Rebecca Leonard
Visit to download the full and correct content document: https://ebookmass.com/product/dysphagia-assessment-and-treatment-planning-a-tea m-approach-fifth-edition-rebecca-leonard/

More products digital (pdf, epub, mobi) instant download maybe you interests ...

Assessment and Treatment Methods for Manual Therapists: The Most Effective and Efficient Treatment Every Time [Team-IRA] [True PDF] Jeffrey Burch
https://ebookmass.com/product/assessment-and-treatment-methodsfor-manual-therapists-the-most-effective-and-efficient-treatmentevery-time-team-ira-true-pdf-jeffrey-burch/

Landscape Architecture, Fifth Edition : A Manual of Environmental Planning
https://ebookmass.com/product/landscape-architecture-fifthedition-a-manual-of-environmental-planning/

Braunwald's Heart Disease Review and Assessment 12th Edition Leonard S. Lilly
https://ebookmass.com/product/braunwalds-heart-disease-reviewand-assessment-12th-edition-leonard-s-lilly/

Functional
Somatic Symptoms in Children and Adolescents: A Stress-System Approach to Assessment and Treatment 1st ed. Edition Kasia Kozlowska
https://ebookmass.com/product/functional-somatic-symptoms-inchildren-and-adolescents-a-stress-system-approach-to-assessmentand-treatment-1st-ed-edition-kasia-kozlowska/

Adult Deliberate Firesetting : Theory, Assessment, and Treatment 1st Edition Theresa
A. Gannon
https://ebookmass.com/product/adult-deliberate-firesettingtheory-assessment-and-treatment-1st-edition-theresa-a-gannon/

Landscape Architecture, Fifth Edition: A Manual of Environmental Planning and Design 5th Edition, (Ebook PDF)
https://ebookmass.com/product/landscape-architecture-fifthedition-a-manual-of-environmental-planning-and-design-5thedition-ebook-pdf/

Veterinary Dentistry: A Team Approach 3rd Edition –Ebook PDF Version
https://ebookmass.com/product/veterinary-dentistry-a-teamapproach-3rd-edition-ebook-pdf-version/

Real estate principles: a value approach Fifth Edition
Archer
https://ebookmass.com/product/real-estate-principles-a-valueapproach-fifth-edition-archer/

Language Disorders: A Functional Approach to Assessment and Intervention
https://ebookmass.com/product/language-disorders-a-functionalapproach-to-assessment-and-intervention/
DYSPHAGIA Assessment
and Treatment Planning
A TEAM APPROACH FIFTH



Rebecca Leonard
Katherine Kendall
DYSPHAGIA
Assessment
and Treatment Planning
A TEAM APPROACH
FIFTH EDITION
DYSPHAGIA
Assessment and Treatment Planning
A TEAM APPROACH
FIFTH EDITION
Rebecca Leonard, PhD
Katherine A. Kendall, MD
9177 Aero Drive, Suite B
San Diego, CA 92123
email: information@pluralpublishing.com
website: https://www.pluralpublishing.com
Copyright © 2025 by Plural Publishing, Inc.
Typeset in 10.5/13 Palatino by Flanagan’s Publishing Services, Inc.
Printed in China by Regent Publishing Services Ltd.
All rights, including that of translation, reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, recording, or otherwise, including photocopying, recording, taping, web distribution, or information storage and retrieval systems without the prior written consent of the publisher.
For permission to use material from this text, contact us by Telephone: (866) 758-7251
Fax: (888) 758-7255
email: permissions@pluralpublishing.com
Every attempt has been made to contact the copyright holders for material originally printed in another source. If any have been inadvertently overlooked, the publisher will gladly make the necessary arrangements at the first opportunity.
Library of Congress Cataloging-in-Publication Data:
Names: Leonard, Rebecca, editor. | Kendall, Katherine (Staff physician) editor.
Title: Dysphagia assessment and treatment planning : a team approach / [edited by] Rebecca Leonard, Katherine Kendall.
Description: Fifth edition. | San Diego, CA : Plural Publishing, Inc., [2025] | Includes bibliographical references and index.
Identifiers: LCCN 2023022305 (print) | LCCN 2023022306 (ebook) | ISBN 9781635504736 (hardcover) | ISBN 1635504732 (hardcover) | ISBN 9781635504736 (ebook)
Subjects: MESH: Deglutition Disorders--diagnosis | Deglutition Disorders--therapy | Patient Care Planning | Patient Care Team
Classification: LCC RC815.2 (print) | LCC RC815.2 (ebook) | NLM WI 258 | DDC 616.3/23--dc23/eng/20230718
LC record available at https://lccn.loc.gov/2023022305
LC ebook record available at https://lccn.loc.gov/2023022306
NOTICE TO THE USER
Care has been taken to confirm the accuracy of the indications, procedures, drug dosages, and diagnosis and remediation protocols presented in this book and to ensure that they conform to the practices of the general medical and health services communities. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. The diagnostic and remediation protocols and the medications described do not necessarily have specific approval by the Food and Drug administration for use in the disorders and/or diseases and dosages for which they are recommended. Application of this information in a particular situation remains the professional responsibility of the practitioner. Because standards of practice and usage change, it is the responsibility of the practitioner to keep abreast of revised recommendations, dosages, and procedures.
Introduction
The initial publication of Dysphagia Assessment and Treatment Planning: A Team Approach took place over 25 years ago! At that time, the text illustrated how the development of a “Dysphagia Team” optimized assessment and treatment for our patients with dysphagia. It also introduced the concept of objective measures made from videofluoroscopy to improve accuracy, detect subtle swallowing abnormalities, and evaluate the impact of interventions. That original text contained the collective clinical experience of a number of phenomenal contributors on our Dysphagia Team. Since that time, four editions of the text have been published. The number of contributors to the text has grown, along with the vast amount of clinical experience contained within it. What has not changed are the foundational concepts of the dysphagia team and the use of objective measures.
This current edition of Dysphagia Assessment and Treatment Planning: A Team Approach covers topics of interest to the graduate student as well as the practicing clinician. We hope that it will serve as a text for students of swallowing function and as a reference for experienced clinicians by including information on fundamental swallowing physiology through advanced medical dysphagia topics. We would like to share with our readers the impressive collective clinical and research experience of the authors who are all
well-established academic speech-language pathologists and physicians with expertise in dysphagia. We also hope to develop in readers an appreciation for the incredible power of objective measurement tools available for dysphagia assessment. By embracing a standardized, objective method of swallowing assessment as presented in this text, even experienced clinicians will improve their abilities to define both subtle and obvious swallowing abnormalities while enhancing communication between clinicians and objectively monitoring patient improvements.
This book is organized so that concepts central to the understanding of dysphagia assessment are presented first, followed by chapters covering the development and implementation of treatment recommendations. Information on specialized dysphagia populations is presented in the latter part of the book. At the end of each chapter, a series of questions allow the reader to evaluate their understanding of the chapter material. In addition, there are numerous clinical video examples available on the companion website to illustrate the concepts presented in the text. The companion workbook contains further opportunities for readers to test their knowledge of subjects presented in the book.
To enable readers to learn and practice how to make objective measures of swallowing function, this book includes
DYSPHAGIA ASSESSMENT AND TREATMENT PLANNING: A TEAM APPROACH
access to Swallowtail™, a software application designed to increase the ease of making measures from dynamic fluoroscopic swallow studies, comparing those measures to normative data and creating a database for patient tracking and documentation purposes. Readers will discover how little extra time is required to make measures using this technology. We encourage all those who are involved in the care of dysphagic patients to adapt the use of objective measures as part of fluoroscopic assessment. We hope to provide the tools for them to do so and the knowledge required to advocate for themselves and their patients when negotiating the purchase of such technology, regardless of their clinical setting.
There have been numerous advances in our understanding of dysphagia over the past 25 years, through the development of new technologies in both assessment and treatment. Every chapter of this latest edition has been updated to reflect the most current information on the topic presented. In addition, a new chapter on the role of telehealth in the evaluation and treatment of dysphagia has been added. Further, as editors and authors, we have done our best to respond to comments and suggestions from our readers for improvements and additional information in each chapter.
The first chapters cover swallowing anatomy and physiology along with the history and physical examination of the dysphagic patient. The concept of the upper aerodigestive tract as a series of chambers and valves that act together to propel the bolus from the lips to the stomach is introduced here and is reinforced throughout the book. Two cranial nerve charts focusing on
normal function and the impairments created by cranial nerve deficits are included for easy reference.
The subsequent chapters cover clinical swallowing evaluation, the use of endoscopy in swallowing assessment and therapy, and the radiographic evaluation of the pharynx and esophagus. These updated chapters form the fundamental knowledge required of the clinician to function well in a medical setting.
Three chapters are devoted to the dynamic swallow study analysis and interpretation with a detailed explanation of making objective measures. These chapters provide not only knowledge about dynamic swallow study analysis but also a wealth of clinical information regarding methods of optimal swallow study performance. An additional chapter devoted to other technologies in dysphagia assessment provides an updated discussion of the latest technological advances.
The treatment section has been divided into two chapters: One addresses the medical and surgical treatment of dysphagia, and the other addresses the application of exercises, positioning, other external therapeutic maneuvers, and interventions to the treatment of dysphagia. Within the chapter, individuals with particular expertise in the latest innovations for dysphagia treatment have contributed information on the role, indications, outcomes, and limitations of new technologies.
Subsequent chapters focus on two ancillary but critically important topics: airway and nutritional concerns. Both subjects impact the management of dysphagia and must be considered in every patient with dysphagia. These chapters provide updated basic, yet
indispensable, information for the dysphagia clinician and underscore the value of a team approach to dysphagia management.
The later chapters focus on special patient populations, including pediatrics, esophageal dysphagia, neurogenic dysphagia, head and neck cancer, spinal abnormalities, and the impact of laryngopharyngeal reflux on swallowing. These chapters present information of an advanced nature and should serve as a reference for clinicians throughout their career.
Lastly, throughout this book, we focus attention on the advantages of working together as a team in the management of patients with dysphagia.
Each person on the team brings their individual insights, expertise, training, and experience to the assessment and treatment recommendations for every patient. Team makeup and participation should be customized to the individual institution. Our team has included speech pathologists, otolaryngologists, nurses, nutritionists, radiologists, gastroenterologists, neurologists, and pediatricians. Fellow and resident trainees have also attended team meetings. Whatever the makeup of the team has been, the experience has been immensely instructive and gratifying. We would like to thank the contributors to this book whose work creates the synergy that illustrates A Team Approach.
Multimedia List
Chapter 1
Video 1–1. Straw Drinking
Chapter 4
Video 4–1. VPPORT
Video 4–2. OROPHX
Video 4–3. HYPOPHX
Video 4–4. FEESPT1
Video 4–5. FEESPT2
Chapter 6
Video 6–1. ZDtwoviews
Video 6–2. AP Aspiration
Chapter 7
Video 7–1. NrmPhPeristalsis
Video 7–2. AbsInc-PhPeristalsis
Video 7–3. ExcPhPeristalsis
Video 7–4. AbsIncEpigInv
Video 7–5. BolusRedirect
Video 7–6. ImpairedPharyngealShortening
Video 7–7. ASPBefore
Video 7–8. ASPDuring
Video 7–9. ASPAfter
Video 7–10. DiffuseEsophSpasm
Video 7–11. Stasis
Chapter 8
Video 8–1. BTSGTiming
Video 8–2. YngEldNormalSwallow
Video 8–3. BP1AEcl
Video 8–4. Hmax
Video 8–5. HL
Video 8–6. PCR
Video 8–7. PESmax
Video 8–8. BCR
Video 8–9. BulletPharynx
Video 8–10. Pharyngeal Shortening Measure
Chapter 9
Video 9–1. GOOSE
Chapter 10
Video 10–1. Strategy 1
Video 10–2. Strategy 2A
Video 10–3. Strategy 2B
Video 10–4. Strategy 3
Video 10–5. Strategy 4
Video 10–6. Strategy 5
Video 10–7. Strategy 6
Chapter 19
Video 19–1. CSpineBolusConsistManipulation
Video 19–2. CSpineBolusVolManipulation
Video 19–3. CSpineBolusRedirect
Acknowledgments
The authors extend a sincere “thank you” to the members of the UC Davis Dysphagia Team, past and present, as well as to our colleagues at other institutions, for their generosity and expertise in the preparation of this text. Many of our authors have contributed to previous editions; others, including James Clark, MD, Assistant Professor at Johns Hopkins School of Medicine, and Deirdre Larsen, PhD, Assistant Professor at Eastern Carolina University, are first-time contributors. Our “team” experience at UCD has convinced us that a highly interactive, interdisciplinary group of individuals with unique
backgrounds and skill sets represents an excellent approach to dysphagia management, as well as a perpetual source of continuing education for individual members. We are hopeful that the text will inspire other professionals to develop similar resources in their own settings. We also thank those patients and volunteer subjects who have played a role in materials used in the book, as well as in our collection of normative and other data. These individuals have graciously shared their time and experiences with us, and we gratefully acknowledge their contributions.
Contributors
Jacqui E. Allen, MD, FRACS, ORL-HNS
Laryngologist
Department of Surgery
University of Auckland
Takapuna, Auckland
New Zealand
Chapters 5, 16
Peter C. Belafsky, MD, MPH, PhD
Professor and Director, Center for Voice and Swallowing
Department of Otolaryngology
University of California, Davis
Sacramento, California
Chapters 15, 18
Ivy Cheng, PhD
Postdoctoral Research Associate
Division of Diabetes, Endocrinology and Gastroenterology
University of Manchester
Manchester, United Kingdom
Chapter 10 Addendum
James H. Clark, MD
Assistant Professor
Department of Otolaryngology-Head and Neck Surgery
John Hopkins University, School of Medicine
Baltimore, Maryland
Chapters 15, 18
James A. Curtis, PhD, CCC-SLP, BCS-S
Assistant Professor of SpeechLanguage Pathology
Department of Otolaryngology-Head & Neck Surgery
Weill Cornell Medical College
New York, New York
Chapter 10 Addendum
Susan J. Goodrich, MS
Ret. Senior Speech-Language Pathologist
Voice-Speech-Swallowing Center Department of Otolaryngology
University of California, Davis
Sacramento, California
Chapter 3
Shaheen Hamdy, MB ChB, PhD, FRCP
Professor and Honorary Consultant Gastroenterologist/Physician
Department of GI Sciences, School of Medical Sciences
University of Manchester
Manchester, United Kingdom
Chapter 10 Addendum
Maggie-Lee Huckabee, PhD
Director and Distinguished Professor
The Rose Centre for Stroke Recovery and Research
School of Psychology Speech and Hearing, College of Science
University of Canterbury Christchurch, New Zealand
Chapter 10 Addendum
Katherine A. Kendall, MD, FACS Professor
Division of Otolaryngology
DYSPHAGIA ASSESSMENT AND TREATMENT PLANNING: A TEAM APPROACH
University of Utah
Salt Lake City, Utah
Chapters 1, 2, 11, 12, 13, 17
Maggie A. Kuhn, MD, MAS
Associate Professor
Department of Otolaryngology-Head and Neck Surgery
University of California, Davis
Sacramento, California
Chapter 9
Deirdre Larsen, PhD, CCC-SLP
Assistant Professor
Department of Communication Sciences and Disorders
East Carolina University
Greenville, North Carolina
Chapter 10
Rebecca Leonard, PhD
Professor, Emeritus
Department of Otolaryngology-Head and Neck Surgery
University of California, Davis
Sacramento, California
Chapters 4, 6, 7, 8, 10
Beverly Lorens, MS, RD
Senior Clinical Dietitian, retired
Food and Nutrition Services
University of California Davis Medical Center
Sacramento, California
Academy of Nutrition and Dietics
Chapter 13
Georgia A. Malandraki, PhD, CCC-SLP, BCS-S, ASHA Fellow
Professor
Department of Speech, Language, and Hearing Sciences
Purdue University
West Lafayette, Indiana
Bonus Online Chapter
Susan McKenzie, MS
Ret. Senior Speech-Language Pathologist
Voice-Speech-Swallowing Center
Department of Otolaryngology
University of California, Davis
Sacramento, California
Chapters 6, 7
Anna Miles, PhD
Senior Lecturer, Speech Science
The University of Auckland
Auckland, New Zealand
Chapter 14
Madeline Mills, BSLP(Hons)
The Rose Centre for Stroke Recovery and Research
School of Psychology, Speech and Hearing, College of Science
University of Canterbury
Christchurch, New Zealand
Chapter 10 Addendum
Derrick R. Randall, MD, MSc, FRCSC
Clinical Assistant Professor and Residency Program Director
Section of Otolaryngology-Head and Neck Surgery
University of Calgary
Calgary, Alberta, Canada
Chapter 19
Catherine J. Rees Lintzenich, MD
Associate Professor Otolaryngology
Head and Neck Surgery
Center for Voice and Swallowing Disorders
Wake Forest University School of Medicine
Winston-Salem, North Carolina
Chapters 15, 18
2. HISTORY AND PHYSICAL EXAMINATION IN DYSPHAGIA
Ann E. F. Sievers, RN, MA, CORLN
ENT Nurse Expert
Department of Patient Care Services and Otolaryngology
University of California, Davis
Sacramento, California
Chapter 12
Alice I. Walker, MS
Ret. Senior Speech-Language Pathologist
Voice-Speech-Swallowing Center
Department of Otolaryngology
University of California, Davis
Sacramento, California
Chapter 3

1 Anatomy and Physiology of Deglutition
Katherine A. Kendall
Familiarity with the anatomy and physiology of normal deglutition enables a focused approach to the evaluation of patients with disordered swallowing. An understanding of how head and neck structures interact to accomplish swallowing allows the clinician to comprehend how various types of pathology are likely to negatively impact swallowing function. Once specific aspects of swallowing dysfunction are identified, therapy can be tailored to focus on those dysfunctional aspects with the goal of achieving safe and effective swallowing, even in the face of ongoing pathology. This chapter discusses the anatomy and interaction of head and neck structures involved in swallowing and reviews the sequence of events resulting in a successful swallow.
PHYSIOLOGY: SERIES OF CHAMBERS AND VALVES
The oral cavity, oropharynx, and esophagus can be thought of as a series of expanding and contracting chambers, divided by muscular sphincters or valves. Propulsion of a bolus through this part of the alimentary tract is the result of forces or positive pressure developed behind the bolus, as well as a vacuum or negative pressure developed in front of the bolus. The positive pressure behind the bolus pushes it forward through the alimentary tract while negative pressure in front of the bolus acts to suck or pull the bolus forward into the next alimentary chamber. The creation of propulsion pressures depends on the sequential contraction and expansion of the chambers of the
upper aerodigestive tract and the competency of the sphincters dividing the chambers. Any disturbance in the functional elements or coordination of this system is likely to cause a less efficient transfer of a bolus from the oral cavity to the stomach, resulting in dysphagia. Swallowing involves coordination of the sequence of activation and inhibition for more than 25 pairs of muscles in the mouth, pharynx, larynx, and esophagus. An understanding of how the structures of the head and neck interact and coordinate to bring about the propulsion pressures required for normal swallowing is vital for the clinician involved in the evaluation and treatment of patients with swallowing complaints.
For simplicity, the act of deglutition is traditionally divided into four parts: the preparatory phase, the oral phase, the pharyngeal phase, and the esophageal phase (Dodds et al., 1990; Miller, 1982).
PREPARATORY PHASE
The preparatory phase of swallowing includes mastication of the bolus, mixing it with saliva, and dividing the food for transport through the pharynx and esophagus. The preparatory phase takes place in the oral cavity, the first chamber in the swallowing system. This oral preparatory phase of swallowing is almost entirely voluntary and can be interrupted at any time.
During bolus preparation, facial muscles play a role in maintaining the bolus on the tongue and between the teeth for chewing. Specifically, the orbicularis oris muscle, the circular muscle of the lips, maintains oral competence
and can be considered the first sphincter of the swallowing system (Figure 1–1). Weakness or incompetence of the orbicularis oris muscle results in difficulty maintaining a bolus inside the oral cavity during bolus preparation with spillage of the bolus from the mouth. Weakness or incompetence of the orbicularis oris muscle will also result in spillage of saliva, or drooling, between meals.
The buccinator muscle of the cheek contracts to keep the bolus from pooling in the pockets formed by the gingival buccal sulci lateral to the mandible. Buccinator muscle fibers run between the lateral aspect of the orbicularis oris muscle and the pterygoid plates of the skull base (see Figure 1–1).
These facial muscles receive neural input from the facial nerve, also known as cranial nerve VII (Figure 1–2). Patients suffering from paralysis of the facial nerve, such as in Bell’s palsy, will experience problems during the preparatory phase of swallowing, characterized by difficulty maintaining a bolus in the oral cavity and lateral pooling of the bolus between the mandible and the cheek on the side of the palsy.
Most of the movement and positioning of the bolus during preparation for swallowing is carried out by the tongue muscles. In addition to four intrinsic muscles, the tongue has four paired extrinsic muscles: the genioglossus, palatoglossus, styloglossus, and hyoglossus muscles (Figure 1–3). Along with the genioglossus muscle, the intrinsic muscles act primarily to alter the shape and tone of the tongue while the other three extrinsic muscles aid in the positioning of the tongue relative to other oral cavity and pha-
Incisivus labii superioris
Zygomatic minor
Levator labii superioris
Levator labii superioris alaeque nasi
Levator anguli oris


Zygomatic major
Risorius
Incisivus labii inferioris
Mentalis











Buccinator
Orbicularis oris
Depressor labii inferioris
ryngeal structures. The genioglossus muscles attach to the interior surface of the mandible and then fan out into the tongue so that contraction of the genioglossus muscles results in movement of the tongue forward in the oral cavity. The styloglossus muscles run inferiorly from the medial aspect of the styloid processes at the skull base to insert into the side and inferior aspects of the lateral tongue. Contraction of these muscles elevates the tongue base. The hyoglossus muscles arise from the hyoid bone and insert into the side and inferior part of the tongue. Contraction








Depressor anguli oris Platysma
Figure 1–1. Facial musculature shown in relationship to the oral cavity. Note the orbicularis oris muscle encircling the mouth and the fibers of the buccinator muscle running anteriorly to insert in the lateral orbicularis oris muscle. Note the attachment of the buccinator muscles to the lateral pterygoid plate of the skull base. From Foundations of Speech and Hearing: Anatomy and Physiology, 2nd ed. (p. 173), by Jeannette D. Hoit, Gary Weismer, and Brad Story, 2022, Plural Publishing. © 2022 by Plural Publishing.
of the hyoglossus muscles results in depression and posterior movement of the tongue (see Figure 1–3).
The palatoglossus muscles originate in the soft palate and insert into the lateral aspects of the posterior tongue, along with the styloglossus muscles (Figure 1–4). Contraction of the palatoglossus muscles elevates the tongue base and approximates it to the soft palate. During the bolus preparatory phase of deglutition, the posterior part of the tongue elevates against the soft palate, which simultaneously is pulled downward against the tongue base.
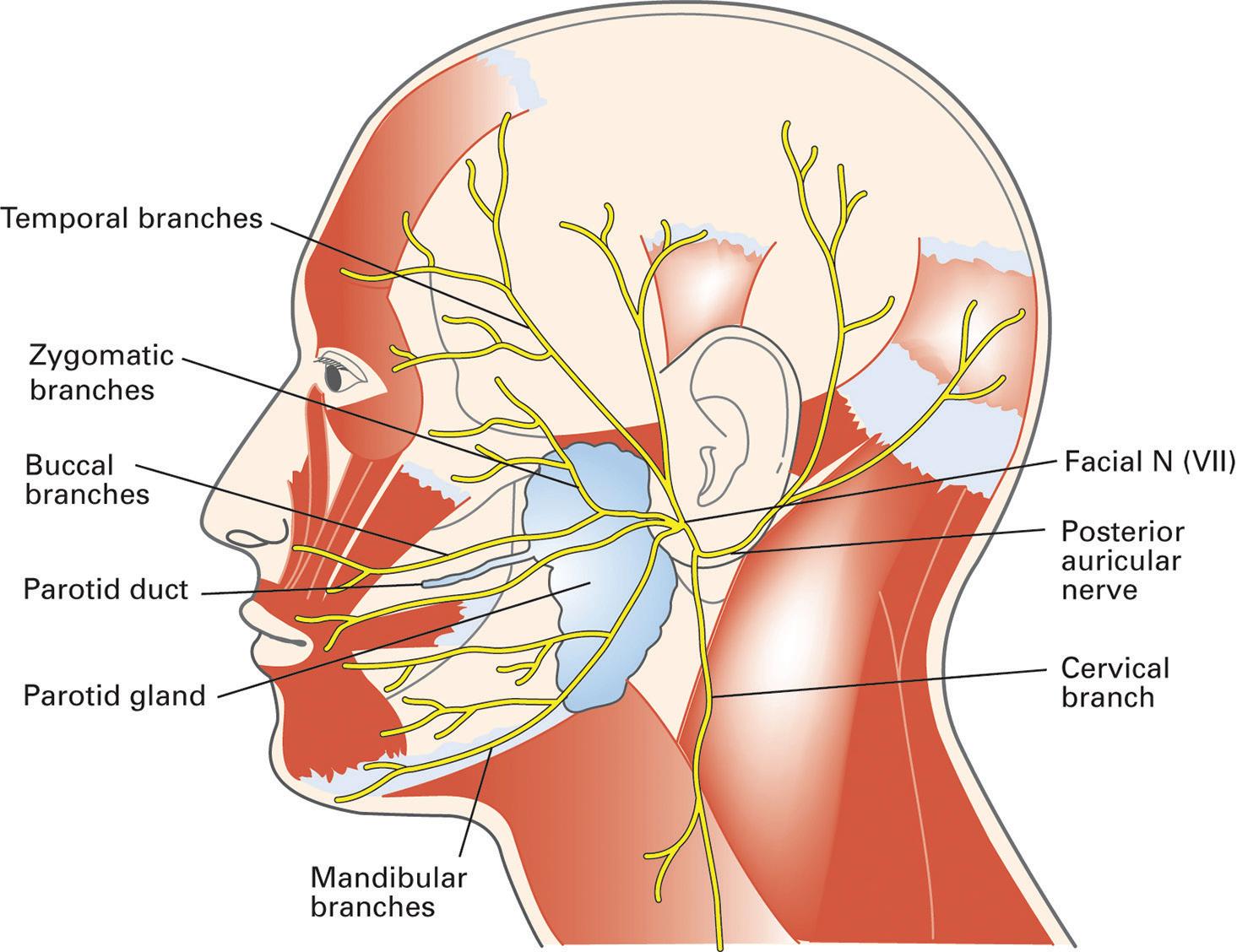

Figure 1–3. Extrinsic musculature of the tongue and course of hypoglossal nerve (XII). Note the tongue muscles: styloglossus, genioglossus, and hyoglossus and their attachments. Note how the fibers of the genioglossus muscle attach to the inner surface of the mandible and the anterior surface of the hyoid bone. Note nerve fibers from cervical nerve rootlets that travel with the hypoglossal nerve and travel to the strap muscles in the neck.

Figure 1–4. Muscles of the soft palate. Note the fibers of the palatoglossus muscle between the palate and the tongue base. Contraction of this muscle approximates the soft palate and the tongue base, effectively closing off the back of the oral cavity from the pharynx during oral bolus preparation and prevents early entrance of the bolus into the pharynx.
This action of the soft palate against the tongue base effectively closes off the back of the oral cavity and prevents the bolus from escaping prematurely into the pharynx. The palate and tongue base constitute the second sphincter in the swallowing system. With the soft palate approximating the tongue base, the nasopharyngeal airway remains open during the oral preparatory phase of swallowing and nasal respiration is uninterrupted. Obstruction of the nose and nasopharynx due to any cause such as a mass, severe septal deviation, enlarged nasopharyngeal adenoid tissue, and so on results in dif-
ficulty with the oral preparatory phase of swallowing due to the requirement for nasal breathing during this phase (Figure 1–5).
Cranial nerve XII, the hypoglossal nerve, carries the motor nerve fibers that innervate both the intrinsic and extrinsic tongue muscles, except for the palatoglossus muscles (see Figure 1–3).
Injury to cranial nerve XII (hypoglossal) can be detected clinically by asking the patient to protrude the tongue. The side of injury will not be able to protrude due to weakness of the musculature on that side and the tip of the tongue will point toward the side of injury.

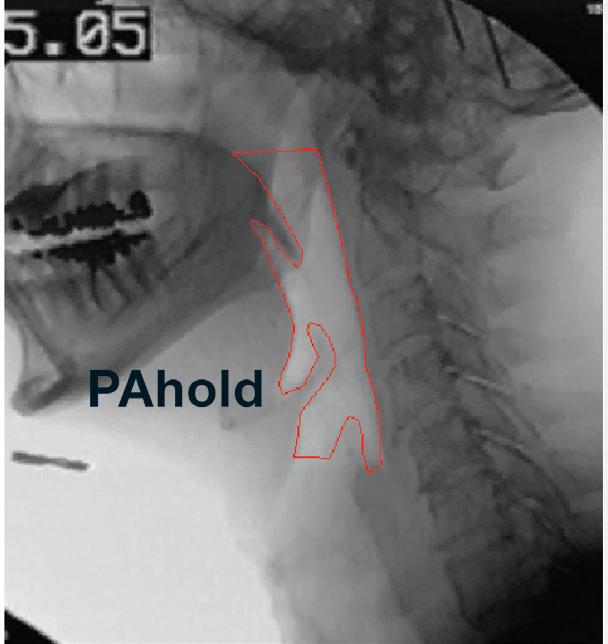
Figure 1–5. Lateral view from videofluoroscopic swallowing study: Preparatory phase. Note bolus in the oral cavity on the superior surface of the tongue. Palate closes against the tongue base to close posterior oral cavity from the oropharynx. Respiration is via nasal cavity as the velopharyngeal valve closes off the oral cavity and opens the posterior nasopharynx.
Tongue weakness results in difficulty with bolus positioning during the preparatory phase of swallowing as well as early spillage of the bolus into the pharynx due to incompetence of the posterior oral cavity sphincter.
A branch of the pharyngeal plexus from the vagus nerve (X) sends motor fibers to innervate the palatoglossus muscles (Figure 1–6). These fibers branch from the vagus soon after the nerve exits the skull base. Injury to these nerve fibers results from pathol-
ogy at the skull base or intracranially. Weakness of the palatoglossus muscle impairs the activity of the posterior oral cavity sphincter and results in early escape of the bolus from the oral cavity into the pharynx before the onset of the pharyngeal phase of swallowing.
A high density of mechanoreceptors within and on the surface of the tongue indicates that the tongue is an important sensory region for determining the size of the bolus. Sensory information from the anterior two-thirds of the

tongue is carried back to central swallowing control centers via the lingual nerve, a branch of the trigeminal nerve or cranial nerve V (Figure 1–7). Sensory information from the tongue is critical to modulation of bolus preparation and in the coordination of subsequent swallowing of the bolus.
Sensory information from the posterior one third of the tongue is carried centrally by the glossopharyngeal nerve, or cranial nerve IX (see Figure 1–6). Stimulation of the sensory portion of the glossopharyngeal nerve in the tongue base elicits the pharyngeal protection reflex known as the gag reflex.
Mastication, or chewing, of the bolus involves the masseter muscles, the temporalis muscles, and the medial and lateral pterygoid muscles to move the mandible relative to the maxilla. This muscle group is known collectively as the muscles of mastication (Figure 1–8).
Motor nerve fibers controlling the contraction of these muscles are carried in branches of the trigeminal nerve (V) (see Figure 1–7). Unilateral weakness of the muscles of mastication results in asymmetry of jaw opening with swing of the mandible toward the normal side. Information regarding the “hardness” of the bolus material is sensed

Figure 1–7. Trigeminal nerve. Note branches that enter the tongue and carry sensory information from the tongue (lingual nerve). Note branches to muscles of mastication.

Figure 1–8. Muscles of mastication. From Foundations of Speech and Hearing: Anatomy and Physiology (p. 167), by Jeannette D. Hoit, Gary Weismer, and Brad Story, 2018, Plural Publishing. © 2018 by Plural Publishing.
via muscle spindles in the muscles of mastication during chewing. This information is relayed to the cerebral central control mechanisms via the trigeminal nerve (V).
Salivation
Successful transfer of a food bolus from the oral cavity into the esophagus requires the mixing of the bolus with saliva. Saliva lubricates and dilutes the bolus to an optimal consistency for swallowing. Saliva contains two major types of protein secretion: an enzyme for digesting starches and mucus for lubricating purposes. Normal salivary secretion ranges from 1.0 to 1.5 liters per day. Saliva also plays an important role in maintaining healthy oral tissues. It is bacteriostatic and controls the pathogenic bacteria normally present in the
oral cavity that are largely responsible for dental caries. The secretion of saliva is controlled by the salivatory nucleus in the brainstem. The nerve fibers of the parasympathetic nervous system carry signals from the salivatory nucleus to the salivary glands. The parasympathetic nerve fibers arrive in the oral cavity as part of the lingual nerve, a branch of the trigeminal nerve (Guyton, 1981) (Figure 1–7).
ORAL PHASE
The bolus is propelled from the oral cavity into the pharynx during the oral phase of swallowing. The top of the tongue is placed on the superior alveolar ridge behind the maxillary central incisors. Voluntary opening of the pharynx then begins with elevation of the soft palate and depression of the
Inferior constrictor
Figure 1–9. Posterior view of the pharyngeal constrictor muscles. The superior pharyngeal constrictor is suspended from the skull base via the pharyngobasilar fascia. Note the paired muscles meet in the midline.
From Foundations of Speech and Hearing: Anatomy and Physiology, 2nd ed. (p. 133), by Jeannette D. Hoit, Gary Weismer, and Brad Story, 2022, Plural Publishing. © 2022 by Plural Publishing.
posterior tongue (see Video 1–1, Straw Drinking on the companion website). In this way, there is expansion of the posterior oral cavity and a chute forms in the tongue base guiding the movement of the bolus into the pharynx. Elevation of the palate occurs as a result of contraction of the levator veli palatini muscle (see Figure 1–4). The levator veli palatini muscle receives motor innervation from the vagus nerve (X) via the pharyngeal plexus (see Figure 1–6). The hyoglossus muscle (innervated by XII) and, to a lesser extent, the styloglossus muscle (also innervated by XII) are active in posterior tongue depression. The anterior half of the tongue is then
pressed against the maxillary alveolar ridge and the anterior half of the hard palate in rapid sequence, moving the bolus posteriorly on the dorsum of the tongue. Coordinated and effective tongue movement, full range of tongue motion, and tongue strength are imperative for the efficient transfer of the bolus from the oral cavity into the pharynx. Tongue muscle weakness, cranial nerve XII injury, or tethering of the tongue secondary to injury or surgery can prevent adequate tongue function and can impair bolus movement into the pharynx.
Contraction of the orbicularis oris and buccinator muscles prevents pressure
escape forward, out of the mouth, or laterally during bolus movement into the pharynx. Patients with facial muscle weakness have difficulty with the oral phase of swallowing due to the incompetence of the first valve, the lips. Try a “dry” swallow of saliva with the lips open for a firsthand experience of the difficulty created by a failure of the anterior oral sphincter!
During the oral phase of swallowing, soft palate elevation allows the bolus to pass through the tonsillar pillars and into the oropharynx. Once the soft palate is fully elevated, it contacts the adjacent pharyngeal walls in a valving action that acts to prevent penetration of the bolus or escape of air pressure into the nasopharynx. The side walls of the nasopharynx, consisting of the superior pharyngeal constrictor muscles, oppose the soft palate to make a
more forceful closure of the nasopharynx. The superior pharyngeal constrictor is suspended from the skull base via the pharyngobasilar fascia and the paired muscles meet and attach to one another in the posterior midline (see Figure 1–9). The anterior attachments of the superior pharyngeal constrictor include the inferior aspect of the pterygoid plates, the buccinator muscle, and the inner surface of the mandible (Figure 1–10).
The effective closing of the nasopharynx, along with the cessation of nasal respiration, is required to prevent pressure or bolus escape into the nasopharynx and weakening the forces that drive the bolus inferiorly into the pharynx. In this way, the soft palate has a dual sphincteric function with respect to swallowing. Along with the tongue base, the soft palate is part
Figure 1–10. Lateral view of the pharyngeal constrictor muscles. Note the anterior attachment of the superior pharyngeal constrictor to the mandible and posterior fascia of the buccinator muscle. The middle constrictor attaches to the hyoid bone and the inferior constrictor to the thyroid and cricoid cartilages. From Foundations of Speech and Hearing: Anatomy and Physiology, 2nd ed. (p. 133), by Jeannette D. Hoit, Gary Weismer, and Brad Story, 2022, Plural Publishing. © 2022 by Plural Publishing.
of the sphincter at the posterior part of the oral cavity that prevents premature movement of the bolus into the pharynx during the preparatory phase of swallowing and the soft palate also forms a sphincter with the superior pharyngeal constrictor muscles between the nasopharynx and the oropharynx during the oral and pharyngeal phases of swallowing. Motor nerve fibers from the vagus nerve (X) via the pharyngeal plexus innervate the superior pharyngeal constrictor and palatal musculature (see Figure 1–6). Palatal defects or weakness result in early spillage of the bolus into the pharynx during the preparatory phase of swallowing and reflux of bolus into the nasopharynx during the oral and pharyngeal phases of swallowing. Even if bolus movement is not significantly impacted by palatal
pathology, forces needed for effective bolus movement are impaired by pressure escape from the active swallowing chamber (the oropharynx) through the incompetent sphincter (palate to nasopharyngeal walls) (Figure 1–11).
Toward the end of the preparatory phase of swallowing, the hyoid bone is moderately elevated in preparation for the pharyngeal phase of swallowing. The anterior displacement of the hyoid bone pulls open the anterior-posterior dimension of the pharynx. This expansion of the pharyngeal chamber creates a vacuum within the oropharynx that aids in movement of the bolus into the pharynx. Early hyoid bone elevation occurs primarily as a result of mylohyoid muscle contraction. The mylohyoid muscle attaches to the lateral interior of the mandible and joins the opposite

mylohyoid muscle in the midline. Posteriorly, the mylohyoid muscle attaches to the hyoid bone. Motor innervation of the mylohyoid muscle comes from a branch of the trigeminal nerve (V) (Figure 1–12).
The muscles involved in the oropharyngeal phase of swallowing represent three anatomical regions: the suprahyoid suspensory muscles (which affect the position of the posterior tongue and the hyoid bone), the muscles surrounding the tonsillar pillars, and the muscles involved in the closure of the nasopharynx. Muscles that discharge during the preparatory phase of swallowing include the muscles of the face (specifically those within the lips and cheeks), the tongue muscles, the superior pharyngeal constrictor, the styloglossus, and stylohyoid, geniohyoid, and mylohyoid muscles, with the palatoglossus and palatopharyngeus muscles dem-
onstrating their maximal activity later. The mylohyoid and the anterior and posterior bellies of the digastric muscle participate in the subsequent elevation of the hyoid and larynx.
PHARYNGEAL PHASE
Passage of food through the pharynx and into the esophagus occurs during the pharyngeal phase of swallowing. Respiration and swallowing must be coordinated during this portion of the swallow, since both functions occur through the common portal of the pharynx but not simultaneously. Respiration must cease during the pharyngeal phase of deglutition with closure of the soft palate against the superior pharyngeal constrictor muscle. Central control of pharyngeal swallowing involves an efficient, automatic mechanism, so that respiration can resume in a timely manner. The pharyngeal phase of swallowing is also involuntary, and once initiated, it is an irreversible motor event.
Figure 1–12. Mylohyoid muscle. The muscle attaches to the interior surface of the mandible anteriorly and the hyoid posteriorly. Contraction results in anterior movement and elevation of the hyoid bone. From Foundations of Speech and Hearing: Anatomy and Physiology, 2nd ed. (p. 168), by Jeannette D. Hoit, Gary Weismer, and Brad Story, 2022, Plural Publishing. © 2022 by Plural Publishing.
At the onset of the pharyngeal phase of swallowing, the tongue carries the bolus into the oropharynx, as the entire posterior mass of the tongue is rolled backward on the hyoid bone while maintaining the bolus on the tongue surface. The mandibular muscles (medial and lateral pterygoid muscles, masseter and temporalis muscles [innervated by V]) contribute to stabilization of the tongue base during the development of the tongue’s piston-like movements, and this stabilization of the tongue is more critical with boluses of thicker consistency. The mandible is held in a closed position during swallowing (see Figure 1–8).
As the bolus is propelled posteriorly by the piston-like movement of
ANATOMY AND PHYSIOLOGY
the tongue, the pharynx, as a whole, elevates and then contracts to create a descending peristaltic wave behind the bolus. Elevation of the pharynx occurs when the paired palatopharyngeus and stylopharyngeus muscles contract. The walls of the pharyngeal chamber stiffen because of the sequential contraction of its three constrictors. The palatopharyngeus muscles and the pharyngeal constrictors are innervated by branches of cranial nerve X and the stylopharyngeus by cranial nerve IX, both via the pharyngeal plexus (see Figure 1–6).
Just like the superior pharyngeal constrictor muscles, the paired middle and inferior constrictor muscles meet in the posterior midline. The middle
constrictor attaches to the hyoid bone anteriorly, and the inferior constrictor attaches to the thyroid and cricoid cartilage anteriorly (see Figures 1–9 and 1–10).
As the oropharynx is a closed cavity at the time of bolus passage (the soft palate has closed off the nasopharynx, and the pharyngo-esophageal segment is closed inferiorly), the pressure generated by the tongue base contacting the pharyngeal walls provides a force that drives the bolus inferiorly. In normal swallowing, the pharyngeal chamber constricts behind the bolus to the point of complete obliteration of the pharyngeal cavity, effectively clearing all the bolus from the pharynx (Figure 1–13).

view from videofluoroscopic swallowing study: pharyngeal phase. Note anterior displacement of hyoid and larynx with expansion of the hypopharynx. The tongue base contacts the posterior pharyngeal wall. Subject has a cricopharyngeal bar at cervical vertebra 5.
Weakness or defects of the tongue base and weakness of the pharyngeal constrictors prevent complete contact of the tongue base with the constrictors and impair development of adequate driving forces behind the bolus. Weak pharyngeal constriction or incomplete posterior tongue base movement therefore results in pharyngeal residue remaining in the pharynx after the pharyngeal phase of swallowing and creates a significant risk for aspiration of residual bolus after the swallow.
While the tongue base and pharyngeal constrictors are creating a pistonlike constriction behind the bolus in the pharynx, the hyoid and larynx rise and are pulled forward under the root of the tongue by the contraction of the suprahyoid muscles. The mylohyoid muscle and anterior belly of the digastric muscle are innervated by a branch of the trigeminal nerve (V) (see Figures 1–7 and 1–12), and the geniohyoid muscle is innervated by a branch of cervical root 1 (C1) that travels with the hypoglossal nerve (XII) (see Figure 1–3). Contraction of these muscles moves the hyoid superiorly and anteriorly toward the anterior arch of the mandible.
The larynx moves superiorly with the hyoid bone because it is attached to the hyoid bone by the thyrohyoid membrane and paired thyrohyoid muscles (innervated by C1). This superior-anterior movement of the larynx simultaneously protects the larynx from penetration by the bolus and expands the hypopharyngeal chamber, causing a decrease of pressure in the pharyngoesophageal (PE) segment. This decrease in pressure in front of the bolus, along with the piston action of the tongue base against the pharyngeal constrictors, drives the bolus through the phar-
ynx and into the upper esophagus (see Figure 1–13).
As the bolus is driven inferiorly and the larynx begins to move forward, the epiglottis folds down over the laryngeal opening. The epiglottis moves from an upright to a horizontal position and then tips downward. This positional change of the epiglottis is caused mainly by elevation of the hyoid and larynx as well as by contraction of the paired thyrohyoid muscles (C1) followed by contraction of the intrinsic laryngeal muscles to close the vocal folds (X, via the recurrent laryngeal nerve). The abductors of the vocal folds, the posterior cricoarytenoid muscles, are inhibited during this phase, ensuring closure of the vocal folds and protection of the airway from the bolus. The true and ventricular vocal folds play a major role in protecting the laryngeal vestibule by constricting the laryngeal aperture. The larynx closes anatomically from below upward: first, the vocal folds, then the vestibular folds, then the lower vestibule (approximation and forward movement of the arytenoids), and then the upper vestibule (horizontal position of the epiglottis that contacts the closed arytenoids). Opening of the larynx proceeds from above downward. Many of the mechanisms that contribute to airway protection also contribute to bolus transportation as closure of the larynx creates pressures that promote movement of the bolus away from the larynx and into the upper esophagus (Figure 1–14) (Doty & Bosma, 1956; Kidder, 1995).
Closure of the larynx during swallowing is carried out by the adductor muscles of the vocal folds. These muscles are innervated by a branch of the vagus nerve, the recurrent laryngeal
