
11 minute read
Exams May be Cancelled, but Humanity is Not: A Medical Student Perspective on the COVID-19 Pandemic
from Delaware Journal of Public Health - Health Sciences Education / COVID-19 special section
by Delaware Academy of Medicine and the Delaware Public Health Association
Exams May be Cancelled, but Humanity is Not: A Medical Student Perspective on the COVID-19 Pandemic
Elizabeth Avakoff, M.P.H. and Omneya Ayoub, M.S.; Philadelphia College of Osteopathic Medicine
“Stay at home!” Public health pleas to help “flatten the curve” amidst the COVID-19 pandemic have led to a wave of societal disruptions. Social distancing, defined as keeping yourself at least six feet away from others and avoiding gatherings of ten or more people, has become the new norm for Americans over the past three weeks. These (among other) dramatic societal changes and growing pressure on our nation’s hospital systems have had a distinct impact on medical education, particularly when it comes to clinical training. As third year medical students, our professional development has heavily relied on in-person clinical experiences, directly interacting with patients and healthcare providers. However, with the national push for a 14-day quarantine, students across the country were pulled from their clinical settings until further notice. 1,2 In a vast departure from our normally structured path to residency, licensing examinations were also temporarily suspended and our professional lives were placed on hold. 3 Medical education institutions across the country have faced the challenge of inventing new ways of supporting student learning in these critical years of clinical training. In many medical schools, this has led to the roll-out of new virtual clinical experiences and greater utilization of dynamic, online training modalities. Students at the University of Illinois, for example, are observing procedures through video conferencing and utilizing mock scenarios to prepare for future patient encounters. 4 Likewise, on the East Coast at the Philadelphia College of Osteopathic Medicine, students log-in to live virtual journal clubs, lectures and morning reports. These “online clerkships” support students’ continued professional development and progression through educational requirements. In an informal survey of medical students across the country, there was a resounding concern for what the sweeping societal changes would mean for our residency preparations and our clinical training overall. Simultaneous with online learning, medical students have taken ownership over their residency preparedness, utilizing their additional time to work on personal statements, curriculum vitaes, and study for licensing examinations. Students also expressed concern for their mental health in these uncertain times, finding relief in connecting with family and friends and catching up on much needed self-care. Whether revisiting lost culinary skills, reading a new book, or even going for a run, many have found this time at home to be grounding and introspective. As medical students, we are constantly engrossed in our education and learning the details needed for each progressive step in our training. This new time out of the hospital has allowed us to take a step back and in light of our nation’s COVID-19 response, see the system as a whole from a new perspective. At the same time, we have not lost sight of our colleagues and mentors on the frontlines in this pandemic. In fact, students across all healthcare professions have voiced an earnest desire to do our part in the COVID-19 pandemic. 5 Through the power of social media, communities across the MidAtlantic have seen an outpouring of volunteerism, donations and camaraderie amongst students across the healthcare spectrum. Through Facebook groups such as the “Philadelphia Organization of Health Professions Students - COVID Response,” 6 nearly 2,000 students in nursing, medicine, dental medicine, podiatry, veterinary medicine and physician assistant programs have come together for a united goal of stepping off the sidelines. This group has allowed students to collaborate, allocate resources, spread awareness and collect much needed personal protective equipment from the community. From blood drives, to child and pet care for healthcare workers, to meals for our region’s most vulnerable populations, this group continues to develop innovative ways of supporting our mentors, colleagues and patients from our new positions at home. Through this enthusiasm for public service, our Mid-Atlantic medical and allied health professions students have found a way to continue making a difference, while forging new inter-professional cross-collaborations. As our nation learns some hard and invaluable lessons in the spread and management of infectious diseases, emergency preparedness, and population health, we too have found this period to be transformative. The COVID-19 pandemic has shed new light on our individual roles as future physicians in the greater community at large. Students have expressed a greater appreciation for the physician’s role in population health, citing the importance of elevating public awareness, preventing the spread of infectious diseases and having resources on hand to effectively treat large numbers of critically ill patients. As future physicians, we are witnessing humanity at one of its most vulnerable times, not only for our nation, but across the world. In this transformative period, “stay at home” has thus become more than a blanket directive to self-isolate. To us, it represents a civic responsibility to protect one another from unnecessary exposures and a movement to individually and collectively do our part in this COVID-19 pandemic. REFERENCES 1. Madhani, A. (2020, March 15). Top US infectious disease expert open to a 14-day ‘national shutdown’ to combat virus spread. Chicago Tribune. Retrieved from https://www.chicagotribune.com/ coronavirus/ct-nw-coronavirus-national-shutdown-infectiousdisease-20200315-abn7gckptbd6tch24nlewgr2je-story.html 2. Ostrov, B. F. (2020, March 17). In Face Of Coronavirus, Many
Hospitals Cancel On-Site Training For Nursing And Med Students. Kaiser Health News. Retrieved from https://khn.org/news/in-faceof-coronavirus-many-hospitals-cancel-on-site-training-for-nursingand-med-students/ 3. American Medical Association. (2020, March 19). Resident & medical student COVID-19 resource guide. Retrieved March 26, 2020, from https://www.ama-assn.org/delivering-care/public-health/ resident-medical-student-covid-19-resource-guide 4. Cheung, A. (2020, March 25). Just as the need soars for health care workers to fight coronavirus, Chicago-area medical students are sidelined from seeing patients. Chicago Tribune. Retrieved from https://www.chicagotribune.com/coronavirus/ ct-coronavirus-medical-school-rotations-chicago-20200323- dn2h3gzbwrd3hgo6ga3iwpmsmu-story.html 5. Lee, Y. J. (2020, March 24). The coronavirus is preventing medical students from getting hands-on training in hospitals. Frustrated future doctors are looking for new ways to help. Business Insider. Retrieved from https://www.businessinsider.com/medical-studentstaken-off-hospital-rotations-want-to-help-2020-3 6. Philadelphia Organization of Health Professions Students - COVID
Response. (2020, March 20). Facebook. Retrieved from https://www. facebook.com/groups/152353182650533/


Coronavirus disease (COVID-19) arrives in Delaware The global outbreak of coronavirus disease (COVID19), reached Delaware on March 11, the same day the World Health Organization (WHO) named it a pandemic. As of March 29, 232 laboratoryconfirmed cases in the state have been reported to the Division of Public Health (DPH) since March 11. The Delawareans diagnosed with COVID-19, by county, are: New Castle County, 141; Kent County, 25; and Sussex County, 66. Nine Delawareans have recovered from COVID-19 and six have passed away due to COVID-19 complications. Thirty-three individuals are currently hospitalized; nine are critically ill. Of the 232 cases, 114 are male and 118 are female; ages range from 1 to 90. The source of exposure for many of these positive cases is unknown, which indicates community spread of the virus is occurring in the state. “Sick persons should not leave their homes, especially if they have fever, cough, shortness of breath, vomiting, or diarrhea; and they should call their health care provider,” said DPH Director Dr. Karyl Rattay. “Those who are well should practice social distancing (6 feet or more from others), practice good hygiene, and clean and sanitize commonly touched surfaces every day. We all have to behave as if we are carrying the virus.” COVID-19 was first detected in mainland China in December 2019. In its M arch 29 Situation Report, WHO reported 634,835 confirmed cases worldwide and 29,891 deaths.

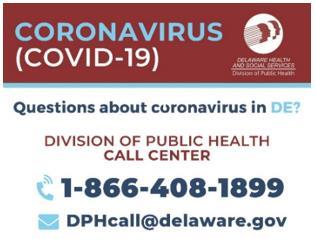
DPH encourages residents who are well to practice social distancing (keeping at least six feet away from others) and avoiding large gatherings or crowds. Individuals with underlying conditions should be especially careful and contact their primary provider if they have any COVID-19 concerns. Individuals who are sick, particularly with fever, cough, and shortness of breath, should stay home and contact their primary health care provider for guidance. COVID-19 symptoms include fever, cough, and shortness of breath and may appear between two and 14 days after exposure. Reported illnesses range from people with little to no symptoms (similar to the common cold) to people being severely ill and dying. While some ill individuals are hospitalized, many recover by resting, drinking plenty of liquids, and taking pain and fever-reducing medications. The CDC recommends that all individuals, especially those who are age 65 and older and those with chronic underlying health conditions: • Stay home. • Wash your hands often with soap and water. • Avoid touching your eyes, nose, and mouth. • Avoid all cruise travel and non-essential air travel. • Avoid close contact with people, especially those who are sick, by keeping six feet away. • Clean and disinfect frequently touched surfaces. • Have enough household items and groceries on hand so you are prepared to stay at home for a period of time. • Have a plan in the event you get sick and discuss with household members, other relatives, and friends what you might need. For the latest information on Delaware’s response, visit de .gov/coronavirus. Those with general COVID-19 questions can call DPH’s Coronavirus Call Center at 1-866-408-1899, or 711 for individuals who are hearing impaired; or email DPHCall@delaware.gov. Hours of operation are 8:30 a.m. to 6:00 p.m. Monday through Friday, and 10:00 a.m. to 4:00 p.m. Saturday and Sunday.
DHSS Press Release
Dr. Kara Odom Walker, Secretary Jill Fredel, Director of Communications Cell: 302-357-7498 Email: DPHMedia@Delaware.gov Date: April 8, 2020 DHSS-4-2020
COVID-19 UPDATE FOR APRIL 8, 2020: DPH ANNOUNCES 188 ADDITIONAL POSITIVE CASES; 30 ADDITIONAL HOSPITALIZATIONS; THREE NEW DEATHS
SMYRNA (April 8, 2020) — The Delaware Division of Public Health (DPH) is announcing three additional fatalities related to coronavirus disease 2019 (COVID-19) and is providing an update on the number of positive cases and recovered individuals.
In total, 19 Delawareans have passed away due to complications from COVID-19. Nine of the deaths have been related to longterm care facilities, including eight in New Castle County (six at Little Sisters of the Poor) and one in Sussex County.
The most recent individuals who died were hospitalized and had underlying health conditions including a: • 88-year-old male long-term care resident from New Castle County • 74-year-old female from Sussex County • 81-year-old male from New Castle County
To protect personal health information, DPH will not disclose additional information about the individuals who passed away, nor will DPH confi rm specifi c information about any individual case, even if other persons or entities disclose it independently.
The latest Delaware COVID-19 case statistics, cumulatively since March 11, include: • 1,116 total laboratory-confi rmed cases • New Castle County cases: 636 • Kent County cases: 201 • Sussex County cases: 279 • Males: 495; Females: 614; Unknown: 7 • Age range: 1 to 97 • Currently hospitalized: 177; Critically ill: 51 (This data represents individuals currently hospitalized in a Delaware hospital regardless of residence, and is not cumulative.) • Delawareans recovered: 159 • 8,323 negative cases* *Data on negative cases are preliminary, based on negative results reported to DPH by state and commercial laboratories performing analysis.
DPH epidemiologists are transitioning to a new data reporting system. During the transition period, not all fi elds (sex) have complete information.
Delaware is considering patients fully recovered seven days after the resolution of their symptoms. Three days after symptoms resolve, patients are no longer required to self-isolate at home; however, they must continue to practice strict social distancing for the remaining four days before returning to their normal daily routine.
Widespread community transmission is occurring throughout the state, which means COVID-19 is actively circulating in the community. If you are sick with any of the following symptoms, stay home: fever, cough, shortness of breath, sore throat, muscle fatigue, or digestive symptoms such as vomiting, diarrhea, abdominal pain or lack of appetite. If you are sick and need essential supplies, ask someone else to go to the grocery store or the pharmacy to get what you need.

If you think you have been exposed to someone with COVID-19, or have symptoms of illness, make sure to distance yourself from others, particularly vulnerable populations. Older adults and people of any age with serious underlying medical conditions - including serious heart conditions, chronic lung conditions, including moderate to severe asthma, severe obesity and those who are immunocompromised, including through cancer treatment - might be at higher risk for severe illness from COVID-19.
Statewide testing at standing health facility testing sites require a physician’s order or prescription to be tested (*Bayhealth patients will be pre-screened via phone without needing to see a provider fi rst). These are not walk-in testing sites. Those without a primary care provider can call the DPH Call Center Line at 1-866-408-1899. In New Castle County, individuals can call ChristianaCare at 1-302-733-1000 and Sussex County residents who do not have a provider can call the Beebe COVID-19 Screening Line at 302-645-3200. Individuals awaiting test results, should wait to hear back from their medical provider. The DPH Call Center does not have test results.
DPH began a new collaboration with the United Way of Delaware to better triage incoming calls related to COVID-19. Anyone with a question about COVID-19, whether related to medical or social service needs, should call Delaware 2-1-1; or 7-1-1 for individuals who are deaf or hard of hearing, or text your ZIP code to 898-211. Hours of operation are 8 a.m. to 9 p.m. Monday through Friday; 9 a.m. to 5 p.m. Saturday and Sunday.
In addition, the Division of Public Health asks any Delaware health care, long-term care, residential, or other high-risk facility with questions or concerns to email: DPH_PAC@delaware.gov or call the DPH Call Center at 1-866-408-1899 and press ext. 2.
Questions can also be submitted by email at DPHCall@delaware.gov.
DPH will continue to update the public as more information becomes available. For the latest on Delaware’s response, go to de.gov/coronavirus. ###








