and tibialfunctionalindices,respectively,withineachgroup comparedwithpre-immobilizationlevelsontheI-AAI4 (MD=12.92,17,14.12;95%CI[10.71-15.13],[14.9819.02],[12.11-16.14]; P b .0001),I-sham(MD=8.541,15, 16.07;95%CI[6.333-10.75],[12.98-17.02],[14.06-18.09]; P b .0001),andI-RF(MD=6.542,14,11.91;95%CI [4.334-8.75],[11.98-16.02],[9.895-13.93]; P b .0001)as wellaswhenI-AAI4,I-sham,andI-RFwerecomparedto naive(I-AAI4:MD=14.79,19,15.79;95%CI[11.5518.03],[16.04-21.96],[12.83-18.75]; P b .0001)(I-sham: MD=9.674,17,17.51;95%CI[6.435-12.91],[14.0419.96],[14.55-20.46]; P b .0001)(I-RF:MD=9.724,17, 14.58;95%CI[6.485-12.96],[14.04-19.96],[11.62-17.53];
P b .0001)andnaive-AAI4(I-AAI4:MD=11.57,16, 14.12;95%CI[8.327-14.8],[13.04-18.96],[11.17-17.08];
P b .0001)(I-sham:MD=6.453,14,15.84;95%CI [3.214-9.692],[11.04-16.96],[12.88-18.8]; P b .0001)(I-RF: MD=6.503,14,12.91;95%CI[3.264-9.742],[11.0416.96],[9.954-15.87]; P b .0001)(Figs4A, 4B,and 4C).The indicesofthesenervesshowedrecoveryinI-AAI4rats.At theendof3weeksoftherapy,thesciaticfunctionalindex wassimilartothepre-immobilization(MD=1.1912;95%CI [-0.2963to4.12]; P N .05)andtothenaive-AAI4groups (MD=0.557;95%CI[-2.682to3.796]; P N .9999),which showsafullrecoveryofthisnerveafterAAI4therapy.We foundanimportantimprovementafter3weeksofAAI4 therapyinthesciatic(post-castremoval:-18.566;post-3 weeksAAItherapy:-7.557;MD=3.726;95%CI[0.48726.965]; P =.01),peroneal(post-castremoval:-23;post-3 weeksAAI4:-10;MD=6;95%CI[3.039-8.961]; P b .0001),andtibialnerveindic es(post-castremoval:-20; post-3weeksAAI4:-9;MD=5.405;95%CI[2.4488.362]; P b .0001),reachingindicesvaluesclosetonaive
with pre-immobilization values (MD = 13.28, 15, 12.02; 95% CI [10.04-16.52], [12.04-17.96], [9.064-14.98]; P < .0001). Despite this, we have found significant differences on I-sham post-cast removal compared to 3 weeks of post I-sham therapy on sciatic, peroneal, and tibial nerve indices (MD = 14.36, -3, -4.053; 95% CI [11.12-17.6], [-5.961 to -0.03926], [-7.01 to -1.096]; P < .05), which would suggest a successful rehabilitation; these indices values post-sham therapy were significantly lower (-18.18, -18, -17.78) and different than I-post-AAI 4 therapy (-7.55, -10, -9.51) (MD = 10.63, 8, 8.273; 95%CI [7.393-13.87], [5.039-10.96], [5.316-11.23]; P < .0001), implying that the AAI 4 therapy was more effective compared with I-sham. The sciatic, peroneal, and tibial post-3 weeks sham therapy were also different than naive (MD = 14.41, 14, 17.51; 95% CI [11.17-17.65], [11.04-16.96], [14.55-20.46]; P < .0001) and AAI 4 (MD = 11.19, 11, 15.84; 95% CI [7.95-14.43], [8.039-13.96], [12.88-18.8]; P < .0001).
Similar to I-sham, I-RF did not show sciatic, peroneal, and tibial indices recovery 3 weeks post-remobilization free compared with pre-immobilization indices (MD = 7.75, 10, 8.17; 95% CI [4.511-10.99], [7.039-12.96], [5.213-11.13]; P < .0001). The sciatic, peroneal, and tibial post-3 weeks remobilization-free therapy were also different than naive (MD = 10.93, 13, 10.84; 95% CI [7.693-14.17], [10.04-15.96], [7.88-13.79]; P < .0001) and naive-AAI 4 (MD = 7.711, 10, 12.91; 95% CI [4.472-10.95], [7.03912.96],[9.954-15.87]; P < .0001). Although some improvement was found on these 3 nerve indices between post-3 weeks remobilization-free therapy compared to 24 hours knee cast removal (MD = 10.88, 13, -6.671; 95% CI [7.641-14.12],[10.0415.96], [-9.628 to -3.714]; P < .0001), the sciatic, peroneal, and tibial indices were significantly lower in the post-3 weeks
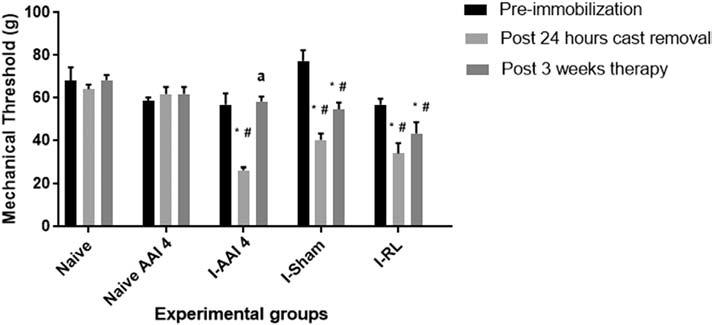
CMCC Research Report 2018–2020 56
390 JournalofManipulativeandPhysiologicalTherapeutics Duarteetal July/August2019 MASMTImprovesAllodynia,NerveFunction,andROS
Fig4. FunctionalrecoveryassessedbytheSFI,TFI,andPFI.Ratsunderwentkneejointimmobilizationfor4weeksand,afterjointcast removal,hadtheAAI4therapyappliedonthelumbarspinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean±standard errorofthemean.*Indicatessignificantdifferencecomparedwithpre-immobilizationvalues.
Fig4FunctionalrecoveryassessedbytheSFI,TFI,andPFI.Ratsunderwentkneejointimmobilizationfor4weeksand,afterjointcastremoval,hadtheAAI4therapyappliedonthe lumbarspinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean±standarderrorofthemean.*Indicatessignificantdifferencecomparedwithpre-immobilization values.#IndicatessignificantdifferencecomparedtoNaivegroups.“a”representssignificantdifferencecomparedwithpost-castremoval.“b”representssignificantdifferences between3weekspost-shamorremobilization-freetherapycomparedwithAAI4therapy(repeated-measures2-wayanalysisofvariancefollowedbyTukeyposthoctest,Pb.05). ExperimentalgroupsareasdescribedinFigure1.AAI4,ActivatorAdjustingInstrument,model4;I,immobilization;PFI,peronealfunctionalindex;RF,remobilizationfree;SFI,sciatic functionalindex;TFI,tibialfunctionalindex.
#Indicatessignificantdifferencecomparedto Naivegroups. “ a ” representssignificantdifferencecomparedwithpost-castremoval. “b” representssignificantdifferencesbetween3 weekspost-shamorremobilization-freetherapycomparedwithAAI4therapy(repeated-measures2-wayanalysisofvariancefollowedby Tukeyposthoctest, P b .05).Experimentalgroupsareasdescribedin Figure1 AAI4,ActivatorAdjustingInstrument,model4; I, immobilization; PFI,peronealfunctionalindex; RF,remobilizationfree; SFI,sciaticfunctionalindex; TFI,tibialfunctionalindex.
animals;however,neithertheperonealindices(MD=4;95% CI[1.981-6.019]; P b .0001)northetibialindices(MD= 3.515;95%CI[1.499-5.531]; P =.0002)fullyreturnedtopreimmobilizationvalues.Inaddition,althougharobust reductionpost-3weeksAAI4therapywasfound,itstill presentedasignificantdifferencecomparedwiththeperoneal naiveandnaive-AAI4indices(MD=6,3;95%CI[3.0398.961],[0.03926-5.961]; P b .0001, P =.0439)andtibial naiveandnaiveAAI4indices(MD=5.182,3.515;95%CI [2.225-8.139],[0.5582-6.472]; P b .01).
remobilization-free therapy group (-14.71, -17, -15.17) than in the post-3 weeks AAI 4 therapy group (-7.55, -10, -9.51) (MD = 7.154, 7, 5.655; 95% CI [3.915-10.39], [4.039-9.961], [2.6988.612]; P < .0001). Interestingly, no difference between 3 weeks post-sham and remobilization-free therapy was found on the sciatic (MD = -2.93; 95% CI [-5.887to0.02676]; P = .0546), peroneal (MD = -1; 95%CI [-3.961to1.961]; P = .9970), and tibial (MD = -2.618;[-5.575 to 0.3388]; P = .1401) indices.
Oxidative Stress Parameters
Thesciatic,peroneal,andtibialindicesofthese3nerves didnotshowrecovery3weekspost-I-shamtherapywhen comparedwithpre-immobilizationvalues(MD=13.28,15, 12.02;95%CI[10.04-16.52],[12.04-17.96],[9.064-14.98]; P b .0001).Despitethis,wehavefoundsignificant differencesonI-shampost-castremovalcomparedto3 weeksofpostI-shamtherapyonsciatic,peroneal,andtibial nerveindices(MD=14.36,-3,-4.053;95%CI[11.1217.6],[-5.961to-0.03926],[-7.01to-1.096]; P b .05),
whichwouldsuggestasuccessfulrehabilitation;these indicesvaluespost-shamtherapyweresignificantlylower (-18.18,-18,-17.78)anddifferentthanI-post-AAI4 therapy(-7.55,-10,-9.51)(MD=10.63,8,8.273;95% CI[7.393-13.87],[5.039-10.96],[5.316-11.23]; P b .0001), implyingthattheAAI4therapywasmoreeffective comparedwithI-sham.Thesciatic,peroneal,andtibial post-3weeksshamtherapywerealsodifferentthannaive (MD=14.41,14,17.51;95%CI[11.17-17.65],[11.0416.96],[14.55-20.46]; P b .0001)andAAI4(MD=11.19, 11,15.84;95%CI[7.95-14.43],[8.039-13.96],[12.8818.8]; P b .0001).
The lipid hydroperoxide levels did not show a significant change in plasma of I-AAI 4 and I-sham rats compared with naive (MD = -0.182, -0.844; 95% CI [-1.34 to 0.97], [-1.96 to 0.27]; P >.05) and naive-AAI 4 (MD = 0.005, -0.656; 95%CI -1.10to1.11,-1.72to0.41; P > .05) groups, respectively (Fig 5A). However, the values of lipid hydroperoxides in plasma of I-sham rats were higher than those found in the plasma of naive, naive-AAI 4, and I-AAI 4 rats, although no significant differences were found among them. In
I-RF rats, the lipid hydroperoxide levels significantly increased in plasma. The increase was 65% compared with both naive (MD = -1.382; 95% CI [-2.54 to -0.22]; P = .0141) and naive-AAI 4 (MD = -1.194; 95% CI [-2.30 to -0.08]; P = .030) and 56% compared to I-AAI 4 rats (MD = -1.2; 95%CI [-2.30 to -0.09]; P = .029). No significant difference was found in lipid hydroperoxides between I-RF and I-sham (MD = -0.537; 95% CI [-1.60 to 0.53]; P =.584).
The level of NO metabolites did not significantly change in the plasma of rats with immobilization that received AAI 4, sham therapy, or remobilization free and were similar to naive and naive-AAI 4 (F [4, 18] = 1.037, P = .415) (Fig 5B).
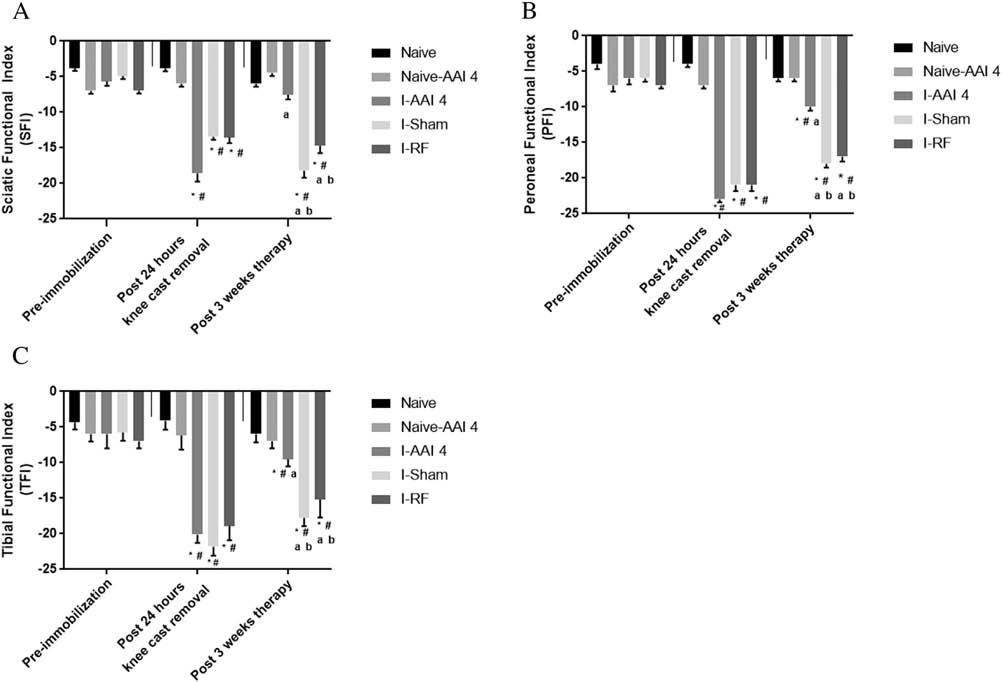
SimilartoI-sham,I-RFdidnotshowsciatic,peroneal, andtibialindicesrecovery3weekspost-remobilizationfree comparedwithpre-immobilizationindices(MD=7.75,10, 8.17;95%CI[4.511-10.99],[7.039-12.96],[5.213-11.13]; P b .0001).Thesciatic,peroneal,andtibialpost-3weeks remobilization-freetherapywerealsodifferentthannaive (MD=10.93,13,10.84;95%CI[7.693-14.17],[10.04-
The SOD activity did not show any significant change in RBCs of I-AAI 4 rats nor I-sham, I-RF, naive, and naive-AAI 4 (F [4, 25] = 0.870, P = .495) (Fig 6A). The GPx enzymatic activity did not show any significant change in RBCs of I-AAI 4, I-RF, nor both naïve groups. However, GPx activity was significantly higher in RBCs
A selection of published research by CMCC faculty 57 Duarte et al
391 Duarteetal JournalofManipulativeandPhysiologicalTherapeutics MASMTImprovesAllodynia,NerveFunction,andROS Volume 42,Number6
Fig5. Assessmentofthebloodpro-oxidativeparameteractivitylipidhydroperoxides(A)andnitricoxidemetabolites(nitrites+ nitrates)(B)inratsthatunderwentkneejointimmobilizationfor4weeksand,afterjointcastremoval,hadtheAAI4therapyappliedon thelumbarspinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean±standarderrorofthemean.*Indicates significantdifferencecomparedwithnaivegroups(1-wayanalysisofvariancefollowedbyTukeyposthoctest, P b .05). # Indicates significantdifferencecomparedwithI-AAI4group(1-wayanalysisofvariancefollowedbyTukeyposthoctest, P b .05).Experimental groupsareasdescribedin Figure1 AAI4,ActivatorAdjustingInstrument,model4; I,immobilization; RF,remobilizationfree.
Fig5Assessmentofthebloodpro-oxidativeparameteractivitylipidhydroperoxides(A)andnitricoxidemetabolites(nitrites+nitrates)(B)inratsthatunderwentkneejoint immobilizationfor4weeksand,afterjointcastremoval,hadtheAAI4therapyappliedonthelumbarspinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean± standarderrorofthemean.*Indicatessignificantdifferencecomparedwithnaivegroups(1-wayanalysisofvariancefollowedbyTukeyposthoctest,Pb.05).#Indicatessignificant differencecomparedwithI-AAI4group(1-wayanalysisofvariancefollowedbyTukeyposthoctest,Pb.05).ExperimentalgroupsareasdescribedinFigure1.AAI4,Activator AdjustingInstrument,model4;I,immobilization;RF,remobilizationfree.
in I-sham rats (higher than 50%) compared with naive-AAI 4 and I-AAI 4 rats (MD = -10.4, -11.74; 95% CI [-20.61 to -0.1873], [-21.65 to -1.831]; P b .05) (Fig 6B). Catalase activity, in turn, decreased 53% in the RBCs of I-AAI 4 rats compared with naive (MD = 3.367, 95% CI [0.09-6.63]; P =.041), naive-AAI 4 (MD = 2.982, 95% CI [0.52-5.43]; P = .011), and I-sham (MD = -3.129, 95% CI [-5.66 to -0.596]; P = .01) groups. No significant change was found when compared wtih I-RF rats (Fig 6C).
Discussion
15.96],[7.88-13.79]; P b .0001)andnaive-AAI4(MD= 7.711,10,12.91;95%CI[4.472-10.95],[7.039-12.96], [9.954-15.87]; P b .0001).Althoughsomeimprovement wasfoundonthese3nerveindicesbetweenpost-3weeks remobilization-freetherapycomparedto24hourskneecast removal(MD=10.88,13,-6.671;95%CI[7.641-14.12], [10.04-15.96],[-9.628to-3.714]; P b .0001),thesciatic, peroneal,andtibialindicesweresignificantlylowerinthe post-3weeksremobilization-freetherapygroup(-14.71, -17,-15.17)thaninthepost-3weeksAAI4therapygroup (-7.55,-10,-9.51)(MD=7.154,7,5.655;95%CI[3.91510.39],[4.039-9.961],[2.698-8.612]; P b .0001).Interestingly, nodifferencebetween3weekspost-shamandremobilizationfreetherapywasfoundonthesciatic(MD=-2.93;95%CI [-5.887to0.02676]; P =.0546),peroneal(MD=-1;95% CI[-3.961to1.961]; P =.9970),andtibial(MD=-2.618; [-5.575to0.3388]; P =.1401)indices.
foundinlipidhydroperoxidesbetweenI-RFandI-sham (MD=-0.537;95%CI[-1.60to0.53]; P =.584).
ThelevelofNOmetabolitesdidnotsignificantlychangein theplasmaofratswithimmobilizationthatreceivedAAI4, shamtherapy,orremobilizationfreeandweresimilartonaive andnaive-AAI4(F[4,18]=1.037, P =.415)(Fig5B).
TheSODactivitydidnotshowanysignificantchangein RBCsofI-AAI4ratsnorI-sham,I-RF,naive,andnaiveAAI4(F[4,25]=0.870, P =.495)(Fig6A).
activity induced by knee immobilization. Previous studies developed and validated the applicability of the AAI 4, replacing its original larger silicone rubber tip with a smaller adapter tip made in nylon, aiming to bridge the contact between the instrument and smaller joint such as those seen in rodents (spine segments, knee, etc).10,25 Thus, the AAI 4 with the adapter becomes a useful tool to examine the effects of chiropractic treatment in animal studies.10,25
OxidativeStressParameters
This study is the first to establish that AAI 4 therapy induces recovery of the sciatic, peroneal, and tibial nerve functional indices decreased by 4 weeks of immobilization. Also, this is the first study showing the effect of the AAI 4 on ROS. Although it is early to speculate on the role of MASMT on oxidative stress, our results demonstrated that this therapy might have a protective role,counteracting ROS formation. Its modulatory effect on systemic oxidative stress may be associated with the antinociceptive effect of MASMT, recovery of peripheral nerve functionality, and motor performance.
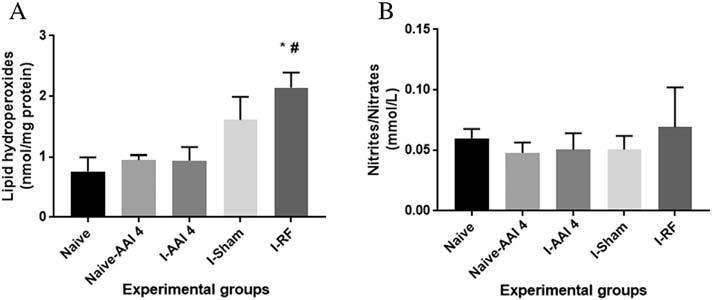
In this study, the immobilization condition increased mechanical nociception and promoted peripheral nerve function impairment and plasmatic changes in oxidative stress parameters. Otherwise, the MASMT induced anti-nociception; recovered the gait pattern assessed through the sciatic, peroneal, and tibial nerve functional indices; and modulated pro- and antioxidative stress parameters in the blood of these animals. Therefore, these findings support our hypothesis that the AAI 4 on lumbar spine segments ameliorates the mechanical hyperalgesia, recuperates the free walking pattern, and stabilizes the ROS
Thelipidhydroperoxidelevelsdidnotshowasignificant changeinplasmaofI-AAI4andI-shamratscomparedwith naive(MD=-0.182,-0.844;95%CI[-1.34to0.97],[-1.96to 0.27]; P N .05)andnaive-AAI4(MD=0.005,-0.656;95% CI-1.10to1.11,-1.72to0.41; P N .05)groups,respectively (Fig5 A).However,thevaluesoflipidhydroperoxidesin plasmaofI-shamratswerehigherthanthosefoundinthe plasmaofnaive,naive-AAI4,andI-AAI4rats,although nosignificantdifferenceswerefoundamongthem.InI-RF rats,thelipidhydroperoxidelevelssignificantlyincreased inplasma.Theincreasewas65%comparedwithbothnaive (MD=-1.382;95%CI[-2.54to-0.22]; P =.0141)and naive-AAI4(MD=-1.194;95%CI[-2.30to-0.08]; P = .030)and56%comparedtoI-AAI4rats(MD=-1.2;95% CI[-2.30to-0.09]; P =.029).Nosignificantdifferencewas
TheGPxenzymaticactivitydidnotshowanysignificant changeinRBCsofI-AAI4,I-RF,norbothnaïvegroups. However,GPxactivitywassignificantlyhigherinRBCsin I-shamrats(higherthan50%)comparedwithnaive-AAI4 andI-AAI4rats(MD=-10.4,-11.74;95%CI[-20.61to -0.1873],[-21.65to-1.831]; P b .05)(Fig6B).Catalase activity,inturn,decreased53%intheRBCsofI-AAI4rats comparedwithnaive(MD=3.367,95%CI[0.09-6.63]; P =.041),naive-AAI4(MD=2.982,95%CI[0.52-5.43]; P =.011),andI-sham(MD=-3.129,95%CI[-5.66to -0.596]; P =.01)groups.Nosignificantchangewasfound whencomparedwtihI-RFrats(Fig6C).
DISCUSSION
ThisstudyisthefirsttoestablishthatAAI4therapyinduces recoveryofthesciatic,peroneal,andtibialnervefunctional indicesdecreasedby4weeksofimmobilization.Also,thisis thefirststudyshowingtheeffectoftheAAI4onROS. AlthoughitisearlytospeculateontheroleofMASMTon oxidativestress,ourresultsdemonstratedthatthistherapymight haveaprotectiverole,counteractingROSformation.Its modulatoryeffectonsystemicoxidativestressmaybe associatedwiththeantinociceptiveeffectofMASMT,recovery ofperipheralnervefunctionality,andmotorperformance.
Similar to other studies, our results showed that 4 weeks of knee immobilization induces mechanical hypersensitivity in the ipsilateral hindpaw.10,18 In addition, the hypersensitivity was persistent, not returning to pre-immobilization levels as verified when spine AAI 4 was applied. Despite the importance of the pain system as a warning and protective system to maintain tissue integrity, its mechanism of function differs when pain becomes persistent or chronic.8,13,16 In such a situation, nociceptors no longer only respond to vigorous suprathreshold stimulus, but the threshold needed to evoke a response is lowered.13,16,37-40 Persistent and chronic pain may be associated with peripheral or central sensitization (CS).8,37,38,42 Previous studies reported that acute peripheral knee inflammation and knee immobilization sensitizes pain-related non-myelinated or low-myelinated fibers in the knee joint, increasing their activity during the rest (spontaneous activity) and when innocuous stimuli are applied.11,13,18,27 One remarkable characteristic of CS is the augmented electrophysiological activity in nociceptive neurons within the spinal cord elicited by normal inputs.8,18,42 Central sensitization can be maintained by an ongoing peripheral noxious input such as occurs in neuropathic pain or during inflammation.37,39,42 Interestingly, an
CMCC Research Report 2018–2020 58
392 JournalofManipulativeandPhysiologicalTherapeutics Duarteetal July/August2019 MASMTImprovesAllodynia,NerveFunction,andROS
Fig6Assessmentofantioxidantenzymeactivitiessuchassuperoxidedismutase(A),glutathioneperoxidase(B),andcatalase(C)inthebloodofratsthatunderwentkneejoint immobilizationfor4weeksand,afterjointcastremoval,hadtheAAI4therapyappliedtothelumbarspinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean± standarderrorofthemean.*Indicatessignificantdifferencecomparedwithnaivegroups(1-wayanalysisofvariancefollowedbyTukeyposthoctest,Pb.05).#Indicatessignificant differencecomparedwithI-AAI4on(B)ortoI-shamgroupon(C)(1-wayanalysisofvariancefollowedbyTukeyposthoctest,Pb.01).ExperimentalgroupsareasdescribedinFigure 1.AAI4,ActivatorAdjustingInstrument,model4;I,immobilization;RF,remobilizationfree.
Fig6. Assessmentofantioxidantenzymeactivitiessuchassuperoxidedismutase(A),glutathioneperoxidase(B),andcatalase(C)inthe bloodofratsthatunderwentkneejointimmobilizationfor4weeksand,afterjointcastremoval,hadtheAAI4therapyappliedtothe lumbarspinalsegmentsL4-L5for3weeks,3timesperweek.Datarepresentmean±standarderrorofthemean.*Indicatessignificant differencecomparedwithnaivegroups(1-wayanalysisofvariancefollowedbyTukeyposthoctest, P b .05). # Indicatessignificant differencecomparedwithI-AAI4on(B)ortoI-shamgroupon(C)(1-wayanalysisofvariancefollowedbyTukeyposthoctest, P b .01).
Experimentalgroupsareasdescribedin Figure1 AAI4,ActivatorAdjustingInstrument,model4; I,immobilization; RF,remobilizationfree.
increase of pro-oxidation peripherally has been suggested as one of the mechanisms contributing to peripheral inflammation after joint immobilization.18 Also, Hamaue et al18 showed an increase of spinal cord neuropeptides related to the onset of the CS (substance P and calcitonin generelated peptide), after 4 and 8 weeks of joint immobilization. Interestingly, He and Dishman24 showed that 4 weeks of immobilization enhances the oxidative activity, triggering neurotoxicity within the spinal cord. Although the cast apparatus itself it is not considered a painful stimulus, a knee cast apparatus for 4 weeks may lead to peripheral inflammation, which in turn sensitizes peripheral nociceptors, altering the expression of factors that are driven up to the central nervous system, such as those related to the onset of CS as substance P, which was previously demonstrated to be increased in rodents after inflammation.42 Therefore, some of the benefits of the AAI 4 in this model might involve the modulation of factors linked to peripheral inflammation and central sensitization.
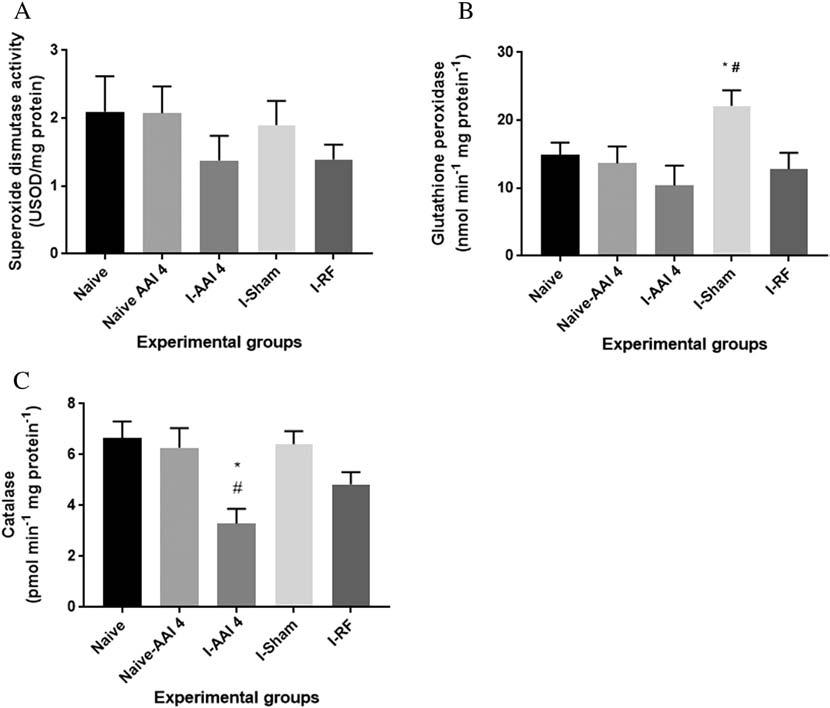
Inthisstudy,theimmobilizationconditionincreased mechanicalnociceptionandpromotedperipheralnerve functionimpairmentandplasmaticchangesinoxidative stressparameters.Otherwise,theMASMTinducedantinociception;recoveredthegaitpatternassessedthroughthe sciatic,peroneal,andtibialnervefunctionalindices;and modulatedpro-andantioxidativestressparametersinthe bloodoftheseanimals.Therefore,thesefindingssupport ourhypothesisthattheAAI4onlumbarspinesegments amelioratesthemechanicalhyperalgesia,recuperatesthe freewalkingpattern,andstabilizestheROSactivity inducedbykneeimmobilization.PreviousstudiesdevelopedandvalidatedtheapplicabilityoftheAAI4,replacing itsoriginallargersiliconerubbertipwithasmalleradapter tipmadeinnylon,aimingtobridgethecontactbetweenthe instrumentandsmallerjointsuchasthoseseeninrodents (spinesegments,knee,etc). 10,25 Thus,theAAI4withthe adapterbecomesausefultooltoexaminetheeffectsof chiropractictreatmentinanimalstudies. 10,25
Similartootherstudies,ourresultsshowedthat4weeksof kneeimmobilizationinducesmechanicalhypersensitivityin theipsilateralhindpaw. 10,18 Inaddition,thehypersensitivity waspersistent,notreturningtopre-immobilizationlevelsas verifiedwhenspineAAI4wasapplied.Despitetheimportance ofthepainsystemasawarningandprotectivesystemto maintaintissueintegrity,its mechanismoffunctiondiffers whenpainbecomespersistentorchronic. 8,13,16 Insucha situation,nociceptorsnolongeronlyrespondtovigorous suprathresholdstimulus,butthethresholdneededtoevokea responseislowered. 13,16,37-40 Persistentandchronicpainmay beassociatedwithperipheralorcentralsensitization (CS). 8,37,38,42 Previousstudiesreportedthatacuteperipheral kneeinflammationandkneeimmobilizationsensitizespainrelatednon-myelinatedorlow-myelinatedfibersintheknee joint,increasingtheiractivity duringtherest(spontaneous activity)andwheninnocuousstimuliareapplied. 11,13,18,27 One remarkablecharacteristicofCS istheaugmentedelectrophysiologicalactivityinnociceptiveneuronswithinthespinalcord
Only the AAI 4 therapy improved the abnormal mechanical threshold, returning to the normal baseline values such as given by naive and naive-AAI 4 groups. The antinociceptive effect of the AAI 4 therapy is in line with a previous study using alike animal model10 and other studies with a similar therapy approach in animals and humans.9,41,43-46 An earlier study demonstrated that the attenuation of dorsal root ganglia and spinal neuron hyperexcitability reduce mechanical allodynia in rats.46 Although we found the critical antinociceptive effects of the AAI 4 focusing on lumbar spine therapy, Trierweiller et al10 found analogous antinociceptive results by applying the AAI 4 therapy directly on the tibial tubercle of the immobilized knee. Thus, the antinociceptive effect of the AAI 4 and the possible modulation of CS likely appear to be independent of the application site, at least in this model of study.
Importantly, because an increase of NO was shown on motor neurons after knee immobilization,24 this neurotoxic factor
A selection of published research by CMCC faculty 59 Duarte et al
393 Duarteetal JournalofManipulativeandPhysiologicalTherapeutics MASMTImprovesAllodynia,NerveFunction,andROS Volume 42,Number6
may be contributing to the findings of the walking track analysis performed through our study. We did show for the first time that I-AAI 4 rats improved sciatic, tibial, and peroneal functional indices decreased after 4 weeks of knee immobilization. In addition, the peripheral nerve functional indices did not recover at the same proportion in the I-sham and I-RF rats. The measures of the sciatic, peroneal, and tibial nerve functional indices from naive and naive-AAI 4 are in line with other studies,24,26 thus reinforcing our measures made in all rats. Although any histological assessment was performed in our study, a mild nerve injury may have occurred since Alves et al21 showed that hind limb immobilization for 14 days causes variation in the nerve excitability and fragmentation in the myelin sheath of the sciatic nerve of rats. Some of these changes were reversible after cast removal.21 Also, He and Dishman24 showed that 4 weeks of knee immobilization leads to motor neuronal degeneration and axonal demyelination. A normal and intact afferent input, which is conducted up to the central nervous system, is a key player for a normal and tuned locomotor activity.47 Again, only animals exposed to AAI 4 therapy had their walking track patterns improved. Thus, we speculate that such an improvement may be due to modulatory effects on the inflammatory cascade and neuronal excitability, such those demonstrated by Songetal.45
On the other hand, abnormal motor activity can be caused by CS.38 In this context, it is possible that 4 weeks of the knee immobilization was enough to fire a salvo of abnormal afferent inputs to the central nervous system, generating improper sensory and motor output. Our results comparing the effectiveness of 3 weeks of different therapies employed through this study suggest that the high-speed force delivery thrust application of the AAI 4 performed in the I-AAI 4 group is the primary factor inducing the physiological effects involved in the recovery of peripheral nerve functional indices and walking track.
Our study also focused on the role of AAI therapy on plasmatic oxidative stress markers owing to the emerging role of ROS in altered nociception and chronic pain16,17,48,50 and the promisor effects of the SMT modulating oxidative stress parameters in patients with neck and back pain.2,11 For the first time, we demonstrated that AAI 4 therapy on lumbar spine L4-L5 segments stables lipid hydroperoxide and decreases catalase activity, but does not change GPx and SOD activities in RBCs in the I-AAI 4 rats. These results differ partially from those found in patients with chronic back or neck pain who received high-velocity, low-amplitude manipulation. In these patients, plasmatic catalase, SOD, and GPx activity increased in the RBCs.2,11 Therefore, these antioxidant enzymes likely acted to prevent the increase of plasmatic lipid peroxidation.2,11 It is possible that AAI 4 activated other enzymatic or non-enzymatic pathways to counteract ROS and therefore prevent lipid peroxidation. In addition, the controversial findings between rats and humans may be related to the difference in the metabolic
rate and the distinct chiropractic protocols used through these studies. Differences in the blood collection points after spinal manipulation therapy may also be another cause of such a difference. However, it is also necessary to consider that these results may be connected to the distinct painful conditions to which patients and rats were exposed. Regardless, MASMT modulated systemic ROS activity, and it may be linked with its antinociceptive effect found throughout the present study. Knee joint immobilization for 4 weeks changed the behavior of the plasmatic oxidative markers. The systemic blood cell activity may be changed by any modification in the immunological system, such as those influenced by inflammation or any biological stress.49,51 Thus, we suggest that the systemic changes 4 weeks post-immobilization may be related to changes in the endothelium and skeletal muscle functions caused by a stressor factor (knee immobilization). Data from animals, and more recently from humans, indicate that cast immobilization increases xanthine oxidase activity.51 Xanthine oxidase seems present in the capillary endothelium and infiltrated leukocytes, and this enzyme catalyzes the oxidation of hypoxanthine and xanthine to produce xanthine and uric acid, respectively; these reactions are coupled with the reduction of dioxygen into superoxide anions. In addition, it also has been demonstrated that cast immobilization increases superoxide and H2O2 emissions in the skeletal muscle.51 Taking these studies into account, we suggested that the immobilization protocol increased ROS in the blood of the immobilized rats by mechanisms that involve xanthine oxidase or emission of superoxide and H2O2 from skeletal muscle.
The enhanced ROS formation might be related to the plasmatic elevation of the lipid hydroperoxides found in the I-RF rats. Augmented production of ROS elevates lipid peroxidation.54 Interestingly, we reported that elevated plasmatic lipid hydroperoxide levels persisted for at least 3 weeks after cast removal. Because the central nervous system and particularly the spinal cord is highly composed of polyunsaturated fatty acids,48 lipid peroxidation may be occurring as consequence of enhanced formation of ROS. These species may contribute to maintenance of the nociceptive signaling, thus decreasing the mechanical threshold found in this group.
Importantly, the lack of significant changes in lipid hydroperoxide levels in the plasma of I-AAI 4 rats might be indicating a protective effect of the AAI 4 on ROS formation and subsequently in the oxidative damage that affects cellular membranes in this group. Interestingly, a decrease of oxidative stress and lipid peroxidation when an oxidative stress scavenger N-acetylcysteine is applied intraperitoneally has been associated with the reverse of the mechanical hyper-algesia and CS.48 Thus, our results suggest that the protective effects of the AAI 4 on ROS formation and its overall inhibition of lipid peroxidation may possibly be linked with the improvement of the mechanical hyperalgesia in rats undergoing knee immobilization. Inflammatory molecules increase ROS
CMCC Research Report 2018–2020 60
formation.45 Because AAI 4 reduces the manifestations of dorsal root ganglia inflammation,44 the lack of significant changes in plasmatic lipid hydroperoxide levels of I-AAI 4 rats may be related to an anti-inflammatory effect of the therapy with AAI 4. Otherwise, the lipid hydroperoxide was elevated in the plasma of I-sham rats when compared with the I-AAI 4 rats. Although this is an exciting finding, it lacks statistical difference. A possible reason for the lack of significant difference would be the limited number of rats used in our study. It is likely that increasing the number of rats would result in a significant difference between the groups because the standard error of the mean was high in the I-sham group. Yet, the difference in lipid hydroperoxide levels in the plasma of I-sham and I-AAI 4 rats may also be related to the proper application of the AAI 4 and not merely casualty. Thus, we speculate that the smaller force developed by the instrument in the sham condition fired a minor modulatory effect on systemic ROS and consequently led to more elevated plasmatic lipid hydroperoxide values in the I-sham rats.
Elevated ROS formation in the blood of the I-sham rats is the latent reason for the increased GPx activity in these rats. Glutathione peroxidase decomposes H2O2 into water and oxygen,12,17,55 and GPx activity is most useful for small amounts of H2O2 produced continuously by cellular metabolic activities.58 Because ROS formation was likely reduced in the blood of the I-AAI 4 group, this reduction potentially contributed to the lack of significant changes in plasmatic GPx activity in these rats. In this context, the lack of significant changes in GPx activity in the blood of the I-RF rats is intriguing, mainly because they showed elevation in lipid hydroperoxide levels. This finding may likely be related to the highest use of the glutathione (GSH) defense system. Glutathione is the primary intracellular thiol-disulfide redox buffer that serves as a cofactor for many antioxidant enzymes, including GPx.52 The oxidation of GSH leads to the production of glutathione disulfide (GSSG). In humans and animals, the GSSG concentration is low, but pro-oxidant overproduction is accompanied by activation of the GSH defense system, which enhanced GSSG levels to protect proteins and membrane lipids from oxidation.56,57 Since in the I-RF a higher lipid hydroperoxide was observed without changes in SOD and catalase, the use of GSH defense system is likely limiting the effects of plasmatic ROS formation in this group.
On the other hand, the catalase activity was decreased in the RBCs of the I-AAI 4 rats, while no changes occurred in the I-sham rats. This result might be related to the effect of the therapy on ROS formation. Catalase has less affinity to H2O2 and is useful during peaks of H2O2 production.53 The ROS formation appeared reduced in the RBCs of the I-AAI 4 rats, but more elevated in I-sham rats, as discussed earlier. Despite that ROS formation was lower in the RBCs of the I-AAI 4 rats, the activity of the catalase is decreased in the RBCs of these rats, without changing the GPx activity. Otherwise, because only the I-sham rats showed an increase in GPx activity, the activity of this enzyme was responsible for maintaining the low ROS
in the RBCs of I-sham rats. Nevertheless, the catalase activity may be associated with the muscle injury. After muscle injury, the induction of the catalase is delayed, and its peak of activity occurs in the second day post-injury, followed by thioredoxin activity.58,59 Thioredoxin is an antioxidant protein that limits the activity of ROS.59 Thus, it is possible that the thioredoxin activity may have some role in the complex interaction of pro-oxidant and antioxidant parameters in RBCs in immobilized rats.
In our study, no significant change was found in NO metabolites in the plasma of the I-AAI 4, I-sham, and I-RF rats. These results suggest that no change occurred in NO production in the immobilized rats. Nitric oxide is the major player for the maintenance of vascular homeostasis, and reduction of its bioavailability and increased NO degradation by superoxide anion mark the onset of endothelial dysfunction.59 Thus, the lack of changes in NO metabolites indicates that a normal bioavailability of NO to maintain the vascular homeostasis in the plasma of the I-AAI 4, I-sham, and I-RF rats is occurring. In addition, the maintenance of NO production could be explained by the GSH system. Glutathione plays a major role in NO metabolism.55 Glutathione reacts with peroxynitrite from S-nitrosothiols. Peroxynitrite is produced by the reaction of NO and superoxide anion.53,56 Peroxynitrite by itself may react with lipids, proteins, and other cellular structures, causing structural and functional modifications.56 The reaction of GSH with peroxynitrite may have prevented the systemic adverse effects of the peroxynitrite in the immobilized rats. The reaction of GSH with peroxynitrite also releases NO over a prolonged time to extend the half-life of NO,55 thereby preventing the adverse effects of NO scavenging by superoxide anions. Thus, the GSH reaction with peroxynitrite possibly contributed to maintaining the NO metabolite levels in the blood of immobilized rats. Indeed, the reaction of GSH with peroxynitrite may be limiting the availability of superoxide anions to SOD. This enzyme converts the superoxide anions to H2O2.12,17,52 Thus, the use of GSH may explain the lack of significant changes in NO metabolites and SOD activity in the plasma of immobilized rats. Because ROS are involved in the nociceptive process, central sensitization, and chronic pain mechanisms,17,22,50 the modulatory action of the AAI 4 therapy on oxidative stress parameters in the blood in the immobilized rats may be contributing to the AAI 4-induced antinociception. However, further studies are necessary to better understand the relation between AAI 4 and oxidative stress parameters in the blood of immobilized rats.
Limitations
This study did not assess other oxidative stress parameters such as the total content of thiols, which would allow for better understanding of the relation between GSH and our results. This study did not evaluate the concentration of oxidized and reduced glutathione (GSH-to-GSSG ratio), which forms the major redox couple in cells. We did not analyze the thioredoxin system and the pro-oxidant cytokine levels in the plasma and other tissues,
A selection of published research by CMCC faculty 61 Duarte et al
such as a spinal cord and dorsal root ganglion of the I-AAI 4 rats. In future studies, investigating the effects of MASMT on ROS at treatment points will help to understand how AAI 4 modulates ROS activity over time. It is necessary to analyze the immobilization-induced muscle changes in future studies.
Future studies on this topic are needed to clarify the relationship between the AAI therapy and the oxidative stress parameters in the blood of immobilized rats and to determine the potential association between the oxidative markers and the antinociceptive effect of MASMT.
Conclusion
Our study showed that MASMT by application of the AAI 4 on lumbar segments L4-L5 induced an antinociceptive effect and a functional recovery of peripheral nerves in rats exposed to the knee immobilization. Also, our findings for the first time showed a modulatory effect of the AAI 4 on plasmatic ROS formation in rodents. Thereby, we speculated that the effects of MASMTonROSformationmaybecontributingtothe improvement of the sensorial and functional abnormalities post knee immobilization.
Funding sources and conflicts of interest
This study was supported by grants from Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). No conflicts of interest were reported for this study.
Contributorship information
Concept development (provided idea for the research): F.C.K.D. (uarte), C.K., W.A.P.
Design (planned the methods to generate the results): F.C.K.D., W.A.P.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): F.C.K.D., W.A.P.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): F.C.K.D., J.A.S., A.P.K.R., C.K., A.B.-K.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): F.C.K.D., C.K., W.A.P.
Literature search (performed the literature search): F.C.K. D., W.A.P.
Writing (responsible for writing a substantive part of the manuscript): F.C.K.D., W.A.P.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): F.C.K.D., C.K., W.A.P.
Practical Applications
• Manually assisted spinal manipulation therapy on lumbar segments improved hind paw mechanical allodynia, a clinical finding of central sensitization, caused by 4 weeks of knee immobilization.
• Manually assisted spinal manipulation therapy on lumbar segments recovered the peripheral nerve function and the locomotor activity impaired after 4 weeks of knee immobilization.
• Manually assisted spinal manipulation therapy on lumbar segments modulated systemic blood oxidative stress parameters, which might be contributing to the antinociceptive effects of SMT.
REFERENCES
1. Pickar JG, Sung PS, Kang Y, Ge W. Response of lumbar paraspinal muscles spindles is greater to spinal manipulative loading compared with slower loading under length control. Spine J. 2007;7(5):583-595.
2. Kolberg C, Horst A, Kolberg A, Belló-Klein A, Partata WA. Effects of high-velocity, low-amplitude manipulation on catalase activity in men with neck pain. J Manipulative Physiol Ther. 2010;33(4):300-307.
3. Chaibi A, Benth JS, Tuchin PJ, Russell MB. Chiropractic spinal manipulative therapy for cervicogenic headache: a study protocol of a single-blinded placebo-controlled randomized clinical trial. Springerplus. 2015;4(1):779.
4. Fuhr AW, Menke JM. Status of activator methods chiropractic technique, theory, and practice. J Manipulative Physiol Ther. 2005;28(2):e1-e20.
5. Kawchuk GN, Prasad NG, McLeod RC, Liddle T, Li T, Zhu Q. Variability of force magnitude and force duration in manual and instrument-based manipulation techniques. J Manipulative Physiol Ther. 2006;29(8):611-618.
6. Sullivan KA, Hill AE, Haussler KK. The effects of chiropractic, massage and phenylbutazone on spinal mechanical nociceptive thresholds in horses without clinical signs. Equine Vet J. 2008;40 (1):14-20.
7. Coetzee N. The effect of the activator adjusting instrument in the treatment of chronic sacroiliac joint syndrome [master’s dissertation]. Durban, South Africa: Durban University of Technology; 2014.
8. Boal RW, Gillette RG. Central neuronal plasticity, low back pain and spinal manipulative therapy. J Manipulative Physiol Ther. 2004;27(5):314-326.
9. Reed WR, Cao DY, Long CR, Kawchuk GN, Pickar JG. Relationship between biomechanical characteristics of spinal manipulation and neural responses in an animal model: effect of linear control of thrust displacement versus force, thrust amplitude, thrust duration, and thrust rate. Evid Based Complement Alternat Med. 2013;2013:1-12.
10. Trierweiler J, Göttert DN, Gehlen G. Evaluation of mechanical allodynia in an animal immobilization model using the von Frey method. J Manipulative Physiol Ther. 2012;35(1):18-25.
11. Duarte FCK, Kolberg C, Barros RR, et al. Evaluation of peak force of a manually operated chiropractic adjusting instrument with an adapter for use in animals. J Manipulative Physiol Ther. 2014;37(4):236-241.
12. Ianuzzi A, Pickar JG, Khalsa PS. Determination of torque-
CMCC Research Report 2018–2020 62
limits for human and cat lumbar spine specimens during displacement-controlled physiological motions. Spine. 2009; 9(1):77-86.
13. Kolberg C, Horst A, Moraes MS, et al. Peripheral oxidative stress blood markers in patients with chronic back or neck pain treated with high-velocity, low-amplitude manipulation. J Manipulative Physiol Ther. 2015;38(2):119129.
14. Poljsak B, Suput D, Milisav I. Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxidative Med Cell Longev. 2013;2013:1-12.
15. Lee AS, Ellman MB, Yan D, et al. A current review of molecular mechanisms regarding osteoarthritis and pain. Gene. 2013;527 (2):440-447.
16. Riffel APK, de Souza JA, Maria do Carmo QS, et al. Systemic administration of vitamins C and E attenuates nociception induced by chronic constriction injury of the sciatic nerve in rats. Brain Res Bull. 2016;121:169-177.
17. Ji G, Neugebauer V. Reactive oxygen species are involved in group I mGluR-mediated facilitation of nociceptive processing in amygdala neurons. J Neurophysiol. 2010;104(1):218-229.
18. Schwartz ES, Kim HY, Wang J, et al. Persistent pain is dependent on spinal mitochondrial antioxidant levels. J Neurosci. 2009;29 (1):159-168.
19. Scheid T, Dal Bosco L, Guedes RP, Pavanato MA, BellóKlein A, Partata WA. Sciatic nerve transection modulates oxidative parameters in spinal and supraspinal regions. Neurochem Res. 2013;38(5):935-942.
20. Hamaue Y, Nakano J, Sekino Y, et al. Immobilizationinduced hypersensitivity associated with spinal cord sensitization during cast immobilization and after cast removal in rats. J Physiol Sci. 2013;63(6):401-408.
21. Bolzoni F, Bruttini C, Esposti R, Cavallari P. Hand immobilization affects arm and shoulder postural control. Exp Brain Res. 2012;220(1):63-70.
22. Beckenkamp PR, Lin CWC, Chagpar S, Herbert RD, van der Ploeg HP, Moseley AM. Prognosis of physical function following ankle fracture: a systematic review with metaanalysis. J Orthop Sports Phys Ther. 2014;44(11):841-851.
23. Alves JSM, Leal-Cardoso JH, Santos-Junior FFU, et al. Limb immobilization alters functional electrophysiological parameters of sciatic nerve. Braz J Med Biol Res. 2013;46(8):715-721.
24. Sameda H, Takahashi Y, Takahashi K, Chiba T, Ohtori S, Moriya H. Primary sensory neurons with dichotomizing axons projecting to the facet joint and the sciatic nerve in rats. Spine. 2001;26(10):1105-1109.
25. Gwak YS, Hassler SE, Hulsebosch CE. Reactive oxygen species contribute to neuropathic pain and locomotor dysfunction via activation of CamKII in remote segments following spinal cord contusioninjuryinrats.Pain. 2013;154(9):1699-1708.
26. He X, Dishman V. Spinal motor neuronal degeneration after knee joint immobilization in the guinea pig. J Manipulative
Physiol Ther. 2010;33(5):328-337.
27. Kato N, Matsumoto M, Kogawa M, Atkins GJ, Findlay DM, Fujikawa T. Critical role of p38 MAPK for regeneration of the sciatic nerve following crush injury in vivo. J Neuroinflammation. 2013;10(1):757.
28. deMedinaceli L, Freed WJ, Wyatt RJ. An index of the functional condition of rat sciatic nerve based on measurements made from walking tracks. Exp Neurol. 1982;77(3):634-643.
29. Bain JR, Mackinnon SE, Hunter DA. Functional evaluation of complete sciatic, peroneal, and posterior tibial nerve lesions in the rat. Plast Reconstr Surg. 1989;83(1):129-136.
30. Gamper N, Ooi L. Redox and nitric oxide-mediated regulation of sensory neuron ion channel function. Antioxid Redox Signal. 2015;22(6):486-504.
31. Sodergren E, Nourooz-Zadeh J, Berglund L, Vessby B. Reevaluation of the ferrous oxidation in xylenol orange assay for the measurement of plasma lipid hydroperoxides. J Biochem Biophys Methods. 1998;37(3):137-146.
32. Jiang ZY, Woolllard ACS, Wolff SP. Lipid hydroperoxide measurement of oxidation of Fe+2 in the presence of xylenol orange. Comparison with the TBA assay and an iodometric method. Lipids. 1991;26(10):853-856.
33. Granger DL, Anstey NM, Miller WC, Weinberg JB. Measuring nitric oxide production in human clinical studies. Methods Enzymol. 1999;301(1992):49-61.
34. Misra HP, Fridovich I. The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. JBiolChem.1972;247(10):3170-3175.
35. Flohé L, Günzler WA. Assays of glutathione peroxidase. Methods Enzymol. 1984;105:114-121.
36. Aebi H. Catalase in vitro. Methods Enzymol. 1984;105:121-126.
37. Lowry OH, Rosebrough NJ, Lewis Farr A, Randall RJ. Protein measurement with the Folin phenol reagent. JBiolChem.1951; 193:265-275.
38. Sivilotti L, Woolf CJ. The contribution of GABAA and glycine receptors to central sensitization: disinhibition and touch-evoked allodynia in the spinal cord. J Neurophysiol. 1994;72(1):169-179.
39. Decosterd I, Woolf CJ. Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain. 2000;87(2):149-158.
40. Sterling M, Jull G, Wright A. The effect of musculoskeletal pain on motor activity and control. JPain.2001;2(3):135-145.
41. Tal M, Wall PD, Devor M. Myelinated afferent fiber types that become spontaneously active and mechanosensitive following nerve transection in the rat. Brain Res. 1999;824(2):218-223.
42. Mannion RJ, Costigan M, Decosterd I, et al. Neurotrophins: peripherally and centrally acting modulators of tactile stimulus-induced inflammatory pain hypersensitivity. Proc Natl Acad Sci USA.1999;96(16):9385-9390.
43. Srbely J. Chiropractic science: a contemporary neurophysiologic paradigm. J Can Chiropr Assoc. 2010;54(3):144.
A selection of published research by CMCC faculty 63 Duarte et al
44. Pickar JG, Wheller JD. Response of muscle proprioceptors to spinal manipulative-like loads in the anesthetized cat. J Manipulative Physiol Ther. 2001;24(1):2-11.
45. Song XJ, Gan Q, Cao JL, Wang ZB, Rupert RL. Spinal manipulation reduces pain and hyperalgesia after lumbar intervertebral foramen inflammation in the rat. J Manipulative Physiol Ther. 2006;29(1):5-13.
46. Crosby ND, Weisshaar CL, Smith JR, Zeeman ME, Goodman-Keiser MD, Inkelstein BA. Burst and tonic spinal cord stimulation differentially activate GABAergic mechanisms to attenuate pain in a rat model of cervical radiculopathy. IEEE Trans Biomed Eng. 2015;62(6):16041613.
47. Haavik H, Niazi IK, Holt K, Murphy B. Effects of 12 weeks of chiropractic care on central integration of dual somatosensory input in chronic pain patients: a preliminary study. J Manipulative Physiol Ther. 2017;40(3):127-138.
48. Horst A, Kolberg C, Moraes MS, et al. Effect of N-acetylcysteine on the spinal-cord glutathione system and nitric-oxide metabolites in rats with neuropathic pain. Neurosci Lett. 2014;569:163-168.
49. Goecks CSB, Horst A, Moraes MS, et al. Assessment of oxidative parameters in rat spinal cord after chronic constriction of the sciatic nerve. Neurochem Res. 2012;37 (9):1952-1958.
50. Pierre N, Appriou Z, Gratas-Delamarche A, Derbré F. From physical inactivity to immobilization: Dissecting the role of oxidative stress in skeletal muscle insulin resistance and atrophy. Free Radic Biol Med. 2016;98:197-207.
51. Kaminskyy VO, Zhivotovsky B. Free radicals in cross talk between autophagy and apoptosis. Antioxid Redox Signal. 2014; 21(1):86-102.
52. Sottero B, Rossin D, Poli G, Biasi F. Lipid oxidation products in the pathogenesis of inflammation-related gut diseases. Curr Med Chem. 2018;25(11):1311-1326.
53. Robaczewska J, Kedziora-Kornatowska K, Kozakiewicz M, et al. Role of glutathione metabolism and glutathionerelated antioxidant defense systems in hypertension. J Physiol Pharm. 2016;67 (3):331-337.
54. Loperena R, Harrison DG. Oxidative stress and hypertensive diseases. MedClinNorthAm.2017;101(1):169-193.
55. Zhou Z, Liang Y, Deng F, et al. Phosphorylated neuronal nitric oxide synthase in neuropathic pain in rats. Int J Clin Exp Pathol. 2015;8(10):12748-12756.
56. Pamplona R, Costantini D. Molecular and structural antioxidant defenses against oxidative stress in animals. Am J Physiol Regul Integr Comp Physiol. 2011;301(4):R843-R863.
57. Singh S, Canseco DC, Manda SM, et al. Cytoglobin modulates myogenic progenitor cell viability and muscle regeneration. Proc Natl Acad Sci. 2014;111(1):E129-E138.
58. He M, Cai J, Go YM, et al. Identification of thioredoxin-2 as a regulator of the mitochondrial permeability transition. Toxicol Sci. 2008;105(1):44-50.
59. Incalza MA, D’Oria R, Natalicchio A, Perrini S, Laviola L, Giorgino F. Oxidative stress and reactive oxygen species in endothelial dysfunction associated with cardiovascular and metabolic diseases. Vasc Pharmacol. 2018;100:1-19.
OriginallypublishedintheJournalofManipulativeand PhysiologicalTherapeutics,2019Jul;42(6):385-398.Epub2019 Jul 30.
ReproducedwithpermissionfromElsevier
AccessOnline:https://doi.org/10.1016/j.jmpt.2018.11.023
CMCC Research Report 2018–2020 64
Comprehensive Nonsurgical Treatment Versus Self-directed Care to Improve Lumbar Spinal Stenosis: A Randomized Trial
Abstract
Objectives:
To compare the effectiveness of a comprehensive nonsurgical training program to a self-directed approach in improving walking ability in lumbar spinal stenosis (LSS).
Design:
Randomized controlled trial.
Setting:
Academic hospital outpatient clinic.
Participants:
Participants (N=104) with neurogenic claudication and imaging confirmed LSS were randomized. The mean age was 70.6 years, 57% were women, 84% had leg symptoms for >12 months, and the mean maximum walking capacity was 328.7 m.
Interventions:
A 6-week structured comprehensive training program or a 6-week self-directed program.
Main outcome measures:
Continuous walking distance in meters measured by the SelfPaced Walk Test (SPWT) and proportion of participants achieving at least 30% improvement (minimally clinically important difference [MCID]) in the SPWT at 6 months. Secondary outcomes included the Zurich Claudication Questionnaire (ZCQ), Oswestry Disability Index (ODI), ODI walk score, and the ShortForm General Health Survey subscales.
Results:
A total of 48 versus 51 participants who were randomized to comprehensive (n=51) or self-directed (n=53) treatment, respectively, received the intervention and 89% of the total study sample completed the study. At 6 months, the adjusted
mean difference in walking distance from baseline was 421.0 m (95% confidence interval [95% CI], 181.4-660.6), favoring the comprehensive program and 82% of participants in the comprehensive group and 63% in the self-directed group achieved the MCID (adjusted relative risk, 1.3; 95% CI, 1.0-1.7; P=.03). Both primary treatment effects persisted at 12 months favoring the comprehensive program. At 6 months, the ODI walk score and at 12 months the ZCQ, Medical Outcomes Study 36-Item Short-Form Health Survey-physical function and -bodily pain scores showed greater improvements favoring the comprehensive program.
Conclusions:
A comprehensive conservative program demonstrated superior, large, and sustained improvements in walking ability and can be a safe nonsurgical treatment option for patients with neurogenic claudication due to LSS.
OriginallypublishedinArchivesofPhysicalMedicineand Rehabilitation2018Dec;99(12):2408-2419.e2. Epub2018Jun 20.
ReproducedwithpermissionfromElsevierandAmerican CongressofRehabilitationMedicine.
AccessOnline:https://doi.org/10.1016/j.apmr.2018.05.014
A selection of published research by CMCC faculty 65
Ammendolia C 1, Côté P1, 2,5 , Southerst D 3 , Schneider M 4 , Budgell B5 , Bombardier C1, Hawker G1, Rampersaud YR6 1UniversityofToronto, 2UniversityofOntarioInstituteofTechnologyandUOIT-CMCCCentreforDisabilityPreventionandRehabilitation, 3New York University, 4UniversityofPittsburgh, 5CanadianMemorialChiropracticCollege, 6UniversityHealthNetwork
The Association Between Psychological and Social Factors and Spinal Pain in Adolescents
Batley S1 , Aartun E 2, 3 , Boyle E 4 ,5 , Hartvigsen J 4, 6 , Stern PJ1 , Hestbæk L 4, 6 1CanadianMemorialChiropracticCollege, 2UOIT-CMCCCentreforDisabilityPreventionandRehabilitation, 3UniversityofOslo, 4Universityof Southern Denmark, 5UniversityofToronto, 6NordicInstituteofChiropracticandClinicalBiomechanics
Abstract
Spinal pain, back pain, and/or neck pain begins early in life and is strongly associated with spinal pain in adulthood. Understanding the relationship between psychological and social factors and adolescent spinal pain may be important in both the prevention and treatment of spinal pain in this age group. We aimed to determine if psychological and social factors were associated with spinal pain in a cross-sectional study of a school-based cohort of 1279 Danish adolescents aged 11-13, who were categorized into “any” and “substantial” spinal pain. “Substantial spinal pain” was defined as a lifetime frequency of “sometimes” or “often” and a pain intensity of at least two on the revised Faces Pain Scale. Logistic regression analyses, stratified by sex, were conducted for single and all variables together. Eighty-six percent of participants reported “any spinal pain” and 28% reported “substantial spinal pain”. Frequency of psychological and social factors was significantly higher in those with spinal pain compared to those without. As the frequency of psychological and social factors increased, the odds of both “any spinal pain” and “substantial spinal pain” also increased.
Conclusion:
Psychological and social factors may be important determinants in adolescent spinal pain.
What is Known:
• Spinal pain begins early in life to reach adult levels by age 18. Spinal pain in adolescence is strongly associated with spinal pain in adulthood.
• In adults, psychological and social factors and spinal pain are strongly related; however, this relationship in adolescence is poorly understood.
What is New:
• Adolescents with spinal pain reported a significantly higher frequency of psychological factors and loneliness and lower levels of pupil acceptance.
• Adolescents reporting higher levels of loneliness, lower levels of pupil acceptance, and increased frequency of psychological factors had increased odds of reporting “substantial spinal pain”.
OriginallypublishedintheEuropeanJournalofPediatrics2019 Mar;178(3):275-286.Epub2018Nov21.
ReproducedwithpermissionfromSpringerNature.
AccessOnline:https://doi.org/10.1007/s00431-018-3291-y
CMCC Research Report 2018–2020 66
Development and Validation of a Model Predicting PostTraumatic Headache Six Months After a Motor Vehicle Collision in Adults
Cancelliere C 1,2 , Boyle E3, Côté P1,2,4.5,6 , Holm LW6 , Salmi LR5,6 , Cassidy JD 4 1OntarioTechUniversity, 2CentreforDisabilityPreventionandRehabilitation,OntarioTechUniversityandCanadianMemorialChiropracticCollege, 3UniversityofSouthernDenmark, 4UniversityofToronto, 5ResearchChairinDisabilityPreventionandRehabilitation, 6OntarioTechUniversity, 7Karolinska Institutet, 8ISPED/BordeauxSchoolofPublicHealth,UniversityofBordeaux
Abstract
Importance:
The prognosis of post-traumatic headache is poorly understood.
Objective:
To develop and validate a prognostic model to predict the presence of post-traumatic headache six months after a traffic collision in adults with incident post-traumatic headache.
Design:
Secondary analyses of adults with incident post-traumatic headache injured in traffic collisions between November 1997 and December 1999 in Saskatchewan, Canada (development cohort); and between January 2004 and January 2005 in Sweden (validation cohort).
Setting:
The Saskatchewan cohort (development) was population-based (N = 4162). The Swedish cohort (validation) (N = 379) were claimants from two insurance companies covering 20 % of cars driven in Sweden in 2004.
Participants:
All adults injured in traffic collisions who completed a baseline questionnaire within 30 days of collision. Excluded were those hospitalized >2 days, lost consciousness >30 min, or reported headache <3/10 on the numerical rating scale. Follow-up rates for both cohorts were approximately 80 %.
Predictors:
Baseline sociodemographic, pre-injury, and injury factors.
Outcome:
Self-reported headache pain intensity ≥3 (numerical rating scale) six months after injury.
Results:
Both cohorts were predominantly female (69.7 % in Saskatchewan, 65.2 % in Sweden), with median ages 35.9 years (Saskatchewan), and 38.0 years (Sweden). Predictors were age, work status, headache pain intensity, symptoms in arms or hands, dizziness or unsteadiness, stiffness in neck, pre-existing headache, and lower recovery expectations. With a positive score (i.e., ≥0.75 probability), the model can rule in the presence of post-traumatic headache at six months (development: specificity = 99.8 %, 95 % CI 99.5 %-99.9 %; sensitivity = 1.6 %, 95 % CI 1.0 %-2.6 %; positive likelihood ratio (LR+) = 8.0, 95 % CI 2.7-24.1; negative likelihood ratio (LR-) = 1.0, 95 % CI 1.0-1.0; validation: specificity = 95.5 %, 95 % CI 91.1 %-97.8 %; sensitivity = 27.2 %, 95 % CI 20.4 %-35.2 %); LR+ = 6.0, 95 % CI 2.8-13.2; LR- = 0.8, 95 % CI 0.7-0.8).
Conclusions and relevance: Clinicians can collect patient information on the eight predictors of our model to identify patients that will report ongoing posttraumatic headache six months after a traffic collision. Future research should focus on selecting patients at high risk of poor outcomes (using our model) for inclusion in intervention studies, and determining effective interventions for these patients.
OriginallypublishedinAccidentAnalysis&Prevention,2020 Jul;142:105580.Epub2020May20.
ReproducedwithpermissionfromElsevier.
AccessOnline: https://doi.org/10.1016/j.aap.2020.105580
A selection of published research by CMCC faculty 67
Clinical Outcomes in Neurogenic Claudication Using a Multimodal Program for Lumbar Spinal Stenosis: A Study of 49 Patients With Prospective Long-term Follow-up
Abstract
Objective:
The purpose of this study was to assess long-term outcomes of a 6-week multimodal program (manual therapy, exercises, and self-management strategies) in patients with neurogenic claudication due to degenerative lumbar spinal stenosis.
Methods:
This study evaluated 49 patients with neurogenic claudication who completed a 6-week multimodal program between 2010 and 2013. Outcomes included Oswestry Disability Index (ODI), Zurich Claudication Questionnaire (ZCQ), and Numeric Rating Scale. Mean differences, paired t tests, and the Wilcoxon ranksum test were used to compare outcomes at baseline, 6 weeks, and long-term follow-up.
Results:
Twenty-three patients completed the follow-up questionnaire (47% response rate). Median follow-up was 3.6 years (interquartile range: 3.3-4.6). The mean age was 73.5 years (standard deviation: 8.5). Between baseline and long-term follow-up, there were statistically significant and clinically important improvements in disability (ODI: -23.7 [95% confidence interval (CI): -15.7 to -31.6]; ODI walking item: -1.96
[95% CI: -1.34 to -2.57]; ZCQ function scale: -0.42 [95% CI: -0.10 to -0.70]) and pain (leg pain: -3.53 [95% CI: -1.80 to -5.20]; ZCQ symptom scale: -0.71 [95% CI: -0.30 to -1.10]), but not low back pain (Numeric Rating Scale: -1.03 [95% CI: -1.00 to 3.10]). There was no statistically significant change in any outcomes between 6 weeks and long-term follow-up.
Conclusion:
In a sample of patients with neurogenic claudication participating in a 6-week multimodal program, clinically important improvements in leg pain and disability, but not low back pain while walking, were maintained in the long term (median duration of 3.6 years) when compared to baseline.
OriginallypublishedintheJournalofManipulativeand PhysiologicalTherapeutics,2019Apr24.pii:S01614754(18)30125-8.[Epubaheadofprint].
ReproducedwithpermissionfromElsevier.
AccessOnline:https://doi.org/10.1016/j.jmpt.2018.11.004
CMCC Research Report 2018–2020 68
Chow NW 1,2 , Southerst D 3 , Wong JJ 2,4 , Kopansky-Giles D 2,5 , Ammendolia A 2,6 1McMasterUniversity, 2CanadianMemorialChiropracticCollege, 3NewYorkUniversityLangoneHealth, 4UniversityofOntarioInstituteofTechnologyCMCCCentrefortheStudyofDisabilityPreventionandRehabilitation, 5UniversityofToronto
The Safety of Spinal Manipulative Therapy in Children Under 10 Years: A Rapid Review
Corso M1, Cancelliere C 1, Mior S1, 2 , Taylor-Vaisey A1, Côté P1,2 1CMCC-UOITCentreforDisabilityPreventionandRehabilitation, 2CanadianMemorialChiropracticCollege
Abstract
Introduction:
The safety of spinal manipulative therapy (SMT) in children is controversial. We were mandated by the College of Chiropractors of British Columbia to review the evidence on this issue.
Objectives:
We conducted a rapid review of the safety of SMT in children (< 10 years). We aimed to: 1) describe adverse events; 2) report the incidence of adverse events; and 3) determine whether SMT increases the risk of adverse events compared to other interventions.
Evidence review:
We searched MEDLINE, CINAHL, and Index to Chiropractic Literature from January 1, 1990 to August 1, 2019. We used rapid review methodology recommended by the World Health Organization. Eligible studies (case reports/series, cohort studies and randomized controlled trials) were critically appraised. Studies of high and acceptable methodological quality were included. The lead author extracted data. Data extraction was independently validated by a second reviewer. We conducted a qualitative synthesis of the evidence.
Findings:
Most adverse events are mild (e.g., increased crying, soreness). One case report describes a severe adverse event (rib fracture in a 21-day-old) and another an indirect harm in a 4-month-old. The incidence of mild adverse events ranges from 0.3% (95% CI: 0.06, 1.82) to 22.22% (95% CI: 6.32, 54.74). Whether SMT increases the risk of adverse events in children is unknown.
Conclusion:
The risk of moderate and severe adverse events is unknown in children treated with SMT. It is unclear whether SMT increases the risk of adverse events in children < 10 years.
OriginallypublishedinChiropracticManualTherapies,2020 Feb25;28(1):12.
OpenaccessarticlereproducedunderthetermsoftheCreative CommonsAttribution4.0InternationalLicense(http:// creativecommons.org/licenses/by/4.0).
AccessOnline:https://doi.org/10.1186/s12998-020-0299-y
A selection of published research by CMCC faculty 69
Symptoms Patients Receiving Manual Therapy Experienced and Perceived as Adverse: A Secondary Analysis of a Survey of Patients’ Perceptions of What Constitutes an Adverse Response
Funabashi M1, Carlesso LC 2
1CanadianMemorialChiropracticCollege, 2McMasterUniversity
Abstract
Background:
Previous qualitative studies demonstrated that the process by which patients determined whether a response to manual therapy is adverse is very complex. However, it remains unknown which responses to manual therapy patients perceived as adverse.
Objective:
To describe symptoms patients experienced and perceived as adverse following manual therapy and to explore predictors of adverse responses (AR) for the body region with the greatest number of AR. We hypothesized that patients receiving manual therapy for neck conditions would present with more symptoms perceived as AR.
Methods:
This was a secondary analysis of a previous cross-sectional survey of 324 patients receiving manual therapy from Canadian physiotherapists. It included questions regarding symptoms patients experienced after a treatment including manual therapy and perceived as adverse. Poisson and negative binomial regression were used to determine factors associated with the number of symptoms that patients experienced and perceived as adverse.
Results:
Symptoms that affected patient’s functionality were most often perceived as AR. The neck region was the body part with the greatest number of perceived AR (n = 83). Patients with neck pain who agreed that education may change their experience with AR had a lower incidence rate of AR.
Conclusion:
Findings indicate that communication regarding post-treatment symptoms between clinicians and patients is important and can potentially influence patients’ perception of post-treatment symptoms.
OriginallypublishedintheJournalofManual&Manipulative Therapy.Thisisan‘OriginalManuscript’ofanarticlepublished byTaylor&FrancisGroupinJournalofManual&Manipulative Therapyon13May2020.Onlineaheadofprint.
ReproducedwithpermissionfromtheauthorsandTaylor& Francis.
AccessOnline:https://doi.org/10.1080/10669817.2020.1761139
CMCC Research Report 2018–2020 70
Clinical Scenarios for Which Cervical Mobilization and Manipulation Are Considered by an Expert Panel to be Appropriate (and Inappropriate) for Patients with Chronic Neck Pain
Herman PM 1 , Vernon H 2 , Hurwitz EL 3 , Shekelle PG 1, Whitley MD 1, Coulter ID 1 1RANDCorporation, 2CanadianMemorialChiropracticCollege, 3UniversityofHawai’iatManoa
Abstract
Objective:
Cervical mobilization and manipulation are 2 therapies commonly used for chronic neck pain (CNP). However, safety, especially of cervical manipulation, is controversial. This study identifies the clinical scenarios for which an expert panel rated cervical mobilization and manipulation as appropriate and inappropriate.
Methods:
An expert panel, following a well-validated modified-Delphi approach, used an evidence synthesis and clinical acumen to develop and then rate the appropriateness of cervical mobilization and manipulation for each of an exhaustive list of clinical scenarios for CNP. Key patient characteristics were identified using decision tree analysis (DTA).
Results:
Three hundred seventy-two clinical scenarios were defined and rated by an 11-member expert panel as to the appropriateness of cervical mobilization and manipulation. Across clinical scenarios more were rated inappropriate than appropriate for both therapies, and more scenarios were rated inappropriate for manipulation than mobilization. However, the number of patients presenting with each scenario is not yet known. Nevertheless, DTA indicates that all clinical scenarios that included red flags (eg, fever, cancer, inflammatory arthritides, or vasculitides), and some others involving major neurological findings, especially if previous manual therapy was unfavorable,
were rated as inappropriate for both cervical mobilization and manipulation. DTA also identified the absence of cervical disk herniation, stenosis, or foraminal osteophytosis on additional testing as the most important patient characteristic in predicting ratings of appropriate.
Conclusions:
Clinical guidelines for CNP should include information on the clinical scenarios for which cervical mobilization and manipulation were found inappropriate, including those with red flags, and others involving major neurological findings if previous manual therapy was unfavorable.
OriginallypublishedinTheClinicalJournalofPain,ClinJPain. 2020Apr;36(4):273-280.
ReproducedwithpermissionfromWoltersKluwerHealth,Inc.
AccessOnline:https://doi.org/10.1097/AJP.0000000000000800
A selection of published research by CMCC faculty 71
Trajectories of Pain Intensity Over 1 Year in Adults With Disabling Subacute or Chronic Neck Pain
Pico-Espinosa OJ 1, Côté P 2 , Hogg-Johnson S2 , Jensen I 3 , Axén I 3 , Holm LW1, Skillgate E1, 4 1MusculoskeletalandSportsInjuryEpidemiologyCenter, 2UOIT-CMCCCentrefortheStudyofDisabilityPreventionandRehabilitation, 3Karolinska Institute, 4Naprapathögskolan-ScandinavianCollegeofNaprapathicManualMedicine
Abstract Objective:
The objectives of this study were to describe the 1-year trajectories of disabling subacute or persistent neck pain and to investigate whether baseline age, sex, pain characteristics, and depressive symptoms are associated with such trajectories.
Study design and setting: Participants (n=617) included in a randomized controlled trial provided weekly pain intensity ratings by responding to text messages over 1 year. We used latent class mixed model analyses to identify clusters of individual trajectories. Thereafter, we used logistic regression to determine the association between baseline age, sex, pain characteristics, depressive symptoms and treatment, and trajectories of neck pain.
Results:
Six different clusters of trajectories were identified. Most participants (73%) followed a trajectory of decreasing pain throughout follow-up. The remaining experienced unfavorable trajectories: persistent pain of high intensity (22%) and slightly (3%) or highly (2%) fluctuating levels of pain reaching high levels of pain intensity. Pain intensity at baseline: odds ratio (OR): 3.76 (95% confidence interval [CI]: 2.49-5.68), depressive symptoms:
OR: 3.46 (95% CI: 2.01-5.95), younger age: OR: 2.29 (95% CI: 1.48-3.54), female sex: OR: 1.51 (95% CI: 1.01-2.26), and sudden onset of pain: OR: 1.74 (95% CI: 1.13-2.69) were associated with unfavorable trajectories.
Conclusions:
Most individuals with disabling subacute or chronic neck pain show improvement in pain intensity over a year. However, a quarter present unfavorable trajectories. High pain intensity at baseline, depressive symptoms, younger age, female sex, and sudden onset of pain are factors associated with unfavorable trajectories.
OriginallypublishedintheClinicalJournalofPain2019Aug; 35(8):678–685
ReproducedwithpermissionfromWalter-Kluwer.
AccessOnline:https://doi.org/10.1097/ajp.0000000000000727
CMCC Research Report 2018–2020 72
Perioperative Pain Management and Chronic Postsurgical Pain After Elective Foot and Ankle Surgery: A Scoping Review
Stiegelmar C1, Li Y1,2 , Beaupre LA1,3 , Pedersen MA1, Dillane D2 , Funabashi M2,3 1UniversityofAlberta, 2Alberta Health Services, 3CanadianMemorialChiropracticCollege
Abstract
Purpose:
Chronic postsurgical pain (CPSP) can occur after elective mid/ hindfoot and ankle surgery. Effective treatment approaches to prevent the development of CPSP in this population have not been extensively investigated. The impact of multimodal strategies to prevent CPSP following elective mid/hindfoot surgery is unknown because of both the heterogeneity of acute pain management and the lack of a recognized definition particular to this surgery. This review aimed to identify and evaluate current pain management strategies after elective mid/ hindfoot and ankle surgery.
Sources:
Manual and electronic searches (MEDLINE, Embase, and Cochrane Library) were conducted of literature published between 1990 and July 2017. Comparative studies of adults undergoing elective mid/hindfoot and ankle surgery were included. Two reviewers independently reviewed studies and assessed their methodological quality.
Principal findings:
We found seven randomized-controlled trials meeting our inclusion criteria. Interventions focused on regional anesthesia
techniques such as continuous popliteal sciatic and femoral nerve blockade. Participants were typically followed up to 48 hr postoperatively. Only one study assessed pain six months following elective mid/hindfoot and ankle surgery.
Conclusion:
There is an overwhelming lack of evidence regarding CPSP and its management for patients undergoing elective mid/hindfoot and ankle surgery. The lack of a recognized and standard definition of CPSP after this group of surgeries precludes accurate and consistent evaluation.
OriginallypublishedintheCanadianJournalofAnesthesia/ Journalcanadiend'anesthésie 2019Aug;66(8):953-965.Epub 2019Apr24.
ReproducedwithpermissionfromSpringerNature.
AccessOnline:https://doi.org/10.1007/s12630-019-01370-3
A selection of published research by CMCC faculty 73
A Pilot Study Assessing Patient-Centred Care in Patients with Chronic Health Conditions Attending Chiropractic Practice
Stuber KJ1 , Langweiler M2 , Mior S1 , McCarthy PW1 1CanadianMemorialChiropracticCollege, 2UniversityofSouthWales,Treforest
Abstract
Objectives:
The primary aim of this pilot study was to determine the feasibility of conducting a mixed- methods study assessing the extent patients with chronic health conditions perceive chiropractic care to be patient-centred.
Design:
A sequential mixed methods feasibility study with a quantitative priority.
Setting:
Two private chiropractic clinics in Calgary, Alberta, Canada.
Main outcome measures:
Feasibility outcomes included pilot study participation, consent and completion rates. Demographic and health information and a modified version of the Patient Assessment of Chronic Illness Care (PACIC).
Results:
Over three weeks, 90 participants were recruited, 86 enrolled, and 78 provided complete data, with only one who commented on the clarity of paperwork. Included participants were on average 47.1 years of age and 60.3% were female. They had an average of 1.8 chronic conditions with 60% having chronic
spinal pain. They reported seeing an average of 2.9 other health professionals for their chronic health condition and averaged 12.9 chiropractic visits in the past year. The average overall modified PACIC score was 3.29 on a 5-point scale. Higher scores were seen on the ‘patient activation’, ‘delivery system design/ decision support’, and ‘problem solving/contextual’ subscales, with lower scores seen on the ‘goal-setting/tailoring’ and ‘follow-up/coordination’ subscales. Interview data generally supported those findings.
Conclusions:
The pilot study results support the feasibility of the methods for a subsequent large-scale study. These preliminary results suggest that the degree of patient-centredness compares favourably to similar studies in primary medical care.
OriginallypublishedinComplementaryTherapiesinMedicine, 2018Aug;39:1-7.
ReproducedwithpermissionfromElsevier.
AccessOnline:https://doi.org/10.1016/j.ctim.2018.05.006
CMCC Research Report 2018–2020 74
Biomechanical Matching of Low Back External Demands During the Open- and Closed-Chain Side Bridge
Tuff T1, Beach TAC 2 , Howarth SJ1 1CanadianMemorialChiropracticCollege, 2UniversityofToronto
Abstract
Background:
The side-bridge (SB) is a commonly used closed-chain task to assess trunk muscle endurance and side-to-side endurance asymmetry. An open-chain variation of the SB, that positions the participant in an inclined side-lying posture, may be useful for those who report shoulder pain or fatigue as the reason for terminating the closed-chain SB. Low back loading demands of the open- and closed-chain variations should be matched to facilitate comparison of SB endurance measures.
Purpose:
To quantify the low back reaction moments during the open- and closed-chain SB and determine the appropriate open-chain angle of inclination that matches the lateral bend moment magnitude of the closed-chain SB.
Study design:
Observational cohort.
Methods:
Upper body and trunk postural data were obtained during the closed-chain SB and during the open-chain SB at each of four inclination angles from a group of eight healthy male adults. Ground reaction force (GRF) data were also collected during the closed-chain SB. Low back reaction moments were calculated using a static ‘top-down’ linked segment model in both SB variations. Latent growth modeling was used to determine the angle of inclination in the open-chain SB that produced a low back lateral bend moment that matched the closed-chain SB. Sensitivity of the matching open-chain inclination angle was evaluated by rotating the measured GRF vector from the closedchain SB by five degrees clockwise and counter-clockwise in the frontal plane.
Results:
The open-chain inclination angle that best matched the loading demands of the closed-chain SB was 38 ± 12 degrees. Clockwise rotation of the measured GRF in the closed-chain SB increased the matching inclination angle to 56 ± 17 degrees. Counterclockwise rotation reduced the matching inclination angle to 17 ± 11 degrees. Secondary descriptive analysis of spine posture and off-axis low back moments revealed biomechanically relevant differences between SB positions.
Conclusion:
The average open-chain SB angle of inclination that matched the closed-chain SB approximated the 45-degree recommendation offered in the literature. Differences in spine posture and offaxis low back reaction moments, and the potential impact on holding times, should be considered if using the open-chain SB.
OriginallypublishedinTheSportsPhysicalTherapySectionof theAmericanPhysicalTherapyAssociation,2020Feb;15(1):5363.
ReproducedwithpermissionfromtheNorthAmericanJournal ofSportsandPhysicalTherapy.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7015030/
A selection of published research by CMCC faculty 75
Prevalence of Low Back Pain, Pelvic Girdle Pain, and Combination Pain in a Pregnant Ontario Population
Weis CA1 , Barrett J2 , Tavares P1, Draper C 1 , Ngo K 3 , Leung J 3 , Huynh T 3 , Landsman V4 1CanadianMemorialChiropracticCollege, 2SunnybrookHealthSciencesCentre, 3Private Practice, 4UniversityofToronto,Toronto
Abstract
Objective:
The purpose of the current pilot study is to determine the point and period prevalence of site-specific back pain, low back pain (LBP), pelvic girdle pain (PGP), and combined pain (Combo Pain) in pregnant women at a large urban centre in Ontario.
Methods:
Point and period prevalence for LBP, PGP, and Combo Pain were determined using a questionnaire and accompanying pain diagram. Women were included in the study if they were healthy, of child-bearing age (18-45 years), currently experiencing a singleton pregnancy (any trimester), and proficient in the English language.
Results:
Data collected from 287 women were included in the analysis. Three-quarters of women suffered from some sort of pregnancy-related back pain. The point and period prevalences for women who were experiencing LBP, PGP, and Combo Pain were 15.7%, 17.8%, and 15.3% and 33.4%, 27.9%, and 30.7%, respectively. Secondary analyses demonstrated that increasing GA and suffering from both pains at some point prior to pregnancy (Prior Both) increased the risk of experiencing PGP and Combo Pain during pregnancy, respectively.
Conclusion:
The current study demonstrates that 76% of sampled women experienced pregnancy-related back pain and the prevalence of site-specific pain (LBP, PGP, and Combo Pain) increases with increased gestation. Risk factors include advanced GA and experiencing both types of pain prior to pregnancy (Prior Both). Furthermore, it is suggested that a standard definition of pain by location should be developed and employed so that future studies can elucidate appropriate prevention strategies and treatment options for each.
AccessOnline:https://doi.org/10.1016/j.jogc.2017.10.032
CMCC Research Report 2018–2020 76
OriginallypublishedintheJournalofObstetricsand GynaecologyCanada2018Aug;40(8):1038-1043. ReproducedwithpermissionfromElsevier.
The Influence of Hip Joint Angle on the Ratio Between Adduction and Abduction Torque in Experienced, Recreational Male Ice Hockey Players
Welsh P, Howitt S, Howarth SJ CanadianMemorialChiropracticCollege
Abstract
Background:
Strains of the adductor muscle group of the hip are common amongst ice hockey players. The ratio of isometric strengths between the hip adductors and abductors has been offered as a risk factor for hip adductor strain; however, there is no description for how the ratio between hip adductor and abductor strength varies as a function of hip abduction angle.
Hypothesis/purpose:
The aim of this study was to determine the influence of hip joint abduction angle on measured ratios of hip adduction to abduction torque in experienced, recreational, male hockey players. The primary null hypothesis for this study was that hip joint abduction angle would not influence hip adduction-toabduction torque ratios in male hockey players.
Study design:
Counterbalanced observational cohort.
Methods:
Twelve uninjured, male, recreational hockey players, with a minimum experience level of midget AAA/minor competitive or equivalent. Participants performed maximal isometric sidelying hip adduction and abduction exertions against a rigidly constrained load cell at 0, 10, and 20 degrees of hip abduction. Measured peak torques from each exertion were used to derive the hip adductor-to-abductor torque ratio. Kinematics of the trunk, pelvis, and lower limbs were monitored using an optoelectronic motion capture system.
Results:
Adductor-to-abductor torque ratio increased from 1.49 (SD = 0.20), to 1.92 (SD = 0.20) and to 2.30 (SD = 0.54) with successively increasing hip abduction angle (p < 0.001). Peak torque was significantly different between all angles (p ≤ 0.016) except between adduction exertions performed at 10 and 20 degrees of abduction (p = 0.895). Small changes in hip angle during the exertion were coincident with exertion direction, which confirmed the isometric nature of the task.
Conclusion:
Hip abduction angle has a significant impact on the measured adductor-to-abductor torque ratio. The ratio increased due to a combination of increased adductor torque and decreased abductor torque as the hip abduction angle increased.
Level of evidence: 2b.
OriginallypublishedinInternationalJournalofSportsPhysical Therapy2020Feb;15(1):22-33.
OpenaccessarticlereproducedunderCreativeCommons CCBY-NC-ND.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ pmc7015023/pdf/ijspt-15-22.pdf/
A selection of published research by CMCC faculty 77
The Passive Voice and Comprehensibility of Biomedical Texts: An Experimental Study with 2 Cohorts of Chiropractic Students
Millar N1, Budgell B2 1UniversityofTsukuba, 2CanadianMemorialChiropracticCollege
Abstract
Objectives:
Authors in the health sciences are encouraged to write in the active voice in the belief that this enhances comprehensibility. Hence, the purpose of this study was to compare objectively measured and subjectively perceived comprehensibility of texts in which one voice or the other was highly prevalent.
Methods:
Objectively rated comprehensibility was obtained by presenting 161 2nd-year chiropractic students with questions pertaining to 2 methods sections of biomedical articles, each presented in its original form with high prevalence of the passive voice, and in a manipulated form with all main verbs in the active voice. The difficulties and sensitivities of questions were compared for the 2 forms of each text. Comprehensibility was obtained by asking students to rate the comprehensibility of authentic sentences from biomedical manuscripts and matched manipulated form in which the voice of the main verb had been changed. Differences in comprehensibility between the 2 texts were assessed with a dependent t test.
Results:
There were no significant differences in the difficulties or sensitivities of questions pertaining to the 2 original texts written in the passive voice versus the active voice (p> .35 for all comparisons). Students rated sentences written in the passive voice as marginally more comprehensible than sentences written in the active voice (p = .003 per 2-tailed paired t test).
Conclusion:
The texts written in the active voice were not more comprehensible than texts written in the passive voice. The results of this study do not support editorial guidelines that favor active voice over passive voice.
Introduction
Writings in the health sciences tend to be complex. This is natural, given what are often the relatively esoteric themes and the argumentative (in a scientific sense) nature of writings in the health sciences; for example, establishing cause-effect relationships
from samples of populations. Efforts to render such writing more comprehensible are therefore laudable, especially as English becomes the lingua franca of health sciences education and research worldwide. As increasing numbers of health professionals undergo training in English, it becomes apparent that the language of their chosen discipline may present challenges.1,2 This is likely as true for chiropractic students as for students in other areas of the health sciences.3 Furthermore, even health sciences students who are so-called native English speakers may be challenged by the vocabulary and writing conventions in their chosen discipline.4
Thus, the more understandable learning resources are, the more efficient the learning process will be.5 The overabundance of articles on how to write readable medical prose is testimony to this conventional wisdom (eg, see Alexandrov,6 Bredan and van Roy,7 and Steen8). However, commonly proposed strategies for comprehensible writing may not be grounded in good evidence. For example, it is not uncommon to see writers encouraged to favor the active voice over the passive voice—‘‘the doctor treated the patient’’ versus ‘‘the patient was treated by the doctor’’— perhaps based on the misconception that the passive voice results in longer and less-comprehensible constructions. Even the American Medical Association Manual of Style continues to encourage authors to ‘‘use active voice whenever possible,’’9 while the British Medical Journal still advises authors to ‘‘use active voice but avoid ‘we did’ or ‘we found.’’’10
On the other hand, it has recently been argued that there are instances in medical writing in which the passive voice is preferable to the active voice, and that sweeping editorial guidelines may be overly simplistic and so do not serve their intended purpose.11 To date, however, no experimental studies have challenged the assumption of enhanced comprehensibility for the active voice. In this age of evidence-based care, it is somewhat ironic that the teaching of health sciences literacy remains largely opinion based. Hence, the purpose of this study was to compare the comprehensibility of authentic samples of biomedical text expressed in the active and passive voices.
Methods
This study was approved by the research ethics board of Canadian Memorial Chiropractic College. As part of an annual
CMCC Research Report 2018–2020 78 Education in Healthcare
Table 1 Characteristics of 2 Convenience (Nonrandomized) Cohorts in Study of Comprehensibility of Passive Versus Active Voice Texts
Table1-Characteristicsof2Convenience(Nonrandomized)CohortsinStudyofComprehensibilityofPassive VersusActiveVoiceTexts
assessment of incoming students, 161 2nd-year chiropractic students were recruited into the study by an in-class announcement on September 10, 2012. Once seated in the testing room and in sequence according to their seating, the students alternatively received 1 of 2 forms of the assessment. Hence, the allocation to cohorts was not randomized. Nonetheless, post hoc analysis of the cohorts showed that they were quite similar (Table 1).
editorialguidelinesmaybeoverlysimplisticandsodonot servetheirintendedpurpose.11 Todate,however,no experimentalstudieshavechallengedtheassumptionof enhancedcomprehensibilityfortheactivevoice.Inthisage ofevidence-basedcare,itissomewhatironicthatthe teachingofhealthsciencesliteracyremainslargelyopinion based.Hence,thepurposeofthisstudywastocomparethe comprehensibilityofauthenticsamplesofbiomedicaltext expressedintheactiveandpassivevoices.
The assessments used 2 strategies to test the effect of the passive voice on the comprehensibility of biomedical texts
METHODS
1. Objectively Rated Comprehensibility
theoriginalandrewrittenversionsofthetexts.Additionally,theprofileofthevocabularywasobtainedby processingthetextsamplesusingtheonlinesoftware WebVPClassicv.4.0.14 Thus,thewordswithineach versionofeachtextsamplewereclassifiedasbelongingto (1)thegeneralservicelist,theapproximately2000most commonlyoccurringwordfamiliesintheEnglishlanguage;(2)theacademicwordlist,theapproximately570 wordfamilies,otherthangeneralservicelistwords, commonlyfoundinacademicwritings;and(3)allother wordsnotbelongingtothegeneralservicelistoracademic wordlist,so-called‘‘off-list’’words.Off-listwordsare morelikelytobetechnicalwordsspecifictothethemeof thetext.AsshowninTable2,thevocabularyprofileswere essentiallyunalteredbyrewritingthesampletextsinthe activevoice.
theme of the text. As shown in Table 2, the vocabulary profiles were essentially unaltered by rewriting the sample texts in the active voice.
The students were asked to answer 10 true-or-false questions dealing with each of the 2 texts. Applying item response theory, the difficulties and sensitivities of each of the 10 questions were calculated for each of the 2 forms (active voice versus passive voice) of the text. The difficulty of each question was defined as the mathematical inverse of the prevalence of correct answers. For example, if half of the students answered a question correctly, that question would have a difficulty of 2.0 (the inverse of 1/ 2). The sensitivity of each question was defined as the prevalence of correct answers among the top-scoring quartile of the cohort divided by the prevalence of correct answers among the bottom-scoring quartile of the cohort.
Thisstudywasapprovedbytheresearchethicsboardof CanadianMemorialChiropracticCollege.Aspartofan annualassessmentofincomingstudents,1612nd-year chiropracticstudentswererecruitedintothestudybyan in-classannouncementonSeptember10,2012.Once seatedinthetestingroomandinsequenceaccordingto theirseating,thestudentsalternativelyreceived1of2 formsoftheassessment.Hence,theallocationtocohorts wasnotrandomized.Nonetheless,posthocanalysisofthe cohortsshowedthattheywerequitesimilar(Table1).
Theassessmentsused2strategiestotesttheeffectofthe passivevoiceonthecomprehensibilityofbiomedicaltexts.
In the first instance, each of the 2 cohorts of students was presented with 1 sample of text in its original published form, with frequent use of the passive voice, and a sample of text in which the passive voice was replaced throughout the text with the active voice (text available from corresponding author). The text samples were extracted from the methods sections of 2 original research papers referenced within the undergraduate curriculum of the students.12,13 The comprehensibility of the 2 examples of biomedical text was tested in the original published form and in the rewritten form. Thus, in more detail, 1 cohort received the original version of text 1 and the rewritten version of text 2. The 2nd cohort received the rewritten version of text 1 and the original version of text 2.
1.ObjectivelyRatedComprehensibility
Thestudentswereaskedtoanswer10true-or-false questionsdealingwitheachofthe2texts.Applyingitem responsetheory,thedifficultiesandsensitivitiesofeachof the10questionswerecalculatedforeachofthe2forms (activevoiceversuspassivevoice)ofthetext.Thedifficulty ofeachquestionwasdefinedasthemathematicalinverse oftheprevalenceofcorrectanswers.Forexample,ifhalf ofthestudentsansweredaquestioncorrectly,that questionwouldhaveadifficultyof2.0(theinverseof1/ 2).Thesensitivityofeachquestionwasdefinedasthe prevalenceofcorrectanswersamongthetop-scoring quartileofthecohortdividedbytheprevalenceofcorrect answersamongthebottom-scoringquartileofthecohort.
Comparisons were also made between the raw and processed (see below) scores of the 2 cohorts for each of the 2 versions (original published form and rewritten form) of each of the 2 texts, essentially asking whether cohort scores were on average different depending on whether the text was presented in the active or passive voice. Raw scores were calculated simply as the percentage of correct answers. Processed scores were calculated by assigning each correct answer a weight equivalent to its calculated difficulty and then dividing the student’s score by the total weight of all questions..
2. Subjectively Rated Comprehensibility
Comparisonswerealsomadebetweentherawand processed(seebelow)scoresofthe2cohortsforeachof the2versions(originalpublishedformandrewrittenform) ofeachofthe2texts,essentiallyaskingwhethercohort scoreswereonaveragedifferentdependingonwhetherthe textwaspresentedintheactiveorpassivevoice.Raw scoreswerecalculatedsimplyasthepercentageofcorrect answers.Processedscoreswerecalculatedbyassigning eachcorrectansweraweightequivalenttoitscalculated difficultyandthendividingthestudent’sscorebythetotal weightofallquestions.
Twenty sentences were extracted from the Biomedical and Health Linguistics randomized controlled trials corpus11 and presented in their original form (active or passive voice) to 1 cohort and then in the alternate (rewritten) form (text available from corresponding author) to a second cohort; for example:
Active voice version presented to 1 cohort: Question 21. ‘‘We also observed this minimal level of correlation in the subgroup of patients who subsequently had recurrent coronary events (r = 0.1, P = 0.004).’’ New England Journal of Medicine
The readability statistics for the texts were obtained from the spelling and grammar checking function of Microsoft Word 2007 (Microsoft Corp, Redmond, WA), and as shown in Table 2, they were essentially identical for the original and rewritten versions of the texts. Additionally, the profile of the vocabulary was obtained by processing the text samples using the online software Web VP Classic v.4.0.14 Thus, the words within each version of each text sample were classified as belonging to (1) the general service list, the approximately 2000 most commonly occurring word families in the English language; (2) the academic word list, the approximately 570 word families, other than general service list words, commonly found in academic writings; and (3) all other words not belonging to the general service list or academic word list, so-called ‘‘off-list’’ words. Offlist words are more likely to be technical words specific to the
Inthefirstinstance,eachofthe2cohortsofstudents waspresentedwith1sampleoftextinitsoriginal publishedform,withfrequentuseofthepassivevoice, andasampleoftextinwhichthepassivevoicewas replacedthroughoutthetextwiththeactivevoice(text availablefromcorrespondingauthor).Thetextsamples wereextractedfromthemethodssectionsof2original researchpapersreferencedwithintheundergraduate curriculumofthestudents.12,13 Thecomprehensibilityof the2examplesofbiomedicaltextwastestedintheoriginal publishedformandintherewrittenform.Thus,inmore detail,1cohortreceivedtheoriginalversionoftext1and therewrittenversionoftext2.The2ndcohortreceivedthe rewrittenversionoftext1andtheoriginalversionoftext 2.
Thereadabilitystatisticsforthetextswereobtained fromthespellingandgrammarcheckingfunctionof MicrosoftWord2007(MicrosoftCorp,Redmond,WA), andasshowninTable2,theywereessentiallyidenticalfor
2.SubjectivelyRatedComprehensibility
Passive voice version presented to the other cohort: Question 21. ‘‘This minimal level of correlation was also observed in the subgroup of patients who subsequently had recurrent coronary events (r = 0.1, P = 0.004).’’ New England Journal of Medicine
TwentysentenceswereextractedfromtheBiomedical andHealthLinguisticsrandomizedcontrolledtrials corpus 11 andpresentedintheiroriginalform(activeor passivevoice)to1cohortandtheninthealternate (rewritten)form(textavailablefromcorresponding author)toasecondcohort;forexample:
Activevoiceversionpresentedto1cohort:Question21. ‘‘Wealsoobservedthisminimallevelofcorrelationinthe subgroupofpatientswhosubsequentlyhadrecurrent coronaryevents(r ¼ 0.1, P ¼ 0.004).’’ NewEnglandJournal ofMedicine
Each version of the test contained the same number of sentences in each voice. Hence, within each cohort (ie, version of the test), students were presented with 10 original and 10 rewritten sentences, and among these sentences, 10 were in the active voice and 10 were in the passive voice. The sentences came from the ‘‘big five’’ medical journals: Journal of the American Medical Association, New England Journal of Medicine, Annals of Internal Medicine, British Medical Journal, and the Lancet. Students were asked to subjectively rate the comprehensibility of each sentence using the following scale:
Passivevoiceversionpresentedtotheothercohort: Question21.‘‘Thisminimallevelofcorrelationwasalso observedinthesubgroupofpatientswhosubsequently hadrecurrentcoronaryevents(r ¼ 0.1, P ¼ 0.004).’’ New EnglandJournalofMedicine
Eachversionofthetestcontainedthesamenumberof sentencesineachvoice.Hence,withineachcohort(ie,
A selection of published research by CMCC faculty 79
Cohort1 (n ¼ 79) Cohort2 (n ¼ 82) Sex 39males, 40females 38males, 44females Meanage,y(range) 25(22–44)24(21–30) NativeEnglishspeakers 54(68%)59(72%) CompletedhighschoolinEnglish73(92%)79(96%) Obtainedundergraduatedegree44(54%)42(51%) Nonscience/healthdegrees2 2 JChiroprEduc2019Vol.33No.1 � DOI10.7899/JCE-17-22 � www.journalchiroed.com 17 Millar et all
Table2-ReadabilityStatisticsandVocabularyProfilesforTextsinOriginal(PassiveVoice)VersionsandRewritten (ActiveVoice)Versions
(ActiveVoice)Versions
Table 2 Readability Statistics and Vocabulary Profiles for Texts in Original (Passive Voice) Versions and Rewritten (Active Voice) Versions
1, completely clear; 2, quite clear; 3, moderately clear; 4, quite unclear; 5, completely unclear.
Seventy-eight complete copies of test 1 and 82 complete copies of test 2 were returned. The numerical ratings for the 2 versions of each sentence were averaged, and the averages for the active-voice and passive-voice versions of each sentence were compared using a paired, 2-tailed t test.
versionofthetest),studentswerepresentedwith10 originaland10rewrittensentences,andamongthese sentences,10wereintheactivevoiceand10wereinthe passivevoice.Thesentencescamefromthe‘‘bigfive’’ medicaljournals: JournaloftheAmericanMedical Association, NewEnglandJournalofMedicine, Annalsof InternalMedicine, BritishMedicalJournal,andthe Lancet. Studentswereaskedtosubjectivelyratethecomprehensibilityofeachsentenceusingthefollowingscale:1, completelyclear;2,quiteclear;3,moderatelyclear;4, quiteunclear;5,completelyunclear.
Results
versionofthetest),studentswerepresentedwith10 originaland10rewrittensentences,andamongthese sentences,10wereintheactivevoiceand10wereinthe passivevoice.Thesentencescamefromthe‘‘bigfive’’ medicaljournals: JournaloftheAmericanMedical Association, NewEnglandJournalofMedicine, Annalsof InternalMedicine, BritishMedicalJournal,andthe Lancet Studentswereaskedtosubjectivelyratethecomprehensibilityofeachsentenceusingthefollowingscale:1, completelyclear;2,quiteclear;3,moderatelyclear;4, quiteunclear;5,completelyunclear.
1. Objectively Rated Comprehensibility
Seventy-eightcompletecopiesoftest1and82complete copiesoftest2werereturned.Thenumericalratingsfor the2versionsofeachsentencewereaveraged,andthe averagesfortheactive-voiceandpassive-voiceversionsof eachsentencewerecomparedusingapaired,2-tailed t test.
2.SubjectivelyRatedComprehensibility
2.SubjectivelyRatedComprehensibility
AsshowninTable5andonthebasisofsubjectively ratedcomprehensibility,theversionsofsentencespresentedintheactivevoicewere,onaverage,somewhatless comprehensible(mean2.21,SD0.48)thantheversions presentedinthepassivevoice(mean2.07,SD0.47; p ¼ .003 per2tailed,paired t test).
The readability statistics and vocabulary profiles for the 2 texts are presented in Table 2 and suggest that the readabilities of the 2 versions of each text (supplementary files) were not substantially different.
Seventy-eightcompletecopiesoftest1and82complete copiesoftest2werereturned.Thenumericalratingsfor the2versionsofeachsentencewereaveraged,andthe averagesfortheactive-voiceandpassive-voiceversionsof eachsentencewerecomparedusingapaired,2-tailed t test.
RESULTS
1.ObjectivelyRatedComprehensibility
2. Subjectively Rated Comprehensibility
As shown in Table 5 and on the basis of subjectively rated comprehensibility, the versions of sentences presented in the active voice were, on average, somewhat less comprehensible (mean 2.21, SD 0.48) than the versions presented in the passive voice (mean 2.07, SD 0.47; p ¼ .003 per 2 tailed, paired t test).
DISCUSSION
AsshowninTable5andonthebasisofsubjectively ratedcomprehensibility,theversionsofsentencespresentedintheactivevoicewere,onaverage,somewhatless comprehensible(mean2.21,SD0.48)thantheversions presentedinthepassivevoice(mean2.07,SD0.47; p ¼ .003 per2tailed,paired t test).
Discussion
Thisstudychallengedthehypothesisthattextswritten intheactivevoicearemorecomprehensiblethantexts writteninthepassivevoice.Thestudywasconducted usingstudentswhowerejustcommencingtheir2ndyearof studyataCanadianchiropracticcollege.Hence,all studentsalreadypossessedatleastanundergraduate universitydegreeandhadcompleted1year(approximately1000classroomhours)ofadditionalstudyfocusingon
DISCUSSION
This study challenged the hypothesis that texts written in the active voice are more comprehensible than texts written in the passive voice. The study was conducted using students who were just commencing their 2nd year of study at a Canadian chiropractic college. Hence, all students already possessed at least an undergraduate university degree and had completed 1
Table 3 Difficulty and Sensitivity for Each of 10 Questions
RESULTS
1.ObjectivelyRatedComprehensibility
Table 3 shows, for text 1, the calculated difficulties and sensitivities of the 10 true-or-false questions when the text was presented in the passive versus the active voice. There was no statistically significant difference, per paired, 2-tailed t test, between the difficulties and sensitivities (p ¼ .69 and .35, respectively) for the true-or-false questions when tested against text 1 in the passive versus active voice.
Thereadabilitystatisticsandvocabularyprofilesforthe 2textsarepresentedinTable2andsuggestthatthe readabilitiesofthe2versionsofeachtext(supplementary files)werenotsubstantiallydifferent.
Thereadabilitystatisticsandvocabularyprofilesforthe 2textsarepresentedinTable2andsuggestthatthe readabilitiesofthe2versionsofeachtext(supplementary files)werenotsubstantiallydifferent.
Table 4 shows, for text 2, the calculated difficulties and sensitivities of the 10 true-or-false questions when the text was presented in the passive versus the active voice. There was no statistically significant difference, per paired, 2-tailed t test, between the difficulties and sensitivities (p ¼ .48 and .81, respectively) for the true-or-false questions when tested against text 2 in the passive versus active voice.
Table3shows,fortext1,thecalculateddifficultiesand sensitivitiesofthe10true-or-falsequestionswhenthetext waspresentedinthepassiveversustheactivevoice.There wasnostatisticallysignificantdifference,perpaired,2tailed t test,betweenthedifficultiesandsensitivities( p ¼ .69and.35,respectively)forthetrue-or-falsequestions whentestedagainsttext1inthepassiveversusactivevoice.
Table3shows,fortext1,thecalculateddifficultiesand sensitivitiesofthe10true-or-falsequestionswhenthetext waspresentedinthepassiveversustheactivevoice.There wasnostatisticallysignificantdifference,perpaired,2tailed t test,betweenthedifficultiesandsensitivities( p ¼ .69and.35,respectively)forthetrue-or-falsequestions whentestedagainsttext1inthepassiveversusactivevoice.
Table4shows,fortext2,thecalculateddifficultiesand sensitivitiesofthe10true-or-falsequestionswhenthetext waspresentedinthepassiveversustheactivevoice.There wasnostatisticallysignificantdifference,perpaired,2tailed t test,betweenthedifficultiesandsensitivities( p ¼ .48and.81,respectively)forthetrue-or-falsequestions whentestedagainsttext2inthepassiveversusactivevoice.
Table4shows,fortext2,thecalculateddifficultiesand sensitivitiesofthe10true-or-falsequestionswhenthetext waspresentedinthepassiveversustheactivevoice.There wasnostatisticallysignificantdifference,perpaired,2tailed t test,betweenthedifficultiesandsensitivities( p ¼ .48and.81,respectively)forthetrue-or-falsequestions
whentestedagainsttext2inthepassiveversusactivevoice.
Thisstudychallengedthehypothesisthattextswritten intheactivevoicearemorecomprehensiblethantexts writteninthepassivevoice.Thestudywasconducted usingstudentswhowerejustcommencingtheir2ndyearof studyataCanadianchiropracticcollege.Hence,all studentsalreadypossessedatleastanundergraduate universitydegreeandhadcompleted1year(approximately1000classroomhours)ofadditionalstudyfocusingon
Pertaining to Text 1, Which Was Presented in the Passive (Original) and Active (Manipulated) Voice
Table3-DifficultyandSensitivityforEachof10 QuestionsPertainingtoText1,WhichWasPresentedin thePassive(Original)andActive(Manipulated)Voice
Table3-DifficultyandSensitivityforEachof10 QuestionsPertainingtoText1,WhichWasPresentedin thePassive(Original)andActive(Manipulated)Voice
CMCC Research Report 2018–2020 80
Text 1.Cavanaughetal12 2.Dishmanetal13 Statistic\voice Passivevoice Activevoice Passivevoice Activevoice Words(tokens) 357 357 304 305 Characters 1857 1830 1591 1582 Paragraphs 1 1 1 1 Sentences 18 18 14 14 Sentences/paragraph 18.0 18.0 14.0 14.0 Words/sentence 19.8 19.8 21.7 21.7 Characters/word 5.0 5.0 5.1 5.0 Passivesentences 72% 0% 50% 0% Fleschreadingease 36.6 36.6 39.0 39.3 Flesch-Kincaidgradelevel 13.0 13.0 13.1 13.1 Generalservicelistwords 63% 63% 67% 67% Academicwordlistwords 11% 11% 7% 7% Off-listwords 26% 26% 26% 26% Types(uniquewords) 177 176 146 147 Type-tokenratio 0.48 0.48 0.47 0.47
Item Difficulty Sensitivity OriginalManipulatedOriginalManipulated 1 1.251.191.731.67 2 1.001.061.001.00 3 1.141.111.461.33 4 1.361.522.001.70 5 1.161.111.731.33 6 1.301.241.641.19 7 1.111.091.361.33 8 1.011.051.061.11 9 1.361.171.421.33 101.161.191.462.00 Mean (SD) 1.19 (0.13) 1.17 (0.14) 1.49 (0.31) 1.40 (0.30)
Text 1.Cavanaughetal12 2.Dishmanetal13 Statistic\voice Passivevoice Activevoice Passivevoice Activevoice Words(tokens) 357 357 304 305 Characters 1857 1830 1591 1582 Paragraphs 1 1 1 1 Sentences 18 18 14 14 Sentences/paragraph 18.0 18.0 14.0 14.0 Words/sentence 19.8 19.8 21.7 21.7 Characters/word 5.0 5.0 5.1 5.0 Passivesentences 72% 0% 50% 0% Fleschreadingease 36.6 36.6 39.0 39.3 Flesch-Kincaidgradelevel 13.0 13.0 13.1 13.1 Generalservicelistwords 63% 63% 67% 67% Academicwordlistwords 11% 11% 7% 7% Off-listwords 26% 26% 26% 26% Types(uniquewords) 177 176 146 147 Type-tokenratio 0.48 0.48 0.47 0.47
Table2-ReadabilityStatisticsandVocabularyProfilesforTextsinOriginal(PassiveVoice)VersionsandRewritten
Item Difficulty Sensitivity OriginalManipulatedOriginalManipulated 1 1.251.191.731.67 2 1.001.061.001.00 3 1.141.111.461.33 4 1.361.522.001.70 5 1.161.111.731.33 6 1.301.241.641.19 7 1.111.091.361.33 8 1.011.051.061.11 9 1.361.171.421.33 101.161.191.462.00 Mean (SD) 1.19 (0.13) 1.17 (0.14) 1.49 (0.31) 1.40 (0.30) 18 JChiroprEduc2019Vol.33No.1 � DOI10.7899/JCE-17-22 � www.journalchiroed.com
year (approximately 1000 classroom hours) of additional study focusing on human biology but also involving a yearlong course in critical appraisal of research literature. The texts presented in this experiment were therefore representative of the reading materials which the students would be expected to access in their current year of study.
Objective measures of readability and vocabulary profiles were obtained for 2 samples of text which, in their original forms, made extensive use of the passive voice, as is conventional in biomedical texts.11 When these texts were rewritten to eliminate the use of the passive voice, the changes in readability measures were miniscule or none. This contradicts the argument that the use of the passive voice produces more-complex or lesscomprehensible texts. Furthermore, when students were asked questions pertaining to the original (passive voice) versus rewritten (active voice) versions of the 2 texts, there were no statistical differences in the mean difficulties or sensitivities of the questions. The individual comprehension questions satisfactorily discriminated between different levels of reading ability among the students. Specifically, 36 of 40 questions had sensitivities of >1.00, while 4 of 40 questions had sensitivities just equal to 1.00, and so overall the questions provide a valid measure of the students’ reading comprehension. This indicates that the 2 versions of the same text were equally comprehensible to the students.
humanbiologybutalsoinvolvingayearlongcoursein criticalappraisalofresearchliterature.Thetextspresented inthisexperimentwerethereforerepresentativeofthe readingmaterialswhichthestudentswouldbeexpectedto accessintheircurrentyearofstudy.
Table 5 Subjectively Rated Comprehensibility for Sentences Presented in the Active and Passive Voice
When students were asked to subjectively rank the comprehensibility of sentences written in the active versus passive voice, they indicated that overall sentences presented in the passive voice were somewhat (and statistically significantly) more comprehensible. When compared with the objective measures of comprehensibility, this seems to reflect a bias on the students’ part in favor of the passive voice, and,
Table4-DifficultyandSensitivityforEachof10 QuestionsPertainingtoText2,WhichWasPresentedin thePassive(Original)andActive(Manipulated)Voice
Objectivemeasuresofreadabilityandvocabulary profileswereobtainedfor2samplesoftextwhich,intheir originalforms,madeextensiveuseofthepassivevoice,as isconventionalinbiomedicaltexts.11 Whenthesetexts wererewrittentoeliminatetheuseofthepassivevoice,the changesinreadabilitymeasureswereminisculeornone. Thiscontradictstheargumentthattheuseofthepassive voiceproducesmore-complexorless-comprehensibletexts. Furthermore,whenstudentswereaskedquestionspertainingtotheoriginal(passivevoice)versusrewritten (activevoice)versionsofthe2texts,therewereno statisticaldifferencesinthemeandifficultiesorsensitivities ofthequestions.Theindividualcomprehensionquestions satisfactorilydiscriminatedbetweendifferentlevelsof readingabilityamongthestudents.Specifically,36of40 questionshadsensitivitiesof .1.00,while4of40questions hadsensitivitiesjustequalto1.00,andsooverallthe questionsprovideavalidmeasureofthestudents’reading comprehension.Thisindicatesthatthe2versionsofthe sametextwereequallycomprehensibletothestudents.
whichthepassivevoicewastwiceratedasmuchmore comprehensiblethantheactivevoice.Theverb obtain was previouslyshowntohaveastrongaffinityforthepassive voiceinreportsofrandomizedcontrolledtrials.11 Onthe otherhand,otherverbswhichhadpreviouslyshowna strongaffinityforthepassivevoice(eg,associate,consider) werenotconsistentlyrankedasmorecomprehensible whenpresentedinthepassivevoiceinthepresentstudy. Hence,thereisnotastrongargumentthatstudentsare conditionedbymedicalwritingtoprefercertainverbsin thepassivevoice.
Table5-SubjectivelyRatedComprehensibilityfor SentencesPresentedintheActiveandPassiveVoice
Whenstudentswereaskedtosubjectivelyrankthe comprehensibilityofsentenceswrittenintheactiveversus passivevoice,theyindicatedthatoverallsentences presentedinthepassivevoiceweresomewhat(and statisticallysignificantly)morecomprehensible.When comparedwiththeobjectivemeasuresofcomprehensibility,thisseemstoreflectabiasonthestudents’partinfavor ofthepassivevoice,and,giventhatstudentsarefamiliar withmedicaltextsthatmakefrequentuseofthepassive voice,thisgeneralpreferenceseemsperhapsnotsurprising. Ontheotherhand,itisnotclearifstudentspreferto encounterparticularverbsin1voiceversustheother.Each ofthemainverbsinthesentenceslistedinTable4was presented4times—twiceintheactivevoiceandtwicein thepassivevoice.Theverb obtain wastheonlyverbfor
humanbiologybutalsoinvolvingayearlongcoursein criticalappraisalofresearchliterature.Thetextspresented inthisexperimentwerethereforerepresentativeofthe readingmaterialswhichthestudentswouldbeexpectedto
Alimitationofthisstudyisthatsubjectswerenot randomizedtothe2testcohorts.Further,theremaybe importantdifferencesintheliteraciesofstudentsat1 institutionversusanother,or,indeed,1countryversus another,limitingthegeneralizabilityofthiswork.
CONCLUSION
given that students are familiar with medical texts that make frequent use of the passive voice, this general preference seems perhaps not surprising. On the other hand, it is not clear if students prefer to encounter particular verbs in 1 voice versus the other. Each of the main verbs in the sentences listed in Table 4 was presented 4 times—twice in the active voice and twice in the passive voice. The verb obtain was the only verb for which the passive voice was twice rated as much more comprehensible than the active voice. The verb obtain was previously shown to have a strong affinity for the passive voice in reports of randomized controlled trials.11 On the other hand, other verbs which had previously shown a strong affinity for the passive voice (eg, associate, consider) were not consistently ranked as more comprehensible when presented in the passive voice in the present study. Hence, there is not a strong argument that students are conditioned by medical writing to prefer certain verbs in the passive voice.
A limitation of this study is that subjects were not randomized to the 2 test cohorts. Further, there may be important differences in the literacies of students at 1 institution versus another, or, indeed, 1 country versus another, limiting the generalizability of this work.
Conclusion
Collectively,theseresultsindicatethatforthetest subjectsandtextsusedinthisstudy,useof1voiceversus theotherdidnotaffectobjectivelyratedcomprehensibility,andthattherewasonlyamarginallygreater subjectivelyratedcomprehensibilityforthepassivevoice. Theseresultsarecongruentwithapreviouspaperwhich proposed,ontheoreticalgrounds,thatthepassivevoiceis appropriateinmedicalwritings.Furthermore,theseresults argueagainsteditorialguidelineswhichadvocatefor deliberateselectionoftheactivevoiceinmedicalwritings. Giventhatarticlesinleadingjournalsandaccessedby
Collectively, these results indicate that for the test subjects and
A selection of published research by CMCC faculty 81
Table 4 Difficulty and Sensitivity for Each of 10 Questions Pertaining to Text 2, Which Was Presented in the Passive (Original) and Active (Manipulated) Voice
Item Difficulty Sensitivity OriginalManipulatedOriginalManipulated 1 1.031.001.111.00 2 1.061.031.121.06 3 1.111.081.331.36 4 1.011.071.051.19 5 1.001.041.001.12 6 1.081.051.181.27 7 1.641.583.173.20 8 1.391.802.384.25 9 3.153.163.332.20 101.861.843.603.20 Mean (SD) 1.43 (0.67) 1.47 (0.68) 1.93 (1.07) 1.99 (1.17)
Sentence* ActiveVoicePassiveVoice 21NEJM 2.5 2.6 22Lancet 2.0 1.9 23Lancet 2.9 2.8 24NEJM 2.0 2.0 25Lancet 1.4 1.5 26JAMA 1.9 1.9 27NEJM 2.1 2.0 28AnnIntMed 3.0 2.6 29JAMA 2.3 1.8 30BMJ 2.2 1.8 31JAMA 2.1 1.9 32NEJM 1.6 1.6 33BMJ 1.8 1.6 34AnnIntMed 3.0 2.9 35BMJ 1.8 1.4 36AnnIntMed 2.4 2.5 37Lancet 3.0 2.8 38AnnIntMed 1.7 1.7 39BMJ 2.4 2.3 40JAMA 2.0 1.7 Mean(SD) 2.21(0.48) 2.07(0.47)
Item Difficulty Sensitivity OriginalManipulatedOriginalManipulated 1 1.031.001.111.00 2 1.061.031.121.06 3 1.111.081.331.36 4 1.011.071.051.19 5 1.001.041.001.12 6 1.081.051.181.27 7 1.641.583.173.20 8 1.391.802.384.25 9 3.153.163.332.20 101.861.843.603.20 Mean (SD) 1.43 (0.67) 1.47 (0.68) 1.93 (1.07) 1.99 (1.17)
Sentence* ActiveVoicePassiveVoice 21NEJM 2.5 2.6 22Lancet 2.0 1.9 23Lancet 2.9 2.8 24NEJM 2.0 2.0 25Lancet 1.4 1.5 26JAMA 1.9 1.9 27NEJM 2.1 2.0 28AnnIntMed 3.0 2.6 29JAMA 2.3 1.8 30BMJ 2.2 1.8 31JAMA 2.1 1.9 32NEJM 1.6 1.6 33BMJ 1.8 1.6 34AnnIntMed 3.0 2.9 35BMJ 1.8 1.4 36AnnIntMed 2.4 2.5 37Lancet 3.0 2.8 38AnnIntMed 1.7 1.7 39BMJ 2.4 2.3 40JAMA 2.0 1.7 Mean(SD) 2.21(0.48) 2.07(0.47) Abbreviations:NEJM, NewEnglandJournalofMedicine;JAMA, Journalof theAmericanMedicalAssociation;AnnIntMed, AnnalsofInternal Medicine;BMJ, BritishMedicalJournal.*Numberreferstothesentence numberofthearticleretrievedfromthejournallisted. JChiroprEduc2019Vol.33No.1 DOI10.7899/JCE-17-22 www.journalchiroed.com 19 Millar et all
Table4-DifficultyandSensitivityforEachof10 QuestionsPertainingtoText2,WhichWasPresentedin thePassive(Original)andActive(Manipulated)Voice
Table5-SubjectivelyRatedComprehensibilityfor SentencesPresentedintheActiveandPassiveVoice
texts used in this study, use of 1 voice versus the other did not affect objectively rated comprehensibility, and that there was only a marginally greater subjectively rated comprehensibility for the passive voice. These results are congruent with a previous paper which proposed, on theoretical grounds, that the passive voice is appropriate in medical writings. Furthermore, these results argue against editorial guidelines which advocate for deliberate selection of the active voice in medical writings. Given that articles in leading journals and accessed by health sciences students are already difficult to read,4,15 editors of publications in the health sciences may wish to take a more evidence-based approach to developing recommendations on language use.
Funding and conflics of interest
The authors declare that they have no conflicts of interest. No external funds were received in support of this work.
About the Authors
Neil Millar is an associate professor, faculty of engineering, information and systems, at the University of Tsukuba (1-11 Tennodai, Tsukuba, Ibaraki 305-8573, Japan; millar.neil. gm@u.tsukuba.ac.jp). Brian Budgell is a professor at the Canadian Memorial Chiropractic College (6100 Leslie Street, Toronto, Ontario, Canada M2H 3J1; bbudgell@cmcc.ca).
Address correspondence to Brian Budgell, Canadian Memorial Chiropractic College, 6100 Leslie Street, Toronto, Ontario, Canada M2H 3J1; bbudgell@cmcc.ca. This article was received September 10, 2017, revised February 1, 2018, and accepted March 2, 2018.
Author Contributions
Concept development: BB, NM. Design: BB, NM. Supervision: BB, NM. Data collection/processing: BB, NM. Analysis/interpretation: BB, NM. Literature search: BB, NM. Writing: BB, NM. Critical review: BB, NM.
References
1. Heming TA, Nandagopal S. Comparative difficulties with non-scientific general vocabulary and scientific/medical terminology in English as a second language (ESL) medical students. Sultan Qaboos Univ Med J. 2012;12(4):485–492.
2. Mann C, Canny BJ, Reser DH, Rajan R. Poorer verbal working memory for a second language selectively impacts academic achievement in university medical students. Peer J. 2013;1:e22. doi:10.7717/peerj.22.
3. Budgell B, Millar N, Fuller K. Assessing the literacy of modern chiropractic students. Proceedings of the 2016 World Federation of Chiropractic/Association of Chiropractic Colleges Education Conference; October 19–22, 2016; Montreal, Canada. J Chiropr Educ. 2016; 30:e167.
4. Fuller S, Horlen C, Cisneros R, Merz T. Pharmacy students’ reading ability and the readability of required reading materials. Am J Pharm Educ. 2007;71(6):111.
5. Olson MA. English-as-a-second language (ESL) nursing student success: a critical review of the literature. J Cultural Diversity. 2012;19(1):26–32.
6. Alexandrov AV. How to write a research paper. Cerebrovas Dis. 2004;18:135–138.
7. Bredan AS, van Roy F. Writing readable prose. EMBO Reports. 2006;7(9):846–849.
8. Steen RG. Writing for publication in a medical journal. Indian J Endocrinol Metab. 2012;16(6):899–903.
9. Christiansen S. Grammar. In: Iverson C, Christiansen S, Flanagin A, et al, eds. American Medical Association Manual of Style. 10th ed. New York, NY: Oxford University Press; 2009. doi:10.1093/jama/9780195176339. 001.0001.
10. British Medical Journal. Article types at the BMJ. http:// www.bmj.com/about-bmj/resources-authors/article-types. Accessed August 31, 2017.
11. Millar N, Budgell B, Fuller K. ‘‘Use the active voice whenever possible’’: the impact of style guidelines in medical journals. Appl Linguistics. 2013;34(4):393–414.
12. Cavanaugh JM, Lu Y, Chen C, Kallakuri S. Pain generation in lumbar and cervical facet joints. J Bone Joint Surg 2006. 2006;88-A(suppl 2):63–67.
13. Dishman JD, Dougherty PE, Burke JR. Evaluation of the effect of postural perturbation on motoneuronal activity following various methods of lumbar spinal manipulation. Spine J. 2005;5:650–659.
14. Cobb T. Web VP Classic v.4. http://www.lextutor.ca/vp/eng/. Accessed September 15, 2015.
15. Weeks WB, Wallace AE. Readability of British and American medical prose at the start of the 21st century. BMJ. 2002;325:1451–1452.
OriginallypublishedintheJournalofChiropracticEducation, 2019Mar;33(1):16-20.Epub2018Aug2.
ReproducedwithpermissionfromtheAmericanChiropractic Association.
AccessOnline:https://doi.org/10.7899/JCE-17-22
CMCC Research Report 2018–2020 82
Promoting the Use of Self-Management in Patients with Spine Pain Managed by Chiropractors and Chiropractic Interns: Barriers and Design of a Theory-Based Knowledge Translation Intervention
Abstract
Background:
The literature supports the effectiveness of self-management support (SMS) to improve health outcomes of patients with chronic spine pain. However, patient engagement in SMS programs is suboptimal. The objectives of this study were to: 1) assess participation in self-care (i.e. activation) among patients with spine pain, 2) identify patients’ barriers and enablers to using SMS, and 3) map behaviour change techniques (BCTs) to key barriers to inform the design of a knowledge translation (KT) intervention aimed to increase the use of SMS.
Methods:
In summer 2016, we invited 250 patients with spine pain seeking care at the Canadian Memorial Chiropractic College in Ontario, Canada to complete the Patient Activation Measure (PAM) survey to assess the level of participation in self-care. We subsequently conducted individual interviews, in summer 2017, based on the Theoretical Domains Framework (TDF) in a subset of patients to identify potential challenges to using SMS. The interview guide included 20 open-ended questions and accompanying probes. Findings were deductively analysed guided by the TDF. A panel of 7 experts mapped key barriers to BCTs, designed a KT intervention, and selected the modes of delivery.
Results:
Two hundred and twenty-three patients completed the PAM. Approximately 24% of respondents were not actively involved in their care. Interview findings from 13 spine pain patients suggested that the potential barriers to using SMS corresponded to four TDF domains: Environmental Context and
Resources; Emotion; Memory, Attention & Decision-Making; and Behavioural Regulation. The proposed theory-based KT intervention includes paper-based educational materials, webinars and videos, summarising and demonstrating the therapeutic recommendations including exercises and other lifestyle changes. In addition, the KT intervention includes Brief Action Planning, a SMS strategy based on motivational interviewing, along with a SMART plan and reminders.
Conclusions:
Almost one quarter of study participants were not actively engaged in their spine care. Key barriers likely to influence uptake of SMS among patients were identified and used to inform the design of a theory-based KT intervention to increase their participation level. The proposed multi-component KT intervention may be an effective strategy to optimize the quality of spine pain care and improve patients’ health-outcomes.
OriginallypublishedinChiropractic&ManualTherapies2019 Oct16;27:44. eCollection2019.
OpenAccessarticlereproducedunderthetermsofthe CreativeCommonsAttribution4.0InternationalLicense(http:// creativecommons.org/licenses/by/4.0/),
AccessOnline:https://doi.org/10.1186/s12998-019-0267-6
A selection of published research by CMCC faculty 83 Education in Healthcare
Eilayyan O1, 2 , Thomas A1, 2 , Hallé MC1, 2 , Ahmed S1, 2 , Tibbles A 3 , Jacobs C 3 , Mior SA 3 , et al. 1McGillUniversity, 2CentreforInterdisciplinaryResearchinRehabilitationofGreaterMontreal, 3CanadianMemorialChiropracticCollege
Promoting the Use of Self-Management in Novice Chiropractors Treating Individuals with Spine Pain: The Design of a Theory-Based Knowledge Translation Intervention
A1,
Hallé MC1, 2
al. 1McGillUniversity, 2CentreforInterdisciplinaryResearchinRehabilitationofGreaterMontreal, 3CanadianMemorialChiropracticCollege
Abstract
Background:
Clinical practice guidelines generally recommend clinicians use self-management support (SMS) when managing patients with spine pain. However, even within the educational setting, the implementation of SMS remains suboptimal. The objectives of this study were to 1) estimate the organizational readiness for change toward using SMS at the Canadian Memorial Chiropractic College (CMCC), Toronto, Ontario from the perspective of directors and deans, 2) estimate the attitudes and self-reported behaviours towards using evidence-based practice (EBP), and beliefs about pain management among supervisory clinicians and chiropractic interns, 3) identify potential barriers and enablers to using SMS, and 4) design a theory-based tailored Knowledge Translation (KT) intervention to increase the use of SMS.
Methods:
Mixed method design. We administered three self-administered questionnaires to assess clinicians’ and interns’ attitudes and behaviours toward EBP, beliefs about pain management, and practice style. In addition, we conducted 3 focus groups with clinicians and interns based on the Theoretical Domain Framework (TDF) to explore their beliefs about using SMS for patients with spine pain. Data were analysed using deductive thematic analysis by 2 independent assessors. A panel of 7 experts mapped behaviour change techniques to key barriers identified informing the design of a KT intervention.
Results:
Participants showed high level of EBP knowledge, positive attitude of EBP, and moderate frequency of EBP use. A number of barrier factors were identified from clinicians (N = 6) and interns (N = 16) corresponding to 7 TDF domains: Knowledge; Skills; Environmental context and resources; Emotion; Beliefs about Capabilities; Memory, attention & decision making; and Social Influence. To address these barriers, the expert panel proposed a multifaceted KT intervention composed of a webinar and online educational module on a SMS guided by the Brief Action Planning, clinical vignettes, training workshop, and opinion leader support.
Conclusion:
SMS strategies can help maximizing the health care services for patients with spine pain. This may in turn optimize patients’ health. The proposed theory-based KT intervention may facilitate the implementation of SMS among clinicians and interns.
OriginallypublishedinBMCMuskuloskeletalDisorders2018 Sep11;19(1):328.
OpenAccessarticlereproducedunderthetermsofthe CreativeCommonsAttribution4.0InternationalLicense(http:// creativecommons.org/licenses/by/4.0/)
AccessOnline:https://doi.org/10.1186/s12891-018-2241-1
CMCC Research Report 2018–2020 84
Eilayyan O1, 2 , Thomas
2 ,
, Ahmed S1, 2 , Tibbles A 3 , Jacobs C 3 , Mior SA 3 et
The Development of a Global Chiropractic Rehabilitation Competency Framework by the World Federation of Chiropractic
Abstract
The World Health Organization (WHO), in its “Rehabilitation 2030 A Call for Action”, identified the need to strengthen rehabilitation in health systems to meet the growing demands of current and future populations. Greater access to rehabilitation services is required to secure the achievement of the United Nation’s third Sustainable Development Goal, “Ensure healthy lives and promote well-being for all at all ages”. To support this mandate, WHO issued a call for non-governmental organizations, associations and institutions to share their rehabilitation-related competency frameworks which will be used to construct a global rehabilitation competency framework. In response to this call, the World Federation of Chiropractic (WFC) developed a chiropractic rehabilitation competency framework. In this article, we present the chiropractic rehabilitation competency framework that will contribute to the development of the global framework in support of WHO’s
strategic planning for rehabilitation. The goal of WHO’s strategic planning is to improve the integration and support of multidisciplinary rehabilitation and establishing opportunities for global networks and partnerships in rehabilitation.
OriginallypublishedinChiropractic&ManualTherapies volume27,29(2019).
OpenAccess articlereproducedunderthetermsofthe CreativeCommonsAttribution4.0InternationalLicense(http:// creativecommons.org/licenses/by/4.0/)
AccessOnline:https://doi.org/10.1186/s12998-019-0249-8
A selection of published research by CMCC faculty 85
Côté P1,2,3,4,5 , Sutton D2, 3 , Nicol R 4 , Brown R 4 and Mior S2,5 1CanadaResearchChairinDisabilityPreventionandRehabilitation-UniversityofOntarioInstituteofTechnology(UOIT), 2 UOIT-CMCC Centre for DisabilityPreventionandRehabilitation, 3UniversityofOntarioInstituteofTechnology, 4WorldFederationofChiropractic, 5 Canadian Memorial ChiropracticCollege
Comparison of Chiropractic Student Lexicon at Two Educational Institutions: A Cross-Sectional Survey
Gleberzon BJ1 , Pohlman KA 2 , Russell E 2 1CanadianMemorialChiropracticCollege, 2ParkerUniversity
Abstract
Objective:
To evaluate student perceptions of chiropractic cultural authority, role in healthcare and use of terms at two chiropractic institutions, the Canadian Memorial Chiropractic College (CMCC) and Parker University (Parker).
Methods:
A unique survey was developed and administered electronically to Year 2-3 students (n=387) at CMCC and as a paper-based surveys to trimester 4-5 (comparison with Year 2) and 6-7 (comparison with Year 3) (n=277) students at Parker. Responses were anonymous. The survey assessed the likelihood that students at both chiropractic programs would use eight different chiropractic terms. The survey also assessed their preference toward different options with respect to chiropractic’s cultural authority.
Results:
Response rates were 36.2% and 78.1% at CMCC and Parker, respectively. Students at both institutions reported that chiropractic cultural authority was ‘neuromusculoskeletal’ (NMSK); however, CMCC students was more favorable toward ‘musculoskeletal’ (MSK) care compared to Parker students, whereas students at Parker favored ‘wellness’ (59.7%)
compared to CMCC students (46.4%). Students at CMCC were more likely to use ‘impingement’ and ‘joint dysfunction’ whereas Parker students were more likely to use ‘innate intelligence’ and ‘vertebral subluxation’. Both institutions were equally likely to use ‘spinal lesion’.
Conclusion:
This survey found significant cultural authority differences between institutions. While this adds to the emerging need in the literature to evaluate the impact of curriculum and co-curriculum within chiropractic training programs on professional identity, explanations were not evaluated.
OriginallypublishedinTheJournaloftheCanadian ChiropracticAssociation,2019Apr;63(1):36-43.
ReproducedwithpermissionfromtheJournaloftheCanadian ChiropracticAssociation.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6493211/
CMCC Research Report 2018–2020 86
“I Stay in Bed, Sometimes All Day.” A Qualitative Study Exploring Lived Experiences of Persons with Disabling Low Back Pain
Esson SA1, Côté P1 2 3 , Weaver R 4 5 , Aartun E1, Mior S1 3 5 1UOIT-CMCCCentrefortheStudyofDisabilityPreventionandRehabilitation, 2CanadaResearchChairinDisabilityPreventionandRehabilitation, OntarioTechUniversity,
3OntarioTechUniversity, 4RowanUniversity, 5CanadianMemorialChiropracticCollege
Abstract
Aim:
To explore the lived experiences of persons with low back pain (LBP) and disability within the context of the International Classification of Function, Disability and Health (ICF) framework.
Methods:
Qualitative study using focus group methodology. We stratified LBP patients into two low (n=9) and one high disability (n=3) groups. Transcript-based thematic analysis was conducted through an interpretivist lens.
Results:
Four themes emerged: Invisibility, Ambivalence, Social isolation, and Stigmatization and marginalization. Participants described how environmental factors affected how they experienced disability and how their awareness of people’s attitudes affected personal factors and participation in social activities. High disability participants experienced challenges with self-care, employment, and activities. The invisibility of LBP and status loss contributed to depressive symptoms.
Conclusion:
LBP patients experience physical, social, economic and emotional disability. Our findings highlight the interaction between domains of the ICF framework and the importance of considering these perspectives when managing LBP patients with varying levels of disability.
Introduction
Lower back pain (LBP) is a leading cause of disability worldwide.1,2 It is one of the most prevalent chronic disorders and imposes a substantial economic burden globally.3
Approximately 80% of adults will experience LBP at some point in their lives.1 LBP manifests itself as stiffness, tension or achiness confined between the costal margin and the inferior gluteal folds; with or without sciatica.4 The pathophysiological causes of LBP are often unidentifiable.5 This creates challenges to its effective treatment and management, especially because patients experience LBP in different ways.6 Others suggest that
this unidentifiable pathology along with unclear diagnoses and often the lack of visible proof can cause LBP sufferers to be labeled as hypochondriacal, malingerers and even mentally ill.7-9 This may lead to disbelief or a dismissal of the seriousness and authenticity of disability associated with LBP.10,11
In addition to the physical effects experienced by LBP patients, there are personal, societal and psychological ramifications associated with the condition.12,5 In some cases, asocial behaviour and negative self-image are additional consequences of living with LBP.13 Furthermore, increased work absenteeism, lower productivity, status loss, and depressive symptoms often accompany chronic LBP.1,14 However, limited qualitative data is available which describes LBP patients’ daily experiences with LBP associated disability from a biopsychosocial perspective.12,15,16 Thus, it is important to understand the everyday lived experiences of people with LBP and explore how psychosocial factors impact pain and disability, in order to effectively address them in their care plan.
The ICF Framework
In consideration of the biopsychosocial attributes of LBP, we framed our qualitative study using the International Classification of Functioning, Disability and Health (ICF) framework as a point of reference for our data collection.17 The ICF is helpful to conceptualize the positive and negative aspects of functioning from a biological, individual, and social perspective.17 The framework emphasizes the role of the environment by stressing the importance of understanding the context in which the person lives and its interactions with health conditions and personal factors. The ICF includes five interacting domains: i) body functions: physiological functions of body systems (including psychological functions); ii) body structures: organs and limbs; iii) activity: execution of a task or action (including cognitive functions); iv) participation: involvement in a life situation; and v) environmental factors: physical, psychological, social, and attitudinal environment in which people live (barriers to or facilitators of functioning) (Figure 1). The ICF framework is the international reference for the conceptualization and evaluation of disability.17 It is in line with the UN Convention on the Rights of Persons with
A selection of published research by CMCC faculty 87 Health and Wellness
Disabilities and provides a common and universal language to understand disability and human functioning across communities.18,19 The ICF framework provides a structured guide for the conceptualization, collection and organization of data necessary to arrive at a comprehensive understanding of an individual’s lived experience, within the context of their health condition. Because disability denotes “the negative aspects of the interaction between an individual (with a health condition) and that individual’s contextual factors”17 a clinician engaged in patient care must seek to understand the individual’s environmental and personal factors, if appropriate care is to be delivered.
We used the ICF framework to guide our analysis and address our objective of exploring the lived experiences of persons with low back pain and disability. Our study is part of an international, collaborative project between the Ontario Tech University and the ICF Research Branch (a cooperation partner within the WHO Collaborating Centre for the Family of International Classifications in Germany at the German Institute for Medical Documentation and Information (DIMDI)). The aim of this international collaborative project is to identify the aspects of functioning that are most important to participants and subsequently develop an ICF assessment schedule, a standardized measurement instrument, specifically designed for manual medicine for
the reporting of functioning. Our study investigates aspects of functioning among patients with LBP in Ontario, Canada.

Materials and Methods
Study design
We used a qualitative design to explore the everyday experiences of persons with LBP. We used Interpretive Phenomenological Analysis (IPA), situated within the interpretivist paradigm, to understand participants’ experiences. IPA reveals complex and dynamic relationships and places value on the subjectivity of participants’ experiences.13
We used focus groups to elicit these everyday experiences. Focus groups offer a forum that enables participants in similar circumstances to share their experiences, and often facilitate disclosure of additional and more nuanced responses regarding their own experiences. Focus groups provide richness in the data that reflects the synergy between participants and explores their perceptions of an issue.20 Ethics approval was obtained through the Research Ethics Boards of Ontario Tech University (REB # 14050) and CMCC (REB # 1629014).
CMCC Research Report 2018–2020 88
Fig1DomainsoftheInternationalClassificationofFunction,DisabilityandHealthModelandrelatedemergentsubcategories.
Participants and recruitment
Participants were recruited from three Canadian Memorial Chiropractic College (CMCC) teaching clinics in the Greater Toronto Area (GTA) in Ontario, Canada. Participants were eligible to participate if they met the following criteria: 1) 20-65 years of age; 2) reported LBP; 3) were receiving chiropractic care for their LBP; and 4) spoke English.
Participants were recruited through advertisements placed in clinic reception rooms and by clinicians informing their patients about the study. CMCC staff clinicians introduced the study to patients and identified interested patients. The first author contacted interested patients and provided them with study information and the informed consent package. Focus groups were scheduled at the convenience of participants. Each focus group was conducted in a private room within the clinic, and situated in a convenient location for participants.
Focus group allocation
We used the World Health Organization Disability Assessment Schedule (WHODAS) to stratify participants into low disability focus groups (LDFG) and high disability focus groups (HDFG). The WHODAS is a 12-item, self-administered questionnaire designed to assess difficulty experienced doing regular, everyday tasks.21 The WHODAS is directly derived from the ICF and evaluates six domains of disability the “activity and participation” dimension of the ICF: cognition; mobility; self-care (hygiene, dressing, eating & staying alone); getting along (interacting with other people); life activities (domestic responsibilities, leisure, work & school); and participation (joining in community activities). The WHODAS is considered to be a valid and reliable measure of disability and thus was appropriate for stratifying our sample.22,23 The WHODAS is useful to measure disability in chronic low back pain patients and significantly positively correlated with the Roland Morris Disability Questionnaire, the Patient Health Questionnaire-9 item, the Screener and Opioid Assessment for Patients with Pain-Revised, the Current Opioid Misuse Measure (COMM) and the Opioid Risk Tool (ORT).24 We used a pre-determined cut point of 36 out of a possible 60 points to allocate participants into LDFG and HDFG. A score above 36 is suggestive of a person having higher levels of disability severity. Previous studies used similar methods of stratification using this questionnaire.25-27 We anticipated recruiting 32 participants, with eight people in each of 4 groups, with an equal distribution of male and female participants. However, we presumed difficulty in recruiting equal distributions due to clinic population and would accept a 5:3 ratio of participants in each focus group.
Data collection
We used a script to guide questioning of participants. The focus group interview script was designed to elicit responses related to the ICF framework. Further probative questions explored answers to the questions in the event that what was said was not understood or required further clarification (Appendix
1). The script was reviewed in advance by the research team and pretested in a sample focus group to ensure clarity and comprehension. Each focus group was led by a trained facilitator (SE) and assisted by a co-investigator (EA). Focus groups were scheduled at different times to accommodate participants availability. The focus groups lasted approximately 90 minutes each.
Each session was audio-recorded and subsequently transcribed verbatim with participants’ consent. The recordings were transcribed by an experienced transcriptionist. Each transcript was checked for accuracy by cross referencing the audio file with the transcribed document. Errors in content and sentence structure were corrected and extraneous sounds/comments noted. Finally, confidentiality of statements made by each focus group participant in transcripts was assured by providing pseudonyms. Transcripts were not returned to participants for review.
Analysis
We used the NVivo11 Software (QSR International Pty Ltd. Version 11, 2015) to organize and analyze the transcripts. There was broad agreement among team members regarding the essential meaning of the core elements of the ICF framework. The framework became part of the scaffolding used during the coding process. These elements provided the foundation for our thematic analysis, where emergent themes were identified and conceptually expanded. The first author imported transcripts into NVivo software and reviewed, identifying, organizing, and coding key passages in NVivo nodes. Team members discussed and resolved ambiguities in the coding process as they arose and until consensus was reached. Once agreement was reached coded nodes were linked to components of the ICF framework. The framework was used to scaffold themes emerging from the data. Once preliminary themes were identified, the team further discussed how they interrelated within the context of the ICF framework until consensus was reached regarding the soundness of the emergent themes.
Results
We enrolled twelve participants in the study - seven women and five men, who participated in one of three focus groups. The two LDFG included five and four participants, respectively. The HDFG included three participants. In addition to their varying degrees of disability, participants also had varying ages, ethnicities, and soci-oeconomic backgrounds, including students, employed, unemployed and retired individuals (Table 1).
ICF Domains
Based on the five a priori domains from the ICF frame-work, participant experiences were coded accordingly. Our findings suggest that the domains of “activity” and “participation” bear similarities that make it difficult to distinguish between them. Similar findings have been also reported by others 28-30; therefore, we merged these two domains (Figure 1).
A selection of published research by CMCC faculty 89 Esson et al
Body Function and Body Structure
Participants described various challenges associated with body structure and body function. These included the exacerbation of, difficulties sleeping and varied emotional responses stemming from their condition and pain. In both the low and high disability focus groups, participants provided conflicting accounts about the location of their pain. Some participants suggested that their LBP was confined to one area – typically the small of the back, while others explained that their pain was not localized but rather travelled from one area to the next, making it difficult to predict when or where the pain would arise.
different times to accommodate participants availability. The focus groups lasted approximately 90 minutes each. Each session was audio-recorded and subsequently transcribed verbatim with participants’ consent. The recordings were transcribed by an experienced transcriptionist. Each transcript was checked for accuracy by cross referencing the audio file with the transcribed document. Errors in content and sentence structure were corrected and extraneous sounds/comments noted. Finally, confidentiality of statements made by each focus group participant in transcripts was assured by providing pseudonyms. Transcripts were not returned to participants for review.
Analysis
“WhenIfirststartedgettingthepainIwouldsayitwas somewhatlocalizedandthenitstartedspreadingand nowIcan’teventellthedifferenceanymorebecauseitis throughoutmyentirebody.”Allan[HDFG3].
Difficulty falling asleep and interrupted sleep are common experiences amongst persons living with disability.31 Participants in the LDFG reported falling asleep was not difficult but they struggled to sleep restfully or remain asleep, often having to change positions to relieve their pain or discomfort:
“FormeIhavereallyroughnightssleepingsolikeevery hourorsoIhavetowakeupandstretchandmovearound. So,inthemorningthesamething,itisaboutahalfan hourofstretchingandmovingaroundbeforeIcanactually function.” Corrina [LDFG1]
We used the NVivo11 Software (QSR International Pty Ltd. Version 11, 2015) to organize and analyze the transcripts. There was broad agreement among team members regarding the essential meaning of the core elements of the ICF framework. The framework became part of the scaffolding used during the coding process. These elements provided the foundation for our thematic analysis, where emergent themes were identified and conceptually expanded. The first author imported transcripts into NVivo software and reviewed, identifying, organizing, and coding key passages in NVivo nodes. Team members discussed and resolved ambiguities in the coding process as they arose and until consensus was reached. Once agreement was reached coded nodes were linked to
In contrast, HDFG participants reported struggling not only with falling asleep but remaining asleep. Allan’s account clearly exemplifies these challenges.
“Iwouldsaybothbecauseitisalmostimpossibletofind acomfortablepositionwhereyousay,‘OKIamnotin paininthispositionsoIwillstayhere.’Youfindyourself tossingandturningallnightlongtryingtofindaposition
components of the ICF framework. The framework was used to scaffold themes emerging from the data. Once preliminary themes were identified, the team further discussed how they interrelated within the context of the ICF framework until consensus was reached regarding the soundness of the emergent themes.
thatworksandusuallyyoudon’tand9timesoutof10the onlyreasonyoudofallasleepisfromrestlessness.”Allan [HDFG3]
Participants described how their LBP negatively impacted their motivation to perform daily activities. Emotional responses and concentration on daily tasks varied by participant group. While LDFG participants experienced few challenges with concentration or maintaining focus, the HDFG participants described a significantly diminished ability to concentrate, having to work much harder than before:
Results
We enrolled twelve participants in the study - seven women and five men, who participated in one of three focus groups. The two LDFG included five and four participants, respectively. The HDFG included three participants. In addition to their varying degrees of disability, participants also had varying ages, ethnicities, and socioeconomic backgrounds, including students, employed, unemployed and retired individuals (Table 1).
ICF Domains
“…Ialsohaveahardtimeconcentrating.So,my concentrationwhenitcomestostudyingdoesn’tlast morethanlike10-15minutes.SoIhavetostudyinlike 10-15minutesfightingtoreadandthenbreak5minutes… beforeIwouldjustgotoclasslistenandbarelyhaveto studyanythingorreadtoomuchnowIfindmyselfdoing10 timesmoreworkjusttogetonesectionoverwith.”Allan [HDFG3]
Based on the five a priori domains from the ICF framework, participant experiences were coded accordingly. Our findings suggest that the domains of “activity” and “participation” bear similarities that make it difficult to distinguish between them. Similar findings have been also reported by others 28-30; therefore, we merged these two domains (Figure 1).
Activity and participation
Body Function and Body Structure
Participants described various challenges associated with
64(1)
There were marked contrasts among the participants in the ability to engage in physical actions, which affected their social relationships, driving and employment. Participants in the LDFGs expressed few activity limitations. They were able to differentiate between activities they could manage and those seen as detrimental to their ability to function. Unlike the HDFG participants, the LDFG participants reported being better able to manage their pain by modifying, rather than limiting, their activities. Many enjoyed cycling, yoga and swimming, but avoided high intensity exercises such as running, which they maintained placed severe pressure on their back and legs/ knees.
“Iwenttoatrampolineparkwithmyfriends…Ihadto
CMCC Research Report 2018–2020 90
20 J Can Chiropr
Assoc 2020;
Low
High disability
Total Gender Male Female 2 3 2 2 1 2 5 7 Age Group 20-35 36-50 51-65 0 1 4 1 1 2 1 0 2 2 2 8 Demographics Employed Unemployed/student Retired 2 2 1 1 3 0 0 1 2 3 6 3 Total 5 4 3 12
Table 1. Demographic characteristics of participants in this study.
CharacteristicsLow disability focus group #1 [LDFG1]
disability focus group #2 [LDFG2]
focus group [HDFG3]
Table 1 Demographic characteristics of participants in this study.
completelystopbecauseofpaininmyneck,paininmy back…andI’mlikewellI’mgoingtowatchyouguys… becauseyouknowyoucan’treallydothesamelevelas theycan...”Leo[LDFG2]
Conversely, the HDFG participants struggled with even elementary body movements and body positions, and described serious exercise restrictions:
“Lyingflatisvery,verypainful.Bendingdownlikeasthe dayprogressestheworseIgetandbytheendofthedayit isnearlyimpossibletofunction.”Helena[HDFG3]
Participants in the HDFG noted that their chiropractors recommended exercises to manage their LBP but felt the chiropractor did not understand the challenges they faced in doing the exercises. This is an example of the dissonance between LBP patients and their healthcare providers which may impact their compliance.32
“Itlimitsyourabilitytodothingsespeciallyexercise. So,itseemslikeeverybodywhereyougofortreatment recommendsexercisebuttheykindofdon’tunderstand thatitisveryhardtodothings,especiallywhenyou squeeze,thepainjustintensifiestimes50.”Allan[HDFG3]
Most LDFG participants suggested their condition did not negatively impact their social interactions. In contrast, participants in the HDFG described a more dramatic change in social relationships, which included loss of friends and the desire to socialize. These findings are typical of persons living with severe back pain and supports findings in previous literature.13,36,37
“Ijustdon’treturncallsiftheycall.Idon’tthinkthey understand,theydon’tunderstandwhatyouaregoing through.”Francine[HDFG3]
The employment status of persons in the LDFGs varied and included retired persons, unemployed persons, students and working persons. Those who worked were aware of their physical capabilities and sought employment accordingly:
“Ican’treallydocertainphysicaljobsbecauseIamnot sureifitisgoingtotightenup…SoItrytostayawayfrom anythinglikethat.Theproblemisalotofjobsaregoingto stillrequirestandinganyways.”Leo[LDFG2]
HDFG participants reported fewer employment opportunities compared to those in the LDFG. All HDFG participants were unemployed. For one participant, it was a personal choice to become full-time caregiver for a loved one. Another participant was no longer able to assume the labour-intensive demands of their work. Yet another participant quit her job because other co-workers assumed her compensatory movements and
gait were related to her being intoxicated. HDFG participants expressed a desire to return to work but noted their LBP prevented them from long periods of sitting and standing. They viewed seeking new employment as a challenge, fearing the potential employers’ reactions after disclosing their LBP.
“Itisalsohardtotryandgetanotherjob…SowhenIgoand tryandgetjobsIwouldratherbehonest…Whenyousay thosekindsofthingstopeopleabouthowyoureallyare,it islikeOK,rightawayyoulookattheirfaceandyou’relike ‘IknowIdidn’tgetthisjob.”Allan[HDFG3]
Environmental factors
Environmental factors that impacted participants included public resources, healthcare and the attitudes of others. Communal spaces and transit were the primary public resources discussed by participants. Many of the participants in the LDFG lived within the downtown core and took advantage of the many available community resources:
“Theywillalsofall-proofyourhouse.Sothatisoneofthe thingsthatyoucanget,youhavetohaveadoctorreferral toitbuttheywillcomeinandlookatyourhouseandhow youhaveitset-upandthendothefallprevention.”Walter [LDFG1]
Participants in the HDFG, who also lived in the down-town core, were significantly less informed about community resources. They knew that some resources were available online but struggled to access them because they did not own a computer, were unaware how to access, or could not afford some resources. A student in the HDFG described classroom design, uncomfortable seating and poor accessibility as a barrier to attending classes. They also noted that although campus buildings were equipped with handicap push buttons to automatically open doors, many simply did not function:
“AtmyschoolIwouldsayabout75%ofthehandicap buttonsdon’tworkandiftheydoworkmaybeitisonlyin thesummertimebecauseinthewintertheygetjammed.” Allan [HDFG3]
Participants with HDFG relied on elevators or escalators to get to higher floors in multi-story buildings. Where neither were available, they relied heavily on the handrails of the stairs:
“SoeverytimeIwalkintoabuildingIalwaysliketoknow wheretheelevatorisorescalatororsomeeasierwayto getupandifthelastresortisthestairsthenIhavetokind ofcoachmyselfintodoingit...”Allan[HDFG3]
Public transit was reported as a significant concern among most participants. Buses and streetcars were the most frequently used modes of transportation amongst participants. Participants in both groups expressed caution and care when moving on and off buses and street-cars. The physical design
A selection of published research by CMCC faculty 91 Esson et al
of the vehicles made travel difficult for participants. One participant suggested that bus seats provided no back support and aggravated their pain:
“Yes,theirseatsarereallybadforpeoplewithlowerback pain.Itislikesittingonametalplate.”Allan[HDFG3]
Participants also described experiences with other transit users, ranging from being helpful by offering a seat to flat-out dismissive. Participants experienced feelings of frustration as their disability often went unnoticed, with few fellow passengers understanding their pain and functional impairment. Whether in interactions with family members or with persons on a bus, LBP sufferers often encounter others’ disbelief of their disability – if they appear fine on the outside, they must be fine on the inside too.33 Since they “look good” and appear to be able-bodied and fully functional, participants felt their pain was misunderstood and delegitimized.
All participants sought treatment from general practitioners and chiropractors. Participants in both low and high disability focus group were pleased with the treatment they received in the chiropractic clinic. A few participants detailed the empathetic and understanding nature of their chiropractor and positive outcomes of care:
“Actually,mychiropractornowisactuallyhavingme… standstraightandyoumoveyourhipsforward,likeatilt kindofthing,andthat’showyouwalkandit’samazing. Thepainismuchlessoverafairlylongperiodoftimeyou canactuallywalkproperly.”Mallory[LDFG2]
“Idolikewhenthechiropractordoesworkonme. Basically,theystretchitoutfirstandthenputmentholor whateverstufftheyputonit.LikethismorningIwasthere andIfindthatIcanmovearoundalotbetteroncetheydo that.” Helena [HDFG3]
In addition to chiropractic treatments, participants in the LDFGs were more actively involved in their care and encouraged interprofessional correspondence between those involved in their treatment, including the fitness expert at the gym. HDFG participants were mindful of what they were feeling so they could appropriately articulate them to their chiropractors. Participants also said their chiropractors made suggestions about strategies or equipment they might use to cope with various everyday challenges.
A unique and interesting finding about participants attending for chiropractic care was their opportunity to interact with others in the waiting room. Some participants did not have healthy social lives and seemed to appreciate the friendly environment in the clinics. They often treated their chiropractic appointments as a part of their social calendar.
“Somepeoplethatgotothebarandtheydrinkandtryto getridoftheirstresswhichactuallymakesthingsworse andtosocialize.Believeitornot…Iactuallygetabitofa highincominginfrommytreatment.SoIamgettingthe medicalhelpanditisalsoasocialstructuretoo.”Mason [LDFG2]
The attitudes of friends, family and the general community were important to all participants. However, there was a disparity between the groups. Participants in the LDFG shared varying experiences about the attitudes of family members and community members. Some reported that healthy family and social relationships did not much differ from when they did not have LBP.
“Yesminehasn’taffectedthingsthatmuchwithgetting togetherwithfriendsandthat,soIamlucky…”Wendy [LDFG2]
Conversely, participants in the HDFG saw living with LBP as the reason why they experienced daily personal strife. They believed their LBP led to the decline of relationships. They felt their friends and family did not understand what it was like to live with LBP and were often reluctant to discuss the pain they experience, and instead would steer conversations away from pain and disability or even distancing themselves from others.
“Ifindthatpeoplesaytheywillbethereforyou,theyare yourfriendsorwhateverandevenfamily,andallofa suddentherewillbedaysortimeswhenIneedsomebody forevenemotionalsupportorphysicalsupporttodo something,andeverybodyisbusyortheydon’twantto comeortheydon’twanttohearaboutit.”Helena[HDFG3]
HDFG participants implied their LBP was wholly responsible for their inability to work or effectively function in social settings. As has been reported elsewhere 13, respondents also were made more aware of their disability when in the presence of those who have not experienced back pain, and they worried about how others perceived them.
Personal Factors
Personal factors that affect participants included age, comorbidities, and financial constraints; gender impacted frequency of activity. Ageing and comorbidities affected participants’ differently. HDFG participants did not perceive that age impacted their level of disability but felt their comorbidities did. In contrast, LDFG participants were less affected by their co-morbidities and questioned whether their experiences with disability were a result of normal ageing processes rather than LBP:
“Ithinkmyemotionalstateisjustunderstandingthatthis isa51-year-oldbodythathasgonethroughalotofsports and athletics and knocks and bruises and stuff like that.”
Val[LDFG1]
CMCC Research Report 2018–2020 92
Financial constraints were a recurrent theme among HDFG but not so in the LDFG participants. HDFG participants’ primary concern was with the cost of engaging in certain activities or using resources such as a gym. Instead they emphasized the need to satisfy basic needs such as securing healthy food and shelter.
“Eatingisexpensive…Youbuywhatishealthyandwhat isonsaleandyoutrytoeathealthy...theysaywiththe inflammationyouhavetowatchwhatyoueat…youhaveto watchdairyandglutenandallthatstuffbutagaintheyare expensivestuff.”Francine[HDFG3]
Self-management was the primary coping mechanism for participants in both low and high disability groups. It allowed them temporary relief from their LBP and gave them the opportunity to function more adeptly in everyday situations. They used various temporary modalities to alleviate their pain such as hot/cold packs, topical pain-relieving creams and painkillers. A few participants also mentioned that they found deep breathing exercises and meditation to be effective. Other enablers to functioning included developing creative self-management techniques and interacting with other LBP patients. One participant in the HDFG decreased the discomfort she experienced when travelling on public transit by carrying a backpack stuffed with soft items (scarves, clothes etc.) and used it as a cushion to ease the pressure on her back. Another participant said that receiving advice from other LBP patients and learning about different coping strategies improved her ability to function.
“Hearingwhatotherpeoplearedoing,Ithinkcommunity supportisabigthing,becauseeverybodyknowsonepiece ofthepuzzlebutnobodyknowsthewholepuzzle.”Corrina [LDFG1]
Interrelated themes
Due to the interrelated nature of the ICF domains, we identified four emergent themes that recurred across all the focus groups and were interwoven among the domains. We summarized participant responses within these respective themes as: Invisibility, Ambivalence, Social isolation, and Stigmatization and marginalization.
Invisibility
Since chronic LBP is not physically visible, non-sufferers often do not validate that the condition is real to sufferers.23 For example, some participants described the attitudes of transit operators who did not recognize their disability, while using public transportation. They expressed concern that operators often maneuvered buses in a less than smooth manner and often accelerated into traffic before they were seated or in a secure standing position. Corrina recounted her experience using transit buses: “They will put the ramp down but they
are not going to put it down for someone who ‘looks good’” [LDFG1]. A participant in the HDFG described an encounter while using public transportation, where another passenger asked her to surrender the accessible seat she was occupying to another passenger who appeared to need it. Participants reported feeling frustrated by the lack of recognition of their disability. Even when LBP sufferers tried to explain their symptoms to others, non-LBP sufferers often failed to recognize or believe the suffering and functional impairment of LBP sufferers. Whether through interactions with family members or strangers, the pain and disability LBP sufferers endure remains invisible. Their pain is not viewed as legitimate because they often appear to be able-bodied and fully functional.
Ambivalence
Participants in the HDFG seemed to display feelings of ambivalence about how to live with LBP. They seemed to grapple with whether to accept that they might be less able to do some things they were previously capable of doing or to attempt to normalize their current situation, despite possibly requiring special consideration. Some used assistive devices to improve functioning. However, all participants in the HDFG were adamant about only using these devices temporarily as they strived to maintain their independence. Helena noted,
“Icandowithoutanyofthosedevices.Iambetteroff becauseonceyoustartusingthem,itisacrutchand basicallyyourmusclesandwhateverfurtherdeteriorates becauseyouarenotusingthem…Myindependencewith thatisnogood”[HDFG3].
Some participants reported refusing to use certain assistive devices altogether such as wheelchairs and walkers as they perceived them as symbols of disablement, choosing not to announce their disability to others. This is consistent with previous studies suggesting persons with disabilities often abandoned the use of assistive devices to avoid the judgement of others and prevent their potential social exclusion.34,35
Despite lamenting that others often did not recognize their disability, participants were nonetheless concerned about appearing disabled and the accompanying perceived loss of social status. This contradiction illustrates an internal struggle that LBP patients must manage as they try to renegotiate and redefine the self to accommodate for lost capabilities.
Social isolation
The theme of social isolation spanned many domains of the ICF framework, reflecting the psychological, relational and emotional aspects of LBP sufferers. The emotional toll chronic LBP had on participants negatively impacted their motivation to perform daily activities. Depressive symptoms sometimes lead participants to withdraw and retreat to their homes for extended periods of time.28 Participants described behavioural changes such as loss of self-esteem and social isolation that resulted
A selection of published research by CMCC faculty 93 Esson et al
from feelings of depression. Both LDFG and HDFG participants felt emotionally drained and disliked being dependent on others and assistive devices. In particular, participants in the HDFG felt especially overwhelmed and withdrawn and wanted to avoid the reality of their current situation. Francine stated, “I stay in bed, sometimes all day which is even worse for the back pain…but if you don’t want to get out, you don’t want to get out…” [HDFG3]. This withdrawal offers some relief from having to defend or explain a condition, which others may not acknowledge or understand.29
Across the focus groups, participants expressed varying experiences related to social relationships. Most LDFG participants suggested that their condition did not negatively impact their social interactions; however, they did acknowledge small changes in their relationships. For example, one participant identified a change in the interests she previously shared with friends. When the interests were no longer shared, friendship ties became frayed:
“ImeanIhadworkfriendsbutonlyatwork.Onceyou leavework,theygohomeyouknowanddidn’treallyhave timetotalk…MyfriendsarenotinterestedinwhatIwantto dooksoIwouldliketoseepeoplemoreinterestedinwhat IwanttodoandIwilljointhem”[Corrina,LDFG1].
Their accounts illustrate the strain on relationships that can occur when the primary subject of conversation revolves around chronic pain and may eventually become bothersome to friends, who may not understand this pain. Respondents felt that friends sometimes shied away from them to avoid such conversation or interaction.
In contrast, participants in the HDFG described a more dramatic change in social relationships, which included loss of friends and loss of the desire to socialize. Allan notes, “You will probably lose all your friends, they will become tired of always having to lag behind” [HDFG3]. Francine illustrates the lost desire to socialize and the perceived dissonance been LBP sufferers and non-sufferers: “Ijustdon’treturncallsiftheycall.Idon’t thinktheyunderstand,theydon’tunderstandwhatyouare goingthrough”[HDFG3]. These changes appear consistent with persons living with severe back pain.36,37,13
Stigmatization and marginalization
Stigmatization, and the marginalization that often accompanies it, became apparent in the focus groups as participants discussed their physical activities as well as employment, or lack thereof. Employed participants in the LDFG were aware of their physical capabilities and limitations, and sought employment within these confines:
“IfIamlookingforworkIcan’treallydocertainphysicaljobs becauseIamnotsureifit(hisback)isgoingtotightenup… SoItrytostayawayfromanythinglikethat”[Leo,LDFG2].
Unlike their counterparts, participants in the HDFG described considerably fewer employment opportunities. At the time of the focus group session, all participants in the HDFG were unemployed. Some expressed a desire to return to work but noted that their LBP caused diminished sitting and standing capabilities. The idea of seeking new employment became a challenge, as participants feared the reaction of potential employers once they disclosed their condition:
“Itisalsohardtotryandgetanotherjob…SowhenIgoand tryandgetjobsIwouldratherbehonest…Whenyousay thosekindsofthingstopeopleabouthowyoureallyare,it islikeOK!Rightawayyoulookattheirfaceandyou’relike ‘IknowIdidn’tgetthisjob”[Allan,HDFG3].
When asked about what would enable them to function in the workplace, participants in the HDFG said that it was important for employers to be empathetic towards their need for frequent breaks. They feared that their LBP would not be recognized and that employers might think they did not take their jobs seriously.
The discomfort, shame, and stigma associated with the negative responses of others towards LBP sufferers has also been directly linked to depressive symptoms and isolated behavior.10 Some participants felt that family members had other concerns and chose not to discuss their LBP. In this regard, the disinterest of family members caused feelings of marginalization. Val noted, “…youareatthediningroomtablewithyourfamily,there isalwaysotherpeople’sissuesthataremoreimportant andmorepressingkindofthing,thanjust‘oh,youjust havelowerbackpain;Whatever!”[LDFG1].
This finding supports previous work by Smith and Osborn13 who found that social situations often intensified the psychological dilemma faced by LBP patients as they become self-conscious and are fearful of the judgement of others.
Discussion
Our findings suggested both commonalities and divergence between LDFG and HDFGs. The ICF conceptualizes activity and participation as two distinct categories. However, numerous researchers have argued that the domains of activity and participation within the ICF model are difficult to distinguish.30-32 Our findings suggest these two domains bear many similarities and often supplement each other. Therefore, the domains of activity and participation were merged and reported together to show individual limitations and the resulting restrictions that LBP patients experience.
The ICF framework and its diverse domains enabled us to capture an array of experiences identified by LBP sufferers in LDFGs and HDFG. Persons in the LDFGs had higher levels of functionality but living with LBP required them to modify several of the activities of daily living. Further, they demonstrated
CMCC Research Report 2018–2020 94
increased awareness of the events and activities they could and could not safely and easily participate in. In most lowdisability cases, familial relationships and friendships were only minimally affected. Nonetheless, several participants expressed some emotional responses and depressive symptoms which they associated with living with LBP.
HDFG participants also experienced emotional challenges living with LBP, but their social isolation and depressive symptoms appeared to be more extreme. Their physical abilities were more diminished and there was evidence of some fear avoidance behaviour. Their interpersonal relationships with family and friends were significantly strained and, in some cases, completely severed. Participants in the HDFG showed a greater proclivity toward social isolation as a result. They also demonstrated a heightened sensitivity toward and awareness of how their illness was perceived by others and how people behaved toward them. They felt they were no longer able to maintain social relationships or carry out gainful employment. These experiences support findings by Walker29 who developed the theme of loss in their article. Our participants reflected upon the physical, social, and economic losses that may occur as a result of high levels of disability associated with LBP.12
Public transportation was a major topic of conversation in our focus groups. Most participants agreed that many of their experiences using public transportation were unpleasant and this provided a clear example of the challenges that LBP sufferers face as a result of living with an invisible condition. The uncomfortable seating and less than smooth rides had physical consequences for LBP patients. However, previous literature has focused primarily on the LBP in transit operators rather than passengers, suggesting that drivers’ seats needed to be ergonomically evaluated and adjusted accordingly.41 Our data suggest an equally important need is to also assess and evaluate the passengers’ perspective. A significant portion of the experiences described by the participants pertain to the effects of environmental and personal factors as articulated in the ICF model.
Previous quantitative studies suggest LBP sufferers are subjected to loss of employment, social identity and inequality; experience isolationism, depression, distressing experiences; as well as pain, disability and low well-being.3,5,13 However, there are fewer qualitative studies exploring the in-depth understanding of patients’ pain experiences with LBP.13,28 A recent systematic review identified three overarching themes emergent from 28 qualitative studies on chronic LBP: impact on self; relationships with family and friends, and health providers and organizations; and coping.13,28 Yet, few of the included the qualitative studies assessed the effect of age, gender, physicality, temporality and disability on patients’ experiences. Our study adds to this gap in the literature by having stratified our focus groups into low and high disability. The two groups described similar experiences, though their salience and
consequences varied considerably. This offers an important first step toward understanding the experiences and impact of different levels of LBP and disability. Future research should go beyond the binary distinction used here, to explore how more subtle differences in levels of LBP and disability affect experiences and behaviours of those afflicted.
Our findings confirm that disability associated with LBP has multiple and often simultaneous effects.42 For example, participants indicated that physical pain contributed to their inability to complete activities or participate in events which in turn influenced people’s attitudes towards them, friendships, and sense of isolation. This supports the reported direct interaction between body function, activities, participation, and environmental factors of the ICF model.43
Our findings highlight the benefits of using a bio-psychosocial model, specifically the ICF model, to interpret our data. Our findings support the connections among the domains of the ICF model as manifested in the lives of those afflicted with LBP. The feedback loop between the domains in the framework is reflected in the description of participants’ lived experiences in our study. Our findings support the contention that personal factors influence the other domains and humanizes the ICF framework by valuing and respecting the uniqueness of the person.11,43 Thus, our study adds to the paucity of literature assessing the potential utility of the ICF in clinical settings.
Strengths and limitations
The use of the ICF framework is a major strength of our study. Its expansive framework has been shown to be useful and generalizable in a variety of scenarios and is applicable to other health conditions and disabilities.23 Additionally, the connections between our data and data previously collected in other studies that also utilized the ICF framework affirms our decision to use this model.44 Other strengths of our study relate to our focus on eliciting participants’ everyday experiences living with LBP. We recruited participants with varying demographic profiles and low and high levels of disability. The qualitative approach encouraged participants to share freely and the results are likely to be clinically applicable.
There were limitations in the study as well. First, despite efforts to recruit participants and extend data collection period, we were unable to achieve our predetermined sample estimate per focus group. Second, we were unable to represent fully the similarities and differences between employed and unemployed participants, as most focus group respondents were unemployed, which may suggest that employed people have less time to participate in focus groups. Third, we were only able to conduct one high disability focus group. Our results showed that LBP patients with high disability experienced greater restriction in mobility (transportation), which could be an indication that attending focus groups was more difficult for these persons. We suggest that further research be conducted in this regard.
A selection of published research by CMCC faculty 95 Esson et al
Fourth, the limited age distribution of participants impacts our ability to interpret their lived experiences. Fifth, the sample only captured the perspectives of chiropractic care seekers, and may underrepresent LBP sufferers with sub-clinical symptomology, or who seek traditional medical care or no care at all. Finally, we crudely differentiated subjects into low and high disability groups that may not account for more subtle distinctions with regard to LBP severity. Further research might include a middle group to help detect more subtle differences with regard to LBP severity.
Significance / implications
Our study raises awareness about the importance of environmental and personal factors in the ICF framework and their unique interaction with, and influence on persons’ lived experiences. This information facilitates clinicians by encouraging them to consider these factors in their understanding of their patients’ disability and modifying their management strategies.
Also, our data contributes an important component to an international, collaborative project by providing a unique local Canadian perspective of how LBP patients experience disability. We were able to determine some of the environmental and personal factors on the ICF framework, which LBP patients describe as affecting their disability and functioning. The data will complement qualitative data collected in Norway and Botswana. Using similar qualitative methodology, the data collected from different regions make it possible to access results across cultures and nations, strengthening the ability for regional and cultural comparisons. This will aid in the creation of a standardized assessment tool which will contribute to improved patient centered models of care and facilitate clinicians’ ability to better assess and document disability in LBP patients within the context of the ICF framework.
Conclusion
Our study supports the notion that LBP is associated with varying social and psychological consequences in sufferers’ daily lives that may not be assessed, documented nor addressed in their clinical care. The ICF framework addresses the often-overlooked social factors of the biopsychosocial model but also includes the impact of environmental and personal factors. The findings of our study support the need to measure and address important social factors, often underrepresented in previous work.45,46 Furthermore, our findings highlight the inherent interrelatedness of the dimensions of the ICF framework as they manifest in the narratives describing the lived experiences of people who suffer from LBP, while valuing and respecting the uniqueness of the person.
References
1. Cassidy JD, Carroll LJ, Côté P. The Saskatchewan health and back pain survey: the prevalence of low back pain and related disability in Saskatchewan adults. Spine 1998; 23(17): 18601866.
2. Vos T, Barber R M, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, Murray C J L, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease 2013. Lancet 2015; 386(9995): 743-800.
3. Mutubuki EN, Luitjens MA, Maas ET, Huygen FJPM, Ostelo RWJG, van Tulder MW, van Dongen JM. Predictive factors of high societal costs among chronic low back pain patients. Eur J Pain. 2019; 24(2): 325-337.
4. Van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol. 2002; 16(5): 761-775.
5. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira MI, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet 2018; 391(10137): 2356-2367.
6. Wong JJ, Côté P, Sutton D A, Randhawa K, Yu H, Varatharajan S, et al. Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain. 2017; 21: 201-216.
7. Glenton C. Chronic back pain sufferers--striving for the sick role. Soc Sci Med. 2003; 57(11):2243-2252.
8. Crowe M, Whitehead L, Gagan M J, Baxter GD, Pankhurst A, Valledor V. Listening to the body and talking to myself – the impact of chronic lower back pain: a qualitative study. Int J Nurs Stud. 2009; 47(5): 586-592.
9. Dima A, Lewith GT, Little P, Moss-Morris R, Foster NE, Bishop FL Identifying patients’ beliefs about treatments for chronic low back pain in primary care: a focus group study. Br J Gen Pract. 2013; 63(612): e490-e498.
10. Holloway I, Sofaer-Bennett B, Walker J. The stigmatisation of people with chronic back pain. Disabil Rehabil. 2007; 29(18): 1456-1464.
11. Darlow B1, Dean S, Perry M, Mathieson F, Baxter GD, Dowell A. Easy to harm, hard to heal: patient views about the back. Spine 2015: 40(11): 842-850.
12. Froud R, Patterson S, Eldridge S, Seale C, Pincus T, Rajendran D, Underwood M. A systematic review and metasynthesis of the impact of low back pain on people’s lives. BMC Musculoskel Dis. 2014; 15: 50.
13. Smith JA, Osborn M. Pain as an assault on the self: An interpretative phenomenological analysis of the psychological impact of chronic benign low back pain. Psychol Health. 2007; 22(5): 517-534.
14. Nolet PS, Kristman VL, Côté P, Carroll LJ, Cassidy JD. Is low back pain associated with worse health-related quality of life 6 months later? Eur Spine J. 2015; 24(3): 458-466.
15. Walker J, Sofaer B, Holloway I. The experience of chronic back pain: Accounts of loss in those seeking help from pain clinics. Eur J Pain. 2006; 10(3): 199-207.
16. Snelgrove S, Edwards S, Liossi C. A longitudinal study of patients’ experiences of chronic low back pain using interpretative phenomenological analysis: changes and consistencies. Psychol Health. 2013; 28(2): 121-138.
CMCC Research Report 2018–2020 96
17. World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva: WHO; 2001.
18. Madans JH, Loeb ME, Altman BM. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: the work of the Washington Group on Disability Statistics. BMC Pub Health. 2011; 11 Suppl 4: S4.
19. Cieza A, Fayed N, Bickenbach J, et al. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil. 2016; Mar 17: 1-10.
20. Morgan D L. Focus Groups. In L. M. Given (Ed.) The SAGE Encyclopedia of Qualitative Research Methods. SAGE Publications, Inc., 2008: 353-355.
21. WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) [Internet]. World Health Organization. World Health Organization; 2019 [cited Jan 30 2020]. Available from: https://www.who.int/classifications/icf/more_whodas/en/
22. World Health Organization (WHO) (2002). Towards a common language for functioning, disability and health: ICF - The International Classification of Functioning, Disability and Health (ICF). Geneva: WHO. http://www. who.int/ classifications/icf/en/
23. Geyh S, Schwegler U, Peter C, Müller R. Representing and organizing information to describe the lived experience of health from a personal factors perspective in the light of the International Classification of Function, Disability and Health (ICF): a discussion paper. Dis Rehabil. 2019: 41(14): 17271738.
24. Wawrzyniak KM, Finkelman M, Schatman ME, Kulich RJ, Weed VF, Myrta E, DiBenedetto DJ. The World Health Organization Disability Assessment Schedule-2.0 (WHODAS 2.0) in a chronic pain population being considered for chronic opioid therapy. J Pain Res. 2019:12 1855–1862.
25. Von Korff M, Crane PK, Alonso J, Vilagut G, Angermeyer MC, Bruffaerts R, Ormel J. Modified WHODAS-II provides valid measure of global disability but filter items increased skewness. J Clin Epidemiol. 2008; 61(11): 1132-1143.
26. Silva C, Coleta I, Silva AG, Amaro A, Alvarelhão J, Queirós A, Rocha N. Adaptation and validation of WHODAS 2.0 in patients with musculoskeletal pain. Revista De Saúde Pública. 2013; 47(4): 752.
27. Marx BP, Wolf EJ, Cornette MM, Schnurr PP, Rosen MI, Friedman MJ, Keane TM, Speroff T. Using the WHODAS 2.0 to assess functioning among veterans seeking compensation for posttraumatic stress disorder. Psychiatric Serv. 2015; 66: 13121317.
28. Snelgrove S, Liossi C. Living with chronic low back pain: a metasynthesis of qualitative research. Chron Illness. 2013: 9(4): 283-301.
29. Ashby S, Fitzgerald M, & Raine S. The impact of chronic low back pain on leisure participation: implications for occupational therapy. Br J Occup Ther. 2012; 75(11): 503-508.
30. Naughton F, Ashworth P, Skevington SM. Does sleep quality predict pain-related disability in chronic pain patients? The mediating roles of depression and pain severity. Pain. 2007;127(3): 243–252.
31. Fu Y, Mcnichol E, Marczewski K, Closs SJ. Patientprofessional partnerships and chronic back pain selfmanagement: a qualitative systematic review and synthesis. Health SocCare Commun. 2015;24(3):247–259.
32. Hopayian K, Notley C. A systematic review of low back pain and sciatica patients expectations and experiences of health care. Spine J. 2014;14(8):1769–1780.
33. Matthews CK. To tell or not to tell: The management of privacy boundaries by the invisibly disabled. In: Annual meeting of the Western States Communication Association, San Jose, CA., 1994.
34. Pape TL, Kim J, Weiner B. The shaping of individual meanings assigned to assistive technology: a review of personal factors. Disabil Rehabil. 2002; 24 (1/2/3): 5-20.
35. Shinohara K, Wobbrock J. In the shadow of misperception: Assistive technology use and social interactions. Paper presented at the CHI 2011, Vancouver BC, Canada May 712, 2011: 705-714.
36. Corbett M, Foster NE, Ong BN. Living with low back pain-Stories of hope and despair. Soc Sci Med. 2007; 65(8): 1584.
37. Walker J, Sofaer B, Holloway I. The experience of chronic back pain: Accounts of loss in those seeking help from pain clinics. Eur J Pain. 2006; 10(3): 199-207.
38. Jette AM, Haley SM, Kooyoomjian JT. Are the ICF activity and participation dimensions distinct? J Rehabil Med. 2003; 35(3): 145-149.
39. Badley EM. Enhancing the conceptual clarity of the activity and participation components of the international classification of functioning, disability, and health. Soc Sci Med. 2008; 66(11): 2335-2345.
40. Resnik L, Plow MA. Measuring participation as defined by the international classification of functioning, disability and health: an evaluation of existing measures. Arch Phys Med Rehabil. 2009; 90(5): 856-866.
41. Okunribido OO, Shimbles SJ, Magnusson M, Pope M. City bus driving and low back pain: a study of the exposures to posture demands, manual materials handling and wholebody vibration. Applied Ergon. 2007; 38(1): 29-38.
42. Arnow BA, Blasey CM, Constantino MJ, Robinson R, Hunkeler E, Lee J, Hayward C. Catastrophizing, depression and pain-related disability. Gen Hosp Psych. 2011; 33(2): 150-156.
43. Geyh S, Peter C, Müller R, Bickenbach JE, Kostanjsek N, Ustun, BT, Stucki G, Cieza A. The personal factors of the International Classification of Functioning, Disability and Health in the literature – a systematic review and content analysis. Disabil Rehabil. 2011; 33(13-14): 1089-1102.
44. Kostanjsek N. Use of The International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems [Internet]. BMC public health. BioMed Central; 2011 [cited Jan 30 2020].
45. Carr JL, Moffett JAK. Review Paper: The impact of social deprivation on chronic back pain outcomes. Chron Illness. 2005;1(2):121–129.
A selection of published research by CMCC faculty 97 Esson et al
46. Campbell P, Jordan KP, Dunn KM. The role of relationship quality and perceived partner responses with pain and disability in those with back pain. Pain Med. 2012;13(2):204–214.
OriginallypublishedintheJournaloftheCanadianChiropractic Association,2020Apr;64(1):16-31.
Reproducedwithpermission.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7250510/
CMCC Research Report 2018–2020 98
The Prevalence of Anxiety, Stress and Depressive Symptoms in Undergraduate Students at the Canadian Memorial Chiropractic College
C
Abstract
Objective:
(1) Determine the one-week prevalence of moderate to extreme symptoms of anxiety, stress and depression in chiropractic undergraduate students. (2) Determine whether the prevalence varies across gender and year of study.
Participants:
Undergraduate students at the Canadian Memorial Chiropractic College (CMCC).
Methods:
A cross-sectional study was conducted in fall 2017 to measure self-reported symptoms of anxiety, stress and depression using the DASS-21.
Results:
The participation rate was 67.0% (510/766). The one-week prevalence of moderate to extreme symptoms was 19.0% (95% CI: 13.0-25.0) for depression; 32.6% (95% CI: 24.7-40.3) for
anxiety and 21.8% (95% CI: 15.6-28.1) for stress. The prevalence of stress varied significantly across gender: 25.4% (95% CI: 20.530.3) for females versus 16.3% (95% CI: 11.2-21.3) for males. The one-week prevalence of depressive (24.8%; 95% CI: 17.632.0) and anxiety (40.9%; 95% CI: 32.6-49.1) symptoms peaked in second year.
Conclusions:
Self-reported symptoms of anxiety, stress and depression are common in CMCC students.
OriginallypublishedintheJournalofAmericanCollegeHealth. 2020May5;1-6.Onlineaheadofprint.
ReproducedwithpermissionfromTaylor&Francis.
AccessOnline:https://doi.org/10.1080/07448481.2020.1751173
A selection of published research by CMCC faculty 99 Health and Wellness
Meckamalil
1 , Brodie B 1 , Hogg-Johnson S 1 2 , Carroll LJ 3 , Jacobs C 1 , Côté P 4 5 1CanadianMemorialChiropracticCollege, 2UniversityofToronto, 3UniversityofAlberta, 4UniversityofOntarioInstituteofTechnology 5UOIT-CMCCCentreforDisabilityPreventionandRehabilitation
Ontario Chiropractors' Knowledge of Exercise Guidelines for Pregnant Patients
Weis CA1 , Baas E 2 , Ciesla K 2 , Kimpinski C 2 , Landsman V 3 1CanadianMemorialChiropracticCollege, 2Privatepractice, 3UniversityofToronto
Abstract
Objective:
To describe the Ontario chiropractors’ knowledge regarding the current guidelines for exercise during pregnancy through a knowledge score and exploring its distribution across different strata of interest including gender, experience, location of practice and type of practice.
Methods:
A previously used survey was modified and sent to 500 randomly selected Ontario chiropractors. Demographic and continuing education questions were included, and the knowledge score was calculated using 10 items.
Results:
The differences between the knowledge score values across the four strata of interest were not statistically significant. The average knowledge score in the sample of respondents was low (5.2 out of 10) and highly variable (SD=1.8).
Conclusions:
The average knowledge score of the respondents was found to be low and highly variable but not statistically or practically
different across various strata of interest. A well-designed curriculum or post-graduate courses may be beneficial for practicing chiropractors in Ontario.
OriginallypublishedintheJournaloftheCanadianChiropractic Association,2019Apr;63(1):5-17.
ReproducedwithpermissionfromtheJournaloftheCanadian ChiropracticAssociation.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6493206/
CMCC Research Report 2018–2020 100
Health-Related Quality of Life and Balance Confidence Among Participants in a Senior Community-Based Exercise (SWIFT) Program Compared to Age Matched Controls: A Cross-Sectional Study
Cougle E1,2 , Black M 3 , Hogg-Johnson S1,4,5 , Decina P1, Tibbles A1, Mior S1,2,4,5 1CanadianMemorialChiropracticCollege, 2UniversityofOntarioInstituteofTechnology, 3Tri-CongregationalChurches, 4UniversityofToronto, 5Centre forDisabilityPreventionandRehabilitationatOntarioTechUniversityandCanadianMemorialChiropracticCollege
Abstract
Background
Staying Well, Independent and Fit Together (SWIFT), a seniors’ exercise program, aims to promote health, strength, mobility and community engagement. We compared quality of life and balance confidence in SWIFT participants and non-participants, aged 60 years and older.
Methods
Cross-sectional study comparing participants and nonparticipants in SWIFT program using Older People’s Quality of Life Questionnaire (OPQOL) and Activities-specific Balance Confidence Scale (ABCS).
Results
Seventy participants completed surveys, 41 in experimental and 29 in control group. We found a statistically significant between group difference favoring the control group in overall OPQOL score but not in OPQOL subscale nor overall ABCS scores. Participants in both groups participating in weekly exercises had non-significantly higher quality of life subscale scores.
Conclusion
Results suggest seniors in both study groups who participate in exercise have non-significantly higher quality of life scores compared to those who do not participate in exercise. Participation in the SWIFT exercise program or activity in general, contributes to quality of life in seniors.
OriginallypublishedintheJournaloftheCanadianChiropractic Association2020Apr;64(1):55–64.
ReproducedwithpermissionfromtheJournaloftheCanadian ChiropracticAssociation.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7250509/
A selection of published research by CMCC faculty 101
The Association Between Psychological and Social Factors and Spinal Pain in Adolescents
Batley S1 , Aartun E 2 3 , Boyle E 4 5 , Hartvigsen J 4 6 , Stern PJ1 , Hestbæk L 4 6 1CanadianMemorialChiropracticCollege, 2UOIT-CMCCCentreforDisabilityPreventionandRehabilitation, 3UniversityofOslo, 4Universityof Southern Denmark, 5UniversityofToronto, 6NordicInstituteofChiropracticandClinicalBiomechanics
Abstract
Spinal pain, back pain, and/or neck pain begins early in life and is strongly associated with spinal pain in adulthood. Understanding the relationship between psychological and social factors and adolescent spinal pain may be important in both the prevention and treatment of spinal pain in this age group. We aimed to determine if psychological and social factors were associated with spinal pain in a cross-sectional study of a school-based cohort of 1279 Danish adolescents aged 11–13, who were categorized into “any” and “substantial” spinal pain. “Substantial spinal pain” was defined as a lifetime frequency of “sometimes” or “often” and a pain intensity of at least two on the revised Faces Pain Scale. Logistic regression analyses, stratified by sex, were conducted for single and all variables together. Eighty-six percent of participants reported “any spinal pain” and 28% reported “substantial spinal pain”. Frequency of psychological and social factors was significantly higher in those with spinal pain compared to those without. As the frequency of psychological and social factors increased, the odds of both “any spinal pain” and “substantial spinal pain” also increased.
Conclusion:
Psychological and social factors may be important determinants in adolescent spinal pain.
What is Known:
• Spinal pain begins early in life to reach adult levels by age 18. Spinal pain in adolescence is strongly associated with spinal pain in adulthood.
• In adults, psychological and social factors and spinal pain are strongly related; however, this relationship in adolescence is poorly understood.
What is New:
• Adolescents with spinal pain reported a significantly higher frequency of psychological factors and loneliness and lower levels of pupil acceptance.
• Adolescents reporting higher levels of loneliness, lower levels of pupil acceptance, and increased frequency of psychological factors had increased odds of reporting “substantial spinal pain”.
OriginallypublishedintheEuropeanJournalofPediatrics2019 Mar;178(3):275-286.Epub2018Nov21.
ReproducedwithpermissionfromSpringerNature.
AccessOnline:https://doi.org/10.1007/s00431-018-3291-y
CMCC Research Report 2018–2020 102
Clinicians’ Views About the Experience of Disability Due to Low Back Pain. Results From a Focus Group Study
Cedraschi C1, Campello M2 , Salmi LR 3,4,5 , Côté P6,7 1GenevaUniversity, 2NewYorkUniversity, 3UniversityBordeaux,, 4INSERM, ISPED, 5CentreHospitalierUniversitairedeBordeaux, 6Center for DisabilityPreventionandRehabilitation,UniversityofOntarioInstituteofTechnologyandCanadianMemorialChiropracticCollege, 7Ontario Tech University
Abstract
Purpose:
For clinicians, treating the cause of non-pathological low back pain (LBP) is central. For patients, it is how LBP limits their activities of daily living. Little is known about clinicians’ understanding of disability and the patient’s perspective. We conducted a qualitative study to examine how clinicians involved in the care of patients with BP describe and define disability, its associated changes, and rehabilitation.
Methods:
Two focus groups (FGs) were conducted with spine specialists including eleven confirmed orthopedic surgeons and neurosurgeons, ten advanced residents, and five other clinicians. Participants were questioned about their views on disability, what it means to them and to the patients. Responses were collected by two independent observers using Metaplan techniques. Large stickers were used to collect participants’ responses/ideas; the stickers were posted on billboards so the FGs could check them during the discussion. Metaplan was used to aggregate responses.
Results:
Disability was viewed as a major source of physical limitations, difficulties in performing daily activities, associated with
emotional distress, and raising legitimacy issues. Changes in roles engaged the social component. Considered from the patients’ perspective, negative emotions and social issues were emphasized, along with the patients’ resources. For rehabilitation, the participants emphasized patient-centered care, teamwork, and objectives for care.
Conclusion:
The participants pointed to disability as an umbrella term for impairments, activity limitations, and participation restrictions. They underlined the necessity for clinicians to help patients define their level of optimal functioning when faced with BP, utilizing adaptation and teamwork within the therapeutic relationship.
OriginallypublishedinEuropeanSpineJournal,2020 Aug;29(8):1953-1958.Epub2020May20.
ReproducedwithpermissionfromSpringerNature.
AccessOnline:https://doi.org/10.1007/s00586-020-06463-y
A selection of published research by CMCC faculty 103
Exploring Chiropractic Services in the Canadian Forces Health Services – Perceptions of Facilitators and Barriers Among Key Informants
Abstract
Introduction:
Musculoskeletal (MSK) conditions have a significant impact on the health and operational readiness of military members. The Canadian Forces Health Services (CFHS) provides a spectrum of health services in managing Canadian Armed Forces (CAF) personnel health care needs with on-base and off-base services provided by civilian and uniformed health care professionals, including chiropractors. Although chiropractic services are available in US DoD and VA systems, little is known about the facilitators and barriers to integrating on-base chiropractic services within the CFHS. This study explored key informants’ perceptions of facilitators and barriers to the integration of onbase chiropractic services within the CFHS.
Methods:
We conducted a qualitative study to describe and understand how an integrated chiropractic service could be designed, implemented, and evaluated within the current interdisciplinary CFHS. Telephone interviews were conducted, using a semistructured interview guide, to explore key informants’ perceptions and experiences of chiropractic care within the CFHS. In total, we invited 27 individuals across Canada to participate; 15 were identified through purposeful sampling, 12 through a snowball sampling technique, and 2 declined. The 25 participants included military personnel (52%), public servants and contractors employed by the Department of Defense (24%), as well as civilian health care providers (24%). All participants were health care providers [physicians (MD) (7), physiotherapists (PT) (13), chiropractors (DC) (5)]. Interviews were audio-recorded and transcribed verbatim. Transcripts were prepared and analyzed using an interpretivist approach that explored key informants’ perceptions and experiences.
Results:
Qualitative analysis revealed numerous facilitators and barriers to chiropractic services in the CFHS. These were categorized under three broad themes: base-to-base variations, variable gatekeeper roles, and referral processes. Barriers to integrating chiropractic
services included: lack of clarity about a chiropractor’s clinical knowledge and skills; CFHS team members’ negative prior experiences with chiropractors (e.g., inappropriate patient-focused communication, clinical management that was not evidencebased, ignorance of military culture); suboptimal bi-directional communication between CAF personnel and DCs across bases; and wide-ranging perspectives pertaining to duplication of services offered by PTs and DCs in managing MSK conditions. Facilitators associated with the integration of chiropractic services within a collaborative and interdisciplinary CAF environment included: patient benefits associated with multiple approaches utilized by different providers; adoption of up-to-date, highquality evidence and guidelines to standardize care and curtail “dependency” between patient and providers; and co-location of providers to strengthen existing interprofessional communication and relationships. Key informants called for patient care that is collaborative, integrated and patient-centered, rather than “patient-driven” care; civilian providers understanding and respecting military culture rather than assuming transferability of patient management processes from the public civilian sector; standardization of communication protocols and measures to evaluate outcomes of care; and the need to move slowly and respectfully within the current CAF health care system if planning the on-base implementation of chiropractic services.
Conclusion:
This study illuminated many opportunities and barriers, in complex and diverse domains, related to introducing collaborative chiropractic services in the CFHS. The findings are relevant to increasing understanding and strengthening interprofessional collaborative care within the unique CAF health care delivery system.
Introduction
Musculoskeletal (MSK) conditions have a significant impact on the health and operational readiness of Canadian Armed Forces
CMCC Research Report 2018–2020 104 Knowledge Translation and Health Policy
Mior SA1 , Vogel E 2 , Sutton D 3 , French S 3, 4 , Côté P1, 2 , Nordin M5 , Loisel P6 , Laporte A 6, 7 1CanadianMemorialChiropracticCollege, 2UniversityofOntarioInstituteofTechnology, 3Queen'sUniversity, 4MacquarieUniversity, 5New York University, 6UniversityofToronto, 7Canadian Centre for Health Economics
(CAF) personnel.1 MSK conditions are the most common reason for CAF personnel not being deployed.2 Further, MSK injuries are responsible for 42% of all medical releases.3 Specifically, back pain is one of the most common reasons for soldiers not being deployed and is the second most common activitylimiting acute injury.2,4 In 2013, 12% of CAF regular force medical releases were attributed to lumbar injuries.3 When symptoms persist, chronic back pain may impact many aspects of a CAF service member’s life, including: physical deconditioning; excessive use of prescription drugs; marked dependence on health care providers, spouse and family; withdrawal from social context; and continued functional impairment.5 The effective and cost-effective management of back pain is an important issue for individual members and the CAF as a whole.6
“Caring for Canada’s Ill and Injured Military Personnel,” a report of the Standing Committee on National Defense (2014) heard evidence about chiropractic services offered to US Military Health System (MHS) personnel and its impact on keeping soldiers at work.7 The US MHS under the Department of Defense (DoD) included chiropractic services for active duty military personnel following the completion of an initial demonstration project in 1995.8,9 Currently, chiropractors provide conservative care, in cooperation with various health care providers, in primary care, physical therapy, orthopedics and sports medicine.10 Chiropractic care is provided on referral and within a set of privileges established within each system and facility.8 Two studies suggest significant improvements in pain, function, global improvement and satisfaction with care in samples of active duty military personnel receiving chiropractic care and standard medical care as compared to those receiving standard medical care alone.11,12
Currently, the Canadian Forces Health Services (CFHS) provides a spectrum of health care services, including care provided in civilian facilities when services are not provided on-base.6 Chiropractic care is an eligible CAF health practitioner benefit when prescribed by a physician, and is accessed off-base, outside the military health system. Care is authorized within a 10-visit limit per condition, after which a physician’s review is required to determine if further care is necessary (http:// ww.forces.gc.ca/en/caf-community-health-services-benefitsdrug-coverage/comprehensive-medical-care. page).
Historically in the CFHS, on-site chiropractic care was available during a 6-month pilot study at a CAF Base hospital, where two chiropractors provided outpatient chiropractic care with physicians’ referrals for treatment of MSK disorders.13 Care was available in 10-visit increments and supported with appropriate clinical documentation. Physicians referred CAF military personnel to chiropractic services for axial, MSK complaints; if the complaint was unresponsive to, or the waiting list too long, for physiotherapy; a prior positive response to chiropractic care; or if the patient requested chiropractic care.13 Patients reported high levels of satisfaction with their chiropractic care, as well
as with office accessibility, clinic hours and the chiropractor’s ability to answer questions; none reported dissatisfaction with their chiropractic care.13 Although specific outcomes were not reported, one-third of patients indicated that they expected better results or rate of improvement.13 Referring physicians perceived an increased demand from patients for chiropractic services and they were satisfied with the chiropractic services provided.13
The Standing Committee on National Defense in Canada recommended that a comprehensive MSK strategy be developed to better understand injury causes, encourage early treatment and reduce barriers for current soldiers to obtain the required care.7 Although chiropractic services are integrated into the US DoD system, barriers to integration exist, particularly if such services are thrust upon them.14 Dunn et al identified barriers to the integration of chiropractic care in the US MHS, including: work place isolation; lost opportunities to influence communication; policy and practice without a chiropractor in a leadership role; precarious employment and decreased integration of chiropractors within the system resulting from contractor-status, or employee of a contractor; supervision by non-chiropractors; and refusal of referral by a gatekeeper. Facilitators to integration included documentation requirements in an electronic health record to aid collaboration between providers and opportunities for clinical education.
In addition to the Standing Committee’s recommendation of a comprehensive management strategy for MSK, the federal government’s response suggested “examining whether earlier interventions by alternative health care professionals to treat MSK injuries are a workable and worthwhile approach.”15 However, we know little about the facilitators and barriers to integrating on-base alternative health care professionals, such as chiropractors within the CFHS.
Purpose
We employed a qualitative, exploratory research design to understand and describe key informants’ perspectives on how an integrated chiropractic service could be designed, implemented, and evaluated within the current interdisciplinary CFHS.
Methods
Approvals and Recruitment
Ethics approval was received from the Research Ethics Boards at the University of Ontario Institute of Technology (# 15-049) and the Canadian Memorial Chiropractic College (# 152019). Agreement to conduct the study was provided by the Canadian Deputy Surgeon General, CFHS (7 June 2016). All study participants provided informed consent.
Purposeful sampling16 was used to recruit participants. Inclusion criteria included: English-speaking health care professionals, military personnel, and researchers with
A selection of published research by CMCC faculty 105
Mior et al
extensive experience and in-depth understanding of health care delivery and interprofessional collaborative practice within the military setting in Canada. Additional participants with expert knowledge and/or experience in relation to the delivery of health care within the CFHS were identified using snowball sampling technique.16
Interview Schedule and Procedures
Telephone interviews were conducted using an interview guide with open-ended questions.17–20 The interview guide was informed by expert opinion, as well as health, social and behavioral theories addressing barriers and facilitators to accessing chiropractic care (See Appendix A). After the first eight interviews, additional probes were developed and questions slightly revised. Interviewing continued until the research team ascertained that saturation of responses to key questions was achieved.21,22
All interviews were conducted by two members of the research team, both health care professionals, who were not physicians, chiropractors nor physiotherapists, thereby mitigating potential researcher bias.20 The interviews were conducted between September 2016 and February 2017 and were 45-to 60-minutes in duration.
Interviews were audio-recorded, exported to an encrypted USB key and transcribed verbatim. The project coordinator reviewed all transcripts for accuracy against the recorded sessions. Content errors were corrected, and names along with other potential identifying information removed from transcripts prior to coding. Each participant was invited to review and edit their transcript (member checking).
Analytic Approach
Transcripts were analyzed using an interpretivist approach that explored participants’ experiences and thoughts.23,24 Each transcript was examined using qualitative content analysis.25,26 Categories and subcategories were collapsed and interconnected to develop meaning and explanation of the patterns identified in the data.
The analysis proceeded in an iterative and inductive manner. After the first three interviews were completed and transcribed, the transcripts were sent to three research team members who independently coded each transcript. The researchers then met regularly to review and reach consensus on coding, examining and defining codes, and developing a referent codebook. The coding structure and the related transcript reference data were entered into qualitative data analysis software (NVivo Pro Version 11.4.1 for Windows, QSR International (Americas) Inc., Burlington, MA, USA).
Results Participant Characteristics
Table I provides information on study participants’ professional
backgrounds. Participants included military personnel (52%), public servants and contractors employed by the Canadian DoD (24%), and civilians (24%), distributed across Canada. Military participants included ranks of Chief Warrant Officer, Captain, Lieutenant, Lieutenant Colonel, and Colonel. Slightly more than half of the military participants were deployed at least once over the course of their career. Participants self-identified as medical doctors (MD), physical therapists (PT), and chiropractors (DC). The chiropractor participants, all situated off-base, had recently provided care for CAF service members. Of the 25 study participants, the majority were male (n = 76%).
Participants identified barriers (Table II) and opportunities (Table III), with categories described within each, that could potentially serve to integrate chiropractic services within the CFHS.
Barriers to Integrated Chiropractic Services in the CFHS During the interviews, participants identified a range of factors and issues that could potentially act as barriers to the design, implementation and evaluation of chiropractic services within the CFHS.
ReferringtoOff-baseChiropracticServices:“Referringtoperson, notprofession.”
One emergent barrier to integration was the significant base-tobase variation with respect to referrals to chiropractic services. Additionally, notable differences were illuminated with respect to the critical “gatekeeper” role in the Care Delivery Unit (CDU) of CAF bases.
Within the CFHS, the function of the CDU is comparable across all CAF bases; however, they differ in structure and administrative processes. Such regional variation is consistent with findings in the Auditor General of Canada report.27 Participants noted that the triage of MSK conditions in sick parade (military medical triage system that occurs every morning for patients with acute ailments) varies between bases, but fundamentally is the responsibility of the CDU Medical Officer, who acts as the “gatekeeper” for referrals both on- and off-base. Participants’ recognized the role of medical physicians in overseeing the primary care of CAF personnel, but noted physicians’ limitations when assessing MSK injuries. Consequently, at adequately resourced bases, the “lead” physiotherapist or designate would triage MSK conditions at sick parade, overseeing the referral process when deemed necessary. A MD participant explained that within the CFHS, there is no “direct access” to a chiropractor.
Participants on larger and better-resourced bases, indicated that Medical Officers may direct uniformed physiotherapists to make decisions regarding the need for, or appropriateness of, referrals off-base.
Thecurrentwaythatitworks…isthataMedicalOfficer canmaketherecommendationtothephysiotherapy
CMCC Research Report 2018–2020 106
ductedbetweenSeptember2016andFebruary2017and
Interviewswereaudio-recorded,exportedtoanencrypted USBkeyandtranscribedverbatim.Theprojectcoordinator reviewedalltranscriptsforaccuracyagainsttherecorded sessions.Contenterrorswerecorrected,andnamesalong withotherpotentialidentifyinginformationremovedfrom transcriptspriortocoding.Eachparticipantwasinvitedto Transcriptswereanalyzedusinganinterpretivistapproach experiencesandthoughts.23,24 EachtranscriptwasexaminedusingqualitativecontentanalCategoriesandsubcategorieswerecollapsedand interconnectedtodevelopmeaningandexplanationofthe
Interviewswereaudio-recorded,exportedtoanencrypted USBkeyandtranscribedverbatim.Theprojectcoordinator reviewedalltranscriptsforaccuracyagainsttherecorded sessions.Contenterrorswerecorrected,andnamesalong withotherpotentialidentifyinginformationremovedfrom transcriptspriortocoding.Eachparticipantwasinvitedto Transcriptswereanalyzedusinganinterpretivistapproach experiencesandthoughts.23,24
EachtranscriptwasexaminedusingqualitativecontentanalCategoriesandsubcategorieswerecollapsedand interconnectedtodevelopmeaningandexplanationofthe
Theanalysisproceededinaniterativeandinductivemanrstthreeinterviewswerecompletedandtranscribed,thetranscriptsweresenttothreeresearchteam memberswhoindependentlycodedeachtranscript.The researchersthenmetregularlytoreviewandreachconsensus ningcodes,anddevelopinga referentcodebook.Thecodingstructureandtherelatedtranscriptreferencedatawereenteredintoqualitativedataanalysissoftware(NVivoProVersion11.4.1forWindows,QSR
Theanalysisproceededinaniterativeandinductivemanrstthreeinterviewswerecompletedandtranscribed,thetranscriptsweresenttothreeresearchteam memberswhoindependentlycodedeachtranscript.The researchersthenmetregularlytoreviewandreachconsensus ningcodes,anddevelopinga referentcodebook.Thecodingstructureandtherelatedtranscriptreferencedatawereenteredintoqualitativedataanalysissoftware(NVivoProVersion11.4.1forWindows,QSR
profesParticipantsincludedmilitarypersonnel (52%),publicservantsandcontractorsemployedbythe CanadianDoD(24%),andcivilians(24%),distributed acrossCanada.MilitaryparticipantsincludedranksofChief cer,Captain,Lieutenant,LieutenantColonel, andColonel.Slightlymorethanhalfofthemilitaryparticipantsweredeployedatleastonceoverthecourseoftheir edasmedicaldoctors(MD), physicaltherapists(PT),andchiropractors(DC).Thechiropractor
profesParticipantsincludedmilitarypersonnel (52%),publicservantsandcontractorsemployedbythe CanadianDoD(24%),andcivilians(24%),distributed acrossCanada.MilitaryparticipantsincludedranksofChief cer,Captain,Lieutenant,LieutenantColonel, andColonel.Slightlymorethanhalfofthemilitaryparticipantsweredeployedatleastonceoverthecourseoftheir edasmedicaldoctors(MD), physicaltherapists(PT),andchiropractors(DC).Thechiropractor
viceswithintheCFHS.
design,implementationandevaluationofchiropracticserviceswithintheCFHS.
ReferringtoOff-baseChiropracticServices: “Referring toperson,notprofession.”
ReferringtoOff-baseChiropracticServices: “Referring toperson,notprofession.”
Oneemergentbarriertointegrationwasthesignificant base-to-basevariationwithrespecttoreferralstochiropractic
Oneemergentbarriertointegrationwasthesignificant base-to-basevariationwithrespecttoreferralstochiropractic
TABLEI.
aWithdrew(n = 1).
bDeclinedtoparticipate(n = 1).
TABLEII. ParticipantPerceptionsofBarrierstoIntegrationof ChiropracticServicesWithintheCanadianForcesHealthServices
TABLEII. ParticipantPerceptionsofBarrierstoIntegrationof ChiropracticServicesWithintheCanadianForcesHealthServices
BarrierstoIntegratedChiropracticServicesintheCFHS
BarrierstoIntegratedChiropracticServicesintheCFHS
Category1:Referringtooff-basechiropracticservices
Bora Laskin
department,butitisultimatelythephysiotherapy departmentthatmakesthe “yes” or “no” call.(PT,K15)
So,frommyexperiencehereandatthemanyprevious postingsthatIhavehad,wehaven’treallyseenasignificant needforchiropracticreferraltoanexternalhealthcare providerforthesimplereasonthatwe[physiotherapists] areabletoprovideeveryskillsetandeverypossible interventionthataCAFmembermayrequireaspartoftheir treatmentplan…Theoddcasewhenaspinalmanipulation isindicatedforaparticularconditionsuchasa fixated facetjoint,somethingofthatnature,wheretheyhavea mechanicalobstructionthatalowamplitudehighvelocity mobilizationmaybebeneficial for, we have the flexibilityto refertoachiropractorastheyspecializeinthistechnique. (PT,K3)
• Base-to-basevariation
Category1:Referringtooff-basechiropracticservices
• Base-to-basevariation
• Gatekeeperroles
• Gatekeeperroles
• CareDeliveryUnitMedicalOfficer(CDUMO)mostresponsible memberforchiropracticreferral
• CareDeliveryUnitMedicalOfficer(CDUMO)mostresponsible memberforchiropracticreferral
• Leadphysiotherapistdesignatedtochiropractorreferralroleby CDUMOatbaseswithgreaterresources
• Leadphysiotherapistdesignatedtochiropractorreferralroleby CDUMOatbaseswithgreaterresources
• Decisiontorefertochiropractorbasedonindividualclinician preferenceandexperience,ratherthanasystematicapproach
• Decisiontorefertochiropractorbasedonindividualclinician preferenceandexperience,ratherthanasystematicapproach
Category2:InterprofessionalCommunication
Category2:InterprofessionalCommunication
• Communicationprocessesrelatedtosite-specificresourcesand currentpractices
• Communicationprocessesrelatedtosite-specificresourcesand currentpractices
• Currentpracticesreflectclinicianperspectiveandpastexperience
• Currentpracticesreflectclinicianperspectiveandpastexperience
• Writtencommunication(referral,reports)notstandardized
• Writtencommunication(referral,reports)notstandardized
• Nodialogbetweenhealthcareprovidersonbaseandchiropractors
• Nodialogbetweenhealthcareprovidersonbaseandchiropractors
Category3:Duplicationofhealthcareservices
Category3:Duplicationofhealthcareservices
• Scopeofpracticechange:PTsandchiropractors
• Scopeofpracticechange:PTsandchiropractors
• Difficultydistinguishingchiropractorasaprofessionratherthanan intervention
• Difficultydistinguishingchiropractorasaprofessionratherthanan intervention
• Non-uniformpersonnel,e.g.,chiropractornotabletodeploy
• Non-uniformpersonnel,e.g.,chiropractornotabletodeploy
As a consequence of base-to-base variations in referral processes, and variable enactments of the “gatekeeper” role, the frequency and nature of referrals vary. Specifically, the decision to refer to chiropractors appears to be up to individual clinicians rather than based on a systematic approach.
Inter-professionalCommunication:“Neverenoughinformation”
ExploringChiropracticServicesintheCanadianForcesHealthServices
TABLEIII. ParticipantPerceptionsofOpportunitiestoIntegrate ChiropracticServicesWithintheCanadianForcesHealthServices
MILITARYMEDICINE, Vol.184,May/June2019
OpportunitiestoIntegrateChiropracticServicesintheCFHS
Category1:MSKdisorders
• PrevalenceofMSKconditionsandneedtoprovidecarewhichis clinicalandcost-effective
Category2:Interprofessionalcollaborativecare
• Collaborative,integrated,patient-centeredcare
• Base-to-basevariationdependentuponlocation,size,resources andprimarypurpose
• Co-locationofprovidersstrengtheninginterprofessional communicationandrelationships
Category3:Evidence-basedapproach
• Standardizationofclinicalcareusingclinicalpracticeguidelines baseduponhigh-qualityevidence
Category4:Thespectrumofcare
• KnowledgeofCAFspectrumofcare
• Utilizechiropractors’ fullscopeofpractice
services.Additionally,notabledifferenceswereilluminated withrespecttothecritical “gatekeeper” roleintheCare
Another barrier focused on interprofessional communication, primarily between on-base physiotherapists and off-base service providers. Variations in communication processes were related to available site-specific resources and current practices. Current practices were influenced by past experiences and perspectives of the lead CFHS provider(s). In general, communication, particularly with respect to off-base referrals, was considered suboptimal. However, some on-base CFHS providers stated that they made an effort to share relevant clinical information with off-base providers. In these situations, a referral note may be followed by a phone call to the off-base provider. However, standardization of communication processes in the CFHS was not typical practice:
requireaspartoftheirtreatmentplan Theoddcase whenaspinalmanipulationisindicatedforaparticular conditionsuchasa fixatedfacetjoint,somethingofthat nature,wheretheyhaveamechanicalobstructionthat alowamplitudehighvelocitymobilizationmaybebeneficialfor,wehavethe flexibilitytorefertoachiropractorastheyspecializeinthistechnique.(PT,K3)
Therehasbeennoefforttotryandstandardizecareacross thecountry,Ithinkateverybasetherewillbedifferent interactionsbetweenthebaseandthechiropractors…(PT, K13)
Asaconsequenceofbase-to-basevariationsinreferral processes,andvariableenactmentsofthe “gatekeeper” role, thefrequencyandnatureofreferralsvary.Specifically,the decisiontorefertochiropractorsappearstobeuptoindividualcliniciansratherthanbasedonasystematicapproach.
So,itisreallyaone-waycommunication.We[off-base chiropractor]getthereferralandthenIsubmitaninitial assessmentandaprogressexamandwedon’treallygeta lotoffeedbackfromthemilitary.So,everythingiswritten,it isbycorrespondence.Thereisreallynoface-to-facetime, orconversationsonthephone.Itisalldonethroughemail orwrittenreportsthatwesendbymail.(DC,K24)
Inter-professionalCommunication: “Neverenough information”
Anotherbarrierfocusedoninterprofessionalcommunication,primarilybetweenon-basephysiotherapistsandoff-base serviceproviders.Variationsincommunicationprocesses wererelatedtoavailablesite-specificresourcesandcurrent practices.CurrentpracticeswereinfluencedbypastexperiencesandperspectivesoftheleadCFHSprovider(s).Ingeneral,communication,particularlywithrespecttooff-base
Similarly, the reports received by on-base CFHS health care providers from off-base chiropractors, often fell short of expectations. Participants noted that chiropractors’ reports
A
research
CMCC faculty 107
selection of published
by
Mior et al
International(Americas)Inc.,Burlington,MA,USA).
design,implementationandevaluationofchiropracticser-
BackgroundInvitedInterviewed PurposivesampleMD 6 6 PT 9a 8 SnowballtechniqueMD 1 1 PT 5 5 DC 5 5 Non-healthcare1b 0 Total 2725 aWithdrew(n = 1). bDeclinedtoparticipate(n = 1).
TABLEI. SamplingStrategiesandBackgroundofStudy Participants
MILITARYMEDICINE, Vol.184,May/June2019 https://academic.oup.com/milmed/article/184/5-6/e344/5194152 by Bora Laskin Law Library user on 04 January 2021 TheinterviewswereconductedbetweenSeptember2016andFebruary2017and
International(Americas)Inc.,Burlington,MA,USA).
BackgroundInvitedInterviewed PurposivesampleMD 6 6 PT 9a 8 SnowballtechniqueMD 1 1 PT 5 5 DC 5 5 Non-healthcare1b 0 Total 2725
SamplingStrategiesandBackgroundofStudy Participants
from https://academic.oup.com/milmed/article/184/5-6/e344/5194152
by
Law Library user on 04 January 2021
Downloaded from https://academic.oup.com/milmed/article/184/5-6/e344/5194152
Table 1 Sampling Strategies and Background of Study Participants
Table 2 Participant Perceptions of Barriers to Integration of Chiropractic Services Within the Canadian Forces Health Services
Table 3 Participant Perceptions of Opportunities to Integrate Chiropractic Services Within the Canadian Forces Health Services
often did not include important patient outcomes that are considered necessary to assess the effectiveness of the care delivered.
Thebiggestprobleminthe[off-basehealthcareproviders’] reportswastheysaidnothing.Theywouldoftensay, “Member has benefitted from treatment, recommend more treatment.”Itwouldn’tsay,“Howhashebenefitted. Is it basedonhisOswestryscores?Isitbasedonhimtellingyou he feels better? Is it based on he can now lift 50 lbs. versus beforehecouldonlylift20?”Ididn’tknow,sotherewas neverenoughinformationandoftenwhenIwouldaskfor information,Iwouldn’treceiveit.(PT,K6)
Currently, off-base providers cannot access health information available in service members’ CFHS electronic health records. Therefore, off-base health care providers are dependent upon information provided within the referral process and discharge notes. Participants agreed that addressing the gaps in bidirectional communication would improve quality of care and strengthen interprofessional relations.
DuplicationofHealthcareServices:“Blurringscopesof practice”.
The third category addressed perceptions and experiences related to the duplication of health care services involving physiotherapists and chiropractors. Participants concurred that over the past decade, the changing scope of practice for both physiotherapists and chiropractors has significantly blurred their unique roles. This blurring of roles creates confusion among patients and health care providers, and a lack of clarity of the unique role each provider can play.
Overtheyears,backwhenI firststartedbeingaphysio, thereseemedtobeaverycleardelineationbetweenphysio andchiropractic.Butastheyearshaveprogressed,what wehaveseenisreallyaconversionofthetwopractices, wherephysiosaretaughtalotofmanipulativetherapyin schoolnowandwecontinuethatwithpostgradstudies. Andchiropractorstendtodoalotmorenon-manipulative typeoftreatment,whetheritbeactivereleasetherapy oracupunctureormoreexercisebasedtherapy.So, the difference that we used to see between the two professionalsisnowalotmoreblurred,andthereisalot moreshadesofgreythanthiscleardelineationbetweenthe two.(PT,K25)
Consequently, participants highlighted perceptions of duplication and/or redundancy of services as a major barrier to the integration of chiropractic services. Similar sentiment was expressed by a minority of North American orthopedic surgeons, suggesting manipulative care can be provided by physiotherapists and athletic therapists.28 If chiropractors and physiotherapists provided similar interventions, and
physiotherapists were already accessible within the CFHS, sentiment was expressed that there was currently no need to provide access to chiropractors, regardless of their inclusion in the CFHS spectrum of care.
So,questionsthatmayneedtobeanswerediswhattype ofconditionswouldbereferredtoachiropractorversus aphysiotherapistandlookattheissueofredundancyof treatment…arethereactuallyanyadditionalskillsets whicharenotcurrentlyavailablewithinourpractice.(PT, K3)
Let’sjustbeclearonwhatitisthey[chiropractors] aregoingtobedoingbecauseotherwisethereisthat perceptionofredundancy.Thephysiosaretellingme, “Well,whynotjusttrainmorephysiosinmanualtherapy,” becausethoseareexpensivecoursesandbecausewe expectourphysiostobedeployableandgotowhereverthe countryasksthemtogowhichwouldn’tbethecaseforthe chiropractorsthatweemploy.(MD,K11)
The preceding quote from a physician illuminates another potential barrier associated with deployment. Concerns related to deployment were raised by participants along with notions of encouraging patient dependency (i.e., perceived reliance on the health care provider and ongoing care). This barrier was particularly pertinent when considering that some contracted services, including chiropractic care, would not be available during military exercises and deployment.
Opportunities to Integrate Chiropractic Services in the CFHS MusculoskeletalDisorders:“It’sasignificant issue for us”
The first category of opportunities underscored the significance of MSK conditions currently within the CAF.
Itisabiginterestatthenationallevelrightnowtoexplore theprevalenceandthepossiblereasonswhyaproportionof thepatientsarereferredback.Thereisgreatpotential,now morethanever,tolookatthepresentsystemofcarefor lowbackpainandmakereal,costeffective,andconcrete changestohowwedeliverthiscare.(PT,K18)
The perspectives shared by participants support the reported high prevalence of MSK conditions in the CAF. Participants noted the significance to service members and how MSK conditions negatively affect the health and well-being of active duty service members, in addition to being a prevalent source of CAF medical releases. These concerns are consistent with the CAF report that 43% of regular force medical releases were attributed to MSK conditions.4
Inter-professionalCollaborativeCare:“Seethepatientfrom differentperspectives”
CMCC Research Report 2018–2020 108
The second category provided insights into opportunities to integrating chiropractic services on-base. The notion of interprofessional collaborative care was considered important by the majority of participants. Participants thoughtfully reflected that collaborative care delivered in a team-based approach provided an opportunity for multiple providers to contribute to patient care through their unique professional “lens.” Hence, viewed from this perspective, different professions could be considered not only for the interventions they provide but also by their approach to clinical care.29
So,thebeautyofcollaborativecareisthatyoucanhopefully seethepatientfromvariousdifferentperspectives…a morecompletepicture,thanifjustonepersonseesthem, throughthelensofwhattheytendtodo.(MD,K11)
Participants shared their perspectives and experiences with various aspects of care delivery, particularly when involving chiropractors. The richness of the data and diverse experiences of the participants provided divergent perspectives of strategies used to manage back pain. This partly reflects base-to-base variations, including location, size, resources and primary purpose. This is highlighted as follows:
Nowin[base]Iusedthem[chiropractors]alotbecause we didn’t have a lot of resources. We didn’t have a lot of physiotherapists,alotofexperiencedphysiotherapists.I foundthechiropracticverysimilartowhatIdo,veryactive, notmodalitybased.So,Itrustedthem,Itrustedtheir clinicaljudgment,andsoIusedthemforthatandIused themformanipulation.So,Ithinkitdependsonthebase andtheresourcesavailableatthebase,ifthathelps”.(PT, K22)
Although considered a challenge, such variation also provides opportunities to implement chiropractic services and compare health care programs on a national level. For example, a recent U.S. study reported significant improvements in pain, function, and satisfaction with care in the group of active duty military receiving chiropractic care and standard medical care compared to standard medical care alone.11,12
Evidence-basedApproach:“Veryimportant”
The third category of opportunities underscored participants’ emphasis on service providers using an evidence-based approach in determining which interventions should be included within a program of care. Without exception, participants advocated for the use of evidence-based interventions, including use of evidenced-based clinical practice guidelines. A participant stated: “Obviously, evidence-based medicine is very important and there is a whole host of different I suppose guidelines as such in regards to how you approach back pain…” (MD, K14)
However, some participants could not differentiate between evidence for an intervention (e.g., manipulation) and the profession delivering the intervention.
Iwouldsaythereisaspecific need for evidence-based managementofmusculoskeletalconditions…Becausethat iswhattheSurgeonGeneralexpects….thereisnothingthat chirooffersthatisbothuniqueandevidence-based,sofor meitisaboutprovidingaccesstoevidence-basedcarefor MSKissues.(PT,K6)
TheSpectrumofCare:“Chiropracticcare,wethinkprimarily spine”
The fourth category addressed participants’ knowledge and experiences pertaining to the “spectrum of care” in the CAF and the tendency to equate chiropractic care with spine care. There was consistency among most participants that access to services within the spectrum of care is for a specific intervention, rather than for the profession’s full scope of practice. Similar to other studies, consideration for referral for chiropractic services was made primarily for spinal manipulation to treat a spinal disorder, most commonly chronic low back pain.
So,Ithinkwhatwerecognizechiropractorsforthemostare theirskillsetsinspinalmanipulation.(PT,K13)
Participants’ perspectives of conditions managed by chiropractors are similar to that provided in a pilot study conducted with on-base chiropractors. In this study, almost 97% of military personnel were referred for spine-related conditions, of which almost 52% involved the low back.8 A minority of participants, particularly physicians who had established both personal and professional relationships with a chiropractor, considered also accessing chiropractors for their expert clinical opinion.
“Whoultimatelyisthespinecarespecialist?”,becausewe lumpallkindsofpeopleinthatdomain.Ithinkgiventhe natureofthespecialty,andhowmuchtimechiropractors spendonthespine,Iwouldhavetoagreethat… chiropractors,…comeclosesttoaspinecarespecialist.(MD, K11)
Ithinkthatingeneralwhenwethinkofchiropracticcare, wethinkofprimarilyspine,spinal,trunkandsortofmid thoracictrunkproblems,andwetendtothinklessofthem forextremitytypesofMSKcomplaints.(MD,K12)
The majority of participants called for a delivery approach involving chiropractors within an integrated team and founded on a patient-centered spine care model. In this model, providers are respected and distinguished for their uniqueness but the care is provided together with others and not in isolation. Hence,
A selection of published research by CMCC faculty 109 Mior et al
providers do not become the intervention, but rather health care professionals providing assessment and treatment, while respecting their scopes of practices and expertise.
Discussion
Currently, CAF members have access to chiropractic services within the spectrum of care and at the discretion of the referring CFHS providers. Within this context, our study results inform processes that could address existing challenges to effective referrals and improve quality of care. CFHS team members’ lack of clarity about a chiropractor’s clinical skills and knowledge was a major challenge emerging from our data. Thus, one recommendation emanating from key informants’ comments would be establishing personal relationships (i.e., one-on-one professional contacts with chiropractors), rather than adopting a broader profession-based approach, with the goal of enhancing understandings regarding the knowledge-base and skill set of chiropractors.
This call for a more personal or idiosyncratic approach, as opposed to relying solely on objective data, was often used to inform referral practices. In this study, key informants’ experiences influenced opinions about the value and role of the chiropractor in managing specific MSK conditions. The reliance on personal relationships for referral is consistent with previous research suggesting that despite positive views of chiropractor’s providing helpful care for MSK conditions, the diversity within the profession limits referrals and creates barriers to interprofessional collaboration.28
In our study, the majority of participants appeared to view chiropractors more as a therapy, specifically manipulation, rather than as a profession providing comprehensive management and multiple treatment approaches. This perspective potentially limited access and timeliness of referrals for care. A minority of participants, based on personal experience, did appreciate the chiropractor’s assessment and therapeutic skills. These differing views of the role of the chiropractor in health care are consistent with a report by Herman and Coulter29, highlighting how health policies that define complementary and alternative professions as individual therapies rather than as a profession with a wider scope of practice, impacts patient access and care. A second recommendation emerging from this study is to explicate the role and responsibilities of the chiropractor in a collaborative CFHS environment based upon their professional scope of practice.
Our findings also suggest that the bi-directional communication between CFHS health care providers and chiropractors varies between bases but in general is considered “suboptimal.” Rather than a standardized format for written and verbal reports, report formats appeared to be individually developed and base-specific. Negative experiences (e.g., inappropriate communication, non-evidenced based clinical management,
ignorance of military culture) may create professional tensions and biases that are then generalized beyond one-on-one encounters. Such experiences have been reported in other studies examining the integration of chiropractors within the US military30 and Canadian primary care.31 A third recommendation is to standardize and enhance the level of interprofessional communication to further continuity of patient care and improve quality care. In addition, educating non-military personnel about the uniqueness of the military culture would encourage the development and implementation of appropriate treatment plans.
Another barrier to integration of chiropractic services is the perceived certainty of duplication of services, based upon the “blurring of scopes of practice” between PTs and chiropractors. Perceived duplication and redundant services were previously reported as barriers for inclusion of chiropractors in health care teams (e.g., in sports medicine32,33). Others attribute such barriers to social constructs related to professionalization34 and the marginalization of professions,35 which impact boundary disputes and negatively influence collaboration.
Fostering collaborative relationships between chiropractors and CFHS health care providers, within a patient-centered model of care, will assist in addressing these barriers.
Limitations
Our study sample consisted of military personnel, public servants and contractors of the Canadian Department of National Defense and civilians. Participants were from different CAF bases, health care services, and geographic regions across Canada. Military personnel were of different ranks and military experience. Nonetheless, individuals who were not invited to participate may have expressed different views. We also did not explore patients’ perspectives of care delivered within the CFHS nor their experiences when requesting or being referred for chiropractic services. Such experiences can significantly impact the inclusion of a health profession within a health care team.33
Conclusions
This study provided the first qualitative analysis of barriers and opportunities related to the integration of chiropractic services within the current CFHS environment. Our findings and recommendations provide an opportunity to address the current challenges identified by key informants for the participation or integration of chiropractors within the unique health care delivery system of the CAF. Further, the findings provide important information to inform the potential design of an implementation study to assess the feasibility of integrating chiropractic services in the CFHS, while strengthening referral processes to chiropractors within the spectrum of care.
Supplementary Material
Supplementary material is available at Military Medicine online.
CMCC Research Report 2018–2020 110
Previous Presentations
Mior SA, Vogel E, Sutton D, French S, Côté P, Nordin M, Loisel P, Laporte A. Exploring Chiropractic Services in the Canadian Forces Health Services – Opportunities and Challenges. 8th Annual Military and Veteran Health Research Forum. Canadian Institute of Military and Veteran Research. Toronto, Ontario. September 25–27, 2017.
Funding
This study was funded by a grant from the Canadian Chiropractic Association and the Ontario Chiropractic Association. The funders did not have a role in study design, analysis, or preparation of this paper.
Acknowledgments
We thank the men and women of the Canadian Forces Health Services for their contributions to this paper.
References
1. Rowe P, Hébert LJ: The impact of musculoskeletal conditions on the Canadian Forces. In: Shaping the Future: Military and Veteran Health Research, pp 377–391. Edited by Aiken A, Bélanger S Kingston, Canadian Defense Academy Press, 2011.
2. Born J, Hawes R, Whitehead J: Results from Health and Lifestyle Information Survey of Canadian Forces personnel 2008/2009: Regular Force Version: Your Health Speaks Volumes. Ottawa, Government of Canada, 2010.
3. Canadian Forces Health Services Group: Surgeon General’s Report 2014: Consolidation, Innovation, Readiness. Ottawa, Government of Canada, Department of National Defence, 2014.
4. Directorate of Force Health Protection: Canadian Forces Health and Lifestyle Information Survey – 2008/2009. Ottawa, Department of National Defence, 2010.
5. Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA: Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician 2009; 12(4): E35–70.
6. Canada, Department of National Defence. Caring for Our Own: A comprehensive approach for the care of CF ill and injured members and their families. Ottawa, 2012.
7. Canada Parliament House of Commons: Caring for Canada’s Ill and Injured Military Personnel (June 2014) 41st Parliament, 2nd Session, pp 1–93. Edited by Standing Committee on National Defence Ottawa, Government of Canada, 2014.
8. Green BN, Johnson CD, Daniels CJ, Napuli JG, Gliedt JA, Paris DJ: Integration of chiropractic services in military and veteran health care facilities: a systematic review of the literature. J Evid Based Complementary Altern Med 2016; 21(2): 115–30.
9. Dunn AS, Green BN, Gilford S: An analysis of the integration of chiropractic services within the United States military and veterans’ health care systems. J Manipulative Physiol Ther 2009; 32(9): 749–57.
10. Green BN, Johnson CD, Lisi AJ: Chiropractic in U.S. military and veterans’ health care. Mil Med 2009; 174(6): vi–vii.
11. Goertz CM, Long CR, Hondras MA, et al: Adding chiropractic manipulative therapy to standard medical care for patients with acute low back pain: results of a pragmatic randomized comparative effectiveness study. Spine 2013; 38(8): 627–34.
12. Goertz CM, Long CR, Vining RD, Pohlman KA, Walter Jγ, Coulter I: Effect of usual medical care plus chiropractic care vs usual medical care alone on pain and disability among US service members with low back pain: A comparative effectiveness clinical trial. JAMA Netw Open 2018; 1(e180105): 1–15.
13. Boudreau LA, Busse JW, McBride G: Chiropractic services in the Canadian Armed Forces: a pilot project. Mil Med 2006; 171(6): 572–6.
14. Green BN, Johnson CD, Lisi AJ, Tucker J: Chiropractic practice in military and veterans health care: the state of the literature. J Can Chiropr Assoc 2009; 53(3): 194–204.
15. Canada Parliament House of Commons. Government Response to the Standing Committee’s Report on “Caring for Canada’s Ill and Injured Military Personnel”. Ottawa; 2014.
16. Robinson OC: Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol 2014; 11: 25–41.
17. Way D, Jones L, Busing N: Implementation Strategies: Collaboration in Primary Care-Family Doctors & Nurse Practitioners Delivering Shared Care. Toronto, The Ontario College of Family Physicians, 2000.
18. Goertz CM, Long CR, Vining RD, et al: Assessment of chiropractic treatment for active duty, U.S. military personnel with low back pain: study protocol for a randomized controlled trial. Trials 2016; 17: 70.
19. Dorflinger L, Moore B, Goulet J, et al: A partnered approach to opioid management, guideline concordant care and the stepped care model of pain management. J Gen Intern Med 2014; 29(Suppl 4): 870–6.
20. Pope C, Mays N: Qualitative Research in Health Care, 3rd ed., Hoboken: NJ, Blackwell, 2007.
21. Glaser B, Strauss A: The Discovery of Grounded Theory. Strategies for Qualitative Research. Chicago, IL, Aldine Publishing, 1967.
22. Strauss A, Corbin J: Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA, Sage, 1998.
23. Morgan DL: The Focus Group Guidebook. Thousand Oaks, SAGE Publications, 1998.
24. Verhoef MJ, Mulkins A, Boon H: Integrative health care: how can we determine whether patients benefit? J Altern Complement Med 2005; 11(Suppl 1): S57–65.
25. Morse JM, Field PA: Qualitative Research Methods for Health Professionals, 2nd ed., Thousand Oaks, SAGE Publications, 1995.
A selection of published research by CMCC faculty 111
Mior et al
26. Sandelowski M: Whatever happened to qualitative description? Res Nurs Health 2000; 23(4): 334–40.
27. Auditor General of Canada. Chapter 4-Military Health Care-National Defence in Report to the Auditor General Of Canada to the House of Commons, October, 2007. Ottawa: Office of the Auditor General of Canada. http://www.oagbvg.gc.ca/internet/English/parl_oag_200710_ 04_e_23828. html.
28. Busse JW, Jim J, Jacobs C, et al: Attitudes towards chiropractic: an analysis of written comments from a survey of North American orthopaedic surgeons. Chiropr Man Therap 2011; 19(1): 25.
29. Herman PM, Coulter ID: Complementary and Alternative Medicine: Professions of Modalities? Policy Implications for Coverage, Licensure, Scope of Practice, Institutional Privileges, and Research. California, RAND Corporation, 2015.
30. Lisi AJ, Khorsan R, Smith MM, Mittman BS: Variations in the implementation and characteristics of chiropractic services in VA. Med Care 2014; 52(12 Suppl 5): S97–104.
31. Mior S, Barnsley J, Boon H, Ashbury FD, Haig R: Designing a frame-work for the delivery of collaborative musculoskeletal care involving chiropractors and physicians in community-based primary care. J Interprof Care 2010; 24(6): 678–89.
32. Theberge N: “We have all the bases covered”. Constructions of professional boundaries in sport medicine. Int Rev Sociol Sport 2009; 44(2): 265–81.
33. Safai P: The demise of sport medicine and science council of Canada. Sport Hist Rev 2005; 36: 91–114.
34. Reeves S, Lewin S, Espin S, Zwarenstein M: Interprofessional Teamwork for Health and Social Care. Chichester, Wiley-Blackwell, 2010.
35. Saks M: Inequalities, margnality and the professions. Curr Sociol Rev 2015; 63(6): 850–68.
OriginallypublishedinMilitaryMedicine2019,2019May 1;184(5-6):e344-e351.
ReproducedwithpermissionfromOxfordUniversityPress.
AccessOnline: https://doi.org/10.1093/milmed/usy319
CMCC Research Report 2018–2020 112
System Dynamics to Investigate Opioid Use and Chiropractic Care for Chronic Musculoskeletal Pain
McGregor M1 , Nielsen A 2 , Chung C 1, Fillery MD2 , Wakeland W 2 , Mior S1 1CanadianMemorialChiropracticCollege, 2PortlandStateUniversity
Abstract
Objective:
The purpose of this investigation was to create a system dynamics (SD) model, including published data and required assumptions, as a tool for future research identifying the role of chiropractic care in the management of chronic, nonmalignant pain in a Canadian population.
Methods:
We present an illustrative case description of how we evaluated the feasibility of conducting a large-scale clinical trial to assess the impact of chiropractic care in mitigating excessive opioid use in Canada. We applied SD modeling using current evidence and key assumptions where such evidence was lacking. Modeling outcomes were highlighted to determine which potential factors were necessary to account for compelling study designs.
Results:
Results suggest that a future clinical study diverting patients with nonmalignant musculoskeletal pain early to the chiropractic stream of care could be most effective. System dynamics modeling also highlighted design challenges resulting from unresearched assumptions that needed to be proxied
for model completion. Assumptions included changing rates in opioid-associated deaths and rates of success in treatment management of addicted patients.
Conclusion:
In this case, SD modeling identified current research gaps and strong contenders for appropriate follow-up questions in a clinical research domain, namely the role of chiropractic care in the management of chronic, nonmalignant pain in a Canadian population.
OriginallypublishedintheJournalofJournalofManipulative andPhysiologicalTherapeutics2019May;42(4):237-246.Epub 2019 Jun 17.
ElsevieropenaccessarticlereproducedundertheCreative Commons CC-BY-NC-ND license.
AccessOnline:https://doi.org/10.1016/j.jmpt.2018.11.007
A selection of published research by CMCC faculty 113 Knowledge Translation and Health Policy
Examining the Effects of Low Back Pain and Mental Health Symptoms on Healthcare Utilisation and Costs: A Protocol for a Population-Based Cohort Study
Wong JJ1, 2 , Côté P1, 2, 3, 4 , C Tricco1, 3, 4 , Rosella LC1,5 1UniversityofToronto, 2CentreforDisabilityPreventionandRehabilitation,OntarioTechUniversityandCanadianMemorialChiropracticCollege, 3OntarioTechUniversity, 4LiKaShingKnowledgeInstituteofStMichael’sHospital, 5ICES
Abstract
Introduction:
Low back pain (LBP) is a leading cause of disability associated withigh healthcare utilisation and costs. Mental health symptoms are negative prognostic factors for LBP recovery; however, no population-based studies have assessed the joint effects of LBP and mental health symptoms on healthcare utilisation. This proposed study will characterise the health system burden of LBP and help identify priority groups to inform resource allocation and public health strategies. Among community-dwelling adult respondents of five cycles of the Canadian Community Health Survey (CCHS) in Ontario, we aim to assess the effect of self-reported LBP on healthcare utilisation and costs and assess whether this effect differs between those with and without self-reported mental health symptoms.
Methods and analysis:
We designed a dynamic population-based cohort study using linkages of survey and administrative data housed at ICES. The Ontario sample of CCHS (2003-2004, 2005-2006, 2007/2008, 2009/2010, 2011/2012; total of ~1 30 000 eligible respondents) will be used to define the cohort of adults with self-reported LBP with and without mental health symptoms. Healthcare utilisation and costs will be assessed by linking health administrative databases. Follow-up ranges from 6 to 15 years (until 31 March 2018). Sociodemographic (eg, age, sex,
education) and health behaviour (eg, comorbidities, physical activity) factors will be considered as potential confounders. Poisson and linear (log-transformed) regression models will be used to assess the association between LBP and healthcare utilisation and costs. We will assess effect modification with mental health symptoms on the additive and multiplicative scales and conduct sensitivity analyses to assess the impact of misclassification and residual confounding.
Ethics and dissemination:
This study is approved by the University of Toronto Research Ethics Board. We will disseminate findings using a multifaceted knowledge translation strategy, including scientific conference presentations, publications in peer-reviewed journals and workshops with key knowledge users.
OriginallypublishedinBMJOpen.2019Sep27;9(9):e031749.
Thisisanopenaccessarticlereproducedinaccordancewith CreativeCommonsAttributionNonCommercial(CCBY-NC4.0)
AccessOnline:https://bmjopen.bmj.com/content/9/9/e031749. long
CMCC Research Report 2018–2020 114
The Global Spine Care Initiative: World Spine Care Executive Summary on Reducing Spine-Related Disability in Low- and Middle-Income Communities
Abstract
Purpose:
Spinal disorders, including back and neck pain, are major causes of disability, economic hardship, and morbidity, especially in underserved communities and low- and middleincome countries. Currently, there is no model of care to address this issue. This paper provides an overview of the papers from the Global Spine Care Initiative (GSCI), which was convened to develop an evidence-based, practical, and sustainable, spinal healthcare model for communities around the world with various levels of resources.
Methods:
Leading spine clinicians and scientists around the world were invited to participate. The interprofessional, international team consisted of 68 members from 24 countries, representing most disciplines that study or care for patients with spinal symptoms, including family physicians, spine surgeons, rheumatologists, chiropractors, physical therapists, epidemiologists, research methodologists, and other stakeholders.
Results:
Literature reviews on the burden of spinal disorders and six categories of evidence-based interventions for spinal disorders (assessment, public health, psychosocial, noninvasive, invasive, and the management of osteoporosis) were completed.
In addition, participants developed a stratification system for surgical intervention, a classification system for spinal disorders, an evidence-based care pathway, and lists of resources and recommendations to implement the GSCI model of care.
Conclusion:
The GSCI proposes an evidence-based model that is consistent with recent calls for action to reduce the global burden of spinal disorders. The model requires testing to determine feasibility. If it proves to be implementable, this model holds great promise to reduce the tremendous global burden of spinal disorders. These slides can be retrieved under Electronic Supplementary Material.
OriginallypublishedinEuropreanSpineJournal,2018 Sep;27(Suppl6):776-785.Epub2018Aug27
ReproducedwithpermissionfromSpringerNature.
AccessOnline:https://doi.org/10.1007/s00586-018-5722-x
A selection of published research by CMCC faculty 115
Haldeman S1, 2 , Nordin M 3,4 , Chou R5 , Côté P6,7,8 , Hurwitz EL9, Johnson CD10, 11, Randhawa K 6,7 et al. 1UniversityofCalifornia, 2WorldSpineCare,SantaAna, 3NewYorkUniversity, 4WorldSpineCare,Europe, 5OregonHealthandScienceUniversity, 6UniversityofOntarioInstituteofTechnology, 7UOIT-CMCCCentreforDisabilityPreventionandRehabilitation, 8CanadianMemorialChiropractic College, 9UniversityofHawai’i,Manoa, 10NationalUniversityofHealthSciences, 11Qualcomm Health Center, Stanford Health
Reliability and Validity of Clinical Tests to Assess Posture, Pain Location, and Cervical Spine Mobility in Adults with Neck Pain and its Associated Disorders: Part 4. A Systematic Review from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration
1InstitutFranco-EuropéendeChiropraxie,
Abstract
Purpose:
To determinue the reliability and validity of clinical tests to assess posture, pain location, and cervical spine mobility in adults with grades I-IV neck pain and associated disorders (NAD).
Methods:
We systematically searched electronic databases to update the systematic review of the Bone and Joint Decade 20002010 Task Force on Neck Pain and Its Associated Disorders. Eligible reliability and validity studies were critically appraised using modified versions of the QAREL and QUADAS-2 instruments, respectively. Evidence from low risk of bias studies were synthesized following best evidence synthesis principles.
Results:
We screened 14302 articles, critically appraised 46 studies, and found 32 low risk of bias articles (14 reliability and 18 validity studies). We found preliminary evidence of:
1) reliability of visual inspection, aided with devices (CROM and digital caliper) to assess head posture;
2) reliability and validity of soft tissue palpation to locate tender/ trigger points in muscles; 3) reliability and validity of joint motion palpation to assess stiffness and pain provocation in combination; and 4) range of motion tests using visual estimation (in cervical extension only) or devices (digital caliper, goniometer, inclinometer) to assess cervical mobility.
Conclusions:
We found little evidence to support the reliability and validity of clinical tests to assess head posture, pain location and cervical mobility in adults with NAD grades I-III. More advanced validity studies are needed to inform the clinical utility of tests used to evaluate patients with NAD.
OriginallypublishedinMusculoskeletalScienceandPractice 2018Dec;38:128-147.Epub2018Oct5.
ReproducedwithpermissionfromElsevier.
AccessOnline:https://doi.org/10.1016/j.msksp.2018.09.013
CMCC Research Report 2018–2020 116
Lemeunier N1,2 , Jeoun EB 3 , M Suri 3 , T Tuff 3 , Shearer H3 , Mior S2,3 , Wong JJ2,3 , da Silva-Oolup S 3 , Torres P4 , D'Silva C 2 , Stern P 2,3 , Yu H2,5 , Millan M6 , Sutton D2,5 , Murnaghan K3 , Côté P 2,3,5
2UOIT-CMCCCentrefortheStudyofDisabilityPreventionandRehabilitation,UniversityofOntarioInstitute ofTechnology, 3CanadianMemorialChiropracticCollege, 4SantiagoSpineGroup, 5UniversityofOntarioInstituteofTechnology, 6Cabinetd'expertise médicale
Brain Drain: Psychosocial Factors Influence Recovery Following Mild Traumatic Brain Injury - 3 Recommendations for Clinicians Assessing Psychosocial Factors
Cancelliere C 1,2 , Mohammed RJ 3 1OntarioTechUniversity, 2CentreforDisabilityPreventionandRehabilitationatOntarioTechUniversityandtheCanadianMemorialChiropractic College, 3CanadianMemorialChiropracticCollege
Abstract
Mild traumatic brain injury is a major global public health concern. While most people recover within days to months, 1 in 5 people with mild traumatic brain injury report persistent, disabling symptoms that interfere with participation in work, school, and sport. People with injuries to regions other than the head may report similar symptoms. The biopsychosocial model of health explains this phenomenon in terms of factors associated with recovery that are not biomedical. Important psychosocial factors include poor recovery expectations and pretraumatic and posttraumatic psychological symptoms. Recent clinical practice guidelines recommend that clinicians examine all relevant biopsychosocial factors that may contribute to persistent postconcussive symptoms and consider them when helping their patients make health-management decisions.
However, because clinical training continues to prioritize biomedical symptoms, clinicians may not feel confident in the psychosocial domain. Our objective is to provide 3 recommendations for clinicians to assess psychosocial factors in patients after concussion, and to argue a case for clinicians to improve their skills in assessing psychosocial factors.
OriginallypublishedintheJournalofOrthopaedicSports& PhysicalTherapy2019Nov;49(11):842-844.Epub2019Jun1.
Reproducedwithpermission.
AccessOnline:https://www.jospt.org/doi/10.2519/ jospt.2019.8849
A selection of published research by CMCC faculty 117
Relationship Between Early Prescription Dispensing Patterns and Work Disability in a Cohort of Low Back Pain Workers' Compensation Claimants: A Historical Cohort Study
and Health,
Abstract
Objectives:
To examine and compare whether dispensing of prescription opioids, non-steroidal anti-inflammatory drugs (NSAIDs) and skeletal muscle relaxants (SMRs) within 8 weeks after a workrelated low back pain (LBP) injury is associated with work disability.
Methods:
A historical cohort study of 55 571 workers' compensation claimants with LBP claims in British Columbia from 1998 to 2009 was conducted using linked compensation, dispensing and healthcare data. Four exposures were constructed to estimate the effect on receipt of benefits and days on benefits 1 year after injury: drug class(es) dispensed, days' supply, strength of opioids dispensed and average daily morphine-equivalent dose.
Results:
Compared with claimants receiving NSAIDs and/or SMRs, the incidence rate ratio (IRR) of days on benefits was 1.09 (95% CI 1.04 to 1.14) for claimants dispensed opioids only and 1.26 (95% CI 1.22 to 1.30) for claimants dispensed opioids with NSAIDs and/or SMRs. Compared with weak opioids only, the IRR for claimants dispensed strong opioids only or strong and weak opioids combined was 1.21 (95% CI 1.12 to 1.30) and 1.29
(95% CI 1.20 to 1.39), respectively. The incident rate of days on benefits associated with each 7-day increase in days supplied of opioids, NSAIDs and SMRs was 10%, 4% and 3%, respectively. Similar results were seen for receipt of benefits, though effect sizes were larger.
Conclusions:
Findings suggest provision of early opioids leads to prolonged work disability compared with NSAIDs and SMRs, though longer supplies of all drug classes are also associated with work disability. Residual confounding likely partially explains the findings. Research is needed that accounts for prescriber, system and workplace factors.
OriginallypublishedinOccupationalandEnvironmental Medicine,2019Aug;76(8):573-581.Epub2019May15.
OpenaccessarticlereproducedinaccordancewiththeCreative CommonsAttributionNonCommercial(CCBY-NC4.0).
AccessOnline:https://doi.org/10.1136/oemed-2018-105626
CMCC Research Report 2018–2020 118
Carnide N1, Hogg-Johnson S1,2 , Koehoorn M1,3 , Furlan AD1,4 , Côté P 2,5 1Institute for Work
2CanadianMemorialChiropracticCollege, 3UniversityofBritishColumbia, 4TorontoRehabilitationInstitute,University Health Network, 5UniversityofOntarioInstituteofTechnology
Non-Pharmacological Management of Persistent Headaches Associated with Neck Pain: A Clinical Practice Guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration
Côté P1, 2, 3 , Yu H2, 4 , Shearer HM2, 5 , Randhawa K 2, 4 , Wong JJ2, 4 , Mior S2, 3, 4 , Ameis A 3 , et al.
1CanadaResearchChairinDisabilityPreventionandRehabilitation,Universityof OntarioInstituteofTechnology(UOIT), 2UOIT-CMCC Centre for theStudyofDisabilityPreventionandRehabilitation,CanadianMemorialChiropracticCollege(CMCC),Universityof OntarioInstituteofTechnology (UOIT), 3Universityof OntarioInstituteofTechnology(UOIT), 4CanadianMemorialChiropracticCollege
Abstract
Objectives:
To develop an evidence-based guideline for the nonpharmacological management of persistent headaches associated with neck pain (i.e., tension-type or cervicogenic).
Methods:
This guideline is based on systematic reviews of highquality studies. A multidisciplinary expert panel considered the evidence of clinical benefits, costeffectiveness, societal and ethical values, and patient experiences when formulating recommendations. Target audience includes clinicians; target population is adults with persistent headaches associated with neck pain.
Results:
When managing patients with headaches associated with neck pain clinicians should (a) rule out major structural or other pathologies, or migraine as the cause of headaches; (b) classify headaches associated with neck pain as tensiontype headache or cervicogenic headache once other sources of headache pathology has been ruled out; (c) provide care in partnership with the patient and involve the patient in care planning and decision making; (d) provide care in addition to structured patient education; (e) consider low-load endurance craniocervical and cervicoscapular exercises for tension-type headaches (episodic or chronic) or cervicogenic headaches >3 months duration; (f) consider general exercise, multimodal care (spinal mobilization, craniocervical exercise and postural correction) or clinical massage for chronic tension-type headaches; (g) do not offer manipulation of the cervical spine as the sole form of treatment for episodic or
chronic tension-type headaches; (h) consider manual therapy (manipulation with or without mobilization) to the cervical and thoracic spine for cervicogenic headaches >3 months duration. However, there is no added benefit in combining spinal manipulation, spinal mobilization and exercises; and (i) reassess the patient at every visit to assess outcomes and determine whether a referral is indicated.
Conclusions:
Our evidence-based guideline provides recommendations for the conservative management of persistent headaches associated with neck pain. The impact of guideline in clinical practice requires validation.
Significance:
Neck pain and headaches are very common comorbidities in the population. Tension-type and cervicogenic headaches can be treated effectively with specific exercises. Manual therapy can be considered as an adjunct therapy to exercise to treat patients with cervicogenic headaches. The management of tension-type and cervicogenic headaches should be patient-centred.
OriginallypublishedintheEuropeanJournalofPain2019 Jul;23(6):1051-1070.Epub2019Feb28.
ReproducedwithpermissionfromJohnWiley&Sons.
AccessOnline:https://doi.org/10.1002/ejp.1374
A selection of published research by CMCC faculty 119
Manipulation and Mobilization for Treating Chronic Nonspecific Neck Pain: A Systematic Review and MetaAnalysis for an Appropriateness Panel
Abstract
Background:
Mobilization and manipulation therapies are widely used by patients with chronic nonspecific neck pain; however, questions remain around efficacy, dosing, and safety, as well as how these approaches compare to other therapies.
Objectives:
Based on published trials, to determine the efficacy, effectiveness, and safety of various mobilization and manipulation therapies for treatment of chronic nonspecific neck pain.
Study design:
A systematic literature review and meta-analysis.
Methods:
We identified studies published between January 2000 and September 2017, by searching multiple electronic databases, examining reference lists, and communicating with experts. We selected randomized controlled trials comparing manipulation and/or mobilization therapies to sham, no treatment, each other, and other active therapies, or when combined as multimodal therapeutic approaches. We assessed risk of bias by using the Scottish Intercollegiate Guidelines Network criteria. When possible, we pooled data using random-effects meta-analysis. Grading of Recommendations, Assessment, Development, and Evaluation was applied to determine the confidence in effect estimates. This project was funded by the National Center for Complementary and Integrative Health under award number U19AT007912 and ultimately used to inform an appropriateness panel.
Results:
A total of 47 randomized trials (47 unique trials in 53 publications) were included in the systematic review. These studies were rated as having low risk of bias and included a total of 4,460 patients with nonspecific chronic neck pain who were being treated by a practitioner using various types of manipulation and/or mobilization interventions. A total of 37 trials were categorized as unimodal approaches and involved thrust or nonthrust compared with sham, no treatment, or other active comparators. Of these, only 6 trials with similar intervention styles, comparators, and outcome measures/
timepoints were pooled for meta-analysis at 1, 3, and 6 months, showing a small effect in favor of thrust plus exercise compared to an exercise regimen alone for a reduction in pain and disability. Multimodal approaches appeared to be effective at reducing pain and improving function from the 10 studies evaluated. Health-related quality of life was seldom reported. Some 22/47 studies did not report or mention adverse events. Of the 25 that did, either no or minor events occurred.
Limitations:
The current evidence is heterogeneous, and sample sizes are generally small.
Conclusions:
Studies published since January 2000 provide low-moderate quality evidence that various types of manipulation and/ or mobilization will reduce pain and improve function for chronic nonspecific neck pain compared to other interventions. It appears that multimodal approaches, in which multiple treatment approaches are integrated, might have the greatest potential impact. The studies comparing to no treatment or sham were mostly testing the effect of a single dose, which may or may not be helpful to inform practice. According to the published trials reviewed, manipulation and mobilization appear safe. However, given the low rate of serious adverse events, other types of studies with much larger sample sizes would be required to fully describe the safety of manipulation and/ or mobilization for nonspecific chronic neck pain.
OriginallypublishedinPainPhysician.PainPhysician.2019 March;22(2):E55–E70.
ReproducedwithpermissionfromtheAmericanSocietyof InterventionalPainandPainPhysicianJournal.
AccessOnline:https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6800035/
CMCC Research Report 2018–2020 120
Coulter ID1,2,3 , Crawford C1, Vernon H1,4 , Hurwitz EL1,5 , Khorsan R 3,6 , Suttorp Booth M1, Herman PM1 1RANDCorporation, 2UniversityofCaliforniaLosAngeles, 3SouthernCaliforniaUniversityofHealthSciences, 4CanadianMemorialChiropractic College, 5UniversityofHawaii,Manoa, 6YoSanUniversityofTraditionalChineseMedicine,LosAngeles,CA. 6RANDCorporation,SantaMonica,CA.
Understanding Patient Profiles and Characteristics of Current Chiropractic Practice: A Cross-Sectional Ontario Chiropractic Observation and Analysis STudy (O-COAST)
Abstract
Objectives:
There is no current detailed profile of people seeking chiropractic care in Canada. We describe the profiles of chiropractors' practice and the reasons, nature of the care provided to their patients and extent of interprofessional collaborations in Ontario, Canada.
Design:
Cross-sectional observational study.
Setting:
Primary care setting in Ontario, Canada.
Participants:
We randomly recruited chiropractors from a list of registered chiropractors (n=3978) in active practice in 2015. Of the 135 randomly selected chiropractors, 120 were eligible, 43 participated and 42 completed the study.
Outcome measures:
Each chiropractor recorded information for up to 100 consecutive patient encounters, documenting patient health profiles, reasons for encounter, diagnoses and care provided. Descriptive statistics summarised chiropractor, patient and encounter characteristics, with analyses accounting for clustering and design effects.
Results:
Chiropractors provided data on 3523 chiropractorpatient encounters. More than 65% of participating chiropractors were male, mean age 44 years and had practised on average 15 years. The typical patient was female (59% of encounters),
between 45 and 64 years (43%) and retired (21%) or employed in business and administration (13%). Most (39.4%) referrals were from other patients, with 6.8% from physicians. Approximately 68% of patients paid out of pocket or claimed extended health insurance for care. Most common diagnoses were back (49%, 95% CI 44 to 56) and neck (15%, 95% CI 13 to 18) problems, with few encounters related to maintenance/preventive care (0.86%, 95% CI 0.2 to 3.9) and non-musculoskeletal problems (1.3%, 95% CI 0.7 to 2.3). The most common treatments included spinal manipulation (72%), soft tissue therapy (70%) and mobilisation (35%).
Conclusions:
This is the most comprehensive profile to date of chiropractic practice in Canada. People who present to Ontario chiropractors are mostly adults with a musculoskeletal condition. Our results can be used by stakeholders to make informed decisions about workforce development, education and healthcare policy related to chiropractic care.
OriginallypublishedinBMJOpen.2019Aug26;9(8):e029851.
OpenaccessarticlereproducedunderthetermsoftheCreative CommonsAttributionNonCommercial(CCBY-NC4.0).
AccessOnline:https://doi.org/10.1136/bmjopen-2019-029851
A selection of published research by CMCC faculty 121
Mior S1, 2 , Wong JJ2 , Sutton D2 , Beliveau PJH 3 , Bussières A 4,5 , Hogg-Johnson S1,2 , French S 3,6,7 1Canadian MemorialChiropracticCollege, 2 UOIT-CMCCentreforDisabilityPreventionandRehabilitation, OntarioTechUniversityandCanadian MemorialChiropracticCollege, 3Queen'sUniversity, 4McGillUniversityHealthCentre, 5 Université du Québec à Trois-Rivières, 6Institute for Work & Health, 7MacquarieUniversity
Opioid Overdose Hospitalization Trajectories in States with and without Opioid-Dosing Guidelines
SearsJM1,2,3 , Fulton-Kehoe D1, Schulman BA1, Hogg-Johnson S 3,4,5 , and Franklin GM1,6 1UniversityofWashington, 2HarborviewInjuryPreventionandResearchCenter, 3Institute for Work and Health, 4CanadianMemorialChiropractic College, 5DallaLanaSchoolofPublicHealth,UniversityofToronto, 6WashingtonState
Abstract
Objectives:
High-risk opioid-prescribing practices contribute to a national epidemic of opioid-related morbidity and mortality. The objective of this study was to determine whether the adoption of statelevel opioid-prescribing guidelines that specify a high-dose threshold is associated with trends in rates of opioid overdose hospitalizations, for prescription opioids, for heroin, and for all opioids.
Methods:
We identified 3 guideline states (Colorado, Utah, Washington) and 5 comparator states (Arizona, California, Michigan, New Jersey, South Carolina). We used state-level opioid overdose hospitalization data from 2001-2014 for these 8 states. Data were based on the State Inpatient Databases and provided by the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality, via HCUPnet. We used negative binomial panel regression to model trends in annual rates of opioid overdose hospitalizations. We used a multiplebaseline difference-in-differences study design to compare postguideline trends with concurrent trends for comparator states.
Results:
For each guideline state, postguideline trends in rates of prescription opioid and all opioid overdose hospitalizations
decreased compared with trends in the comparator states. The mean annual relative percentage decrease ranged from 3.2%-7.5% for trends in rates of prescription opioid overdose hospitalizations and from 5.4%-8.5% for trends in rates of all opioid overdose hospitalizations.
Conclusions:
These findings provide preliminary evidence that opioid-dosing guidelines may be an effective strategy for combating this public health crisis. Further research is needed to identify the individual effects of opioid-related interventions that occurred during the study period.
OriginallypublishedinPublicHealthReports,2019Sep-Oct; 134(5):567–576.Publishedonline2019Jul31.
ReproducedwithpermissionfromSagePublishing.
AccessOnline:https://doi.org/10.1177/0033354919864362
CMCC Research Report 2018–2020 122
Faculty Presentations: 2018-19 Academic Year
Kopansky-Giles D, Beavers L. Cultivating collaborative teams using an interprofessional collaboration competency framework in performance appraisals. 18 Jun 20; Toronto, ON: Interprofessional Collaboration Showcase 2018.
Peranson J, Kopansky-Giles D, Waters I. Recognizing our Hidden Faculty: Integrating and Supporting the Role of Health Professional Educators in Family Medicine. 18 Aug 25; Basel, Switzerland: Association for Medical Education in Europe (AMEE) 4th International Conference.
Newton C, Kopansky-Giles D. Teaching and assessing collaborative practice competencies in family medicine residency and health professional training program. 18 Aug 25; Basel, Switzerland: Association for Medical Education in Europe (AMEE) 4th International Conference. (workshop)
Fillery M, Mior SA, Gamble B. Retaining a health workforce with the potential to aid musculoskeletal pain in Canada’s most populous province: A longitudinal study of chiropractors. 18 Oct 3; Gatineau, QC: Canadian Health Workforce Conference. (poster)
Brodie L, Côté P, Meckamalil C, Hogg-Johnson S, Smith K, Jacobs C, Carroll L. The association between musculoskeletal pain and psychological stress, CMCC mental health and wellness study. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Côté D, Smith K, Côté P. The association between substance use and psychological distress in students enrolled at CMCC. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Eilayyan O, Thomas A, Ahmed S, Tibbles A, Jacobs C, Alzoubi F, Bussières A. Promoting the use of a self-management strategy among novice chiropractors treating individuals with spine pain. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Hammerich K, Stuber K, Abbas A, Harris M, Hogg-Johnson S, Lauridsen HH, Lemeunier N, Maiers M, Mior SA. Assessing attitudes of patient-centered care among students across chiropractic colleges. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Kopansky-Giles D, Beavers L, Dewhurst N, Whelan L, Leung FH, Skiffington A, McNeil B. Cultivating collaborative teams using an interprofessional collaboration competency framework
in performance appraisals. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Lemeunier N, Yu H, Côté P. How to teach diagnostic tests when there is not enough evidence on their utility? 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Meckamalil C, Côté P, Brodie L, Hogg-Johnson S, Smith K, Jacobs C, Carroll L. The prevalence of anxiety, stress and depressive symptomology in chiropractic undergraduate students at the Canadian Memorial Chiropractic College. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Osterbauer PJ, Lester S, Starmer DJ. Four month skill retention using force sensing feedback after simulated, prone, thoracic adjustments. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Sovak G, Wickes D. Virtual microscopy for the study of histology in a chiropractic program: is it the future? 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Suri M, Kopansky-Giles D, White K, Jeffs L, Mior SA. Evaluating the integration of interprofessional collaborative competencies within team-based simulation training: a randomized trial. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Verville L, Côté P, Grondin D, Mior SA, Moodley K, Kay R, Taylor-Vaisey A. Are technology-based educational interventions effective in improving knowledge about clinical practice guidelines? A systematic review of the literature. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Verville L, Côté P, Grondin D, Mior SA, Kay R. The development and evaluation of a technology-based learning tool to improve knowledge about the evidence-based management of neck pain by teaching faculty at a Canadian Chiropractic College. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Wickes D. Evidence mapping of lecture capture research in chiropractic programs: a preliminary analysis. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
A selection of published research by CMCC faculty 123
Wingrove J, Ridding A, Tibbles A. Development of an educational app for clinic observation. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference.
Bradaric-Baus C, Dunham S. Operationalizing a strategic plan – where do we start? 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (poster)
Budgell B. Constructing and analyzing a spoken corpus of the chiropractic curriculum. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (poster)
Coulter ID, Crawford C, Vernon H, Hurwitz E, Whitley M, Herman P, Aliyev G. Manipulation and mobilization for treating chronic neck pain: a systematic review and meta-analysis. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (poster)
Dunham S, Bradaric-Baus C. Development of graduate exit competencies at the Canadian Memorial Chiropractic College. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (poster)
Kinsinger S. What do professionals profess? Teaching the principles of professionalism. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (poster)
Azad A, Howard L. Towards a model of business education for chiropractic. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (workshop)
Budgell B. Good biomedical writing: how to recognize it, how to produce it, how to teach it. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (workshop)
Gleberzon B, McCarthy P, Du Rose A. Toward the development of a standardized chiropractic curriculum for jurisprudence, ethics and business management course content. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (workshop)
Kinsinger S. Principles in setting doctor:patient boundaries. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (workshop)
Kopansky-Giles D, Newton C, Dunham S. Coaching for competence in collaborative practice: practical resources for the clinical preceptor. 18 Oct 24; London, UK: World Federation of Chiropractic Association of Chiropractic Colleges 10th Chiropractic Education Conference. (workshop)
Barbier-Cazorla F, Yu H, Côté P, Stern P, Côté D, Taylor-Vaisey A, D'Silva C, Lemeunier N. Reliability and validity of orthopaedic tests to assess low back pain patients: a systematic and critical review. 18 Mar 14; Baltimore, MD: ACC RAC 2019.
Gold P, Ellul N. TMJ trauma as a cause of lingual nerve impingement: A case report. 18 Mar 14; Baltimore, MD: ACC RAC 2019.
Green B, Johnson C, Haldeman S, Kane E, Clay M, Griffith E, Castellote J, Smuck M, Rajasekaran S, Hurwitz E, Nordin M, Randhawa K, Yu H. Recommendations for public health and prevention interventions for common spine disorders in low- and middle-income communities. 18 Mar 14; Baltimore, MD: ACC RAC 2019.
Lardon A, Yu H, Côté P, Taylor-Vaisey A, Lemeunier N. Reliability and validity of muscular endurance tests in low back pain population: a systematic review. 18 Mar 14; Baltimore, MD: ACC RAC 2019.
To D, Alexopulos S, Bartosik A, Starmer D. An evaluation of educational resources in an evidence-informed curriculum: a descriptive study. 18 Mar 14; Baltimore, MD: ACC RAC 2019.
Yu H, Mallard F, Côté P, Taylor-Vaisey A, Lemeunier N. Reliability and validity of neurological tests in low back pain population: a systematic review. 18 Mar 14; Baltimore, MD: ACC RAC 2019.
Yu H, Mohammed R, Côté P, Taylor-Vaisey A, Lemeunier N. Reliability and validity of self-reported disability questionnaires in low back pain population: A systematic review. 18 Mar 14; Baltimore, MD: ACC RAC 2019.
Kinsinger FS. What do Professionals Profess? Affirming the Principles of Professionalism. 18 Mar 14; Baltimore, MD: ACC RAC 2019. (poster)
Adeboyejo A, Jensen RK, Hogg-Johnson S, Hartvigsen J. The association between low back pain, self-perceived fatigue, and physical performance in community-dwelling Danish citizens over 75 years of age: A cross-sectional study. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Barbier G, Lemeunier N, Côté P, Houart G, Pigeon S, Audo Y, Lardon E, Lanlo O, Lardon A. Effect of High velocity, low amplitude spinal manipulation on Range of Motion: A systematic literature review. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ ECU Congress.
CMCC Research Report 2018–2020 124
Cancelliere C, Côté P, Nordin M, Connell G. Proposal for an evidence-based guideline on the rehabilaltion of disability in adults with spinal disorders: an interdisciplinary, multisectoral, and multi-society guideline. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Carpino G, Howarth SJ. Does manual therapy affect functional and biomechanical outcomes of a sit-to-stand test in a low back pain population? A secondary data analysis. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Esson SA, Åartun E, Mior SA, Weaver R, Côté P. The daily experience of patients with low back pain: a qualitative study. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Funabashi M. Quantification of lumbar vertebral motion during two different spinal manipulative techniques: a feasibility investigation. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Funabashi M. Force distribution within spinal tissues during a posterior to anterior spinal manipulative therapy. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Lemeunier N, Yu H, Salmi RL, Nordin M, Côté P. Diagnosing low back pain: how to assess patient with non-specific LBP? Evidencebased recommendations. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Mior SA. The daily experience of patients with lower back pain: A qualitative study. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Moser N, Mior SA, Noseworthy M, Côté P, Wells G, Behr M, Triano JJ. A Cross-over Randomized Trial of the Effect of Cervical Manipulation on Vertebral Artery and Cerebral Hemodynamics in Neck Pain Patients. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ ECU Congress.
Saugstrup M, Côté P, Hogg-Johnson S, Kongsted A, Hartvigsen J. Why do people with LBP choose to contact a chiropractor? A casecrossover study. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Stockendahl M, Rezai M, Torres P, Sutton D, Tuchin P, Brown R, Côté P. Chiropractic Health Resources: A Global Review. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Sorondo D, Delpierre C, Côté P, Salmi RL, Taylor-Vaisey A, Lemeunier N. A scoping review of literature on clinical practice guidelines use for the assessment and management of musculoskeletal disorders. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress.
Azad A, Weis CA. Attitudes Towards Chiropractic Care: A Crosssectional Survey of South Asians living in Ontario. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Batley S, Åartun E, Boyle E, Hartvigsen J, Stern P, Hestbaek L. The Association between Psychological and Social Factors and Spinal Pain in Adolescents. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ ECU Congress. (poster)
Corso M, Howitt S, Srbely J, Tran S, Liang C, Mior SA. The immediate effect of spinal manipulation on ball velocity and neuromuscular function during an instep kick in former varsity soccer players: a feasibility study. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
deGraauw C, Rutherford S, Howitt S. Exercise is a vital sign: Utilization in Canadian Chiropractic teaching clinics. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Fillery M, Mior SA¸ Gamble B. A longitudinal analysis of the chiropractic profession in Ontario: How the health workforce opened up to global markets from 1996-2007. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Germann D, El Bouse A, Shnier J, Abdelkader N, Kazemi M. Effects of Local Vibration Therapy on Various Performance Parameters: A Narrative Literature Review. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Kazemi M, Choi G, Millard M. The effects of spinal manipulative therapy on sports performance: A systematic review. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Lee A, deGraauw L, Belchos M, Muir B, Szabo K, Howitt S, deGraauw C. A Qualitative Study Investigating Research Directives for Sports-Focused Chiropractic Research: A Second Phase Study to Develop A Sports-Focused Research Agenda for Canadian Sports Chiropractors. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Lundgaard Saugstrup M, Côté P, Hogg-Johnson S, Kongsted A, Hartvigsen J. Why do people with LBP choose to contact a chiropractor? A case-crossover study. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Mior SA, Hogg Johnson S, Ammendolia C. The association between patient expectation and improved walking distance in patients receiving non-surgical care for lumbar spinal stenosis. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Olesen K, Kopansky-Giles D, Leung F-H, Peranson J, Vernon H Measuring and improving patient empowerment and enablement within an Ontario Academic Family Health Team: a quality improvement initiative. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ ECU Congress. (poster)
A selection of published research by CMCC faculty 125
Plener J, Choi G, Lester S, Starmer D. Determining the Feasibility of Using a Hand Held Load Cell as an Objective Measure of Extremity Manipulations. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Tavares P, Adeboyejo A. Overview of Conditions Seen on the CMCC Outreach Mission to the Dominican Republic 2017. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Wang S, Hogg-Johnson S. The Effects of Standing-Biased Desks on Student Pain, Engagement and Fatigue. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Weis CA, Stuber K, Wynd S. Update: Critical review on the use of chiropractic care during pregnancy and the reported iatrogenic injuries associated with the treatment of low back pain. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Weis CA, Russo A, Ellul N, Draper C. Assessing the knowledge, attitudes and perspectives of chiropractors towards chiropractic care for pregnant and postpartum patients following an educational intervention. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Johnson C, Kopansky-Giles D. The Global Spine Care Initiative: Delivering community-based, sustainable models of care. 19 Mar 20; Berlin, Germany: EPIC 2019 WFC/ECU Congress. (poster)
Antao V, Lazor J, Kopansky-Giles D. Realignment of an established faculty development program for new teachers: A systematic approach. 19 Apr 29; Toronto, ON: Society of Teachers in Family Medicine. (poster)
Kopansky-Giles D, Peranson J. Recognizing our hidden faculty: Integrating and supporting the role of health professional educators in Family Medicine. 19 Apr 29; Toronto, ON: Society of Teachers in Family Medicine. (seminar)
Faculty Presentations: 2019-2020 Academic Year
Funabashi M. Preliminary findings from an active surveillance reporting system for spinal manipulative therapy regulated providers and low back pain patients. 19 Oct 28; Antwerp, Belgium: 10th Interdisciplinary World Congress on Low Back & Pelvic Girdle Pain.
Funabashi M. Predictors of patients who are likely to experience adverse responses following manual therapy: Secondary analysis of a survey of patients’ perceptions of what constitutes an adverse response. 19 Oct 28; Antwerp, Belgium: 10th Interdisciplinary World Congress on Low Back & Pelvic Girdle Pain. (poster)
Weis CA. A systematic review of manual and nonpharmacological procedures for pregnancy and post-partum back and pelvic girdle pain. 19 Oct 28; Antwerp, Belgium: 10th Interdisciplinary World Congress on Low Back & Pelvic Girdle Pain. (poster)
Kopansky-Giles D, Peranson J, Antao V. Integrating and Supporting Health Professional Educators in Family Medicine. 19 Oct 30; Vancouver, BC: Family Medicine Forum 2019. (poster)
Welsh P, Howitt S, Howarth SJ. The Influence of Hip Joint Angle on the Ratio Between Adduction and Abduction Torque in Experienced, Recreational Male Hockey Players. 19 Nov 9; Toronto, Canada: FRRCCSS(C) East Sports Conference 2019.
CMCC Research Report 2018–2020 126
Accepted Presentations at Cancelled Venues
Kopansky-Giles D. Recognizing our Hidden Faculty: 3-Year outcomes of the Health Professional Educators (HPE) program in the Department of Family and Community Medicine at the University of Toronto. 20 Apr 19; Vancouver, BC (virtual): Canadian Conference on Medical Education.
Kopansky-Giles D. Evaluating the integration of interprofessional collaboration competencies within simulation training. 20 Apr 19; Vancouver, BC (virtual): Canadian Conference on Medical Education. (poster)
Abbas A, Howarth SJ. The 1-year Prevalence of Occupational Musculoskeletal Disorders in Practicing Chiropractors in Ontario. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Choi G, Funabashi M. Manipulation force characteristics and clinical outcomes of prone thoracic spinal manipulation in chiropractic students with neck pain: a pilot study. 20 Mar 19; San Diego, USA: ACC RAC 2020.
da Silva-Oolup S. Evaluating the baseline abilities of second year chiropractic students to identify cardiac and lung sounds at the Canadian Memorial Chiropractic College using high fidelity manikin simulators and standardized human patients: a pilot study. 20 Mar 19; San Diego, USA: ACC RAC 2020.
De Luca K, Funabashi M, Mior S, Hogg-Johnson S. Conditions and management of the older chiropractic patient: a secondary analysis of 6927 adult-patient encounters from Australian (COAST) and Canadian (O-COAST) studies.: Factors influencing the transmission of force in human tissues during manual therapy: a crossover study. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Dunham S. Experiential Learning: Ten years of Reflection. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Funabashi M. Factors influencing the transmission of force in human tissues during manual therapy: A crossover study. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Funabashi M. Quantification of the Forces Applied and Transmitted Through the Body during Thoracic Spinal Manipulation in Asymptomatic Adults. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Funabashi M. Strategies to mitigate benign adverse events for spinal manipulation: Exploring clinicians and patients' perceptions. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Gleberzon B. Survey of Students' Perceptions Of The Jurisprudence, Ethics And Business Management course at the
Canadian Memorial Chiropractic College. 20 Mar 19; San Diego, USA: ACC RAC 2020. (poster)
Gleberzon B. Toward the development of a Standardized Chiropractic Technique program. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Kopansky-Giles D. Cultivating collaborative teams using an interprofessional collaboration competency framework in performance appraisals. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Lee A. Exploring patient and clinician experiences and beliefs about benign adverse responses to spinal manipulation in chiropractic teaching clinics: a cross-sectional survey. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Pohlman K, Funabashi M. Patients’ and Interns’ Expectations of Adverse Events: Data from an Electronic Active Surveillance Study at a Teaching Clinic. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Stainsby B. Multicentric reticulohistiocytosis presenting to a chiropractor: A case report. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Suri M, Kopansky-Giles D. Evaluating the integration of interprofessional collaboration competencies within simulation training. 20 Mar 19; San Diego, USA: ACC RAC 2020.Thomas J, Funabashi M. Quantification of the Forces Applied and Transmitted Through the Body during Thoracic Spinal Manipulation in Asymptomatic Adults. 20 Mar 19; San Diego, USA: ACC RAC 2020.
To D. Lessons learned from cases of rib fractures after manual therapy: a case series to increase patient safety. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Wang S. Discomfort during setup of side posture hypothenar/ ilium push manipulation. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Yu H. Non-pharmacological Management of Soft Tissue Disorders of the Shoulder: A Clinical Practice Guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. 20 Mar 19; San Diego, USA: ACC RAC 2020.
Duarte F. Investigating the Link Between Skeletal Muscle Substance P levels of Rats and Quantitative Ultrasound Image Texture Utilizing Multiple Regression: An Exploratory Pilot Study. 20 Mar 19; San Diego, USA: ACC RAC 2020. (poster)
A selection of published research by CMCC faculty 127
Funabashi M. Manipulation force characteristics for older adults using mannequin simulators. 20 Mar 19; San Diego, USA: ACC RAC 2020. (poster)
Kopansky-Giles D. Recognizing our Hidden Faculty: 3-year outcomes of the Health Professional Educators (HPE) program in the Department of Family and Community Medicine at the University of Toronto. 20 Mar 19; San Diego, USA: ACC RAC 2020. (poster)
Tukhareli N. The “5 A’s Instruction”: A novel approach to teaching the Evidence-Based Practice to chiropractic students. 20 Mar 19; San Diego, USA: ACC RAC 2020. (poster)
Wang S. The effects of the side bridge exercise on immediate internal rotation range of motion of the hip. 20 Mar 19; San Diego, USA: ACC RAC 2020. (poster)
Dunham S. Moving from an Administrative to Student-Centered Syllabus: So What? 20 Mar 19; San Diego, USA: ACC RAC 2020. (workshop)
Funabashi M. Building Effective Mentoring Relationships. 20 Mar 19; San Diego, USA: ACC RAC 2020. (workshop)
Kopansky-Giles D. Uncovering the Hidden Curriculum in Medical Education. 20 Apr 24; Toronto, ON: Department of Family and Community Medicine Annual Conference. (workshop)
Pohlman K, Funabashi M. A Session with CARL - Fostering the Fundamentals Resources to Support Early Career Researcher. 20 Mar 19; San Diego, USA: ACC RAC 2020. (workshop)
Funabashi M. Characteristics for forces transmitted through older adults during thoracic spinal manipulation therapy –preliminary results. 20 Apr 27; Melbourne, Australia: SpineWeek 2020.
Funabashi M. Beliefs, perceptions and practice on mitigation strategies for benign adverse events after spinal manipulation therapy. 20 Apr 27; Melbourne, Australia: SpineWeek 2020. (eposter)
Funabashi M. Force distribution within spinal tissues during posterior to anterior spinal manipulative therapy. 20 Apr 27; Melbourne, Australia: SpineWeek 2020. (poster)
Kopansky-Giles D, Maiers M, Thistle S. Our Next Guest Needs No Introduction… If You’re a Chiropractor. 20 May 1; Halifax, NS: Canadian Chiropractic Association NCT.
CMCC Research Report 2018–2020 128
The CMCC Research Report 2018-2020 is produced by the Division of Marketing and Communications.
AVP. Institutional Advancement + Communications: Mara Bartolucci
Copyeditor: Margaret McCallen
Art Director: Dora Kussulas
Designer: Tariqa Manji
Contributors: Mark Fillery, Margaret McCallen
Canadian Memorial Chiropractic College 6100 Leslie Street, Toronto, ON, M2H 3J1
Copyright 2021 Canadian Memorial Chiropractic College
To request a copy, contact the Division of Marketing and Communications at: Phone: 416 482 2340 Fax: 416 482 3629 Email: communications@cmcc.ca
www.cmcc.ca
Canadian Memorial Chiropractic College 6100 Leslie Street, Toronto, Ontario M2H 3J1 Telephone: 416 482 2340 www.cmcc.ca