










I feel like I’ve blinked and we’re now almost halfway through the year. I’m completely mind blown at the thought that I’m writing this for the May/June issue!
I feel that so much has already happened this year, which is both exhausting and exhilarating at the same time. While we have been go-go-going all the time, has it really been five months already? When I checked with a few friends, it seems that many have been feeling the same way and are really in need of some downtime.
Now I have some good news and some not so good news. I’m a “not so good” news first kind of person (always end on a high note, right?) so I’ll start with that. Our AHIMA members have noticed that we do not have any new CEU packages for them past Package 98. We had received notification that our CEU packages would not be able to be CEU certified and we had been under the impression that we would be able to meet their requirements once they finished their guidelines review, but we learned this week that we were incorrect. There will be no new CEU packages for our AHIMA members moving forward. Please know that all webinars will be CEU approved for our AHIMA members; it is only our CEU packages that are affected. We apologize for this and are actively reviewing how we can help our AHIMA

subscribers meet their CEU needs.
Onto the good news – We are unveiling a new website shortly! We have streamlined and tweaked things throughout, removed others, and have a great new look. Watch this space for more information!

Finally, onto this issue. We have another great issue for y’all with so much to write about that I’m just going to let you go and explore, read, and do! Enjoy!
Until next time.
Subscriptions:
ceo - publisher Storm Kulhan storm@billing-coding.com




Renewals: Keep your rate locked in for life! www.billing-coding.com/renewals
Change of address: Email - subscriptions@billing-coding.com or call 864 228 7310



Latique T. Auguster, CPC, CPMA, CEMC, CRC, is a physician’s documentation trainer and auditor at UCLA Health System. She has worked in the healthcare industry for 19 years and has been an AAPC certified coder for 11 years.
Sandy Coffta, Vice President of Client Services, oversees the team responsible for achieving and maintaining the company’s consistently high retention and referral rates. Ms. Coffta has over 17 years of experience in client relationship management, including reimbursement analysis, workflow optimization, and compliance education. She specializes in business intelligence and reporting development, is a subject matter expert in radiology practice billing, and has deep expertise in resolving payer disputes and contract issues.www.hapusa.com
Ebony D. Foster, MBA, CPC, CPMA, is the Coding Director with UCLA Physician’s Billing Office. She has over 25 years of combined experience in billing, coding, management, and healthcare operations consulting.
Betty Hovey, CCS-P, CDIP, CPC, COC, CPMA, CPCD, CPB, CPC-I, is the Senior Consultant/Owner of Compliant Health Care Solutions, a medical consulting firm that provides compliant solutions to issues for all types of healthcare entities. Chcs.consulting
Glenn Krauss, BBA, RHIA, CCS, CCS-P, CPUR, FCS, PCS, CCDS, C-CDI, C-DAM, is CEO and Founder of Core-CDI.com, and CDI Manager at University Medical Center Las Vegas. www.core-cdi.com
Sonal Patel, BA, CPMA, CPC, CMC, ICDCM, is CEO and Principal Strategist at SP Collaborative, LLC.
Sheri Poe Bernard, CPC, CRC, CDEO, CCS-P, is Director of Risk Adjustment Assessment and Compliance at Granite GRC Consulting granitegrcconsulting.com She is the author of the American Medical Association’s book, Risk Adjustment Documentation & Coding, in its second edition. Sheri has worked in healthcare coding education and training for 30 years, specializing in risk adjustment for the past 12 years. She can be reached at SPB@granitegrcconsulting.com.
Rachel V. Rose, JD, MBA, is an Attorney at Law, in Houston, TX. Rachel advises clients on healthcare, cybersecurity, securities law, and qui tam matters. She also teaches bioethics at Baylor College of Medicine. She has been consecutively named by Houstonia Magazine as a Top Lawyer (Healthcare) and to the National Women Trial Lawyer’s Top 25. She can be reached at rvrose@rvrose.com. www. rvrose.com
Matt Tamez, CPCO, CPB, is the Chief Operating Officer at Phoenix Coding & Consulting Services, a Texas-based coding company that works with many FECs across Texas. www.phoenixccs.com
Natalie Tornese, CPC, Natalie is a Senior Group Manager responsible for Practice and Revenue Cycle Management at MOS. She brings 25 years of healthcare management experience to the company. Natalie has worked in varied leadership roles with practices and specialties. Her primary focus is revenue cycle management with an emphasis on Medical Billing, Coding and Insurance Verification Management. She has written numerous articles on all aspects of Practice Management and presently manages a large team focused on Medical Billing, Medical Coding, Verification, and Authorization services for MOS. For more information on how MOS can help your practice, contact 1-800-670-2809 or visit (www.outsourcestrategies.com).
Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT, is a medical coding, billing, and auditing consultant, author, and educator with more than 30 years of clinical and administrative experience in healthcare, coding, billing, and auditing. Medicine, including coding and billing, is a constantly changing field full of challenges and learning and she loves both.
Cameron Wood is the Head of Client Services & Chief Operating Officer at NGA Healthcare. NGA Healthcare specializes in negotiating reimbursement rates for providers of all specialties all over the country. They also offer ongoing credentialing services and ensure that groups receive fair market rates and guarantee their fees. www.ngahealthcare.com
PAHCOM supports our active duty and veteran brothers and sisters. - https://my.pahcom.com/military

Firmly grounded in military culture, PAHCOM was conceived through a Naval Postgraduate School master’s thesis, entitled, “Administrative Management of Small Group Physician Practices.” More than 30 years later, we remain the industry’s leading collaborative network and offer the most advanced and nationally accredited medical management credential: the Certified Medical Manager (CMM). See https:// my.pahcom.com/cmm
The CMM credential is approved for DOD COOL funding, meaning CMM is approved for all services:
• Army
• Navy
• Air Force
• Coast Guard
• Marine Corps
• DOD Civilian https://www.cool.osd.mil/
The CMM Exam is Approved for Reimbursement Through the Post-9/11 GI Bill
The Certified Medical Manager exam is approved under Chapter 36 for the purposes of that chapter and Chapters 30, 32, and 35 of the Title 38, U.S.C., and Chapter 1606 of Title 10, U.S.C.
Visit: https://inquiry.vba.va.gov/weamspub/buildSearchCountryLCCriteria.do and then paste “Certified Medical Manager” into the L&C Name field. Select “Certification” for category type. Then Submit.
A proposal that would require healthcare vendors to supply patients with an itemized bill of services provided has a large bipartisan backing but is opposed by the Texas Hospital Association. House Bill (HB) 1973 by Rep. Caroline Harris (R-Round Rock)
would establish in code a requirement that hospitals, physicians, and other healthcare providers seeking payment for services provided supply an itemized list of charges. For each service, that bill must include the full-payment price, a “plain language description,” and the details associated with partial or full reimbursement from the involved insurance company.
Patients would be statutorily entitled to this itemized bill and it may be provided electronically, including through an online patient portal.
HB 1973 also reads, “A healthcare provider may not pursue debt collection against a patient for a provided healthcare service or supply unless the provider has complied with this section.”
Violation of these provisions would be punishable by penalty from the licensing authority overseeing the provider in question.
Source: https://thetexan.news/
A registered nurse and nurse practitioner, who defrauded commercial health insurers and Medicare of nearly $12 million by devising and executing fraudulent billing schemes in three states seeking payment for patient services that were never performed, has been sentenced to seven years in federal prison, announced United States Attorney Zachary A. Cunha.
Alexander A. Istomin, 57, pleaded guilty in October 2022 to an eleven-count Information charging him with healthcare fraud, mail fraud, aggravated identity theft, and causing the introduction of misbranded drugs into interstate commerce. Istomin admitted that he routinely submitted fraudulent claims for in-person patient services that he did not perform, including supposed patient visits at a “ghost office” in Rhode Island and at offices in Florida and New York. Istomin used seven different tax identification numbers while defrauding eight insurers out of a total of $11,923,686.30.
The “ghost office” was an address that Istomin maintained in East Greenwich, Rhode Island, that he claimed was part of his medical practice when, in fact, he used the location solely for the purpose of receiving mail, including fraudulently obtained insurance payments.
“By billing for services that he never performed, including at a Rhode Island location that was little more than a mail drop,
Alexander Istomin thought he could make off with millions in taxpayer and insurance dollars that were meant to fund real medical care, for real people, all without consequence,” remarked U.S. Attorney Zachary Cunha. “He was very much mistaken. The sentence imposed reflects both this Office’s commitment to bring to justice individuals who perpetrate this kind of brazen fraud and abuse of our healthcare system, and should serve notice of the consequences for those who seek to enrich themselves through schemes like these.”
Source: justice.gov
The FY2023 ICD-10-CM codes are to be used from April 1, 2023 through September 30, 2023.
Note: This replaces the FY 2023 – October 1, release. These files listed below represent the ICD-10-CM FY2023 April 1, 2023 release. The April 1, 2023 FY2023 ICD-10-CM is available in both PDF (Adobe) and XML file formats. Most files are provided in compressed zip format for ease in downloading. These files have been created by the National Center for Health Statistics (NCHS), under authorization by the World Health Organization. Any questions regarding typographical or other errors noted on this release may be reported to nchsicd10cm@ cdc.gov.
https://www.cdc.gov/nchs/icd/Comprehensive-Listing-of-ICD-10CM-Files.htm
The study found that California FQHCs were still conducting 20% of primary care visits and 40% of behavioral care visits by telephone or audio-only computer platform.
• Audio-only telehealth platforms, such as the phone, were largely prohibited prior to the pandemic because they didn’t meet the standards of the healthcare visit, but state and federal regulators relaxed those rules during the pandemic to boost access to care.
• Telehealth use soared during the pandemic as patients and providers sought to replace in-person services with
virtual care, and many healthcare organizations found value in audio-only telehealth platforms in reaching those facing barriers to care.
• Telehealth advocates say audio-only access should be preserved to help underserved populations access needed care services.
Source: healthleadersmedia
• CMS is proposing a 2.8% pay increase for hospitals in 2024, which would result in $3.3 billion in additional funding that year. Hospitals say it’s not enough.
• The Biden administration released its annual Medicare payment rule for inpatient hospitals and long-term care facilities, which also includes a 2.9% bump for long-term care hospitals.
• Hospital lobbies including, the American Hospital Association and Federation of American Hospitals slammed the rule as insufficient to help hospitals address inflation and rising labor costs, though research signals hospitals are more financially stable than such groups suggest.
Source: healthcaredive
A bill proposed in Louisiana would repeal the state provision that an employer and their workers compensation insurer are not required to pay for medical marijuana for injured workers.
H.B. 351, introduced recently and sent to committee, would set parameters for workers who receive recommendations to use medical marijuana, for treatment.
The bill mostly addresses that a worker would not be barred from benefits such as unemployment if they use medical marijuana yet includes language that would call on comp insurers to cover the drug for a “qualifying medical marijuana patient,” which is described as “an individual who has been clinically diagnosed as suffering from a debilitating medical condition and an authorized clinician has recommended marijuana for therapeutic use.”
Source: businessinsurance
CMS (Centers for Medicare and Medicaid) is always implementing various programs and initiatives aimed at reducing fraud, waste, and abuse. One such initiative is Comparative Billing Reports (CBRs). In this article, an overview of CBRs, their purpose, and how they can benefit coding professionals, auditors, and practice managers will be discussed.

CBRs are educational reports produced by CMS that provide feedback to physicians and other providers regarding their billing practices. These reports compare a physician’s and other healthcare provider’s billing practices to those of their peers on specialty-specific, local, and national levels, and highlight any variations or anomalies that may indicate potential fraud, waste, or abuse. CBRs are produced for a variety of healthcare services and specialties, including durable medical equipment (DME), home health, hospice, and Part B physician services.
The purpose of CBRs is to offer physicians/other providers information that they can use to improve their billing practices and ensure that they are in compliance with CMS bill-
ing guidelines. The reports can also help identify potential areas of fraud or abuse and allow the physicians/other providers to take corrective action before any issues arise. So, it’s like a “Heads up; you’re an outlier” letter.
The introduction to the CBR states that it is “not an indication of wrongdoing, and can support internal compliance review efforts, especially those related to coding and billing of code sets. Receiving a CBR is not an indication of, or precursor to, an audit, and it requires no response on a provider’s part.” So, it is stating that just because the practice received this does not mean that a records request is coming next. But it goes on to state, “Select providers, however, may be referred for additional review and education as a part of CMS’ routine CBR Program.” So, it does not
mean that you won’t get a records request either. This is why it is important to review these and, if applicable to the practice, perform a small audit to see if there may be an issue that needs to be addressed.
CBRs are produced using data from the Medicare Administrative Contractors (MACs) and other CMS systems. The data is analyzed using statistical methods to identify providers who have billing patterns that are significantly different from their peers. The reports are then reviewed by CMS staff to make sure they are accurate and complete.
CBRs are usually produced on a monthly basis, and healthcare providers receive the reports via email or mail. The reports are confidential and are only available to the physician/other provider and their designated representatives. CBRs can be found on the CBR/PEPPER website: www.cbrpepper.org. PEPPER is the Program for Evaluating Payment Patterns Electronic Report, and it summarizes data statistics for Medicare Part A claims. There will be one CBR introduced for a particular month, and the report will match the year and month. For example, the February CBR for this year is labeled CBR 202302.
A CBR will contain the following components:
• A cover letter
• An introduction of the issue addressed in the CBR
• A coverage and documentation overview
• Metrics
• Methods and results
• References and resources
The cover letter will give general information on what the CBR is, along with links to the CBR PEPPER site, the CBR portal, webinar registration, and CBR Help Desk. The introduction will give specific information on the CBR analysis, supportive documentation, and the criteria for receiving the particular CBR.
For example, CBR 202301 (on chiropractic manipulative treatment [CMT] of the spine) lists criteria to receive the CBR, stating that a provider:
1. Is significantly higher compared to either state or national average or percentage in any of the three metric calculations (i.e., greater than or equal to the 90th percentile); and
2. Has at least 60 beneficiaries with paid claims submitted for
CMT of the spine; and
3. Has at least $20,000 in total charges for CMT of the spine. (Source: cbrpepper.org: CBR202301 Mock Provider Data Sample Report: 1234567890CBR202301-508)
The coverage and documentation overview section identifies the CPT/HCPCS II codes used in the CBR analysis and a summary of the receiving physician/other provider’s utilization (including allowed charges) of the codes. The metrics section lists the specific metrics used in the CBR. It will list how the CBR defined the peer group and the possible outcomes for the comparisons between the recipient and his/her peers.
There are four possible outcomes for the comparisons:
1. Significantly Higher - Provider’s value is greater than or equal to the 90th percentile from the state or national mean.
2. Higher - Provider’s value is greater than the state or national mean.
3. Does Not Exceed - Provider’s value is less than or equal to the state or national mean.
4. Not Applicable (N/A) - Provider does not have sufficient data for comparison.
The methods and results section is where the data, charts, and graphs are located. The charts and graphs can be useful for identifying trends or patterns that may not be immediately apparent when looking at raw data. It also lists information on the provider’s peers, such as the average number of claims submitted, and the average amount billed. It first states how many providers nationwide submitted claims related to the CBR and claim totals during the analysis period. It also lists the specific metrics out for each CBR. This is where the CBR will list the recipient’s outcomes (higher, significantly higher, etc.).
CBRs can provide valuable information to coding professionals, auditors, and practice managers, as they can use the reports to identify potential issues and make improvements to their billing practices. Here are specific ways that CBRs can benefit the professionals listed above.
CBRs can help coding professionals identify potential errors or
discrepancies in billing practices. For example, if a physician is consistently billing for a higher number of services than their peers, this could be an indication that there is an issue with coding or documentation. By reviewing the CBR, coding professionals can work with their physicians/other providers to identify the root cause of the issue and take corrective action, if needed.
CBRs can be a valuable tool for auditors, as they can use the reports to identify potential areas of fraud or abuse. For example, if a physician is consistently billing for services that are significantly different from their peers, this could be an indication that there is an issue. By reviewing the CBR, auditors can perform a targeted internal audit of the areas listed in the CBR to evaluate if there are any issues and take appropriate action, when warranted.
CBRs can help practice managers identify potential issues with billing practices and take corrective action to improve compliance. A practice manager should review the CBRs every month to see if there are any current ones that may affect their specialty(ies) so they can take appropriate steps to check on them (internal audits, education, etc.).
If the practice receives a CBR for one of their physicians/other providers, the practice manager should take the following steps:
1. Evaluate the information on the issue in the CBR.
2. Evaluate the physician/other provider’s billing patterns related to the CBR subject.
3. Perform an audit and address any errors by providing education.
4. Monitor the issue to ensure that compliance is attained and continued.
It is important to note that being an outlier does not necessarily indicate a problem. There are several factors that could contribute to higher usage of certain services in a specific geographic location or with a certain patient base. For instance, a surgeon may be the sole provider of a particular procedure in the area, and patients come from all over to receive it. It’s important not to jump to conclusions and panic. If an internal audit confirms proper documentation and coding of the services highlighted in the CBR, then there is no cause for concern. Just remember that continued reporting of the service in the same manner may

trigger an audit. But if the practice has already performed an internal check with a good outcome, there should not be a problem. There are always going to be outliers, and some with valid reasons.
The CBR PEPPER website offers valuable information alongside each listed CBR. Sample CBRs with fabricated provider data are included to aid in cases where none of the physicians/other providers in the practice have received a CBR, but the practice performs the services that are relevant to the CBR. Live training sessions are available for each CBR, and their corresponding recording and handouts are also provided. Additionally, an Excel spreadsheet containing state and national data on the CBR topic is listed for each CBR. In the cannot be found, each CBR access.
By analyzing the data in a CBR, identify potential billing errors or under coding. This information ments to their billing practices, increased efficiency, reduced patient care. Additionally, CBRs their billing practices against nities for further education powerful tool for providers tices and enhance the quality

Betty A. Hovey, BSHAM, CCS-P,
Betty is a nationally recognized er. She is an expert auditor pliant and profitable. Betty practices and they should be
Betty brings over thirty years has worked for practices both intensity and attention. She has spent years on the “front lines” for practices handling medical billing, coding, claims, and denials. She has also managed practices and directed healthcare system departments. Her areas of expertise include Evaluation and Management, Primary Care, Dermatology, Plastic Surgery, Cardiology, Cardiothoracic Surgery, General Surgery, GI, E/M and procedural auditing, and ICD-10-CM.
https://chcs.consulting/

In 2021, the office/other outpatient codes and guidelines went through revisions. For 2023, the rest of the E/M sections underwent a major overhaul. We cover all sections revised with comprehension checks to ensure attendees will be able to:


• Apply the 2023 E/M definitions and guidelines in CPT to the medical record.






• Utilize the revised 2023 Medical Decision Making (MDM) Table in CPT to review E/M services.
• Demonstrate to physicians and other providers proper documentation that supports the level of services reported.






































CHCS provides many types of audits for CPT and/or diagnosis.






































• Physician/provider education on multiple specialties.

























• CPT, ICD-10-CM, E/M, and specialty specific education solutions.






Education can be customized for your practice, department, or group. Services can be performed on-site, or virtually through our eLearning platform.







Betty A. Hovey is a seasoned healthcare professional with over three decades of experience in the field. She has extensive experience conducting audits for medical practices and payors. She specializes in educating various groups including coding professionals, auditors, doctors, APPs, payors, and others on coding, billing and related topics. Betty is a highly sought-after speaker and has co-authored manuals on ICD-10-CM, ICD-10-PCS, E/M, and various CPT specialty areas.

Did you report all of your time?
Prolonged preventive services are provided in outpatient settings and can be provided via telehealth. Annual wellness visits and the Welcome to Medicare visit include a thorough review of the patient’s health and medical history. The physician performs an exam that consists of a blood pressure check, height and weight assessment, and a vision screen. Depending on the medical history information provided by the patient and the results of the physical examination, the physician orders or performs additional tests as medically necessary. The physician also provides preventive medicine education and counseling services based on the patient’s medical history and examination results, in addition to a written plan of care to the patient, detailing any follow-up
screening or preventive services that the patient should receive. Let’s be frank: To provide all required elements of the Medicare preventative visits, you will spend a lot of time with the patient. Most providers are not aware that there is an opportunity for additional reimbursement when that time qualifies as a prolonged amount of time.
Medicare accepts HCPCS codes G0513 and G0514 (RVU 1.17) as an addition to preventive medicine services. These codes are time based and can be billed with preventive services, such as the Initial Preventive Physical Exam (IPPE) visit, initial and subsequent annual wellness visits, and other covered preventive services effective January 1st, 2018.

The Patient Protection and Affordable Care Act (PPACA) enacted May 2010 by the House of Representatives states that health plans must provide patients with comprehensive preventive care services at no cost. Offering preventive care lowers the overall healthcare cost by preventing diseases from developing rather than taking on the higher cost associated with treating disease after diagnosis, according to SEC. 2713 [42 U.S.C. 300gg–13].
Chronic diseases account for 75 percent of the nation’s healthcare spending and lowered economic output in the U.S. by $260 billion a year that were avoidable through preventive care, according to the CDC. And if everyone in the United States received the recommended preventive services, the healthcare system could save over 100,000 lives a year.
Physicians and other healthcare providers may shy away from offering Annual Wellness Visits to their Medicare patients for numerous reasons. For example, preventive services can sometimes be complex and time consuming to document due to the extensive AWV elements and requirements. Heath Risk assessments must be provided, patients must receive a written 5-10 year scheduled screening plan, not to mention staffing shortages; this can all be challenging and make providing the AWV not profitable. Codes G0513 and G0514 allow providers to increase reimbursement associated with these services when an extensive amount of time is spent on the visit.
The time reported for the prolonged preventive service must be beyond the typical service duration time of the primary procedure:
• G0513 - Prolonged preventive service(s) (beyond the typical service of the primary procedure) in the office or other outpatient setting requiring direct patient contact beyond the usual service; first 30 minutes
• G0514 - Prolonged preventive service(s) (beyond the typical service of the primary procedure) in the office or other outpatient setting requiring direct patient contact beyond the usual service; each additional 30 minutes
Medicare preventive services are not reported based on time but rather based on the required documentation and service elements such as depression screening, advance directives, activities of daily living, and provision of immunization schedules. The following intra-service time guidelines are provided to help physicians report prolonged service codes when appropriate.
See Table 1
Note: Provider documentation must include the total time spent on the visit to support the addition of the prolonged service code.
Example: A 66-year-old female patient is being seen for an initial Annual Wellness Visit. The patient’s son explained to the physician that the patient has an extensive repeat fall history and would like to talk about prevention options. The physician recommended some DME options in the home, railing attachments in the bathtub/shower, and a walker to sit and stand. Counseling, coordinating care for the DME, and the initial visit together total a time of 65 minutes. Vignette supports billing G0438 and G0513.
Prolonged Services in 2023
Effective January 1st, 2023, the AMA (American Medical
Association) and CMS (Centers for Medicare & Medicaid Services) have created new prolonged services for inpatient Evaluation and Management (E/M) services to follow the current guidelines of billing by total time. We now have several prolonged service codes to choose from dependent on the setting the services are provided in. It is necessary that providers are aware of the appropriate time threshold and appropriate code to report.
Keep in mind code requirements:
• CPT codes 99417 and 99418 - for each 15 minutes of total time beyond the minimum required time; see Table 2.
• Medicare requirements for HCPCS codes G2212, G0316, G0317, and G0318 - each additional full 15-minute increments after the maximum time the base code is reached; see Table 3.
These codes replace the outpatient CPT codes 99354
and 99355 and inpatient CPT Codes 99356 and 99357. In 2023, Medicare and other commercial payors are ceasing coverage of non-face-to-face prolonged service codes 99358 and 99359.
See Table 2
See Table 3
Latique T. Auguster, CPC, CPMA, CEMC, CRC, is a physician’s documentation trainer and auditor at UCLA Health System. She has worked in the healthcare industry for 19 years and has been an AAPC certified coder for 11 years.
Ebony D. Foster, MBA, CPC, CPMA, is the Coding Director with UCLA Physician’s Billing Office. She has over 25 years of combined experience in billing, coding, management, and healthcare operations consulting.
99417 Prolonged office or other outpatient evaluation and management service(s) beyond the minimum required time of the primary procedure which has been selected using total time, requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service, each 15 minutes of total time
99418 Prolonged inpatient or observation evaluation and management service(s) time with or without direct patient contact beyond the required time of the primary service when the primary service level has been selected using total time, each 15 minutes of total time
HCPCS Code Description
G2212 Prolonged office or other outpatient evaluation and management service(s) beyond the maximum required time of the primary procedure which has been selected using total time on the date of the primary service; each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact
G0316 Prolonged hospital inpatient or observation care evaluation and management service(s) beyond the total time for the primary service (when the primary service has been selected using time on the date of the primary service); each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact
G0317 Prolonged nursing facility evaluation and management service(s) beyond the total time for the primary service (when the primary service has been selected using time on the date of the primary service); each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact
G0318 Prolonged home or residence evaluation and management service(s) beyond the total time for the primary service (when the primary service has been selected using time on the date of the primary service); each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact
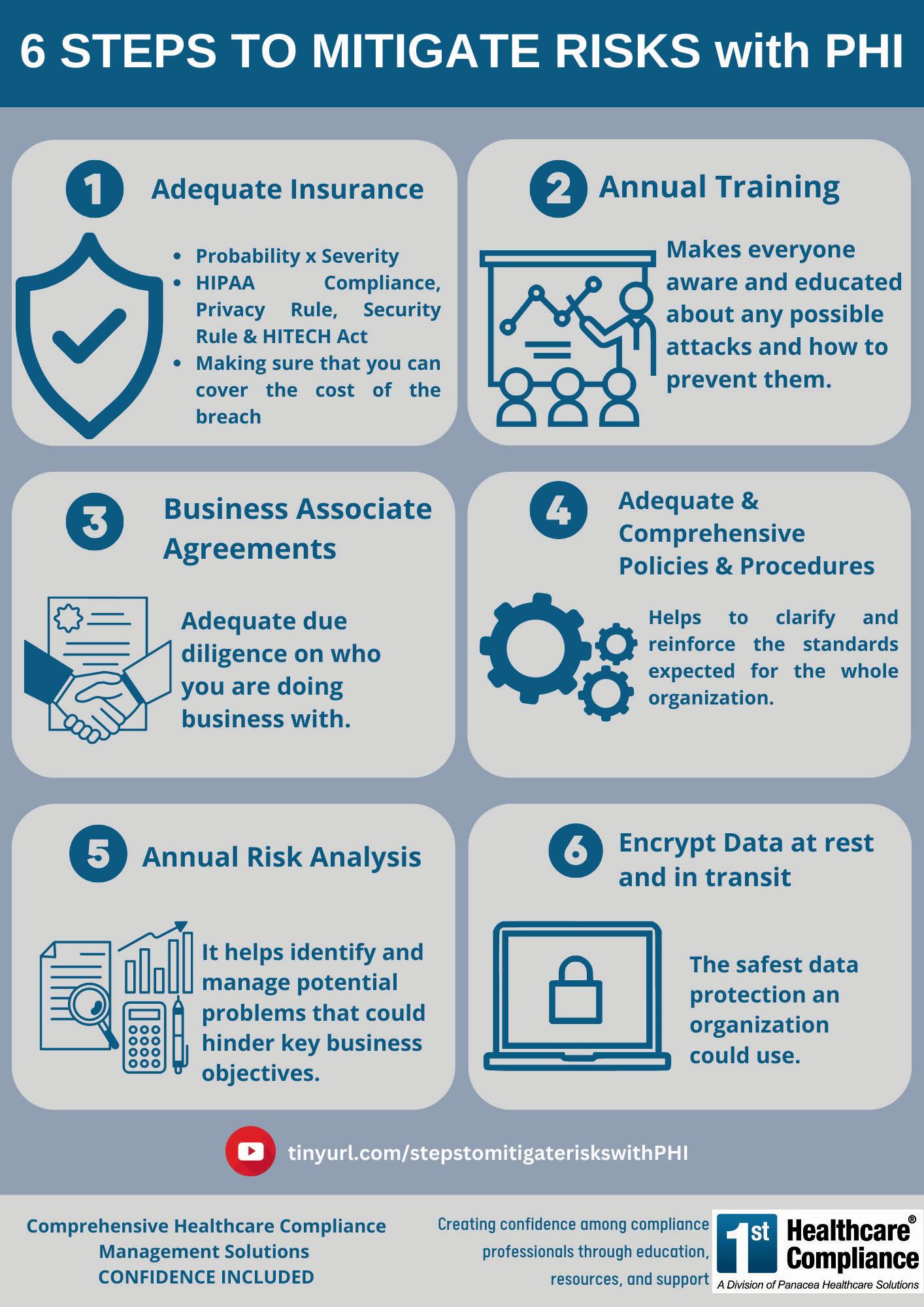
Expert presenter, Rachel V. Rose, JD, MBA, principal with Rachel V. Rose –Attorney at Law, P.L.L.C., Houston, TX, guides us during this important and informative webinar. Breaches and the lack of the requisite technical, administrative, and physical safeguards can have criminal consequences. While most people are familiar with civil cases, there is the potential for HIPAA violations and ransomware attacks to be prosecuted criminally.
Expert attorneys Sean McKenna, Lauren Nelson, and Vincent Aiello of Spencer Fane LLP will discuss the interplay between enforcement and liability proceedings with asset protection, explore how government and private litigation matters can impact healthcare companies, clinicians, and executives, and provide

In September of 2022, the Office of Inspector General (OIG) released a report, “Medicare Telehealth Services During the First Year of the Pandemic: Program Integrity Risks,” in which they identified that approximately two in five Medicare beneficiaries used telehealth services within the first year of the pandemic to receive healthcare services from a Medicare provider. This is approximately 88 times more often than beneficiaries engaged through telehealth services prior to the pandemic.
To meet the demand for telehealth services by Medicare beneficiaries throughout the pandemic, many major changes to the rules governing for who, when, how, and where beneficiaries could receive telehealth services were changed dramatically. Even allowing for telehealth services to be received in the patient’s own home, likely one of the biggest benefits to Medicare beneficiaries. Because of these many changes, and the massive
increase in the use of telehealth services, it became vital to safeguard Medicare from potential fraud, waste, and abuse (FWA) related to these services through a series of data analyses and audits.

The U.S. Department of Health and Human Services (DHHS), with the input from OIG investigators and Medicare data, developed a set of seven measures they used in their
review to root out and identify Medicare provider behavior that indicates poten tial FWA.
The seven measures are as follows:
1. Billing for both a telehealth service and a facility fee for the majority of visits
DHHS calculated the percentage of visits that included both an originating site facility fee and a telehealth service and discovered that it was billed this way for more than 75% of the providers’ visits.
2. Billing telehealth services at the highest, most expensive level, every time
Most providers rarely, if ever, bill at the highest level of service, but these providers always billed the highest level of service in the office, nursing home, assisted living, and home settings.
3. Billing telehealth services for a high number of days

By reviewing claims over a one-year period, DHHS noted that these providers regularly billed more than 300 days of telehealth services when the median is just 26 days of the year.

4. Billing both Medicare fee-for-service (FFS) and a Medicare Advantage (MA) plan for the same service for a high proportion of services
Most providers never bill both Medicare FFS and MA plans for the same service; however, these providers billed more than 20% of their services this way.
5. Billing a high average number of hours of telehealth services per visit
The average length of a telehealth visit is just 21 minutes; however, these providers consistently billed for a two-hour visit, on average.
6. Billing telehealth services for a high number of beneficiaries
The median number of beneficiaries for which a single provider bills telehealth services in a single year is 21. These providers, on average, billed for telehealth services for 2,000 or more beneficiaries in a single year.
7. Billing for a telehealth service and ordering medical equipment for many of their beneficiaries
Occasionally, providers may recommend certain durable medical equipment, compounded medications, or other supplies during a telehealth or in-person visit. However, these providers ordered these additional services, supplies, and/or equipment for more than half of the Medicare beneficiaries they served via telehealth.
This review of Medicare providers who performed telehealth services on Medicare beneficiaries revealed that out of the identified 742,000 providers
who billed telehealth services during the timeframe of March 1, 2020, through February 28, 2021, a total of 1,714 providers demonstrated what the OIG considers to be “concerning billing on at least 1 of 7 measures.”
While the seven measures are not related to a solid claim of fraud, waste, or abusive billing habits, they make a good starting point for additional investigations to occur into these questionable billing practices. Interestingly, further scrutiny of the 1,714 providers revealed that more than half of them were actually part of a medical practice where at least one other Medicare provider already showed questionable billing practices, which posed a threat to Medicare. Additionally, based on the application of these seven measures to these 1,714 providers, it was noted that many of them may even be associated with telehealth companies, which from past Department of Justice (DOJ) investigations have been noted to act fraudulently.
As there is no systematic way to identify providers who are associated with telehealth companies within the current Medicare data, this appears to be something that needs to be evaluated and rectified.
The OIG recommends two options:
• Adding a taxonomy code that identifies telehealth companies on claims
• Updating the Medicare provider enrollment application to require telehealth companies to identify themselves when they enroll in Medicare
It is estimated that these simple changes may then allow CMS to identify beneficiaries who receive telehealth services from providers who are associated with telehealth companies, and ensure beneficiaries are not being taken advantage of or being put at risk by receiving care outside of their regular providers, which may be incomplete or lacking in quality.
While this is just a quick review of some of the issues
identified with telehealth service reviews, additional issues have been noted or identified as problematic for regulating and ensuring proper use of funding for Medicare beneficiaries, such as valid incident-to services and verification of when clinical staff vs physicians/nonphysician providers are performing telehealth services. In fact, the OIG has recommended to CMS that they consider the additional requirement of adding a modifier to a claim where incident-to services were performed.
We recommend setting internal policies for performing, documenting, and coding all telehealth services to remain compliant with the payer contracts your organization honors. Carefully review the new Evaluation and Management (E/M) service changes for 2021 and 2023 to ensure the documentation supports the correct level of service reported, and all telehealth service requirements have been met. Do not engage or contract with questionable telehealth companies and definitely avoid prescribing additional services that are “recommended” by the telehealth company. Make sure to question the patient before signing off on a telehealth service to ensure they were not promised certain DME or supplies by a telehealth customer service agent prior to an encounter. Vetting the companies you work with to ensure your patients are receiving quality care is important when it comes to protecting your organization from accusations of fraud, or even the appearance of it.
Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT, is a medical coding, billing, and auditing consultant, author, and educator with more than 30 years of clinical and administrative experience in healthcare, coding, billing, and auditing.
Medicine, including coding and billing, is a constantly changing field full of challenges and learning and she loves both. Aimee believes there are talented medical professionals who, with proper training and excellent information, can continue to practice the art of healing while feeling secure in their billing and reimbursement for such care.
www.findacode.com





Summary: Clean Air Month in May is a nationwide campaign to encourage people to preserve the environment and make the world a more sustainable, healthy planet.

Air pollution has evolved into a global threat that is impossible to evade. The World Health Organization (WHO) defines air pollution as the “contamination of the indoor or outdoor environment by any chemical, physical, or biological agent that modifies the natural characteristics of the atmosphere.” Ninety-nine percent of the global population breathes in polluted air daily, according to the World Economic Forum (WEF). The United States Environmental Protection Agency (USEPA) notes that the U.S. emitted a staggering 67 million tons of pollution into the air in 2021. As sustained exposure to unhealthy air is linked to chronic respiratory
diseases such as asthma, chronic obstructive pulmonary disease (COPD), and lung cancer, air pollution is called a silent killer.
With toxic contaminants being released into the air all the time, clean air has become a rare commodity. May is observed as Clean Air Month in the United States to encourage people to preserve our environment, and make the world a more sustainable, livable, and healthy planet for future generations. Taking proactive steps to fight air pollution outdoors, at home, in school, and at work is critical to prevent or reduce risk of various respiratory conditions, especially in children and older adults.

Air pollution is affecting human health and the planet in many ways and the future is at stake unless we act on it now.
Here are the key reasons why we should care about air pollution:
1. Air pollution has been identified as the fourth-largest threat to human health, after high blood pressure, dietary risks, and smoking (WEF).
2. Breathing polluted air increases the risk of many health conditions such as respiratory infections, cardiovascular diseases, stroke, chronic lung disease, and lung cancer.
3. Every year, air pollution accounts for around 7 million premature deaths—a staggering 800 people every hour or 13 every minute, according to WHO.
4. 600,000 children die prematurely every year from polluted air.
5. The economic and health costs of air pollution due to fossil fuels cost the U.S. $2.9 trillion in 2018 (Center for Research on Energy and Clean Air).
The main source of air pollution is energy use and production. Fossil fuel burning, fumes from chem-
ical production, vehicle emissions, by-products of manufacturing and power generation, and natural gas to heat homes are common sources of air pollution.
Indoor air quality in homes is affected by factors such as excess moisture, building materials, furnishings, and products like air fresheners, malfunctioning appliances, smoking, cleaning, poor ventilation, etc. Factors that compromise indoor air quality in workplaces include improper or inadequately maintained heating and ventilation systems, contamination by construction materials, glues, fiberglass, particle boards, silica and wood dust, paints, vehicle spray paints, welding fumes, chemicals, etc. These elements release solid and liquid particles and certain gases that remain suspended in the air. Common air pollutants include carbon monoxide, lead, nitrogen oxides, ozone, particulate matter, and sulfur dioxide.
The effects of air pollution on human health will vary depending on the exposure type, (type of pollutant), and level and length of exposure. It will also depend on a person’s specific health risks and the combined impacts of multiple pollutants or stressors. For instance, people with breathing issues can experience a sudden onset of symptoms when exposed to higher pollution on busy roads and from factories, power plants, and waste incinerators.
Clean air is essential for healthy lungs. Most air pollutants cause the muscles in airways to contract, narrowing the airway (airway hyperreactivity). Asthma and COPD are two common chronic respiratory diseases caused by exposure to elevated levels of air pollution. These conditions can trigger cough, breathing difficulties, and other symptoms. Lung disease caused by breathing in polluted air increases the risk of heart and blood vessel disorders and lung cancer.
Neither asthma nor chronic obstructive pulmonary disease can be cured, but treatment can reduce symptoms, prevent deterioration of health, and improve quality of life.
Treatment for these air-pollution-related illnesses focuses on:
• Relieving the symptoms
• Improving breathing function
• Avoiding triggers
Millions of Americans have asthma, a chronic condition that often starts during childhood. This chronic condition causes inflammation and swelling in the lungs, which narrows the airways and restricts air supply. Severe cases of asthma can result in “airway remodeling,” which is permanent changes to the walls of the airways, which in turn, can result in scarring of the lungs (www.healthcentral.com).
The common symptoms of asthma are shortness of breath, chest tightness or pain, and wheezing and coughing attacks triggered by exposure to specific environmental factors. Causes of asthma include inherited genes, viral respiratory tract infections, chronic inflammation of the tissues in the sinuses, smoking tobacco, obesity, and occupational exposures.
Diagnosing asthma usually involves a physical exam, medical history, lung function tests including spirometry (pulmonary function testing), peak expiratory flow (PEF) tests, fractional exhaled nitric oxide (FeNO) tests, and allergy skin or blood tests.
• Inhaled medications – Inhalers work fast to open the airways, and long-term control medications taken daily help relieve symptoms and prevent narrowing of the airways.
• Immunotherapy – Administration of relevant allergens
improve the control of asthma, as well as other allergic diseases complicated by asthma.
• Bronchial thermoplasty – A bronchoscopic procedure for severe asthma involves delivering radiofrequency-generated thermal energy to open the airways.
• Supplemental oxygen and mechanical ventilation –Treatments given for life-threatening asthma.
Asthma treatment also includes strategies to avoid triggers that can aggravate the condition.
Though there is no way to prevent or cure asthma, the condition can be effectively controlled with inhaled medications so that people with asthma can lead a normal life.
Like asthma, COPD causes breathing problems and affects millions of Americans, especially older people. This common lung disease is a leading cause of serious long-term disability and death in the U.S.
COPD causes inflammation and thickening of the airways in the lungs, destroys the tissue where oxygen is exchanged, and reduces airflow into and from the lungs. The body tissues become deprived of oxygen and carbon dioxide is harder to remove.
The common symptoms of COPD are cough, sputum production, wheezing, and shortness of breath (dyspnea). Airway obstruction is less reversible in people with COPD than in those with asthma. As the disease progresses, shortness of breath makes it difficult to stay active.
The two main types of COPD are:
• Chronic bronchitis - a long-term cough with mucus
• Emphysema - damage to the lungs over time
Most people with COPD have both of these conditions.
While up to 85% to 90% of COPD cases are linked to cigarette smoking, long-term exposure to air pollution is a significant cause. Work-related COPD is the result of exposure to dust, fumes, and chemicals, and exposure to heavy amounts of secondhand smoke and pollution.
COPD is preventable and treatable. COPD-induced lung airway inflammation is less responsive to steroids.
Treatment options include:
• Bronchodilators – Based on the severity of the condition, short-acting and long-acting bronchodilators are prescribed to alleviate bronchial obstruction.
• Pulmonary rehabilitation – Includes using special breathing techniques, exercise training, education, support, and behavioral intervention.
• Oxygen therapy – Improves breathing through the delivery of extra oxygen to the lungs.
• Lung volume reduction surgery – Removal of small wedges of damaged lung tissue to allow the remaining tissue to function better.
• Bullectomy – Surgery to remove enlarged, damaged lung air sacs (bullae).
• Implantation of endobronchial valves – A minimally-invasive procedure to treat severe emphysema, where tiny valves are implanted in the airways to block off diseased parts of the lung and improve lung function.
• Lung transplantation – Replace a diseased lung with a healthy one from a donor.
As they treat patients with asthma and lung disease, pulmonary and allergy/immunology specialists need to stay up to date on how to bill and code diagnoses and treatments.
Here is a list of relevant CPT codes for respiratory disease treatments/procedures:
• 95115 - Professional services for allergen immunotherapy not including provision of allergenic extracts; single injection
• 95117 - Professional services for allergen immunotherapy not including provision of allergenic extracts; 2 or more injections
• 95165 - Professional services for the supervision of preparation and provision of antigens for allergen immunotherapy; single or multiple antigens (specify number of doses)
• 95199 - Unlisted allergy/clinical immunologic service or procedure
• 94010 - Spirometry complete, includes graphic record total and timed vital capacity, expiratory flow rate measurement(s) with or without maximal voluntary ventilation
• 94060 - Bronchodilation Responsiveness, spirometry as in 94010, pre- and post-bronchodilator or exercise
• 94070 - Bronchospasm Provocation Evaluation, multiple spirometric determinations as in 94010, with administered agents (e.g., antigen(s), cold air, methacholine)
• 94200 - Lung Function Test (MBC/MVV) - Maximum Voluntary Ventilation
• 94016 - Review Patient Spirometry, 30-day period of time; physician review and interpretation only
• 94375 - Respiratory Flow Volume Loop
• 95070 - Inhalation Bronchial Challenge Testing (not including necessary pulmonary function tests), with histamine, methacholine, or similar compounds
• 95071 - Inhalation Bronchial Challenge Testing (not including necessary pulmonary function tests), with specified antigens or gases
• 94640 - Airway inhalation treatment
• 94664 - Bronchodilator administration, demonstration and/ or evaluation of patient utilization of an aerosol generator, nebulizer, meter dose inhaler, or IPPB device
Lung Volume Determination
• 94013 - To measure lung volume through 2 yrs.
• 94726 - Plethysmography to measure lung volumes and capacities
• 94727 - Pulmonary function tests by gas
• 94728 - To measure airway resistance by oscillometry
Diffusion Capacity
CPT codes for diffusion capacity include 94729 (usually an addon code commonly used in conjunction with codes 94726 and 94010).
Pulse Oximetry
• 94760 - Noninvasive ear or pulse oximetry for oxygen saturation, single determination
• 94761 - Noninvasive ear or pulse oximetry for oxygen saturation; multiple determinations (e.g., during exercise)
Bronchial Thermoplasty
• 31660 - Bronchoscopy, rigid or flexible, including fluoroscopic guidance, when performed; with bronchial thermoplasty, 1 lobe
• 31661 - Bronchoscopy, rigid or flexible, including fluoroscopic guidance, when performed; with bronchial thermoplasty, 2
or more lobes
• 94625 - Physician or other qualified healthcare professional services for outpatient pulmonary rehabilitation; without continuous oximetry monitoring (per session)
• 94626 - Physician or other qualified healthcare professional services for outpatient pulmonary rehabilitation; with continuous oximetry monitoring (per session)
Codes 94625 and 94626 should not be reported in conjunction with 94760 and 94761 for noninvasive ear or pulse oximetry.
94002-94005 - Ventilation assist and management, initiation of pressure or volume preset ventilators for assisted or controlled breathing
32491 - Removal of lung, other than pneumonectomy; with resection-plication of emphysematous lung(s) (bullous or non-bullous) for lung volume reduction, sternal split or transthoracic approach, includes any pleural procedure, when performed
32853 - Lung transplant, double (bilateral sequential or en bloc); without cardiopulmonary bypass
Claims must also include the appropriate ICD-10 codes to capture the anatomic site, etiology, comorbidities and complications, and illness severity.
• J41.0 - Simple chronic
• J41.1 - Mucopurulent
• J41.2 - Mixed simple and mucopurulent bronchitis
• J42 - Unspecified chronic bronchitis
Emphysema
• J43.1 - Panlobular
• J43.2 - Centrilobular
• J43.8 - Other
• J43.9 - Unspecified
• J44.0 - With (acute) lower respiratory infection
• J44.1 - With (acute) exacerbation
• J44.9 - Unspecified
Asthma – Mild, Intermittent
• J45.20 - Uncomplicated
• J45.21 - With (acute) exacerbation
• J45.22 - With status asthmaticus
Asthma – Mild, Persistent
• J45.30 - Uncomplicated
• J45.31 - With (acute) exacerbation
• J45.32 - With status asthmaticus
Asthma - Moderate
• J45.40 - Uncomplicated
• J45.41 - With (acute) exacerbation
• J45.42 - With status asthmaticus
Asthma - Severe
• J45.50 - Uncomplicated
• J45.51 - With (acute) exacerbation
• J45.52 - With status asthmaticus
Asthma - Unspecified
• J45.901 - With (acute) exacerbation
• J45.902 - With status asthmaticus
• J45.909 - Uncomplicated
Asthma - Other
• J45.990 - Exercise induced bronchospasm
• J45.991 - Cough variant asthma
To ensure proper care and receive appropriate reimbursement, providers should ensure accurate, complete documentation and coding that reflects the true nature of a patient’s current health status at the highest level of specificity. Knowing the specific guidelines for reporting asthma and COPD is also important.
Since May 1972, the American Lung Association has celebrated
Clean Air Month to educate people about the importance of clean air and how air pollution poses a serious threat to the nation’s health.
Reports from the USEPA indicate that federal and state implementation of regulations has substantially reduced emissions of the common air pollutants since 1980. However, the agency notes that despite considerable progress in air quality improvement, over 100 million people nationwide lived in counties with pollution levels above the primary National Ambient Air Quality Standards (NAAQS) in 2021. A nationwide study from Harvard T.H. Chan School of Public Health suggested that counties with higher pollution levels had a higher death rate from COVID-19.
Healthcare providers, especially pulmonary physicians, can educate patients and their communities about the risks of indoor and outdoor air pollution and on strategies for reducing these risks.
Simple steps at the individual level can make a big difference over time:
• Use public transport.
• Keep your car in good condition.
• Avoid an idling engine; turn it off.
• Do not burn your garbage; arrange for trash hauling.
• Limit and control backyard fires.
• Plant and nurture trees.
• Use less energy; choose efficient appliances and heating systems and turn off devices when you are not using them.

Anyone can become a champion for clean air. Join the campaign and celebrate Clean Air Month!
Natalie Tornese, CPC, is a Senior Group Manager responsible for Practice and Revenue Cycle Management at MOS. She brings 25 years of healthcare management experience to the company. Natalie has worked in varied leadership roles with practices and specialties. Her primary focus is revenue cycle management with an emphasis on Medical Billing, Coding, and Insurance Verification Management. She has written numerous articles on all aspects of Practice Management and presently manages a large team focused on Medical Billing, Medical Coding, Verification, and Authorization services for MOS. Contact us at 1-800-670-2809 or visit us at (www.outsourcestrategies.com).

The move is from Version 24 (V24) for hierarchical condition categories (HCCs) to Version 28 (V28). This affects payers, physician offices, and hospitals who serve the 31 million patients enrolled in Medicare Advantage programs, care for 11 million patients enrolled through accountable care organizations, and reimbursement to others being reimbursed through shared savings programs or Medicaid risk adjustment.
Risk adjustment is a payment model that predicts costs for patients based on their demographics and health status. In MA risk adjustment, a subset of ICD-10-CM diagnosis codes is mapped into risk groups or HCCs. These HCCs are each assigned a risk coefficient. An individual patient’s risk score is determined by aggregating all diagnoses assigned to
them during a calendar year, then predicting costs for the following year. These risk scores determine how private insurers who offer Medicare Advantage plans are reimbursed for the services provided to their enrollees.
A copy of the 140-page Advance Notice can be found at: https://www.cms.gov/files/document/2024-advance-notice.pdf. The 200-page Announcement can be found at: https://www.cms.gov/files/document/2024-announcement.pdf. Both documents should be downloaded and referenced for a comprehensive understanding of the changes. Only medical HCCs are affected by this Announcement: CMS will continue in CY 2024 to use the 2020 RxHCC risk adjustment model to calculate Part D (pharmaceutical) risk scores.

In the new V28, CMS has reduced the number of risk-adjusting ICD-10-CM codes from 9,797 to 7,770. The changes are complex, sophisticated, and clearly informed by past risk adjustment validations (RADVs) and Office of Inspector General (OIG) audits. Three HCCs were removed entirely: HCC 47 - Malnutrition; HCC 88Angina Pectoris; and HCC 108 - Vascular Disease. Multiple HCCs were added to further differentiate disorders in existing categories or to add new categories. All but the first three HCCs were renumbered. While there are 86 HCCs in V24, the total swells to 115 in V28. The highest HCC number in V24 is 186; the highest HCC number in V28 is 463, indicating CMS is allowing for potential expansion, and for inclusion of “nonpayment” HCCs, so that some groups of diagnoses can be evaluated in the future (e.g., codes for atherosclerosis of arteries of the extremities, with intermittent claudication, aortic atherosclerosis, and aneurysm were placed in nonpayment HCC 265).
V28 changes include removal of many controversial diagnoses that consultants and coding managers have long targeted as either revenue opportunities, or compliance risks. CMS, in responding to comments from the Advance Notice, made clear in the Announcement its position on many of these changes in a candid condemnation of some Medicare Advantage organizations’ (MAOs’) practices:
“The risk adjustment model used for MA payment is not designed to drive clinical behavior to look for specific conditions or to be the sole purpose for MA organizations or healthcare providers to identify and treat conditions that are potential precursors to adverse medical events or complicating factors in the identification and treatment of other conditions. MA organizations are required, by their contracts with CMS and section 1852(a) of the Act, to furnish medically necessary Part A and Part B benefits to their enrollees.”
To say CMS is telling MAOs to get their house in order is an understatement. CMS wants a full remodel, or even a demolition and rebuild, for payers who are abusing or defrauding the system. And although there are many who focus on compliance, no one working in risk adjustment will be unaffected by the breadth of change,
which will require re-education of coders, software revisions, process changes, and assessments of financial impacts. This includes not only MAOs, and Medicaid programs, but fee-for-service physicians who receive bonus payments under the Merit-based Incentive Program System (MIPS), which uses HCCs in its calculations.
Because so many risk-adjusting conditions have been seen as incidental findings in diagnostic tests or are underreported by overworked providers, many MAOs over the years have developed chart review processes to optimize HCC capture. Chart review works like this: Prior to a scheduled encounter, chart-prep staff (usually a nurse or experienced coder) will review a patient’s complete history of the medical record to determine if there are any risk-adjusting diagnoses that have not been captured during the current calendar year. (Riskadjusting diagnoses must be submitted on claims at least once annually to be captured for payment). The chart prep staff assigns these “missing” diagnoses to the provider with a request that these diagnoses be addressed and documented during the upcoming encounter. As a result, diagnoses that otherwise would not have been considered pertinent to the visit are theoretically reported.
Ideally, the patient is benefitting from a focus on these missed conditions. A patient’s stroke sequela, HIV positive status, or mild dementia is easily overlooked if their visit is for sinusitis, but this is a chance to check up on these conditions, especially in patients who eschew preventive care. But realistically, busy providers may document just enough information in the chart to capture the assigned diagnoses. This may be contrary to the ICD-10-CM guideline IV.J: “Code all documented conditions that coexist at the time of the encounter/ visit and that require or affect patient care, treatment, or management.” If the discretionary condition didn’t affect patient care, treatment, or management, it should not be reported, and plans are seeing an increase in scrutiny from the OIG, which in the past two years has asked for hundreds of millions of dollars in repayment for “unsupported diagnoses.” Indeed, Inspector General Christi A. Grimm of HHS, said in her presentation at RISE National 2023 in March, “I can tell you with great certainty that you will see us expanding our oversight of Medicare
Advantage in the coming months and years. Now is truly the time to embrace the benefits of proactive, effective compliance actions and oversight.”
Alert: V28 Is Already Applicable!
The Medicare Advantage is a prospective payment system, meaning this year’s payments are calculated based on last year’s diagnoses. V28 becomes effective January 2024. Therefore, payments in 2024 will be based on claims data from 2023. These HCC changes are retroactive to codes that were assigned to claims months ago. The good news is that V28 will be phased in over three years. Payments to MAOs for 2023 are unaffected. For 2024, risk scores will be calculated with a blend of 67% V24 mappings and 33% V28 mappings. For 2025, 33% will be based on V24, and 67% on V28. In 2026, all risk scores will be calculated using V28 mappings.
In other news, both good and not so good, CMS is assigning “nonpayment” HCC status to many of the conditions that are being removed from the mappings. According to CMS in the Announcement, “These codes represent less severe conditions with lower cost implications.” Retaining their data in nonpayment HCCs allows CMS to analyze or reconsider them in the future.
CMS aims to discern the financial impact of complications of diabetes. For V28, there are still the three diabetes HCCs we will find somewhat familiar: HCC 36 - Diabetes with Severe Acute Complications; HCC 37Diabetes with Chronic Complications; and HCC 38 - Diabetes with Glycemic, Unspecified, or No Complications. A fourth diabetes HCC reports pancreas transplant because all system-specific transplants have been separated out into their system specific HCC groupings. The big news in HCCs 36, 37, and 38 is that they have all been assigned the same value: 0.166. By comparison, in V24, uncomplicated diabetes was assigned a value of roughly one-third the value of complicated diabetes. The effect of this change on individual plan revenue will depend upon its case mix. This de-incentivizes providers and payers from linking conditions to diabetes that are typically not caused by diabetes, for example, identifying obesity as a complication of diabetes. Similarly, because hyperglycemia and hypoglycemia can present with mild symptoms
and can usually be easily resolved, these conditions were moved to HCC 38, with uncomplicated diabetes. CMS calls this action “constraint,” and has said that it could lead to lower risk scores for beneficiaries.
In its move away from V24, CMS targets diagnoses that are not the focus of the encounter but are discretionary conditions documented and abstracted chiefly because they risk adjust. These are the controversial codes that consultants and coding managers have focused a lot of energy on in the past five years.
“Diagnoses that are particularly subject to intentional discretionary coding variation or inappropriate coding by health plans/providers, or that are not clinically or empirically credible as cost predictors, should not increase cost predictions,” the Advance Notice reads. “Excluding these diagnoses reduces the sensitivity of the model to coding variation and coding proliferation.” CMS indicates that the medical definitions of diagnoses CMS calls “discretionary” varies from provider to provider, further exacerbating consistency issues in diagnosis reporting.
Some examples of the type of excluded diagnoses from V28 include (V24 mappings and 2023 community, nondual, aged risk coefficient included in parentheses):
• Peripheral vascular disease. This is a vague circulatory term that has been associated with venous and arterial disease, commonly of the lower extremity. It has no clear and specific definition. (HCC 108, 0.257)
• Aortic aneurysm without rupture, ectasia, or dissection. The natural diameter of aortas has some variation based on sex and patient size. Although some patients have a normal abdominal aorta measuring 3 cm, an abdominal aortic aneurysm is usually defined as 3 cm or larger. This is a good example of “discretionary” diagnosis, as most Medicare patients already take statins and monitor blood pressure, two noninvasive treatments for aneurysms. (HCC 108, 0.257)
• Cachexia and malnutrition. While the American Society for Parenteral and Enteral Nutrition (ASPEN) has published clear diagnostic criteria for malnutrition and cachexia, some providers have been
reporting malnutrition when the patient’s BMI or weight drops, without the confirmatory lab tests or documentation of signs and symptoms associated with malnutrition. (HCC 21, 0.549)
• Atherosclerosis without manifestations.
Atherosclerosis is ubiquitous in the Medicare population, and unless significant, is not usually actionable without noticeable symptoms (e.g., gangrene, ulceration, etc.). CMS found these codes were reported even when the only evidence was an incidental finding on a radiograph of atherosclerosis in the aortic arch, lower extremities, or other vessels. Atherosclerosis of extremities with intermittent claudication were also removed from risk adjustment. Atherosclerosis with rest pain still maps for payment, but to a higher valued HCC. (HCC 108, 0.257)
• Simple angina pectoris. Angina is chest pain that is predictable, responds to medicine, and is short-lived. It is usually caused by exertion. Unstable angina, which continues to risk adjust in V28, occurs without provocation, and is less responsive to medications. It gets worse over time. (HCC 88, 0.136)
• Brain atrophy. Normal aging causes atrophy of tissues, including those in the brain. This change may be noted on a radiograph performed for an unrelated symptom. Because it is a normal sign of aging seen in almost all adults over 60, this type of cerebral degeneration no longer risk adjusts. (HCC 52, 0.314)
• Thrombocytopenia. Platelet count normally drops with aging. Determining whether a patient has thrombocytopenia is very subjective and mild thrombocytopenia often is not treated. Therefore, unspecified or secondary thrombocytopenia no longer risk adjusts. (HCC 48, 0.192)
• Senile purpura. Thin skin in the aging population can lead to purple spots on the forearms and hands. This condition is common and not usually treated. (HCC 48, 0.192)
• Spinal enthesopathy. Inflammation of the entheses (connective tissues between bones and tendons or ligaments) is a form of arthritis in which pain increases with movement. It is usually a diagnosis based on symptoms and examination of the patient. Also deleted were codes for other specified inflam-
matory and unspecified inflammatory spondylopathies. (HCC 40, 0.414)
• Sjögren’s disease. Symptoms of Sjögren’s disease may be limited to dry eye or low salivary secretions. Mild cases may be diagnosed subjectively. More complex cases may involve joints. (HCC 40, 0.414)
• Sacroiliitis. Often a diagnosis of exclusion, sacroiliitis is an inflammation of the sacroiliac joint, causing pain in the upper buttocks or lower back. (HCC 40).
• Unspecified spondylopathy. Spondylopathy is inflammation of the spine and its joints. Whether inflammatory or in diseases classified elsewhere, when unspecified spondylopathy is removed from V28. (HCC 40, 0.414)
Subjectivity of diagnoses like those above are only one of the criteria CMS considered when amending the HCC model. “Changes to the condition categories – including additions, deletions, and revisions – are based on each condition category’s ability to predict costs well – for example, because the coefficient is small, the t-value is low, a small number of beneficiaries have a certain condition, or the condition does not have well-specified diagnostic coding – are not included in the model,” the Advance Notice reads. (A t-value, in actuarial work, measures the size of a difference relative to the variation in the data. A “low t-value” indicates that a particular diagnosis is not of significant financial value.)
Other broad categories of deletions in V28 include removal of conditions caused by medications or chemicals, including more than 100 diabetes codes in ICD-10-CM rubric: E09 - Drug or chemical induced diabetes mellitus; 44 codes in subcategory M87.1 - Osteonecrosis due to drugs; G21.19 - Other drug induced secondary parkinsonism; D84.821 - Immunodeficiency due to drugs; M32.0 - Drug induced systemic lupus erythematosus; and M34.2 - Systemic sclerosis induced by drugs and chemicals.
Another area of big change is in behavioral health, where dozens of less severe diagnoses are omitted from payment. In the Announcement comments, CMS writes, “For depression, the 2024 CMS-HCC payment model is limited to ICD-10 codes specifying moderate or severe major
depression. Remaining diagnosis codes (includes depression codes for mild, unspecified, or in remission, as well as codes for bipolar disorders in remission) from the 2020 CMS-HCC model HCC 59 were remapped to the nonpayment depression HCC.” Similarly, sequela of intentional self-harm codes were removed from the mappings. Initial codes for attempted suicide and self-harm continue to risk adjust in V28. In total, and in part because the self-harm codes are so numerous, 95% of the codes that previously mapped to HCC 59 - Major Depressive, Bipolar, and Paranoid Disorders no longer risk adjust.

There are significant changes to many of the HCC groupings unexplored above. A complete HCC table comparing all V24 codes to V28 codes can be found in PY 2024 Proposed Clinical Revision Part C Model ICD-10 Mappings at: https://www.cms. gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/RiskAdjustors-Items/RiskOtherModel-Related. This file is essential for determining which codes are deleted in V28, or new in V28. Download the file and use Excel sorting functions to identify changes. Simply search for fields that say “No”; these are indicative of a status change from V24 to V28. If there is “No” in the V24 column and “Yes” in the V28 column, the code is a new mapping for V28—a code that didn’t map until V28. If there is “Yes” in the V24 column and “No” in the V28 column, it indicates that this code risk adjusted for V24 but no longer maps for V28. Users should be able to sort and resort, by code number, or by “No” in either column, to gain a complete understanding of the thousands of changes .
See Table 1 next page.
Note: In this sorted Excel spreadsheet of V28, Z89.421 - Acquired absence of other right toe(s) does not risk adjust in V28, but did risk adjust in V24. Conversely, D3A.00 - Benign carcinoid tumor of unspecified site did not risk adjust in V24, but risk adjusts as a metastatic cancer in V28. In this instance, medical research has determined that all carcinoid tumors carry some level of malignancy, and so benign carcinoid tumor codes now map to HCC 22, Bladder, Colorectal, and Other Cancers.
“Now is truly the time” is a bit of an understatement regarding the urgency of converting to V28, effective for calendar


ICD-10-CM Codes, V24, V28 CMS-HCC Models Includes ICD-10 codes valid in FY2022 and FY2023
year 2024. As a retrospective payment system, Medicare Advantage payments are based on codes submitted the previous year. Plans need to calculate where to focus their revenue. These will still risk adjust but at a fraction of previous years. Similarly, codes that did not map to HCCs in V24 but do map to HCCs in V28 may have been overlooked earlier this year. Among the newly mapping diagnoses are codes for sarcoidosis of the skin, sarcoid arthropathy, and sarcoid myositis; anorexia and bulimia nervosa; retinal vein occlusion, malignant pericardial, or pleural effusion; toxic liver disease; pemphigus; and benign carcinoid tumors. HCC recapture efforts will require significant revision, and coders or nurses involved in recapture must pivot immediately to address V28 so that the work they do is worthwhile. Coding policies and
procedures will need revision, as will any coding or clinical support materials focused on risk adjustment.
Similarly, coders must take a deep dive into new V28 codes and V28 deletions as soon as possible. For HCConly coding, this is critical for efficiency and for all HCC code capture. For example, codes identifying sarcoidosis of the lung, lung and lymph, and cranial nerves all were deleted for V28, possibly because the manifestations for these conditions would also risk adjust. However, sarcoid arthropathy, myositis, and sarcoidosis of the skin were added to V28, likely because those manifestations do not risk adjust separately and sarcoidosis needs to be captured. See Table 2.
CMS anticipates that the removal of so many “discretionary” diagnoses from the HCC mappings will allow provider payments to more appropriately reflect the work and utilization associated with encounters because these conditions did not accurately reflect resource utilization as seen in the fee-for-service reporting. According to the Announcement, “The updates improve the accuracy of the risk adjustment model and help ensure that higher payments are available to plans that serve beneficiaries with more costly healthcare needs.”
But not all the news is bad. In its Announcement, CMS stated, “If a specific HCC (or diagnosis code mapped to a specific HCC) is no longer included in the payment model, coefficients of other HCCs and demographic factors will be increased such that the model continues to predict the overall total expenditures,” and “we estimate that the overall impact of the CY 2024 Rate Announcement will be a net increase of 3.32 percent.” Some of the HCC values increased substantially in V28, and most went up at least a bit. For example, lysosomal storage disorders mapped to HCC 23 in V24, with a value of 0.194 (community, nondual, aged). Under V28, these disorders, including Hurler’s syndrome, mucopolysaccharidosis, and glycogen storage disease, map to HCC 49 - Specified Lysosomal Storage Disorders, with a RAF value of 9.256. Heart failure has one HCC in V24, but is broken into several HCCs in V28, most notably, HCC 222 - End-Stage Heart Failure, with a RAF of 2.505. V24’s all-inclusive HCC 85, Congestive Heart Failure, has a RAF of 0.331. Most of the increases are not as substantial, and some HCCs drop in value. See Table 3.
Organizations have the rest of 2023 to evaluate how much revenue is at risk for 2024 due to the lost “discretionary” codes, and what gains might be realized by some of the increased RAFs in V28. There is a significant amount of information to digest in
V28, including revisions to the star rating system. Payment HCC counts are also affected. Five diagnoses are required for any RAF scoring, and with the elimination of some of the more common HCCs, this will be harder to achieve.
The overall impact of the changes for most organizations is likely a reduction in revenue. CMS projects that the impact from these changes will be a net savings of $7.6 billion to the Medicare Trust Fund for 2024.
Sheri Poe Bernard, CPC, CRC, CDEO, CCS-P, is Director of Risk Adjustment Assessment and Compliance at Granite GRC Consulting. She is the author of the American Medical Association’s book, Risk Adjustment Documentation & Coding - in its second edition. Sheri has worked in healthcare coding education and training for 30 years, specializing in risk adjustment for the past 12 years. She can be reached at SPB@granitegrcconsulting.com. Learn more at: granitegrcconsulting.com.
MEDPAC’s March 2023 Medicare Advantage Report to Congress
Medicare Advantage programs now account for 49% of Medicare enrollees, according to the March 2023 MEDPAC Report to Congress.
According to MEDPAC, CMS spends 6% more on Medicare Advantage enrollees than it would spend if they were enrolled in Part B instead—a difference of $27 billion. Its analysis of 2021 data found higher diagnosis coding intensity leading to risk scores that were 10.8% higher than similar fee for service (FFS) beneficiaries. “MA plans’ diagnostic coding practices inflate payments and undermine the goal of plans competing to improve quality and reduce healthcare costs,” the report said, and “a major overhaul is urgently needed to reduce the gap between MA and FFS payment.”
MEDPAC’s report stated that MA chart review programs mining for evidence of diagnoses uncaptured for the calendar year account for some of this discrepancy, as FFS programs do not benefit from chart review processes. The report highlighted several lawsuits alleging improprieties in the MA chart review process. This process is used almost exclusively to add diagnosis codes; less than 1% of chart reviews were used to remove erroneous codes in an OIG study cited by MEDPAC.
The entire Medicare Advantage status report can be viewed at: https://www.medpac.gov/wp-content/uploads/2023/03/Ch11_Mar23_MedPAC_ Report_To_Congress_SEC.pdf
*Community, nondual, aged population RAFs used in these tables


The following cases highlight fraud, waste, and abuse (FWA) and serve as a reminder to uphold high ethical standards when providing patient care and services.
A doctor and companies he owned and operated have agreed to pay the United States $3 million to resolve claims they improperly billed to Medicare.

Allegedly, the psychiatrist and his companies knowingly and willfully submitted, or caused the submission of, false claims to Medicare. The allegations included intentionally pressuring patients to accept unnecessary medical treatments and billing for those treatments, falsifying treatment records and billing Medicare for services they did not provide.
The investigation began when two individuals who worked at one of the clinics filed a qui tam, or whistleblower, lawsuit under seal in 2021.
During their terms of employment, they allegedly witnessed patients being pressured to accept unnecessary medical treatments, as well as the falsification of treatment records and billing Medicare for worthless services or services the clinic did not provide.
The doctor and his clinics had allegedly submitted claims for payment to Medicare for Transcranial Magnetic Stimulation (TMS) procedures that were not performed, and/or routinely administered without medical necessity or a valid medical purpose. They also billed Medicare for phy-
sician assessments when the physician did not see the patient or supervise the TMS session.
The complaint indicated the fraudulent conduct continued until the business was sold in April 2022.
An FBI Special Agent in Charge on the case stated, “Billions upon billions of taxpayer dollars are stolen by healthcare fraudsters each year.”
Under the False Claims Act, a private party known as a relator can file an action on behalf of the United States and receive a portion of the recovery. In this case, the relators will receive a total of $300,000.
Read the specifics of this case at www.justice.gov.
A national supplier of durable medical equipment (DME) has paid $7 million to resolve civil allegations that it made false statements in connection with claims for reimbursement it submitted to Kentucky Medicaid, two Kentucky Medicaid Managed Care Organization contractors (MCOs), MO HealthNet (Missouri Medicaid), and D.C. Medicaid.
This supplier provides supplies such as hospital beds, manual wheelchairs, power wheelchairs with accessories, and gait trainers. The investigation involved DME that was “manually priced” by Medicaid payers in Kentucky, Missouri, and D.C. Those Medicaid programs reimbursed manually priced DME based on the cost the supplier actually paid the manufacturer for the equipment. Specifically, in Kentucky, reimbursement is based on “a manufacturer’s actual charges” billed to the supplier, or the “invoice price”; in Missouri, reimbursement is based on the “actual invoice of cost”; and in D.C., reimbursement is based on “original documentation reflecting all discounts.”
In the Settlement Agreement, the United States alleged that the supplier did not disclose all discounts it received, or the cost it actually paid to DME manufacturers when submitting
claims for manually priced DME to Kentucky Medicaid, two Kentucky Medicaid MCOs (Aetna Better Health of Kentucky and WellCare of Kentucky), MO HealthNet, and D.C. Medicaid. The supplier’s failure to disclose all discounts, or the actual cost paid, resulted in these Medicaid programs paying it higher reimbursements than it was entitled to receive. The United States contended that the conduct violated the False Claims Act, 31 U.S.C. § 3729(a)(1)(B), a federal law that prohibits knowingly making or using a false statement material to a false claim for reimbursement.
As part of the settlement, the supplier also entered into a 5-year Corporate Integrity Agreement (CIA) with the U.S. Department of Health and Human Services Office of Inspector General. The CIA requires, among other things, that the supplier implement a centralized risk assessment program, as part of its compliance program, and hire an Independent Review Organization to complete annual reviews of some of its Medicare and Medicaid claims.
“By hiding or failing to disclose discounts, to receive higher reimbursement from Medicaid programs across the country, [the supplier] prioritized its financial incentives, to the detriment of these Medicaid programs,” said a United States Attorney on the case.
The settlement resolves a lawsuit originally brought by a former employee of the supplier under the qui tam, or whistleblower, provisions of the False Claims Act. Under those provisions, a private party can file an action on behalf of the United States and receive a portion of any recovery. As part of this resolution, he will receive approximately $1.05 million of the settlement amount.
The claims resolved by the settlement are allegations only, and there has been no determination of liability.
Read more about this case at www.justice.gov.

As consumers, we all face challenging inflationary pressures in our lives, with everything presenting challenges to our budgets. Essential groceries and other items are up significantly, posing tremendous financial obstacles for all consumers. The Consumer Price Index (CPI), a closely watched gauge of inflation, recently showed that price increases continue to slow. The CPI measured 6% for the year at the end of February, down from January’s 6.4%. Just the same, consumers are still faced with increasing prices, which obviously puts a damper on the economy since consumer spending accounts for nearly two thirds of the economy. So, what does this have to do with hospitals’ finances and overall operations?
All hospitals and health systems are facing the same inflationary pressures as most consumers but to a larger scale and degree considering all the fixed expenses and high costs associated with operating a healthcare operation 24 hours a day, 365 days a year. All hospitals and health systems are facing nursing and physician shortages, as well as discipline shortages where hospitals and health systems have paid 258% more for contract labor during the pandemic as compared to pre-pandemic rates. Couple this with the same
inflationary pressures that consumers are presently facing but to an even greater extent with high pharmacy spend, continued use of contract labor, food costs and supply increases, costs to retain current workforce with wage and benefit increase, retention bonuses, and information technology infrastructure costs, including the electronic health record—to name just a few.
A successful business must closely manage costs and grow revenue to ensure financial performance, allowing suffi-
cient revenue to continue to invest back in the business. Labor costs account for upwards of 60% of total costs of operating a hospital. Hospitals and health systems are faced with high fixed operational costs. Growing patient and nonpatient revenue is critical to ensuring the hospital can meet its financial obligations while continuing to meet the healthcare needs of the community. The key to the revenue cycle is net patient revenue from operations, the money from operations that drops to the hospital’s bottom line. Unfortunately, net patient revenue from continued hospital operations is where hospitals are facing monumental financial headwinds.
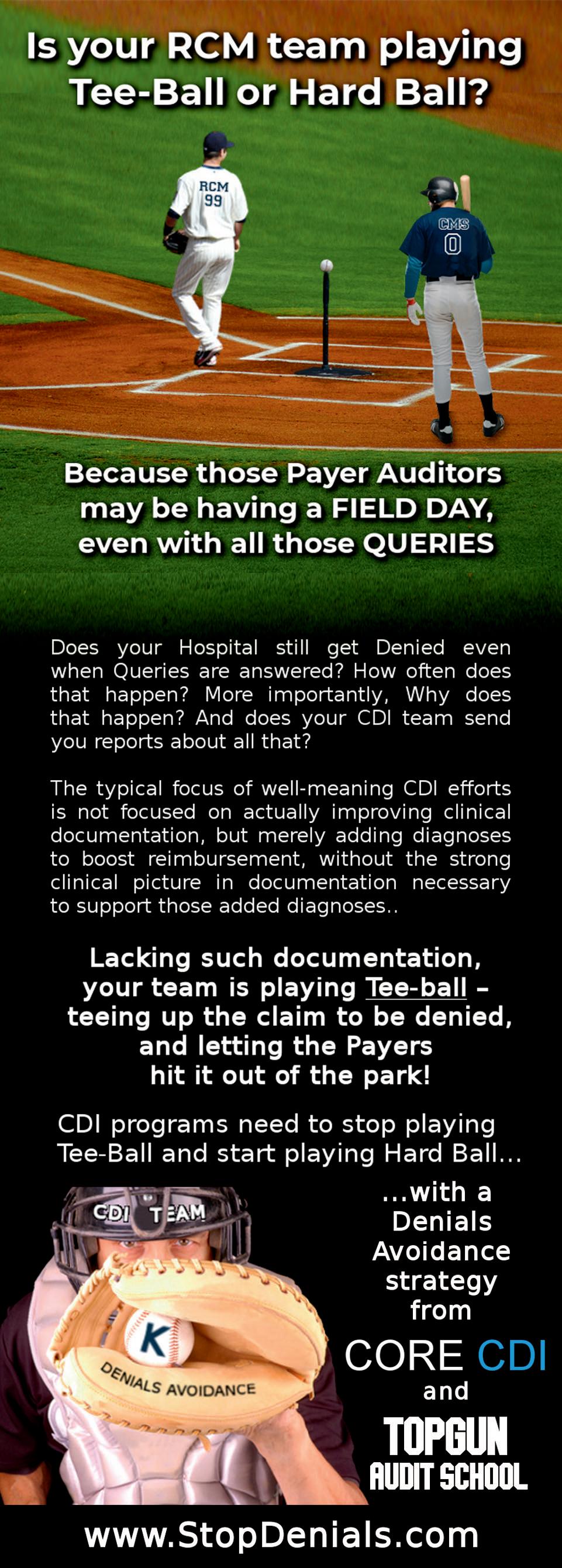
Net patient revenue (NPR) is the aggregate money generated from patient services collected from payers, including private insurance, Medicaid, and Medicare. The calculation for NPR is the total patient revenues minus patient discounts. NPR does not factor in contractual adjustments, charitable donations, foundation earnings, or bad debt. Gross patient revenue is defined as the total charges at the hospital’s full established rates for the provision of patient care services. Net patient revenue represents what the hospital actually collects in revenue from the payer or patient. Here is where hospitals and health systems are facing daunting hurdles, where payers are engaging in strategies to reduce their reimbursement to providers, attempting to reduce their Medical Loss Ratio—the share of total healthcare premiums spent on medical claims and efforts to improve the quality of care. The remainder is the share spent on administration costs and fees, as well as profits earned. These strategies used by the payers include, but are not limited to, issuing medical necessity and clinical validation denials, as well as DRG and level of care downgrades. If you are a medical record coder or Clinical Documentation Integrity Specialist, you are undoubtedly familiar with DRG downgrades and clinical validation denials. This is an area that accounts for a large proportion of payer denials where payers utilize sophisticated data mining and data analysis to select claims for either prepayment or post payment review, in a concerted attempt to drive down their expenditures for their members’ patient care. Remember that payers have amassed a vast amount of claims data, using the claims data to devel-
op rules in conjunction with artificial intelligence and machine learning to identify “hit” cases to review and make a case for not reimbursing as coded and billed and paid under contractual arrangements.
All hospitals and health systems continue to struggle financially, dealing with decreasing reimbursement from payers, as well as experiencing lower patient volumes in the face of increasing expenses. Highly profitable surgeries are at lower volumes considering higher patient copays and deductibles in conjunction with inflationary pressures that patients face. Hospital margins continue to be negative with negative 1.0 percent in January 2023. (See Kaufman Flash Report February 2023). Couple these phenomena with payers issuing more denials that are time consuming and costly to appeal and you have a recipe for difficulty in maintaining positive operating margins. What is required to fervently address rapid fire payer denials is total transformation and cultural change throughout the organization.
Every employee involved in the revenue cycle plays a vital role in driving down often self-inflicted payer denials by embracing a mindset of “Denials Avoidance,” embracing the notion that one avoidable denial is one too many. While no one role in the revenue cycle is more important than the other, let’s spotlight the critical role of Coding and Clinical Documentation Integrity. Clinical Documentation Integrity Specialists’ roles and responsibilities include concurrent review of medical records, identification of opportunities for physician documentation clarification, issuing of physician queries when clinically warranted, tracking of physician queries, and physician education on documentation improvement. CDI program popularity and their implementation in hospitals really took off around 2008 with the advent of the MS-DRG reimbursement system. CDI consulting companies promoted to CFOs that implementing their CDI programs were the answer to increasing reimbursement with the capture of more CCs/MCCs. This message still prevails but has been expanded to include Risk of Mortality/Severity of Illness scores and other quality measures that factor into publicly reported quality scores. One would assume that Clinical Documentation Integrity Programs would alleviate payer denials through better
physician documentation. Unfortunately, this assumption is not accurate as explained further below.
As a practicing coder who is still engaged in day to-day coding, I can appreciate the duties and responsibilities of coding staff. The logic goes that with more complete and accurate physician documentation, the coder will be able to more accurately assign all clinically relevant diagnoses that impact quality data reporting, as well as achieve optimal MS-DRG assignment and reimbursement. In other words, as a result of CDI intervention, the record will speak for itself and the coder will best assign ICD10 codes, thereby alleviating bill holds associated with retrospective queries for clarification of documentation. Excessive bill holds tie up much needed hospital revenue. So, why does this logic of CDI supporting better physician documentation, coding, and reimbursement not materialize as is evident by increasing reimbursement?
Clinical Documentation Integrity programs can be a formidable force in alleviating unnecessary payer denials if the profession embraced the notion of denials avoidance by partnering with physicians, case management, utilization review/management, denials and appeals, and physician advisors to make significant inroads in achieving clinical documentation excellence. Today’s model of CDI processes merely scratches the surface of what can be achieved in meaningful, measurable, and sustainable improvement in physician documentation, best telling and describing the patient story necessary to help the physician establish medical necessity for hospitalization. Without medical necessity, there simply is no need for CDI activities since no payment negates the efforts of CDI in capturing CCCs/MCCs. Clinical validation denials and DRG downgrades abound attributable to insufficient physician documentation that does not meet the Medicare expectation of complete and accurate physician documentation. The CDI profession must expand its breadth and depth of knowledge, skill sets, and core competencies in best practice standards and principles of documentation. This will position and equip the CDI professional with the ability to work collectively with physicians and other providers, taking the lead and serving as the change agent to really move the needle on documentation integrity. In many aspects, the term “integrity”
is a misnomer in the sense present day CDI activities fail to improve the integrity of the record with secured diagnoses from the query process standing to generate more clinical validation denials. Querying for financial impact as the mainstay of CDI will continue to contribute to increasing payer denials.
Hospitals and health systems will continue to experience significant financial challenges complicated by inflationary pressures. Ongoing payer denials are a definite drag on hospital finances. Rather than resorting to the perpetual inefficient process of appealing payer denials, hospitals should be ingraining in staff an attitude of denials avoidance versus denials management. A logical starting point is physician documentation quality and completeness, transforming CDI from a reactive repetitive reactionary approach to a far more efficient process of working towards achieving proactive preemptive denials avoidance physician documentation. CDI professionals are encouraged to realize and respect the medical record as a primary communication tool first and foremost, working with physicians as guides, mentors, facilitators, and resources to physicians and other providers on anything related to documentation. There is no time like the present for CDI to engage as the “Beacon of Hope” for our hospitals and health systems by doing our part to really improve the integrity of the medical record from both a patient care and high performing revenue cycle perspective.
Description:
Glenn Krauss is a well-recognized and respected subject matter expert in the revenue cycle with a specialized emphasis and focus upon collaborating and working closely with physicians in promoting, advocating for, educating, and achieving sustainable improvement in clinical documentation that accurately reflects and reports the communication of fully informed coordinated patient care. His experiences include working with a wide variety of healthcare systems, spanning the entire spectrum and ranging from critical access hospitals, community hospitals, and Federal Qualified Healthcare Centers to large academic medical centers and fully integrated healthcare systems. He possesses 25+ years of progressive practical hands-on experience in clinical coding and documentation improvement, subscribing to the philosophy that quality of medical record documentation strongly correlates with overall quality of care achieved and the overall achievement of a high performing revenue cycle. Glenn has demonstrated the unique skill sets and core knowledge of principles and standards in best practices of clinical documentation, effectively and successfully driving physician engagement through proven strategies that create and foster a sustainable model for clinical documentation improvement. https://Core-CDI.com
This webinar discusses HBAI services, focusing on coding and billing. Medical necessity is explored, including Optum/ APA examples. The speaker points out changes from the 2019 HBAI services CPT codes to the current codes. Documentation requirements to support proper billing and coding for HBAI services are shared, including time tips to remember.

A large metropolitan-area radiology group covers several departments within a hospital system. They have on-site staff daily at each location to handle all modalities, including sub-specialists to be sure pediatric, neuro, and body imaging are handled with the right expertise. They find that on some days a particular department is overloaded, while on the same day another department is slow. The subspecialists don’t always have enough work in their area to keep them busy. Lately, trying to hire enough hands in the tight radiology job market has become more and more difficult, as well as costly. Unfortunately, the various hospitals do not all employ the same Picture Archiving and Communication System (PACS) even though they’re part of the same parent system. This group’s situation is not unique.
An article by Shinagare and Khorasiani in the February Korean Journal of Radiology describes a hospital system that created a radiology network across its several academic and community hospitals and other imaging sites, with a centralized pool of images in a common PACS from which the radiologists pull cases to read based on their assignment. This allows subspecialty expertise to reach cases where the appropriate radiologist cannot be physically located, including the opportunity to cover more remote, rural sites. It also reduces the need to have as many of each subspecialty within the same group, since they can be available to all the sites at once. The system helps the radiology practice balance its workload so that excess volume from one site can be absorbed by radiologists from another site.
The authors explain that by creating shared resources, including electronic medical records (EMR), PACS, dictation, and result-communication systems, they are able to distribute cases based on radiologist availability and expertise regardless of where the patient was scanned. It’s easy to see how such a system can help a group become more efficient by allowing more work to be done by fewer individuals. For a growing practice, this offers the ability to expand without taking on more payroll and, for a practice with attrition, it allows the remaining radiologists to pick up the slack without a one-for-one replacement of those who have left. Both scenarios offer enhanced net revenue
to the group.
However, development of such a system is costly and requires effort to achieve. When hospital hierarchies are involved, the complexity increases. With a long-range view, the benefit would certainly
The idea of networking a single practice. Assuming itive with each other, two physicians across their established, which is especially same systems.
A number of networking
• Two or more radiology capacity in one area another area. Such dance or lack of subspecialists eral readers to handle
• Two groups might FTE slot. Working that meets their needs,
• Two or more groups readers, obviating it teleradiology company.
When groups share a full-time employee, the most likely arrangement would be for one group to subcontract with the other for the services it needs. A pool of radiologists shared by two or more groups would probably be best handled by creating a separate entity that is controlled in common by the sharing groups. In either case, the covering radiologists need to be on the hospital medical staff to read for patients that are hospital-based (either in or out-patient), and in all cases, they need to be credentialed with the billing group’s insurance payers, as well as with their federal programs (Medicare, Medicaid, etc.).


Conclusion
The concept of having a radiologist cover a wide range of patient locations from a single seat is a viable and valuable strategy in today’s environment. The difficulty for practices to hire sufficient staff, coupled with steadily declining reimbursement, makes radiologist efficiency the highest priority. Rather than sending a radiologist to the patient’s location, transferring
the patient’s images to the radiologist provides a solution to maximize the use of specialists within a single practice, as well as to bring high quality services to under-served areas. The technical environment can be created, albeit with some cost and effort, but the challenge for practices is to be able to use the technology to their best advantage.
Sandy Coffta, Vice President, Client Services, Healthcare Administrative Partners. Healthcare Administrative Partners (HAP) provides revenue cycle management, clinical analytics, and comprehensive practice management solutions for radiology practices. We also provide coding services for multispecialty practices. HAP produces results, not promises. Our key to optimizing your success is to aggressively improve all areas of your practice’s financial health – maximizing reimbursements and accelerating cash flow while reducing cost and compliance risk. www.hapusa.com
On May 23, 2016, the Federal Trade Commission (FTC) announced that it approved a final order with Henry Schein Practice Solutions, Inc. (HS) to resolve allegations that HS falsely advertised the level of encryption it provided to protect patient data. The consent order requires HS to pay $250,000 and prohibits it from “misleading customers about the extent to which its products use industry-standard encryption or the extent to which its products help ensure regulatory compliance or protect consumers’ personal information.”
Fast forward to 2022. On March 8, 2022, Department of Justice (DOJ) announced settlement under its Civil Cyber-Fraud In the interest of full disclosure, I represent ed the only whistleblower who raised allegations Comprehensive Health Services LLC (CHS), which “fail to disclose to the State Department that consistently stored patients’ medical records EMR system. When CHS staff scanned medical the EMR system, CHS staff saved and left scanned of some records on an internal network drive, accessible to non-clinical staff.”
In October 2022, a major health system, Aurora gave patients, the media, and the United States of Health and Human Services (HHS) notice health information (PHI), including sensitive identifiable information, may have been exposed to Google, Meta, and other third parties without their knowledge or consent. The Health Insurance Portability Act of 1996 (HIPAA) has long had provisions related to prohibited marketing and selling of PHI.
Now, in 2023, the FTC announced two consent orders related to the prohibited poaching and use of PHI by known third parties and the DOJ announced another settlement under its Civil Cyber-Fraud Initiative.
The take-away is fundamental. The illicit taking and utilization of patient/consumer data without knowledge or

consent can result in government action.
The FTC’s enforcement authority is derived from Section 5The Federal Trade Commission Act of 1914 as amended.
Two recent enforcement action settlements, which occurred between February and early-March 2023, underscore its authority and both are notable for distinct reasons:
• GoodRx (February 1, 2023) – This was the first case
where an enforcement action was taken under the FTC’s Health Breach Notification Rule. Here, GoodRx, a telehealth and prescription drug discount provider did “fail to notify consumers and others of its unauthorized disclosures of consumers’ personal health information to Facebook, Google, and other companies.” Moreover, “In a first-of-its-kind proposed order, filed by the Department of Justice on behalf of the FTC, GoodRx will be prohibited from sharing user health data with applicable third parties for advertising purposes, and has agreed to pay a $1.5 million civil penalty for violating the rule. The proposed order must be approved by the federal court to go into effect.” GoodRx paid the government $7.8 million to settle the allegations.
• BetterHelp, Inc. (Mar. 2, 2023) – In another first-of-its-kind case, the FTC provided remuneration to customers who were harmed by “online counseling service BetterHelp revealed consumers’ sensitive data with third parties such as Facebook and Snapchat for advertising after promising to keep such data private.”

The DOJ and whistleblowers utilize the False Claims Act. As the March 14, 2023 DOJ press release illustrates, concerning Jelly Bean Communications Design and its Manager (collectively “JellyBean”), cybersecurity failures and not having the requisite technical, administrative, and physical safeguards are two areas that may form the basis of a False Claims Act cause of action. As a disclaimer, the False Claims Act is a very complex and intricate area of law.
Some key take-aways from the JellyBean settlement include the following:
• From January 1, 2014 through December 14, 2020 – a period of over six years – JellyBean failed to provide secure hosting of protected health information (PHI) despite its representations in its agreements and invoices, and put patients, specifically children, and their PHI at risk.
• JellyBean created, hosted, and maintained a federally funded Florida children’s health insurance website and failed to secure personal information. Over 500,000 applications were hacked and the settlement amount to resolve the allegations amounted to $293,771.
• “The agreement required that JellyBean provide a fully functional hosting environment that complied with the protections for personal information imposed by the Health Insurance Portability and Accountability Act of 1996” (DOJ Press Release).
• The government alleged that numerous outdated and vulnerable software applications were being utilized and fundamental patches were not being done.
Compliance officers and counsel alike should learn from these recent actions. One fundamental step that should be included as part of any HIPAA Risk Analysis is the evaluation of the ingress and egress of patient/consumer data, whether or not patient consent is required in order for the information to be taken and utilized, and whether the third-party has the appropriate safeguards in place. Cultivating a culture of compliance that is genuine and can pass legal muster is something that should also be considered. Cybersecurity risk management is not going away and it would behoove everyone to re-evaluate their risk tolerance.
Rachel V. Rose, JD, MBA, is an Attorney at Law, in Houston, TX. Rachel advises clients on healthcare, cybersecurity, securities law, and qui tam matters. She also teaches bioethics at Baylor College of Medicine. She has been consecutively named by Houstonia Magazine as a Top Lawyer (Healthcare) and to the National Women Trial Lawyer’s Top 25. She can be reached at rvrose@rvrose.com. www.rvrose.com



The healthcare landscape is constantly evolving, with changes in technology, patient care, and the business of medicine all occurring at a rapid pace. One area that is often overlooked but is equally critical to the success and sustainability of a medical practice is the negotiation of payer contracts.
With the rising costs of providing healthcare, it’s essential that physician offices stay on top of their contracts with payers, such as insurance companies and government agencies. This article will explore the importance of renegotiating payer contracts every 18 months, focusing on three key factors: inflation, payer rate reductions, and the cost of retaining talented employees. Negotiating your contracts on your own may lead to increases, but you can also retain companies that specialize in this service. Researching both options is important, but negotiating your contracts is essential.
Inflation is a natural economic phenomenon that results in
the general increase in prices and a decrease in purchasing power over time. According to the U.S. Bureau of Labor Statistics, the average inflation rate from 2010 to 2020 was approximately 1.5% per year. When applied to healthcare, this means that the costs associated with providing medical services continue to rise over time.
For physician offices, inflation can have a significant impact on their bottom line. As prices for goods and services increase, so do the costs associated with running a medical practice, such as rent, utilities, and supplies. To maintain profitability, it’s essential for physician offices to ensure their payer contracts keep pace with inflation. By renegotiating contracts every 18 months, practices can better account for rising costs and maintain a more stable financial footing.
Insurance companies and other payers are continually seeking ways to cut costs and improve their bottom line. One common strategy is to reduce reimbursement rates for medical services over time. For example, Blue Cross Blue Shield, one of the largest health insurance providers in the United States, has a history of implementing rate reductions to control costs.

When payer contracts are not renegotiated regularly, physician offices may find themselves locked into agreements with steadily decreasing reimbursement rates. This can lead to significant financial strain, as practices struggle to maintain profitability while still providing high-quality care to their patients. By renegotiating contracts every 18 months, physician offices can ensure they are receiving fair and accurate compensation for their services, preventing the erosion of their revenue streams.
Retaining top talent is essential for any medical practice, as it directly impacts the quality of care provided to patients. With an increasingly competitive job market, the cost of retaining skilled and experienced employees has been on the rise. According to the U.S. Bureau of Labor Statistics, the median annual wage for healthcare practitioners and technical occupations increased by 2.7% between May 2020 and May 2021. This trend shows no signs of slowing down, making it more important than ever for
physician offices to offer competitive salaries and benefits to retain their best employees.
In order to maintain a talented workforce, physician offices must ensure their payer contracts provide sufficient revenue to cover the costs of competitive compensation packages. Renegotiating contracts every 18 months enables practices to stay ahead of market trends and offer their employees the financial incentives necessary to stay with the practice, ensuring the continued delivery of high-quality care to patients.
The importance of renegotiating payer contracts every 18 months cannot be overstated. With inflation steadily devaluing contracts over time, payers reducing rates to control costs, and the increasing expenses associated with retaining top talent, physician offices must stay vigilant in their contract negotiations to ensure the long-term success and stability of their practice. By maintaining updated and fair agreements with payers, physician offices can better manage their financial health and continue to provide the highest quality care to their patients.
Cameron Wood is the Head of Client Services & Chief Operating Officer at NGA Healthcare. NGA Healthcare specializes in negotiating reimbursement rates for providers of all specialties all over the country. They also offer ongoing credentialing services and ensure that groups receive fair market rates and guarantee their fees. www.ngahealthcare.com
Where: https://shop.namas.co/
Your Price: $199.00
Hundreds have attended NAMAS’ live events to become trained auditors and prepared for certification, and now you have access to the NAMAS Medical Auditing Resource Guide. The NAMAS Medical Auditing Resource Guide is designed to educate individuals in the field of medical auditing, as well as be a valued resource to auditors in day-to-day operations. For those individuals who are wishing to become a medical auditor, there is no better learning guide and tool. Remember that NAMAS is the original creator of the nationally recognized auditing credential.
Our standard method of delivery is electronic; upon purchase, you’ll receive a link to download the .pdf copy of the manual. Or, elect to have a printed manual shipped to the address provided on your order.
Your Price: $289.00
Where: https://training.rccsinc.com/Online-Store/Products
This industry-leading reference manual is one of Revenue Cycle Coding Strategies® most popular products, year after year. It provides comprehensive information about coding for radiation oncology services and is a must-have if you work in a radiation oncology practice, cancer center, or hospital radiation therapy department. The manual covers all phases of treatment from the initial visit to post-treatment follow-up, and all treatment modalities, including external beam, IMRT, radiosurgery, and brachytherapy. Each section of the manual discusses documentation requirements, coding guidelines, bundling issues, and coverage restrictions, as well as compliance issues such as physician supervision, clinical trials, standing orders, and ABNs.
Your Price: $199.00
Where: https://training.rccsinc.com/Online-Store/Products
This comprehensive and easy-to-use medical coding book is indispensable for compliance officers, administrators, billing managers, and anyone else involved in billing compliance for radiology services. It covers orders for diagnostic tests, physician supervision, documentation, reporting the date and place of service, ABNs, teaching physician services, IDTF rules, and much more. The coding book also tells you where to find federal laws and regulations related to billing compliance and how to evaluate your organization’s coding compliance program to make sure it is providing the protection you need.
Have a new product or want BC Advantage to list your company / products here?
Send us your information and interest to sales@billing-coding.com


In early February, members of the National Association of Freestanding Emergency Centers (NAFEC) went to Washington D.C. to meet with various members of Congress to gain support for two items: the continued recognition of Freestanding Emergency Centers post pandemic and for oversight of the No Surprises Act Independent Dispute Resolution process.
During the pandemic, Freestanding Emergency Centers (FECs) provided critical relief to the overcrowding of medical facilities across the state of Texas. This was made possible in April 2020 when the Centers for Medicare & Medicaid Services (CMS) issued guidance allowing independent FECs to provide care to Medicare and Medicaid beneficiaries during the public health emergency. Since this time, over 100 facilities across the state of Texas enrolled and became critical health resources within their communities. The current administration has determined that the public health emergency is no longer needed and set to expire on May 11, 2023. With that end, so does the recognition of FECs by CMS. Members of the NAFEC delegation met with members of the Texas delegation to Congress to stress how the loss of access to these facilities will impact the communities that they serve within their districts. In addition, the NAFEC delegation asked for bipartisan support for the Emergency Care Improvement Act (H.R. 8597), to be re-filed again this Congress, which would improve Medicare beneficiary access to emergency care in rural areas and improve access and competition in urban areas by providing permanent Medicare and Medicaid recognition of FECs.
Enacted in 2020, the No Surprises Act (NSA) was meant to protect consumers’ out-of-pocket liability for surprise medical bills when receiving out-of-network healthcare. Among other things, the bill established a federal independent dispute resolution process (IDR) to resolve out-ofnetwork payment disputes between providers and insurers. Unfortunately, the implementation of the NSA has not gone smoothly, and the IDR process is riddled with issues causing major delays in the IDR process, which is paying providers a fraction of their typical reimbursement, delaying payment, and putting routine claims into arbitration.
The NAFEC delegation has asked for more oversight of the
IDR process and the implementation of the NSA. The IDR process as a whole has already put a significant strain on many providers and the continued lack of clear guidance and oversight will continue to put patient access to critical emergency care at risk.
It is critical, no matter the type of practice, to continue to use the appropriate channels to bring visibility to these and many other issues. Only through united persistence can providers hope to make an impact. Please contact your representative today and show your support.
Matt Tamez, CPCO, CPB, is the Chief Operating Officer at Phoenix Coding & Consulting Services, a Texas-based coding company that works with many FECs across Texas. www.phoenixccs.com