Transforming the Future of CRITICAL CARE


Transforming the Future of CRITICAL CARE



















Volume 13 . 2023
COVER
2 Message from the Chair
10 Division Highlights
DREAM CAMPAIGN
41 Donor Honor Roll
42 About DIG
44 2023 DREAM Innovation Grant Recipient
INNOVATIVE RESEARCH
48 The Quest for New Therapies to Improve Ischemic Stroke Outcome Wei Yang, PhD, FAHA
50 Defining the Neural Architecture of the Murine and Human Temporomandibular Joint for Advancing Orofacial Pain Therapies Christopher Donnelly, DDS, PhD
52 Neuro-Immune Interactions in Postoperative Delirium Niccolò Terrando, BSc (hons), DIC, PhD

GLOBAL HEALTH

54 Blogs from Abroad: Ghana
RESIDENCY RECAP
60 Resident Spotlight
62 Alumni Shoutout
ALUMNI NOTES
64 Q&A with Sir Winston CV Parris, KCSL, CMG, MD, FACPM
DEPARTMENTAL
68 Departmental Faculty
BluePrint is published once a year by Duke Anesthesiology. This issue was published in October 2023. Your comments, ideas and letters are welcome.

VIEW ISSUES ONLINE: blueprint.duhs.duke.edu
PLEASE CONTACT US: Duke Anesthesiology
BluePrint Magazine
DUMC 3094 Durham, NC 27710 blueprint@duke.edu
EDITOR IN CHIEF
Stacey Hilton
CREATIVE DIRECTOR
Stacey Hilton
GRAPHIC DESIGNER
Lacey Chylack, phase5creative.com
CONTRIBUTING WRITERS
Jennifer Bringle
Stacey Hilton
Ratna Swaminathan
Duke Anesthesiology Faculty & Staff
PROOFREADERS
Lynet Gonzales
Christopher Keith
Melinda Macalino
John “Jack” Newman
CONTRIBUTING PHOTOGRAPHERS
John “Jack” Newman
Duke Anesthesiology Faculty & Staff
WEB ADMINISTRATOR
Christopher Keith
CONNECT WITH US: anesthesiology.duke.edu
Years ago I came across an illustration titled the bookends of life. It was essentially two dates separated by a dash as follows: _____ —_____. In that illustration, author John Ortberg notes that “we had no say at all in the number on the left. We arrived on this planet one day without being consulted ahead of time. We did not get to vote on our parents, birthplace, family order, or DNA. One day the question mark on the right will be replaced by a date that we don’t have much to say about as well. That is part of what gives life its urgent value. We have one shot at it. Which brings us to the next question: What are we going to do with our dash? That little dash is ours to spend: to choose hope or cynicism, to grow or to stagnate, to be known or to hide, to seize initiative or to reign in passivity;” or… to change the face of anesthesiology
As you will read, our clinical and education missions continued to excel this year, evidenced by the #3 and #5 national rankings, respectively. Our researchers also secured NIH grant funding at levels never before attained in the history of the department, culminating in a #2 NIH ranking. While individual researchers deserve recognition for this accomplishment, the research teams comprised of faculty, trainees, nurses, and staff must also be celebrated. This year, we also marked the 50th anniversary of the department in a gala that featured keynote speaker Jay Bilas, a former Duke basketball player and preeminent television basketball personality. Summarized here are his key points for maintaining success beyond our 50 years: 1) Never give less than the best, 2) Be relentless in your preparation, 3) Focus on the next play, 4) Have empathy, 5) Be the best teammate, and 6) Don’t take special for granted. Duke Anesthesiology is special but let’s not take it for granted. Let us stand together, build each other up, focus on the “one more thing,” and be relentless in our preparation so that we, together, can reach heights we can only dream of today.
And now, ready or not, you have been given a turn. What will you do with your dash?
Sincerely,
Joseph P. Mathew MD, MHSc, MBA
https://anesthesiology.duke.edu/alumni




find ways that make a difference in the lives of her patients.
“
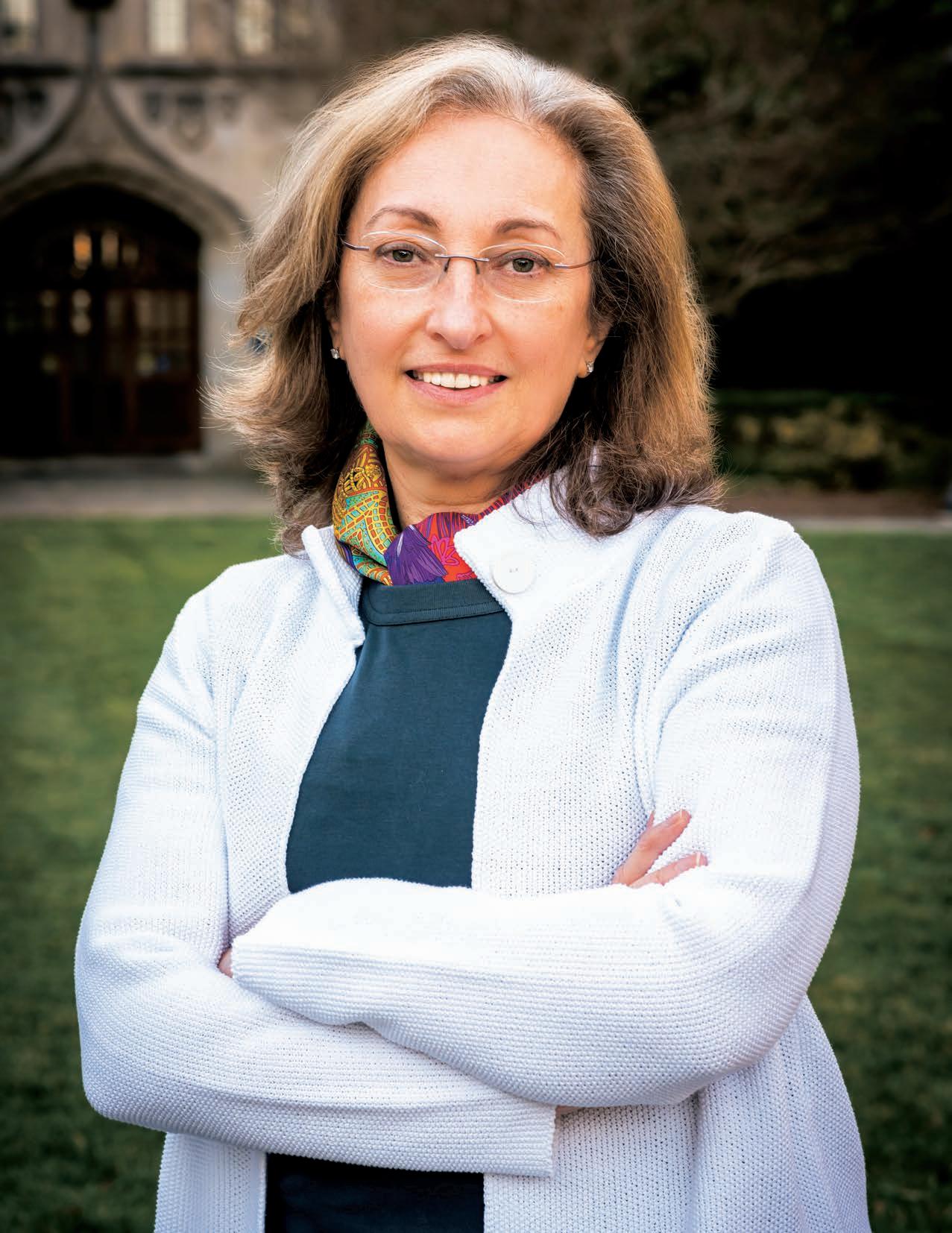
Volere é potere,” says Treggiari softly in Italian as she translates the old English proverb “where there is a will, there is a way” that has been her guiding mantra to navigate daunting research landscapes with obstinate persistence, enduring perseverance, and a whole lot of resilience. “I have always been very determined and not easily dissuaded from goals I intended to achieve.”
Curiosity, intuition, and observation push her to question current approaches and test the limits of possibilities in research work. “It is incredibly rewarding because you can see the results of your work producing a direct benefit to patients. I like to think that I have saved many more lives with my research than providing direct patient care at the bedside,” says Treggiari, vice chair for research in the Department of Anesthesiology at Duke.
“I have always been very determined and not easily dissuaded from goals I intended to achieve.”
Growing up near the Swiss-Italian border, Treggiari developed an interest in becoming a cardiac surgeon shortly after her father suffered a heart attack and cardiac arrest when she was just 11 years old. She resolved then that her future career would involve learning how to save him if this recurred. Interestingly, she assisted in his coronary revascularization procedure later in life. He is 88 years old and doing well, she informs with a smile.

While surgery and neurosurgery fascinated her during medical school at the University of Pavia, it was the quick thinking of the anesthesiologist “on the other side of the drapes” in the operating room (OR) that led her to choose a career in anesthesiology. Treggiari was particularly attracted by the critical care environment and energized by its intensity, the variety of clinical conditions, the challenges of problem solving, and the comprehensive nature of the medical knowledge involved. “It was the ability to see intervention and its effect, the diversity of the situations, and the intellectual stimulation that I found most rewarding,” she adds.

Treggiari’s research career started with unexpected success during a medical student exchange program sponsored by the European Community’s ERASMUS Program. With no prior research background as a medical exchange student at Ninewells Hospital and Medical School in Dundee, Scotland, she set up a project to study the recurrence of esophageal strictures and their predictors, collect data, analyze it, and write a manuscript.
“I really didn’t know much about conducting research; I was just following instructions. I presented the data to the statistician and looked over his shoulder as he ran the code for
the statistical analysis on an old-frame computer. I can still remember the excitement when we discovered that we had identified an important predictor of esophageal stricture. It was an exciting and thrilling moment the first time I made a contribution, albeit small, to the scientific community.” The ability to answer a question convinced her to do research for the rest of her life, informs Treggiari.
The guidance of extraordinary mentors shaped Treggiari’s academic trajectory. During her residency, Dr. Peter Suter, dean of the School of Medicine in the University of Geneva, channeled her research path forward. She was selected in a scholar’s program (Programme de Relève Académique) established for the career development of future academic leaders, especially women, to address the imbalance of leadership positions that then favored men, she informed.
Concurrently, Treggiari learned cardiovascular and respiratory physiology from giants in the nascent critical care environment in Europe, including Suter, founding father of the European Society of Intensive Care Medicine, and Dr. Jacques-Andre Romand, a renowned anesthesiologist and intensivist.
Her thirst for knowledge widened her geographic and academic horizons. After residency in 1999, Treggiari earned a second Swiss Medical Doctor degree in Geneva and headed to the United States as a visiting scholar in the Division of Pulmonary and Critical Care Medicine at the University of Washington (UW), Seattle. Five board certifications, an MPH in public health, a PhD in epidemiology, and several exams later, Treggiari focused on gaining valuable clinical work experience. She served as professor of anesthesiology and pain medicine with adjunct appointments in the Department of Neurological Surgery and the Department of Epidemiology (2011-2014) at UW, endowed professor and vice chair for research in the Department of Anesthesiology and Perioperative Medicine at Oregon Health & Science University until 2019, and a tenured professor and vice chair for clinical research in the Department of Anesthesiology at Yale University.
In 2022, Treggiari joined Duke Anesthesiology inspired by the diverse research programs from basic science

to population health, its prominent scientists, and a strong commitment to academic excellence. A dedicated researcher in clinical and outcomes research, she envisions carrying forward the rich legacy of her predecessors and taking the department’s research endeavors to the next level. Among her goals is to bring the late Dr. David Warner’s unfinished work on antioxidants and brain ischemia to completion. She also plans to help restart the late Dr. William Maixner’s drug discovery program in the Centers for Translational Pain Medicine and Perioperative Organ Protection.
Excited to work in an environment especially supportive of junior faculty, Treggiari plans to ensure both opportunity and resources for those committed to the success of Duke Anesthesiology’s research mission. She aspires to make Duke Anesthesiology the best research program in the country with a focus on drug discovery and
development of new therapies for pain and stroke. “We are growing our translational and clinical research footprint incorporating novel research methods based on either mechanistic or pragmatic approaches. We will also grow new clinical trial programs in partnership with the Duke Clinical Research Institute.”
Funded through federal, foundation, and industry support, Treggiari has brought about a paradigm shift in the medical practice guidelines for critically ill patients, both nationally and globally. Not afraid to challenge traditional dogma, Treggiari’s research has deeply influenced critical care management from sedation and hemodynamic management to glucose control. In the early 2000s at UW, Treggiari made an important observation that critically ill patients who were routinely given deep sedation during mechanical ventilation were more likely to experience complications like

“Helicopter rescuing was exciting and extremely intense. It required preparing for the unexpected, real-time problem solving and fast thinking. I learned about emotional intelligence and how to think outside the box in very challenging scenarios. There are no limits to what we can accomplish. ”Dr. Treggiari taking part in a helicopter rescue in Geneva, Switzerland with Rega – Swiss Air-Rescue while completing her critical care fellowship.
delirium and prolonged mechanical ventilation. Consequently, Treggiari presented an evidencebased systematic investigation that would later change culture. “It was a very odd concept to introduce that it’s okay for a patient to be awake while being mechanically ventilated,” she added. Her work contributed to a profound change in the approach to ICU sedation for mechanically ventilated patients. Adopted first in UW, it soon influenced ICU sedation practice worldwide.
Treggiari’s work has highlighted the potential negative effect of interventions related to hemodynamic management and fluid administration in patients with subarachnoid hemorrhage. “We first demonstrated this in a metanalysis that was published in the Journal of Neurosurgery, and then a pilot study that was
Explore and seek out great mentors, and establish strong relationships with them. Mentorship relationships start with a mutual connection and are built on trust and mutual respect.
Direct, honest, actionable feedback is of huge value, although it may not always be perceived that way. Be open to accept the feedback and use it as an opportunity to learn, grow and increase your self-awareness.
It takes time and energy to develop a mentee, and it is necessary to be accessible/available and allow time to give input and to monitor progress. Have clear expectations and rely on milestones and timelines to stay on target and to revisit goals as needed.
Mentors can also be sponsors that advocate and identify opportunities for their mentees through opening doors and investing in their success (e.g., employment recommendations, networking, etc.).
Early career physicians/scientists, women in particular, should be encouraged and prepared to assume leadership roles by enhancing their self-awareness and realization that these opportunities are within their reach. Preparing leaders to assume such roles will help shape a strong and rich future for anesthesiology.
published in Neurosurgery.” She was then invited to join the international consensus conference panel to recommend medical management guidelines of subarachnoid hemorrhage that are now followed globally. “The updated guidelines have been recently published in Neurocritical Care,” informs Treggiari, adding that these guidelines have been endorsed by societies, including the American Heart Association, the Society of Critical Care Medicine, and the American Association of Neurological Surgeons, among others.
In an observational study on 10,000 patients in the early 2000s, Treggiari’s team showed no improved outcomes with tight glucose control, thereby refuting an earlier study that had indicated benefit. Her findings, confirmed

by subsequent studies, led to a global unanimous decision to abandon the tight glucose control approach in critically ill patients, and revert to standard glycemic control practice. Treggiari’s work on ICU organization and structure has received national media recognition.
Her roles—as a clinician in several ICUs and ORs, an administrator as vice chair for research, and as an internationally recognized researcher with more than 150 peer-reviewed articles in high-impact journals to her credit—all work in harmony to enhance patient care.
a shift to grow stronger mentors and introduce the concept to mentoring early on in careers,” says Treggiari. “Most of my mentors have been men,” she adds, emphasizing the need for diversity with more women and minority mentors to foster a better mutual relationship with young researchers. At Duke, she appreciates the ongoing efforts to develop and grow a diverse group of leaders.
Treggiari sees the field of anesthesiology evolving dramatically over the next decade. “We can envision patient care in the OR where we will no longer have cords or cables and patients will arrive to the room with their
PASSION: Good research requires hard work, selfdetermination and takes time. New investigators should consider research areas that they have a passion for; it is far easier to spend time working on something that inspires you than working in areas that do not.
While Treggiari chiseled a roadmap for success through methodological rigor, she also made mistakes and learned from them. As a resident in the mid1990s, she conducted an ambitious study following the excitement in the anesthesia community about the newly discovered pulmonary vasodilator, nitric oxide. “There was really no experience of human exposure, therefore we collected extensive data showing that not every patient improved when exposed to this agent.” However, her study was initially rejected by prominent journals citing methodological flaws. Although disheartened by these rejections, Treggiari humbly recognized that her data were complex and had limitations.
“Occasionally, failure is to be expected. Learn from failures and move on,” she stresses. She advises researchers to adequately plan, adhere to methodological rigor, break down long-term goals into bite-sized achievable steps, and pivot in the face of roadblocks.
Her goal is to customize learning for researchers to address gaps upstream and prevent problems downstream using existing resources at Duke. “There’s
wearable devices placed preoperatively. Telemedicine will replace most in-person visits and patients will be monitored remotely. Surgeries will become less and less invasive. Large data-driven research and pragmatic trials will replace traditional placebo-controlled trials. Precision medicine with endotyping of subpopulations will become part of usual care and providers will need to rely on artificial intelligence (AI) tools for decision support for patient care to implement personalized approaches.”
While working in high-acuity environments drives this physicianscientist to scale new heights, her family keeps her grounded. She cherishes spending time watching her daughter, Sofia, ride a horse they just acquired, or cheering on her son, Malcolm, as he competes in a Carolina Junior Hurricanes game. Getting in a competitive game of tennis with her husband, David, on a sunny winter day helps Treggiari recalibrate her personal and professional roles. “I plan my life in a very deliberate way and arrange my life around things that I need to do,” she says, as she looks for the next big thing in research. BP
PERSEVERANCE: There is great satisfaction when projects are successful, and you see the impact of your work on advancing science, practicing change or improving care, but there will invariably be challenging times along that path. However, there is typically more than one way to solve a problem.
FOCUS: It is important to stay focused on the overall objective and not be discouraged by the unexpected disappointments. It helps to keep an open mind and to remember the big picture.
OPPORTUNITIES: Chances for growth and enrichment are all around us. Recognize meaningful opportunities and prioritize in steps so that the tasks will not be overwhelming, and the opportunities will not be lost.
HARD WORK: “I genuinely believe that hard work –exceptional hard work – is the key factor to succeed in medicine.”
“Mentorship and sponsorship are key drivers of success. Extraordinary leaders will set great expectations, help shape careers and create excellent opportunities.”
Over the past year, the Ambulatory Anesthesiology Division has made tremendous strides in its pursuit of excellence in patient care, research and education. The division will experience significant growth with the addition of three new hires, Juhnnel Vera Santiago, Emily Chen and Akayla Gillians. These talented professionals will bring new perspectives and expertise to the division, further enhancing its capabilities and commitment to excellence.
In collaboration with the Critical Care and Perioperative Population Health Research (CAPER) Program, the division has been focusing on the impact of COVID-19 on the transition of total hip arthroplasty to the Duke Ambulatory Surgery Center (ASC). This research has analyzed patient and hospital characteristics associated with total hips moving to the ambulatory setting, providing valuable insights into the optimization of surgical procedures during the pandemic.

Furthermore, the division has played a key role in the continued expansion of Duke Ambulatory Surgery Center Arringdon’s total joint replacement program. Dr. Steve Melton developed an electronic capture system to track immediate postoperative recovery, allowing for more efficient monitoring of patient progress and enhanced clinical decision-making. Melton has also been appointed
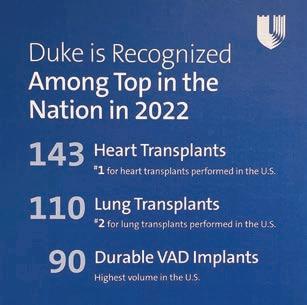
A testament to extraordinary clinical competencies, Duke became the largest thoracic organ failure program in the country this year and surpassed 100 donor after cardiac death (DCD) heart transplants - placing the medical center among the highest volume and most experienced in DCD heart transplantation in the world. Additionally, Duke earned a platinum level Center of Excellence for its ECMO program from the Extracorporeal Life Support Organization (one of only 50 centers in the world at the platinum level) and became the first medical center in the nation to be awarded accreditation in perioperative transesophageal echocardiography by the Intersocietal Accreditation Commission. This extraordinary milestone was achieved under the leadership of Dr. Alina Nicoara, director of the Perioperative Echocardiography Service.
Numerous quality improvement efforts continue to yield significant results as part of the Cardiothoracic (CT) Learning Health Unit - focused on prolonged mechanical ventilation, acute kidney injury and reoperation, as well as standardization of clinical practice for perioperative management of CT surgical and critically ill patients (Drs. Negmeldeen Mamoun and Ian Welsby); thoracic organ transplant innovation and quality improvement (Dr. Brandi Bottiger). Members of our
medical director of ASC Arringdon, where his leadership will ensure the continued growth and success of the facility and further strengthen its reputation for providing high-quality ambulatory anesthesia services.
Additionally, the high-speed, high-volume nerve block environment at ASC Arringdon has significantly augmented the educational experience for regional anesthesia fellows. This unique setting offers valuable hands-on training opportunities, ultimately benefiting patient care and preparing the next generation of anesthesiologists for successful careers in the field.

These collective achievements have not only benefited the Duke community, but have also made a lasting impact on the broader medical community.
team continue to be at the forefront of operational leadership for optimizing CTOR workflow and capacity, expanding the repertoire of procedures conducted in the electrophysiology and cardiac catheterization labs to include laser lead extractions and TAVR (Mamoun, Bottiger, CRNA Chad Ragains).
The division continues its strong representation for both institutional and national leadership, including the appointments of Dr. Sharon McCartney as director of Duke’s Center for Blood Conservation and Dr. Anne Cherry as chair of the Society of Cardiovascular Anesthesiologists’ Research Committee. Other honorable mentions include Dr. Madhav Swaminathan earning the American Society of Echocardiography 2023 Outstanding Achievement in Perioperative Echocardiography Award and Duke’s CTICU participation as one of 14 ICUs in the country in the NIHfunded Bridge2AI Program.

The Community Division is comprised of 23 faculty who provide comprehensive and state-of-the-art anesthesia services at Duke Regional Hospital, Duke Raleigh Hospital, Davis Ambulatory Surgery Center, Duke Fertility Center, and Pioneer Ambulatory Surgery Center, while supporting the academic mission of the department.
After serving as division chief for 16 years, Dr. Edward Sanders retired in 2023 and Dr. Nicole Scouras was appointed division chief. In this role, she is responsible for maximizing the quality and efficiency of daily practice functions and operations at the community-based practices, while supporting departmental and institutional initiatives.
The Community Division provides a wide breadth of clinical services caring for both pediatric and adult patients in ambulatory, inpatient, obstetric, and emergency settings. The division utilizes a variety of enhanced recovery after surgery pathways, a multimodal approach for pain control, and a wide variety of regional anesthesia techniques for the management of acute postoperative pain. This year, the Community Division, with departmental support, deployed Multidisciplinary
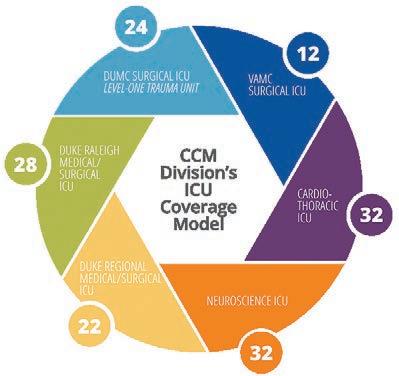
The Critical Care Medicine (CCM) Division’s mission is to improve the lives of critically ill patients at Duke and worldwide through: 1) delivery of high-quality, compassionate, equitable, and data-driven clinical care, 2) discovery of new knowledge, using rigorous and cutting-edge research methods, and 3) creation of diverse leaders in critical care, through innovative education and career development programs. The CCM Division experienced another year of progress in all of these pillars. In the clinical domain, multiple new faculty members were recruited from Duke and nationally to provide outstanding care across the division’s six intensive care units (including supporting the expansion of Duke Raleigh Hospital’s ICU to 28 beds).
Additionally, the division made progress in building a learning health care system for CCM through creation and utilization of a robust data infrastructure for CCM (Duke ICU Universe) and development of a health system-wide
Perioperative Outcomes Group metrics for Duke community facilities, allowing the faculty to promote safe and evidence-based perioperative care.
Many faculty hold hospital committee and leadership roles. This division has state representation on health care facility regulations with Dr. Neel Thomas being appointed by Governor Roy Cooper to the North Carolina Medical Care Commission. In 2023, Dr. Daniel Kovacs graduated from the Duke Clinical Leadership Program and was named medical director of anesthesia services at Duke Raleigh Hospital. Additionally, faculty in this division train anesthesiology residents at Duke Regional Hospital and SRNAs from two programs.



CCM quality improvement committee, learning health care conference, and ICU collaborative.
Several quality improvement milestones were achieved across our ICUs, including achieving significant reductions in centralline associated bloodstream infections (under the leadership of Dr. Nitin Mehdiratta). In the research domain, the division continued successful programs in basic science, translational research, clinical trials, and population health. Faculty published research in high-impact journals, including The Lancet, Critical Care Medicine and Anesthesiology. In the education domain, greater collaborations continue across CCM fellowships within the health system, creating a multidisciplinary learning environment. The CCM Fellowship curriculum (under the leadership of Dr. Nazish Hashmi) continues to innovate through the addition of simulation experiences, re-vamped conferences (including PBLD/case conferences), greater integration of quality improvement methods/practice into the curriculum, and greater personalization of training (including dual trainees in CCM/cardiac and CCM/OB). Additionally, the fellows all had the opportunity to present their research findings at major international conferences in the spring.
The GVT Division has always been very diverse, and continues to provide innovation, leadership and clinical excellence in many different areas. A highlight of the division is the abdominal transplant program, which takes care of patients undergoing liver, intestinal and kidney transplants, as well as an increasing number of multi-organ and multi-visceral transplants.
Dr. Jonathan Dunkman was appointed director of Liver Transplant Anesthesia in July 2023. He oversees a team of 10 liver transplant anesthesiologists and a growing program with more than 120 liver transplants last year and some of the best outcomes in the country. Recent innovations include the increased use of regional anesthesia with Dr. RJ Krom investigating the impact of external oblique blocks, early extubation in the operating room, and the use of a standardized enhanced recovery postoperative pain pathway on patient outcomes. Other research includes
Dr. Michael Manning investigating the use of hydroxocobalamin C for post-reperfusion syndrome and the use of transesophageal echocardiogram in liver transplantation, and Dunkman investigating the incidence and treatment of fibrinolysis.

The team also kept pace with innovations in surgical practice, such as an increased use of DCD donors and hepatitis C donors, and a dramatic increase in the use of ex vivo machine perfusion devices for transporting and preserving cadaveric livers. Future research aims to examine the effect of machine perfusion on patient outcomes.
Faculty of the Neuroanesthesiology, Otolaryngology and Offsite Anesthesiology Division have received numerous accolades for successes across the clinical, educational and research missions in the past year. Divisional faculty received nearly $2 million in funding from the National Institutes of Health (NIH), accounting for approximately 10% of the funding that led to Duke Anesthesiology’s historic #2 ranking in NIH funding by the Blue Ridge Institute for Medical Research. Dr. Miles Berger received four NIH grants, including two R01 grants for which he is the primary investigator, and his group published 13 papers related to delirium and neurocognitive disorders. Dr. Michael “Luke” James was awarded an R21 grant on a new brain cooling device and was selected as the treasurer of the newly-formed Neurocritical Care Foundation. Dr. Leah Acker received both the William L. Young Neuroscience Research Award and the John D. Michenfelder New Investigator Award from the Society for Neuroscience in Anesthesiology and Critical Care and was the first anesthesiologist to be awarded the Physician-Scientist “Strong Start” Award from the Duke University School of Medicine.
Clinically, the division’s footprint in the Neuroscience Intensive Care Unit has grown; it is now staffed by three neuroanesthesiologists: Drs. Amanda Faulkner, Luke James and Miriam Treggiari. Faulkner completed her ABLE project - leading the successful transition of anesthesia for electroconvulsive therapy from Duke South to the new Duke Behavioral Health Center. In the fall of 2022, Dr. Dhanesh Gupta was appointed the anesthesia medical director at Duke University Hospital with Dr. Nicole Guinn now serving as division chief; she continues

to lead nationally in the field of blood management, having been named the chair of the American Society of Anesthesiologists’ Patient Blood Management Committee.
This past spring, the division hosted the first annual Duke Advanced Airway Course in the Duke Human Simulation and Patient Safety Center, led by Drs. Vijay Ramaiah, Bret Stolp, and Chakib Ayoub. Course highlights included evidence-based lectures, difficult airway workshops, surgical cricothyrotomy, airway ultrasound, and case-based discussions.

The Orthopaedics, Plastics and Regional Anesthesiology Division took home the majority of awards at the 48th Annual Regional Anesthesiology and Acute Pain Medicine (RAAPM) meeting in Hollywood, Florida. Each year, more than 350 abstracts are presented at the annual meeting, from which three are selected as “Best in Meeting.” This year, two of the three prestigious awards went to abstracts submitted by Duke Anesthesiology trainees.

Dr. Emily Chen, a then regional anesthesiology and acute pain medicine fellow, presented her work on the safety of lidocaine spinals in total joint arthroplasty. She challenged the widely-held view that lidocaine spinal anesthesia has a high incidence of transient neurologic symptoms (TNS). Chen and colleagues have queried more than 240 patients in an ongoing prospective observational study and found that the incidence of TNS was zero, a surprising finding but one that she attributed to the comprehensive multimodal regimen used today.
Dr. Emily Barney Hall, a then CA-2 resident, presented the results of an experiment evaluating needle trajectories in adductor canal block and the risk of trauma to the nerve to vastus medialis. In simulated blocks in cadaveric lower limbs, this group
demonstrated that needles contacted or even transfixed that nerve in more than 50% of instances, and in her presentation, Hall was able to offer some solutions to mitigate that risk, including the use of nerve stimulation.
“Both trainees did an incredible job representing Duke Anesthesiology,” says Dr. Jeff Gadsden, division chief. “It’s clear to everyone in the global RAAPM community that Duke is at the forefront of generating new and exciting knowledge, and I’m thrilled that our trainees are able to be recognized for their scholarly accomplishments and leadership.”
The Pain Medicine Division has seen significant growth in advanced interventional procedures, including neuromodulation, as well as regenerative medicine. As neuromodulation technology has evolved and improved, we are now able to successfully target peripheral nerves with minimally invasive peripheral nerve stimulation systems with lasting benefit. There has been significant growth in utilization of these procedures at both Duke Pain Medicine and our Wake County pain practices (Duke Raleigh Hospital Pain Clinic, Duke Spine and Pain Management of Raleigh). Patients have seen quite dramatic improvement in pain and function, and some of these patient stories were featured in local news media. Additionally, Dr. Thomas Buchheit has seen steady growth in his regenerative medicine practice at Duke Innovative Pain Therapies.
Dr. Peter Yi, director of the Pain Medicine Fellowship, has brought innovative approaches to pain medicine fellowship

education and recruitment since his arrival in 2020. Recently one of these initiatives, performed in collaboration with Drs. Neil Ray and Noa Segall, was published on the use of an artificial intelligence chat bot to facilitate fellow recruitment in combination with live Q&A sessions. The study demonstrated that this innovation assisted in providing the information applicants were seeking, potentially improving the perception of the Duke Pain Medicine Fellowship. As pain medicine fellowship recruitment has shifted to primarily a virtual format, the chat box tool has assisted with recruitment of high-quality pain medicine fellows.


The Pediatric Anesthesiology Division continues its growth in all areas. It welcomed two new faculty: Dr. Martha Kenney, a doubleboarded pediatric anesthesiologist, joined the division on an NIH HEAL Diversity Supplement and has a strong research interest in improving pain outcomes for those with sickle cell disease; Dr. Matt McDaniel has returned home, bringing his pediatric cardiac expertise and interest in education and simulation.
Our educational mission has been strengthened by the approval and summer launch of an ACGME-accredited Pediatric Cardiothoracic Anesthesiology Fellowship – one of the first in the country – led by Dr. Warwick Ames. As the division seeks to expand its perioperative home and respond to the need for increased access and decreased length of stay, it has expanded the off-site coverage of all locations, almost doubling volume in the past year.
The Duke Pediatric and Congenital Heart Center was ranked #7 in the US News and World Report rankings in 2022, making it #1 in North Carolina and the only non-freestanding children’s hospital in the top 20. The pediatric anesthesiology team is a crucial part of this success and touches all aspects of the heart center.

Faculty member, Dr. Jon Andrews, was promoted to the
rank of major in the United States Army Reserve in January. He enlisted in the Army after the attacks on September 11, 2001. Upon successfully completing the Army Special Forces Qualification Course and Special Forces Medical Sergeant Course, he was awarded the Green Beret and assigned to an A-team with the 5th Special Forces Group. Between 2006 – 2011, he was deployed to Iraq and Afghanistan. In 2011, he was commissioned as a second lieutenant in the Army National Guard. His military career includes more than 20 years of combined service as an enlisted soldier and officer with the US Army, the Army National Guard, and the US Army Reserve. Major Andrews is currently assigned to Fort Bragg, North Carolina as an anesthesiologist with the 7458 Medical Operational Readiness Unit. We thank him for his service.

The Veterans Affairs (VA) Anesthesiology Service Division is piloting a new preoperative optimization intervention for frail patients undergoing high-risk surgery. The project titled, “Prehabilitation of Veterans with Exercise and Nutrition (PREVENT),” offers telehealth-based supervised exercise and nutritional support to deconditioned patients scheduled for highrisk surgery.
Using a telehealth platform, a dedicated exercise physiologist conducts aerobic and resistance exercise sessions tailored to each patient’s fitness level three times per week in the three to four weeks leading up to surgery. A nutritionist provides personalized nutritional advice and prescribes protein and vitamin supplements for the duration of the program. These interventions are resumed once the patient returns home and continue for another four to six weeks.
The PREVENT program combines the fundamentals of physical medicine and rehabilitation with state-of-the-art nutritional support and innovations in
care, such as telehealth, to optimize patients before high-risk surgery. This program has the potential to not only reduce complications and hospital readmissions, but also to maximize functional recovery and quality of life for thousands of veterans undergoing high-risk surgery every year. It is also the first step in the design and implementation of more widespread prehabilitative services for veterans living in rural areas and those with inadequate support or transportation. The results to date are very encouraging: the team has found marked improvements in fitness, as well as improved anxiety, depression and quality of life scores in patients following the intervention. The next step is to obtain support for the permanent implementation of this program and dissemination across other VA and nonVA sites.
Exercise physiologist, Leigh Ann Yeager, assesses a patient’s fitness following three weeks of nutritional and physical prehabilitation.
Members of the Women’s Anesthesiology Division are leading the way in managing high-risk pregnancies and developing national guidelines for the management of those complex cases. Cardiac disease is a leading cause of maternal mortality. To provide the highest level of care for women with cardiac disease in pregnancy at Duke, a multidisciplinary team of cardiologists, maternal-fetal medicine physicians, anesthesiologists, and cardiac surgeons have collaborated to form the Pregnancy Heart Team, which is unique to Duke and highlights the specialty cardio-obstetric care that patients receive at this institution. Dr. Marie-Louise Meng is the obstetric and cardiothoracic anesthesiology champion on this team; she works with team members to optimize all aspects of care for obstetric patients with cardiac disease, as well as plan for delivery and postpartum care. She was also the chair of the writing group and lead author of the recently published American Heart Association scientific statement regarding anesthetic care of the pregnant patient with cardiovascular disease.
Obstructive sleep apnea (OSA) is associated with several maternal and neonatal complications, but until recently, there were no guidelines available for the diagnosis or management of OSA during pregnancy. Dr. Jennifer Dominguez, in her capacity as the chair of the Obstetric Subcommittee of the Society of Anesthesia


and Sleep Medicine, led an international multidisciplinary group of pulmonologists, sleep medicine physicians, anesthesiologists, and obstetricians, and was the lead author for the recently published consensus guidelines for the management of the pregnant patient with OSA.
Sepsis is another high-risk condition associated with significant maternal morbidity and mortality. Dr. Melissa Bauer serves as the chair for the Alliance for Innovation on Maternal Health/American College of Obstetricians and Gynecologists Sepsis in Obstetrical Care Patient Safety Bundle; this bundle is planned for national implementation across 48 states to reduce maternal morbidity and mortality from maternal sepsis. She also serves as the physician lead for the Institute for Healthcare Improvement’s Innovation Change Package that is distributed to state perinatal quality collaboratives to provide step-by-step instructions and resources to guide operationalizing implementation and metrics.
The Center for Perioperative Organ Protection (CPOP) is achieving new standards in innovative clinical and translational research and publishing in the foremost prestigious journals. In a recent article published in Neuron, Dr. Luis Ulloa, director of CPOP, presented the fundamental implications of somatotopic autonomic networks in bioelectronic medicine.* These mechanisms are providing critical information to control perioperative organ function and design novel therapeutic strategies for perioperative organ protection.


Neuromodulation is emerging in this center as a promising therapeutic strategy to control organ function and resolve inflammatory disorders in several clinical settings. The CPOP is forming multidisciplinary translational research teams of competitive investigators for National Institutes of Health (NIH) proposals, including program project grants. Ulloa is collaborating on a prospective, randomized, controlled clinical trial of perioperative music medicine to improve surgical outcome. And, Ulloa and Dr. Wei Yang are collaborating on a newly-funded NIH project to study vagal control of tissue
SUMOylation as a novel anti-inflammatory target in inflammatory bowel disease.
CPOP faculty members are achieving
recognition and striving to improve perioperative care through innovative research. Yang received two NIH R01 grant awards to study “The Unfolded Protein Response in Ischemic Stroke” and “Immunosuppression After Cardiac Arrest and Resuscitation.” Dr. Huaxin Sheng has achieved significant goals on post-cardiac arrest recovery and was awarded (with Yang) an NIH U01 grant for a Duke testing site for the Stroke Preclinical Assessment Network (see pages 48-49).
CPOP faculty members are also fostering an environment to develop new investigators. Dr. Jamie Privratsky completed his studies on annexin A1 modulating mitochondria in ischemic kidney injury in collaboration with Ulloa and Dr. Hagir Suliman; Privratsky was awarded his first NIH R01 grant to study “Novel Mitochondrial Protective Properties of Annexin A1” and recently published his studies on septic acute kidney injury in Kidney International, one of the most prestigious journals in kidney research (impact factor of 19).
*Ulloa L. Neuron 111:10-4 (2023).

The United States Association for the Study of Pain meeting in April 2023 marked the first time that Duke Anesthesiology has hosted an annual society meeting. The local organizing committee consisted of multiple CTPM members and was chaired by CTPM director, Dr. Ru-Rong Ji. He is also a co-author of the newly-published book, “Neuroimmune Interactions in Pain: Mechanisms and Therapeutics,” which

provides a comprehensive review of neuroimmune interactions in various types of pain conditions. It features 16 chapters (with contributions from multiple CTPM faculty members) on immune cells, glial cells, toll-like receptors, immunotherapy, regenerative medicine, neuromodulation, exercise and diet, mechanisms-based pain treatment, and what patients need to know about pain therapy.
Congratulations to CTPM faculty Christopher Donnelly, assistant professor, Katherine Martucci, assistant professor, Satya Achanta, assistant professor, and Shad Smith, associate professor, on their new National Institutes of Health awards from the National Institute of Dental and Craniofacial Research, the National Institute on Drug Abuse and the National Institute of Environmental Health Sciences.
Congratulations to Drs. Andrea Nackley and Katherine Martucci on being elected to the US Association for the Study of Pain’s Board of Directors.
Duke’s
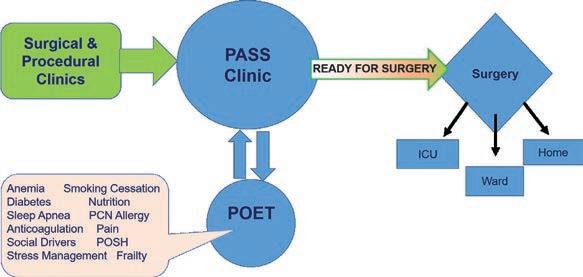

are celebrating another year of programmatic growth and expansion. In 2022, referrals to our seven optimization teams and our collaboration with the Duke Perioperative Optimization of Senior Health (POSH) program remained strong.
The influence and reputation of the Duke POET program have also continued to grow. In 2022, we welcomed four teams from other top academic medical centers as part of a new *PASS-POET preceptorship, which offers access to our Preoperative Anesthesia and Surgical Screening (PASS) and POET clinics for other hospitals to learn about the Duke method for preoperative optimization and population health. This year, we have continued to welcome more teams interested in adopting our paradigm—including
our first international team from Australia. Other advancements within our program over the past year include
1) welcoming Dr. Sharon McCartney as medical director of the POET anemia team. McCartney follows Dr. Nicole Guinn in this role and will continue to build upon the incredible foundation that she built;



2) undergoing a significant revision of Duke’s perioperative antibiotic policy, thanks in part to the work of our POET penicillin allergy team. Based on the clinical data generated from our POET patients, cefazolin is now recommended as the firstline antibiotic for patients with a reported penicillin allergy, even in the absence of formal testing; and
3) implementing a new optimization program focused on social drivers of health. The Perioperative Anesthesia and Surgical Screening (PASS) Clinic now has a case manager who is working with patients scheduled for total joint replacement surgery to improve their readiness for discharge to their home environment instead of a skilled nursing facility.

The Coaching, Advising, Mentorship, and Professionalism (CAMP) Program was developed as a way to combine coaching with mentorship, advising and professionalism in order to provide another valuable resource for faculty development within Duke Anesthesiology. Dr. Allison Ross, a pediatric anesthesiologist and an International Coaching Federation certified business, professional and team coach, leads the CAMP Program. This initiative is responsible for training a small group of departmental faculty (“flex coaches”) on techniques of coaching so that they may use these skills to help other faculty (“coachees”) navigate challenges and opportunities during career development. Flex coaches will gain expertise in listening and inquiry, which allows them to guide their coachees in finding their own passion and areas of interest, and in turn, will add to their own leadership development.



CAMP Flex Coaches:
Drs. Aurelio Alonso, Brandi Bottiger, Jennifer Dominguez, Sarada Eleswarpu, Nicole Guinn, Dhanesh Gupta, Grace McCarthy, Abigail Melnick, Marie-Louise Meng, Richard Moon, Becky Schroeder, Timothy Stanley, Ian Welsby, and Peter Yi.

As the health care industry continues to evolve, it is evident that innovative technology will remain a vital tool in the quest for improving patient outcomes while decreasing costs.
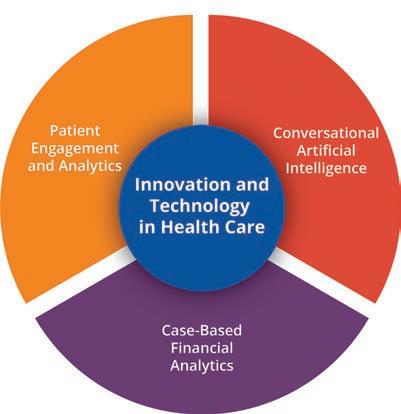
One of the leaders in this field is Neil Ray, MD, MBA, MMCi, the chief innovation and technology officer for the Duke Health Integrated Practice. Ray has played a central role in implementing and expanding the use of conversational artificial intelligence (AI) for patients and staff at Duke Health, resulting in decreased costs, improved efficiency and a reduction in workload for call center agents. Duke Health has implemented use cases related to patient appointment scheduling on the phone lines and a chat bot for patients live on MyChart. Ray was instrumental in bringing together multiple stakeholders for this foundational AI technology, which is now a component of Duke Digital Health’s strategic plan. Duke Health will soon have more use cases related to MyChart account creation, password management and patient records requests.
Ray is also exploring the concept of a comprehensive patient engagement platform that measures feedback through the various touchpoints and interactions a patient has with the health care system. Real-time patient engagement is an integral part of this platform and a pilot using multiple vendors has already successfully been completed. One of the key technologies with such a platform is machine learning and natural language processing, which are used to analyze every call that comes into the access centers. This will help Duke Health better understand a patient’s experience with our call centers in addition to the experience after a clinical visit. Using these analytics, call center agents can also focus on opportunities for improvement and identify areas of strong performance. Platforms like these can ultimately help Duke Health separate itself as a leading customer-focused and experience-obsessed health care organization.
Additionally, Ray and team are developing a financial analytics and visualization tool to help make better informed decisions based on case-based analytics. By using this type of data analytics, Duke Health can gain insights to improve patient care and optimize financial resources.
48 NEW GRANTS totaling nearly $14 million
BASIC SCIENCES 12 $5,529,328
CARDIOTHORACIC ANESTHESIOLOGY 7 $1,454,545
WOMEN’S ANESTHESIOLOGY 2 $1,396,317
ORTHOPAEDICS, PLASTICS AND REGIONAL ANESTHESIOLOGY 2 $1,152,823
HYPERBARIC MEDICINE 3 $1,141,840
NEUROANESTHESIOLOGY 4 $1,107,262
GENERAL, VASCULAR AND TRANSPLANT ANESTHESIOLOGY 7 $1,092,081
CRITICAL CARE MEDICINE 7 $1,051,287
PEDIATRIC ANESTHESIOLOGY 1 $24,320
PAIN MEDICINE 1 $10,628
VA ANESTHESIOLOGY SERVICE 2 $4,999 (not represented)
$5.5 million
TOTAL OF 16 NON-COMPETING CONTINUING GRANTS
Medical Countermeasures and Pain Translational Laboratory
Satya Achanta, DVM, PhD
Peri-Operative Neurocognitive Research Team (PORT) Laboratory
Miles Berger, MD, PhD
Regenerative Pain Therapies Program
Thomas Buchheit, MD
Neuroimmunology and Applied Pain Research Laboratory
Christopher Donnelly, DDS, PhD
Oxygen Transport Laboratory
Heath Gasier, PhD
Pain Relief and Opioid Mitigation Innovation Science (PROMIS) Laboratory
Padma Gulur, MD
Sensory Plasticity and Pain Research Laboratory
Ru-Rong Ji, PhD
Chemical Sensing, Pain and Inflammation Research Laboratory
Sven-Eric Jordt, PhD
Mechanistic and Clinical Pharmacology Laboratory
Evan Kharasch, MD, PhD
Critical Care and Perioperative Population Health Research (CAPER) Program
Vijay Krishnamoorthy, MD, MPH, PhD, and Karthik Raghunathan, MBBS, MPH
Molecular Pharmacology Laboratory
Madan Kwatra, PhD
Human Pharmacology and Physiology Laboratory (HPPL)
David MacLeod, MBBS
Human Affect and Pain Neuroscience Laboratory
Katherine Martucci, PhD
186
CURRENT ACTIVE RESEARCH GRANTS
Neurocognitive Outcomes Research Group
Joseph Mathew, MD, MHSc, MBA
FG Hall Environmental Laboratory
Richard Moon, MD, CM, MSc, FRCP(C), FACP, FCCP
Translational Pain Research Laboratory
Andrea Nackley, PhD
Kidney Protection Laboratory
Jamie Privratsky, MD, PhD
Multidisciplinary Neuroprotection Laboratory
Huaxin Sheng, MD
Pain Omics and Informatics Research Laboratory
Shad Smith, PhD
Neuroinflammation and Cognitive Outcomes Laboratory
Niccolò Terrando, PhD
Outcomes and Clinical Epidemiology in Anesthesiology (OCEAN) Laboratory
Miriam Treggiari, MD, PhD, MPH
Neuromodulation Laboratory
Luis Ulloa, PhD, MS
Nerve Injury and Pain Mechanism Laboratory
Thomas Van de Ven, MD, PhD
Duke Multi-Disciplinary Metabolic and Body Composition Assessment Team (MCAT) Laboratory
Paul Wischmeyer, MD
Molecular Neurobiology Laboratory
Wei Yang, PhD, FAHA
Multidisciplinary Brain Protection Program
Wei Yang, PhD, FAHA
Satya Achanta
National Institutes of Health: $241,500
Inhibition of Soluble Epoxide Hydrolase Protects Against Phosgene-Induced Lung Injuries
Ru-Rong Ji
Department of Defense: $1,444,257
Prevention of Pain Chronification and Neuroinflammation After Traumatic Brain Injury by Neuroprotectin D1 and GPR37 Signaling
Department of Defense: $1,601,314 Monoclonal Antibody-Based Therapeutics for Targeting MMPs and Diabetic Neuropathy
Madan Kwatra
ASLAN Pharmaceuticals: $368,690 IL-13Ra1 Signaling in Atopic Dermatitis
Galderma: $393,960
Prurigo Nodularis: Disease Burden and Rationale for Novel Therapeutics
Johns Hopkins University: $271,343 Biomarker Study of NCT05038982
Andrea Nackley
National Institutes of Health: $352,733
A Novel Clinically-Relevant Mouse Model of Chronic Overlapping Pain Conditions for Screening Analgesics
Joseph P. Mathew
July 1, 2021—June 30, 2022
Rachel Lance
Triton Systems, Inc.: $143,585
Massachusetts Institute of Technology: $118,851
Identification and Validation of a Novel Central Analgesia Circuit
National Institutes of Health: $740,086
Neurocognition and Greater Maintenance of Sinus Rhythm in AF (NOGGIN AF)
Madhav Swaminathan
Potrero Medical, Inc. Accuryn Registry Study
Ian Welsby
Global Blood Therapeutics, Inc.
GBT ESR
Michael Devinney
National Institutes of Health: $161,000
The Association of Blood-Brain Barrier Breakdown with Sleep Apnea and Postoperative Delirium
Jamie Privratsky
National Institutes of Health: $322,000
Novel Mitochondrial Protective Properties of Annexin A1
Joseph P. Mathew and Miriam Treggiari
National Institutes of Health: $342,852 Integrated Training in Anesthesiology Research
Wei Yang
National Institutes of Health: $414,468
Immunosuppression After Cardiac Arrest and Resuscitation
National Institutes of Health: $402,500
The Unfolded Protein Response in Ischemic Stroke
Miriam Treggiari
Edwards Life Sciences Corporation
HPI SMART BP 2021-01
Paul Wischmeyer
Abbott Nutrition: $196,000
Clinical Nutrition Training Virtual Fellowship Program
fNIRS Performance Monitor in Navy Divers at Depth
Miles Berger
National Institutes of Health: $810,435
APOE4 Dependent Regulation of CSF Complement Pathway Activation in the Development of Alzheimer’s Disease
National Institutes of Health: $214,794
Neuroinflammation in Postoperative Cognitive Dysfunction: CSF and fMRI Studies
David MacLeod
Medtronic, Inc.: $900,149
MDT DIGI2 Study
Noninvasix, Inc.: $252,674 NonInvasix
Melissa Bauer
National Institutes of Health: $810,961
Large-Scale Implementation of Community Co-Led Maternal Sepsis Care Practices to Reduce Morbidity and Mortality from Maternal Infection
Ashraf Habib
Heron Therapeutics, Inc.
Heron HTX-019-203
Marie-Louise Meng
Foundation for Anesthesia Education and Research: $124,911
Cardiovascular Risk Prediction for Improved Maternal Health
The only program created by anesthesiologists for anesthesiologists
Diagnostic point-of-care ultrasound (POCUS) is emerging as a useful bedside tool to rapidly narrow the differential diagnosis of acute organ dysfunction. Since 2019, Dr. Yuriy Bronshteyn has been working within the American Society of Anesthesiologists (ASA) to systematically add diagnostic POCUS to the armamentarium of anesthesiologists. From 2019 - 2020, as the chair of the ASA’s Ad Hoc Committee on POCUS, Bronshteyn led the effort to achieve
“Anesthesiologists may be reluctant to practice this skill set because of a lack of standardized training and/or push-back from hospital privileging committees. We hope this certificate program helps p racticing anesthesiologists surmount these two obstacles.”
DR. YURIY BRONSHTEYNpublication of expert panel recommendations on diagnostic POCUS, specifically for anesthesiologists, and propose a standardized curriculum in diagnostic POCUS for anesthesiologists to be administered by an ASA editorial board. In 2020, the ASA chartered the creation of the ASA POCUS Editorial Board in which Bronshteyn was named as its editor-in-chief. In this role, Bronshteyn has led the ASA’s efforts to develop a five-part certificate program in diagnostic POCUS that has already enrolled approximately 2,000 anesthesiologists since launching in 2020. The certificate covers the diagnostic POCUS applications identified by the American Board of Anesthesiology as being of highest relevance to perioperative anesthesiologists: 1) focused cardiac ultrasound; 2) lung; 3) gastric; and 4) abdominal free fluid scanning.
Duke University Medical Center has become one of the first medical centers in the nation to offer an Accreditation Council for Graduate Medical Education (ACGME) Pediatric Cardiothoracic Anesthesiology Fellowship Program; the first fellow, Dr. Michael Greenberg, began the program on August 1, 2023, officially launching the newly-established fellowship.


In early 2022, the ACGME published the milestones for a new pediatric cardiothoracic anesthesiology fellowship program; this was in response to the growing need for a recognized training pathway for pediatric and congenital cardiac anesthesiology as the patient population with congenital heart disease continues to expand. The Duke Pediatric and Congenital Heart Center was recently ranked seventh in the nation by US News & World Report and offers the perfect platform for education in an environment of clinical excellence and innovative thinking. This fellowship is led by Duke Anesthesiology faculty, Dr. Warwick Ames, who says, “We aim to make this another reason why Duke is deemed a center of educational excellence.”
MAY 23, 2023
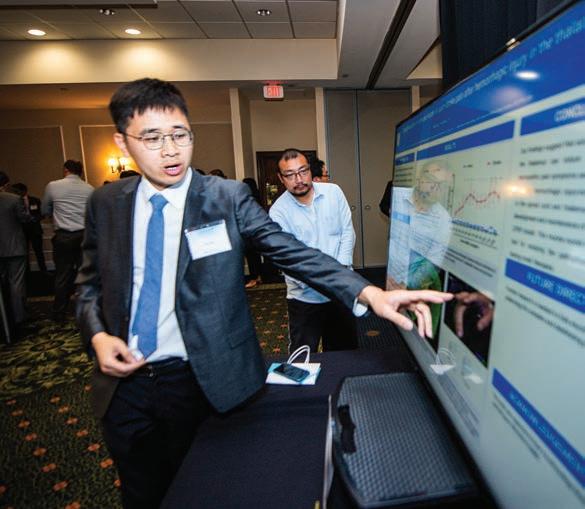
An abundance of scholarly activity and scientific excellence were on display at the 31st anniversary of Academic Evening — the department’s annual event aimed at advancing anesthesiology, critical care and pain management— ultimately enhancing the care of patients.
This year, an unprecedented number of 100 poster abstracts—ranging from basic science, clinical research and case reports—were showcased by junior-level investigators and faculty at Duke Anesthesiology’s 31st Annual Academic Evening, which took place on May 23 at the Millennium Hotel Durham.
“Once again we have been simply thrilled to see the depth and breadth of scholarly pursuits that both our faculty and trainees are engaged in throughout our department,” says Dr. Jeffrey Gadsden, event co-chair and professor of anesthesiology. “The fact that we emerged from a two-year pandemic MORE productive than ever tells you everything you need to know about the spirit of discovery and the value placed on research at Duke Anesthesiology.”
Dr. Miriam Treggiari, event co-chair and vice chair for research, kicked off the event with the traditional ringing of the late Dr. David S. Warner’s bell—signifying the beginning of presentations and in honor of Warner—recognizing the integral role he played in mentoring numerous investigators and advancing both basic science and clinical research within the department for nearly 30 years. The newly-established David S. Warner Award for post doc basic science research was presented to Dr. Yanting Chen. She received first place in this category for her project titled, “A Macrophage-Endothelial Immunoregulatory Axis Ameliorates Septic Acute Kidney Injury.”
“I am excited to share our findings at Academic Evening. And I am deeply grateful to receive the award for the recognition,” says Chen. “I would like to express my gratitude to my mentor Dr. Jamie Privratsky, whose expertise and mentorship were invaluable throughout the project. This recognition motivates me to continue pursuing this research study in the future.”
Another anticipated highlight of the annual event is the presentation of the Bill White Award for resident research. White was involved in the design, data control and examination, and statistical
analysis of biomedical studies in both observational and clinical trials within Duke Anesthesiology for more than 20 years. Dr. Andrew Breglio received first place in this category for his project titled, “A Novel In Vivo Model of Arrhythmogenic Cardiomyopathy.”
“I have always found Academic Evening to be an impressive display of meaningful research conducted by my colleagues. To be recognized amongst this group of peers is truly an honor,” says Breglio. “I owe much of the success of this project to the fantastic mentorship I have received from Dr. Andrew Landstrom and to the combined efforts of the other members of our research team.”
Dr. Talmage D. Egan, chairman of the Department of Anesthesiology at the University of Utah Health Sciences Center, was selected to serve as this year’s guest judge. In this role, he received the honor of determining the award winners in each category.

“The Duke Department of Anesthesiology enjoys a stellar reputation as a premiere anesthesiology program. My experience at the annual Academic Evening further bolstered the admiration and respect I have for the department,” says Egan, who is internationally regarded as a pioneer in the development of total intravenous anesthesia techniques. “Duke achieves the trifold mission of academic anesthesiology with great distinction. I was delighted to be part of the proceedings!” In his closing remarks, he left the crowd with an insightful message about why being an anesthesiologist requires the brain of an internist, the hands of a surgeon, and the heart of a psychiatrist. “There is no other time in human-to-human interaction where one person voluntarily surrenders their well-being more fully and absolutely to another person. The anesthetized patient is utterly and completely helpless. They can do nothing for themselves. In this very vulnerable and powerless state, the anesthetized patient is depending on the anesthesiologist to keep them safe by conducting the anesthetic, supporting their vital functions, and defending their human dignity.”
“We are very proud to see the rich, impactful and innovative work that has been accomplished just over this past year,” adds Treggiari. “This is a testament to the strong department culture of advancing discovery and changing the world, and the unwavering commitment to the academic mission.”

Post Doc Basic Science Research (David S. Warner Award)

1st Place: Yanting Chen, “A Macrophage-Endothelial Immunoregulatory Axis Ameliorates Septic Acute Kidney Injury.” Mentor: Jamie Privratsky.
2nd Place: Junli Zhao, “Electrophysiological and Behavioral Characterization of AnesthesiaActivated Neurons in the Central Amygdala in Mice.” Mentor: Ru-Rong Ji.
3rd Place: Angela del Aguila, “Glucocorticoid Signaling Mediates Occurrence of Lymphopenia After Cardiac Arrest.” Mentor: Wei Yang.
Fellow Clinical Research (Dick Smith Award)
1st Place: Mathew Makowski, “Sex Differences in Susceptibility to Central Nervous System Oxygen Toxicity.” Mentor: Heath Gasier.
2nd Place: Liliane Ernst, “The ED90 of Hyperbaric Bupivacaine for Cesarean Delivery in Super Obese Patients: An Up-Down Sequential Allocation Dose-Response Study.”
Mentor: Ashraf Habib.
3rd Place: Ivy Co, “Comparative Study of Bilateral Rectus Sheath Blocks with Liposomal Bupivacaine Versus Epidural Analgesia in Elective Radical Cystectomy Patients.”
Mentor: Hector Martinez-Wilson.
Resident Research (Bill White Award)
1st Place: Andrew Breglio, “A Novel In Vivo Model of Arrhythmogenic Cardiomyopathy.”
Mentor: Andrew Landstrom.
2nd Place: Kayla Pfaff, “Impact of Race, Ethnicity, and Developmental Status on Regional Anesthesia Technique for Calcaneal Osteotomy in Pediatric Patients.” Mentor: Lisa Einhorn.
1st Place: Megan Wong, “A Role for Blood-Brain Barrier Dysfunction in Delirium Following Non-Cardiac Surgery in Older Adults.” Mentor: Michael Devinney.
2nd Place: Andrew Padilla, “Anesthetic Management of Cesarean Hysterectomy for Placenta Accreta Spectrum: A Multicenter Retrospective Cohort Study.”

Mentor: Ashraf Habib.
1st Place: India Little, “Hyperoxia Reduces Heme Oxygenase 1 and Mitochondrial Dynamic Regulation in a Rodent Model of Sarcopenic Obesity.” Mentor: Heath Gasier.
1st Place: Chinwe Anumudu, “Medically Challenging Case: Non-Anesthesia Induced Malignant Hyperthermia in a Patient with STAC3 Disorder Undergoing Craniosynostosis Surgery.” Mentor: Lisa Einhorn.


1st Place: Andre Savadjian, “Reduce Intraoperative Albumin Utilization in Cardiac Surgical Patients: A Quality Improvement Initiative.”
Mentor: Negmeldeen Mamoun.



First medical center awarded accreditation in perioperative transesophageal echocardiography by the Intersocietal Accreditation Commission
Alina Nicoara, MD, FASE
Three Duke anesthesiologists earned ASE’s Outstanding Achievement in Perioperative Echocardiography Award
Madhav Swaminathan, MD, MMCi, FASE
Solomon Aronson, MD, MBA, FASE
Jonathan Mark, MD



Four Duke anesthesiologists served as chairs of ASE’s Council on Perioperative Echocardiography




Joseph Mathew, MD, MHSc, MBA
Solomon Aronson, MD, MBA, FASE











Alina Nicoara, MD, FASE

Madhav Swaminathan, MD, MMCi, FASE
First anesthesiologist elected president of ASE


Madhav Swaminathan, MD, MMCi, FASE



Obtain CME/CE credit through an interactive clinical nutrition training program led by internationally renowned experts.
Participants will learn:
• The newest cutting-edge science on nutrition risk identification




• Evidence-based nutrition care of pediatric and adult patients
• How to optimize patient outcomes with nutrition therapy
Course Co-Director Paul E. Wischmeyer, MD, EDIC, FASPEN, FCCM
Course Co-Director Sundar Krishnan, MBBS

I hope this letter finds all of you in good health and good spirits. This year marks the start of a new era for the School of Medicine and the Duke University Health System with the full implementation of the Duke Health Integrated Practice (DHIP). This new model integrates our clinical care into a single entity, allowing closer alignment with our research, education, and community health missions. DHIP will better equip the Duke Health enterprise to integrate patient care across entities as we move toward the promise of population health as well as to improve access and grow. It will facilitate the recruitment and retention of top providers and staff, all while supporting our academic, research, and community engagement missions.
particularly intractable areas, such as cancer, Alzheimer’s, infectious disease, and transplant immunology. Studying the very early and fundamental perturbations in biologic process will allow us to develop prevention strategies that can delay the onset and minimize the harmful effects of systemic health issues, such as heart, vascular, and metabolic diseases.
The School of Medicine has once again been recognized as one of the nation’s leading academic medical institutions. Earlier this year, the Blue Ridge Institute for Medical Research reported that the School of Medicine ranked 9th overall in federal research funding. Ten of our departments ranked among the top 10, with Duke Anesthesiology securing the No. 2 spot — a big jump from its already impressive 8th place ranking last year. Our consistently strong record of research funding, both school-wide and by department, is a testament to the excellence and innovation of our faculty, staff, and students.
We are committed to ensuring that every patient receives the compassionate, state-of-the-art care they expect from Duke, and that every physician and provider in our enterprise has the support they need to succeed and thrive. Together we are continually improving how we deliver health care to our patients, expanding our research capabilities, preparing the next generation of health care leaders, and building partnerships with our communities. Our research mission continues to accelerate through recruitment and retention of exceptional faculty and critical investments in science. With Duke Science and Technology, we are strategically focused on expanding Duke’s scientific leadership in areas where we can make the most transformational advances and improvements in health. By identifying our strengths and aligning our vision, Duke will be better equipped to address
We are now two years into the implementation of our “Dismantling Racism and Advancing Equity, Diversity, and Inclusion at the School of Medicine” strategic plan. We have made great progress, and much more must be done. Each new step fortifies our resolve to continue the necessary work of creating and sustaining a more just and equitable environment in which every member of the Duke community feels valued, important, and involved.
I am incredibly proud of the efforts of faculty, staff, and students across the School of Medicine. Through dedicated patient care, visionary research, innovative education, and active engagement in the community, you play essential roles in ensuring that we fulfill our missions and advance human health.
With warm wishes,
Mary E. Klotman, MD Executive Vice President for Health Affairs, Duke University Dean, Duke University School of Medicine Chief Academic Officer, Duke Health
I am incredibly proud of the efforts of faculty, staff, and students across the School of Medicine.

In 2022-23, Duke Anesthesiology formally established both the Paul G. Barash Professorship and the David S. Warner Professorship at the Duke University School of Medicine. These highly-coveted, permanently named memorials preserve the legacies of the late Dr. Warner, Distinguished Professor of Anesthesiology – one of the world’s most respected neuroanesthesiologists and one of the department’s most beloved faculty; and the late Dr. Barash, Professor Emeritus of Anesthesiology at the Yale School of Medicine – a renowned educator who held a special connection to Duke and departmental faculty.
These professorships honor their exceptional achievements, fuel scientific discovery, and invest in teaching and mentoring the next generation of leaders. Make a gift at anesthesiology.duke.edu/gift.



The Duke University School of Medicine selected four Duke Anesthesiology faculty members as recipients of a 2023 Faculty Award. Jennifer Dominguez, MD, MPH, earned the Excellence in Professionalism Award; Ashraf Habib, MBBCh, MSc, MHSc, FRCA, and Catherine Kuhn, MD, both earned the Leonard Palumbo Jr., MD, Faculty Achievement Award; and Chairman Joseph Mathew, MD, MHSc, MBA, earned the Research Mentoring Award (in the Career Mentoring Award in Clinical Science category). Dean Mary Klotman presented the awards to the recipients at the annual Spring Faculty Celebration on May 17 at the Doris Duke Center. Additionally, Joseph DeBlasio, a clinical nurse in Duke’s hyperbaric chamber, received a 2022-23 Duke Presidential Award –the institution’s highest honor for embodying Duke’s values – for fulfilling the wish of a terminally ill patient.

Dr. Ru-Rong Ji, William Maixner Professor of Anesthesiology, and Dr. Evan Kharasch, Merel H. Harmel Professor of Anesthesiology, have been named among the most “Highly Cited Researchers” in the world. These pioneers in their
fields represent the most influential researchers who have published multiple papers frequently cited by their peers that rank in the top one percent of citations for field and year in the Web of Science.
Duke
6,938 researchers
 Dr. Vijay Krishnamoorthy CCM Division Chief
Dr. Vijay Krishnamoorthy CCM Division Chief
Intensivists come to work every day in six intensive care units (ICUs) across four hospitals guided by one shared purpose - to improve the lives of critically ill patients at Duke and around the world. They weave compassionate humanity and detailed medical knowledge into the fabric of critical care medicine and provide high-quality, data-driven, and equitable clinical care for patients facing lifethreatening illness or injury.
They know that care for the critically ill cannot be delivered alone. It is a symphony of exceptional leadership skills and strong teamwork of health care providers that work in concert to build trust with patients and their families and help them navigate through a host of decisions, emotions, and choices, including end-of-life discussions.
The focus, says the new chief of the Critical Care Medicine Division, Vijay Krishnamoorthy, MD, MPH, PhD, is on “developing a ‘learning health system’ where science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the care delivery process - ultimately keeping patients and their families at the center of everything we do.”
Under the dynamic leadership of Krishnamoorthy,
appointed division chief in February of 2022, Critical Care Medicine at Duke is well-poised in realizing its vision to discover, deliver, and transform the future of critical care and become a world leader in this niche domain.
Krishnamoorthy has ambitious strategies to engage all stakeholders for expanding Duke’s critical care footprint well beyond its brick-and-mortar walls, especially in the clinical operations and learning health, research, and education domains.
The main principles that underscore all efforts are innovation and collaboration. Krishnamoorthy meets every week with his core leadership team (Nitin Mehdiratta, MD, clinical operations director, and Nazish Hashmi, MBBS, fellowship program director) and quarterly with all six ICU medical directors, to discuss innovative care processes, adopt best practices to improve patient outcomes, and keep efforts collaborative across various ICUs. Additionally, an annual retreat of the leadership team (comprising Mehdiratta, Hashmi, and all ICU medical directors) is held to develop broader strategic goals for the division.
As part of his clinical strategy (Figure 1), the team captures new knowledge through data derived directly from the delivery of care, informs Krishnamoorthy.
This data is transformed to become knowledge to help implement the best evidence into daily practice. The loop is complete when clinical practice improves and continues to capture data and inform subsequent management. “Through our informatics systems, we are able to capture data, evaluate it rigorously, and use it to optimize and innovate our practice,” adds Krishnamoorthy.
At the heart of this strategy is the Duke ICU Collaborative and the “ICU Universe,” conceived to collect and curate the entire critical care data generated across all ICUs in the Duke University Health System (DUHS) in Epic, the electronic medical record. “The data updates every midnight giving both historical and contemporary information to critical care teams,” informs Krishnamoorthy. The Duke ICU Collaborative helps to operationalize the “learning health system” and represents key stakeholders across all ICUs in the health system who work together to review data, share learnings across ICUs, and implement best practices. The Duke ICU Collaborative learning health system activities include: 1) a weekly summary of global evidence shared with providers to update them and encourage discussions on ways to optimize evidence-based practice and reduce variation in the processes of care; 2) a monthly learning health collaborative newsletter; 3) a quarterly learning health conference (to review Duke ICU data and share best practices) as part of CCM Grand Rounds; 4) a quarterly
ICU quality improvement committee discussion about case learnings, strategic implementation, and outcomes of improvement projects; and 5) rigorous research to evaluate the outcomes of interventions conducted across ICUs.
Information is developed and shared in a variety of ways. A WhatsApp forum provides a platform for faculty across ICUs to engage in informal (non-PHI) discussions surrounding evidence and best practices, while the quarterly learning health care conference (organized with Mehdiratta and pulmonologist, Daniel Gilstrap, MD) disseminates lessons learned from captured data and evaluates the impact of interventions. Local ICU data is also shared with medical directors for discussion in their respective faculty meetings.
Co-leading the Duke ICU Collaborative Quality Improvement Committee, Mehdiratta ensures that safety and quality of critical care services are maintained in six ICUs with 150 critical care beds across DUHS. “I am trying to create a more cohesive QI Committee throughout the hospital system.” He employs the “Plan, Do, Study, Act” strategy to identify problems and develop and implement workable solutions in clinical practice, while monitoring the transition of knowledge to practice. Participants, including physicians, advance practice providers, and nurses, work together to achieve this goal.
CLINICAL EDUCATION RESEARCH
6 ICUs
faculty
4 hospitals
40 intensivists 150 beds
8 CCM fellows per year
4 broad domains (Basic Science, Translational, Clinical Trials, Population Health)
6 NIH-funded investigators
Mehdiratta implements evidence-based strategies to see change happen in real time. One example of this tangible outcome is the central line-associated bloodstream infection (CLABSI) project, first implemented in 2021 in the Surgical ICU. With a multipronged approach, “we were able to reduce our CLABSI rates within one year, and we subsequently went without a single CLABSI for over 400 days,” he says proudly. Mehdiratta, along with his team (Staci Reynolds, Brandie Slagle and Christopher Sova) were awarded the Karsh Award for their outstanding work on reducing CLABSI rates in the SICU in 2022. They have received health system-wide accolades for their efforts in reducing hospital-acquired infections.
Along with his focused QI efforts, Mehdiratta is making concerted efforts to improve workflow by creating
a robust training and education process for a standard of care practice that can be successfully replicated to improve patient outcomes across the entire spectrum of critical care at Duke and beyond. As part of the CCM Fellowship, all eight fellows are required to complete quality improvement projects, coordinated by a designated QI fellow every year, informs Mehdiratta.

The CCM Division’s footprint in research is expansive and covers areas “from the level of the cell all the way to an entire population,” says Krishnamoorthy. For the population-level impact, Krishnamoorthy highlights the role of the Critical Care and Perioperative Population
Health Research (CAPER) Program that he co-founded and co-directs with Karthik Raghunathan, MBBS, MPH. This novel research program facilitates rigorous observational research using population health methods (epidemiology, health services research, health economics/policy, and implementation science) to advance knowledge and improve patient health outcomes in the perioperative and critical care space. Funded through department, industry, foundation, and federal grants, CAPER is a cross-collaborative hub for research on methodological innovation, injury epidemiology, resuscitation, analgesia and nutrition, multi-organ dysfunction, learning health care, and health equity.
Federally funded research programs among CCM Division investigators span a variety of critical care topics, including acute kidney injury, nutrition, rehabilitation after critical illness, traumatic brain injury, spinal cord injury, pneumonia, sleep, delirium, and host-microbiome interactions in critical illness, among many others. With a strong mentorship component, says Krishnamoorthy, “the division also
“Through our informatics systems, we are able to capture data, evaluate it rigorously, and use it to optimize and innovate our practice.”
- DR. VIJAY KRISHNAMOORTHYDrs. Mehdiratta (left) and Krishnamoorthy in the SICU at Duke University Hospital.
serves as a training ground for medical students, residents, fellows, and junior faculty interested in research in critically ill populations.”
Artificial intelligence and machine learning have opened up a myriad of future possibilities in the critical care space. “It’s another tool in our toolkit,” informs Krishnamoorthy, highlighting how it can help the intensivist analyze large volumes of high-fidelity granular data, especially waveform data that is too complex for traditional statistical models. “We are going to see more of these innovative models for disease deterioration, risk prediction, and predictive analytics,” he adds, urging physicians to also use qualitative judgment and
working to generate and maintain interest in ICU rotations and engage residents in education, such as grand rounds, lectures, and problem-based learning.”
In the face of a national shortage in critical care applicants, exacerbated by the pandemic that led to burnout in this high-acuity, high-stress environment of subspecialties, the division’s fellowship recruitment efforts have increased. Social media and the CCM website have been leveraged to showcase the critical care fellowship.
On offer are carefully curated didactics, simulation, echocardiography, and research experience during training. Fellows learn from faculty with expertise in various streams
be responsible stewards of these models as they define and refine clinical decision support.
Meanwhile, high-quality care requires high-caliber care providers. Krishnamoorthy’s focus is on recruiting faculty with widely recognized expertise that aligns with the broad and diverse spectrum of critically ill patient populations in the ICUs.
“We continue to attract and retain top talent to fulfill our clinical mission,” says Krishnamoorthy, adding that national leadership positions in education and research allow Duke Anesthesiology Critical Care Medicine to build its brand as one of the leading programs in the country. “Top recruits not only want to contribute and help grow some of our areas of excellence, but we also provide a fertile ground for career development in almost every domain of critical care,” he informs, pointing to a strong mentoring culture to ensure a pipeline of recruiting talent.
Hashmi concurs. “As the fellowship director, I spend a lot of time interviewing applicants and recruiting both internal and external candidates to the fellowship. In general, residents tend to gravitate towards subspecialties where they have had the best experiences. The faculty and I are actively
of critical care as they rotate in the SICU, CTICU, MICU, Neuro ICU, Duke Regional ICU, and various elective rotations where they interact with providers outside their department. In turn, the MICU and Neuro ICU fellows rotate in the SICU and Duke Regional ICU to gain a more comprehensive experience. Additionally, all critical care fellows, faculty and advanced practice providers are invited to attend virtual lectures, journal clubs and problem-based learning sessions. The virtual learning platform can be accessed by both faculty and trainees. And, the CCM Division invites experts from within Duke and nationally to collaborate on various aspects of critical care medicine.
Growing careers of faculty is also prioritized. “It’s not one size fits all,” says Krishnamoorthy, emphasizing pathways - research, education, and clinical operations - for faculty development and engagement with structured mentorship that supports and nurtures growth. “There are so many great established programs, like the ABLE Program, within our department and across the institution to help faculty in these domains. Faculty have different goals, and we really try to personalize
“Our strategy for success involves recruiting, developing and retaining our incredibly talented faculty. With this foundation, we will integrate and align our efforts in each domain (clinical care, education, research) to discover, deliver and define the future of critical care medicine together.”
- DR. VIJAY KRISHNAMOORTHYFIGURE 1: Moving from quality improvement to learning health.
their career development into how they want to see themselves grow.”
As clinical operations director, Mehdiratta shares Krishnamoorthy’s “big picture” view of operations across the critical care space focusing on strategic recruitment, creation of optimal work schedules for physicians, along with ensuring that transparency is maintained in professional billing and clinical documentation. He also keeps lines of communication open to help address concerns quickly and efficiently. “Listening to what people have to say is more powerful than telling them what to do,” says Mehdiratta. “I find it very satisfying when you can see a problem, make a plan, and then actually enact a change in real time to make a difference with our staff, faculty, patients and their families.”
Keenly aware of the issue of physician burnout, the leadership team has employed a four-point strategy to address this ongoing crisis, informs Krishnamoorthy. The first step is to recreate a feeling of community and encourage more in-person gatherings to “decrease depersonalization” caused by the pandemic. The second effort is to improve daily workflow and streamline scheduling to increase predictability. “In many of our ICUs, we have started to schedule our ICU time one year in advance,” adds Krishnamoorthy. Mehdiratta also emphasizes the importance of optimizing schedules for physicians, as well as respecting their non-clinical time and time away from work. Third, institutional resources, including Duke’s Personal Assistance Service and various programs, are also available to assist faculty and staff while maintaining confidentiality and privacy. Finally, and most importantly, Krishnamoorthy stresses the need to monitor signs of burnout and take preemptive measures. Divisionwide surveys, in addition to ACGME and Duke Culture Pulse surveys, help keep them informed.
CUTTING-EDGE
The shortage of critical care specialists is making the ICU leadership find creative ways to provide access to intensivists for underserved populations. According to Krishnamoorthy, the team is working on a plan with the health system to develop a proposal that would expand Duke’s consultative and collaborative reach across rural North Carolina. The plan involves the use of telehealth for local physicians in ICUs that lack intensivists in these underserved communities.
Undoubtedly, critical care at Duke is a service that requires an entire health care team, including bedside nurses, respiratory therapists, speech and language pathologists, physical and occupational therapists, dietitians, pharmacists, advanced practice providers, and physicians, to work cooperatively with a focused goal of improving critical illness outcomes.
It’s a job the CCM Division and its leader know well as they strive to innovate and stay contemporary by seamlessly merging detailed medical knowledge and best evidence-based practices with the humanity of critical care. BP
rowing up in the US as a Cuban American, Jennifer E. Dominguez, MD, MHS, witnessed how social determinants of health such as language and cultural differences, or level of education can negatively impact patients’ health outcomes.
“I’ve seen my own family members navigate a number of health issues that were complicated by low medical literacy, mistrust of and difficulty navigating the health system, and by barriers in access to health care,” she says. “So, early in life I learned that those social determinants can negatively impact patients’ health outcomes and need to be addressed.”
Those personal experiences made a lasting impression on Dominguez, who sought to learn more about how to support patients navigating these types of challenges while she was a student in New York City. She volunteered with a Harlem Hospital-based organization to help patients identify resources in the community to address issues such as food and housing instability, employment, domestic violence, and childcare. Once she entered medical school at Yale, Dominguez volunteered in her school’s free clinic and became a leader of the Latino medical students’ organization. There, she advocated for diversity and inclusion in the medical school’s admission process, provided support to underrepresented in medicine (URiM) students, and ran a program for local URiM high school students to learn more about pathways
to careers in health professions. “Being a part of that community of URiM medical students at Yale was crucial to my success in medical school,” recalls Dominguez.
When she joined Duke Anesthesiology faculty in 2013, Dominguez sought a similar community and became active in the department’s Anesthesiology Inclusivity Committee (AIC), which was established more than a decade ago. In 2020, she was named the co-chair of the AIC, along with Dr. Adeyemi Olufolabi Those years of experience prepared Dominguez for her newly-appointed role as interim associate vice chair for equity, diversity and inclusion within Duke Anesthesiology, in which she aims to expand the visibility and scope of the department’s commitment to advance equity and inclusion; she is the first person to serve in this newly-created role. Her initial steps involved developing and implementing a strategic plan for the program and building an Equity, Diversity and Inclusion (EDI) Leadership Team. She was supported in these efforts along with other EDI leaders as a participant in the Duke University School of Medicine’s Racial Equity Learning Arc, a program focused on building competency around collaborative EDI planning and strategic development.
As an obstetric anesthesiologist, Dominguez draws passion and motivation for the EDI Program’s vision, mission and strategy from witnessing patient
Mission Statement:
To cultivate a just and inclusive culture in which individuals thrive and are dedicated to alleviating suffering, improving health and well-being, and promoting social justice for all, through excellence in innovation, education, research, service, and professional growth.
Dr. Jennifer Dominguez, Interim Associate Vice Chair for EDI
experiences during the peripartum period. She points to the high maternal mortality and morbidity rate in the United States compared to peer countries as an indicator of how disparities can impact patient outcomes. According to the Centers for Disease Control and Prevention, the maternal mortality rate in the US in 2021 was 32.9 maternal deaths per 100,000 live births, while the risk of dying in the peripartum period for non-Hispanic Black mothers was 2.6 times the rate for white mothers (69.9 deaths per 100,000 live births).
“We have the highest rate of maternal mortality of any developed country in the world, and the rates have increased in recent years. Marginalized groups suffer a disproportionate burden of the morbidity and mortality,” Dominguez says, adding that she and the EDI team are focused on implementing a strategic plan to develop a more
and support for the EDI leaders across the school under the leadership of its first vice dean for EDI, Dr. Kevin Thomas.
“The School of Medicine has been undergoing a robust process over the last couple of years, launching an anti-racism campaign called ‘Moments to Movement,’ which has allocated more resources and greater institutional attention to EDI issues,” Dominguez says. “They have provided structure, resources and training to all of the School of Medicine EDI leaders to support their work within their individual departments.”
The five strategic pillars of the anesthesiology department’s EDI Program are aligned to support its vision and mission: 1) representation; 2) education; 3) environment and culture; 4) quality and patient care; and 5) research. With Dominguez’s leadership, she and the EDI champions will advance strategic
robust program that advances health equity for marginalized populations. “Identifying and eliminating health disparities within anesthesiology, critical care and pain medicine is my North Star for this program,” says Dominguez of the program’s vision.


Bringing a wide range of voices and stakeholders into the EDI conversation is a major focus of Dominguez’s approach. Within the EDI Leadership Team, she has appointed champions among faculty and trainees across the department, who will work within their focus areas to identify opportunities, implement programs, and foster and support an inclusive culture.
The Duke Anesthesiology EDI Program is aligned with the School of Medicine’s strategic plan for advancing equity, diversity and inclusion, which was implemented in 2021 and serves as a guide for individual departments to coordinate their efforts. Dominguez also serves on the School of Medicine’s EDI Leader Council, which provides development, community
goals and initiatives within these domains that are impactful and sustainable.
The representation pillar addresses recruitment and retention of diverse faculty, trainees and staff. While women are no longer underrepresented in US medical schools, says Dominguez, they remain underrepresented within anesthesiology training programs and among academic faculty. Physicians of American Indian or Alaska Native, Black, Latino, or Native Hawaiian or other Pacific Islander identities remain underrepresented in medicine (URiM) and anesthesiology, according to the Association of American Medical Colleges. Resident recruitment is a vital component of Duke Anesthesiology’s EDI Program. When Dominguez became cochair of the department’s AIC in 2020, one of her first initiatives was to work closely with Dr. Annemarie Thompson, the residency program director, to look at the recruitment process and address any potential biases or barriers.
“We looked at each step of the process, from the ways in

which people learn about our programs, to how we screen applications, and who interviews or interacts with our applicants on their interview days,” she says.
From that analysis, a team of diverse faculty that included the EDI Leadership Team’s Dr. Eric JohnBull was assembled to develop a standardized set of behavior-based questions for potential candidates to ensure all applicants would get similar questions during their interviews. They also were revised to include questions about cultural competency, such as how candidates would care for patients from different backgrounds. Several of the department’s fellowship programs also implemented similar changes to their recruitment processes.
“With these changes, we’ve already been able to attract and recruit more diverse trainees into our residency and fellowship programs in the last few years than we had previously. The
students connect with mentors within the department for shadowing opportunities. The EDI team also has established a scholarship program to support travel and living expenses for qualified URiM visiting medical students to rotate at Duke University Hospital in anesthesiology. In 2022, the department supported two URiM fourth-year medical students during their visiting rotations; and there are plans to continue offering this type of support.
Additionally, Dominguez says the department has forged a strong relationship with the Student National Medical Association (SNMA), which represents the interest of Black medical students. She and Dr. Grace McCarthy, the EDI Leadership Team’s champion for medical student education, have plans to strengthen ties with other medical student affinity groups. As part of that collaboration with SNMA,
2022 intern class was the most diverse group of residents ever at Duke Anesthesiology. We also have seen continued growth in the representation of women in our residency program to exceed national averages for anesthesiology residency training programs,” reports Dominguez.
She says the department also has been able to retain several of those fellows to stay on as faculty, increasing the diversity of faculty that future students and trainees are taught and mentored by. Strategies to increase the representation of URiM faculty within the department have been implemented in tandem and have started to yield results. “The input of EDI champions for residents, fellows and faculty will be crucial in helping us improve recruitment and retention efforts across all of these groups. In the future, we plan to add a staff champion to the EDI Leadership Team,” says Dominguez.
And to support diverse students once they’re admitted to medical school, Dominguez and her team have established several programs that enrich their education. For example, Duke Anesthesiology helps women and underrepresented

Duke Anesthesiology works with Duke’s Health Professions Recruitment and Exposure Program, which provides professional development and mentoring to URiM high school students interested in pursuing careers in health care, often through on-campus workshops. During a recent event, the department hosted students in the Duke Human Simulation and Patient Safety Center to practice procedures and interact with medical students, faculty and residents.
“They learned how to place endotracheal tubes and intravenous lines in mannequins in the simulation lab, but I think most importantly, they heard from individuals on a diverse panel about their paths to a career in medicine, the different obstacles that they overcame and how they navigated them,” says Dominguez.
For her, an effective EDI strategy must include an education component; not only has she modified the curriculum for the Duke Obstetric Anesthesiology Fellowship, of which she is the program director, she led a national committee to revise the ACGME curriculum for all obstetric anesthesiology fellowship programs to include more health equity topics, among other updates. One of her strategic goals for the EDI Program is to collaborate with the residency program leadership and the department’s two appointed EDI education champions, Drs. Amanda Kumar and Peter Yi; together, they will create a comprehensive health equity
“There has been a lot of literature that suggests that patients do better with a diverse workforce that represents their backgrounds and interests. Diversifying the workforce is an important strategy to address health inequities.”
- DR. JENNIFER DOMINGUEZ
STRATEGIC PILLARS
EDUCATION
ENVIRONMENT AND CULTURE
CORE OPERATING VALUES

Inclusion
REPRESENTATION
RESEARCH
Humility
Holistic
QUALITY AND PATIENT CARE
Empathy
Collaborative
“Identifying and eliminating health disparities within anesthesiology, critical care and pain medicine is my North Star for this program.”
- DR. JENNIFER DOMINGUEZ
curriculum for anesthesiology residents that will prepare them to be astute in recognizing and responding to the barriers that may prevent certain patients from receiving the care they need. Global health equity will be a part of this curriculum; the team is considering ways for members of the department to learn from the experiences of trainees, faculty and CRNAs who travel abroad for global health initiatives under the leadership of Olufolabi.
“One of the most effective ways to address health disparities is by educating our next generation of physicians and continuing to educate ourselves,” says Dominguez. She and Yi both serve as course instructors for the medical






of the department to participate in together.
Under the fifth EDI pillar of research, Dominguez is focused on supporting health disparities research within the department, fostering collaborations and connections, and impacting the way departmental research is conducted to be more inclusive and equitable; these efforts are in collaboration with the vice chair for research, Dr. Miriam Treggiari, and the EDI research equity champion, Dr. Melissa Bauer, who brings a wealth of experience in conducting equity-focused research to the team. In addition, a health equity research working group has been formed within the department’s Critical Care and Perioperative Population Health Research (CAPER)




school’s Cultural Determinants of Health course for second-year medical students. And many departmental faculty, including leadership, have gone through in-depth racial equity training since 2020. “I’ve learned so much by participating in these courses and engaging in thoughtful discussions with members of our community.”
Other initiatives under the newly-restructured EDI Program will include quality and patient safety strategies to examine and address potential health disparities within the care that the department delivers. Dominguez will collaborate with Dr. Abigail Melnick as the EDI Program’s quality and patient safety champion and Dr. Brad Taicher, director of anesthesia patient safety and quality, to identify opportunities to improve health equity for all of the patients that receive anesthetic care at Duke. She also aims to strengthen ties between the department and the community by planning and encouraging volunteer events for members
Program, and the department hosted its first ever “Equity in Action” Grand Rounds in January where researchers from across the department presented their health equity work.
As Dominguez looks to the future of the EDI Program, she points to its mission statement as the guiding principle for what she hopes to accomplish: To cultivate a just and inclusive culture in which individuals thrive and are dedicated to alleviating suffering, improving health and well-being, and promoting social justice for all, through excellence in innovation, education, research, service, and professional growth.
“There are plenty of opportunities for any member of our department to contribute to this work in a way that is meaningful and impactful to them, and that will really influence our department and institution, our specialty, and our patients in the future,” she says. “I am energized by and grateful for the opportunity to collaborate and make a difference in ways that are lasting.” BP
Top row, left to right: Education Champions: Drs. Amanda Kumar and Peter Yi, Medical Student Education Champion: Dr. Grace McCarthy, Trainee Recruitment Champion: Dr. Eric JohnBull, Faculty Champion: Dr. Jeanna Blitz, Fellow Champions: Drs. Liliane Ernst and Miguel Yaport, Resident Champions: Drs. Ashley Vincent and Theresa Rizk, Quality and Safety Champion: Dr. Abigail Melnick, Research Equity Champion: Dr. Melissa Bauer, Global Health Equity Champion: Dr. Adeyemi OlufolabiBy encouraging the entrepreneurial spirit, unfettered imagination, and unchecked ambition, the DREAM Campaign inspires Duke Anesthesiology faculty and provides them with the wherewithal to achieve the impossible. Together with our supporters, we are transforming the future of patient care.


Help us continue to train the leaders of tomorrow, develop the careers of our faculty, and protect quality of life for years to come.

Satya Achanta
Leah Acker
Solomon Aronson
Karsten Bartels
Helene Benveniste
Randall Brewer
Sorin Brull
Thomas Buchheit
William Bundschuh
James Caruso
Anne Cherry
Richard D’Alonzo
Lisa Einhorn
James Eisenach
James Feix
Jeffrey Feldman
Manuel Fontes
Brenda Gerhardt
Stephen Gidley
William Greeley
Katherine Grichnik
Alina Grigore
Dhanesh Gupta
Ashraf Habib
Sabet Hashim
Lawrence Haynes
Paul Jaklitsch
Sven-Eric Jordt
Laurie Kaiden
Jonathan Katz
Tamara Kim
Kathryn King
Jerry Kirchner
David Klein
Harry Kochat
Stephen Kushins
Michael Lasecki
Richard Leber
Andrew Lutz
Family of William Maixner
Jonathan Mark
Katherine Martucci
Joseph Mathew
John McManigle, Jr.
Timothy Miller
Holly Muir
Nancy Murray
Mark Newman
Stephen Packer
John Parham, Jr.
Helen Pavilonis
Nicole Peloquin
Cathleen Peterson-Layne
Ann Pflugrath
Vincent Phillips
Walter Plunkett
Margo Powell
Patricia Pritchard
Jamie Privratsky
Francis Quinn, Jr.
Teodulo Remandaban
Russell Roberson
E. June Santa
Kenneth Sauve
David Schinderle
Noa Segall
Robert Sladen
Mark Stafford-Smith
Thomas Stanley, III
Timothy Stanley
Stanley Research Foundation
Dawn Sweeney
Miriam Treggiari
David Tunnell
Kevin Vorenkamp
Deryl Warner
Lindsay Warner
Seth Warner
Richard Watson
Richard Wolman

Noriko Yokoo
Daniel Yousif
15 years of giving DREAMCAMPAIGN.DUHS.DUKE.EDU
DREAM CAMPAIGN | WILLIAM MAIXNER PROFESSORSHIP | PAUL G. BARASH PROFESSORSHIP | DAVID S. WARNER PROFESSORSHIPThe Duke DREAM Campaign was established to support Duke Anesthesiology’s research programs and initiatives. As implied by our motto, we empower great minds to turn dreams into reality.
The DREAM Innovation Grant (DIG) supports innovative high-risk investigations with potential for high-reward to accelerate anesthesiology, perioperative, critical care, and pain management research.


DREAM CAMPAIGN GOALS
Establish Endowed Professorships to invest in world-class faculty who would, in turn, secure extramural funding. Interest dollars from these endowments are to be used to support investigator salaries and provide them with the time and resources necessary to develop research programs.
Raise Funds to support research through the DREAM Innovation Grant, known as DIG.
DREAM CAMPAIGN UPDATE
$17M $1,021,109 15 Years
of the DREAM Campaign
Establish Philanthropic Support as a long-term mechanism of limiting the adverse consequences of cyclical federal funding. > > in extramural funding received to-date
in DREAM Innovation Grants have led to more than . . .
Read more about the campaign and make a gift! Visit: dreamcampaign.duhs.duke.edu

The concept behind the DREAM Innovation Grant (DIG) – first launched in 2010 – is simple, yet brilliant. An annual competition is held among early to midcareer faculty members within Duke Anesthesiology, who do not have established NIH funding (past or present). Competitors submit their most innovative research ideas to a panel of judges for review. Proposals that demonstrate the perfect blend of ingenuity and practicality are selected, and winners are announced at the department’s annual alumni reception.
DIG recipients can receive up to $40,000 in seed money for their innovative pilot studies, which ultimately help them apply for and obtain extramural funding.
This grant creates an avenue for healthy competition among faculty, inspires ingenuity, promotes the careers of young physician investigators, enhances donor communication, and furthers the department’s academic mission.
DIG funds are reserved to support an early career scientist (within five years of completion of a residency, fellowship or PhD) and/or used as a seed grant to help mid-career investigators obtain preliminary data to support a new application to the National Institutes of Health or other federal agency.
DIG IMPACT:
“I was fortunate to receive Dream Innovation Grant funding as I progressed from trainee to independent investigator. It supported a new research direction for our group, integrating our prior work with mitochondrial quality control in sepsis with a newlyavailable mouse model of graft dysfunction after heart transplantation, which is directly relevant to my clinical work as a cardiothoracic anesthesiologist. Through this supported work, we created a strong collaboration with the Duke Surgery Transplant Immunology group and generated preliminary data that then led to a National Institutes of Health application and two extramural foundation career development grants. In turn, these have supported my completion of coursework for the Clinical Research Training Program, which will continue to pay dividends well into the future.”
- ANNE CHERRY, MD: 2016 DIG RECIPIENT
DREAM INNOVATION GRANTS ARE FUNDED THROUGH A COMBINATION OF: Alumni Faculty Private Companies Private Donors

DIG IMPACT:
2022 TOP DONOR: Stanley Research Foundation: $15K
“The Dream Innovation Grant infused renewed energy into my research, allowing me to explore new therapeutic targets for curing neurological diseases. The preliminary data from the pilot work was crucial to secure our current brain research funding. Furthermore, the experiences we acquired were invaluable and positioned our team to successfully serve as a testing site for the National Institutes of Health’s multicenter Stroke Preclinical Assessment Network.”
-
HUAXIN SHENG, MD: 2012, 2019 DIG RECIPIENT

MD: Duke University
PhD: Massachusetts Institute of Technology
Residency: Duke University
“A Pilot Feasibility Study of Day-of-Surgery: PeriOperative Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) Effects on Neurocognitive and Neuroinflammatory Trends (POTENT+)”
DR. LEAH ACKER and colleagues seek to evaluate transcutaneous auricular vagus nerve stimulation (taVNS) as a non-invasive therapy for the prevention of postoperative delirium in older patients. Her proposal addresses the topic of brain health, specifically an intervention to reduce postoperative cognitive dysfunction in older patients. The project addresses the significant problem of postoperative delirium occurring in older adults and leverages the regulation of inflammatory pathways mediated by the vagus nerve via the cholinergic anti-inflammatory reflex.
With this DREAM Innovation Grant, Acker and investigators plan to implement a non-pharmacological and non-invasive intervention consisting of applying transcutaneous auricular vagus nerve stimulation during the intraoperative and postoperative periods to reduce postoperative cognitive dysfunction. The team proposes a set of feasibility studies to assess treatment timing (intra- vs immediately postoperative) and a set of preliminary studies to assess the effects of intra- vs immediately postoperative taVNS on heart rate and plasma biomarkers of inflammatory resolution or postoperative delirium incidence/severity.
This work is based on promising preclinical data and extends a currently ongoing study involving the preoperative application of transcutaneous auricular vagus nerve stimulation. The scientific rationale for using taVNS, a non-pharmacological approach, is well supported by preclinical data and holds promise to help achieve the long-term goal of developing this novel technology for human patients.
Strong enthusiasm for this project stems from several considerations: the novelty, simplicity, and non-invasiveness of the approach; the mechanistic and clinical relevance of the project; the thoughtful design of the feasibility pilot study; and the high potential for follow-up funding. Acker has assembled a strong team of mentors and collaborators for this project, including Drs. Heather Whitson (primary), Niccolo Terrando, Marat Fudim, Luis Ulloa, Miles Berger, Joseph Mathew, Kamrouz Ghadimi, Carl Pieper, and Ms. Mary Cooter-Wright.


Providing state-of-the-art methodology for clinical, basic science and translational research empowers Duke Anesthesiology to explore revolutionary clinical inquiries by using innovative investigation methods.

Through significant research in neuroscience, molecular biology, molecular and human pharmacology endeavors, our team is making crucial advancements for patients worldwide.
Wei Yang, PhD, FAHA
RESEARCH: The Quest for New Therapies to Improve Ischemic Stroke Outcome
Christopher Donnelly, DDS, PhD
RESEARCH: Defining the Neural Architecture of the Murine and Human Temporomandibular Joint for Advancing Orofacial Pain Therapies
Niccolò Terrando, BSc (hons), DIC, PhD

RESEARCH: Neuro-Immune Interactions in Postoperative Delirium

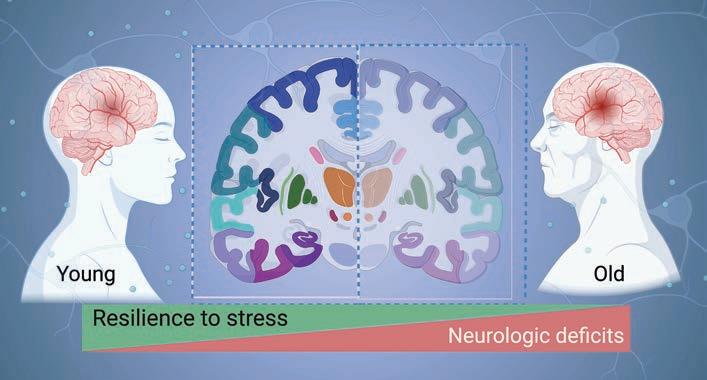 WEI YANG, PHD, FAHA
WEI YANG, PHD, FAHA
An ischemic stroke occurs when the blood flow to part of the brain is cut off. It is the most common type of stroke and accounts for about 87% of all strokes in the nation. The high incidence of stroke-induced disability presents a major burden on families and health care systems. This burden will only increase as our population ages since age is the key non-modifiable risk factor for stroke. We currently have very few treatment options to offer stroke victims. Thus, new stroke treatment strategies are urgently needed.
Dr. Wei Yang’s long-term research goal is to develop new treatments that will improve outcome after ischemic stroke, especially in elderly patients (Figure 1). The current stroke research in his lab is focused on strategies that boost recovery of stroke-impacted brain cells and harness brain remodeling processes.
Proteins are the key biologic molecules
that do most of the work in cells. Thus, protein homeostasis (proteostasis) is essential for cell survival and organismal health. Cellular proteostasis is rigorously maintained by a complex network that underpins the cell’s resilience to stress. However, this resilience declines with aging. One major component of this network resides in the endoplasmic reticulum (ER), a critical organelle for protein maturation. Disruption of ER proteostasis leads to ER stress, which activates multiple adaptive response pathways, collectively known as the unfolded protein response (UPR). The primary purpose of the UPR is to restore cellular proteostasis and thereby promote cell survival. Yang and others have demonstrated that ischemic stroke disrupts cellular proteostasis and causes
ER stress in the brain. Therefore, a promising therapeutic strategy to help restore proteostasis in brain cells after stroke is to boost the UPR within the proper time window. Yang’s Molecular Neurobiology Laboratory has uncovered a wealth of insights into the role of the three UPR branches in neurons after stroke. However, little is known about the involvement of the UPR in astrocytic cells after stroke. This knowledge deficiency constitutes a major barrier to the development of UPR-based stroke
therapeutics. To address this knowledge gap, his on-going research (a five-year $2,012,500 NIH R01 renewal grant) is using mouse genetic tools to manipulate individual UPR branches specifically in astrocytes and to clarify their roles in stroke. Such new knowledge will then empower the field to evaluate the therapeutic potential of targeting the UPR using various selective pharmacologic tools.
Another area of Yang’s stroke research aims to advance our understanding of the role of neuronal activity in stroke recovery. To enhance brain plasticity, neuromodulation strategies, including brain stimulation, have been explored in stroke therapy. However, clinical studies that have used various forms of brain stimulation after stroke have yielded inconsistent results, highlighting a knowledge gap about the role of neuronal activity in stroke recovery. Indeed, the underlying roles of specific neuronal populations during the stroke recovery phase are poorly understood, and it is not yet known how modulation
DUKE UNIVERSITY became one of just six medical institutions in the nation to be selected as a testing laboratory site for the renowned National Institutes of Health’s (NIH) Stroke Preclinical Assessment Network (SPAN).
The Multidisciplinary Brain Protection Program aims to discover novel and effective therapeutic strategies of brain protection and recovery through a deep mechanistic understanding of the pathophysiology that underpins brain disorders.

of specific neuronal cell activity affects stroke outcome as a function of age. To address these critical questions, Yang has been closely working with his collaborators, Drs. Huaxin Sheng, Dennis A. Turner and Junjie Yao, and has designed a comprehensive, novel approach, capitalizing on DREADDbased chemogenetics, in vivo gene delivery, and advanced acoustic angiography imaging. This on-going research (a two-year $442,750 NIH R21 grant) is expected to generate critical information for the development of innovative stroke therapeutics by optimizing
neuromodulation paradigms and developing new neurotechnology. Stroke is a complex disease, demanding collaborative efforts for discovery of new, effective therapeutics. To foster team research in stroke, Yang has assumed the role as director of the Multidisciplinary Brain Protection Program (MBPP), established by Duke Anesthesiology; its investigators have expertise ranging from basic molecular biology to clinical science and span multiple departments across Duke (Figure 2). Earlier this year, Duke University became one of just six medical institutions in the nation to be selected as a testing
laboratory site for the renowned National Institutes of Health’s (NIH) Stroke Preclinical Assessment Network (SPAN) to assess the efficacy of interventions selected by SPAN to improve long-term stroke outcome. The Duke SPAN site, which is funded by a three-year $1,764,172 U01 grant and led by Sheng and Yang (both of Duke Anesthesiology and the MBPP), is expected to accelerate the translation of the research pipeline and advance the discovery of promising interventions that can then be successfully advanced into clinical trials to achieve better recovery for stroke patients nationwide. BP
Temporomandibular disorders (TMD) are the most common form of chronic orofacial pain, affecting five percent of adults in the United States. Despite substantial clinical and research interest in this area, progress to identify and target pathophysiological mechanisms underlying TMDs has been slow. The lack of meaningful progress is due in large part to our relatively primitive understanding of the basic neuroanatomical, molecular, and physiological features of sensory afferents present within the temporomandibular joint (TMJ) tissues.
Dr. Christopher Donnelly is the recipient of a UC2 award, titled “Neural Architecture of the Murine and Human Temporomandibular Joint,” in response to the National Institutes of Health’s Restoring Joint Health and Function to Reduce Pain (RE-JOIN) Consortium. The scope of this consortium is to acquire a comprehensive understanding of the types and distribution of nerve endings present in joint tissues to aid in the identification of molecular mechanisms that underlie chronic pain conditions involving the joints, thereby accelerating the development of new therapeutic modalities.
In this multi-PI application with collaborators from the University of Michigan, Donnelly and his team have set the ambitious goal of defining the innervation of articular and peri-articular tissues that compose joints, with an emphasis on the sensory neurons that mediate nociception. This work is significant because it will lead to an understanding of the neurological mechanisms that underlie chronic orofacial pain in patients with temporomandibular disorders and other orofacial pain conditions. With a background in dentistry, Donnelly not only brings innovation to this project, but also relevant clinical expertise in the field.
The project focuses on elucidating the anatomy of the temporomandibular joint due to the severe health burden of temporomandibular disorders, one the most common orofacial pain conditions. The team’s overarching objective is to create a comprehensive atlas of the sensory neurons that innervate the tissues which compose the temporomandibular joint in mice and in humans. This anatomical atlas with physiological and functional mapping will be developed both in health and pathological states.

To accomplish their goals, the team proposes to develop and implement several innovative new tools and techniques to study the TMJ, including magnetic resonance imaging with stereotactic injections of TMJ tissues, fluorescent labeling of afferents fibers with transcriptomic analyses reflective of innervation plasticity. They will also use advanced techniques to map somatosensory neuron subpopulations innervating the TMJ. One of the highly progressive and innovative aspects of this research that brings a very comprehensive characterization of the structure, function and dysfunction of the TMJ relies on the in vivo recording of sensory neuron activity during orofacial function and in the presence of acute or chronic pain stimuli, with concurrent behavioral phenotyping and chemogenetic modulation.
The research experiments are expected to produce synergistic information describing the neuroanatomical, molecular, and functional properties of TMJ-innervating sensory neurons in mice and humans, culminating in the creation of a publicly accessible platform to facilitate the conceptual understanding of TMJ sensory function in health and chronic pain states. While this project is focused on the TMJ, the innovative tools and techniques developed in this research will be useful as a template for future studies of other joints. BP
AWARD: Three-year $5,734,530 UC2 grant
FUNDING SOURCE: The National Institutes of Health’s (NIH) National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
HIGHLIGHT: Selected as one of just five UC2 awards that make up the RE-JOIN Consortium – part of the broader NIH Helping to End Addiction Long-term (HEAL) Initiative, an aggressive trans-agency effort to accelerate scientific solutions to treat pain and end the national opioid epidemic.
“This research will comprehensively define the cellular, molecular and neurophysiological properties of the sensory neurons that innervate tissues of the temporomandibular joint. Beyond accelerating our understanding of orofacial somatosensation, this research will reveal mechanisms of joint pain that can be used to develop new clinical interventions and pain therapies.” – DR.
 CHRISTOPHER DONNELLY
CHRISTOPHER DONNELLY
Delirium is a quintessential neurologic complication characterized by changes in cognition, attention and arousal. Aging is the most prominent risk factor for postoperative delirium; however, it remains unclear how aging contributes to the pathogenesis of this common neurologic complication. Delirium is observed frequently after routine surgical procedures such as orthopedic surgery, where it greatly impacts patients, families and caregivers, and adds significant costs to our health care. Delirium is particularly insidious in vulnerable patients, especially those with pre-existing neurodegeneration such as Alzheimer’s disease (AD). More than five million people in the United States suffer from dementia, including AD, and commonly require surgical interventions, such as orthopedic surgery. After a common fracture repair, postoperative delirium
occurs in up to 89% of patients with preexisting dementia. Delirium in these vulnerable subjects further associates with poorer prognosis and even two-fold greater risk for one-year mortality compared to patients without dementia or delirium. Despite its prevalence, the mechanisms underlying this complication remain unknown and without effective therapies.
Dr. Niccolò Terrando and his team of investigators are dedicated to understanding how surgery drives delirium in aged and vulnerable individuals. Using an integrated multidisciplinary and translational approach, they are particularly interested in how the activation of the immune system drives brain inflammation (i.e. neuroinflammation), impairing neuronal function and leading to acute changes in behavior during aging and neurodegeneration (Figure 1). Their long-term goal is
FIGURE 1: Putative mechanisms involved in the pathogenesis of postoperative delirium during aging and neurodegeneration. Aging and dementia are the most significant risk factors for delirium. Both states are characterized by chronic inflammation (including inflammaging). The AD brain has additional hallmarks of vulnerability, herein the focus is on preexisting Aβ pathology. Surgery triggers a systemic inflammatory response that can disrupt the blood-brain barrier (BBB) and amplify delirium risk in patients. Detailed characterization of the neuro-immune signaling after surgery is currently missing. Factors, such as fibrinogen, are known to activate microglia cells. Astrocytes also represent another cell type that respond to surgery. Astrocytes directly release specific neurotoxins that can compromise surrounding neurons, further contributing to BBB dysfunction, and overall neuronal damage in delirium.

to define the mechanisms underlying delirium and to develop effective approaches to reduce this devastating complication. Over the years, these efforts have been supported by multiple grants from the National Institute on Aging. And, through the recent renewal of a five-year $4,311,630 R01 grant, they continue to advance new knowledge on how surgery impacts brain function in ADlike mice by focusing on specific neuro-immune signaling at the blood-brain barrier. Previous work from Terrando and his team has discovered that orthopedic surgery in mice triggers acute changes in beta-amyloid, a key hallmark of the AD brain, and is accompanied by marked changes in the brain vasculature. The blood-brain barrier is a key interface responsible for protecting and regulating the brain microenvironment from peripheral signals and is gaining significant attention in postoperative delirium. To better interrogate the immune interactions at the blood-brain barrier, Terrando and his team have developed new tools leveraging organ-on-chip technology (Figure 2) combined with animal models that have uncovered changes in new cellular targets, including pericytes and perivascular macrophages, that become dysfunctional after surgery. They are currently applying these tools to model more complex interactions in the ADvulnerable brain and better reflect the brain state during delirium superimposed on dementia.
Over the duration of this project, multiple collaborations have generated new paradigms to 1) better characterize delirium-like behavioral states with William Wetsel and Ramona Rodriguiz at the Duke Behavioral and Endocrine Core, 2) develop novel bioelectronic approaches to safely regulate the immune response after surgery harnessing the vagus nerve with Warren Grill at Duke Biomedical Engineering (BME), 3) implement new microphysiological systems to model neuroimmune interactions with Shyni Varghese at Duke BME and the Harris Gelbard and James McGrath laboratories at the University of Rochester Medical Center, and 4) apply innovative analytical tools to define the single-cell landscape in response to surgical trauma and delirium with Katerina Akassoglou at the Gladstone Institutes. These efforts are contributing
FIGURE 2: Blood-brain barrier (BBB) on chip to study neuroimmune interaction in delirium. The device was developed in collaboration with the Varghese lab at Duke BME. Image of the microphysiological platform for brain cells co-culture to generate a model of the BBB. The BBB-on-chip device consists of two layers of polydimethylsiloxane substrate separated by the polyester track etched (PETE) membrane, which acts as a basal membrane. The bottom layer has a vascular channel dividing into eight branches of 300 μm width each to culture human brain microvascular endothelial cells, and the top layer has a 5 mm × 5 mm square well that forms the brain chamber. The brain chamber is located on top of the vascular channels to co-culture brain cells with a brain microvascular endothelial cells separated by the PETE membrane.
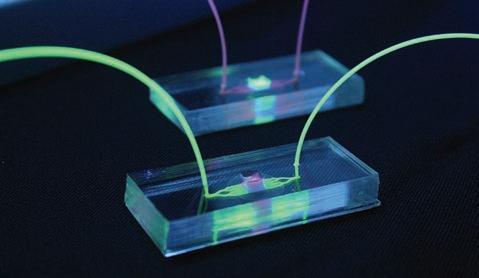
to an advanced understanding of how surgery affects the brain and are already resulting in translational studies that support the premise that similar pathological features are also present in the human brain after anesthesia and surgery.
Over a decade ago, in collaboration with the Akassoglou laboratory, Terrando and research teams discovered that fibrinogen, a critical driver of neuroinflammation in multiple neurologic conditions, is deposited in the brain after orthopedic surgery. In this R01 renewal, these teams will continue to define how surgery impairs the blood-brain barrier, both using animal models as well as organ-on-chip technology to dissect neuroimmune communication in AD. The rationale for the proposed research is that successful completion will advance our understanding of how surgery affects the immune system and will provide new tools of relevance to delirium, neurodegeneration and aging. Such knowledge is highly significant because it has the potential to explain how surgery impacts the vulnerable brain and identify novel targets to prevent postoperative delirium. BP
MTDS: Mitochondrial damage associated molecular patterns
PMN: Polymorphonuclear Leukocytes
ROS: Reactive Oxygen Species
PVM: Perivascular Macrophage
RM, Wetsel WC, Varghese S, Terrando N. Protective effects of omega-3 fatty acids in a blood-brain barrier-on-chip model and on postoperative delirium-like behaviour in mice. Br J Anaesth. 2023;130(2):e370-e380. PMID: 35778276.

In February, I had the incredible opportunity to participate in my very first global health trip to Ghana. The experience left me with unforgettable memories that I will always cherish and that have had a positive and lasting impact.

During the two-week trip, we spent half of our time at Tema General Hospital, where we focused on improving maternal care during and after cesarean delivery and gynecological procedures. One of the most significant lessons we taught the care team was appropriate dosing for intrathecal opioids and utilizing multimodal analgesia for postoperative pain control. Additionally, we helped change the current practice of having mothers lie flat for six hours post-cesarean to prevent spinal headache and hypotension, to having them sit up immediately in the Post-Anesthesia Care Unit to help facilitate neonate bonding and decrease Neo-
natal Intensive Care Unit admissions. Overall, the nurse anesthetists were very appreciative and open to receiving helpful tips on how to improve care for their patients. We were able to witness practice changes happen in real time after our training sessions.
During the second half of the trip, we spent time observing the anesthesia teams at the Greater Accra Regional Hospital and taught very bright anesthetist students about blood products, respiratory mechanics, monitors utilized in the Intensive Care Unit, and burn management at the Ridge Hospital Nurse Anesthesia School. While in
the operating rooms, I witnessed firsthand how the hospital staff made the best use of their limited resources. Even with limited supplies, they managed to think about the big picture of utilizing their resources to provide for the population of patients instead of giving one patient all the medications they had available. I also witnessed the use of thiopental for induction during a case, which is a drug I have only ever read about in anesthesia textbooks. Furthermore, it was interesting to see how the hospital systems are structured and how patients are supposed to pre-buy most of the medications they will need for their procedure, as well as bring in items from home including clothes, sheets, food, and toiletries prior to admission into the hospital. It was an eye-opening experience to see how they can make do with what they have. Outside of the hospital, we were able to explore the city of Accra. As a group, we experienced the enriched cuisine, culture, art, music, and most importantly, the traffic. My interactions with the Ghanaian people were nothing short of positive. They are very welcoming and hospitable. We visited historical sites such as Kakum National Park, Elmina Castle (the biggest slave castle for transatlantic slave trade), and the Ghana National Mosque (the second largest mosque in West Africa). Dr. Adeyemi Olufolabi was kind enough to arrange for me to pray with the Muslims in Accra in the Grand Mosque on a Friday, which is the day of worship for Muslims.

It was a wonderful experience to see different cultures all come together to observe the Friday lecture and pray in unity.
I would like to thank Dr. Olufolabi for making this global health experience one that I will never forget and Dr. Jennifer Dominguez for making this trip happen during our fellowship. I’m grateful to have participated in such a meaningful experience, and I will end this with Dr. Olufolabi’s favorite saying for the trip, “T.I.A. This is Africa.” BP

This past February, I had the opportunity to travel to Ghana with Dr. Adeyemi Olufolabi and the organization Kybele. In Ghana, our goals included teaching nurse anesthesia students, observing anesthetic care on labor and delivery as well as in the main operating rooms, helping introduce enhanced recovery after cesarean delivery (ERAC) protocols, and helping collect data for quality improvement (QI) initiatives. It was especially meaningful to be involved in the implementation of ERAC and QI initiatives in order to help improve efficiency and minimize cost in a setting where resources are limited.

What I appreciated most about our work there was the focus on selfsustaining improvements. The trip was not a self-limited “drop in” mission, but the goal was to provide the participating hospitals with the knowledge and skills needed to make sustainable improvements in anesthetic care even after we left. Seeing how outcomes and patient satisfaction were improved by rolling out small changes, like allowing mothers to breastfeed immediately after a cesarean, was very empowering. Moreover, one of my biggest clinical takeaways was that providing safe and effective anesthesia can be done with simple resources, and perhaps we sometimes overcomplicate things in our

resource rich environment.
Outside of the clinical experience, my favorite part of the trip was the people I got to meet. What struck me the most was that everyone in Ghana was entrepreneurial. From food blogging to roofing companies, the majority of people had their own side businesses, and there is a general atmosphere of growth and development. It was very exciting to feel how much potential Ghana has.
My experience in Ghana was one of
the most impactful experiences I have had in health care. I am so grateful to Dr. Olufolabi and the department for making this trip a possibility. BP
Every year during my time as a Duke Anesthesiology resident, like clockwork, CA-3s would appear back in the resident lounge having been noticeably absent for the month prior. “How was it?” everyone would invariably ask—to which the responses were unanimously some version of “it was incredible – I didn’t want to come back.” This was, of course, my first exposure to the global health rotation with Dr. Adeyemi Olufolabi. Early in residency, before having rotated through labor and delivery, I hadn’t yet met Dr. O, but I somehow felt as if I knew him, having heard the endless stories of other residents’ trips with him and the incredible work he was doing year after year in Africa. When I finally did get the chance to work with him (“on a typical, peaceful and quiet, week of labor and delivery nights”), I knew without a doubt that I had to sign up to travel with him.
For our trip in February, we traveled to Ghana, where we worked with the Kybele organization to learn from, and
teach, a multidisciplinary group of clinicians and health care workers— all in an effort to improve maternal and neonatal outcomes after childbirth. Our dayto-day experiences were more varied than I could have ever anticipated — delivering classroom-based lectures, rounding in the Intensive Care Unit, and both observing and teaching in the perioperative environment of three separate facilities. What was constant, though, was the openness and welcoming nature of our Ghanaian hosts. While a limited and, at times, a complete lack of important resources was easy to appreciate throughout our time in Ghana, it was the resiliency of the people that left the greatest impression on me. We met so many motivated, talented and truly exceptional health care workers who, without fail, were relentlessly optimistic about the future of their system and who were tirelessly working to help
It is rare that you have an opportunity to spend an extended period encapsulating yourself within another people’s culture.
When I heard about the global health opportunity all the way back when I was applying to residency, I immediately wanted to be involved. As I prepared myself for the trip to Ghana, I had simple goals: go with the flow, be adaptable and try something new every day.



As I sit here reflecting on the experiences I have had, I am surprised by my two biggest realizations during this trip. Foremost, my time there helped me remember why I chose to be in medicine. At some point, we all started our journey with the intention of helping others. The people of this country live that message every day. The health care workers of this country are at a disadvantage; whether it be staffing or lack of resources, there is a limitation to the care they can provide. Yet, they never once complain or make excuses. They come to the hospital every day with pride, with good intentions and a love for their patients. During the time I spent with these workers, all they asked was for advice on how they can provide better care. There is a pride
their patients.
Even outside the hospital we found friendly and welcoming Ghanaians at every turn as we learned about their history, culture, cuisine, and their triumphs and struggles as a nation. Through the entirety of our trip, Dr. O went out of his way to enrich our limited time in Africa and, as he put it, give us the “true global health experience.” It was an experience I will never forget.
And so, at the end of February, after a life- and perspective-changing trip, just like the CA-3s I saw all the years prior, I walked back into the lounge. It was incredible – I didn’t want to come back. BP
the people of Ghana have for their work and their institution that is overlooked here in the United States.
Secondly, I was amazed by which we were welcomed with open arms by the Ghanaian people. The people we met wanted us to know and understand the place they proudly call home. Whether it was sharing their life stories or an authentic meal, the only hope was that we would better understand their love for their country. I am forever grateful for my time abroad and all those who were kind enough to share their experiences with me. I hope to remember that when you open yourself to others, they will show you the same in return BP









I tell people that my journey to Duke was a slow and steady journey eastward - starting in California where I grew up and attended college. Then I was off to Wisconsin for four years of not just learning medicine, but attempting to tolerate the cold and like the Packers. This all led to a place that I now consider home. I came into medical school unsure of what my path would ultimately be. However, I knew that I was entering a field where I would have the privilege of connecting with people in their most vulnerable of moments. I found anesthesiology rather serendipitously and found it to be the perfect mix of all the aspects of medicine I enjoyed, with high acuity, thoughtful medical management and procedures. The relationships you
forge in anesthesiology are brief, intense and important, and I cherish the ability to be there for patients at a time when they may be at their most vulnerable.
I feel incredibly lucky to train at Duke, to say the very least. The acuity and breadth of cases is unmatched. The faculty make great role models, and I aspire to emulate them as I start my training. It’s also inspiring to be at an institution that is at the forefront of so many different aspects of the field, from research to perioperative medicine.
On a more personal level, I have felt a level of support here that I never could have imagined possible from a residency program. Residency is challenging, and with good reason. We are training to be exemplary physicians that can make the right decisions for patient care. Residency is also hard, however, because “life” still happens in the midst of the challenges of training. I feel lucky to be at a program where I know from first-hand experience that my co-residents, faculty and administration truly care about me and each other. Our department has a saying of “what we do changes lives,” and I can say with certainty that this program has changed mine.

Studying medicine at the National University of Ireland, Galway, I remember thinking that the anesthetists always seemed like the coolest people in the hospital. They thought about the nuts and bolts of acute illness with problem solving style that appealed to my background in physics. But it was during research electives with the Xtreme Everest group at University College London that my path really started to cross with the world of anesthesia and perioperative medicine.
After that summer in London, spent crashing anesthesia conferences as a student, it seemed that Duke’s name was synonymous with modern anesthesia. From this point on, I realized that coming to the US for residency would provide unparalleled training. As a PGY3, having worked as house staff in Dublin and London hospitals, I jumped ship and came to Duke. The journey itself was surreal; the COVID lockdowns in Dublin stopped us traveling more than two kilometers from home for most of the spring and now I was packing my bike and kitesurfing gear onto a flight.
From my first days at Duke, I was struck by the passion and inquisitive approach of the staff here in both the clinical and research settings. At Duke, it is possible to find an expert in any field; this creates an incredible environment to develop as a clinicianscientist. The CAPER research group welcomed me into their world and have been an immense support during my time here. Together, we formed a research team with collaborators across the university and internationally, including Duke National University Singapore. This team has now been supported by the Duke Climate + Health initiative, demonstrating the university’s and health system’s innovative and forward facing approach. My biggest clinical takeaway so far has been learning to identify challenging cases and trusting my training when they arise.
The residency program here keeps us all on a consistently steep learning curve, creating a culture of continuous growth in which we all progress together. Whether it’s in the hospital, biking in the mountains, kitesurfing off the Outer Banks, or playing music together, the experiences I’ve had with the residents and faculty speak to the unique environment that the people at Duke create.
I have felt a level of support here that I never could have imagined possible from a residency program.
At Duke, it is possible to find an expert in any field; this creates an incredible environment to develop as a clinicianscientist.















How has your training accelerated your practice of anesthesiology?
The fast-paced nature of the OR environment at Duke prepared me well. I am grateful for faculty who allowed me to be hands on with both bread and butter and advanced pain procedures as a resident, which allowed me to hit the ground running as a fellow. And, the robust and cutting-edge regional anesthesiology experience at Duke allowed me to be very comfortable with ultrasound-guided procedures and bring new skills to my hospital.
How did your training prepare you for being an anesthesiologist in a pandemic?
Duke’s stance on protecting residents during the peak of the pandemic is something that really stands out to me in hindsight. Most places are not as protective of their residents, and you see the difference when residents are the primary workforce compared to greater collaboration between CRNAs and residents that is seen at Duke. You can tell a lot about the leadership of the department during crisis, and I am thankful that I was able to train in a department run by Drs. Joseph Mathew and Annemarie Thompson and others, who truly made me feel seen and appreciated throughout the pandemic and beyond.
What are your greatest lessons from the Duke Anesthesiology Residency Program?
You do not have to change who you are and what you value in order to accomplish your goals. I was intimidated by the perceived faster pace and personality differences of those in the northeast compared to the south. I remember being told that I don’t have to change my personality to fit in; that discussion made a world of difference as I have seen those words come to fruition, and I realize that something that could be seen as a deficit in a certain environment can actually be what sets you apart. Additionally, Duke does an amazing job in building well-rounded anesthesiologists. The robust research arm, the clinical volume, paired with great faculty teaching is second to none, and I think it molds residents who can hold their own in those respects wherever they go.
What do you miss the most about Duke/Duke Anesthesiology?
The camaraderie amongst residents, fellows and faculty.
To train in an environment with such great leaders in the field and brilliant peers who are incredibly humble was such a blessing, and I am incredibly grateful for that. More so Durham related, I also miss Mkokko Ramen.
Why anesthesiology?
While to us, the day-to-day events that encompass the practice of anesthesiology become very routine, for the patients, oftentimes they are presenting for a surgery that will change their lives, so being able to care for them in this most vulnerable time is a great privilege. I chose pain as a subspecialty because of its interventional nature and being able to utilize procedural skills to impact patients’ lives and function. Pain is debilitating for so many people and there are so many psychological, physiologic and social aspects that influence pain. I have found great joy and purpose working with this population of patients.
What keeps you going?
What keeps me going is when I think back to my senior year in high school, sharing a two-bedroom apartment with eight other people, trying to limit any distractions and achieve my dream of getting into Duke University; when I visit my mom in rural Virginia and wanting to get into a position to do more for her; thinking about all the tears shed after visiting my brother in prison for the majority of my teenage and adult life. Residency is extremely challenging. Fellowship is hard. Medicine in general can be incredibly exhausting, but given some of the things I have overcome, it keeps things in perspective. I am very privileged to be able to take care of patients every day, and I am incredibly grateful for Duke Anesthesiology for allowing me an opportunity to change my family’s life.
Take full advantage of all the opportunities afforded to you. From the clinical opportunities, to research, to global health, Duke really is a unicorn of an anesthesiology program. Now that I have graduated and have had the opportunity to see how things are done elsewhere, I have an even greater appreciation for my experience at Duke. The opportunities to grow as an anesthesiologist and a human are endless in this department.

Pediatrics, Duke University Hospital
What was the draw to become a faculty member of Duke Anesthesiology?


For me, the draw is the same as it was as a trainee – this is a department that believes in constant innovation in its clinical, research and educational missions, and backs that belief up with an investment of time and energy to help each team member identify and pursue their career goals. I was able to begin that journey as a resident in the ACES Program, with worldclass mentoring and resources for my research projects. And as a faculty member, I’m lucky enough to continue that journey with further mentoring and investment in my development in innovation and technology alongside the clinical mission.
How did your training prepare you for being an anesthesiologist in a pandemic?
Core to an anesthesiologist’s practice is flexibility and working with the resources available. Going through the CA-3 year at the beginning of the COVID-19 pandemic, my class learned to take each day as it came. Some days brought lots of cases requiring prioritization, others brought ICU airways with best-available protective equipment, others brought emergency cases in patients with uncertain clinical status. Our faculty modeled decision making under pressure, and our residency class is now taking those lessons forward into a health care environment where pandemic effects linger and new challenges are always on the horizon.
What are your greatest lessons from the Duke Anesthesiology Residency Program?
The program provided the opportunity to get to know role models who are innovating in anesthesiology, critical care medicine and pain medicine in truly profound ways. One of the best features of our program is seeing how faculty approach the same clinical situation with different strategies. We as trainees could draw on that variety to build our own approaches to clinical problems. But the biggest lesson I hope to carry forward in medicine and in life is that there will always be more styles to learn. I hope to keep an open mind going forward in practice and in life, and never be afraid to learn a new technique or explore a new viewpoint.
What is your fondest memory of residency?
I remember being a fresh CA-1 doing big cases under the
watchful supervision of fantastic senior residents; it seemed like every time I was at risk of getting in over my head, one of them would miraculously appear and guide me on the next steps. My fondest memory of residency was being a senior resident on call a couple of years later and recognizing that same look of relief on junior residents’ faces when I stopped by their operating rooms to check on them. This residency program and the department really focus on giving people the tools and support to grow at every stage.
Why anesthesiology?
Anesthesiology is full of contradictions – we are focused experts in hemodynamics, airway management, and resuscitation, and yet we are generalists who care for the whole spectrum of a patient’s medical issues while they are in the perioperative world. We pride ourselves on the careful planning required to make every day in the operating room as boring as possible, and yet we are trained to guide catastrophic events to the best possible conclusions when plans fall apart. We base our practice on data, trials and mechanisms of action, but in the moment, anesthesia can be a very intuitive practice. I chose anesthesiology because I relish in these contradictory mindsets, and I take pride in quietly helping patients through some of the most difficult days of their lives.
Advice for graduating residents?
The perioperative arena, especially at a big center like Duke, has so many moving parts that you can be lulled into a sense of complacency and trust that all of the pieces will fall into place and the outcomes will follow, regardless of our actions or attention at any given moment. As anesthesiologists, it is imperative that we interrupt this complacency by considering the differential, even when the answer seems obvious, by listening to the patient’s concerns, even when we’ve done the same case hundreds of times, by stopping to engage in the time-out and by paying attention to the surgeons’ work. In an environment where it is easy to be passive, we need to make the effort to actively do right by our patients and our colleagues.
Q: Why anesthesiology?
A: I was intrigued with the principles and science of producing “sleep for surgery” while simultaneously maintaining the satisfactory integrity of other bodily systems. It also occurred to me that St. Lucia, my country of birth, never had a local anesthesiologist. In an attempt to correct that deficiency, I completed the anesthesia training program at the University of the West Indies in Jamaica and returned to St. Lucia in 1971 where I served as the only anesthesiologist on the island for nearly five years.
Q: How did your experience in St. Lucia help to shape your career?
A: Knowing that there would be no one to collaborate with nor to give me any clinical support, I was filled with initial trepidation; I had to mature very quickly and develop the confidence that was necessary to execute the skills to run that service in our hospital. It also provided me with the humility to recognize my limitations in certain subspecialties, which led me to seek additional training at Vanderbilt University in 1975.
Q: What attracted you to the field of pain management?
A: I was fascinated with the administration of epidural anesthesia, and I spent a good deal of time learning and perfecting that skill in the obstetric suites. This newfound experience permitted me to try a variety of nerve blocks at a time when these procedures were seldom used. I was frequently asked to do various interventional pain procedures for patients with intractable chronic pain. I remember doing a celiac plexus block (without fluoroscopy) for a patient with advanced pancreatic cancer and observing their remarkable pain relief. I voiced at that time that it appeared to be futile to repeat the same surgery for back pain on a patient multiple times. Leadership agreed, and that is how the Vanderbilt Pain Management Center was born—the first pain center in the state of Tennessee—with me as its medical director.
Q: Key lessons from your leadership roles?
A: In the process of establishing a multidisciplinary pain control center at Vanderbilt University and also establishing pain centers in diverse parts of the world as president of the WSPC, while dealing with multinational and multicultural personalities with diverse habits and egos, the following lessons stand out: the need for thorough planning, meticulous organization, patience, humility, and the need to learn to “listen more than you speak.”
Q: Key qualities of a good mentor?
A: In my humble opinion, the following qualities are critical: 1) patience, 2) disciplined tolerance, 3) meticulous planning, 4) trust and understanding that people have different personalities and diverse interests, 5) meaningful communication, 6) compassion, fairness and integrity, and 7) the ability to motivate especially the ‘not-so-gifted’ mentees and to recognize when “one is not having a good day.”

Q: At what point in your career did mentorship most influence your path?
A: The late Dr. Bradley E. Smith, professor and chairman of the Department of Anesthesiology at Vanderbilt, was by far the most important mentor in my anesthetic career. He admitted me into the anesthesiology residency program in 1975 at a time when people who looked like me were seldom seen in white coats. In fact, I was the first Black anesthesia resident and the second Black resident in the Vanderbilt Medical Center. I was grateful to observe that Brad’s bold moves have helped to open the door for other department chairs to diversify their residency programs. He was also very supportive of my bold plans to establish the first pain center in Tennessee.
Q: You have published extensively on the anesthetic management of many complex diseases. What is your advice for early career physician-scientists looking to navigate the research environment?
Founding member American Academy of Pain Medicine; American College of Pain Medicine; American Board of Pain Medicine; Tennessee Pain Society
President World Society of Pain Clinicians (WSPC); helped develop pain clinics in Africa, Latin America, the Caribbean, the Far East, and Eastern Europe
Founding medical director Vanderbilt Pain Management Center
Chief Pain Medicine Division Duke Anesthesiology
Earned the Companion of the Most Distinguished Order of St. Michael and St. George (CMG) for his service and accomplishments in the field of pain medicine

Received the St. Lucia Cross for his contributions in pain medicine
Awarded a Knighthood (Knight Commander of St. Lucia) on the recommendation of the Prime Minister and government of St. Lucia, with the approval of the late Queen Elizabeth II
Completed the clinical trial of Bonipar and the product development of Fidapin—two topical analgesics

A: My advice is to develop and aggressively practice intellectual curiosity whenever possible and to learn to collaborate with other colleagues, within and outside of one’s own department. And if possible, this collaboration could extend to other institutions and when practical, to other countries. It is also important to recognize that procrastination is never your friend.
Q: You are credited with developing a protocol for the anesthetic management of systemic mastocytosis. How did this discovery impact you as an anesthesiologist and researcher?
A: My early exposure to this condition heightened my sensitivities in preoperative evaluation and also in paying close attention to patients’ past history of anesthetic complications. That sensitivity allowed me to identify those cases preoperatively rather than intraoperatively, and also allowed me to develop alternative methods for the induction and maintenance of anesthesia for patients with systemic mastocytosis and related disorders. Systemic mastocytosis results in the massive release of histamine when various intravenous anesthetics, muscle relaxants, sedatives, and other drugs are administered in those patients during anesthesia. The net result of those injections is a significant development of tachycardia and severe hypotension followed by cardiovascular collapse, which if not treated promptly, could usually result in death. The best way to treat systemic mastocytosis is to avoid its development. This can be best done by avoiding most intravenous agents and adopting the good old-fashioned inhalational halogenated anesthetic
agents for induction and maintenance of general anesthesia. Preoperatively, meticulous skin tests can identify those patients who might develop severe complications during anesthesia.
Q: What publication are you most proud of?

A: My publication on the anesthetic management of systemic mastocytosis is very dear to me. Prior to my publication, this condition was frequently associated with perioperative death. It has been very rewarding to learn that many anesthesiologists have followed the clinical recommendations proposed in my paper. I still receive phone calls from physicians all over the world requesting assistance with some intraoperative difficulty in the anesthetic management of patients with that condition, and it is gratifying to know that my publication was of assistance to those patients.
Q: What are some critical steps in advancing science in general?


A: I think some of the critical steps include data collection and intermittent review of that data, intellectual curiosity to always ask questions (no matter how ridiculous they might at first appear to be) and attempting to seek answers or solutions to the problems, meticulous observation of anomalies or unusual phenomena, and utilization of sophisticated or even unusual methods to attempt to connect basic science with clinical practice.
Q: Since retiring from clinical practice, you’ve been actively involved in research and clinical trials of topical

analgesics for the treatment of musculoskeletal pain syndromes. What is your advice for a successful clinical trial?

A: Prerequisites for a good clinical trial include preparation of a sound protocol with good clinical methods, a reliable and competent statistician, and a good team to help execute that clinical trial. Since most physician anesthesiologists taking on clinical trials also have clinical responsibilities, it is imperative to have an individual or team to assist in communications with the IRB for getting approval of the clinical trial and for interacting with the FDA in facilitating an IND, if necessary. One should also clearly determine the cost and funding for the clinical trial.
Q: How did your time in academia and private practice aid in your product development?
A: My academic background and the business and medical political experiences that I gained in private practice prepared me to successfully approach this new challenge with confidence and positivity. My interest in product development evolved after I retired; I spent winters in my island home of St. Lucia, and it was during one of my trips there that I became intrigued by the use of local coconut oil and related oils for treating a variety of ailments, including chronic pain syndromes. Intense evaluation and research of those essential oils precipitated my successful clinical trial and subsequent development of the topical analgesic, Fidapin. Earlier this year, I completed a clinical trial at Duke Anesthesiology on a second generation of topical analgesics, called Bonipar.
Q: What is your viewpoint on product development/ partnering with industry?
A: Since the issuance of my product patents from the US Patent and Trademark Office, I have been inundated with requests for partnership from various venture capitalists. I have steadfastly avoided any such relationships because although initially the financial assistance would be wonderful, my best instincts are to maintain my independence. However, I plan to work with suitable pharmaceutical companies to assist me in the development and launch of Bonipar.
Q: What are the critical steps to be successful in the realm of clinical research?
A: In my opinion, the steps include a critical assessment of current clinical methods and the intellectual curiosity to understand the fabric of those methods and also to try to improve on those methods; a desire to correct any unfavorable outcomes and if necessary, to try to establish protocols to prevent them; to try to link various clinical methods with the basic sciences and hopefully evolve new methods; and to be open to new ideas and criticisms from other sources.
Q: How have you been able to sustain such a productive career spanning decades?
A: I have been blessed with good health, a reasonably good memory and the capacity to require very little sleep; I believe that combination contributed a great deal to the success in my career. Nevertheless, I would give credit to my late mother, my late wife, and my current wife, whose nurturing, love and care created the environment and the sustenance that made any modest accomplishments of mine possible. My family has provided me the strength, the stability, the endurance, and the ambience to be able to think clearly and to work hard. I am eternally grateful to all of them and of course, to the Almighty God who made it all possible.
Q: What is your philosophy on work-life balance?
A: My late mother used to say to me, “All work and no play makes Jack a dull boy.” Most of the time I have listened to my dear mother. Through much of my life, I’ve played tennis, and now, I golf multiple times a week. I believe that regimen of activity helped not only to keep me physically fit, but it also helped clear my mind of any potential distractions which might otherwise interfere with my daily routines. Thus, I think it is critical to have some outlet, preferably physical, to serve to optimize the work-life balance that is necessary to have great success in one’s endeavors.
Q: What is your best advice to those looking to enter the anesthesiology specialty?
A: With the passage of time and the physical rigors of this specialty, one can opt to focus on a subspecialty and get tremendous satisfaction in the process. Although the administration of general anesthesia provides the cornerstone training for the management of patients undergoing surgery, that process exposes you to the various horizons that may fulfill your innate passion and ambition. Those with a basic interest in pharmacology, cardiorespiratory physiology, and the central and peripheral nervous system, can easily fall in love with the specialty and appreciate the wise words, “Eternal vigilance is the price of safety.”
Q: Last year, the key word in “Alumni Notes” was bravery. What would you say is the key word of your journey?
A: My suggestion for 2023 is CURIOSITY. BP
Joseph P. Mathew, MD, MHSc, MBA
Jerry Reves, MD, Professor of Cardiac Anesthesiology

CHIEF: Stephen M. Klein, MD
Ambulatory Anesthesiology
Emily Chen, MD
Alex Cravanas, MD, MBA
Akayla Gillians, MD
Michael Kent, MD
Steve Melton, MD
Karen Nielsen, MD
Juhnnel Vera Santiago, MD
Christopher Young, MD, FCCM
CHIEF: Mihai V. Podgoreanu, MD, FASE
Cardiothoracic Anesthesiology
Brandi Bottiger, MD
Anne Cherry, MD
Sarah Cotter, MD
Michael Cutrone, DO
Kamrouz Ghadimi, MD, MHS
Loreta Grecu, MD
Nazish Hashmi, MBBS
Rebecca Klinger, MD, MS
Sundar Krishnan, MBBS
Jerrold Levy, MD, FAHA, FCCM
Yasmin Maisonave, MD
Negmeldeen Mamoun, MD, PhD
CHAIR’S COUNCIL: (pictured left to right)

Padma Gulur, MD
Gavin Martin, MB ChB, FRCA, MMCi
Miriam M. Treggiari, MD, PhD, MPH
Evan Kharasch, MD, PhD
Atilio Barbeito, MD, MPH
John Borrelli, MBA
Dan Cantrell
Jennifer Dominguez, MD, MHS
Adam Flowe, CRNA
Jeffrey C. Gadsden, MD, FRCP(C), FANZCA
Nicole Guinn, MD, MBA
Padma Gulur, MD
Ashraf S. Habib, MBBCh, MSc, MHSc, FRCA
Edmund H. Jooste, MB ChB
Evan Kharasch, MD, PhD
Stephen M. Klein, MD
Joseph P. Mathew, MD, MHSc, MBA
Madhav Swaminathan, MD, MMCi, FASE
John Borrelli, MBA
Annemarie Thompson, MD
Luiz Maracaja, MD
Joseph Mathew, MD, MHSc, MBA
Sharon McCartney, MD, FASE

Sachin Mehta, MD
Alina Nicoara, MD, FASE
Angela Pollak, MD
Madhav Swaminathan, MD, MMCi, FASE
Annemarie Thompson, MD
Ian Welsby, MBBS, FRCA
Meredith Whitacre, MD
Vijay Krishnamoorthy, MD, MPH, PhD
Melinda F. Macalino
Gavin Martin, MB ChB, FRCA, MMCi
Joseph P. Mathew, MD, MHSc, MBA
Timothy E. Miller, MB ChB, FRCA
Mihai V. Podgoreanu, MD, FASE
Dana Rawls
Nicole Scouras, MD, MBA
Madhav Swaminathan, MD, MMCi, FASE

Annemarie Thompson, MD
Miriam M. Treggiari, MD, PhD, MPH
Kevin Vorenkamp, MD, FASA
Community
Lu Adams, MD
Lindsey Bewley, DO
Ryan Bialas, MD
CHIEF: Nicole Scouras, MD, MBA
Stephanie Cooper, MD
Benjamin Dunne, MD
Matthew Glass, MD
Elsje Harker, MD
Erica Heniser, MD
Daniel Kovacs, MD
Jonathan Mathew, MD
Elizabeth Nichols, MD
Shannon Page, MD
Gary Pellom, MD
Lisette Ramos, MD
Benjamin Redmon, MD
Richard Runkle III, MD
Siddharth Sata, DO
Zaneta Strouch, MD, MPH
Leonard Talbot, MD
Neel Thomas, MD

Danai Udomtecha, MD
Andrew Wong, MD
Catherine Kuhn, MD
Rachel Lance, PhD
Michael Manning, MD, PhD
Richard Moon, MD, CM, MSc, FRCP(C), FACP, FCCP
Eugene Moretti, MD, MHSc
Hagir Suliman, DVM, PhD
Ankeet Udani, MD, MSEd
Kerri Wahl, MD, FRCP(C)
Thomas Buchheit, MD
Cain Dimon, MD
Padma Gulur, MD
Dimitri Putilin, PhD
Scott Runyon, MD
Jean Elie Tabbal, MD
Daniela Vivaldi, DDS
Peter Yi, MD, MSEd
CHIEF: Ashraf S. Habib, MBBCh, MSc, MHSc, FRCA
Women’s Anesthesiology
Terrence Allen, MBBS
Melissa Bauer, DO
Matthew Buck, MD
Jennifer Dominguez, MD, MHS
CHIEF: Vijay Krishnamoorthy, MD, MPH, PhD
Critical Care Medicine
Omar Al-Qudsi, MD
Sandy An, MD, PhD
Adjoa Boateng, MD
Yuriy Bronshteyn, MD
Kathleen Claus, MD
Blair Costin, MD, PhD
Desiree Coutinho, MD
Michael Devinney, MD, PhD
Taylor Herbert, MD, PhD
Ehimemen Iboaya, MD
RJ Krom, MD, PhD
Nitin Mehdiratta, MD
Rachael Mintz-Cole, MD, PhD
Jamie Privratsky, MD, PhD
Galen Royce-Nagel, MD
Mara Serbanescu, MD
Arturo Suarez, MD
Miriam Treggiari, MD, PhD, MPH
Paul Wischmeyer, MD, EDIC
CHIEF: Nicole Guinn, MD, MBA
Neuroanesthesiology, Otolaryngology & Offsite
Anesthesiology
Leah Acker, MD, PhD
Miles Berger, MD, PhD
Amanda Faulkner, MD
Dhanesh K. Gupta, MD, MBA
Jennifer Hauck, MD
Michael “Luke” James, MD, FAHA, FNCS
Andrew Peery, MD, MPH

Vijay Ramaiah, MBBS
Bryant Stolp, MD, PhD
CHIEF: Edmund H. Jooste, MB ChB
Pediatric Anesthesiology
Warwick Ames, MBBS
Jon Andrews, MD
Guy Dear, MA, MB, BChir, FRCA, FUHM
Natalia Diaz-Rodriguez, MD
John Eck, MD
Lisa Einhorn, MD
Hercilia Homi, MD, PhD
Martha Kenney, MD
Elizabeth Malinzak, MD
Matthew McDaniel, MD
John McManigle, MD
Allison Ross, MD
Brad Taicher, DO, MBA
Andrea Udani, MD
Jean He, MD
Jennifer Mehdiratta, MD, MPH
Abigail Melnick, MD
Marie-Louise Meng, MD
Adeyemi Olufolabi, MBBS, DCH, FRCA
Cameron Taylor, MD
Mary Yurashevich, MD, MPH

DIRECTOR: Luis Ulloa, PhD, MS
Center for Perioperative Organ Protection
Madan Kwatra, PhD
Huaxin Sheng, MD
Wei Yang, PhD

CHIEF: Jeffrey C. Gadsden, MD, FRCP(C), FANZCA
Orthopaedics, Plastics & Regional Anesthesiology
W. Michael Bullock, MD, PhD
Joshua Dooley, MD
Amanda Kumar, MD
David MacLeod, MBBS, FRCA, Dip IMC
Erin Manning, MD, PhD
Gavin Martin, MB ChB, FRCA, MMCi
CHIEF: Atilio Barbeito, MD, MPH
Veterans Affairs
Anesthesiology Service
Sophia Dunworth, MD
Juliann Hobbs, MD, MPH
Hung-Lun (John) Hsia, MD
Eric JohnBull, MD, MPH
DIRECTOR: Ru-Rong Ji, PhD
Center for Translational Pain Medicine
Satya Achanta, DVM, PhD
Andrey Bortsov, MD, PhD
Christopher Donnelly, DDS, PhD
Sven-Eric Jordt, PhD
Francis Keefe, PhD
CHIEF: Timothy E. Miller, MB ChB, FRCA
Chakib Ayoub, MD, MBA

Jeanna Blitz, MD, FASA
Derek Covington, MD

Bruce Derrick, MD
Jonathan Dunkman, MD
Sarada Eleswarpu, MD
Arun Ganesh, MD
Heath Gasier, PhD
Evan Kharasch, MD, PhD
Hector Martinez-Wilson, MD, PhD

Brian Ohlendorf, MD
Neil Ray, MD, MBA, MMCi
John Lemm, MD
David Lindsay, MD
Amy Manchester, MD
Grace McCarthy, MD
Harika Nagavelli, MD
Srinivas Pyati, MD, MBBS
Karthik Raghunathan, MBBS, MPH
CHIEF: Kevin Vorenkamp, MD, FASA


Pain Medicine
Aurelio Alonso, DDS, MS, PhD
Muhammad Anwar, MD, MBA
Evander Britt, MD
Lance Roy, MD
Rebecca Schroeder, MD
Timothy Stanley, MD
Thomas Van de Ven, MD, PhD
Katherine Martucci, PhD
Andrea Nackley, PhD
Shad Smith, PhD
Niccolò Terrando, PhD
OCTOBER 14, 2023
























SAN FRANCISCO, CALIFORNIA

10.23.22
After a pause since the pandemic, Duke Anesthesiology marked its 32nd Annual American Society of Anesthesiologists (ASA) Alumni Event by once again hosting an in-person reception on October 23, 2022 at The Chicory in New Orleans for a night of celebration and creole cuisine.






The anticipated highlight of the evening was the reveal of the 2023 DREAM Innovation Grant (DIG) recipient, Dr. Leah Acker (see page 44), for her project, “A Pilot Feasibility Study of Day-of-Surgery: PeriOperative Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) Effects on Neurocognitive and Neuroinflammatory Trends (POTENT+).”
The evening’s guests also celebrated a successful ASA meeting; 27 faculty and trainees participated in the conference, which included 70 lectures, workshops, panel discussions, presentations, and more.


On September 10, 2022 departmental faculty, trainees, alumni, and Duke leadership gathered at the Cotton Room in Durham for the Duke Anesthesiology 50th Anniversary Gala; an evening that honored Duke Anesthesiology’s legacy of excellence and celebrated the department’s health care professionals and their 50 years of exceptional patient care, innovative research, education, and more.


KEYNOTE:
“Lessons Learned from Coach K“
Everything we do is Important | Be Relentless in Your Preparation
Next Play | Have Empathy | Don't Take Special for Granted
JAY BILAS ‘86, JD’92 | Keynote Speaker Emmy-nominated college basketball analyst, ESPN Duke Men’s Basketball Duke University School of Law“We are not here to do things, but to be things. And by the fruit of our being, change the world.
Compassion, courage, grace, and kindness require being. We don’t do compassion or do courage. We are compassionate and we are courageous.”
- DR. JOSEPH MATHEW, CHAIRMAN (quoting Susanna Mathew)



VISION:
To be the leader in advancing perioperative medicine and pain management.
MISSION:
Extraordinary care through a unique culture of innovation, education, research, and professional growth.