TheOralMicrobiome's RoleinInflammationand Disease
Your Guide to Ultimate Health Through the Mouth-Body Connection


Your Guide to Ultimate Health Through the Mouth-Body Connection

Our mouth is the gateway to our body It allows us to perform critical functions like eating, drinking, breathing and yes, smiling But when we think about wholebody health, our oral health tends to be overlooked
Part of that is driven by the healthcare industry’s separation of dentistry from the rest of the medical world - dental insurance, for example, is different than medical insurance.
There has also been a societal emphasis on the aesthetic and external appearance of our smiles (look no further than the explosion of products touting they help whiten teeth) rather than the health of our teeth and gums.
The key to personalized, preventionfocused, and evidence-based medicine
for oral health lies in addressing the root cause of oral disease, the oral microbiome Luckily, we now have the ability to look into our mouths at the microbial level.
At Bristle we're has created a first-ofits-kind at-home, comprehensive oral microbiome test to help measure, understand, and improve oral health
Our oral microbiome controls our risk for oral diseases and impacts our overall health, but everyone’s oral microbiome is different With Bristle, we can understand our unique oral microbiome, how it’s impacting our disease risk, take steps to improve our oral health, and then monitor progression over time Let’s dig into what the oral microbiome is and how it’s connected to our health
Over 700+ unique species of bacteria live in the oral cavity and they can work for or against you.
The gut microbiome has come into the spotlight over the last decade, and for good reason. It is the largest microbiome in our bodies and holds clues to many aspects of our overall health including everything from gut disorders to mental health to our risk for certain types of cancer
After the gut, our mouth is the secondlargest and diverse microbial community in our body. The oral microbiome is the community of bacteria, fungi, and viruses that live in our mouths
There are trillions of microbes and over 700+ unique species of bacteria that live throughout our oral cavity - on our tongue, cheeks, teeth, and in every little crevice On average, an individual has between 100 - 200 unique species of oral bacteria.
Some of these microbes are beneficial and are vital to keeping us healthy, while others are harmful and directly causative of diseases like cavities and gum disease.
These microorganisms can be found as free-swimming planktonic cells or assembled together to form a biofilm, a complex structure of microbes attached to a surface like a tooth (forming plaque or dental calculus).
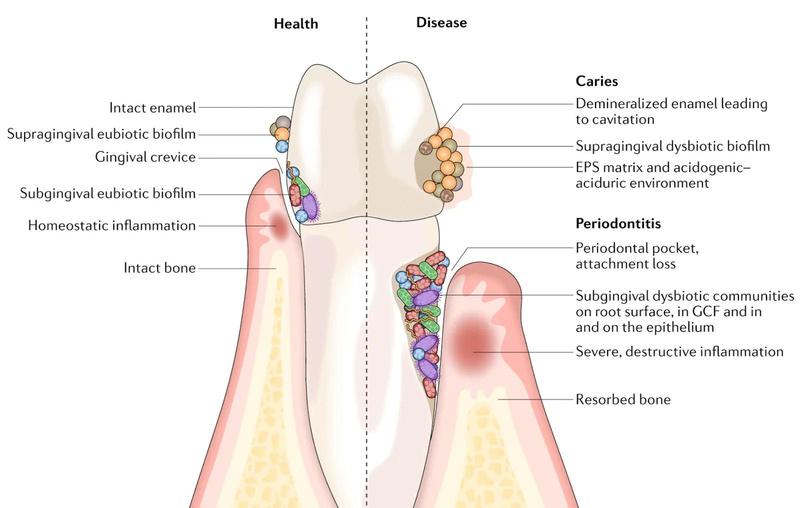
Our mouths are a delicate balance between these good and bad bacteriawhen that balance is tipped and the bad start outnumbering the good, we become more susceptible to complications like cavities, tooth loss, gum disease, and bad breath This is called dysbiosis of the oral microbiome
Let’s start with the heroes, our microbial buddies that play a critical role in keeping us healthy and functioning at our best. These beneficial bacteria typically thrive in a neutral or high pH environment and examples include Lactobacillus reuteri, Neisseria mucosa, and Streptococcus sanguinis.
Digesting food begins in our mouth where certain bacteria help break apart proteins and sugars They also help
Bacteria in our mouths also help facilitate a process in our body called denitrification, which is critical to our overall health Nitrate is a chemical compound found in many foods we eat and particularly abundant in vegetables and fruits such as beets and leafy greens Certain oral bacteria reduce nitrate to nitric oxide, a molecule in our body that powers vasodilation - the dilation of blood vessels, essential for reducing blood pressure. promoting metabolic and cardiovascular regulation, and improving cognitive function
Various oral care products boast killing 99 9% of bacteria but beware! Antimicrobials often wipe out not only the harmful bacteria, but also the commensal & probiotic species which are necessary to achieve better health
ith every hero comes a villain, and the oral microbiome is no exception. Tooth decay and cavities are the most prevalent chronic diseases on the planet in both children and adults, and are driven by specific bacteria
Certain bacteria in our mouth convert sugar from the foods and drinks we consume into acid Streptococcus mutans is the primary type of bacteria involved in this process, but there are a number of other species that contribute An acidic environment in our mouth supports the buildup of biofilm into plaque, a sticky film containing bacteria that coats teeth
As that plaque hardens, it becomes tartar which gives harmful species a place to “hide” and continue
producing more acid, which weakens the strength of our teeth by eating away at the enamel
This leads to cavities - holes in our teeth that develop from tooth decay (dental caries). It is commonly accepted that tooth decay is largely preventable, and even reversible in its early stages through changes to diet, hygiene, and lifestyle.
Despite this, the statistics are staggering. Among adults aged 20 and older, about 90% have had at least one cavity and over 25% of adults between 24 and 60 have untreated decay Your oral microbiome and the levels of acidogenic bacterial species can help inform your risk for cavities and guide what changes you can adopt to reverse dysbiosis
An estimated 65% of Americans struggle with bad breath and often it's a warning sign of something bigger...
This condition is incredibly important but not often discussed - it impacts our day-to-day lives, causes anxiety and stress in social situations, and often is a signal of other health issues It’s not something most dentists diagnose or treat with their patients, so we’re left turning to our own research on the causes and treatments. With almost 50% of people experiencing halitosis regularly, the issue is widespread. So what actually causes halitosis?
Halitosis causes can be divided into two categories: intraoral (in the mouth) and extraoral (outside of the mouth). Intraoral halitosis is responsible for 90% of halitosis cases, which are caused by a buildup of molecules called volatile sulfur compounds (VSCs) that have an unpleasant odor. VSCs include hydrogen sulfide (rotten egg smell) and methyl mercaptan (bad cabbage smell), and oral bacteria are the primary producers of VSCs.
Certain bacterial species like S moorei, P. gingivalis, and P. nigrescens, break down proteins in our diet and release VSCs as a byproduct.
There is a direct association between the abundance levels of these oral bacterial species and the amount of VSCs they produce. The bacteria associated with gum disease are also associated with the production of VSCs, and these halitosis-causing species are often found on the tongue (particularly towards the back near your throat) Tonsils are another home for these bacteria, and in each location, the bacteria form colonies and multiply to create biofilms or coatings
Saliva is a natural defense against halitosis as it contains proteins like lysozymes that attack bacterial cell walls and antibodies that prevent bacteria from settling on our tongue or teeth As such, dry mouth (low salivary flow rate) is a major contributor to halitosis
Extraoral halitosis (originating outside the mouth) can be caused by ear, nose, throat, or respiratory diseases (like sinusitis or tonsillitis), chronic diseases like gastric reflux, diabetes, and carcinoma, and medications Our diets can also contribute to temporary halitosis (think garlic and onions which contain high levels of VSCs).
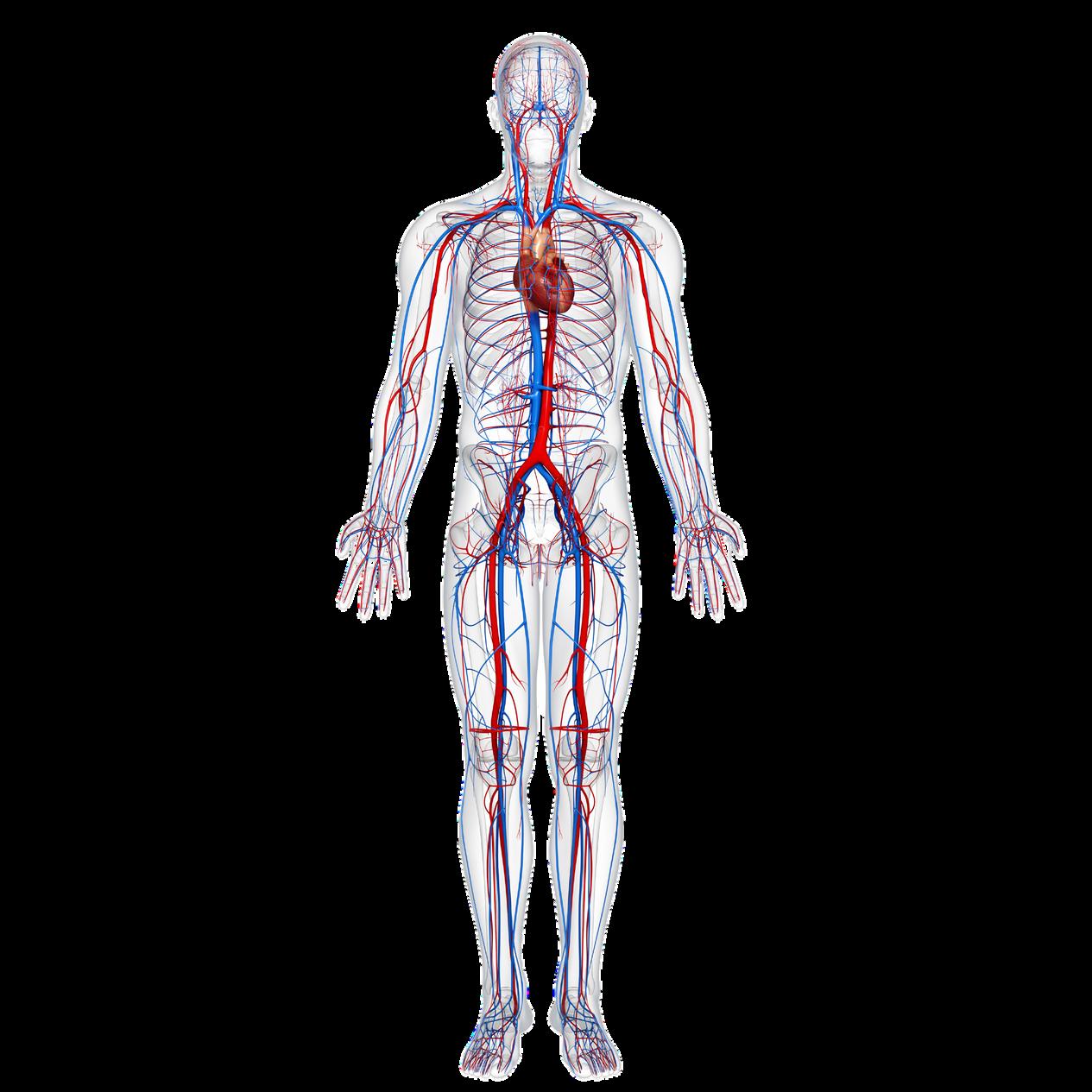
Did you know that oral bacteria and poor oral health is associated with a range of systemic diseases and conditions including Alzheimer’s, cardiovascular disease, diabetes, adverse pregnancy outcomes, colorectal cancer, and more?
Everything in our body is connected and the bacteria found in our mouths can travel throughout the rest of our body, causing inflammation and a number of major downstream effects
Our oral health and microbiome is a marker for our overall health, and we can’t truly be healthy without a healthy mouth

As we' think about longevity and the connection between our bodies and aging, let's explore the link between oral healh and cognitive decline
We've noted that there are millions, even billions, of microbial neighbors: bacteria, fungi, and viruses living in our mouths.
Many of these microbes have lived and evolved with humans over millions of years what we call a "symbiotic relationship" similar in some ways to how clownfish and anemones live together.
Some of these microbes are beneficial: they assist us with digesting food and fighting off disease These are some of the same bacterial species you might find in your probiotics
Other bacteria, called "pathogens, "cause disease One example you may be familiar with is Escherichia coli, otherwise known as E coli We all have commensal strains of E. coli living peacefully in our lower bowels
But unfamiliar strains can cause some serious digestive issues if they happen to be in your food. A few strains (e.g., E. coli O157:H7) can even produce toxins that lead to life-threatening illness.
Luckily, most microbes are either harmless or beneficial and only a small percentage are pathogenic The type and abundance of pathogenic microbes in your personal microbiome influence your risk for disease. In a healthy mouth, the ecosystem of harmless and beneficial microbes keep the pathogens from growing out of control
Your oral microbiome is said to be in "dysbiosis" when the cumulative abundance of disease-causing microbes in your mouth passes a certain threshold and, like other infections, starts to provoke a reaction from your immune system.
Pathogenic microbes typically cause disease through one of two mechanisms of action:
Direct: the microbes produce harmful byproducts like toxins or acids that directly damage cells and tissue in our bodies Indirect: the microbes trigger an excessive or inappropriate immune response that may damage our bodies
Research shows how oral health status, specifically the mix of bacteria in our oral microbiome, influences our risk of diabetes or heart disease, as well as overall metabolic health
Now, growing research suggests that cognitive decline (including forms of Alzheimer's and other dementias) is connected to some of the same bacteria that cause gum disease
Let's explore...
Alzheimer's disease (AD) is a form of dementia that affects memory, thinking and behavior. AD is the most common cause of dementia, producing some 60-80% of cases affecting an estimated 6M+ people in the US
AD is the sixth leading cause of death among Americans Most patients are 65 or older and risk increases with age, although there are early-onset cases of AD AD is a chronic and progressive neurodegenerative disease, meaning that the disease lasts for years, and worsens over time, eventually proving fatal if the patient doesn’t die of something else first.
There are currently no cures, and only a handful of potential treatments are available Therefore, an enormous amount of research is being conducted to find better ways of detecting, diagnosing, and treating AD.
Our brains are made up of billions of interconnected nerve cells, called "neurons." Neurons behave like an integrated circuit board, sending and receiving information via neurotransmitter chemicals and electric signals that control all of our body's functions basically biological programming
Groups of neurons can have special functions. Some are involved in helping us think, remember, and learn, while others focus on processing sight, smells, and sounds. These groups cluster in specific parts of the brain
Our entire bodies are managed by nerve cells and, like car engines, they require a steady stream of fuel and oxygen to keep working well Scientists believe that AD starts with accumulating damage in groups of nerve cells, particularly those involved in learning, memory and orientation
Also like an engine, breakdowns in one part of the brain can cause damage in other parts, too. Nerve damage becomes more severe over time, resulting in increasing loss of function.
Early symptoms include short-term memory loss (recent events are more likely to be forgotten than distant ones), but progress to wider memory loss, confusion, disorientation, mood and behavior changes and eventually, inability to walk, speak or swallow
The brains of patients with AD change drastically compared to patients without it, and a lot of research is focused on determining what changes cause AD and what changes are caused by it Two prevailing suspects are in the lead as potential causes of nerve cell damage and death: plaques and tangles.
"Plaque" That sounds familiar you've likely heard it from your dentist. Don't worry though, dental plaque a sticky film produced by microbes in your oral microbiome is different from plaque in your brain. In the case of AD, plaque refers to deposits of protein fragments that build up in the spaces between nerve cells.
"Tangles" are twisted fibers of certain proteins that build up inside nerve cells
Amyloid-beta proteins (AB) are small fragments of a larger protein called "amyloid precursor protein" (APP) AB is chemically stickier than other fragments of APP, meaning it is more likely to clump to form plaque
Plaque buildup is thought to disrupt cell functions like communication. Studies have shown that the brains of patients with AD have higher abundances of plaque. The major component of plaque formation comes from AB
Three pieces of evidence are often cited for AB being a major factor in AD:
Scientists have identified rare genetic mutations highly related to increased risk of AD These mutations occur in only three genes, all three involved in biological processes associated with AB production However, it's worth noting only ~1% of all AD patients have one of these mutations
Scientists have genetically engineered mice to carry some of these mutations
Those mice developed AB and showed signs of cognitive decline - for example, difficulty in navigating a maze they had run successfully many times before
Individuals with Down Syndrome (trisomy 21) have extra copies of the gene involved in APP production (three instead of the normal two) and almost invariably develop amyloid plaques Not all people with Down Syndrome develop AD, but individuals with Down Syndrome are at greatly increased risk of cognitive decline especially as they age
There are a variety of treatments being developed that target AB - attempting to slow down its production, remove it once it has formed, or prevent its formation altogether.
But so far, none have succeeded in preventing neurodegeneration
Tangles, on the other hand, are proteins that become...well, tangled.
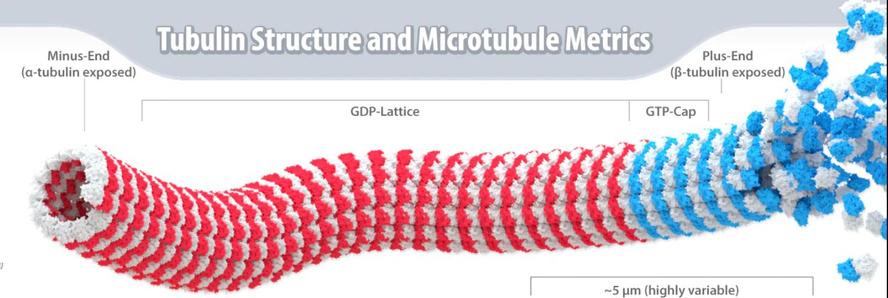
Our cells - including our neurons - are supported internally by structures called microtubules, similar to how houses are supported by beams and scaffolds Microtubules also help transport nutrients into and within the cell
In healthy cells, a protein called Tau binds to microtubules to help stabilize them However, chemical changes can cause Tau molecules to detach from microtubules and stick to each other instead This results in a "tangle" of Tau proteins that blocks nutrients from being transported inside the neuron and weakens the microtubules affecting the cell's structure The damaged neuron is no longer able to communicate with other cells.
Realistically, Alzheimer's disease is driven by a variety of complex factors that are interconnected. Research shows that abnormal tau protein often accumulates in regions of the brain involved with memory. AB clumps in the spaces between neurons As the levels of AB reach a tipping point, there is a rapid spread of tau throughout the brain
While AB, plaque, tangles and Tau remain the lead theories, the unhappy truth is that nearly 20 years of intense research has not shed much light on why and how AD develops. Nor has it led to any more than marginally successful drug treatments; most clinical trials have failed So research is slowly pivoting to investigate alternative hypotheses
As we know from research into periodontal and autoimmune disease, chronic inflammation is bad news Research now proposes that chronic neuroinflammation is a third key player, along with AB and Tau, in the development of AD.
This may start with chronic activation of microglia, immune cells that normally keep the brain clear of waste and debris Normally, such activation is in response to infectious microbes: bacteria or viruses. Microglia also activate in response to AB At first, that’s healthy, as the microglia mop up AB molecules But if there is too much AB, the microglia can’t keep up and begin to build up, along with stray molecules of AB This may also trigger a build up of Tau tangles. Microglia also produce signaling chemicals (cytokines) that increase inflammation and can be toxic to neurons
Poor oral health has long been associated with cognitive decline Research has shown correlations between tooth loss and dementia with a range of hypotheses attempting to explain the apparent link
Like AD, the risk and prevalence of oral disease increases greatly with age Both diseases are chronic, primarily affect US adults over 65 years old, and worsen over time One theory is that missing teeth make chewing food more difficult, which results in nutritional deficiencies that can impact cognitive function
A study at NYU found that adults with more tooth loss had a 1 48x higher risk of developing cognitive impairment and 1 28x higher risk of being diagnosed with dementia, even after controlling for other factors
In fact, they found that each additional missing tooth was associated with a 1.4% increased risk of cognitive impairment and a 1 1% increased risk of being diagnosed with dementia.
“Given the staggering number of people diagnosed with Alzheimer’s disease and dementia each year, and the opportunity to improve oral health across the lifespan, it’s important to gain a deeper understanding of the connection between poor oral health and cognitive decline,” said Bei Wu, PhD, Dean's Professor in Global Health at NYU Rory Meyers College of Nursing, co-director of the NYU Aging Incubator, and senior author of this paper investigating the relationship between tooth loss and cognitive decline
However, many studies to date have only correlated the occurrence of poor oral health and cognitive decline. New technologies are enabling a deeper view of the relationship between these two conditions
Sometimes these processes continue in a harmful feedback loop, causing a chronic inflammatory response in the brain
As with all complex biological diseases, your genes matter, too. In particular, TREM2 is a gene that tells microglia when it's time to clean up a cell If it's not functioning properly, there will be a buildup of debrisincluding AB and damaged neurons. The immune system will call in another type of cell, an astrocyte, to clean up the resulting mess But astrocytes, too, may become part of a cell and protein pile-up that eventually permanently destroys neurons
Over time, the brain becomes crowded with microglia, astrocytes, damaged cells, stray protein molecules and plaque. The immune system will continue to launch attacks, further damaging the neurons it was meant to protect.
We already know that chronic inflammation in the gums is connected to systemic disease, adding to the likelihood of a connection between oral infection and AD
Autoimmune connection
Chronic inflammation is a component of autoimmune disease as well So it is not surprising that another theory about the causes of AD includes autoimmunity
In autoimmunity, immune system cells attack cells and tissue of their own host, confusing self antigens (chemicals that signal the identity of a cell) with antigens from pathogens. This confusion likely started with an infection by bacteria or viruses that have similar antigen patterns to host cells.
A very large (n=1 8 million!) UK study found a significant correlation between hospitalization for certain autoimmune disease and later development of AD. Other research has suggested a link between herpes simplex virus (HSV) and AD
Yet other research is exploring autoantibodies and their connection to AD.
Blood vessel (vascular) conditions
While AD is considered the most prevalent dementia, vascular dementia is also common and may be confused with AD or Lewy body dementia
Primary vascular dementia is when damage to bl d l th h blockage (at (stroke) caus But vascular combined w However, ch plaque build blood vesse blood throug brains need brings nutrie passing thro which protec agents while nutrients and
Low blood f to our brain brain barrier from crossin clearing of p brain
This results beta and tau inflammation feedback lo
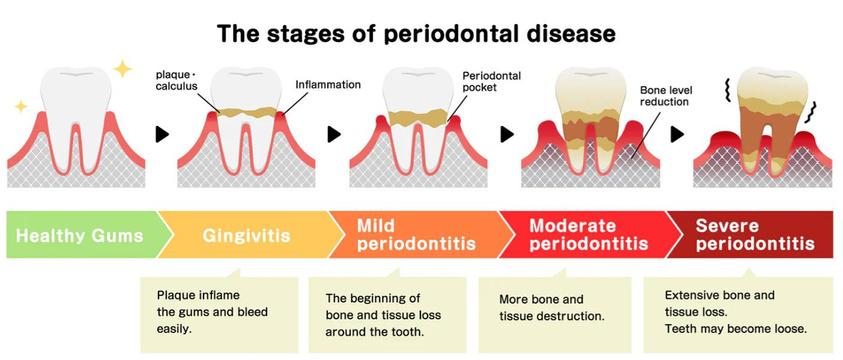
Periodontitis, or gum disease, is a serious gum infection that damages the soft tissue and can destroy the bone that supports your teeth Gum disease can cause teeth to loosen or lead to tooth loss Periodontitis is common but largely preventable.
A subset of the microbes in your oral microbiome are pathogenic and can lead to periodontal disease These microbes produce toxins that irritate our gums and stimulate a chronic inflammatory response, which can cause the tissue and bone that support our teeth to break down Gums separate from the teeth, forming pockets (spaces between the teeth and gums) that become even more infected
Gum disease progresses in stages, from the mildest form (gingivitis) to more severe stages. Once it advances to a certain point it becomes chronic and irreversible - requiring regular treatments and procedures to manage symptoms.
Gum disease is EXTREMELY common and affects an estimated 47% of US adults - over 60M people It is most common in adults over the age of 50 and becomes more prevalent with age - 70% of adults over 65 years old have gum disease
Gum disease is a major cause of tooth loss, which as we've discussed, is associated with cognitive decline, making gum disease a major area of interest in understanding the emergence and progression of Alzheimer's
Studies have found correlations between periodontal disease and Alzheimer's One hypothesis is that the pathogenic bacteria associated with gum disease travel outside of our mouths by entering the bloodstream, causing systemic inflammation that can lead to a variety of disorders including cancer, diabetes, and cardiovascular and neurological diseases
Periodontitis and AD often coexist. However, research is focused on answering a key question: which comes first?
Some studies have demonstrated that people with periodontitis present a major risk of developing AD while others suggest that those with AD or dementia have poor oral hygiene habits stemming from cognitive decline, and therefore are more likely to develop gum disease
With that said, it's a fact that good oral health (at the very least) is an important component to overall health We encourage you to take the steps to improve your oral health and minimize the risk for oral disease
If these hypotheses prove to be correct that means addressing your oral health may reduce or eliminate cognitive decline and possibly your risk for other systemic diseases too!
There are over 700 characterized types of bacteria known to be in the oral microbiome, and on average we each live with around 250 in our mouths. One of these species, Porphyromonas gingivalis (P gingivalis), is among the most well-characterized. Why is there so much interest in this single species?
Well, have you ever heard of "gingivitis"? Now you know where the name comes from!
P gingivalis is an infamous bacteria associated with the emergence and progression of gum disease. You might see it in your Bristle oral health insights
A study in 2008 showed P. gingivalis was present in over 85% of samples from patients with chronic periodontitis.
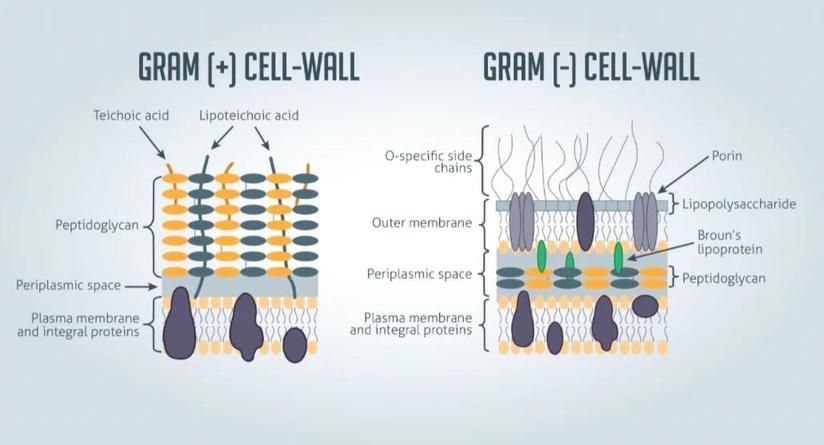
Non-motile, asaccharolytic, Gramnegative bacterium, an obligately anaerobic rod which forms blackpigmented colonies on blood agar plates
Translated into language we can all understand:
Non-motile: lacks the structures that enable free movement. This makes perfect sense given that P gingivalis lives in dental plaque!
Asaccharolytic: incapable of breaking down carbohydrates (like sugar) for energy Why is this relevant? P gingivalis lives below the gum-line, where access to sugar is low If P gingivalis relied on sugars to survive, then it would starve Instead, P gingivalis processes amino acids, the building blocks of proteins, which are more readily available
Bacteria associated with cavities, on the other hand, tend to live on the surface of teeth, where there is more access to sugar As expected, these bacteria feed on carbohydrates and convert them into acids, which lead to decay.
Gram-negative: Gram-staining is a method used to differentiate types of bacteria into two large groups (positive and negative). Gram-negative bacteria have a fat+sugar coating (lipopolysaccharide) on their cells which resists the violet Gram-stain
Gram-positive bacteria, lacking this coat, take up the dye and turn violet Gram-negative bacteria tend to be more resistant to antibiotics and other therapeutics, in large part because of their lipopolysaccharide coats
Anaerobic: survives and grows in areas that lack oxygen Obligate means they only survive in the absence of oxygen.
This is an important characteristic for P. gingivalis since oxygen is absent beneath our gum line Oxygen destroys anaerobes, which is a big part of why flossing is so important!
So P gingivalis doesn't move on its own, it doesn't feed on carbohydrates, it is resistant to many antibiotics and therapeutics, and it thrives in areas that lack oxygen All of these factors make it the perfect candidate for infiltrating our gums and causing disease.
P gingivalis produces direct and indirect mechanisms that lead to gum disease.
P. gingivalis has been identified in the brains of patients diagnosed with Alzheimer's, which may not come as a surprise given the correlation between poor oral health and cognitive decline
Gingipains a family of toxins produced by P. gingivalis have drawn the majority of attention from researchers investigating oral health and cognitive decline.
A landmark study uncovered a correlation between the levels of gingipains and amyloid-beta / tau protein levels in the brains of patients with AD
The researchers also identified P gingivalis in the brains and cerebrospinal fluid (CSF) of those same patients. In fact, further research showed that gingipains were found in neurons of over 90% of patients' brains diagnosed with AD.
The study suggests that P. gingivalis can migrate from the oral cavity into the bloodstream, eventually making its way to the brain
Once there, P gingivalis produces gingipains, which are associated with increased levels of amyloid-beta and tau proteins, eventually leading to cognitive decline
Our identification of gingipain antigens in the brains of individuals with AD and also with AD pathology but no diagnosis of dementia argues that brain infection with P. gingivalis is not a result of poor dental care following the onset of dementia or a consequence of latestage disease, but is an early event that can explain the pathology found in middle-aged individuals before cognitive decline
We also demonstrate that P gingivalis bacterial load can be detected in the CSF of clinical AD patients, providing further evidence of P gingivalis infection of the CNS... Although not specifically addressed in this report, once the oral cavity is infected, P gingivalis may access the brain and spread via a number of pathways After entering the brain, we suggest that P. gingivalis may spread slowly over many years from neuron to neuron
Let's do a quick recap on what we've learned so far:
Amyloid-beta (AB) and tau are two proteins that are thought to play a key role in the formation and progression of AD. Increased levels of each are found in the brains of patients diagnosed with AD and are thought to form plaques and tangles that may lead to neuron damage associated with cognitive decline. AB is found in the spaces between neurons, whereas tau is found inside the neurons themselves.
Poor oral health has long been associated with cognitive decline Similar to AD, the risk and prevalence of oral disease and tooth loss increases steeply with age In particular, gum disease has been a key area of interest due to its link with chronic inflammation, which is thought to also play a role in AD. We know that pathogenic bacteria involved in gum disease are implicated in other systemic inflammatory conditions including diabetes and heart disease by way of these bacteria entering our bloodstream
While there are a variety of microbes that trigger gum disease, P gingivalis is the most infamous and wellcharacterized species Studies have identified P. gingivalis in the brains and cerebrospinal fluid of patients diagnosed with AD. One toxin specifically produced by P gingivalis, gingipains, has also been found in the brains of patients diagnosed with AD at levels that correlate with AB and tau increases.
Contrary to what you might believe based on what we've discussed so far, some studies have suggested that amyloid-beta is normally beneficial!
Amyloid-beta is found across all humans and throughout our lives Researchers believe AB plays a key role in protecting the body from infections, repairing leaks in the bloodbrain barrier, promoting recovery from injury, and regulating synaptic function
So how does something that should be helpful end up harming us? Like everything else in health and biology: context and moderation are key
Amyloid-beta has shown antibacterial, antifungal, and antiviral properties effective against several species of microbes When we are infected by these microbes, our bodies increase the production of amyloid-beta to combat them.
While more infection-fighting AB sounds like a good thing, it also increases the chance for error in production. Errors in AB can lead to loss of function it may be less effective in fighting off an infection or may take longer to clear out from our bodies.
If we accumulate malfunctioning AB, effects may be more severe and the infection it was supposed to protect us from may actually get worse.
Evidence from our work reported here lends support to the emerging concept that Aβ is an antimicrobial peptide, and mutations contributing to loss of this function could allow more robust infection with P. gingivalis and higher risk for disease
In addition, sustained high levels of antimicrobial Aβ driven by chronic P gingivalis infection of the brain may be toxic to host cells
We develop gum disease:
Our mouths become host to P gingivalis, originally in small quantities with mild symptoms (like gingivitis).
Without treating early gum disease, P. gingivalis proliferates, leading to more severe symptoms Some symptoms, such as bleeding gums and tooth loss, provide opportunities for P gingivalis to enter our bloodstream.
The pathogens causing gum disease travel throughout our bodies
P gingivalis in distant tissues leads to an inflammatory response. Eventually, they reach our cerebrospinal fluid (CSF) and cross the blood-brain barrier
P gingivalis leads to cognitive decline
Our immune response produces an excess of malfunctioning amyloidbeta that builds up as plaque between neurons, impacting communication and function Gingipains produced by P gingivalis break down tau inside of neurons, further impacting their function and enabling more buildup of amyloidbeta
Over time, significant portions of the brain lose functionality beginning in areas associated with memory.
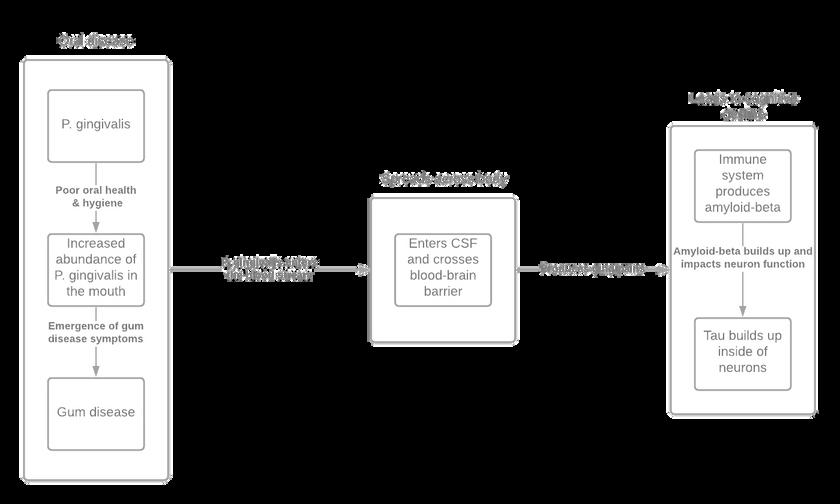
AnexampleofhowP.gingivalismaycontributetotheonsetandprogressionofcognitivedecline.
Deeper insights into the drivers and mechanisms of disease provide opportunities to create more effective therapeutics and treatments against them.
While there are a variety of companies and researchers investigating new ways to detect and treat cognitive decline, we wanted to highlight two exciting companies in this space, as it relates to P. gingivalis and Alzheimer's.
*Bristle does not have any personal or professional relationships with the companies cited below!
Cortexyme is a clinical stage pharmaceutical company based in South San Francisco, CA, focused on creating new therapeutics to improve the lives of patients diagnosed with Alzheimer's and other cognitive diseases
Keystone Bio
Keystone Bio is another company leveraging the connection between oral health and cognitive decline to develop new therapeutics.
recognized connections between alth, but new technologies allow us hat drives them.
ealth through your oral microbiome overall health and reduce your risk
In 2015, one study showed that antimicrobial mouthwash use led to increased blood pressure and reduced levels of salivary and blood nitrite
In 2016, a follow up study in normotensive individuals found similar results across multiple types of antimicrobial mouthwash containing chlorhexidine, cepacol, or alcohol.
Then in 2020, a separate study was published across over 1000 participants demonstrating that people who use mouthwash twice per day had an increased risk of hypertension compared to people who used it once per day or not at all
In 2021, a mechanistic study found that antiseptic mouthwash inhibited the production of nitrite and nitric oxide, and reduced the efficacy of L-arginine anti-hypertension supplementation
In 2021, a meta-analysis revealed that chlorhexidine mouthwash shifted the oral microbiome toward lower diversity, reduced levels of nitrate-reducing species, and altered nitrite levels in both saliva and plasma

oral microbiome are responsible for xample, Haemophilus, Neisseria, and Veillonella species, among wn to play a role in the enterosalivary apacity. Here are a few things that crease salivary and plasma nitric
a critical component of especially through its ability to and increase levels of nitric oxide
Bristle measures your oral health by analyzing the oral microbiome of a sample of your saliva
Typically, you have about 250 unique species of bacteria living in your mouth. Bristle’s technology enables us to identify all of them!
To date, our microbiome analyses have identified over 700 different bacterial species that comprise the oral microbiota
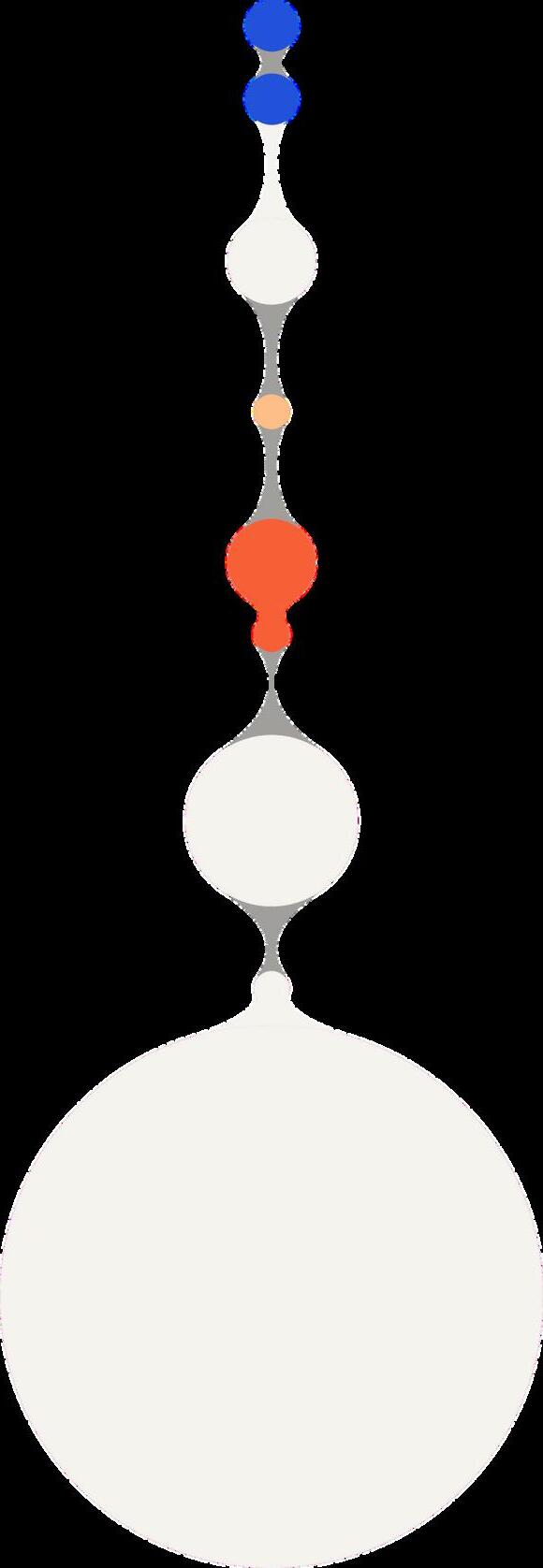
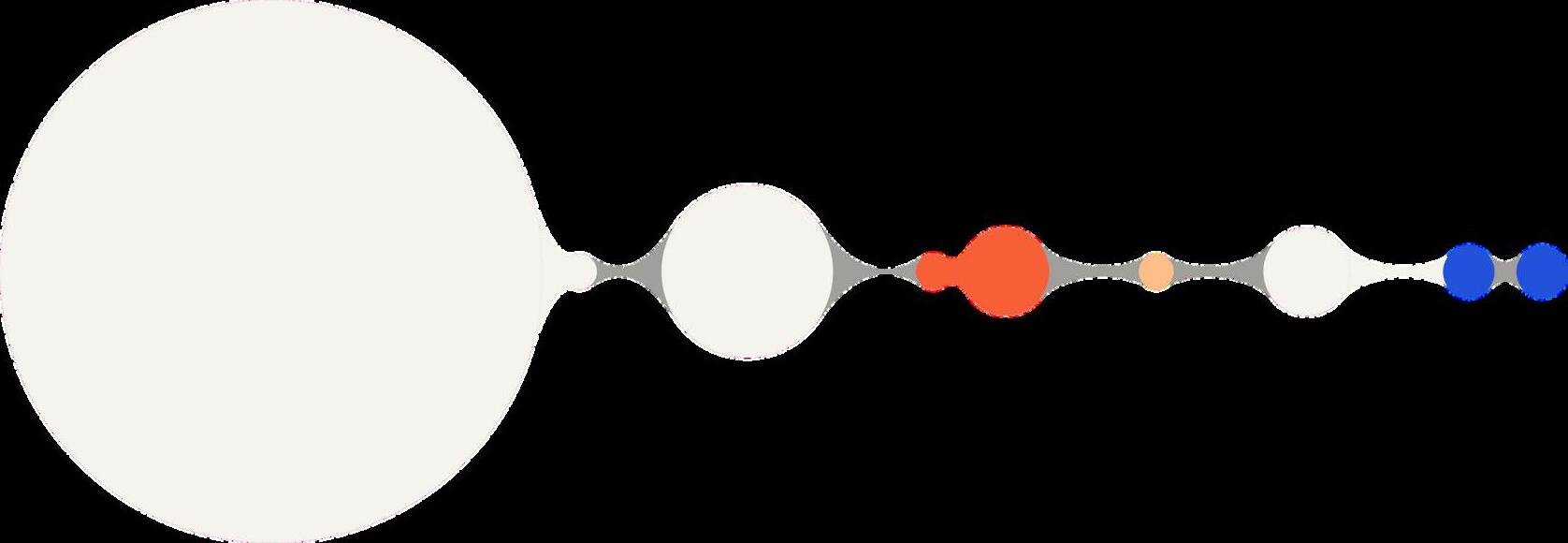
This illustration compares a healthy, balanced mouth, with an out-of-balance, dysbiotic, diseased one The difference is the mix of microbes
A subset of the 700 bacterial species in our mouths are pathogenic and can cause cavities, gum disease, and bad breath
By understanding the types and abundances of the bacteria in your saliva, Bristle can help you get insights into your oral health and risk for oral disease.
We can suggest steps including hygiene, dietary, and lifestyle changes to eliminate pathogenic bacteria in your saliva - improving your oral health and lowering overall risk for disease
"Biogeographyoforalmicrobiotacolonizationinthediversehabitatsoftheoralcavity"Lamont,RJ,Koo,H &Hajishengallis,G Theoralmicrobiota:dynamiccommunitiesandhostinteractions NatRevMicrobiol16,745–759(2018)
So how do we avoid dysbiosis of our oral microbiome and get on the fast track to a healthier mouth and body?
Here are some tips:
Brush your teeth twice a day for two minutes each to disrupt all that biofilm formation Conventional wisdom may tell you to brush right after a meal. But foods and drinks push your mouth into an acidic state and if you brush your teeth then, you risk damaging your enamel so wait at least 30 minutes.
Floss with string floss or a water flosser to get into the crevices where bacteria hang out that your brush can’t reach (check out Bristle’s data on how flossing can affect your oral microbiome)
Tongue scrape to wipe away the bacterial biofilm on your tongue
Beware of certain antimicrobial mouthwashes that can cause damage to your oral microbiome by eliminating beneficial bacteria
Sugar and refined carbohydrates - you’ve probably heard eating sugar and candy causes cavities, and it’s because bacteria feed off sugar and release acid as a byproduct If you are eating sugar, the key is to eat it all at once the shorter the span, the less time for feeding
Acidic foods and drinks - these include coffee, tea, fruit drinks, soda, sports drinks, sweetened carbonated drinks, and even fruit juices that are naturally high in sugar and acids (including ascorbic acid or Vitamin C) Foods like fruits, especially citrus fruits or dishes like pies, jellies, and jams, as well as candies fall in the same bucket Again, the key here is that if you are going to consume these, do so over a short period of time and drink water in between or after to dilute the acid attacks Using a straw with the drinks can help minimize direct contact with your enamel, and always wait at least 30 minutes to brush your teeth!
Sulfur-containing foods (if you have high periodontal pathogens or existing gum disease) - sulfur-reducing bacteria are important pathogens in periodontal disease, and sulfate-reduction may promote their pathogenesis. Sulfur-containing foods also promote the production of volatile sulfur compounds responsible for halitosis. These foods include arugula, asparagus, cruciferous vegetables, animal proteins, dairy, and legumes (see resource here for low sulfur diet).
High-fiber vegetables and fruits - these stimulate saliva production and neutralize acid, plus they tend to be high in vitamins A and C which help rebuild enamel and heal gums These include vegetables like carrots, celery, broccoli, leafy greens, and fruits like apples, bananas, and berries
High pH alkalizing vegetables - certain vegetables have a naturally higher pH meaning more alkaline and less acidic These include cruciferous vegetables like broccoli and cabbage and leafy greens like kale, arugula, spinach, and lettuce
Foods high in nitrate - the oral microbiome plays an important role in nitrate reduction, and nitric oxide production, which is a key molecule responsible for maintaining normal blood pressure Foods in this category include beet roots and leafy green such as kale, arugula, and spinach
Foods with high levels of arginine - early research shows arginine, an amino acid, can help reduce plaque build-up Foods in this bucket include poultry, lentils, soybeans, chickpeas, peanuts, and pumpkin seeds
Foods rich in vitamin K2 - foods like chicken, pastured eggs, and grass-fed meats can help remineralize teeth and prevent cavities.
Drinking water and staying hydrated - water not only helps increase saliva production, but also wash away food particles lingering in the mouth.
There are a number of different oral probiotics like S salivarius K12 and M18 that have shown with some initial efficacy data to help with halitosis and tooth decay
Xylitol is a natural sugar alcohol that helps prevent cavities It reduces the levels of cavitycausing bacteria like S mutans by disrupting their energy production processes, leading to cell death, less adhesion to teeth surfaces, and reduced acid production It also stimulates saliva production, a key component of preventing bad breath! You can find xylitol in gums and lozenges, making it a perfect after-meal treat
We’ve all heard the mantra that you should “brush and floss more” to improve your oral health. But there is so much more we can be doing to promote a healthy mouth We are all biologically different, so the question becomes, what works for me?
At Bristle we've made it incredibly easy for all of us to take ownership of our oral microbiome and health! Our easy to use, athome test measures all 100+ unique bacterial species in your saliva, both beneficial and harmful, to provide an overview of your oral health status.
You can order a Bristle test (either a single kit or our Bristle Reset Program) through our website and receive a kit right to your home
You'll fill out a short questionnaire and collect a saliva sample in a tube, which takes only a minute or two.
Send off your saliva sample to their lab for processing using the included prepaid return envelope, and access your results online within 2 - 3 weeks.
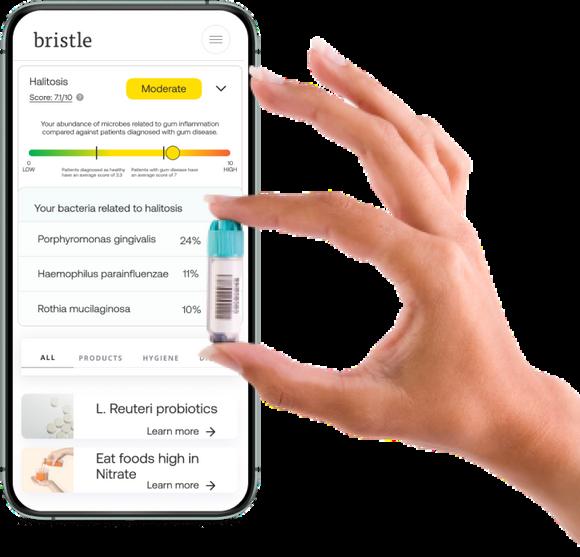
The report begins with high-level health scores for tooth decay, gum inflammation, bad breath (halitosis), gut inflammation, and beneficial bacteria
The scores are from 0 - 10 and bucketed by Low, Moderate, and High for easy interpretation.
Each score includes the contributing bacterial species detected in your saliva, at what levels they were detected (relative abundance), and a description of the bacteria’s function. You’ll also receive a raw breakdown of all the bacterial species detected in your microbiome and their relative abundance
Based on test results, Bristle provides prevention-focused diet, lifestyle, hygiene, and oral care recommendations that go far beyond brushing and flossing. What is unique about our recommendations is the focus on oral care product ingredients to look for, rather than specific products themselves.
Bristle also provides a confidence score based on the amount of scientific research and efficacy data that exists You can read more about how their team researches recommendations here.
You also receive access to a 1:1 coaching session with one of Bristle’s oral health & hygiene specialists to review your test results, get any questions you have answered, and work on a tailored action plan together.


ConsultingwithImanaboutmylabresultsprovidedmuch neededclarity!
ItwaseasytospeakopenlywithmyBristlecoachaboutmy concernsandgoals(Iamneverabletobethatvulnerablewith mydentist)
MuchoftheinformationthatIknewaboutmyfood intoleranceswerefurtherexplainedbymyoralhealth information

ItwasextremelyeasytosendinthesampleandIreceived myresultsquickly
Mycoachreviewedmyresultsindetailwithme,offering uphersuggestionsaswewentandchoosingitemsthatfit withinmylifestyle
I’msohappytohavestumbledacrossBristleandcan’t recommenditenoughtoothers!