Faculty member Quyen Phan plays a leading role alongside students in community-based health care training and delivery programs.

COLLABORATING WITH PARTNERS, WE DO TOGETHER WHAT WE CANNOT DO ALONE




Faculty member Quyen Phan plays a leading role alongside students in community-based health care training and delivery programs.

COLLABORATING WITH PARTNERS, WE DO TOGETHER WHAT WE CANNOT DO ALONE



The same can be said of health care. It takes a host of players to address the health and well-being of individuals and communities. Undoubtedly, health care professionals including nursing clinicians, leaders, researchers, and educators are part of this effort. But to have a real and lasting impact, health care must be a partnership with the individuals and communities we are called to serve. It must involve a myriad of stakeholders — nonprofit organizations, governmental leaders and agencies, corporate partners, volunteers, donors, and many others.
The Nell Hodgson Woodruff School of Nursing has embraced this kind of partnership throughout its history. Over the past 20-plus years, this partnership has been embodied in the Lillian Carter Center for Global Health & Social Responsibility, which focuses on community engagement, student service learning, and global health. This center’s work has evolved more recently to incorporate a laser focus on community-engaged research, resulting in over $20 million in federal funding for research projects benefiting the health of communities.
This work would not be possible without partnerships — without the entire orchestra. No one knows a community better than the community itself; no one understands the social determinants of their community’s health more so than they do. That’s why we walk alongside community organizations and other partners so that we can learn together and create lasting progress. This knowledge and expertise inform every facet of our curriculum, and our students are better prepared for it.
This issue of Emory Nursing is focused on community engagement — understanding that the last five letters of the word “community” are central. It takes the unified efforts of our faculty, staff, and students — along with our community partners — to move the needle toward greater health and well-being.

 Linda A. McCauley 79MN, PhD, RN, FAAN, FRCN Professor and Dean Nell Hodgson Woodruff School of Nursing
Linda A. McCauley 79MN, PhD, RN, FAAN, FRCN Professor and Dean Nell Hodgson Woodruff School of Nursing
“No one can whistle a symphony. It takes a whole orchestra to play it.”
— H.E. Luccock
Dean, Nell Hodgson Woodruff School of Nursing
Linda A. McCauley 79MN, PhD, RN, FAAN, FRCN
Chief Engagement Officer
Tricia Benson 86MN
Senior Director of Communications and Marketing
Melanie Kieve
Director of Communications and Marketing
Lauren Powers
Managing Editor
Pam Auchmutey
Art and Creative Director
Erica Endicott
Editorial Contributors
Jim Auchmutey
Chelsea Shackelford
Sylvia Wrobel
Photography Contributors
Brandon Clifton
Sydney Foster
Jennifer Girtman
Patrick Heagney
Kay Hinton
Jack Kearse
Lauren Liz Photo
Audra Melton
Stephen Nowland
Ted Pio Roda Photography
Parker Clayton Smith
Emory Nursing is published by the Nell Hodgson Woodruff School of Nursing (nursing.emory.edu), a component of the Woodruff Health Sciences Center of Emory University. ©2023


Emory University is an equal opportunity/ affirmative action employer fully committed to achieving a diverse workforce and complies with all federal and Georgia state laws, regulations, and executive orders regarding nondiscrimination and affirmative action.
Emory University does not discriminate on the basis of race, age, color, religion, national origin or ancestry, gender, disability, veteran status, genetic information, sexual orientation, or gender identity or expression.
How the school works alongside community partners – and prepares students to do the same

From dementia to mobile health, the school and its community partners are unified in addressing access to health care
14 Making African American churches more dementia-friendly
15 Educating clinical instructors and preceptors
16 Increasing research opportunities for aging and caregiving LGBTQIA+ populations
17 Boosting clinician well-being
20 Supporting the community health workforce
21 Preventing acute kidney injury in Florida farmworkers
22 Equipping Black women to avoid toxic environmental exposures
23 Strengthening culturally sensitive acute care

26 Expanding mobile health in Atlanta and rural Georgia
27 Helping African American mothers avoid prenatal and postpartum complications
 By Pam Auchmutey | Photos by Audra Melton
By Pam Auchmutey | Photos by Audra Melton
 A couple waits for their appointment at Boat People SOS, one of the School of Nursing’s community partners. Left: BSN students and clinical instructor Deborah Silverstein (second from left) chat with a patient at Boat People SOS.
A couple waits for their appointment at Boat People SOS, one of the School of Nursing’s community partners. Left: BSN students and clinical instructor Deborah Silverstein (second from left) chat with a patient at Boat People SOS.
For more than 15 years, the School of Nursing assistant clinical professor has worked with the local branch of Boat People SOS (BPSOS), which provides citizenship, occupational, and other social services to Vietnamese and Asian populations in Atlanta. Eleven years ago, with input from the BPSOS community, she developed a free community clinic to serve low-income individuals from across the metro area. Each semester, students from her population health course spend Saturdays at the weekly BPSOS clinic, providing health screenings, primary care, and vaccinations for adult and senior clients. Also, it is where the social determinants of each client’s health
and the power of community partnerships come alive for students.
Phan’s connections to BPSOS and other community organizations proved especially valuable during the COVID-19 pandemic. At the time, BPSOS had a steady supply of COVID vaccines, Atlanta’s Mexican Consulate — where Emory nursing students also provide health screenings — had plenty of clients, and the School of Nursing had expertise in administering vaccines. As she worked alongside these groups, Phan saw a great opportunity.
“On a given day at the Mexican Consulate, we brought the three groups together,” says Phan 03MSN, DNP, APRN, FNP-BC. “Our nursing faculty and students served hundreds of clients. It was community partnership in its truest form.”
In 2022, the School of Nursing received a record amount of federal funding to expand such initiatives. The U.S. Department of Health Resources and Services Administration (HRSA) awarded six grants totaling more than $15.4 million to support health care delivery

The clinic is where the social determinants of each client's health and the power of community partnerships come alive for students.




As a young nurse in Kenya, Jacob Kariuki, PhD, discovered the revelatory power of data collection and analysis — and the value of global perspectives to better understand health issues.
That background will serve him well in his new role as assistant director for global health research with the Lillian Carter Center for Global Health & Social Responsibility (LCC), where he will drive innovation and develop partnerships, primarily in Africa.
Before joining the LCC, Kariuki knew about its global health success, such as reducing household air pollution from cookstoves in Guatemala and strengthening the nursing workforce infrastructure and data collection in Kenya. He was particularly drawn to the School of Nursing’s Emory-Ethiopia Partnership, which includes a successful initiative to improve maternal-child health using simple, low- or no-cost measures in remote communities. The same partnership gave rise to Ethiopia’s first nursing PhD program, and “could become the North Star of the center’s engagement with the African continent,” he says.
Kariuki sees potential for growing research in a variety of ways. For example, the LCC’s International Visiting Scholars Program attracts health professionals from across the globe. These scholars, he believes, could foster new research collaborations.
“I’ve long admired the Lillian Carter Center’s work in global health, service learning, and community empowerment,” says Kariuki. “When Dean McCauley described the center’s plans to strengthen global health research, I knew immediately I wanted to play a part.” — Sylvia Wrobel
Newborn health initiatives are part of the Emory-Ethiopia Partnership, which Kariuki believes could be a good model for the Lillian Carter Center’s work in Africa.


and training programs. Phan plays a role in four of these projects and leads two of them.
“All of the HRSA grants will help us address the social determinants of health and health equity at the community level,” says Phan. “Often, when people are disenfranchised, they don’t get the care they deserve. As nurses, we need to be better prepared to close that gap.”
In recent years, “community engagement” has taken on greater significance as a defining principle of Emory University, one that Linda McCauley 79MN, PhD, RN, FAAN, FRCN, understands well as a public health nurse, environmental and occupational health researcher, and dean of the School of Nursing.
Community engagement and the HRSA projects are part of the work of the nursing school’s Lillian Carter Center for Global Health & Social Responsibility.


“The community is where much of care happens,” says McCauley. “As nurses, we have a responsibility to be part of the solution of making sure every individual has access to care. The funding from HRSA bolsters our efforts in preparing future nurse leaders to serve people in the communities where they live.”
Community engagement and the HRSA projects are part of the work of the nursing school’s Lillian Carter Center for Global Health & Social Responsibility (LCC). Established in 2001, the center aims to improve the health of vulnerable people worldwide through nursing education, research, practice, and policy.
“During its formative years, the LCC focused on strengthening the global nursing workforce and formalizing service-learning programs for students in Georgia and other countries,” says Tricia Benson 86MN, the School of Nursing’s chief engagement officer and executive director of the Lillian Carter Center.
“Today, the LCC’s work in community engagement, service learning, and global health is more deeply rooted than ever,” she continues. “Support from HRSA and other federal agencies is broadening the impact of the LCC’s work, especially in collaborative partnerships with Atlanta-area organizations. Our students will take this communitycentered understanding, skill, and sensitivity forward to their future careers in nursing.”
“We’ve always had partnerships with community agencies,” says Elizabeth Downes 04MPH, DNP, FNP-C, CNE, FAANP, ANEF, FAAN, assistant dean of global health and co-director of the LCC. “When the Lillian Carter Center was formed, we began to focus more on how to meet the needs of the communities we’re serving. Community impact and creating meaningful change are the bases of our program.”
Students and faculty collaborate with longtime partners to provide clinical care and health education in metro Atlanta and other parts of Georgia, as well as the Bahamas, Haiti, the Dominican Republic, Jamaica, Peru, and other countries. For more than 20
years, students, faculty, and alumni have spent two weeks in South Georgia providing health care for migrant farmworkers and families in collaboration with the Georgia Ellenton Farmworker Health Clinic and health professions students from other Georgia colleges and universities.
Nursing students are drawn to Emory because of these experiences. Among them are the Fuld Service Learning Fellows, MN+MSN pathway students who plan to work with underserved populations. The Fuld Fellowship was established through a gift to the School of Nursing from the Helene Fuld Health Trust (see page 11).
At the School of Nursing, students learn about the social determinants of health in every course they take, based on goals set by the Association of American Colleges of Nursing, the U.S. Department of Health and Human Services, and other agencies.
“It’s important that we fully embrace the social determinants of health so that we provide the best care to our patient populations,” says Professor Jill Hamilton 21MRPL, PhD, RN, FAAN,
the National Institutes of Health and the Department of Health and Human Services. Research projects include preventing heat-related illnesses among farmworkers and reducing children’s environmental health risks.

“Community engagement work takes place in different ways, and scholarship is an important part of that work,” says McCauley. “To do meaningful research on the social determinants of health, you have to partner with communities where people work and live. Federal agencies understand that. Funding this type of research is an investment in health equity. It helps people who need it most.”
Going forward, the nursing school’s roots in community engagement will continue to spread. The school’s new Emory Nursing Learning Center is helping the school expand its community partnerships, locally and globally.
The center, which houses the school’s clinical skills and simulation labs, opened last August in a city brimming with learning and service opportunities.
This focus on social determinants has played a big role in the school's community-engaged initiatives, the funding of which has grown substantially in recent years. In addition to HRSA funding, the school received a record $23 million in federal funding from
“When you walk out the doors of the Emory Nursing Learning Center, you’re in the heart of the community,” says Benson. “The learning center allows us to partner and engage in Fulton and DeKalb counties in deep and meaningful ways.”
Whether the work is in Decatur — or other parts of the city, state, nation, or world — the nursing school is embracing the reality that health care and community care go hand in hand.
“All of the HRSA grants will help us address the social determinants of health and health equity at the community level. Often, when people are disenfranchised, they don’t get the care they deserve. As nurses, we need to be better prepared to close that gap.” — Quyen Phan
NURTURING STUDENT INTEREST IN SOCIAL RESPONSIBILITY
Currently, the school has three Fuld Service Learning Fellows: Guadalupe Castaneda (second from left), Leah Bercovitch, and Heather Allstrom. Lalita Kaligotla (left) oversees the Fuld Fellowships.

Heather Allstrom 22MN 24DNP had no ties to Emory University. She grew up a thousand miles away in Rhode Island, earned her undergraduate degree from the University of Connecticut, and volunteered with AmeriCorps at a shelter for pregnant and parenting women in Tempe, Arizona.
But when she decided to go to nursing school and started researching the possibilities, the Nell Hodgson Woodruff School of Nursing jumped to the top of her list.
20 YEARS OF GRATITUDE
With a mission to support the health, welfare, and education of student nurses, the Helene Fuld Health Trust is the nation’s largest private funder devoted to nursing students and nursing education.
“It has such an amazing name and reputation, and you can tell just from the website how much the school stands for community service,” she says.
The clincher in her decision to come to Emory: a fellowship that paid half of her tuition.
Allstrom was awarded a Fuld Service Learning Fellowship, a program that supports MN+MSN pathway students with a special interest in underserved communities. She’s a work-study student in the Lillian Carter Center, which houses the fellowships, and volunteers as a nurse with Community Advanced Practice Nurses, helping to staff a free walk-in clinic at an Atlanta homeless shelter.
“We select students who are interested in community engagement and social responsibility,” says Lalita Kaligotla, MSW, MBA, who oversees the Fuld Fellowships as senior director of leadership and engagement at the School of Nursing. “The whole idea is to have a broader role in providing health care to underserved populations.”
The fellowships started in 2002 with a grant from the Helene Fuld Health Trust. In Allstrom’s case, the fellowship supported her accelerated master’s degree, which she earned in 2022. She’s now pursuing her doctorate in nursing practice and expects to graduate in 2024 as a women’s health and gender-related nurse practitioner.
There are two Fuld Fellows in addition to Allstrom: Leah Bercovitch 23MN, who works on issues of food insecurity among children with Strong4Life, an initiative at Children’s Healthcare of Atlanta; and Guadalupe Castaneda 23MN, who works with Latino Community Fund Georgia to provide health screening and health education to community members.
Fuld Fellows have gone on to do everything from working as nurse practitioners to leading community service organizations.
Allstrom would be happy to follow a similar path. After completing her DNP, she hopes to continue her work in free walk-in clinics. — Jim
AuchmuteyIn 1935, Dr. Leonhard Felix Fuld and his sister, Florentine, created a foundation in honor of their mother, Helene Shwab Fuld, who died in 1923. During her lifetime, Helene Fuld was passionately interested in health issues, and the foundation named for her was originally dedicated to the “relief of poverty, suffering, sickness, and distress.” In 1961, Dr. Fuld limited the foundation’s focus to “the improvement of the health and welfare of student nurses.”
The School of Nursing is grateful to the Helene Fuld Health Trust for the gifts of over
$12 million to fund the Fuld Service Learning Fellowship, the Fuld Fellowship Program in Palliative Care, and additional scholarships for Master of Nursing students.
The school’s first gift from the Helene Fuld Health Trust was in 2002. Over the past 20 years, more than 100 students have benefited from tuition support provided by the trust.






FROM DEMENTIA TO MOBILE HEALTH, THE SCHOOL AND ITS COMMUNITY PARTNERS ARE UNIFIED IN ADDRESSING ACCESS TO HEALTH CARE








African American faith communities
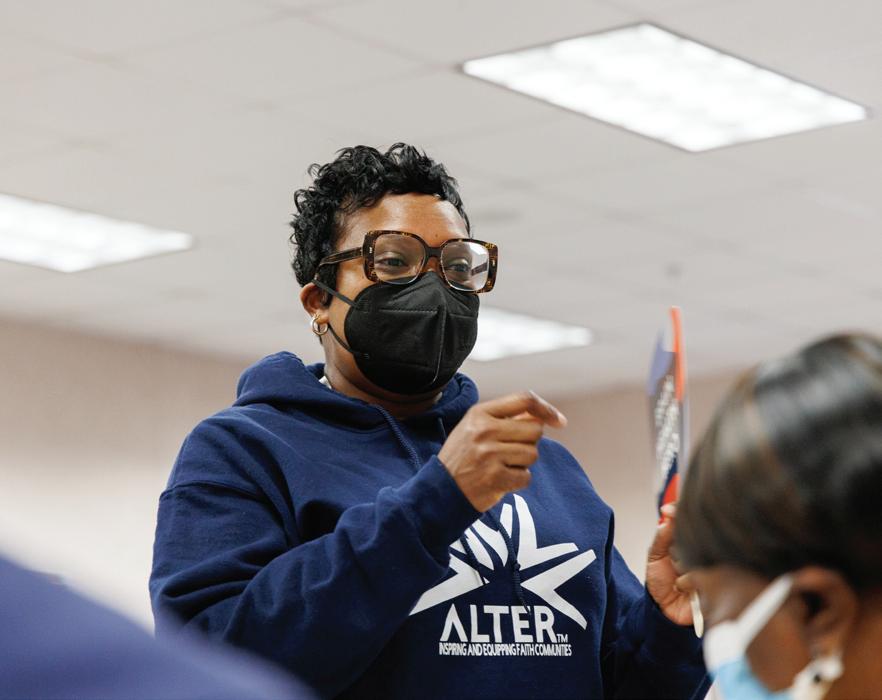
Living with or caregiving for dementia is challenging enough. Layering it with race makes it even more so. Fayron Epps wants to change that.
Established in 2019, the Faith Village Research Lab aims to provide African American caregivers, families, and faith communities with the tools they need to more easily and comfortably access care, education, and research resources related to dementia.

Lab founder and director Fayron Epps knew many African Americans thought of dementia as a “white disease,” but she saw clearly how it more often impacted communities of color — and how often these communities were underserved.

When she arrived at the School of Nursing as an assistant professor, those were the communities she wanted to target, creating culturally responsive programs “for us, by us.”
The Faith Village Research Lab’s Alter program currently partners with more than 45 African American faith communities in 10 states.
To participate, each organization must commit to 16 initiatives, which include training church leaders, making church buildings more accessible, creating special worship services for memory-impaired parishioners, finding new ways to make patients and families feel more
accepted, and offering memory screenings, coffee hours, home visits, and respite care.
One of Epps’ most rewarding moments occurred when a woman thanked her for helping her father continue to participate in worship. The daughter was also grateful to participate in research she knew would help others; Epps’ lab connects community members with social science studies and clinical trials.
Alter is conducted in partnership with Georgia State University and supported by the Health Resources and Services Administration and other agencies. — Sylvia Wrobel
FACULTY MEMBER
Quyen Phan 03MSN, DNP, APRN, FNP-BC, assistant clinical professor
PARTNERS/COMMUNITY
Emory Healthcare, DeKalb County Board of Health, Mercy Care, Atlanta Harm Reduction Coalition, Boat People SOS, and other community agencies
Like all professionals, nurses benefit from the guidance of experienced colleagues as they begin their careers. That reality is at the heart of the CAPES Academy, which will recruit and prepare nurses to serve as clinical faculty and preceptors to nursing students and newly licensed nurses in underserved areas of the Southeast.
On a Saturday morning at a free clinic for uninsured and low-income residents in metro Atlanta, School of Nursing student Rebecca Deal 22Ox 24BSN vaccinated a patient for COVID-19. Deal carefully administered the booster shot under the guidance of Deborah Silverstein 78C 83BSN 17MSN 20DNP, FNP-C, her clinical instructor from the Emory School of Nursing, and Thao Nguyen, program coordinator at Boat People SOS.
Nurses like Silverstein play an important role in bridging the gap between theoretical learning and clinical practice for students. The need for more instructors and preceptors is critical to growing the nursing workforce in medically underserved communities — the impetus behind a project at the School of Nursing.
The Clinical Instructor and Preceptor Excellence in the Southeast (CAPES) Academy will prepare 128 licensed nurses to serve as
nurse educators in eight states — Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee. It is part of an initiative funded by the Health Resources and Services Administration to bolster nursing education through partnerships among academics, clinicians, and community organizations.
Over the next four years, the CAPES Academy will recruit 32 nurses annually. All will receive stipends to complete the yearlong program. Instruction will include online classes, in-person exercises at the Emory Nursing Learning Center, shadowing experiences, and professional development.

Quyen Phan, assistant clinical professor in the School of Nursing, directs the CAPES Academy.
Emory Healthcare, DeKalb County Board of Health, Mercy Care, Atlanta Harm Reduction Coalition, and Boat People SOS are among the partners Phan has tapped to provide education and shadowing experiences for CAPES Academy nurses in the Atlanta area. — Pam Auchmutey
FACULTY MEMBER
Whitney Wharton, PhD, associate professorLeaders in the local and national LGBTQIA+ community, with support from the Alzheimer’s Association and the National Institute on Aging
Some aspects of aging and caregiving among members of the LGBTQIA+ community are more prominent, less recognized, and too seldom included in clinical research. The RISE initiative helps address those challenges.
As a child, Whitney Wharton watched her parents’ arduous journey as caregivers for her grandmother. It was a powerful introduction to challenges faced by Alzheimer’s patients and caregivers.
Years later, as a cognitive neuroscientist, she recognized that some communities have fewer resources and greater fears about how they are perceived or stigmatized as they age.
Many LGBTQIA+ persons, she found, didn’t know where to find resources for aging and caregiving. Also, many clinicians and researchers did not know the right questions to ask them.
Working with colleagues at the University of Nevada, Las Vegas, and the University of Tennessee, Knoxville, Wharton created RISE (Research Inclusion Supports Equity) to address both challenges. The website includes resources related to aging, living with memory loss, and caring for a family member or friend.
RISE also includes a registry (theriseregistry. org) to help ensure that LGBTQIA+ patients and caregivers are better represented in Alzheimer’s and aging research.
Not collecting information about sexual orientation and gender identity can weaken
research, Wharton says. The LGBTQIA+ community faces different challenges, especially when race is a factor. LGBTQIA+ individuals are more likely to become caregivers because they are less likely to have children and more likely to live alone.

Caregiving is even more stressful when LGBTQIA+ individuals have not come out to parents or relatives or if families disapprove of their partner or living situation. Close-knit families of choice within the LGBTQIA+ community often have caregiving responsibilities not represented in traditional family dynamics.
Through its website and registry, RISE strives to make health care providers and researchers more responsive to these challenges. — Sylvia Wrobel
“The overwhelming interest in RISE since its founding one year ago speaks to the urgent and previously unmet needs of the aging and caregiving LGBTQIA+ population and those who work with them.” — Whitney Wharton
FACULTY MEMBER
Nicholas A. Giordano, PhD, RN, assistant professor
PARTNERS/COMMUNITY
Emory Healthcare, Grady Health System, Emory Healthcare Public Safety, and Emory University Police Department
Because of the pandemic, work-related stress and burnout are more pervasive among workers across clinical care settings. An initiative called ARROW — Atlanta’s Resiliency Resource fOr frontline Workers — is helping foster resiliency among frontline workers, including those who care for underserved populations.
Nicholas A. Giordano, an assistant professor in the School of Nursing, is working toward a sustainable systems-level solution as director of ARROW. Through this initiative, health care and other frontline workers are learning how to use mindfulness and compassion-based skills to strengthen self-care.
ARROW is funded by the Health Resources and Services Administration as part of its nationwide resiliency training program. Instruction is free for Emory Healthcare and Grady Health System clinicians and staff and Emory Healthcare and Emory University public safety and police officers.
To date, Giordano and his Emory nursing, medicine, public health, and spiritual health colleagues
Clinicians participate in Cognitively Based Compassion Training, a program offered through ARROW to enhance mental well-being and resiliency.
have trained more than 250 frontline workers.
Once a week, wellness workshops are held in departments and units within the hospitals. Those wanting to learn more may take an eighthour program grounded in spiritual health that combines classroom instruction and contemplative exercises.


Some participants have become certified trainers themselves, a development that will have a sustainable effect on worker well-being.
Grady is a prime example. When a newly certified instructor there held a workshop, more than 70 people attended. Grady now has 10 certified trainers. Mindfulness and self-compassion skills are now taught to Grady nurses during orientation and to a unit incident response team, says Michelle Wallace, DNP, RN, FRCN, NEA-BC, FACHE, chief nursing officer at Grady Health System.
Online mindfulness instruction will soon be available through the Emory Nursing Experience, which provides continuing education for nurses. — Pam Auchmutey
A NEW BOOK SHOWS PROMISE FOR CHANGING HOW NURSING SCHOOLS TEACH ABOUT THE SOCIAL DETERMINANTS THAT AFFECT PATIENTS’ HEALTH
 By Pam Auchmutey | Photo by Patrick Heagney
By Pam Auchmutey | Photo by Patrick Heagney
Jill Hamilton 21MRPL, PhD, RN, FAAN, FAACE, has always been guided by faith. More than once, it has helped the Emory nursing researcher tackle a challenge by answering the question, “How am I going to do this?”
Years ago, the question helped her put others’ skepticism aside to understand how religious songs help African Americans during stressful life events. Her studies dovetailed with her interest in the social determinants of health (SDOH) — the conditions in the communities where people live that affect their health.
Hamilton’s faith saw her through once more when Dean Linda McCauley 79MN, PhD, RN, FAAN, FRCN, asked her to lead an initiative to integrate the SDOH throughout the Emory School of Nursing curriculum. By fall 2021, the social determinants spanned the curriculum for all students.
The following spring, Hamilton, McCauley, and Beth Ann Swan, PhD, RN, FAAN, began work on a textbook describing the framework for integrating the SDOH into every course at the school.

“While there are books out about the social determinants of health, there isn’t one like this,” says Swan, associate dean and vice president for academic practice partnerships at the School of Nursing. “Numerous reports have come out in nursing, medicine, and health care about how significant the SDOH are in relation to a person’s illness and overall health and well-being. The publisher saw a gap in this arena and jumped at the chance to publish this book.”
Published in February by Springer Publishing, Integrating a Social Determinants of Health Framework into Nursing Education centers on the framework Hamilton developed for the School of Nursing curriculum. The framework includes four SDOH pillars — social, cultural, environmental, and policy and law — that affect health and well-being.

“It was clear to me that nursing needed a framework that could guide us in the way we approach social determinants among the diverse populations we serve,” she once said of her concept. “Nurses are in hospitals, in clinics, in communities, and in schools. We needed a framework that’s useful, regardless of the setting or population.”
The book's editors and publisher see it as a resource for nursing school leaders and faculty, professional nursing organizations, community organizations, public health agencies, nurses, and legislators. In the long run, the book could lead to improved health care quality and access, especially for patients from different backgrounds.
“It’s more important than ever for nurses to understand the populations they are taking care of,” says McCauley. “We need to understand, as best we can, their lived experiences and how that affects their health. We must all strive to be agents of change for our patients.”
“It was clear to me that nursing needed a framework that could guide us in the way we approach social determinants among the diverse populations we serve.”
— JILL HAMILTON
FACULTY MEMBER
Beth Ann Swan, PhD, RN, FAAN, associate dean and vice president for academic clinical partnerships and Charles F. and Peggy Evans Endowed Distinguished
Professor in Simulation and InnovationPARTNERS/COMMUNITY
AID Atlanta, Atlanta Harm Reduction Coalition, Boat People SOS, Four Corners Primary Care Centers, Emory Hillandale Hospital, Fulton County Board of Health, Fulton County Jail, Georgia Department of Public Health, Latino Community Fund Georgia, and other community organizations
Community health workers often have different job titles: community health advisor, outreach worker, patient navigator, peer counselor, and promotore de salud. The School of Nursing will lead a training program to expand this workforce to serve vulnerable individuals in five Atlanta-area counties.
During COVID-19, community health workers played a vital role in vaccine outreach and building vaccine confidence. These workers, U.S. Department of Health and Human Services officials note, are trusted voices in their communities. They help their neighbors stay healthy by connecting them to well-child care, chronic disease care, mental health and substance use prevention and treatment, and other vital services.
Numbers show that Atlanta needs more of these workers. In a recent ranking of the nation’s top 20 cities, Atlanta ranked next to last in health care cost, quality, and access.
The School of Nursing aims to improve this through the Atlanta Region Community Health Workforce Advancement (ARCHWAy) Program. Through this program, the school will provide 12 weeks of training for new and existing
community health workers serving vulnerable populations in Clayton, Coweta, DeKalb, Fulton, and Gwinnett counties. The program will also assist trainees with stipends, field and job placements, support services, referrals, financial literacy support, and mentoring.
Classes will be taught online and onsite at the Emory Nursing Learning Center in Decatur, utilizing simulated experiences and hands-on learning.
Over the next three years, faculty from the School of Nursing will lead 11 cohorts to train 450 community health workers.
ARCHWAy is funded by the Health Resources and Services Administration. Emory is the only nursing school in Georgia and one of three in the nation to receive funding for this type of program. — Pam
 Auchmutey
Auchmutey

FACULTY MEMBERS
Linda McCauley 79MN, PhD, RN, FAAN, FRCN, dean of the School of Nursing; Vicki Hertzberg, PhD, FASA, professor; and Roxana Chicas 16BSN 20PhD, assistant research professor
PARTNERS/COMMUNITY
The Farmworker Association of Florida and the Southeastern Coastal Center for Agricultural Health and Safety
Harvesting crops, flowers, and greenery is grueling work — one that can lead to heatrelated illnesses, according to a study led by the School of Nursing. Equipped with this information, Florida farmworker leaders are working to advocate for better working conditions for workers.

During summers in Central Florida, daily temperatures typically rise into the 90s. For migrant farmworkers working for area fern growers, the heat is more than uncomfortable. It can lead to acute kidney injury (AKI), according to the School of Nursing’s recent Occupational Health Exposure and Renal Dysfunction (OHEaRD) study.
Heat-related kidney damage among workers is caused by different factors. The material used to deflect sunlight off fern beds tends to keep heat in, causing farmworkers’ body temperatures to rise to the fever threshold of 100.4 degrees. Workers often don’t drink enough water to maintain a normal temperature and hydration.
How farmworkers are paid is also a factor, the study found. Workers who are paid by the hour take water and meal breaks and experience lower rates of kidney illness. Workers paid by
the piece — the number of ferns they pick — often skip water breaks. They push their bodies harder, leading to a higher incidence of AKI as well as rapid heart rate and nausea.
The AKI findings are based on a 32-month study that followed 115 agricultural workers in two Florida communities.
Going forward, OHEaRD results will help the Farmworker Association of Florida’s efforts to persuade growers and policymakers to continue to improve working conditions for these workers, who have the highest heatrelated mortality of all occupation groups in the United States.
OHEaRD is funded by the National Institute for Occupational Safety and Health and the Centers for Disease Control and Prevention. Researchers from Emory’s School of Medicine and Rollins School of Public Health are collaborators. — Pam Auchmutey

FACULTY MEMBER
Abby Mutic 19PhD, CNM
PARTNERS/COMMUNITY
The Center for Black Women’s Wellness and the Region 4 Pediatric Environmental Health Specialty Unit (PEHSU), a network of reproductive and children’s environmental health experts

Through Prescriptions for Preventions, a partnership with the Center for Black Women’s Wellness in Atlanta, Black mothers will have a much-needed resource to address environmental health risks in and around their homes.

As a young, certified nurse-midwife caring for pregnant women in rural Missouri, Abby Mutic was struck by how many of them experienced environmental stressors. They wondered if exposures at work or home were affecting their health and threatening the health of their families and unborn babies.
To find more answers, Mutic entered the PhD program at Emory’s School of Nursing, where she studied prenatal exposure to flame retardant materials. Now an assistant professor, Mutic continues to focus on environmental impacts on health, especially in children of color.
Through research, community presentations, and health fair screenings, Mutic strives to identify the people most affected by harmful environmental exposures and help them address their concerns. She is partnering with Atlanta’s Center for Black Women’s Wellness (CBWW) on a program called Prescriptions for Prevention (RxP), which is set to roll out this year.
RxP will employ an environmental health screener to work with CBWW patients and families, sharing guidance from the Region 4 PEHSU in culturally relevant ways. During clinic visits, the screener will evaluate exposure risks and factors that may protect against risk or increase risk of poor health.
Reports of exposures or environmental concerns will automatically generate a flag in the electronic medical record, alerting health care providers to address and possibly investigate further. The “prescription” they give to clients will consist of information on how to find and use available resources to reduce exposure. — Sylvia Wrobel
Equipping Black women to avoid toxic environmental exposuresAbove: Abby Mutic (center) discusses soil health with clinicians and staff at the Center for Black Women's Wellness in Atlanta. Below: Mutic enjoys a moment with Center for Black Women’s Wellness staff members at their office.
FACULTY MEMBERS
Roxana Chicas 16BSN 20PhD, assistant research professor, and Carrie McDermott, PhD, APRN, ACNS-BC, assistant professor
PARTNERS/COMMUNITY
Atlanta Harm Reduction Coalition, Boat People SOS, and Latino Community Fund Georgia
The School of Nursing has integrated the social determinants (SDOH) of health into its courses. The next step is to teach students how to address these factors in clinical practice. The place to begin: hands-on learning in the school’s clinical skills and simulation labs and working with community partners.
Nurses today must know how to deliver high-quality patient care within the context of a patient’s cultural, ethnic, racial, and gender identity.
A new program, Toward Health Equity and Literacy: Training for Optimal RN Efficacy in Acute Care (2HEAL), will ensure that Emory undergraduate nursing students are prepared to address these factors.

2HEAL will expand how students address SDOH in clinical training and deepen their insight into health equity and health literacy for underserved populations in metro Atlanta.
Beginning this fall, BSN students will take part in simulations with manikins
and standardized patients at the Emory Nursing Learning Center. They will also learn about SDOH by interacting with three community partners: Atlanta Harm Reduction Coalition, Boat People SOS, and Latino Community Fund Georgia. Through these partnerships, students will see how SDOH affect diverse populations and how community organizations improve health literacy and equity.
The faculty leading 2HEAL will also create web-based learning modules for clinical instructors and preceptors through the Emory Nursing Experience continuing education program.
2Heal is funded by a grant from the Health Services and Resources Administration. — Pam Auchmutey
Students and faculty provided blood pressure and diabetes screenings at a festival sponsored by Latino Community Fund Georgia,
THE EMORY NURSING

LEARNING CENTER PLAYS
A KEY ROLE IN U.S. PUBLIC HEALTH SERVICE EMERGENCY PREPAREDNESS TRAINING
 By Jim Auchmutey |
by Jack Kearse
By Jim Auchmutey |
by Jack Kearse
In the span of a few weeks last year, the Emory Nursing Learning Center went from a construction zone to a disaster zone. During four two-day sessions just weeks after the learning center opened, hundreds of U.S. Public Health Service (USPHS) officers from across the country gathered in Decatur for emergency drills designed by Emory’s Office of Critical Event Preparedness and Response (CEPAR) in partnership with the USPHS and the School of Nursing.
In the most dramatic exercise — the mass casualty drill — the terrace-level parking deck was turned into a scene of pain and chaos meant to resemble a partial building collapse caused by a hurricane. Volunteer
students made up with faux blood and wounds depicted a range of casualties, from lacerations and missing limbs to cardiac arrest and death.
“The goal is to make it realistic enough that it gets everyone’s pulse up,” says Sam Shartar, MSN, RN, NRP, CEN, FAAN, senior director of operations for CEPAR.
Since its creation 15 years ago, CEPAR has led training drills for emergency responders across Georgia.


The simulations at the learning center were the culmination of a yearlong refresher course for commissioned public health officers that began with online classes in 23 subjects such as IV therapy, airway management, common OB/GYN emergencies, and Introduction to Mass Casualty and Emergency Triage. More than 600 officers — physicians, nurses, nurse practitioners, and physician assistants — enrolled.

In the mass casualty drill, the officers were divided into groups of 12 to practice triage by sorting casualties into several categories of medical need.
“Triage is extremely stressful,” Shartar says. “You have very little data and a short time in which to make Solomon-like decisions for the greatest good for the greatest number of people.”
These sessions — and the lessons learned — are vital to enhancing clinicians’ readiness to deploy during disasters, public health emergencies, and humanitarian assistance missions.
FACULTY MEMBER
Quyen Phan 03MSN, DNP, APRN, FNP-BC, assistant clinical professor
PARTNERS/COMMUNITY
Georgia Ellenton Farmworker Health Clinic, Atlanta Harm Reduction Coalition, Boat People SOS, and Atlanta’s Mexican Consulate
For many people, access to health care is minimal or nonexistent. Emory In MOTION will help change that by providing mobile health services in nine Georgia counties. Mobile health units will be equipped to provide nurse-led health care in partnership with community agencies. Emory nursing students will also benefit as they learn to provide culturally sensitive clinical care.
On Wednesdays, the Atlanta Harm Reduction Coalition (AHRC) mobile van heads to a public park, a store parking lot, or another location to provide needle exchanges, Narcan, fentanyl test kits, health education, and HIV and hepatitis C testing.
Along for the ride is a nurse-led team of Emory BSN students who provide health screenings, health care, wound care, and telehealth services for the people served by AHRC, an organization that works to reduce the impact of substance use, HIV/AIDS, and other conditions.

The students are among the first to participate in Emory In MOTION, a mobile health training program funded by the Health Resources and Services Administration (HRSA). The project will help expand health care access and culturally aligned care in Atlanta and rural Georgia and provide learning opportunities for pre- and post-licensure students.
In South Georgia, Emory In MOTION is working with the Georgia Ellenton Farmworker Health Clinic, a longtime School of Nursing partner near Moultrie, to purchase and staff a nurseled mobile van that operates year-round. The van will also provide services at the school’s successful Farmworker Family Health Program, offered two weeks every summer. A nurse practitioner, supported by HRSA funding, will oversee the expanded mobile health services and precept Emory nursing students.
In Atlanta, a new family nurse practitioner will oversee students and expand mobile health services for AHRC. Another family nurse practitioner will guide students on a mobile health team with Boat People SOS. Nurse practitioners and students will work with the Mexican Consulate to provide mobile health care for the area’s Hispanic population.
One of the largest Health Resources and Services Administration grants in the history of the school, Emory in Motion also includes funding to support 10 mobile health student scholars annually. — Pam Auchmutey
FACULTY MEMBER
Alexis Dunn Amore, PhD, CNM, FACNM, FAAN, assistant professorPARTNERS/COMMUNITY
Nurse-midwives and other clinicians, the Healthy Mothers, Healthy Babies Coalition of Georgia, and other pregnancy-related organizations
Not recognizing the severity of physical or emotional symptoms during or after pregnancy can be life-threatening. MAMA LOVE gives African American mothers a tool to prevent that.

Early in 2023, the web-based program MAMA LOVE (mamalove.love) went live. Pregnant women now have a free, accessible, and user-friendly tool to determine the urgency of any symptoms and what they should do and when.
Founder and director Alexis Dunn Amore is an assistant professor in the School of Nursing and a certified nurse-midwife whose work focuses on highrisk pregnancies in communities of color.
Many of her patients, with few other resources at their disposal, often turn to Google or a friend to ask for advice about symptoms. Should I be worried? Call someone? Wait? For symptoms suggesting life-threatening conditions like sepsis, eclampsia, cardiomyopathy, or acute postpartum depression, even a short delay in intervention can be deadly. Amore decided to build a site where women could quickly and easily find information.
When entering the site, 10 boxes pop up with symptoms such as breathlessness, blurred vision, chest pain, thoughts of harming oneself, and not wanting to touch the baby. If the woman
acknowledges any of these symptoms, the site tells them to go to the ER or call 911.
If none apply, the pregnant person can select physical, mental, or social factors they are experiencing, and the program assigns them colorcoded advice.
RED indicates symptoms that need immediate emergency follow-up.
YELLOW assures the woman that a symptom needs follow-up with a provider.
BLUE advises the woman to call a clinic or nurse helpline to get more information.
The website also includes links to helplines and other resources.
MAMA LOVE is a community effort, says Amore, built with guidance from local doulas, OB-GYNs, nursemidwives, patients, community organizations, and focus groups. Amore and nurse-midwife and doctoral student Abby Britt 13MSN, CNM, FACNM, MA, met regularly with experts in the APP Hatchery, part of the Georgia Clinical & Translational Science Alliance. The American College of Nurse Midwives helped with the rollout, and the Robert W. Woodruff Fund supported the project. — Sylvia Wrobel IMPACT
“I wish MAMA LOVE had existed during my pregnancy when I was facing lifethreatening eclampsia. Recognizing my symptoms early — and knowing what to do about them — would have made a world of difference.” — MAMA
LOVE focus group participant
Multiple graduate specialties also earned high rankings:
No. 5
AdultGerontology Acute Care (DNP)
The School of Nursing continues to be ranked among the nation’s top nursing schools for research funding from the National Institutes of Health (NIH), according to an independent ranking of peer institutions.
School of Nursing master’s degree programs are the best in the nation, according to U.S. News & World Report’s annual ranking of graduate schools, which was released April 25.
The Master of Science in Nursing (MSN) and Master of Nursing (MN) programs came in at the top spot, while the Doctor of Nursing Practice (DNP) program retained its impressive No. 6 standing. U.S. News placed the school No. 2 in its undergraduate program rankings last fall.
“We are always honored to be recognized among the top nursing programs, and for our master’s programs to be named the best in the nation is just a thrill,” says Dean Linda McCauley 79MN, PhD, RN, FAAN, FRCN. “This recognition provides an opportunity for the public to see what we know to be true — that our students are receiving top-notch preparation, our faculty and students are engaging in life-changing research and service alongside our partners, and our alumni are making a difference every day as visionary nurse leaders. I am incredibly proud of our entire school community.”
No. 4 AdultGerontology Acute Care (MSN)
No. 6 AdultGerontology Primary Care (DNP)
No. 4
AdultGerontology Primary Care (MSN)
No. 5 Family (DNP)
No. 6 Family (MSN)
The Fiscal Year 2022 rankings from the Blue Ridge Institute for Medical Research compare schools, departments, and all institutions across the United States on the basis of NIH funding.
The school posted the thirdhighest total among nursing schools during 2022, with approximately $15 million in research and training grants, fellowships, and other awards.

The school’s NIH-funded grants supported various research areas, including health disparities and equity, environmental health, dementia and related caregiving, HIV, chronic pain management, kidney disease, gut microbiome, machine learning, and cancer pain management.
funding
The school posted the third-highest total of NIH
during 2022.
The School of Nursing has launched a Master in Cardiovascular Perfusion Science program.
A cardiovascular perfusionist is responsible for operating cardiopulmonary bypass or support machines used for the temporary replacement of heart and/or lung function. With more than 340,000 coronary artery bypass surgeries performed annually, perfusionists are in high demand.
A perfusionist is a member of an interprofessional health care team who works in an operating room environment. Perfusionists provide mechanical support using extracorporeal membrane oxygenation (ECMO), blood transfusion devices, intra-aortic balloon pumps, ventricular-assist devices, and more.

Emory’s cardiovascular perfusion program is designed for individuals with a bachelor’s degree in a
science or health-related discipline. It is a full-time, five-semester program that includes classroom, laboratory, simulation, and clinical experiences at sites largely in the Atlanta area. Students will complete simulated learning experiences at the school’s new Emory Nursing Learning Center.
Program graduates will be prepared to enter the field as competent perfusionists and will be eligible to sit for the American Board of Cardiovascular Perfusion certification examination.
The program is currently under review by the Southern Association of Colleges and Schools Commission on Colleges. Pending review approval, the inaugural cohort will begin in Fall 2023.
The Oncology Nursing Society (ONS) has announced that Eun-Ok Im, PhD, MPH, RN, CNS, FAAN, is the 2023 recipient of its Distinguished Researcher Award. Im is a professor and Edith Folsom Honeycutt Endowed Chair at the School of Nursing.


The award recognizes an ONS member with a sustained program of substantive research that advances the delivery of quality cancer care by nurses and contributes to the cancer community at large.
Im’s research involves the adoption of Internet and computer technologies to examine gender and ethnic disparities in the health and illness experience of midlife women, including those with cancer. Over the years, she has obtained approximately $20 million in funding for oncology and other areas of women’s health research, including five National Institutes of Health R01 grants.
School of Nursing faculty and Atlanta-area colleagues are seeking answers to issues affecting the health of farmworkers and Black expectant and birthing women, bringing in a combined $5.86 million in grant funding for the research projects.
School of Nursing professor Vicki Hertzberg, PhD, FASA, and assistant professor Roxana Chicas 16BSN 20PhD were among a group of Emory and Georgia Tech researchers receiving a $2.46 million grant from the National Institute of Environmental Health Sciences to develop a multi-sensor biopatch for farmworkers that can predict symptoms of heat-related illness.
Hertzberg is a principal investigator on the four-year grant, which will allow the team to develop a wearable wireless unit for farmworkers with sensors that can predict adverse heat-related medical events and generate warnings about them in real time. The Farmworker Association of Florida is also part of the grant.
The National Institute of Nursing Research awarded a $3.4 million grant for Morehouse School of Medicine and Emory nursing and medicine researchers to study the impact of the integration of community-based, perinatal patient navigation into the continuum of maternal care for Black women in a safety-net health system.

The R01 Research Project provides funding for five years to conduct a randomized controlled trial of the patient navigation intervention to discern its effectiveness in reducing maternal morbidities and mortality and improving unmet social needs, health care utilization, and timeliness of care.
Using equity-focused research frameworks, the multidisciplinary team will evaluate maternal health outcomes and implement a high-fidelity care model intervention.
Rasheeta Chandler, PhD, RN, FNP-BC, FAANP, FAAN, associate professor with the School of Nursing, is among the researchers working on the grant.

The Emory Nursing Learning Center is home to the world’s first commercial installation of HAL® S5301, an advanced interdisciplinary patient simulator with artificial intelligence capabilities.
Made by Gaumard Scientific Co., the school’s HAL S5301 — known as “Emory HAL” — features AI-enhanced conversational speech, lifelike motor movement, and next-generation simulated physiology that allows HAL to simulate stroke symptoms and other medical conditions.

By using HAL, educators can facilitate true-to-life clinical training experiences in the areas of emergency, trauma, ICU, and med-surg care.
“HAL represents the new generation of technology that will be used to educate and empower tomorrow’s nursing and medical graduates with an unprecedented level of real-world skill, confidence, and preparation,” noted John Eggert, Gaumard’s executive vice president.
Three faculty members brought home awards from the Southern Nursing Research Society annual conference, held in March in Orlando.
Assistant professor Glenna Brewster, PhD, RN, FNP-BC, received the Research in Health Disparities Award, given to an individual or group conducting research that has significance for improving the health care of minorities and other underrepresented groups.


Associate professor Christina Calamaro, PhD, CPNP-BC, FAANP, received the Clinical Researcher Award, recognizing an individual working in a clinical setting for more than half of their appointment whose research has enhanced the science and practice of nursing. Calamaro also directs research and evidence-based practice at Children’s Healthcare of Atlanta.
Assistant professor Nicholas Giordano, PhD, RN, received the Early Science Investigator Award, acknowledging the contributions of a nurse scientist in early career stages who shows potential to develop a sustained program of research to enhance nursing science and practice.

Numerous faculty and students shared their research during workshops, poster sessions, and roundtable discussions throughout the conference, which focused on the topic of building partnerships in population health through research, education, and practice.

The School of Nursing has appointed two of its faculty members to serve in significant endowed chair positions.
Beth Ann Swan, PhD, RN, FAAN, has been named the Charles F. and Peggy Evans Endowed Distinguished Professor in Simulation and Innovation.
The professorship was made possible by a bequest to the school in 2003 by the late Charles F. Evans and his wife, Peggy. This new chair underscores Emory’s commitment to developing research and technologies to enhance nursing education and patient care.
Swan is associate dean and vice president for academic practice partnerships at the School of Nursing. She is the primary investigator for two recent Health Resources and Services Administration grants and a contributor on additional grants. Her publications focus on primary and ambulatory care, innovations for education and practice, and health care policy.
Xiao Hu, PhD, has been appointed as the Asa Griggs Candler Chair of Nursing Data Science.
The Asa Griggs Candler professorships help recruit and retain senior faculty members at Emory across all disciplines. The professorships are named for Candler, founder of The Coca-Cola Company and a key Emory benefactor and trustee leader.

Hu is known for his scholarship in machine learning, artificial intelligence, and predictive analytics monitoring. His research has contributed to neurological monitoring for acute brain injuries, noninvasive intracranial pressure, and precise patient monitoring with few false alarms. He has served as principal investigator on multiple grants including four National Institutes of Health-funded R01 awards.

“One
Rose B. Cannon 74MN, 95PhD Professor Emeritus, School of Nursing — 1836 Legacy Society Member
As a graduate of the Nell Hodgson Woodruff School of Nursing, you are an experienced health care professional who makes a difference in the lives of others. You also have a chance to make a difference in another way — by participating in our network of more than 10,000 Emory Nurses around the globe.
The Emory Nurses’ Alumni Association has many opportunities for you to be involved in the School of Nursing throughout the year:

• Serve as an alumni mentor
• Join the Nurses’ Alumni Association board
• Write welcome notes to admitted students
• Serve as a preceptor
• Host a social activity for students and/or alumni
• Help new graduates moving to your city network
• Serve as a class representative or a class reunion volunteer
• Participate in a service project
• Serve as a panelist or guest lecturer
• Give financially to the School of Nursing
• Attend an alumni event
As you can see, there are many ways to stay connected with the School of Nursing long after you have graduated. And as you do, you will find the joy of camaraderie and the satisfaction that your efforts will encourage future generations of nursing leaders. If you want more information about how to be involved, please visit nursing.emory.edu/alumni-and-giving.
Kay Bohanan Kennedy 80Ox 82BSN 90MN President, Emory Nurses’ Alumni Association
The opioid crisis is just that — a crisis, with increasing illnesses and deaths and ripple effects that touch every sector of our communities.
Few people are more aware of that reality — and more determined to combat it — than Andy Gish 06BSN, RN, CEN.
Gish is an award-winning BoardCertified Emergency Nurse, overdose prevention educator, and legal nurse consultant. She teaches overdose prevention and harm reduction to health care staff, students, community groups, and universities.

A longtime advocate for opioid overdose prevention education, she practices compassionate, open-minded care to destigmatize this marginalized and ever-growing population. She is a registered nurse at the Addiction Alliance of Georgia, a partnership between Emory Healthcare and the Hazelden Betty

Ford Foundation. She also volunteers with Georgia Overdose Prevention and the Atlanta Harm Reduction Coalition, serving as a community distributor and educator on naloxone. Also known as Narcan, naloxone is an FDA-approved medication that can rapidly reverse an opioid overdose.
Gish was influential in the passage of Georgia’s Medical Amnesty Law “Don’t Run, Call 911,” which expands access to Narcan and provides limited immunity from arrest and prosecution for individuals seeking medical help for themselves or others for a drug overdose. She testified before lawmakers in support of legislation that put Georgia ahead of most states in addressing the opioid crisis.
Gish has been recognized by The Atlanta Journal-Constitution as one of the top 10 nurses in Georgia, and she received the Commander’s Coin from the U.S. Public Health Service for her work.
The School of Nursing held its Homecoming Weekend in October, culminating with a Homecoming Awards Celebration at the Druid Hills Golf Club in Atlanta that honored alumni, faculty, and friends.

The honorees included:
Award of Honor — Carolyn Clevenger 02MSN 04N 14N
Carolyn Clevenger, DNP, RN, GNP-BC, AGPCNP-BC, FAANP, FGSA, is a professor at the School of Nursing and a gerontological nurse practitioner. She is the co-creator and clinical director of the Integrated Memory Care Clinic, a nurse-led clinic practice that fully integrates dementia and primary care.
Distinguished Nursing Achievement Award — Tim Cunningham
October 20-22, 2023
For more information:
Chelsea Shackelford, Director of Alumni
cmshack@emory.edu
Tim Cunningham, DrPH, MSN, RN, FAAN, is vice president of practice and innovation at Emory Healthcare and adjunct associate professor at the School of Nursing. He also serves as the co-chief well-being officer for the Woodruff Health Sciences Center Office of Well-Being.
Distinguished Nursing Achievement Award — Mary Gullatte 81MN 95N
Mary Gullatte, PhD, RN, ANP-BC, AOCN, LSSYB, FAAN, is the corporate director of nursing research and evidence-based practice for Emory Healthcare and former vice president of patient services and chief nursing
officer at Emory University Hospital Midtown. She also holds an adjunct faculty position at the School of Nursing.
Excellence in Nursing Award — Erica Ailes 07BSN
Erica Ailes, BSN, RN, CPN, is a clinical learning coordinator at Children’s Healthcare of Atlanta and a national leader in the field of health literacy.
Honorary Alumni Award — Roy Simpson
Roy Simpson, DNP, RN, DPNAP, FAAN, FACMI, is a professor at the School of Nursing and has more than 30 years of experience in nursing informatics and senior executive administration.
Recent Graduate Award — Chelsea Hagopian 12BSN 14MSN 18DNP
Chelsea Hagopian, DNP, APRN, AGACNP-BC, is an assistant professor at the School of Nursing and an American Nurses Credentialing Center boardcertified adult-gerontology acute care nurse practitioner.
The evening also included a recognition of School of Nursing alumni who are
celebrating 30 or more years of service with Emory Healthcare:
Kara (Kwint) Botters 98MSN — Cardiology/EKG, The Emory Clinic
Laura Brannon 99MSN — Kidney Transplant Center, Emory Healthcare
Dorothy Ann Ferguson 08MSN — Orthopaedics, Emory Saint Joseph’s Hospital
Jacqueline Francis 95MSN — Special Care Nursery, Emory University Hospital Midtown
Diana Harmon 19N — Emory Decatur Hospital
Angela Murphy 92MN (retired) — Cardiology Department, Emory University Hospital
Mary K. Potter 97MSN — Hematology and Medical Oncology, The Emory Clinic
Diane Teagarden 97MSN 23N — Neurology and Epilepsy Center, The Emory Clinic
Terry (Taylly) Walker 11N — Cardiovascular Intensive Care Unit, Emory Critical Care Center
The School of Nursing is grateful for the work of the Nurses’ Alumni Association, which seeks to strengthen relationships among alumni worldwide, provide lifelong learning and leadership opportunities for alumni, and advance nursing practice, education, and service.

The association’s board is key to these efforts, working collaboratively with the Office of Advancement and Alumni Engagement to develop programs that engage alumni and support the mission of the school. We thank the following individuals for their tireless work:
President
Kay Kennedy 80Ox 82BSN 90MN
President-Elect
Donté Flanagan 04Ox 06BSN
Emory Alumni Board
Representative and Development and Annual Giving Committee Chair
Kay Lawton 78BSN 84MN
Diversity, Equity, and Inclusion Committee Chair
Beverly Quirós 15BSN 18MSN 19N
Immediate Past President and Nominations and Awards Committee Chair
Cheryl Murphy 77BSN
NAA Communications Task Force
Chelsea Hagopian 12BSN 14MSN 18DNP
Recent Graduate Committee Co-Chairs
Alexis Perkins 20BSN and Madeline Williford 18Ox 20BSN
Student-to-Alumni Committee Chair
Colleen Closson 18BSN
Amy Berk 01MSN
Rose Cannon 74MN 95G
Colleen Closson 18BSN
Taryn Connelly 17BSN
Betty Daniels 51BSN 67MN (emeritus member)
Latronda Davis 16BSN
Donté Flanagan 04Ox 06BSN
Chelsea Hagopian 12BSN 14MSN 18DNP
Leslie Jeter 17DNP
Kay Kennedy 80Ox 82BSN 90MSN
Kathryn Martel 19BSN
Maggie McMahon 19BSN
Angela Murphy 92MN
Maggie O’Mahoney 22BSN
Alexis Perkins 20BSN
Beverly Quirós 15BSN 18MSN 19N
Barbara Reed 57BSN 79MN (emeritus member)
Betty Marie Stewart 52BSN (emeritus member)
Olga Turner 18DNP
Madeline Williford 18Ox 20BSN
Sarah Woodmansee 17Ox 19BSN
The association board welcomes the involvement of alumni in this work. To learn more about the application process to serve as a board member, contact Chelsea Shackelford at cmshack@emory.edu.



As a community member, practicing nurse, and the well-known mother of a U.S. president, Lillian Carter worked to prioritize public health and social justice. A force for good, she was the namesake — and inspiration — for the creation of the Lillian Carter Center for Global Health & Social Responsibility, which seeks to improve health for vulnerable individuals and communities through nursing education, research, practice, and policy. The center celebrated its 20th anniversary in October, featuring remarks by Miss Lillian’s greatgrandson, Josh Carter, and a myriad of participating faculty members, students, and community partners. The event also included reflections by Steven Ullman, who produced a recent documentary about Lillian Carter.
“The Lillian Carter Center has been a true partner in helping us assess and support the health-related needs of our community,” said Yolanda Pawar of the One Eleuthera Foundation, Rock Sound, Bahamas, who spoke at the event via video. “In the process, we have forged so many meaningful friendships and a deeper cultural appreciation that has brought joy, curiosity, and purpose to our work.”
The Lillian Carter Center provides students opportunities to deliver care in domestic and international settings, supports students with an interest in socially responsible health care, invites international scholars to engage in health research at Emory, and serves as a hub for Health Resources and Services Administration research grants improving health in under-resourced communities.
kyle. hines@emory.edu
Beth Geisler Singel 96BSN was appointed team leader of neurosurgery at Children’s Health Dallas in Texas.
Debra R. Meadows 99MSN is a legal nurse consultant at Hall Booth Smith Law Firm in Atlanta. She also serves on MARTA’s Riders’ Advisory Council for 2022–2024.
Kathleen M. Kearney 06MSN is an associate professor at Texas Tech University Health Sciences Center School of Nursing and secretary of The American Association of Nurse Attorneys Foundation Board of Trustees. A board-certified nurse educator and primary
10,000
care pediatric nurse practitioner, she represents people who are severely injured in the state of Texas.
April Le 20N 21MSN is a nurse practitioner at Palo Alto Medical Foundation in California.
Bryanna Marshall 21MN was featured in the Atlanta Business Chronicle as one of Inno Under 25, which recognizes young innovators. Marshall is CEO
and founder of Carit, which supports mothers through every stage of pregnancy and postpartum. The startup connects mothers to licensed mental, physical, and community health specialists.
Sophie Ahn 22BSN is a registered nurse in the surgical ICU at MedStar Georgetown University Hospital in Washington, D.C. Ahn was also named Rookie of the Year during her first year as a newto-practice nurse.

Please send your news and latest contact information to alumni@nursing.emory.edu or visit engage.emory.edu/ updateinfo.
ALUMNI
In December, 310 students crossed the stage at graduation — marking an important moment in their lives and the life of the school. With their graduation, the school now has more than 10,250 alumni, pushing it over the 10,000 mark for the first time.
Your support is essential to prepare visionary nurse leaders and positively impact our research and service efforts. Make a gift today.

Virginia Corley Freeman 48BSN of Sylvania, Georgia, October 22, 2022.
Caroline Clements Rael 51BSN 67MN of Corrales, New Mexico, September 9, 2022.
Anna J. Allen 52BSN of Morristown, Tennessee, November 26, 2022.
Sara H. Harrington 52BSN of Homewood, Illinois, October 25, 2022.
Carol Northcutt Worley 53BSN of Marietta, Georgia, December 2, 2021.

Joann Walter Richardson 54BSN of Jupiter, Florida, August 18, 2022.
Melissa Hood DeVane 56BSN of Shelby, North Carolina, January 13, 2023.
Marian Henderson Leslie 56BSN of Madison, Georgia, January 22, 2023.
Diane Friedrich VanderKraats 62BSN of Venice, Florida, September 17, 2022.
Marsh Goodyear Green 64BSN of Atlanta, Georgia, November 18, 2022.
Jane Boyce Caroll 65MN of Lancaster, South Carolina, November 5, 2022.
Julia Garner 65BSN 66MN of Atlanta, Georgia, January 15, 2023.
Naomi Doris Bechtold 70MN of Lancaster, Pennsylvania, December 4, 2022.
Judith Aycock Jamison 70Ox 74BSN of Jacksonville, Florida, September 19, 2022.
Karen Louise Weber-Mullican 78BSN of Decatur, Georgia, August 10, 2022.
Margaret Lois Wood 85MN 93MN of Cleveland, Georgia, December 28, 2022.
Michael Tanner 92MN of Villa Rica, Georgia, February 2, 2023.
Julie Elizabeth Boyd 06MSN of Cookeville, Tennessee, September 8, 2022.
Persephanie Re’al Shepperson 15BSN of Kennesaw, Georgia, December 12, 2022.



The community is where much of care happens. As nurses, we have a responsibility to be part of the solution of making sure every individual has access to care. The funding from HRSA bolsters our efforts in preparing future nurse leaders to serve people in the communities where they live.
 LINDA MCCAULEY, DEAN EMORY SCHOOL OF NURSING
LINDA MCCAULEY, DEAN EMORY SCHOOL OF NURSING