THE FUTURE'S GETTING BRIGHT
When two become one
The creation of a new combined voice for the industry
Future Leaders Program
Discover






When two become one
The creation of a new combined voice for the industry
Future Leaders Program
Discover






DHAA MEMBERS RECEIVED an email in May outlining the proposed pathway for creating a new association to represent dental hygienists, dental therapists, and oral health therapists by July 2025. This significant milestone is the result of ongoing hard work by DHAA and ADOHTA representatives through the Towards One Professional Association (TOPA) project, which began in October 2019.
Throughout this project, the boards of both associations recognised our shared mission to improve oral health outcomes for the community and the importance of supporting and developing oral health practitioners. While the benefits of a unified association—such as pooled resources, stronger advocacy, improved efficiency and productivity, and enhanced member services— are widely acknowledged, we remain mindful of the challenges ahead.
The new association will ensure equitable support and development for all three professional divisions of oral health practitioners, and we are committed to protecting and enhancing member benefits across all demographics. The proposed board and team will be dedicated to delivering quality services and support, aiming to provide a strong value proposition for members.
We have received overwhelming support from members through their feedback and are excited to proceed as proposed to create the new unified association. We will be seeking member approval through a ballot in the coming months.
Thanks to the dedication of many volunteers and staff over the years, DHAA is in a sound financial position. We have kept our membership fee and PI insurance premium unchanged despite rising business costs. Additionally, the DHAA board is committed to investing in our members and our profession. The first step is building leadership capacity through the DHAA Future Leaders Program. This program aims to develop leadership skills within our profession and empower members' personal development and career growth. This prestigious program is fully funded, and I encourage you to submit your application as soon as it opens.

In parallel to the TOPA project, DHAA and ADOHTA will host our inaugural joint congress in Sydney from 17-19 October this year. This milestone event will bring together all three divisions of our profession to share, learn, and network. The program reflects the depth of expertise within each division while recognising their commonalities. This is the event of the year for every oral health practitioner, and I look forward to seeing you there in October.
A/Professor Carol Tran DHAA PresidentKey Contacts



04 Self-care matters
A new IFDH white paper identifies opportunities
06 From the top
CEO Bill Suen explains, ‘we’re with you for the long run.’
08 Ask DHAA
Your questions answered.
10 Get an online CPD fix
Enjoy learning from home.
16
Workplace wellbeing
A look at ways that can help you stay in your happy place.
COVER STORY
20 Bright futures
Discover how the DHAA is maximising opportunities with the new Future Leaders Program and the upcoming inagural joint national congress with ADOHTA .
25 Insurance assurance
PI Insurance for extended leave and retirement.
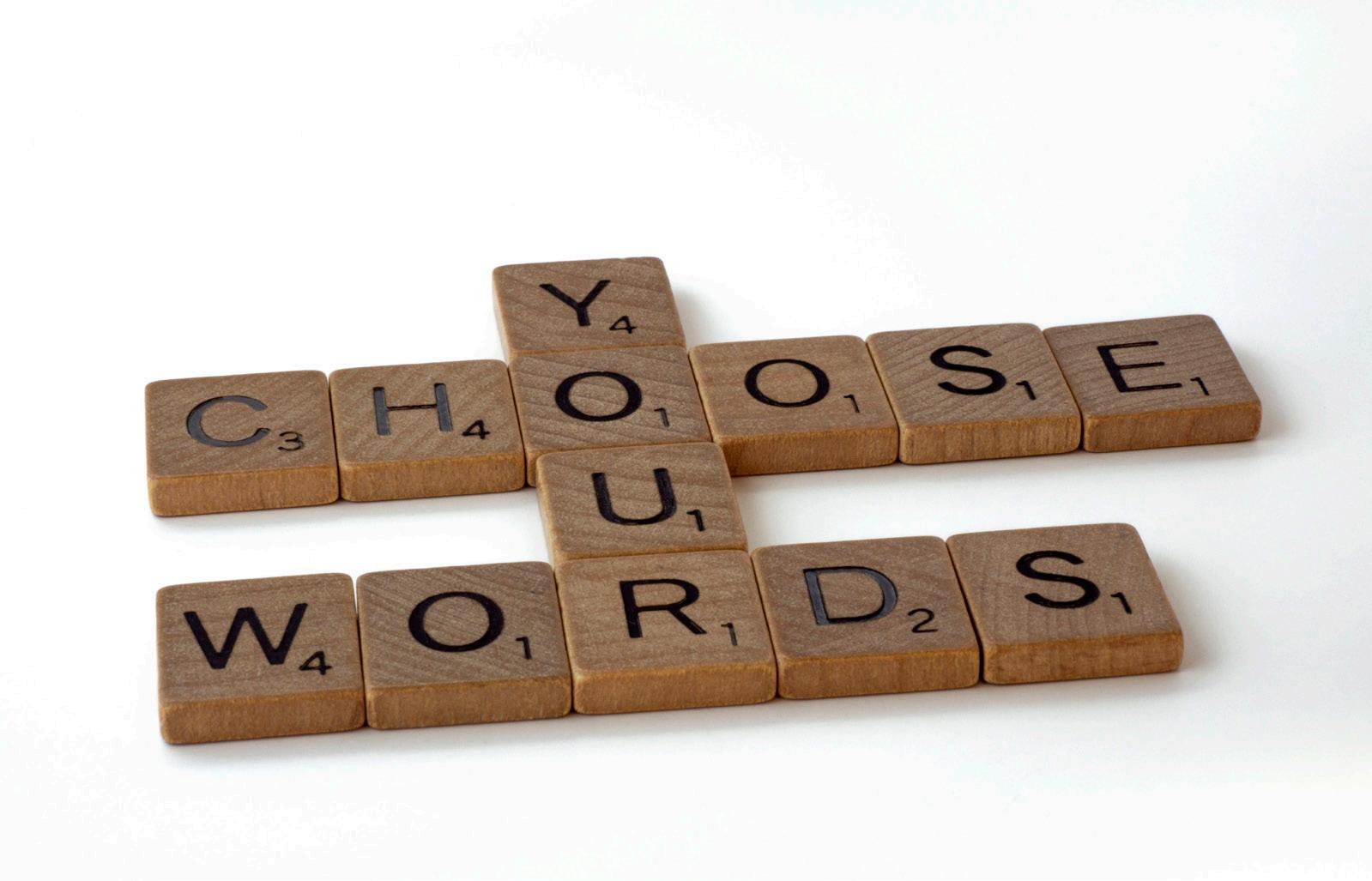
28 Mind your language
How your choice of words can impact your patients.
34 Saliva Secrets
Part two of our feature looking at dry mouth
42 State of the Nation
Our regular round-up of state happenings.
New IFDH white paper identifies opportunities and dental hygienists to make even more impactful evidence-based preventative self-care recommendations
Globally, periodontal diseases are prevalent, and the disease burden is high for both patients and for society.
The World Health Organisation (WHO) has turned its attention to the issue of prevention in a recent publication, stating that, “the primary focus of oral health professionals’ activities should therefore be on delivering evidencebased preventive care and minimally invasive interventions, supporting patients in effective self-care practices”.
The International Federation of Dental Hygienists (IFDH) has taken up the challenge by working to understand current practices in hygiene through a series of global surveys. The culmination of this work is a new IFDH White Paper titled evidence-based self-care recommendations matter: Findings from IFDH global surveys. Released in 2023, the report identifies opportunities and suggests strategies for dental hygienists to make even more impactful preventive recommendations.
The paper presents a compelling call to action, summarised here.
Staying on top of the evidence
While we aim to make evidence-based decisions, it can be hard to stay on top of the research. The white paper suggests monitoring and utilising secondary publications. Secondary publications such as systematic reviews, meta-analyses and clinical guidelines allow insights into a body of evidence. This allows clinicians to quickly understand and interpret the highest level of evidence.
Follow the evidence for home plaque control
Effective oral hygiene requires both mechanical and chemical intervention.
n Mechanical intervention
For almost two decades, the vast majority of systematic reviews and meta-analysis have confirmed the superiority of electric toothbrushes in general, and oscillating-rotating toothbrushes in particular.
ACTION: Dental clinicians can make more impactful recommendations by sharing with patients the evidence supporting the superiority of electric toothbrushes over manual, and discussing with them the evidence behind the differences between the various electric toothbrushes.
n Chemical intervention
The white paper addresses the differences between fluorides, and draws on the evidence of systematic reviews and metaanalysis to highlight stannous fluoride as delivering superior plaque biofilm inhibition and reduction in gingival bleeding. ACTION: Effective toothpaste ingredients maximise the benefits of a brushing session. For best results, clinicians can inform their patients of the difference between toothpastes, and the benefits of stannous fluoride for control of plaque and gingival bleeding.
Make recommendations with impact
The most impactful recommendations can be either intentional or experiential. Intentional recommendations are those that are tailored to the patient, and are based on strong scientific evidence. Experiential recommendations allow a patient to trial a product, either in the chair or at home. The more impactful the recommendation, the more likely the patient is to follow the advice.
Make learning continuous
Behaviour change takes time. By implementing strategies and technology, the time between appointments can lead to skill acquisition and development. Interactives tools, such as an interactive electric toothbrush and app, can train a patient to brush more thoroughly, or with the correct amount of pressure for plaque removal. Disclosing agents are another tool that can be used by a patient to measure their outcomes. Dental clinicians can also support
“The
International Federation of Dental Hygienists (IFDH) has taken up the challenge by working to understand current practices in hygiene through a series of global surveys”

patients by giving recommendations of trusted social media and websites so that patients can continue on their oral health education journey.
Conclusion
As a profession, oral health therapists and dental hygienists are specialists in health promotion and disease prevention. Uniquely, OHTs and hygienists are well positioned to meet the challenge of delivering evidencebased recommendations for daily selfcare products to control plaque biofilm.
How to get your copy
Effective recommendations help to
• Improve patients’ periodontal health
• Positively impact overall health and well-being
• Contribute to sustainable dentistry
Implementing the action points raised in the IFDH white paper will help the profession respond to the WHO Global Oral Health recommendations, and make a difference to the oral health of our community. n
Click here to download the IFDH white paper or scan QR code
Click here to download the World Health Organisation. Global oral health status report: Towards universal health coverage for oral health by 2030. World Health Organisation.

About the author
Dr Elizabeth Milford is a dentist with a passion for prevention and evidence based dentistry.
A graduate of the University of Queensland, she went on to gain a Master of Business Administration (Prof) from the Melbourne Business School. Elizabeth is an experienced consultant in dental regulatory compliance, working as an auditor and educator, approved by the Dental Board of Australia.
She has extensive experience in management of health-professional businesses and associations. She has assisted not-for-profit organisations diversify their income streams. She has also implemented strategies that respond to workforce challenges; support of new graduates, rural shortages, under-performing clinical staff. This has required an understanding of human resource and industrial relations issues.
Dr Elizabeth Milford is the Professional and Scientific Relations Consultant for Oral-B to Australia and New Zealand.
We’re
The DHAA continue to have your best interests at the top of our agenda
 Bill Suen DHAA CEO
Bill Suen DHAA CEO
TIME FLIES, AND it is end of financial year time once again. Over the next couple of months, many of us will need to gather our work-related expense documentation for our income tax return and renew various subscriptions. This is also the time when many of us take the opportunity to reflect on our financial situation, particularly in light of the current escalation of cost-of-living pressure on many fronts.
As CPD and professional indemnity insurance are mandatory requirements for Ahpra registration, the DHAA has always worked hard to ensure oral health practitioners are able to look to the DHAA for quality services at the lowest possible cost in these areas. I am pleased to inform you that there is again no fee increase this year for both the DHAA membership and professional indemnity insurance. In fact, the DHAA professional indemnity insurance premium has been around the $200 mark since its inception six years ago.
Despite common marketing ploys from businesses linking price to quality, the DHAA constantly reviews our products and services to ensure the
best quality is provided while keeping the cost down for our members. I am pleased to announce a service enhancement to our professional indemnity insurance in which members subscribed to the DHAA PI insurance are able to access clinical support advice 24/7. This is not just a support hotline; the advisor can help with: Lodging the notification report with BMS;
• Explaining the claims process so you know what to expect;
• Providing updates on the progress of the claim; and,
• Discussing the incident and offering support from a clinical perspective.
There is really no need to pay too much for your professional indemnity insurance. Further details of the DHAA PI insurance and other member services can be found here:
DHAA MEMBERS ARE provided with 20 hours of webinars per year as part of their membership, plus many more other events and online activities, as well as our flagship national symposium. Besides CPD and PI insurance, DHAA offers its members support in every aspect of their career and professional needs. Examples of some of these services are:
• Ongoing update of development and changes to oral health practice
• Networking events to meet local and national colleagues—F2F and virtual
“You should not need to manage your career alone; the DHAA connects you to people, organisations, and resources that you may require throughout your journey”
• Skills development and mentoring through various programs
• Advice on clinical and practice matters (expert panel)
• Industrial relations support and advice line
• Peer support service
• Employment and recruitment services and advice
• Business advice and business development support
• Member discounts on a wide range of products and services (including financial services, car purchases, laptops, white goods, general retail, entertainment, holidays, etc)
You should not need to deal with your career journey alone, as DHAA connects you to people, organisations, and resources that you will need throughout your career.
Current DHAA members should have received your renewal notice via email by now, and I am grateful for your ongoing support. If you are not yet a member, simply visit the DHAA website to join.Never forget, we are here to support you. n
Congratulations to Olivia Tan for being the 2023 recipient of the DHAA award for Outstanding academic achievement at the La Trobe University. Below is her reflection on her student journey:
“I am honoured to have received the DHAA Student Award.
Studying Bachelor of Oral Health Science at La Trobe University has been a journey filled with challenges and rewards. The program’s holistic approach to care has not only equipped me with technical skills but also emphasised the importance of empathy and understanding in patient interactions.
One of the toughest aspects of the program has been the rigorous coursework and clinical training, pushing me to constantly strive for excellence as a clinician. However, these challenges have been incredibly fulfilling as they have prepared me to provide comprehensive oral health care to diverse populations.
The program’s focus on holistic care has taught me to consider not just the oral health of patients but also their overall well-being. This approach has enabled me to address underlying issues that may impact oral health, leading to more effective treatment outcomes and improved patient satisfaction.
Overall, studying Bachelor of Oral Health Science at La Trobe University has been a transformative experience, shaping me into a competent and compassionate oral health professional ready to make a positive impact in the field.
I am staying in Bendigo to work part-time at an orthodontic practice and part-time in a general practice. Looking to the future, my goals are to continue learning and honing my skills especially in the new area of orthodontics and to provide strong general care using the skills learnt during my coursework and become a confident and independent clinician.”

June Sinclair sadly passed away recently aged 84 years
June Sinclair had. She was a New Zealand-trained dental nurse (therapist) that attended reunions in NZ for many years.


She trained in Adelaide at Gillies Planes to become a hygienist in 1989. Working in many general dental practices in Melbourne she continued to work until 74 years of age. She was a networker and gave back to her profession with many years on the Victorian Hygiene Association . She joined DHAA Victorian Branch in 1994. June held committee positions, ( doing beautifully handwritten secretarial notes) and attended many symposiums internationally and nationally. She deserved the honour of becoming the first life member of the DHAA and her colleagues held her in high esteem.
June never liked public speaking until in her later years. She spoke of her career to our delight at a CPD function, a high tea at the Stamford Hotel.
She loved playing bridge, exceptional card making skills and routinely catching up with friends, her church and work colleagues. The regular carrot cake for a dental practice where a birthday was happening was most appreciated from June.
“Friends are like teeth, care for the ones you want to keep.”
“I make sure every dental patient I see leaves plaque-free after my thorough debridement” she stated.
We will miss her friendship, bringing friends together and her amusing stories of a long dental career. Rest in peace, dear June. A life well lived. n
Dear DHAA... Thank you so much for providing us with such wonderful webinars. I really appreciate them! I am booked for the webinar on Wednesday night but now have to attend a work meeting. I’m loath to miss the webinar and am wondering if it will be available to watch after the event (and if so, if CPD points can still be earned watching it ). Thanks, Yes, with a few exceptions when presenters did not provide consent for recording of their presentations, most DHAA webinars are recorded and made available
a few weeks later on the DHAA webinar library for on demand viewing by members. However you will need to self record your own CPD points on your CPD log.
Dear DHAA...I am opening a dental hygiene business and would like to explore best options for insurance. Can you please help me with this or direct me to the appropriate contact? (I am insured with BMS at this stage for dental hygiene indemnity).
Great news about your new venture. The BMS offers a comprehensive

range of business related insurance, e.g. public liability ( and others) as an adjunct to your DHAA-BMS PI insurance. Please contact them to discuss your needs and they should be able to advise you and offer a package for your new business. Please contact: dhaa@bmsgroup.com or call 1800 940 762.
Dear DHAA... I graduated as an OHT without adult scope. However, I am interested in developing new skills and techniques from some CPD events so I can start doing adult treatment planning and restorations. Will my current indemnity insurance cover and protect me from learning and using this new skill and technique in the workplace?
If you are insured with us (DHAA-BMS), you are covered for all activities that fall within your scope. Anything not within your scope is not covered regardless whether you are learning or not.
The Dental Board has
indicated that no CPD can extend your scope, so you cannot treat adults in any way if you do not have adult scope. If you are keen to extend to adult scope, please enrol in a proper university adult scope extending program and in such case the education institution should cover you for relevant activities while you are learning under they wings.
Dear DHAA...Hey there! I am a member of DHAA and currently practising in rural Australia.
I am trying to find out how to establish a dental study club and wanted to know what the requirements were for it to be deemed as CPD. Is there any information that can be provided?
As a DHAA member you can access the DHAA study club materials. Please log in via the DHAA member portal. Go to ‘events and CPD’ and select ‘resources’ and you will find a button to the ’study club”. There are instructions and kits for six topics, all clinical CPD.

Dear DHAA... Hi there, I’m looking at purchasing a portable unit to get me started in mobile hygiene services. Does this equipment have requirements for Australian TGA approval if, for example, it is coming directly from China or somewhere overseas? Could you please let me know what protocols I need to adhere to in order for me to purchase overseas equipment? All dental /medical devices need to be TGA approved to be used with patients. Generally the distributor can show you a TGA certificate or will advise as TGA approved. I would advise to ensure all equipments used with patients are TGA approved.
Dear DHAA...We are thinking of hiring a hygienist with 15 years of experience. What is the suitable level for her in terms of award rate? Great to hear that you’re hiring and accounting for the correct award level. When doing so, please note the following important points regarding award rates:
1. It only lists MINIMUM wage rate and working conditions, not the benchmark. We know that the vast majority of our peers receive well above what the award stipulates .
2. Award rate setting is based on responsibility and not years of experience - however, we do expect practitioners with more experience and skills
usually undertake jobs with more complex responsibilities.
Please refer to the Health Professionals and Support Services Award 2020. In doing so, you will notice that Section 17 outlines the pay rates of all levels of health professionals covered by the award.
Schedule A.2 provides definitions all levels of health professionals in this award. These sections should
assist you to determine the MINIMUM wage as required by law.
The actual pay rate should be based on market rate, which is published on the University of Queensland Open Source e-space library
You will see that Table 3.5 provides detailed information on what is happening in the market. n
If you have a question to ask then please email it to bulletin@dhaa.info

Our regular update on some great reading to improve your skills and top up your CPD hours
Take advantage of any downtime by studying at home and keep racking up your CPD points. In this edition's round-up we cover sugar tax, oral health promotion apps, long COVID effects and the overall oral health of the world's population. Whatever your special interest, we strive to include something for everyone.
Association between modifiable lifestyle pattern and periodontitis: a cross-sectional study based on NHANES
• BMC Oral Health volume 24, Article number: 591 (2024)
• CPD hours 0.25 scientific
Periodontitis can be avoided with a healthy lifestyle. However, studies have only looked at one lifestyle, ignoring the connection between lifestyle patterns and periodontitis. The purpose of this study was to look at the association

between modifiable lifestyle patterns and periodontitis.
Three lifestyle latent classes were found by fitting 2–10 models: “Class 1” (52%), " Class 2” (13%), and " Class 3” (35%). The “Class 1” displayed a prevalence of oral examination (75%), favorable self-rated oral health (92%), and engagement in physical activity (50%). The ‘Class 2’ exhibited the lowest alcohol consumption (64%) and smoking rates (73%) but the highest prevalence of physical inactivity (98%). The ‘Class 3’ showed a tendency for smoking (72%), alcohol consumption (78%), shorter sleep duration (50%), absence of oral examinations (75%), and suboptimal selfrated oral health (68%). The influencing variables for the latent classes of lifestyle were age, education, and poverty level. Periodontitis risk may rise by 24% for each additional unhealthy lifestyle practiced by participants. The ‘Class 3’ (had a greater risk of periodontitis compared to the ‘Class 1’.
Our analysis revealed that unhealthy lifestyle patterns are associated with periodontitis. These different lifestyle patterns need to be taken into account when developing public health interventions and clinical care.
Sickly sweet: It’s time for a sugary drinks tax
• 5 May 2024
• Grattan Institute
• CPD hours: 0.5 non-scientific
Australia should introduce a sugary drinks tax to reduce obesity and diabetes. Australia should introduce a sugary drinks tax to reduce obesity and diabetes. There are sugary drink taxes in more than 100 countries, including the UK, France, Portugal, and Mexico. Australia needs many policies to improve our diets and our health, but a tax on sugary drinks is the cheapest and easiest to implement.
The taxes work: they slash sales and get manufacturers to put less sugar in their drinks. The government should get on with it, as part of a multi-pronged assault on the twin scourges of obesity and diabetes.

Comment: The ongoing fight for population oral health
• The Lancet
• March 19, 2024
• DOI:https://doi.org/10.1016/S01406736(24)00536-1
• CPD hours 0.25 non-scientific
Oral diseases are the most widespread health conditions, with nearly half of the world's population living with one or more of them, spanning from young children to older adults. Despite important progress made until the early 1990s, no clear improvement has been reported in the past three decades.
Dental care should be fully integrated in primary health-care initiatives, overcoming the historical separation of dentistry from medicine that was further strengthened by medical insurance practices. Tackling the inverse care law and investing in public dental care infrastructure within universal public health systems are key elements
in the achievement of that goal. Action on the broad upstream social and commercial determinants of oral health must be prioritised, including holding accountable those who privilege profit motives and interfere in the research agendas and public health policy decision making. In addition, engaging
marginalised populations in policy and service planning and joining existing health social movements are key ways to move forward—eg, through formal social participation forums that inform health policies.
All these strategies can help to bring oral health to the forefront as part of the wider efforts towards promoting the right to health and health care, and the struggles towards fairer societies.
Experiences and learnings from developing and implementing a codesigned value-based healthcare framework within Victorian public oral health sector
• 28 March 2024
• Australian Health Review 48(2) 134-141 https://doi.org/10.1071/ AH24017
• CPD hours 0.25 non-scientific
This paper describes the development and implementation of a co-designed >>
The rotten truth about sugary drinksvalue-based healthcare (VBHC) framework within the public dental sector in Victoria.
Building a case for VBHC implementation required intensive work. It included co-designing, collaborating, planning and designing services based on patient needs. Evidence reviews, value-stream mapping and development of patient reported outcomes (PROMs) and patient reported experience measures (PREMs) were fundamental to VBHC implementation. Following VBHC implementation, a 44% lower failure to attend rate and 60% increase in preventive interventions was reported. A higher proportion of clinicians worked across their top scope of practice within a multi-disciplinary team. Approximately 80% of services previously provided by dentists were shifted to oral health therapists and dental assistants, thereby releasing the capacity of dentists to undertake complex treatments. Patients completed baseline International Consortium for Health Outcomes Measurement PROMs, which have been used for social/ clinical triaging, determining urgency of care based on risk, segmentation and tracking health outcomes. Following their care, patients completed a PREMs questionnaire. Patients agreed or strongly agreed that: the care they received met their needs (87%);
they received clear answers to their questions (93%); they left their visit knowing what is next (91%); they felt taken care of during their visit (94%); and they felt involved in their treatment and care (94%).
Long COVID in a highly vaccinated but largely unexposed Australian population following the 2022 SARS CoV 2 Omicron wave: a crosssectional survey
• 1 April 2024
• Med J Aust 2024; 220 (6): 323-330. doi: 10.5694/mja2.52256
• CPD hours 0.25 scientific
The estimated prevalence of long COVID varies widely between studies (range, 9–81% of people with SARS CoV 2 infections). In a highly vaccinated population not broadly exposed to earlier SARS CoV 2 variants, 18% of people infected with the Omicron variant reported symptoms consistent with long COVID 90 days after infection; 18% of these people had not fully resumed previous work or study by three months, and
Oral health promotion apps: providing answers?
38% required care from general practitioners for their symptoms two to three months after infection. Long COVID affects a considerable number of people in Australia, and general practices play a major role in managing its burden.
We’ve got an app for that
Oral health promotion apps: an assessment of message and behaviour change potential
• 10 September 2020
• International Journal for Quality in Health Care, Volume 33, Issue 1, 2021, mzaa112
• CPD hours 0.25 non-scientific


Oral health worldwide needs improving: untreated dental caries is the most common health condition affecting people globally. Mobile applications (apps) have potential to provide preventative oral health

interventions. This study aimed to investigate the quality of available oral health promotion apps, assessing information provided and the barriers to oral health addressed using psychological frameworks. A content assessment of oral health promotion apps targeted at adults in the UK iTunes store was conducted. The quality of 22 apps was assessed against three objective indices derived from the Delivering Better Oral Health toolkit, Theoretical Domains Framework and Behaviour Change Technique Taxonomy. Index scores were calculated and descriptive analyses were completed.
The quality of information available in oral health apps requires improvement with the majority addressing only a few barriers to oral health. Currently, there is no recognized scale for evaluating oral health apps: this study provides a suggested method for future app evaluation. There is opportunity for a new app to be created based on health behaviour change theory which includes all the Delivering Better Oral Health messages.
The 2023 report of the MJA–Lancet Countdown on health and climate change: sustainability needed in Australia’s health care sector
• 25 March 2024
• Med J Aust doi: 10.5694/mja2.52245
• CPD hours 0.25 non-scientific
The report highlights the health and economic costs of inaction on health and climate change. A series of major flood events across the four eastern states of Australia in 2022 was the main contributor to insured losses from climate-related catastrophes of $7.168 billion — the highest amount on record. The floods also directly caused 23 deaths and resulted in the displacement of tens of thousands of people.
Overall, the urgency of substantial enhancements in Australia’s mitigation and adaptation responses to the enormous health and climate change
challenge cannot be overstated. Australia’s energy system, and its health care sector, currently emit an unreasonable and unjust proportion of greenhouse gases into the atmosphere. As the Lancet Countdown enters its second and most critical phase in the lead up to 2030, the depth and breadth of the assessment of health and climate change will be augmented to increasingly examine Australia in its regional context, and to better measure and track key issues in Australia such as mental health and Aboriginal and Torres Strait Islander health and wellbeing.
A new approach to oral health can lead to healthier societies
• BMJ 2024;385:q925
• CPD hours 0.25 non-scientific
New definitions of oral health provide an opportunity to change mindsets and promote innovation to tackle high levels of unmet needs, but this will only be realised with a radical change in practice.
Oral health is everyone’s job. Improving it will require an expanded oral health workforce that should include physicians, nurses, midwives, pharmacists, social workers, dietitians, community health workers, speech language pathologists, and other health providers, as well as non-traditional providers such as civic and religious leaders and teachers.
Taking action on the social determinants of oral health inequity is at the heart of radical action to end the neglect of oral health. Ensuring oral health for all requires an approach involving the whole of government and society, including fixing broken food systems whose marketing, advertising, and sale of products contribute to poor oral health. n


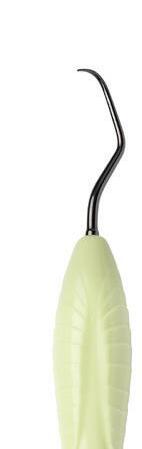
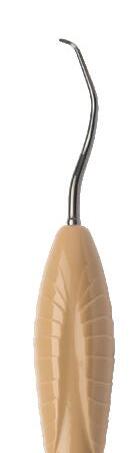
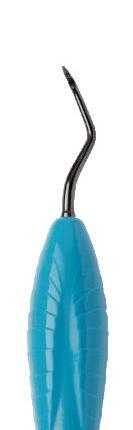
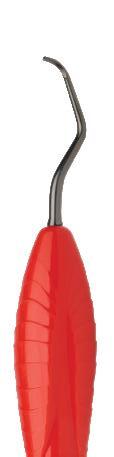
These sharpen free, razor sharp instruments are made from exceptionally durable metal alloy. Wear resistance is enhanced by a protective micro membrane coating.
They feel great, save time and have a more comfortable experience all around.
Cost comparison of sharpen free instruments and instruments that can be sharpened.







The comfort grip handles feel soft, have low slip texture and enable less finger force and less forearm fatigue for same effect at instrument tip.
Switching to sharpen free instruments a small clinic can potentially reduce costs by up to $16,000 AUD a year.
The purchase price of sharpen free instruments is ~25% higher compared to instruments that can be resharpened. However, the cost of sharpening services or doing it yourself, counting time, amounts to easily $8-$15 AUD per sharpening.
As a result, the price difference between sharpen free hand instruments and those that require sharpening becomes negligible after approximately 3-4 sharpening sessions.
By choosing sharpen free hand instruments it , the need for sharpening is eliminated. This not only saves valuable time but also reduces expenses, which can then be redirected towards more productive work.
Sharpen free coated instruments






Optimal rigidity
- Excellent sensitivity and e ciency.
- Outstanding corrosion resistance.
Precision formed tips and high-quality nishing


Metal-to-metal connection for enhanced tactile sensitivity.

- Anterior scaler
- Sickle end for removing interproximal calculus and stain
- Disc end for lingual surfaces of incisors
- Extremely sharp and smooth cutting edge.
collection has now four new instruments!

Sickle LM23 Slim SD
- Universal scaler for anterior and posterior areas
LM317-318SDES

Sickle NV2 SD
- Posterior scaler
- Heavily angled long shank allows for posterior access
- Thin and long blades provide easy access to interproximals LM ErgoSense
LM

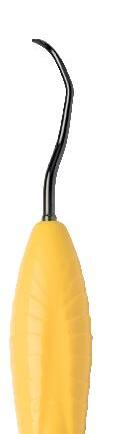









- Thin version of LM23 scaler
LM ErgoSense
LM343-344SDES

Mini McCall 13S-14S SD
- For deep, narrow pockets
- Slightly sharp, rounded tip





LM ErgoSense
LM222-223MSDES





In such a high-stress working environment, it is essential that we keep on top of our own health and wellbeing. We look at ways that can help you stay in your happy place
By Associate Professor Melanie AleyThe World Health Organisation (2024) defines mental health as “a state of well-being in which an individual realises his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community.” Wellbeing is not a fixed position, it is process that is experienced on a continuum (Ryan & Travis, 2004). Five zones of the mental health continuum have been identified, from being in crisis to excelling (Delphis, 2020). It is shaped by a range of influences, such as lifestyle and behavioural factors, cultural and psychological considerations, and spiritual and meaning elements (Ryan & Travis, 2004) In fact, some ten dimensions of wellbeing have been identified in the literature, including physical, social, emotional, environmental, cognitive, spiritual (Albrecht, 2014).
Wellbeing is fundamental to our ability to be happy, healthy and productive. Many of us engage in behaviours or activities to promote positive mental health – but how much of this is in the workplace?
Dentistry is known to be a high-stress profession, with a high prevalence of self-reported psychological stress, burnout, anxiety and depression among Australian dental practitioners (Hopcraft et al., 2023). Research exploring the careers of dental practitioners has identified that they suffer from stressors related to complex and demanding patients, their own perfectionist tendencies, and meeting production targets (Chen et al., 2023; Hopcraft et al., 2023). We spend onethird of our lives at work, often spending more time with colleagues and patients than our own family and friends – so it’s important for us to be mentally healthy at work so we can thrive in all areas of our lives.
to wellbeing by Butler and colleagues (2016). These pathways have wide applicability, having been used in educational settings and workplaces globally to help individuals flourish. Let’s explore the evidence for how we can use these six pathways in the workplace to promote positive mental health.
Positive emotions relate to an individual’s happiness and life satisfaction, their interest, enthusiasm, and absence of stress (Mayer, 2019). Gratitude interventions, such as writing gratitude letters or in journals, “count your blessings’ and ‘three good
“Dentistry is known to be a high-stress profession, with a high prevalence of self-reported psychological stress, burnout, anxiety and depression among Australian dental practitioners”
Seligman (2011) suggests that humans flourish through balancing feeling good and having purpose, and highlights five pathways for fostering wellbeing: Positive Emotions, Engagement, Relationships, Meaning, and Accomplishments. Health has been suggested as a sixth pathway
things’ exercises, and performing acts of kindness have all resulted in increasing positive emotions, with participants happier, more optimistic and connected (Duckworth, Steen & Seligman, 2005). Another exercise discussed in the literature for promoting positive emotions is to create a “Feel Good” song playlist to encourage, inspire or promote feelings such as happiness and joy (Morgan & Simmons, 2021).

Being engaged involves being enthusiastically engrossed or immersed in a task or activity (Mayer, 2019).
A range of mindfulness exercises and meditations have resulted in participants having reduced stress levels and depressive feelings and improve wellbeing (Baer, 2003). Mindfulness involves “intentionally bringing one’s attention to the internal and external experiences occurring in the present moment” (Baer, 2003 p.125). Support for mindfulness practice is widely available through digital platforms and applications, providing mindfulness meditations that can be accessed from anywhere, anytime, and with meaningful benefits – that includes the workplace! (Mrazek et al., 2019).
Social wellbeing requires positive relationships, connection and belonging. Zins & Elias (2007) advocate for developing social-emotional competence for improved wellbeing. Strategies such as establishing group norms can help staff to create a sense of community and belonging through shared expectations (Weeks, Denham & Thoeming, 2023). Encouraging a positive relationship with the self through selfcompassion can also improve wellbeing; evidence-based activities include loving-kindness meditations (Fredrickson et al., 2008) and supportive touch (Germer & Neff, 2013; Neff, 2023). There are a range of free supportive >>

touch exercises that are easy and quick to integrate into your daily work routine. Any evidence-based activities focused on developing psychological safety, empathy, teamwork, or communication skills would also help encourage and foster positive relationships.
Meaning is related to purpose, feeling connected to something bigger than the self (Morgan & Simmons, 2021). Values affirmation exercises can help individuals to identify what values give their life meaning and how they can entrench them into their daily lives, boosting confidence and positive outcomes (Bridgemen, 2019; O’Hara, 2018). Opportunities to participate in professional development activities or leadership, especially those aligned to personal strengths and values, can foster a sense of purpose (Noble & McGrath, 2015). Look at how you can align your CPD to your values, or what roles in the workplace might help your work to your values. For example, if one of your core values is ‘organised’ then you might want to take responsibility for reorganising the stock room, if you value ‘connection’ you might organise a social event for staff, or offer to mentor new staff. Another easy way to create meaning and connect at work is to perform a random act of kindness for someone.
Setting, pursuing, and achieving goals is an evidence-based approach for increasing one’s positive accomplishments, having a positive influence on wellbeing (Norrish et al., 2013; Sheldon et al., 2010). Zins & Elias (2007) describe responsible decision making and self-management as key components of effective socialemotional learning, which is positively associated with positive mental health and numerous other health outcomes. Activities focused on goal setting using SMART (specific, measurable, achievable, relevant and time-bound) goals, time management strategies, conflict resolution, and different ways of thinking have been used effectively in other social and emotional learning programs (Zins & Elias, 2007). These are great ideas for your regular performance reviews or team meetings.
It is well-known that our physical and mental health, is influenced by a range of modifiable health behaviours. Health-

based activities for improving wellbeing might focus on physical movement, self-care practices, stress management, nutrition, sleep, social activities and screen time (Nosakhare & Picard, 2020). In a study exploring combinations of behaviours impacting on wellbeing, positive social interactions, sufficient sleep (8-10 hours) and exercise (1-2 hours) per day were associated with calmness and reduced stress (Nosakhare & Picard, 2020). You might consider going for a walk during your lunch break, or incorporating stretches throughout the day.
Keep in mind, that these different pathways to wellbeing can be approached independently, but they can also converge for even more wellbeing benefits! For example, going for a walk with a work friend at lunch not only has positive benefits for health, but has flow-on positive effects on your emotions and relationships. Hopefully these evidence-based strategies have inspired you to try something new to support your wellbeing in the workplace. n
Associate Professor Melanie Aley (nee Hayes) is a dental hygienist who has enjoyed a diverse career in clinical practice, teaching, research and management. She has a Masters of Education majoring in Career Development, and after working in multidisciplinary roles, is now an Associate Professor and the Bachelor of Oral Health Program Director at the University of Sydney.



Aims
• Build leadership capacity for our profession
• Be empowered for personal development and career positioning
• Co-design and drive mentoring for oral health practitioners
This six-month program provides an opportunity for individuals who are comfortable as clinicians and are now ready to explore and expand their professional horizons.
The highly-interactive collaborative program will give participants an opportunity to reflect on their personal career trajectories, explore their leadership potential and enable them to use their combined experiences to design a mentoring program tailored to the needs of the next generation of oral health practitioners.
Cost and eligibility
Free. All course materials, online and face to face training cost, flights and accommodation will be provided by the DHAA from a special fund allocated to invest in the future of our profession. You must be a DHAA member to be eligible to apply.
Format
All sessions will be highly interactive and participantdriven. Participants will be expected to contribute proactively during each session and to commit to some reflective practice and collaboration between the sessions.
n Webinar 1
Saturday 2 November 2024 11.00 – 12.30 AEDT
n F2F workshop in Melbourne
– Thursday 6 February 2025: dinner at 7.00pm
– Friday 7 February 2025: 8.30am end 3.00pm
n Webinar 2
Saturday 15 March 2025 11.00 – 12.30 AEDT
n Webinar 3
Saturday 3 May 2025 11.00 – 12.30 AEST
Facilitators
A/Professor Nicky Kilpatrick AM Dr Trudy Lin, SA Young Australian of the Year 2022
Details and application form
Click here to go to the DHAA website.
As our industry experiences ground-breaking change, the DHAA focuses on maximising opportunities with the new Future Leaders Program and the upcoming inagural joint national congress with ADOHTA
Our profession has made significant progress in recent years with the acquisition of full independent practice status and provider numbers. The evolving environment has opened up new opportunities for our profession to practise to full scope in existing dental teams and new service models.
More than ever, we face a range of opportunities and challenges, including emerging technologies, post-pandemic backlogs, and in the oral health sector, specifically the pending creation of a new professional association to support dental hygienists, dental therapists and oral health therapists. To not just manage but to excel in such uncertain but exciting times, practitioners deserve to be supported both professionally and personally to develop a range of non-clinical skills, including advocacy, leadership, self-care, public speaking and mentorship. Furthermore, the DHAA recognises the particular benefit of supporting future generations of clinicians in making a successful transition from university into their chosen career with confidence.
The first step in this process is to build capability and confidence in the existing membership, targeting members who have made the transition into the profession, are clinically

confident and are now seeking new opportunities to expand their horizons and explore new career options. After an extensive search across the country for appropriate consultants to provide a tailored program to achieve this goal, the DHAA has engaged Dr’s Nicky Kilpatrick and Trudy Lin, who are both dental specialists with experience in coaching, leadership and mentoring.
Prof Nicky Kilpatrick
Professor Nicky Kilpatrick has over 30 years of clinical, academic and management experience both in Australia and the United Kingdom. She is currently Director of the Melbourne Cleft Lip/Palate Service, a research fellow at the Murdoch Childrens Research Institute and a visiting professor at Peninsula Dental School in the south-west of England. Following successful completion of both her Graduate Diploma in Coaching and Executive Coach Certification, Nicky is now an accredited professional with the International Coach Federation. In addition to a thriving coaching practice, Nicky works with organisations including the University of Melbourne, the Murdoch Children’s Research Institute and the Australian Dental Association to support the development of long-term sustainable mentoring behaviours and promote broader cultural change.
Dr Trudy Lin
Dr Trudy Lin, awarded Young Australian of the Year for South Australia in 2022, is one of 26 specialists in ppecial needs dentistry providing care to people with disabilities, complex medical conditions (such as cancer) and complex psychosocial circumstances (e.g. domestic violence victims). She has experience across both private and public sectors in the Special Needs Unit of the Adelaide Dental Hospital (2016–2022) and currently provides specialist consulting services as well as domiciliary services for people in their homes and residential care facilities in South Australia. Trudy is an honorary senior clinical lecturer at the University of Adelaide and is on the Royal Australasian College of Dental Surgeons (RACDS) Board of Studies for Special Needs Dentistry. Trudy is involved in various national and international advocacy roles, including being the Australasian representative for the International Advisory Committee for the International Association for Disability and Oral Health (IADH).
Trudy has attained two coach certifications: a certification specialising in mindset coaching and an advanced certification in intersectional coaching. In addition to her private coaching practice, Extra Mile Coaching, which specialises in mindset coaching for oral healthcare professionals, she is >>





“The first step is to build capability and confidence in the existing membership, targeting members who have made the transition into the profession, are clinically confident and are now seeking new opportunities”








































































a leadership coach and a workshop facilitator for the SA Health Leading Clinicians program, with her first involvement in 2017.
A unique opportunity
Nicky and Trudy have now developed the Future Leaders Program for the DHAA, which aims to:
• Build leadership capacity for our profession.
• Be empowered for personal development and career positioning.
• Co-design and drive mentoring for oral health professionals.
This highly interactive collaborative program will be delivered between October 2024 and May 2025, with three online webinars and a full-day face-toface workshop in Melbourne. It will give participants an opportunity to reflect on their personal career trajectories, explore their leadership potential and enable them to use their combined experiences to design a mentoring program tailored to the needs of the next generation of oral health practitioners.
The DHAA Board will fully fund the programme, including flights and accommodation for all participants. Applications to participate in this program are now open until 31 July 2024. All DHAA members are encouraged to apply for a place in this prestigious program, and be part of the driving force to shape our profession into a bright future. Further details and application forms are available on the DHAA website.
Discover what’s on offer to attendees of the inagural joint congress with ADOHTA in OctoberBy Jinous Eighani-Roushani, DHAA Director and CPD Chair

My name is Jinous Eighani-Roushani, a practicing oral health therapist with a background in private, hospital,
and corporate dental settings. I’ve also been involved with BOH programs at Newcastle University and Sydney University as a casual academic-clinical educator, sharing my passion for oral health education. Currently, I actively contribute to an oral health promotion committee within the Sydney Local Health District and serve as a clinical lead, offering training and support to dental practices within Bupa Dental Corporation to enhance patient care. I’m dedicated to promoting oral health awareness and prevention through my work.
As a committed DHAA board member, I am honoured to serve on the inaugural Joint ADOHTADHAA Congress Organising Committee. I am filled with a profound sense of excitement and joy. We are on the brink of a historic transformation—one that not only promises a unified front for advancing our profession but also embodies a harmonious symphony of progress and collaboration through this momentous education and networking event.
I am excited to share the incredible opportunities awaiting you at the upcoming ADOHTA-DHAA Congress, set to take place at the prestigious Hilton Sydney. This event is not just a gathering; it’s a transformative experience designed to elevate your knowledge, expand your network, and inspire meaningful change in the field of oral healthcare.
The Hilton Sydney provides a sophisticated backdrop for our congress, offering state-ofthe-art facilities and luxurious accommodations. Immerse yourself in the vibrant atmosphere of Australia’s iconic city while participating in plenary sessions that inspire thought and challenge conventions.
“This is not just a social event; it’s an opportunity to forge connections, exchange ideas, and cultivate relationships that can propel your career forward”
Imagine being in a room filled with leading experts and visionaries in oral health from around the globe. We have carefully curated a stellar lineup of speakers, including esteemed international guest speaker Professor Nicola Innes, a renowned authority in paediatric dentistry, joining us all the way from the UK. Additionally, distinguished national and local speakers such as Dr Thomas Murray, Dr Sam Koh, Dr Roisin McGrath, and
many more will each bring invaluable insights and expertise to the table.
Our upcoming congress, themed “Three Divisions, Two Associations, One Future,” is designed to celebrate this unity and honour the rich legacies of both associations.
The congress program features a diverse and exciting range of topics, from cutting-edge clinical innovations to comprehensive patient management strategies and oral health prevention. Topics include geriodontology, paediatrics, periodontology, population health, restorative practices, professional practice, and updates on infection control standards. Whether you are a dental hygienist, dental therapist, or oral health therapist, whether you are interested in the latest advancements in dental technology or seeking insights into holistic patient care, there’s a plenary session awaiting you. These sessions will provoke discussions on the future of oral health and explore emerging trends and transformative approaches.
All sessions are tailored to meet your needs and ensure valuable insights for all attendees, addressing current challenges and advancements in our profession.
Don’t miss out on the interactive workshops, where you can engage in hands-on learning and collaborative discussions. Refine your clinical skills, explore innovative approaches to practice management, and delve into
“This congress is not just about professional development; it’s a celebration of unity, progress, and camaraderie”
unique topics like “Emotional Wellbeing for the Oral Health Practitioner,” led by Dr. Trudy Lin, Sarah Harwood, and Associate Professor Carol Tran, designed to support and rejuvenate oral health practitioners.
This congress is not just about professional development; it’s a celebration of unity, progress, and camaraderie. We invite you to join us for an unforgett able experience filled with valuable networking opportunities and engaging sessions that meet the needs of every attendee, whether focused on personal growth or career development.
And let’s not forget the Gala Dinner. Mark your calendars and get your dancing shoes ready for an evening of celebration, dancing with a band, and exciting entertainment, topped off with unparalleled networking. Picture yourself mingling with colleagues and industry leaders in the elegant ambiance of a great venue, all while enjoying fine dining and live entertainment. This is not just a social event; it’s an opportunity to forge connections, exchange ideas, and cultivate relationships that can propel your career forward.
I hope everyone, especially those new to abstract submissions, takes advantage of this opportunity to showcase their hard work and dedication. Let’s embrace diversity and highlight the incredible work being done across our profession. We are truly fortunate to have such a wealth of expertise under one roof. Take advantage of this rare opportunity to learn from and engage with leaders in our profession. Each speaker brings a unique perspective and wealth of experience that can enrich your practice and inspire new approaches to patient care.
This joint national congress is more than an event; it’s a call to action. Together, we can shape the future of oral healthcare, advocate for excellence in patient care, and drive positive change in our communities. Your participation is instrumental in advancing our profession and ensuring that oral health remains a priority on healthcare agendas.
Secure your place now and be part of this extraordinary gathering of minds and hearts. Celebrate unity, embrace innovation, and chart a course towards a brighter future for oral health. We look forward to welcoming you to the ADOHTA-DHAA Congress at the Hilton Sydney, an experience that promises to inspire, educate, and transform.




Planning on retirement?
Why would you need to worry about your professional indemnity insurance when you’ll no longer be practising?
In this article, BMS (the DHAA insurance partner) explains what runoff cover is and how to apply for it under the DHAA Member Insurance Program. Note, this article specifically relates to the DHAA Member Insurance Program, Professional Indemnity and Public & Products Liability Insurance policy, with BMS. For more information about the program, visit the DHAA website or speak to a BMS broker.
What is run-off cover and why is it important?
Run-off cover is designed to cover you when you permanently cease practising or retire.
You may not be aware that your professional obligations continue even when you have ceased practising. It may take months or years for a claim to arise after treating a patient. This is why it’s important to maintain cover even after you’ve ceased practising.
You will need to activate run-off cover with BMS prior to your Professional Indemnity insurance expiry date to utilise this benefit.
Run-off cover is not needed if you’re
taking temporary leave such as a short break from practising or a holiday. In these circumstances, you should continue to renew your Professional Indemnity insurance to ensure you’re covered.
“You may not be aware that your professional obligations continue even when you have ceased practising. It may take months or years for a claim to arise after treating a patient. This is why it’s important to maintain cover even after you’ve ceased practising”
Q: I am going on maternity leave, do I need to renew my cover?
A claim could still be made against you while on maternity leave.
We recommend you maintain your DHAA membership and Professional Indemnity insurance while on maternity leave.
Q: I plan on retiring at the end of this year. Should I let my cover lapse as I won’t be practising anymore?
A claim can occur even after you’ve retired.
To ensure coverage, you will need to activate run-off cover with BMS prior to your insurance expiry date (30 June) to utilise this benefit.
Q: I am going on an extended holiday overseas. Do I need to renew cover? Run-off cover does not apply when going on holiday or taking an extended break from the profession. Maintain an active DHAA membership and insurance policy to ensure you are covered.
Q: How do I activate run-off cover under my DHAA Member Insurance with BMS?
Contact BMS prior to your insurance expiry date via the BMS Portal Connect with us form or email the team at dhaa@ bmsgroup.com.
If you’re unsure about how to maintain cover or planning on a change to your work activities, please reach out to the BMS team prior to your insurance expiry date. The team can discuss your situation and help you maintain continuous cover.
W: dhaa.bmsgroup.com
P: 1800 940 762
E: DHAA@bmsgroup.com
You must be a current DHAA member to be eligible for the DHAA member insurance program. If your membership ceases you will not be offered renewal when your policy expires. In arranging this insurance for our members DHAA is acting as a distributor of BMS Risk Solutions Pty Ltd (BMS) AFSL 461594, ABN 45161187980. This insurance is issued by BMS under binder with Certain Underwriters at Lloyds. When acting under a binder BMS acts as agent for the insurer and not as your agent. This is general advice only and BMS has not considered whether it was suitable for your particular objectives, needs or financial situation. Please read the Policy Wording/Product Disclosure Statement and the BMS Terms of Engagement which contains the Financial Services Guide before making a decision about purchasing this policy. DHAA may receive a percentage of the commission paid to BMS by the insurer and/or a fee per policy.
26th - 27th July 2024 at Rydges World Square, Sydney Up to 12 hours of CPD
3 Interactive Workshops & Full Day Presentations

MDPA24 is a fantastic opportunity for all dental practitioners to explore or dig deep world of mobile dentistry as our comprehensive program has it all.
This year MDPA24 is spread over 2 days, delivering 3 x workshops and a 6hr CPD full day of lectures. Not to mention a huge trade expo featuring the latest technologies, equipment and services and the opportunity to network with likeminded professionals and industry leaders!



JOIN US FOR OUR THIRD MOBILE DENTAL PROVIDERS AUSTR CONFERENCE THAT IS SET TO REDEFINE THE WAY YOU PRACTICE DENTIST Use Promo Code: “MDPA10" for 10% Off


in the

27TH JULY 2024






9:30 AM - 11:30 AM 12:30 PM - 2:30 PM 3:00 PM - 5:00 PM
Atty. Marianne Nicolle FRI, 26TH JULY 2024
“Treatment planning and treatment provision to maximise oral health outcomes”
“Taking it on the road: Tackling practical Infection Control Issues for Mobile Dental Services”
Prof. Laurence Walsh
“Claiming confidence: How to comply with Medicare and health funds”
Dr. Martin Webb
Clinical Governance Considerations for Mobile Dental Providers: A Risk focused approach
Prof. Alexander Holden

“Preserving Smiles, Protecting Rights: A Legal Insight into Patient Data Control”
A study of the behavioural influence on a patient of a clinician’s choice of topic specific wordsBy Hafeez Ahmed
It has been recognised that not only does the patient interview need to be empathetic but the discussion content needs to be topic specific.1
In recent years, clinicians have been encouraged by the General Dental Council to move towards patientcentred care.2 In addition to this, it has been described that simply “being nice” and maintaining a good relationship with the patient are not sufficient for patient-centred care. Patient-centred care requires detailed topic-based discussions.3 However, there appears to be no studies reporting on topic-specific words and their influence on patient understanding.
Freeman in 1999.4 The importance of effective communication and behaviour change is further underlined by the fact that the majority of dental care requires patients to adhere to advice, otherwise the care is undermined.5
It is intriguing that despite the dental profession believing they are actively engaging in effective patient communication the prevalence of periodontal diseases remains largely unchanged. Chronic periodontitis occurs in 45% of the UK population6 and in 11.2% of the global population7.
Beyond that, it is accepted that ‘effective communication’ is essential to behaviour change and was comprehensively covered and discussed in detail in a series of articles by Ruth
Experience suggests that, when patients find it difficult to make the necessary behavioural changes, it is generally for a variety of reasons, including: they do not fully understand periodontal diseases; they do not appreciate the long-term implications and legacy of the disease; they do not entirely recognise the pivotal role of homecare; or they are individuals who understand all the advice but do not want to change.
In my practice I created a table with a list of 20 topic-specific words and phrases (Table 1). The words and phrases were selected from those I heard being used most commonly

by patients and dental professionals. On the right-hand side of the list, I placed a Likert-type scale numbered from one to five. My plan was to ask potential participants to rate the words/phrases by circling one number on the scale for each of them, to indicate the degree of perceived encouragement or motivation each word/phrase offered them.
Starting in June 2022, every new patient referred was invited to take part with the aim of compiling 100 lists. By virtue of the referral, all patients had received at least one course of periodontal therapy from the referring dentist. Potential participants were recruited by discussing the purpose of the study with them in the waiting room, following the completion of their initial consultation. The following >>
“Despite the dental profession believing they are actively engaging in effective patient communication the prevalence of periodontal diseases remains largely unchanged”
statements were made as an invitation to take part:
“I am conducting a small study in an attempt to identify if some of the words we use when we discuss gum disease with our patients affect their enthusiasm more than other words. Essentially, I want to see if some words create more of a feeling of seriousness and also if some words create a greater feeling of enthusiasm or motivation to act on the advice than other words.”
‘Motivation’ was defined as: “It makes you feel like taking the matter seriously” and “It makes you want to do your part in resolving the matter”. Potential participants were also advised: “What I really want to see is if any of the words or phrases makes you feel more like sitting down for 8 to 10 minutes each evening to use floss or inter-dental brushes or wood sticks to clean inbetween your teeth and the margins of your gums.”
During the discussion, and before the patients agreed to participate, they were given the list so they could see what was being described. They were also given the guidance for the Likert-type scale (Table 2).. To maintain anonymity, patients were advised that they were not required to put their name on the list - only their age and gender.
Those patients who agreed to take part were then shown to a seat and asked to read the list and rating scale carefully and to confirm their understanding. Reassuringly, a few of them smiled and said: “It’s pretty straight forward,” others laughed and said: “It’s not rocket science.”
One hundred lists were rated between June 2022 and January 2023; a record was kept of the participants, although at no point were their names written on the list. Fifteen patients declined the invitation to
take part in the study. Of the reasons given, the two main ones were: “It’s not something that I’m interested in” and, “I
On the
lists
and 39 males. The average age was 57years; the youngest patient was 18 and the oldest

“They [the authors] claim that 30 seconds of language is all the brain can understand and, accordingly, they encourage fewer words for greater impact”
most likely to encourage/motivate the patient; the lowest score was one - the word/phrase was least likely to encourage/motivate the patient. Although it was not the original intention, the Mean Score became known as the “Encouragement Value”.
The findings suggest that, in the opinion of susceptible patients with experience of periodontal diseases, certain words when used to describe the disease can, somehow, generate different feelings, with some being more motivational than others. This indicates that patients form different meanings from different words. It also suggests that words can change the way a patient thinks. These points align well with research carried out by Andrew Newberg and Mark Waldman, in their book Words Can Change Your Brain.8 The authors also propose that the mechanism behind how we process a communication is directly related to the number of words that are used. They claim that 30 seconds of language is all the brain can understand and, accordingly, they encourage fewer
words for greater impact.
The findings also revealed a trend: the more severe sounding words scored higher mean values. This finding aligns with the consensus that the more immediate and severe the threat, the greater the chance of positive behaviour changes.9 DeMatteo and DiNicola also found that patients with mildly threatening problems tend not to comply with their therapists’ advice. Worryingly, this suggests that some of our patients, irrespective of how we communicate with them, will fail to comply until a stage when tooth loss is inevitable.
In a more recent study, which investigated the collaboration between medicine and dentistry in relation to diabetes management10 patients reported inconsistency in the information and advice they were given by different healthcare providers. It was suggested that consistency would be beneficial to communication. Diabetes and periodontitis are inextricably linked as chronic inflammatory diseases that adversely influence one another. The creation and use of universal statements as scripts, using the topicspecific words reported by patients as more encouraging, makes sense. The scripts would increase consistency in information sharing and thus increase the potential for a positive impact on a patient’s periodontal health.
The short- and long-term aim of periodontal therapy is to keep the inflammatory response below the threshold of bone loss or further bone loss. This is entirely dependent upon us, as clinicians, persuading our patients to take our advice and follow it.
Compliance is defined as: “the extent to which a person’s behaviour coincides with medical and dental advice”.11 Compliance requires that a patient is more than just a passive receiver of information. The estimates of compliance range from 20% to >>
over 80%.12 Generally, the rates of compliance for long term therapy tend to converge at 50%, regardless of setting or illness.13 Although we know that patients do not follow oral hygiene recommendations consistently, we do not know specifically why they do not. One reason it is not understood could be that compliance research has been dominated by the perspective of the healthcare professional. These findings offer an insight into these patients’ perspectives.
The degree to which a patient complies with oral hygiene instruction is of more importance than the choice of any particular treatment method.14 The literature shows that compliance in general decreases as treatment time or the complexity of the required behavioural change increases.14 It is often the case that by the time some susceptible patients appreciate what their type of periodontal disease is and what self-care is necessary to treat, stabilise and maintain it, insufficient bone remains to retain some of their teeth. Therefore, if we are to succeed with a preventative approach, we need to empower patients and achieve compliance at early stages of bone loss. Around 2006, I had carefully devised the following statements to explain gum disease to my patients in a way I thought would be most effective:
1. Gum disease is an infection that irreversibly destroys the bone that holds your teeth in place.
2. When a significant amount of bone has been destroyed, your teeth will feel loose or wobbly.
3. When insufficient bone remains to support your teeth, they will start to drift or fall out.
A few of the words and phrases I put in the list in this study closely resemble some of the ones in these statements. In fact, it is my use of the above statements with my patients that inspired me to conduct this study.
Table 3: The results present the actual number of patients who circled each score. The mean is represented on the right-hand side and the words/phrases have been listed in descending order of “Encouragement Value”.
For example, the Mean Score for ‘Will result in tooth loss’ was calculated as follows: 13x4 + 87x5 divided by 100 (52+435 divided by 100 = 4.87)
To avoid bias I deliberately avoided using the above statements in the initial consultations during the period of this study.
The above statements might not be to everyone’s liking but they are simple, short, topic-specific and to the point. They accurately reflect the seriousness of the condition. I devised them to increase the likelihood of patients fully understanding what is being said, as amongst other things, understanding helps allay anxiety.15
I appreciate that the statements have a negative tone; however, once patients appreciate the seriousness of their condition positive tones can be introduced by discussing the benefits of resolving the condition. Since using these statements, I have found my patients clearly understand the seriousness of their condition and, almost always, express their gratitude for the unambiguous nature of my communication. The message contains bad news, but I deliver it gently with

“I have found my patients clearly understand the seriousness of their condition and express their gratitude for the unambiguous nature of my communication”
a measured polite firmness aimed at ensuring patients understand the potential seriousness of periodontal infection. 16,17,18
Conclusion
In respect to the patient discussion, these findings suggest that the information which is conveyed by a single word or phrase does have the potential to affect the communication. Each word has a meaning but more importantly each word creates a mood.
The author is a clinician operating a private referral practice restricted to periodontal care, some minor oral surgery and implant dentistry. Most daily treatments involve helping patients resolve their periodontal problems. The author is not a researcher, and has no experience of statistical analysis. This opinion paper was prompted by the fact that a poor understanding of ‘gum disease’ was relatively common among patients, despite the fact that they had regularly seen a dentist and/or a dental hygienist. Some had received multiple courses of periodontal therapy but still could not demonstrate a good understanding of gum disease. It is hoped this article stimulates wide-spread debate as to how we communicate with our patients. It is also hoped that researchers will be inspired to use resources to produce a more robust and in-depth study so that we can all learn form best practice. n
About the author:

Dr Hafeez Ahmed, Specialist Periodontist BDS(Wales)1991, FDS, MRD, MSc, MClinDent, DGDP. Binswood House Dental Practice, Royal Leamington Spa, Warwickshire CV32 5SE UK.
Contact: binswoodhousedentalpractice@ btinternet.com
References
1. Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathetic communication in the medical interview. JAMA. 1997: 277(8):678-682.
2. General Dental Council. Standards for the dental team. 2013.
3. Asimakopoulou K. A good relationship and good communication are not sufficient for patient-centred care; Brit Dent J. 2015; 219(3):105-106. Published online: 14 August 2015 | doi:10.1038/sj.bdj.2015.589.
4. Freeman R. The psychology of dental patient care: The common-sense approach, Brit Dent J. 1999; 186(9):450-452.
5. Brown JC. Patient non-compliance - a neglected topic in dentistry. JAmDent Assoc. 1981; 103(4):567-569.
6. Adult dental health survey 2009- summary report and thematic series 2011.
7. Kassebaum N J, Bernabe E, Dahiya M, Bhandari B, Murray C J L, Marcenes W. Global burden of severe periodontitis in 1990–2010: A systematic review and metaregression. J Dent Res. 2014; 93(11):1045–1053.
8. Newberg, A., Waldman, M. R Words can change your brain. Hudson Street Press (2012).
9. DeMatteo, M.R., DiNicola, D.d. Achieving patient compliance. New York: Pergamon Press Inc.(1982).
10. Bissett SM, Stone KM, Rapley T, PreshawPM. An exploratory qualitative interview study about collaboration between medicine and dentistry in relation to diabetes management. BMJ Open 2013; 3(2):e002192 doi:10.1136/bmjopen-2012-002192.
11. Haynes RB. Introduction. In: Compliance in health care. Baltimore: John Hopkins Univ. Pr. (1979).
12. Buckalew LW, Sallis RE. Patient compliance and medication perception. J Clin Psychol. 1986: 42(1): 49-53.
13. Morris LS, Schulz RM. Patient compliance- an overview. JClinPharmTher. 1992:17(5):283-295.
14. Ramjford SP, Morrison EC, Burgett FG, Nissle RR, Shick RA, Zann GJ et al. Oral hygiene and maintenance of periodontal support. JPeriodontol. 1982; 53(1):26-30.
15. Freeman R. Communication, body language and dental anxiety. Dental Update 1992; 19(7):307-309.
16. Ptacek JT, Eberhardt TL. Breaking bad news. A review of the literature. JAMA 1996;276(6):296-502.
17. Davis, K. Power words in periodontal communication. Reg Dent Hyg.2011;31(9):74.
18. Davis K. The Art & Science of Effective Communication for Non-surgical Periodontal Treatment. Contin Educ.2007: 58-68.

We continue our focus on the recognition and diagnosis of dry mouth plus the subsequent treatment of this underappreciated conditionby Brie Jones
As clinicians, we have a vital role in ensuring the well-being of our patients. Our dedication is not only concerning their oral health but to the general well-being of every patient we see. As I mentioned in the previous DHAA Bulletin (Issue #70), dry mouth is one of the most underappreciated, underdiagnosed and undermanaged oral health conditions. A dry mouth can significantly impact an individual’s quality of life, with symptoms extending beyond mere discomfort; including oral health complications and disease, difficulty in speaking and swallowing. Stress, anxiety, and decreased social interactions due to discomfort and embarrassment further lead to a diminished quality of life for our patients. Diagnosis and open discussions with our patients are important to bring this condition to their attention. You don’t know what you don’t know; therefore it is our job as
health care professionals to educate our patients.
Saliva is our body’s first line of defence. It contains specific enzymes and proteins that identify pathogenic bacteria, destroying them and flushing them away before they can cause harm. Saliva moisturises the oral cavity to aid in speech, swallowing and digestion and allows us to taste our food. A dry mouth can arise due to various factors, such as dehydration, medication side effects, and certain medical conditions and therapies. Commonly there will be more than one combination of these factors which only compound the debilitating condition of dry mouth. For example, many of my elderly patients take two or more pharmaceutical medications (increasing their risk of dry mouth by 40%), suffer from dehydration because they only like drinking tea and coffee (especially during the cooler months) and many of them suffer from diabetes. Diabetic patients often experience reduced
saliva production due to salivary gland hypofunction and thus exacerbating their dry mouth condition further.
The problem with many of today’s oral care products is that they contain detergents and chemicals such as sodium lauryl sulphates (SLS), or alcohol. These products upset the delicate oral flora and can cause irritation and dry the mouth out with constant use. Have you ever had a patient that looks like their mucous membrane is sloughing off? This can be caused by the harsh detergent, sodium lauryl sulphate. Kazi et. al (2022) discuss that the effects of SLS were reported as mucosal desquamation, irritation or inflammation of oral mucosa or the dorsal part of the tongue, ulcerations, and toxic reactions in the oral cavity. A further double-blind cross-over study tested the oral mucosal effects of SLS-containing toothpastes in 28 healthy females. seven kinds of toothpaste were used, differing only in detergent concentration and one
placebo toothpaste. Forty-two reactions were recorded whilst using the SLS toothpaste, whereas the detergentfree toothpaste did not result in oral desquamation (Herlofson & Barkvoll, 1996).
Oral 7, is the only product in Australia that contains four natural salivary enzymes and proteins (Glucose Oxidase, Lactoperoxidase, Lactoferrin, and Lysozyme). These powerful enzymes and proteins help boost the protective benefits of saliva and strengthen the mouth’s natural defence system. It is specially formulated to provide gentle, yet effective oral care and relief without the use of harsh chemicals (NO SLS and NO Alcohol). As discussed in my previous article, Biotene used to contain salivary enzymes, however, they have changed their formula and have removed these enzymes. This highlights the importance that we must read the labels and know what is in the products we recommend to our patients, and ideally, try them ourselves first.
Recognising the profound impact dry mouth can have on our patients, I am pleased to report that Oral 7 has helped many of my patients. I have managed to reduce and control dental decay and periodontal disease with my diabetic patients and my patients have reported that they are much more comfortable; the burning sensation has eased or stopped and they can taste their foods again. I have even seen improvement and a relatively shortened healing time with aphthous ulcers and hand foot and mouth lesions in my neighbour’s children whilst using the Oral 7 mouth spray. It has been very rewarding to see the quality of life improve for these patients. Oral 7 has an innovative range of products that have been meticulously
“The problem with many of today’s oral care products is that they contain detergents and chemicals such as sodium lauryl sulphates (SLS), or alcohol. These products upset the delicate oral flora and can cause irritation and dry the mouth out with constant use”
designed to alleviate the symptoms of dry mouth effectively. The Oral 7 product range includes moisturising mouthwash, toothpaste, mouth gel, mouth spray and chewing gum; all specially formulated to provide gentle, yet effective relief of dry mouth. Oral 7 also has a baby and kids range of toothpaste. The baby’ product is a delicious apple flavour, fluoride-free, and contains enzymes to promote a healthy microbiome and replicate the protective benefits of breast milk. The kids’ version is a hit with its tutti frutti flavour, which contains protective enzymes and sodium monofluorophosphate (equivalent to 1,000ppm of sodium fluoride protection). It is important to note that I do recommend my patients use the Oral 7 products in conjunction with each other and that the ones who have the best results use all three products (toothpaste, mouthwash/ or spray, and gel). The reason for this is that SLS, along with sodium fluoride, denature the protective enzymes found in the Oral 7 range and in natural healthy saliva. Yamaguti et.al (2013) discuss that many studies suggest that fluoride exposure can inhibit the activity of various enzymes and can generate free radicals, which interfere with antioxidant defence mechanisms in salivary glands.
All Oral 7 products are SLS-free and contain Sodium monofluorophosphate instead of sodium fluoride. Sodium monofluorophosphate has a different composition to sodium fluoride and stannous fluoride and thus does not interact with the protective enzymes. It does however still provide fluoride remineralisation and protection.
By incorporating Oral 7 products into your patients’ daily oral care routines, you can help them manage dry mouth symptoms proactively, fostering improved comfort and overall well-being. Moreover, these products are suitable for individuals of all ages, will not interfere with their current medications, and can complement existing treatment regimens seamlessly.
As an advocate for comprehensive patient care, I invite you to empower your patients and explore the benefits of Oral 7 solutions. Together, we can make a significant difference in the lives of individuals grappling with dry mouth.
For further information or to request brochures and samples for your practice, please don’t hesitate to contact me: brie. jones@oral7.com.au n
References:
• Yamaguti, P., Simoes, A., Ganzerla, E., Souza, D., Nogueira, F., & Nicolau, J. (2013). Effects of single exposure of sodium fluoride on lipid peroxidation and antioxidant enzymes in salivary glands of rats. Oxidative Medicine and Cellular Longevity, Article 674593. https://doi. org/10.1155/2013/674593
• Herlofson BB, Barkvoll P. (1996). Oral mucosal desquamation caused by two toothpaste detergents in an experimental model. Eur J Oral Sci. Feb;104(1):21-6. doi: 10.1111/j.16000722.1996.tb00041.x.PMID: 8653493
• Alli BY, Erinoso OA, Olawuyi AB. (2019). Effect of sodium lauryl sulfate on recurrent aphthous stomatitis: A systematic review. J Oral Pathol Med. May;48(5):358-364. doi: 10.1111/jop.12845. Epub 2019 Mar 27. PMID: 30839136.
• Kasi SR, Özcan M, Feilzer AJ. (2022). Side effects of sodium lauryl sulfate applied in toothpastes: A scoping review. Am J Dent. Apr;35(2):84-88. PMID: 35506963.
If you’re looking for a new challenge, this might be it!By Dr Arosha Weerakoon
It’s easy to forget that much of what we practice today was scientifically explored by people like you who sought to improve techniques to help the people they served. For instance, in the 1980s, it was common practice to electively extract all traumatised teeth, that is, until the controversial efforts of Jens O Andreasen and Frances M Andreasen. Andreasen and Andreasen pioneered the field of dental traumatology to help us save millions of people from unnecessary extractions, post-trauma.1 But it took a clinician like Jens, who wanted to help victims of dental trauma, to change the way we think and practice.
Do you have a burning question about our clinical practice that needs investigating? Do you want to diversify or explore an alternative career path? Do you want to improve how we work or optimise patient care? Could someone like you become a clinician-scientist?
Whether you are a student, new graduate or an experienced dental practitioner, research may be your unidentified calling.
Here are five ways you could benefit as a clinician-scientist.
1. You could answer a burning question.
Research can help you solve or help understand clinical challenges. After five years in clinical practice2 I sought a challenge. I noticed that my ‘temporary’ glass ionomer restorations lasted longer than my resin fillings in my older patients. It made me wonder if there was a difference between resin-
based adhesives and glass ionomers, and if tooth structure, particularly dentine, characteristically changed as we aged.
My burning questions led me to enrol in a PhD program at the University of Queensland. Thanks to the generous funding by Colgate, through my research, I discovered little difference in adhesive longevity between glass ionomers, and some of the popular resin-based systems,3 and that dentine mineral distribution4 and collagen qualities5 changed as we age. My research outcomes helped me understand why my restorations lasted variably in older patients, and why we observe more fractured teeth in mature people.6
2. Discover a new career pathway. Research can forge new or alternate career pathways.
Engaging with research may lead you to roads less travelled. You could partner with the dental industry, not-for-profit agencies, become an academic or even work for global companies such as Colgate.
3. Travel to unexpected places. Research can take you to unexpected places. One of my research-related highlights was a trip to Sweden after winning the Colgate pre-doctoral research award at an International Association for Dental Research meeting. Over the years, my awards and bursaries have funded travel to conferences based in Jackson Hole, USA, Canberra, Brisbane, and Perth.

“Whether you are a student, new graduate or an experienced dental practitioner, research may be your calling”
4. Make new friends. Sometimes, you have to step outside your comfort zone to meet new people. During the early stages of my PhD, a co-investigator encouraged me to present at the Light Microscopy Conference. I was the only nonmicroscopist who presented at the conference; my imposter syndrome was on hyper-drive. But as it turned-out, my research and interest in teeth sparked a conversation with many of the attendees who in turn wanted to help and collaborate with me.

5. Stay ahead of your peers. Doing research helps you stay in touch with the latest developments in our industry.
Attending the occasional continuing professional development course will enhance our capacity to meet new people and learn new skills, but doing research affiliated with a University helps maintain a connection that we often lose after graduation.
As a clinician-scientist, you could help find a solution that improves our clinical practice, diversify your skill-set to enter an alternate career pathway, travel to unexpected places, meet and collaborate with new people outside of Dentistry, and keep up with the latest developments in our profession. Do you have what it takes? n
References
1 https://www.iadt-dentaltrauma.org/history.html
2 Gladwell M. Outliers: The story of success. Little, Brown; 2008 Nov 18.
3 Weerakoon AT, Cooper C, Sokolowski KA, Meyers IA, Thomson D, Ford PJ, Sexton C, Symons AL. Effect of dentine site on resin and cement adaptation tested using X‐ray and electron microscopy to evaluate bond durability and adhesive interfaces. European Journal of Oral Sciences. 2022 Oct;130(5):e12890.
4 Weerakoon AT, Cooper C, Meyers IA, Condon N, Sexton C, Thomson D, Ford PJ, Symons AL. Does dentine mineral change with anatomical location, microscopic site and patient age?. Journal of structural biology: X. 2022 Jan 1;6:100060.
5 Weerakoon AT, Condon N, Cox TR, Sexton C, Cooper C, Meyers IA, Thomson D, Ford PJ, Roy S, Symons AL. Dynamic dentin: A quantitative microscopic assessment of age and spatial changes to matrix architecture, peritubular dentin, and collagens types I and III. Journal of Structural Biology. 2022 Dec 1;214(4):107899.
6 Weerakoon AT, Meyers IA, Thomson D, Cooper C, Ford PJ, Symons AL. Coronal dentin differs between young and mature adult humans: A systematic review. Archives of Oral Biology. 2022 Sep 26:105553

About the author
Dr Arosha Weerakoon is a Principal Dentist and owner of Tewantin Family Dental. She is also a lecturer (Hon) and PhD candidate from the School of Dentistry, University of Queensland. She holds a Fellowship with the Royal Australasian College of Dental Surgeons, and a Masters in Public Health. Arosha is a Fellow of the International College of Dentists. Arosha advocates for community engagement, interdisciplinary collaboration and patient empowerment. She hopes to use her role as a Colgate® Advocate for Oral Health to create meaningful discussions with oral and general health professionals to improve health practices, patient outcomes and to encourage more clinicians to engage with research.
Republished with permission from Colgate Advocate’s for Oral Health
colgateprofessional.com.au/Advocates

ACT contacts:
Director Amy McDermott directoract@dhaa.info
Chair Kate Spain. chairact@dhaa.info
n The ACT welcomes new committee members Holly Murphy, Melissa Koroday and Elissa Noris.
The Committee has been working hard in planning the next full day seminar at the East Hotel on Saturday 17 August. The impressive six-hour program features Oral Macillofacial Surgeon Dr Jacqueline Dobes on oral pathology, Periodontist Dr Clarence Da Cruz providing an update of assessment and care of peri-implantitis, Pharmacist Belinda Mackenzie on
“ The six-hour program features Oral Macillofacial Surgeon Dr Jacqueline Dobes on oral pathology, Periodontist Dr Clarence Da Cruz providing an update of assessment and care of periimplantitis, ”
pharmacology, Population health researcher Sinan Brown on E-cigarettes. The day will conclude with dentist Dr Ornella Delli-Rocili providing a presentation on the latest technological advancement in digital dentistry, while Audiologist Kim Gordon will run through strategies to minimise hearing damage at the workplace for dental practitioners. With such a great program places are filling fast so please register ASAP to avoid disappointment.
For further information and to register please



NSW contacts: Director Jinous Eighani-Roushani directornsw@dhaa.info
Chair. Belinda Hines chairnsw@dhaa.info
Deputy Chair Angelee Murdock (contactnsw@dhaa.info)
n A big thank you to NSW for hosting the joint DHAA - ADOHTA board meeting on 13-14 April to progress the creation of a new association for our profession. The meeting was a success with a unification proposal
sent to members of both associations for feedback. Members of the organising committee also took the opportunity to conduct a site visit to Sydney Hilton, the venue for the inaugural Joint ADOHTA DHAA Congress in October this year.
The next NSW event will be held on Saturday 22 June as a full day seminar with an impressive program and speakers. We are fortunate to have dentist Dr Louis Chan, who is also a Chinese Medicine Practitioner to present on TMJ integrating
“ We are fortunate to have dentist Dr Louis Chan, who is also a Chinese Medicine Practitioner to present on TMJ integrating Chinese medicine principles”
Chinese medicine principles. Professor Sue Ching Yeoh will present on comprehensive oral mucosal examination and discuss potential red flags oral health practitioners
For all the latest info on DHAA events please visit www.dhaa.info/events
must look out for. ENT specialist Dr Gregory Lvoff will present on dentofacial growth and sleep apnoea, while Orthodontist Dr Roshanak Boustan will provide a session on the role of oral health practitioners in the treatment process. An update on common orthognathic surgery procedures and the use of modern technologies including virtual surgical planning and patient specific implants to optimise treatment outcomes will be provided by Specialist Oral and Maxillofacial Surgeon Dr Anthony Chellappah Dental Hygienist and Academic Associate Professor Melanie Aley will provide practical tips on the management of physiological distress, burnouts and self care for oral health practitioners. Registration is closing soon so please REGISTER now to secure your place:
A big thank you to Ian Epondulan and Patricia Pacleb for leading the volunteer team to provide a successful World Oral Health Day Information session in Western Sydney on 17 March. There was an excellent turn out from all age groups. This is now an annual event that attracts great interest from many local community groups.



NT Contact: Staff Bill Suen bill.suen@dhaa.info
n A special NT member briefing was held Wednesday 3 April at 7:30pm. A big thank you to NT members Katy Smith and Leonie Brown for putting their hands up to help organising CPD events in both Darwin and Alice Springs for our members. Please look out for information when details are finalised.
If you are interested in helping out, please email bill. suen@dhaa.info
Qld Contacts: Director Carol Tran. directorqld@dhaa.info
Chair Gabby Williamson chairqld@dhaa.info
Deputy Chair Courtney Dicken contactqld@dhaa.info
n Thanks to QLD committee member Jessica Horwood who led Griffith students to present to CURA Aged Care
residents in May. Feedback was very positive with most participants said the experience was informative and interesting, while the manager invited us back to present in future sessions.
After the successful Toowoomba half day education in March, the Queensland Committee is offering a remarkable full-day education program scheduled for Saturday 13 July at the voco Brisbane City Centre.
Come along to find out from endocrinologist Dr Jessica Triay the important role of oral health practitioners in helping to identify potential diabetes risk factors and signs and to contribute to early diabetes detection and intervention.
Orthodontist Dr Desmond Ong will discuss the clinical challenges of 10 patients and how collaborative interdisciplinary case management was able to fulfill the desired treatment objectives. Paediatric >>
“ Find out from Dr Jessica Triay the important role of oral health practitioners in helping to identify potential diabetes risk factors”
Dentist Dr Alexei Mogilevski will take us through new successful trends in the management of paediatric dental patients covering SDF, Hall technique and Zirconia Paediatric crowns.
For further details and to REGISTER
SA Contacts:
Director Michelle Kuss michelle.kuss@dhaa.info
Chair Courtney Rutjens chairsa@dhaa.info
Deputy Chair Jesse Kourakis contactsa@dhaa.info
n SA members were treated a memorable education experience at the beautiful destination Auchendarroch House on Saturday 23 March 2024 It was another full house event attracted by the impressive array of
“ We are offering a face-to-face mental health first aid course in Adelaide on Saturday 27 and Sunday 28 July. This accredited course is presented by our own Marcy Patsanza-Mkonto”
expert presenters including Periodontist Dr Ying Guo, research pioneer Professor Gordon, outreach dentist
Dr Harry Perkins, mobile dentistry OHT Shay Shehata and Claire Damon, as well as highly regarded oral health business owners
Lyn Carman and Jessica Bottrall, providing a balance of clinical and management topics to the audience.
On 22 May, a dinner gettogether was held at Fine & Fettle with guest Mario Aparicio speaking on the implementation of digital workflow at our practice. His presentation had enlightened many on the positive impact of technology on daily operation. All enjoyed a fantastic evening of great food and company.
On popular demand we are offering a face-to-face mental health first aid course in Adelaide on Saturday 27 and Sunday 28 July. This accredited course is presented by our own Marcy Patsanza-Mkonto and all participants who complete the course will receive the MHFA certificate which is valid for three years.
Come along on Friday 2 August to the Kooyonga Golf Club for a full day of superb education and networking. Relax and enjoy the sweeping panoramic views of the green while updating and upskilling yourself on antibiotic prophylaxis, special



care, TMJ, sleep disorders and many more from our expert presenters.
For all the details please REGISTER
The DHAA has also teamed up with the Academy of Impact Mastery to offer a workshop “Implants and the Dental Hygienists/
OHTs” on 16 August. DHAA members receive a huge 20% discount on the course fee. For more information CLICK HERE https://www. academyforimplantmastery. com/service-page/implantsand-the-hygienist-oht LOG IN to register and get that great discount?
For all the latest info on DHAA events please visit www.dhaa.info/events
TasTAS Contacts:
Chair Karen Lam chairtas@dhaa.info
Staff Bill Suen bill.suen@dhaa.info
n We farewell TAS Chair Karen Lam who resigned from the chair’s role in May. Karen has been instrumental in organising so many great events for our Tasmanian members over the past two years and we are grateful for her dedication and hard work. Before she left, Karen ran another great education day for our members on Saturday 11 May at the Tonic Bar, Country Club Launceston. We were fortunate to have highly regarded presenters including A/Professor Gary Kilov AM, respiratory & sleep physician Dr James Markos, A/Professor Catherine Butler and DHAA life member for former director Hellen Checker presented a variety of hot
“ We are now seeking expression of interest for volunteers to take the Tasmania chair’s role, or to help out in planning and running TAS events ”
topics covering sleep apnea, diabetes, oral microbiome, mind-body-mouth connection and alternative medicine in dentistry. Attendees were also treated with lots of samples and giveaways from sponsors and the DHAA.
We are now seeking expression of interest for volunteers to take the TAS chair’s role, or to help out in planning and running TAS events. The next scheduled event will be a full day in Hobart on Saturday 16 November. If you are able to help, please email bill.suen@ dhaa.info.
VicVic Contacts
Director Roisin McGrath directorvic@dhaa.info
Chair Cathryn Carboon chairvic@dhaa.info
Deputy Chair Sarah Laing contactvic@dhaa.info
n Together with the ADA Victorian Brunch, we are offering a face to face mental health first aid course on Saturday 20 and Sunday 21 July at the ADA Victorian training room in South Yarra. The course will run for two full days and places are limited so please REGISTER ASAP.
The next Victorian event will be a full day of
“
Congratulations to Melbourne University graduate Toan Nguyen who was presented with the DHAA Award for exhibiting the best clinical skills”
exceptional speakers, hosted at the stylish Courtyard by Marriott, inspired by the beautiful tranquil surrounds of Flagstaff Gardens in the city. The program of six hours CPD covers a range of innovations in diagnosis, mobile and minimal intervention dentistry, large language models in dentistry, paediatric special needs as well as exploring opportunities in innovative private practice for OHPs. Hit the link below for further details and to REGISTER : Congratulations to Melbourne University graduate Toan Nguyen who was presented with the DHAA Award for exhibiting the best clinical skills, with an emphasis towards patient care and management by CEO Bill Suen at the 2024 Melbourne Dental School Awards Ceremony on 1 May. We also congratulate Olivia Tan for winning the La Trobe University DHAA Award. Her reflection is published in this issue of the DHAA Bulletin. Click here to read it.
WA Contacts
Director: Ron Knevel directorwa@dhaa.info
Deputy Chair: Michelle Wrights contactwa@dhaa.info
Staff: Bill Suen bill.suen@dhaa.info
n It was a near full house at the education day for WA at Aloft Perth on 4 May. Attendees to this urbanstyle and award-winning venue were treated with great decor to support its exceptional education program. Topics from expert
“ The next WA event will be Saturday 30 November for a half-day end-of-year celebration”
speakers included dental infections, special needs dentistry, volunteerism in domestic violence space and endocarditis.
The next WA event will be Saturday 30 November for a half-day end-ofyear celebration. The WA Committee is at present planning for this highly popular event so please keep your eyes out for further information to be released in due course, but mark it in your diary for the time being. n
www.dhaa.info