THE POWER OF TOGETHERNESS







It is our great pleasure to make this joint announcement on behalf of the Australian Dental and Oral Health Therapists’ Association Ltd (ADOHTA) and Dental Hygienists Association of Australia Limited (DHAA).
At the respective special general meeting of each association last week, members of both associations overwhelmingly supported and passed the special resolution to establish a new peak professional association to represent and support Oral Health Practitioners (OPHs, including Dental Hygienists, Dental Therapists and Oral Health Therapists) in Australia.
The new association will be called Oral Health Association of Australia Ltd (OHAA). It is anticipated that the OHAA will take over full operation from ADOHTA and DHAA on 1 July 2025. It will offer streamlined and fit-for-purpose services, highquality CPD, and significantly enhanced representation for OHPs in Australia.
We would like to express our heartfelt thanks to our fellow board directors, the project team Towards One Professional Association (TOPA) Working Group, external stakeholders and the many members of both associations who provided their advice and support over the past five years leading to this momentous milestone for the profession.
In the meantime, the ADOHTA and DHAA will continue to operate as usual to support our own members until the end of June 2025, while work has begun behind the scene to prepare for the launch of the unified new association in July.
We will keep you up to date of any further progress on this exciting project.

Jessica Pennay Jinous Eighani-Roushani President President
Australian Dental and Oral Health Therapists’ Association
Dental Hygienists Association of Australia

MY SECOND TERM as DHAA President concluded on 30 November and this is my last President’s report. I congratulate Jinous-Eighani-Roushani who has taken over as the incoming President at the recent board meeting.
I would like to thank my fellow board directors for their support and hard work during my tenure. We worked as a cohesive team and I am proud to reflect on the key achievements we have made together over the past year, which have strengthened our association and advanced the profession of oral health practitioners across the country.
Here are some of the significant milestones we have accomplished:
Provider numbers implementation: A major milestone for our profession, we successfully implemented provider numbers, and now all private health insurers are on board. This has been a crucial step in expanding access to oral health services for patients.
Membership and PI insurance: We continue to offer comprehensive professional indemnity (PI) insurance, including 24/7 clinical advisory support for members, ensuring they feel supported in all aspects of their professional practice.
Sydney ADOHTA/DHAA National Congress 2024: This was just completed last month, and I’m pleased to report that we welcomed more than 450 delegates at our inaugural ADOHTA/DHAA congress in Sydney. The event was an incredible success, fostering collaboration and showcasing the latest developments in oral health.
Community Outreach Oral Health Promotion sessions: We have expanded our engagement with local communities, offering oral health promotion sessions that align with our mission to improve public oral health and raise awareness about preventive care.
Financial management: Thanks to prudent financial management, we ended the financial year with a profit of over $190,000, putting the association in a strong position to continue investing in member services and future initiatives.
Future Leaders Program: This year we launched the Future Leaders Program, aimed at developing the next generation of leaders in dental hygiene. We are thrilled to have selected 18 participants who are already showing great promise as they embark on this journey.
In addition to these key achievements, representation at federal and state levels has been a cornerstone of our advocacy efforts. This year, the DHAA has contributed to critical policy discussions through various submissions and consultations, including: Federal budget submission, advocating for policies that support dental hygienists and enhance oral health care delivery.
Continued on page 4

Bill Suen

Carol Tran

A meeting of like minds
We take a look at what happened at the first joint DHAA and ADOHTA event.
Your questions answered.
Get your online CPD fix
Enjoy learning from home.
Polyworking and portfolio careers: A new path for dental professionals. 20 STIs and oral health
What oral health care professionals need to know about STIs.
32 A special feeling
One woman’s journey to fulfilment in special needs dentistry. 34 Erosive tooth wear
We look at the causes, prevention and treatment of tooth erosion. 36 All the best for Christmas
Introducing and thanking our corporate members.
Part two of a series that looks at end-stage disease presentations.
State of the Nation
Our regular round-up of state happenings.
Continued from page 3
Multiple Ahpra, TGA and DBA consultation responses, ensuring that the evolving regulatory landscape considers the needs of our profession.
Briefings for key federal representatives, including Dr. Mike Freelander and The Hon. Emma McBride, highlighting the importance of oral health in public health policy.
Additional submission to the Senate Select Committee into the provision of and access to dental services in Australia, advocating for better access to preventive dental services.
I will continue to be the DHAA Queensland Director and work on the Mouth Matters Campaign to seek access to both Medicare Allied Health Item code for Chronic Diseases, as well as the GP Work Force Incentive Program so that Oral Health Practitioners are funded to provide oral health assessment and hygiene education in the primary care setting.
These activities reflect our commitment to empowering our members, advancing the profession, and improving oral health outcomes for the broader community.
I would like to pay special tribute to Michelle Kuss who retired from the DHAA board in October. Besides being an effective board director, her exceptional effort as Treasurer over the past six years had been a key factor of our great financial position through some fairly challenging periods. Michelle has left a big shoe for the board to fill for sure.
Thank you for your dedication, engagement, and support in making this year such a success. Together, we are building a strong future for dental hygiene in Australia. With the festive season approaching, I would also like to wish everyone a joyful time with your family, and look forward to seeing you in the New Year.
Dr Carol Tran
Outgoing DHAA President
Three professions, two associations – and one fantastic combined oral health congress! We take a look at what happened at the first joint DHAA and ADOHTA event
By Melanie Aley
How exciting to finally have a combined congress, with members of both ADOHTA and DHAA coming together to plan, organise, and attend this groundbreaking event! It was wonderful to have dental hygiene, dental therapy and oral health therapy colleagues (plus a few dentists) all in the same venue, enjoying a program designed to cover our diverse range of interests and passions.
There was so much to learn across the three days – practical workshops designed to improve your clinical practice, internationally recognised keynote speakers presenting the latest evidence on paediatrics, periodontics, and oral care for the aged, and an array of early-career and experienced researchers presenting their findings in the concurrent sessions.
The short, sharp nature of the concurrent sessions meant researchers had to get their point across clearly and quickly – I was surprised to learn that our oral health can impact our heart health in as little as three weeks, and the early childhood caries related hospital admissions are greater than other preventable diseases like asthmas – thanks to Lauren Church and Rebecca Chen for the insights.
Holistic sessions on wellbeing and mindful movement also helped remind us that we need to look after
ourselves to be able to look after our patients. The Student of the Year competition saw three outstanding students present their inspiring oral health initiatives to an expert panel and captive audience, leaving us in no doubt that the future of our profession is bright. (Go to page 10 to find out more).
For me, connecting with familiar faces, and new and interesting conversations with fresh faces, is the most valuable part of any conference. The welcome drinks and generous breaks provided
“I was surprised to learn that our oral health can impact our heart health in as little as three weeks!”
ample time to catch-up with friends, colleagues and students (both past and present), share ideas and perspectives, and introduce likeminded peers. It also provided a great opportunity to chat with our industry partners, and learn about all the latest innovations in oral care products and technologies. I love being able to try out all the new flavours/toys/gadgets when I get home!
The Gala Dinner is always a highlight at conferences, providing a opportunity to enjoy the>>







“I really enjoy being a part of the professional community and am looking forward to a single professional association in the future”
evening with your peers. While I didn’t personally make it to the Gala Dinner this year (an eight-week-old baby will do that to you!) However, I heard that a great time was had by all, and I admired all the glitz and sparkles in the array of social media posts and on a fair few glittery faces the next day!
Given I couldn’t get to every session, I asked a couple of other delegates to share why they registered for the conference, their favourite presentation and their conference highlights.
”I registered for the symposium for professional growth – to enhance my knowledge and skill in dentistry and
keep up to date with the latest research and advancements.
”My favourite presentation was Enamel Matrix Derivative in Periodontal Regeneration by Dr Ehsan Mellati. Speaker was very knowledgeable and provided a current perspective by sharing case studies. A very interesting topic.
”The highlight for me was the networking opportunities and it was great seeing familiar faces, catch up while meeting new people with shared interests!”
Dorothy Koh OHT and PhD student
“I registered for the symposium because I was excited to be a part of the first joint DHAA and ADOHTA Congress. It was a great opportunity for both associations to come together to further enhance the future of our professions. It’s always great to be able to meet new individuals and catch up with past and present colleagues!
“I thoroughly enjoyed all the presentations especially the
presentations on Wellness by Associate Professor Melanie Aley and the Yoga by Patrick Westhoff. Given burnout is such a prominent issue within today’s society, it was great to see strategies to overcome this as well as physical exercises to reduce the risk of musculoskeletal damage.
“I think the highlight for me was being able to see our two associations come together with so many individuals from all three professions and unite to have one joint congress. I loved catching up with so many familiar and new faces and look forward to seeing how the new joint association unfolds!”
Nathan Aulsebrook Oral Health Therapist and Lecturer
Final thoughts: I really enjoy being a part of the professional community that is the DHAA, and am looking forward to a single professional association in the future were we can have a diverse, inclusive oral health community with our ADOHTA colleagues. This congress was such a positive sign of things to come! n




CONGRATULATIONS TO BEST poster winner Lauren Church, and best paper winners Jennifer Ha, Aisha Alie Nadif, Amy Patterson, Grace Wong and Lauren Church with their excellent presentation at the Congress.
DHAA members are encouraged to share their personal experience and expertise with colleagues through these contributed paper and poster sessions in the coming Congress.
Lauren Church’s award winning poster abstract is as follows:
Title
Can oral hygiene practices impact on the risk, incidence, and mortality in cardiometobolic diseases? A systematic review.
Rationale
To evaluate if oral hygiene practices including: toothbrushing, interdental cleaning, toothpaste and/or mouthwash use impact on the risk, incidence, and/or mortality rate of cardiometabolic conditions.
Method
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement. The review protocol is registered with PROSPERO ID: CRD42021269584. Searches were conducted using electronic databases: MEDLINE, EMBASE, Scopus, and CINAHL, as well as grey literature and hand searching.
Results
Forty-eight eligibles studies were identified. Toothbrushing
and interdental cleaning were found to have positive impacts on cardiometabolic disease risk, incidence, and mortality. While the benefits of mouthwash proved inconclusive, with a potential detrimental impact. Toothpaste was not independently associated with disease outcomes.
Conclusion
Interdental cleaning daily, followed by twice daily toothbrushing for at least two minutes has significant positive impacts on cardiometabolic disease outcomes. The provision of basic oral health education should be expanded beyond dental setting and integrated into routine health messages for patients with cardiometabolic diseases.
Clinical significance
Oral and cardiometabolic diseases are major public health issues. Oral health education is rarely provided outside of the dental clinic. This systematic review highlights the importance of simple oral health practices in reducing cardiometabolic risk and could encourage non-dental clinicians to integrate this information into general health promotion for patients with chronic disease.
A round up of the great work being done by our volunteers to better our profession

Bill Suen DHAA CEO
LAST MONTH’S INAUGURAL joint ADOHTA and DHAA Oral Health Congress at the Sydney Hilton was a great success with over 450 delegates attending the three day education program and social functions. Besides the usual invited speakers we had nearly 40 colleagues participating in the contributed paper and poster sessions. They generously shared their personal experiences and expertise as well as some academic research projects through these presentations. Congratulations to best poster winner Lauren Church, and best paper winners Jennifer Ha, Aisha Alie Nadif, Amy Patterson, Grace Wong and Lauren Church with their excellent and inspiring presentations at the Congress.
The 2024 DHAA Oral health Award was presented to Dr Victoria Perchyonok at the Congress Gala Dinner. Dr. Perchyonok’s voluntary contributions, leadership in community initiatives, and extensive research efforts exemplify a level of commitment that truly sets her apart in the oral health profession. Her accomplishments have not only advanced the field of oral health but have also had a direct and meaningful impact on the health and wellbeing of the public, making her an exemplary leader and advocate for her profession and the most worthwhile recipient for the award.
The 2024 DHAA Oral Health Student
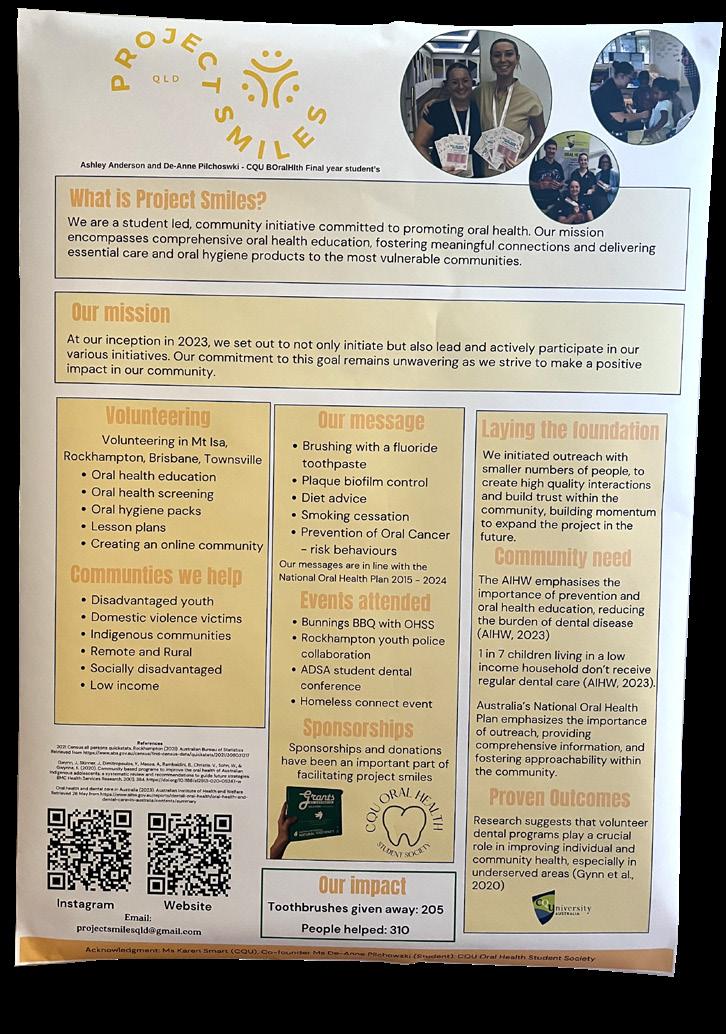
of the Year finalists were Ashley Anderson (Central Queensland University), Allison Walsh (La Trobe University) and Tahmina Rahimy (University of Sydney). It was a tight contest and the judges spent an extensive length of time to determine the final winner and the 2024 national title eventually went to Ashley Anderson for her exceptional involvement with the profession and involvement with academic life. Her winning project is ‘Project Smiles’ which is a student-led initiative to promote oral health to target communities. CQU has now won the competition two years in a row and we extend our congratulations to all finalists for their great work.
Life members Rhonda Kremmer (WA) and Cathryn Carboon (VIC) received their life membership certificate from DHAA President Dr Carol Tran at the Congress. It was inspiring to hear about their exceptional career achievements and enduing contributions to both the DHAA and the profession. A big thank you and congratulations to both legends. Please note that next year’s Congress will be held on the Gold Coast, Queensland from 16-18 October 2025. Please mark this in your diary and be ready to attend the eminent oral health event of the year.
The DHAA Future Leaders Program had its first session with facilitator Professor Nicky Fitzpatrick and Dr Trudy Lin at the beginning of November with 18 participants chosen through a stringent selection process. The participants are Angie Ioannidis, Belinda Hines, Courtney Dicken, Courtney Rutjens, Gemma Collins, Jessica Horwood, Jesse Kourakis,
Michelle Cantwell, Michaela Pitcaithly, Michelle Wright, Madara Dreimane, Marcy Patsanza-Mkonto, Maryam Slewa, Payal Nand, Rachael Walton, Sarah Laing, Shivani Kashyap and Wan Ying Chia. The program will run for the next six months and concludes in May with the aim of developing an ongoing leadership and mentoring program for the profession with the support of our future leaders.
As the returning officer and company secretary of the DHAA, I am pleased to inform you of the new DHAA Board:
• President: Jinous Eighani-Roushani
• Vice President: Carol Tran
• Directors: Roisin McGrath, Amy McDermott, Cheryl Dey, Ron Knevel, Carmen Abramich
We farewell Michelle Kuss who retired from the board after serving as director and treasurer since 2019. We also say goodbye to Christina Zerk who left her DHAA staff role to pursue a new career in IT consulting in October. We wish her well and we are thankful that she will continue to support the DHAA as a member and volunteer.
As 2024 draws to a close, I would like to thank our president Dr Carol Tran, the DHAA Board and my dedicated staff, as well as all the committee members and volunteers for their tireless work and advice. It has been the DHAA team that works so well in making everything happen throughout the year. I wish you all a very happy festive season and look forward to seeing you in the new year. n
THE DHAA IS recognising oral health practitioners who are making a meaningful contribution to our profession with the annual DHAA Oral Health Award.
Dental hygienists, oral health therapists and dental therapists share a focus on prevention, and collectively are known as oral health practitioners.
This award recognises the excellent contribution of oral health practitioners at the grass root level in improving health outcomes and the well-being of the general public.
This award seeks to tell the stories of the vital work of the quiet achievers within the oral health profession.
Dr Perchyonok is an oral health therapist with adult scope, who graduated from the University of Melbourne in 2018 and completed the Adult Restorative Course for oral health therapists. She also completed an undergraduate certificate in dementia care from the University of Tasmania as well as numerous short courses in dental management of geriatric and special needs patients as well as advanced paediatric dentistry to provide the best care for our patients of all ages.
Dr Perchyonok has transitioned into the oral health profession after a successful scientific career both nationally and internationally and completing a PhD in Free Radical Chemistry in 2001 from the University of Melbourne. She has authored over 95 publications, authored seven books, 45 book chapters in the areas of dental materials, free radical chemistry and bio-functional dentistry.
She has pursued her passion and scientific interest in biomaterials for dental and health applications and has published extensively in scientific literature as well as well as acts as unit coordinator in dental material and lecturer in Geriatric Dentistry as part of Bachelor of Oral Health program at the University of Melbourne.
Dr Perchyonok combines her passion for delivering evidence-based health care to children and adults. Victoria has been practicing in private practice since graduation and

is a passionate advocate for bringing dental care to anyone in need. She has established numerous charity dental days in conjunction with Ccare to provide free health oral health assessment for elderly and underprivileged participants of the Ccare charity. This work led to several elderly participants being assisted with appropriate referrals and subsidised dental care for the ones at need. She was able to secure sponsorship for this event from NSK and GC as well as several private donors and will continue to seek further opportunities to engage more likeminded clinicians, BOH and dental students as well as anyone who can help to make a difference in the lives of people in need.
She has volunteered her time in mentoring numerous young practitioners as well as presented numerous educational webinars, CPD lectures and seminars in order to share the knowledge, experience and passion in the special area of Geriatric and Paediatric dentistry. The motto is “To provide best patient centred dentistry to everyone in need with the heart and care”
Dr. Perchyonok’s voluntary contributions, leadership in community initiatives, and extensive research efforts exemplify a level of commitment that truly sets her apart in the oral health profession. Her accomplishments have not only advanced the field of oral health but have also had a direct and meaningful impact on the health and wellbeing of the public, making her an exemplary leader and advocate in her profession.
Dr. Perchyonok’s innovative approach, academic achievements, and unwavering dedication to improving oral health outcomes make her the most worthwhile recipient for the 2024 DHAA Oral Health Award. Congratulations. n
HOLIDAY CLOSURES
The DHAA office will be closed for the Christmas and New Year’s holidays from midday Tuesday 24 December 2024. The office will re-open for normal business from Thursday 2 January 2025. If you need urgent advice or service during this time, please contact Bill Suen on 0412 831 669.
We wish all our members and friends a very happy holiday season and a wonderful start to the new year.


WINNER
Ashley Anderson
“I am humbled to win the national title of the 2024 DHAA Student of the Year. I would like to thank the association for the opportunity to be involved in the competition and awarding me the prize.
I am a third-year Bachelor of oral health therapy student at CQUniversity, originally from Brisbane and now based in Rockhampton. My journey into oral health began with a deep passion for improving health outcomes in my community, stemming from my experience as a dental assistant in 2016.
Participating in professional competitions has been an invaluable learning experience. It has sharpened my communication skills, deepened my clinical knowledge, and highlighted the importance of innovation in patient care. These opportunities have also strengthened my confidence in delivering exceptional care while fostering a sense of camaraderie among peers and mentors in the industry.
The Dental Hygienists Association of Australia (DHAA) has been instrumental in my professional growth. As a DHAA representative, I’ve had access to an extensive network of experienced professionals who have generously shared advice and insights. Their support has guided me in preparing for my transition into the workforce, equipping me with skills for leadership, collaboration, and excellence.
Looking ahead, I am excited to begin my career as an oral health therapist, aiming to empower patients with accessible and inclusive care. My ultimate goal is to continue advocating for oral health equity and to explore opportunities to mentor future professionals.
Tahmina Rahimy
“My name is Tahmina Rahimy, and I am currently in my final year of the Bachelor of Oral Health program at the University of Sydney.
My passion for dentistry began during a two-week voluntary work experience in high school, where I assisted chairside in a dental clinic. Although my time there was brief, it provided me with invaluable exposure to patient interactions, the dental field, and the collaborative environment between staff and patients. This experience sparked my interest in dentistry, which has only grown since then.

A pivotal moment in my journey occurred when I had the opportunity to be part of the Student of the Year Competition and present my research on the impact of early childhood illness on enamel development and the onset of severe early childhood caries at the DHAA and ADOHTA Joint National Congress.
Presenting for the DHAA Student of the Year award was both exciting and nerve-wracking, but it was also a chance to showcase a topic I am deeply passionate about—paediatric dentistry. This topic resonated with me personally, as the case I presented involved a member of my extended family. I saw this as an opportunity to explore and highlight the critical connection between early systemic health issues, their impact on enamel development, and the subsequent risk of early childhood caries. This experience reinforced the essential role that OHTs play in the prevention, intervention, and management of
caries, particularly in younger, more vulnerable populations.
The DHAA has played a crucial role in shaping my professional development. Through various events, workshops, and networking opportunities, I’ve connected with experienced professionals who have shared valuable insights about transitioning into the workforce. Their guidance has boosted my confidence and broadened my understanding of the diverse roles OHTs can play in healthcare.

Looking forward, I am eager to continue working in the adult scope of practice while maintaining my focus on paediatric dentistry. I hope to contribute to public health initiatives, especially those that promote early intervention and equitable access to care. I am particularly interested in working with mobile dental services to reach underserved communities. The DHAA competition reaffirmed my commitment to becoming a compassionate and informed practitioner, dedicated to making a positive impact in my community.
FINALIST
Allison Walsh
“Hello, my name is Allison Walsh, I am a third-year graduate student from the Bachelor of Oral Health Science program, including adult scope, at La Trobe University in Bendigo, Victoria. I reside in rural Victoria on a small farm with my family of three kids
and my partner. My home is based in the beautiful Macedon ranges, approximately one hour north west of Melbourne.
One of the reasons I chose to study oral health is that I have a background in dentistry working initially as a dental assistant and then as a dental technician for many years while serving in the Australian Defence Force. Having raised my family in rural Victoria, I understand the challenges with access to oral health care for rural and regional Victorians.
I am passionate about prevention and educating the wider community on how to care for their, and their family’s oral health. Understanding that there are many factors affecting peoples’ daily lives and their motivational levels, I am dedicated to respecting their individual needs without judgement and supporting them to achieve their health goals.
The opportunity to be part of the DHAA student of the year competition and present at the Oral Health Congress was a special highlight for 2024 and has helped me to further develop my networking and presentation skills.
DHAA have been very supporting offering student interaction opportunities with other universities and online learning programs to help support my development. Attending the Oral Health Congress in Sydney last month was a fabulous opportunity to network with other OHTs and hygienists, make new friends, learn valuable information and see what new products are available for my patients, supporting my role as an oral health therapist.
I enjoy finding solutions to solving problems, so I see myself undertaking further studies in the field of oral health and dentistry in my future. I look forward to working with other health professionals with a view to accelerate my holistic understanding of my patients and my ability to support them along their journey to good health. n
Dear DHAA... With the special resolution to create a new association – the Oral Health Association of Australia (OHAA), will the vote be anonymous?
This is a special resolution that is to be voted on at the special general meeting requiring 75% of votes in favour to pass. You can either vote in person at the meeting, or by appointing a proxy. Online proxy is allowed but you will need to nominate your proxy by identifying both yourself and your proxy so that your vote can be counted at the special general meeting. This is different from the online election of directors where it is conducted via a secret ballot and the votes are anonymous.
Dear DHAA... I have just started my own practice and would like to run an initial promotion to offer a gift voucher and entry into a competition for a significant prize. I just want to check if I am permitted to do so? Ahpra has very stringent guidelines on advertising for health services. Please refer to this link. We generally advise members not to use incentives to entice people to seek health services as it is extremely difficult to meet the stringent Ahpra requirements and there are too many grey areas (e.g. the requirements to provide full details of the terms and conditions of the competition, and reference to the code of conduct).
We are not allowed to encourage the indiscriminate or unnecessary use of regulated health services in anyway, including through our marketing activities such as competitions or social media posts.
Dear DHAA... I was wondering if you could please provide guidance in regards to treating individuals who are currently going through active chemotherapy treatment (both oral and IV infusions). There are a number of considerations for oral health practitioners: • You need to gain consent from your patient to speak with
their treating physician
• What generation of chemotherapy being used (both oral and infusions)
• You need to understand any baseline changes in their blood picture in particular to White blood cell count, Neutrophils and any inflammatory marker changes ( if any)
• Some of the newer generation treatments have minimal exclusions, but you need to know this conclusively
• Gain the information, talk to the dentist and the specialist in particular to see if there are any risks in creating and infection due to lowered immune status.

Dear DHAA... We have recently started our own mobile business and are still waiting for our HICAPS machine to arrive. Are we able to claim CDBS through PRODA while we wait?
Yes, you can put in a manual claim via Proda, and it should be fairly straightforward if you follow the instructions.
Dear DHAA... I’m looking for clarification regarding taking of an orthopantomography (OPG) on a cone beam computed tomography (CBCT) machine.
I have trained and am licensed in OPG but not CBCT. My practice has just swapped the old
OPG for a CBCT unit.
My understanding is I can’t use this machine to take OPG as it is CBCT and this requires a completion of course and machine specific training course.
It depends on whether the CBCT machine has a separate OPG function. Or if it takes a CBCT and converts it into an OPG?
If it has a separate function - (most machines have a button for OPG and a button for CT), you can still take an OPG on it without further training. n
If you have a question to ask then please email it to bulletin@dhaa.info

Our regular update on some great reading to improve your skills and top up your CPD hours
Take advantage of any downtime by studying at home and keep racking up your CPD points. Subjects in this edition include; antimicrobial management, oral health integration into rural and remote communities and oral care for cardiovascular patients. Whatever your interest, we strive to include something for everyone.
Risk of tooth loss with supportive periodontal care
• Journal of Clinical Periodontology, Volume 51, issue 5 (May 2024), 583-595
• CPD hours: 0.25 scientific
The risk of tooth loss during supportive periodontal care has been examined in only a few studies. These studies – predominantly retrospective –demonstrated a correlation between tooth loss and background factors including smoking, diabetes, and high plaque scores. Local factors of

relevance were tooth type, furcation involvement, probing pocket depth (PPD), clinical attachment level (CAL), tooth mobility, bleeding on probing, angular bony defects, and endodontic pathology. Accurate tooth-by-tooth prognosis is of importance in clinical decision-making and in patient communication.
A prospective observational study
was carried out on previously treated periodontitis patients followed up for five years in SPC. The risk profile (low, moderate, high) of each patient based on periodontal risk assessment (PRA) scoring at baseline was evaluated, and tooth loss rates were analysed.
Two hundred patients were included in the study, and 143 had five-year follow-up data available

Poor lifestyle choices demonstrate worse clinical outcomes

for analysis. Overall, the tooth loss rate of periodontitis patients in this prospective cohort study under SPC in private practice was low. Both toothbased and patient-based prognostic systems can identify high-risk cases, but their positive predictive value should be improved.
Healthy lifestyles are associated with a better response to periodontal therapy: A prospective cohort study
• Journal of Clinical Periodontilogy, Volume 50, Issue 8, 1089-1100
• CPD hours: 0.5 scientific
To evaluate the association between lifestyle behaviours and clinical periodontal outcomes following steps 1/2 of periodontal therapy.
A total of 120 subjects with untreated Stage II/III periodontitis participated in this study.
Subjects with unhealthy lifestyle behaviours showed worse clinical outcomes three months after Steps 1/2 of periodontal therapy.
Effect of zinc on improving silver diamine fluoride-derived tooth discoloration in vitro
• BMC Oral Health volume 24, Article number: 1410 (2024)
• CPD hours: 0.25 scientific
FIND OUT MORE
Silver Diamine Fluoride (SDF) is effective for arresting dental caries, presenting a valuable non-invasive treatment option in dentistry.
Despite its therapeutic advantages, a significant drawback is the tooth discoloration that follows its application, which can affect patient acceptance.
Addressing this aesthetic concern without diminishing the treatment’s efficacy remains challenging in dental
practice. This study explores strategies to improve the aesthetic outcomes of SDF treatments.
Zinc significantly reduced SDFinduced tooth discoloration in a dosedependent manner without affecting the etched dentin’s micro-hardness and roughness, potentially improving patient acceptance, especially in visible areas of the mouth.
Cultural safety in Australia, discussion paper
• Lowitja Institute; 2024.
• CPD hours: 1 non-scientific
FIND OUT MORE
The Lowitja Institute has released this discussion paper highlighting the need to improve access to quality healthcare, addressing the social determinants of health, and elevating the importance of the cultural determinants of health for Aboriginal and Torres Strait Islander peoples. >>
The paper’s purpose includes proposing recommended and nationally consistent standards, setting a platform for the accreditation of workplace-based cultural safety training, and calling for further action that can lead to cultural safety being embedded and measured at individual and institutional levels in practice and policy across health and human services.
The effect of hemostatic agents and dentin cleansing protocols on shear bond strength of resin composite using universal adhesive: an in vitro study
• BMC Oral Health, volume 24, Article number: 1413 (2024)
• CPD hours: 0.25 scientific
During restoring class II and V cavities with resin composite, hemostatic agents are frequently used to control gingival bleeding and/or gingival fluid to provide a dry field which is crucial for efficient bonding. Hemostatic agents may adversely affect the bonding procedure, thus their removal prior to bonding is essential. The current study evaluates the effect of two hemostatic agents and different dentin cleansing protocols on the shear bond strength of resin composite to dentin using a universal adhesive.
The use of hemostatic agents can adversely affect the bond strength of universal adhesives to dentin.

Phosphoric acid provided the best hemostatic agent-cleansing protocol while katana cleaner and air abrasion demonstrated inferior results.
The loneliness epidemic: a holistic view of its health and economic implications in older age
• Med J Aust || doi: 10.5694/mja2.52414 26 August 2024
• CPD hours: 0.25 non-scientific
Loneliness has been described as an epidemic and is one of the most pressing public health concerns in Australia and internationally.
In contrast to social isolation, which is an objective measure of social interactions and relationships, loneliness is defined as a subjective experience where one perceives a discrepancy between desired and actual social relationships in terms of quality or quantity.
Although it is common and natural to feel lonely at times, prolonged and intense periods of loneliness have been linked to adverse health outcomes. Older
adults are more prone to loneliness and social isolation compared with other age groups. Reasons for this include significant life transitions and events, such as retiring from work, increased financial difficulties, loss of friends and widowhood, changes in living arrangements (eg, transitioning to residential aged care), increase in solitary living, and a decline in both health and independence.
Older people at particular risk of loneliness include those living on low incomes, living with a disability, living in rural areas or with housing stress, who are single, childless or living alone, who are vulnerable or at risk of elder abuse, and those with low levels of literacy or communication technology skills.
A growing body of evidence has highlighted the significant health burden associated with loneliness, with more recent studies also suggesting that loneliness has become an economic problem due to an increase in service use and demand for institutional care. This development requires both effective and cost-effective strategies to tackle loneliness. n



By Associate Professor Melanie Aley
Have you ever thought about mixing things up in your career—taking on a side gig or exploring a passion project alongside your dental practice? That’s exactly what a portfolio career, or polyworking, is all about. Instead of sticking to just one full-time job, polyworkers juggle multiple roles, combining their skills and interests to create a career that’s as unique as they are.
This trend has been growing fast, and for good reason. People today want more flexibility and balance in their lives. The idea of “one job for life” doesn’t feel right for everyone anymore, especially when there are so many ways to explore new opportunities. For dental hygienists and oral health therapists, polyworking might mean balancing clinical work with teaching, consulting, writing, or even something completely different—like starting a wellness business or creating educational content for social media.
Polyworking isn’t just about keeping your career exciting—it’s also packed with practical perks that can make your professional and personal life so much better. For starters, it’s a fantastic way to prevent burnout. Let’s face it, clinical
work can be intense, both physically and mentally. Balancing it with something different, like writing about oral health or consulting for a dental company, gives you a change of pace and a chance to recharge while still staying connected to the field you love.
It’s also smart financially. When you’re polyworking, you’re not relying on a single paycheck. Maybe your consulting work takes a dip during the holidays, but your part-time teaching gig or online course sales pick up the slack. Having multiple income streams creates a safety net, which is a huge relief in a world where things can change quickly.
Another big plus is how it helps you grow. Let’s say you start hosting workshops for new dental hygienists on patient communication. You’re not only sharing what you know—you’re sharpening your own skills too. Teaching, consulting, or creating content can help you develop abilities like public speaking, problem-solving, and even business savvy, all of which make you more versatile and valuable.
security of your clinical role. There’s something deeply satisfying about designing a career that reflects who you are and what matters most to you.
“Polyworking might mean balancing clinical work with teaching, consulting, writing, or even something completely different”
And then there’s the personal side. Polyworking gives you the freedom to explore what really lights you up. Maybe you’ve always loved mentoring others or dreamed of creating a blog about simplifying oral health for everyday people. Polyworking lets you dive into those passions without giving up the
Let’s say you’re a dental hygienist working part-time in a busy clinic. On your days off, you could start a side project offering oral health promotion sessions to schools. This might involve creating simple, engaging presentations for kids and parents about cavity prevention and oral hygiene. These workshops can be scheduled flexibly, allowing you to earn extra income while making a positive impact in your community. Or imagine you’ve developed a knack for explaining dental procedures in ways that patients really connect with. You might use that skill to create a blog or a series of videos aimed at demystifying oral health topics. By sharing content like “Five Myths About Gum Disease,” you could build an online presence that opens doors to opportunities like sponsored content, consulting with dental product companies, or even launching an eBook. Or, if you’ve spent years refining chairside communication skills, why not share your expertise? You could become a speaker at dental conferences

or webinars, offering tips to other hygienists on patient education or building trust. Public speaking can feel intimidating at first, but even small events can help you build confidence and establish yourself as an expert in the field.
If these ideas spark your interest, the first step is self-reflection. What are you passionate about? What do patients or colleagues often praise you for? Once you’ve identified a niche, start small. Set aside a few hours each week to explore your idea, whether it’s writing a draft blog post, reaching out to local schools, or researching dental conferences where you could present. Networking is key, so connect with peers who are already polyworking. Many dental hygienists and oral health therapists share their journeys on
platforms like LinkedIn, Instagram, or professional forums. These connections can offer tips, collaboration opportunities, or just encouragement to get started.
If you need extra skills for your chosen path, don’t worry—there are countless online resources to help. For example, platforms like Coursera offer courses on public speaking, content creation, and marketing, while professional associations often provide training for educators or consultants. For inspiration, check out books like “The Portfolio Career” by Steve Preston or “Rethinking Work” by Julia Hobsbawm.

There are also excellent blogs, podcasts and webinars specifically for dental professionals looking to diversify their careers – just choose a topic and search away!
Polyworking isn’t about doing more; it’s about creating a career that reflects who you are and what you love. Whether you’re mentoring the next generation, designing oral health workshops, or building an online presence, this approach allows you to explore your passions while keeping your clinical work. The possibilities are endless, and your next adventure could be just around the corner. n
Associate Professor Melanie Aley (nee Hayes) is a dental hygienist who has enjoyed a diverse career in clinical practice, teaching, research and management. She has a Masters of Education majoring in Career Development, and after working in multidisciplinary roles, is now an Associate Professor and the Bachelor of Oral Health Program Director at the University of Sydney.
By Margie Steffens OAM, Victoria Perchyonok, Danielle Gibbens and Angie Ioannidis of the DHAA Special Care Dentistry Special Interest Group
CPD 0.5 hours scientific
PART 1
As oral health care professionals, it is essential to document medical histories accurately and remain vigilant about oral conditions that may suggest an underlying systemic issue, such as a sexually transmitted infection (STI). Understanding the oral manifestations of STIs is a key part of our duty of care, especially when observations do not align with a patient’s disclosed medical or social history. This article provides a brief overview of some common STIs— HIV/AIDS, syphilis, gonorrhoea, and chlamydia—and their oral manifestations, along with guidelines for clinical management.
Sexually transmitted infections have been documented throughout history, with early references found in ancient texts like the Hebrew bible
and Egyptian papyri. The terminology has evolved from “venereal disease” (VD) to “sexually transmitted disease” (STD), and now, “sexually transmitted infections” (STIs).
The ancient Greek physician Hippocrates, around 400 BC, described conditions resembling gonorrhoea. In the medieval period, syphilis and gonorrhoea were especially prevalent and are believed to have spread globally through sailors’ travels. Some research suggests that gonorrhoea originated from cattle and syphilis from cattle or sheep, transferring to humans possibly through sexual contact.
In recent times, the incidence of certain STIs has risen dramatically. According to the Medical Journal of Australia, syphilis infections in women of childbearing age increased by 500% between 2011 and 2021.
Around 1981 Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome
(AIDS) created a global concern along with its general and oral health implications.
The following sections provide an overview of STI’s and their oral manifestations:
Human Immunodeficiency Virus (HIV) and acquired immunodeficiency syndrome (AIDS) are significant global health concerns, affecting millions of individuals worldwide.
Oral manifestations are among the earliest indicators of HIV infection and are often critical for diagnosis >>

“According to the Medical Journal of Australia, syphilis infections in women of childbearing age increased by 500% between 2011 and 2021”
and prognosis. As the immune system becomes progressively compromised in HIV and AIDS, patients are more susceptible to opportunistic infections and oral diseases.
Understanding the oral manifestations, the impact of antiretroviral therapy (ART) also referred to as Highly Active Antiretroviral Therapy (HAART) and the dental implications are essential for providing effective oral care and improving the overall quality of life for affected individuals.
Oral lesions are commonly observed in HIV-positive individuals and can be indicative of the progression to AIDS. The prevalence of these lesions varies depending on factors such as immune status, viral load, and ART (HAART) adherence. Common oral manifestations include:
Oral candidiasis, particularly Candida albicans infections, is the most frequent oral manifestation in HIV patients. Pseudomembranous candidiasis presents as creamy white plaques on the buccal mucosa, palate, and tongue, which can be wiped away, leaving a red, erythematous surface. Angular cheilitis and erythematous candidiasis are also prevalent. These infections arise due to the weakened immune system, and persistent oral candidiasis may signal the onset of AIDS.
Caused by Epstein-Barr virus (EBV), oral hairy leukoplakia is characterised by white, corrugated lesions on the lateral borders of the tongue. These lesions are generally asymptomatic and do not scrape off, distinguishing them from candidiasis. OHL is associated with severe immunosuppression and is often a marker of HIV disease progression.
Kaposi’s sarcoma (KS) is an AIDSdefining malignancy that can present in the oral cavity, primarily on the palate, gingiva, or tongue. It appears as reddish-purple lesions that may be flat or raised. KS is associated with human herpesvirus-8 (HHV- 8) and tends to increase in size over time, potentially causing discomfort, pain, and bleeding. (this condition however is less commonly seen now with the advent of HAART, earlier diagnosis and better supportive care)
(NUP) and necrotising ulcerative gingivitis (NUG)
NUP and NUG are severe periodontal diseases associated with HIV infection. They manifest as painful ulceration of the gingival tissue, rapid bone loss, and bleeding. These conditions can progress quickly and
“Understanding the oral manifestations, the impact of antiretroviral therapy (ART) also referred to as Highly Active Antiretroviral Therapy (HAART) and the dental implications are essential for providing effective oral care and improving the overall quality of life for affected individuals”
The introduction of ART has significantly reduced the incidence of many oral lesions associated with HIV. ART works by suppressing viral replication, improving immune function, and reducing the overall viral load. Consequently, patients on ART generally, experience fewer oral opportunistic infections and malignancies. However, there are dental implications associated with long-term ART use, including:
cause significant destruction of oral tissues, leading to tooth loss if untreated.
Recurrent HSV infections, particularly in the form of herpes labialis or intraoral herpes, are more frequent and severe in HIV-positive individuals. The lesions present as painful vesicles that progress to ulceration, commonly on the lips or hard palate.
Oral warts, caused by HPV, are also more common in individuals with HIV. These lesions can present anywhere in the oral cavity and may appear as single or multiple growths, which are usually benign but may cause discomfort or interfere with function.
ART, particularly regimens involving protease inhibitors, can cause xerostomia (dry mouth), increasing the risk for dental caries, periodontal disease, and oral discomfort. Saliva plays a crucial role in maintaining oral health by buffering acids and controlling bacterial growth, so reduced salivary flow necessitates additional preventive care.
Some ART medications have been associated with the development of oral lesions, such as oral ulcers, mucosal pigmentation, and lichenoid reactions. It is important for dental professionals to recognise these side effects and differentiate them from HIV-related oral conditions.
While ART improves immune function, HIV-positive individuals remain at a higher risk for recurrent oral infections. The continued need for vigilant oral hygiene and regular dental visits cannot be overstated in this population.
Providing dental care to patients with HIV/AIDS requires special considerations due to their compromised immune systems and increased susceptibility to oral diseases. The following are key aspects of dental management:
Regular oral examinations are essential for early detection of oral manifestations related to HIV. Dentists should thoroughly assess for signs of candidiasis, oral hairy leukoplakia, and other opportunistic infections. Biopsies may be necessary for definitive diagnoses of suspicious lesions, such as Kaposi’s sarcoma.
Preventive care is critical in HIV-positive patients to reduce the risk of oral infections and complications.
This includes:
• Fluoride treatments, in particular those containing Calcium Phosphate and use of saliva substitutes to prevent dental caries, as many of these patients present with xerostomia.
• Regular scaling and root debridement for patients with periodontal disease.
• Patient education on proper oral hygiene, including brushing with fluoride toothpaste, flossing, and the use of antimicrobial mouthwashes.
Management of oral infections
Prompt treatment of oral infections is vital to prevent systemic complications. For example:
• Antifungal medications like nystatin or fluconazole are used to treat oral candidiasis. >>
“Gonorrhea is of particular interest to dental professionals due to its potential to cause oropharyngeal infections, which are often asymptomatic but can lead to local oral manifestations and systemic complications”
aspect of care for individuals living with HIV and AIDS. Recognising and managing oral manifestations, understanding the effects of HAART on oral health, and providing tailored dental care can significantly improve the quality of life for these patients. Oral Health professionals play a crucial role in the early detection of HIV-related oral conditions and in the long-term management of oral health in this vulnerable population.
• Antiviral agents, such as acyclovir, are indicated for recurrent HSV infections.
• Local and systemic antibiotics may be required for bacterial infections such as NUP and NUG.
Pain management and palliative care
Many oral lesions in HIV-positive patients can be painful, affecting their ability to eat and speak. Dentists, hygienists and oral health therapists must provide appropriate pain management strategies, including topical anaesthetics and analgesics, as well as palliative care for advanced cases like oral Kaposi’s sarcoma.
Interprofessional collaboration
Collaboration between dental professionals and medical teams is essential to optimise the overall health care of HIV-positive individuals. All Oral Health Professionals should work closely with infectious disease specialists and other health care providers to monitor the patient’s immune status and adjust dental care accordingly.
In summary, oral health is a vital
Syphilis is a contagious infectious disease caused by Treponema pallidum, a gram-negative bacterium transmitted primarily through sexual intercourse, blood transfusion, direct contact with lesions, and contaminated objects. In Australia, syphilis is a nationally notifiable disease, and recent years have seen a marked increase in cases. Between 2023 and 2024, 6,103 cases of infectious syphilis were reported, reflecting a broader trend where cases have more than tripled since 2013. This rise indicates that syphilis is no longer limited to specific regions or populations, with cases now spanning urban, regional, and remote areas.
Oral health professionals play a crucial role in recognising syphilisrelated oral manifestations, as the disease often presents with characteristic lesions in the mouth. The dental setting is particularly sensitive to the transmission of syphilis, as contact with patient saliva, blood, or direct lesion contact could lead to potential spread. Patients may also seek treatment for oral lesions associated with syphilis, making it essential for oral health professionals to be vigilant about identifying these symptoms and making appropriate referrals.
Syphilis presents in several stages, each with distinct oral manifestations:
n Primary syphilis
Primary syphilis commonly presents as a single, painless ulcer or chancre at the infection site, although multiple, atypical, or painful lesions can occur. The most frequent locations for these chancres in the oral cavity include the lips, mucosa, lateral tongue, soft palate, gingiva, and tonsils. Lesions typically present as elevated, ulcerated nodules with induration and may have a greyish-white membrane. Additional symptoms may include edema, erythema, and ulcerated tonsils.
n Secondary syphilis
During the secondary stage, syphilis may present with more ulcerated and irregular lesions in the oral cavity. Common manifestations include mucocutaneous lesions and lymphadenopathy. Oral manifestations include multiple mucous patches covered by grey pseudomembrane, surrounded by erythema, often painful and forming “snail-track” ulcers. These are commonly seen on the tongue, faucial pillars, soft palate, and vestibular mucosa.
n Tertiary syphilis
In tertiary syphilis, the infection may spread to affect multiple organs, including the brain, eyes, liver, bones, and joints. Oral manifestations in this stage include granulomatous lesions known as gummas, which start as small ulcers and can enlarge into large, ulcerated masses, frequently seen on the hard palate. The condition may progress to cause significant bone destruction, leading to hard palate perforation or oronasal fistula formation. Atrophic interstitial glossitis,

which results in a fissured appearance of the tongue, can also develop due to fibrosis and hyperkeratosis.
Congenital syphilis, transmitted from mother to child during pregnancy, results in distinctive dental abnormalities. Affected children often present with Hutchinson’s incisors, characterised by barrel-shaped, short, and narrow teeth with a vertical notch at the incisal edge. Molars may show dome-shaped crowns (known as Moon’s molars or bud molars) with enamel hypoplasia.
Although syphilis can affect anyone, certain groups have higher risk, including men who have sex with men, female sexual partners of men who have sex with men, Aboriginal and Torres Strait Islander populations, and infants born to mothers who have not received adequate syphilis screening and treatment during pregnancy.
Diagnosis of syphilis typically involves blood tests, although a swab of an ulcer (chancre) may also be tested if present. Blood tests can detect syphilis as early as three months post-infection, with many cases diagnosed sooner.
The World Health Organisation (WHO) recommends treating syphilis with injectable penicillin (benzathine penicillin G), with one to three doses depending on the stage of the disease.
Due to the frequent occurrence of syphilitic ulcers at various stages in the oral cavity, dental professionals >>
need to be alert and conduct thorough lesion assessments. Primary chancres and secondary mucosal lesions can have nonspecific appearances, leading to potential misdiagnosis as fungal infections, aphthous stomatitis, or stress-related issues. Incorrect treatments, such as antifungals or corticosteroids, will not effectively address syphilis and may even worsen the condition.
Oral health professionals should avoid biopsy on suspected syphilitic lesions, as the histopathology of syphilis is nonspecific and shows only inflammatory changes. Dental treatment unrelated to syphilis management should be postponed until lesions resolve. Strict adherence to standard infection control practices is essential to protect healthcare providers and patients from potential transmission.
Gonorrhoea is a sexually transmitted infection (STI) caused by the gramnegative bacterium Neisseria gonorrhoeae. This pathogen primarily infects mucous membranes of the genital tract but can also affect the oropharynx, eyes, rectum, and, less commonly, joints and blood. Gonorrhea is of particular interest to dental professionals due to its potential to cause oropharyngeal infections, which are often asymptomatic but can lead to local oral manifestations and systemic complications. The rising incidence of antibiotic-resistant strains of N. gonorrhoeae further emphasises the need for vigilance and appropriate management.
Gonorrhoea is one of the most commonly reported STIs globally. In recent years, cases have surged, partly due to increasing antibiotic resistance and limited public awareness. In 2023, the World Health Organisation (WHO) reported that approximately 87 million new cases of gonorrhoea occur globally each year. The infection disproportionately affects young adults and men who have sex with men (MSM), though it can infect any sexually active individual.
Transmission of N. gonorrhoeae occurs through direct contact with infected body fluids, including during vaginal, anal, or oral sex. Oropharyngeal gonorrhoea is most acquired through oral-genital contact and can be a source of infection transmission even in the absence of symptoms. Dental professionals should be aware of the potential for transmission through exposure to saliva or respiratory droplets, especially in patients with active oropharyngeal infections.
Oropharyngeal gonorrhoea often presents asymptomatically, which can make it difficult to diagnose. However, in symptomatic cases, oral manifestations may include:
Pharyngitis: Gonococcal pharyngitis is the most common oropharyngeal manifestation. It may present as a sore throat, erythema, and inflammation of the pharynx, often resembling streptococcal pharyngitis. It is important to distinguish between bacterial pharyngitis and viral causes to provide accurate treatment.
Tonsillitis: Patients may develop swollen, tender tonsils with erythema
“In Australia, syphilis is a nationally notifiable disease, and recent years have seen a marked increase in cases”
and exudate. In some cases, the tonsils can have a white or yellowish coating, which can be misinterpreted as bacterial tonsillitis or even a fungal infection.
Ulcerative lesions: Less frequently, gonorrhoea may cause ulcerations on the oral mucosa, lips, and gingiva. These lesions can mimic herpetic stomatitis or aphthous ulcers, making diagnosis challenging without laboratory confirmation.
Mucopurulent discharge: A hallmark of gonococcal infection is mucopurulent discharge. In the oropharynx, this may appear as a yellowish or white exudate on the posterior pharynx or tonsils. This discharge can be mistaken for other infections, such as bacterial pharyngitis.
Lymphadenopathy: Infected individuals may present with enlarged, tender cervical lymph nodes, particularly if the infection has spread to the regional lymphatic system.
Halitosis: The presence of exudative discharge and tissue inflammation can lead to halitosis (bad breath), which may be noticeable to both the patient and the clinician.

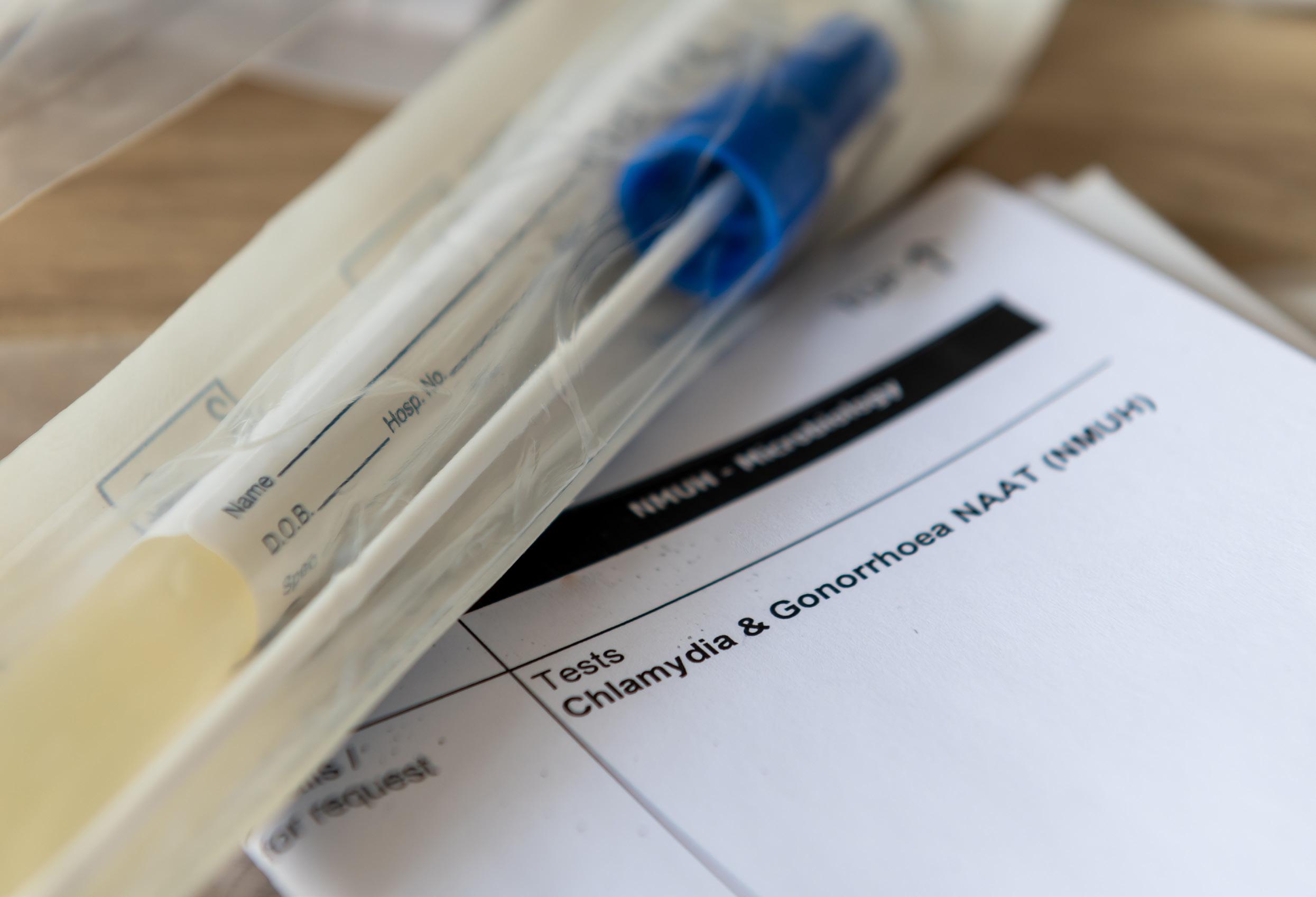
Diagnosing oropharyngeal gonorrhoea can be challenging due to its asymptomatic nature in many cases. However, if gonorrhoea is suspected based on clinical findings, a sample can be collected from the oropharynx using a sterile swab for nucleic acid amplification testing (NAAT), which is highly sensitive and specific. Traditional culture methods are also used but are less sensitive for oropharyngeal specimens compared to genital samples. NAAT remains the preferred method for its high sensitivity.
Due to the potential for asymptomatic oropharyngeal gonorrhoea, dental professionals may encounter patients with undiagnosed infections, posing a risk for cross-infection. The following considerations are crucial in a dental setting:
Infection control and standard precautions:
Dental professionals should adhere to strict infection control practices, including the use of personal protective equipment (PPE) such as gloves, masks, and eye protection. Proper sterilisation of dental instruments and surfaces is essential to prevent potential transmission through contact with saliva or respiratory droplets.
Differential diagnosis:
Oral health professionals should be aware of the signs of oropharyngeal gonorrhoea and consider it in the differential diagnosis for patients presenting with pharyngitis, tonsillitis, or unexplained oral lesions, particularly in those with risk factors for STIs. Misdiagnosis can lead to inappropriate treatment and persistence of infection.
Avoiding aerosol-generating procedures:
For patients with suspected or confirmed gonococcal infection, dental
practitioners should minimise aerosolgenerating procedures (AGPs), such as ultrasonic scaling, to reduce the risk of pathogen spread. If AGPs are necessary, they should be performed with appropriate PPE and high-efficiency suction.
Patient education and referrals: If oropharyngeal gonorrhoea is suspected, dental professionals should refer the patient to a physician or sexual health clinic for confirmation and treatment. Educating patients about safe sexual practices and the potential oral health implications of STIs is also essential in managing and preventing gonorrhoea and other infections.
Antibiotic resistance concerns: N. gonorrhoeae has developed resistance to multiple antibiotics over the years, including penicillin, tetracycline, and fluoroquinolones. As such, treatment protocols are limited, and current guidelines recommend >>
combination therapy with ceftriaxone and azithromycin or doxycycline.
Dental professionals should be aware of these resistance patterns, as delayed or inadequate treatment can lead to complications and continued transmission.
Untreated gonorrhoea can lead to various complications, some of which may affect the oral cavity indirectly.
These include:
Disseminated gonococcal infection (DGI):
Gonorrhoea can spread to other parts of the body, leading to joint pain (arthritis), skin lesions, and endocarditis. Oral health professionals should be aware that patients with systemic symptoms may have DGI, which requires urgent treatment.
Patients with gonorrhoea are at higher risk of acquiring other STIs, including HIV. This is of particular importance to oral health professionals, as they may be exposed to multiple pathogens if a patient is co-infected. Dual testing for STIs, including HIV, is often recommended for patients diagnosed with gonorrhoea.
In summary, gonorrhoea presents unique challenges and considerations for oral health professionals due to its potential oropharyngeal manifestations and the risk of asymptomatic transmission. Awareness of oral presentations of gonorrhoea, combined with adherence to strict infection control protocols and appropriate patient referrals, can aid in managing this infection effectively within the

dental setting. As antibiotic-resistant N. gonorrhoeae strains continue to emerge, vigilant monitoring, accurate diagnosis, and adherence to treatment guidelines remain crucial in reducing the spread and impact of this STI.
Chlamydia is a common sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis, known primarily for affecting the genital tract but also capable of infecting other areas, including the oropharynx. Oral chlamydia is less common than genital chlamydia, with studies indicating that while about 10% of people visiting STI clinics in the United States have genital chlamydia, only approximately 1.5% have an oral chlamydia infection. Dental professionals must be aware of chlamydia’s potential oral
“Chronic infections [of chlamydia], particularly if undiagnosed, may increase the risk of periodontal disease due to the inflammatory responses elicited by the pathogen”
manifestations, as asymptomatic cases can lead to undiagnosed infections that may contribute to secondary health concerns.
Oral chlamydia can occur when C. trachomatis bacteria contact mucus membranes in the mouth, typically through oral-genital contact. However, the pathogen more readily infects the mucosal surfaces of the genital area than those in the mouth, likely due to differences in tissue composition and local immune responses in these areas. Consequently, oral infections are less common, yet possible, and can be a source of transmission.
Oral chlamydia often presents asymptomatically, complicating diagnosis. When symptoms do arise, they can be non-specific and are easily confused with other common oral and systemic conditions, such as strep throat, allergies, or viral infections.
Common oral symptoms of chlamydia include:
• Sore Throat: Patients may experience mild to severe throat pain.
• Mouth Pain and Sores: Persistent oral discomfort or ulcer-like sores that do not readily heal may indicate infection.
• Tonsil Inflammation: Swelling and erythema of the tonsils are common and can be confused with bacterial tonsillitis.
• Perioral Lesions: Sores or inflammation may appear around the lips and mouth.
• Erythema and Leukoplakia: Redness in the oral cavity, especially on the soft palate, and white patches (leukoplakia) in the throat are possible.
• Fever: Systemic symptoms such as fever may arise, indicating the body’s immune response to the infection.
• Lymphadenopathy: Swollen lymph nodes in the neck may accompany oral symptoms.
• Risk of Dental Problems: Although rare, untreated chlamydia can lead to secondary infections that may contribute to periodontal disease or other dental issues.
Due to these vague symptoms, dental professionals should consider chlamydia in the differential diagnosis for patients presenting with persistent sore throat, oral sores, or tonsil inflammation, especially those with known STI risk factors.
Oral chlamydia can occasionally contribute to secondary infections and inflammatory responses that impact oral health. Chronic infections, particularly if undiagnosed, may increase the risk of periodontal disease due to the inflammatory responses elicited by the pathogen. Additionally, oral manifestations, though rare, can cause discomfort that affects patients’ ability to maintain optimal oral hygiene, potentially leading to complications such as gingivitis or periodontal disease over time.
Diagnosing oral chlamydia can be challenging due to its asymptomatic nature and non-specific symptoms. When oral chlamydia is suspected based on clinical presentation, a nucleic acid amplification test (NAAT) using a swab from the oropharynx can confirm the presence of C. trachomatis. However, oral testing for chlamydia is not routinely performed and may require specific patient consent and cooperation. >>

“Understanding the oral implications of STIs is crucial for oral health care professionals, not only for patient health but also as part of our duty to refer and collaborate with allied health providers when needed”
Chlamydia is generally treatable with antibiotics, with doxycycline or azithromycin being commonly prescribed. A single dose is often effective, but if a secondary infection is present, extended treatment may be required. Dental professionals encountering patients with suspected or confirmed oral chlamydia should provide referrals to appropriate healthcare providers for definitive diagnosis and management.
implications and professional considerations
Infection control and precautions
As with all STIs, strict adherence to infection control protocols is critical. Dental professionals should use appropriate personal protective equipment (PPE) and take precautions to minimise potential crosscontamination when working with saliva or respiratory droplets.
Patient education and referrals: Patients should be educated on the potential oral health implications of STIs and advised on safe sexual practices to reduce transmission. If oral chlamydia is suspected, referral to a sexual health clinic or physician is necessary for confirmation and treatment.
Preventive care for secondary infections: Patients diagnosed with oral chlamydia should be monitored for secondary infections and encouraged to maintain good oral hygiene. Dental professionals should remain vigilant for signs of periodontal disease or other complications.
Awareness of symptom overlap: Given that oral chlamydia symptoms may mimic other common conditions, a thorough patient history and awareness of risk factors are essential. Misdiagnosis can lead to inadequate treatment and persistence of infection, emphasising the importance of differential diagnosis in cases of unexplained oral symptoms. In summary: While oral chlamydia
remains a less common manifestation of C. trachomatis infection, awareness of its potential oral implications is essential for dental professionals. Recognising symptoms, adhering to infection control protocols, and providing patient education and referrals are fundamental steps in managing this STI in dental settings. Appropriate diagnosis and treatment are crucial for reducing transmission and preventing secondary complications, ultimately contributing to improved patient outcomes.
Conclusion: Understanding the oral implications of STIs is crucial for oral health care professionals, not only for patient health but also as part of our duty to refer and collaborate with allied health providers when needed. HIV/ AIDS, syphilis, gonorrhea, and chlamydia are a few of the many STIs that may present with oral manifestations. With careful documentation, vigilant observation, and open communication, oral health professionals can help mitigate the spread and effects of STIs, contributing to better systemic health outcomes. n
General references:
Broadgate GP. The History Of STIs From The Earliest Records To Modern Day. Available at: https://www. broadgategp.co.uk/the-history-of-stis-from-the-earliestrecords-to-modern-day/.
Understanding Animal Research. Available at: https://www. understandinganimalresearch.org.uk/news.
Insight Plus, Medical Journal of Australia. Infectious Syphilis and Other STIs on the Rise. August 2024. Available at: https:// insightplus.mja.com.au/2024/32/infectious-syphilis-andother-stis-on-the-rise/.
Australian STI Guidelines. What’s New. Available at: https://sti. guidelines.org.au/whats-new/.
Ong JJ, Bourne C, Dean JA, et al. Australian sexually transmitted infection (STI) management guidelines for use in primary care 2022 update. Sexual Health. 2023;20(1):1-8. HIV.gov. A Timeline of HIV and AIDS. Available at: https://files. hiv.gov/s3fs-public/aidsgov-timeline.pdf.
References related AIDS/HIV
Patton LL, McKaig R, Strausbaugh LJ, et al. Changing prevalence of oral manifestations of human immunodeficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(3):299-304.
Greenspan D, Greenspan JS. HIV-related oral disease. Lancet. 1996;348:729-733.
Reznik DA. Oral manifestations of HIV disease. Top HIV Med. 2005;13(5):143-148.
Shiboski CH, Patton LL, Webster-Cyriaque J, et al. Oral
HIV/AIDS Research Alliance: research report on the oral manifestations of HIV disease. Adv Dent Res. 2011;23(1):78-81.
Dodds MW, Yeh CK, Johnson DA. Salivary alterations in HIV-infected individuals: associated complications and treatments. Adv Dent Res. 2006;19(1):44-48
References related to syphilis:
Little J.W. Syphilis: An update. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005;100:3–9. doi: 10.1016/j. tripleo.2005.03.006.
pmc.ncbi.nlm.nih.gov/articles/PMC9231211/ Ficarra G, Carlos R. Syphilis: the Renaissance of an old disease with oral implications. Head Neck Pathol. 2009;3:195–206.
Dybeck Udd S, Lund B. Oral syphilis: a reemerging infection prompting clinicians’ alertness. Case Rep Dent. 2016;2016:6295920.
Hertel M, Matter D, Schmidt-Westhausen AM, Bornstein MM. Oral syphilis: a series of 5 cases. J Oral Maxillofac Surg. 2014;72:338–345.
CDC. Syphilis Treatment Guidelines. Available from: www.cdc. gov/std/treatment-guidelines/syphilis WHO. Syphilis Health Topics. Available from: www.who.int/health-topics/syphilis Australian Government Department of Health. National Syphilis Surveillance Report. Available from: www.health. gov.au
References related to Gonorrhoea: Centres for Disease Control and Prevention (CDC). “Sexually Transmitted Infections Treatment Guidelines, 2021.” Available from: www.cdc.gov/std/treatment-guidelines/gonorrhea. Fifer H, Saunders J, Soni S, Sadiq ST, Fitzgerald M. “Gonorrhoea: Diagnosis and Management.” British Medical Journal. 2020;368:m119.
Rowley J, Vander Hoorn S, Korenromp E, et al. “Chlamydia, Gonorrhoea, Trichomoniasis and Syphilis: Global Prevalence and Incidence Estimates, 2016.” Bulletin of the World Health Organization. 2019;97(8):548–562.
Alirol E, Wi TE, Bala M, Bazzo ML, Chen XS, Deal C, et al. “Multidrug-Resistant Gonorrhoea: A Research and Development Roadmap to Discover New Medicines.” PLOS Medicine. 2017;14(7):e1002366.
Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. “Sexually Transmitted Infections Treatment Guidelines, 2021.” MMWR Recommendations and Reports. 2021;70(4):1-187.
Starnbach MN, Roan NR. “Confronting the Threat of Gonorrhea.” Journal of Infectious Diseases. 2020;222(Suppl 2):S111–S117.
Boskey E. “The Oral Cavity and Sexually Transmitted Infections.” Dimensions of Dental Hygiene. 2017;15(1):1–4. Available from: https://dimensionsofdentalhygiene.com/ article/oral-cavity-sexually-transmitted-infections/ WHO. “Global Health Sector Strategy on Sexually Transmitted Infections 2016–2021.” Available from: www.who.int
References related to chlamydia: Queirós C, Costa JBD. Oral Transmission of Sexually Transmissible Infections: A Narrative Review. Acta Med Port. 2019;32(12):776-781. doi: 10.20344/amp.12191.
Chlamydia Coalition. “Chlamydia 101: Transmission.” Available from: chlamydiacoalition.org.
Healthdirect Australia. “Chlamydia: Overview and Symptoms.” Available from: healthdirect.gov.au.
Zink, Christine. “Oral (Throat) Chlamydia: Symptoms and Causes.” Verywell Health, 2024. Available from: verywellhealth.com
By Yung Starling
“I WILL NEVER forget the moment when a remarkable lady, using just her chin, confidently maneuvered her wheelchair toward me. She was so proud to show me how it worked, her smile filled with pride and independence. That encounter was just one of many that deepened my commitment to special needs dentistry.”
My journey into special needs dentistry didn’t start with a specific plan. Instead, it grew from a deep desire to make a difference in the lives of individuals who face unique challenges. Over my 24 years in dental care, I’ve encountered many patients with disabilities and complex needs who struggled to access appropriate dental services. It’s been eye-opening to see how something as routine as a dental appointment can be so daunting for some families.
This realisation ignited a question in me: what would it take to create a supportive and inclusive environment for these patients?
In response to this need, I opened Starling Mobile Dental Care. I wanted to ensure that quality, compassionate dental services could reach those who find it difficult to visit a traditional clinic.
Our mobile clinic allows us to bring care directly to patients in their homes or other familiar settings, making dental visits less stressful for those with mobility issues, sensory sensitivities, or complex health conditions. A year ago, while attending a course with Dr. Derek, I stumbled upon a flier seeking
volunteer dental practitioners for a cerebral palsy clinic. The moment I saw it, I felt a strong pull to apply. It felt like the perfect fit for my mission. Since then, volunteering at the clinic has been incredibly fulfilling. It has enriched my understanding of inclusive care and reinforced my commitment to making dental services accessible for everyone, regardless of their circumstances. Every patient interaction reminds me of why I embarked on this journey, and I couldn’t be more grateful for the opportunity to make a difference.
While volunteering at the cerebral palsy clinic brings immense joy, it also comes with its challenges. One of the most significant hurdles is the travel— each trip takes me about 2.5 to 3 hours each way. Despite this, I still love doing it. The journey is a small price to pay for the rewarding experiences and connections I make with the patients. Each appointment is an opportunity to impact lives positively, and that makes every hour spent on the road worthwhile. I’ve learned that the
“Every interaction reminds me of why I embarked on this journey, and I couldn’t be more grateful for the opportunity to make a difference.”
dedication to serve often requires sacrifices, but the smiles and gratitude from my patients are more than enough motivation to keep me coming back. Additionally, working alongside different clinicians each time I volunteer has greatly enriched my professional development. Collaborating with various dentists allows me to learn new techniques, share insights, and adapt my approaches based on their expertise. This collaborative environment not only enhances my skills but also fosters a spirit of camaraderie and continuous improvement among our team.
The true heart of this journey lies in the stories of my patients. For instance, I recently saw a patient for the first time three weeks ago, who had been experiencing pain whenever she ate. After our appointment, she beamed at me and said, “You have made my day; it has made me feel great.” Her relief and happiness reminded me of the profound impact we can have. Another patient, who initially struggled to let his mother leave the clinic room, surprised us all after three months. Before we began, he confidently told her she could go sit at the cafe if she wanted. Witnessing such breakthroughs not only warms my heart but also reinforces my commitment to this vital work.
Learned volunteering at the cerebral palsy clinic has been a profound journey



of personal and professional growth. Through my experiences, I’ve developed essential skills that extend beyond clinical practice:
Working with patients who have diverse needs has honed my ability to communicate effectively and sensitively. I’ve learned to adapt my approach to ensure that each patient feels understood and comfortable, whether through verbal explanations or non-verbal cues.
Engaging with patients who often face daily challenges has deepened my empathy. I now appreciate the importance of patience and compassion, especially when someone is experiencing fear or discomfort. Each interaction reinforces the notion that every patient deserves kindness and understanding.
The
Volunteering in special needs dentistry has been one of the most rewarding experiences of my career. It has shown me firsthand the incredible difference we can make in the lives of those who often feel overlooked. I encourage dental Professionals and students alike consider volunteering their time and skills. Not only does it provide an opportunity to give back, but it also enriches your understanding of diverse patient needs and broadens your perspective on the importance of inclusive care. If you’re inspired to get involved, I invite you to explore local opportunities in special needs dentistry. Many organisations, including cerebral palsy clinics and mobile dental programs, are often looking for passionate volunteers. You can also check with dental schools and professional associations for resources on how to get started. Your skills could be the key to making a significant impact in someone’s life.
The dynamic nature of special needs dentistry has taught me to be flexible and innovative. Each patient presents unique circumstances, and I’ve learned to tailor my techniques and strategies to meet their individual needs. This adaptability not only enhances the patient experience but also enriches my professional practice. Beyond skill development, my time at the clinic has provided valuable insights into the special needs community. I’ve come to understand the critical importance of inclusive care—recognising that dental health is not just about treatment but also about ensuring that every individual feels welcome and valued. This experience has inspired me to advocate for greater accessibility and inclusivity in dental practices, underscoring that a compassionate approach can make a world of difference for those we serve.
Reflecting on my journey, I realise how transformative volunteering has been for me—not just professionally but personally. Each patient interaction reinforces the idea that compassion is at the heart of healthcare. The smiles, the gratitude, and the breakthroughs remind me that our work goes beyond just treating dental issues; it’s about building trust and creating a safe space for our patients. In a world where access to care can be a significant barrier, our commitment to inclusivity and empathy in dentistry is vital.
I hope my story inspires others to embrace the call to serve, making dental care a more compassionate and accessible experience for everyone. n
If you’re interested in learning more about Yung’s journey in special needs dentistry or how you can get involved, feel free to reach out! You can contact her via her website starlingmobiledentalcare.com.au

We look
By Dr Elizabeth Milford
The prevalence in Australia has been studied, and according to an Australian study by the time children are 15, around one in four will show signs of erosion on their permanent teeth. As an irreversible condition, the number only increases through adulthood.
It is no wonder that erosive tooth wear is so prevalent, when we consider how prevalent acids are in a modern diet. From soft drinks to sports drinks, from gut health diets and kombucha drinks to polypharmacy, at each lifestage and for a range of lifestyles, there are contributors to tooth erosion.
Erosive tooth wear is defined as a loss of tooth structure, by acid, without the involvement of bacteria. The phrase
Erosive Tooth Wear has been developed to highlight that erosion is only part of the problem, and that abrasion and attrition are also present, contributing to and accelerating the loss of hard tissue in the mouth.
Erosive tooth wear can lead to outcomes for patients like compromised aesthetics, sensitivity, pulpal damage, and occlusal changes.
Acid damage that leads to erosive tooth wear is different from the caries process in a number of ways. For starters, the acids produced by bacteria are relatively weak, like lactic acid, compared with dietary acids such as citric acid. In the caries process, the naturally occurring pellicle offers some protection from the weaker caries acids, and saliva can also provide buffering and dilution for the caries causing acids. By comparison, when faced with the acids that contribute to erosion, saliva’s buffering capacity is overwhelmed,
and the pellicle is unable to protect the tooth mineral. Finally, whereas caries starts as a sub-surface lesion that can be reversed in its early stages, erosion happens on the surface and is irreversible. Put together, it is clear that to prevent erosive tooth wear, prevention of demineralisation is critical.
Fluoride can assist with prevention of erosion. While the critical pH of hydroxyapatite is around 5.5, for fluorapatite it is around 4.5. That pH difference demonstrates how fluoride helps a tooth be more resistant to acids. With so many lifestyles lending themselves to exposure to strong acids, well below that fluoride threshold; there are many times that patients’ mouths are exposed to acid. But how can tooth enamel be protected when the pH drops below 4.5?
A simple toothpaste ingredient, stannous fluoride, has been proven to be protective.
Stannous fluoride works differently from sodium fluoride and other fluorides because both the fluoride ion and the stannous ion will provide protection to the tooth. Fluoride will offer incremental assistance, and then stannous builds on that and gives additional protection. Stannous works by forming a mineral layer is highly protective and highly resistant to acids. This has been studied extensively and can be demonstrated in in-vitro studies, where erosion-cycling experiments test hydroxyapatite resistance to acid when protected with different toothpastes by measuring the depth of enamel loss on the tooth surface.
To really highlight the extra benefit that stannous brings compared with a conventional fluoride like sodium fluoride, or sodium monoflurophosphate, research has compared stannous fluoride with high-dose prescriptionstrength 5,000ppm sodium fluoride. In a paper published by Eversole et al, an Oral-B stannous paste was compared to a regular sodium fluoride toothpaste and 5,000ppm sodium fluoride. After in-vitro acid cycling, there was little difference between the protection from sodium fluoride at 1100ppm and 5000ppm. In contrast, stannous fluoride paste provided clinically significant more protection, leading to markedly less surface enamel loss.
In a recently published metaanalysis of six RCTs among 186 subjects found that use of stannous fluoride conferred 83% more protection from enamel loss, or tooth erosion, as compared to marketed controls which included sodium fluoride and arginine toothpastes. In further support of this, the European Federation of Conservative Dentistry have recognised stannous fluoride’s potential to slow the progression of tooth erosion, stating “Toothpastes or mouth rinses containing

“It is no wonder that erosive tooth wear is so prevalent, when we consider how prevalent acids are in a modern diet. From soft drinks to sports drinks, from gut health diets and kombucha drinks to polypharmacy”
will prevent erosion, and its physical presence is an enduring protection against sensitivity. To treat sensitivity properly, it is vital that the layer that occludes the tubules is durable and long lasting, and is able to resist further tooth surface loss via erosion.
By forming a protective layer on the tooth surface, stannous fluoride has been demonstrated to provide 83% more protection against tooth erosion vs marketed controls in in situ models.
Neither sodium monofluorophosphate nor sodium fluoride, at 1,100ppm or at 5,000ppm provides the level of anti-erosion benefit provided by stabilised stannous fluoride.
There is a large body of evidence on the benefits of stannous containing products for the prevention of erosive tooth wear, making it an important and easy intervention, working alongside behaviour change strategies. n
stannous fluoride or stannous chloride have the potential for slowing the progression of erosive tooth wear. For other products, the data so far is sparse.”
When it comes to addressing erosive tooth wear, it is important to remember that tooth wear is multifactorial. The predominant factor is erosion driven by diet, but it is important to remember that abrasion may also be a factor.
Individual habits play a huge role in abrasion, things like aggressive brushing or choosing the wrong toothbrush can impact on teeth and may compound the rate of tooth wear. Recommending a softer brush, or an electric toothbrush with pressure sensor, can help to decrease the rate of tooth wear from toothbrushing.
Tooth wear is often associated with sensitivity for your patients. The acid resistant layer that stannous offers
About the author
Dr Elizabeth Milford is a dentist with a passion for prevention and evidence based dentistry. A graduate of the University of Queensland, she went on to gain a Master of Business Administration (Prof) from the Melbourne Business School. Elizabeth is an experienced consultant in dental regulatory compliance, working as an auditor and educator, approved by the Dental Board of Australia.
She has extensive experience in management of health-professional businesses and associations. She has assisted not-for-profit organisations diversify their income streams. She has also implemented strategies that respond to workforce challenges; support of new graduates, rural shortages, under-performing clinical staff. This has required an understanding of human resource and industrial relations issues.
Dr Elizabeth Milford is the Professional and Scientific Relations Consultant for Oral-B to Australia and New Zealand.
REFERENCES
Kazoullis et al. (2007) Pediatr Dent. 29(1):33-9
Eversole et al. (2015) J Clin Dent. 26: 44–49
West et al. (2021) J Dent 105: 103566
Carvalho et al. (2015) Clin Oral Investig 19(7): 1557-61
We look towards the festive period with hope for the future and thanks for those that have supported us in 2024
By Shida Taheri

As we wrap up another remarkable year, I want to take a moment to celebrate our wonderful industry partners who have consistently supported our profession throughout 2024. Their commitment to advancing oral health has been invaluable.
Speaking as a dental professional, my Christmas wish list this year reflects both practical needs and professional aspirations. I’m dreaming of a new saddle chair (my back will thank me!), the latest air polisher handpiece, and perhaps Santa could slip a few hand scalers into my stocking?
But beyond the tangible tools, what I really wish for is continued innovation in our field and even stronger partnerships that will help us provide better care for our patients. As we look forward to the opportunities of a joint association, my greatest wish is for our collective voice to grow stronger in advocating for improved dental health access for those who need it most.
From all of us at the DHAA and your Partnership Officer, we wish you a joyous holiday season and a prosperous New Year filled with healthy smiles!

Shida Taheri DHAA Partnership Officer

Since 1965, TePe has been at the forefront of innovation, with a strong focus on interdental cleaning. The company has been producing high-quality interdental brushes since 1993, with all products manufactured in Sweden in collaboration with dental professionals to guarantee premium quality. Sustainability is deeply embedded in TePe’s values, with most products crafted from renewable materials and produced using 100% renewable energy.
Introducing our corporate members:

Oral-B has transformed our approach to patient education with their cutting-edge digital tools and innovative power brushes. The iO Series continues to impress both practitioners and patients, making our recommendations easier and more effective than ever.
oralb.com

piksters.com

colgate.com.au
Piksters has shown remarkable growth this year, expanding their range of interdental solutions while maintaining their commitment to affordability and accessibility. They are the distributors of the LM instrument range which is are fantastic, stylish ergonomic hand instruments.

Curaprox brought their Swiss precision to new heights this year with their expanded range of ultrasoft toothbrushes and their revolutionary “Be You” toothpaste line. Their dedication to combining science with style continues to resonate with professionals and patients alike.
Colgate deserves special recognition for their extensive professional development programs this year. Their investment in continuing education and research has helped countless hygienists stay at the forefront of our field. They have relaunched their Bright Smiles, Bright Future program and we are in for a great year of oral health promotion.

Ozdent has proven themselves invaluable in the Australian market, providing exceptional service and support to our members. Their comprehensive range of dental supplies and equipment has made them an indispensable partner for many practices.
Part two of a series that looks at end-stage disease presentations – a symptom of the inaccessibility and poor user experience of dental care?
By Emma Turner
Working in a hospital setting provides tangible insight into the extreme outcomes of missed windows for early intervention in oral disease processes, with daily presentations to our emergency departments for spreading odontogenic infections in high-risk patients lost to follow-up for dental trauma, deep caries or previously-initiated root canal treatment.
A recent systematic review 1 suggests that approximately half of the adult population has signs of untreated endodontic infection, with many patients failing to seek dental treatment in the absence of pain. However, such presentations can catastrophically culminate in obliterated airways, anatomic spread throughout the head, neck and mediastinum, or sepsis, and can thus be associated with significant biological and psychological costs to the patient. Sleep-deprived, cortisol-fuelled admissions with hours spent in agony in hospital waiting rooms can cultivate mental scars and
dental anxiety. Unluckier patients may experience greater procedural trauma from interventions such as awake intubations, returns to theatre and prolonged hospital stays on IV antibiotics. Physical morbidity, such as scarring from extraoral drainage sites, may serve as permanent reminders of life-saving surgery. Beyond the cost to the individual, a 2020 South Australian audit concluded that deepspace odontogenic infections requiring admission for drainage under general anaesthetic incur mean costs to the health system of upwards of $15,000 per patient.2
One might think that a trip to hospital would suffice to awaken a patient to the benefits of early intervention to address oral disease. However, non-modifiable risk factors and systemic issues lead to frequent fliers re-presenting to ED with no dental follow-up between admissions for successive facial swellings. Of course, being empowered with greater health literacy helps individuals to prioritise accessing care. Nonetheless, even patients with an appreciation of oral disease processes may not receive
“Such presentations can catastrophically culminate in obliterated airways, anatomic spread throughout the head, neck and mediastinum, or sepsis, and can thus be associated with significant biological and psychological costs to the patient”
appropriate and timely dental care if they are unable to overcome their unique tapestry of financial, logistical or psychological barriers to doing so.
Previous experiences and ongoing

challenges inform patients’ attitudes towards regular dental visitation. Almost daily, the warm greetings that we offer to new patients are met with an unprompted “no offence, but I hate the dentist.” Procedural anxiety is rampant in our profession because of patients’ lived experiences and the propagation of dental horror stories (often through vertical transmission of dental anxiety from generations where anaesthetic was inaccessible and knees on chests were supposedly the picture of a typical extraction). If a patient only presents to us when they have a raging toothache, the association between dental care and pain is heightened, perpetuating the vicious cycle of dental fear and avoidance.3 Anticipatory pain can deter patients from seeking even preventive treatments such as ultrasonic cleaning and the sensory
overload on entry into a clinic (from the quintessential minty aroma that assaults the olfactory system to the noises of our handpieces), can be enough to classically condition a visceral response to setting foot in our rooms.
Sometimes, despite having the zeal to walk through our doors, patients may be reluctant to participate fully in health screening or accept comprehensive dental care. We’ve all heard “I just want a clean, not a check-up please” whether for fear of opening a Pandora’s box of asymptomatic disease or surprise costs, with financial opacity in the private system representing a significant deterrent to accessing dental care. In contrast to services such as blood pressure monitoring, eye and hearing tests, diagnostic imaging, routine bloods and screening for cervical, breast and bowel cancer, dental check-ups
cannot be bulk billed. In the absence of a universal dental care system in Australia, low-income patients without healthcare cards fall through the cracks in the system, especially those without private health cover. While most dentists carefully outline costs for a range of possible treatment plans following an initial diagnostic appointment, that initial consult itself could range from anywhere from $90 to over $300, with variable levels of reimbursement from health funds.4 Approximately 40% of Australians delay seeking dental treatment due to cost and a quarter of those that do attend struggle to afford recommended dental treatments.4 While the rise of interest-free payment plans can help to finance dental care privately for some patients, they can also be dissuaded by a lack of trust in the necessity of a dentist’s proposed >>
treatment, given the perceived propensity of private sector providers to ‘up-sell’ or over-service.5 This is increasingly pertinent with rising costs of living diminishing patients’ capacity for what they perceive to be discretionary spending. Teeth should not be the “luxury bones” of the body.
Unfortunately, patients without facial swellings or systemic dissemination of odontogenic infections will be turned away from free services in public hospital emergency departments, as tertiary centres do not have the capacity to cater to otherwise well patients who can be managed in a community or private setting. In engaging with community dental services, obtaining a same-day or imminent emergency appointment for relief of pain is relatively straightforward for eligible healthcare card holders. However, the same cannot be said of preventive services, with many public patients waiting hundreds to thousands of days for routine examination. Extensive public waitlists (even pre-pandemic as per Australian Institute of Health and Welfare data 6) have not been aided by the COVID-induced disruption to service provision and community-based dental care incurs a co-payment in most states other than the NT, posing an additional barrier to accessing routine dental services.
Despite voucher schemes allowing private dental providers to service public patients with unmet treatment needs in the face of increasing public waitlists, the focus of these vouchers is largely on addressing established disease with minimal capacity to focus on preventive health. Additionally, patients with high oral disease burdens often struggle to have their issues comprehensively addressed with the limited funds available through such initiatives.

Perhaps here is where we look to the progressive expansion of a public-inprivate dental rebate system beyond the offerings of the current Child Dental Benefits Schedule to overcome the deficiency of public sector services, while still providing financially-accessible care. The Australian Dental Association’s Australian Dental Health Plan outlines a proposed Adult Dental Health Scheme, which they wager could be funded by increasing the compulsory Medicare levy by as little as 0.5%, implementing a sugar tax and increasing taxation on tobacco, 7 both of which would have their own inherent benefits to oral disease prevention. Taxation of highwealth individuals and corporations has also been proposed to fund the addition of dental care to Medicare.8 Both approaches would represent active steps towards improving the affordability of dental care in Australia in a model analogous to accessing care in general
“Importantly, not every dental visit needs to be invasive – there’s so much to be gained by building patients’ confidence to set foot in our clinics for a look and a chat”
medical practice and allow for inclusion of a greater scope of preventive services. While we may not be able to control-Z patients’ traumatic historical dental experiences or overhaul the system in our practicing lifetime, improving the user experience (UX) of patients who choose to engage in dental care is within our individual capabilities. A quick internet search will yield innumerable handy tips relating to so much more

than the dentistry itself. Dental UX begins well before patients enter our surgeries - from service shopping, to booking, to entry into waiting rooms. First impressions, both in-person and in the lead-up, arise from the contributions of the whole staff – clinical and nonclinical alike – as well as our digital infrastructure and physical spaces. It’s important that we create a safe space that is accessible and welcoming to all. Some private clinics design their UX based on models from the beauty and wellness industries, disguising dentistry as a spa or salon experience with connotations as positive as other self-care activities such as haircuts or pedicures. However, it’s often the human touches that make a dental experience feel more comfortable and inviting. Our clinic isn’t at the cutting edge of interior design, there’s not a television or VR headset in sight, and my patients aren’t leaving with goodie bags, but they’re
leaving with a sense that we genuinely care about their health and wellbeing. We show this care through active listening, attention to detail and clear, respectful communication. Importantly, not every dental visit needs to be invasive – there’s so much to be gained by building patients’ confidence to set foot in our clinics for a look and a chat. Ultimately, setting a constantly interventional precedent for dental visitation is unproductive, because our procedural endeavours represent bandaid solutions to treat established disease that is preventable by appropriate athome prophylaxis with consistent oral self-care. Building the expectation that attending a dental appointment can just be an opportunity to work on patients’ oral health goals can be much less overwhelming to patients and still allows them to move forward in their care.
So, even if patients hate dentistry, they don’t need to hate the dentist. n
References
1. Tibúrcio-Machado CS, Michelon C, Zanatta FB, Gomes MS, Marin JA, Bier CA. The global prevalence of apical periodontitis: a systematic review and meta-analysis. Int Endod J 2021;54:712-735.
2. Han J, Liau I, Bayetto K, et al. The financial burden of acute odontogenic infections: the South Australian experience. Australian Dental Journal 2020;65:39-45.
3. Armfield JM. What goes around comes around: revisiting the hypothesized vicious cycle of dental fear and avoidance. Community Dentistry and Oral Epidemiology 2013;41:279-287.
4. Australian Institute of Health and Welfare. Oral health and dental care in Australia. Canberra: AIHW, 2023.
5. Leggett H, Csikar J, Vinall-Collier K, Douglas GVA. Whose Responsibility Is It Anyway? Exploring Barriers to Prevention of Oral Diseases across Europe. JDR Clin Trans Res 2021;6:96-108.
6. Australian Institute of Health and Welfare. A discussion of public dental waiting times information in Australia: 2013–14 to 2016–17. Canberra: AIHW, 2018.
7. Australian Dental Association. The Australian Dental Health Plan. 2019. URL: ‘ https://treasury.gov.au/ sites/default/files/2019-03/australian_dental_ association_-_supporting_document.pdf’.
8. The Australian Greens. Bring Dental Into Medicare: Our plan to make dental care free. Canberra, 2023. URL: https://greens.org.au/sites/default/ files/2022-04/Greens-2022-Policy-Platform--Health-Dental.pdf’.

About the author
Emma Turner, a founding member of the Colgate Advocates for Oral Health: Editorial Community, completed her Doctor of Dental Medicine at the University of Western Australia as the Australian Dental Graduate of the Year 2020. She is an avid hospital dentist, having worked in Melbourne’s southeast and more recently in the Top End and is passionate about contributing to the future of oral health through dental education, community engagement and research. She hopes to share her insights to encourage members of the dental profession to reflect on opportunities for personal and professional growth to benefit our patients and the wider community.
Republished with permission from Colgate Advocate’s for Oral Health
colgateprofessional.com.au/Advocates

ACT contacts:
Director Amy McDermott directoract@dhaa.info
Chair Kate Spain chairact@dhaa.info
n The ACT end-of-year Christmas dinner was held on Friday 22 November at the Southern Cross Club. It was an enjoyable and cosy evening with orthodontist Dr Tom Ethell who discussed the types of periodontal patients requiring orthodontic advice, and how these referrals may be communicated. He also covered the indication and appropriate timing of OPGs and CBCT.
ACT Director Amy McDermott represented
“ While oral health practitioners are recognised dental service providers for DVA patients, the DVA is still yet to accept our provider numbers ”

the DHAA at the Health Provider Partnership Forum, of the Department of Veterans Affairs (DVA) on Wednesday 6 November in Canberra. She raise the issue that while oral health practitioners are recognised dental service providers for DVA patients, the DVA is still yet to accept our provider numbers. The DHAA is continuing to advocate on this front.
Congratulations to ACT Committee member Rachael Walton for her selection into the DHAA Future Leaders Program.
The first ACT event for 2025, will be a dinner meeting on Tuesday 18 February. Please mark this in your diary and look out for updates regarding further details.
NSW contacts: Director Jinous Eighani-Roushani directornsw@dhaa.info
Chair. Belinda Hines chairnsw@dhaa.info
Deputy Chair Angelee Murdock contactnsw@dhaa.info
n The NSW end-of-year Perio Dinner Celebration was held on Friday 15 November at Novotel Parramatta. Periodontist Dr Judd Sher spoke of periodontal regeneration and the biological principles involved, and provided an update on relevant new techniques.
NSW was also the host to the inaugural Joint ADOHTA DHAA Oral Health Congress at the Sydney Hilton between 17-19 October. The
“ The flagship
event
[ADOHTA DHAA Oral Health Congress]
was a great success and we thanks the many NSW members and volunteers for their support”
flagship event was a great success and we thanks the many NSW members and volunteers for their support.
The 2025 NSW program will kick off with a full day event on Saturday 22 February and members are encouraged to put this date
For all the latest info on DHAA events please visit www.dhaa.info/events
aside so you can attend and network with colleagues.
Well done to NSW Chair Belinda Hines and members Maryam Slewa and Payal Nand who have been selected to join the DHAA Future Leaders Program which commenced in November this year.
Qld Contacts:
Director Carol Tran. directorqld@dhaa.info
Chair Gabby Williamson chairqld@dhaa.info
Deputy Chair Courtney Dicken contactqld@dhaa.info
n Congratulations to QLD Chair Gabby Williamson for her baby daughter born in October.
The Queensland endof-year celebratory half day seminar was held on Saturday 7 December at The Garden’s Club in Brisbane. The education program included Diabetic Educator Karen Bragg on Childhood Diabetes, Sepsis Survivor Caitlin Alsop on patient’s experience with tooth/facial sepsis, and celebrity dentist Dr Grace Sha in burnout and wellbeing.
We also thank the Queensland leadership
“ We also thank the Queensland leadership team of Carol, Gabby and Courtney’s for their contribution as part of the 2025 Congress Organising Committee in planning for the Congress to be held on 16-18 October 2025” “ Invited speaker, Erfanullah Abidi, shared his story of his exceptional resilience and dedication in both his personal and professional life. He served as an interpreter and cultural adviser for NATO armed forces during the war in Afghanistan”
SA Contacts: Director Michelle Kuss michelle.kuss@dhaa.info
Chair Courtney Rutjens chairsa@dhaa.info
Deputy Chair Jesse Kourakis contactsa@dhaa.info
n On Sunday 8 December at Fuego by the Sea, South Australia hosted a half day private themed Christmas brunch to celebrate the end of 2024. The invited speaker Erfanullah Abidi shared his story of his exceptional resilience and dedication
team of Carol, Gabby and Courtney’s for their contribution as part of the 2025 Congress Organising Committee in planning for the Congress to be held on 16-18 October 2025 on the Gold Coast. Please mark your diary and look out for further announcement of program and venue.
We also congratulate Queensland Deputy Chair Courtney Dicken and members Jessica Horwood for their selection to the DHAA Future Leaders Program which is well deserved.

in both his personal and professional life. He served as an interpreter and cultural adviser for NATO armed forces during the war in Afghanistan.
South Australia’s 2025 destination event is scheduled for Saturday 29 March at the Mount Lofty Retreat. This is a special wellness retreat packed with excellent education and wellness program. Due to the nature of the activity there is a limit on the delegate numbers for this event. Please look out for registration release date and book early to avoid disappointment.
South Australia is well represented at the DHAA Future Leaders Program and the five SA candidates are Courtney Rutgers, Jesse
Kourakis, Marcy PatsanzaMkonto, Shivani Kashyap and Gemma Collins. Well done team.
TasTAS Contacts:
Staff Bill Suen bill.suen@dhaa.info
n The Tasmanian team hosted its second full day seminar at the Lenna of Hobart on Saturday 16 November. Delegates were treated with three blocks of education covering periodontics, oral health practice as well as interprofessional oral health in primary care with GP and pharmacists.
We thank the valuable
“ Seminar delegates were treated with three blocks of education covering periodontics, oral health practice as well as interprofessional oral health in primary care with GP and pharmacists”
Jessica Pennay of ADOHTA and DHAA CEO Bill Suen through their excellent presentations.
contribution of presenters including Periodontists Dr Theodore Pang, Dr Alex Du Bois, GP Dr Boris Tan, Pharmacist Professor Greg Peterson, President

Vic Contacts
Director Roisin McGrath directorvic@dhaa.info
Chair Cathryn Carboon chairvic@dhaa.info
Deputy Chair Sarah Laing contactvic@dhaa.info
n The final event of the year was our highly popular Kooyong Christmas lunch held on Saturday 23 November, featuring a variety of hot topics including digital health, implant maintenance update and periodontitis.


For all the latest info on DHAA events please visit www.dhaa.info/events

“ The event was fortunate to have highly regarded expert Dr Susan Wise on Peri-implantitis; oral health advocate and researcher Tan Nguyen on applied health economics on clinical practice and our own Brie Jones sharing her experience in using intramural scanners in children.”
The event was fortunate to have highly regarded expert Dr Susan Wise on Peri-implantitis; oral health advocate and researcher Tan Nguyen on applied health economics on clinical practice and our own Brie Jones sharing her experience in using intramural scanners in children. As usual, the highlight was the champagne lunch and networking to celebrate a successful year of hard work and achievements.
Congratulations to the six members taking part in the DHAA Future Leaders Program, and they are:
Angie Ioannidis, Michelle Cantwell, Michaela Pitcaithly, Madara Dreimane, Sarah Laing and Wan Ying Chia.



WA Contacts
Chair: Michelle Wright contactwa@dhaa.info
Staff: Bill Suen bill.suen@dhaa.info
n Western Australia hosted the half day end-of-year celebration on Saturday 30 November at the Pagoda Resort & Spa in Como.
The event was again at capacity with Periodontist Wendy Gill providing a lecture on implant and followed by Hygienist Esther Carder presented on implant maintenance. Pharmacist Kiran Parsons then provided an extensive presentation on
“ We welcome WA Chair Michelle Wright to the DHAA Future Leaders Program and look forward to her contributions from the west.”
collaboration between real health and pharmacy - a topical approach in support of the move to encourage multidisciplinary team approach to address the oral health needs in the community.
We welcome WA Chair Michelle Wright to the DHAA Future Leaders Program and look forward to her contributions from the west. n

www.dhaa.info