2023 Family Medicine Report

2023 University of Toronto Family Medicine Report
Editor
Alisa Kim
Design
Trajectory Brands Inc.
Writers
Alicia Fung, Alisa Kim and Elaine Smith
Photography
Brian Da Silva
Cover illustration
Pui Yan Fong
We wish to acknowledge this land on which the University of Toronto operates. For thousands of years it has been the traditional land of the Huron-Wendat, the Seneca, and the Mississaugas of the Credit. Today, this meeting place is still the home to many Indigenous people from across Turtle Island and we are grateful to have the opportunity to work on this land.










Contents Message from the Chair .......................................................................... 2 LEADERSHIP Critical Engagement ............................................................................. 5 RAAM Clinic Founder Bullish on Addictions Support .............................................. 8 In Support of Health System Resilience ......................................................... 12 Looking Upstream for Solutions to Health System Challenges ................................... 16 Feedback Loop ................................................................................. 20 ‘We Watch Teachers Grow’ ..................................................................... 24 COMMUNITY Speaking Their Language ...................................................................... 29 Have a Health Concern? Call Auntie. ............................................................ 32 Bringing the Winds of Change to Toronto’s Primary Care ‘Desert’. ............................... 36 Prescribing Better “Pills” to Swallow ............................................................ 38 Q&A: Dr. Melanie Henry. ........................................................................ 42 Cultivating a Culture of Curiosity and Continuous Quality Improvement. ........................ 46 RELATIONSHIPS A Little Help from my Friends ................................................................... 49 Healthy Barrie ................................................................................. 52 Finance 101 for MDs ........................................................................... 56 Office of Health System Partnerships Engages Primary Care Providers to Address the Health System’s Most Pressing Needs 60 1 2023 Family Medicine Report
Table of

2 Department of Family & Community Medicine,
Photo: Ed Rek
University of Toronto
Too often these two words conjure up visions of endless flip charts and sticky notes, long afternoons of time lost culminating in documents that quickly prove to be too general, too specific, or too unrealistic.
That’s not how I feel. To me, a good strategic plan is a clarion call: a lucid, inspiring articulation of what we stand for, and a promise about how we will spend our time, energy and resources. And in a massive department such as ours—with more than 2,000 faculty members, hundreds of learners, and countless internal and external partners—a strategic planning process is also an opportunity to build community, get to know each other better and strengthen bonds.
Our academic collaboration with Addis Ababa University, for example, is fostering the development of Ethiopia’s first emergency medicine residency program to build the nation’s capacity in this domain. The partnership, which you can read more about on page 24, is also a beautiful example of our expansive network, and the importance of considering the specific needs of a community in all we do.
The OurCare initiative, which you can read about on page 5, is engaging the Canadian public in reimagining the future of primary care in Canada—how it can be more equitable, accessible and sustainable. This feedback, wrought through connection and collaboration with everyday Canadians, forms the basis of unprecedented engagement with policymakers who are deeply interested in the public’s perception about the current state and future of primary care in Canada.
Increasingly, the work of primary care and public health are intertwined. In this report, we profile Healthy Barrie, a project that integrates public health, family medicine and municipal government action. The collaboration looks at data on various health indicators and neighbourhood characteristics to inform service policy and public health planning to drive change leading to a healthier population.
In late 2022, our Department of Family and Community Medicine concluded a community-building exercise of impressive breadth and depth, and launched a new strategic plan that I hope fulfills that dual function of community-builder and clarion call.
The three pillars of our plan—Community, Leadership and Relationships—are at the heart of everything we do in academic family medicine. The stories in this report are organized around these pillars, and of course they easily cut across themes. Each uses data from various sources to tell a story, and also engages with the narrative of our discipline, globally and locally.

The stories on these pages are just some examples (of many!) of the incredible work done across our department every day. Each story has a face—people whose work speaks of their incredible skills and commitment, as well as the people we serve. Each also uses data to propel us towards our vision: Outstanding primary care for all, powered by world-leading research, education, and innovation. In that sense, the work is just like family medicine itself: grounded in evidence and propelled by stories.
I am inspired by the depth and breadth of the work of our community for the good of our patients, our faculty and learners, and the health care system writ large—locally, nationally and globally.
Enjoy!
Dr. Danielle Martin Professor and Chair Department of Family and Community Medicine University of Toronto
3 2023 Family Medicine Report
There are lots of reasons to dislike, or distrust, “strategic planning.”
LEADER SHIP
4 Department of Family & Community Medicine, University of Toronto
CRITICAL ENGAGEMENT
By Alisa Kim
OurCare Initiative Brings the Public’s Voice to the Dialogue on the Future of Primary Care in Canada.
The second phase of OurCare engages the public and patients through provincial reference panels. In Ontario, more than 1,200 people volunteered to participate; 35 people representing the demographics of Ontario were selected. In February 2023, the Ontario panel met in Toronto to learn about primary care and put forward recommendations for a better system.

LEADER
Photo credit: Yuri Markarov, Unity Health Toronto
5 2023 Family Medicine Report – Leadership
The issues besetting primary care in Canada are immense and predate the COVID-19 pandemic. For one, it is very difficult for people without a family doctor to find one—particularly those in rural and remote areas. The problem will only get worse as family doctors retire in the coming years with fewer medical students choosing to specialize in family medicine to take their place. As decisionmakers try to address these matters and reform primary care in Canada, a key voice is missing—that of patients and the public.
Dr. Tara Kiran, Vice-Chair of Quality and Innovation at the Department of Family and Community Medicine (DFCM), is correcting that omission. She is spearheading a bold national initiative called OurCare that engages patients and the public in reimagining the future of primary care in Canada. The goal is to enable the average person living in Canada to have a say in developing a primary care system that is more accessible, equitable and sustainable, and to bring that feedback to policy makers.
As a scientist and family physician, Dr. Kiran understands the imperative need for users of the primary care system to be part of any reforms. “Primary care is in crisis right now. Far too many people don’t have a family doctor; those who do can’t get seen in a timely way. There have been lots of changes in primary care and the health care system including the introduction of virtual care and increased footprint of corporations. All of these things together make it the right time to have dialogue around what the system of the future should look like,” she says.
The first phase of OurCare launched in September 2022 with a national online survey that asked about people’s experiences with primary care and what they valued most in primary care. More than 9,000 people completed the survey which, among other things, inquired about whether people had a primary care provider, if they had used a walk-in clinic in the past year, how they access their medical information, and the importance of having a primary care provider or team. Results of the survey are posted online, where anyone can interact with the data and see how different groups responded to the questions.
Dr. Tara Kiran, Vice-Chair of Quality and Innovation at DFCM and the Fidani Chair in Improvement and Innovation, is leading OurCare, a national initiative that is engaging the public on the future of primary care in Canada.

The second phase of the project engages patients and the public via reference panels. In Ontario, more than 1,200 people volunteered to participate; 36 people representing the demographics of Ontario were randomly selected. The panel met to learn about primary care and put forward recommendations for a better system. There will also be reference panels in British Columbia, Quebec, Nova Scotia and one territory.
It is a priority to discuss the future of primary care in a way that is inclusive and equitable, says Dr. Kiran, who notes the team is engaging with members of the public who may not have a regular care provider. “When we think about patient engagement, we think about people who are actually taken care of. Primary care is something that should be available for everyone so we want to have that broad conversation with members of the public whether or not they have a family doctor,” she says.
More than 6.5 MILLION adults in Canada don’t have a regular family doctor or nurse practitioner.
6 Department of Family & Community Medicine, University of Toronto
The third phase is a series of community round tables to hear from people who are underserved by primary care systems in Canada. The OurCare team is collaborating with local organizations to understand who it should be engaging, and to rely on the groups’ relationships and expertise to bring people together. “[The round tables] are designed to focus on equity issues and bring voice to marginalized communities and their specific needs and priorities,” says Dr. Kiran.
After each phase, the researchers will produce a report about the findings. The reports will be shared with the public and a long list of stakeholders including government and health care organizations—all of whom are deeply interested in the public’s perception about the current state and future of primary care in Canada. “I don’t think there is any government that isn’t interested in what the public has to say about what the future of primary care should be. I think often they don’t have a direct vehicle to converse with the public to understand the perspective,” says Dr. Kiran.
OurCare reflects the priorities of DFCM through its work in the Quality and Innovation program, which, in 2022, established a Family Medicine Patient Advisory Committee. The committee is comprised of 16 patient partners who receive care at one of DFCM’s clinics. Its members come from a variety of backgrounds to form a diverse and inclusive group.
When the call for patient partners was made, there was a strong response, notes Dana Arafeh, DFCM’s first Patient
and Family Engagement Specialist. “We had 150 apply for the role. From there, we selected 16. We wanted representation from all of the clinics and looked at sociodemographic information and the type of connection patients might have to a primary care clinic. There is definitely a diverse range of perspectives,” she says.
The Patient Advisory Committee, which meets bi-monthly, advises DFCM on a variety of topics related to improving the quality of care delivered in family medicine. It helps the department form questions for its patient experience survey, assists in interpreting results of the survey and gives feedback on new projects aimed at improving care. The group will also provide advice on the education of family medicine residents by helping the department communicate the role of residents to patients, and will provide input on curriculum and advice on how to give feedback to residents. “We are getting the patient perspective on what’s missing at our clinics, how can we start communicating better about what we do, what a teaching clinic looks like, and what people can expect from a resident,” says Ms. Arafeh.
Engaging patients to try and improve the health care system is critical, says Dr. Kiran. “I’ve learned over the years how important it is to hear directly from the people using the system how we should design it. Each time I’ve done it, I’ve learned a lot. The public and patients provided stakeholders with important insights we wouldn’t have gotten otherwise that helped shed light on what the priorities are and how we should move forward.”
Some Recommendations from the Ontario OurCare Priorities Panel:
• Expand team-based care to every resident
• Ensure patient access to personal health data
• Legislate and enforce interoperability data standards
• Invest a greater proportion of total health care funding in primary care
• Strengthen links between primary care practitioners and community agencies
The OurCare initiative engaged people across Canada about their care experiences and what’s important to them when it comes to primary care. Learn more at OurCare.ca.
7 2023 Family Medicine Report – Leadership
DFCM Assistant Professor Dr. Hasan Sheikh is a physician in the emergency department at University Health Network and in the Rapid Access Addiction Medicine clinic he cofounded there in 2018.

RAAM CLINIC FOUNDER BULLISH ON ADDICTIONS SUPPORT
By Elaine Smith
8 Department of Family & Community Medicine, University of Toronto
Dr. Sheikh, a faculty member in the University of Toronto’s Department of Family and Community Medicine (DFCM), says, “I don’t think you have to be in a formal position of authority to be a leader and empower others to make change. I try my best to be a leader, but as to whether or not I’m successful, you’d have to ask others.”
His colleagues are happy to praise his leadership abilities.
“Dr. Sheikh is a very effective leader,” says Dr. Jennifer Hulme, a physician in the emergency department at the University Health Network (UHN) and in the Rapid Access Addiction Medicine (RAAM) clinic he co-founded there in 2018. “He leads by example and is very inclusive, but he is good at making executive decisions when we need action.”
DFCM and the provincial government also recognize Dr. Sheikh’s leadership potential. The emergency and addictions physician is the most recent winner of DFCM’s Louise Nasmith Award, given annually to provide an early career faculty member with protected time to research, prepare, and disseminate a lecture or workshop on a change-relat-
ed topic. In fall 2022, he was also named the provincial clinical lead for substance use disorders at the Mental Health and Addictions Centre of Excellence at Ontario Health.
Dr. Sheikh has been involved with public health and government policy in the past. In addition to his clinical experience, while earning a master’s degree in public administration at Harvard University, he worked with the City of Calgary on creating a municipal mental health and addiction strategy, the first city in North America to do so.
“I wanted to take a person-centered view of the addictions sector in the city, and to do that I consulted with a very diverse group,” he says. “That included many members of the community: I consulted with people who were actively using substances, those in treatment programs including the injectable Opioid Agonist Treatment (iOAT) program, and those who were in abstinence-based recovery programs. I also connected with community agencies that worked with people experiencing homelessness and with people who were using substances, and even connected with law enforcement as well to hear their perspectives.”
Dr. Hasan Sheikh’s favourite definition of leadership comes from Marshall Ganz, a professor at the Harvard Kennedy School of Government who teaches community organizing: “Enabling others to achieve shared purpose in the face of uncertainty.”
9 2023 Family Medicine Report – Leadership
The Louise Nasmith Award will provide Dr. Sheikh with some protected time to do systemic work that he can bring back to DFCM.
“I’d like to develop a framework of how to reframe our most frustrating clinical experiences and redirect our attention to look at the upstream failure,” Dr. Sheikh says. “Can we create a framework to systemically figure out policy failures and where to intervene?”
“This desire is based on my clinical experiences; I want to take a step back to see how I can help others who are doing similar work. We don’t get medical school training on how to diagnose or treat policy failures, despite the fact that we are the ones who see their effects every day.”
“For example, homelessness and the lack of affordable housing is a significant challenge,” he says. “Housing first strategies have shown to improve people’s mental health and substance use. Many of my patients tell me that homelessness is a major driver of their substance use.”
One of Dr. Sheikh’s proudest achievements to date is co-founding the RAAM clinic at UHN as part of a network of such clinics across Ontario. A RAAM clinic is a low-barrier, drop-in clinic that patients can attend to get help for a substance use disorder without an appointment or formal referral. It provides time-limited substance use care that includes pharmacotherapy, brief counselling, and referrals to community services.
“META:PHI (Mentoring, Education and Clinical Tools for Addiction, Partners in Health Integration) pioneered this model and built a ton of resources and a good community of practice,” Dr. Sheikh says. “It is a complete game-changer for people. It really works for people suffering from substance use disorders. We published a study on our first six months of data and patients with alcohol use disorder that came to us from the ED did even better than those referred from primary care, even though they started with more severe illness.”
In fact, the clinic began by operating for only two half days each week and is now open five half days a week. Currently, the clinic is trying a new intervention for people with stimulant use disorder that uses the reward centre of the brain to motivate them by offering vouchers for positive steps.
“The clinic fits with a DFCM pillar that says we should integrate research into our interventions and be accountable to the people we are trying to help,” Dr. Sheikh says.
Notes his colleague Dr. Hulme, “Although RAAM is not unique, it’s unique to have emergency physicians there. Dr. Sheikh has been instrumental in changing the culture of our emergency department with continuing medical education and support to our emergency providers about which medication to start people with and how to counsel them. He’s done a lot of outreach to the family health team, because people do much better with support from their family physicians. He has also helped ensure that addiction medicine is a core rotation in a family medicine residency.”
10 Department of Family & Community Medicine, University of Toronto
“We don’t get medical school training on how to diagnose or treat policy failures.”
417 patient visits to the RAAM clinic at Toronto Western Hospital in the first six months of 2022.
In addition to his clinical work, Dr. Sheikh is also involved in research. He is a co-author of a study published in 2020 in the Canadian Medical Association Journal that grew out of curiosity about what happened to ED patients with repeated visits for alcohol intoxication.
“We looked a year forward from their ED visits and discovered that of those who had two visits or more in a year, one in 20 died, while among those who visited five or more times in a year, one in 10 died,” he notes. “This is comparable to the mortality after having a heart attack. We should be wrapping care around these people; but they aren’t treated with the same priority or severity as they should be.”
He is committed to helping as many people with alcohol use disorder as possible.
“We know that for some part of the emergency department population, the RAAM clinic works, but for others, it isn’t the model of care they need,” Dr. Sheikh says. “We need to determine what those supports are so we can work on the silent epidemic of alcohol-related harms. Can we move away from siloed, stigmatized care toward a more compassionate system that works with the realities people face?”
Dr. Sheikh has a long career in which to answer those questions and it’s apparent he’s off to a running start.
Opioid poisonings result in about 7 ED visits in Ontario daily and more than 13 hospitalizations per day across Canada.
1 in 3 Canadian adults meet the criteria for substance use disorder during their lifetime.
11 2023 Family Medicine Report – Leadership
Source: Wiercigroch, D et al. A rapid access to addiction medicine clinic facilitates treatment of substance use disorder and reduces substance use (2020); 15:4.
Dr. Danielle Martin, Professor and Chair of the Department of Family and Community Medicine at U of T, conceived a three-part brief for the Ontario COVID-19 Science Advisory Table on the strengths and challenges of primary care in Ontario during the pandemic. She is also a family doctor in the Women’s College Hospital Family Practice Health Centre.

12 Department of Family & Community Medicine, University of Toronto
IN SUPPORT OF HEALTH SYSTEM RESILIENCE DFCM RESEARCHERS HIGHLIGHT THE ROLE OF PRIMARY CARE DURING THE PANDEMIC IN ONTARIO
By Alisa Kim
A team led by researchers from the Department of Family and Community Medicine at the University of Toronto authored a threepart brief on the strengths and challenges of primary care in the pandemic for the Ontario COVID-19 Science Advisory Table.

13 2023 Family Medicine Report – Leadership
The reports, published on Oct. 3, 2022, detail the work of primary care providers during the first two years of the pandemic, outline issues affecting primary care in Ontario, and offer lessons learned to improve access to primary care.
“The pandemic is not over, and COVID-19 is increasingly an illness that will be managed in the community, supported by family doctors, nurse practitioners and primary care teams. The Science Table wanted to understand the evidence base around the contributions of primary care to the pandemic response so far, as well as current strengths and challenges that will affect response to future waves. At this time it is critical to understand the lessons learned from the last two and a half years ,” says Dr. Danielle Martin, Professor and Chair of the Department of Family and Community Medicine at U of T, who conceived the briefs. The core authors include experts in primary care from across Ontario with a wide variety of backgrounds, including Drs. Imaan Bayoumi, Azza Eissa, Noah Ivers, Tara Kiran, Derelie Mangin, Sarah Newbery, Andrew Pinto and Kamila Premji. The team analyzed more than 200 articles for the research and consulted experts broadly in its work.
The release of the briefs is the last official act of the Ontario COVID-19 Science Advisory Table. Comprised of scientific experts and health system leaders, the advisory table evaluated and reported on evidence relevant to the pandemic to guide Ontario’s response. Research shows health systems with strong primary care have better health outcomes and improved health equity at lower cost; an examination of the lessons learned about primary care in the pandemic seems a fitting capstone activity for the Science Table.
The three-part brief is an ambitious undertaking involving dozens of researchers and primary care experts from across Ontario, Canada and internationally. The briefs outline the evidence on how primary care clinicians—family doctors, nurse practitioners, pharmacists, social workers and other allied health care providers—took on new roles and worked more days to support COVID-19 care in addition to their routine clinical work, which includes preventive, chronic and acute care. Primary care clinicians in Ontario assumed new responsibilities like COVID testing, assessment and isolation; vaccine counselling and delivery; treatment prescribing and referral and post-COVID acute care. They also aided other areas of the health system like emergency departments, intensive care units and long-term care, and assisted people experiencing mental health issues as well as poverty and food insecurity.
“As misinformation rises around COVID-19, primary care clinicians are highly trusted members of their communities—they are an invaluable resource for conveying fast-changing scientific developments around prevention and treatment of COVID-19 to the public,” says Dr. Fahad Razak, scientific director of the Ontario COVID-19 Science Advisory Table and an associate professor in the Department of Medicine at U of T.
Ontario faces a significant challenge in keeping up with demand for primary care, the researchers note. About 2.2 million Ontarians do not have a regular family doctor, with new immigrants and people living on low incomes least likely to have one. Moreover, 1.7 million Ontarians have a family doctor who is of retirement age. Compounding this shortage is the decline in medical school graduates choosing to specialize in family medicine. These challenges, along with inequitable access to team-based care, shape the ability of primary care to respond to future pandemic waves and support health system recovery.
Based on their findings, the researchers outlined lessons learned:
1. Care provided in formal attachment relationships and through team-based models provides superior support for COVID-19- and non-COVID-19-health issues in the community.
2. In the absence of additional resources, COVID-19 response results in tradeoffs and unmet needs in other areas.
3. Innovative models and new partnerships supported patients to get needed care, but infrastructure is needed for sustainability, spread, and scale.
4. The absence of an integrated data system compromised the pandemic response in primary care.
5. Primary care can leverage its longitudinal relationships to achieve public health aims.
Dr. Martin says the ultimate goal of the work, which received widespread local and national media coverage, is to provide evidence to help decisionmakers, including governments, professional associations, and front-line providers to improve the ongoing pandemic response. “We’re in a state where we’re facing significant health human resources shortages, inequitable access to teams and uncertainty about the future. My hope is that the crisis we’re facing will motivate all leaders in the system to look to the evidence about how we can best improve access to high-quality primary care for all Ontarians.”
14 Department of Family & Community Medicine, University of Toronto
Lesson 1






Care by a regular primary care provider or team provides better support for health issues in the community.
Lesson 2

In the absence of more resources, COVID-19 response results in tradeoffs and unmet needs in other areas.


Lesson 3

Innovative models and new partnerships helped patients get the care they needed, but infrastructure is required for sustainability, spread and scale.
Lesson 4
The absence of an integrated and inclusive data system compromised the pandemic response in primary care.


Lesson 5
Primary care can leverage long-term relationships to improve population health and health system sustainability.
15 2023 Family Medicine Report – Leadership

16 Department of Family & Community Medicine, University of Toronto
LOOKING UPSTREAM FOR SOLUTIONS TO HEALTH SYSTEM CHALLENGES
By Elaine Smith
Dr. Andrew Pinto, an Associate Professor in the Department of Family and Community Medicine at the University of Toronto, wears many hats: family physician, public health specialist and scientist. He also holds an Applied Public Health Chair from the Canadian Institutes of Health Research and is the only family physician among the seven researchers nationwide who received this honour.
17 2023 Family Medicine Report – Leadership
The award, worth $1.15 million, provides mid-career researchers with an opportunity to collaborate with policy makers to support evidence-informed decision-making that improves health and health equity. Dr. Pinto attributes the recognition to the work being done by his Upstream Lab based at MAP Centre for Urban Health Solutions, St. Michael’s Hospital, one of the University of Toronto teaching hospital partners.
He created the lab in 2016 as a way to make medicine more effective by looking upstream to the social determinants of health and the interventions that could create change at an individual, organizational or policy level.
“My selection speaks to the fact that the Upstream Lab is recognized in Canada and elsewhere for showing leadership in a challenging area,” he says of the five-year Applied Public Health Chair. “I see the lab as a resource for the community to use to create change and innovative solutions. We have a social justice focus and we seek to both describe and solve problems.
“It’s something I can’t do by myself, but I have a fantastic team of 26 staff and a dozen graduate students and post-doctoral fellows. We’re also starting to be the home for other research scientists,” says Dr. Pinto.

Dr. Archna Gupta, PhD is a member of the Upstream team. The family physician is finishing her post-doctoral fellowship in the lab and will soon become one of its scientists.
“The fact that Dr. Pinto started this lab well before others recognized the problem is impressive and the dedication he puts into pushing the envelope is amazing,” Dr. Gupta says. “The growth of the lab is a testament to his leadership and his ability to get grants for projects that aren’t traditionally funded.”
With his new appointment, he hopes to establish a repository of evidence around what works in terms of upstream actions; determine what works to help health organizations look at the external factors that could be addressed to prevent various health problems; create a network of upstream clinics across Canada; and examine policy and opportunities for policy change through the Upstream Policy Observatory.
His CIHR chair and the Upstream Lab aren’t the only balls Dr. Pinto is juggling when it comes to research. In 2022, he was awarded $10 million in federal funding for CanTreatCOVID, which stands for Canadian Adaptive Platform Trial of Treatments for COVID in Community Settings. The trial is a national study of the effectiveness of current and future oral COVID-19 therapies to reduce symptoms faster and prevent long COVID. It is designed to identify useful and affordable medications so they can be made readily available in community settings.
“People needed better evidence about whether these treatments work, especially in a highly vaccinated population,” says Dr. Pinto. “They are expensive and we need to
18 Department of Family & Community Medicine, University of Toronto
Dr. Andrew Pinto (far left), an Associate Professor at DFCM, leads the Upstream Lab based at MAP Centre for Urban Health Solutions, St. Michael’s Hospital. The lab aims to improve health through upstream social interventions. Photo: MAP Centre for Urban Health Solutions.
know if it’s a good use of public money. It’s a great way to identify what works and test it in a continuous way.”
The team comprises primary care researchers and infectious disease and public health specialists. The goal is to attract 3,000 people to the study for each treatment, starting with Paxlovid and adding more therapeutics as they emerge. Participant recruitment is happening through primary care physicians, emergency rooms, pharmacies, COVID assessment centres and appeals to the public. Provincial hubs in British Columbia, Alberta, Manitoba, Quebec, Newfoundland and Ontario will help connect patients to treatments.
The researchers hope to have feedback within six months and are looking at ways to disseminate the findings quickly, while continuing to assess other treatments. They are working in conjunction with colleagues in the United Kingdom who are doing a similar study, looking for ways to collaborate and pool their data.
“We’ll follow the patients over the course of their treatment and for six months afterward,” Dr. Pinto says. “Our main question is whether any of these treatments reduces hospitalization, emergency room visits or deaths. We will also look at recovery times and whether these medications reduce the chances of getting long COVID and its side effects.”
The study has been approved by Health Canada and supported by the Canadian Institutes of Health Research and Public Health Agency of Canada. It features more than 90 investigators, staff and patient partners, something he calls “a real team effort.” The team has a communications plan to disseminate pre-prints of their findings as quickly as possible.
Dr. Pinto wants the platform to be accessible to people beyond the research who have treatment ideas and there will be a committee who studies their proposals. Over the long term, he hopes that CanTreatCOVID will grow into a platform that encompasses other respiratory conditions such as influenza and respiratory syncytial virus, becoming CanTreatResp and helping public health prepare for future pandemics.
Dr. Gupta, his colleague, doesn’t doubt the future success and growth of CanTreatCOVID after seeing how he has assembled the team at the lab.
“We’ve grown over time and his ability to manage that speaks to his capacity as a leader,” she says. “He’s trying to develop a sustainable system of researchers so that the lab is bigger than one person—an organism that can perpetuate. It’s not a one-man-show. We’re all part of a team working toward a common vision. He’s developing a living entity.”
What is Paxlovid?
Paxlovid contains two antiviral medicines, nirmatrelvir and ritonavir, which are co-packaged together. Paxlovid stops the virus from multiplying in the body. Paxlovid is used in adults to help people overcome COVID-19 infection and recover faster.
A study involving more than 185,000 patients with COVID-19 showed Paxlovid reduced rates of hospitalization or death by 78%.
Source: Q Zheng et al. Efficacy and safety of Paxlovid for COVID-19: a meta-analysis. J Infect 86.1 (2023): 66–117.
19 2023 Family Medicine Report – Leadership
FEEDBACK LOOP DR. PETER SELBY USES PATIENT-CENTRED APPROACH AND CONTINUOUS LEARNING TO ENHANCE TREATMENT FOR TOBACCO ADDICTION
 By Elaine Smith
By Elaine Smith
Illustration: Pui Yan Fong 20 Department of Family & Community Medicine, University of Toronto
Dr. Selby, the Vice-Chair, Research, for the Department of Family and Community Medicine at the University of Toronto, is a Senior Scientist at the Centre for Addiction and Mental Health (CAMH) and the principal investigator and director of its Nicotine Dependence Service, a project that first began in 2005–2006. He is also the driving force and principal investigator behind its Nicotine Dependence Clinic (NDC), Ontario’s STOP (Smoking Treatment for Ontario Patients) program and the TEACH (Training Enhancement in Applied Counselling and Health) program.
The TEACH program offers continuing education and is aimed at capacity-building by training health care providers to support their patients with tobacco addiction and cessation, and address e-cigarette use or vaping. Taken together, these components also form the basis for
the Learning Health System that informs the treatments used by both clinic and STOP practitioners.
“Many family medicine problems had common causes, including smoking,” Dr. Selby says. “About four million Canadians smoke and it’s killing about 45,000 every year. However, when treating patients for other conditions, such as COPD (chronic obstructive pulmonary disease), high cholesterol or blood pressure, the benefits are wiped out if the person continues to smoke. In addition to preventing numerous chronic diseases, ongoing smoking harms almost all of them. As family physicians we also see the harms of smoking in pregnancy and the effects of second-hand smoke on children in our practice. Governments were also waking up to see smoking’s connection with other illnesses, but there were no leaders to take this on using this approach.”
Dr. Peter Selby has big goals: helping people to stop smoking successfully and continuously improving the system that makes this possible. Even bigger is the news that he’s succeeding.
21 2023 Family Medicine Report – Leadership
Dr. Selby has become that leader.
“We needed to research and create a separate system, since no single treatment seemed to work,” he says. We’ve created a system to look at who smokers are and treat them based on the context of their lives. With data, we could see that many smokers are also dealing with poverty, mental health conditions, drinking to excess, or other conditions. We looked at what we could add as additional interventions and supports.”
The result has been the provincewide STOP program, in addition to the CAMH Nicotine Dependence Clinic. The CAMH program is site-specific and focused on the hospital’s outpatient population, creating individual treatment plans and offering individual and/or group counselling supports. STOP, meanwhile, is a provincewide tobacco cessation treatment program funded by the Ontario Ministry of Health, and delivered either through local Ontario-based healthcare providers, or online via the STOP on the Net program. Smokers or vapers who qualify receive nicotine replacement therapy like gum and patches, and counselling supports.
“We created a system that we could scale up across the province,” says Dr. Selby.
STOP is available at more than 300 sites provincewide through collaborations with family health teams, community health centres, Aboriginal health centres, nurse practitioner-led clinics and addiction and mental health agencies. As of January 2023, STOP has treated 346,000 people across Ontario. People who participate in STOP are eight times more likely to quit than if they attempt to stop using tobacco unassisted.
Given the challenges of in-person interactions during the COVID-19 pandemic, Dr. Selby and his team initiated STOP on the Net, an online version of the program that is now a permanent option, given its popularity and effectiveness.

“We pivoted to provide services that people could access safely and virtually and the enrolment numbers continue to grow,” says Eva Huang, a CAMH knowledge translation specialist.
Adds Dr. Selby, “We created STOP on the Net to assist a workforce under strain. Since it is delivered directly to the smoker [or vaper], they can enrol themselves and reduce pressure on health-care providers. It’s all about improving population health by empowering people to take action.”
22 Department of Family & Community Medicine, University of Toronto
Dr. Peter Selby, Vice-Chair, Research at the Department of Family and Community Medicine, is Director of the Nicotine Dependence Service at the Centre for Addiction and Mental Health.
STOP has a small footprint, he notes, needing little space of its own. Dr. Selby and his team explore the needs of the setting and create training programs tailored to their populations. These include initiatives targeting women and youth and efforts targeting homeless shelters or Indigenous communities.
STOP sites and the NDC provide Dr. Selby and his team with data about the success or failure of various interventions, as well as patient demographics; they form the basis for a learning health system. It is a system that relies upon continuous cycles of research, analysis, development and implementation of improvements to achieve better health for individuals and improved performance for health care systems.
“As I did traditional research, I recognized that making changes to frontline services took years,” says Dr. Selby. “We needed to take the current problems our patients are facing and rapidly develop solutions that we could simultaneously study and deploy in real-world settings.
“This is an adaptive learning system. We learn what works, create and adapt. The research setting is often different than the real-world setting. We look at the real-world settings and see what’s required to get the outcomes a site needs and make sure what is offered fits with their DNA. We offer intelligent research and support to do it.”
Nadia Minian, PhD, is an implementation scientist with the Nicotine Dependence Service and an assistant professor at DFCM. She is heavily involved in its learning health system and knowledge translation.
“These are evidence-based smoking cessation programs,” Dr. Minian says. “We collect data to see how well the programs are working, then make adjustments. Every time a participant enrols, we collect baseline data to match with treatments and look for trends and gaps. Everything is evidence-based.
“We either identify gaps in the literature and data or hear from our own partners. If we need to develop specific resources, there is also TEACH training and tools to assist patients.” TEACH is also led by another member of DFCM, Rosa Dragonetti. It is an award-winning program with a community of practice that has demonstrated the impact of this training model on patient level outcomes.
Dr. Selby says that a sound learning health system can help planners make health care service decisions. He and his team are currently collaborating with Diabetes Action Canada to determine how the model can provide integrated mental and physical health care to people with diabetes.
“A good learning health system that is designed for the patients and clinicians should make a difference in health system planning and evaluation,” he notes. “It connects various siloes and gets them to work together on an alignment of purpose, and family medicine should be at the centre of a good learning health system, since family physicians co-ordinate whatever patients need.”
10% of Canadians report smoking cigarettes on a regular basis.
Vaping is more prevalent among younger adults than older age groups.
Smoking is more prevalent among men than women, with 12% of men reporting they were current smokers compared with 9% of women.
23 2023 Family Medicine Report
Source: Canadian Tobacco and Nicotine Survey, 2021

24 Department of Family & Community Medicine, University of Toronto
Dr. Don Melady (right), an Associate Professor at DFCM and an emergency medicine physician, reviews a CT head scan with a resident, prior to digitization of diagnostic imaging.
‘WE WATCH TEACHERS GROW’ LEARNING PARTNERSHIP WITH ADDIS ABABA UNIVERSITY YIELDS ETHIOPIAN LEADERS IN EMERGENCY MEDICINE
By Elaine Smith
Dr. Whynot was in Ethiopia’s capital city for an elective during her emergency medicine fellowship with the University of Toronto’s Department of Family and Community Medicine (DFCM).
“We learned to work around issues like these,” says Dr. Whynot. “Working as part of the Toronto Addis Ababa Academic Collaboration in Emergency Medicine (TAAAC-EM) was eye-opening. I got so much out of it, but first and foremost was insight into what emergency medicine looks like and how things work in a resource-limited setting.”
TAAAC-EM began in 2010, as one of the many offshoots of an initial collaboration with Addis Ababa University (AAU) begun in 2003 under the leadership of Dr. Clare Pain, an associate professor of psychiatry at U of T, and psychiatrists at AAU. Drs. Megan Landes, head of DFCM’s Division of Emergency Medicine, and James Maskalyk, a TAAAC-EM strategic director, were the inaugural co-directors of the program.
“Addis Ababa University approached U of T with several priority areas for expansion and one of the first was emergency medicine,” says Dr. Landes. “James and I worked really closely with Clare to ensure we were implementing a partnership built on an ethical, thoughtful way of engaging across the North-South divide. We’d seen partnerships elsewhere, some done well and some done poorly, and we wanted to make our partnership a model of how you can engage in a truly bilateral fashion.”
At the time, Ethiopia had no training available for an emergency medicine specialty, and TAAAC-EM was created to meet that need by assisting AAU in building its own emergency medicine residency program. Faculty from the Division of Emergency Medicine at the DFCM and Department of Medicine (DOM) travelled to Addis Ababa three times a year, for a month at a time, to hold training sessions for residents. Teaching trips covered a longitudinal, three-year curriculum through didactic teaching sessions, practical seminars,
25 2023 Family Medicine Report – Leadership
While working in an Addis Ababa emergency room, Dr. Sarah Whynot recalls being shocked to discover that there was a shortage of paper for the ECG machine.
point-of-care ultrasound, simulation and bedside clinical supervision. One or two emergency residents from DFCM or DOM with an interest in global health joined the trips as one of their residency electives, working in the emergency room alongside AAU residents and/or assisting with teaching.
The original goal of TAAAC-EM was to assist in the graduation of a self-sustaining critical mass of emergency medicine leaders at AAU who would continue to train future generations of Ethiopians, and spread emergency medicine expertise throughout the country and East Africa.

“For the first three-to-five years, U of T faculty did the bulk of the training,” says Dr. Eileen Cheung, a family and emergency medicine physician who travelled to Addis Ababa in 2014 as a resident and has since been there twice as a faculty member. She is now the program’s director of education and programming, working closely with Dr. Jennifer Bryan, TAAAC-EM’s director of operations.
“Now, the graduates of the residency program have assumed larger teaching roles.
“We had planned to make that transition and our inability to travel during the COVID-19 pandemic sped some things up and slowed some things down. Our Ethiopian colleagues now do the didactic teaching, but we haven’t handed over all the teaching. On our trips now, we run workshops and simulations and the faculty want continuing professional development, which would be the logical next step,” says Dr. Cheung.
Dr. Landes adds, “TAAAC-EM is a true expression of what we do as educators; we watch teachers grow.”
The collaboration began with a class of just six Ethiopian physicians. The current class of TAAAC-EM residents has 25 physicians. In addition, graduates of the residency program have started at least three similar programs in other Ethiopian hospitals, says Dr. Cheung. To date, there are 82 graduates of the emergency medicine residency practising in 13 hospitals across Ethiopia and there are 42 others in training. There are also graduates employed in high-level positions in Ethiopia’s Ministry of Health.
Suturing workshop with AAU EM residents using pigs’ feet.
26 Department of Family & Community Medicine, University of Toronto
(Left to right:) DFCM Associate Professor Dr. Dominick Shelton with Dr. Tilahun Jiru and Dr. Woldesenbet Waganew.
“There is a more than 95 per cent retention rate of these physicians in Ethiopia’s public medicine system,” Dr. Cheung notes. “That’s unprecedented. It speaks volumes.
“The key to building capacity at this level is providing in-country training to avoid a brain drain. I am continually blown away by the capacity of Ethiopian physicians. It’s interesting how far things have come, since Ethiopia didn’t have an emergency medicine specialty at all before TAAAC-EM.”
She anticipates the TAAAC-EM partnership will continue to change as the needs at AAU change.
“TAAAC-EM is a model that can be replicated elsewhere. Queen’s University is now with Haramaya University and the University of Calgary is involved in Uganda. Ethiopians are now seen as emergency medicine leaders in East Africa. The first two South Sudanese TAAAC-EM residents have just graduated in Ethiopia with the idea of returning home to have an impact. AAU can now be their own experts in helping other African countries build emergency care capacity and U of T could facilitate and mentor other universities in becoming engaged.”
Notes Dr. Landes, “There is still a role for the partnership, but it will change over time. A lot of us feel we have created deep friendships as a result.”
Dr. Cheung is very proud of the program’s success.
“It is rewarding to see the growth in emergency medicine in Ethiopia and how it has evolved differently than it has in
Canada; the pathology and structure are so different,” she says. “Meanwhile, we are also building a cadre of Canadian instructors who understand global health engagement in a longitudinal model. I love the model and medical education in general.”
Dr. Landes believes the TAAAC-EM program emphasizes humility in global health.
“There are often a lot of colonial overtones to global engagement, but so much bi-directional learning has happened through TAAAC-EM,” Dr. Landes says. “Our Canadian residents and physicians learn to practise in a different context, understand complex disease management, learn to work in a low-resource setting and to teach across different cultures. It makes us better physicians and we bring these lessons back to our own emergency departments.”
Seven DFCM residents have participated to date, along with 25 DFCM faculty members, and Dr. Whynot confirms that learning during a TAAAC-EM residency goes both ways.
“I was both a learner and a teacher,” says Dr. Whynot. “It is hard to be engaged in global health work without understanding the day-to-day issues. I learned a lot clinically from the Ethiopian physicians because they see diseases we don’t see here and I improved my own skills as a teacher in teaching simulations and getting feedback.
“It was a helpful growth experience and increased my desire to be part of global health initiatives throughout my own career.
82
25 DFCM faculty members have participated in the TAAAC-EM program.
graduates of TAAAC-EM practicing in 13 hospitals across Ethiopia
27 2023 Family Medicine Report – Leadership
COMM UNITY
28 Department of Family & Community Medicine, University of Toronto
SPEAKING THEIR LANGUAGE CREDIT VALLEY FAMILY HEALTH TEAM MEETS COMMUNITY’S URGENT NEED FOR PRIMARY CARE IN FRENCH
By Alisa Kim
Research shows people do better when they receive medical care in their primary language.
Astudy published in the Canadian Medical Association Journal in 2022 shows people who speak languages other than English are up to 54% less likely to die or have other severe health outcomes when cared for by a doctor who speaks the same language as them.
“There are many benefits to patients’ health when they are served in their first or maternal language,” says Dr. Kerrie Shaw, a faculty member of the Department of Family and Community Medicine (DFCM) and a physician at the Credit Valley Family Health Team’s bilingual site which cares for Francophone patients.
L’Équipe de Santé Familiale Credit Valley was established in 2012 to serve French-speaking residents of Ontario’s Peel and Halton regions. Under the French Language Services Act, these are designated areas in which access to primary health care in French is guaranteed.
Being attached to a Family Health Team has significant benefits. Family health teams specialize in proactively managing chronic conditions like depression, asthma, diabetes and chronic obstructive pulmonary disorder. They are recognized for their expertise in health promotion including weight management, smoking cessation and newborn wellness.
Dr. Paul Cheung, who is also a faculty member of DFCM and a family doctor at the Credit Valley Family Health Team’s bilingual site, says the clinic serves about 2,100 patients. It is one of just a few Francophone Family Health Teams in Ontario Health’s Central Region, an area that serves more than five million people. Dr. Cheung notes some of his patients come from as far away as Hamilton or Belleville to receive primary care services in French because it is an urgent need. The interprofessional team includes three family physicians, a nurse practitioner, registered nurses, a dietician, social worker and a diabetes specialist team—all of whom speak French.
29 2023 Family Medicine Report – Community
Dr. Cheung, who was born and raised in Quebec and did his medical training in French, notes patients of the bilingual site have diverse backgrounds; many are Canadians, but they also hail from Europe, Africa and the Caribbean. “Our patients describe their care as ‘one-stop shopping,’” he says. “We are bringing everything we’ve done well in team-based primary care in French. Our patients benefit from a team of bilingual health care providers who promote wellness and manage chronic disease together in our journey to offer high quality comprehensive care to the Francophone population.”
Dr. Sandra Toutounji is the clinic’s third family physician. She completed her residency at DFCM in 2020 while working at the Credit Valley Family Health Team’s bilingual site. She, like other residents and clerks, was drawn to the site for clinical training in French. For Dr. Toutounji, who grew up in Mississauga and attended French elementary and high schools in the area, working there as a staff physician is a full-circle moment. “I love this community. I find it’s a rewarding patient population. They’re quite appreciative for the care in their primary language. It’s special to be able to provide that care,” she says.

Dr. Toutounji’s former teachers and other staff of her high school are also patients of the clinic, which speaks to its connections to the local Francophone community. “Whenever new immigrants get here, they’ll choose a francophone school for their kids. The principals or leadership of the school board know us and direct them to us to get their
vaccines updated and health care needs taken care of,” says Dr. Cheung.
He recalls one patient in particular—a pregnant single mother who was a refugee. She was referred to the clinic by the principal of her children’s French school. Over time, the patient was able to set down roots, trained as an early childhood educator and now works as a teacher. “We managed her medical care and helped her settle in the community in collaboration with our team and social services agencies. Our patients feel safe here and they feel like they get complete care,” says Dr. Cheung.
In addition to the clinic’s ties with the local French school boards, it also works closely with community organizations. For example, staff at the clinic refer patients to Oasis Centre des Femmes, a Francophone organization that helps women and children experiencing domestic violence. In turn, the centre refers its clients who are in need of a family doctor to the clinic. “I think because the francophone resources and services that exist are so sparse, you really do have to work as a community to maximize what’s out there,” says Dr. Shaw. “We can provide preventive care, update vaccinations, screen for diabetes and all the great stuff family doctors do, but we also have to be mindful of the social determinants of health and whether this person is connected with different community resources, or their kids are in school. Everything we do is at the level of the community because it is very hard to find services in French.”
30 Department of Family & Community Medicine, University of Toronto
[Left to right:] DFCM faculty members Drs. Sandra Toutounji, Kerrie Shaw and Paul Cheung are physicians at the Credit Valley Family Health Team’s bilingual site, which offers primary care services in French to the clinic’s 2,100 patients.
Caring for patients in their primary language is gratifying, but can also be tricky at times, says Dr. Shaw. “It definitely adds a layer of challenge—oftentimes patients may not understand specialists’ recommendations. You have to spend more time explaining things,” she says. For Dr. Toutounji, who did not do medical school in French, taking care of Francophone patients was initially daunting. Still, she encourages trainees who speak French—even if they are rusty—to pursue clinical opportunities working with Francophone patients as the experience is deeply rewarding. “Patients are so appreciative. Even in those tough conversations where I’ve had trouble finding the words, they’re able to get their feelings across so much more easily and feeling heard in their language means so much to them. Even when I have to use the odd English word here or there—I struggle a bit more with those conversations—it still goes a long way. It’s normal for people to feel anxious if French is not their first language, but I would encourage them to pursue it.”
Where
were
French-Speaking Immigrants in Ontario born?
622,415
Ontario has the largest Frenchspeaking minority community in Canada
2,100
Francophone patients cared for by the Credit Valley Family Health Team’s bilingual clinic
French is the mother tongue of 4% of Ontario’s population Americas Africa Europe Asia 17% 37% 27% 20%
Source: Office of the Commissioner of Official Languages
31 2023 Family Medicine Report – Community
HAVE A HEALTH CONCERN? CALL AUNTIE
 By Alicia Fung
By Alicia Fung
32 Department of Family & Community Medicine, University of Toronto
When
You might turn to your family doctor—a trusted primary care provider with whom you have built a relationship over time and knows your specific health needs. But what happens when you don’t have a family doctor you trust? Or crucially, what happens when you can’t trust the health care system as a whole? This is the case for many Indigenous people in Canada.
Indigenous people regularly experience racism, stigma, stereotyping, and discrimination in health care. An independent investigation performed in the B.C. health care system in 2020 found that 84% of Indigenous people surveyed reported experiencing some form of discrimination in health care. The same investigation also found more than one-half of the Indigenous health care workers surveyed reported they had personally experienced racism in their work environment because of their Indigenous identity.
But this isn’t unique to B.C. According to the Our Health Counts Toronto research project, more than one in four Indigenous adults reported that they have been treated unfairly by health care professionals because of their Indigenous identity. Of the Indigenous adults who have reported unfair treatment, 72 per cent indicated that it had occurred more than once in the past five years.
These harmful experiences have turned many Indigenous people away from accessing the health care they need, says Dr. Suzanne Shoush, a First Nations and Black family physician, and the inaugural Indigenous Health Faculty Lead at the University of Toronto Department of Family and Community Medicine. “We know that anti-Indigenous racism is prevalent. The Our Health Counts data shows that 71% of Indigenous adults in Toronto have said that experiences of racism from a health care provider have either stopped, prevented, or delayed them from seeking follow-up health care,” she explains.
But this comes as no surprise—when negative experiences in the health care system outweigh positive ones, it’s unlikely that you will go to get the care you deserve.

you have a health issue, whom do you go to for help?
33 2023 Family Medicine Report – Community
DFCM faculty Dr. Suzanne Shoush co-founded the Call Auntie Clinic, which provides primary care grounded in Indigenous ways of knowing and being.
“Primary health care is a great concept and model, but the way that it currently exists can be very uncomfortable for people who have been treated poorly by institutions— which is a common experience for Indigenous people,” says Cheryllee Bourgeois, a Métis midwife at Seventh Generation Midwives Toronto.
All of these negative experiences accumulate over time, inducing the systemic exclusion of Indigenous people from the health care system—an exclusion that became much clearer and more profound when COVID-19 hit. But that’s not all. Health disparities experienced by Indigenous communities were also magnified in the pandemic, and it was clear that this was a group who would face more dire consequences from COVID than others.
“Whenever there are gaps in health care or a crisis impacting health care, it will always impact Indigenous communities disproportionately. So, when there was an abrupt shutdown of public health care services due to COVID, we were very worried. These are communities that already have less access to primary care than others and often have no health care provider whatsoever. So, we were worried about the disproportionate exclusion, about stigma, about barriers to accessing testing and information, about social isolation—the list goes on. And there was this heightened fear among the Indigenous community during the pandemic about where it was safe to go, what to do, and who to turn to,” says Dr. Shoush.
Data from the Our Health Counts survey speak to inequitable access to primary care. Results show 63% of Indigenous adults in Toronto have a regular family doctor or nurse practitioner compared to 90% of adults in Toronto who have a regular physician.
To address this exclusion during a critical time, Ms. Bourgeois and Dr. Shoush started the Call Auntie COVID-19 Indigenous Pathways Hotline in April 2020, a COVID information hotline focused on supporting Indigenous communities staffed by Indigenous health experts called “aunties.” The hotline’s name comes from the cultural concept of calling your auntie: a trusted relative —whether blood-related or not—who you can turn to whenever you’re facing difficulty.
“In the Indigenous community, when you’re in trouble, trying to figure something out, or just don’t know what to do next, you call your auntie—somebody you can actually trust. Somebody you know is reliable, consistent, available, and will drop everything to help you,” says Ms. Bourgeois.
Initially, the hotline was meant to be a COVID information resource for Indigenous people and their families who were having trouble navigating the healthcare system. They could “Call Auntie,” and the aunties would provide expert advice about COVID and how they could protect their health and that of their families. But soon, people began calling the aunties for more than just pandemic information.
“People started calling us for things like, ‘I can’t get birth control,’ ‘I can’t get my blood pressure medication,’ or ‘I’m having a mental health crisis’—things that were so bread and butter primary care, that we ended up saying, ‘Ok, let’s open an in-person clinic,’” says Dr. Shoush.
In September 2020, Call Auntie expanded their services to include the full scope of primary care for Indigenous people and their families. But, unlike other primary care clinics in the city, the Call Auntie Clinic takes an Indigenous kinship approach to providing primary care.
34 Department of Family & Community Medicine, University of Toronto
“People started calling us for things like, ‘I can’t get birth control,’ ‘I can’t get my blood pressure medication,’ or ‘I’m having a mental health crisis’—things that were so bread and butter primary care, that we ended up saying, ‘Ok, let’s open an in-person clinic.”
“This idea of kinship care pulls from teachings and kinship systems that already exist in Indigenous communities to support community wellbeing. It’s this idea of shared responsibility for caring for the community because it doesn’t always make sense to have one person who is the expert at meeting the needs of every other person,” says Ms. Bourgeois.
This shared responsibility of care means that the Call Auntie Clinic is a truly team-based model: every auntie on the team is an equal provider and patients can choose who they feel safest with as their pathway to care. Patients can come to receive any primary health care service including reproductive health, harm reduction, pregnancy and postpartum support; they can also come in for food, traditional medicines or for advice around difficult family or community situations.

“The lack of culturally safe care is the largest barrier to healthcare for Indigenous people, so creating these community-based Indigenous-led safe spaces as entry points to care are essential in lowering barriers and creating a for-us, by-us existence within medicine. With Call Auntie, you could come into a very safe space that was very different from hospital spaces and hospital clinics—different from a lot of the way primary care exists in the city. The
More than 1 in 4 Indigenous adults have reported that they have been treated unfairly by health care professionals because of their Indigenous identity
Of the Indigenous adults who have reported unfair treatment, 72% indicated that it had occurred more than once in the past five years.
71% of Indigenous adults in Toronto have said that experiences of racism from a health care provider have either stopped, prevented, or delayed them from seeking follow-up health care
centre of care is the patient, and they can come in and speak to anyone on the team as an entry point into care. Patients can come at a time that works for them and they’re not turned away if they’re ‘late.’ They can come and get traditional medicine. They can come just to get food or a drink if they want—because care doesn’t only mean caring for physical health,” Dr. Shoush explains.
Two years later, the Call Auntie Clinic has a small but mighty team of nine aunties and continues to provide culturally safe care to Indigenous communities across Toronto, improving access to primary health care for a group that has great unmet need.
“By using the systems of culture we know and are used to, we can create entryways and lower barriers to access for a community that we know doesn’t engage in health care in the same way,” says Ms. Bourgeois. “It’s not enough to assume that people don’t have family doctors and having one is the solution. You have to get people to the point where they’re even willing to consider having a relationship with a family doctor—and sometimes that can take a little work. So, our goal is to try and create spaces where people can practice being involved in primary care in a way where they feel comfortable.”
Cheryllee Bourgeois, a Métis midwife and co-founder of the Call Auntie Clinic, examines a pregnant patient.
35 2023 Family Medicine Report – Community
Source: Our Health Counts Toronto
BRINGING THE WINDS OF CHANGE TO TORONTO’S PRIMARY CARE ‘DESERT:’ HUMBER RIVER HOSPITAL JOINS DFCM AS THEIR NEWEST TEACHING HOSPITAL SITE
 By Alicia Fung
By Alicia Fung
For some Torontonians, the most notable thing about the northwest region of the city is Yorkdale Mall, a two million square foot shopping centre that is home to an exclusive lineup of luxury brands and boasts itself as “Toronto’s ultimate shopping destination.” Yorkdale attracts both local and international visitors to Toronto’s northwest and even has a subway station named after it.
But don’t let the extravagance fool you—the same neighbourhoods that house one of Canada’s largest collections of designer brands also houses some of the city’s most socially and economically disadvantaged populations. Over the years, the residents of Toronto’s northwest neighbourhoods have been identified by several reports from Public Health Ontario and the City of Toronto as some of the most impoverished and materially deprived neighbourhoods in the city. These regions also have an aging population with a higher proportion of racialized groups, greater housing density, as well as some of highest rates of crime and lowest rates of post-secondary education completion.
These intersecting inequities have a compounding effect on health. Studies have shown that social and economic factors—also known as the social determinants of health—account for anywhere between 80 to 90 per cent of health outcomes. Health is about more than just access to health care services; the environment and circumstances in which we are born, live and work greatly impact our health and wellbeing. Family physicians can look to their own practices to see clear evidence of this.
“Throughout my practice in the Jane and Finch neighbourhood I have witnessed how social determinants of health impact patient care. It is a challenge for some patients to afford medication, physiotherapy, or even take time off work for specialists’ appointments,” says Dr. Ryan Banach, a family physician practicing in Toronto’s northwest and the Family Medicine Health Human Resources Lead in the Office of Health System Partnership at the University of Toronto Department of Family and Community Medicine (DFCM).
Given that Toronto’s northwest communities face some of the most inequitable outcomes in the city, it comes as no surprise that they were also among the hardest hit by COVID-19. At the start of the pandemic, the rate of COVID-19 was more than 10 times higher in these neighbourhoods than in the least-affected Toronto neighbourhoods. Moreover, despite being disproportionately affected by the pandemic, vaccine rollout in these neighbourhoods was much slower than other areas of the city.
36 Department of Family & Community Medicine, University of Toronto
On top of this, Toronto’s northwest has also been described as a primary care desert: there is clearly a great need for primary care in the region, but there are a low number of primary care physicians available to address those needs. Dr. Banach notes this may be due to a rising share of family physicians who are now retiring or near-retirement age.

“I have noticed recently that more physicians in our area are retiring, leaving many patients looking for new family physicians. Most of the family physicians I know in my area have been practicing for 30 to 40 years and are generally older physicians,” he says.
“There isn’t a lot of interest from new family physicians to move into this community,” says Dr. Art Kushner, Chief of the Department of Family and Community Medicine at Humber River Hospital (HRH), one of the hospitals serving the northwest communities of Toronto. “And as family physicians retire, attachment rates will decrease.”
Only between 11 and 25 per cent of the patient population in the area are attached to a family doctor or family health team. Between low attachment rates, low supply of incoming physicians, and retiring physicians, patients in the area are now finding themselves struggling to access comprehensive primary care.
To address what is quickly becoming a dire situation in primary care in the area, HRH recently joined DFCM as their newest teaching hospital site. The hope is that incoming residents would become a continuous source of new doctors for Toronto’s northwest communities.
“Studies have shown that physicians are more likely to set up their practice in the communities they were educated and trained in. Since they become familiar with the community, the patients, the hospital and the specialists, it’s more comfortable for them to set up practice there after they graduate,” says Sudha Kutty, Vice-President of Strategy and External Relations at HRH.
Humber River Hospital will welcome the first cohort of family medicine residents at their Wilson site in July 2023. Residents can expect to learn from award-winning physicians and experience working in a diverse community—both in their needs and their makeup, says Upasana Saha, Director of Integrated Health Systems and Partnership at HRH.
“This is clearly an equity-deserving population, but that’s not all there is to it. Beyond that is a vibrant community that comes alive through its diversity, and there are a lot of great opportunities for residents to get exposure to many different patient populations and learn how they can serve them better,” says Ms. Saha.
Residents can also expect to work with leading edge technologies. Humber River Hospital prides itself on being North America’s first digital hospital and is consistently at the forefront of innovation. For example, its department of surgery makes use of robotics, which have allowed the hospital to treat more patients in less time with better outcomes. Additionally, its state-of-the-art command centre allows for real-time analytics and tracking of patient care. Residents will have the opportunity to learn and practice with these technologies during their rotations.
Innovation is embedded in HRH’s mindset, and the hope is that incoming residents will embrace this culture of innovation. Dr. Abhimanyu Sud is the Research Chair in Primary Care and Population Health Systems at HRH, a role that creates an important link to scholarship and aligns with DFCM’s interest in community research.
“Our communities need residents and their support,” says Ms. Kutty. “So we’re hoping that incoming residents will take an active role in helping us shape the future of family medicine education and primary care at Humber River.”
37 2023 Family Medicine Report – Community
Gaps in Primary Care Areas of the city with higher primary care needs but surrounded by lower physician supply are clustered in the northwest.
PRESCRIBING BETTER “PILLS” TO SWALLOW
By Alicia Fung

38 Department of Family & Community Medicine, University of Toronto
Avisit to your family doctor may end with a prescription for medication. But what if, instead of medication, you were prescribed a choir class?
This was one of the unconventional prescriptions that Nafisa Nezam Omar had received from her family doctor at Rexdale Community Health Centre (CHC). But perhaps an unconventional prescription was just what Nafisa needed, considering her journey in coming to Toronto.
Nafisa and her daughter came to Canada from Kabul as asylum seekers in 2017. After losing her sister and her home to a rocket attack, her brother to gunfire, and her husband to a heart attack, she packed her life into one suitcase and fled the country with her daughter. The grief of losing her loved ones and everything she once knew, compounded with the stress of starting anew in an unfamiliar country, took a heavy toll on Nafisa’s health.
“A few weeks after I came to Canada, I found this small space in the basement of a bungalow house. There weren’t any bedrooms—it was just a small room. I looked at what I had compared to what I had in Kabul, and I missed my parents, my brothers and sisters, my loving husband, my job—everything. And after living in Toronto for 10 months, I lost 15 kilograms of weight. My family doctor was really concerned, sending me for every kind of examination thinking that it was possibly cancer,” says Nafisa.
After several consultations and examinations, Nafisa was diagnosed with post-traumatic stress disorder. She was prescribed anti-anxiety medication, antidepressants and sleeping pills, among other medications to help her manage her health. Despite this, nothing seemed to help. In fact, to Nafisa, it seemed that the medicines were making her feel worse, making it even more difficult for her to provide for herself and her young daughter in a new country.
“I was taking so many medicines and each one of them has its own side effects. I put them all in front of me and just looked at them, thinking that although I’m living with the
help of all these medicines, it’s giving me more pain and depression,” she says. “But it wasn’t just me having a hard time—all of this really affected my daughter as well. She was only 10 years old when we came to Canada and she was also suffering. She was being bullied in school, her marks were bad, and she was looking to me for support but I couldn’t help her because of my health.”
In 2018, Nafisa finally received a prescription that made all the difference. It wasn’t a prescription for more medication, but rather, a social prescription. But what exactly is a social prescription?
Health is not only influenced by genetics, biology, and lifestyle, but also by a broad range of social, environmental and economic factors. These factors are collectively known as the social determinants of health. Research has shown that the social determinants of health can have a greater impact on health than individual biology, driving between 80 to 90 per cent of health outcomes. Yet, while many primary care professionals are aware of this fact, it can seem difficult to address social needs in clinical practice. Social prescribing helps health professionals support their patients by giving them the tools to formally connect social care and clinical care. By meaningfully “prescribing” social services and resources as they would medicine, primary care professionals can practically address the social needs of people in their practices.
39 2023 Family Medicine Report – Community
“Primary care professionals are in a position to recommend community and social services that can help to improve their patient’s health.”
“Family doctors are specialists in the relationship. When we’re building relationships with people, we often see things that have a huge impact on health, but aren’t the classic medical factors that people think of in the medical model. These are things like food security, housing, income, social connection or social safety nets. Social prescribing is about recognizing that these things come out of the relationships that we build with people and looking at how we can address these social needs in day-to-day practice,” says Dr. Dominik Nowak, a family doctor and an Assistant Professor at the University of Toronto Department of Family and Community Medicine (DFCM).
“If you’re a physician and you’re thinking about how you can support your patients in getting the supports they need, you have to navigate the system yourself and it’s not easy on your own. So, social prescribing looks at how we can improve the pathway and the processes so that clinical care and social care work better together. It’s just putting more tools in a physician’s toolbox,” says Dr. Jennifer Rayner, an Assistant Professor at DFCM. “If we think about this from a health equity lens, people experience barriers in our health care system in all sorts of ways. As one of the most trusted professionals in a person’s life, primary care professionals are in a position to recommend community and social services that can help to improve their patient’s health. So, by leveraging that trusted relationship with a physician and improving the pathway to accessing the programs and supports people need, primary care professionals can help to break down some of those barriers to access.”

So, instead of going to a pharmacist to fill her prescription as usual, Nafisa was referred by her family doctor to a social prescribing navigator who worked collaboratively with her to connect her with non-clinical, community-based supports based on her interests. In her case, the social
prescription came in the form of a senior group at Rexdale CHC, where she joined a choir class, learned tai chi and exercised with a Zumba group, among many other activities. Being part of this group not only helped Nafisa find a community where she felt welcomed, but also helped improve her physical health immensely.
“I slowly stopped taking all the medicine and I was able to return to my normal weight. I also stopped having nightmares,” says Nafisa.
The social prescribing program at Rexdale CHC was part of a larger social prescribing pilot called the Rx: Community project led by the Alliance for Healthier Communities, where Dr. Rayner is Director of Research and Evaluation. Eleven CHCs across Ontario participated in the pilot project, in which 147 providers referred more than 1,100 clients to 3,295 social prescriptions. Participating clients noted that connections to non-medical interventions helped to reduce stress and anxiety, increase sense of self-confidence and purpose, and give them the knowledge and tools to better manage their own health. Overall, providers saw improvements to their clients’ health and wellbeing, and clients self-reported a 49 per cent decrease in feelings of loneliness, a 12 per cent improvement in mental health, and a 16 per cent increase in a sense of community belonging.

Although the word “prescribing” may imply a one-way relationship between a healthcare provider and a client, this is not the case with social prescribing. A core component of social prescribing is to invite clients to co-create solutions that are tailored to their interests and community. When people are involved in creating solutions for themselves, it gives them a sense of agency and empowerment over their own health.
 Left to right: Dr. Jennifer Rayner
Dr. Gary Bloch
Left to right: Dr. Jennifer Rayner
Dr. Gary Bloch
40 Department of Family & Community Medicine, University of Toronto
Dr. Dominik Nowak
“Some clients might have certain passions or skills and when we find or create spaces that support them in using those skills, they can then take the lead to create diverse programs and offerings for others. And I think that’s one of the most amazing pieces of social prescribing—sometimes the patients themselves become the solutions. Social prescribing moves beyond just looking at their presenting problems and asking them ‘What’s the matter with you?’ but instead asking them, ‘What matters to you?’” says Dr. Rayner, who is one of the authors of the Rx: Community project.
“There isn’t a one-size-fits-all approach. Different communities are impacted differently by the social and structural determinants of health, so social prescriptions are co-designed with patients and tailored toward community needs. It’s about listening and learning about what a person or a community is sharing is most important and would be helpful,” adds Dr. Nowak, who supported the project.

While social prescribing is a useful tool for primary care professionals, it is not a catch-all solution that replaces clinical care or robust social policies that address the social determinants of health on an upstream level. Social inequities come about because of structural issues in society and without working to try and shift those structures, it is unlikely that we will see a significant impact on the health of our communities. We cannot ignore, however, the downstream interventions for purely upstream ones, says Dr. Gary Bloch, a family physician and an Associate Professor at DFCM.
“I don’t think purely upstream interventions are enough, and certainly purely downstream interventions are not enough. We need to look at these issues from a broad understanding of what social needs are for patients, but also from a very practical perspective of what we can do dayto-day to deal with the very real social needs our patients
present with. And it’s these day-to-day social needs that I think social interventions such as social prescribing are attempting to address. It’s giving physicians easy-to-understand and easy-to-implement tools to intervene in a patient’s social needs,” says Dr. Bloch.
Over the last few years, the social prescribing movement has been gaining traction as the medical community’s understanding of the underlying drivers of health continue to evolve. As we learn more about the social determinants of health and its influence on health inequity, medical schools have increased their commitment and investment in teaching future physicians about these topics and how they can respond to and advocate for the needs of their patients and communities beyond their clinical practice.
“I routinely feel like I’ve come across medical students and residents who have a far deeper understanding of social inequity than I ever have, and they really push my understanding of where we’re at and where we need to go in this work in incredibly powerful ways,” says Dr. Bloch. “We’re seeing new physicians joining us with a whole different level of comprehension of social issues and a whole different skillset for dealing with these issues, and I think this will really transform clinical practice well into the future.”
There is still much to learn about how health professionals can best support their patients faced with social challenges, but social interventions such as social prescribing have proven to be transformative for many people, including Nafisa and her daughter: “Every medicine has its own effect, but this social prescription was really like magic— especially for me, but also for my daughter. She is 16 now and she looks like she’s really enjoying her life. This program saved me from a period of worry and deep grief and brought me hope and thankfulness.”
41 2023 Family Medicine Report – Community
Source: Alliance for Healthier Communities

42 Department of Family & Community Medicine, University of Toronto
Q&A: DR. MELANIE HENRY MEET DFCM’S INAUGURAL VICE-CHAIR, COMMUNITY AND PARTNERSHIPS
Dr. Melanie Henry had never considered becoming a doctor until her high school English teacher suggested it. “I remember turning to him and saying, ‘I can’t do that,’” recalls Dr. Henry, who, despite having parents who worked in health care (her mother is a nurse and her father, a respiratory therapist) hadn’t thought about a career in medicine. Dr. Henry, who was interested in health policy, health systems and health equity during undergraduate studies, ended up proving her teacher right. She is the first Vice-Chair of Community and Partnerships at the Department of Family and Community Medicine (DFCM) at the University of Toronto. The creation of this leadership role is one of the priorities of DFCM’s strategic plan. The aim is to build and steward partnerships with community organizations and groups, public health units, and other health system and social service associations—especially those serving equity-deserving communities—to promote better health outcomes.
It is a role for which Dr. Henry is well suited. She is a family physician on the Health For All Family Health Team, an interprofessional primary care clinic that is the site of the Markham Family Medicine Teaching Unit. In addition to caring for her patients and supervising family medicine resi-
dents, Dr. Henry is also the organization’s board chair and interim physician lead, working to advance its mandate of increasing access to family health teams, particularly for people who do not have a regular primary care provider. As the site’s global health director, Dr. Henry oversees the global health curriculum which, for example, teaches staff, faculty and trainees about social determinants of health, and provides Indigenous cultural safety training for residents. She also partners with York Region, Public Health and community paramedics to provide primary care to people staying at emergency housing shelters in the York Region.
Having grown up in Newmarket, Dr. Henry knew that when she completed her fellowship in global health and vulnerable populations, she wanted to work in the York Region to develop services for people in her community. “A lot of the people who’d done the fellowship previously had gone back to the city [to work downtown]. I recognized that the community I grew up in didn’t really have any of those services. It didn’t have any sort of physician looking after either the homeless population or people with addiction or mental health issues. There wasn’t a service like this up here like there was in Toronto. I wanted stay in the area and see what we could develop up here,” she says.
43 2023 Family Medicine Report – Community
Outside of work, Dr. Henry is busy raising two children—a daughter, aged nine years and a son, aged five years—and playing on various sports teams. Here, she sits down with Alisa Kim of DFCM Communications to talk about what drew her to the Vice-Chair role, what she hopes to accomplish in the short-term and the pitfalls of multitasking.
Why did you want to be a family doctor?
Stories are my big thing. I really think there’s a huge privilege in being able to understand where people are coming from. One of the lovely things about family medicine is that you’re there at various intersections, when people are going through good things and bad things, and you’re able to walk with them through those parts of their health care journey.
One of the major reasons I chose family medicine is I felt like I could have some impact on some of the social determinants of health that affect people’s health care in a way I that couldn’t address in another specialty.
What drew you to the role of DFCM Vice-Chair, Community and Partnerships?
I think there are a lot of parallels between my choice of family medicine and choosing the Vice-Chair role. I think the stories piece continues. It’s growth from individual stories and understanding where individuals are coming from, to understanding where whole communities are coming from.
I had a really lovely experience working with the Black Health Vaccine Initiative and the Black Physicians’ Association of Ontario working with my own community doing work to try and increase vaccine awareness in the region. That was hugely impactful for me because I was impacting
my own community, but also understanding as a physician in this role, I’ll be able to impact the story and the way in which those communities are seen and able to access care, which is really important to me.
What is your vision for the role?
It’s in development, but I think the strategic plan is a guidepost for what this position is going to look like and how we’re going to work to embed some of the work we’re doing at the DFCM in the community. I want to see that collaboration happen.
Part of my vision is to understand the communities the DFCM impacts—what they need from us and how best we can work with them to be able to support the things they need. That’s one of the things I learned in the work that I did with the Black Health Vaccine Initiative: it’s so important to listen to the communities and really understand what it is they need and want. And it’s appreciated when you do that. It’s going to be enacting the DFCM strategic plan while really trying to understand how the strategic plan can help the communities based on what they are telling us they need.
What are some of the immediate priorities?
One will be to look into community health centre partnerships. There are lots of community health centres in the GTA and we don’t have a lot of great connections with them. We’re going to work on those connections. That’s certainly a priority.
We’ll be working with the equity, diversity and inclusion specialist to get the Black Health Advisory Table up and running—something Dr. Onye Nnorom [DFCM’s inaugural
44 Department of Family & Community Medicine, University of Toronto
“It’s so important to listen to communities and really understand what it is they need and want.”
EDI Lead] had recommended. That’s another priority. And to continue some of that work she started in her role as the EDI Lead. Those are two things I will get going on pretty quickly. I am looking forward to meeting with faculty and staff of the DFCM, and building strong community partnerships.
How will you measure success?
I think right now it will be about sorting out what responsibilities, according to the strategic plan, we’re looking at and using some of the benchmarks from the plan to measure any success we’re able to achieve.
Measuring success in a new role is challenging because we’re going to be creating new things and projects. Creation of new projects is important in and of themselves because we need to start something to be able to measure it, but I think ultimately, we’re looking for community engagement in the work that we’re doing and having those community organizations we’ll be partnering with feeling like they are part of the DFCM and the work we’re doing.
If you hadn’t gone into medicine, what would you have done?
I don’t know! [Laughs.] In my undergrad program, I minored in bio and chem thinking I’d eventually write the MCAT or go into the medical field. Both of my parents are in health care. My mom is a nurse and my dad is an RT [respiratory therapist]. Because of that, I knew I wanted to work in health care.
The more I learned about the system and health inequality, the more I wanted to be able to impact that. I’m not sure if there’s a profession I would have gone into otherwise. I al-
ways had a sense as I narrowed down what I wanted to do, that impacting health equity and the social determinants of health in the community at large was something I wanted to do. I think I’m in the right profession!
What do you like to do outside of work?
I love coaching soccer. My daughter is a soccer player and I have coached her soccer team since she was three. I also play soccer and have been on the same women’s team for the last almost 20 years. It is a great community for me. My son has just started to get interested in basketball and so he inspired me to join a league this year. We’re testing my knees and seeing if that’s something I can continue to do. I like being outside, and have also started skiing with my family. When I’m trying to relax, I play piano. I’m no performer, but it’s something that I do just for me.
What is a typical day for you?
I’d say most days I start work when I roll out of bed at around 6 a.m. I think one of the things that helps me be successful is my ability to multitask. I have to be careful about that because sometimes it distracts me from things that are important like family time, but I typically am trying to answer emails as I’m getting ready for the day and organizing my kids in the morning. I try and get into the office by 8:30 a.m. and work until 4 to 5 p.m. I do the kids’ activities in the evening and then start again when they go to bed. I try to protect certain times of my day, and try to keep weekends for my family as much as possible. I’m so lucky to have an amazing partner who supports the work that I do. It really helps to make things run smoothly.
45 2023 Family Medicine Report – Community
CULTIVATING A CULTURE OF CURIOSITY AND CONTINUOUS QUALITY IMPROVEMENT
 By Alicia Fung
By Alicia Fung
Providing the highest quality care for everyone should be the goal that all those involved in delivering health care strive for. As our understanding of high-quality care evolves, we must adapt and improve our systems and processes to meet ever-changing standards of quality. Change-making can be a slow process, but the healthcare system will not fully realize its potential unless continuous efforts to improve are made by those who have the ability to change the system from the inside. A good starting point for this is cultivating a culture of curiosity where errors made, questions asked, and areas of improvement are seen as opportunities rather than failures. What better place to start fostering such a culture than during postgraduate medical education?
The University of Toronto Department of Family and Community Medicine (DFCM) Postgraduate Program, under the leadership of Dr. Risa Freeman, Vice-Chair of Education and Scholarship, formalized the development of a continuous quality improvement (CQI) program with the goal to improve educational outcomes for residents. The program was created in response to a new national standard maintained by the College of Family Physicians of Canada for the evaluation and accreditation of family medicine residency programs; the Postgraduate Program at DFCM saw the value of creating a process that ensures that CQI is embedded in medical education.
“While we had already been collecting multiple forms of education data to evaluate our educational offerings, we needed a formal process to really assess areas of improvement and develop measurable action plans. DFCM has been leading QI in patient care for the last 10 years, and it is time to bring that culture and lens to our educational programs,” says Dr. Stuart Murdoch, who is an Associate Professor and Postgraduate Program Director at DFCM.
Dr. Carolyn McQuarrie instructs former resident Dr. Alia Dharamsi (right) in the emergency department.
46 Department of Family & Community Medicine, University of Toronto
While many are familiar with quality improvement in clinical practice, bringing this perspective to medical education is relatively new, says Dr. Gurpreet Mand, an Assistant Professor and the CQI Lead at DFCM. “There was no guidebook or other postgraduate programs that we could look to as a reference, but that doesn’t mean that QI wasn’t happening in medical education before. We were always trying to improve and always trying to get better, but I think part of this new CQI program at DFCM has really been about capturing those endeavors,” she says.

The first step was to gain insight into the residency program at DFCM. To do this, the CQI team developed the CQI Promotion survey to get direct feedback from the residents at each academic teaching site about their experience, the learner environment and learner treatment. The feedback received would then be analyzed and used to inform improvement goals and guide action planning at each of the teaching sites. While work in this area has just started, Dr. Mand is already starting to see CQI being integrated into the culture of medical education at DFCM.
“We’ve had a lot of engagement from the sites. People have really opened their calendars to meet with the CQI team and review the data to identify what the opportunities are for improvement, but also to celebrate what’s working well—because that’s important, too. CQI is becoming a standing agenda item at our sites’ committee meetings, and program directors have plans to share the data with faculty and residents at their sites,” says Dr. Mand. “We want to show residents that we care about their learning environment and that we’re responding to their feedback. We don’t do surveys to put them on a shelf…This work is real and in time, the residents will start to see action plans based on their feedback.”
Plans for improvement are already underway at many of the teaching sites. For example, survey results at Scarborough Health Network (SHN) noted that residents did not find field notes very helpful. Field notes are short reflections by both residents and preceptors to record, assess and provide feedback on resident performance. Not only are they useful for tracking progress throughout their residency, but they are also required by the College of Family Physicians of Canada to ensure that competencies are being met. Getting documented feedback for improvement should be useful; Dr. Jennifer McDonald, the site director at SHN, says she finds it curious that residents at her site do not find the field notes helpful. She plans to review the importance of field notes with preceptors and residents at SHN, so they understand their value and get the most out of it.
“We know people are getting lots of good feedback all the time, but the question is whether we’re writing it down as a field note. So, we want to make sure preceptors are capturing verbal feedback as field notes, but also that residents understand that as a professional family doctor, learning also comes through self-reflection. So, we’re hoping to bring this message better to residents, so they really understand the importance and value of field notes,” says Dr. McDonald.
The CQI process is on-going. Although it has been less than a year since the CQI team launched their inaugural survey, they are gearing up to launch the next survey, with plans to improve it to capture actionable feedback more effectively and to ensure that the resident voice is represented when developing change initiatives within the residency program.
“No matter how good something is, there’s always room for improvement, and I think that allows for a dynamic environment where we’re always looking to be better. I genuinely believe that if residents and learners feel that we are being responsive to the feedback they’re giving, then they will be more engaged in their learning. And if people feel engaged, they do better work,” says Dr. Mand.
“Our overall aim is to set a positive tone and create a culture of CQI,” adds Trish O’Brien, the Education Development Projects Manager at DFCM who works closely with Dr. Mand on the CQI team. “Sometimes the feedback is unexpected and hard to understand, but we’re willing to explore the messiness of improvement. We try to model the mantra ‘start where you are, use what you’ve got, do what you can’ and acknowledge that better is always possible.”
47 2023 Family Medicine Report – Community
RELATION SHIPS
48 Department of Family & Community Medicine, University of Toronto
A LITTLE HELP FROM MY FRIENDS: DFCM MENTORSHIP PROGRAM SUPPORTS FACULTY AT ALL CAREER STAGES
By Alisa Kim
Looking back on her career, Dr. Joyce Nyhof-Young says she has benefitted richly from different kinds of mentorship.
Whether it came in the form of people supporting her by taking her out for dinner when she was a stereotypical starving student, or colleagues who gave strategic advice that helped her apply for senior promotion, mentorship has shaped her career trajectory.
“Mentorship has been absolutely essential for my career development. That’s one of the reasons I like being a mentor for so many other people, because it passes on the kindness that I’ve been shown,” says Dr. Nyhof-Young, a Professor in the Department of Family and Community Medicine (DFCM) at the University of Toronto.
RELATION
“The delicate balance of mentoring someone is not creating them in your own image but giving them the opportunity to create themselves.”
49 2023 Family Medicine Report – Relationships
— Steven Spielberg
As an education scientist, Dr. Nyhof-Young is building capacity in education scholarship at DFCM by supporting faculty working in this discipline. She helps clinicians and clinician teachers with scholarly projects that involve everything from developing resources and curricula, evaluating programs and studying related theoretical issues. She views this collaboration as a form of mentoring. “I really enjoy working with teams. I give consultations before they start to help them get off on the right foot and save time and give them a shoulder to lean on as they make their way in education scholarship,” says Dr. Nyhof-Young.
In 2020, Dr. Nyhof-Young was promoted to full professor. She says her promotion effort occurred over several years, and she could not have navigated the process of senior promotion alone. Several DFCM faculty members provided support and advice, but it was the counsel of colleagues like Dr. Ruth Heisey that informed her approach, Dr. Nyhof-Young says. “I think promotion is a very intimidating process. It’s often like starting in education scholarship. It really helps to have people who are on your side, helping you to move forward in the best way possible. The ideas and insight of supportive colleagues throughout the promotion process really made a huge difference and made my path through promotion a lot smoother than it otherwise would have been,” she says.
Mentorship for faculty at all stages of their career is a departmental priority, says Dr. Viola Antao, DFCM’s Faculty Mentorship Lead. “There are many people who may benefit from mentorship but never connect. That’s a huge gap and need,” says Dr. Antao, an Associate Professor at DFCM and a family physician at Women’s College Hospital.
Dr. Nyhof-Young is paying the good advice she has received forward. In August 2022, she participated in a DFCM mentorship panel event aimed at providing guidance on senior promotion. In it, she talked about the value of seeking mentorship, how to build one’s CV and dossier efficiently, challenges she faced, and the importance of guarding emotional health and well-being throughout the process.
The panel discussion on senior promotion is one of many mentorship initiatives Antao is leading at DFCM. She is developing best practices and strategies in mentorship, an area about which she is passionate. “Research shows people who get high-quality, well-matched mentorship are more likely to report job satisfaction, less likely to burn out, and more likely to advance in terms of their career,” says Dr. Antao.
To build mentorship capacity at the department and understand what the needs are, Dr. Antao conducted a department-wide survey of faculty. Results showed the top pri-
50 Department of Family & Community Medicine, University of Toronto
“Research shows people who get high-quality, well-matched mentorship are more likely to report job satisfaction, less likely to burn out, and more likely to advance in terms of their career.”
orities are teaching, wellness, promotion, and supporting faculty who have recently graduated and faculty who are from equity-deserving groups.
Some of the mentorship program’s activities include virtual coffee chats, to provide flash mentoring between faculty at different teaching hospital sites on a one-off basis, as well as matching faculty for longer-term, one-to-one mentoring relationships. Dr. Antao notes a pilot program with 16 mentees is being conducted and has received positive feedback from participants.
She encourages faculty who want mentoring or are willing to provide mentorship to reach out to her office. “People who have suffered challenges like life transition or illness have said, ‘I wish I had mentorship during that time because it would’ve made a huge difference.’ There are many reasons why people want a mentor, and they don’t necessarily know how to connect,” says Dr. Antao.
The reasons people want mentorship are varied and personal. Dr. Nyhof-Young recalls a former colleague who was close to retirement needing support during that period. She says having guidance is especially meaningful during times of change. “I think that mentorship is key at transition points in our careers. Gaining the mentorship you need makes things so much easier.”
Dr. Viola Antao (right) is the faculty mentorship lead at DFCM. She is a mentor to Dr. Sofia Solar, who is in the second year of her family medicine residency. Dr. Antao says mentorship is critical not only during the first few years after graduation, but throughout all stages of a faculty member’s career.

Top Three Areas of Mentorship that most Interest DFCM Faculty
1. Career trajectory
2. Academic support
3. Work/life balance and wellness
(Source: 2022 survey of faculty N=116)
51 2023 Family Medicine Report – Community

52 Department of Family & Community Medicine, University of Toronto
HEALTHY BARRIE: A DATA-DRIVEN APPROACH TO BUILDING HEALTHIER COMMUNITIES
By Elaine Smith
The project aimed to use population health indicators to measure health and social well-being in local neighbourhoods and use that information to inform city policy and planning.
“Matt was a young rock star health care provider and leader,” says Dr. Stuart Murdoch, former chief of family medicine at RVH and the project’s original academic chief, who tapped Dr. Orava for the role.
Today, eight years later, Dr. Orava is a family physician, member of the Barrie & Community Family Health Team and faculty member with the University of Toronto’s Department of Family and Community Medicine (DFCM). He is not only responsible for training the U of T’s family medicine residents at RVH, but serves as Healthy Barrie’s primary care lead. He has been instrumental in ensuring the project meets its goals.
“Barrie seemed like an ideal place to think about initiating a better integration of community health, public health and family medicine with the assistance of the municipal government,” says Dr. Ross Upshur, a Professor at DFCM and U of T’s Dalla Lana School of Public Health (DLSPH). He worked with other U of T leaders, Dr. Adalsteinn Brown, Dean of DLSPH, and Dr. Murdoch, DFCM’s Director of post-graduate education, to get Healthy Barrie off the ground. “There was one large family health team, a health unit with a progressive medical officer of health and a mayor and council that wanted innovations in community health. It was an opportunity to engage in long-term thinking and undertaking a long-term project with impact,” Dr. Upshur says.
In 2020, representatives from the city, the Simcoe Muskoka District Health Unit, Simcoe County, the Barrie Police Service and RVH signed the Healthy Barrie Accord, formalizing
53 2023 Family Medicine Report – Relationships
Dr. Matthew Orava was a new family medicine resident at Royal Victoria Regional Health Centre (RVH) in Barrie when he was asked to take on the additional role of research lead for Healthy Barrie—an incipient citywide vehicle for innovative, collaborative efforts to improve community health.
support for projects like Healthy Barrie that started in 2015 and committing to collaborate on future planning for community wellness in the city.
As the project got underway, Dr. Orava and representatives for the other partners participated in a regular working group. Each organization agreed to provide data to allow for a more complete snapshot of the health of the community. “The health unit had access to anonymized data we could share and we received ethics approval this summer to share and study it,” Dr. Orava says.
Initially, each partner organization compiled potential indicators based on available data. The indicators were reviewed and then ranked using an indicator prioritization tool. After rounds of discussion and ranking, 29 health indicators were included in a 2018 Community Snapshot and these fell into the four theme categories: health behaviours, health outcomes, service utilization and neighbourhood characteristics, and social determinants of health.
Some of the many indicators available were statistics about: alcohol use, diabetes, life expectancy, traffic-related air pollution, frequency of primary care use, utilization of city recreation programs, median household income and food security.
To create the Community Snapshot, in accordance with the Healthy Barrie project charter, Dr. Orava and team were to map and describe the characteristics of Barrie neighbourhoods, which he did with the help of data from UTOPIAN, the U of T Practice-Based Research Network and the Simcoe Muskoka District Health Unit. The team analyzed the principal components of the data and aligned it with Statistics Canada census areas. Next, they worked with a geographic information specialist to create a series of maps visually illustrating how each area fared with regard to the indicators. For example, the colour-coded maps allow the viewer to see at a glance the prevalence of smoking in the city’s neighbourhoods or the median household income in these same neighbourhoods.
COVID slowed down the project. Dr. Orava has since re-run the data provided by the family health team, which will alter the snapshot. His next step will be to take all the data and conduct analyses to see if there are correlations between various indicators and whether those correlations have statistical significance. He plans to begin with diabetes or body mass index and correlate it with each area’s walkability, income level and availability of healthy food sources, taking care not to stigmatize individual neighbourhoods.

“There’s a strong culture of health change here, so we’re set up for success.”
54 Department of Family & Community Medicine, University of Toronto
—Dr. Matthew Orava, Healthy Barrie Research Lead
Community ‘snapshots’ like these show the relationship between a condition, like diabetes, and income level. This type of data can help municipal government and health system leaders with public health planning and developing service policy to help build healthier communities.
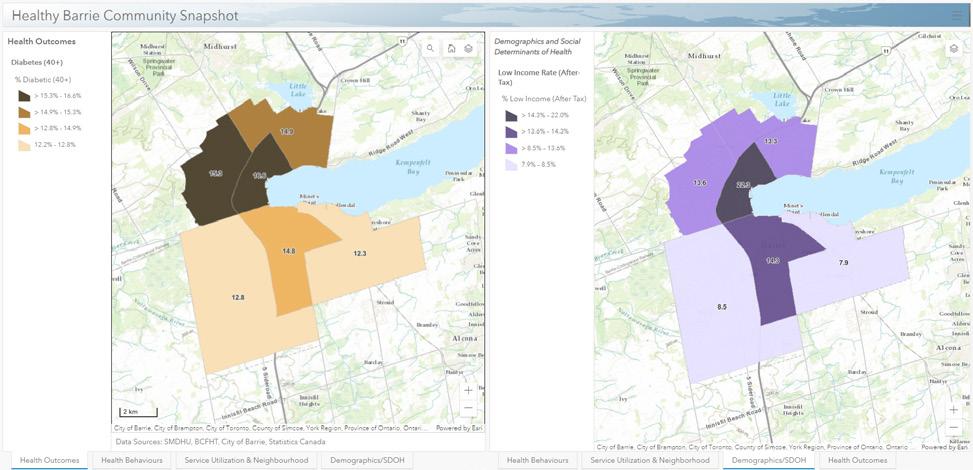
Meanwhile, Dr. Orava and his partners strengthened their own ties and built relationships with other organizations interested in the project and the information it can provide. The Dalla Lana School of Public Health has funded a project manager, Dr. Patrick Feng, and Dr. Orava has connected with the Upstream Lab at St. Michael’s Hospital in Toronto, run by DFCM’s Dr. Andrew Pinto, to tap into their expertise on urban health interventions. The Simcoe Muskoka District Health Unit continues to provide epidemiological and knowledge translation support. The Joannah and Brian Lawson Centre for Child Nutrition at U of T appointed Dr. Orava the Tristan Lawson Distinguished Fellow in Child Nutrition and Community Engagement to devote time to the project and the RVH Foundation funded a summer student to assist him.
Locally, the food bank has expressed interest in the data so it can make people aware of healthy food options, and Dr. Orava is hoping Barrie businesses and the city government will promote healthier choices that are available.
“There’s a strong culture of health change here, so we’re set up for success,” Dr. Orava says.
The project charter commits him to providing the data to Barrie’s mayor, council and health care administrators to inform service policy and public health planning and drive change that leads to a healthier population.
“Once we have the new maps, we can start making changes,” says Dr. Orava. “We can sit down with council and talk about what can be done in each ward and perhaps be proactive when new developments are planned, too.”
With a newly elected council, there may be a learning curve, but he is hopeful and has visions of expanding the program to include the entire Simcoe Muskoka region.
Dr. Upshur sees Healthy Barrie as a potential prototype for other cities to use.
“Healthy Barrie emerged out of trends in health system thinking,” he says. “It could be a real model for other communities to think about similar partnerships, since the rest of the province is more like Barrie than like Toronto in terms of system complexity. It makes sense for communities to take the long view and invest.”
55 2023 Family Medicine Report – Relationships

56 Department of Family & Community Medicine, University of Toronto
FINANCE 101 FOR MDS FROM SAVING AND INVESTING, TO RUNNING A PRACTICE LIKE A BUSINESS, DR. STEPHANIE ZHOU

TEACHES TRAINEES
FINANCIAL LITERACY
By Alisa Kim
Social media is often blamed for the sense of FOMO (fear of missing out) people feel when comparing their lives to those of people in their network.
57 2023 Family Medicine Report – Relationships
Dr. Stephanie Zhou, an Assistant Professor in the Department of Family and Community Medicine (DFCM) at the University of Toronto, understands how people feel pressured to “keep up with the Joneses” when scrolling on social media. “You’re friends with people in your class. You see them go on expensive vacations and buy expensive clothing. This is very common on Instagram, which is a highlight reel of people displaying lavish lifestyles,” she says.
For years, Dr. Zhou, who did her medical training at the Temerty Faculty of Medicine at U of T, has been on a mission to educate and equip others to enhance their financial health. Her foray into this space began with a talk she gave called “Affording Medical School,” aimed at encouraging students—particularly those from economically disadvantaged backgrounds—to choose a career in medicine by tapping into scholarships, resources and assistance programs designed to lower the barrier to entry to medical school.

The positive response to the talk led her to work with the Dean’s office at the Temerty Faculty of Medicine to develop a financial literacy curriculum for medical students and residents. Courses for medical students cover topics like budgeting, credit scores and choosing a line of credit, paying down student loans and the basics of investing. “A lot of students don’t know what compounding is, how it works, and how it can snowball your debt,” says Dr. Zhou, who cites 2020 data showing the median debt for graduating medical students is about $100,000. “A lot of students don’t get financial literacy teaching because in medicine, you’re so focused on learning the medical content. There are times when students have finished watching one of my
lectures and asked what a TFSA [tax-free savings account] was. You realize by talking to students and getting the feedback, their financial literacy is very low.”
A unique feature of the curriculum is a section she teaches on social determinants of wealth. “We talk about financial abuse, intergenerational debt and Black debt, the economics of poverty and what perpetuates poverty. We also talk about why is it that certain racial groups may have experienced discrimination in the financial system and how that impacts them in our generation,” she says.
The courses she teaches residents deal with billing, how to manage their practice, negotiating contracts for shortterm locum positions and incorporating their business. Every doctor is a small business owner, says Dr. Zhou, who is also an addiction medicine physician at Sunnybrook Health Sciences Centre and the lead physician at the Don Mills Family Health Team. She makes the link between poor financial literacy among physicians and the decreasing number of new and existing practices. “Expenses are getting much higher in terms of rent and paying staff. If doctors don’t learn how to bill, which is the main way they earn income, they’re not able to make enough to help them run their practice. There’s also administrative work that’s not paid so doctors may not be figuring out how to make that portion more efficient. That’s not stuff doctors are taught or think about, such that once they go into practice, it leads to them not feeling experienced enough, so there’s no incentive to open a new family clinic or any clinic for that matter, because it’s not financially sustainable.”
Dr. Stephanie Zhou, an Assistant Professor in the Department of Family and Community Medicine, led the development of the financial literacy curriculum for medical students and residents in the Temerty Faculty of Medicine at U of T.
58 Department of Family & Community Medicine, University of Toronto
“Financial literacy is what allowed me to get out of poverty and learn how to maximize the power of money as a tool.”
She notes prior to her talks on billing, she surveys the class—who are nearing graduation—about their comfort level with opening a practice. “Everyone chooses ‘least comfortable’ as their answer. It is surprisingly high. ‘Have you ever been taught billing?’ ‘Are you comfortable asking your preceptor about billing?’ The majority say no and they’re about to graduate in four months.”
Dr. Zhou also connects poor financial skills to another major health system problem: physician burnout. “When you are very much in debt, you have pressure to work harder and harder and longer hours just to service that debt. You can’t out-earn a spending problem. That’s what leads to a lot of doctors burning out because the more they work, the more time it takes away from family and their personal lives. They work really hard and then think, ‘now I have to treat myself’ and it perpetuates a cycle of poor spending habits and high debt,” she says.
Such insights resonate with Dr. Alis Xu, who is completing her final year of the Integrated 3-Year Program in Leadership at DFCM and is also co-president of the Family Medicine Residents Association of Toronto. “Dr. Zhou does a great job of not just telling us the technical things about billing, but also giving us life wisdom. I think sometimes that’s what a resident needs—a bit of financial coaching. I think her teaching helps with lifestyle changes we can make to help us with financial wellness,” she says.
Dr. Xu also links financial stress with physician burnout. She cites research showing part of the reason graduates of family medicine do not pursue comprehensive office-based family medicine is because they hope to circumvent burnout. “Some people want to avoid that, and that’s totally
fair, but if we want to encourage people to take on the role of family physician—the ‘quarterback’ who coordinates care—then we need to think about what are some of the things we can do to prevent people from burning out? Having that financial literacy is a key part of that,” she says.
During the pandemic, Dr. Zhou started accounts on social media, both with the handle Breaking Bad Debt to share her content with a wider audience. Many of her YouTube lectures have racked up thousands of views, with students from across Canada from various disciplines commenting on her videos. Due to enormous interest in financial education, Dr. Zhou started the Canadian Physicians Financial Wellness Conference to bring the financial literacy curriculum to a national audience. Each year, ticket proceeds have gone to charitable causes.
When asked why she thinks this area is so important, Dr. Zhou, who worked part-time jobs and applied for scholarships and bursaries to fund her education says, “Financial literacy is what allowed me to get out of poverty and learn how to maximize the power of money as a tool. I always tell my students money is one of the most powerful tools in society, especially as a way to advocate.”
In a full circle moment, she, along with her partner, Colin Lynch, have created an endowment fund called The Equity Award, to provide scholarships in perpetuity for students in need who have also developed opportunities and resources for others with financial need. “It’s not just a bursary. It encourages you that even if you come from a low-income background, you can still pay it forward,” says Dr. Zhou. “Having income to do that through my investments allows me to empower other people.”
specialties
Source: Pisaniello et al. Effect of medical student debt on mental health, academic performance and specialty choice: a systematic review. 2019
$61K
in Ontario
30.7%
Canadian medical school graduates who rank family medicine as their first-choice discipline
Source: Association of Faculties of Medicine in Canada and Canadian Resident Matching Service
High debt levels negatively impact wellbeing & academic outcomes, driving students to higher paying
median
for
medical
salary
graduate
1
debt
graduating
students in Canada $100K
of post-
year
resident
59 2023 Family Medicine Report – Relationships
OFFICE OF HEALTH SYSTEM PARTNERSHIP ENGAGES PRIMARY

CARE
PROVIDERS TO ADDRESS THE HEALTH SYSTEM’S MOST PRESSING NEEDS
By Elaine Smith
Dr. Catherine Yu is the Engagement Lead of the Office of Health System Partnership at the Department of Family and Community Medicine. She is also a family physician and medical director of Health Access Thorncliffe Park.
60 Department of Family & Community Medicine, University of Toronto
The Office of Health System Partnership (OHSP) at the Department of Family and Community Medicine (DFCM) was established to bring to bear the department’s academic expertise in family medicine and primary care on the needs of the health system.
“As governments look to rebuild health systems post pandemic, there is an understanding that the foundation of these recovery efforts must be robust family medicine and primary care,” says Dr. Danielle Martin, Professor and Chair of DFCM. “We need better access, equitable services and consistent quality—all at a cost we can afford. The Office of Health System Partnership applies our department’s tremendous academic strengths to these health system challenges and provides primary care leadership at the local, provincial, national and global levels.”
It’s a large task, but Dr. Martin has assembled a stellar team to lead the work of the OHSP. She envisions a local team, deeply embedded in the health systems of Toronto and the GTA; a provincial and national group of leaders providing advice to governments and system leaders about how to improve family medicine and primary care; and a global team, working in concert with the WHO Collaborating Centre on Family Medicine and Primary Care.
One initiative of the OHSP is a local partnership with the Toronto Region of Ontario Health to model and test ways of bringing better primary care to all Ontarians, as well as enhanced health care overall.
“Dr. Martin saw the opportunity for DFCM to lead and support the formation of a co-ordinated engagement structure for primary care leadership in the Toronto Region,” says Dr. Catherine Yu, an Assistant Professor at DFCM and the OHSP’s Engagement Lead.
“The five OHSP-Toronto Region leads will try to make sense of what needs to be done to participate operationally in health system transformation; we can implement and test solutions,” says Dr. Yu, who is also chair of the board for the East Toronto Family Practice Network, a community of family physicians with a mission to create equitable access to inter-professional care for all family practices.
“We want to empower primary care. As the ‘front door’ of our public health care system, we need a scaffold to coordinate the breadth of services that primary care provides. In other words, we require regional and local strategic, administrative and operational supports, to be able to pivot when priorities shift for the populations we serve, especially for those in equity-deserving neighborhoods. These structural supports already exist in other wide-reaching public services like hospitals and public schools. We are articulating this need to Ontario Health and the Ministry of Health and working to establish a primary care network infrastructure for each of the Ontario Health Teams in Toronto. [OHTs are charged with looking after the health-care needs of the entire population in a specific geographic region.] We need the right resources to respond to the community in a co-ordinated way.”
Primary care is the starting point for most of the health care people receive. It stands to reason, therefore, that we should involve family physicians and other primary care clinicians and scholars in making health care delivery more effective, efficient and equitable.
61 2023 Family Medicine Report – Relationships
In the Toronto region, the priorities of the OHSP include exploring care gaps in COVID recovery efforts; supporting patient attachment (the connection to a family physician or primary care provider); building a stable and responsive primary care workforce as the population increases; and engaging primary care leaders across the region, connecting them to one another so that they can work together on shared issues across the city.
The OHSP will also conduct evidence reviews to provide relevant information in a timely manner to health system decision makers and build capacity globally to support primary health care implementation through the work of the WHO Collaborating Centre on Family Medicine and Primary Care at DFCM. “Through the centre, we will assist the WHO in researching, evaluating and strengthening family medicine and primary care globally. The designation speaks to our reputation as a valued collaborator and an international leader in family medicine and primary care education and research,” says Dr. Katherine Rouleau, who is the centre’s Director, and the Global Primary Health Care Lead within the OHSP.
Primary care is a serious concern in Ontario. More than 2.2 million Ontarians are without a family doctor, according to a report released by Inspire-PHC, a health care research and policy group that is co-led by DFCM Professor Rick Glazier.
“We want to look at how we as a department can help alleviate this issue, learning from best practices internationally as well as across Canada,” says Dr. Avnish Mehta, who is the OHSP’s Attachment Lead. “The initial step has involved a review of international jurisdictions with high attachment rates, as well as local work interviewing key leaders across Ontario who have tried innovative approaches. We feel confident that we can learn from the very best.”
Dr. Mehta, who is also chief of family medicine at Scarborough Health Network, says family physicians in his neighbourhood are working at capacity, so the solution isn’t simply to assign more patients to each doctor.
“One key is to find a variety of ways to expand their capacity, such as interdisciplinary teams,” says Dr. Rouleau. “Through our global networks we can explore the macro-, meso-, and micro-level approaches to expanding capacity, such as the contributions that community health workers can make in primary care.”
Engaging busy family doctors in system work isn’t easy when they are all working at capacity. Dr. Yu has put together a leadership table of the primary care leads for each of the eight Ontario Health Teams (OHTs) based in Toronto to explore approaches to making access to high-quality care more equitable in Canada’s largest city. Integration efforts at the OHT level are part of that journey. Building partnerships, not only among family physicians but with hospitals, specialists, social service organizations and beyond, takes time and effort, but the team is eager to contribute.
“The implementation science behind breaking down siloes in health care is a growing field. In fact, many primary care champions among our own faculty members have been contributing to this body of knowledge for decades,” says Dr. Yu. “The OHSP seeks to gather and spread the learnings from existing models, so that integration across our health care system can be scaled quickly.”
“The most important changes we can make to the health care system aren’t complicated, but they do require an investment in sustained structures and processes to enable change management of a large community of service providers,” says Dr. Noah Ivers, who is the OHSP’s Scientific
62 Department of Family & Community Medicine, University of Toronto
“We need to harness the power of data to drive evidence-based, patientcentred improvements in health care.”
Lead. Critical to these reforms is an inclusive and integrated data system. “We need to harness the power of data to drive evidence-based, patient-centred improvements in health care,” he adds.
Both Drs. Mehta and Yu can point to successful examples from their own experiences that might someday become templates for networks of family care practitioners.
At the Scarborough Health Network, there is a cancer screening pilot project that allows patients to call in, speak to a physician and get signed up for ongoing screening. It is based on the VaxFacts program rolled out by the Network during the COVID-19 pandemic that allowed people to call in for a one-on-one, judgment-free consultation with a physician to get the most accurate information about vaccines and treatments for diseases like Monkeypox and COVID-19, childhood vaccines, flu vaccines, and preventative health counselling.
415,870
Number of people in Toronto without a family doctor
“The percentage of vaccine-hesitant people who went on to get vaccinated was very high,” says Dr. Mehta.
Meanwhile, Dr. Yu puts forth the work of the East Toronto Family Practice Network during the pandemic as an example of a successful way of organizing primary care providers and physicians to partner with an OHT to advance integrated care and population health. During the pandemic, Michael Garron Hospital, Family Health Teams, Community Health Centers and the East Toronto Primary Care Network and other health care and social service providers collaborated to ensure that vaccines were available throughout the catchment area in an equitable fashion that required co-ordination and outreach.
“We’re all part of the solution,” Dr. Yu says. “We’re gathering what works and hoping to produce generalizable knowledge to share and support locally fit solutions for our health care system.”
1,200
Average number of patients a family doctor takes on
As of 2022, compared to those in the highest income group, a higher proportion of residents in the lowest income group are without a family doctor (14.9% in the lowest income group, compared with 11.7% in the highest income group).
Source: INSPIRE Primary Health Care 2023 data
63 2023 Family Medicine Report – Relationships
Meet the OHSP Team








 Dr. Danielle Martin Professor and Chair, DFCM
Dr. Tara Kiran Vice-Chair, Quality and Innovation, DFCM
Dr. Catherine Yu Engagement Lead
Dr. Katherine Rouleau Global Primary Health Care Lead
Dr. Avnish Mehta Attachment Lead
Dr. Raj Girdhari Digital Health Lead
Dr. Noah Ivers Scientific Lead
Dr. Ryan Banach Family Medicine Health Human Resources Lead
Dr. Danielle Martin Professor and Chair, DFCM
Dr. Tara Kiran Vice-Chair, Quality and Innovation, DFCM
Dr. Catherine Yu Engagement Lead
Dr. Katherine Rouleau Global Primary Health Care Lead
Dr. Avnish Mehta Attachment Lead
Dr. Raj Girdhari Digital Health Lead
Dr. Noah Ivers Scientific Lead
Dr. Ryan Banach Family Medicine Health Human Resources Lead
64 Department of Family & Community Medicine, University of Toronto
Dr. Karen Weyman Education Lead
2,072 FACULTY MEMBERS
PLACES
15 CORE TEACHING SITES
1,000+ LEARNERS AT ALL LEVELS
40+ TEACHING PRACTICES, FROM RURAL TO URBAN CENTRES
4 INTEGRATED COMMUNITY STREAMS
DFCM in NUMBERS
10
83
CONTINUING EDUCATION STUDENTS 374 FAMILY MEDICINE RESIDENTS
GRADUATE STUDENTS 40+ STAFF PEOPLE
500 University Avenue, 5th Floor Toronto, Ontario M5G 1V7 t. 416-946-5938 f. 416-978-3912 e. dfcm.communications@utoronto.ca dfcm.utoronto.ca































 By Elaine Smith
By Elaine Smith




 By Alicia Fung
By Alicia Fung


 By Alicia Fung
By Alicia Fung



 Left to right: Dr. Jennifer Rayner
Dr. Gary Bloch
Left to right: Dr. Jennifer Rayner
Dr. Gary Bloch


 By Alicia Fung
By Alicia Fung




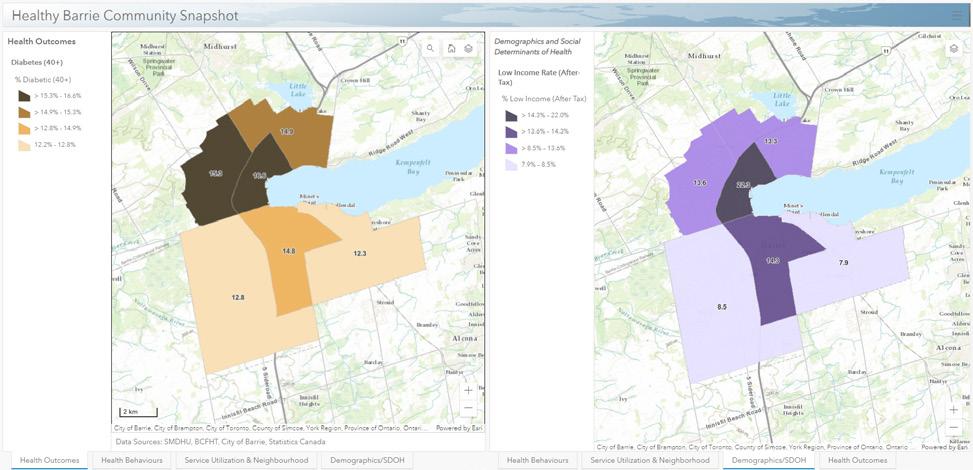












 Dr. Danielle Martin Professor and Chair, DFCM
Dr. Tara Kiran Vice-Chair, Quality and Innovation, DFCM
Dr. Catherine Yu Engagement Lead
Dr. Katherine Rouleau Global Primary Health Care Lead
Dr. Avnish Mehta Attachment Lead
Dr. Raj Girdhari Digital Health Lead
Dr. Noah Ivers Scientific Lead
Dr. Ryan Banach Family Medicine Health Human Resources Lead
Dr. Danielle Martin Professor and Chair, DFCM
Dr. Tara Kiran Vice-Chair, Quality and Innovation, DFCM
Dr. Catherine Yu Engagement Lead
Dr. Katherine Rouleau Global Primary Health Care Lead
Dr. Avnish Mehta Attachment Lead
Dr. Raj Girdhari Digital Health Lead
Dr. Noah Ivers Scientific Lead
Dr. Ryan Banach Family Medicine Health Human Resources Lead
















