

Flu Prevention 101:
Tips for Older Adults
Do you stock up on tissues and cough drops at the first sign of a chill in the air? Are you bracing for that first telltale sniffle of the season?
In winter, getting sick might seem inevitable. However, while we can’t completely avoid seasonal germs, we can take steps to avoid a flu infection. This is especially important as we get older, when our immune system isn’t as robust as it used to be—and serious illness and complications from the flu are more likely.
See FLU on page 6.

It all adds up. Every dollar, hour, or effort you give strengthens our mission. We hope you’ll help us continue making a lasting difference, one act of kindness at a time.
Support our mission at MySourcePoint.org/give
Staying Motivated to Exercise ...and more!



WINTER CONTENT
SourcePoint is a nonprofit 501(c)(3) organization that provides professional expertise, services, and programs for Delaware County adults who want to thrive after 55, as well as family caregivers. Services and programs are supported by the local senior services levy, private and corporate donations, grants, and the Central Ohio Area Agency on Aging.
2025 Board of Directors
President: Pamela Foster, Orange Township
Vice President: Cheri Thompson, Delaware
Secretary: Annie Horstman, MD, Delaware
Treasurer: Dennis Mowrey, Delaware
Randy Bournique, Delaware
Bill Brown, Delaware
Adrienne Corbett, Delaware
Todd Everingham, MBA, Dublin
Ron Fantozzi, Columbus
Beth Fligner, JD, Dublin
Alice Frazier, MD, Delaware
Liz Gitter, MSSW, Delaware
Wren Kruse, JD, New Albany
Beth Long-Higgins, MDiv, Delaware
Michael Tucker, JD, Delaware
Roger Van Sickle, Delaware
Jodie Wegmiller, BSN, MBA, Delaware
The board typically meets the last Wednesday at noon for six months out of the year. Members of the public who wish to attend may call the chief executive officer at 740-363-6677.
My Communicator is published quarterly and is made possible through advertisers, donors, and volunteers. About 5,000 copies of each edition are printed and distributed throughout Delaware County. My Communicator is available for pick-up at SourcePoint and 50 other locations, such as libraries, senior living communities, health care facilities, and other nonprofit organizations. To find a nearby pickup site, contact SourcePoint at 740-363-6677. Read My Communicator online at MySourcePoint.org/publications
To advertise or submit
content for
Chief Advancement Officer Alison
The appearance of advertising does not represent an endorsement by SourcePoint. We reserve the right to refuse any
IN OUR COMMUNITY
SourcePoint Welcomes Two New Board Members
SourcePoint announces the appointment of two new members to its board of directors, as well as the full slate of officers and board members for 2025. Joining the board of directors are Todd Everingham and Beth Long-Higgins.
Todd Everingham is a financial advisor for First Citizens National Bank. A Dublin resident and U.S. Army veteran, Everingham is an active member of the Delaware Area Chamber of Commerce and the Delaware Rotary. He earned a bachelor’s degree in family resource management from The Ohio State University and an MBA from Ohio Dominican University.
Beth Long-Higgins, a Delaware resident, is the vice president for engagement at United Church Homes. She holds a bachelor’s degree in psychology and music from Heidelberg University and a Master of Divinity degree from the United Theological Seminary of the Twin Cities. Long-Higgins has extensive volunteer experience, including serving as a member on the Ageism and Culture Advisory Council of the American Society on Aging and as a trained facilitator with the National Center to Reframe Aging with the Gerontological Society of America.
The full 2025 board includes 17 individuals: President Pamela Foster, Vice President Cheri Thompson, Secretary Annie Horstman, Treasurer Dennis Mowrey, Past President Alice Frazier, Sustaining Director Roger Van Sickle, Randy Bournique, William
SPEAKERS BUREAU


SourcePoint’s board of directors is responsible for establishing the mission and ensuring that the organization continues to fulfill that mission with legal and ethical integrity. The board determines the strategic direction and provides financial oversight of the nonprofit organization. The board employs a chief executive officer to supervise staff, implement policy, and oversee day-to-day operations.
SourcePoint, the comprehensive aging services provider in Delaware County, provides free presentations to community groups and employers. Our aging experts are available for in-person or virtual events and can customize presentations based on your needs.

Brown, Adrienne Corbett, Todd Everingham, Ron Fantozzi, Beth Fligner, Liz Gitter, Wren Kruse, Beth Long-Higgins, Michael Tucker, and Jodie Wegmiller.
HEALTH & WELLNESS
Halting Heart Attack and Stroke
A heart attack or stroke can happen within seconds. Getting treatment fast for these medical emergencies can mean the difference between life and death or disability. But do you know the symptoms of these dangerous events? And do you know if you’re at risk for having one?

More than 1.5 million people have a heart attack or stroke every year in the U.S. Heart attack happens when blood flow to the heart gets blocked, most commonly by a blood clot. Stroke happens when blood flow to the brain gets disrupted. The most common type of stroke is caused by a blood clot stuck in a blood vessel that feeds the brain. Stroke can also be caused by a blood vessel in the brain that breaks open and bleeds into nearby tissue.
“Early treatment is key to improving your chances of survival,” says Dr. Gina Wei, a heart-health expert at NIH. Treatment may include either rapidly dissolving or removing the clot to open up the blocked blood vessel. For some heart attack cases, emergency surgery is used to redirect blood flow around the blockage.
Getting help immediately can save a life and reduce damage to the heart or brain. Less damage to these vital organs can also mean less disability afterward, and a faster recovery, explains Dr. Clinton Wright, a neurologist and stroke researcher at NIH. So it’s important to be on alert for symptoms of a heart attack or stroke for both yourself and the people around you. Every minute matters.
Know the Symptoms, Act Fast
The most common symptoms of a heart attack are pain, heaviness, or discomfort in the center or left side of your chest. But they’re not the only symptoms. Women are more likely than men to have other symptoms, like pain or numbness in the left arm.
Some people may also feel a rapid or irregular heartbeat. Others feel pain or discomfort in one or both arms, the back, shoulders, neck, jaw, or above the belly button. You may also feel short of breath or suddenly sweat a lot for no apparent reason. Rarer symptoms include feeling extremely tired for no reason, nausea and vomiting, and dizziness.
For stroke, the most common symptoms are facial drooping, arm weakness, and trouble speaking. “There can also be a sudden loss of balance or coordination, or sudden trouble seeing in one or both eyes,” Wright says.
If you or anyone around you has these symptoms, call 9-1-1 immediately. Don’t wait. Treatment can start in an ambulance on the way to the hospital. This helps improve the odds of survival and recovery. Don’t drive yourself to the ER or ask someone to drive you. It may delay treatment.
Other health conditions can mimic symptoms of a heart attack and stroke. “But it’s better to be safe than sorry,” Wei says. “Call an ambulance to go to the ER and get checked out.”
Are You At Risk?
Most heart attacks and strokes happen in people who have certain risk factors. If you know your risk, you can be on the lookout for symptoms. You can also take steps to lower that risk.
One major risk factor for heart attack is high cholesterol in the blood. High cholesterol can also increase the risk for stroke. Cholesterol can build up on the walls of blood vessels, causing plaques. If a plaque breaks open, a blood clot can form. But cholesterol isn’t the only contributor to this process.
Dr. Paul Ridker from Harvard University is working to understand the role of inflammation in heart disease. His research has shown that high cholesterol and inflammation work together to increase heart-attack risk. “Heart disease involves both accumulation of cholesterol and an inflammatory fire lighting the match underneath it all,” he says.
In a recent study, his team measured inflammation using a test called hsCRP, as well as blood cholesterol, in women in their 30s. Women with high levels of inflammation had a higher risk of heart attack or stroke later in life than those who only had high cholesterol.
“Get these things measured,” Ridker advises. Knowing your numbers “can give you an opportunity to start prevention much earlier in life,” he says.
Hypertension, or high blood pressure, is another important risk factor for stroke and heart attack. High blood pressure has no symptoms. So you may not know you have it.
You can check your blood pressure at home with automatic cuff monitors. These are available at all major pharmacies. Measuring your blood pressure at home if you have hypertension and getting your cholesterol checked by your doctor regularly can help you assess your health risk. Your doctor can advise you on how to lower your risk based on your blood pressure and cholesterol numbers.
Lower Your Risk
If you’re at risk for a heart attack or stroke, lifestyle changes and medications can help you lower that risk.
“Eating more vegetables and less red meat, exercising, and quitting smoking all lower heart attack and stroke risk,” Ridker says. “And it turns out they all reduce inflammation as well.”
Other steps you can take to reduce your
maintaining a healthy weight, getting enough sleep, and managing stress.
“It’s never too early to start making healthy changes,” says Wei. “It’s easy to feel overwhelmed. You can start with small steps. Like taking the stairs instead of an elevator or parking your car a little farther away when you go shopping. Or adding one fruit or vegetable to your day. Then work your way up gradually.”
Sometimes, lifestyle changes alone aren’t enough to reduce your risk. Medications can also help.
Drugs called statins can help lower cholesterol levels. The U.S. Food and Drug Administration recently approved the first drug to lower inflammation in adults at very high risk of a heart attack or stroke. It’s called low-dose colchicine.
Drugs that lower blood pressure can also
naturally goes up,” Wright says. So it’s important to make sure to manage your blood pressure as you age.
A large NIH-funded study showed that using more than one medication to reduce blood pressure substantially reduced the number of strokes in people at high risk who couldn’t get their blood pressure low enough with only a single drug. “And we’ve continued to gain more evidence that the lower your blood pressure, the better,” Wright says.
“We all have the power to protect our hearts and lower our risk for heart disease and stroke,” Wei explains.
Source: National Institutes of Health. Read more at newsinhealth.nih.gov.






From page 1
How can older adults prevent the flu?
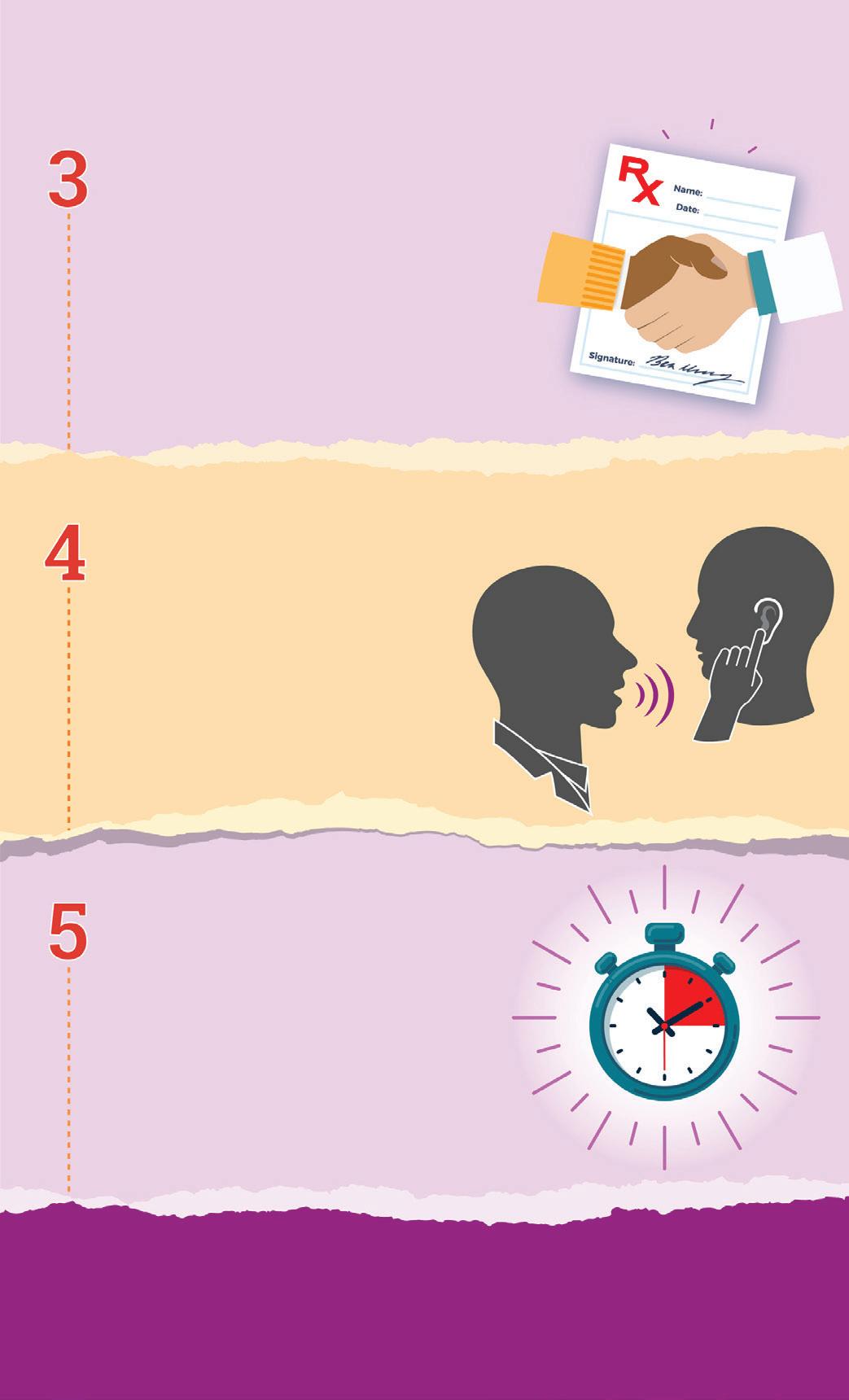
Below are seven simple-yet-effective flu prevention tips tailored for older adults.
1. GET VACCINATED
The best way to prevent the flu is to stay up to date with your flu vaccine. The Centers for Disease Control and Prevention (CDC) recommends everyone age 6 months and older receive a flu shot annually, but it’s especially critical for older adults. “People age 65 and older should opt for high-dose flu vaccines or adjuvanted flu vaccines, which are specifically designed to boost the immune response in older adults,” said Kathleen Cameron, Senior Director of NCOA’s Center for Healthy Aging.
You can get your flu shot from your doctor, pharmacy, or community health clinic (visit Vaccines.gov to find a site near you).
Pro tip: Get your flu shot early in the flu season, ideally by the end of October. But later is ok, too—the flu season can last into May.
2. PRACTICE GOOD HYGIENE
The flu virus spreads through respiratory droplets when an infected person coughs, sneezes, or talks. You can also catch the flu by touching contaminated surfaces and then touching your face. Someone who has the flu can spread the virus to others for about one day before they start experiencing symptoms and up to five days after getting sick.
Practicing basic good hygiene can significantly lower your risk of getting the flu (and infecting others when you’re sick):
Wash your hands frequently with soap and water for at least 20 seconds—especially after being in public places, touching shared surfaces, and before preparing and eating food. No soap or water available? Use a hand sanitizer that contains at least 60% alcohol.
Avoid touching your face, particularly your eyes, nose, and mouth, as these are key entry points for the influenza virus.
Cover your coughs and sneezes with a tissue or your elbow. Throw used tissues away immediately.
Disinfect high-touch surfaces like doorknobs, light switches, computer keyboards and mouses, remote controls, and cell
phones regularly. The flu virus can live on different surfaces for up to 48 hours.
Improve air quality by opening up the windows in your house (if the weather allows) and/or using a high-efficiency particulate air (HEPA) filter at home and at work.
3. PRIORITIZE GOOD NUTRITION AND HYDRATION
Older age, chronic disease, environmental toxins, and other factors can weaken our immune system. Good nutrition can help counteract some of these effects by priming our body to fight off infection:
Eat nutrient-dense foods like whole grains and colorful whole fruits and vegetables—especially citrus fruits, leafy greens, and bell peppers, which are rich in vitamin C (a natural immune booster).
Incorporate lean proteins like chicken, fish, eggs, and beans. Protein plays an important role in the building of antibodies, which help us ward off viruses and prevent infection.
Limit your intake of ultra-processed foods (e.g., potato chips, frozen dinners, prepackaged snacks, fried foods), which have been found to negatively impact the immune system.
Focus on whole, natural foods instead with no or limited processing and additives.
Take vitamin and mineral supplements to address any nutrient deficiencies (e.g., vitamin D) if your health care provider has instructed you to do so.
Stay hydrated by drinking plenty of water throughout the day to keep your body functioning optimally. Herbal teas and broths can also help keep you warm and hydrated during colder months.
Avoid tobacco use of any kind and limit your alcohol consumption.
4. GET PLENTY OF SLEEP
Sleep is crucial for a healthy immune system, but many older adults struggle with getting enough rest. To power up
your slumber:
Aim for 7 to 9 hours of quality sleep each night.
Create a consistent sleep schedule by going to bed and waking up at the same time every day. A set routine helps to support your body’s natural sleep rhythms.
Establish a soothing bedtime routine to help you wind down from the day, such as reading, meditating, journaling, or listening to soothing music.
Limit daytime naps—these small snoozes, especially later in the day, can deplete your “sleep drive” and make it difficult to fall sleep at bedtime.
Avoid screens for at least 60 minutes before bed. The blue light produced by TVs, smartphones, tablets, and computers can interfere with your natural sleep cycle.
Do not consume caffeine, nicotine, or alcohol too close to bedtime. These substances can all wreak havoc with sleep, either making it difficult to fall asleep or causing you to wake up and not be able to fall back asleep.
If sleep problems persist despite your best efforts, talk to your doctor for help in creating a plan of action.
5. STAY PHYSICALLY ACTIVE
Regular exercise not only keeps your body fit, it also enhances your immune system. A recent study found that exercising at moderate intensity for 15 minutes may help boost immunity by increasing levels of natural killer (NK) cells. These cells help our body destroy harmful pathogens, even if we’ve never been exposed to them before. Physical activity can also help flush bacteria out of your lungs and airways, reducing your odds of becoming ill.
To add more healthy movement to your life:
Aim for 20 to 30 minutes of moderate exercise most days of the week—such as walking, swimming, golfing, or bicycling. Your local senior center likely offers group classes that add an element of fun and socialization to staying fit!
If you’re new to exercise or have mobility limitations, lowimpact activities like stretching or chair exercises can still provide benefits.
6. AVOID CLOSE CONTACT WITH PEOPLE WHO ARE SICK
Since the flu is highly contagious, avoiding exposure to those who are already sick is another key strategy for preventing the flu. If you know someone has the flu (or flu-like symptoms), maintain a safe distance:
Encourage friends and family members who are sick to stay home and fully recover before visiting.
If you must be around someone who is ill, wear a mask and take extra hygiene precautions. This also applies to visiting your doctor’s office where infected people may be present.
Avoid crowded indoor public spaces. If you must be in a crowded setting, wear a well-fitting mask.
And of course, if you’re ill, stay home and avoid contact with others until you’re feeling much better.
7. MANAGE STRESS AND MOODS AS MUCH AS POSSIBLE
It’s no secret that stress and poor health go hand in hand. Chronic stress can compromise our immune system functioning and make us more vulnerable to illnesses like the flu. To keep your immune system working the way it should, make it a point to manage your stress from day to day:
Practice mindfulness techniques like deep breathing, meditation, and positive visualization. This can help combat the physical effects of stress (e.g., rapid heart rate and tense muscles).
Stay connected with friends and family for emotional support and take part in hobbies or activities that bring you joy and relaxation.
Prioritize your physical well-being by getting enough sleep, eating well, and exercising most days of the week.
Avoid social media, the news, and other things that might trigger your stress.
If you are feeling overly anxious or are experiencing symptoms of depression, seek help from your primary care doctor or a mental health provider.
IF YOU’RE FEELING UNWELL, CONTACT YOUR DOCTOR. Should you start experiencing flu symptoms—such as fever, chills, body aches, or fatigue—contact your health care provider right away. CDC recommends prompt antiviral treatment for high-risk people who have flu (or suspected flu), such as those 65 years and older. Early treatment with antiviral medications can reduce the severity of your symptoms, shorten the duration of your illness, and prevent serious complications that can land you in the hospital.
Preventing the flu as an older adult requires a combination of proactive measures, from eating healthy to getting vaccinated. By taking charge of your health, you can improve your odds of enjoying a safe, flu-free season.
Source: National Council on Aging. Read more at ncoa.org.
Play
From page 1
You may be aware that staying active is essential for maintaining your physical health, but did you know it also improves brain function and emotional well-being?
Another benefit: If your family and friends join in your physical activity routine, you can:
• Enhance your social connectedness
• Strengthen bonds with loved ones
• Encourage healthy behaviors
• Playing recreational sports
• Engaging in imaginative play
These intergenerational interactions can amplify the play experience by bringing in novel perspectives and broadening collective knowledge and skill sets. In intergenerational play, there are no right or wrong answers. Everyone involved can reap the physical, emotional, social, and intellectual payoffs of being both a teacher and a learner.

We are hardwired to seek out playful opportunities to have fun with others through physical movement and expression, with the feel-good neurotransmitters endorphin and dopamine being released through activities that combine physical and social elements. Bringing the children, teens, or young adults in your life into play and physical activities provides bonus benefits for everyone.
No matter your current fitness level, increasing your movement and activity engagement through intentional intergenerational play—such as recreational sports—is a great way to reinforce healthy behaviors across the lifespan while having fun.
What is intergenerational play?
We all know what it feels like to get lost in an engaging activity or pastime with those around us—just think of the common phrase, “Time flies when you’re having fun.” But have you ever thought about the impact of play on your own or your loved ones’ health and well-being?
Play is an essential aspect of what it means to be human and is not just about amusement; it is critical for connecting with and learning from those around us. Since the beginning of time, individuals from different generations have joined together in intergenerational play to foster meaningful connections that strengthen families and communities.
Intergenerational play refers to activities and shared experiences that bring together people of different ages, typically within a family or community setting, for the purpose of fun or fulfillment. This might include:
• Completing puzzles or board games
The benefits of physical forms of intergenerational play
While there are many forms of play, one of the most impactful throughout the lifespan is play through physical activity. Physical forms of play involve engaging in activities that mimic the natural movements humans have performed throughout history in creative and purposeful ways and require moving our bodies in ways that strengthen key muscles and support balance. Physical play can include a wide variety of activities ranging from short bursts that increase one’s heart rate (like sprinting, skipping, or jumping) to endurance-building activities (like hiking, swimming, or completing repetitive movements).
Another essential aspect of physical play is that it is collaborative. Whether on the playground or through rough and tumble play, children benefit from physical play with others by developing a critical awareness of social norms while refining their fine and gross motor skills. Teenagers and young adults see improvements in mental health, self-esteem, and confidence, and sense of social connectedness through physical forms of play. As adults, we continue to benefit from cooperative play in team and competitive activities by improving our collective decision-making skills, navigating social requirements, strengthening relationships, and breaking down ageist attitudes and stereotypes. When generations come together through physical play, everyone wins.

In addition to providing social and emotional benefits, intergenerational play through physical activity impacts areas of health that are especially important to consider as we age:
• Brain health: Throughout the lifespan, regular physical activity engagement has been linked to many aspects of brain health, including heightened memory,
faster processing, better concentration and problemsolving, and a decrease in the chemicals that are present in several forms of dementia. Engaging in physical activities with others through intergenerational play also boosts brain health by supporting social connectedness, sense of purpose and meaning, and mental health—all of which have been tied to cognitive function in older adulthood.
• Bone and muscle health: Engaging in intergenerational play through physical activities can support your bone health and reduce the risk of hip fracture. By participating in weight bearing activities, such as walking, jogging, or climbing stairs, you’re sending signals to your bones that improve their strength and slow down bone loss.
You might also incorporate some muscle-strengthening work (like resistance band or weight exercises) or balance work (like Tai Chi or yoga) for added benefits to your bones and overall physical health. The good news is that no matter what age you start these activities, there will be benefits to your bones; the younger you start, the healthier your bones will be as you age. This means incorporating multiple generations in activities, such as going for a walk, dancing, or trying a new sport, sets everyone up for a healthier future.
Intergenerational play builds lasting memories
Between cell phones and tablets providing constant stimulation, high proportions of jobs that require being tied to Zoom meetings and email, and a virtually limitless number of entertainment options available 24/7 through television and streaming services, it can be challenging for people of all ages to disconnect and get moving.
But finding ways to play together across generations through recreational sports and physical activities can be a fun opportunity to maintain your health and fitness while strengthening relationships with family members and other loved ones. Engaging in safe physical activities benefits everyone—no matter what age—and builds lasting memories in the process.
Source: National Council on Aging. Read more at ncoa.org.

TRANSITIONS IN AGING
Older Americans Living Alone Often Rely on Neighbors or Others
Donald Hammen, 80, and his longtime next-door neighbor in south Minneapolis, Julie McMahon, have an understanding. Every morning, she checks to see whether he’s raised the blinds in his dining room window. If not, she’ll call Hammen or let herself into his house to see what’s going on.
Should McMahon find Hammen in a bad way, she plans to contact his sister-inlaw, who lives in a suburb of Des Moines. That’s his closest relative. Hammen never married or had children, and his younger brother died in 2022.
Although Hammen lives alone, a web of relationships binds him to his city and his community—neighbors, friends, former co-workers, fellow volunteers with an advocacy group for seniors, and fellow members of a group of solo agers. McMahon is an emergency contact, as is a former co-worker. When Hammen was hit by a car in February 2019, another neighbor did his laundry. A friend came over to keep him company. Other people went on walks with Hammen as he got back on his feet.
Those connections are certainly sustaining. Yet Hammen has no idea who might care for him should he become unable to care for himself.
“I’ll cross that bridge when I come to it,” he told me.
These are fundamental questions for older adults who live alone: Who will be there for them, for matters large and small? Who will help them navigate the ever more complex health care system and advocate on their behalf? Who will take
out the garbage if it becomes too difficult to carry? Who will shovel the snow if a winter storm blows through?
American society rests on an assumption that families take care of their own. But 15 million Americans 50 and older didn’t have any close family— spouses, partners, or children—in 2015, the latest year for which reliable estimates are available. Most lived alone. By 2060, that number is expected to swell to 21 million.

families that are essential to their well-being,” said Sarah Patterson, a demographer and sociologist at the Institute for Social Research at the University of Michigan.
Beyond that, millions of seniors living on their own aren’t geographically close to adult children or other family members. Or they have difficult, strained relationships that keep them from asking for support.
These older adults must seek assistance from other quarters when they need it. Often they turn to neighbors, friends, church members, or community groups— or paid help, if they can afford it.
And often, they simply go without, leaving them vulnerable to isolation, depression, and deteriorating health.
When seniors living alone have no close family, can nonfamily helpers be an adequate substitute? This hasn’t been well studied.
“We’re just beginning to do a better job of understanding that people have a multiplicity of connections outside their
The takeaway from a noteworthy study published by researchers at Emory University, Johns Hopkins University, and the Icahn School of Medicine at Mount Sinai was this: Many seniors adapt to living solo by weaving together local social networks of friends, neighbors, nieces and nephews, and siblings (if they’re available) to support their independence.
Still, finding reliable local connections isn’t always easy. And nonfamily helpers may not be willing or able to provide consistent, intense hands-on care if that becomes necessary.
When AARP surveyed people it calls “solo agers” in 2022, only 25% said they could count on someone to help them cook, clean, get groceries, or perform other household tasks if needed. Just 38% said they knew someone who could help manage ongoing care needs. (AARP defined solo agers as people 50 and older who aren’t married, don’t have living children, and live alone.)
Linda Camp, 73, a former administrator with the city of St. Paul, Minnesota, who never married or had children, has written several reports for the Citizens League
in St. Paul about growing old alone. Yet she was still surprised by how much help she required this summer when she had cataract surgery on both eyes.
A former co-worker accompanied Camp to the surgery center twice and waited there until the procedures were finished. A relatively new friend took her to a follow-up appointment. An 81-year-old downstairs neighbor agreed to come up if Camp needed something. Other friends and neighbors also chipped in.
Camp was fortunate—she has a sizable network of former co-workers, neighbors, and friends. “What I tell people when I talk about solos is all kinds of connections have value,” she said.
Michelle Wallace, 75, a former technology project manager, lives alone in a singlefamily home in Broomfield, Colorado. She has worked hard to assemble a local network of support. Wallace has been divorced for nearly three decades and doesn’t have children. Though she has two sisters and a brother, they live far away.
Wallace describes herself as happily unpartnered. “Coupling isn’t for me,” she told me when we first talked. “I need my space and my privacy too much.”
Instead, she’s cultivated relationships with several people she met through local groups for solo agers. Many have become her close friends. Two of them, both in their 70s, are “like sisters,” Wallace said. Another, who lives just a few blocks away, has agreed to become a “we’ll help each other out when needed” partner.
“In our 70s, solo agers are looking for support systems. And the scariest thing is not
having friends close by,” Wallace told me. “It’s the local network that’s really important.”
Gardner Stern, 96, who lives alone on the 24th floor of the Carl Sandburg Village condominium complex just north of downtown Chicago, has been far less deliberate. He never planned for his care needs in older age. He just figured things would work out.
They have, but not as Stern predicted.
The person who helps him the most is his third wife, Jobie Stern, 75. The couple went through an acrimonious divorce in 1985, but now she goes to all his doctor appointments, takes him grocery shopping, drives him to physical therapy twice a week, and stops in every afternoon to chat for about an hour.
She’s also Gardner’s neighbor—she lives 10 floors above him in the same building.

Why does she do it? “I guess because I moved into the building and he’s very old and he’s a really good guy and we have a child together,” she told me. “I get happiness knowing he’s doing as well as possible.”
Over many years, she said, she and Gardner have put their differences aside.
“Never would I have expected this of Jobie,” Gardner told me. “I guess time heals all wounds.”
Gardner’s other main local connections are Joy Loverde, 72, an author of eldercare books, and her 79-year-old husband, who live on the 28th floor. Gardner calls Loverde his “tell it like it is” friend—the one who helped him decide it was time to stop driving, the one who persuaded him to have a walk-in shower with a bench installed in his bathroom, the one who plays Scrabble with him every week, and offers practical advice whenever he has a problem.




“I think I would be in an assisted living facility without her,” Gardner said.
There’s also family: four children, all based in Los Angeles, eight grandchildren, mostly in L.A., and nine greatgrandchildren. Gardner sees most of this extended clan about once a year and speaks to them often, but he can’t depend on them for his day-today needs.
For that, Loverde and Jobie are an elevator ride away. “I’ve got these wonderful people who are monitoring my existence, and a big-screen TV, and a freezer full of good frozen dinners,” Gardner said. “It’s all that I need.”
Source: KFF Health News. Read more at kffhealthnews.org.
CAREGIVING
Who Cares When the Caregivers Fall?
On Labor Day, I developed a fever. Chills, aches, and that creeping sense of something not being right filled my body. This wasn’t new—my rheumatoid arthritis does a version of this sometimes. During a flare, my body aches, temperatures fluctuate, and I ride it out, hoping for relief within a day or two. But this time was different. Two days passed, and I could barely move, let alone keep up with basic tasks. My partner and I finally called an ambulance.
By the time I was being wheeled into the emergency room, I could barely spell my own name.
For a week, I fought for my life.

Three of the medications I take to manage my rheumatoid arthritis leave me immune-compromised. So, when a viral infection, COVID-19, a bacterial infection, and bronchitis all decided to visit me at once, my body could barely hold its ground. The doctors didn’t know where to start and made guesses while I gasped for air, debating which infection to treat first.
I survived.
But even now, weeks later, I’m still grappling with the long-term impacts, physically and emotionally.
On one of those endless days in the hospital, I finally sat up in bed, feeling a window of clarity after days of fog. My first instinct wasn’t to rest—it was to worry. I scrambled to text and call from my hospital bed to make sure my parents were okay, to check if my child missed me, and to navigate the impossible question of whether I’d be safe to return home. I was terrified I’d bring illness back to my parents or be exposed to something new by my school-age child.
‘For so many caregivers, there is no safety net when we fall.’
These were impossible choices, but they were also inevitable ones. For so many caregivers, there is no safety net when we fall. No contingency plan. No backup caregiver. The only plan for my parents was me. And there I was—hooked to machines, drifting in and out of consciousness, but still expected to make sure things were okay at home.
Our caregiving system is broken. It assumes that family, specifically daughters like me, will pick up the slack where the infrastructure fails. But what happens when the caregiver can’t?
This experience made me reflect deeply on the work I’ve done in care advocacy, and how the lessons I learned in my time at Caring Across Generations—an organization working to shift how care is valued in this country—shaped my understanding of this fragile system.
I’m transitioning to a new role in a new organization, but the language I’ve gained about caregiving has been invaluable. We are part of a much larger ecosystem—one that should be connected and resourced, but too often, the path toward solutions is riddled with barriers.
In the disability community, there’s a rallying cry: Nothing about us without us. And as I navigate my disability and its evolving impact on my life and health, I know how true that statement is. As a Black, Latina woman, I am acutely aware of how much more complex this becomes. Navigating a health care system that was never designed for people like me—disabled, historically excluded, and inundated with caregiving responsibilities—feels like fighting a battle on all fronts.
But I’m not alone. There are millions of us in this army that was invisible for too long. We’re all doing what we must for those we love. What we need is a system that recognizes and supports that labor. Because it’s not sustainable, nor just, to keep relying on the already stretched to hold it all together.
We need a better plan. A safety net for the caregivers who fall before they fall—aging and disability care, paid leave, early childhood care—equitable access to respite coverage for caregivers like me. We deserve more. A system that doesn’t leave us gasping for air, but instead ensures that no one has to bear the weight of caregiving alone.
We are at a critical juncture in our country’s political landscape. The pandemic laid bare the fractures in our care systems, and we now have the opportunity to demand that care be placed at the center of our political priorities. This moment—where conversations about caregiving, labor, and health care are
becoming impossible to ignore—offers a chance to build a care infrastructure that works for everyone. But we must act now.
I’ve been unlocked, I am awakened, and I am ready to continue the fight. I know that real change is only possible when caregivers like me are at the center of these conversations. For all our sakes, we can’t



Take Care of Yourself as a Caregiver



HEALTH & WELLNESS
5 Healthy Aging Tips Every Woman Should Know
As a woman, you may have many responsibilities on your plate, but your health should be a top priority.
Women are often the first line of defense when protecting their family’s health, but in doing so tend to put their concerns on the back burner.

These quick tips can help keep you happy and healthy as you juggle your everyday responsibilities.
1. GET BREAST CANCER SCREENINGS EVERY 1–2 YEARS
One in eight women in the U.S. will be diagnosed with breast cancer, making it the most commonly diagnosed cancer in women and this risk increases with age. Mammograms are the best way to screen for breast cancer, especially during the early stages. The good news is that breast cancer can usually be treated successfully when found early. Medicare covers a free yearly mammogram screening.
2. ROUTINE PAP EXAMS ARE THE BEST WAY TO DETECT CERVICAL CANCER
Known as the “silent killer,” cervical cancer is one of the most common types of cancer for American women, but thanks to widespread use of the Pap test, early detection has significantly improved and boosted U.S. survival rates. Cervical cancer may not have any signs or symptoms, so it’s recommended women ages 21 to 65 get routine test about every three years. Medicare covers cervical and vaginal cancer screenings once every 24 months
or every 12 months if you are at high risk.
3. EXERCISE WILL IMPROVE YOUR OVERALL HEALTH
Roughly 150 minutes (2.5 hours) of moderate exercise a week could improve not only your physical but also mental health. Being active helps improve moods and reduce feelings of depression. It can also help manage diabetes, heart disease, and osteoporosis.
4. FOCUS ON YOUR MENTAL HEALTH
Approximately 15% of adults aged 60 and over suffer from a mental illness, depression being one of the most common. There’s often confusion around what exactly depression is, especially since many older adults experience major changes in their life like the death of loved ones or medical problems that could cause sadness. The difference is that the feeling is only temporary. If your feelings of sadness begin to interfere with daily life and normal functioning, you may be experiencing depression. Start by speaking with your doctor and determine if a Medicare depression screening is right for you.
5. HEALTHY EATING CAN PREVENT SERIOUS HEALTH CONDITIONS
Proper nutrition is essential for the body. As you get older you lose muscle mass, bone density, and burn fewer calories. It takes extra effort to make up for the natural changes of your body which is why eating high nutrient foods make a
big difference. Decreased bone density can result in one of the major health concerns affecting about 8 million women, osteoporosis, due to calcium deficiencies in diet.
“Take care of your body now and your body will take care of you for the long haul. When you invest in your well-being, you’ll set yourself up for healthy aging success,” says Gretchen Tanbonliong, Associate Director for Health & Wellness at NCOA. As a woman, you may have many responsibilities on your plate, but your health should be a top priority.
Source: National Council on Aging. Read more at ncoa.org.
IN OUR COMMUNITY
Scholarships Support Older Adults in Community Programs
SourcePoint invites Delaware County residents ages 55 and older to explore its enrichment center with a free community pass (ComPASS). Located at 800 Cheshire Road in Delaware, the 44,000-square-foot center offers a wide range of free activities. For programs with fees, such as fitness, arts, and education classes, financial assistance is available through the Edie Balser Scholarship Fund.
Established in 2016 by private donors, the fund honors the legacy of Edith “Edie” Balser, a dedicated employee and volunteer who passed away in 2019. The scholarships ensure that individuals with modest incomes can participate fully in enriching activities. Assistance covers up to $150 per calendar year, with 50% and 100% scholarships available based on need. While most programs are eligible, trips and personal training are limited to 50% assistance with a $50 cap per year.

Applying is simple: Visit MySourcePoint. org/scholarship or contact SourcePoint’s customer service supervisor at 740-3636677. Scholarships must be used within the calendar year, but reapplication is encouraged annually.
SourcePoint is committed to supporting active, engaged older adults in the community, regardless of financial standing.
HEALTH & WELLNESS
CDC Recommends Lowering the Age for Pneumococcal Vaccination from 65 to 50 Years Old
In October, CDC Director Mandy Cohen endorsed the CDC Advisory Committee on Immunization Practices’ (ACIP) recommendation for lowering the age for pneumococcal vaccination from 65 to 50 years old.
Lowering the age for pneumococcal vaccination gives more adults the opportunity to protect themselves from pneumococcal disease at the age when risk of infection substantially increases. Pneumococcal bacteria can cause serious illnesses, including pneumonia, meningitis, and bloodstream infections, and older adults are at increased risk for pneumococcal disease.

Adults 50 years or older should talk with a health care provider to make sure they’re up to date with pneumococcal vaccination. This is a great time to get vaccinated against pneumococcal disease for the winter respiratory season.
FROM THE SOURCE
The latest news, programs, and resources available at SourcePoint.
Fitness & Wellness
AQUA JAMMIN’ NEW
Tuesday with Whitney, 9:15–10 a.m., 10:15–11 a.m., 12:15–
1 p.m. or 1:15–2 p.m.
Beginner-advanced. Get your groove on with funky tunes as we stretch and warm up. Then, turn up the heat with a highenergy circuit workout using noodles and waterbells. No judgment zone, all fitness levels welcome! Let’s make waves together and burn those calories! Fee: $40 for a one-time per week series.
BALANCE BOOST ONLINE
Mondays with Dyan or Austin, 1–1:45 p.m.
Thursdays with Dyan, 11‒11:45 a.m.
Participate from home in a beginner-advanced strength training class to improve balance. The National Institute of Health recommends strength training for older adults to prevent falls. Fee: $15 for a two‒time per week series.
BANDS & BELLS ONLINE
Mondays or Wednesdays with Austin, 10–10:45 p.m.
Intermediate-advanced. Specifically programmed to strengthen muscle and improve bone density to increase the healthy years of life. Fee: $15 for a two‒time per week series.
GOLDEN MARATHON OUTDOOR HIKING
Mondays with Bob, 1:30–3 p.m. at various parks. Get moving this winter with SourcePoint’s Golden Marathon outdoor hikers! We hike and walk, rain/snow or shine except for temperatures below 10 degrees or a Level 2 or 3 snow emergency! Meet at locations listed, bring your own water, and be prepared for the weather and terrain. Remember to register at MySourcePoint.org or call 740-363-6677.
MEDITATION HYBRID
Mondays, Wednesdays* and Thursdays, 8:30–9:05 a.m.
*All Wednesday sessions will be on Zoom only.
Meditation has numerous mental, physical, and emotional benefits including lowering blood pressure, reducing stress, and increasing mental clarity and focus. 20-minute sessions will vary, including guided meditation, focusing on the breath, and intention setting. Fee: $20 per month.
Transitions in Aging
CAREGIVER CONVERSATIONS
Third Thursday of each month, 5:30–6:30 p.m., at Community Library, 44 Burrer Drive, Sunbury. This group fosters supportive conversations, allows you to share experiences, meet other caregivers, discover new resources, and ask questions.
CAREGIVER CRASH COURSE
Tuesday, March 4, 10:30–11:30 a.m. or Thursday, March 6, 6–7 p.m. at Orange Township Hall, 1680 E. Orange Road, Lewis Center.
All you need in the time you have: A one-hour class for new, current, and future family caregivers that includes information on safety, falls, getting organized, legal information, community resources, and self-care. Not for professional caregivers.
FIGHTING FINANCIAL FRAUD: SCAMS TARGETING SENIORS
Thursday, Jan. 23, 11 a.m.–noon.
Financial fraud can have devastating and far-reaching effects, particularly on older adults. Join us for an insightful presentation by the Better Business Bureau to learn about common scams targeting older adults, how to recognize warning signs, and strategies to protect yourself and your loved ones from becoming victims.
MEDICARE: NEW TO MEDICARE
Tuesday, Feb. 11, 10 a.m.‒noon at DCDL Orange Branch, 7171 Gooding Blvd., Lewis Center.
Saturday, March 8, 1–3 p.m. at Unity Community Center, 50A Ross St., Delaware.
Learn the basics of Medicare and what options are available. Whether you’re becoming eligible for Medicare for the first time or assisting a loved one with insurance needs, this is the place to start.
Learning
THRIVING WITHOUT DRIVING: TODAY’S ALTERNATIVE TRANSPORTATION NEW
Thursday, Feb. 13, 1–2:30 p.m.
Today’s transportation landscape makes living well without a car a real possibility—if only it weren’t so confusing. Ever wanted to call an Uber but didn’t know how? Do you want to better understand our local public transportation system? Does a loved one need transportation? Or do you worry about the day you must cut back on driving? SourcePoint’s mobility coordinator, Jill Smith, will walk (not drive!) you through the ins and outs of ridesharing, ride-hailing, and SourcePoint’s medical transportation program. Lose the fear of being stranded and embrace the backseat!
The Arts
PAPER QUILLING: BEGINNING MINI SPRING WREATH
Friday, March 28, 1–4 p.m.
Expert quiller Lora Davenport will show you how to create flowers for a mini spring wreath. Fee: $17.
PIANO: BEGINNER
Saturdays, Jan. 25, Feb. 1, 8, 15, 22 and March 1, 9–10 a.m.
Learn the basics of piano with musician Kathleen Mergler using the Faber and Faber, Primer Level books (Amazon). Purchase books ahead of time or see how class goes. Bring your keyboard if you have one. Fee: $60 for six-week series.
REVERSE STENCIL WATERCOLOR PAINTING NEW
Wednesday, March 12, 5:30–7:30 pm.
Create a unique watercolor with stencils by lifting paint away from the surface. Make one 11x15 piece and a few smaller complimentary pieces. Instructor Carol Wallenfelsz will guide you through this process. Fee: $20.
STAINED GLASS MOSAIC GARDEN PAVER
Tuesdays, Feb. 4 and 18, 3:30–5:30 p.m.
In the first class you will learn how to cut stained glass. You will then use the glass to create a colorful mosaic design on a 12x12 concrete paver. The second class will involve adding grout to the piece. Wear old clothes for the second class. Led by Instructor Carol Wallenfelsz. Fee: $35.
Social Connections
KARAOKE! MARDI GRAS KARAOKE PARTY
Tuesday, March 4, 5:30–7:30 p.m.
Grab the mic and have some fun on Fat Tuesday! When everyone starts singing with you, you’ll know you have chosen a good song. Feel free to bring your own dinner and beverage of choice.
SUNBURY SOCIALS
Third Monday of Feb. and March, 1–3 p.m. at Sunbury Township Hall, 51 E. Cherry St., Sunbury. In partnership with the city of Sunbury, SourcePoint is hosting three social gatherings for people to meet others at Sunbury’s Town Hall. With food, fellowship, and fun, these events focus on engaging with others in the Sunbury area. We will be learning and playing the card game, “Trash.”
WELCOME TO SOURCEPOINT!
Wednesday, March 5, 11:15 a.m.–1:30 p.m.
Join us to learn more about what SourcePoint has to offer. There will be guided tours and the opportunity to chat with staff members. If interested, you may also enjoy lunch in Cafe 55 with others in our group. For Delaware County residents 55 and better, lunch is available on a donation basis.
Trips
JERRY SEINFELD & JIM GAFFIGAN
Friday, March 21; estimated timing: 6:15 p.m. bus departure, 10:45 p.m. return. Registration through Feb. 8. Fee: $170 for members; $190 for non-members.
BROADWAY IN COLUMBUS: FUNNY GIRL
Tuesday, March 25; estimated timing: 6:15 p.m. bus departure, 11:30 p.m. return. Registration through Jan. 25. Fees: $105 for members; $125 for non-members.
SCENIC SEDONA: CANYONS & RAILS
May 18-23, 2025 (6 days/5 nights). Fee: $2,899 per person based on double occupancy. Other rate info available in World of Travel flyer.
DISCOVER EASTERN CANADA
June 22-29, 2025 (8 days/7 nights). Fee: $2,799 per person based on double occupancy. Other rate info available in World of Travel flyer.
IN OUR COMMUNITY
SourcePoint Champions Community Impact with 19 Grant Recipients
SourcePoint’s board of directors approved $444,410 in grant funding for 21 programs in Delaware County. Each year, SourcePoint awards grant funding to local nonprofits and government organizations to ensure that the critical needs of the community’s older adults are met without duplicating existing services. By strategically supporting programs that address service gaps, SourcePoint fosters a cost-effective, collaborative network of care for older adults and family caregivers in Delaware County. This approach leverages existing resources and partnerships to efficiently broaden support for the community.
Grant applications are reviewed annually by a committee composed of SourcePoint board members, staff, and community representatives. The committee carefully selects organizations that provide essential services where gaps exist, strengthening the overall system of care for the county’s older population. Those awarded grants for 2025 include the following:
The Alzheimer’s Association: $49,810 to provide supportive services to individuals living with dementia and their caregivers.
Big Walnut Friends Who Share: $2,000 to secure donations of clothing, food, and household items and distribute free of charge to eligible families and individuals.
Catholic Social Services: $21,600 for the Senior Companion Program, which prevents social isolation among homebound older adults.
Central Ohio Area Agency on Aging: $10,000 for the Volunteer Guardian Program, which advocates for the rights of older adults who are unable to do so themselves.
Central Ohio Symphony: $2,500 to transport older adults with mobility issues to and from symphony concerts on the Ohio Wesleyan University campus.
Common Ground Free Store: $19,900 to support a portion of operating expenses for the agency providing food, clothing, and household items to low-income county residents.
Delaware County Guardianship Services Board: $10,000 to provide exemplary guardianship services to individuals 55 and older who do not have appropriate guardian candidates in the community.
Delaware County District Library: $10,000 to supplement largeprint book purchases and expand digital library access.
Delaware Speech and Hearing Center: $84,000 to expand and enhance hearing and speech health services to older adults and their caregivers.
First Presbyterian Church: $8,000 for the Laundry Love Program, which provides free laundry services to individuals who may otherwise be unable to afford such services.
Grace Clinic: $39,000 to expand hours of operation to increase accessibility of low-cost health care and services to rural areas of the county.
HelpLine of Delaware and Morrow Counties: $49,500 for continued support of the Connections Volunteer Program; $41,250 to support management and oversight of volunteer matches and client referrals for the Senior Companion Program; and $5,150 to expand Sages & Seekers, an evidence-based, intergenerational program that brings together older adults and high school students.
Humane Society of Delaware County: $10,000 for the Pet Care Assistance Program, which provides vaccines, medication, surgeries, and grooming for pets in older-adult households.
Lutheran Social Services: $18,000 to support operations and food costs for older adults at the local food bank.
Main Street Delaware, Inc.: $4,000 to improve accessibility to the welcome center.
National Alliance on Mental Illness Delaware and Morrow Counties: $25,200 to support recovery and educational programming for individuals with mental illness and their families.
OhioHealth Grady Memorial Hospital: $23,000 for the Driver Rehabilitation for Instruction and Vehicle Education (DRIVE) program intended to improve driver safety.
Ohio Wesleyan University Lifelong Learning Institute: $4,000 to improve access to the Lifelong Learning Institute’s adult educational programming.
Unity Community Center: $7,500 to expand free older adult programming that supports physical fitness, balance, and social interaction.
TRAVEL & LEISURE
Top Trending Destinations for Educational Travel in 2025
Road Scholar, the not-for-profit world leader in educational travel for older adults, released the top trending destinations for educational travel in 2025, ahead of its 50th anniversary this year. Based on year-over-year program enrollment increases, Road Scholar identified the top 10 trending destinations —five domestic and five international— that are capturing the attention of lifelong learners as they head into the new year. These destinations reflect the highest increase in demand from 2024 to 2025, highlighting a growing enthusiasm for experiential learning through travel as more older adults seek opportunities to expand their knowledge and explore the world.
“As we celebrate our 50th anniversary in 2025, the interest in our new and ongoing programs is a testament to Road Scholar’s exceptional experiences offered across the world and the growing demand for educational travel,” said Maeve Hartney, chief program officer at Road Scholar. “Across the U.S., Road Scholar participants are embracing the postpandemic trend of discovering enriching, educational experiences closer to home. For international programs, we’re seeing a growing enthusiasm for deepening knowledge through once-in-a-lifetime learning adventures, exploring hidden gems off the beaten path, and immersing in the culture of more remote, lessertraveled destinations.”
Based on the largest year-over-year increases of confirmed enrollments in Road Scholar’s programs, here’s a look at the top trending domestic
and international destinations:
Top Trending Domestic Destinations
1. Lincoln, New Hampshire
2. San Francisco, California
3. Norfolk, Virginia
4. Santa Rosa, California
5. Stowe, Vermont

Top Trending International Destinations
1. Namibia, Africa
2. Tanzania, Africa
3. Peru, South America
4. Greenland, Europe
5. Mongolia, Asia
The Top 3 Trending Domestic Destinations for Educational Travel
1. Lincoln, N.H. – As a leader in the skipgen travel movement, Road Scholar’s Nature of New Hampshire program provides a unique opportunity for grandparents to travel and learn alongside their grandkids in Lincoln. On this six-day, sea-to-sky adventure, participants ride along the Cog and Lake Winnipesaukee Railroads, sail on Squam Lake and Lake Winnipesaukee, discover regional wildlife, taste maple syrup delicacies, and more.
2. San Francisco, Calif. – To experience the best of the “City of the Bay,” Road Scholar’s six-day Signature City San Francisco program invites travelers to immerse themselves in the captivating story of San Francisco with the guidance of experts. Participants
explore Alcatraz Island, learn about the fire of 1906, wander the markets of Chinatown, and see iconic landmarks.
3. Norfolk, Va. – Perfect for music enthusiasts, Road Scholar’s five-day The Best of Norfolk & the Virginia International Tattoo program takes travelers back to the 17th century to discover the city’s military and art culture. Participants experience the nation’s largest military musical celebration at the Virginia International Tattoo, stroll through the Botanical Garden, attend an exclusive private musical performance, and take a narrated Norfolk Naval Base cruise.
The Top 3 Trending International Destinations for Educational Travel
1. Namibia, Africa – Home to the world’s oldest desert and timeless cultures, Namibia offers travelers the chance to meet native communities and learn about wildlife conservation initiatives. Over a 16-day journey, Road Scholar’s Namibia’s Splendor: Desert, Culture and Magnificent Wildlife program... See TRAVEL on page 20.
Travel
From page 19
...brings participants to the AfriCat Foundation for up-close experiences with Africa’s big cats, exciting safaris, and a visit to a Himba settlement.
2. Tanzania, Africa – Road Scholar’s 13-day Tanzania and the Great East African Migration program invites travelers to follow the largest movement of wildlife on Earth, from the Serengeti to Maasai Mara Reserve. Participants stay in tents along the migration path, visit the Ngorongoro Crater and Olduvai Gorge, and learn how the migration impacts the lives of Indigenous people.
3. Peru, South America – Road Scholar’s most popular program in Peru, A Taste of Peru: Discover Lima, Sacred Valley and Machu Picchu, gives travelers a unique perspective on the country during a nine-day journey from Lima to Cusco. In 2025, a new solo-only date will be offered. Participants explore mountain villages, experience a traditional Pachamama ceremony, visit Machu Picchu, and learn about ancient weaving traditions and music.
Maeve Hartney has served as the Chief Program Officer at Road Scholar since 2021. In this role she is responsible for the development and operation of all Road Scholar Programs offered worldwide and virtually. She leads multiple teams of program staff around the world to ensure Road Scholar adventures meet the highest travel industry standards for operational efficiency and practicality, while providing excellent educational content; diverse cultural integrity; and meaningful, transformational experiences for Road Scholar participants. Hartney joined Road Scholar in 1998 as Manager of Program Assessment and Evaluation, quickly rising to Senior Manager and then Director of Program Services. In 2006, Hartney was promoted to associate Vice President of Special Programs. She also serves on the Board at the Huntington Theatre Company, Friends of Abbot Public Library and is on the Advisory Board of Atout France.
Not-for-profit Road Scholar is the world leader in educational travel for older adults, serving 90,000 lifelong learners annually. Founded as “Elderhostel” in 1975, Road Scholar will be celebrating their 50th anniversary in 2025 with a Great Global Giveaway, among other

special projects. Road Scholar programs combine travel and education to provide experiential learning opportunities featuring an extraordinary range of topics, formats, activity levels, and locations— on all seven continents and throughout the United States. Alongside renowned experts, participants experience indepth and behind-the-scenes learning opportunities by land and by sea on educational travel adventures designed for curious adventurers over 50.

NUTRITION
Thai Veggie Salad
This dish is easy to prepare with minimal prep and no cooking, unless you want to add meat to it. Shredded chicken or thinly sliced steak would go very well tossed in with this salad. You can trade out or add any extra veggies. Suggested added veggies include shredded baby bok choy, finely sliced napa cabbage, broccoli, mushrooms, or bean sprouts.
Makes 4 Servings
For the Dressing
1 1/2 tsp minced garlic
1 1/2 tsp minced ginger
4 tsp honey
4 tsp lime juice
4 tsp rice wine vinegar
4 tsp lite soy sauce
4 tbsp creamy peanut butter
4 tbsp sesame oil
Water to thin out
Spinach-Mushroom Shells

Oil
This dish is simple, but does take a little time to prepare. You can substitute or add some veggies to the filling, but make sure to reduce the amount of each vegetable so that there is still a decent amount of ricotta in the stuffing of each shell. This dish can be served with your sauce of choice: recommendations are marinara, butternut squash sauce, or a creamy roasted red pepper sauce.
Makes 4 servings of 2-3 shells each.
Jumbo shells
2 cups of sliced mushrooms
3 tsp minced garlic
3 tsp minced shallots
¼ cup white wine
3 cups spinach
1 cup ricotta
3 tsp minced fresh oregano
4 tbsp parmesan
1. Mix all ingredients, except oil, using a whisk or immersion blender.
2. Add oil in slowly.
3. Taste and adjust as needed. If too thick, add water to thin out.
For the Salad
2 cups shredded romaine lettuce
1/3 cup shredded carrots
1/3 cup sliced red pepper
1/3 cup sliced red cabbage
1 cup edamame (thawed)
¼ cup thin sliced green onions
1/3 cup diced cucumbers
Granulated/chopped peanuts
1. Thaw edamame, if bought frozen.
2. Wash then thinly slice romaine.
3. Wash then thinly slice red pepper.
4. Wash then thinly slice red cabbage.
5. Wash then thinly slice green onions.
6. Wash then dice cucumbers.
7. Toss all ingredients together, except peanuts.
8. Toss in dressing a little at a time until you have the desired amount.
9. Plate salad then top with peanuts.
Sauce of choice
1. Boil the pasta until al dente (or until mostly cooked, you don’t want it to be mushy).
2. Shock in ice cold water to stop the cooking process.
3. Mince shallots and garlic.
4. In a hot saute pan, cook onions, garlic, and mushrooms in a small amount of oil.
5. Season with salt and pepper.
6. Reduce heat to medium and add wine. Reduce liquid by half.
7. Give the spinach a quick chop.
8. Add the spinach and cook.
9. Stir occasionally, until spinach is completely wilted and most of the liquid is evaporated.
10. Remove from heat and let the mushroom mixture cool.
11. Finely chop the oregano.
12. Once cool, add ricotta, parmesan, and oregano to the mushroom mixture and combine.
13. Using a spoon, fill the pasta shells, careful not to overfill.
14. Use your favorite sauce to fill the bottom of a pan.
15. Top the sauce with shells then top with mozzarella and parmesan cheese.
16. Put oven on broiler and bake until cheese is golden and melty.
CREATIVE WRITING
White Pants
There are things I’ve always associated with women growing older and have, thus far, doggedly avoided in the inexorable march of time. These things aren’t based in reality, such as wrinkles or grey hair, but are telltale signs to me nonetheless. One such conjecture is white pants.
Admittedly I have spent too much time overthinking this conundrum and have landed on the following shaky premise. Only the bravest of parents would dare dress their little girl in white, what with mud puddles and green lawns waiting to pounce at every turn.

Nipping at the heels of adolescence is the onslaught of puberty where every girl thinks twice about running the gauntlet of white pants so as not to be caught out embarrassingly. No sooner does a gal get a grip on her hormones, then her own children and their grubby hands surround her, and the wearing of white pants is shoved farther and farther back into the closet of her life.
Then, seemingly overnight, a woman of a certain age owns white; white pants, white capris, white golf shorts. It is a juxtaposition then that where women of a certain age are gathered, there are white pants in their midst.
Not to be outdone in bizarre juxtapositions of women growing older is the awkward decorum of menu substitutions. Admittedly, I’ve had friends of every age who find it impossible for reasons of health, indecisiveness, or self-importance to simply order what’s written on the menu. In my 30s, my friend Linda, upon being presented with ANY menu at ANY restaurant, behaved as if she had just stepped through the Looking Glass with Alice and had encountered a fantasy culinary world. She couldn’t make a decision on what to eat in less than 15 questions to the waiter if the hounds of hell were on our tails.
There were the friends in yoga pants who piously rehearsed the woes of gluten, carbs, and sugar to the teenager behind the McDonalds counter, asking them to make their double cheeseburger without the bun.
Now I encounter dinner mates who feel it necessary to explain their digestive ailments and bowel intolerances to the waitstaff before launching into such a plethora of substitutions that they’ve essentially rewritten the menu. A polite waitress wanting
to get the order correct should not be mistaken for someone who needs the entire background story. My philosophy is that a young woman, or at least young at heart, does her best to order something straight from the menu, picks off the things that are going to keep her awake all night, and keeps shtum.
Clichés are the kiss of death, or in this case, a pretty darn good sign of growing older. At what age do women begin saying “bless her heart” when what they mean to say is “she’s a complete airhead who was the only one who couldn’t see that catastrophe coming a mile away.” To young people, the statement-slash-question “Hi. How are you?” is rhetorical. To those who are no longer spring chickens, that innocuous greeting opens a Pandora’s box of aches, pains, and prescription recitals.
Every once in a while, I catch myself starting a sentence with “when I was younger.” I’ve also garnered the evil eyebrow raise from my husband in church when I unwrap a piece of candy too loudly. And with sad resignation, I realize that somewhere along the way, I’ve swapped bubble gum for Starlight peppermints packaged in the noisiest cellophane on earth. Like it or not, age is marching toward me faster than I can run from it. And last I saw, it was wearing white pants.
Wendy Bauder is a creative writing participant at SourcePoint’s enrichment center.
There is so much
to be grateful for in this moment
1. It’s the freedom
a) Freedom to live in America. We are truly blessed.
b) Freedom to say what I think. Even if I am wrong.
c) Freedom to make mistakes. And learn from my blunders.
d) Freedom to go where I want. At the time of my choosing.
e) Freedom to worship God. So important to grasp real meaning.
2. It’s the grand things
a) The sun rose today. I had the nerve to expect that it would.
b) The stars are so beautiful. Especially on a dark night.
c) I am alive. My spirit hears and sings a song.
d) I am alive. I am not alone
e) I am alive. My spirit has a home.
3. It’s the obvious things
a) The technology and the toilets. They give and they take away.
b) Gratitude brings peace. Peace yields to rest.
c) Blood pulses through my veins. And my body continues to live.
d) I have my body. It mostly listens to what I ask it to do.
e) I have my mind. It gives reason to my longings.
4. It’s the little things
a) The smile of a baby. Full of innocence and joy.
b) The sound of the ocean. Peaceful and soothing.
c) The color blue. Predictable and true.
d) My friends for many years. They anchor and add stability.
e) My new friends. They add variety and fun.
5. It’s the hidden things
a) Gravity is constant. I don’t float off the planet.
b) Although expanding, the universe hangs together.
c) Dreaming and snuggling with my wife. Life is good.
d) Love of a child. A tether and a hope.
e) The rhythms of life. That take us to back to where we began.
CarlVon Patterson is a creative writing participant at SourcePoint’s enrichment center.
FUN & GAMES
Sudoku
EASY
Print and play more Sudoko at www.livesudoku.com
Print and play more Sudoko at www.livesudoku.com

Sudoku Hard #1357915 - Play this sudoku online Sudoku
Sudoku Easy #324790 - Play this sudoku online Sudoku
HARD

Sudoku Hard #1005883 - Play this sudoku online Sudoku
See Sudoku Solutions on page 31.
Sudoku Easy #235020 - Play this sudoku online Sudoku
HEALTH & WELLNESS
Preparing for a Doctor’s Appointment
A basic plan can help you make the most of your appointment whether you are starting with a new doctor or continuing with the doctor you’ve seen for years. The following tips will make it easier for you and your doctor to cover everything you need to talk about.

MAKE A LIST AND PRIORITIZE YOUR CONCERNS
Make a list of what you want to discuss. For example, do you have a new symptom you want to ask the doctor about? Do you want to get a flu shot? Are you concerned about how a treatment is affecting your daily life? If you have more than a few items to discuss, put them in order and ask about the most important ones first. Don’t put off the things that are really on your mind until the end of your appointment—bring them up right away!
TAKE INFORMATION WITH YOU TO THE DOCTOR
Some doctors suggest you put all your prescription drugs, over-the-counter medicines, vitamins, and herbal remedies or supplements in a bag and bring them with you. Others recommend you bring a list of everything you take and the dose. You should also take your insurance cards, names and phone numbers of other doctors you see, and your medical records if the doctor doesn’t already have them.
CONSIDER BRINGING A FAMILY MEMBER OR FRIEND TO THE DOCTOR’S OFFICE
Sometimes it is helpful to bring a family
member or close friend with you. Let your family member or friend know in advance what you want from your visit. Your companion can remind you what you planned to discuss with the doctor if you forget. She or he can take notes for you and can help you remember what the doctor said.
Don’t let your companion take too strong a role. The visit is between you and the doctor. You may want some time alone with the doctor to discuss personal matters. If you are alone with the doctor during or right after the physical exam, this might be a good time to raise private concerns. Or, you could ask your family member or friend to stay in the waiting room for part of the appointment. For the best results, let your companion know in advance how he or she can be most helpful.
Getting
started with a new doctor
Your first meeting is a good time to talk with the doctor and the office staff about some communication basics.
Introduce yourself. When you see the doctor and office staff, introduce yourself and let them know by what name you prefer to be called. For example: “Hello, my name is Mrs. Martinez,” or “Good morning, my name is Bob Smith. Please call me Bob.”
Ask how the office runs. Learn what days are busiest and what times are best to call. Ask what to do if there is an emergency, or if you need a doctor when the office is closed.
Share your medical history. Tell the doctor about your illnesses, operations, medical conditions, and other doctors you see. You may want to ask the doctor to send you a copy of the medical history form before your visit so you can fill it out at home, where you have the time and information you need to complete it. If you have problems understanding how to fill out any of the forms, ask for help. Some community organizations provide this kind of help.
Share former doctors’ names. Give the new doctor all of your former doctors’ names and addresses, especially if they are in a different city. This is to help your new doctor get copies of your medical records. Your doctor will ask you to sign a medical release form giving him or her permission to request your records.
KEEP YOUR DOCTOR UP TO DATE
Let your doctor know what has happened in your life since your last visit. If you have been treated in the emergency room or by a specialist, tell the doctor right away. Mention any changes you have noticed in your appetite, weight, sleep, or energy level. Also tell the doctor about any recent changes in any medications you take or the effects they have had on you.
Winter 2025
BE SURE YOU CAN SEE AND HEAR AS WELL AS POSSIBLE
Many older people use glasses or need aids for hearing. Remember to take your eyeglasses to the doctor’s visit. If you have a hearing aid, make sure that it is working well and wear it. Let the doctor and staff know if you have a hard time seeing or hearing. For example, you may want to say: “My hearing makes it hard to understand everything you’re saying. It helps a lot when you speak slowly and face me when you’re talking.”
REQUEST AN INTERPRETER IF YOU NEED ONE
If the doctor you selected or were referred to doesn’t speak your language, ask the doctor’s office to provide an interpreter. Even though some English-speaking doctors know basic medical terms in Spanish or other languages, you may feel more comfortable speaking in your own language, especially when it comes to sensitive subjects, such as sexuality or depression. Call the doctor’s office ahead of time, as they may need to plan for an interpreter to be available.
Always let the doctor, your interpreter, or the staff know if you do not understand your diagnosis or the instructions the doctor gives you. Don’t let language barriers stop you from asking questions or voicing your concerns.
Using an interpreter at the doctor’s office
Consider telling your interpreter what you want to talk about with your doctor before the appointment.
If your language is spoken in multiple countries, such as Spanish, and your interpreter does not come from the same country or background as you, use universal terms to describe your symptoms and communicate your concerns.
Make sure your interpreter understands your symptoms or condition so that he or she can correctly translate your message to the doctor. You don’t want the doctor to prescribe the wrong medication!
Don’t be afraid to let your interpreter know if you did not understand something that was said, even if you need to ask that it be repeated several times.
Source: American Society on Aging.
Read more at generations.asaging.org.
5 Ways to Make the Most of Your Doctor Visit
Being able to talk with your doctor is important, especially if you have health problems or concerns.

Use these TIPS to make the most of your doctor visit.
Prepare for your visit. Be ready to ask three or four questions. Share your symptoms, medicines or vitamins, health habits, and any major life changes.
Take notes or ask for written materials. Don’t be afraid to ask the doctor to repeat or clarify important information.
Make decisions with your doctor that meet your needs.
Discuss risks, benefits, and costs of tests and treatments. Ask about other options and preventive things you can do.
Be sure you are getting the message. If you have trouble hearing, ask your doctor to face you when talking and to speak louder and more clearly.
Tell the doctor if you feel rushed, worried, or uncomfortable. You can offer to return for a second visit or follow up by phone or email.
Learn more about communicating with your doctor: https://www.nia.nih.gov/health/
HEALTH & WELLNESS
Millions of Aging Americans are Facing Dementia by Themselves
Sociologist Elena Portacolone was taken aback. Many of the older adults in San Francisco she visited at home for a research project were confused when she came to the door. They’d forgotten the appointment or couldn’t remember speaking to her.
It seemed clear they had some type of cognitive impairment. Yet they were living alone.
Portacolone, an associate professor at the University of California-San Francisco, wondered how common this was. Had anyone examined this group? How were they managing?

When she reviewed the research literature more than a decade ago, there was little there. “I realized this is a largely invisible population,” she said.
Portacolone got to work and now leads the Living Alone With Cognitive Impairment Project at UCSF. The project estimates that that at least 4.3 million people 55 or older who have cognitive impairment or dementia live alone in the U.S.
About half have trouble with daily activities, such as bathing, eating, cooking, shopping, taking medications, and managing money, according to their research. But only 1 in 3 received help with at least one such activity.
Compared with other older adults who live by themselves, people living alone with cognitive impairment are older, more likely to be women, and disproportionately Black or Latino, with lower levels of education, wealth, and homeownership. Yet only 21% qualify for publicly funded programs like Medicaid that pay for aides to provide services in the home.
In a health care system that assumes older adults have family caregivers to help them, “we realized this population is destined to fall through the cracks,” Portacolone said.
Imagine what this means. As memory and thinking problems accelerate, these seniors can lose track of bills, have their electricity shut off, or be threatened with eviction. They might stop shopping (it’s too overwhelming) or cooking (it’s too hard to
follow recipes). Or they might be unable to communicate clearly or navigate automated phone systems.
A variety of other problems can ensue, including social isolation, malnutrition, self-neglect, and susceptibility to scams. Without someone to watch over them, older adults on their own may experience worsening health without anyone noticing or struggle with dementia without ever being diagnosed.
Should vulnerable seniors live this way?
For years, Portacolone and her collaborators nationwide have followed nearly 100 older adults with cognitive impairment who live alone. She listed some concerns people told researchers they worried most about: “Who do I trust? When is the next time I’m going to forget? If I think I need more help, where do I find it? How do I hide my forgetfulness?”
Jane Lowers, an assistant professor at the Emory University School of Medicine, has been studying “kinless” adults in the early stages of dementia—those without a live-in partner or children nearby. Their top priority, she told me, is “remaining independent for as long as possible.”
Seeking to learn more about these seniors’ experiences, I contacted the National Council of Dementia Minds. The organization last year started a biweekly online group for people living alone with dementia. Its staffers arranged a Zoom conversation with five people, all with early-to-moderate dementia.
One was Kathleen Healy, 60, who has significant memory problems and lives alone in Fresno, California.
“One of the biggest challenges is that people don’t really see what’s going on with you,” she said. “Let’s say my house is a mess or I’m sick or I’m losing track of my bills. If I can get myself together, I can walk out the door and nobody knows what’s going on.”
An administrator with the city of Fresno for 28 years, Healy said she had to retire in 2019 “because my brain stopped working.”
With her pension, she’s able to cover her expenses, but she doesn’t have significant savings or assets.
Healy said she can’t rely on family members who have troubles of their own. (Her 83-year-old mother has dementia and lives with Healy’s sister.) The person who checks on her most frequently is an ex-boyfriend.
“I don’t really have anybody,” she said, choking up.
David West, 62, is a divorced former social worker with Lewy body dementia, which can impair thinking and concentration and cause hallucinations. He lives alone in an apartment in downtown Fort Worth, Texas.
“I will not survive this in the end—I know that—but I’m going to meet this with resilience,” he said when I spoke with him by phone in June.
Since his diagnosis nearly three years ago, West has filled his life with exercise and joined three dementia support groups. He spends up to 20 hours a week volunteering, at a restaurant, a food bank, a museum, and Dementia Friendly Fort Worth.
Still, West knows that his illness will progress and that this period of relative independence is limited. What will he do then? Although he has three adult children, he said, he can’t expect them to take him in and become dementia caregivers— an extraordinarily stressful, time-intensive, financially draining commitment.
“I don’t know how it’s going to work out,” he said.
Denise Baker, 80, a former CIA analyst, lives in a 100-yearold house in Asheville, North Carolina, with her dog, Yolo. She has cognitive problems related to a stroke 28 years ago, Alzheimer’s disease, and serious vision impairment that prevents her from driving. Her adult daughters live in Massachusetts and Colorado.
“I’m a very independent person, and I find that I want to do everything I possibly can for myself,” Baker told me, months before Asheville was ravaged by severe flooding. “It makes me feel better about myself.”
She was lucky in the aftermath of Hurricane Helene: Baker lives on a hill in West Asheville that was untouched by floodwaters. In the week immediately after the storm, she filled water jugs every day at an old well near her house and brought them back in a wheelbarrow. Though her power was out, she had plenty of food and neighbors looked in on her.
“I’m absolutely fine,” she told me on the phone in early October after a member of Dementia Friendly Western North Carolina drove to Baker’s house to check in on her, upon my request. Baker is on the steering committee of that organization.
Baker once found it hard to ask for assistance, but these days she relies routinely on friends and hired help. A few examples: Elaine takes her grocery shopping every Monday. Roberta comes once a month to help with her mail and finances. Jack mows her lawn. Helen offers care management advice. Tom, a cab driver she connected with through Buncombe County’s transportation program for seniors, is her go-to guy for errands.
Her daughter Karen in Boston has the authority to make legal and health care decisions when Baker can no longer do so. When that day comes—and Baker knows it will—she expects her long-term care insurance policy to pay for home aides or memory care. Until then, “I plan to do as much as I can in the state I’m in,” she said.
Much can be done to better assist older adults with dementia who are on their own, said Elizabeth Gould, co-director of the National Alzheimer’s and Dementia Resource Center at RTI International, a nonprofit research institute. “If health care providers would just ask ‘Who do you live with?’” she said, “that could open the door to identifying who might need more help.”

Source: KFF Health News. Read more at kffhealthnews.org.
HEALTH & WELLNESS
Staying Motivated to Exercise
Physical activity is a great way for older adults to gain substantial health benefits and maintain independence. Try to make exercise a priority. Remember that being active is one of the most important things you can do each day to maintain and improve health. Try these tips to help you stay motivated to exercise.

ways to add physical activity to your regular schedule:
• Take the stairs instead of the elevator.
• Take a walk with co-workers during your lunch break. An exercise buddy can help you stick with your plan to be more active!
• Walk down the hall and talk with a co-worker instead of sending an e-mail.
Update your exercise plan as you progress.
QUICK TIP: REWARDS FOR BEING ACTIVE
Don’t forget to build rewards into your plan. Write down something you will do for yourself when goals are achieved. Treat yourself to something special: a movie, a trip to the museum, a new audiobook, or a massage. Celebrate your successes!
TIPS FOR COPING WITH BREAKS IN YOUR EXERCISE ROUTINE
1. Find simple ways to make exercise fun and enjoyable
Some people like to walk on a treadmill at the gym. Others find that kind of activity boring. The key to sticking with exercise is to make it interesting and enjoyable. Be creative. Do things you enjoy but pick up the pace. Do all four types of exercise— endurance, strength, balance, and flexibility. The variety helps keep things interesting! Try some new activities to keep your interest alive.
2. Find ways to fit exercise into your day
You are more likely to exercise if it’s a convenient part of your day. Try exercising first thing in the morning. Combine physical activity with a task that’s already part of your day, such as walking the dog or doing household chores. If you don’t have 30 minutes to be active, look for three 10-minute periods. As you progress, add more 10-minute sessions until you hit your goal!
WORK OUT AT WORK
There are many ways to fit physical activity into your regular schedule, even while you are at work! Look for easy
• Park a little farther away from your office and enjoy the walk.
• Join your company’s fitness center if there is one.
3. Make exercise a social activity
Many people agree that an “exercise buddy” keeps them going.
• Take a walk during lunch with coworkers.
• Try a dance class—salsa, tango, square dancing—it’s up to you!
• Use family gatherings as a time to play team sports or do outdoor activities.
4. Keep track of your exercise progress
The best way to stay motivated is to measure and celebrate your successes:
• Make an exercise and physical activity plan that works for you and track your daily physical activity. (PDF, 345K)
• Find new ways to increase your physical activity.
• Keep track of your monthly progress to see improvement.
It is normal to have life events and changes get in the way of staying active. However, there are ways to get yourself back on track. Remember, to get the most out of exercise and physical activity, they need to be a regular part of your life.
You’re on vacation:
• Many hotels now have fitness centers. Check out the facilities where you’ll be staying, and bring along your exercise clothing or equipment (resistance band, bathing suit, or walking shoes).
• Get out and see the sights on foot rather than just by tour bus.
Caring for an ill spouse is taking up much of your time:
• Work out to an exercise video when your spouse is napping.
• Ask a family member or friend to come over so you can go for a walk.
Your usual exercise buddy moves away:
• Ask another friend to go with you on your daily walk.
• Ask other older adults in your area where they go for walks or what
physical activity resources are available nearby.
• Join an exercise class at your local community center or senior center. This is a great way to meet other active people.
You move to a new community:
• Check out the fitness centers, parks, and recreation associations in your new neighborhood. Look for activities that match your interests and abilities.
• Get involved!
The flu keeps you out of action for a few weeks:
• Wait until you feel better and then start your activity again.
• Gradually build back up to your previous level of activity.
You are recovering from hip or back surgery:
• Talk with your doctor about specific exercises and activities you can do safely when you’re feeling better.
• Start slowly and gradually build up your activities as you become stronger.
Source: National Institute on Aging. Read more at nia.nih.gov.

TECHNOLOGY
Is AI Age-Friendly?
The annual ASA conference in San Francisco this past year included a panel that addressed the question: “Is AI Age Friendly?” In addition to four in-person panelists (of which I was one), the session started with a video presentation from a fifth participant who provided a short introduction to the topic, identifying some of the potential uses of AI to improve the lives of older adults but also noting some of AI’s potential problems.
As you may have surmised, this attractive and articulate presenter was not human. In fact, prior to the session, one of the panelists, Davis Park, had logged on to Chat GPT and given it the following prompt: “create a script for a narrated video under 2 minutes about how Generative AI can help older adults, and outline some of the things we should be careful about.” He briefly edited the resulting script, then submitted it to heygen.com, an AI-powered platform that allows users to generate high-quality videos featuring realistic human speakers. According to Davis, the entire process required a total of about 20 minutes.

‘Early trials of AI have shown success in rapidly and accurately interpreting medical test results.’
Because Generative AI, even in its current form, is so useful and so easy to use, it has already been integrated into many existing software programs and implemented for a wide range of business applications, including marketing and advertising, customer support, software development, and finance and banking.
Not surprisingly, there has also been a lively interest in Generative AI among providers of services to older adults, who are excited about the technology’s potential to improve the lives of older people by improving the delivery of health care and accelerating the development of new medical treatments, improving the effectiveness of services for older adults, and empowering them with new tools for managing their lives.
Some Promising Uses
Following this introduction, which demonstrated the power as well as some of the limits of the technology, the four of us humans shared our views of this question. Here is our summary:
What’s the Big Deal About Generative AI?
Even though the field of AI is more than 50 years old, Generative AI, introduced just two years ago, represents perhaps the first major paradigm shift since computers were invented in how humans interact with them. Traditionally software has been designed to follow user commands to carry out a specific action (e.g., perform a calculation, retrieve data) based upon predefined rules or logic. Generative AI goes beyond this by autonomously generating new content. Rather than being programmed in advance, Generative AI uses learned patterns from vast datasets (known as large language models, or LLMs) to write essays, generate artwork, compose music, and even create code in response to a simple conversational query.
And because the power of Generative AI is continually being improved, many experts have predicted that this technology will, in a relatively short time, achieve what is known as Artificial General Intelligence (AGI), which means it will essentially equal the cognitive flexibility and problem-solving skills of human beings.
Generative AI already has demonstrated its potential in a number of different areas to improve the quality of health care. For example, early trials of AI have shown success in rapidly and accurately interpreting medical test results, in some cases identifying patterns of symptoms that are too subtle for humans to identify.
Another experiment found that doctors assisted by an AI chatbot did better than a control group without AI in making decisions about how to treat complex medical cases. Generative AI also is accelerating the process of drug discovery by identifying promising drug candidates, as well as finding new uses for existing drugs. And on a practical level, Generative AI is saving physicians time by automating the process of preparing notes from clinical sessions with patients and drafting responses to patients’ email messages.
Generative AI also is being used to improve products and services designed for older adults. For older adults with severe hearing loss, a company called Xander has developed a pair of smart glasses equipped with microphones that use AI to capture speech and project a transcript of what is said that is visible only to the wearer. For people who are blind, Envision has created AI-
powered glasses that can read text aloud, detect colors, describe a scene, or recognize a face.
Monitoring systems, such as Care Predict, have incorporated AI to spot changes in the patterns of activity of older adults living alone that may indicate an increased propensity to fall or other health risks. AI-based services like Lumosity offer AI-generated mind-training games aimed at improving memory and cognitive function. Chatbots like Elliq and care.com are designed to act as AI companions that can combat the isolation of older adults by engaging them in conversations on topics of interest to them, as well as providing timely reminders about taking medications or engaging in healthy physical activity.
Some Caveats
Given how recent Generative AI is, this flurry of activity is impressive. Chatbots have already been used by more than 100 million people, making Generative AI the fastest growing app of all time. But these are still early days, and there are reasons for caution, if not skepticism about where these new capabilities may be taking us, particularly when it comes to their use with older adults. It is always wise to remember that every technology can be a two-edged sword—it could come with unintended consequences that can cause harm as well as bringing benefits.
Here are a few more caveats to keep in mind:
First, Generative AI programs create responses based upon what they have learned from extremely large sets of existing content (LLMs). Unfortunately, ageist messages are widespread in our culture and online, with countervailing content often hard to find. To the extent that the input side of the AI learning space reflects a prevalence of ageist stereotypes and negative points of view, Generative AI is likely to replicate biased messaging in its outputs. While users can create prompts to correct for bias, there is a real possibility that, as the general public engages with AI tools over millions of interactions, the AI programs will magnify negative bias against older adults.
There is a real possibility that AI programs may magnify negative bias against older adults.
Second, AI tools are making it more possible to replace in-person care with digitized services. Over time, this could result in fewer care providers and more social robots, less human touch, and more technology to care for older adults. If AI provides medical care, social interaction, entertainment, and other services without the need for in-person staffing, it could lead to reduced employment in senior care and a further reduction in the human capital dedicated to caring for older adults.
Third, AI may serve as a great accelerator of predatory behavior against older adults. Seniors are already disproportionately targeted with scams, fraud, and misinformation: Calls from people pretending to be a relative in trouble, offers that are too good to be true, password phishing emails. As AI enables more sophisticated, personalized, and lifelike impersonations of people and circumstances, attacks on the security and finances of older adults will become more effective, further increasing the risks for older people who participate in the digital world.
Finally—and perhaps fortunately—the pace of change may be considerably slower than AI enthusiasts are predicting. There remain significant obstacles to full-scale implementation of AI, including inconsistent factual reliability (“hallucinations”), problems with copyright and intellectual property of the source materials used to train AIs, and the potential for regulatory restrictions.
It’s worth remembering that other technology breakthroughs in recent decades—such as self-driving cars, social robots, and virtual reality environments—that had been touted as “gamechangers” for older adults have failed to be widely deployed. In general, older adults tend to be “late adopters” of new technologies, and AI may be another example of this pattern. For those who are hoping for dramatic improvements in senior care and services from AI, some timeline caution is in order. This slower pace could provide the opportunity to be thoughtful, and a bit cautious, about how potential AI applications are developed and deployed.
Source: Generations, American Society on Aging. Read more at generations.asaging.org.


| 740-363-6677
Easy Sudoku Booklet #1 - Solutions
Sudoku Solutions











