
10 minute read
THEN AND NOW

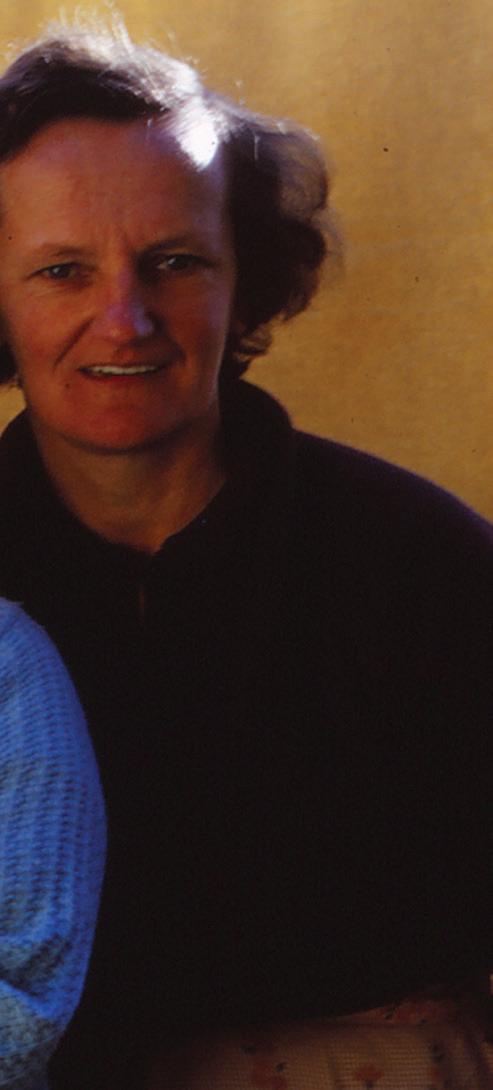
Left: Kate Wright, far left, with her baby daughter (Jess Medforth’s mother), grandmother and mother in 1966.
Women’s experiences of pregnancy and birth have changed dramatically over the last few decades, driven by social change and the revival of midwife-led care in New Zealand. On the thirtieth anniversary of the law change that allowed midwives to practise autonomously, Annie Oliver speaks to a grandmother and granddaughter about their contrasting experiences.
ANNIE OLIVER JOURNAL ADMINISTRATOR
kate’s story
When 73-year-old Kate Wright mentioned to her 19-year-old granddaughter that she was pregnant at her age, her granddaughter was horrified. But this was perfectly normal in the 1960s.
“We were all young when we got married and had our babies,” she says. “If you weren’t married by 21, you were basically on the shelf!”
When Kate realised she was pregnant, she went straight to her GP. “We didn’t have midwives in those days; we always went to the doctor. But I was so lucky with my doctor, he was a lovely man and I felt very well cared for.”
She had monthly antenatal appointments until about seven months, followed by fortnightly appointments, then weekly closer to the birth. She says that doctors didn’t tell pregnant women much about what to expect “but we didn’t worry too much about being pregnant. There was no fuss or bother; we just got on with it.”
She feels fortunate that her mother was a great support and had had her last baby only three years earlier. So Kate felt a close connection to pregnancy, birth and a new baby.
She and her husband Gavin also attended antenatal classes, so she felt quite prepared at the time and wasn’t anxious about the birth. “Although, looking back, I didn’t really know much,” she admits.
Kate was living in Timaru and recalls the Jean Todd maternity unit in Timaru Hospital as being the only choice of birth place. She knew of no-one having a home birth.
So when labour started she rang the hospital, and the nurses contacted her doctor. Gavin drove her to the hospital and was allowed in the pre-birthing room but not in the theatre, where Kate went once labour was more advanced. As was standard practice at the time, she was ‘prepped’ by being shaved and given an enema.
Of her three children (born in 1966, 1968 and 1970), the births of her eldest and youngest were straightforward, with no complications or pain relief. Not so with her second baby.
“They let me go too far over. I was three-and-a-half weeks overdue and he ended up being 10lb 2oz (4.6kg). Twice I thought I was going to have him so Gavin took me to the hospital and they ‘prepped’ me but then they sent me home again as he wasn’t ready to come.
“The third time they took an x-ray to see if my pelvis was wide enough and yes it was, so they decided to induce me. My legs were up in stirrups – they were up in stirrups for all three babies, that’s just how it was then. And the only pain relief was the gas mask – it was great though; it took you to another planet,” she laughs.
After each birth, Kate stayed in hospital for 10 days. “That’s what new mums did. There was no choice to

Jess and Dave Medforth with their sons Samuel and baby Liam in 2017.
After each birth, Kate stayed in hospital for 10 days. “That’s what new mums did. There was no choice to leave earlier. Gavin could visit me every day but our older children were only allowed to visit on Sundays.”
leave earlier. Gavin could visit me every day but our older children were only allowed to visit on Sundays.”
Kate breastfed all three of her babies – the eldest and youngest for several months. However, after the birth of her second baby she’d lost so much weight that the doctor advised her not to continue feeding him. “It was his decision but I was feeling very weak and was totally ok with that.”
Kate was lucky enough to have her own room when in hospital, and her baby would be with her during the day, then taken to the nursery overnight. “Although, thinking about it now, I’m not sure what they did about feeding the babies overnight.
“We had breakfast brought to us in bed and had the other meals in the community room, where it was good to meet lots of other mums. But it was a long 10 days. I had a nice rest but was well ready to come home by the end of it.”
Once home, Kate looked forward to her weekly visits from Plunket, which gave her a sense of security that someone would be there to answer questions.
“On reflection, we probably could’ve had a lot more knowledge and support, although I was lucky that I had Mum so close. I felt sorry for women who didn’t have their mother nearby.”
Having seen the experiences of her children and grandchildren, including granddaughter Jess Medforth, Kate says that there is definitely more support for new mothers now. And for fathers, who are now far more involved in pregnancy, birth and early parenting.
“As time has gone on, Gavin has felt more strongly about being denied the experience of being at his children’s birth,” says Kate.
“He thinks that men today are so lucky to be able to be part of the birth but, at the time, it wasn’t the practice at all then. It wasn’t even considered.”
jess’s story
When Jess Medforth, then 28, discovered that she was pregnant five years ago she started looking for a midwife straightaway as she had heard that it might be difficult to find one.
Living in Auckland but with her family in the South Island, there weren’t a lot of opportunities to hear about the experiences
of her mum, or her nana, Kate Wright. “Also, Mum’s births were all C-sections and I was planning a natural birth,” says Jess.
Jess found a midwife and saw her regularly from eight weeks. “I was one of the first of my close friends to have kids, so mostly I researched a lot on the internet and then went to my midwife with any other questions,” she says.
Although she had moments of uncertainty about the birth, she would talk to Dave and her midwife about how she felt. “I’d hear stories about awful labours because everyone wants to share those with you when you’re pregnant.”
While Jess attended most antenatal appointments by herself, she and Dave went to the scans and antenatal classes together and it was a joint decision to have the baby in hospital. When Jess’s waters broke in the night, they tried to go back to sleep but it was short lived, as the contractions started coming pretty quickly.
“So I rang the midwife at 3.30am, we were in hospital by 4am, and Samuel was born at 6.50am.“I ended up having a waterbirth. I said I’d like to try the water for pain relief and I found it was calming so stayed in the water for the rest of the labour. It all went pretty well and I just had some gas towards the end.”
Dave was as involved as possible. He held the gas mask for her, offered her a drink of water between contractions and together they picked up Samuel out of the water when he was born.
“In the end the midwife didn’t catch him. I just changed positions and he flew out.”
Jess stayed in the pool with Samuel for about five minutes, and then moved to the bed for an hour or so, putting him to the breast. “Then he had cuddles with Dave and they stayed together while I went to the theatre.
“They thought I had a third degree tear, so I had to have an epidural and get sewn up.”
She had also haemorrhaged while in the pool. “I lost a lot of blood and ended up having to stay in hospital for five days and had two transfusions. Dave stayed in hospital with Jess and Sam the entire time. “Dave did everything. He was so supportive. I couldn’t feel my legs for 12 hours and then I was hooked up for the blood transfusion, so I mainly stayed in bed and he changed all the nappies and brought the baby to me to feed.”
Dave was equally supportive and involved for the birth of their second son, Liam, two years later.
After the complications with Sam, they planned another hospital birth. But unlike Sam’s birth, when Jess felt that she made decisions throughout, the labour turned “dramatic”.
Again a fast labour – only three hours from start to finish – her midwife didn’t make it to the hospital in time for the birth.
“The hospital midwife said the baby’s heartbeat was too slow and they were worried he wouldn’t breathe when he was born, so I had to have an episiotomy without any pain relief.
“The midwife asked Dave, ‘is it ok to cut her, we have to get this baby out’. I remember him saying ‘yep’ but I wasn’t in any condition to make any decisions about anything.”
Their midwife arrived to do the suturing and, fortunately after an initial low Apgar score of 2, baby Liam bounced back in five minutes.
The three of them stayed the night in hospital, before spending two nights in Birthcare.
Jess feels fortunate that breastfeeding went “pretty well”. She says the hospital midwives were “lovely” and were happy to check anytime that baby was latching on well.Although it was challenging finding a midwife initially, overall Jess and Dave feel extremely grateful for the care and support they received, both antenatally and postnatally.
“Having a midwife and continuity of care definitely made the experience less overwhelming with both my pregnancies,” Jess says. square
CLINI C AL L Y PR O VEN 100% S AFETY RECORD E S T . 1992

More restful, safer sleep Natural, free limb and hip movement Ensures swaddling, sleepwear, Sleepingbag use is safer and cosier Excellent for babies requiring varied sleep


safely lasts two babies aged 0-2 yrs positions or cot elevation C L I N I C A L L Y P R O V E N • S A F E • T R I A L L E D • 2 5 Y ears O VER The World’s Safest Baby Wrap *safely lasts two babies aged approximately 0-2 yrs
20% OFF online only ‘NZCOM’ www.safetsleep.com
prepares the perineum
EPI-NO is clinically proven to signifi cantly increase the chances of an intact perineum, reduce episiotomy, and is safe to use. EPI-NO is a dual purpose CE approved medical device designed to strengthen the pelvic fl oor muscles from early in pregnancy, and again postpartum. The perineal stretching exercises commence concurrently after Week 36. EPI-NO Childbirth Training has been accepted in Australia & New Zealand for over 15 years as an effective preparation for women choosing a natural vaginal birth.
EPI-NO Patient Brochures can be requested for New Zealand via info@starnbergmed.co.nz

Over 50,000 EPI-NO births in Australia and New Zealand. Available in over 20 countries worldwide. www.starnbergmed.co.nz Available online with shipment from Auckland and at selected pharmacies.

‘The human body performs to maximum effi ciency in any physical activity when correctly trained and prepared. Childbirth is no exception.’ Dr Wilhelm Horkel, Starnberg (EPI-NO inventor) Made in Germany









