COLORADO MEDICINE
ADVOCATING


ADVOCATING




MEDICAIDDISENROLLMENTUNINSUREDRATESPIKE





Safety net clinics that care for the most vulnerable are taking drastic measures to keep their doors open following disenrollments in Medicaid, higher rates of uninsured patients and increasing costs to run a business. A severe state budget shortage and threats of funding cuts from the federal level further complicate the issue. A coalition is asking legislators to consider the long term to reinforce the safety net.











8 UNDERSTANDING UNIVERSAL LIFE INSURANCE WITH A LONG-TERM RIDER
The Colorado Medical Society is proud to launch a new, exclusive member benefit in partnership with Copic Financial and BuddyIns. The new simplified issue life insurance plus long-term care insurance product is an investment in your family’s future.
10 KEEPING COLORADO PHYSICIANS AT THE FOREFRONT: THE VALUE OF ACCREDITED CME
Continuing medical education is a crucial component of professional development. The Colorado Medical Society provides accredited CME to physicians and accredits providers of CME.
12 CULTIVATING WELLNESS IN MEDICAL TRAINING
Attention physicians in training: Healthy wellness habits formed early in your medical career can set a strong foundation for a life in medicine.
FINAL WORD: SAVE OUR SAFETY NET
Emergency medicine physician Rebecca Kornas, MD, FACEP, discusses the impact of Medicaid disenrollments on emergency departments and the need to support the health care safety net.
Advocacy
of the
Medical Society and membership of
2024-2025
Kim Warner, MD
President
Brigitta Robinson, MD
President-elect
Omar Mubarak, MD, MBA
Immediate Past President
Hap Young, MD
Treasurer
Dean Holzkamp
Chief Executive Officer
Brittany Carver, DO
Kamran Dastoury, MD
Amy Duckro, DO, MPH
Rachelle M. Klammer, MD
Marc Labovich, MD
Justin McCoy, DO
Katie McDermott, MSC
Michael Moore, MD
Rhonda Parker, DO
Lynn Parry, MD
Sean Pauzauskie, MD
Leto Quarles, MD
Davis Witt, MD
Hap Young, MD
Dean Holzkamp
Chief Executive Officer
Dean_Holzkamp@cms.org
Kate Alfano
Director of Communications and Marketing
Kate_Alfano@cms.org
Mike Bintner
Director of Membership
Mike_Bintner@cms.org
Virginia "Ginny" Castleberry
Executive Director
Denver Medical Society
Virginia_Castleberry@cms.org
Cecilia Comerford-Ames
Executive Director, Colorado Society of Eye Physicians and Surgeons Communications Manager
Cecilia_Comerford@cms.org
Dorcia Dunn
Program Manager, Membership
Dorcia_Dunn@cms.org
Crystal Goodman
Executive Director, Northern Colorado Medical Society
Crystal_Goodman@cms.org
Mihal Sabar
Director of Accounting
Mihal_Sabar@cms.org
COLORADO MEDICINE Vol 122 No. 1 Winter 2025 (ISSN-0199-7343)
80230-6902. 720-859-1001.
17550, Denver, CO 80217-0550.
Editor, and Kate Alfano, Managing Editor. Design by Scribner
David Downs, MD, FACP
Carolynn Francavilla, MD
Mark Johnson, MD, MPH
Jan Kief, MD
Rachelle Klammer, MD
A. "Lee" Morgan, MD
Tamaan Osbourne-Roberts, MD
Lynn Parry, MD
Brigitta J. Robinson, MD
Michael Volz, MD
Jeremy A. Lazarus, MD
Chet Seward Chief Strategy Officer
Chet_Seward@cms.org
Kim Vadas, MABMH, CHCP, FACEHP Director of Continuing Medical Education and Recognized Accreditor Programs
Kim_Vadas@cms.org
Debra Will Director of Business Development
Debra_Will@cms.org
Kim Warner, MD, CMS President
Advocacy is the backbone of our profession. It shapes policy, protects our ability to care for patients, and ensures that health care policy is heavily influenced by physicians: the people who understand it best. It is also the top member benefit of the Colorado Medical Society, and one all Colorado physicians rely on – regardless of membership. I’ll return to that point in a moment and tell you why every single Colorado physician must become a CMS member and continue to invest in membership year after year.
As physicians, we see firsthand how legislation impacts health care access, affordability, and provider sustainability; it’s about real people and real lives. Our CMS lobbyist, Dan Jablan, explains that health care policy is like your New Year’s resolutions. These are high-level goals that you set to improve your life, like being healthier or getting finances under control. Advocacy is the work you put in to achieve that policy. In the resolutions example, this is committing to a regular fitness class, eating fewer processed foods, putting aside more in savings.
You’re not going to achieve your year’s goal of becoming healthier if you go on one run. Physician advocacy also requires returning to the work again and again. This consistency is what makes policies to improve patient care a reality, whether it’s dismantling barriers to care or defending the integrity of peer review. Our work on prior authorization took years of relationship building, surveys, data analysis, and collecting stories from patients and physicians, plus two sessions with an active bill.
Similarly, last session’s liability caps battle was decades in the making. CMS leaders championed the original tort reforms back in the late ’80s and early ’90s, and founded Copic when other liability insurance carriers left the state and insurance premiums skyrocketed. From that point on, the Colorado Medical Society closely monitored all threats to our stable medi -

cal liability climate – and there are many every single session.
Then 12 years ago, we helped bring together physicians and the business community to form Coloradans Protecting Patient Access (CPPA) that continued this critical work. It came to a boiling point last session when the Colorado Medical Society, within the CPPA coalition, had the fight of our lives as trial attorneys attempted to eliminate all caps on liability and eliminate confidentiality in peer review. We came through that fight keeping a cap and peer review intact, and avoided a costly ballot fight.
CMS regularly builds coalitions to pass good policy. Nearly 20 years ago, we were entrenched in the fight to ban smoking in indoor public spaces, facing significant backlash from businesses and the tobacco industry. Yet, through bipartisan support and relentless advocacy, we succeeded in making a lasting impact on public health with the passage of the Colorado Clean Air Act.
For me, advocacy is personal. It’s about using my expertise as a physician to inform decision-makers and shape better policies. It’s about the privilege of walking into the Capitol, engaging directly with legislators, and having my voice heard. Building relationships with policymakers, sharing the perspective of practicing physicians—even when we disagree—demonstrates why physicians' involvement is crucial. Legislators don’t always have a deep understanding of evidence-based medicine, and it’s our job to bridge that gap.
Here’s the call to membership that I promised. Advocacy doesn’t happen in a vacuum; it requires numbers, resources and strategic action. Membership growth is a key priority for our organization because the strength of our voice in the legislature is directly tied to the size of our membership and the resources we can allocate to advocacy efforts.
Make sure every physician at your practice is a member. Build membership into your budget to ensure you and your group renew every year. Talk to other colleagues in your area and urge them to join. Political engagement may be uncomfortable for some, but the reality is that financial support for our political action committee, COMPAC, is one of the most effective ways to ensure medicine has a seat at the table.
As we work through another legislative session, I encourage each of you to stay engaged. Attend our legislative events, contribute to our PAC and small donor committee, and most importantly, continue to speak up for our patients and profession. Together, we can ensure that the needs of our patients drive the future of health care in Colorado. ■
Kate Alfano, CMS Director of Communications
At Clinica Family Health and Wellness, actions taken over the past year tell a devastating story – one that is unfolding across Colorado. Medicaid disenrollments have driven thousands of patients into the ranks of the uninsured, forcing deep cuts to essential services and threatening communities’ access to care. Clinics like Clinica, which has locations in Boulder, Denver, Lafayette, Thornton, Westminster, Nederland and Black Hawk, are lifelines for low-income and rural families and are now on the brink of closure.
“We are a canary in the coal mine, but not the only one,” says Simon Smith, CEO of Clinica Family Health and Wellness. “We are hollowing out primary care and prevention services that keep people healthy and save our system money. The safety net, like the health of the people we serve, is fragile. Insurance status may change, but the needs of the human being do not.”
Before the pandemic, Clinica’s payer mix of patients was 45.7 percent Medicaid and 37.5 percent uninsured. Today, it is 37.5 percent Medicaid and 43.4 percent uninsured. This represents an 8.2 percent drop in Medicaid and a 6 percent rise in the uninsured population from pre-pandemic levels.
“I know there are questions about what has happened to those who have lost their Medicaid coverage,” Smith says. “At Clinica, it appears that over 70 percent of them are now uninsured. That is thousands and thousands and thousands of newly uninsured patients within our organization.”
Due to lower revenue, Clinica has been forced to eliminate critical programs –from maternal health visits to homeless outreach—while cutting over 100 staff positions across two rounds of layoffs, over 15 percent of their workforce. They have dipped into their limited reserves, executives and high earners have voluntarily


cut their pay, and still they are forced to turn away new patients who have nowhere else to go. The safety net is fraying.
Meanwhile, lawmakers need to cut $1 billion in state spending in the next fiscal year to balance a budget that is short pandemic-era federal funding and limited by how much state spending can increase under the Taxpayer’s Bill of Rights (TABOR) cap. Add in increased state spending in the Medicaid program due to an aging population, changes in the amount and mix of services utilized, and underestimating growth, plus uncertainty in continued federal funding, and this convergence means legislators are having tough conversations to prioritize what gets funded and what gets cut.
Physicians, patients and organizations like the Colorado Medical Society are strongly advocating for minimal damage to the health care safety net, fearing that drastic cuts could devastate infrastructure for vulnerable patients and be nearly impossible to rebuild in the future.
Health First Colorado, Colorado’s Medicaid program, provides free or low-cost health insurance for Colorado children and adults who qualify based on income and household size, around $45,000 annually for a family of four. Child Health Plan Plus (CHP+) provides low-cost health insurance for Colorado children and pregnant women with a slightly higher income than those in Medicaid, around $81,000 for a family of four. Both programs are funded by a federal-state partnership, and the share paid by the federal government for Medicaid increased to 90 percent under the Affordable Care Act when Colorado expanded eligibility to low-income adults. Both programs are administered in our state by the Colorado Department of Health Care Policy and Financing (HCPF).





During the Covid-19 public health emergency (PHE), many Coloradans lost their jobs and their employer-sponsored health insurance, and Health First Colorado rosters swelled by 45 percent, or 550,000 Coloradans. At the height of enrollment, Health First Colorado covered one-third of the state population, according to HCPF.
Once the PHE ended in May 2023, and with it the federal continuous coverage requirement that guaranteed patients could keep their health coverage, the 1.7 million members of Health First Colorado and CHP+ had to go through a redetermination process to assess if they still qualified for coverage. That 14-month process started in March 2023 with notifications and concluded May 2024.
Before redetermination began, HCPF estimated that 325,000 Medicaid members would lose eligibility. According to the Kaiser Family Foundation, an independent health policy research organization, by September 2024, 563,000 Medicaid members lost eligibility—a decline of 9 percent—dropping the total enrolled in Medicaid to 1.04 million enrolled in Medicaid.
And though HCFP’s reported numbers of enrolled Medicaid and CHP+ members have been consistently higher than KFF’s, the agency’s published numbers are close; as of December 2024, HCPF reported enrollment in Health First Colorado was 1.13 million and enrollment in CHP+ was 92,000, for a total of approximately 1.2 million covered lives; still a loss of eligibility for more than 500,000 individuals.
Save Our Safety Net Colorado – a coalition of health care providers, consumer advocacy groups and other health care
2023
1.7 MILLION 1.04 MILLION 2024
Source: Kaiser Family Foundation
organizations including the Colorado Medical Society – is sounding the alarm about negative effects of disenrollment, especially for those are still eligible but not enrolled.
In an issue brief published in October, the group cited that 65 percent of the more than 500,000 Coloradans who were disenrolled from Medicaid lost coverage due to administrative burdens or procedural reasons such as application processing delays, never receiving and enrollment pack, or onerous enrollment requirements. Some of those have since come back to the program, but others may have been pushed out of the insurance market altogether. The impact for patients and providers is bleak, and the economic implications touch the entire state.
“Over the last 18 months, over 2,000 of our patients have lost Medicaid coverage,” says Dustin Moyer, CEO of Mountain Family Health Centers, which provides care to Roaring Fork, Colorado and Eagle Valleys. “One year ago, 38 percent of our patients were uninsured; today that figure is 47 percent. In fact, our current payer mix is nearly identical to what it was prior to the state expanding Medicaid through the Affordable Care Act in 2013: 47 percent uninsured and 28 percent Medicaid.”
Moyer continues: “The decline in Medicaid coverage has led to barriers to care for our patients who need specialty or hospital services, and a significant financial challenge for Mountain Family. We have calculated that our total lost revenue stemming from the 2,000 of our patients who have lost Medicaid is $1.5 million on a $25 million budget.”
To account for the loss of revenue and to ensure they can continue serving their community, in the last 12 months, Mountain Family has eliminated 10 positions and laid off five people, closed two school-based health centers and reduced hours of operation at three others, instituted hiring freezes, and implemented
LOSS OF 600,000+ PEOPLE
a 3-month suspension of employer retirement contributions.
That brings in the impact of disenrollments on the state economy. The Colorado Health Foundation recently published a study of the positive economic impact of Colorado’s Medicaid expansion under the ACA and negative effects of disenrollment.
At the high end of a scenario where 504,000 otherwise eligible are disenrolled, the state economy is 0.9 percent smaller with an output loss of $4.7 billion and employment loss of 28,000 jobs. At the low end of the scenario where 100,000 otherwise eligible are disenrolled, the state economy is 0.2 percent smaller with an output loss of just under $1 billion and an employment loss of 5,500.
Phyllis Resnick, PhD, is executive director and lead economist for Colorado Futures Center, and authored the study. “It's hard to measure things in isolation, but if we could, this is what our models tell us the impact of the disenrollment was: That the economy would be anywhere between 0.2 percent and 0.9 percent smaller depending on that high to low scenario. Then when economies contract, everything related to the economy contracts. Typically, you have higher levels of unemployment. When you have higher levels of unemployment, household earnings go down, and when household earnings go down people spend less in restaurants and retail shops and going skiing and going to the spa and all the other things you spend household income on, and then as a result of that, the tax revenue that's generated by the state contracts as well.”
“The reason everyone should care about disenrollment is that even if you're not directly affected with respect to your health care, because of our state-federal relationship around Medicaid, when we disenroll, we draw down fewer dollars and it does slow the Colorado economy,” Resnick says.
The good news is that key Colorado lawmakers on the Joint Budget Committee and Senate and House Health and Human Services committees are educated on these issues, thanks to the advocacy work led by the Colorado Medical Society and made possible by members’ dues investment.
“When it comes to Medicaid, I think there is a commitment by the vast majority of the legislature to try to preserve and protect the Medicaid program,” Rep. Kyle Brown said in a Jan. 23 panel hosted by the Colorado Health Institute. He chairs the House Health and Human Services Committee.
“In particular, I think there’s a concern that we would use Medicaid and cutting provider rates or services for folks as a way of filling a hole. We may not have a choice, but I think there is a recognition that Medicaid is usually about life and death for folks, and of all the things that should be on the chopping block, those issues that are literally life and death for people should be towards the bottom.”
Sen. Kyle Mullica, member of the Senate Health and Human Services Committee, and Sen. Barbara Kirkmeyer, member of the Joint Budget Committee, co-wrote an editorial published Nov. 20 in the Denver Post in which they said, “While Colorado
As the legislative sess ion unfolds, the Colorado Medical Society is at the forefront of key policy decisions affecting physicians and patients. CMS is spearheading a transparency bill to ensure patients know exactly who is providing their care. Clarity in health care is essential, and this legislation aims to prevent confusion by patients about provider qualifications and training.
Meanwhile, naturopaths once again wanted to expand their scope of practice, pushing for diagnostic and prescriptive authority for most Schedule III-V medications. Through CMS leadership and great relations at the statehouse, this bill was killed in committee.
has never reached a point where every resident has health insurance, we have done much better in ensuring coverage in recent years. A return to ‘the bad old days’ is unacceptable. In the year ahead, we must make stabilizing our health care safety net and restoring Medicaid coverage for eligible Coloradans our state’s top priority.”
AS PART OF SAVE OUR SAFETY NET, IS ASKING LEGISLATORS TO:
• Resist attempts to cut Medicaid and other behavioral and physical health care safety net funding for individuals who use the public programs for their health coverage and in-home services that allow people with disabilities to live independently in their communities.
• Support funding the Primary Care Fund, an important financing strategy established by the 2004 tobacco tax, at $10 million, and allow gifts, grants and donations to be used to provide additional funding.
• Put greater effort and focus on supporting Coloradans who are eligible but not enrolled in the Medicaid benefits to which they are entitled by expanding points of entry for Medicaid enrollment and supporting additional funding for county enrollment activities.
CMS is also strongly supporting a bill that strengthens protections for physicians by limiting restrictive employment agreements. This legislation ensures that non-compete clauses do not unreasonably hinder medical professionals from continuing to care for their patients, ultimately promoting better access to health care across Colorado.
CMS is opposing a bill that aims to boost funding to Colorado’s safety-net health centers by setting reimbursement rates for providers under state and small employer health plans. The bill does not address the crisis in Colorado’s health care safety net. With rising uninsured patients and expected Medicaid cuts, capped physician rates may only worsen access to care, making it harder for doctors to serve vulnerable communities.
NO MEDICAID CUTS
FUND PRIMARY CARE FUND
EXPAND MEDICAID ENROLLMENT EFFORTS
DATA DASHBOARD FOR TRANSPARENCY
COLLABORATIVE COMMITTEE
MAXIMIZE FEDERAL FUNDING
• Support efforts to require HCPF to create a shared data dashboard cataloging key data points so all interested parties can work together to find solutions.
• Support our calls for a collaborative committee structure to allow consumer advocates, provider groups, health stakeholders and the Polis administration to work together on shared solutions to both the Medicaid disenrollment crisis and the broader issue of the growing number of uninsured Coloradans who need access to health care.
• Seek ways to maximize federal funding and explore innovative options for securing additional revenue, so we can grow state investment in health care and better meet the health care demands of residents.
Together with our partners, we are focused on key issues including supporting batching bills for out-of-network services to streamline arbitration for similar claims and combating efforts to destabilize the liability climate. As the session progresses, additional health-related bills will undoubtedly emerge.
With nearly 700 bills expected this session, CMS remains vigilant in tracking legislation that impacts physicians and their ability to provide high-quality care. Your voice is vital – watch for opportunities to take action and make a difference.
The Colorado Medical Society is working to ensure that sound policy decisions protect both our profession and our patients.
“Legislators are fired up and eager to help,” says Cody Belzley, an expert on health care policy and Medicaid. “The options are limited given the overall budget challenges, but it’s early in session and we’re working with them to
explore what is possible. We’re still holding out hope that it will be possible to make some investments in the safety net – even if they are ‘down-payments’ or initial steps on a longer-term strategy.” ■




Physicians began 2025 facing bad news from Medicare: a 2.83 percent cut in payment. The positive update that was strongly advocated for by the American Medical Association (AMA) and supported by a bipartisan majority of Congress was promised but ultimately left out of the year-end omnibus bill necessary to temporarily fund the government.
Even worse, this cut comes as the Centers for Medicare and Medicaid Services (federal CMS) projects another 3.5 percent rise in the Medicare Economic Index, which measures the cost of running a medical practice.
That’s five straight years of cuts in Medicare pay, and AMA research shows that Medicare physician payment, when adjusted for inflation, has dropped by 33 percent since 2001.
Many don’t realize how Medicare payment affects what private insurers and other payers are willing to pay for care. Commercial carriers frequently peg their contracts to Medicare rates, so ongoing rate cuts in Medicare have a compounding effect as those lower rates in turn decrease commercial rates.
In late January, a bipartisan group of 10 U.S. House members introduced a bill to stop the 2.83 percent cut in Medicare payments to physician practices this year while providing a 2 percent payment update, aiming to stabilize physician practices and protect patients’ access to care.
The AMA and Colorado Medical Society, with many other state and national specialty societies, strongly support the legislation to ensure sustainability for practices now and in the future.

Marc Glickman, FSA, CLTC

Life insurance and long-term care insurance traditionally serve two different but essential purposes in financial planning.
Life insurance provides financial protection for your loved ones after you pass away, while long-term care insurance helps cover the costs of extended medical care as you age. Understanding how these two types of coverage can work together in a single policy helps when evaluating your insurance options.
Universal life insurance policies that include long-term care riders combine both types of protection, allowing the death benefit to also help pay for nursing home care, assisted living facilities, or home health care services if needed during your lifetime.
Transamerica Universal Life with Long Term Care Rider is a two-in-one benefit that offers simplified issue life insurance for family needs plus long-term care benefits. With the Restoration Rider, the life insurance benefit pays out even if you use the long-term care benefit.
The death benefit can help protect your loved ones financially after you pass away. During your lifetime, it also responds to a long-term care need—one of the most expensive health-related events we face that is not covered by health insurance. Planning for long term care can be one of the most important decisions you can make, and it’s a gift for your family, too.
KEY BENEFITS OF TRANSAMERICA UNIVERSAL LIFE WITH LONG TERM CARE RIDER
• No medical exams or blood work required to qualify
• Guaranteed death benefit protection
• Builds cash value you can access during your lifetime
• Long-term care coverage that doesn’t expire
• Waiver of premium payments if you’re laid off or on strike
• Convenient payroll deduction payment options
Universal life insurance functions differently from traditional term life insurance. It has three main components: a death benefit, a cash value account, and flexible premiums. The policy combines permanent life insurance protection with a savings element that builds value over time.
This dynamic structure allows the policy to provide both protection and potential cash value growth, while maintaining the flexibility to adapt to changing financial circumstances over time.
KNOW THE COST: CHOICE OF CARE SETTING
⚪
⚪ ASSISTED LIVING ($5,350/MONTH)
⚪ LONG TERM CARE ANNUAL BENEFIT
⚪ REMAINING OUT OF POCKET EXPENSES
⚪ PRIVATE NURSING HOME ($320/DAY) ⚪ LONG TERM CARE ANNUAL BENEFIT ⚪ REMAINING OUT OF POCKET EXPENSES
One of the most valuable features of this benefit is the Long Term Care (LTC) Rider. This optional benefit helps cover costs if you need nursing home care, assisted living, or home health care services. The rider provides monthly benefits equal to 4 percent of your death benefit for nursing facility/assisted living care, or 2 percent for home health care/adult day care.
For example, with a $100,000 death benefit, you could receive up to $4,000 per month for nursing home care or $2,000 monthly for home care services. This can help preserve your savings and reduce the financial burden on your family if you require long-term care.
The graph shows examples of how a Universal Life with a Long Term Care Rider benefit can provide a long term care benefit of $4,000 per month. The care costs shown in the graphic reflect a national median.
The policy also includes an Accelerated Death Benefit for Terminal Condition Rider at no additional cost. This allows you to access up to $150,000 or 75 percent of your death benefit if diag nosed with a terminal illness, helping cover medical expenses or other needs during a difficult time.
Additionally, if you use all your long-term care benefits, the Extension of Benefits Rider continues your long-term care coverage while maintaining a portion of your death benefit for your beneficiaries.
While no one likes thinking about needing long-term care or leaving family behind, having proper protection in place provides invaluable peace of mind. Transamerica’s Universal Life Insurance with Long Term Care Rider offers comprehensive protection for what matters most – your family’s financial security and your care needs as you age.
Enrollment is now open. To learn more about coverage options or to see estimated costs versus benefit of this unique offer, visit enroll.buddyins.com/cms
Remember, the best time to get coverage is before you need it. Taking action today




As your life changes, your insurance needs may change, too. This policy allows you to increase or decrease coverage, adjust premium payments, and access cash value when needed. You’re not locked into a one-size-fits-all solution.
The policy is available to members of the Colorado Medical Society who are practicing full time, with face amounts starting at $25,000. Monthly premiums are based on your age and selected coverage amount, with options to fit various budgets.




Kim Vadas, MABMH, CHCP, FACEHP, CMS Director of Continuing Medical Education and Recognized Accreditor Programs
The Colorado Medical Society’s Continuing Medical Education (CME) program aims to enhance learners’ awareness, knowledge, competence, and performance across several critical domains. These key areas include patient safety, professional accountability, quality improvement, patient access to care, and current medical and technical skills knowledge. By focusing on these aspects, the program strives to equip health care professionals with the latest insights and capabilities, ultimately leading to improved patient outcomes and a more efficient health care system in Colorado. This comprehensive approach ensures that learners not only gain theoretical understanding but also develop practical skills that can be directly applied in their medical practice, fostering a culture of continuous improvement and excellence in health care delivery.
CMS is recognized by the Accreditation Council for Continuing Medical Education (ACCME) as an accreditor of intrastate/ interstate providers of CME and is also accredited by ACCME to provide CME for physicians.
CME is a crucial component of professional development for health care providers, ensuring they stay current with the latest advancements in medical science and patient care. CME involves educational activities that develop, maintain, or increase the skills, knowledge, and professional performance of physicians and other health care professionals. The importance of CME cannot be overstated. It helps health care providers stay up to date with rapidly evolving medical technologies, techniques, and best practices. This continuous learning process is essential for maintaining high standards of patient care and safety. CME also offers opportunities for health care professionals to gain new skills, experience professional development, and advance their careers.


Accreditation plays a vital role in ensuring the quality and integrity of CME programs. The Accreditation Council for Continuing Medical Education (ACCME) oversees and enforces standards for CME in the United States. Only organizations approved by the ACCME or recognized state medical associations can designate and award CME credits to physicians.
• Quality assurance: Accreditation ensures that medical education programs meet specified quality standards, protecting patients’ wellbeing and the integrity of the health care system.
• Independence from commercial influence: Accredited CME providers must adhere to strict guidelines to ensure that educational content is free from commercial bias.
• Relevance and effectiveness: Accredited CME is designed to be relevant to physicians’ needs, practice-based, and effective in improving health care outcomes.
• Recognition for licensing and certification: Many state medical boards and professional organizations accept only accredited CME credits for maintaining licenses, certifications, and professional memberships.
Accredited CME plays an invaluable role in helping physicians and health care professionals improve patient care. For physicians, accredited CME can improve performance by focusing on the unique needs of the individual learner, while for organizations it can be a catalyst for change by providing practical solutions to many of their most pressing or urgent problems.
CME HAS BEEN SHOWN TO:
• Improve patient safety: One of the most effective methods for improving physician performance.1
• Control spending: Unnecessary medical procedures, prescriptions, and hospital readmissions are averted. 2,3
• Increase physician recruitment and retention: CME has been linked to a decrease in physician burnout and turnover.4,5,6
The benefits of CME extend beyond individual health care providers to impact the broader health care system:
• Improved patient care: By keeping health care professionals updated on the latest medical developments, CME directly contributes to better patient outcomes and experiences.
• Enhanced patient safety: Accredited medical schools are more likely to offer rigorous clinical training programs and emphasize patient safety measures.
• Ethical practice: CME programs often include a focus on ethical principles and professionalism, contributing to a culture of responsible medical practice.
• Standardization of medical education: Accreditation helps standardize medical education across different regions, promoting consistency in health care delivery.
• Global mobility: Accredited education facilitates the mobility of medical professionals across different health care systems and countries.
While the importance of CME is widely recognized, the field faces ongoing challenges. These include ensuring that
CME activities translate into meaningful improvements in clinical practices and patient outcomes. There is a growing emphasis on outcomes-based education, designed to prepare physicians for broader aspects of competence beyond medical expertise. The future of CME is likely to see increased integration of technology, such as virtual reality and artificial intelligence, to enhance learning experiences. There may also be a greater focus on interprofessional education to improve team-based care and communication among different health care specialties and within care teams.
In conclusion, continuing medical education, particularly when it is accredited programs, plays a crucial role in maintaining and improving the quality of health care. It ensures that medical professionals remain competent, confident, and capable of providing the best possible care to their patients throughout their careers. As the medical field continues to evolve, the importance of robust, accredited CME programs will only grow, serving as a cornerstone of excellence in health care delivery. CMS’s accredited CME program
plays a vital role in ensuring Colorado’s health care professionals remain competent and capable of providing high-quality patient care in an ever-evolving medical landscape.
To learn more about CMS’s educational offerings go to www.cms.org and click on the Education tab.
To find out how to become a CME accredited provider or how to have your activity accredited for AMA PRA Category 1 Credit(s) TM email us at CME@CMS.org ■
1 Cervero, Ronald, and Julie Gaines. “The Impact of CME on Physician Performance and Patient Outcomes: An Updated Synthesis of Systematic Reviews.” Journal of Continuing Education in the Health Professions 35, no. 2 (2015): 131-138.
2 Cook, David A., Chistopher R. Stephenson, John M. Wilkinson, Stephen Maloney, and Jonathan Foo. “Cost-ef -
fectiveness and Economic Benefit of Continuous Professional Development for Drug Prescribing: A Systematic Review.” JAMA Network Open (2022).
3 Decreases in patient readmissions were reported by ACCME-accredited providers who achieved Accreditation with Commendation in July 2021-March 2022.
4 Griebenow, Reinhard, Henrik Hermann, Michael Smith, Mohamed Bassiony, Arcadi Gual, Philip K. Li, Essam Elsayed, Robert D. Schaefer, Siham A. Sinani, and Graham T. McMahon. “Continuing Education As a Contributor to Mitigating Physician Burnout.” Journal of CME 12, no. 1 (2023).
5 McMahon, Graham T. “The Leadership Case for Investing in Continuing Professional Development.” Academic Medicine 92,no. 8 (2017): 1075-1077.
6 National Academy of Medicine. “National Plan for Health Workforce Well-Being.” The National Academies Press (2022): 64.
These cutting-edge seminars are offered as live events and as a web-based enduring material.








Scott A. Humphreys, MD, Medical Director, Colorado Physician Health Program
I have interviewed thousands of physicians over decades; everyone was foundationally affected by how their life was shaped during medical training. It’s a period marked by immense growth, but also profound challenges. These years can set the tone for your career—not only in how you practice medicine but in how you live your life.
The habits you establish early will follow you for the rest of your professional journey. This is both an opportunity and a warning. Prioritizing your wellbeing is not just beneficial, it is essential. Your ability to care for patients effectively and safely hinges on your own mental, emotional, and physical health.
Medical trainees across the United States (and Colorado), are facing significant mental health challenges. Studies consistently show high rates of depression, anxiety, and burnout among medical students and residents. For example, a 2016 meta-analysis published in JAMA reported that 27 percent of medical students globally experience depression, and 11 percent experience suicidal ideation. Closer to home, surveys of Colorado residents echo these struggles.
Unfortunately, the medical culture has often perpetuated a “grin and bear it” mentality, discouraging help-seeking. Yet, there’s no heroism in suffering silently. Physician wellbeing is directly linked to patient outcomes, with studies indicating that burnout can lead to increased medical errors. Taking care of yourself is taking care of your patients.

Here are a few principles I hope will guide you:
1. Establish sustainable habits early Learning restorative patterns for good sleep hygiene, regular exercise, and balanced nutrition during your training years will pay dividends throughout your career. Although the number of hours demanded of you as a physician may decrease after training, there are more responsibilities that add complexity: administrative responsibilities, personal financial obligations, building our families and communities, etc.
2. Prioritize connection
Medicine can be isolating, but it doesn’t have to be. Foster relationships with your peers, mentors, and loved ones. Talking openly about your challenges can help normalize your experiences and ease the burden.
3. Practice self-compassion
You will make mistakes — that’s inevitable. Learn from them, but don’t let them define you. Remind yourself that you are in a process of growth, and perfection is neither realistic nor expected.
4. Seek support early
If you’re struggling with depression, anxiety, or other concerns, reaching out for professional help is a sign of strength. The Colorado Physician Health Program (CPHP) exists to provide confidential support for physicians, physician assistants and trainees.
LOOKING AHEAD: As I look back on my career, I realize that the most rewarding moments are best appreciated during the times I have found balance—allowing myself to be fully present for both my patients and my family.
TO THOSE IN TRAINING, REMEMBER: medicine is our identity and a life-long commitment. Take care of yourself so that you can enjoy the incredible journey ahead. Your wellbeing is not a luxury; it is the foundation upon which great patient care is built. ■




Isabella Narváez Montesdeoca


Isabella Narváez Montesdeoca is a fourth-year student at the University of Colorado School of Medicine. She was born in Cali, Colombia and moved to Connecticut with her family at the age of 16. She went on to pursue her undergraduate degree at Wellesley College in Massachusetts where she studied Biology and Psychology while competing as a Division III athlete in track and field. Isabella worked in Clinical Research for four years after graduation during which she cemented her love for medicine, education and health equity. She is now pursuing a career in OBGYN, where she hopes to use her medical and surgical skills to serve a diverse population. Above all, she is a proud wife and mother to a loving Aussiedoodle.
Right outside O.R. 1, a man is dressed in a white surgical suit, a mask and a hair cover. He is nervously waiting, the weight of his hopes and fears held in a silent pause. What is happening beyond those white, heavy double doors that I am not allowed to see yet? Then, a nurse in green scrubs opens the door, beckoning him in. “You can sit by your wife’s head and keep her company,” she says softly. A blue curtain is obscuring his view, but he can see her face. Her eyes are filled with love and a tint of fear. He strokes her hair gently and kisses her forehead as they eagerly await the birth of their child together.
On the other side of the curtain, the OBGYN team works in calm concentration, their requests for instruments rising above the silence. His anxiety swells, but he knows that this is necessary to welcoming their child safely. Finally, he hears the doctor announce that their baby has arrived. Tears fall as he leans close to his wife in adoration. He hears his son cry for the first time—his heart bursts with love.
A pediatric nurse places their newborn son in his arms, a tiny bundle wrapped in a white blanket with blue and pink footprints. The baby’s sweet cry makes his vulnerability palpable. The man holds the baby near his wife’s head, all their bodies connected in space for the first time. This is one of the most precious and pure
moments of his life. Suddenly, the world narrows to just the three of them. Nothing else matters now.
Days later, they leave the hospital, tired yet elated to know that they are bringing a healthy boy home. He is unprepared for the ways his life is about to change. In that moment, though, he is filled with gratitude for every moment they will share as a family.
Right outside O.R. 2, a man is dressed in a white surgical suit, a mask and a hair cover. He is nervously waiting, the weight of his hopes and fears lingering in a silence far heavier than words. He wonders what lies beyond those white doors that seem so impenetrable. Finally, a nurse in green scrubs invites him in. “You can sit by your wife’s head and keep her company,” she says softly. The room is eerily silent aside from the quiet shuffle of feet in blue shoe covers. The surgical tables are covered with sterile drapes to both hide and protect the instruments that will soon be used to honor his wife’s final gift. The rigidity in the air makes the room feel colder. It had been a long week of hard decisions and drastic changes to his reality.
Sitting on a black stool by her head, he strokes her hair gently and kisses her forehead. Once so vibrant, the love of his life now lies very still, the machine no longer
breathing for her. The team is watching the monitor closely waiting for her heart to stop beating. “She should still not be feeling any pain,” the nurse mentions. We all suspect that she has not felt any pain during her hospitalization given that her brain was already herniating on arrival. Regardless, the ICU nurse continues to give her morphine pushes to protect whatever humanity she has left.
For 24 minutes, he leans close, resting his forehead against hers. The tears have run dry, yet a silent question lingers in him—why? He still can’t understand how anyone could die of asthma. Who gave her COVID? What if she hadn’t taken her methadone that morning? She would’ve been in pain, but maybe she would still be alive. None of those stipulations have brought him comfort this week, and yet they continue to cycle through his head. Maybe my CPR was not good enough. As her body gets colder, the air feels thicker passing through his airway. He wishes he could give it all to her.
The nurse informs him that her heart has stopped beating. He knows it is time to leave her. Struggling to block the images of her organs being removed one by one, he rises and feels a hollowness in his body. He is unprepared for the ways his life is about to change. The excruciating pain he feels in every part of his being makes him feel that life will be completely impossible to navigate without her.
These two stories were inspired by my experiences in the operating room as a second- and third-year medical student. I distinctly remember the second patient, who was a donor after circulatory death (DCD). She had arrived at the hospital after cardiac arrest secondary to acute respiratory failure. She was given CPR for 38 minutes and her brain was already herniating from anoxic injury on arrival. After a long week of waiting and painful conversations, the family had decided to let her go and fulfill her wish of becoming an organ donor. I remember the conflicting feelings I had that day. The heaviness in my heart was complicated by the excitement of learning about a new surgical procedure and the knowledge that other people around the country were eagerly waiting for a new organ. I feel very grateful to have been part of this patient’s medical team and will remember her story forever.
I was most shocked by the juxtaposition of “Mark’s” experience compared to the common participation of partners like “Joe” during a C-section, both beginning with them walking into the O.R. dressed in the same outfit. At first glance, the scenarios seemed superficially similar, yet the circumstances and outcomes were drastically different. One highlights the arrival of life and the other the departure, each a powerful moment shaped by love, vulnerability and the intensity of change. As a future OBGYN, I will use these contrasting scenarios to remind myself that every patient encounter is unique. My role is to approach each and every one with humility and dignity. ■
Reflective writing is an important component of the University of Colorado School of Medicine curriculum. Beginning in the first semester, medical students write essays, stories or poetry that reflect what they have seen, heard and felt. The Reflections column was co-founded by Steven Lowenstein, MD, MPH, and Tess Jones, PhD. It is now co-edited by Dr. Lowenstein and Kathryn Rhine, PhD. It is dedicated to the memory of Henry Claman, MD, Distinguished Immunologist and Professor at the University of Colorado, and founder of the Arts and Humanities in Healthcare Program.





Owned and operated by the Colorado Medical Society, and backed by history of physician ownership, MTC is uniquely focused on the needs of its clients. Serving medical professionals is all we do.
MTC’s management team has over 50 years of combined experience in medical answering services. Our operators are professional, friendly, and expertly trained to handle any client situation. We offer a full range of customizable services to ensure your patients enjoy personal, timely communication while you stay on top of your busy schedule.
MTC is committed to providing the highest level of customer service. MTC is a member of the Association of TeleServices Int’l (ASTI) and a proud recipient of the prestigious ASTI Award of Excellence for service quality. MTC continually upgrades its technology and our servers and your data are kept in a secured state-of-the art data center with redundant internet and power supply.





Madison Crew
Critical reflective writing holds a prominent place in the Medical Humanities curriculum at Rocky Vista University. Students engage in critical reflection to explore their own assumptions and biases and to understand how their values impact their practice and professional identity. This submission is selected and edited by Nicole Michels, PhD, Chair of the Department of Medical Humanities, Alexis Horst, MA, Writing Center Manager, and Hope Ruskaup, MFA, Writing Center Coordinator.

Madison Crew is originally from Stephenville, Texas, and earned her bachelor’s degree in biomedical science from Tarleton State University before pursuing a master’s degree in medical science from the University of North Texas Health Science Center. She is currently a second-year medical student at Rocky Vista University in the global medicine track with an interest in pursuing a surgical specialty. Her interest in global medicine was piqued during a trip as a premedical student to Mombasa, Kenya, where the following story took place. Outside of medicine she enjoys crocheting, knitting, and reading.

I was looking out the hospital window at the bluest of skies as I began taking a patient’s blood pressure, and I could not help but think about how lucky I was to be in Mombasa, Kenya. There was a nurse’s strike at the public hospital, so I was filling in that particular duty: patient intake, maintaining patients in the wards, assisting physicians with procedures, etc. It was a hot day, as it usually is in Mombasa, but – my thoughts were interrupted by a woman crashing through the waiting room, crying out for someone to help her baby. I lunged forward, instinct taking over, and immediately began triaging the patient while his mother went to
the check-in desk to pay the consultation fee. I heard her wails the entire way.
I worked quickly to gather the patient’s vitals but stopped dead in my tracks when I read the pulse oximeter. Surely, I was doing something wrong. I repositioned it on his foot, then tried the other foot. My body went cold; it continued to read 55% on room air. My stomach turned as I called out, “I need help over here, please!” John, the only nurse on staff, ran to my side. After performing a quick assessment, he paged for a doctor and started the baby on oxygen. The decision was made to move the baby to a ward.
Since the hospital was short staffed, I asked to keep watch over him to ensure someone was with him if the worst was to occur. John gave me instructions for the patient’s oxygen and, with a worried look in his eye and a gentle touch to my shoulder, reminded me where he would be and to call for help “when” I needed it.
The patient’s mother and I sat vigil at his bedside all night, she on one side and I on the other. Throughout the night, the two of us began chatting and forming a relationship. Her son was four months old and had aspirated milk while feeding some time before this hospital visit. She


knew he was getting sicker, but they lived in a village several hours away from the hospital, which, unfortunately, was the closest facility to them, and she had to find a way to get him there. After some time and lots of asking, she finally gathered enough money from kind strangers to take a bus but feared she was too late. I did my best to keep her spirits up, but even with my minuscule medical knowledge, I knew his chances were slim. He was likely suffering from pneumonia from the milk in his lungs, which, if this occurred in a high-income country like the United States, would be much more survivable than in Kenya, a middle-income country. This is due to many factors, mainly the availability and accessibility of health care in Kenya. They lived in a small village without much of a health care system, according to the mother, and she had struggled to get him to a physician at all, thus both the availability and accessibility of health care had failed her and her son. Health care should not be a privilege that is granted just because someone is lucky enough to live in a better economy. This little boy deserves just as much of a chance to live as a 4-month-old in a different country.
As these thoughts were circling my mind in the early morning, I noted how strong his grip was on my finger, and it made me smile, even though he was, in no uncertain terms, deteriorating. It was not much later when I felt this strong grip loosen around my finger. After a moment of foggy confusion, I jumped to my feet and ripped my stethoscope from around my neck. I listened to his chest and checked for a pulse simultaneously. Nothing. His mother shrieked, “No. No. My baby!” As tears welled up in my eyes I told her, “I’m going to start pushing on his chest to try to start his heart again.” “Yes! Please! Do it!” She cried. I wrapped both my hands around his tiny chest and began rhythmically pressing my thumbs into his sternum. “Page John. Please!” I yelled down the hall, praying for someone, anyone to hear me.
When his time of death was called, I knew I had to control my emotions. It was not my time to feel his death. It was his mother’s time to grieve the loss of her son – her child, who was taken away from her entirely too young. But when I looked at her, she was not crying nor wailing. Instead, she slowly and steadily walked over to me, grabbed my hand, and said, “Are you okay, dear?”
I was completely and utterly shocked down to my very core. This poor woman had just lost her only child when he was just four months old, and here she was, holding my hand, asking how I was. With tears streaming down both our faces, I took her hand in both of mine and said, “I will remember you and your son and the kindness you have shown me for the rest of my life.”

Her selfless act of checking on me in her own time of need, the simple gesture of holding my hand and looking deep into my eyes – this is what humanistic medicine looks like. I think that, all too often, in our post-pandemic world, that aspect of health care delivery is lost. The knowledge we can learn from one another by holding another’s hand or by truly looking into someone’s eyes is vast and far outweighs what any verbal communication can relay. When this child’s mother put her hand in mine, I felt her grief. I could see it in her eyes. And through her grief, I felt her intense emotional strength and could feel what she was truly asking of me. She was asking me never to forget her child and this story of true and raw emotion – and I have kept that promise all these years later. ■
Few can contest physicians and healthcare providers when they say they’re busy. They truly are. They barely have seconds to scarf down vending machine chips for lunch, let alone transcribe their patients’ medical charts. By bringing Ditto Transcripts on board, time’s back on your side to juggle more administrative tasks and care for patients—the work that matters most to you. The way it should be.


• Experienced, U.S.-based medical transcriptionists skilled in EHR and EMR systems
• 99% accuracy for all transcription—guaranteed
• Access to speech recognition software editors
• Rapid turnaround and on time for fast access to medical records and reports 24/7
• Electronic file delivery in 24 hours or less
• Speech recognition software editing
• Secure, private, confidential and HIPAA compliant
• Adhere to AHDI/AAMT standards
• Unlimited customer support services
• No long-term contract required

• E-signature/digital signature available
When we say specific, we mean specific. We have deep medical transcription service expertise for cardiology, clinical, dermatology, emergency medicine, hematology/oncology, mental health, neurology, ophthalmology, orthopedic, pathology, podiatry, psychiatry, radiology, urology, among others.
Take us for a test drive. Enjoy 1,000 lines or 60 minutes free.
No credit card needed—this trial’s on us.
For pricing models and to learn more about our Free Trial, visit us at dittotranscripts.com




Gerald Zarlengo, MD, Chairman & CEO, Copic Insurance Company

Difficult patient encounters are something all medical providers may face and patient factors such as strong emotions, somatization, unrealistic expectations, and mental health issues commonly contribute to these. Additionally, we need to take into account environmental or situational factors such as busy patient schedules, multiple people in the exam room, language or literacy issues, and provider issues such as fatigue/burnout, anecdotal previous patient experiences, and defensiveness.
Although it may sound obvious, it is important to first recognize that you are perceiving an encounter as difficult. This may occur as early as seeing a patient name on your schedule or may not occur until you are in the middle of a visit. No matter when the sense of difficulty is recognized, it is important to reflect on why the patient and/or encounter is evoking your strong emotions.
Emotions are never wrong but can be detrimental to a provider-patient relationship depending upon how they are identified and managed. While a patient’s anger may be a frequently cited emotion in a difficult encounter, it is important to remember that anger is often the result of an underlying primary emotion such as fear or sadness.
Acknowledge emotions: Acknowledge the patient’s and your emotions. Don’t be afraid to call out an emotion, such as, “I can see you are angry.” If the patient corrects you and says, “No, I am not angry just frustrated,” take that as a positive as you have already begun to deescalate the situation. Let the patient know you are having challenges as well, “I am having difficulty
as I really want to help you, and I am frustrated we haven’t found a better solution for you.”
Reflective and active listening: Summarize what you are hearing from the patient, “I hear you saying you are frustrated as your pain has not improved and it is limiting you at your job.” Brief summary statements are an effective way of expressing empathy. Pay attention to your body language as nonverbal communication contributes more to interaction than the words you say—stay calm, lean in, and pay attention.
It’s okay to say I am sorry: While sorry statements are not necessarily a form of empathy, it may be appropriate to say things as, “I am sorry I kept you waiting so long,” and then follow it with an empathic statement, “I know you must be very frustrated.”
This is a partnership: You may discover that in your exploration that the patient has unrealistic expectations (i.e., “I want to be pain free.”) and you can work toward an agreement to work together on a reasonable goal. “I want to be transparent—I may not be able to relieve all of your pain, but we can work together to improve your symptoms such that you can return to work and enjoy your life outside of work.”
Recognize it will take time: Building a relationship and/or behavior modification takes time. Set reasonable goals on what may be accomplished in one visit.
Communication skills require practice: Remember that we all have differing skills and patient communication is a clinical skill that is devel -

oped with practice. There are plenty of wonderful workshops on communications skills. We encourage you to take an opportunity to be videotaped as it is a powerful way to understand nonverbal skills in particular.
When all else fails, take the appropriate steps: Despite your best efforts, not all relationships may be salvageable. You are never required to maintain a relationship that is potentially dangerous or abusive to you or your staff. You can set limits on patient behavior that is particularly disruptive. Remember there are important guidelines to follow when terminating a relationship. You should never terminate a relationship based on characteristics that may be considered discriminatory such as gender, race, ethnicity, age, or disability. Draft a termination letter that is succinct but spells out that you will provide emergency care and non-controlled refills for 30 days. Suggest resources for identifying a new provider and assure them that all records will be transferred. Avoid restating your side of the story in the letter and make sure your staff knows your plans. Finally, send the letter via certified mail.
The information provided herein does not, and is not intended to, constitute legal, medical, or other professional advice; instead, this information is for general informational purposes only. The specifics of each state’s laws and the specifics of each circumstance may impact its accuracy and applicability; therefore, the information should not be relied upon for medical, legal, or financial decisions and you should consult an appropriate professional for specific advice that pertains to your situation. ■
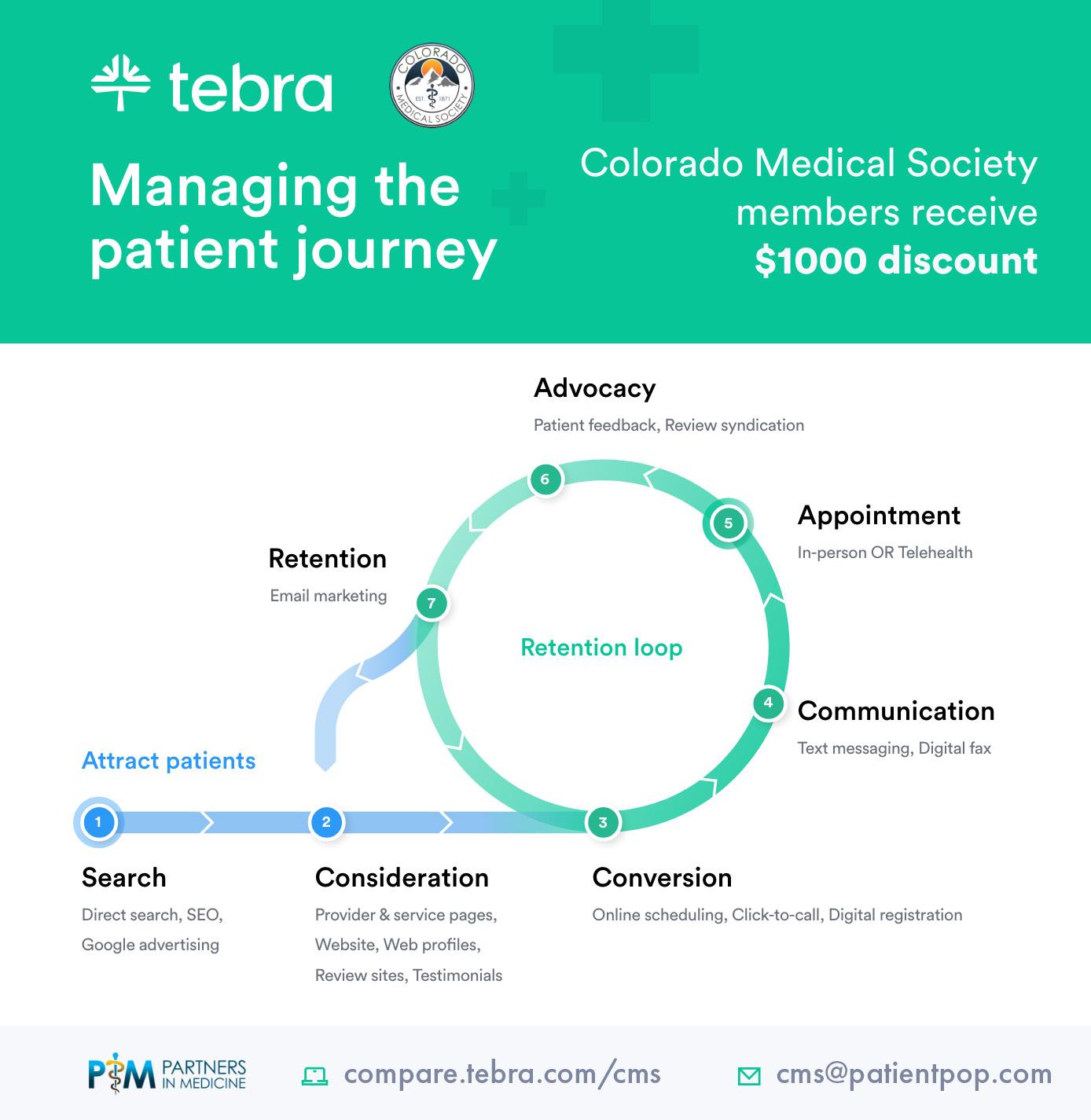
Noah Goldman, Founder and CEO, Clyck


Running your practice is already a fulltime job. Between patient care, administrative duties, and staying on top of industry changes, who has time to figure out marketing? But here’s the thing: patients today expect more than great care. They’re looking for convenient, digital-first experiences—and if they can’t find you online, they’ll choose someone else. That’s where we come in.
At Clyck, we make marketing simple so you can focus on what you do best: caring for your patients. Whether it’s attracting new patients, building trust, or growing your practice, we’re here to help every step of the way.
If you’ve ever wondered why it seems so hard to stand out, you’re not alone. Colorado physicians face some tough challenges:
• COMPETING ONLINE: Big health systems dominate search rankings, making it hard for smaller practices to get noticed. Without visibility, even the most qualified providers can struggle to attract new patients.
• MANAGING REVIEWS: A few negative reviews can feel like a gut punch, especially if you’re not sure how to handle them. It’s not just about fixing mistakes—it’s about highlighting the great work you’re already doing.
• KEEPING PATIENTS ENGAGED: Patients expect more these days—like online scheduling, timely communication, and social media updates. Practices without these tools can seem outdated, even if their care is exceptional.
• JUGGLING PRIORITIES: With so much on your plate, finding time to focus on marketing might feel impossible. It’s easy for your efforts to feel scattered or ineffective without a clear plan.
Sound familiar? The good news is these challenges are easier to overcome than you might think.
We know every practice is different, so we create marketing strategies that fit your unique goals. Here’s how we make it easy:
Your website is more than just a digital business card. It’s your first chance to make a great impression. We’ll make sure it’s professional, easy to navigate, and shows up where your patients are searching. Plus, features like online scheduling make it simple for patients to book with you.
Staying connected with your patients doesn’t have to be a hassle. We’ll help you share helpful tips, updates, and reminders through social media and email campaigns. Whether it’s a flu shot reminder or a post about healthy living, you’ll stay top-of-mind.
Let’s face it: reviews matter. We’ll help you encourage happy patients to leave
Let’s face it: reviews matter. We’ll help you encourage happy patients to leave glowing feedback.
glowing feedback and show you how to respond to reviews in a way that builds trust. Think of it as turning every review into an opportunity to shine.
Marketing shouldn’t feel like guesswork. We’ll track what’s working—from website visits to new patient inquiries—so you know exactly how your investment is paying off.
As a Colorado Medical Society (CMS) Partner in Medicine, we’re dedicated to helping physicians across the state succeed. Through this partnership, CMS members get access to exclusive consultations, resources, and personalized marketing solutions designed just for you.
You don’t have to tackle marketing alone. With Clyck, you’ll have a trusted partner who’s just as committed to your success as you are. Ready to attract more patients, enhance your reputation, and grow your practice? Let’s get started.
Contact us today to schedule your consultation and see how we can help your practice thrive. www.clyckdigital.com ■

Rebecca Kornas, MD, FACEP,
and Cody Belzley
While most of the world has seemed to move on from the COVID crisis, Colorado’s health care safety net is still reeling from its impacts. We’re counting on Colorado’s lawmakers to chart a path forward to stabilize and secure the coverage programs and help providers who serve Colorado’s most vulnerable residents, before irreparable damage is done.
COVID impacted supply chains and labor markets, driving up costs in health care significantly. Colorado’s poor management of the “Medicaid unwind” compounded the challenge. More than half a million Coloradans, most of whom are low income and/or face other health or economic barriers, found themselves uninsured and led to increased uncompensated care across the board in our state. Taken together the financial strain has been crushing for hospitals, Federally Qualified Health Centers, community safety net clinics, comprehensive behavioral health providers and specialty behavioral health

clinics, and school-based health centers. (More detail in the cover story of this issue.) I’m guessing many of you are seeing this in your practices.
My emergency room physician colleagues and I are seeing it in our departments. As a physician at AdventHealth Avista, my team has worked closely with the clinicians at Clinica Family Health and Wellness over the years. For more than 40 years, Clinica has existed as a medical and dental care provider for low-income and underserved patients in the Boulder, Broomfield, Gilpin and West Adams counties. Over the past two years as the unwind has unfolded, community members who would typically go to Clinica for their care have been getting shuttled away from the high quality, preventive medical care previously provided by their primary care clinic teams to the only safety net that remains for them, the emergency department.
In the emergency department, we are bound by the federal Emergency Medical Treatment and Labor Act (EMTALA)

to see any patient, regardless of their ability to pay, with any complaint, day or night, 365 days a year, 24 hours a day. Emergency department teams also provide high-quality care, but in a more stochastic and disruptive manner than the wholistic approach that a well-functioning primary care clinic can. Data from the Colorado Hospital Association bears it out. Hospital emergency departments (EDs) are seeing 50 percent more uninsured patients than before or during the pandemic – over 18,000 more uninsured patients are visiting the ED every quarter. We cannot sustain this trend.
Historically, Colorado lawmakers have made investing in the health care safety net a priority because they know it is important to the health of individual Coloradans and the vitality of Colorado communities. As a state, we created a Medicaid disability buy-in program to allow Coloradans living with disabilities to be able to access the benefits of Medicaid without having to quit work and impoverish themselves to do it. We opted in to the Affordable Care Act (ACA) Medicaid expansion and cut our uninsured rate in half. We funded primary care clinics and hospitals to preserve and protect access to care in all corners of Colorado. Together, we have made incredible progress in Colorado over the last 20 years.
But that progress we’ve made and the infrastructure we’ve built are now at risk. Hospitals are announcing service line closures, clinics are closing sites, physician groups are taking furloughs and Coloradans are struggling to find coverage they can afford.
We need Colorado’s lawmakers to take bold action this year to stabilize the health care safety net providers and ensure a Medicaid eligibility and enrollment system that will allow Coloradans to get and keep coverage. The budget is tight, and we cannot solve our challenges in one state budget cycle, but we must make a meaningful downpayment on the solution this year and commit to continually work together in the years to come to strengthen what was lost after COVID. There is no more important or more urgent priority than protecting the health of the people of Colorado. ■

The Touchstone Advantage delivers CONFIDE NCE for the medical insights you need, and CONVE NIE NCE that matters for you and your patients, while giving patients COST- E FFEC TIVE alternatives to save them time and money.


• Diagnostic imaging at up to 60% less than hospital imaging
• In-network with 99% of healt h insu ra nce pla ns in Colorado
• Fast prior authorizations assistance for easy sched uling
• sa m e d ay/nex t d ay a ppoint m ents with extended and weekend hours
• su bspecialized radiologists available for consultation
• Prompt standard repor ts delivered within hou rs
• Obtain repor ts quickly through easy- to - access physicia n por tal
• 97% patient satisfac tion rate
Refer your patients to our 11 convenient locations t hroughout met ro Denver
