7 minute read
Retinal complications of
Complications of the anterior segment
The retina is mysterious and intimidating and retinal complications are dreaded by all ophthalmologists. Dr Soosan Jacob, MS, FRCS, DNB reports
Peri-ocular blocks can be associated with a risk of globe perforation, with higher risk in high myopes, previously buckled eyes, use of sharp long needles, retro-bulbar injection, inexperienced anaesthetists and uncooperative patients. Recognised by sudden loss of vision, a hypotonic eye, localised retinal or sub-retinal haemorrhage and absent red reflex, it can be avoided by the use of topical, intracameral and/ or sub-Tenon anaesthesia, especially in high risk cases.
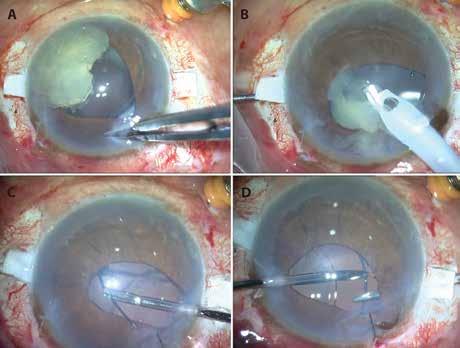
Posterior Capsular Rent (PCR), vitreous loss, nucleus or IOL drop and retained lens fragments occur even in the most skilled hands. Though small amounts of cortex may be tolerated, larger amounts as well as retained nuclear fragments cause severe inflammatory reaction, glaucoma, corneal oedema (CME) and even retinal detachment (RD). It requires management at primary surgery or at least within three weeks by vitreo-retinal (VR) backup. The IOL scaffold technique (Agarwal et al) can be used to prevent fragment drop by preplacing a three-piece foldable IOL above the iris and below the prolapsed nuclear fragments to plug the pupil and allow safe phacoemulsification. Vitrectomy and residual cortex removal is done with vitrector via pars-plana alternating between cutting and aspiration modes. The IOL is finally translocated as either sulcus with optic capture or as glued IOL depending on residual capsular support.
Retinal tears, RD and CME are increased with PCR, nucleus and IOL drop, chamber fluctuations, postoperative inflammation, vitreous strands etc. They are more common in complex cataracts such as subluxated, brown, hypermature, posterior polar, small pupil, IFIS, shallow or deep anterior chamber (AC), high myopes, vitrectomised eyes, traumatic cataracts, secondary IOL fixation, eyes with co-morbidities such as pseudoexfoliation and in complicated surgeries.
Improper vitreous management such as aspirating with vitrector, phaco or I/A probe or even Symcoe cannula without first cutting vitreous; blind manoeuvres to save a sinking nucleus; checking for vitreous by sweeping the AC with a rod or using a Weck-Cel at the wound can all lead to vitreous base traction and giant retinal tears and hence, should be strictly avoided. Proper vitrectomy with use of preservative-free intravitreal triamcinolone acetonide (IVTA) to stain the vitreous should be employed. Though small, localised PCR with limited vitreous prolapse may be handled trans-limbally, generally pars-plana vitrectomy is preferred, especially with larger PCR. The correct technique should be learnt or VR backup requested. Using a fixed infusion cannula frees both hands for bimanual manoeuvres. With pars-plana infusion, the tip must be visualised in the vitreous cavity before starting infusion to prevent accidental suprachoroidal or subretinal infusion. Its position should be constantly checked as manipulations of the eye may cause some retraction of the cannula. A slightly shorter scleral tunnel or longer infusion trocar helps prevent the cannula
from slipping out, but longer trocars risk injury to the capsule. The Agarwal trocar anterior chamber maintainer (ACM) or even a routine ACM are alternate options for anterior segment surgeons not used to placing pars-plana infusion. Sclerotomies for secondary IOL fixation should be at the correct distance and intra-operative hypotony should be avoided to prevent ciliary body bleeding and vitreous haemorrhage.
Pseudophakic rhegmatogenous RD has a rate of about 1%, and 50% occur within the first year of surgery. Risk factors include young age, high myopia, peripheral retinal degenerations, past history of RD, PCR, vitreous loss, vitreous incarceration and YAG capsulotomy. Multiple breaks and poor visibility secondary to opacified capsule and IOL reflections may make surgery difficult. Pseudophakic cystoid macular oedema (CME) is one of the most common causes of visual loss after cataract surgery and is due to a blood aqueous barrier breakdown. Risk is higher in diabetics, uveitis, older patients and following complicated cataract surgery. Postoperative topical NSAIDs are helpful for prevention and treatment.
Suprachoroidal haemorrhage (SCH) is a devastating complication that may occur intra- or early postoperatively. Risk factors include older age, arteriosclerosis, hypertension, use of adrenaline, systemic anticoagulants, large incisions, intra- and extra-capsular cataract extraction, aphakia, glaucoma, vitreous loss, raised intra-orbital or intraocular pressure, myopia, pressure from speculum, uncooperative patient, Valsalva manoeuvre such as coughing, sneezing, squeezing lids, history of expulsive in other eye, postoperative hypotony etc. It is recognised as sudden hardening of the eye, shallowing of AC, forward movement of lens or posterior capsule, vitreous presenting at wound, appearance of dark uveal mounds, loss of
red reflex, bleeding from eye and partial or complete extrusion of intraocular contents. Immediate recognition and sutural closure of all wounds is paramount. Posterior sclerotomies are not very effective in draining the rapidly clotting blood and besides, may increase bleeding by removing tamponading effect and are therefore no longer advocated. Prompt management can limit SCH to a localised, self-limiting haemorrhage with reasonably good visual potential. Small SCH are observed for spontaneous resolution. Larger ones with compressive effect need drainage once the clot liquefies and this together with any other definitive procedure required is performed between one and two weeks later.
Endophthalmitis, another dreaded complication, can cause irreversible loss of sight. Prevention includes careful preoperative examination of the eye, adnexa and lacrimal sac; preoperative topical antibiotics and povidone iodine asepsis; intra-cameral antibiotics, especially if posterior capsular rent (PCR) occurs; proper management of PCR and good wound closure without vitreous wicks and with, if required, sutures. Avoiding postoperative hypotony; confirming an adequately pressurised eye at end of surgery, especially after loosening speculum; use of postoperative antibiotics and maintenance of good hygiene are important. 23 or 25 gauge pars plana vitrectomy ports created for PCR should be self-sealing, tunnelled entries and conjunctiva should be displaced before entering. Cluster endophthalmitis can occur from contaminated intraocular fluids and medications. Early diagnosis and prompt VR referral and intervention are essential for any suspected endophthalmitis.
Finally, exacerbation of diabetic retinopathy and other retinal conditions may occur and needs pre-, intra- or postoperative treatment for the underlying condition.
RETINAL COMPLICATIONS OF REFRACTIVE SURGERY Though the risk is quite low in corneabased refractive surgeries such as LASIK, changes in VR vector forces from application of suction ring or applanation cone can lead to vitreous base and posterior pole traction, PVD, retinal breaks and RD. These complications occur more frequently with lens-based refractive surgeries (refractive lens exchange [RLE] and phakic IOLs). High myopia, low scleral rigidity, pre-existing peripheral retinal degeneration, breaks and holes, AC depth fluctuations, transient IOP changes and other risk factors as discussed with cataract surgery increase risk. RLE has a higher risk of RD than even general cataract surgery, especially in young myopes who have premature vitreous liquefaction and strong VR adhesions. YAG laser capsulotomy for posterior
Glued IOL Scaffold: A, B: A three-piece foldable IOL placed as scaffold below nucleus and above iris prevents fragment drop during emulsification; C, D: After pars-plana vitrectomy and cortex aspiration with vitrector, the IOL is translocated as glued IOL using handshake technique
capsular opacification also predisposes to breaks, RD and CME. Capsular polishing and use of hydrophobic, square-edge IOLs decreases this risk. Patients with phakic IOLs and RLE can develop CME, similar to that discussed previously. Rare reports of macular haemorrhage, choroidal neovascular membrane (CNVM), macular holes and central retinal artery occlusion after refractive surgery exist, risk factors being pre-existing lacquer cracks, CNVM, high myopia, macular traction, PVD, hypercoagulable states etc. Before any refractive surgery, a comprehensive preoperative retinal examination, including the periphery with scleral indentation, is a must, together with treatment of all indicated lesions. Postoperative routine retinal examinations are also a must for all patients.
RETINAL COMPLICATIONS OF OTHER ANTERIOR SEGMENT SURGERIES Complications discussed previously can occur here as well. Open-sky penetrating keratoplasty (PK) and glaucoma surgeries have a much higher risk of expulsive haemorrhage. Short open-sky time, use of general anaesthesia, head-end elevation and avoidance of all risk factors discussed previously is important. In PK, the opensky site should be immediately plugged with a finger (Osher M) until acute build-up in pressure subsides and a graft can be quickly sutured on. Preoperative uncontrolled IOP and postoperative hypotony both contribute to higher risk with glaucoma surgeries.
Glaucoma valves and strabismus
surgery may be associated with scleral and retinal perforation during needle pass, especially with thin scleras or if inadvertently passed deeply. This is generally ‘felt’ by the surgeon as having gone through and should also be suspected if uveal pigment or a vitreous bead is seen on the needle tip. Immediate retinal examination may identify it as localised retinal haemorrhage and retinal tear and laser or cryopexy at the site may be required. Mytomicin-C (MMC), which is often applied for glaucoma surgeriwes, or pterygium excision can cause scleral melt and necrosis, uveal show, retinal detachment and endophthalmitis if applied in too high a concentration or for too long. Inadvertent intraocular injection of MMC can cause retinal oedema, necrosis and atrophy.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com







