UNIVERSITY OF ILLINOIS CHICAGO DEPARTMENT OF MEDICINE





We are proud to present our annual report for the Department of Medicine for 2021-22.
In the last annual report, we shared stories from the COVID-19 pandemic. Even though COVID-19 remains a constant in our lives, we have remained steadfast in our commitment to research, education, the care of all patients and ourselves. We continue to adapt to and triumph over changes as they unfold in the post-COVID era.
After 10 years leading our Department of Medicine, Patricia heads to the University of New Mexico (UNM) to serve as the fifth dean in the UNM’s School of Medicine 61-yearhistory. The department has thrived despite many challenges over these past 10 years, and I have been proud to serve alongside Patricia as vice head. I am honored to serve as interim head and will continue to lead the department by staying true to its mission to strive for excellence, innovation, and exceptional care for all.
As I look to the future, I will continue to be mindful of our departmental goals which include continuous improvement to reduce costs and improve efficiency while enhancing excellence in the areas of clinical, education, faculty affairs, scholarly activities, diversity and inclusion, and service to local and global communities.
As we all know, change is challenging. It’s only through change that we continually examine our mission, our values, and our goals as we look towards the future. I would like to thank everyone for their support of the Department of Medicine and each other.
Best, George T. Kondos, MD A. Tom Petropulos Professor and Interim Head Department of Medicine - University of Illinois Chicago
A. Tom Petropulos Professor and Interim Head Department of Medicine - University of Illinois Chicago


There are no words to describe what I am feeling as I write this note. I am eternally grateful for the opportunity to lead this spectacular department, and I am even more grateful for all your support these past ten years. While change is never easy for anyone, I am excited for this new chapter in my life.
It has been an honor to lead and serve you. We strove to integrate inclusion into all our missions: scientific discovery, exceptional care for all and finding our replacements as we train the next generation. With your input, we brainstormed at our retreats, developed goals that informed our councils, celebrated victories, embraced and overcame challenges, danced at unforgettable parties, and never forgot to breathe. I am proud of each and every one of you and all your accomplishments both large and small. This is not good-bye, this is see you soon.
Sincerely,
Patricia W. Finn, MD Earl M. Bane Professor and Head Department of Medicine - University of Illinois Chicago
Earl M. Bane Professor and Head Department of Medicine - University of Illinois Chicago
The University of Illinois at Chicago Department of Medicine (DOM) has a long tradition of providing thorough and comprehensive training in medicine. Since 1882, we have been moving academic medicine forward for the people of Illinois and beyond.
The Department of Medicine is the largest of 25 academic departments in the College of Medicine (COM). We are comprised of nine divisions, with faculty engaged in teaching, scholarly activity and patient care services.
OUR MISSION IS TO STRIVE FOR EXCELLENCE, INNOVATION, AND EXCEPTIONAL CARE FOR ALL.
The DOM is committed to stewardship in the communities it serves by providing high-quality and cost-effective patient care while increasing financial stability. We align with UI Health’s UI CARE (Compassion, Accountability, Respect, Excellence) values.
Our commitment to scholarly activity is essential to our overall mission. Germane to this concept is the naming of research and investigative activity as “scholarly
activity”. In recognition of the fact that collaboration and teamwork are essential to success, the DOM does not define roles as “research” or “clinical”, but rather enhancing scholarly activity for all DOM members whether trainee, faculty or staff.
The DOM plays a significant role in the education of medical students, internal medicine residents, and specialty fellows throughout their years of training.
Fundraising for the DOM has a renewed emphasis on both research grants and private philanthropy, engaging alumni, community leaders, residents, and faculty.
It is a pleasure to welcome you to our Annual Report that highlights the accomplishments of the Department of Medicine through high-quality clinical care, scholarly activity, and education. In this report you will find a detailed overview of activities that span 2021 and 2022 for all our department’s divisions. The report also includes faculty honors and awards, leadership biographies, division highlights, well as featured news stories on diversity, inclusion, and bias reduction. The COVID-19 pandemic again influenced our operations as we saw the persistence and adaptability of the SARS-CoV-2. Still, our clinical volumes rebounded and grew nicely across all areas while, at the same time, caring for significant numbers of patients affected by COVID-19. On behalf of the entire leadership team, I want to end by extending immense gratitude to our faculty, staff, partners, and friends across the institution: Thank you for all the ways in which you look after our community — and each other.
 R. Bryan Blaha, MS Director of Administrative Operations
R. Bryan Blaha, MS Director of Administrative Operations

Ece Mutlu, MD, MBA, MS, professor of medicine, was appointed chief of the Division of Gastroenterology and Hepatology. Dr. Mutlu received her medical degree from Istanbul University and trained in gastroenterology at Loyola University. She also earned an MBA from the University of Chicago. She has substantial expertise in all aspects of clinical and translational research as well as a vast background in management and leadership. She is a clinician-scientist with 18 years of experience who specializes in inflammatory bowel disease. Her diligent approach to patient care and safety has earned her top-physician awards. Dr. Mutlu is nationally and internationally known for her patient-oriented research studying nutrition and the intestinal microbiome. Her work has been supported by foundations and federal agencies. Dr. Mutlu serves on multiple advisory panels, conducts clinical trials, teaches, lectures, and publishes in the same fields.

George T. Kondos, MD, A. Tom Petropulos professor of medicine, was appointed as interim head of the Department of Medicine. Dr. Kondos has served as senior associate head of the Department of Medicine since 2017. He earned his medical degree from the Chicago Medical School. He completed his residency in internal medicine and fellowship in cardiology at the University of Illinois College of Medicine. During his four decades at UIC, Dr. Kondos has taken on multiple leadership roles for the Department of Medicine, the College of Medicine, and the University of Illinois Chicago. He previously served as Interim Head of the Department of Medicine from 2011-2012. Dr. Kondos has been instrumental in pioneering the use of coronary calcium imaging to detect early cardiovascular disease. He has participated and continues to participate in a number of NIH studies evaluating coronary calcium imaging in various patient populations. Additionally, Dr. Kondos is interested in the development of cardiovascular simulation using Harvey, a life-size manikin simulating over 60 cardiovascular diseases. Dr. Kondos’ clinical interests include coronary artery disease, valvular heart disease and lipid disorders.

Adam Mikolajczyk, MD, assistant professor of clinical medicine, was appointed program director for the Internal Medicine Residency program with his first academic year beginning in fall of 2022. Dr. Mikolajczyk earned his medical degree with honors from the University of Chicago Pritzker School of Medicine. He then completed Internal Medicine Residency, Gastroenterology fellowship, and Transplant Hepatology fellowship at the University of Chicago. During his chief residency year at University of Chicago, he also completed the Medical Education Research, Innovation, Teaching, and Scholarship (MERITS) fellowship. His research focuses on improving deficits in hepatology education in undergraduate and graduate medical training. He serves on several education-focused committees within hepatology and gastroenterology societies and is the lead faculty advisor for the Liver Fellow Network. Dr. Mikolajczyk has a deep passion for teaching, mentorship, and medical education research.

Department Head
Patricia W. Finn, MD
Administrative Operations Director
R. Bryan Blaha, MS Advisory Committee
Finance and Accounting Director
Maritza Delgado, MS
HR and Faculty Affairs Director
Michael Paprzyca, MBA
Information Technology Manager
Robert Rios
Research Operations Director
Maritza Delgado, MS
Business Development and Strategy Director
Karishma Parekh, MS
Associate Director of Clinical Revenue and Call
Caryn Riley, MSW Division
Assistant Director of
Institute for Minority Health Research
Martha Daviglus, MD, PhD - Director Angie Herrell - Administrator
Center for Dissemination and Implementation Science
Geri Donenberg, PhD - Director
Academic Internal Medicine and Geriatrics
Rachel Caskey, MD - Chief Ainoa Coltri - Administrator
Endocrinology, Diabetes and Metabolism
Brian Layden, MD, PhD - Chief Pam Terrell - Administrator
Hematology and Oncology
Damiano Rondelli, MD - Chief Onesima Martinez - Administrator
Nephrology
James Lash, MD - Chief Ted Ebersold - Administrator
Sr. Associate Head of Medicine
George T. Kondos, MD
Sr. Associate Head Strategic Programs
Jeffery Jacobson, MD
Head’s Office Administrative Staff
Cardiology
Dawood Darbar, MD - Chief
Daniela Nita - Administrator
Gastroenterology and Hepatology
Ece Mutlu, MD - Chief
Alejandra Moore - Administrator
Infectious Diseases
Richard Novak, MD - Chief
Ted Ebersold - Administrator
Pulmonary, Critical Care, Sleep and Allergy
Steve Dudek, MD - Chief
Alejandra Martinez - Administrator
Rheumatology
Nadera Sweiss, MD - Chief
Beena Mathew, MHA- Administrator
Department Councils
Scholarly Activities
Waddah Alrefai, MD
Geri Donenberg, PhD
Paul Grippo, PhD
Jeff Jacobson, MD
James Lash, MD
Irena Levitan, PhD
Jun Ma, MD, PhD
Conner Olsen, MD - Resident
Aamir Twing, MD - Resident
Claire Shin, MD - Resident
Krystle Stewart- Coordinator
Faculty Affairs
Joan Briller, MD
Michael Fischer, MD
Min Joo, MD
Claudia Lora, MD
Jun Sun, PhD
Michael Paprzyca
We are committed to stewardship in the communities we serve by providing high-quality and cost-effective patient care. We are fully engaged on all fronts with the University of Illinois Hospital and Health Sciences System (UI Health) to expand clinical programs. Our commitment to addressing community needs goes well beyond the traditional service role of an academic medical center. We advocate for reducing health disparities, which requires a multidisciplinary, collaborative approach to the inequities in healthcare access and quality of care.
To maintain and enhance the clinical mission, the DOM appointed Dr. Ece Mutlu to lead the division of Gastroenterology and Hepatology. Dr. Adam Mikolajczyk was appointed program director of the Internal Medicine Residency program and Dr. Anne Polick was appointed deputy director of the Internal Medicine Residency program. Division chiefs oversee the clinical activities, education, and scholarly activities of their division. Internal Medicine leadership oversee the Residency Training program and resident activities.
The DOM regularly conducts outpatient meetings with clinic medical directors, clinic directors, staff, division chiefs, and DOM business administrators. These meetings have resulted in the coordination of activities among the DOM clinics, improvements in services and the formation of new clinical programs which we invite you to learn more about within our division profile pages.

In June of 2022, Dr. Jonathan Radosta, associate professor in the Division of Academic Internal Medicine was appointed Interim Chief Medical Officer (CMO) for the University of Illinois Hospital and Clinics. Dr. Radosta has served UI Health in a number



of leadership roles focused on improving patient care and quality, patient and physician satisfaction, and clinical financial performance, including as the Clinic Medical Director for Primary Care Plus/Internal Medicine and the Senior Medical Director for Managed Care. As Co-Chief Medical Information Officer for Epic Implementation, Dr. Radosta spearheaded changes across the UI Health enterprise to improve the patient experience and clinical workflows through a new unified electronic health record and financial system. Dr. Radosta completed his residency at the University of Illinois Chicago and served as Chief Resident. His clinical interests include quality improvement and population health research. Dr. Radosta is the Assistant Dean for Clinical Affairs in the University of Illinois College of Medicine. He has been instrumental in the leadership of many initiatives aimed at substantial process improvements and infrastructure activation.
University of Illinois President Tim Killeen honored seven UI Health leaders with the Presidential Medallion, an award given to recognize individuals who support and bring distinction to the University of Illinois System, as part of the system’s COVID-19 response. The Presidential Medallion is the highest honor that the system president can bestow. Killeen honored leaders of clinical trials for COVID-19 vaccines at UIC, which were the first trials conducted in Chicago, and UI Health’s mass-vaccination effort that inoculated University of Illinois Hospital & Clinics staff, patients, students, faculty and, so far, tens of thousands of members of the public. Three of the seven awardees are members of the DOM. Dr. Susan Bleasdale, chief quality officer, Dr. Jerry Krishnan, associate vice chancellor for Population Health Sciences, and Dr. Richard Novak, chief of the Division of Infectious Diseases.
A new state-of-art Specialty Care Building (SCB) on the UI Health campus opened to patients in September 2022. Located in the heart of the Illinois Medical District, the SCB is a new home for expert care and same-day surgery. The building includes six floors of patient care space with eight operating rooms and 24 pre-/post-surgery bays. It also includes 182 clinic rooms for Gastroenterology (GI), Ophthalmology, Otolaryngology, Transplant, Urology care, and a pharmacy. The building is projected to serve 600 to 800 patients per day and perform 8,000+ surgeries and 8,000+ GI procedures annually.
The new building features new technology and functionality for an improved patient experience, from check-in kiosks to valet parking and intuitive wayfinding.
The UI Health 55th & Pulaski Health Collaborative provides comprehensive healthcare services for the residents of Chicago's Gage Park and West Elsdon communities. The TARGET Health Collaborative Partnership brings together seven community partners committed to transforming the health of these neighborhoods by expanding care services, improving patient outcomes, and reducing health disparities.
This collaboration has increased access to specialty care provided by the Department of Medicine in Cardiology, Diabetes and Endocrinology, Gastroenterology, Nephrology, Oncology, Pulmonology, and Rheumatology as well as care coordination to ensure adequate support through the care journey.

The American Heart Association/American Stroke Association recognized UI Health for our commitment to providing effective stroke and heart failure care using the most advanced procedures available. UI Health was awarded the Get With The Guidelines®–Target: Stroke Honor Roll Elite Plus and Advanced Therapy — the highest level of recognition from the AHA/ASA — and UI Health was awarded the Get With the Guidelines® — Target: Heart Failure Gold Plus Quality Achievement Award. This is the sixth consecutive year UI Health has received the top stroke award and the fourth consecutive year it has achieved the heart failure designation. UI Health also was recognized and awarded the Get With The Guidelines® Resuscitation Bronze Award.
The Cardiology program at UI Health was awarded the Mission: Lifeline® NSTEMI Gold and Mission: Lifeline® STEMI Receiving Silver awards for meeting care criteria guidelines for ST-elevation myocardial infraction (STEMI), a serious type of heart attack, and non-ST-elevation myocardial infraction (NSTEMI), which involve blockage of the coronary arteries.


The University of Illinois Hospital was featured in hospital rankings from U.S. News & World Report. Six service areas were included in the U.S. News Best Hospitals 2021–2022 list. The following services were listed as “High Performing”: Heart Failure, Heart Attack, Kidney Failure, Stroke, Chronic Obstructive Pulmonary Disease and Pneumonia.


The response throughout all corners of UI Health and the Department of Medicine has truly been unprecedented. It is humbling to consider where we began in March of 2020 and how far we have come together. Through the chaos of successive variants and waves, our department members found new ways to pivot and counter pandemic barriers while delivering exceptional care for the people of Illinois. We began fiscal year 2021 hopeful that we could continue the department’s upward trajectory in clinical activity. Volumes normalized in the fourth quarter of 2021 across all specialties; returning to pre-pandemic levels in the first quarter of 2022. We continue to experience significant growth fueled by added volumes due to COVID-19 pandemic as well as expanding our clinical footprint with the successful opening of University Village Primary and Specialty Care and 55th & Pulaski Collaborative Health clinics.
HOSPITAL DISCHARGES

INPATIENT PROCEDURES




Nineteen of the Department of Medicine physicians were named among the region’s top physicians by Castle Connolly, the consumer healthcare guide. Physicians were nominated by peers in a nationwide survey, then chosen by a physician-led research group. Our physicians were featured in Chicago magazine’s January 2022 ”Top Doctors” list.



















The COVID-19 pandemic put enormous strain on the hospital, physician group, staff, and ancillary groups. Our shared UI Health COVID-19 journey has taught us the importance of collaboration, dynamic surge and staffing models as well as the need to use technology to extend our specialists across a larger inpatient census.
The entire ID faculty continued to be engaged in the response to COVID-19. Dr. Susan Bleasdale, as director of infection control, and chief quality officer for UI Health, with the assistance of Dr. Scott Borgetti, assistant director of infection control, continues to lead the medical center at large on policy changes to the evolving pandemic. While the routines in the medical center continue, they have worked tirelessly behind the scenes to keep up with changes in infection control guidelines and treatment practices.
Dr. Susan Bleasdale continued to be a key consultant to the Illinois Department of Public Health (IDPH) and continued to work with university leadership providing guidance on how to keep campus activities open and safe.
The city's Strike Team response to outbreaks in homeless shelters, long term care facilities and other congregate settings in collaboration with the College of Nursing was led by Dr. Stockton Mayer. Dr. Mayer’s team was awarded a new contract with Chicago Department of Public Health (CDPH) that will expand testing and vaccination beyond COVID-19. The University will serve as a community-based outbreak response team, investigating outbreaks of influenza, legionella, candida auris, and other pathogens.
Dr. Scott Borgetti helped develop and implement the clinical program for COVID-19 outpatient management, which continues to evolve as new treatments come on line, and provides guidance to the treatment team.
In addition to providing clinical, organizational and policy leadership, infectious diseases faculty continued to move the coronavirus research agenda forward.

Dr. Richard Novak, chief of the division of infectious diseases, became an investigator for the Coronavirus Prevention Network and leads the ongoing Moderna COVID vaccine trial, and the Janssen Ensemble vaccine trial. Dr. Novak collaborated with OB/GYN and pediatrics on the Momivax study to understand vaccine effects on both pregnant women and their newborn children.
Dr. Borgetti leads the CPAT study of vaccine booster doses in organ transplant recipients. All members of the ID faculty as well as fellows contribute to the research effort, evaluating study participants and conducting study visits. Any time not committed to clinical work or committees are devoted to these research efforts. Dr. Novak was honored this year by the dean with a Distinguished Service Award. Drs. Novak, Bleasdale, and Jerry Krishnan were honored by the University of Illinois President with the Presidential Medallion award.

In June 2021, a new Post-COVID Clinic began seeing patients at the University Village Primary & Specialty Care Clinic and the Outpatient Care Center. The multidisciplinary clinic for COVID-19 long haulers, patients who previously had COVID-19 and still experience long-lasting symptoms, brought together a variety of specialties — primary care, pulmonology, nephrology, neurology, immunology, and rheumatology. Unique to the clinic is the critical role of the patient care navigator who coordinates a patient’s care across specialists and assists with activities like appointment scheduling. Our physicians are dedicated to helping patients manage their chronic symptoms as a result of COVID-19.
The Division of Nephrology faced unique challenges posed by the Omicron surge. Not only was there an increased demand for in-patient dialysis services due to the influx of critically ill patients, but the division faced critical staffing shortages. Working closely with hospital leadership and Infection Control, Dr. Claudia Lora (medical director of the Dialysis Unit) and Mary Ann Medina, RN (director of Patient Care Services for Dialysis) addressed these challenges by coordinating a successful multidisciplinary effort which included nephrology faculty, fellows, as well as dialysis technicians and nurses.
The COVID-19 pandemic offered numerous challenges


which required the Division of Gastroenterology and Hepatology staff to adapt the way we provide patient care and also the way we interact with each other. One of the highlights of the calendar year was the fellows graduation, which takes place every June and typically includes a celebratory dinner and speeches. In 2020, the division resorted to a backup plan by Zoom meeting, which was still sentimental but understandably muted.
This past June saw the return of an in-person ceremony for graduating fellows Mitali Agarwal, Najib Nassani, and Dino Melitas. Using masks, socially distanced seating and boxed meals, we were able to combine appropriate precautions (at the cusp of the onset of the Delta variant), with a shared space which allowed us to more properly celebrate the accomplishments of our
departing trainees.
During a time of unprecedented change in the world around us, the DOM APP’s have met this change with professionalism and resilience. In the face of the pandemic, our APP’s have stepped up to meet the issues facing all providers, from extending your clinic practice, staffing the vaccine clinics, moving to telehealth and rounding on the inpatient medicine teams. We had another year of growth, as we continued to add APP’s to the DOM to expand clinical practice and develop new programs.
Left to right: Dr. Aaron Young (fellow), Dr. Jerrold Levine, and Mary Medina, RNIn the midst of one pandemic, the Outbreak Response Team, co-led by Stockton Mayer, assistant professor in the UIC College of Medicine and UIC Nursing assistant professor Rebecca Singer coordinated a mass vaccination event that provided nearly 1,200 people with monkeypox vaccinations at UIC in August 2022.
Through a partnership with Rush University and UIC, a team of 90 people was formed, many of whom were volunteering their time.
The Outbreak Response Team is an extension of the COVID Rapid Response Team, which was formed to provide testing and vaccinations in high-risk and underserved parts of Chicago.
The Fellow of the Year personifies the core values of UI Health: Compassion, Accountability, Respect, and Excellence. These physicians put their patients first in all encounters and consistently contribute to the delivery of world class patient care.
Dr. Christen Vagts is the ultimate example of what it means to live up to our clinical mission in everyday work. Dr. Vagts spent several weeks directly caring for our sickest COVID-19 patients. During the most difficult and grueling clinical work, she served on the front line in an environment that posed significant risk to our providers. She cared for patients with this lifethreatening illness — one we did not fully understand, had limited ability to treat, and at the time, very limited PPE — with leadership and excellence. She took on extra clinical obligations, and because of her leadership we were able to deliver the highest levels of patient care and provider safety.
Dr. Vagts is an exemplary fellow who has demonstrated a high degree of passion for her work, including a dedication to her dual roles as educator and clinician. She has the promise of a remarkable career going forward.

Over the last 31 years, Dr. George Kondos, professor and interim head in the Department of Medicine, has taught thousands of first-year University of Illinois Chicago medical students how to perform the cardiovascular physical exam using a highly advanced simulator who goes by the name Harvey.
Dr. Kondos typically conducts the teaching sessions inperson, but with COVID-19, these in-person teaching sessions needed to be converted to virtual teaching sessions. This was not an easy task since heart sounds and other subtle physical exam findings need to be displayed so students would understand the difference between a normal patient and a patient with one of the various cardiac diseases.
Harvey is a lifesize manikin able to simulate 50 different cardiovascular diseases through heart sounds and lifelike pulses in the neck and chest. It serves as a simulator for students to be able to hear sounds mimicking various diseases and feel the pulse that would correspond to these diseases.
“You can give 20 common heart sounds and murmurs to primary care physicians and they’ll get about 10% of them correct, and that’s because they’ve never been really taught how to listen to the heart sounds,” said Kondos.
Comparing Harvey to airplane simulators that have taught pilots how to react to events in the air from the safety of the ground, Dr. Kondos said Harvey is used to train young doctors how to assess and treat a patient by simulating conditions a new doctor would confront bedside with a patient.
Normally, Harvey would join Dr. Kondos as he traveled to the College of Medicine’s Peoria, Rockford and UIC campuses, where he would teach more than 300 students yearly. Prior to the pandemic when he would have had to drive to each of the campuses, he would give the same lessons independently to the students on each of the campuses. He previously conducted the sessions surrounded by the students, who would break out into small groups.
Since COVID-19 forced teaching to go virtual, Harvey, which was developed by UIC College of Medicine Class of ’61 alum Michael Gordon, also has was forced to do its teaching online.
“Obviously COVID made a little bit of a problem for us, but we converted it from an actual in-person course to an online course,” said Kondos. “I ran them through the normal physical and gave them findings of the abnormal physical exam.”
Kondos used Harvey to simultaneously teach more than 300 students — 182 in Chicago, 55 in Rockford and 66 students in Peoria — who took part in an online cardiology plenary course introducing them to the cardiac exam.
He did this by using various examples that students could see virtually; for example, he used cotton swabs to dramatize the strength of the carotid pulse by laying the stick of the swab flat across Harvey’s neck as the pulse sent the stick and swab tip moving up and down

along with the sound of the pulse.
“Even though you don’t have the actual patient here, you can simulate to students what they are actually seeing and hearing and can show students various examples of disease states,” Kondos said. “We all recognize simulators are no substitute for a real patient. However, if you can’t make the diagnosis on a simulator you probably would miss the diagnosis on a real patient.”
One of the benefits that happened with them having to go online is that it allowed it to become more manageable.
“Many times these class sizes are so big that everybody can’t really see everything and these are subtle kinds of things that you’re showing,” Kondos said. “So with Harvey, it’s actually helped because here the students can see, they can hear — probably better than they can in a large group — and you can engage them in discussion.”
The DOM plays a significant role in the education of medical students, internal medicine residents and specialty fellows throughout their years of training.

DOM faculty actively participates in training approximately 200 M1, M2, M3 and M4 students. Dr. Asra Khan is the course director and Dr. Ananya Gangopadhyaya is the associate course director for the M1 and M2 Doctoring and Clinical Skills (DoCS) course formerly known as Essentials of Clinical Medicine (ECM). The course provides instruction on basic and advanced communication and doctoring and clinical skills. Students work in small group settings to develop their skills in the systematic interviewing of patients with varying medical and psychosocial conditions, learn physical exam skills, clinical reasoning, how to present and write patient histories and to work collaboratively with peers. In addition, to serving as working group tutors, numerous DOM faculty members also participate in the Introduction to Patient Care program, Physical Exam and Communication workshops and as Hospital Immersion Tutors.
Drs. Fred Zar and Pavan Srivastava serve as the synthesis course directors. This 18-month longitudinal course allows students to see how their basic science knowledge facilitates care of patients. Class sessions focus on cases that illustrate the interdependence of the organ systems studied to date and the management of complex, multi-system diseases.
Drs. Radhika Sreedhar, Ananya Gangopadhyaya, Anne Polick, Mahesh Patel and Waddah Alrefai serve as block leaders during phase 1 of the curriculum. In addition, Dr. Sreedhar was recently named director of curricular integration.
Drs. Khan and Gangopadhyaya serve as the M3/M4 Internal Medicine clerkship directors and associate clerkship directors. Dr. Khan is also an active member of the College of Medicine Education Coordinating Committee (ECC). The ECC sets the learning objectives, program evaluation and student assessment for the M3 medicine clerkship. This clerkship is the highest rated M3 experience on the AAMC survey for two years as well. Approximately half of the M4s interact with members of the DOM in every division while doing their medicine sub-internship or electives in subspecialty internal medicine divisions. Numerous DOM faculty participate in COM Essentials of Clinical Practice and Professionalism (ECPP) course which acts as a bridge between medical school and residency covering numerous important educational topics.
Dr. Alana Biggers serves as the sub-theme lead in Population Health. She is responsible for integrating population health topics into the curriculum including how to approach population health outcomes, social determinants of health, and clinical considerations for underserved populations.
We train 119 residents in our Preliminary and Categorical Internal Medicine (IM) Residency programs in addition to training 16 Medicine/ Pediatrics residents, 15 Emergency Medicine/Internal Medicine residents and 6 Neurology interns during the 20212022 academic year. In addition, the Department of Medicine sponsors 14 subspecialty fellowships. All totaled, there are 256 trainees in our programs. All the residencies and fellowships are fully accredited by the ACGME and none of them have any citations.
Dr. Fred Zar has been the program director for over 2 decades and has trained over 800 residents in his career. He has received numerous awards from the University of Illinois College of Medicine which include a 3 time recipient of the C. Thomas Bombeck MD Award for Excellence in Medical Education, 6 time recipient of the Alpha Omega Alpha Outstanding Faculty Award and 14 time winner of a Golden Apple for Excellence in Teaching. The residents have selected Dr. Zar as the Attending of the Year award 16 times.

The Internal Medicine Residency program is supported by 6 associate program directors: Drs. Christopher Fernandes, Patrick Godwin, Anne Polick, Adam Mikolajczyk, Robert Sargis, and Alfredo Mena Lora.
Dr. Christopher Fernandes completed his internal medicine residency at the University of Chicago. After completing a chief residency he returned to UIC, where he had been a medical student, to become a hospitalist. Dr. Fernandes was promoted to associate program director in 2021 and became the director of the Hospitalist Service at UIH in 2022.

Dr. Patrick Godwin has been a faculty member since 2001 and became section chief of Hospital Medicine
at the Jesse Brown VA Medical Center in 2008. He was promoted to associate chief of staff for quality in 2021. Dr. Godwin's interests include clinical teaching, quality improvement, patient safety, health system reform, and telehealth.
Dr. Anne Polick was an internal medicine resident and chief resident at UIC and is an academic internist teaching in the General Medicine Clinic, Clinical Decision Unit and the General Medicine Wards. She was awarded the New Attending of the Year award her first 3 years as an attending and also the Attending of the Year award on 4 occasions.

Dr. Mikolajczyk completed his internal medicine residency at the University of Chicago where he was also a chief resident. While there he completed fellowships in Gastroenterology, Transplant Hepatology, and Medicine Education. He joined the faculty in 2018 and has since won the New Attending of the Year award his first year and the Attending of the Year award 3 times since.


Dr. Rob Sargis completed his internal medicine residency and Endocrinology fellowship at the University of Chicago. He is the director of our Physician Scientist Development Program that leverages the immense and diverse resources at UIC to create future leaders in academic medicine and has matched numerous physician-scientists into our IM Residency and subsequent fellowships at UIC.
Dr. Mena Lora was an internal medicine resident, chief resident, Infectious Diseases fellow and became the program director of our Infectious Diseases fellowship in 2020. He is an active member of our Department of Medicine Diversity and Inclusion Committee and has been instrumental in our institution’s response to the COVID-19 pandemic.


For 2022 Internal Medicine Residency Match, 108 DOM faculty interviewed 804 applicants to successfully fill all 46 of our PGY1 positions. Our positions were filled at the highest level of our match list since 2013. 22% of the students were from UICOM, 11% were from other Chicago schools, 60% from US programs outside of Chicago and 7% from international schools. We continue to increase our diversity. This year 49% of the Categorical Internal Medicine interns are students that are underrepresented in medicine.


In 2021, the IM Residency achieved a pass rate of 91% (32/35). Prior pass rates are shown below. We remain at a very competitive 3-year rolling pass rate of 96% (93/97) and 6-year rolling pass rate of 97% (188/193).
Year Pass/Total (%)
2016 32/32 (100%)
2017 30/30 (100%)
2018 33/34 (97%)
2019 28/29 (97%)
2020 33/33 (100%)
Last year 17/20 (85%) successfully entered the subspecialty of their choice. The mean distance down their match list they went to match was 1.6, thus the average resident matches at his/her first or second choice. The last 4 years having the match rates of 26/27 (96%), 19/21 and 20/21 matching, 26/27 (96%) resulting in a 5-year success rate of 108/116 (93%).

The DOM is training clinicians in internal medicine to serve the people of Illinois and beyond. It is also essential to train the next generation in academic medicine, i.e., “finding our replacements”. The newly formed residency tracks, described on the next page, and diversity and inclusion initiatives are contributing toward this goal.

The DOM developed and maintains a database of scholarly activities including all divisions. Trainees at all levels can search the database to identify potential faculty mentors and available scholarly activities to participate in. The website providing an interface to search the database also includes additional information on mentoring, starting a research project, presentation, innovations, various tools and resources, and a list of frequently asked questions.
The DOM sponsors 4 tracks within the Internal Medicine Residency to enhance residents’ experiences.
The Academic Internal Medicine Residency Track provides additional academic training to internal medicine residents who have an interest in conducting clinical research as generalists. The AIM Track is an opportunity for residents to receive training in public health and clinical and translational research, and actively participate in scholarly activities under the mentorship of DOM faculty. This track provides experience in various areas including clinical epidemiology and population health, behavioral science, public health, medical informatics, health interventions, research methods, health economics, and health services research. Since its inception, 4 years ago, the program has supported and trained 10 residents.
Quarterly didactic sessions are available in conjunction with the Center on Global Health on conducting and presenting research (e.g., study design, ethics and literature search).
In addition, formal mentorship to support research is provided and the opportunity for applicants to obtain a certificate through the School of Public Health (e.g., Health Disparities or Medical Informatics).
Overseen by Dr. Robert Sargis, the goal of our Physician-Scientist Development Program is to train the next generation of physician-scientists by providing an intensive multi-year commitment that combines both residency and sub-specialty fellowship training along with training and mentorship in the formulation of scholarly work and successful grant programs. Our overall mission is to develop outstanding clinician-scientists who will become highly successful investigators on our faculty and at medical schools across the country.
The Urban Global Health Track provides training to internal medicine residents who have an interest in pursuing health equity, locally and internationally. The goal of this track is to enhance awareness and knowledge regarding delivery of health care to vulnerable populations and to provide research opportunities and mentorship at both local and global levels. Under the leadership of Drs. Max Brito and Stockton Mayer the program has continued to match 4 applicants each year into this track which provides additional training in urban (Chicago) and international medicine.
This track provides monthly didactic sessions, journal clubs, clinic opportunities in our HIV community clinics, international experience in the Dominican Republic, India, Guatemala along with local experiences including our Needle Exchange Van, HIV Community Clinics, and outreach to Chicago youth.
The Innovation in Internal Medicine Track is our newest residency track and we were the first DOM to sponsor one in the country. Initiated by Drs. David Perkins, Jalees Rehman, and Ben Gerber, this three year track trains residents in R programming, provides monthly didactic sessions, journal clubs and allows residents protected time to work on technology and creating intellectual property. Our goals are to offer opportunities through research collaborations across all schools and departments at UIC, stimulate the development of novel ideas, practices, and products, and tailor experiences for those with advanced degrees and extensive research experience.
Amina Basha, MD Chief Resident: Research and Education


I was born and raised in Lake Forest, IL and would have been an Illinois lifer if it wasn’t for my undergrad experience at MIT and brief stint in Seattle, WA. After traveling to both coasts, medicine brought me back to my roots in Chicago, and I’m very glad it did. I was fortunate to go to medical school and then residency at UIC, where the diversity in patient population and cases has helped prepare me for future clinical practice. I wanted to stay on as chief resident because the people at UIC shaped the type of doctor I am today and I wanted to give back to the program as much as I could and help incoming trainees as well. I hope to pursue a fellowship in Endocrinology after chief year. During my time away from the hospital you’ll find me playing or reading with my 4-year-old son, Zain.
Brian Borah, MD Chief Resident: Ambulatory
As a member of a Chicago-based family that includes seven children and dozens of first cousins, I have always felt most comfortable in large groups of passionate people who thrive in active environments. It is no surprise, then, that UIC has felt like a second home to me. Not only has UIC given me friends and mentors for life, but it has also molded me into a confident physician who is committed to addressing health disparities both here and abroad. Through the Urban Global Health track, I have researched barriers to HIV care in Guatemala and have fostered collaborations to address the opioid epidemic in Chicago. Outside of the hospital, you can find me jogging on the 606, exploring jazz venues around the city, and obsessively baking sourdough bread. Next, I plan to pursue a fellowship in infectious disease.
Ashley Darlington, MD Chief Resident: Jesse Brown VA Medical Center
I knew I wanted to train at UIC after my interview day because of the diverse patient population we serve and the coveted autonomy praised by the residents. Three years later, I've had the privilege to learn more than just medicine from the brilliant faculty, fellows, and peers during my time at UIC. I chose to stay and serve as a Chief Resident to help residents reach their most excellent potential. After Chief Residency, I plan to pursue a Cardiology fellowship. In my free time, you can find me chasing after my son or listening to the latest popular podcast for future clinical practice.
Sanket Gokhale MD Chief Resident: Quality Improvement and Patient Safety
I’m originally from the northern suburbs of Chicago and earned a pharmacy degree prior to attending medical school. When not in the hospital I enjoy Netflix, the NBA and spending time with family. UIC was my first choice for residency and I have thoroughly enjoyed my last three years here.
Gabriel Marrero-Rivera, MD Chief Resident: University of Illinois Hospital

Being born and raised in Puerto Rico, moving to Chicago for residency was challenging. Nonetheless, from the moment I came to UIC, seeing the opportunity to care for such diverse patient populations and the amazing camaraderie among residents and program leadership made the transition effortless and gratifying. Also, being in the heart of the multicultural city of Chicago brings activities, hobbies and new discoveries to your life that enrich you as medical residents. My time as a resident in UIC has been filled with many experiences that have shaped me as a professional physician and I will cherish forever throughout my training and career. I chose to stay as chief resident in UIC as an opportunity to help others develop into excellent physicians and leaders of the future as well as assisting all to reach their utmost potential. After chief residency, I plan to apply for Gastroenterology fellowship. During my free time, I like cooking, eating at new restaurants, running, playing tennis, or playing some piano/guitar.

Isaye Barton, MD Chief Resident: Ambulatory

After my interview day at UIC, I knew that I wanted to train here for residency. The passion for working with patients from historically underserved populations, the camaraderie amongst residents and unique educational opportunities were all apparent after just one day. These features of UIC have been present throughout my training and have helped me begin to develop into the physician I dream of becoming. I decided to remain as a Chief Resident to continue making improvements to our program and support residents during a pivotal phase of their career. I hope to pursue Endocrinology fellowship next year. When I’m not in the hospital, you can usually find me at a new restaurant with friends or watching Netflix with my cat.
Marco Colamonici, MD Chief Resident: Quality Improvement and Patient Safety
I was born in Chicago and raised in Memphis TN, but have always had family roots in the Windy City. I moved up North to Champaign-Urbana in Illinois for college and stayed in the U of I system for medical school here at UIC. When it came time to choose residency, I decided to stay at UIC because I wanted to continue focusing my time on the diverse patient population that we serve. I wanted to stay on as a Chief Resident so I could give back to the institution that has taught me how to provide multidimensional care for patients. In my free time, you can find me smoking barbecue, fly fishing, and hanging out with my dog.
Jina Kwak, DO Chief Resident: Jesse Brown VA Medical Center

UIC has an institutional mission to serve the community, and this culture of service is what attracted me most to the program. Our residents are deeply invested not only in training to be excellent physicians, but work tirelessly to improve the system we work in. I am excited to serve as a Chief Resident to support our residents in every way possible and act as a vehicle in actualizing their goals and ambitions. I grew up in the north suburbs of Chicago (hey Libertyville!) and spent my college years in Boston before returning to my beloved home of Portillo’s. Following Chief year, I plan to pursue a career as an academic hospitalist. Outside of medicine, I am an avid podcast listener, enjoy time with family and friends, and spend a (slightly) unhealthy amount of time planning what to eat next.
Conner Olsen, MD Chief Resident: University of Illinois Hospital

I was born and raised in Northbrook, IL and consider myself an Illinois lifer having attended the University of Illinois at Urbana Champaign for undergrad and UIC for medical school. At UIC, I found a home where I matched for residency and now serve as Chief Resident of the University Hospital. I chose to stay on as a Chief to continue serving our amazing patient population, advocate for my co-residents, and assist them in their quest to become excellent, well-rounded physicians. While not at the hospital, I love to hang out with my co-residents, meditate, and play intramural sports. Next, I plan to pursue a fellowship in Palliative Care.
Aamir Twing, MD Chief Resident: Research and Education

Having grown up on the east coast of the US, I was drawn to Chicago and UIC in particular for the camaraderie exhibited by the resident community that was so prominently evident on interview day. As I progressed through my training here, it was abundantly clear that the internal medicine residents truly viewed each other as family, an attribute that has made my experience here more than worthwhile. This sense of community and cohesiveness has only been surpassed by the rich diversity of our patient population and resident commitment to research, education, and innovation. I decided to stay on as chief resident because I wanted to continue to help residents develop as clinicians and provide them with as much support as possible in their career paths. After chief residency, I hope to pursue a fellowship in Cardiology. In my free time I enjoy hiking with my wife and looking for the next big wilderness expedition!


CHIEFS: 2020-2021
Basha, Amina
Borah, Brian
Darlington, Ashley
Gokhale, Sanket
Marrero-Rivera, Gabriel
CHIEFS: 2021- 2022
Barton, Isaye
Colamonici, Marco
Kwak, Jina
Olsen, Conner
Twing, Aamir
PGY -1
Abraham, Kristy
Acaba-Berrocal, Luis A. (Ophtho)
Al-Khaled, Tala (Ophtho)
Alverio, Jonathan
Ambalavanan, Manoj
Aronov, Avi
Babwah, Amaara
Bahia, Jaspreet (P)
Beam, David
Bliley, Roy (P)
Brett, Rachel
Bundy, Jonathan (Neuro)
Carleton, Lena (IM/EM)
Chelebian, Hovig (P)
Desai, Kevin V.
Diamond, Sarah M. (P)
Dulle, Abygail (P)
Eisenberg, Amy (IM/EM)
El-Saied, Mohammad U.
Faraji, Farshid (P)
Fernandes, Nayson (Neuro)
Freij, Laith (Neuro)
Gilani, Mehul
Glait, Lyall
Gorski, Michal
Horowitz, Joseph (M/P)
Houshyar, Samin
Janike, Katherine
Jeffers, Johnathan (Ophtho)
Khan, Amir
Koplowitz, Jake
Krule, Alexander
Kumar, Ashwath S.
Kwak, Daniel (P)
Love, James
Luebs, John
Luo, Jerry (M/P)
Lynch, Connor (P)
Massengill, Michael T. (Ophtho)
Mirza, Miriam (Neuro)
Montes Rivera, Monica
Nagaraj, Suraj
Padmanabhan, Manoj (Neuro)
Parker, Paul R. (Ophtho)
Perez, Madelyn (M/P)
Pham, Ha H. (P)
Punal, Natalie M.
Raju, Prianka
Ramadan, Amina (IM/EM)
Santiago Cruz, Miguel (Neuro)
Shah, Love M. (P)
Shanker, Anita (M/P)
Shi, Kevin X.
Song, Minhyuk M.
Sreepathy, Pranati N.
Thermozier, Stephanie (Ophtho)
Tompkins, Sean (PhysSci)
Torres, Guadalupe (P)
Truong, Minh Chau
Vedak, Shivam C.
Weinfeld, Michael S.
Whitehead, Aldon J.
Yang, James J.
Yellen, Meredith C.
Zayyad, Zaid A.
Ali, Mansoor
Baghikar, Sara (PhysSci)
Bricknell, Ryan
Castillo, Brianna
Cho, Ha Young
Cho, Nicole
Cohen, Jeffrey (M/P)
Danley, Adam
Fernandez, Katia
Gallagher, Colin
Gartmond, Tori
Giuliani, Adriana (M/P)
Hsueh, Jessica (M/P)
Jain, Roshni
Jarman, Alan
Jarsania, Dhairya
Khan, Mahir
Kim, Catherine
Konold, Anthony
Langer, Tessa Marie
Vaughn (Lebert), Ariel
Manansala, Michael
Montgomery, Maureen
Nasrollahi, Farrah (IM/EM)
Patel, Brij
Rebhun, Jeffrey
Sanchez, Julienne
Sandhu, Sukhindervir
Shanker, Erin (PhysSci)
Shin, Claire
Solans, Christine
Sun, Tianlin
Taylor, Jeffrey
Uraizee, Aisha (M/P)
Webb, Adam (IM/EM)
Wenk, Arianne (IM/EM)
Wu, Johnny
You, Tian
Zhu, Hobart
Barton, Isaye
Blessing, Paul (IM/EM)
Caldwell, Jillian
Calero, Humberto
Cardona-Matos, Zulma
Casalegno, Maria Laura
Cheng, Renee
Chow, Kevin
Chung, Nakia
Colamonici, Marco
Collons, Danielle
Cooper, Paul (M/P)
Dwyer, Ryan (IM/EM)
Edwards, Tyler
Fang, Jiali
Genco, Matthew
Gildersleeve, Robert
Goldenberg, Benjamin
Gonzales, Janae
Hudak, Meghan (M/P)
Jindia, Jonathan
Joseph, Augustin
Kang, Ian
Khorsandi, Pedram
Kwak, Jina
Kwok, Alyssa
Lee, Kevin
Mehta, Vivek
Molinary Jimenez, Luis
Niroumandpour, Mike
Olsen, Conner
Pagan Pirallo, Patricia
Pagani Lopez, Wilfredo
Rivera Matos, Lucia
Rodriguez-Rivera, Yolanda
Simon, Erik
Singh, Avani
Stobierska, Dorota (IM/EM)
Swanson, Charles (M/P)
Twing, Aamir
Wei, Monica
Xie, Xiangyu
PGY - 4

Cheng, Lily (IM/EM)
Flores, John (Jack) (M/P)
Haemer, Zoe (M/P)
Hodge, David (M/P)
Kreston, Rebecca (IM/EM)
Zilberstein, Ashley (M/P)
PGY -5
Brumley, William (IM/EM)
Case, Aaron (IM/EM)
Wheelis, Emily (IM/EM)
FELLOWS
Cardiology
Abdul-Kafi, Owais
Ajala, Oluremi
Arasar,Kavin
Behan, Sean
Bryska, David
Hill, Michael
Janes, Adam W.
Jonna, Yogesh
Kudinov, Alexander
Meyer, Jonathan
Mishra, Satish
Rajyaguru, Chirag
Sanghvi, Saagar
Sargsyan, Marianna
Sehgal, Vinod
Shah, Anish
Simon, Erik
Slostad, Brody
Yurevich, Oleg
Endocrinology
Calero, Humberto
Obeid, Michelle
Pradeep, Pallavi
Gandhi, Shriya
Geriatrics/AIM
Ahmed, Chaudhary
Burton, Tristesse
Elziny, Moustafa
Freedman, Michael
Grand, Jacob
Haemer, Zoe
Hallihan, Hagar
Jackson, Ronald
Kang, Ian
Manst, Deborah
Marrero-Rivera, Gabriel
Nehme, Christian
Tarte, Nikhil
Wainwright, Samuel
Zimmerman, Melissa
Gastroenterology
Agarwal, Mitali
Agrawal, Rohit
Eng, Jason
Ghoulam, Elie
Griggs, Theodor
Lakhoo, Krutika
Naffouj, Sandra
Nassani, Najib
Pajot, Gregory
Pan, Alexander
Thaker, Sarang
Hematology/Oncology
Arain, Saad
Avila Rodriguez, Ana Maria
Chaudhry, Amina
Khaddour, Karam
Khan, Meshaal
Kodali, Abhigna
Kennedy, Kathleen
Maahs, Lucas
Ng, Ronald
Nguyen, Ryan
Prescott, Kevin
Schwartz, Candice
Seifter, Ari
Shah, Eshana
Simons, Yael
Weiss, Jennifer
Infectious Diseases
Ali, Taha
Amusu, Senate
Cable, Tracy
Fisher, Steven
Ladner, Benjamin
Nephrology
Abdou, Ahmed
Alyamani, Tariq
Alkasir, Amr
Deeb, Reem
Iskander, Kirolos
Rodriguez Rivera, Claudia
Sinha, Urshita
Suh, Edward
Young, Aaron
Transplant Nephrology
Mahmood, Sajid
Pulmonary/Critical Care
Acosta Sanchez, Israel
Anis, Mariam
Barreras, Nicholas
Freedman, Michael
Gonzales, Janae
Green, Chelsi
Gupta, Preeti
Htwe, Yu Maw
Hussain, Jawad
Kalra, Salil
Kashyap, Sarung
Kaul, Malvika
Krow, Solomon
LaBedz, Stephanie
Mbae, June
Naaman, Rami
Pham, Trinh
Reddy, Manasa
Vagts, Christen Lee
Yaqoob, Maidah
Sleep
Mann, Harkirat
Mechineni, Ashesha
Munoz, Thomas
Patel, Palak
Pattisapu, Anil
Viswanath, Shilpa
Interventional Fellow
Mehrotra, Anurag
Tan, Ai-Yui
Rheumatology
Alawneh, Diala
Berry, John Thomas
Hassan, Romesa
Parmar, Prashant
The Department of Medicine (DOM) is committed to the generation of new knowledge. Scholarly activity is a core tenet and ensures that our faculty, staff, and learners provide state-of-the-art patient care, are trained in the most current clinical practices and research methods, and produce rigorous and reproducible science. The department maintains a long-standing expectation that all members will engage in scholarly activity, and provides structured activities led by the Scholarly Activities Council (SAC). The SAC provides services and trainings to strengthen the department’s academic enterprise.
In the past year, the DOM’s funding came from multiple sources resulting in a 13% increase in awards during FY22 from FY20. The DOM’s NIH and non-NIH funding increased to $57.8 million from $45.4 million.



Grant Peer Review: The DOM provides internal reviews for all sections of grant applications. Documents are reviewed by at least one senior faculty with grant review experience and membership on an NIH study sections. Reviewers offer advice and guidance concerning the science and grantsmanship. In 2021, over 21 faculty from all 9 divisions and diverse ranks utilized the service. In addition, trainees are also able to utilize this service to obtain reviews of abstract submissions to professional conferences.
Grant Writing Boot Camp: The DOM led its sixth annual grant writing boot camp in the spring of 2022. Seven junior faculty were selected to participate from a competitive pool of applicants. The 4-week Boot Camp consists of eight sessions co-facilitated by an experienced faculty and prior boot camp participants. Sessions included mini-presentations by facilitators, cohort/peer mentoring, and individualized feedback on grant sections (e.g., aims, strategy, letters of support). A mock study section is offered at the end for interested participants. To date, 19 out of 25 faculty participants - 75% - have received grant funding.
Research Training Opportunities: The DOM Division of Academic Internal Medicine with support of the chief residents hosts the Project And Investigative Research
(PAIR) database. PAIR lists opportunities for resident and medical student research involvement and includes over 35 active projects, and innovative tools and resources to enhance research productivity. PAIR has increased resident and medical student research engagement and faculty to resident mentorship. Early career investigators have the opportunity to leverage NIH-funded training initiatives: four T32s and a resident-focused R38. At present,10 DOM faculty members are recipients of K-awards.
Expert Consultations - Specific Aims, Summary Statements, and Implementation Science: New in 2021, the DOM offered quarterly consultation sessions to improve specific aims sections and strategize how to respond to summary statements. Led by at least two experienced NIH-investigators, topics covered basic science, translational research, and behavioral study designs. DOM also provided monthly implementation science consultations through the Center for Dissemination and Implementation Science. Together, over 25 faculty and students took advantage of these sessions.
Ideas on Tap: The DOM sponsors a quarterly research mixer, “Ideas on Tap” (IOT), to strengthen collaborations and increase awareness of departmental scientific discoveries. The IOT is an informal social experience where faculty and students present their research and enjoy refreshments. In 2021, each IOT focused on a specific topic. January featured DOM training grants, August showcased resident research, and October was open for all research areas.
Scholarly Activities Day: 2022 marked DOM’s 9th annual Scholarly Activities Day. The keynote speaker was Avery August, PhD, Howard Hughes Medical Institute Professor, Cornell University. Additional speakers were Andrea Pappalardo, MD, Nadim Mahmud, MD, PhD, Abeer Mohamed, MD, PhD and Shiva Shahrara, PhD. Due to the COVID-19 pandemic, the annual poster session was not held but this session with awards will resume in 2023.
The Center for Dissemination and Implementation Science (CDIS) was founded in 2017 to advance implementation research, practice, and education to achieve health equity and reduce health disparities among underserved populations in partnership with communities. Despite challenges related to the COVID-19 pandemic, CDIS expanded its robust program of extramural research funding, scholarship, and mentorship.

In the past year, CDIS faculty, post-doctoral students, and staff produced 26 peer reviewed publications, delivered 12 presentations at national and international conferences, gave four invited talks, and participated in four NIH study sections.

We highlight a few publications. Crooks, Donenberg, & Matthews (2021) discussed how to conduct ethical research with Black populations in the time of COVID-19 and Black Lives Matter, recommending three strategies: ensure research settings are emotionally and physically safe; share findings with communities to facilitate trust and encourage feedback to guide interpretation of the findings; and have honest conversations with Black participants about their
feelings regarding the risks, strengths, and barriers to research involvement. Donenberg, Merrill, Atujuna, Emerson, Bray, & Bekker (2021) reported pilot data on the mental health outcomes of a two-arm randomized controlled trial of a HIV-prevention program, Informed Motivated Aware and Responsible Adolescents and Adults - South Africa (IMARA-SA), for South African adolescent girls and young women and their female caregivers. At 6-month follow up, findings revealed that the IMARA-SA group reported significantly less anxiety than the control group and were less likely to report depression and PTSD symptoms than baseline.
Center investigators submitted 28 grant proposals for new sponsored projects and managed 18 active research grants with awards totaling over $3.9 million in extramural research funding. Two notable projects are described here. One is a “Sexual and Reproductive Health Program for Latina Teens and Mothers” (PI Kate Merrill, PhD), a K99/R00 career development award to adapt an evidence-based sexual and reproductive health intervention for Latina adolescents and their mothers/female caregivers. The second project, funded by the National Institute on Minority Health and Health Disparities, represents Phase II of a Small Business Innovation Research grant (MPIs: Donenberg, Smith, Feil). This study is completing the development of a web-based training platform teaching people to
deliver PHAT Life, an empirically supported groupbased HIV and STI prevention intervention for juvenile offenders. The platform will be evaluated in a 2-arm randomized controlled trial.
CDIS faculty trained two clinical psychology interns and more than 20 undergraduate and graduate mentees in 2021. We hosted a ten-week CDIS Summer Internship program for undergraduate students and recent graduates. The internship enrolled eight individuals who engaged in CDIS research projects and attended workshops on implementation science and professional development. Two CDIS post-doctoral fellows, Drs. Nyssa Snow-Hill and Kate Merrill each submitted a NIH career development application - F32 and K99/R00 respectively, and both were awarded.
CDIS sponsored an undergraduate capstone project through the Latin@s Gaining Access to Networks for Advancement in Science (L@S GANAS) program, and supported a Bridge to Faculty post-doctoral fellow in the College of Education. Over 20 junior faculty from public health, nursing, pharmacy, pediatrics, internal medicine, and psychiatry, received formal (via K-awards and the CDIS Faculty Affiliate program) and informal mentorship by CDIS faculty and staff.
• Monthly Works-in-Progress seminars for scholars to share their scholarship, receive feedback, and explore potential partnerships
• One-on-one and small-group consulting for researchers seeking guidance with grant reviews, implementation framework/theory, methods, or measure selection across six UIC colleges and 12 investigators
• Professional development lecture series for center faculty and post-doctoral fellows exploring a wide range of topics such as grant mechanisms, foundation funding, social media strategies
• An annual one-day workshop on the foundations of dissemination and implementation science attended by over 70 faculty, staff and students from seven UIC’s colleges
• The CDIS Colloquium Series, co-sponsored by the Center for Clinical and Translational Sciences and the Richard Weber lecture series, hosted expert implementation science scholars including Daniel Almirall, PhD and Ana Baumann, PhD
• The CDIS Faculty Affiliate program, a multidisciplinary group of scholars committed to CDIS’ mission expanded in 2021. Eight affiliates represent four UIC colleges, including Medicine, School of Public Health, College of Nursing, and the College of Pharmacy, and the Institute for Public Health Research and Policy.


Julie Bobitt, PhD, is a faculty member in the Center for Dissemination and Implementation Science and a Research Investigator at Hines Veterans Affairs. Dr. Bobitt is a highly productive scholar who is bringing implementation science to the fields of aging, chronic pain, and dementia. With funding from the Midwest Roybal Center for Health Promotion and Translation, she is delivering and evaluating a cognitive health program, Wits Workout, for underserved (i.e., rural, racialized, low-income) older adults and leads several projects on cannabis and opioid use in persons living with dementia.
She is actively engaged in Illinois statewide initiatives for the aging, serving on key committees and advisory boards to develop a strategic plan for older adults in Illinois and through her appointment by Governor Pritzker to the Illinois Council on Aging. Dr. Bobitt engaged two top policy and aging journals to publish special issues (on which she will serve as co-editor) on implementation science. Her scholarship comes at a critical time as the need to reduce opioid use is front and center in the country, and the US population is aging. Finally, Dr. Bobitt is a highly collaborative and important contributor to the CDIS, leading UIC’s first course in implementation science and the CDIS colloquium series featuring experts in implementation science and health equity.
1. Biggers A, Feasibility of Text Message Sleep Assessment in African American and Latino Patients with Type 2 Diabetes. J Clin Sleep Med 17, no. 1. 2021 Jan. 69-78.
2. Handler A, A Two-Generation Approach to Postpartum Care: Building on the Well-Baby Visit. Birth 48, no. 3. 2021 Sep: 347356.
3. Jindal M, It Makes Me a Better Person and Doctor: A Qualitative Study of Residents' Perceptions of a Curriculum Addressing Racism. Acad Pediatr. 2021 Dec.
4. Kringle EA, Sedentary Behavior Patterns over 6 Weeks among Ambulatory People with Stroke. Top Stroke Rehabil 28, no. 7. 2021 Oct. 537-544.
5. Leung V, Reexamining the Classification of Older Adults with Diabetes by Comorbidities and Exploring Relationships with Frailty, Disability, and 5-Year Mortality. J Gerontol A Biol Sci Med Sci 76, no. 11. 2021 Oct. 2071-2079.
6. Man B, A Clinical Diabetes Risk Prediction Model for Prediabetic Women with Prior Gestational Diabetes. PLoS One 16, no. 6. 2021: e0252501.
7. Weiner SJ, Impact of an Unannounced Standardized Veteran Program on Access to CommunityBased Services for Veterans Experiencing Homelessness. J Public Health (Oxf) 2021 Apr.
1. Huggett TD, Assessment of a Hotel-Based Protective Housing Program for Incidence of SARS-
CoV-2 Infection and Management of Chronic Illness Among Persons Experiencing Homelessness. JAMA Netw Open. 2021 Dec 1;4(12):e2138464.
2. Krantz S, Mitophagy mediates metabolic reprogramming of induced pluripotent stem cells undergoing endothelial differentiation. J Biol Chem. 2021 Dec;297(6):101410.
3. Xiong S, Interleukin-1RA Mitigates SARS-CoV-2-Induced Inflammatory Lung Vascular Leakage and Mortality in Humanized K18hACE-2 Mice. Arterioscler Thromb Vasc Biol. 2021 Nov;41(11):27732785.
4. Slostad B, A Novel Two-Dimensional Echocardiography Method to Objectively Quantify Aortic Valve Calcium and Predict Aortic Stenosis Severity. Am J Cardiol. 2021 Oct 1;156:108-113.
5. Gao S, A Bayesian inference transcription factor activity model for the analysis of single-cell transcriptomes. Genome Res. 2021 Jun 30;31(7):1296–311.
6. Hong L, Human induced pluripotent stem cell-derived atrial cardiomyocytes carrying an SCN5A mutation identify nitric oxide signaling as a mediator of atrial fibrillation. Stem Cell Reports. 2021 Jun 8;16(6):1542-1554.
7. Kim YM, Mitofusin-2 stabilizes adherens junctions and suppresses endothelial inflammation via modulation of β-catenin signaling. Nat Commun. 2021 May 12;12(1):2736.
8. Chalazan B, Association of Rare Genetic Variants and Early-Onset Atrial Fibrillation in Ethnic Minority Individuals. JAMA Cardiol. 2021 Jul 1;6(7):811-819.
9. Darbar D, Unraveling the genomic basis of congenital heart disease. J Clin Invest. 2021 Jan 19;131(2):e145377.
10. Briller JE, Pregnancy Associated Heart Failure With Preserved Ejection Fraction: Risk Factors and Maternal Morbidity. J Card Fail. 2021 Feb;27(2):143-152.
11. McCauley MD, Atrial Fibrillation and Longitudinal Change in Cognitive Function in CKD. Kidney Int Rep. 2021 Jan 5;6(3):669-674.
12. Twing AH, Improvements in global longitudinal strain after transcatheter aortic valve replacement according to race. Am J Cardiovasc Dis. 2021 Apr 15;11(2):203-211.
13. Hudzik B, Conquering Radial Artery Occlusion: New Skill to Learn. JACC Case Rep. 2020 Dec 16;2(15):2408-2410.
14. Kansal MM, Adaptive Coronary Artery Rotational Motion Through Uncaging of a Drug-Eluting Bioadaptor Aiming to Reduce Stress on the Coronary Artery. Cardiovasc Revasc Med. 2022 Jun;39:52-57.
15. Kim SJ, Addressing Racial/Ethnic Equity in Access to COVID-19 Testing Through Drive-Thru And Walk-In Testing Sites in Chicago. Med Res Arch. 2021 May;9(5):2430.
1. Priyadarshini M, Gestational Insulin Resistance Is Mediated by the Gut MicrobiomeIndoleamine 2,3-Dioxygenase Axis. Gastroenterology. 2022 May;162(6):1675-1689.e11.
2. Lee SM, Hepatocyte-Specific Loss of PPARγ Protects Mice From NASH
and Increases the Therapeutic Effects of Rosiglitazone in the Liver. Cell Mol Gastroenterol Hepatol. 2021;11(5):1291-1311.
3. Poudel SB, Sexually dimorphic impact of adult-onset isolated GH deficiency on bone cartilage, lifespan and health-span. Aging Cell Aug;20(8):e13427.
4. Carmean CM, Dietary Selenium Deficiency Partially Mimics the Metabolic Effects of Arsenic. Nutrients. 2021 Aug 23;13(8):2894.
5. Jagai JS, Diabetes control is associated with environmental quality in the USA. Endocr Connect. 2021 Aug 25;10(9):1018-1026.
6. Scannell BM, Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago. Ann Epidemiol. 2021 Apr;56:47-54.e5.
7. Noblet B, Dual regulation of TxNIP by ChREBP and FoxO1 in liver. iScience. 2021 Feb 20;24(3):102218.
8. Ye H, An estrogen-sensitive hypothalamus-midbrain neural circuit controls thermogenesis and physical activity. Sci Adv. 2022 Jan 21;8(3):eabk0185.
1. Ticho AL, NPC1L1-dependent transport of 27-alkyne cholesterol in intestinal epithelial cells. Am J Physiol Cell Physiol. 2021 May 1;320(5):C916-C925.
2. Anbazhagan AN, miR-29a, b, and c regulate SLC5A8 expression in intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2021 Aug 1;321(2):G223-G231.
3. Gupta A, Increasing driving distance to screening colonoscopy negatively affects bowel preparation quality: an observational study. Journal of General Internal Medicine. 36: 1666-1672, 2021.
4. Rebhun J, Outcomes of Open, Laparoscopic, and Percutaneous Drainage of Infected Walled-Off Pancreatic Necrosis: A Nationwide Inpatient Sample Study. Cureus. 2021 Jan 28;13(1):e12972.
5. Pan AY, Recently Graduated Medical Students Lack Exposure to and Comfort with Chronic Liver Diseases. Dig Dis Sci. 2021 Aug 7.
6. Lipowska AM, Ergonomics of endoscopy. Gastrointestinal Endoscopy Clinics of North America. 2021;31(4):655-669.
7. Rong L, Paneth cell alertness to pathogens maintained by vitamin D receptor. Gastroenterology. 160:1269-1283. 2021.
8. Chatterjee I, Overexpression of Vitamin D Receptor in Intestinal Epithelia Protects Against Colitis via Upregulating Tight Junction Protein Claudin 15. J Crohns Colitis. 2021 Oct 7;15(10):17201736.
9. Zhang Y, Aberrant enteric neuromuscular system and dysbiosis in amyotrophic lateral sclerosis. Gut Microbes. 2021 JanDec;13(1):1996848.
10. Chesnokov MS, Novel FOXM1 inhibitor identified via gene network analysis inducesautophagic FOXM1 degradation to overcome chemoresistance of human cancer cells. Cell Death Dis. 2021 Jul 14;12(7):704.
11. Hopson P, An assessment
of pancreatology education in North American pediatric gastroenterology fellowship programs. Pancreatology. 2021 Oct 31:S1424-3903(21)00611-6.
12. Singh SK, MAP4K4 promotes pancreatic tumorigenesis via phosphorylation and activation of mixed lineage kinase 3. Oncogene. 2021 Oct;40(43):6153-6165.
13. Mancinelli G, Role of stromal activin A in human pancreatic cancer and metastasis in mice. Sci Rep. 2021 Apr 12;11(1):7986.
14. Kumar A, A Novel Role of SLC26A3 in the Maintenance of Intestinal Epithelial Barrier Integrity. Gastroenterology. 2021 Mar;160(4):1240-1255.
15. Stassen PMC, Safety and efficacy of a novel resection system for direct endoscopic necrosectomy of walled-off pancreas necrosis: A prospective, international multicenter trial. Gastrointestinal Endoscopy 2021.
1. Goligher EC, Therapeutic Anticoagulation with Heparin in Critically Ill Patients with Covid-19. N Engl J Med. 2021 Aug 26;385(9):777-789.
2. Lawler PR, Therapeutic Anticoagulation with Heparin in Non-critically Ill Patients with Covid-19. N Engl J Med. 2021 Aug 26;385(9):790-802.
3. Zeiser R, Ruxolitinib for Glucocorticoid-Refractory Chronic Graft-versus-Host Disease. N Engl J Med. 2021 Jul 15;385(3):228-238.
4. Frangoul H, CRISPR-Cas9 Gene Editing for Sickle Cell Disease and β-Thalassemia. N Engl J Med. 2021 Jan 21;384(3):252-260.
5. Prchal JT, HIF-2 inhibitor, erythrocytosis, and pulmonary hypertension. Blood. 2021 May 6;137(18):2424-2425.
6. Page GP, Epidemiology Donor Evaluation Study–III (REDSIII) program. Multiple-ancestry genome-wide association study identifies 27 loci associated with measures of hemolysis following blood storage. J Clin Invest. 2021 Jul 1;131(13).
7. Tolaney SM, Adjuvant Trastuzumab Emtansine Versus Paclitaxel in Combination With Trastuzumab for Stage I HER2-Positive Breast Cancer (ATEMPT): A Randomized Clinical Trial. J Clin Oncol. 2021 Jul 20;39(21):2375-2385.
8. Hoskins KF, Association of Race/Ethnicity and the 21-gene Recurrence Score with Breast Cancer-Specific Mortality Among US Women. JAMA Oncol. 2021 Mar 1;7(3):370-378.
9. Thompson MA, COVID-19 and Cancer Consortium. Association of Convalescent Plasma Therapy With Survival in Patients With Hematologic Cancers and COVID-19. JAMA Oncol. 2021 Jun 17;7(8):1167-75.
10. Aissa AF, Single-cell transcriptional changes associated with drug tolerance and response to combination therapies in cancer. Nat Commun. 2021 Mar 12;12(1):1628.
11. Kanter J, American Society of Hematology 2021 guidelines for sickle cell disease: stem cell transplantation. Blood Adv. 2021 Sep 28;5(18):3668-3689.
12. Ruiz MA, Thrombomodulin and multiorgan failure in sickle cell anemia. Am J Hematol. 2021 Dec 20.
13. Johnson S, Exercise-induced
changes of vital signs in adults with sickle cell disease. Am J Hematol. 2021 Dec 1;96(12):1630-1638.
14. Longoria JN, Patient-reported neurocognitive symptoms influence instrumental activities of daily living in sickle cell disease. Am J Hematol. 2021 Nov 1;96(11):1396-1406.
15. Minniti CP, Clinical predictors of poor outcomes in patients with sickle cell disease and COVID-19 infection. Blood Adv. 2021 Jan 12;5(1):207-215
1. Donenberg GR, A 2-Arm Individually Randomized Trial of TI-CBT Enhanced to Address ART Adherence and Mental Health for Rwandan Youth Living With HIV. J Acquir Immune Defic Syndr. 2022 May 1;90(1):69-78.
2. Donenberg G, Mental Health Outcomes of aPilot HIV-Prevention Program for South African Adolescent Girls and Young Women and their Female Caregivers. BMC Public Health. 2021.
3. Chaisson LH, Yield of repeat tuberculin skin testing for people living with HIV in Brazil. JAIDS. 2021. Jul 30.
4. Chaisson LH, State of the Art Review: A systematic review of the number needed to screen for active TB among people living with HIV. Int J Tuberc Lung Dis. 2021. Jun;25(6):427-435.
5. Brito MO, Birth Defects and Long-Term Neurodevelopmental Abnormalities in Infants Born During the Zika Virus Epidemic in the Dominican Republic. Ann Glob Health. 2021 Jan 5;87(1):4.
6. Brito MO, Infectious Diseases/ Human Immunodeficiency Virus Physician Ambassadors: Advancing Policy to Improve
Health. Clin Infect Dis. 2021 Oct 5;73(7):e2243-e2250.
7. Mena Lora AJ, Feasibility and impact of inverted classroom methodology for coronavirus disease 2019 (COVID-19) pandemic preparedness at an urban community hospital. Infect Control Hosp Epidemiol. 2021Jun;42(6):743-745.
8. Trotter AB, Preparing for COVID-19 Vaccination: A Call to Action for Clinicians on Immunization Information Systems. Ann InternMed. 2021 May;174(5):695697.
9. Matthews AK, The use of strategies from the social sciences to inform pipeline development programs for under-represented minority faculty and students in the health sciences. J Clin Transl Sci. 2020 Dec 14;5(1):e73.
10. Baden LR, Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021 Feb 4;384(5):403-416.
11. Borgetti S, Implementation and outcomes of a severe acute respiratory coronavirus virus 2 (SARS-CoV-2) monoclonal antibody treatment program at an academic medical center serving a high-risk patient population. Antimicrobial Stewardship & Healthcare Epidemiology,1(1), E3.
12. O'Brien MP, Subcutaneous REGENCOV Antibody Combination to Prevent Covid-19. NEJM. 2021 Sept;385(13):1184-1195.
13. Chang YS, Transmission Dynamics of Large Coronavirus Disease Outbreak in Homeless Shelter, Chicago, Illinois, USA, 2020. Emerg Infect Dis. 2022;28(1):76-84.
14. Ghinai I, Risk Factors for Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Homeless
Shelters in Chicago, Illinois-MarchMay, 2020. Open Forum Infect Dis. 2020;7(11):ofaa477.
15. Cohen MS, Effect of Bamlanivimab vs Placebo on Incidence of COVID-19 Among Residents and Staff of Skilled Nursing and Assisted Living Facilities: A Randomized Clinical Trial. JAMA. 2021 Jul 6;326(1):46-55.
16. Novak RM, Aging, trends in CD4R/ CD8R ratio, and clinical outcomes with persistent HIV suppression in the HIV Outpatient Study. AIDS. 2022 Jan 10.
1. Alfego D, Chronic Kidney Disease Testing Among At-Risk Adults in the U.S. Remains Low: RealWorld Evidence from a National Laboratory Database. Diabetes Care. 2021; 44(9):2025–2032.
2. Al-Kindi SG, The Benefits of Intensive Versus Standard Blood Pressure Treatment According to Fine Particulate Matter Air Pollution Exposure: A Post Hoc Analysis of SPRINT. Hypertension. 2021; 77(3):813-822.
3. Chen Y, Obesity Management and Chronic Kidney Disease. Semin Nephrol. 2021; 41(4):392-402.
4. Fischer MJ, Depression Screening and Clinical Outcomes Among Adults Initiating Maintenance Hemodialysis. Clin Kidney J. 2021; 14(12):2548-2555.
5. Hannan M, Risk Factors for CKD Progression: Overview of Findings from the CRIC Study. Clin J Am Soc Nephrol. 2021; 16(4):648-659.
6. Iglesias JI, COVID-19-associated renal involvement and acute kidney injury, pp. 103-115. In: Challenges in the Pandemic: A Multidisciplinary Approach, 1st edition, Thieme Medical and Scientific Publishers
Private Limited, Uttar Pradesh, India, 2022.
7. Hannan M, Sedentary Behavior and Change in Kidney Function: The Hispanic Community Health Study/ Study of Latinos (HCHS/SOL). Kidney360. 2021; 2(2):245-253.
8. Hu EA, Adherence to Healthy Dietary Patterns and Risk of CKD Progression and All-Cause Mortality: Findings from the CRIC (Chronic Renal Insufficiency Cohort) Study. Am J Kidney Dis. 2021; 77(2):235-244.
9. Missikpode C, Cardiovascular Disease and Risk of Incident Diabetes Mellitus: Findings from the Hispanic Community Health Study/ Study of Latinos (HCHS/SOL). J Diabetes. 2021; 13(12):10431053.
10. Pierce DR, Clinical Implications of Tacrolimus Time in Therapeutic Range and Intrapatient Variability in Urban Renal Transplant Recipients Undergoing Early Corticosteroid Withdrawal. Transplant Direct. 2021; 7(6):e698.
11. Schrauben SJ, CRIC Study Investigators. Mobile Health (mHealth) Technology: Assessment of Availability, Acceptability, and Use in CKD. Am J Kidney Dis. 2021; 77(6):941-950.
12. Toth-Manikowski SM, Sex-related differences in mortality, acute kidney injury, and respiratory failure among critically ill patients with COVID-19. Medicine (Baltimore). 2021; 100(50):e28302.
13. Toth-Manikowski SM, Periodontal Disease and Incident CKD in US Hispanics/Latinos: The Hispanic Community Health Study/Study of Latinos. Kidney Med. 2021; 3(4):528-535.
14. Toth-Manikowski SM, Sex Differences in Cardiovascular
Outcomes in Chronic Kidney Disease: Findings from the CRIC Study. Am J Kidney Dis. 2021; 78(2):200-209.
15. Turturice BA, Perinatal granulopoiesis and risk of pediatric asthma. Elife. 2021.
1. Volerman A, Ensuring Access to Albuterol in Schools: From Policy to Implementation. An Official ATS/AANMA/ALA/NASN Policy Statement. Am J Respir Crit Care Med. 2021 Sep 1;204(5):508-522.
2. Mahdavinia M, African American Children Are More Likely to Be Allergic to Shellfish and Finfish: Findings from FORWARD, a Multisite Cohort Study. J Allergy Clin Immunol Pract. 2021 Jul;9(7):28672873.e1.
3. Martin MA, Trends in School Attendance for Low-Income Children with Chronic Health Conditions: Results from a Randomized Controlled Trial. J Sch Health. 2021 Mar;91(3):187-194.
4. Fu P, Essential role for paxillin tyrosine phosphorylation in LPSinduced mitochondrial fission, ROS generation and lung endothelial barrier loss. Sci Rep. 2021 Sep 2;11(1):17546.
5. Fu P, NOX4 Mediates Pseudomonas aeruginosaInduced Nuclear Reactive Oxygen Species Generation and Chromatin Remodeling in Lung Epithelium. Antioxidants (Basel). 2021 Mar 17;10(3):477.
6. Ha AW, Sphingosine kinase 1 regulates lysyl oxidase through STAT3 in hyperoxia-mediated neonatal lung injury. Thorax. 2022 Jan;77(1):47-57.
7. REMAP-CAP Investigators, Therapeutic Anticoagulation with Heparin in Critically Ill Patients with Covid-19. N Engl J Med. 2021 Aug 26;385(9):777-789.
8. ATTACC Investigators, Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19. N Engl J Med. 2021 Aug 26;385(9):790-802.
9. Ahn SJ, Cholesterol-Induced Suppression of Endothelial Kir Channels Is a Driver of Impairment of Arteriolar FlowInduced Vasodilation in Humans. Hypertension. 2022 Jan;79(1):126138.
1. Umar S, IRAK4 Inhibition, A Promising Strategy for Treating RA Joint Inflammation and Bone Erosion. Cell Mol Immunol. Cell Mol Immunol. 2021 May 15.
2. Umar S, CCL25 and CCR9 is a unique pathway that potentiates pannus formation by remodeling RA macrophages into mature osteoclasts. Eur J Immunol. 2021 51:903-914.
3. Van Raemdonck K, In psoriatic
arthritis, TLR7 endogenous ligands remodel glycolytic macrophages to trigger skin-to-joint crosstalk. Eur J Immunol. 2021 51:714-720.
4. Palasiewicz K, Tofacitinib therapy intercepts macrophage metabolic reprogramming instigated by SARS-CoV-2 Spike protein. Eur J Immunol.2021; 51:2330-2340.
5. Umar S, Metabolic regulation of RA macrophages is distinct from RA fibroblasts and blockade of glycolysis alleviates inflammatory phenotypein both cell types. Molecular and Cellular Life Sciences 2021.
6. Kahlmann V, COVID-19 infection in patients with sarcoidosis: susceptibility and clinical outcomes. Curr Opin Pulm Med2021; 27: 463-471.
7. Umar S, IRAK4 inhibitor mitigates joint inflammation by rebalancing metabolism malfunction in RA macrophages and fibroblasts. Life Sciences 2021.
8. Van Raemdonck K, Metabolic reprogramming of macrophages instigates CCL21-induced arthritis. Immunology & Cell Biology 2021.
9. Song M, Sarcoidosis and autoimmunity. Curr Opin Pulm Med. 2021 Sep 1;27(5):448-454.
10. Kondle S, Treatment of COVID-19 in Patients With Sarcoidosis. Front Med (Lausanne). 2021 Jul 16;8:689539.
11. Levin B, Detection of early phenotype cardiac sarcoidosis by cardiovascular magnetic resonance. Curr Opin Pulm Med. 2021 Sep 1;27(5):478-483.
12. Casanova NG, MicroRNA and protein-coding gene expression analysis in idiopathic pulmonary fibrosis yields novel biomarker signatures associated to survival. JGN.Transl Res. 2021 Feb;228:112.
13. Baughman RP, Evaluating the Minimal Clinically Important Difference of the King's Sarcoidosis Questionnaire in a Multicenter Prospective Study. Am Thorac Soc. 2021 Mar;18(3):477-485.
14. Levin B, Detection of early phenotype cardiac sarcoidosis by cardiovascular magnetic resonance. Curr Opin Pulm Med. 2021 Sep 1;27(5):478-483.
The Vitoux Program on Aging and Prevention was made possible with generous support from the Vitoux family. Beth and George Vitoux, both 1937 graduates of the University of Illinois at Urbana-Champaign, believed in education and research as a means to make the world a better place. They greatly valued the education they received at the University of Illinois and their gratitude extended to the University of Illinois Chicago. Their 1 million dollar gift to UIC led to the creation of the Beth Fowler Vitoux and George E. Vitoux Distinguished Professorship in Geriatric Medicine in the College of
Medicine. Dr. Jun Ma, MD, PhD, serves as the inaugural vitoux distinguished professor of medicine. This professorship supports advancements in the medical and social aspects of aging and prevention.
The high prevalence and burden of lifestyle-related chronic diseases in the U.S. call for proven behavioral treatments and prevention programs that can help individuals to adopt healthy lifestyles across the lifespan. The Vitoux Program is committed to the

development, evaluation, and implementation of innovative lifestyle interventions and disseminating and training in high-quality research to promote healthy aging and disease prevention.
Richard Weber, MD, a 1976 College of Medicine alum and gastroenterologist, shared his story on the reason he chose gastroenterology as his specialty. A guest speaker in gastroenterology had such an impact on him while he was a resident that this speaker became his mentor. This experience is at the core of why he generously established a gift for education and learning in the Department of Medicine in 2016 and is still ongoing. Weber believes this will add value and impact to our institution, specifically the Department of Medicine.
Thanks to the generous gift to the DOM donated by Richard Weber, MD, we formed the Life Long Learning committee which has been instrumental in developing the Richard Weber Lecture series. The mission of the Richard Weber Lecture Series is to elevate the DOM as a leader in training our replacements and enhance the experience of our students, faculty and trainees. The lecture series provides ongoing access to world class speakers as a way to stay attuned to the latest information, cutting edge advancements in medicine, and provide the best care for all.
In 2021, the Richard J. Weber, MD A.C.E. Award was created and named in honor of Dr. Richard Weber. The award recognizes and honors exceptional Department of Medicine faculty that exhibit the qualities of an altruism, compassion, and excellence. 105 DOM faculty were awarded this award in 2021.
2021 Weber Lectures
• Mark J. Mulligan, MD, COVID-19 Research in New York City
• Richard Chaisson, MD, The Long Road to Shorter TB Treatments
• Andre Kalil, MD, Why Randomized Controlled Trials Are Necessary to Save Lives During Covid-19 Pandemic
• Amit Patel, MD, Assessment of Coronary Artery Disease: Is It Time to Change our Diagnostic Paradigm?
• Frank Bogun, MD, The Value of Imaging for Ventricular Arrhythmia Management Focusing on CMR
• Warren J. Manning, MD, Role of Echocardiography in Atrial Fibrillation and Decisions Regarding Cardioversion and Anticoagulation
• Michael Davidson, MD, Utilizing Genomics to Personalize Lipid Management
• Tiffany Pulcino, MD, Growing up Sick: A Great Leap Forward or Falling Off a Cliff
• Leslise T. Cooper, MD, Cardiac Sarcoidosis Within the Clinical Spectrum of Myocarditis
• David R. Karp, MD, PhD, Can We Prevent Rheumatic Diseases
• John H. Stone, MD, MPH, IgG4 Related Disease
• Marc A. Judson, MD, Clinical Aspects of Sarcoidosis
• Bishal Gyawali, MD, Reading Between the Lines- Understanding Trial Design Issues That Can Distort the Appraisal of Clinical Benefit of Cancer Drugs
• Elliot Tapper, MD, Ensuring the Best Outcomes for Hospitalized Patients With Cirrhosis
• Zena Sharman, PhD, Keep them from harm and injustice: Strategies for providing LGBTQ+ -inclusive healthcare
• Vanessa Grubbs, MD, MPH, Racism in Medicine: Why and How I Confront It
• Avery August, PhD, R0 and the culture club in diversifying the biomedical sciences
2022 Weber Lectures
• Steven Shoptaw, PhD, Evidence-Based Integrated Strategies for Addiction Medicine and HIV Prevention
• Dee Dee Wang, MD, Heart Failure-Structural Heart, What Are My Patient's Options?
• Steven Hsu, MD, Old Dog, New Tricks: Updated Applications of Invasive Hemodynamics
• Erin D. Michos, MD, Female Specific Factors That Enhance Women's Cardiovascular Risk Across the Lifespan
• Fazal Khan, MD, Telehealth post-covid- The New Future of Medicine?

• Jacob Walker, MD, HIV and Aging: Cross Disciplinary Geriatrics
• Gerald Appel, MD, Treating Lupus Nephritis in 2022
• Debbie Cohen, MD, Resistant Hypertension
• Susan Quaggin, MD, An Eye opening case; revisiting TMAs in the Molecular era
• Omar Lattouf, MD, The Impact of Digital Transformation on the Future of Medical Education and Practice
• Marco Matucci Cerinic, MD, The Vasculopathy Journey In SSc, From The Digits To Internal Organs
• Mehrdad Maz, MD, ACR/VF GCA Vasculitis Guidelines
• Beth Jonas, MD, Rheumatoid Arthritis What the Internist needs to Know
• Matifadza Hlatshwayo Davis, MD MPH, Public Health Leadership in the CoVID-19 Era
• Janice P. Nimura, The Doctors Blackwell: How Two Pioneering Sisters Brought Medicine to Women--and Women to Medicine
Thank you to all of our donors for your continuing support.
The Bias Reduction in Internal Medicine (BRIM) initiative was developed at the University of Wisconsin-Madison to “break the bias habit” and challenge cultural stereotypes that impact interactions with others even unconsciously.
“Nobody thinks that their thoughts or actions are based on internalized stereotypes or biases, but the truth is that these ideas can be so ingrained that even the most sensitive person can be influenced by them in their behavior at work, towards colleagues, patients, or towards students,” said Dr. Patricia Finn. “BRIM has been shown in early trials to help faculty recognize and reduce biased thoughts and behavior. I knew immediately after I saw the results presented at a conference that I wanted our department of medicine to participate in the next phase of evaluating the program.”
The Department of Medicine (DOM) was the first to enroll in the 2017 nationwide study of BRIM developed by Dr. Molly Carnes, professor of medicine, psychiatry and industrial and systems engineering at the University of Wisconsin-Madison and her colleagues. The NIH-funded study included 20 departments of medicine and lasted approximately two years at each institution. The DOM initially selected four local leads for the study: Drs. Waddah Alrefai, Alana Biggers, Geri Donenberg, and Andrew Trotter.
“Ensuring a positive departmental climate by reducing racial/ethnic, gender, and other biases will improve faculty retention,” explained Dr. Carnes. “The average cost of losing a faculty member exceeds $400,000, so climate is also important regarding cost-savings,” said Dr. Carnes. “UI Health — our health enterprise comprised of UIC’s seven health science colleges and the University of Illinois Hospital and Clinics — is dedicated to advancing health equity for all. That commitment is rooted in a faculty and staff who are aware of and can recognize biases and inequities they themselves might hold,” said Dr. Robert Barish, vice chancellor for health affairs at the University of Illinois at Chicago. “Engaging in the BRIM program is one way we can foster this mission in interactions with fellow faculty, staff, patients and students.”
“Research indicates that professional interactions, performance evaluations and hiring decisions are often inadvertently influenced by opinions people hold about others, like where they’re from or the language they speak, without getting to know the individual, Dr. Carnes explained. Race/ethnicity, gender, age, sexual
preference, and even weight can drive biases. At the heart of BRIM is a three-hour workshop designed to “break the bias habit” in Internal Medicine. Participants are taught to recognize their implicit biases and identify strategies to reduce them. For example, participants are encouraged to take the other person’s perspective — or put themselves in another’s shoes and replace a stereotypical perception with real information based on the individual. At the end of the workshop, participants indicate “commitments to action;” the most common ones were challenging microaggressions, practicing perspective-taking, and recognizing and challenging stereotypes. Ten DOM faculty were initially trained by Dr. Carnes’ team to deliver the workshops and are now certified BRIM implementers.
As part of the research study, half of the DOM divisions received the workshops led by the team at the University of Wisconsin-Madison, and half of the divisions received the workshop delivered by UIC-trained implementers. Prior to workshop delivery, DOM faculty completed a baseline survey on the departmental climate. Three months after the workshops, participants completed a follow-up survey about the department climate, the BRIM workshop, and changes in their behavior. A final survey was completed by participants at the conclusion of the study.
The UIC-DOM-BRIM team modified the original workshop to create a two-hour version. The BRIM team has delivered several sessions of this modified version of the workshop to all members of DOM including faculty, internal medicine residents, fellows, post-docs, and administrators during the last four years. Last year, the BRIM team began a collaborative initiative with the College of Medicine (COM) to provide BRIM training to all members of the college on all three campuses. The BRIM team trained new facilitators and the group now includes 20 certified implementers from different departments and from the three campuses. In 2022, 55 sessions were held; 50 of the sessions were for the College of Medicine, three for residents, and two sessions for family medicine and MSTP students. The DOM-BRIM team will continue to collaborate with other departments in the COM at UIC to expand the program and explore options for scholarly activities centered around best practices to promote equity.
The Department of Medicine Inclusion Council (DOMIC) mission is to advance the diversity and inclusion of faculty and trainees through education, advocacy, scholarly activities, mentorship, and networking.
Urban Mentorship Program
Our collaboration with the College of Medicine Urban Health Program and Department of Pediatrics pairs first and second year medical students with a faculty and resident mentor. We had 4 students join their faculty and resident mentors 8 times a year in clinic, hospital rounds and/or procedure rooms to expose them to the daily practice of internal medicine (IM) and subspecialties. Drs. Claudia Lora and Sharmilee Nyenhuis led the program along with Dr. Kristen Kenan and Dr. Felicia Scott-Wellington from pediatrics. Students received formal and informal sessions on patient experience, importance of mentorship, career advancement, test taking, and residency application topics.
Dr. Shikha Jain joined Drs. Cheryl Connor and Anne Polick as faculty leads, and launched the Women

Faculty and Trainees Collaborative Education Series, with “It’s Not You, It’s Them: Unmasking the Real Impostor” by Dr. Jain. In conjunction with Women in Medicine Month, women faculty and residents held “Women Just Wanna Network” event at a local park on September 13, 2021 (pictured above).
The recruitment season continued virtually with “2020 Vision: Be the Change You Needed to See”, the Region II Student National Medical Association (SNMA) Regional Medical Education Conference (RMEC) hosted by The University of Kansas Medical Center, on November 7th, 2020, attended by Dr. Rachael King. In March 2021, “Potenciar El Cambio: Creating Interconnection in Healthcare to Create Change” was the theme for the Latino Medical Student Association’s (LMSA) national conference attended by Dr. Olga Garcia-Bedoya and Dr. Claudia Lora. In April 2021, our involvement at the national SNMA Annual Medical Education Conference (AMEC) “Redefining Obstacles as Opportunities to Transcend Rooted in Excellence” resumed, attended by Drs. Alana Biggers, Rachael King, Keith Naylor, Fred Zar and several residents.
We ended 2021 returning to in-person conferences. “Medicine in a Recovering World: Bringing Us Back Together”, the Region II SNMA RMEC on November 6th followed by “Health Leaders of Tomorrow: Continuando la Lucha por la Equidad”, LMSA’s Midwest Regional Conference on February 12, 2022, both held locally at Northwestern University. LMSA’s “Cincuenta Años de Comunidad: Fostering Service, Health Equity, and Leadership” in March in Philadelphia, PA attended by resident Dr. Carlos Dohse followed by SNMA AMEC
“THE EMERGENCE – Achieving Purpose in an Era of Health Advocacy, Equity & Reform” in April in Orlando, FL attended by Drs. Ashley Binder, Rachael King and residents Drs. Isaye Barton and Meredith
Yellen. Establishing a new collaboration with the Graduate Medical Education program, we had a larger presence at both conferences. With these endeavors and ongoing holistic evaluation of ERAS applications, we continue to increase the diversity of our residency program.
DOMIC planned the Culturally Sensitive Care and Inclusion Series following the successful launch of the Diversity and Inclusion COVID Health Disparities sessions in response to the coronavirus pandemic. These presentations continue to elevate DOMIC’s presence and provide opportunities for co-sponsoring with other programs, departments, and colleges within UIC and receive invites to present at outside institutions. DOMIC continues its work in developing ways to receive feedback and implement solutions. Videos of our lectures are available at https://go.uic. edu/DOMDiversity.
Our initial series included three sessions:
The Impact of COVID-19 Pandemic on Women and Work Life Blend: Challenges and Call For Solutions, by Drs. Ashley Darlington, Sai Sunkara, and Sarah Messmer on September 30, 2020, followed by The Racial Caste System and It’s Impact on Patient Outcomes, with Henrika McCoy, MSW, MJ, PhD, LCSW and Joseph Day, DrPH, MA on October 1st and A conversation on COVID-19 in Chicago’s Latinx Community, by Dr. Allison Arwady, Dr. Max Brito, and Miguel Blancarte, Jr. on October 29th.
The need to provide ongoing education, dialogue and action around topics of diversity, health disparities, racism, women, LGBTQIA+, and more, expanded to become our core educational series to reach a broader audience in 2021.
Richard J. Weber Supported Lectures were Keep them from harm and injustice: Strategies for providing LGBTQ+ -inclusive healthcare, by Zena Sharman on February 9th, Racism in Medicine: Why and How I Confront It, by Dr. Vanessa Grubbs on September 17th, co-sponsored with UIC Women's Leadership and Resource Center, UIC College of Medicine, and Department of Medicine, Division of Nephrology, and R0 and the culture club in diversifying the biomedical sciences, by Avery August, PhD on September 28th.
Other educational series lectures were Introduction to LGBTQI+ Health: An Inclusive Approach to Clinical Care, by Dr. Andrew Trotter on March 11th, Beyond the Binary: Providing Gender Affirming Care by Dr. Sarah Messmer on March 26th, Women’s History Month Lecture Co-sponsored with College of Pharmacy, Gender Equity in Academic Medicine during COVID-19: Challenges and Solutions, by Dr. Min Joo on March 30th, It’s Not You, It’s Them: Unmasking the Real Impostor by Dr. Shikha Jain on April 22nd, Tales from the Survive Study: Victimization and Adversity in Young Black Males, by Drs. McCoy and Day, on June 30th, and Providing LGBTQIA+ Inclusive Care: A Case Based Discussion, by Drs. Messmer and Trotter on August 26th, and Faith, Health Inequities, and COVID-19 Vaccine Hesitancy in the Latinx Community, by Dr. Max Brito, Fr. Manuel Dorantes, STL, MBA, and Miguel Diaz, PhD on October 6th.
Our Culturally Sensitive Care and Inclusion Series continued in 2022 with two Richard J. Weber Supported Lectures, Public Health Leadership in the CoVID-19 Era by Dr. Matifadza Hlatshwayo Davis on February 3rd, for National Women Physicians Day and Women’s History Month Lecture and The Doctors Blackwell: How Two Pioneering Sisters Brought Medicine to Women--and Women to Medicine by Janice P. Nimura on March 8th. Our season concluded with Asian American and Pacific Islander Heritage Month Lecture, A New Yellow Peril? Exploring the Histories and Legacies of Anti-Asian Racism in the US by Gayatri Reddy, PhD and Anna Guevarra, PhD on May 26th.

The objective of the ARIM Lecture Series is to learn about racism in medicine and provide tools for making change moving forward. We began co-sponsoring this series with Internal Medicine Residency in fall of 2021 with Moving Beyond Bias and Microaggressions, by Dr. Kalilah Gates on October 27th, Mass Incarceration: Its Causes and Consequences, by Maria Hawilo, J.D.
on November 18th, Beyond Tuskegee: Understanding the Role of Racism in Shaping of History in Medical Research, by Dr. Alana Biggers on December 10th, Intersectionality and Health Care by Dr. Messmer on January 12, 2022, and A Brief History of Race and Racism in Chicago by Dr. Rachael King on May 2nd.
We were honored to participate in the following Invited Presentations in 2021. AAPI Heritage Month Panel with Dr. Min Joo on May 20th, a student panel discussion sponsored by Asian Pacific American Medical Student Association (APAMSA) at UIC. Introduction to LGBTQIA+ Populations and Creating Inclusive Clinical Care Environments on June 24th and Primary Care for LGBTQIA+ Populations presentation on June 30th by Dr. Trotter as part of the Creating Inclusive Clinical Care series at Texas Tech University Health Sciences Center.
DOM and DOMIC initiated Family Leave Policy for Residents and Fellows was updated to provide for a more comprehensive and supportive family leave and
the Lactation Policy was updated to provide for more designated lactation spaces and support.
A Microaggressions Committee was established by Drs. Trotter, Biggers, and Joo, and chief residents, Drs. Isaye Barton and Jina Kwak to develop programming, educating and awareness of microaggressions in the workplace and with patients. A survey was developed and distributed to collect data on microaggression encounters with faculty, staff, and house staff.


BRIM – Bias Reduction in Internal Medicine lead by Dr. Waddah Alrefai hosted workshops for the DOM and other departments. Growth and development of BRIM expanded to include workshops for the entire College of Medicine.
Education and Support – DOMIC published statements of support and educational profiles throughout the year. Biographies of notable current and past Black doctors were distributed for Black History Month, including highlighting DOMIC member, Paula Allen-Meares, PhD. Additionally, DOMIC published a statement on anti-Asian attacks following a rise in hate crimes, a congratulatory announcement on the confirmation of Rachel Levine, the first transgender woman, as assistant secretary for health in the Department of Health and Human Services, an acknowledgement and reflection of Juneteenth, and a recognition of Pride Month and the anniversary and significance of Stonewall.
Top Photo: LMSA March 2022, Internal Medicine/Emergency Medicine Residents Bottom Photo: Regional SNMA November 2021

Zohair Ahmed, MD, joined the faculty of the Division of Gastroenterology and Hepatology in July 2020. Shortly after his acceptance as a fellow in Gastroenterology & Hepatology in 2016, Dr. Ahmed expressed an interest in learning endoscopic techniques for obesity and weight management. He worked with the UIC Interventional Endoscopy team to craft a one-year curriculum of learning advanced endoscopy techniques and training for bariatric endoscopy. At the time, UI Health did not offer endoscopic weight loss therapy. Throughout 20192020, Dr. Ahmed honed his skills as an advanced endoscopy fellow, while also working closely with the existing Bariatric Surgery team to plan and initiate a bariatric endoscopy program here at UIC. Through his efforts in marshalling support across multiple departments and gaining the appropriate expertise, UI Health now offers endoscopic procedures for weight management without the need for surgery. We celebrate Dr. Ahmed’s initiative and vision in bringing these new services to our patient population.

Mina Al-Awqati, MD, is passionate about providing outstanding clinical care for patients. She is an excellent teacher and mentor to the residents and students. Dr. Al-Awqati is developing a structured program of musculoskeletal ultrasounds in the diagnosis and the treatment of rheumatoid arthritis, crystal induced arthritis, and
osteoarthritis. She is a perfect example of a woman in medicine who deserves recognition. She is well received by the staff, faculty, fellows, and trainees for her incredible devotion towards academic rheumatology.

Scott Borgetti, MD, embodies the role of academic physician. He has assumed the leadership role for transplant infectious diseases and is a mentor for fellows and junior faculty. He is an assistant program director for the infectious diseases fellowship and assistant director of infection control for UI Health and provides guidance for the use of newly developed COVID-19 outpatient treatments to the hospital. He is director of our Outpatient Antibiotic Treatment program. He has been actively engaged in the division’s COVID-19 research efforts from the beginning, while serving on numerous committees to advise the hospital and university at the outset of the pandemic. He currently is the Principal Investigator for the NIH CPAT Trial, testing the safety and effectiveness of decreasing immunosuppression on response to an additional dose of vaccine in solid organ transplant recipients. Dr. Borgetti has been called upon many times to take on these added responsibilities and has accepted all these roles without complaint. He managed each one with diligence and a high level of competence, which is why he is entrusted with these responsibilities. His clinical skills are superior, as is his teaching ability. Dr. Borgetti was selected by the fellows for their annual teaching award. He sets a very high bar for all of us in the Division of Infectious Diseases.


Oana Danciu, MD, is an outstanding clinical investigator who serves as principal investigator in over a dozen clinical trial in breast cancer, as well as in the Big Ten Cancer Research Consortium Steering Committee. In 2021, she was the recipient of a large pharmaceutical sponsored research grant and of the UI Cancer Center Clinical Trial Development award. In addition, thanks to Dr. Danciu’s leadership the UI Cancer Center Clinical Trial office has increased its clinical trial enrollment across the entire Campus supporting many investigators in multiple departments and colleges.

Medicine
Erin Hickey, MD, started a Transition Consult Service that provides resources, support, and education for adolescents and young adults aging into the adult healthcare system and their families. The consult service sees patients while they are admitted to the hospital and continues to follow them longitudinally to work on improving their healthcare status, access to resources, and independence. Dr. Hickey has worked on establishing a primary care clinic for adolescents and adults to provide accessible and comprehensive care to people with intellectual and developmental disabilities. She is involved in research focused on improving the care of people with disabilities. She is part of the INTERACT trial (Improving Communication and Healthcare Outcomes for Patients with Communication Disabilities), a multi-
institutional, PCORI-funded grant studying ways to improve communication between healthcare teams and people with communication disorders. She is working on a grant funded through the Robert Wood Johnson Foundation’s Health Data for Action (HD4A) program studying the gaps in care coordination for adolescents and young adults with complex medical conditions by analyzing national Medicaid data. Dr. Hickey also serves as a physician house advisor through the College of Medicine, advising and mentoring a small group of medical students longitudinally through their medical school journeys.
KHALIL IBRAHIM, MD Assistant Professor of Clinical Medicine CardiologyKhalil Ibrahim, MD, is the Division of Cardiology’s Rockstar due to his many contributions to the division, department, and the college. From a clinical perspective, he provides daily leadership and technical expertise in the Cardiac Catheterization Laboratory as well as the UI Health Hybrid Operating Room. Dr. Ibrahim has expanded the Structural Heart Program over the past 2 years and has demonstrated continued growth while maintaining outstanding quality outcomes. He is among the most productive providers in the Department of Medicine. Dr. Ibrahim serves as a cochair of the Emergency Care Committee where he helps to improve the emergency cardiac care programs within the UI Hospital. He is a tireless teacher of students, residents, fellows, nurses, and technical staff. Finally, Dr. Ibrahim has made valuable contributions to scholarly activities providing educational seminars to providers at UI Health and in the region, authored peer-reviewed papers, and developed innovative teaching programs. It is for these reasons that we believe Dr. Khalil Ibrahim is most deserving to be
highlighted as our Divisional Rockstar.
 JEFFREY
JEFFREY


As professor of medicine, director of the Medical ICU, and senior associate head of the Department of Medicine, Jeffrey Jacobson, MD, makes invaluable contributions to our institution through high-quality clinical care, impactful research, inspirational education, and dynamic administrative leadership. He has led efforts to improve sepsis care at UI Health and rapidly optimized MICU operations in response to the COVID-19 pandemic. In 2021, he received a well-earned nomination for Physician of the Year at UI Health. He is an R01-funded physician scientist and leader in lung vascular biology whose research focuses on improving mechanistic understanding of ARDS and radiationinduced lung injury. As a specific example, his work has characterized the potential for “repurposing” medications such as statins or anti-psychotics to reverse vascular leak during these inflammatory lung conditions. He has served as chair of the Department of Medicine's Scholarly Activities Council. More recently, he serves as principle investigator for our new Stimulating Access to Research in Residency(StARR) program, an NIHfunded career development program that seeks to recruit medicine residents of varied backgrounds to be mentored in research careers in cardiovascular, pulmonary, or hematologic diseases. UIC is one of the few institutions in the country to receive funding for this prestigious R38 program, which would not have been possible without Dr. Jacobson’s leadership and because of these contributions and many others, he is an essential member of our division.
Abeer Mohamed, MD, PhD, is a junior faculty member recruited to the Division of Endocrinology, Diabetes and Metabolism within the past 2 years. Prior to coming to the division, she had already secured funding through a competitive grant program at the NIH (K99/R00). Despite the pandemic, since arriving at UIC she has setup her basic and translational laboratory, published multiple high impact papers, and secured her first NIH R01. Dr. Mohamed is well on her way to being a leading expert in her field and we highlight her impressive achievements.
Dr. Ruchi Naik received her PhD at the Veer Narmad South Gujarat University. She subsequently completed her Internal Medicine Residency training in 2007 in Surat, Gujarat, India and went on to complete a fellowship in nephrology at Temple University, which she completed in 2019. She then completed a transplant nephrology fellowship at Vanderbilt. Dr. Naik joined our faculty in the Division of Nephrology in July 2020. Dr. Naik is an excellent clinician and is dedicated to provide the highest level of care for her kidney transplant patients. During periods of short-staffing, Dr. Naik was always willing to pitch in to help her colleagues and continued to provide excellent care. On top of her outstanding clinical work, Dr. Naik is deeply committed to developing skills in clinical research and is enrolled in the MS in Clinical and Translational Science program.

2022 UI Health Physician of the Year Award

Dr. Jeffrey Jacobson is the quintessential doctor's doctor. He communicates with honesty and clarity, and he is respected by all for his gift of explaining complicated concepts in simple terms. Dr. Jacobson led the team of Critical Care physicians to help care for those most impacted by COVID-19; he truly embodies the values of putting the patient first and delivering world-class care to all. Dr. Jacobson has an outstanding breadth of knowledge and shares selflessly with everyone. He has a calm demeanor and displays strong yet kind leadership in the ICU. Dr. Jacobson always ensures that we are doing what is best for the patients and the staff.
The Departmental Faculty of the Year Award is presented to one faculty member in honor of their outstanding contributions and achievement in at least one of three areas: teaching, research, or service.
2021 Recipient Min Joo, MD, Professor of Medicine


2022 Recipient Brian Boulay, MD, Associate Professor of Medicine



The Departmental Rising Star Award is presented to one faculty member who has demonstrated strong potential to be a future leader in their chosen field.

2021 Recipient Stockton Mayer, DO, Assistant Professor

2022 Recipient Pingwen Xu, PhD, Assistant Professor
The UIC Teaching Recognition Award is awarded to instructors with a history of teaching excellence over the past three academic years and have demonstrated a long-term commitment to teaching at UIC.
2022 Recipient Pavan Srivastava, MD
Award of Excellence in Compassionate Care of Oncology
Dominic Ho, MD, PhD

UIC Janice Watkins Award
Dauphine Gregory
2022 UI Health Physician of the Year award ceremonyInternal Medicine Residency Program Awards
2021
New Attending of the Year
Dr. Christopher Fernandes
Clifford Pilz MD Attendings of the Year
Drs. Tanjeev Kaur, Adam Mikolajczyk, Anne Polick, Fred Zar
The John E. Tulley MD Academic Internal Medicine
Attending of the Year
Dr. Christopher Fernandes
The Paul K. Schlesinger MD JBVA Attending of the Year
Dr. Min Joo
Chief Residents' Choice Award
Dr. Cheryl Conner
PGY-1 Resident of the Year
Dr. Natalie Puñal
PGY-2 Resident of the Year
Dr. Alan Jarman
PGY-3 Resident of the Year
Dr. Conner Olsen
Ergün Önal Award for Excellence in Teaching
Dr. Aaron Case
Humanistic Resident of the Year
Drs. Laura Casalegno and Conner Olsen
Jose Arruda Fellow of the Year Award
Dr. Alexander Pan
Faculty Award for Outstanding Graduate
Dr. Laura Casalegno
Patrick Belvitch, MD – Associate Professor
Susan Bleasdale, MD – Professor
Rodrigo Burgos, PharmD – Associate Professor
Rachel Caskey, MD – Professor
Cheryl Conner, MD – Associate Professor
Dustin Fraidenburg, MD – Associate Professor
Kevin Haas, MD – Associate Professor
Kent Hoskins, MD – Professor
Shikha Jain, MD – Associate Professor
Marci Laragh, MD – Associate Professor
Brian Layden, MD, PhD – Professor
Amanda Osta, MD – Professor
2022
New Attending of the Year
Dr. Ashley Binder
Clifford Pilz MD Attendings of the Year
Drs. Ashley Binder, Adam Mikolajczyk, Anne Polick, Fred Zar
The John E. Tulley MD Academic Internal Medicine
Attending of the Year Award
Dr. Adam Kosloff
The Paul K. Schlesinger MD JBVA Attending of the Year Award
Dr. Ambareen Khan
Chief Residents' Choice Award
Dr. Stefan Tchernodrinski
PGY-1 Resident of the Year
Dr. Spencer Hill
PGY-2 Resident of the Year
Dr. Natalie Puñal
PGY-3 Resident of the Year
Dr. Briana Castillo
Ergün Önal Award for Excellence in Teaching
Drs. Lily Cheng and Paul Cooper
Humanistic Resident of the Year
Dr. Tori Gartmond
Jose Arruda Fellow of the Year Award
Dr. Ryan Knodle
Faculty Award for Outstanding Graduate
Dr. Alan Jarman
Mahesh Patel, MD – Professor
Anne Polick, MD – Associate Professor
Bharati Prasad, MD – Professor
John Quigley, MD– Professor
Ana Ricardo, MD – Professor
Adam Rodos, MD – Associate Professor
Sunit Singla, MD – Associate Professor
Ignatius Tang, MD, PharmD – Professor
Daniel Toft, MD, PhD – Associate Professor
Carissa Tyo, MD – Associate Professor
Yinglin Xia, MD – Professor
The Division of Academic Internal Medicine and Geriatrics (AIM) encompasses general medicine, hospital medicine and geriatric medicine. AIM has been actively growing and developing our clinical footprint, educational efforts, and scholarship.
AIM physicians provide general medicine and geriatric care in both the inpatient and outpatient settings. Outpatient care is provided in four on-site clinics and one off-site clinic at the South Loop Physicians Group. In addition, AIM provides geriatric care at three nursing home facilities: Pearl of Hillside (Hillside, IL), Center Home for Hispanic Elderly (Chicago, IL) and Barton Senior Residences of Chicago (Chicago, IL). The division has five robust general medicine inpatient services at the University of Illinois hospital; and runs an observation unit in collaboration with the Department of Emergency Medicine.
Over the past two years AIM has expanded in all clinical areas:
• FY21, AIM welcomed six new faculty members: Drs. Adam Kosloff, Colin Goodman, Jenna Schulte, Christopher Fernandes, Arthur Moswin, and Bhanu Settipalle.
• FY22, AIM welcomed seven new faculty: Drs. Anna Mauro, Erin Hickey, Monique Jindal, Sagar Harwani, Geoffrey Stetson, Awati Neha, and Elisabeth Poorman.
• As a result of the COVID-19 pandemic and closure of a nearby hospital, patient census in the hospital significantly increased over the past year necessitating a 6th general medicine inpatient team (faculty only).
• In May 2021, Geriatric faculty began to provide clinical care at a 4th nursing home, Warren Barr South Loop.
• In May 2021, the Michael Reese Care Program, directed by Arthur Moswin, MD, joined AIM at the South Loop clinic. This group provides comprehensive HIV medical services to adult’s living on Chicago’s South Side.
• In 2021, the 2-Generation Clinic (Director: Rachel Caskey, MD) was established. The 2-Generation Clinic is dedicated to women and children and provides comprehensive medical care, social support and a
mental health collaborative care model.
• In 2021, Dr. Erin Hickey initiated 2 new clinics, Transitional Clinic and Adults with Complex Care Clinic, both seeing patients at the South Loop clinic. The Transitional Clinic provides care to young adults transitioning to adult primary care. The Complex Care Clinic provides comprehensive care to adults living with complex medical needs and/or disabilities.
• December 2022, the South Loop Physician Group moved to a newly renovated space, expanding from 6 to 10 exam rooms.
All AIM faculty actively participate in numerous educational efforts at UIC including undergraduate and graduate medical education. AIM faculty hold leadership roles in both the Internal Medicine Residency program and in the medical school. As a whole, AIM faculty contribute more effort to medical school education than any other unit in the College of Medicine.
The Geriatric Medicine Fellowship program at UIC is a one year highly collaborative ACGME-accredited program and is one of the largest programs in the country that provides medical and inter-disciplinary education on normal aging, geriatric chronic diseases, palliative care and evidence-based senior healthcare. Two fellows, Chaudhary Ahmed and Nikhil Tarte, completed training through our fellowship program in 2021 and 2 fellows, Moustafa Elziny and Christian Nehme, will complete the program in 2022.
The CLASS Fellowship program launched on July 1, 2018, led by Dr. Saul Weiner. The goal of the Clinical Leaders and Academic Scholars (CLASS) fellowship is to graduate collaborative and self-directed continuous learners who identify and respond to the most significant clinical, research and educational
challenges in the organizations they serve. The fellowship is designed to develop a set of core competencies, complemented with specialized expertise depending on the track. Three fellows completed the program in 2021 and 3 fellows began the program in 2021, Zoe Haemer and Gabriel Marrero-Rivera are both on the medical education track, and Sam Wainwright is on the research track.
The POCUS (Point of Care Ultra Sound) Fellowship was launched in July 1, 2020. POCUS fellow, Michael Freedman, completed the program in 2021, remained at UIC post-fellowship and is currently a pulmonary disease and critical care medicine research fellow. Two fellows will complete the program in 2022, Xiangyu Xie and Ian Kang.
The Vitoux program in Aging and Prevention, directed by Jun Ma, MD, PhD, who serves as the inaugural vitoux distinguished professor of medicine, focuses on lifestyle interventions to promote healthy aging and disease prevention. The Vitoux program faculty, staff, and trainees are engaged in research on lifestyle and preventative care across the lifespan, education and mentorship and creating evidence-based programs that transform research into practice. The Vitoux program includes multiple research initiatives including the ALOHA trial: Addressing Quality of Life, Clinical Outcomes, and Mechanisms in Uncontrolled Asthma
Following the DASH Dietary Pattern is an active study to evaluate behavioral interventions to promote Dietary Approaches to Stop Hypertension (DASH) among adults with uncontrolled asthma.
In calendar year 2021, AIM welcomed three postdoctoral Fellows, Tristesse Burton, PhD, MSL, Hagar Hallihan, PhD, RN, Ronald Jackson, PhD for the T32 Precision Lifestyle Medicine and Translation
Research (PREMIER) Postdoctoral Training Program (T32 MPI’s: Ma, Caskey). In addition, we have had several experienced research staff join our division (Amruta Barve, Vikas Kumar, Sushanth Dosala and Nancy Wittels) for Dr. Jun Ma’s research study entitled “Study of a PST-Trained Voice-Enabled Artificial Intelligence Counselor (SPEAC) for Adults with Emotional Distress” and the ALOHA trial.
We hired research staff Alia Jamison and Lawrie Zhang for Dr. Caskey’s HRSA grant “Innovations to ImPROve Maternal OuTcomEs in Illinois (I PROMOTE-IL)”.
Monique Jindal, MD, a junior faculty member, was recruited to expand the health services research faculty in AIM. Dr. Jindal completed a fellowship in health equity research at the Johns Hopkins School of Medicine prior to joining UIC.
Elisabeth Poorman, MD joined us after completing an addiction fellowship at the University of Washington School of Medicine. Dr. Poorman is working with Dr. Sarah Messmer and the UI-TEAM: Utilizing Interdisciplinary Training to Educate and increase Access to Medication Assisted Treatment project.
In FY21, AIM received 23 new sponsored awards and AIM faculty had over 70 peer-reviewed publications this year.

Despite the challenges of the COVID-19 pandemic, we have experienced modest growth in the clinical practice in 2020. Over the last year, we have focused on growing the Structural Heart Disease (SHD), CardioOncology, and Inherited Heart Disease (IHD) programs, establishing the T32 research training program, enhancing faculty development and mentorship, and recruiting new faculty.
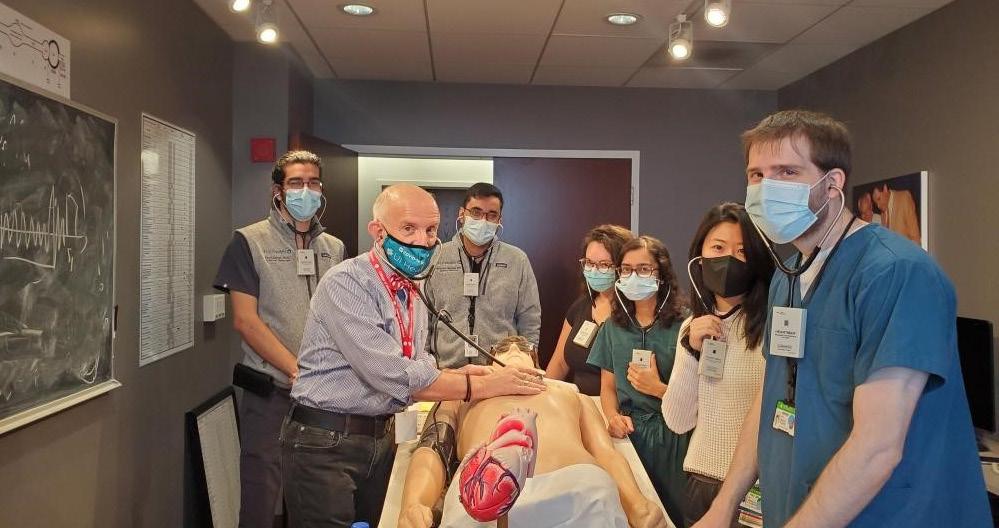
Growth in Faculty: We have promoted diversity, equity, and inclusion by recruiting underrepresented minority (URM) and women cardiologists. In 2020, we recruited two of our former chief fellows, Drs. Mary Rodriguez (URM) and Hema Krishna for the vacant noninvasive/heart failure (HF) and SHD imaging positions respectively, a second SHD cardiologist (Dr. Michael Bode), and an experienced electrophysiologist (Dr. Srinath Yeshwant).
Growth in Clinical Practice: We experienced a decline in services, especially over the months of March to June of 2020 due to COVID-19 pandemic with a steady increase towards the end of the calendar year. During this timeframe, professional charges from patient care in the division decreased by 11%, (with a 52% decrease during the COVID-19 shutdown months alone). During the last quarter of calendar year (CY) 2020, the charges increased by 13% compared to CY2019, as our team returned to normal operations.
Innovations in Patient Care: We continue to expand our clinical footprint by establishing innovative clinical care programs and partnering with local community hospitals, JBVA and Mile Square Main Federally Qualified Health Center (FQHC). a) SHD Program: We performed over 75 transcatheter aortic valve replacements (TAVRs), 30 Watchman devices and 15 Mitraclips in 2020. b) Program in Cardio-Oncology: Established in 2018 by Dr. Chris Gans, the CardioOncology Program continues to provide invaluable
service to cancer patients. c) IHD Program: This program continues to serve our patients and their families as well as the referring community and enables us to provide high quality clinical care but also conduct clinical and translational research. d) Advanced HF Program: Dr. Gans has partnered with Northwestern University Medical Center to create a joint Advanced HF Clinic at UIC. e) Heart Disease in Women Program: Dr. Joan Briller, Director, continues to broaden the referral base for pregnant women and women with heart disease.
In alignment with the Center for Cardiovascular Research (CCVR), the division is expanding its research focus to NeuroCV Biology based on a.) existing expertise in vascular biology, metabolism, and stem cell biology; tissue and organoid engineering, metabolomics and single-cell analysis; b.) like CV Disease, cognitive decline and Alzheimer’s disease are key public health challenges associated with significant morbidity and increased mortality; and c.) long-term sustainability of a NeuroCV Biology program as it is becoming increasingly apparent that CV pathologies exacerbate neurodegenerative diseases.
We have created an interdisciplinary training program to mentor predoctoral and postdoctoral trainees in Personalized Medicine. Trainees from Endocrinology, Diabetes and Metabolism, Biomedical Engineering and Stem Cell Biology & Regeneration as well as CV Medicine are developing into the next generation of physician scientists and scientists. The broad applicability of our program has enabled us to recruit fellows from distinguished programs like the University of Chicago and Emory University for the Cardiology Fellowship.
The Division of Endocrinology, Diabetes and Metabolism made substantial strides in our goal to
become a leading division in the coming years in clinical and research activities.
With support from the department and College of Medicine, we continue to make great strides. While this year has brought continued challenges in the face of the persistent COVID-19 pandemic, our group of physicians and scientists have continued to adapt and met the unique challenge it has presented to us. Important on-going projects have emerged to investigate the relationships between COVID-19 and diabetes, through which we are aiming to define risk factors in these patients.
During this period, we developed a robust Emergency Room Screening program for diabetes. This program diagnoses 300 people a month with prediabetes and diabetes. Our next steps are to develop a plan to integrate these newly diagnosed individuals into primary care and diabetes education classes. We continue to have success of our Diabetes Management Education program and inpatient Diabetes Management program and developed a combined diabetes-nephrology clinic, to manage complex patients. We are actively working to start a promising new development in the Illinois Department of Correction (IDOC) around diabetes care.
Focused on Bone health, we plan to expand our outreach for bone density studies. About 20 percent of referrals for bone density studies come from community providers. Our goal is to reach out to these providers to better serve their patients' needs. In addition, we are reaching out to our internal customers within the UIH community. We expanded our clinical practice into Mile Square clinic and have coordinated with the weight management and islet transplant programs. Our focus is quality improvement for bone health and leveraging the electronic medical healthcare records system.
In FY22, we took over transgender care within IDOC. For each facility within the state of Illinois, we manage their hormonal and medical needs around transgender care with the goal of improving outcomes and better meet the patient's goals.
The division's research program continues to grow. Our federal funding increased from $700,000 in 2016 to over $5 million annually. Our research spans islet biology and transplant programs, adipose functional studies, hepatic metabolism, environmental impact on metabolism, and central nervous systems (CNS) driven mechanism of obesity and diabetes. The divisions' researchers are involved in numerous clinical trials, working with clinical researchers and using emerging technologies including artificial intelligence to address diabetes and metabolism questions that impact patient care and outcomes. Moreover, we are making significant strides to develop a UI Health/UIC diabetes center, which will better consolidate research activities.
All of our faculty participate in the educational efforts of our fellowship program. Our two-year fellowship training program is accredited by the Accreditation Council for Graduate Medical Education (ACGME). Fellows receive educational and clinical instructions from faculty using our inpatient and ambulatory facilities at the clinics and hospital. In addition, they attend weekly, monthly, and annual conferences, and participate in national conferences. Our fellows have published papers and presented posters at the endocrinology society meeting, AACE Illinois Chapter meeting as well as won the National ACE Award.
The Division of Gastroenterology and Hepatology is staffed by physicians and scientists who specialize in the diseases of the liver and gastrointestinal (GI) tract, including diseases of the esophagus, stomach, gallbladder, pancreas, small and large intestine (colon) and rectum. Our team offers specialized care for
numerous complex disorders such as: inflammatory bowel disease, short gut syndrome and small intestinal transplantation, gastrointestinal oncology, pancreaticobiliary disorders, and gastroesophageal reflux and swallowing disorders.
The past year was marked by the ongoing Coronavirus pandemic, including the rise of the Delta variant. However, the division has now adapted to the realities of practicing medicine within this environment, including preprocedural testing, social distancing, personal protective equipment, and telehealth clinic visits. After a decline to only 5533 endoscopic procedures in FY 2020, UIC gastroenterologists performed 6793 endoscopic procedures in FY 2021, even more than the 6565 procedures performed in FY 2019. We rebounded from the disastrous onset of the pandemic, and we are poised for increased success as we transition to a new endoscopic procedure suite in the Ambulatory Services Center.
In FY 2021, our endoscopic team continued to explore the leading edge of endoscopic therapies. We now offer endoscopic therapies for weight loss, including intragastric balloon placement and endoscopic sleeve gastroplasty. We are also expanding the use of novel lumen-apposing metallic stents to treat acute cholecystitis or gastric outlet obstruction in patients for whom surgery is not a good option. Our esophageal program now offers EndoFLIP procedures for investigation of swallowing disorders.
We also provide patient care for the treatment and management of all liver disorders, including viral hepatitis (hepatitis B and C), autoimmune liver disease, nonalcoholic fatty liver disease, primary biliary cirrhosis, primary sclerosing cholangitis, hepatocellular carcinoma, liver lesions, alcohol liver disease, cirrhosis, and patients in need of liver transplantation. Teams of expert physicians at the Bobbie and Marvin Fink Liver Clinic and the Walter Payton Liver Center bring innovative care, scientific collaboration and patientfocused methods to combat liver diseases. We provide dedicated inpatient and outpatient care to GI and
liver patients of Illinois and beyond and also provide hepatology services at four clinics outside Chicago.
The UI Health Liver Transplant team is one of the most experienced and innovative programs in transplant and research in Chicago and the region. Our center is a pioneer in living-donor liver transplantation. Our hepatologists work closely with a team of pharmacists and mid-level providers to take advantage of new treatments for liver disease and develop the best treatment plans for patients. Unlike other transplant programs, we closely monitor and provide one-on-one care throughout the entire transplant process, from the pre-transplant workup to postoperative care. Our team strives to provide culturally sensitive care to all ethnicities, races and religions, providing the best experience possible for the patient and their family. For the third straight year, UIC has performed over 50 liver transplants and we seek to grow the program further.
Our research encompasses a broad array of investigations with particular focus on epithelial transport and diarrheal disorders, GI cancer research, host-pathogen interactions and gut microbiota, inflammation and nutrition and metabolism. We are fortunate to have garnered substantial extramural funding, including government and private foundations sources as well as philanthropy.
We offer 1-4 fellowship positions each year, for highly qualified applicants seeking the highest quality training in all aspects of gastroenterology and hepatology. Our

program is distinctive because of its commitment to provide the fellows with:
• The opportunity to learn all diagnostic and therapeutic procedures.
• An intensive exposure to all aspects of clinical hepatology, including transplantation.
• The ability to obtain additional formal education, including a Masters of Public Health (MPH) degree.
• Exposure to clinical, bench and translational research opportunities.
Fellowship training is provided by full-time faculty who are clinical, translational and basic science investigators and who are experts in their particular subspecialties. Fellowship graduates are skilled in endoscopic procedures, as well as the art of providing consultation and expert care for complex patients. Our program is fully accredited by the Accreditation Council of Graduate Medical Education (ACGME). We also offer advanced fellowship training in areas including transplant hepatology and advanced endoscopy.
Advanced Endoscopy Fellowship - The Advanced Endoscopy fellowship is a one-year curriculum of intense immersion in therapeutic endoscopy. The trainee maintains a junior faculty position and gains exposure to specialized procedures treating patients with pancreaticobiliary disorders and GI cancer, as well as managing the consult service for pancreaticobiliary disorders. Trainees complete the program with a skillset that includes endoscopic retrograde cholangiopancreatography, endoscopic ultrasound, luminal stent placement, resection techniques to large polyps and masses, and deep enteroscopy.
The Transplant Hepatology Fellowship program at UIC offers one fellowship position each year for highly qualified physicians dedicated to obtaining high quality training in Transplant Hepatology. Fellows are exposed to ambulatory pre and post-transplant clinics, inpatient transplant hepatology, inpatient transplant surgery, interventional radiology, and clinical hepatology.
Past graduates have gone on to practice in academic settings across the country. Our 2021 graduates, Mitali Agarwal, MD, is now at the Cleveland Clinic for IBD fellowship and Najib Nassani, MD, MS, is now at the University of Chicago for an Advanced Endoscopy Fellow position. Our Advanced Endoscopy fellow, Constantine Melitas, MD, is now practicing at the Arroyo Grande Community Hospital in Arroyo, CA.
The Division of Hematology/Oncology has been growing its clinical and research work in each of its main programs, Hematology, Bone Marrow Transplant (BMT) & Cellular Therapy (CT), Medical Oncology and Sickle Cell Disease. Seven new faculty members were recruited in 2021, increasing not only the overall number of faculty but also the diversity of the team.
The division now has multiple tumor-focused working groups that are instrumental for providing cancer patients with the most accurate clinical approach by selecting new clinical trials, initiate or participate in translational research, engage other key providers in surgery, radiation therapy or pathology. The main working groups include: breast cancer with Drs. Hoskins, Danciu, Gadi and Ibraheem; lung, head and neck cancer with Drs. Feldman, Weinberg and Mary Pasquinelli, APN, PhD; GI with Drs. Jain and Chen, heme malignancy with Drs. Rondelli, Quigley, Khan, Patel, Rubinstein and Uzoka. Other faculty, such as Dr. Reizine and Dr. Ho collaborate very actively with surgical departments in genitourinary cancer and sarcoma, respectively. In FY 2021, the BMT&CT program
treated its first 5 patients using chimeric-antigen T cells (CAR-T) against CD19+ B cells present in NonHodgkin lymphomas or acute lymphoblastic leukemia.
Among the many clinical highlights of the division, the recruitment of Dr. Paul Rubinstein brought to UIC a nationally recognized program for HIV related malignancies, particularly lymphomas, with the opening of new clinical trials, as well as translational research projects. Within the Section of Medical Oncology, Dr. Kent Hoskins led a team of investigators in a seminal work on the Molecular Characterization of Luminal Breast Tumors in African American Women that was selected for an oral presentation at the 2021 American Society of Clinical Oncology meeting last June, and a related study was published in JAMA Oncology.
The HEM/ONC Genetics Team initiated an ongoing Hereditary Cancer Tumor Board. These meetings are a unique feature for oncology genetics programs and were initiated to improve oncology genetic patient care by increasing multispecialty integration and discussion of complex cases, and to expand cancer genetics educational opportunities among faculty and trainees. The creation and continuation of this tumor board was used as the 2021 annual programmatic goal for the UI Health Cancer Committee for accreditation by the Commission on Cancer, receiving accolades from the committee for patient care and provider development. These twice monthly Hereditary Cancer Tumors Boards have recently been made available to a variety of learners, University wide, to increase cancer genetic education.
The Annual Global BMT Training Program for physicians in Low Middle Income Countries (LMIC) was held remotely due to the pandemic. From October 2020 to March 2021, 32 physicians from Argentina, Bolivia, Cuba, Dominican Republic, Ethiopia, Greece, India, Nepal, Nigeria, and Ukraine could attend 14 live lectures delivered by our BMT team and followed by Q&A. In November 2021, Dr. Rondelli visited Civil Service Hospital in Kathmandu (Nepal) and Ramaiah
Medical College in Bangalore (India) to give lectures and share rounds with faculty and fellows.

A Global Health project in breast cancer was started in 2021 thanks to Dr. Ibraheem who joined the Division of HEM/ONC to develop her research on implementation of clinical trials in breast cancer in Nigeria.
Members of the division authored or co-authored 63 peer reviewed publications in 2021, and 14 of these in very high impact factor (IF >10) journals, such as The New England Journal of Medicine, Nature Communications JAMA Oncology, Journal of Clinical Oncology, Journal of Clinical Investigation, Blood, and the American Journal of Hematology.
The first part of 2021 was still challenged by many patients with COVID-19 infection. Hematology/ Oncology patients were continuously followed and treated for their primary disease both in the outpatient and inpatient setting. In addition, members of HemOnc were actively involved in a multidisciplinary research project related to COVID-19, that led to important publications and a conspicuous NIH grant to UIC. This included a sub-grant to Dr. Quigley as the leader
of studies on thrombotic complications in patients admitted to UI Health for COVID-19. Our division was also an active part of a national research project analyzing the outcome of cancer patients affected by COVID-19, thanks to the effort of Dr. Feldman and our chief fellow Dr. Ryan Nguyen.
The Sickle Cell Center led by Dr. Gordeuk and including Drs. Saraf, Molokie, Njoku, Hussain, Farouqui and Rizvie, had extensive scholarly productivity. Dr. Saraf was awarded an RO1 grant for his basic science research on the effects of sickle cell in renal function. As a result of the close interaction between the Sickle Cell team and the BMT&CT, our center is part of a worldwide consortium limited to a small group of centers that were involved with the design of the first Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) clinical trial in patients with sickle cell disease. CRISPR technology was utilized to delete the BCL11A gene in patients’ hematopoietic stem cells in order to restart the production of fetal hemoglobin (HbF). Dr. Rondelli was a co-author of the report in the New England Journal of Medicine with the first two patients followed for 12 months after being cured with CRISPR technology.
The Division of Infectious Diseases faculty serves in leadership roles for the hospital, college, as well as University-wide response, and have ongoing contract agreements with both Chicago Department of Public Health (CDPH) and Illinois Department of Public Health (IDPH) to provide consultative support and direct services. We continue to actively engage in national and international, federally funded cutting edge clinical research to treat and prevent COVID-19. As we have adjusted to life in a pandemic, we continue to maintain our other research, educational, clinical, and service missions with both local community and global activities.
The entire ID faculty continues to be engaged in the response to COVID-19. Susan Bleasdale, MD, as director of infection control and chief quality officer for UI Health, with the assistance of Scott Borgetti, MD, assistant director of infection control, continues to lead the medical center at large on policy changes to the evolving pandemic. While the routines in the medical center continue, they have worked tirelessly behind the scenes to keep up with changes in infection control guidelines and treatment practices.
Richard Novak, MD, is the director of the UIC Community Clinic Network (UCCN), with six community-based clinics located in the highest prevalence communities in Chicago serving about 1,200 active patients with HIV. The UCCN has been in operation since 1992 with continuous federal funding. These clinics offer comprehensive services including case management, outreach, mental health, pharmacy, women’s health and clinical care. Our community presence addresses health disparities and offers a unique training experience for our trainees. In partnership with the Department of Emergency Medicine’s opt out HIV screening program, we provide linkage to care for all patients diagnosed with HIV in the medical center. Many ID faculty are actively involved with this program.
Max Brito, MD, MPH, received a Health Resources and Services Administration (HRSA) award this year entitled USTART, to engage people newly diagnosed with HIV into care, and rapidly initiate treatment, or re-engage those lost to follow up.

Andrew Trotter, MD, MPH focuses on HIV care, HIV prevention, viral hepatitis, and sexually transmitted infections. He worked with Dr. Novak as a coinvestigator in the CDC-funded Network Epidemiology of Syphilis Transmission (NEST) study and worked on the HVTN 706/MOSAICO HIV vaccine study, HPTN 083 HIV prevention study, in addition to being a consultant in a HRSA grant partnering with the UIC Mile Square clinics to expand access and uptake of HIV PreExposure Prophylaxis. Dr. Trotter continues to work as the co-chair of the Chicago Department of Public Health’s Syphilis Task Force.
Project Wish is our clinical research center which for decades primarily focused on HIV prevention trials and STI clinical research. Since the onset of the COVID-19 pandemic, COVID-19 research has overshadowed the
HIV clinical trials. We are currently working with the Covid-19 Prevention Network (COVPN), HIV Vaccine Trials Network (HVTN), HIV Prevention Trials Network (HPTN), Division of Microbiology and Infectious Diseases (DMID), CDC and others.
Max Brito, MD, MPH, is the chief of infectious diseases at the Jesse Brown VA Medical Center. He currently leads the Chicago Latinx Task Force, a partnership of international consulates, academia and community organizations that aims to help deliver the prevention message on the COVID-19 epidemic to Latinx communities in Chicago.
Dr. Brito developed and leads an extramural Global Medicine elective, based in the Dominican Republic, to educate trainees on tropical infectious diseases, social determinants of health and the practice of medicine in resource-constrained settings. The 2-week trip includes a series of lectures on tropical medicine and global health and rounds with the ID services of two hospitals. More than 130 trainees have participated in the Department of Medicine’s Global Medicine elective over the past 18 years. Dr. Brito was recently elected to the board of directors of the Infectious Diseases Society of America.
Geri Donenberg, PhD, directs the Center for Dissemination and Implementation Science and the Healthy Youths Program. In 2021, she was the principal investigator and co-investigator on 10 NIH-funded grants and the co-director of a Fogarty International Training grant. Her work spans 4 countries in SubSaharan Africa, Indonesia, and the United States. She has over 130 peer-reviewed publications underscoring the impact of individual, social, and structural determinants on sexual and reproductive health, mental health, and substance use in adolescents and young adults, implementation science, and HIV prevention and intervention outcomes for youth and families. In 2021, she served as the primary mentor on 8 funded projects.
Vijay Yeldandi, MD, is a member of the urban global health team and spends most of the year in India. Dr. Yeldandi works with multiple hospitals (Hyderabad, India) on design and implementation of patient safety and infection control programs. He provides technical support to the National AIDS Control program, ministry of health and family welfare, and Government of India for improving care of HIV and tuberculosis. Under a cooperative agreement with the CDC, he is developing implementation strategies for “Prevention of airborne transmission of tuberculosis” in the government hospitals in Mumbai as well as HIV treatment centers in India. He directs the “Global Health Education” program at SHARE MediCiti in Hyderabad India, which was the site for a project on “Hands only CPR” executed by UIC residents as part of the urban global health program.
Stockton Mayer, DO, partners with the School of Public Health and the School of Nursing to deliver care to People Who Inject Drugs (PWID). The program aims to deliver comprehensive care to PWID, treating Opioid Use Disorder, skin and soft tissue infections, and Hepatitis C, among other illnesses. In July 2021, Dr. Mayer and his collaborators received SUPR funding to expand mobile van services. The multidisciplinary team offers 6 days of clinical services from its mobile van, distributing buprenorphine in strategic locations on the city’s west side. This upcoming year, Dr. Mayer will lead the section’s advanced fellowship in Infectious Disease and Opioid Use Disorder. Internationally, Dr. Mayer continues to make regular journeys to rural Guatemala to provide training for local physicians in HIV medicine. He works closely with the Jalapa Department of Public Health in Guatemala to deliver HIV services in the Jalapa community - the first HIV clinic in this region of the country.
Susan Bleasdale, MD, is a lead investigator for a study to reduce surgical site infections as part of the CDC Epicenters for Prevention of Healthcare Associated Infections (HAIs).
As the medical director of Infection Control and Antimicrobial Stewardship at Saint Anthony Hospital (SAH), Alfredo Mena Lora, MD, works with Dr. Bleasdale on implementation research. Dr. Mena Lora also works on defining antimicrobial resistance and antimicrobial use in his native Dominican Republic, where he has reported on multi-drug resistant organisms in the community and in various local hospitals.
Gus Alonto, MD, is the director of Infection Prevention and Control Department at Jesse Brown VA (JBVA), as well as the Antibiotic Stewardship program physician champion at JBVA. Dr. Alonto led the COVID-19 response and implemented the COVID-19 protocols and procedures for JBVA Medical Center and its community-based outpatient clinics.
Paula Allen-Meares, PhD, is the director of the Office of Health Literacy which provides education and training to the College of Medicine and the UIC health system. During the COVID-19 pandemic, Dr. AllenMeares worked with the objective of training credible messengers to bring accurate information about the COVID-19 vaccine to our communities.
Dr. Allen-Meares serves as a Co-PI for the Rockford Citywide Health Literacy Initiative that aims to evaluate and address health literacy, COVID-19 vaccine hesitancy and general mistrust of the healthcare system among African American/Black and Hispanic/ Latinx adults that live in the identified zip codes (61101, 61102 and 61104) through the context of social determinants of health.
In 2021, the UIC Office of Health Literacy received a two-year sub-award to collaborate with the Center for Disease Control (CDC) and the Cook County Department of Public Health (CCDPH). Dr. AllenMeares leads a team that is tasked with providing health literacy and cultural humility training for the CCDPH staff and community-based organizations who are partnering with CCDPH for this initiative.
Dr. Allen-Meares serves as a Co-PI for the UIC DPI
funded “Developing and Evaluating a Contextualized Dialogue Agent to Promote Health Literacy: Addressing Health Disparities Among Urban African American and Latinos with Heart Failure”. She also serves as a Co-I for the Chicago Center for Health Equity Research (CHER) grant and the NIH UIC Behavioral and Biomedical Science Bridges to Baccalaureate Grant. Dr. AllenMeares is an elected member of the National Academy of Medicine.
The HIV/AIDS and Hepatitis C (HCV) telemedicine program, is a partnership with Illinois Department of Corrections. Mahesh Patel, MD, directs the UIC telemedicine effort, providing telehealth to the 26 state correctional facilities in Illinois, serving 500700 patients. This program facilitates continuity of care when our patients are released back to their communities. During the pandemic, Dr. Patel worked on early evaluation of nursing home and correctional center outbreaks of COVID-19 under the IDPH contract. He serves on the medical school curriculum committee for the M2 year, and was honored with a Golden Apple award by the students, which he has received multiple times.
Lelia Chaisson, PhD, MSc, current research, based in Brazil and Uganda, focuses on implementing novel strategies to improve diagnosis of tuberculosis (TB) infection, uptake of TB preventive therapy, and adherence to TB preventive therapy for people living with HIV. From 2020-2021, she served as a researcher for the World Health Organization Guidelines Development Group on Systematic Screening for Tuberculosis. As a core faculty member of the Center for Global Health, Lelia also serves as a mentor for students in the Global Medicine (GMED) program.
The Division of Nephrology provides clinical services for the evaluation and treatment of the full spectrum of kidney diseases, hypertension, and fluid-electrolyte
disorders, with a strong commitment to serving minority populations. At the University of Illinois Hospital, the division provides over 4,000 dialysis treatments per year. Faculty and fellow-staffed outpatient clinics accommodate up to 100 patients per week. The division has a robust program for outpatient in-center and home dialysis which is based at the University and at a nearby Fresenius Medical Care unit. The division has a comprehensive multidisciplinary Chronic kidney disease (CKD) education program for English and Spanish speaking patients.
In collaboration with the Division of Endocrinology, the Division of Nephrology launched a new Diabetes Kidney Health Clinic in January of 2021. Diabetes and CKD are among two of the most prevalent co-morbid chronic diseases in the US. Given the increasing complexity of health-care delivery for people with these conditions, there is a clear need to integrate across specialty health services. With the development of new therapies for patients with diabetes and kidney disease, we anticipate that this new partnership will have a positive impact on the care of our patients. This multidisciplinary clinic is led by Drs. Ana Ricardo of Nephrology and Kristen Decarlo of Endocrinology.
The Division of Nephrology excels in providing care to transplant patients. Led by Dr. David Perkins and four full-time faculty members, the transplant nephrology service provides comprehensive care staffing both outpatient and inpatient services. In 2020-2021, the transplant program performed the highest number of kidney transplants in the United Network for Organ Sharing Region 7, with over 300 kidney transplants. The program also did highest number of pancreas transplants in the US. The program is known for its expertise in obese and high immunological risk patients.
The division has a strong commitment to training the next generation of clinicians and researchers in nephrology. The Nephrology Fellowship Program is one of the largest in Chicago providing a rich exposure to the full spectrum of clinical nephrology with training at three large public hospitals. Rotations take place at the University of Illinois Hospital and Jesse Brown VA Medical Center. In addition, trainees rotate at John H. Stroger, Jr. Hospital of Cook County, which has had a long-standing academic affiliation with the division.

Nephrology fellows have consistently been top prize winners at the National Kidney Foundation of Illinois Controversies in Nephrology annual debates. Nephrology fellows Drs. Kirolos Iskander and Anas Kizawi were second place winners in the 2020 debate which was focused on treatment with peritoneal dialysis as a first line of treatment for patients requiring renal replacement therapy.
Nephrology fellows also have access to a recently funded research training program. This NIH-funded inter-institutional training grant offers research training in kidney diseases, benign urology and hematology. The program provides training for both pre- and postdoctoral fellows. Nephrology fellows are also able to enroll in the School of Public Health Master of Science in Clinical and Translational Science program. The division has had significant success in transitioning trainees to academic positions.
The Division of Nephrology operates the largest clinical research program in kidney disease in the Chicago area with a prominent focus on health disparities. Ongoing research studies include the NIH sponsored Chronic Renal Insufficiency Cohort (CRIC) Study, Hispanic CRIC, Mexican CRIC, and the Hispanic Community Health Study/Study of Latinos. The division also has active basic and translational research programs focused on cell biology, autoimmunity, acute kidney injury, integrative systems biology and bioinformatics.
Other ongoing major NIH studies include Dr. Ana Ricardo’s R01 which is evaluating the impact sleepdisordered breathing on the progression of chronic kidney disease; and Dr. Michael Fischer’s U01 study which is investigating non-opioid pain management strategies for people on hemodialysis. Dr. Stephanie Toth-Manikowski was supported by an NIH Research Supplement to Promote Diversity in Health-Related Research to study the impact of access to health care in Hispanics with chronic kidney disease, and she also received a National Kidney Foundation of Illinois Young Investigator award to conduct a pilot study evaluating
the impact of cognitive behavioral therapy on insomnia in patients in CKD.
Despite the challenges of the ongoing COVID-19 pandemic, the Division of Pulmonary, Critical Care, Sleep, and Allergy has continued to advance the mission of the Department of Medicine along multiple fronts, including clinical care, scholarly activities, educational endeavors, and service. The division continues to evolve and grow and is now one of the largest divisions in the Department of Medicine, consisting of 37 faculty and 18 fellows.
The division provides many valuable and essential clinical services to our institution’s patients and is honored to participate in the care of the underserved patient population that comprises the majority of those receiving healthcare at UI Health and the Jesse Brown VA Hospital. An important priority is expanding access to the medical services we provide for these patients. Our clinical operations at UI Health and the Jesse Brown VA continue provide the highest quality care to hundreds of patients each week. Our sleep medicine, allergy, and interventional pulmonary programs, in particular, have seen significant clinical growth in recent years. In 2021, our Interventional Pulmonology program introduced state-of-the-art robotic bronchoscopy here at UIC. Vibrant sub-specialty clinics are devoted to sleep medicine, allergy, pulmonary hypertension, lung nodules, bronchiectasis, sarcoidosis, and COPD. The Lung Cancer Screening program continues to grow and provides an invaluable service, particularly for our most underserved patients.
The educational mission of the division is to train and develop leaders in the fields of pulmonary medicine, critical care, sleep medicine, and allergy. The division houses three high quality fellowship programs that are fully accredited by the Accreditation Council for
Graduate Medical Education (ACGME)—Pulmonary and Critical Care Medicine, Sleep Medicine, and Interventional Pulmonology, our newest fellowship program that began in FY2019. These training programs are thriving in terms of demand, curriculum growth, and graduate success. Our division has a highly successful NIH T32 training program for developing future leaders in pulmonary-related research. Fellows trained in this program have earned multiple NIH K awards in the recent past and constitute the physician-scientist leaders for the next generation. The educational success of our division is also reflected in the multiple teaching awards earned by our faculty.
Our faculty are nationally and internationally recognized as leaders in their respective fields. Division members are highly engaged in advancing the science of practice of medicine with diverse areas of expertise including vascular biology, immunology, clinical outcomes and implementation research spread across pulmonary, critical care, sleep and allergy specialties. We have a very active portfolio of research projects, funded by the National Institutes of Health, VA system, American Hospital Association, and various other private foundations and pharmaceutical companies.

In FY2021, the total number of active external grants was 54, including 10 new awards received in the past year. Our entire grant profile now totals more than $31 million annually (direct and indirect funding). The highly productive members of the division published more than 130 original scholarly works
in FY 2021, including multiple publications in high impact journals. This active scholarship produces many collaborative pursuits within the departments of Medicine, Pharmacology, the School of Public Health, and others here at UIC which have generated national and international recognition. We are particularly proud of our success in training and nurturing the next generation of pulmonary-focused scientists, with our division earning multiple NIH K level Career Development awards in the past several years, which pursued important research questions relevant to a diverse array of clinical problems—asthma, ARDS, pulmonary hypertension, and COPD.
Our faculty serve on numerous committees and other service and leadership positions that positively impact the Department of Medicine, College of Medicine, University, and the community at large. These include multiple clinical directorships (MICU, PFT laboratories, sleep center, etc.), educational leadership (program director, competency committees, leadership of research training grants, etc.), departmental and hospital administrative roles, campus-wide committees, community education and volunteer service, and national and international professional organization leadership. Through these efforts the members of our division positively affect change throughout the University and the communities we serve, while at the same time raising the profile and reputational status of our institution.
The Division of Rheumatology is dedicated to promoting excellence in clinical care, research, and education. We are fully committed to our mission of service to minority patients and educating future rheumatologists while pursuing scholarly activities. The division is well known internationally for expertise in sarcoidosis and rheumatoid arthritis.

approach to treating systemic sarcoidosis. The sarcoidosis team of experts are motivated through innovative care and collaboration to provide the best experience for each patient. Lori E. Lightfoot, Mayor of the City of Chicago, designated April 21, 2021 to be Sarcoidosis Day in Chicago to raise awareness about sarcoidosis and encourage all residents to support the Bernie Mac Foundation.
Dr. Huan Chang is leading clinical efforts in osteoarthritis. Dr. Pim Jetanalin is leading the clinical efforts in lupus and gout. Dr. Mina Al-Awqati is leading the clinical efforts in myositis and connective tissue disease associated in interstitial lung disease and Dr. Shiva Arami is leading clinical efforts in scleroderma.
In FY21, rheumatology's clinical volume rose by 14% as compared to FY20.
The Division of Rheumatology is staffed by physicians who focus on clinical care of patients with complex rheumatologic disorders. The division provides patient care and management for all rheumatologic disorders including rheumatoid arthritis, system lupus, inflammatory eye disease, vasculitis, myositis, systemic sclerosis, osteoarthritis, crystal arthropathies, behcet’s syndrome, antiphospholipid syndrome, interstitial lung disease and sarcoidosis.
Dr. Nadera Sweiss, the founder and director of the Bernie Mac Sarcoidosis Translational Advanced Research (STAR) Center leads the multidisciplinary
The division is involved in basic, clinical, and translational research, funded through the National Institutes of Health, the Department of Veterans Affairs, the Foundation of Sarcoidosis Research (FSR), Bernie Mac STAR Center, national research organizations, industry and philanthropy. Dr. Shiva Shahrara leads the efforts of translational research in the field of rheumatoid arthritis. These studies determine novel targets that inhibit neovascularization, leukocyte migration and bone erosion in the RA joint and identify biomarkers that reflect RA disease severity and/or response to effective treatments. Dr. Nadera Sweiss leads the efforts in clinical trials in sarcoidosis and several landmark studies in rheumatoid arthritis and sarcoidosis.
The Division of Rheumatology has a strong education program for fellows, residents, and medical students. The division offers two fellowship positions each year. Fellows are trained in various aspects of clinical rheumatology as well as clinical and translational research. Dr. Shiva Arami is the interim program director.
The University of Illinois Chicago Department of Medicine is committed to high-quality care for all, scholarly activity, and education. The Department of Medicine is dedicated to increasing the diversity of the clinical, research and educational workforce.

We invite you to visit our giving website. Your gift to the Department of Medicine brings us closer to our goal of providing state of the art medical care to all, excellent training to the next generation of physicians, innovative programs and conduct groundbreaking research. Please consider making a gift today.
To give please visit our website at https://go.uic.edu/givedom.
Contributors/Reviewers:
Patricia W. Finn, MD George T. Kondos, MD Bryan Blaha, MS DOM Administration Staff Division Administrators Division Chiefs and CouncilsProject Manager/Designer/Editor
Krystle Stewart, BS Project Consultant/Editor Lisa Butler, MPAUniversity of Illinois Chicago

840
www.dom.uic.edu
