Potential warning signs for breast cancer

What to know about prophylactic mastectomy
Movember shines a light on various men’s health issues




Breast cancer is the most commonly occurring cancer in women across the globe. According to the World Cancer Research Fund International, there more than 2.26 million new cases of breast cancer in women in 2020. Such figures are sobering, but it’s important to recognize that breast cancer survival rates have improved dramatically in recent decades, providing hope to the millions of women who may be diag nosed with the disease in the years to come.
Various factors have helped to im prove breast cancer survival rates, and education about the disease is cer tainly among them. Women are their own greatest allies against breast can cer, and learning to spot its signs and symptoms is a great first step in the fight against this potentially deadly, yet treatable disease.
The American Cancer Society urges women to take note of how their breasts
normally look and feel. That knowledge is vital because it helps women recog nize when something does not look or feel good to the touch with their breasts.
Screening alone may not be sufficient, as the ACS notes that mammograms do not find every breast cancer.

When women are well acquainted with how their breasts look and feel, they’re in better position to recognize any abnormalities, which may or may not be indicative of breast cancer. The ACS reports that the following are some potential warning signs of breast cancer.
✦ A NEW LUMP OR MASS: The ACS indicates that this is the most com mon symptom of breast cancer. A lump or mass that is cancerous is often painless, but hard and has irregular edges. However, lumps caused by breast cancer also can be soft, round and tender. Some even cause pain.
✦ SWELLING : Some women experience swelling of all or part of a breast even if they don’t detect a lump.
✦ DIMPLING: The skin on the breast may dimple. When this occurs, the skin on the breast sometimes mim ics the look of an orange peel.
✦ PAIN : Pain on the breast or nipple could indicate breast cancer.
✦ RETRACTION: Some women with breast cancer experience retraction, which occurs when the nipple turns inward.
✦ SKIN ABNORMALITIES: Breast cancer may cause the skin on the breast to redden, dry out, flake, or thicken.
✦ SWOLLEN LYMPH NODES: Some women with breast cancer experi ence swelling of the lymph nodes under the arm or near the collar bone.
The presence of any of these symp toms merits a trip to the doctor. Wom en with these symptoms should not immediately assume they have breast cancer, as the ACS notes that various symptoms of breast cancer also are in dicative of non-cancerous conditions that affect the breasts. Only a physician can diagnose breast cancer, which un derscores the importance of reporting symptoms to a doctor immediately.
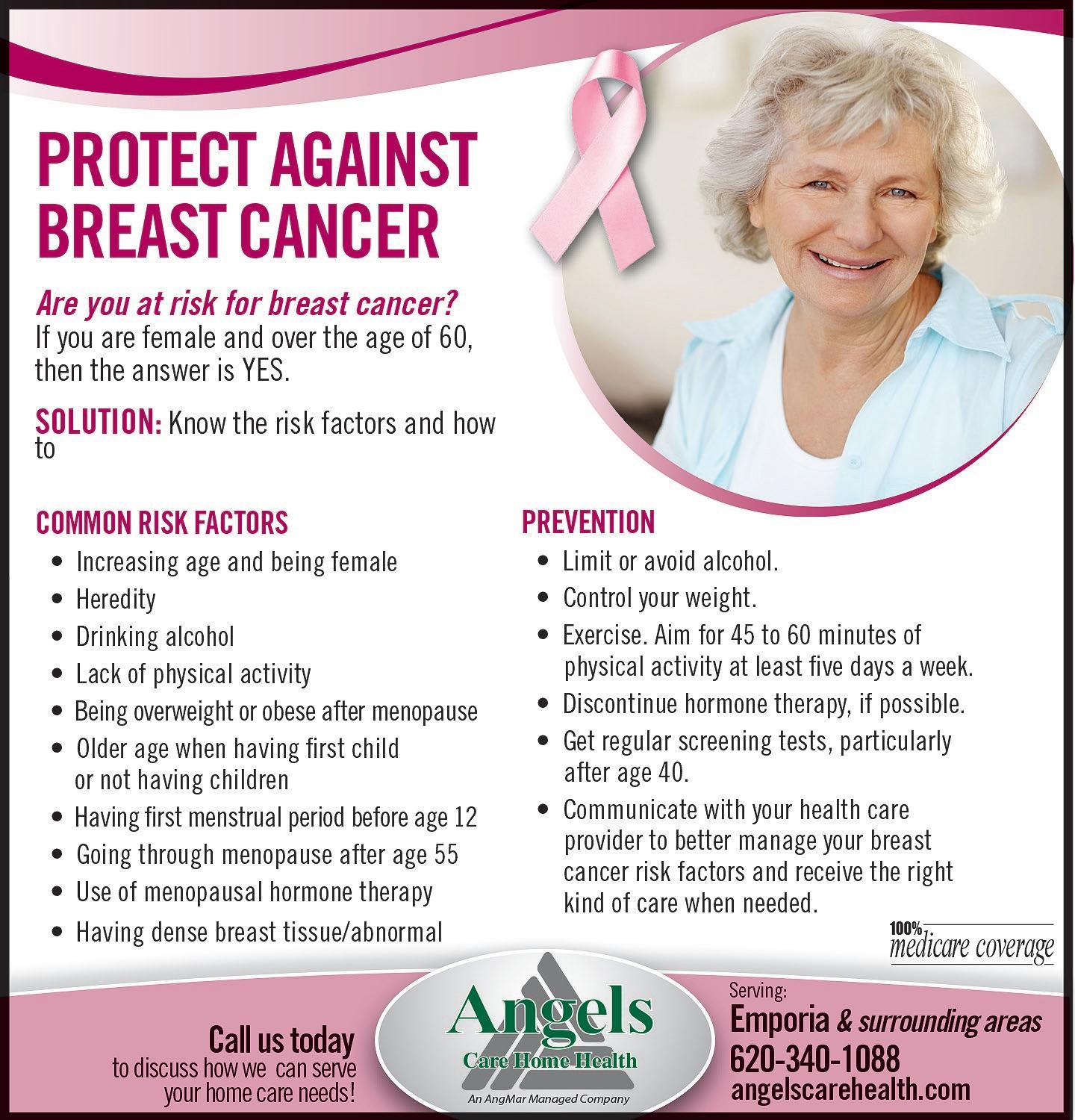
Many women are concerned about the potential for developing breast cancer in their lifetimes. Breast cancer is the secondmost common cancer among women in the United States and Canada. Despite that prevalence, there are ways for women to re duce their risk for breast cancer.
While it is impossible to change family history or genetic markers like gene muta tions that increase breast cancer risk, the following are seven ways women can lower their risk.
1. Exercise regularly and maintain a healthy weight. Physical activity and moni toring calories can keep weight in check. The Mayo Clinic recommends at least 150 minutes per week of moderate aerobic ac tivity or 75 minutes per week of vigorous aerobic activity. Strength training at least
twice a week also is recommended. Being overweight or obese increases a woman’s risk for breast cancer.
2. Consume a healthy diet. The link between diet and breast cancer risk is still

being studied. However, research suggests that a diet high in vegetables and fruit, and calcium-rich dairy products, but low in red and processed meats may lower breast can cer risk.
3. Avoid or limit alcohol consumptions. Alcohol increases risk of breast cancer, even in small amounts. For those who drink, no more than one alcoholic drink a day should be the limit. The more a woman drinks, the greater her risk of developing breast cancer, states the Mayo Clinic.
4. Undergo genetic counseling and test ing. Women concerned about a genetic con nection or family history of breast cancer can speak to their doctor about testing and counseling that could help them reduce their risk. Preventive medicines and sur geries might help those at elevated risk for
breast cancer.
5. Limit hormone therapy. Combination hormone replacement therapy for postmenopausal women may increase risk of breast cancer, indicates the Centers for Dis ease Control and Prevention. Similarly, tak ing oral contraceptives during reproductive years may increase risk. Women can speak with their physicians to weigh the pros and cons of taking such hormones.
6. Breastfeed children, if possible. Breastfeeding has been linked to reducing a woman’s risk of developing breast cancer.
7. Learn to detect breast cancer. Women should get to know their bodies so they can determine if something is awry as early as possible. Early detection of breast cancer increases the chances that treatment will prove successful.
Breast cancer is the most common cancer diagnosed in American women, and is the leading cause of cancer death in less developed countries, says the Breast Cancer Research Foundation. Ac cording to Susan G. Komen, more than 680,000 breast cancer deaths occurred worldwide in 2020.
Breast cancer affects the anatomy of the breasts and can often spread to the lymph nodes. While breast cancer can affect just about any woman (as well as men), certain women are at higher risk for developing breast cancer than others. Such women include those with a family history of breast cancer and/or the pres ence of genetic markers called BRCA1 or BRCA2 gene mutations, according to the Bedford Breast Institute. Those women have a lifetime risk of up to 87 percent for getting breast cancer and 53 percent for developing ovarian cancer. Other risk factors include the presence of dense breast tissue, exposure to radiation at an early age and having already had cancer in one breast.
In instances when breast cancer risk is particularly high, women may opt to undergo prophylactic mastectomy, also called preventative mastectomy. This is the surgical removal of one or both breasts with the intent to dramatically
reduce the risk of developing breast can cer.
The Mayo Clinic says prophylactic mastectomy reduces the risk of devel oping breast cancer by 90 to 95 percent among women with BRCA gene muta tions. It is roughly the same risk reduc tion for women who already have had breast cancer or have a strong family his tory of the disease and then have a breast removed.
Studies indicate that preventative mas tectomy of the unaffected breast (called contralateral prophylactic mastectomy) in cases when breast cancer occurred in the other breast, when no genetic muta tions or hereditary risk factors are pres ent, has little to no effect on overall sur vival rate. This is a surgery only for those with very high risk.
Not all breast tissue can be removed during a prophylactic mastectomy. That is because breast tissue can sometimes be found in the chest, armpit, skin, above the collarbone, or on the upper part of the abdominal wall, states the Mayo Clinic. It is impossible to remove all breast tissue cells during surgery. Although risk reduc tion is significant after mastectomy, that risk cannot be eliminated entirely.
There are some risks associated with prophylactic mastectomy, both during the procedure and afterwards. BreastCancer. org says bleeding or infection, fluid collect ing under the scar, delayed wound healing, scar tissue formation, loss of sensation in the chest, and complications while be ing put under anesthesia are all possible. Women are urged to carefully consider the pros and cons before opting for the surgery.
Prophylactic mastectomy is only one option for women at high risk for devel
oping breast cancer. Some alternatives include:
✦
Ultrasounds, physical exams, and mammograms every three to six months for the rest of the patient’s life.
✦ Medication that can reduce risk of de veloping breast cancer.
✦ MRIs in addition to mammograms.
✦ Surgery to remove the ovaries, which can decrease both the risk of breast and ovarian cancers. It may reduce breast cancer risk by up to 50 percent if performed before age 50.
Breast cancer risk is higher in some in dividuals, which may prompt discussions about prophylactic mastectomies.

No one is immune to breast cancer. Even men can be diagnosed with breast cancer, though the threat of the disease looms much larger for women. In fact, the World Cancer Research Fund International reports that breast cancer is the most commonly occurring cancer in women across the globe. However, the World Health Or ganization indicates that, as of the end of 2020, roughly 7.8 million women who had been diagnosed with breast cancer in the previous five years were alive. So while no woman wants to receive a breast cancer diagnosis, mil lions of women worldwide are living testaments to the effectivenesss of treatments for the disease.
There are various things women can do to increase their chances of surviving a breast cancer diagnosis. Recognizing one’s own risk of developing the disease is especially important, as it may compel women to pri oritize screening and make changes that could reduce their cancer risk.
There are many risk factors for breast cancer, and ethnicity is one of them. Data from the National Cancer Institute and the American Cancer Society indicates that breast cancer rates and survival rates differ among
ethnic groups. Though the relationship between ethnic ity and breast cancer is complicated and intertwined with other risk factors, data from the NCI and ACS indi cates that incidence and death rates are higher among certain ethnic groups than others.
Highest incidence rate: White, non-Hispanic
Lowest incidence rate: Korean American
Highest death rate: African American
Lowest death rate: Chinese American
The MD Anderson Cancer Center notes that socio economic factors such as education and income level and access to medical screening and services undoubt edly affect incidence and death rates among different ethnicities. But other factors, such as cultural practices and beliefs within certain ethnic groups, also affect those rates. Women concerned about breast cancer are urged to prioritize screening for the disease and dis cuss factors such as diet, physical activity and cultural practices to determine if there’s anything they can do to lower their cancer risk.
According to the American Cancer Society, breast cancer mainly occurs in middle-aged or older women. In fact, the median age at the time of a breast can cer diagnosis is 62. Though it’s possible for women far younger than 62 to be diagnosed with breast can cer, the ACS reports that only a very small number of women younger than 45 are diagnosed with the disease each year. Despite the average age of onset being over 60, breast cancer is highly treatable. The World Health Organization notes that breast cancer treatments routinely achieve survival probabilities of 90 percent or higher. However, those probabilities de cline considerably in lower-income countries where access to screening and other medical services is limit ed. For example, the WHO notes that five-year surviv al rates for breast cancer routinely surpass 90 percent in high-income countries like the United States and Canada. However, those rates are as low as 40 percent in South Africa, where early detection of the disease is less likely than it is in wealthier nations. That disparity in survival rates underscores the need for greater re source allocation in lower-income countries, but also highlights the effectiveness of screening and other measures in high-income countries where women are taught to report any abnormalities with their breasts.

Started in Melbourne, Australia, by two friends nearly 20 years ago, Movem ber® has become a global, mustachioed phenomenon that has since helped to fund more than 1,250 men’s health projects.

Each November, men across the globe agree to grow a moustache in an effort to raise awareness about men’s health is sues. Dubbed Movember®, this annual ef fort is the brainchild of two friends, Travis Garone and Luke Slattery, who had been joking about how to bring moustaches back into fashion. The two men were in spired to tie their efforts into a campaign to raise awareness about men’s health by the mother of a friend who, at the time, was raising funds for breast cancer.
Since its inception, Movember® has helped raise awareness about three par ticular issues, prostate cancer, testicu lar cancer and men’s suicide, that might
otherwise have garnered considerably less attention. Taking time to understand these issues can help make Movember® an even greater success than it already is.
The World Cancer Research Fund In ternational reports that prostate cancer is the second most commonly occurring cancer in men and the fourth most com mon cancer overall. In fact, more than 1.4 million men across the globe are di agnosed with prostate cancer each year. Education about prostate cancer can in
clude an emphasis on the factors and be haviors that increase a man’s risk for the disease, which the WCRFI indicates in clude height (being tall increases a man’s risk) and weight (being overweight and obese also increases risk).
The American Cancer Society reports that the average age at the time of diagno sis of testicular cancer is about 33, which underscores the notion that no man is too young to learn about men’s health is sues. Though testicular cancer is not as prevalent as prostate cancer, the Ameri can Society of Clinical Oncology notes that diagnoses of the disease have been on the rise for decades. The reasons for that are unknown, but lack of awareness of the disease and what can be done to
detect it early could be contributors to the increase.
The American Foundation for Suicide Prevention reports that suicide is the 12th leading cause of death in the Unit ed States. The rate of suicide is highest among middle-aged white men, and in 2020 men died by suicide at a rate nearly four times higher than women. Globally, the Institute for Health Metrics and Eval uation reports that suicide rates in men are just over twice as high as those for women. A greater awareness of suicide, including how much more prevalent it is among men than women, could help prevent more suicides. More information about suicide prevention is available at afsp.org.
Data from the World Cancer Research Fund International indicates that more than 2.2 mil lion people were diag nosed with lung cancer in 2020. That makes lung cancer the second most common cancer worldwide.
The prevalence of lung cancer underscores how important it can be to learn about the dis ease. Many incidents of lung cancer can be pre vented, and some basic knowledge of the dis ease could potentially go a long way toward reducing diagnoses.
Lung cancer is any cancer that begins in the lungs. The American Cancer Society notes that the lungs are two sponge-like organs in the chest. When people breathe air in, it enters through their mouth or nose and goes into the lungs through the tra chea. The trachea divides into tubes called bronchi, which enter the lungs and divide into smaller bronchi. Lung cancers typically start in the cells lining the bronchi or small
er branches of the bronchi known as bronchioles. Lung cancers also may start in the alveoli, which are tiny air sacs at the end of the bronchioles.
How many types of lung cancer are there?
The Lung Cancer Founda tion of America notes that the term “lung cancer” refers to a group of diseases defined by which type of lung tissue the abnormal cells originated in. In order to develop a treat ment plan, physicians must first identify which type of lung cancer a person has, and the LCFA indicates there are two main types of the disease:
Non-small cell lung cancer (NSCLC)
Small cell lung cancer
The ACS reports that between 80 and 85 percent of lung cancers are NSCLC. SCLC is much less common, affecting around 10 percent of all people diagnosed with lung cancer.

It’s a misconception that all lung cancers can be prevented. Though many incidents
of lung cancer are tied to lifestyle choices, not all cases can be prevented. And even people who make healthy lifestyle choices can still get the disease. However, the ACS notes that there are many things people can do to lower their risk for the disease.
AVOID TOBACCO: The ACS indicates that avoiding tobacco is the best way to reduce lung cancer risk. Not smoking at all and avoiding breathing in other people’s smoke can greatly reduce your risk for lung cancer. Even current smokers can reduce their risk by quitting immediately, especially if cancer has not yet begun to develop in their lungs.
AVOID RADON: Radon is a colorless, odor less and radioactive gas that occurs natural ly in soil and rock throughout the world. Ac cording to the ACS, most exposure to radon occurs indoors, and long-term exposure can lead to lung cancer. Routine radon testing and immediate treatment can reduce risk for lung cancers caused by the gas.
EAT HEALTHY: The ACS indicates that some evidence supports the idea that a diet high in fruits and vegetables can help pro tect both smokers and non-smokers from lung cancer.
Many of the more than two million cases of lung cancer diagnosed each year can be prevented. More information about lung cancer can be found at lcfamerica.org.
Lung cancer is the second most common cancer worldwide. Accord ing to the World Cancer Research Fund International, lung cancer is the most common cancer in men and the second most common cancer in women. But even families affected by lung cancer may be surprised to learn that children are not immune to the disease. Though lung cancer is very rarely found in children, kids can get it. The Centers for Disease Control and Prevention report that cigarette smoking is the number one risk factor for lung cancer, which could be why the disease is so often associated with adults. However, the National Cancer Institute reports that incidences of lung cancer in children could be ge netic. According to the NCI, a specific change in the DICER1 gene increases the risk for a childhood lung cancer known as pleuropulmonary blasto ma, which forms in the tissues of the lung and pleura (the organs between the lungs). Families with a history of DICER1 syndrome, a rare, inherited disorder caused by a mutation in the DICER1 gene, are urged to speak to a physician about testing children for pleuropulmonary blastoma.

The results of two studies recently published in the British medical journal The BMJ found that eating a lot of ultra processed foods significantly increases men’s risk of colorectal cancer. Published in August 2022, the studies, which ex amined individuals in both the United States and Italy, also found that diets high in ultraprocessed foods can lead to heart disease and early death in both and men and women. Processed and ul traprocessed foods include meats such as bacon, beef jerky, corned beef, ham, hot dogs, and salami. Various organizations, including the World Health Organization, the American Cancer Society and the American Institute for Cancer Research, have previously warned that those meats are associated with a higher risk of bowel cancer in men and women. The studies published in August 2022 reported that it’s not just ultraprocessed meats that in

crease risk for cancer, but also other pro cessed or ultraprocessed foods, including ready-to-eat-or-heat foods such as french fries, prepackaged soups, sauces, frozen pizza, doughnuts, and store-bought cook ies and cakes, among others.
According to the American Cancer Society, the average age a man is diagnosed with prostate cancer is about 66. In fact, six out of every 10 prostate cancer di agnoses are in men who are 65 and older. Though prostate cancer is the second leading cause of cancer death among American men, most men diagnosed with the disease do not die from it. Screening could play a role in that, and the ACS recommends that men thinking about getting tested for prostate cancer learn as much as they can about screening so they can make the most informed decisions possible. Speaking with a personal physician about screening is recommended, as the effects of screening continue to be studied by researchers.

