P A G E 2 2 TABLE OF CONTENTS PART 1: RELATIONSHIP OF MULTIPLE SCLEROSIS, CONSTIPATION, AND DIGESTIVE ISSUES 4 WHAT IS MULTIPLE SCLEROSIS? 5 WHAT IS CONSTIPATION 7 HOW IS CONSTIPATION LINKED TO MS? 7 PART 2: MULTIPLE SCLEROSIS AND GENERAL BOWEL SYMPTOMS ...................................................................10 ARE DIGESTIVE ISSUES INVOLVED IN MS? ......................................................................................................................... 11 Diarrhea.............................................................................................................................................................. 11 Irritable Bowel Syndrome (IBS) 11 Inflammatory Bowel Disease 11 Anxiety & Depression 11 Fatigue 12 WHY DO SERIOUS BOWEL SYMPTOMS COMMONLY OCCUR WITH MS?.................................................................................. 12 PART 3: MULTIPLE SCLEROSIS AND CONSTIPATION......................................................................................... 15 REVIEW OF HOW MULTIPLE SCLEROSIS CAN CAUSE CONSTIPATION....................................................................................... 16 OTHER ROOT CAUSES OF CONSTIPATION 16 UNDERLYING ROOT CAUSES OF CONSTIPATION 17 SIBO 17 Dysbiosis 17 Infections and Pathogens 17 Low Stomach Acid............................................................................................................................................... 18 Medications ........................................................................................................................................................ 18 Food Sensitivities or Intolerances 18 Low Fiber Diet 18 Low Fat 19 Micronutrient Imbalances 19 Dehydration 19 Stress................................................................................................................................................................... 19 Ignoring the Urge................................................................................................................................................ 20 Diseases or Conditions........................................................................................................................................ 20
P A G E 2 3 PART 4: LAB TESTING..................................................................................................................................... 21 LAB TESTS TO GET TO THE ROOT CAUSE OF CONSTIPATION................................................................................................. 22 The SIBO Test 22 The Stool Test 23 Food Sensitivities or Intolerances Testing 24 PART 5: RECOMMENDATIONS FOR THE TREATMENT OF CONSTIPATION ......................................................... 26 DIET........................................................................................................................................................................... 27 Fiber.................................................................................................................................................................... 27 Chia Seeds........................................................................................................................................................... 27 Fats ..................................................................................................................................................................... 29 Gluten/ Dairy 29 Water 29 BATHROOM SCHEDULE 29 EXERCISE 30 OTHER THERAPIES ........................................................................................................................................................ 30 Abdominal Massage........................................................................................................................................... 30 Foot Reflexology ................................................................................................................................................. 31 Irrigation............................................................................................................................................................. 31 Stress Reduction 31 Sunlight 32 Medication 32 PART 6 : SUMMARY OF MULTIPLE SCLEROSIS AND CONSTIPATION.................................................................. 33 SUMMARY .................................................................................................................................................................. 34 REFERENCES: ................................................................................................................................................. 35
SCLEROSIS, CONSTIPATION, AND
P A G E 2 4 PART 1: R
ELATIONSHIP OF MULTIPLE
DIGESTIVE ISSUES TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
WHAT IS MULTIPLE SCLEROSIS?
● In the US, 1 million people are living with MS (National MS Society, 2023)1 .
● MS is the most common non-traumatic cause of disability in young adults today (Preziosi G, 2018)2 .
● MS is unpredictable and affects different people in different ways.
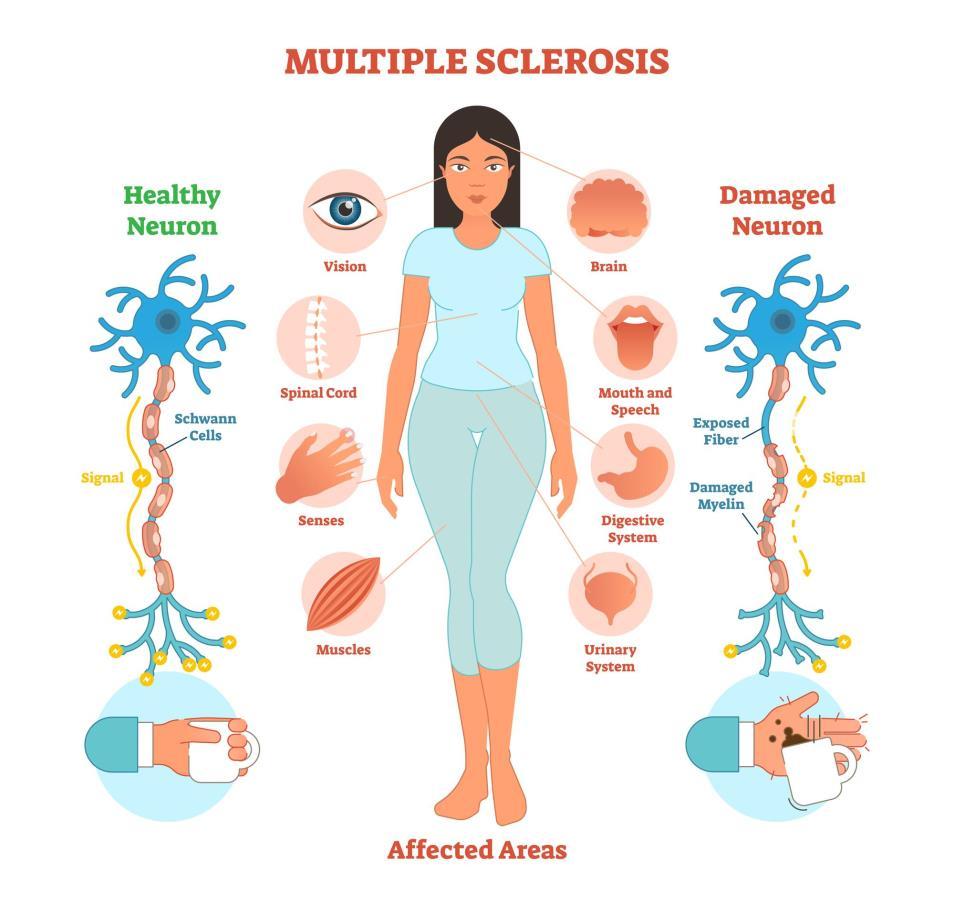
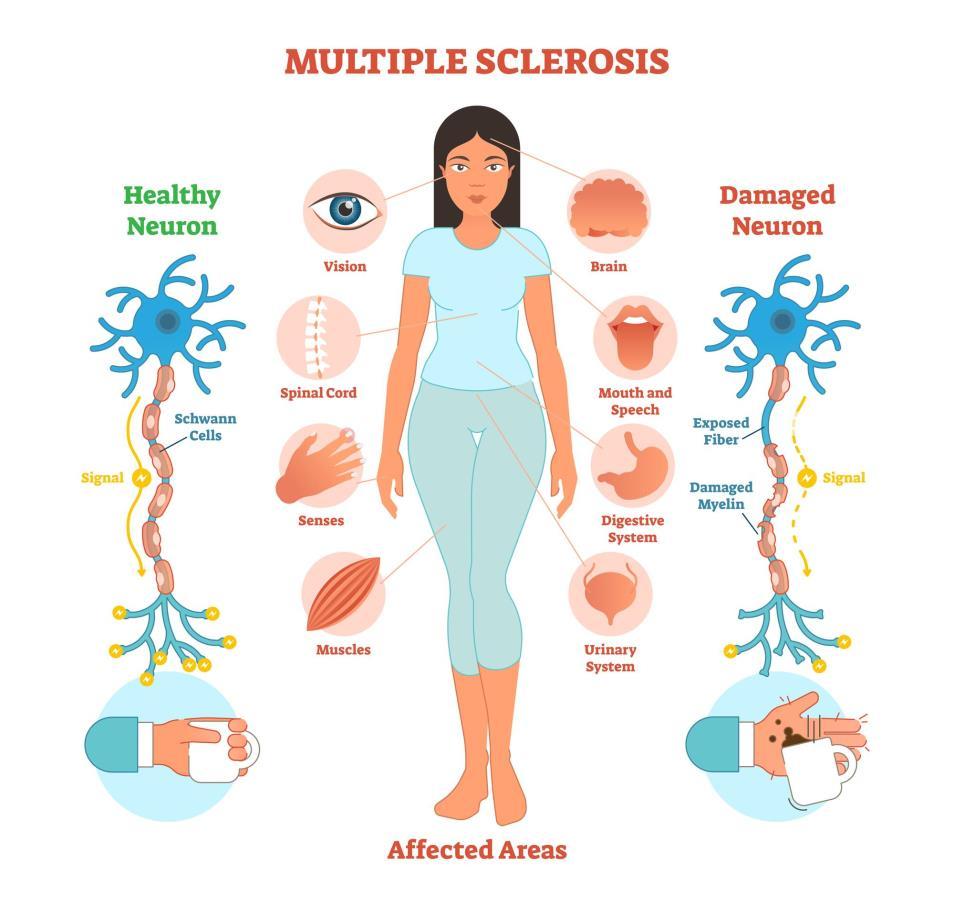
Multiple Sclerosis is a chronic disease affecting the central nervous system, including the brain and spinal cord. It is an autoimmune condition in which the body attacks itself by mistake.
In MS, the immune system attacks nerve fibers and the myelin sheath in the brain and spinal cord. The myelin sheath is the fatty tissue that surrounds and protects nerve fibers. The autoimmune attack damages the myelin sheath which normally protects nerves. In addition to myelin, nerve fibers and neurons in the central nervous system (i.e. the brain and spinal cord) are damaged. Myelin gets destroyed in many areas and there is chronic inflammation from the autoimmune damage to myelin and nerve cells.
Once the myelin protection is damaged, the nerves become damaged leading to communication problems between the brain and the rest of the body. Normally, nerves transmit electrical signals to help with sensory perception and movement. But damaged nerves cannot transmit electrical messages to and from the brain as they are meant to. This affects nerve signaling and how different parts of the body function, including the digestive tract. This type of damage to myelin, neurons and neurological pathways eventually leads to neurodegeneration and neurological symptoms.
P A G E 2 5
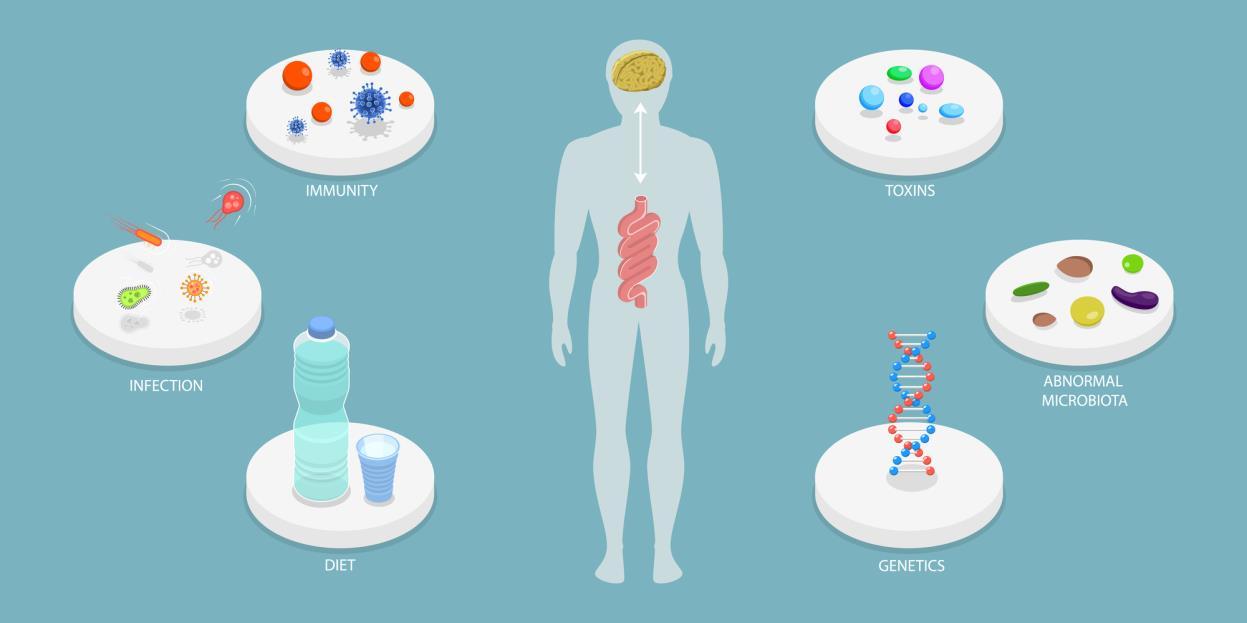
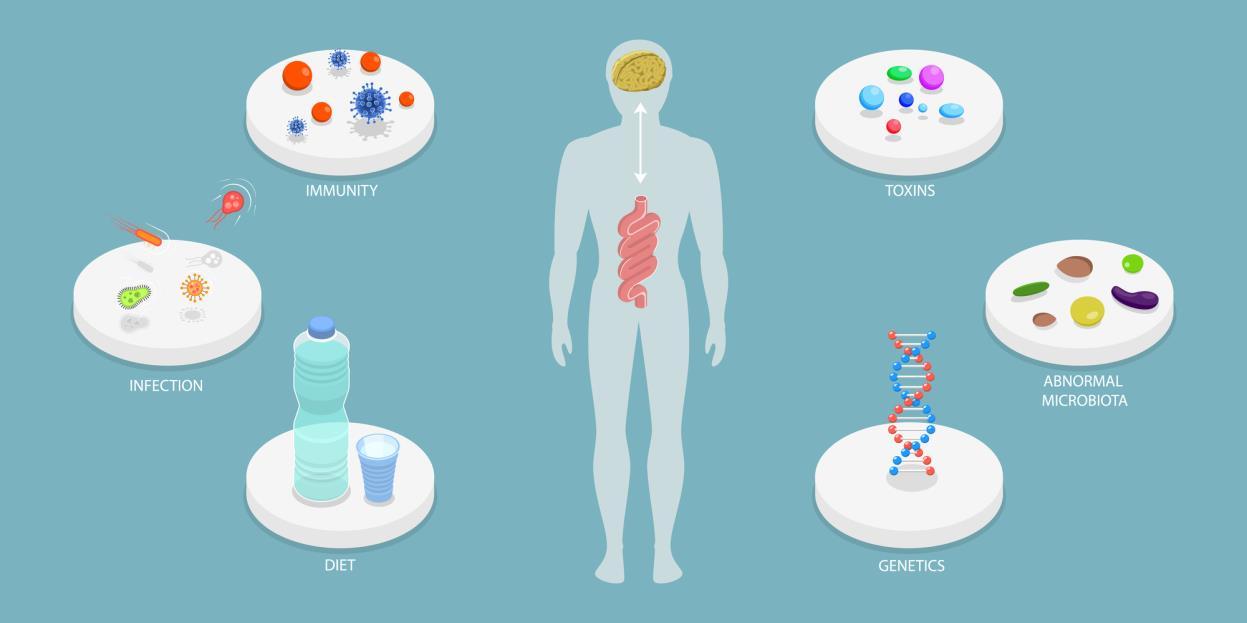
The precise cause of MS is not known, but certain factors are involved:
● People with certain genes may have a higher risk.
● More women than men develop MS.
● Smoking and a vitamin D deficiency may increase the risk.
● A viral infection, such as Epstein-Barr virus, can be a trigger for MS. The infection affects the immune system and immune response, and this can prompt the onset of MS or cause a relapse.
P A G E 2 6
WHAT IS CONSTIPATION
Constipation is not having a regular bowel movement or being unable to completely empty the bowel. It is generally defined as having fewer than three bowel movements a week. Constipation can cause stools to be hard and lumpy, or unusually large or small. Constipation is a very common issue with MS and often becomes chronic.
HOW IS CONSTIPATION LINKED TO MS?
The gut is linked to the brain via the gut-brain axis. The gut and the brain are actually in constant communication, even though we don’t realize it.
Part of the gut-brain axis is made up of nerves and neurotransmitters. A neurotransmitter is a signaling molecule released by a neuron or nerve cell. It sends a chemical message to another cell. The cell receiving the signal may be another neuron, a gland or a muscle cell. These nerves and neurotransmitters constantly communicate back and forth between the central nervous system and the gut.
Nerves in the nervous system regulate gut motility and sensations. Gut motility refers to the small movements of muscles and nerves along the GI tract. We might not be aware of or feel this constant communication, but it is important for the gut to function properly.
In people with MS, damage to nerves and nerve signaling can lead to neurogenic bowel dysfunction. People have disruptions or malfunction in both sensations and motility actions in the gut. This is when motility is impaired and the intestines do not contract as they should to keep stools moving. This slows down stool transit time through the intestines. Stools become larger and harder to pass leading to digestive
P A G E 2 7
problems. The main symptoms of neurogenic bowel dysfunction (NBD) are constipation and fecal incontinence. Fecal incontinence (FI) is the involuntary loss of stools, lasting for at least one month (Preziosi G, 2018)2 .
In many cases, digestive symptoms happen years before an MS diagnosis. In fact, constipation and FI as bowel symptoms are known to predate the onset of MS by 3 to 7 years (Gulick, 2022)3 . In one study of people later diagnosed with MS, 28% reported constipation and FI before their diagnosis of MS (Gulick, 2022)3 .
● Constipation and FI affect about 50% of MS patients at some point and are ongoing symptoms in about 25% of MS cases (Preziosi G, 2018)2. In the general population, constipation affects 2%–20%, and FI affects 2% of people (Preziosi G, 2018)2. As seen from these numbers, constipation/fecal incontinence are much more common in MS patients than in the general non-MS population (Preziosi G, 2018)2 .
● Severe constipation, urinary bladder dysfunction and fecal incontinence often occur together. In one study of MS patients, 74% had bladder problems, 49% had constipation and 32% had fecal incontinence (Camilleri, 2021)4 .
● In another study, 59% of people with MS had constipation and 35% fecal incontinence (Lin SD, 2019)5 .
● These bowel problems are significantly associated with the degree of disability in MS and are more common in those with higher levels of disability (Lin SD, 2019)5 .
These digestive symptoms are also common in patients with other chronic neurological diseases, such as spinal cord injury and Parkinson’s disease (Emmanuel,
P A G E 2 8
2019)6. The neurological diseases which most frequently affect digestive function are stroke, Parkinson’s, MS and diabetic neuropathy (Camilleri, 2021)4 .
Serious digestive issues have a major impact on a person’s life. They negatively affect quality of life and social interaction. Bowel symptoms are considered the primary cause of inability to work with MS, after poor coordination and mobility issues (Preziosi G, 2018)2 . These factors, amongst the other physical challenges of MS, can lead to significant psychological and emotional stress (Lin SD, 2019)5. They can be very inconvenient and contribute to social isolation, decreased quality of life, mood issues and increased morbidity (Lin SD, 2019)5 .
P A G E 2 9
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
MULTIPLE SCLEROSIS AND
GENERAL BOWEL SYMPTOMS
P A G E 2 10
ART 2:
P
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
ARE DIGESTIVE ISSUES INVOLVED IN MS?
DIARRHEA
While constipation is the most common type of bowel dysfunction in people with MS, diarrhea is also an issue. Bowel function can actually ‘speed up’ and cause diarrhea, loose stools and incontinence. Other symptoms might be hemorrhoids, abdominal pain, bloating and nausea (Preziosi G, 2018)2 .
IRRITABLE BOWEL SYNDROME (IBS)
IBS is a common condition that is more common in people with MS. It affects 20% of people with MS (Levinthal DJ, 2013)7. That is twice the rate of the overall population (Levinthal DJ, 2013)7 .
INFLAMMATORY BOWEL DISEASE
People with MS are up to 50% more likely to get Inflammatory Bowel Disease (IBD) than others (Preziosi G, 2018)2. Likewise, people with IBD have an equally increased risk of developing MS (Preziosi G, 2018)2 .
ANXIETY & DEPRESSION
Anxiety and depression are often present once neurogenic bowel dysfunction starts to develop. They also improve once NBD is successfully treated (Preziosi G, 2018)2 . This shows the significant psychological aspect linked to bowel problems in MS patients, which is also seen in the general population (Preziosi G, 2018)2. Please see our e-book on mental health and gut health for more details on the connection between the gut and mental health.
P A G E 2 11
FATIGUE
There is a positive correlation between the severity of fatigue and bowel problems in people with MS. Fatigue is one of the most common symptoms in MS, and it may be that significant bowel dysfunction may cause the fatigue. There may also be a vicious cycle in which fatigue causes an inability to exercise, which worsens symptoms of constipation. Worries around bowel problems may contribute to mental fatigue. Fatigue may make going to the toilet more difficult in some cases. MS patients may feel depressed as a result of their digestive symptoms. Depression typically contributes to fatigue. Some medications used to treat MS may have sedative/depressive effects or contribute to constipation (Lin SD, 2019)5 .
WHY DO SERIOUS BOWEL SYMPTOMS COMMONLY OCCUR WITH MS?
To understand why constipation, FI and other digestive symptoms can be such an issue with MS, it helps to understand the digestive process in detail.
The central nervous system (CNS) is the brain and spinal cord. The CNS is part of the digestive process. It controls motility and transit time, which speeds up or slows down digestion and bowel movements.
In MS, communication between the CNS and the gut is disrupted due to the damage to myelin, nerves and nerve signaling. This damage interrupts the messages nerves send to and from the brain that signal that it's time for a bowel movement. The impaired communication affects digestion, slowing down the bowels. These nerve issues reduce the frequency and intensity of the desire to defecate (Gulick, 2022)3. MS can also
P A G E 2 12
keep pelvic floor muscles from relaxing, which helps the body to eliminate or get rid of stool.
Having a bowel movement involves neural control and detailed coordination of several muscles. MS can damage these neural pathways in the brain. Demyelination, and the resulting effect on neurons of the brain, may affect voluntary control over defecation (Preziosi G, 2018)2. For example, a bowel movement leaving the body requires contractions of abdominal muscles to generate a strong force to move stool. Struggling to contract those abdominal muscles can lead to constipation or other issues (Levinthal DJ, 2013)7 .
The spinal cord is important for normal bowel function. In patients with MS, it has been shown that there are delays in neuronal signals generated in the spinal cord (Preziosi G, 2018)2. There are also delays in the motor pathways to the anal sphincter.
MS can affect the speed of contractions in the colon. The colon re-absorbs fluids and waste for elimination. If stool sits in the colon for too long, the waste can become very solid or hard, which is then more difficult to eliminate or pass (Levinthal DJ, 2013)7 .
MS also increases the chances of fecal incontinence or involuntary stool leakage. This happens as a result of weakening anal sphincter muscles. The anal sphincter muscle tone is important. It works like a gate to regulate the flow of waste out of the rectum (Levinthal DJ, 2013)7. Not being able to delay a bowel movement by contracting the sphincter muscle contributes to fecal incontinence (Gulick, 2022)3. People with MS have reduced rectal sensitivity, which means they have less awareness of rectal fullness. This can be followed by a sudden urgency, resulting in FI (Preziosi G, 2018)2 .
There may also be non-neurological causes like medications and diet or lifestyle issues (Preziosi G, 2018)2 .
P A G E 2 13
The degree of digestive symptoms an MS patient has appear to be correlated to the severity of disability and how long they have had MS (Preziosi G, 2018)2. At the same time, however, some MS patients with low disability and a short duration of the illness can also have serious bowel symptoms. In fact, severe constipation has been reported as the first presenting symptom of MS (Preziosi G, 2018)2 .
P A G E 2 14
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
P A G E 2 15
ART 3:
P
MULTIPLE SCLEROSIS AND CONSTIPATION
REVIEW OF HOW MULTIPLE SCLEROSIS CAN CAUSE CONSTIPATION
● MS interrupts messages that the nerves send to and from the brain. Among other important information for bodily functions, these messages signal that it’s time for a bowel movement.
● MS can affect pelvic floor and anal sphincter muscles, which are part of the process of a bowel movement.
● Motility, or the movement of food through the intestinal tract, may be slowed with MS.
● Insufficient fluid intake contributes to constipation. MS patients with difficulty being mobile may simply not be able to get to the toilet often or easily, so they may intentionally drink less water.
● Too little exercise is a factor in constipation. Again, people with MS and mobility issues may not be able to exercise very much, or at all.
● Some medications used for MS can cause constipation.
OTHER ROOT CAUSES OF CONSTIPATION
Constipation is the most common gastrointestinal problem in the US (NIH, 2018)8. It can significantly effect and lower one’s quality of life.
● 16 in 100 adults have symptoms of constipation (NIH, 2018)8 .
● 33 in 100 adults aged 60 and older have symptoms of constipation (NIH, 2018)8 .
● The causes of constipation can be complex.
P A G E 2 16
● Diet and a sedentary lifestyle have a significant influence on constipation. Changing diet and lifestyle are the first‐line recommendations to treat constipation.
Apart from issues related to MS, there may be other underlying root causes for constipation. This applies to people with MS as well as people who don’t have MS. Many things can contribute to, or directly cause, constipation.
UNDERLYING ROOT CAUSES OF CONSTIPATION
SIBO
SIBO, or Small Intestinal Bacterial Overgrowth, is an abnormally high amount of bacteria in the small intestine, especially bacteria types not typically found in the small intestine. Generally speaking, bacteria should be in the large, not the small, intestine.
DYSBIOSIS
Dysbiosis is when the ‘bad’ pathogenic bacteria in the gut outnumber the ‘good’ health-promoting bacteria. This imbalance can lead to constipation and other digestive issues.
INFECTIONS AND PATHOGENS
Infections, like the H pylori bacteria, or other pathogens, like parasites or bad gut bacteria, can cause constipation. The pathogenic bacteria can produce toxins which affect the muscles in the intestines and slow down peristalsis or intestinal movement.
P A G E 2 17
This means the pathogens don’t get excreted with the stool as quickly as they should. It is a self-protective act to help the pathogens survive. It can lead to constipation and an environment in which the pathogens can survive and grow.
LOW STOMACH ACID
If stomach acid is low, then the whole digestive system is not functioning as it should. Constipation can be a common symptom. Low stomach acid may delay bile and pancreatic enzyme production. These are needed to break down foods and promote gut motility. It is important to understand why stomach acid is low. This could be due to stress, aging, an H pylori infection, an autoimmune condition or other reasons.
MEDICATIONS
Some medications can cause constipation.
FOOD SENSITIVITIES OR INTOLERANCES
An intolerance or sensitivity to certain foods (gluten, dairy, eggs, nuts for example) can be a trigger for IBS, constipation and other digestive issues. The most common food sensitivities associated with constipation are gluten and dairy.
LOW FIBER DIET
Fiber is found in fruits and vegetables. Processed foods have little to no fiber. A diet too low in fiber can contribute to constipation. Fiber absorbs water and causes stools to be larger, softer and easier to pass. Increasing fiber intake helps cure constipation in many people. But, in some cases with more severe constipation, increasing fiber can make constipation worse and leads to gas and abdominal discomfort.
P A G E 2 18
LOW FAT
Low fat diets can contribute to constipation. Getting enough fat helps normalize intestinal motility and lubricate the bowels.
MICRONUTRIENT IMBALANCES
Nutrients, such as low magnesium, low vitamin B12, high or low vitamin D, and high calcium can be an issue. Magnesium, for example, is helpful because it relaxes the muscles. It attracts water and increases the amount of water in the intestines. This softens stools, making it easier to pass a bowel movement. Low vitamin D status is strongly linked to chronic constipation (Panarese A, 2019)9 . This is thought to be due to the increase in inflammation and poor immune response that comes with a vitamin D deficiency. Interestingly, low vitamin D is common in MS patients (Bäcker-Koduah P, 2020)10. The D deficiency may affect disease progression and outcome in MS (BäckerKoduah P, 2020)10. Maintaining a healthy vitamin D level can decrease the risk of developing MS. One study found that people with vitamin D levels greater than 40 ng/ml were 62% less likely to develop Multiple Sclerosis (Munger KL, 2006)11 .
DEHYDRATION
Drinking plenty of fluid, especially water, softens the stool and makes it easier to pass. The water allows waste to be flushed from the body. Inadequate water intake and dehydration can lead to hard stools and constipation.
STRESS
Stress has multiple effects on gut and overall health. It can lower stomach acid, contribute to leaky gut, deplete magnesium levels, and change levels of neurotransmitters in the bowel. Stress hormones can directly influence bowel
P A G E 2 19
movements. In addition, people under stress are more likely to have a poor diet, drink too little water, and get less exercise which all contribute to constipation.
IGNORING THE URGE
Holding in a bowel movement may lead to constipation. Repeatedly ignoring the urge to move the bowels may mean you eventually stop feeling the urge to go.
Sedentary lifestyle.
A lack of exercise can cause constipation. The colon responds to activity and good muscle tone is important for regular bowel movements. The abdominal wall muscles are involved in the process of a bowel movement. If these muscles are weak, they cannot perform well and may lead to constipation.
DISEASES OR CONDITIONS
Certain diseases such as celiac, depression, hypothyroidism, cancer and many others can cause constipation as an effect of the illness. As discussed, neurological disorders, such as Multiple Sclerosis, Parkinson's Disease, spinal cord injury or a stroke may also be responsible.
P A G E 2 20
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
PART 4:
LAB TESTING
P A G E 2 21
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
LAB TESTS TO GET TO THE ROOT CAUSE OF CONSTIPATION
One way to get to the root cause of constipation is to run lab tests and it is very important to identify root cause(s). Once we know the root cause, we can target treatment and resolve the constipation. Various gut issues can cause constipation in anyone. For example, SIBO (Small Intestinal Bacterial Overgrowth) can cause either constipation or diarrhea. Dysbiosis, other gut infections and pathogens can also be responsible for constipation or other digestive symptoms. In order to get to the underlying cause, it is important to run lab tests.
While laboratory testing is not perfect for infections and toxins, there are some good tests to identify possible root causes for constipation.
‘Test Don’t Guess’ is our motto in Functional Medicine. Because there are various root causes for digestive issues such as constipation, it is very helpful to test for which are most likely in any given case. We run tests at the Medicine with Heart clinic so we can drill down to the precise root cause(s). With the information from the tests, we can target the right treatment and not waste time with treatments that are not relevant. There are some standard tests that we can do to identify the different gut infections that may contribute to constipation.
THE SIBO TEST
SIBO is a sign of gut dysbiosis and is common in IBS (Takakura W, 2020)12. Due to gut dysbiosis, people with IBS may have increased intestinal permeability, dysmotility, chronic inflammation, autoimmunity, decreased absorption of bile salts, and even altered central neuronal activity (Takakura W, 2020)12. SIBO and IBS share symptoms including abdominal pain, gas, constipation or diarrhea, and bloating (Takakura W, 2020)12. In fact, SIBO can be a major cause of IBS.
P A G E 2 22
Various things can cause SIBO. It can happen when there is a motility issue with the Migrating Motor Complex or MMC. The MMC is meant to move bacteria from the small intestine into the large intestine between meals and during the night. But if MMC function is impaired, bacteria do not get cleared from the small intestine correctly, and SIBO can develop. Other causes of SIBO include low stomach acid. Stress, for example, lowers stomach acid. Food poisoning is a frequent cause of damage to the MMC.
There is not a lot of research on the SIBO – MS link. One study indicates that people with Multiple Sclerosis may have a high prevalence of SIBO (Zhang Y, 2016)13. We know that IBS is more common in people with MS: IBS affects 20% of people with MS (Levinthal DJ, 2013)7. IBS was once thought to be a psychological issue. But we now know that a key reason for IBS is gut dysbiosis, and is often SIBO. Up to 78% of patients with IBS have SIBO (Ghoshal UC, 2017)14 .
To test for SIBO, we use a noninvasive test. It involves breathing into a device that measures the amount of hydrogen or methane in the breath after drinking a mixture of glucose and water. A rapid rise in exhaled hydrogen or methane may indicate bacterial overgrowth in the small intestine. For example, constipated people can have very different gut bacteria composition than non-constipated healthy people, with higher levels of methane producing bacteria in their intestines, which slows intestinal transit time. In our clinic, we run this test in order to identify or rule out SIBO as a root cause of constipation or other digestive symptoms.
THE STOOL TEST
We also run the GI Map Stool Test on many of our patients. The GI Map provides insight into gut health. It is a comprehensive stool test that shows a variety of
P A G E 2 23
bacteria, both harmful and normal, as well as fungi, parasites and viruses. It might identify dysbiosis, parasites, harmful bacteria, H pylori, fungi or other microorganisms that can be the cause of constipation.
For example, constipation can result from intestinal dysbiosis, involving an imbalance of gut bacteria (Zhao Y, 2016)15. The gut bacteria help to control motility, the rate at which food moves through the digestive tract. When gut motility is too slow, constipation occurs. The bad bacteria literally secrete toxins into the gut which slow down the motility, so that they can stay in the body longer.
Running the GI Map Stool Test allows us to see the potential issues in a patient’s gut and target treatment to the particular microorganisms causing the constipation. This saves time in the treatment process so someone can feel better quickly.
FOOD SENSITIVITIES OR INTOLERANCES TESTING
Food sensitivities or intolerances are often not a root cause in themselves. They are typically caused by another gut issue such as infection and leaky gut that may result from the infection. We can perform testing to look at food issues but these often just show us a person has leaky gut. It can be helpful in the case of gluten issues.
The most effective way to check for food intolerances or sensitivities is to do an elimination diet. This involves removing typical allergenic foods like gluten, dairy, nuts or others from the diet for a period of 6 weeks. After the elimination phase, we add back one food at a time for 3 days. If no reaction occurs, then we can add back the next food. In our clinic, we can explain in great detail how to do an elimination diet for the best results.
P A G E 2 24
The other option is to do a food sensitivity panel lab test to identify food triggers. Then we can remove those foods from the diet. But this lab test is not perfectly accurate. If a person has leaky gut, then results will show many food sensitivities. It really is much better and more accurate to do the elimination diet.
Although food triggers make symptoms like constipation worse, they are usually not the root cause and we need to find and resolve the underlying root cause. Once this is done, it is not necessary to avoid a particular food forever.
P A G E 2 25
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
P A G E 2 26 PART 5: RECOMMENDATIONS FOR THE
REATMENT
ONSTIPATION
T
OF C
DIET
There are certain foods within a healthy diet that can help constipation. If you are not consuming any of these helpful foods, that may explain your constipation. Even if constipation is due to a condition like MS, it is still important to get the basics, like diet, right
FIBER
A well-rounded, healthy diet includes foods for good digestion and regular bowel movements. This includes eating lots of fresh fruit and vegetables to get enough fiber. Pulses (beans, lentils and peas) are also high in fiber. If you are struggling with constipation, one thing to try is high-fiber prunes or figs (in whole fruit or juice form). Prunes have a lot of insoluble fiber and sorbitol, which is a natural compound with laxative properties. Try 1/2 to 1 cup of prune juice in the morning to get things moving. You can also eat dried figs or prunes. Taking one to two servings every day can help increase fiber intake and resolve constipation.
CHIA SEEDS
Chia seeds are a great source of fiber. They have more fiber than dried fruits, cereals or nuts. Chia seeds are mainly insoluble fiber, with some soluble fiber. The insoluble fiber bulks up stool to prevent constipation. Insoluble fiber attracts water into the stool, so it is softer and easier to pass with less straining. Insoluble fiber can help with good bowel movements and regularity.
Chia seeds also have healthy fats, plant protein and antioxidants. One tablespoon of chia seeds provides 6 grams of fiber, 3 grams of protein, 5 grams of fat (mainly Omega3) and 80 calories.
P A G E 2 27
Chia seeds absorb water and swell up. It is best to eat chia seeds that have already been soaked in liquid or are served with a moist food, such as oatmeal or yogurt. Avoid eating dry chia seeds by themselves as they could potentially swell up once they are in the esophagus.
We recommend a chia pudding with full fat coconut milk and some berries. A healthy coconut chia pudding is great for breakfast or dessert.
COCONUT CHIA PUDDING16
This recipe serves 4.
Ingredients
1 14-ounce can full fat coconut milk
5 tablespoons chia seeds
1 tablespoon raw honey or maple syrup
1/2 teaspoon pure vanilla extract
Tiny pinch Himalayan or sea salt
Blueberries, strawberries, raspberries, or a mixture of various berries
Instructions
Stir together the coconut milk, chia seeds, honey or maple syrup, vanilla, and salt so that the chia seeds are evenly distributed throughout. Cover and refrigerate overnight. Give the mixture one more stir before bed.
In the morning, stir once more to evenly combine the seeds throughout. Pour one portion into a bowl, add the berries of choice and enjoy!
P A G E 2 28
FATS
Get enough good fats in the diet. A low-fat diet can contribute to constipation. Use olive and flaxseed oils, which have a slight laxative effect. Other good fats to include are avocado and fatty fish such as wild salmon, sardines, and mackerel.
GLUTEN/ DAIRY
Gluten or dairy can often be a cause of constipation. Trial a gluten-free/dairy-free period for 30 days and see how your digestion reacts.
WATER
Staying hydrated is important. Drink about 8 glasses of water per day. Better hydration can help with fatigue for people with MS. A good habit to get into is to drink warm water with lemon as the first thing you consume in the morning. This can help the bowels start moving and is detoxifying.
BATHROOM SCHEDULE
Go when you need to go and don’t hold it in. Set a regular time to go to the bathroom. Going right after meals helps, as eating is a natural way to prompt a bowel movement.
We are all occasionally in a situation where it seems embarrassing to defecate or you can’t find a private place to go. So, we hold it in. But what happens to the body when we do this? This uses muscles in the rectum to push the stool away from the rectum and send it back into the large intestine. This causes the water contained in the stool to be re-absorbed back into the body, drying out the fecal matter. This can make it harder to go later on when there is an opportunity, because now the stools are dry.
P A G E 2 29
It’s okay to do this once in a while, but frequently holding it in can lead to constipation because the water that should be lubricating the stool is no longer there. Holding in feces can eventually also lead to more serious medical problems, like anal fissures, hemorrhoids and other issues.
EXERCISE
Exercise is an effective treatment for constipation as it gets the digestive tract moving. Exercise shortens the time it takes food to move through the large intestine. Aerobic exercise speeds up breathing and heart rate. This stimulates the natural muscle contraction in the intestines. Intestinal muscles that can contract better move stools out quickly (Gao R, 2019)17 .
OTHER THERAPIES
ABDOMINAL MASSAGE
Abdominal massage, biofeedback, trans anal irrigation and reflexology can be helpful. Biofeedback can be used for pelvic floor incoordination. It teaches patients to relax the anal sphincter and to improve anal-rectal coordination and sensory perception (Gulick, 2022)3 .
P A G E 2 30
FOOT REFLEXOLOGY
One study showed that foot reflexology can be effective to manage constipation in patients with MS (Sajadi M, 2020). Foot reflexology for 6 weeks significantly decreased the severity of constipation in MS patients with constipation (Sajadi M, 2020)18 .
IRRIGATION
Trans anal irrigation is irrigating or clearing the lower bowel with water. It has proved to be an effective way to manage chronic constipation and fecal incontinence.
STRESS REDUCTION
Stress can affect gut function and cause constipation. Epinephrine, or adrenaline, is the stress hormone that is released when we go into flight-or-flight mode. It causes blood flow to be re-directed from the intestines toward vital organs, like the heart, lungs, and brain. This slows down intestinal movement and can cause constipation.
Another stress hormone called corticotrophin-releasing factor (CRF), is released and acts directly on the gut. It slows down the intestines and causes inflammation. Stress causes increased intestinal permeability (also known as leaky gut). This lets inflammatory substances enter the gut and can cause various digestive issues including constipation.
Stress also affects the normal healthy bacteria in the gut. Stress can reduce the number of healthy gut bacteria in the body, which slows down digestion.
P A G E 2 31
We recommend focusing on various practices to reduce and manage stress. We will never completely get rid of the stress in our lives so the next best thing is to learn how to manage stress. Practices like yoga, exercise, meditation and deep breathing can help to decrease stress.
SUNLIGHT
Regular exposure to sunshine can boost low vitamin D levels. It is recommended to get tested for vitamin D. This can be done by a simple blood test. Levels should be about 55. We don’t support pushing vitamin D levels too high, nor should they be too low. In Functional Medicine, we aim for an optimal range between 50 and 80 ng/mL.
MEDICATION
There may be medications that can help with constipation, which may be required in some cases.
Digestive symptoms and problems with bowel function may be frustrating or embarrassing to talk about. There is no ‘one size fits all’ solution to managing bowel function in MS. But it is important to talk to a Functional Medicine doctor to find a way to manage issues like constipation, in order to improve overall health and quality of life.
P A G E 2 32
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
P A G E 2 33 PART 6 : S
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
UMMARY OF MULTIPLE SCLEROSIS AND CONSTIPATION
SUMMARY
● MS is a chronic autoimmune condition in which the nerves of the central nervous system are attacked by the immune system. This causes problems with nerve signaling and can affect many functions of the body.
● Digestion and good gut function can be impaired by this nerve damage. Constipation and other digestive symptoms are common with MS.
● There are other root causes of constipation. These may include SIBO, gut dysbiosis, or other gut issues. The root causes may be lifestyle issues like diet, dehydration, or a sedentary lifestyle.
● There are some simple tips that can help, like increasing water and/or fiber intake for some (fiber in others may make things worse especially when SIBO is present). Certain therapies like abdominal massage, reflexology, trans anal irrigation, and others may be able to help.
● Talk to your Functional Medicine doctor if digestive problems are a symptom of your MS. It may feel embarrassing to discuss, but solutions may be found that can make life with MS more comfortable.
Our Functional Medicine clinic works with complex issues like MS and other chronic disease. Please get in touch with us if you would like to explore Functional Medicine solutions for your case of MS or other health concerns.
P A G E 2 34
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)
REFERENCES:
1. National MS Society. (2023). MS Prevalence.
2. Preziosi G, Gordon-Dixon A, Emmanuel A. Neurogenic bowel dysfunction in patients with multiple sclerosis: prevalence, impact, and management strategies. Degener Neurol Neuromuscul Dis. 2018 Dec 6;8:79-90. doi: 10.2147/DNND.S138835. PMID: 30584387; PMCID: PMC6287516.
3. Gulick EE. Neurogenic Bowel Dysfunction Over the Course of Multiple Sclerosis: A Review. Int J MS Care. 2022 Sep-Oct;24(5):209-217. doi: 10.7224/1537-2073.2021-007. Epub 2022 Jun 20. PMID: 36090242; PMCID: PMC9461721.
4. Camilleri M. Gastrointestinal motility disorders in neurologic disease. J Clin Invest. 2021 Feb 15;131(4):e143771. doi: 10.1172/JCI143771. PMID: 33586685; PMCID: PMC7880310.
5. Lin SD, Butler JE, Boswell-Ruys CL, Hoang P, Jarvis T, Gandevia SC, et al. (2019) The frequency of bowel and bladder problems in multiple sclerosis and its relation to fatigue: A single centre experience. PLoS ONE 14(9): e0222731. https://doi.org/10.1371/journal.pone.0222731
6. Emmanuel A. Neurogenic bowel dysfunction. F1000Res. 2019 Oct 28;8:F1000 Faculty Rev-1800. doi: 10.12688/f1000research.20529.1. PMID: 31700610; PMCID: PMC6820819.
7. Levinthal, David & Rahman, Ambreen & Nusrat, Salman & O'Leary, Margie & Heyman, Rock & Bielefeldt, Klaus. (2013). Adding to the Burden: Gastrointestinal Symptoms and Syndromes in Multiple Sclerosis. Multiple sclerosis international. 2013. 319201. 10.1155/2013/319201.
8. https://www.niddk.nih.gov/health-information/digestive-diseases/constipation/definition-facts
9. Panarese A, Pesce F, Porcelli P, Riezzo G, Iacovazzi PA, Leone CM, De Carne M, Rinaldi CM, Shahini E. Chronic functional constipation is strongly linked to vitamin D deficiency. World J Gastroenterol. 2019 Apr 14;25(14):1729-1740. doi: 10.3748/wjg.v25.i14.1729. PMID: 31011257; PMCID: PMC6465937.
10. Bäcker-Koduah P, Bellmann-Strobl J, Scheel M, Wuerfel J, Wernecke KD, Dörr J, Brandt AU, Paul F. Vitamin D and Disease Severity in Multiple Sclerosis-Baseline Data From the Randomized Controlled Trial (EVIDIMS). Front Neurol. 2020 Feb 25;11:129. doi: 10.3389/fneur.2020.00129. PMID: 32158426; PMCID: PMC7052055.
11. Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-Hydroxyvitamin D Levels and Risk of Multiple Sclerosis. JAMA. 2006;296(23):2832–2838. doi:10.1001/jama.296.23.2832
12. Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome - An Update. Front Psychiatry. 2020 Jul 10;11:664. doi: 10.3389/fpsyt.2020.00664. PMID: 32754068; PMCID: PMC7366247.
13. Zhang Y, Liu G, Duan Y, Han X, Dong H, Geng J. Prevalence of Small Intestinal Bacterial Overgrowth in Multiple Sclerosis: a Case-Control Study from China. J Neuroimmunol. 2016 Dec 15;301:83-87. doi: 10.1016/j.jneuroim.2016.11.004. Epub 2016 Nov 16. PMID: 27890460.
14. Ghoshal UC, Shukla R, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017 Mar 15;11(2):196-208. doi: 10.5009/gnl16126. PMID: 28274108; PMCID: PMC5347643.
15. Zhao Y, Yu YB. Intestinal microbiota and chronic constipation. Springerplus. 2016 Jul 19;5(1):1130. doi: 10.1186/s40064-016-2821-1. PMID: 27478747; PMCID: PMC4951383.
P A G E 2 35
16. https://www.wellplated.com/coconut-chia-pudding/
17. Gao, Ruitong & Tao, Yujia & Zhou, Changli & Li, Jinwei & Wang, Xige & Chen, Lei & Li, Feng & Guo, Lirong. (2019). Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scandinavian Journal of Gastroenterology. 54. 1-9. 10.1080/00365521.2019.1568544.
18. Mahbobeh Sajadi, Fahimeh Davodabady, Vahid Naseri-Salahshour, Mehdi Harorani, Mohsen Ebrahimimonfared,The effect of foot reflexology on constipation and quality of life in patients with multiple sclerosis. A randomized controlled trial, Complementary Therapies in Medicine, Volume 48, 2020,102270, 102270, ISSN 0965-2299.
P A G E 2 36
TO BOOK A DISCOVERY CONSULTATION WITH A STAFF MEMBER AT THE CLINIC, CALL 720 722 1143 WE WORK WITH PEOPLE LOCAL TO DENVER, CO AREA AND ALL OVER THE US (SOME INTERNATIONAL)