8 minute read
‘Cell Therapy Is the Future’
from March/April 2023
by HadassahMag
New made-in-Israel immunotherapy targets myeloma
By Wendy Elliman
Advertisement
Elisheva milo is a 73-yearold retired industrial designer from Haifa. Descended from a family that has lived in the Land of Israel continuously for over 2,000 years, she is a devoted aunt and great aunt.

Uri Lahav, 49, is an occupational therapist from Jerusalem. Husband to Karni and father to three children ages 15 to 20, he is the son of parents who immigrated to Israel from the United States about 50 years ago.
Despite their very different backgrounds, Milo and Lahav share something critical: This past year, both ran out of options in their battles against multiple myeloma, a cancer that relentlessly destroys bone marrow. For years—13 for Milo, seven for Lahav—they moved from one therapy to the next, until there was nothing left to try. Both are among the first group of 57 seriously ill Israeli patients who readily agreed to take part in the trial of an experimental made-in-Israel immunotherapy treatment.
The outcome of three years’ work by physicians and scientists at the Hadassah Medical Organization and
Bar-Ilan University, the trial’s interim results are “outstanding,” said Dr. Polina Stepensky, head of HMO’s bone marrow transplantation and cancer immunotherapy department. Ninety percent of myeloma patients in the trial have seen improvement so far, and over half—57 percent—have gone into remission. Patients in the trial were between the ages of 44 and 84, and there has been no evidence that age affected successful outcomes.
“With Israel the startup nation, it had been clear to me that we should and could find an answer for the growing numbers of people with incurable multiple myeloma,” said Dr. Stepensky. A hematologist-oncologist, pediatrician and stem cell transplantation expert, she is co-inventor of this new Israeli immuno- therapy—a treatment that uses the immune system to battle disease— for multiple myeloma. Incidence of the illness, the second most common blood cancer, is steadily growing for apparently unexplained reasons. This year, an estimated 176,000 people worldwide—550 of them in Israel, 35,730 in the United States— will be diagnosed with this disease, which causes blood cells manufactured in the spongy bone marrow to be crowded out by fast-proliferating cancer cells.

“When I graduated from Hadassah Medical School in 1998, median survival for multiple myeloma patients was less than three years,” said Dr. Stepensky. “With new medications and bone marrow transplantation, we’ve stretched this to over a decade. But in the end, all existing therapies lose effectiveness. We needed another approach.”
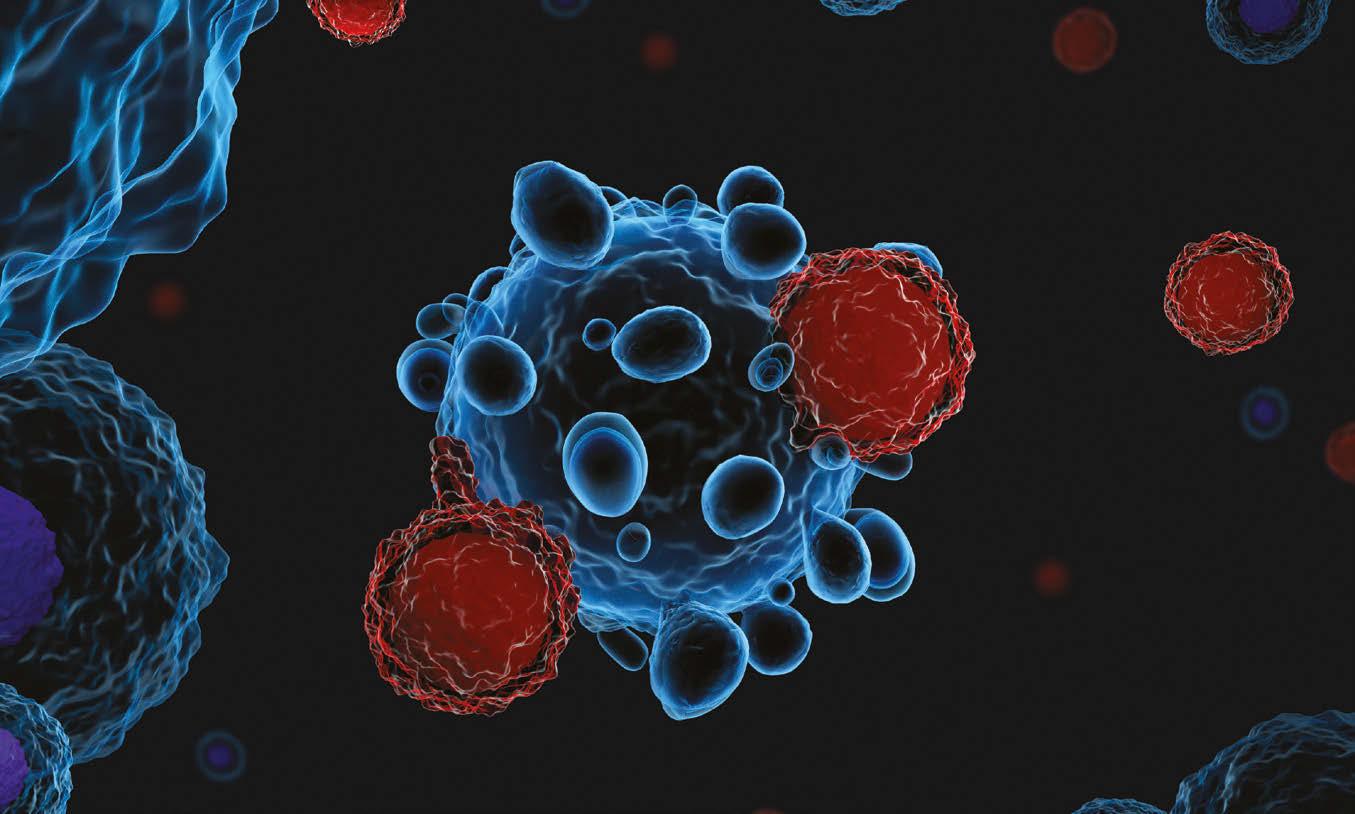
That other approach, called chimeric antigen receptor (CAR) T-cell therapy, circumvents the slashand-burn of conventional cancer treatments—surgery, chemotherapy and radiotherapy and their brutal side effects—and weaponizes the
Hadassah On Call
Hadassah On Call, Hadassah’s premier podcast, helps decode today’s top developments in medicine, from new treatments to tips for staying healthy. In each episode, American Israeli journalist Maayan Hoffman, a third-generation Hadassah member, interviews one of the Hadassah Medical Organization’s top doctors, nurses or researchers. In upcoming months, she will talk to a specialist on eating disorders and interview medical professionals for a special episode commemorating the 75th anniversary of Israel.
Look for past episodes on topics from women’s mental health to heart health and how environmental toxins have impacted men’s fertility over the past decade. Subscribe and share your comments at hadassah.org/hadassahoncall or wherever you listen to podcasts.
patient’s own immune system. After seeing the work of immunologist and genetic engineer Dr. Michel Sadelain at the Memorial Sloan Kettering Cancer Center in New York in 2017, Dr. Stepensky convinced Hadassah that Israel could manufacture and develop this treatment, too.
She brought on board a Bar-Ilan University team led by renowned French-born immunologist Cyrille J. Cohen, head of the university’s Laboratory of Tumor Immunology and Immunotherapy. Their role was to create a synthetic cellular molecule that instructs the patient’s immune system T-cells which cancer cells to target.

“It took many different designs until we identified the optimum molecule, but we got there,” said Cohen.
The Israeli CAR T-cells are formally classified as HBI0101—the HBI referencing its creators, Hadas- sah and Bar-Ilan—and use the same general approach as CAR T-cells engineered in the United States and China, which lead the world in CAR T-cell therapy trials and applications. In America, where researchers have focused on molecules and vectors different from the Israeli team’s research, CAR T-cell therapy was approved by the Food and Drug Administration six years ago, though it is still considered experimental.
The treatment is also expensive, costing hundreds of thousands of dollars. In China, its cost is lower, but regulatory standards there differ radically from the West. As Dr. Stepensky noted, the potentially far more modest Hadassah price tag makes Israel’s CAR T-cell therapy accessible to the estimated 120 Israelis needing it at any one time as well as to patients from outside Israel. She expects it to be in mainstream use within five years.
Proof of concept and preclinical studies of the CAR T-cells were the task of Hadassah, which “raised millions of donor dollars to take this technology through its crucial initial stages,” said Dr. Yoram Weiss, HMO’s director general. Those steps included “building Good Manufacturing Practice-graded master cell banks and manufacturing facilities, ones that use globally recognized production guidelines.”
In 2020, within a record-breaking three years, Israel’s Health Ministry approved clinical trials of the Hadassah-Bar-Ilan CAR T-cell therapy.
It was in october of last year, after Uri Lahav learned he had reached the end of the conventional treatment road, that doctors proposed the new treatment.
“I’d heard of it as something promising but not yet available in
Israel,” recalled Lahav, whose mother, Elisheva, volunteers at Hadassah Hospital Mount Scopus. “When Hadassah suggested it, I thought: ‘Wow! It’s here in Israel!’ And leapt at it.”
For Lahav, Milo and other participants, the trial, which took place in Hadassah’s bone marrow transplantation and cancer immunotherapy department, began with collecting the patient’s T-cells. A catheter in one arm drew out blood and passed it through a gently pinging plasmapheresis machine, which extracts plasma and the immune system cells it contains and then returns the remainder of the blood. Next came three days of light chemotherapy to ease introduction of the enhanced cells.
Meanwhile, in Hadassah’s specially built lab, researchers isolated the T-cells, enhanced them with the artificial molecules developed by the Bar-Ilan team and replicated them. To the delight of all, when the enhanced T-cells were infused back into the patient, the cells did exactly as programmed. They hunted down and
‘COMING FULL CIRCLE’: HWZOA’S NEW HEAD IN ISRAEL
When Suzanne (Suzie) Patt Benvenisti became executive director of the Israel offices of Hadassah, the Women’s Zionist Organization of America, she felt she was “coming full circle,” given her multiple and longtime connections to the organization.
Born in Houston to Israeli parents—her mother was born at Hadassah Hospital Mount Scopus—the 44-year-old has helped develop public policy for a number of health care organizations in the United States and been involved in child welfare and youth programs as well as in nonprofit management. Patt Benvenisti is a former director of public policy for Aetna, an American health insurance company, and has consulted on strategic and operations planning for Community Partnership for Protecting Children in Portland, Maine.
In 2010, she went with her husband, Ido, to volunteer at the Agahozo-Shalom Youth Village in Rwanda, which is modeled on Israel’s youth villages, two of which are sponsored by Hadassah. The couple spent their year in Rwanda mentoring youngsters orphaned by the 1994 Rwandan genocide and its aftermath, teaching destroyed the multiple myeloma cells.

“It’s only a short time since the treatment, so too early for results,” said Lahav, “but my energy is returning. I feel good and I’m very hopeful.”
For Milo, too, joining the trial was “an easy decision because I had nowhere else to go. It wasn’t too hard a treatment, easier than my two bone marrow transplants,” she said.
“I spent two weeks in hospital in iso- piano and singing—both of them are musical—and helping the village develop fundraising and economic plans.
The following year, she and Ido moved to Israel, where she was appointed managing director of Jerusalem’s Taub Center for Social Policy Studies, later becoming CEO of the independent research institute. The two live in Jerusalem with their three children—Ariel, 11; Noa, 9; and Aya, 5.
“Hadassah has been a household name as long as I can remember,” said Patt Benvenisti, who started her new position in January, succeeding longtime executive director Audrey Shimron, who stepped down to become executive director emeritus. This interview has been edited for brevity and clarity.
What attracted you to directing Hadassah’s Israel offices?
I saw it as an exciting, multifaceted position that merges many aspects of my personal and professional backgrounds. And all this at Hadassah, an organization at the forefront of Israeli health care innovation, and a place with which I have strong personal connections.
Can you share more about your Hadassah connections?
Both my mother and father graduated Hadassah’s medical school. I grew up in Hadassah’s Young Judaea youth movement—as camper, regional president, national board member and finally staffer at YJ camps. I met my husband when we both worked at Young Judaea’s teen leadership camp, Tel Yehudah.
What do you see as your main priorities in the role of executive director?
Foremost is serving as HWZOA’s representative on the ground here in Israel—as the daily connector between the organization in the United States and its Israel projects. Allied to this is representing Hadassah’s interests to the Israeli government and Knesset.
Another key aim is strength - ening and enhancing the image and name of HWZOA in Israel and worldwide—reminding a new generation of Hadassah’s historic role in building the state’s health care infrastructure and Youth Aliyah. Beyond that, I’ll be identifying opportunities to reinforce our Israel role in both traditional areas and new, developing relationships with Israel’s civil society and government, and building and strengthening partnerships with other Jewish organizations in Israel. I’m working on a strategic plan to meet these goals.
Why did you make aliyah?
I always felt connected to both Israel and the United States, where I grew up. I spent 1997 in Israel on Year Course and made aliyah (for the first time) in 2004, returning to the United States to complete a postgraduate degree at Harvard. It was only a matter of time till I went back to Israel, especially after meeting Ido, who is a Jerusalemite.
Did your Rwanda experience impact your career path?
Definitely! Our year in the village reinforced for me the importance of infusing my professional life with meaning and remembering to use my skills and experience to make a difference. —Wendy Elliman lation, then came back regularly for several weeks for follow-up. Ten months later, I’m still in remission and feel good.” greater automation and optimization of our cell production and continuation of our clinical studies,” said Dr. Stepensky. “We’re also waiting for Israeli Health Ministry authorization for frozen cell production as well as fresh, which will allow us to take more people into our trial. At the moment, we can handle only one new patient a week, and our waiting list is six months long.”
By january 2023, the results of Hadassah’s clinical trial were making medical headlines. The Los Angeles-based Immix BioPharma proposed a collaboration. Under the research and licensing agreement signed between Immix and the technology transfer companies of Hadassah and Bar-Ilan— Hadasit and BIRAD—next-generation Israeli CAR T-cell therapy will be developed and commercialized, and its production extended to the United States.
The therapy, she pointed out, is still in its early stages. While Hadassah’s CAR T-cell therapy puts multiple myeloma patients into remission of unknown duration, it does not cure them. Dr. Stepensky anticipates, however, that repeated CAR T-cell therapy treatment will convert the cancer from a fatal to a chronic disease. And she looks to the world of patients beyond those with multiple myeloma.
“We’ll be evaluating new targets and technologies,” she said. “Other blood cancers, such as leukemia and lymphoma, are an obvious first step, perhaps followed by solid tumors.
“I believe that this type of personalized cell therapy is the future,” added Dr. Stepensky. “I dream of a facility here at Hadassah that develops individualized cellular treatments for children and adults, for different cancers and for all other diseases where gene engineering can play a critical role.”











