Walking Straight Into Retirement
Network Health member, Dewey, shares how knee replacements gave him his life back and new hope for the future.
2023
LIFE, HEALTH & WELLNESS A PUBLICATION OF
EDITORIAL STAFF

Chief Administrative Officer Penny Ransom
Strategic Marketing and Communications Manager Romi Nor ton
Strategic Marketing and Communications Coordinator Julie Heinzel
Graphic Designer Jami Greshay
ASK NETWORK HEALTH
If you have questions about anything you read in this issue of Concierge, call the member experience team at 855-232-2814 (TTY 800-947-3529) Monday–Friday, 8 a.m. to 5 p.m. We're available every day, 8 a.m. to 8 p.m. October 1–March 31
Concierge is an annual publication of Network Health. The health information contained in Concierge is meant to supplement, not replace, the advice of health care professionals. © 2023 Network Health Insurance Corporation. No portion of this newsletter may be reproduced without written permission from Network Health Insurance Corporation.
In this issue of Concierge, we’ll focus on providing you with informative content and great feature stories about our members. Additional content and articles are available on our blog, Grow In the Know; and through social media.
If you’d like to go paperless and receive Network Health communications via email, select your communication preferences through your member portal at login.networkhealth.com. Log in (or create an account if you haven’t yet), click your name in the upper right corner and select Change My Communication Preferences. From there, choose email for any or all the available categories.
Connect With Us Here
H5215_4673-01b-0823_C
lif e. health. wellness. networkhealth.com 2 | C on C ierge • 2023 11 6 CONTENTS 3 Join Us In the Community 3 New Green Bay Packers Partnership 4 Test Your Digital Literacy 5 Do You Love Your Network Health Medicare Advantage Plan? 5 Requir ed Information FEATURE STORY 6 Walking Straight Into Retirement 9 Ther e Are Pharmacists at My Health Plan? 10 Complementar y and Alternative Medicine, What Does This Mean? 10 Social Deter minants of Health 11 Exchange of Information BACK COVER Network Navigate: We'll Be Your Guide Plan Business Phone Calls
Join Us In the Community
At Network Health, living and working in the areas we serve allows us to focus on our mission of building healthy and strong Wisconsin communities. Whether it’s a farmer’s market, local health fair or volunteer experience, you can find your Network Health team at events throughout Wisconsin.


To find an event near you, visit networkhealth.com/community or scan the QR code using the camera on your phone.
New Green Bay Packers Partnership
Partnering with the Green Bay Packers supports Network Health’s mission of creating healthy and strong Wisconsin communities. And, as the sponsor of the Packers’ Operation Fan Mail, we can help honor military families and veterans in our communities who exhibit excellence and performance throughout their lives. We are grateful for our military service members and through this sponsorship, we’re able to show our appreciation. The Green Bay Packers have a long tradition of excellence and performance, something Network Health stands behind. We look forward to partnering with another Wisconsin-based organization like the Packers, who share our mission and values. If you're a Packer fan, you'll see more of Network Health than ever before. Go Pack Go!
networkhealth.com 2023 • C on C ierge | 3
Test Your Digital Literacy
By Amber Smits, quality revenue and health equity program manager Laura Schneider, member experience process lead
The most important person on your health care team is not your doctor, it’s you. One way to stay healthy and get involved in your care is by keeping track of your health and insurance benefits by using the free tools, information and trackers found in your Network Health member portal.
Your member portal is the gateway to secure information about your Network Health plan. In it, you’ll find links unique to you as well as tools, tips and important information to help you enhance your life, health and wellness. Access your personal member portal at login.networkhealth.com, or visit networkhealth. com/portal-guide for instructions on how to get started.
Millions of older adults are motivated to get online and participate in digital offerings after remaining inside during the pandemic. Many need assistance and aren’t sure where to get it.
Digital Health Care Literacy Scale
A recent survey from The American Association of Retired Persons (AARP) discovered that older adults boosted technology purchases during the pandemic, with 54 percent stating they need a better grasp of the devices they’d acquired. Nearly four in 10 people admitted they weren’t confident about using these technologies.
Apply the best point score to each of these questions, then add them up to learn your personal digital literacy level. The higher the score, the higher your digital health care literacy.
Digital Health Care Literacy Scale Score
I can use applications or programs (like Zoom) on my cell phone, computer or another electronic device on my own, without asking for help.
I can set up a video chat using my cell phone, computer or other electronic device on my own, without asking for help.
I can solve or figure out how to solve basic technical issues on my own, without asking for help.
I don’t feel comfortable, but I have dependable access to someone to help me.
Response options
Strongly disagree = 0 points
Disagree = 1 point
Neutral = 2 points
Agree = 3 points
Strongly agree = 4 points
Sum scores of individual items to create your total score. Possible scores range from 0 to 16, with higher scores indicating higher digital health care literacy.
If you scored eight or below on the digital health care literacy scale, you may benefit from extra help on how to navigate digital health care. If you would like additional assistance, contact your Network Health Member Experience Team at 855-232-2814 (TTY 800-947-3529) for information on resources and events in your area.
lif e. health. wellness. networkhealth.com 4 | C on C ierge • 2023
Total Score Scale adapted from cmsatoday.com and formative.jmir.org.
Do You Love Your Network Health Medicare Advantage Plan?
If you love the high-quality service and support you receive from Network Health, share your excitement with your friends and family and get them that same service in 2024.
Our Medicare member referral program continues and is very popular amongst our current members. We have you to thank for that. Our referral program allows you to earn gift cards for sharing Network Health with your friends and family. You can earn up to four $15 gift cards for a variety of stores each year.*
The people you refer must meet these criteria.
Have Medicare Parts A and B Reside in our service area
Are not already enrolled in a Network Health plan
Simply have your friends or family members call our Wisconsin-based sales advisors at 844-850-5284 (TTY 800-947-3529), Monday–Friday from 8 a.m. to 8 p.m. From October 1–March 31, they’re available every day from 8 a.m. to 8 p.m. When you refer someone to Network Health, you’ll receive a phone call from a Network Health employee to determine which gift card you want.
*Licensed agents who are appointed with Network Health are not eligible for these gift cards
Required Information
There are several organizations that exist to help improve the quality of health care across the United States, including the National Committee for Quality Assurance (NCQA), the Wisconsin Office of the Commissioner of Insurance (OCI) and the Centers for Medicare and Medicaid Services (CMS). They use a variety of performance measurement tools and regulations to help ensure consumers are protected and receive quality health care services.
You can find a downloadable PDF of this information at networkhealth.com/required-info. If you do not have access to the internet and need a hard copy of the NCQA information, please call our member experience team at the number on the back of your Network Health member ID card.
At the link provided, you'll find information on these specific topics.
• Access to Network Health Care Management Employees and Services
• Ensuring You Receive the Service You Deserve
• Falls/Osteoporosis
• The Impor tance of Exchanging Information
• Keep Yourself Safe from Medicare Fraud
• Know Your Member Rights and Responsibilities
• Networ k Health’s Focus on Quality
• Submitting a Claim for Reimbursement
• What is Population Health Management?
networkhealth.com 2023 • C on C ierge | 5
WALKING STRAIGHT Into RETIREMENT
 By Julie Heinzel
By Julie Heinzel
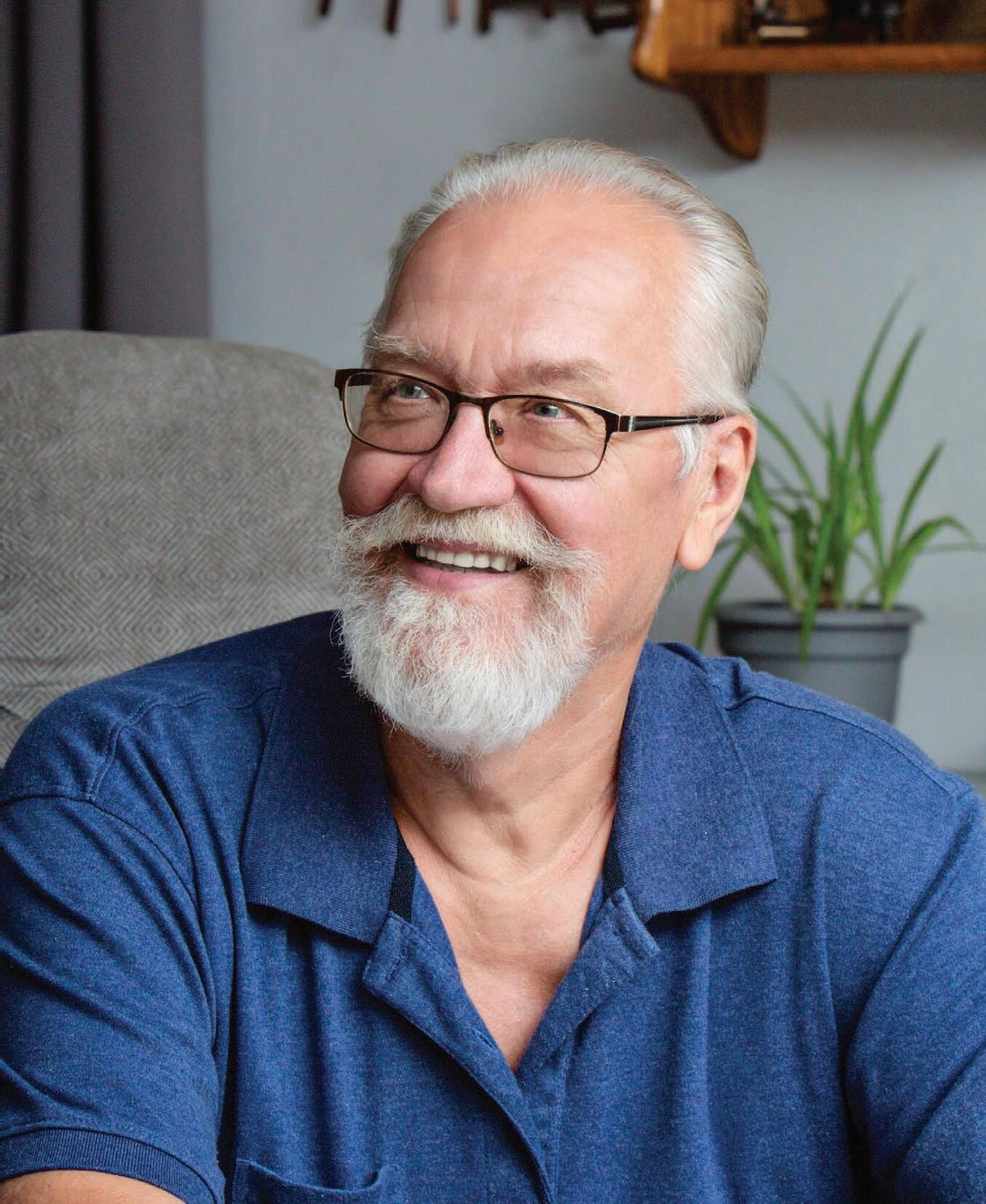
Dewey and Linda are pictured together on their vacation to South Dakota. On this vacation, Dewey wanted to take Mount Rushmore’s walking tour, but was not capable. They came home from vacation and called Dr. Eggert right away to schedule a consultation.

6 | C on feature story
Photography by Beth DesJardin, Trove Photography
Like many of you, Dewey and his wife Linda were headed into retirement ten years ago and looking forward to this new phase in their lives together. Their plans included more time with their three children, 12 grandchildren and seven great-grandchildren on the lake, daily meetups with their friends and neighbors, but mostly, the option to travel more. They love to explore, go off the beaten path on road trips to Colorado, South Dakota, Florida and other states.
At the time of retirement, they became Network Health members after attending a seminar, researching their options and speaking with friends and their agent about their experiences.
They were simply told “Network Health is the one you want.” Linda explained, “There were so many different options we could have. We’ve only got a basic plan since we don’t need a lot of medications and it works wonderfully for us.”
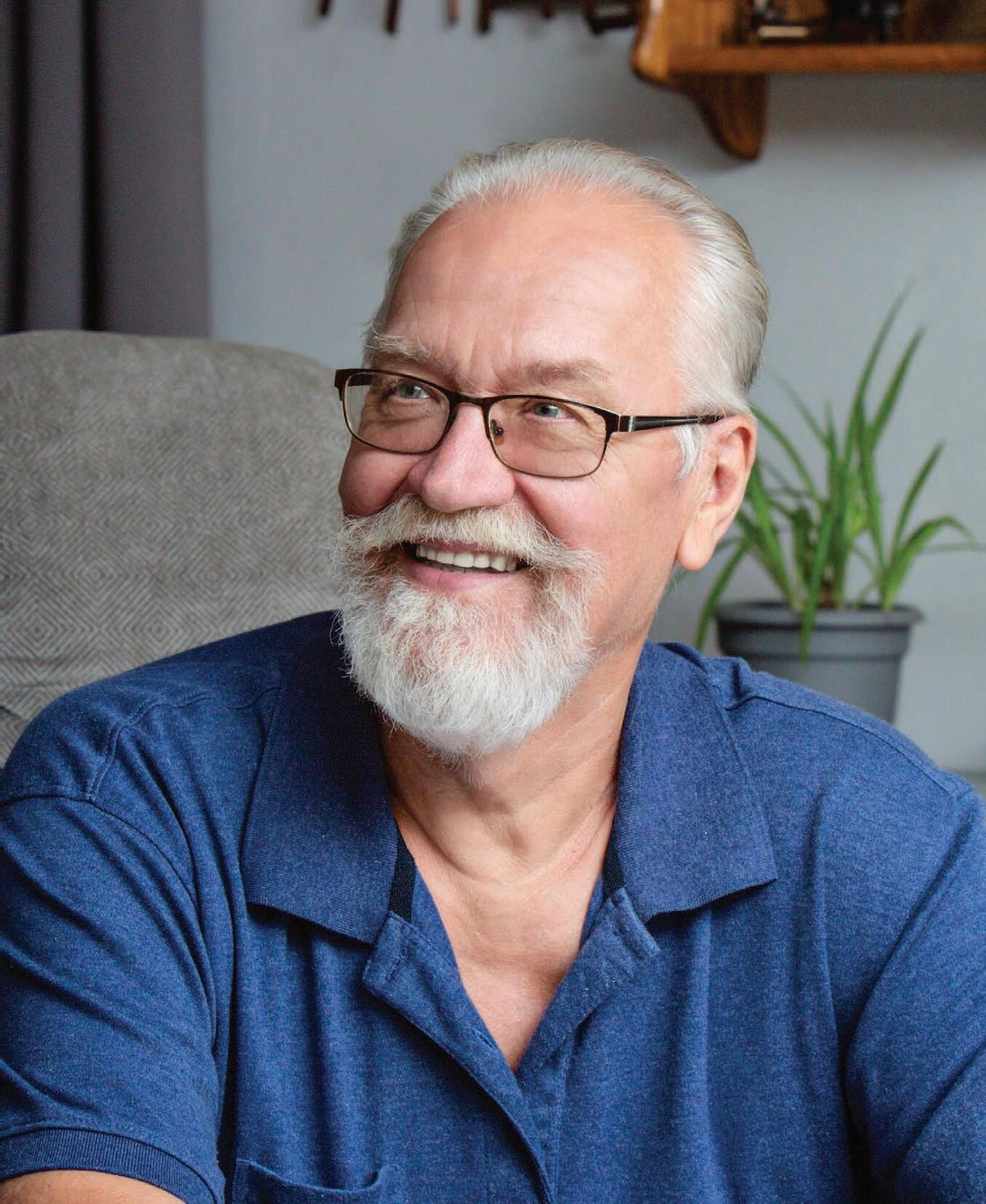
Dewey worked as an operating engineer for heavy machinery and since retiring, he continues to keep himself busy building wood projects, maintaining the local cemetery grounds, hunting, chopping wood and maintaining their beach lot on the lake. Most of their home was built by Dewey from 2016 to 2019. He walks with his neighbors on a regular basis and was planning on completing the challenge of a 5K. There is not much that slows him down.
Dewey’s legs have been severely bowed his whole life. He always had occasional pain and it became more frequent about five years ago. He pushed through and didn’t let the increased pain stop the activities he enjoyed most. The pain became more intense last August and grew quickly while on vacation in South Dakota a month later. That’s when he had enough.
I didn’t want to get up from my chair to walk to the mailbox because every step hurt. I was paralyzed. My quality of life was declining. There is nothing like chronic pain, it takes over your life.
Linda dove right into researching options for Dewey. That is when she found Dr. Eggert, a Board-Certified Orthopedic Surgeon, who has been practicing for 35 years. Dr. Eggert performs robotic joint replacements at the Orthopedic & Sports Institute of the Fox Valley in Appleton. He believes in the success of robotic replacements not only for his patients but for himself. He has had both hips replaced in this way.
“Dewey had so much deformity and the x-rays were significant, so the treatment was obvious,” Dr. Eggert explained. They discussed the options, and robotic joint replacement was the best option for Dewey.
He was not comfortable sitting, standing or walking and when the pain started waking him up at night, he knew he had to do something.
He walked out of the consultation feeling confident that it would work for him.
Luckily, there was coverage for Dewey’s robotic knee replacement surgery. Dewey shared, “I believe in robotic surgery. My knees would not have turned out as good as they did without it. Other plans don’t cover it, but Network Health does. There’s an advantage with going with Network Health.”
Over the last six years, Dr. Eggert has performed close to 2,000 robotic joint replacements. He explained, “Robotics is so accurate and reproducible and gives patients such a great result, like Dewey. It’s so satisfying for me to be able to offer it to those who truly need it.”
Dewey went on to explain the similarities between his experience with Dr. Eggert and Network Health. “We knew what we were getting into right from the start, it was all laid out for
networkhealth.com 2023 • C on C ierge | 7
Dewey P., Network Health member
Dewey P., Network Health member
I’m a hard person to convince. I’m the guy that says ‘never’, but I really needed it, so I did not delay.
us. Everything was explained to us, they made it simple. I didn’t have to think or worry about anything, just focused on healing.”
Dr. Eggert cares about his patients’ success and goes out of his way to connect with them throughout the process. He thoroughly explains and draws pictures of the procedure to help patients better understand. He calls them the night before surgery to answer questions and remind them of the prep-work that is needed. He calls again post-surgery to review therapy, pain medications and other simple, yet important, things. “They are given a lot of instructions to remember, it’s important,” explained Dr. Eggert.
Linda is comfortable using their Network Health member portal to review claims and track their progress. They stayed on top of the information that followed surgery that way. They knew exactly what was coming, the information was easy to understand and they appreciated how much the member portal cut down on the amount of paper they received.
Linda shared, “For us, we’ve been really happy with Network Health … really happy. I love the choices. We tell our neighbors about our experience. We tell them ‘You should have our insurance’.”
Their 55th wedding anniversary was spent replacing Dewey’s first knee on November 4, 2022. He proudly shared, “In three days, I threw away the walker. In three more days, I threw away the cane. Six weeks later, I had the other knee done. I’ve been walking ever since.”
He stuck to his therapy which helped him recover fully. He feels taller, stronger and more energetic than ever. Their family and friends laugh that they no longer recognize him from behind.
Before surgery, Dewey could not stand for longer than two minutes before having to sit down. Now, he is back on his feet, headed forward, with straight legs, back into the enjoyment of retirement.

networkhealth.com 8 | C on C ierge • 2023
feature story
Dewey P., Network Health member
I’m a different person, it’s life-changing.
By Beth Coopman, pharmacist




Network Health employs clinical pharmacists to support medication access and affordability for all members. These pharmacists are experts on knowing our formulary. Interactions with the pharmacy team can range from one-on-one connections to behind-the-scenes work, all with the goal of enriching your pharmacy plan experience.
You may get a call from a Network Health Pharmacist regarding a Comprehensive Medication Review (CMR), which is a part of the Medication Therapy Management (MTM) program. The MTM program is required by the Centers for Medicare & Medicaid Services (CMS) to be offered to Medicare Part D members and it contributes to Network Health’s Medicare Star Rating. The call takes about five minutes and provides the opportunity to review medications and discuss the topics of affordability, timing of medications, side effects, drug interactions and more. We do this because successful management of medications is important for your overall health. For example, the MTM program helped one member switch to a local pharmacy, which lowered the cost of their medication, saving them over $8,000 this year.
Qualification for the MTM program is year-round and is based on members having eight or more chronic medications, three or more chronic conditions and an estimated yearly medication spend of at least $4,935. These calls will come from either the Network Health Clinical Pharmacist Team or SinfoniaRx, an MTM company that assists Network Health with the completion of CMRs.
In addition, Network Health Clinical Pharmacists work on projects to help you in a variety of ways. Past projects were focused on how to get certain medications at a more affordable rate and how to optimize therapy by eliminating high cost/low value products.
Finally, Network Health Pharmacists participate in teaching community programs that provide education on preventing or living with diabetes, preventing the risk of falls with medications and more. They participate in flu shot clinics, member advisory board discussions, new and existing member event presentations and educational videos.
There Are Pharmacists at My Health Plan? PHARMACY TEAM
Unlike other health plans, Network Health offers all members a direct phone line to our pharmacists. The toll free number is 888-665-1246. You can also email them at pharmacist@networkhealth.com
networkhealth.com 2023 • C on C ierge | 9
Sarah Wilczek
Beth Coopman
Anna Peterson Sanders
Gary Melis
Complementary and Alternative Medicine, What Does This Mean?
By Sarah Dencker MSN, RN, vice president of care services
Complementary and alternative medicine can be the term used for medical products and practices that are not part of standard medical care. Standard medical care is treatment that is accepted by medical experts as proper treatment for certain conditions and is widely used by health care professionals.

When deter mining coverage for the services you receive, Network Health follows standard medical care practices, ensuring the care and treatment you receive is safe and effective. Network Health does not typically cover services that are considered complementary or alternative medicine. We want you to be aware to protect yourself from unexpected financial burden.

Some examples of complementary and alternative medicine not covered include, but are not limited to, the following.
• Meditation
• Vitamins/minerals
• Tai chi
• Reiki therapy
• Botanicals (plants such as herbs and spices)
If you have questions about whether a particular complementary or alternative product or practice is covered, call your Network Health Member Experience Team at 855-232-2814 (TTY 800-947-3529) Monday–Friday, 8 a.m. to 5 p.m. From October 1–March 31, seven days a week.
Social Determinants of Health
By Amber Smits, quality revenue and health equity program manager

According to the Centers for Disease Control and Prevention (CDC), Social Determinants of Health (SDoH) are conditions in the places where people live, learn, work and play that affect a wide range of health risks and outcomes. Studies indicate that medical care only accounts for around 20 percent of the population’s health outcomes whereas 80 percent can be traced back to where they live, learn, work and play. Research has shown that in addition to SDoH issues impacting overall health, some races and ethnic minority groups, throughout the United States, experience higher rates of illness and death across a wide range of health conditions, including diabetes, hypertension, obesity, asthma and heart disease than other ethnic groups.
Our mission at Network Health is to create healthy and strong Wisconsin communities, and we strive to have a positive impact on your health and well-being. To uphold our mission, we gather data to help us achieve health equity for all members. At times, we may ask you about your race, ethnicity and preferred written and spoken languages. By asking these questions, we can deliver a better health care experience.
We understand that you are unique and by learning this information, we can plan for services that fit your needs.

This information will allow us to ...
• Better know you and the community we serve
• Pr ovide interpreter services
• Suppor t programs and benefits to improve your quality of care
• Plan and develop additional member-centered services
All your information at Network Health is confidential, private and protected by strict privacy laws and will be kept in your member records. Answering these questions is voluntary and helps us better serve you.
lif e. health. wellness. networkhealth.com 10 | C on C ierge • 2023
Exchange of Information
By Mary Zamost, RN, quality care coordinator
Many medical conditions can be connected to other non-related conditions or their treatments. Effective coordination of care depends upon clear and timely communication among patients, providers and facilities. Keeping communication open increases your safety and can help to control cost.
Here’s how you can help.
• Communicate with your personal doctor. You are a team and one way to make your team stronger is by letting your doctor know about any visits you have with other providers, specialists and behavioral health providers.
• Keep your doctor up to date on your medications and doses. Being aware of all medications you take helps your doctor see the complete picture. This helps you avoid unwanted medication interactions and duplicated tests, leading to improved outcomes and increased safety.
• Sign a release if you visit providers outside of your personal doctor’s organization. When your doctor refers you to a specialist, information is typically shared as allowed by privacy laws. However, if you choose to seek services outside of your personal doctor’s organization, ask whether a release needs to be signed so new information can be shared with your doctor.
Open communication and exchange of information allows you and your personal doctor to develop a complete and more successful plan of care. Think of them as your copilot, helping you navigate the way to a healthier you.
networkhealth.com 2023 • C on C ierge | 11
We’ll Be Your Guide
By Melanie Draheim, vice president of marketing and communications
Have you ever felt stuck or frustrated trying to navigate the health care system? Health care shouldn’t cause you stress. As a Network Health Medicare Advantage member, our Network Navigate program is automatically part of your plan to ensure you have an exceptional health insurance experience.

If you need help, our Network Navigators go above and beyond to directly communicate your needs to your Froedtert Health and Ascension Wisconsin health care providers. Our exclusive processes are designed to make sure those most in need get access to necessary medical care quickly. It’s a straightforward approach that allows you to worry less. We treat you with courtesy and respect and empower you to be an informed health care consumer. You’ll receive a personal welcome call to explain your benefits, easy-to-understand materials and opportunities to connect with our local staff, in-person at member events.
Plan Business Phone Calls
If you would like to opt out of phone calls from us about Network Health products or services available to you outside of your current coverage, you can do so at any time. To opt-out, please submit a written request to the following.
Network Health
Attn: Compliance
Plus, Network Navigators are ALWAYS someone located here in Wisconsin—not across the country or anywhere else. This means they understand your health insurance, doctors, clinics, local health care delivery and your local area. Learn more at NetworkNavigate.com. ProHealth
1570 Midway Place Menasha, WI 54952
Please note, you may still be contacted by phone to discuss your current plan offerings and may also be contacted in writing about other products and services available to you.
in-network
for all Network
Medicare
Plans as of October 1. NEW
Care is an
provider
Health
Advantage
COVER STORY
EGWP PRESORT STD US POSTAGE PAID PERMIT 1033 GREEN BAY, WI
1570 Midway Pl. Menasha, WI 54952 Health and wellness or prevention information




 By Julie Heinzel
By Julie Heinzel










