
5 minute read
Kimberly Jones-Beatty
Kimberly Jones-Beatty Seeks Data-Driven Solutions to Maternal Mortality Crisis
It’s one thing to identify a problem. It’s quite another to find a solution. Yet that is what Kimberly Jones-Beatty, CNM, DNP, Class 37, is striving to do.
Advertisement
The problem has become increasingly well known, as the alarming numbers depicting the maternal mortality crisis in the United States persist. In 2018, there were 17 maternal deaths for every 100,000 live births in the U.S. — a ratio more than double that of most other high-income countries, and the U.S. has the highest maternal mortality rate among developed countries.^ The data is even more concerning for Black and American Indian/Alaska Native (AIAN) women, who have pregnancy-related mortality rates that are over three and two times higher, respectively, compared to the rate for white women.*
The data confirm the problem, but it does not offer a solution. Jones-Beatty, who works as a certified nurse-midwife within the OB/GYN department at Johns Hopkins University in Baltimore, Maryland, has been practicing midwifery for 12 years.
“I work in a dual clinical/research role through providing ambulatory obstetric care and overseeing clinical research in the Johns Hopkins Integrated Research Center for Fetal Medicine,” Jones-Beatty said. “As a clinical practitioner, I strive to provide evidence-based care. As a researcher, I see that we contribute to evidence-based care through translational research; by generating new knowledge or validating existing knowledge in both basic science and clinical research and applying it to clinical practice to improve patient care and outcomes. It’s the best of both worlds.” Jones-Beatty put her research passion and skills to work in her DNP project, which focused on learning more about the maternal mortality crisis and its potential solutions.
“My DNP project focused on improving postpartum care,” she said. “Maternal morbidity and mortality are at an all-time high in the United States, and research shows that the majority of cases occur within the postpartum period. The American College of Obstetricians & Gynecologists (ACOG) has called for a paradigm shift in postpartum care by moving away from the single sixweek visit and instead incorporating an ongoing postpartum process beginning in the antenatal period to impact adverse pregnancy outcomes and maternal morbidity and mortality rates. The aim of the project was to increase effective postpartum care through patient preparedness, early one-to-three-week patient follow-up, and comprehensive postpartum visits from 0% to 80% in eight weeks.”
-- Kimberly Jones-Beatty
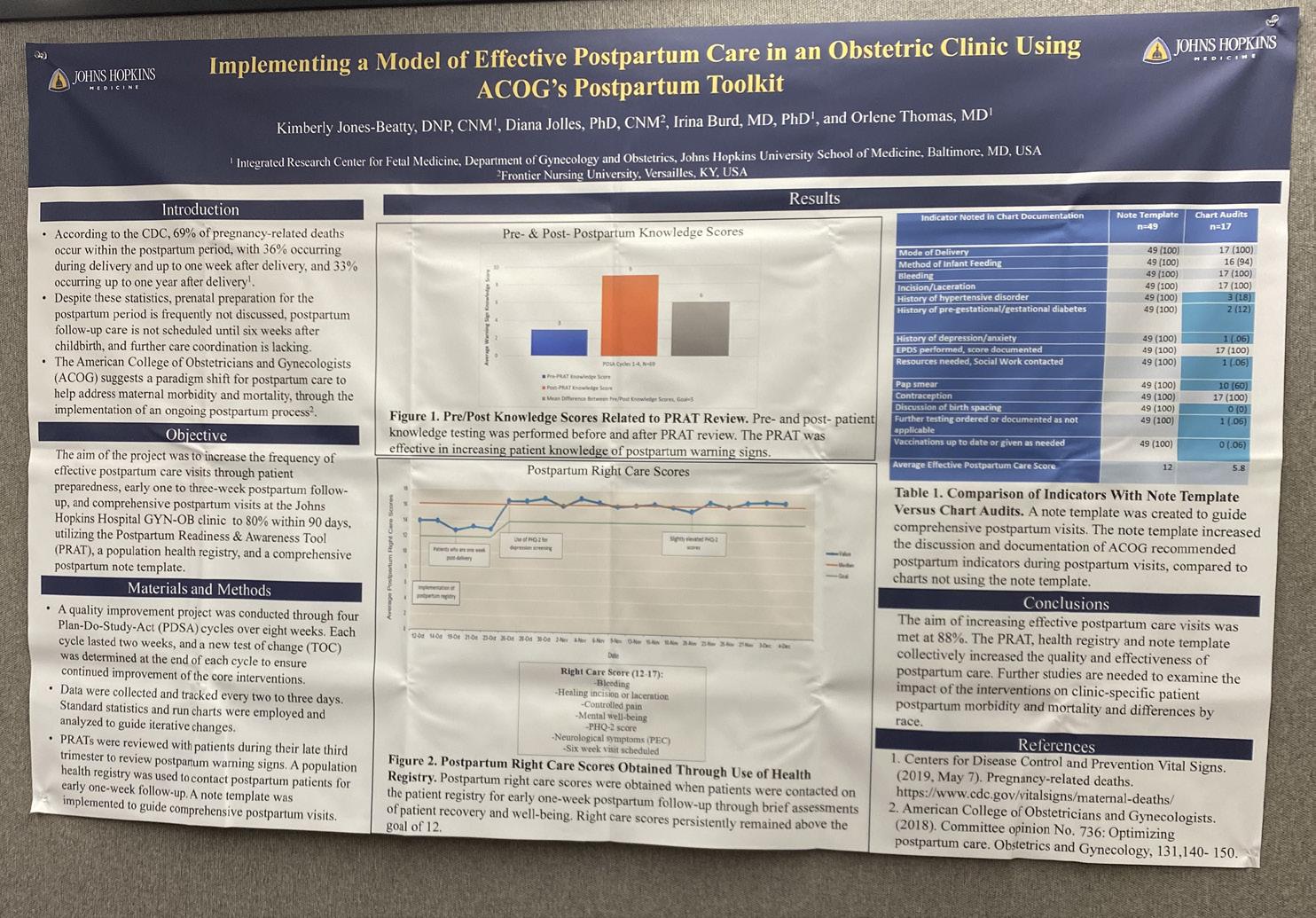
To implement the project, Jones-Beatty followed ACOG’s recommendations in creating a postpartum planning tool. The tool included reviewing the importance of postpartum care and postpartum warning signs that warrant further evaluation. It also incorporated a population health registry for early one-to-three-week postpartum follow-up to ensure that postpartum patients were recovering from childbirth as expected and a comprehensive postpartum note template to help provide complete documentation of recommended postpartum visit components.
“The project aim was met at 88%,” Jones-Beatty said. “The planning tool effectively increased patients’ knowledge of postpartum warning signs. The registry was effective in obtaining postpartum right care scores, which translates into patients recovering from childbirth as expected. The note template was effective in guiding effective postpartum care office visits. Next steps will include reviewing the impact of the interventions on clinic-specific patient populations, overall maternal morbidity and mortality rates, and examining differences by race.”
While more study and research are required to address maternal mortality, Jones-Beatty’s work was duly recognized for its significance. She recently presented her project as a poster presentation at the Society for Reproductive Investigation’s Annual Meeting in Boston, Massachusetts.
“Attending the meeting was a great experience, with networking opportunities and the chance to hear about new practice perspectives, guidelines, and other original research within reproductive health,” she said. Jones-Beatty’s love for research and information paired well with Frontier’s emphasis on data-driven analysis and decision-making.
“I decided to pursue a doctorate in nursing practice at Frontier due to its strong reputation, online format, and faculty expertise,” she said. “FNU’s DNP curriculum provides instruction on leading quality improvement in the clinical setting, as well as exposure to evidence-based practice, health policy and advocacy, and system/ organizational leadership. Collectively, I feel prepared to impact any healthcare setting I choose to work in through a deep understanding of the education and skills that exemplify nurse leaders who are ready to change the landscape of the current healthcare environment.”
Jones-Beatty is well-prepared to continue to excel as both a researcher and a clinician. Both roles hold equal value to her as she seeks to positively impact her current and future patients and colleagues.
“I plan to continue working both clinically and in research, contributing to evidence-based practice, improving obstetric healthcare, and decreasing adverse pregnancy and neonatal outcomes,” she said.
-- Kimberly Jones-Beatty
^Roosa Tikkanen et al., Maternal Mortality and Maternity Care in the United States Compared to 10 Other Developed Countries (Commonwealth Fund, Nov. 2020). https://doi. org/10.26099/411v-9255 *Artiga, S., Pham, O., Orgera, K., Ranji, U. (2020). Racial Disparities in Maternal and Infant Health: An Overview. Issue Brief. Kaiser Family Foundation, November 10, 2020

Be a Leader for Change with the DNP
Many who enter the healthcare field do so not only wanting to serve others but also to be a leader in improving quality of care as a provider and clinician. The Doctor of Nursing Practice (DNP), which is the highest degree for clinical nursing practice, helps prepare for this level of expertise. Simply put, the DNP is designed for registered nurses who want to take their nursing career, leadership skills, and clinical expertise to the next level.
FNU’s DNP program helps students advance their skills as well as develop as leaders, researchers, and innovators. The DNP Program draws on the clinical expertise of the faculty and students to prepare nurses at the highest clinical level to use their knowledge and clinical expertise to impact the health care of not only the individual but also the health care of the community, the region, and the nation.
FNU’s DNP curriculum provides education in evidence-based practice, quality improvement, and systems leadership; building on knowledge already acquired. As part of the curriculum, DNP students complete a Quality Improvement Project, generally in the hospital or clinic where they are currently working. This allows the student to tailor their project to their practice and the patient population which it serves.
To learn more about the DNP, please visit https://frontier.edu/ doctor-of-nursing-practice/.






