KAMUZU CENTRAL HOSPITAL PLANNING FRAMEWORK
End of Semester Thesis / Process Book
by Hardi Shah
Project presented to the Faculty of the Department of Architecture
College of Architecture and the Built Environment
Thomas Jefferson University
In partial fulfillment of the requirements for the degree of BACHELOR OF ARCHITECTURE
Arch 507 / Design 9: Research and Design Faculty
Associate Professor Chris Harnish
Philadelphia, Pennsylvania
December 2018
3 Thomas Jefferson University - East Falls | Kamuzu Central Hospital perception 4 immersion 5 pediatric research & systematic review 9 gender disparity inventory & analysis 17 pediatrics schematic design & KCH Proposal 26 44 emergency & mass casualty research 54 development of a thesis bibliography 56 table of contents
PERCEPTION
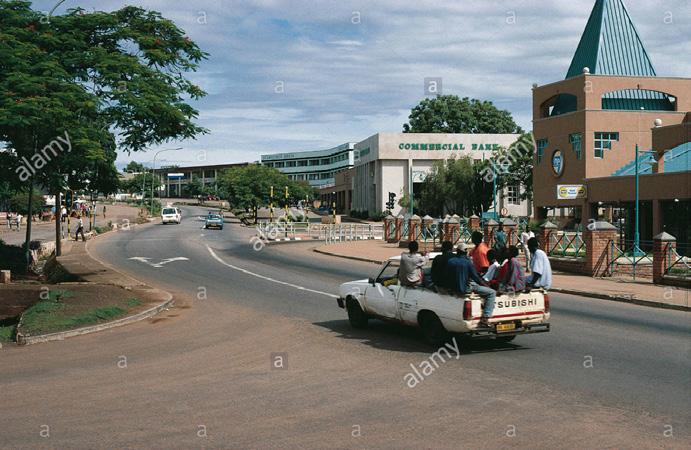
Addressing Preconceptions of Africa & Malawi
Thesis:
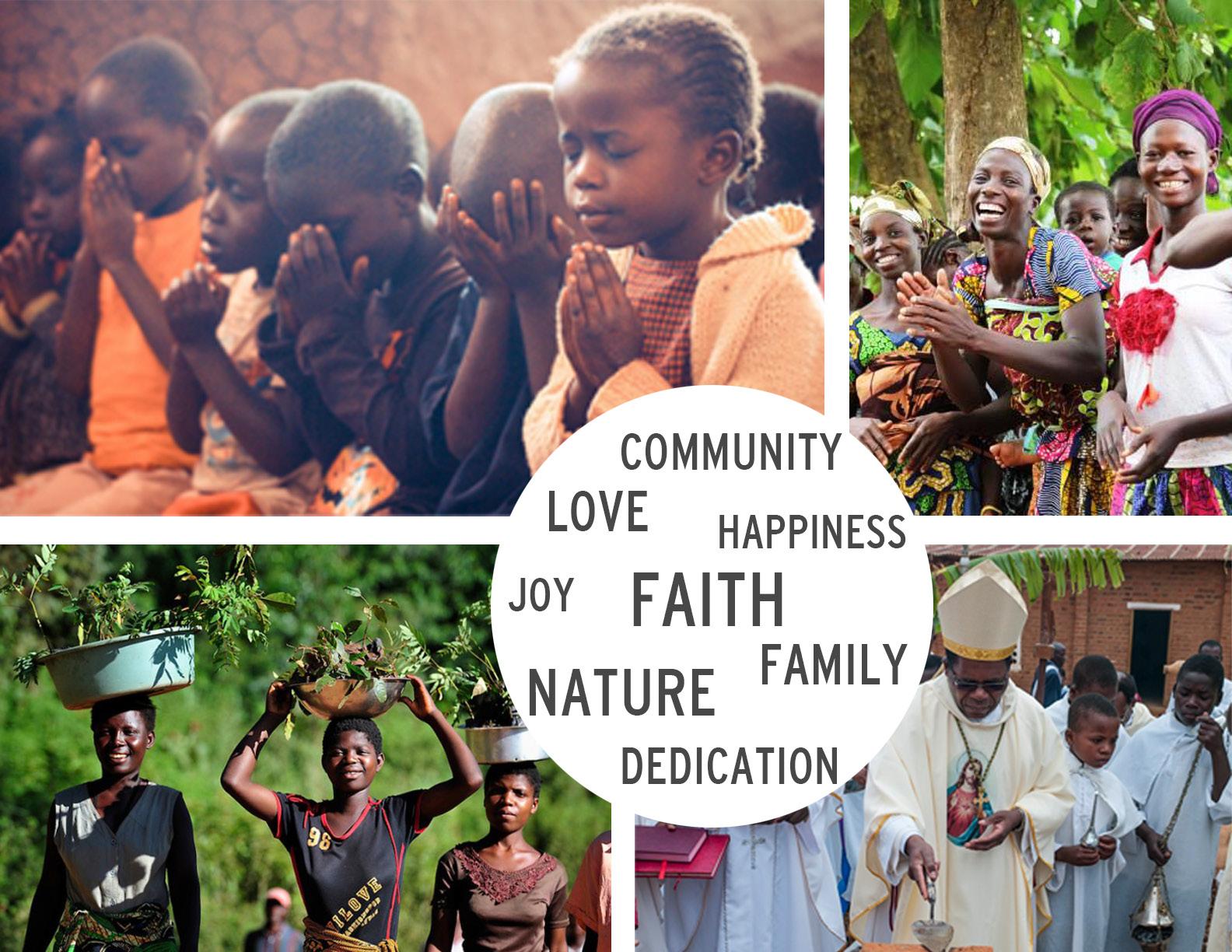
Malawi’s people are deeply connected with their fertile lands, climate, and resources as they construct their lives around the basic responses to their environment. As they progress towards becoming a “developed” nation, they face issues embracing their agrarian way of life and deep understanding of their lands and climate.

Something I appreciate about Malawi:
Malawi’s people have a lifestyle which leads them to live with the environment and not separate from it. They limit their usage of mechanical systems and man-made environments and instead focus on working with their climate to create comfortable spaces. This philosophy runs through their culture, some religious rituals, as well as their societal structure.
I began this semester with this exercise called “Perceptions” which asked us to portray our preconcieved ideas about Africa and Malawi beside our perspective of the United States. The themes that I preconceived of the United States were themes of abundance of resources & opportunities, hardships climbing the career ladder, multi-culturalism, and capitalism. Themes revolving around
Malawi that I identified after doing some research were scarcity in resources, scattered development, close relationship with nature and their seasonal changes, and untapped potential.
1
4
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
SCENARIO: You’re a 42 year old surgeon from a rural village. You were privileged enough to go to a good school, and from there received sponsorship to study medicine in South Africa. Now, you’ve returned to KCH and are disheartened by the poor facilities, lack of staff, and suffering of patients. On a weekly basis you personally have to decide who will live and who will die due to limited capacity to perform life-saving surgeries.
June 30, 2018:
I am so lucky to have had the privilege to study at the University of KwaZuluNatal’s School of Nursing and Public Health in South Africa. I have been exposed to so much knowledge here that I would not have been able to achieve if I had stayed back in Malawi. The time has come for me to leave South Africa and return to Malawi. I have seen the possibilities of medicine at my University here and I’m so excited to be able to go back to where I was born and assist the Kamuzu Central Hospital in serving my people.
June 31,2018:
I’ve been in this minibus for a day now. My back aches from trying to stay sitting upright on these bumpy roads. I have kept my passport and travel papers with me in my bag in my lap for the entire ride while my other belongings are on the roof of the minibus. The heat feels as though it is multiplying every second as my fellow passengers add to it with every breath they take in this congested vehicle. The only relief is the short minutes of sleep before I am jolted awake as we go over yet another bump in the road. Malawi, I hope I arrive at your borders soon.
August 1,2018:
We left in the morning of June 31st, and now 33 hours later, here I am at KCH. I settle in my room at my quarters not too far from the hospital, knowing
“Signed: Just Another Surgeon” IMMERSION
I was to be awake in 4 hours to start my first shift in Kamuzu Central. The anticipation was eating at me. I will finally be able to put my education to use to help my people.
I woke up in four hours and shook myself out of the exhaustion from my travels and made my way down to the hospital. On my way there I pass by hundreds of people traveling in and out of the pedestrian corridor off of Kenyatta Road and I walk past the outpatient center in the hospital. I saw the state of the seating provided for the patients; scorching bicycle seats would be more comfortable than the stumps they have available for patients to wait on. I shook that image out of my mind and made my way to the operation theater where I was to serve. I walk past the emergency and mass casualty ward and immediately notice the small sizes of the spaces available for patients if an accident was to occur. Like the outpatient ward, I put it out of my mind to focus on the tasks that I will have at hand soon. As I walked toward the operation theater, I walked through the pediatrics ward out of curiosity of the condition. Immediately I noticed how few the staff was compared to the children in need. I watched the doctor consistently diagnose conditions such as hydrocephalus and other congenital disorders which tend to be quite advanced. These children weren’t presented in the hospital when they should be because their parents aren’t able to easily reach services and children are only brought in once they experience severe conditions. Would I also be dealing with the same issue? Would my patients also be at the same disadvantage of time? I felt stretched just watching the doctor treat the children; I wanted to do more for them. There were only two doctors attending to the 116 children in the ward. I shook that thought and cleared my mind as well as I could as I walked into the operation theater. Upon arriving, I was immediately handed the list of patients I was to attend that day by a nurse. She just gave me the list, made a second of eye contact to welcome me to the hospital, and rushed to resume her rounds.
5
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
IMMERSION
“Signed: Just Another Surgeon”
I shouted a thank you to her as she scurried away and looked ahead to my first patient. Boy, was I in for a surprise. I had four patients at one time. Three of the four were bleeding, two of them were screaming in pain, and one was being calmed down by a nurse. I got my head in the game and started to think of my studies. First step is the uniform in a theater. I was shocked to see that the uniform consisted of a towel on my head and a dressing gown over my scrubs. I also noticed there weren’t a large supply of gloves either. They had to be used sparingly. As I made my way from patient to patient, hour after hour, I began to notice myself running out of supplies. I began to notice myself ask for assistance but not being able to get any because of the lack of staff. I scraped through the adversity of the first day and I made it to the end of my shift. I was exhausted. I did not know how to feel at the end of the day. Do I feel proud for joining a workforce where manpower is of such need and value? Or do I feel as though I am not able to do my job to the best of my ability and am being limited? Do I think that conditions at the hospital are so disheartening that it makes me question if I can survive helping others survive?
August 2,2018:
I thought it would get easier as I got more familiar with the hospital and the conditions. It did not. It wasn’t any easier and I don’t understand how it will ever get easier to watch the conditions fail the patients while I am working so hard to give them the best possible care that I can. There weren’t enough resources. I found myself reaching for more pain medication and not finding any. I found myself stepping over family who lay next to their ailing relatives. I found myself watching the guardians try to feed and change and care for their relatives during their short visitation hours. They gave me hope though. If they were willing to help their relatives despite not having a medical background, how could I, a medical professional, give up hope? God, I was
trying to not give up hope!
August 3,2018:
I need to write today’s events down to get them out of my head. It was a cruel day. The water stopped running mid-surgery today and we lost the patient on the table. I was performing a surgery and the water stopped flowing halfway. I did not know how to go about this issue and I lost my patient on the table. It was my decision to take his operation first before the other two who were waiting for treatment. Because of my decision now she is dead and it was because of the sequence that I set. What gives me the right to govern death in that way?
August 4,2018:
I am trying to get past what happened yesterday in my mind but it is stuck on replay. I can still hear her husband crying when I told him what had happened and that sound will haunt me for the rest of my life. Today I was treating two patients with similar ailments; they both had cancerous tumors. One’s was in her breast and the other’s tumor was in his abdomen. I turned to look for Acetaminophen medication to manage their pain while I figured out my next steps but could only find enough for one dose. I gave it to the woman, I don’t know if it was my bias or if I just felt more responsible for her as she had a young son clinging to her body as she lay in bed. It was a split second decision but it also meant that the man who lay in bed with a tumor in his abdomen would have to deal with the pain and it would be my fault as it was my decision. A few hours later, we all realized how terrible his condition was getting as he was getting sicker and weaker with every passing minute. He had not presented himself at a hospital for help though he had symptoms of the tumor for a year now. He was in a critical condition and there wasn’t more we could do for him except ease his pain with medication. After a few hours, the next dose of
6
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
August 5,2018:
I don’t know what more to say. Every day is the same struggle between life and death, resources and staff, medical knowledge and human instinct. I do not know how else to go through the day except for doing the best I could for these people.
August 6,2018: Another day.. Same story.
August 7,2018: Dear God, Let tomorrow be different.
August 8,2018:
I see too much pain and I feel helpless. I need someone to take the wheel. It has only been 7 days since I started this position and I am already torn mind and soul.
August 9,2018:
The highlight of my day today was the joy I found handing a baby to a mother who I had just finished operating on. She was in pain and I did not have the means to dedicate more medication to her for it but she would live. That baby
would have her mother and that was a beautiful sight.
August 10,2018:
“Signed: Just Another Surgeon” IMMERSION medication which was available was in my hand to give to my patients. Do I give it to the man who I know is not going to last the night and ease his suffering? Or do I use it towards a mother with a breast tumor laying in bed with her young son who still has a chance at survival? I did not want to have to make this choice. But I did and she rested easy after I administered the medicine, but I was not able to rest after making that decision.
I lost two patients today. One presented too late and the other just was too weak even after making it to the hospital that close quarters caused him to catch an infection. We did not have the manpower to assign someone to look after him and he did not have any guardians present. The case was too short. I have no time to make my decisions. It is all instant split second decision making and many times those decisions have to be made about someone’s life.
August 11,2018: I haven’t even been here for two weeks and I am struggling with coping with my mental state and the guilt I am projecting onto myself for every patient I am unable to save. This is bearing down on my mind. I don’t know how people do this for so long.
August 12,2018: Another day of the same; I saw the same lack of resources, lack of staff, and abundance of ailments. It is truly starting to beat down on my mental strength. After the first incident of having to choose which patient needed the pain medication more than the other, I have been in that same position 4 more times since then. It is as though God is testing me. He is asking me to take over his role for the day as I perform my four surgeries at a time and have to make split second decisions which would change my patients’ lives forever.
Signed: Just Another Surgeon
7
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
2, 3
IMMERSION Reflection
This exercise was a great way to introduce myself to the medical situations in Malawi through some research and empathetically apply myself to beginning to understand the needs and feelings of the people and the medical staff as well. One thing that I took away from this in particular is that people typically focus on the medical issues and how they affect the patients and guardian populations
but the needs of the staff treating the patients are also important. The mental state and psychological wellbeing of the staff directly affects the quality of care that is given to patients at Kamuzu Central and other medical facilities.

8
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
PICO Question & Research Strategy
P patients, children, pediatrics, LMICs, hospital, pediatric patients, people under the age of 15, facilities, health services, pediatric wards of LMICs
separation OR integration OR distribution OR configuration, outdoor spaces OR activity spaces OR incorporation of play space, bed configuration, hospital organization, division of departments, programming OR intention OR education, configuration of beds, ward configuration, dividers or divisions between the beds, storage space, presence of guardian, programming OR intention OR education
World Health Organization
length of stay, mortality rate, stress indicators, satisfaction
PICO Question: Which elements of pediatric ward configuration are associated with improved outcomes in these patients?
Almost 80% of Malawi’s current population of 16 million resides in rural areas and about 50% of them are under 15 years of age. Due to the lack of able, trained human resources, the pediatricianto-child ratio is 1:500,000. To aid the staff in providing care to the children in pediatric wards, it becomes crucial to consider the architectural implications of the ward design in the treatment and
fast recovery of the patients. This need led to the emergence of the question which was researched within the review.
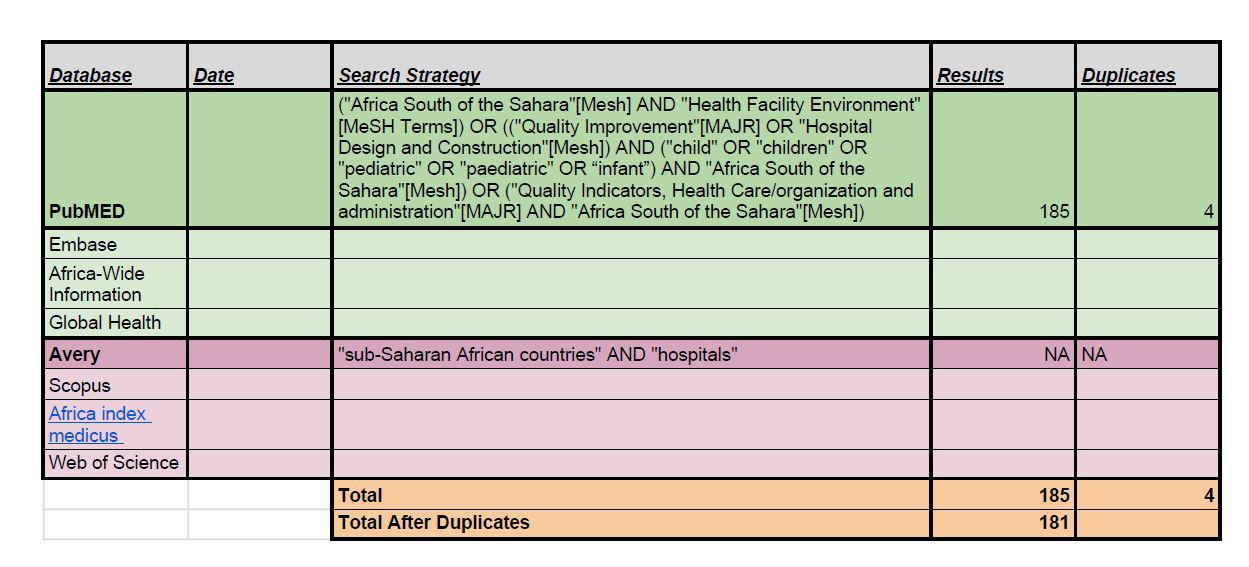
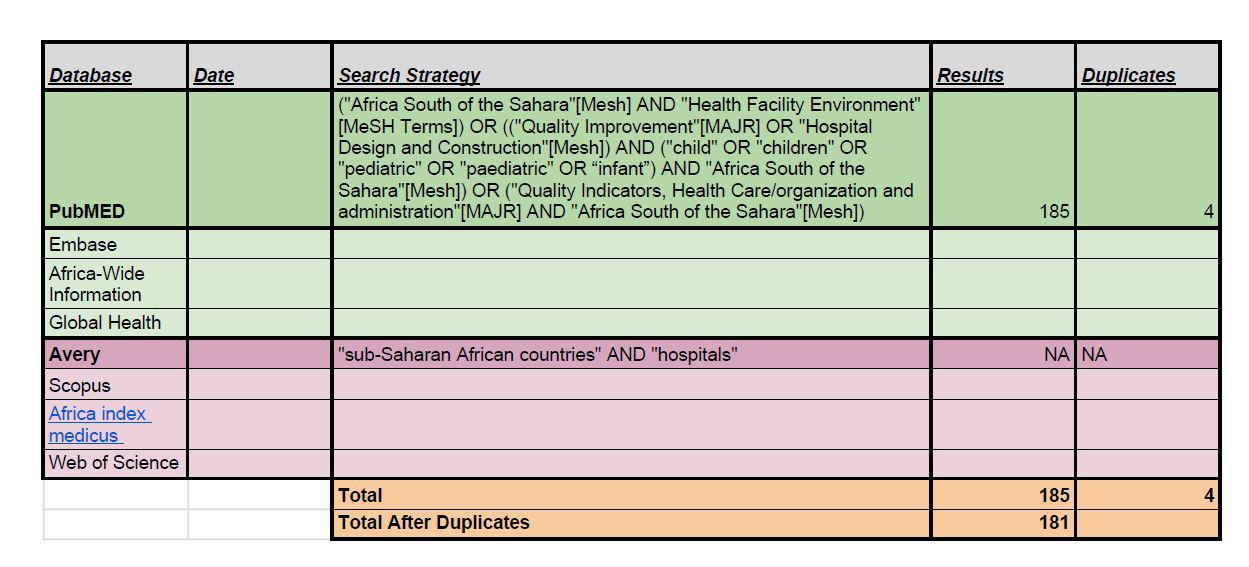
Once the PICO question was created, my groupmates and I conducted a systematic review on PubMed and Avery to find scholarly sources for the research,
9
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
I C O
4, 5
PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
Systematic Review _Protocol Template & Process
Review title: Systematic review of patient outcome in various pediatric ward configurations
1. Background
I. Important characteristics
What are the important population and/or disease characteristics (diagnostic criteria, epidemiology, aetiology, prognosis)?
The primary population being studied is pediatric patients. This population is specific enough to study but is also of interest in a lot of modern research in order to improve infant and child mortality rates. We are not choosing to specify a disease or condition
II. Relevance
Does the review topic have important implications for health (individual and/or public), as well as health care, policy and research?
The review of a topic rooted in pediatric health and healthcare is important to study for the growth of populations and improvement of healthcare policies. Understanding how to reduce disease and illness at an early age will work to prevent disease in the future for those patients and advocate for healthcare research aimed towards improving outcomes.
III. Rationale
Does the evidence (including existing systematic reviews) fail to answer the review question, and why?
Studies and systematic reviews that have already been done have pursued approaches in medicinal and clinical changes to improve
mortality rates and the quality of healthcare in sub-Saharan African countries. This does not address as many spatial and design components like the review question is. Some studies begin to explore them, but not in their entirety, so the hope is to collect and analyze what has been studied to produce a more holistic answer.
IV. Justification
Is the need for the review justified in the light of the potential health implications and current limitations of the evidence base?
The review is justified because more studies need to be done on spatial configuration of hospitals in order to maximize their function and efficiency. The more data that can be collected on how to do so, a better baseline for healthcare facilities can be developed for low- and middleincome countries. It is even more justified in the focus on pediatric care because under-5 years old mortality rates are very low in many subSaharan African countries.
V. Specification
What are the PICO components of the review question / objective?
We are addressing the configuration, organization, and facility efficiency (I) of pediatric care wards in African hospitals (P). This does not need a specific comparison because the lack of intervention acts as such. The objective is to explore improved patient outcomes in a variety of forms, both qualitative and quantitative (O).
10
-
Thomas Jefferson University
East Falls | Kamuzu Central Hospital
PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
Systematic Review _Protocol Template & Process
2. Methods
I. Search strategy
Which electronic databases will you search?
We will be searching PubMED and Avery Index to Architectural Periodicals.
What are your key search terms?
Our key search terms are as followed: pediatric patients, hospital, pediatric wards, health facilities, configuration, spaces [indoor, outdoor, activity], organization, division, programming, length of stay, mortality, outcome, stress, satisfaction.
What other sources will you search?
If necessary, we can search through other scholarly journals and publications relating to both medicine and architecture. However, the majority of information will be collected through the databases mentioned above.
II. Selection criteria
What are the inclusion / exclusion criteria for the titles/abstracts screening?
The focused inclusion criteria for screening purposes are the mention of physical design or design components, a quality of treatment assessment, and the quality of the facility itself. We decided not to specify a pediatric inclusion criteria as to not limit the results too much. Our exclusion criteria state that articles cannot be in a language besides English, be studied outside of Africa or LMICs, or be based on medicinebased testing (no design components).
What are the inclusion / exclusion criteria for review of the full manuscripts?
For the full manuscripts, we aim to focus our inclusion criteria on the prioritization of design element and physical or spatial discussions within a hospital rather than those that briefly mention it. Having more emphasis on the relation between layout and configuration and actual health outcomes will produce a more effective review.
Will you impose any additional limits, e.g. language, publication type, study design?
These additional limits were already addressed in the preliminary criteria. However, we will try to limit the use of personal or secondhand accounts in the type of publication. While they are valid, some may be more inferencing than fact and we would like to focus on alreadycompleted research studies and reports.
How will study selection be performed?
After searching through a variety of search terms in PubMed and Avery indexes, we will apply the above criteria and limitations to the results in order to narrow them down to the most valuable information.
III. Data extraction
What are the key data to be extracted?
The key data will be design elements and proposals that have proved to be effective in improving the experience of patients, mortality rate, overall outcome, and similar quality assessment factor for pediatric patients, visitors, and hospital staff.
11
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Systematic Review _Protocol Template & Process PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
How will data extraction be performed, and how will extracted data be presented?
Each selected manuscript will be read by at least two of the three group members with a focus lens on design, physical, and spatial discussions. This information will be either highlighted or collected in a separate document in order to place it with similar findings from other manuscripts. It will then be presented as a collection of viable design tools for improving patient outcome in hospitals with poor conditions.
IV. Data synthesis
How will data be combined (statistical or narrative), and why?
We think it is valuable for data to be combined in both statistical and narrative forms. The collection of statistics will be valuable in advocating for with interventions were quantitatively the most effective. However, the use of narrative will allow us to place those interventions into a “bigger picture” of why the problems that exist do and the ways we have found to combat them through design and planning.
Environment”[MeSH Terms]) OR ((“Quality Improvement”[MAJR] OR “Hospital Design and Construction”[Mesh]) AND (“child” OR “children” OR “pediatric” OR “paediatric” OR “infant”) AND “Africa South of the Sahara”[Mesh]) OR (“Quality Indicators, Health Care/organization and administration”[MAJR] AND “Africa South of the Sahara”[Mesh])
Once a full list of the searches was exported from PubMed, they were reviewed based on their abstracts against the inclusion and exclusion criteria which were set.
Inclusion Criteria: articles including some design (or design components), articles talking about quality of treatment assessment, and articles mentioning the quality of the facilities it is addressing
Exclusion Criteria: articles including clinical/ medicine- based testing studies (lack of mention of design), articles not in the English language, articles not based on studies conducted in Africa or lower or middle income countries (LMICs), accessibility to full manuscript
These articles were then filtered once again based on which articles were accessible for review. Once that list of articles fulfilling the criteria was extracted, they were filtered once again based on the same inclusion and exclusion criteria but this time the entire body of the article was taken into consideration not only the abstract. After that last screening, the final list of selected manuscripts was extracted for consideration in this review.
Search Terms: (“Africa South of the Sahara”[Mesh] AND “Health Facility
12
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
General Architactural Findings
The built environment, ward layout, and facility condition and placement all play a key role in the treatment quality of the patient in a hospital. In a study conducted in Zimbabwe, the quality of multiple hospitals was surveyed by the users. Findings from this test concluded that the aspects of the hospital that rated the effectiveness and quality for the patients were low availability of drugs, overcrowding of floor beds, inadequate facility placement, lack of functional equipment, and the overall health of the building. These factors contribute to the actions that are taken to improve medical centers and hospitals. Quality improvement programs put into action in the Democratic Republic of Congo incorporate design criteria such as “A clean latrine should be available and at least 20 metres from the health centre” and “the floors should be washed with disinfectant at least twice a week” within their requirements for a high quality medical center. All of these criteria are improvements to the overall quality of the user experience through changes made in the building condition and layout.
Another study which was conducted in Jimma University, emphasized the importance of monitoring the interactions between the building design and microbial load. Factors such as overcrowding, improper design and poor ventilation can impact the growth and survival of microorganisms which is harmful to human health. The studies showed that there are higher microbial loads for buildings that do not incorporate vents, a proper fenestration strategy as well as a low floor-to-ceiling height compared to buildings which did contain all of those things. If building design could passively tend to festering issues such as microbial growth it could make a significant impact on hospital operations as well as
the patient experience by improving working and temporary living conditions.
Another aspect of the built environment is overall building health and cleanliness. This involves designing the layout of available and accessible facilities as well as being able to maintain them at the quality that meets health standards for a hospital. The need to provide effective and accessible facilities for pediatrics especially during the neonatal state when children are most vulnerable to diseases and infections is crucial and so being able to create an efficient layout within the buildings and ward design is a vital part of any hospital. For the hygiene and safety of children, staff, and caretakers, it is important to consider the inclusion and placement of facilities such as sinks for handwashing, clean and accessible toilets, access to running water and a space to wash her and her child’s clothes, as well as adequate beds for each individual mother and child.
13
University -
|
Thomas Jefferson
East Falls
Kamuzu Central Hospital
5, 6, 7, 8
PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
Communication-Specific Findings
Human interaction tends to have a profound impact on one’s perception, treatment, and education in a healthcare setting. While being in a hospital, doctor’s office, or clinic might be scary, ultimately, we are all human. Studies showed that direct human communication aligned with patient satisfaction. This human interaction is inferred to be at the time of intake and consultation. At intake, communication with the staff leads to satisfaction of patients, making them feel like they are cared for; however, this study similarly had patient dissatisfaction in the point of treatment because because 50% of the doctors “did not introduce themselves to their patients and parents”. One might suggest that this is because of the fast paced and stress environment of a medical setting, with long wait times and long lines for treatment. How can we as designers change this dialogue with the doctor and patient?
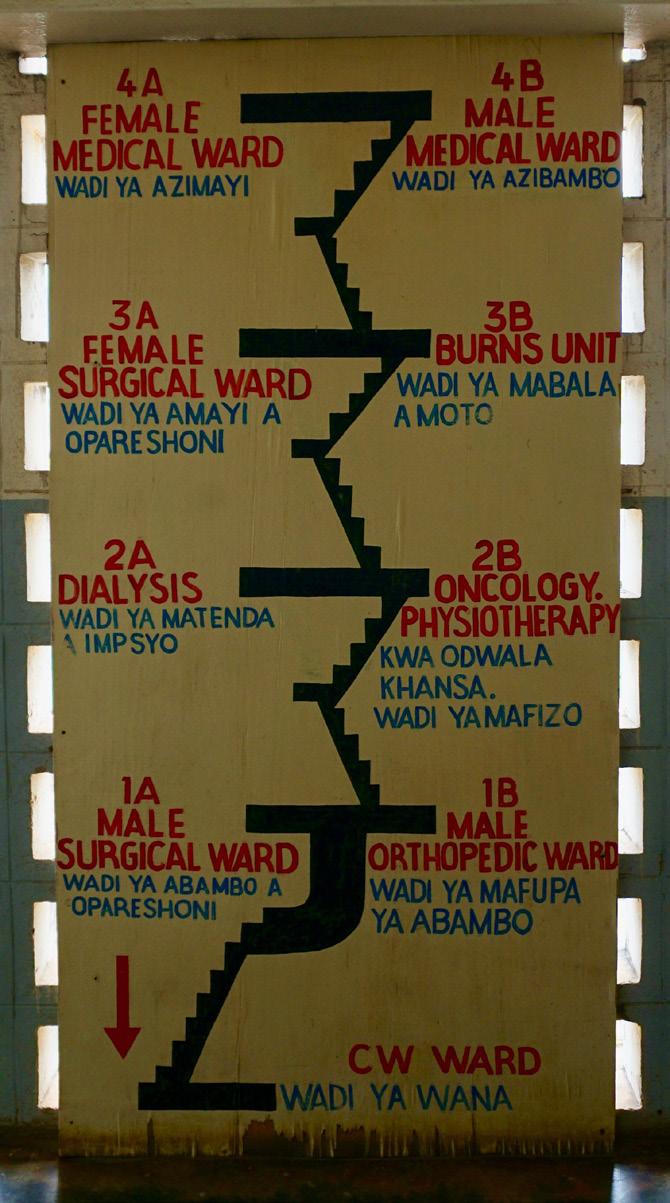
Graphic and visual communications such as wayfinding and illustrations have proven effective in conveying a message and/or the experience one has within a hospital setting. These graphic communications are key, when a hospital is experiencing high volume and renovations, allowing doctors and nurses to do their job, and not direct traffic. The communication of such spaces or instructions need to have clarity and distinction to maximize efficiency. In addition to circulation, visuals are key to patient maintenance and care, especially in any waiting period. This is evident in studies that suggested visibility of clocks from any location and glazing where barriers are needed physically but not visually . These design interventions allow for easier communication with patients, coworkers, and caregivers, so that they always have a place to reference the location of the patient or tools needed, such as a clock.
Lastly, patients are best understood by other patients, because of their shared experience; while overcrowding is a common problem in many Sub Saharan Africa hospitals, a study shows that other patients and social interaction can be a source of comfort and distraction. This study continues to state “conversations as a major activity” within the hospital as a patient, encouraging family to visit, and suggesting flexibility needing to be embedded in ward configurations for these activities to occur. By layering all these communication interventions, the experience of not only doctors, patients, and caregivers can be improved, but if done with clarity and ease, will improve the experience for children as well.
9,10,11,12,13,14,15
14
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
Pediatric-Specific Findings
After evaluating the various sources on general interventions and communication within a hospital for patient health, the initial research question must still be addressed by discussing these interventions in terms of pediatric health and outcomes. There must also be the consideration that newborn patients in the pediatric department will have different needs than those up to the age of 14-18 . One of the primary concerns for neonatal care is access to a 14 resuscitation center or room. In conditions where there was only one room not easily accessible by all patient rooms, there was a higher likelihood of patient mortality . Life-sustaining equipment and materials should be placed centrally, if they cannot be dispersed evenly throughout a space, to maximize the number of staff who can access them in dire situations . Not only will this allow nurses 16 and doctors to be able to reach supplies quickly, but it will also ensure that the staff members can watch each patient from the same distance.
To understand demands for space in a pediatric ward, it is important to acknowledge the number of people that may come to the hospital with these children. In order to keep these children under as little stress as possible and cared for entirely, family members and guardians are typically present . It has been suggested to design adjacent rooms for mothers and guardians to sleep so as to be close to their child or patient at all times through an outer corridor. This allows mothers and nurses to navigate through different halls . Maintaining separate circulation routes for staff and visitors is vital to the reduction of infection for them and the patient, as well as the reduction of traffic in situations where staff needs to access patients quickly. Access can also be discussed in terms
of visibility: the use of glass panelling is helpful to delineate spaces for different uses, while maintaining sightlines to patients . Since pediatric patients may not always be verbal in asking for help due to their young age, it is important for the professional staff to have maximum opportunities to notice visual signs of distress.
There have also been suggestions for how to break down the percentage of space for different kinds of care within the walls of the pediatric ward. General patient care should take up about 36% of the layout, equipped to handle lesser-dependency cases. Intensive care near reception and specialized care after intake should occupy 10% and 14% respectively, for a total of one-fourth of the space, to maximize the number of staff and equipment addressing high-need patients at multiple points along the patient-flow timeline . This type of layout is based on the fact that many young patients are lost during the intake process or shortly after because symptoms may escalate if they are not already addressed.
Bottlenecks of patients and staff were issues in certain pediatric case studies where patients are being admitted, so allowing for adequate room to move patients into their respective units will prevent flow-lines from crossing or reversing to avoid high-trafficked areas .
15
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
16,17,18,19,20,21,22
Conclusions & Reflections PEDIATRIC RESEARCH & SYSTEMATIC REVIEW
As a designer, it is our duty to see the events, experiences, and actions of the users (whom which we are designing for) in action. In us looking at our profession through the lens of another, we become better communicators and empathizers. By going through a systematic review, we can make connections of our equivalent in our field of architecture and landscape architecture--the case study. Similarly sources are collected that have similar criteria (program) to the proposed project at hand, and they are analyzed in terms of strengths and weaknesses. While not as tailored and reproducible as a systematic review, ultimately we are doing the same thing, but at different scales and with different lenses. For the medical profession, this reproducible quality is crucial to show validity, whereas architecture and landscape architecture may not require this as each client is unique and different, so our research methods are going to range from project to project engaging with the users in a way that is comfortable and useful to them and us. Most likely their might be a similar project again, but not identical. Clients don’t want to be treated as another number or person in the books, but rather want to be treated as a person, which forces us to have more organic and on the fly researching.
However, while different to our tradition of organic interactions, research, conversations, and analyzing, it is often hard to quantify the success and effects of our designs. Often as designers we might use a narrative to explain the effects or we will interview the users postdesign. The systematic review and the medical profession give great validity and assessment criteria to which we can prove the effectiveness of our design. While we as designers get lost in the ambiguity and what
if’s of design, we can use this evidence based design to say, it was proven effective in X Project with a similar program, so here is why it will work for you. By working through the lenses of interdisciplinary methods, we can give reassurance to our clients and eliminate some biases we may have as designers, and replace it with backed research. While this method is very explicit in showing one’s credibility and validity through the reproducibility of their systematic review, the turn around is long for the design profession, and the collection method for sources is timely, and may rule out other sources of another topic that might be beneficial. Ultimately our goal would be to implement the sources found, not write them--us using them will bring the interventions and studies to life as effective or ineffective.
REFLECTION:
This process was a valuable insight into where architecture and medicine need to meet to successfully create impactful healthcare. Being able to see how healthcare truly works and the issues they face when delivering healthcare in these settings, we are better equipped as designers to addressing those specific problems.
16
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Infographics on the Current State of Gender Disparity in the Medical System
On average, women assess nursing care lower than men
Men tend to look for social support from their spouse Without that support, women look for competancy in nurses
1 in 6 women experience a lack of privacy







during visiting hours
In the women’s surgery ward, there is only 1 nurse for every 80 patients
why is this relevant?
- In KCH, patient beds are arranged in a line down a hallway.


















































































- Guardians all come in at once to take care of the patients, creating a very crowded and hectic environment.



why is this relevant?
- Malawi is a patriarchal society where it is usually the woman’s job to be a guardian at the hospital.


19
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
GENDER DISPARITY
Current State of Guardian Circulation & Housing
We began the inventory by identifying that the guardian population was largely female and so to improve their experience would be one step towards achieving an overall balance in gender inequalities in the country. The issue that was identified in this situation, was the congestion of circulation and the mixing of populations namely : nurses, doctors, patients, and guardians.
As shown in the diagram, the main axis is where these population traverse through to get to the other areas of the hospital. The proposed solution for this was the next step. The goal was to alleviate the congestion in that axis and create special circulation routes for the guardians.


20
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
GENDER
AUNDRY GUARDIANHOUSING KITCHEN MARKET walls & boundaries guardian circulation 1800’ HOUSING TO LAUNDRY 1200’ HOUSING TO LAUNDRY 1800’ HOUSING TO LAUNDRY 800’MARKETTOHOUSING 830’MARKETTOKITCHEN
DISPARITY
LAUNDRY 200 2 40 260 1 00 180 100 100 100 80 80 120 100 1 20 60 60 200 200 210 190 190 260 260 200 290 140 circulation within the hospital 150 180 50 150 165 165 180 180 75 50 1 50 1 50 1 70 1 50 1 50 1 00 1 00 1 20 320 50 50 50 50 80 80 300 1 00 1 60 1 60 1 60 1 40 1 80 75 75 80 260 280 GUARDIANHOUSING
This first diagram is of travel distances within the campus through the main circulation paths.
This second diagram is of travel distances within the campus between the areas that guardians would typically need to go to provide care to their patient.
In this proposal, my group proposed to divide the current resources for the guardians that are available in terms of their living area into six pieces. These six pieces could then be distributed around the campus so that each unit caters to a specific program or node of the hospital. This would result in shorter travel distances for the guardians to their patient and it would also pull guardian cirulation away from the central axis of the hospital where most congestion and population conflict happens.

Current State of Guardian Circulation & Housing GENDER DISPARITY
21
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
= volume of current guardian housing volume of separated guardian housing LAUNDRY GUARDIANHOUSING MARKET circulation for guardians main circulation DISTANCE TO MARKET: 1210’ DISTANCE TO LAUNDRY: 1410’ DISTANCE TO KITCHEN: 980’ DISTANCE TO MARKET: 1410’ DISTANCE TO LAUNDRY: 1510’ DISTANCE TO KITCHEN: 860’ DISTANCE TO MARKET: 1330’ DISTANCE TO LAUNDRY: 870’ DISTANCE TO KITCHEN: 260’ DISTANCE TO MARKET: 940’ DISTANCE TO LAUNDRY: 580’ DISTANCE TO KITCHEN: 80’ FORMAL KITCHEN INFORMAL KITCHEN INFORMAL KITCHEN DISTANCE TO MARKET: 790’ DISTANCE TO LAUNDRY: 30’ DISTANCE TO KITCHEN: 120’ DISTANCE TO MARKET: 520’ DISTANCE TO LAUNDRY: 430’ DISTANCE TO KITCHEN: 390’ DISTANCE TO MARKET: 630’ DISTANCE TO LAUNDRY: 560’ DISTANCE TO KITCHEN: 100’ DISTANCE TO MARKET: 610’ DISTANCE TO LAUNDRY: 260’ DISTANCE TO KITCHEN: 670’
GENDER DISPARITY
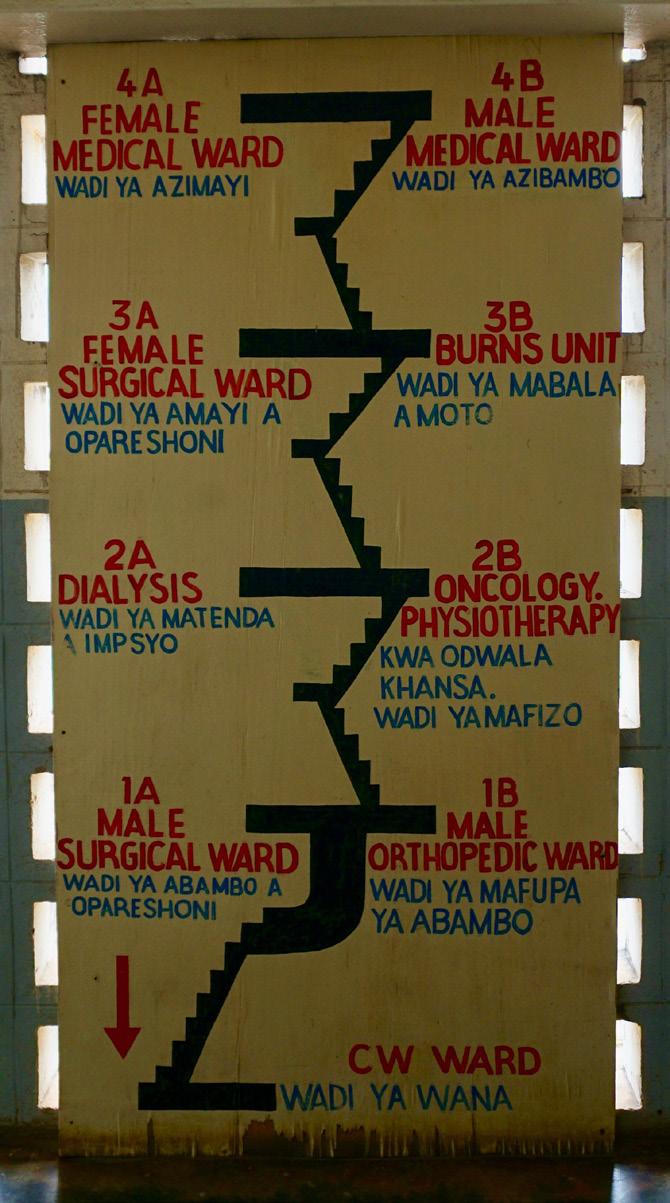
Current Gender Distribution by Floor
Due to the lack of available information on the current wards at KCH, my team worked off of images we could find of the surgical ward and the outpatient tower. As shown above, many areas of the hospital are categorized by gender and the women recieve less care from the nurses as they are placed farther away and they do not have the time to reach each patient during their rounds.

22
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
men’s ward women’s ward mixed Current End of Day Current doctor time with men doctor time with women mixed
In this proposal, the male and female wards are placed side by side to allow for equal attention from the medical staff. This allows nurses to travel past both genders before their shift is over and they can treat individuals equally and efficiently.
In the current system, nurses are so overwhelmed that they are
GENDER DISPARITY
Proposed Gender Distribution by Floor
unable to reach every patient, and so if women are placed at the top of the tower, nurses will most likely miss them during their shift. As shown in the diagram above, if the wards are reorganized as proposed, the nurses may not be able to reach everyone but at least there is no inequality in the people that he/she is able to reach.
23
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
End of Day Current Ideal doctor time with men doctor time with women mixed
Ideal men’s ward women’s ward mixed
DISPARITY
Current State of Maternity Ward & Guardian Relationship
Informal Guardian Housing only Used During the Day
Maternity Wards
The specific maternity ward layout is unknown but it might be similar to the pediatric ward layout. This bed configuration was inferred from the photos we had available of Kamuzu Central. In the maternity ward, the guardians stay with the patient at night on a mattress on the floor next to the bed. This results in circulation congestion and overcrowding.
24
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Current maternity guardian Patient Bed Guardian Bed Guardian Bed Guardian Bed Guardian Bed Patient Bed Patient Bed Patient Bed a p p r o x 5 ’ approx. 5.5’ Maternity Guardian Bed Guardian Bed
GENDER
_Maternity might be similar layout. _Guardians on a mattress
Constraints
_Lack of resources to construct new guardian housing closer to the maternity ward.
Proposed State of Maternity Ward & Guardian Relationship GENDER DISPARITY
Guardian housing containing beds, kitchen, and laundry space
Proposed stae maternity ward guardian relationship
Opportunities
_Can persuade and be guardians because both genders comfortable during hospital.
Constraints
_Lack of new guardian housing maternity ward.
Maternity Wards
In this proposal, we explored opportunities to possibly persuede more men to come and be guardians for their family members. if this happened it could possibly lead to both genders feeling more comfortable during their stay at the hospital. The constraints with this are the lack of resources to construct new guardian housing closer to the maternity ward.
Maternity Wards
kitchen,
25
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Patient
Patient
a p p r o x . 5 ’ approx. 5.5’
Patient Bed
Bed Patient Bed
Bed
PEDIATRICS SCHEMATIC DESIGN
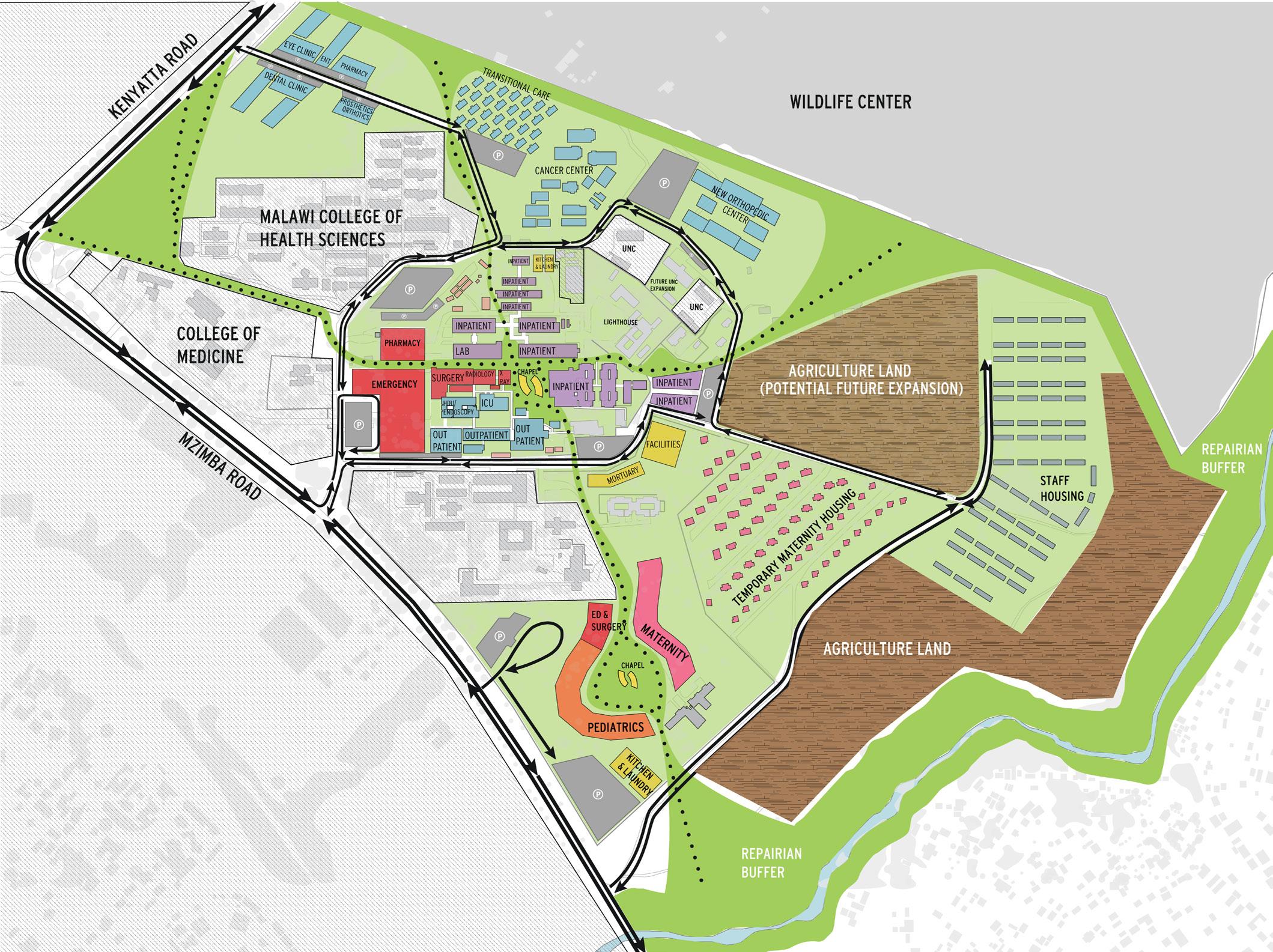
Once the inventory and analysis phase was complete, I was placed in a five person group to create an effective master plan for KCH. Our focus for this exercise was pediatrics and maternity.
We began the planning exercise by utilizing the site-wide inventory and analysis done by the class and identifying key factors that will need to be addressed in the 20 year master plan. We identified that the emergency services, pediatric services, and maternity services will be the populations of the hospital that will have the most growth. This meant that in our design, we had to accomodate a larger square footage for these programs.
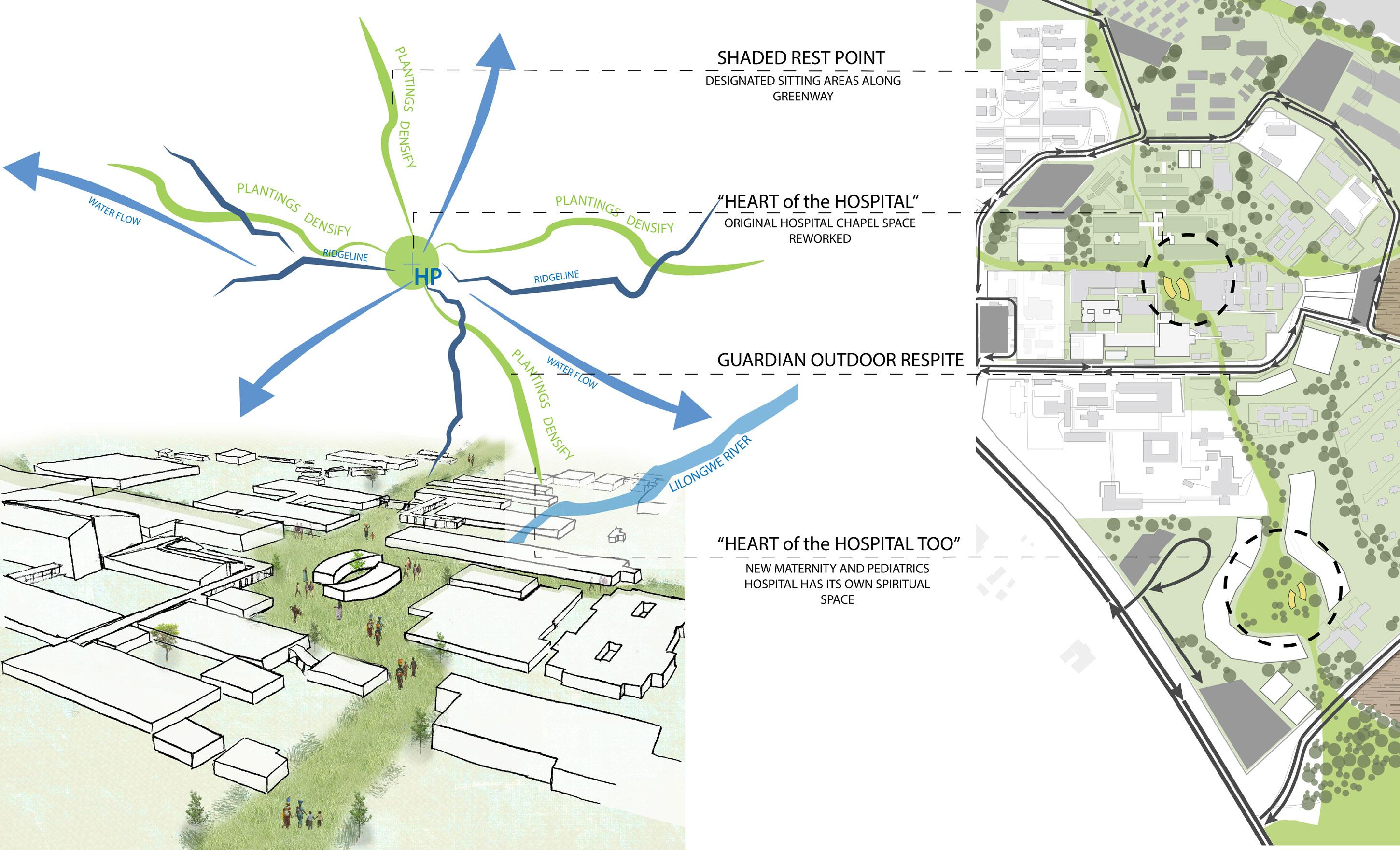
While we tackled the practical aspect of the hospital growth and development, it was also necessary to look at healing through the landscape. As a group, we also took into account how the landscape is affected by our design as well as how we should want the landscape to impact the design.
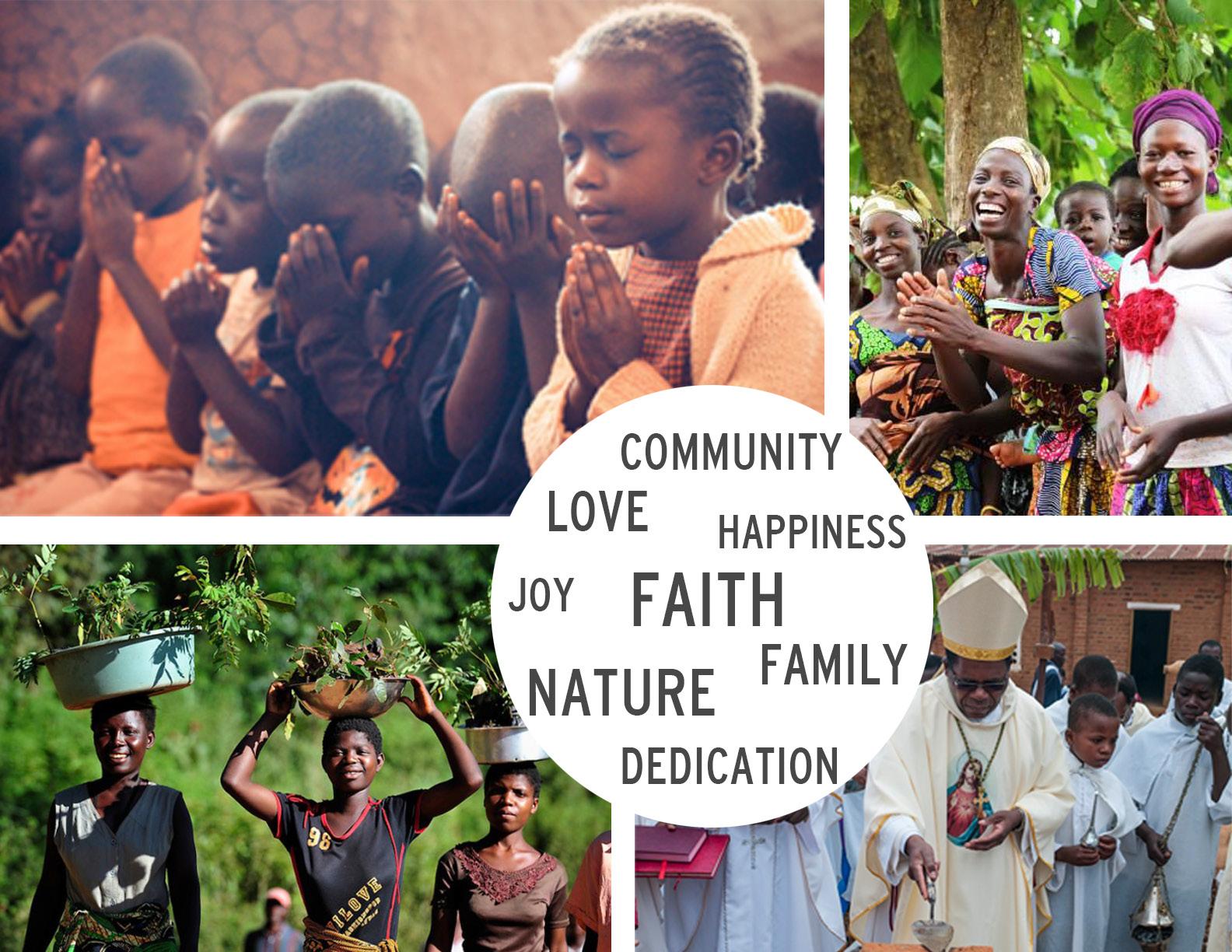
Finally we brought it all down to our learning of the culture of Malawi and its people. The strength in the communities of Malawi inspired us to create a tightly knit society within the hospital. We also looked at this cultural aspect to be spiritual as well due to the influence that religious beliefs has in the societies of Malawi and how important it is to the people.
We wove all of these threads together to create the design: practicality and hospital needs, the landscape, and the culture of Malawi.
When we began planning our design for KCH, we recognized that Malawian’s faith, relationship with nature, and strong sense of community were crucial to their way of life. We use these concepts to guide our design and ensure that we are creating spaces that best celebrate the people that will be using them.
26
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Site Analysis

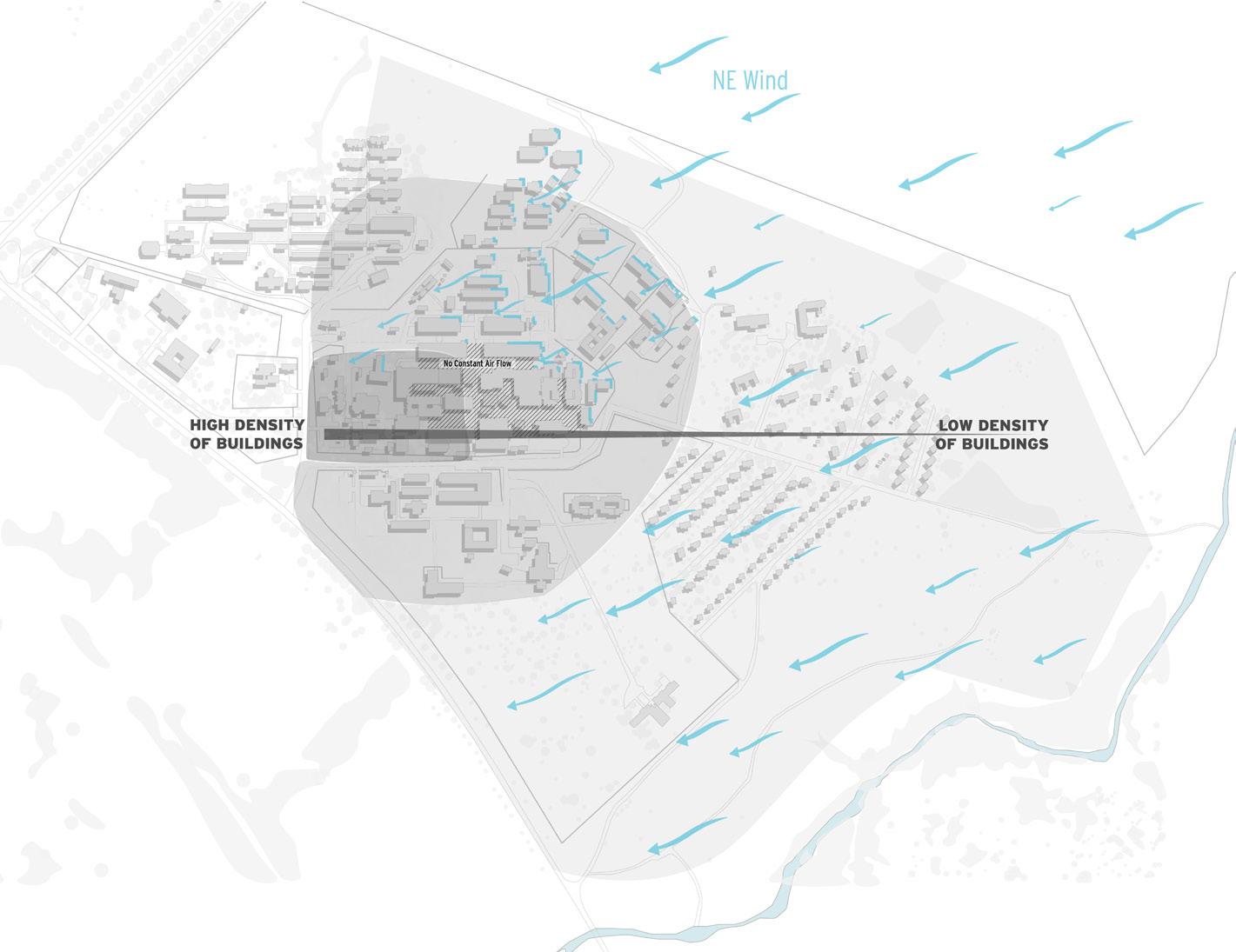
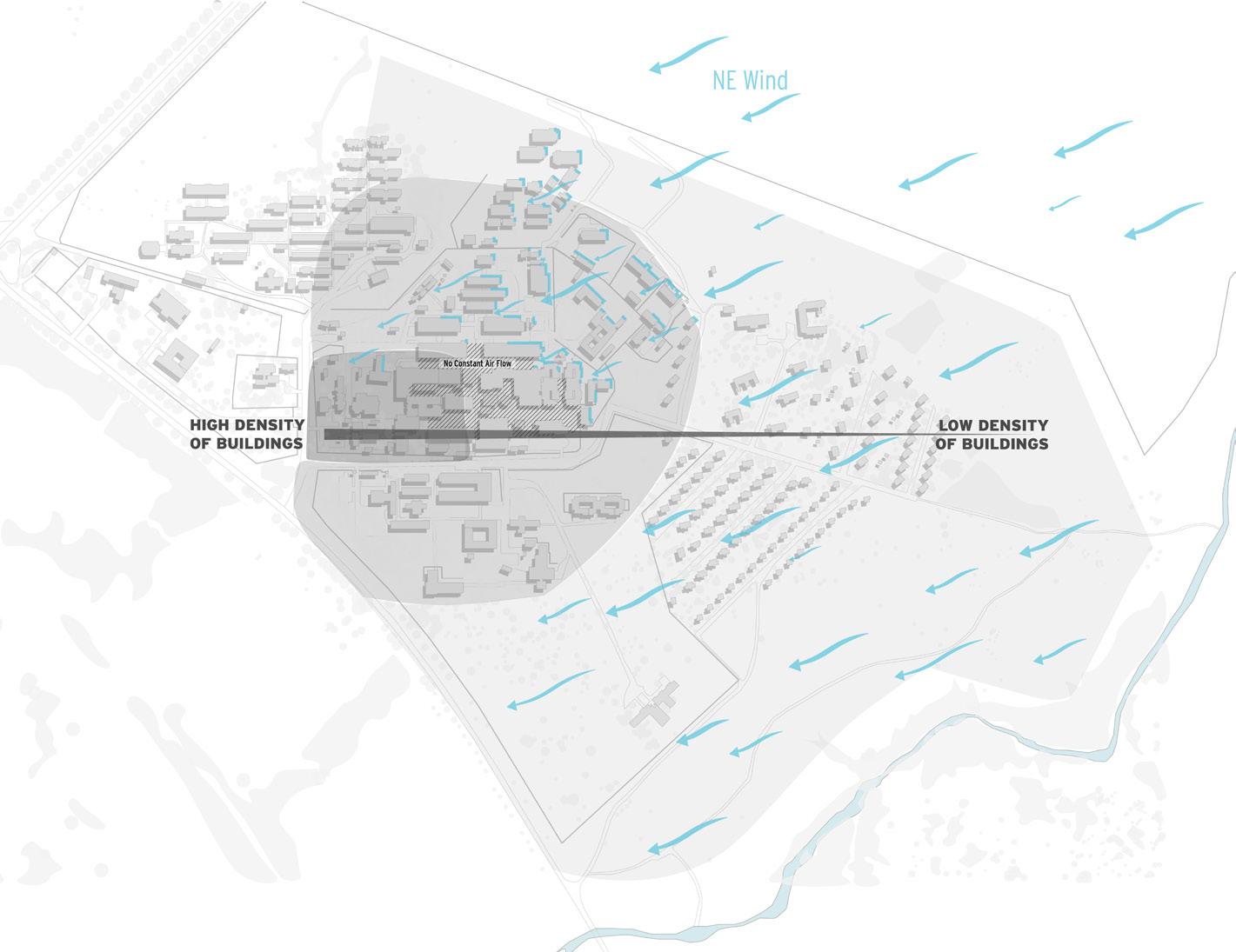
Density & Wind Solar, Green Buffers & Stormwater
The need for proper air circulation for the hospital is vital, so we studied wind conditions of the site to consider where building footprints might lessen during expansion to allow for natural air circulation. Examined also were opportunities where solar panels would be of best use, as well as the movement of water for capture and management. Green buffer zones create a natural boundary
next to nearby natural elements to be preserved. Combined, the analysis reflects some of our priorities in planning for the future pediatrics and maternity wards: proper air ventilation and comfortable outdoor spaces.
27
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Community Spaces
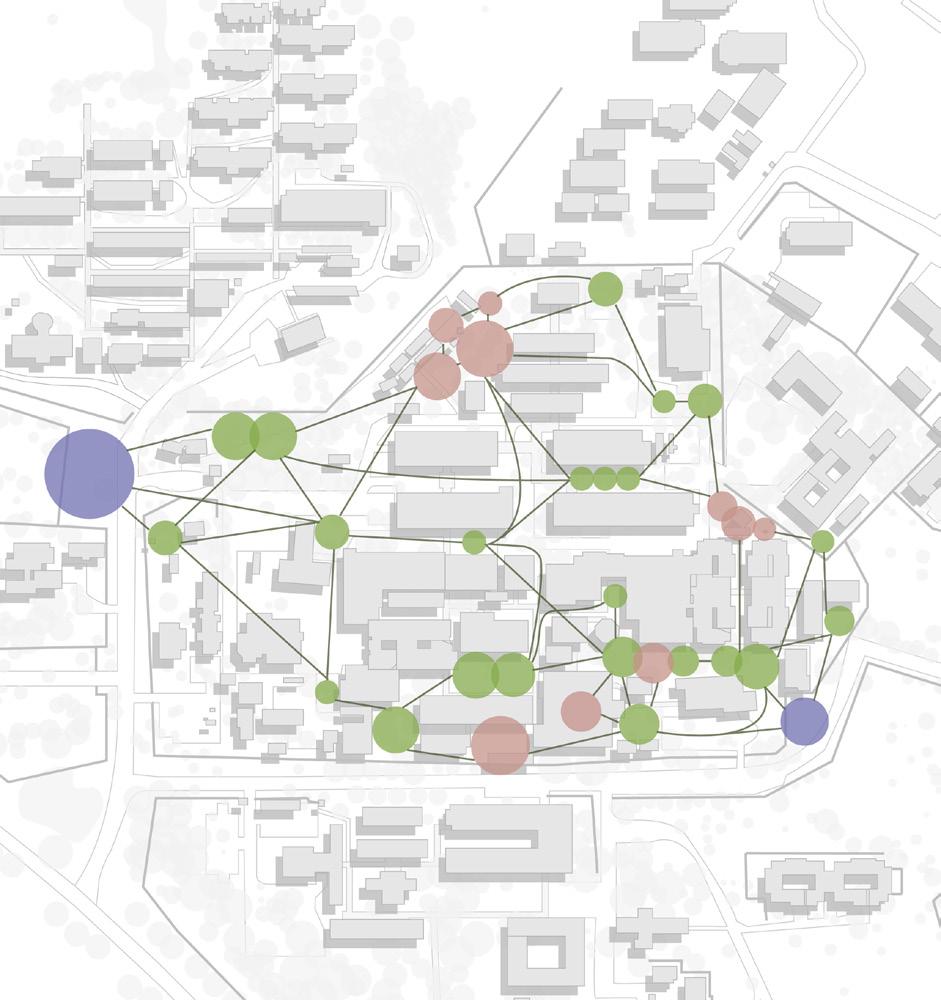
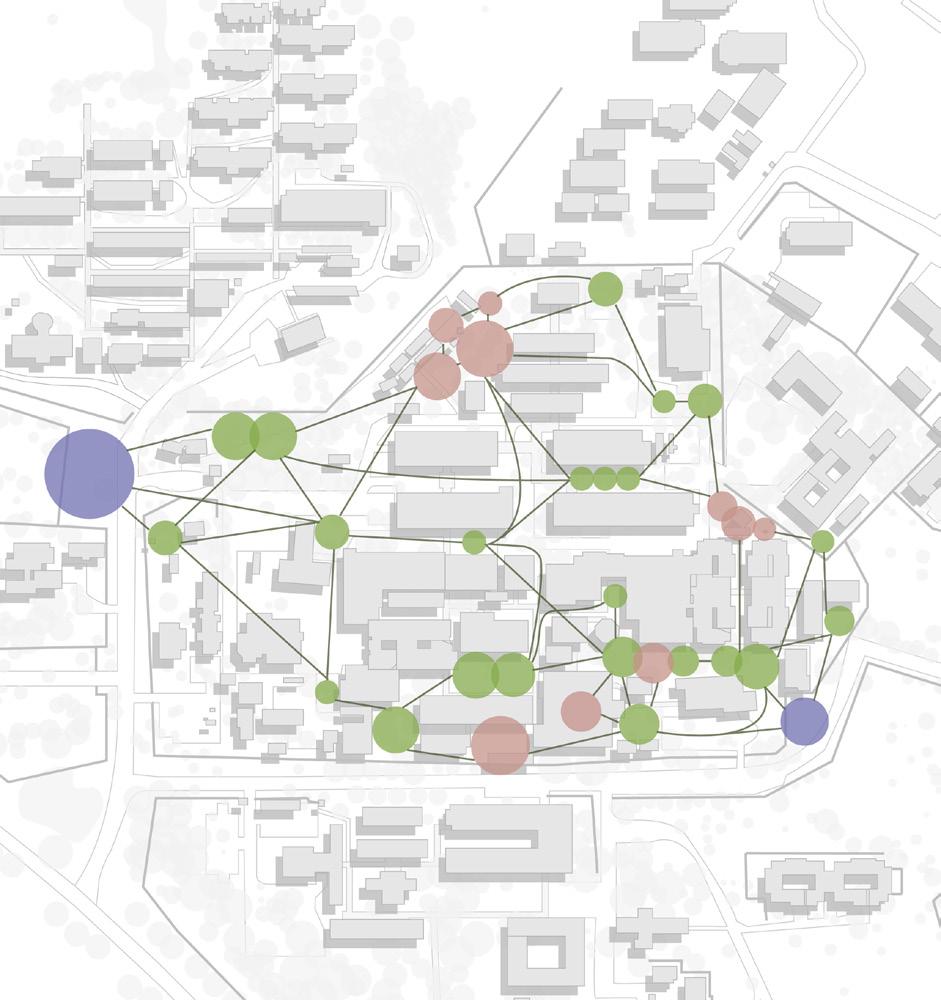
We also identified how the existing hospital campus nurtures one’s relationship with nature. By locating different types of outdoor spaces and their seemingly random connections, our proposal begins threading these spaces together through four main circulation corridors that guide users throughout.


28
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Existing Outdoor Spaces Existing Arbitrary Circulation Proposed Connecting Circulation MARKET GREENSPACES GUARDIAN SPACES
CRITICAL RELATIONSHIPS
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Goals & Targets
Reduce travel distance between maternity and pediatric wards
Reduce travel distance between wards and the surgery wing MORTALITY RATES
GAURDIAN EFFECTIVENESS
Provide housing facilities closer to wards, w/laundry & kitchen
Provide seperate facility with surgery for maternity & peds POPULATION GROWTH
Move emergency department closer to the main entrance EMERGENCY ACCESS
Harvest solar power gains with northern faced solar panels CONSISTENT POWER
Capture and store 50% of the stormwater that falls on site CONSISTENT WATER
Provide ample green space for patients, gaurdians and staff GREEN SPACE
Prior to design, we also worked to identify issues that we found most prominent for both Malawi and KCH. We began by identifying goals, both large and small, and then worked to come up with a
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
quantitative target that we could use to determine if we met our goals. For example, reducing child mortality rates BY providing resuscitation areas at equal intervals throughout a pediatrics ward.
29
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Concept Diagram & Statement
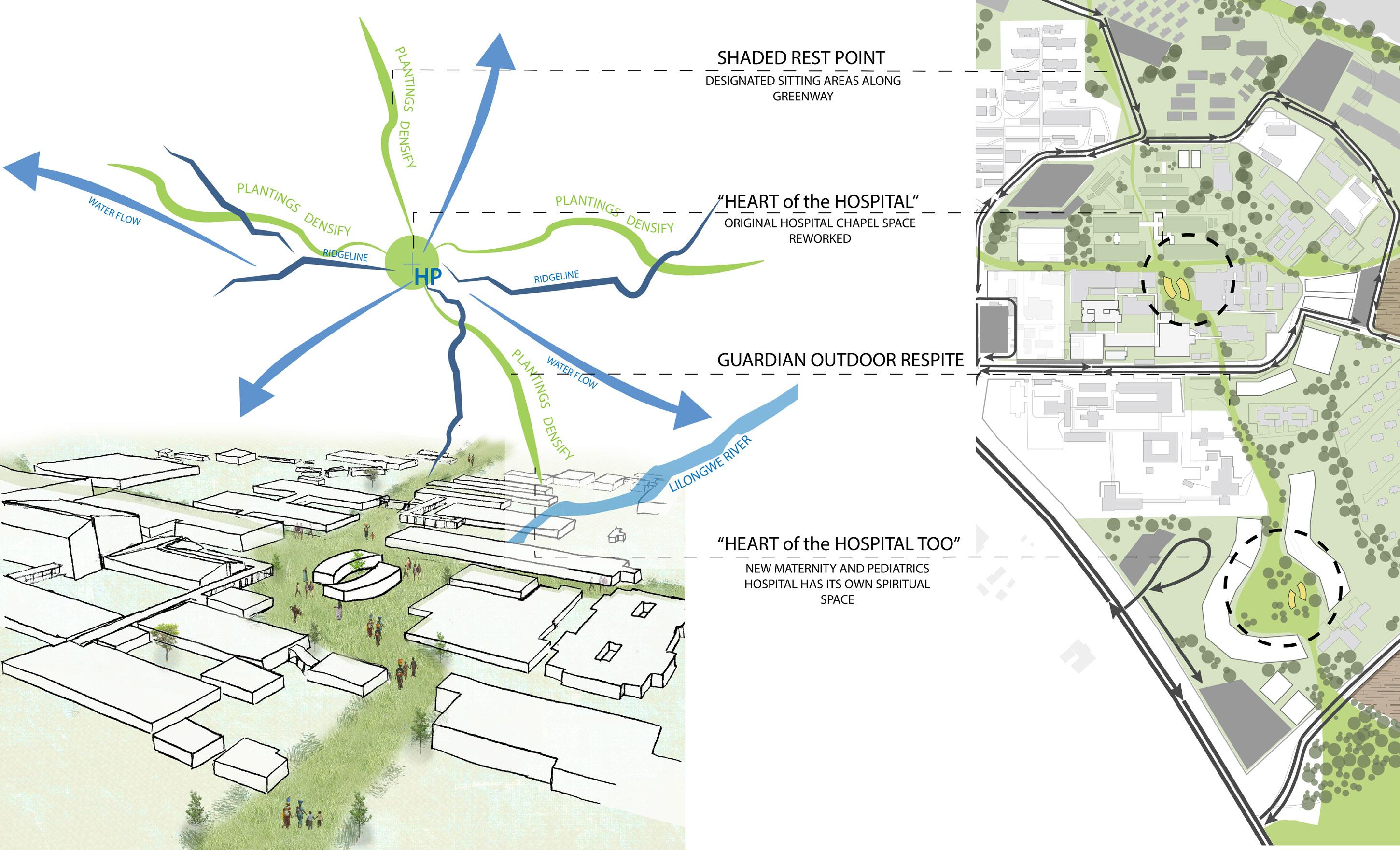
This scheme celebrates the strengths of the religious and social aspects of the Malawian culture by creating a spiritual center in the heart of the hospital that radiates via the landscape corridors.
Derived from both the analysis and values that have been identified, our design concept will work to celebrate the strengths of the spiritual and social aspects of the malawian culture by creating a faith driven center in the heart of the campus that radiates via landscape corridors.
According to the site analysis and the projection of the necessary square footage growth over the next 20 years, we proposed a number of changes on the site to create a better connection between the programs and allow for the radiating green corridor to form originating from the central social and cultural hub.

30
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Final 20-Year Plan

This final 20 year proposal depicts the new relationships that are able to form by creating zones for different types of program that allow efficiency in function while also maintaining an experiential quality within the campus through human-landscapeand program interaction. It features an outpatient clinic complex, a separate pediatric and maternity hospital, and an easily accessible emergency department. Strategies for agriculture and site health are also put in place with this scheme.
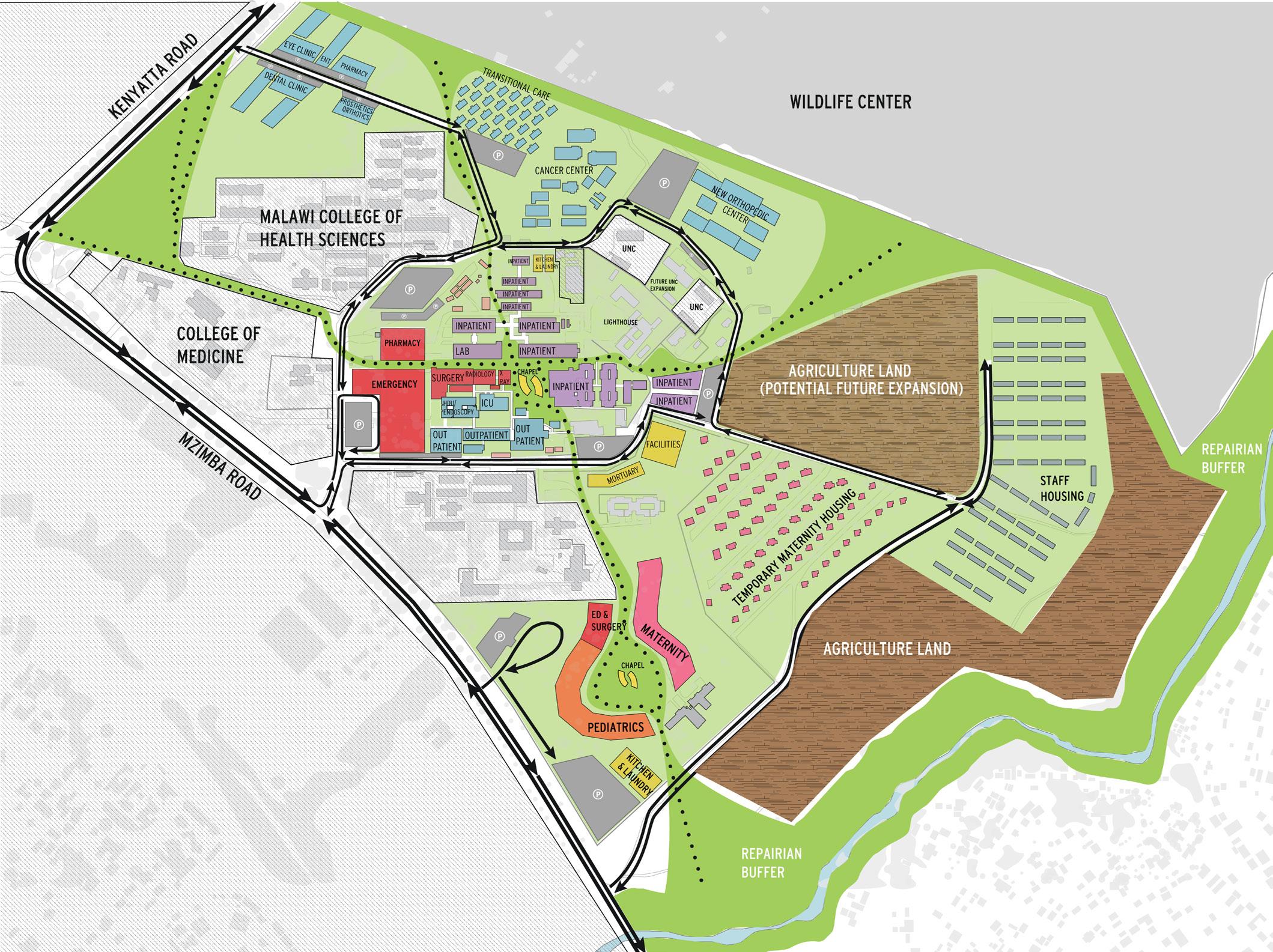
Vehicular Parking
Pedestrians
37
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRICS SCHEMATIC DESIGN

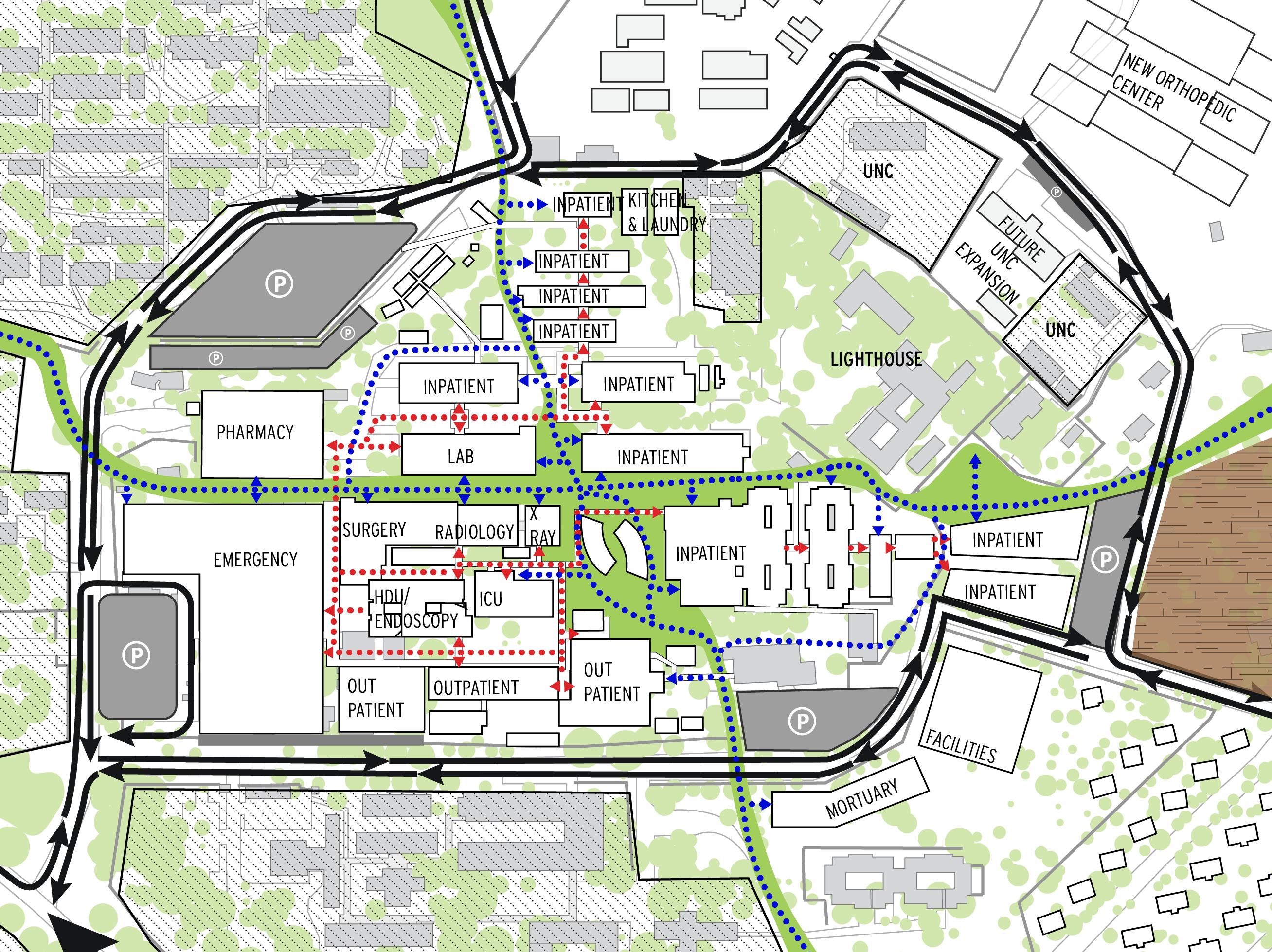
KCH Presentation: Final 20-Year Plan Micro
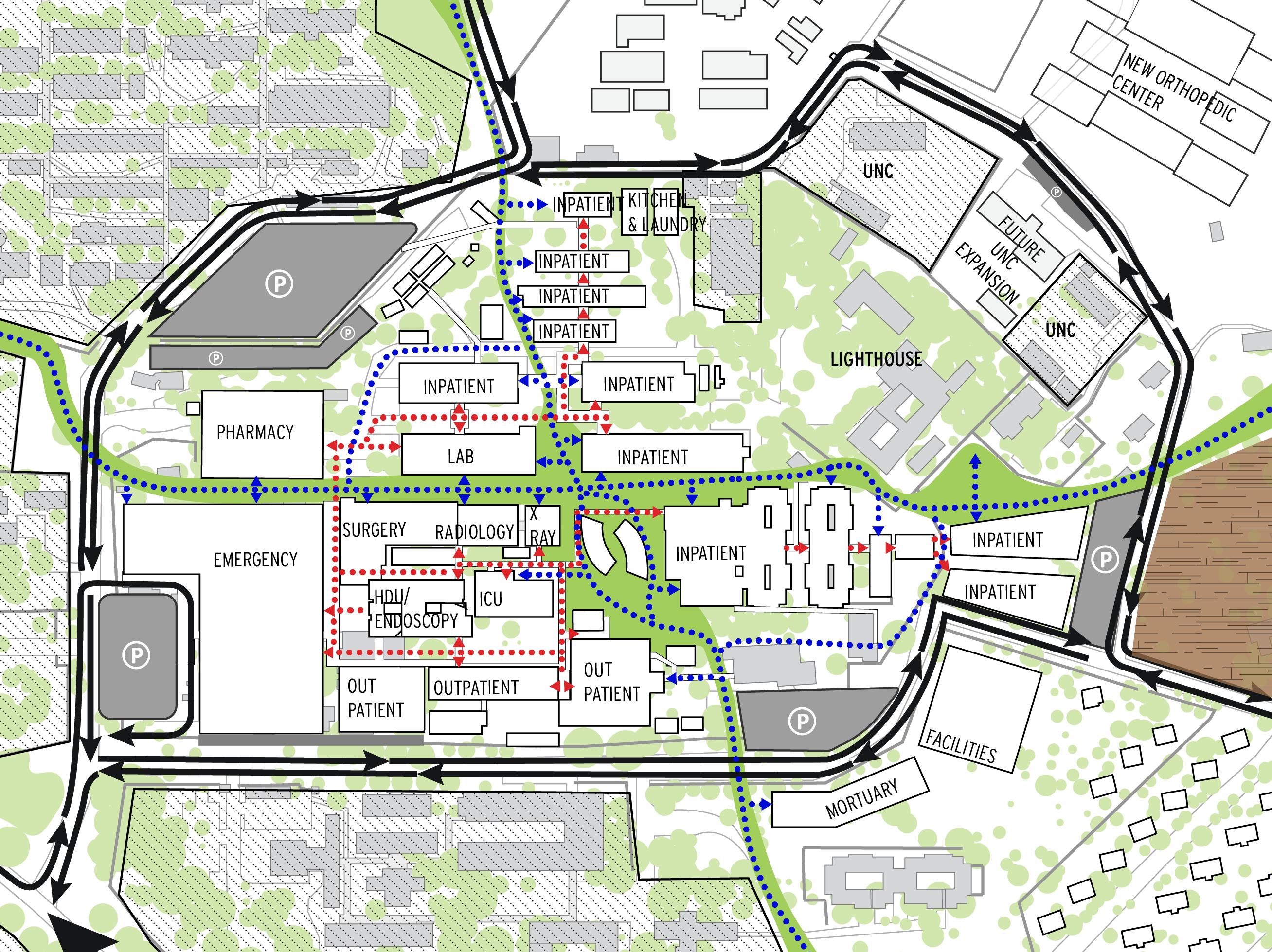
Zooming into the main center of the hospital, you can see the chapel as the spiritual core where the four green corridors radiate off of. These corridors provide circulation routes for guardians that is seperate from staff circulation between buildings, critical for saving time and optimizing patient care.
Vehicular
Guardians Staff
38
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Landscape Design
The proposed greenway mimics the way water flows through the campus: starting at the central “heart of the hospital” and branching through the rest of the site. The heart is where all user activity converges.
39
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Experiences
The emergency department shown in this rendering, will be located at the new main entrance of the hospital to allow for patients in critical conditions to be handled with immediacy.

The proposed pediatric ward will aim to create convertible, flexible and multi-use spaces for education and play. Giving each patient easy access to a restroom while also providing views to the outdoors was a requirement for each ward we proposed.

40
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Emergency Department Entrance
Proposed Pediatric Ward
Additionally, where our green corridors intersect with vehicular traffic,, we propose an overhead trellis structure that signifies to drivers that pedestrians will be crossing at these points.


PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Experiences
This scheme accommodates the projected growth while also striving to cultivate community within the hospital. The spiritual center shown here will function as a place of contemplation and revitalization where the hospital users may indulge in a peaceful environment that radiates throughout the hospital via the landscape corridors.

41
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Green Corridor - Street Intersection Chapel Courtyard
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Conclusion
PASTORAL CARE
HDU/ENDOSCOPY
CHAPEL LAB
PHARMACY
EMERGENCY
OUTPATIENT
INPATIENT
To evaluate the success of the scheme, we compared the projected growth of the hospital with the development of our proposal. While the colored bar represents the proposal’s potential, the black bar represents the 20 year needs. As you can see, our proposal can accommodate and fulfill the needs of nearly all departments for the projected 20 year growth of population
EYE CLINIC
EAR, NOSE, THROAT
DENTAL CLINIC
LAUNDRY KITCHEN FACILITIES
MORTUARY
PROGRAMMATIC NEEDS OF 2038 POPULATION
DESIGN PROPOSAL PROGRAM SIZES
42
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
PEDIATRICS MATERNITY MATERNITY WAITING HOUSING
SURGERY RADIOLOGY HIGH DEPENDENCY PROGRAM PRIORITY MISC. WARDS RELIGION CLINICS UTILITIES X RAY
PROSTHETICS/ORTHOTICS ICU
By focusing on the needs of Malawi’s projected population expansion while being sensitive to the cultural needs of the people and surrounding landscape, this group proposes expansion of Kamuzu Central Hospital’s maternity and pediatrics wards into their own hospital entity. In years past, Malawi reported the highest maternal mortality rate in Sub-Saharan Africa, and in order to combat this in future, we propose maternity expand to have its own full hospital departments like emergency and surgery, adjacent to an expanded pediatrics ward. The design scheme encourages user interaction with nature through circulation while separating guardians and staff at critical points to improve hospital efficiency, connecting new buildings to existing structures through greenways. Where most of the hospital’s current program resides, the repurposing of buildings over a 20-year timeframe creates distinction between inpatient and outpatient services. The approach to circulation includes keeping clinical services like dental and optometry at the hospital’s outskirts and the most critical patient needs like emergency services at Kamuzu’s main entrance, making it the first point of contact for most crucial patient needs. The chapel area is designed to be the heart of the hospital, located at the center of campus with multiple green corridors stemming from this point. Pedestrian circulation meanders along these corridors of plantings branching out from one chapel area to all
PEDIATRICS SCHEMATIC DESIGN
KCH Presentation: Submitted Abstract
hospital programming, including a second chapel space for the new maternity and pediatrics sector. Staff, guardians and patients alike may enjoy the fruit trees and aloe, the flora densifying as building footprints thin leaving the campus. By taking on the challenge to maintain 70-percent green space on campus with the addition and expansion of building footprints, this group intersects celebration, agriculture and other outdoor respite spaces, encouraging the outdoors and indoors of the hospital are equal in user engagement .
Research has shown that women in Malawi may shy away from birthing at facilities they do not feel are adequate, and with future projections of populations, the current maternity ward at Kamuzu Central Hospital would quickly become insufficient. The expansion of maternity from a ward to its own hospital entity will improve patient confidence in hospital facilities, and with proximity to pediatrics, there is opportunity for day-care programs to be developed in the hospital that will further increase patient confidence in birthing at Kamuzu, thus reducing mortality rates among delivering mothers. Our approach to the maternity and pediatric ward expansion also desires to decrease staff turnover by creating spaces of greenery that offer relief or delight.
43
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
EMERGENCY & MASS CASUALTY RESEARCH
From the Overall Plan
Once we had presented the overall master plan to KCH, our group decided to divide and conquer the main aspects of the scheme: the pediatrics ward, the maternity ward, the emergency ward, and the landscape by conducting more research and developing a thesis for the future develoment of that program. We also looked at these programs at multiple scales: the scale of a central hospital (KCH),
the scale of a district hospital, and the national scale as well. I focused on emergency with a specification of mass casualty. Due to the lack of resources, KCH cannot cope with a mass casualty in their ED and with the projected population growth in the next 20 years this number of emergency visits is only going to grow. This urgency to address this issue is what drove me to chose this topic.


44
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
OUTPATIENT CLINIC ZONE OUTPATIENT ZONE INPATIENT ZONE INPATIENT ZONE EMERGENCY ZONE FACILITIES & MORTUARY MATERNITY ZONE PEDIATRICS ZONE KITCHEN & LAUNDRY KITCHEN & LAUNDRY TEMPORARY HOUSING CANCER CENTER NEW ORTHOPEDIC CENTER LIGHTHOUSE UNC UNC RIPAIRIAN BUFFER RIPAIRIAN BUFFER WILDLIFE CENTER COLLEGE OF MEDICINE MALAWI COLLEGE OF HEALTH SCIENCES COLLEGE OF NURSING MZIMBAROAD KENYATTAROAD STAFF HOUSING TEMPORARY MATERNITY HOUSING POTENTIAL FUTURE EXPANSION TRAUMA WARD COLLEGE OF MEDICINE MALAWI COLLEGE OF HEALTH SCIENCES SURGERY ICU HDU RADIOLOGY X-RAY LAB MORTUARY HOSPITAL ENTRANCE
1.
EMERGENCY CARE
EMERGENCY & MASS CASUALTY RESEARCH
The Abstract
failure of health workers to identify serious complications and refer patients to tertiary care
care in the community
2.
care during transportation
PICO
QUESTION
3.
care on arrival at the receiving health facility
lack of appropriate vehicles, the absence or inadequacy of roads, and the inability to pay for transport services
slow or inefficient triage, overcrowding, lack of medical resources at facility, lack of water and electricity, insufficient human resources
_ Can faster emergency transportation and a more efficient triage system decrease the mortality rate of road traffic incident victims?
The main issues in the current emergency healthcare system revolve around a few main categories: the patient, the facility, the transportation methods, and the emergency healthcare triage. Due to a lack of structured and well equipped emergency transport, large distances to adequate health facilities, and lack of immediate access to preliminary basic emergency care road traffic accident victims present late.
Once they do arrive at a healthcare facility such as KCH, they are met with chaos, overcrowding, or have not been able to reach the hospital in the time they should have. There is also an overwhelming
lack of supplies and resources at these healthcare facilities whether it is a district hospital or a large central hospital which contributes to the facility’s inability to treat a large flux of mass casualty patients.
The development of a highly efficient and easily replicated trauma center model could possibly aid in achieving the PICO goal. Along with the replicated architecture, having a plan established for ambulatory circulation (on main roads such as the N-S road) to provide road traffic incident victims better emergency care in transit within a shorter time frame could also aid in saving lives.
45
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
EMERGENCY & MASS CASUALTY RESEARCH
Prominence of Road Traffic Injuries in Malawi
Large number of individuals involved
HOW DO INJURY BASED HOSPITAL VISITS COMPARE TO ILLNESS BASED HOSPITAL VISITS? 31
Lack of emergency medical support
Lack of ambulatory circulation
TRAUMA, BURNS, AND INJURIES
MALARIA, AIDS, AND HIV
Poor road quality
Road traffic injuries (RTIs) are a common cause of hospital visits in Malawi, and they are also the leading cause of adult injury-related deaths. Malawi has one of the world’s highest rates of traffic-related fatalities.
The mortality and disability burden from road traffic injuries in Malawi can be reduced by ensuring that every central and district hospital has a dedicated trauma unit with qualified staff who have completed primary trauma care courses and have access to the equipment necessary to save lives.
31
46
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
31
Distance to nearest health center INITIAL ISSUES 31
EMERGENCY & MASS CASUALTY RESEARCH
Prominence of Road Traffic Injuries in Malawi
Road Traffic Incidents are more prevalent during the rainy season while burn cases are more prevalent during the cold season.
Number of Trauma Cases
47
Road Traffic 23% Homicide 11% Suicide 15% Drowning 7% Fires 6% Falls 8% War 3% Poisoning 6% Other 21% CAUSES OF INJURY RELATED DEATHS SEASONALITY
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
OF TRAUMA INJURIES
March May July September November February April June August October December Rainy Season Cold Season Fall Season Hot Season
January
28 31 31 31
Annual Traffic-related Mortality Rate 35 per 100,000 residents
EMERGENCY & MASS CASUALTY RESEARCH
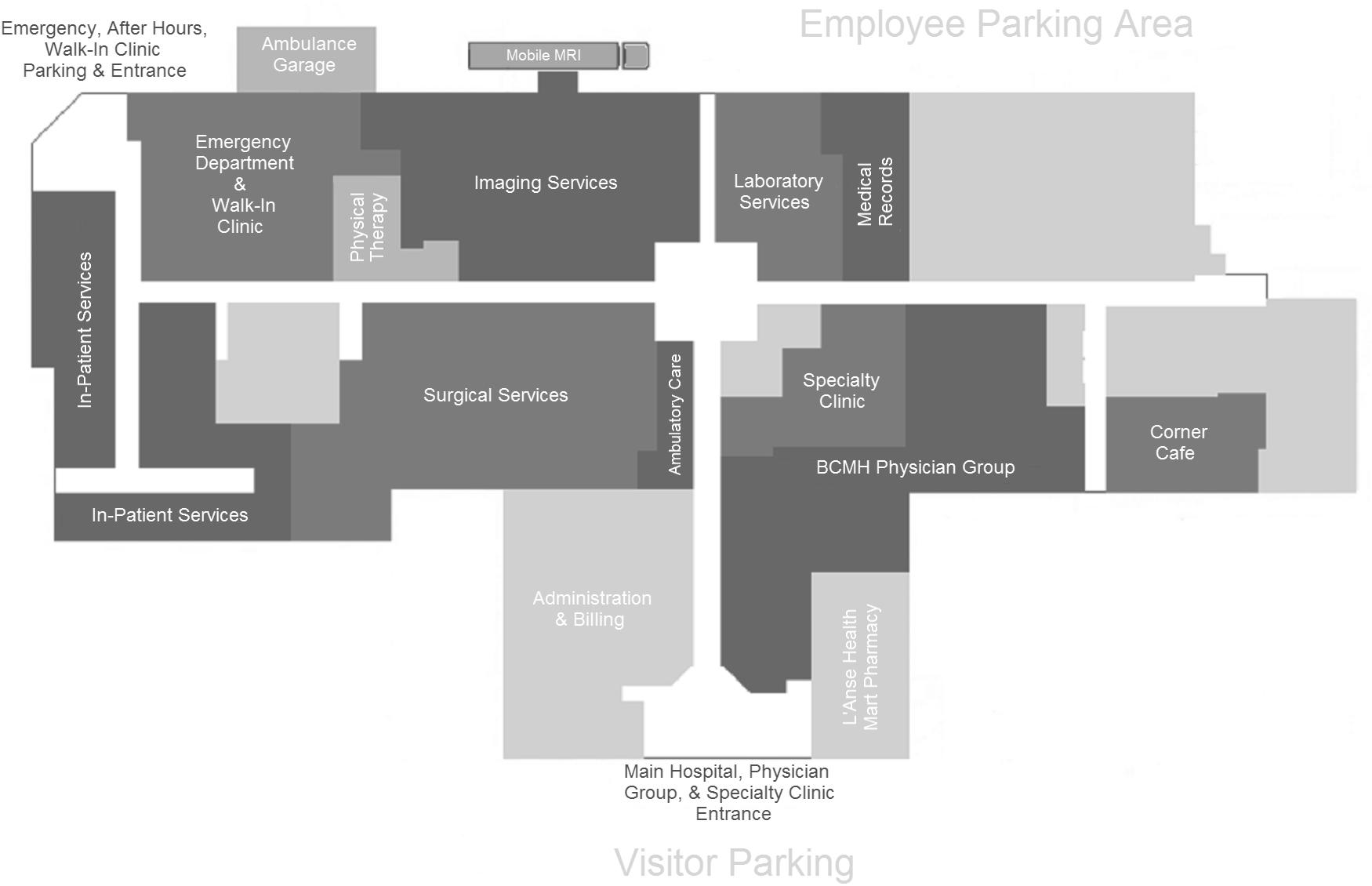
Emergency Services at District Hospitals
Each district or mission hospital has 100–200 beds and offer basic surgical services such as trauma management and obstetric emergencies. Four central hospitals (such as KCH), each with capacity of 600–1500 beds, form the tertiary level of care and offer more specialized medical and surgical treatment. KCH has 8 district hospitals which refer patients to it.
There are 2 surgery theaters at each district hospital and there are 3 at Mchinji. The bulk of the surgeries that happen at these hospitals are C-sections, not emergency trauma related cases. The personnel present at these district hospitals are also not certified (surgeons, anesthesiologists, obstetrician/gynecologists). Clinical officers are the primary providers of surgery and the sole providers of anesthesia.

48
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
6 7 8 9 10 11 15 17 Nkhotakota Kasungu Ntchisi Dowa Salima Mchinji Dedza Ntcheu District Hospitals N 6 7 8 9 10 11 15 17 MALAWI central southern northern MOZAMBIQUE ZAMBIA MOZAMBIQUE TANZANIA 0 25 50 100 km DISTRICT HOSPITALS THAT REFER TO KCH KCH 9.Dowa 49.2 km 1 - 1.5 hours 10 hours 10.Salima 98 km 1.5 - 2 hours 20- 23 hours 15.Dedza 86.3 km 1.5 - 2 hours 18 hours 7.Kasungu 126 km 2 - 2.5 hours 25 hours 6.Nkhotakota 194 km 3 - 3.5 hours 33 hours 8.Ntchisi 92.1 km 1.5 - 2 hours 20 hours 11.Mchinji 109 km 1.5 - 2 hours 24 hours 17.Ntcheu 167 km 2.5 - 3 hours 33 hours 33 33
EMERGENCY & MASS CASUALTY RESEARCH
Emergency Services at District Hospitals
There are almost 1,000-2,200 surgical cases per district hospital
Most common recorded procedures:
Cesarean section
Dilatation & Curettage
Tubal ligation
Fracture management
General Surgery
•I&D and Debridement
•Hydrocele repair
•Inguinal Hernia repair
•Laparotomy for peritonitis
Mass Casualty Incidents include those that occur with some level of frequency, also known as “conventional MCIs”: transportation incidents, burn, and severe weather events. When these types of incidents occur, the victims seek out the closest healthcare center that they can find. This is usually a District Hospital which may or may not, depending on the hospital, have the services and supplies to provide them with adequate healthcare.
This is why healthcare at the district level is given emphasis in the development model; because multiple geographic locations in a setting such as Malawi is more beneficial than one all-purpose healthcare center in a country where transport is either by foot or it is by minibus or truck. In this case, proposing an easily replicated and efficient trauma model which is flexible with the issues that Malawi’s healthcare facilities face everyday is a possible solution.
The benefits of that proposal lie in the access that it would afford the population in terms of transportation and quality of healthcare.
49 Thomas
University -
Jefferson
East Falls | Kamuzu Central Hospital
33 33 32
The Issue of Emergency Transportation and Travel Distance EMERGENCY & MASS CASUALTY RESEARCH
The Problem Statement
Malawi is a country that struggles with the quality of their roadways and their pedestrian- vehicular traffic. When road traffic accidents occur, the victims are faced with a number of initial issues: the quality of the roads, the travel distance to the nearest health center(district or central), the massive number of individuals involved in the accident, the lack of ambulatory circulation, the lack of emergency medical support to stabilize the victim prior to a health facility, etc.
Supporting Facts
About 5,700 of Malawi’s 17 million residents died from RTIs in 2015, even though there is only one motor vehicle on the road for every 40 residents. Road traffic injuries (RTIs) are a common cause of hospital visits in Malawi, and they are also the leading cause of adult injury-related deaths. Malawi has one of the world’s highest rates of traffic-related fatalities.
Is ambulatory transport like that in the USA possible in Malawi?
In Los Angeles, basic emergency ambulance transport is about $1,000 to $1,100. The cost is more like $1,200 to $1,300 for a transport that requires advanced life support. Included is the cost for paramedics and the ambulance ride itself. However, companies can charge extra for mileage, supplies and equipment.
There is also a shortage of human resources to be able to carry out more ambulatory circulation than already exists.
How is it being addressed?
Currently motorboats, canoes, bicycles with trailers, tricycles with platforms, tractors with trailers, reconditioned vehicles, and ox carts are used to transport injured road traffic incident victims to the nearest healthcare facility.
There is an emphasis that has been made to focus capital and resources to developing the district hospitals to reduce the burden on the tertiary healthcare centers
*There has been some information about ambulatory circulation being started on the road between Lilongwe and Blantyre. That portion of the road is the most heavily traveled on roadway in the country and so the introduction of ambulatory care on this major roadway could drastically make an impact on the outcomes of road traffic accidents.
50
University -
Thomas Jefferson
East Falls | Kamuzu Central Hospital
24 31
29 23
The Issue of Emergency Transportation and Travel Distance EMERGENCY & MASS CASUALTY RESEARCH
No barrier between heavy pedestrian population & vehicular traffic
Large volumes of people in open vehicles
Majorly dirt roads which make driving during the rainy season very difficult

Buses and Minibuses with large volumes of people are usually the vehicles that are in the mass casualty road traffic incidents
Between July 2013 and March 2014, more than 9,200 road traffic injuries (RTIs) and 100 RTI deaths were recorded by the participating hospitals along Malawi’s main north-south highway.



Thomas
6 Nkhotakota District Hospitals 6 7 8 KCH 9 10 11 15 17
Jefferson University - East Falls | Kamuzu Central Hospital
The Issue of Emergency Triage System and Ward Overcrowding EMERGENCY & MASS CASUALTY RESEARCH
The Problem Statement
When road traffic incident victims arrive at the healthcare facility (district or central), they are met with an inadequate triage system which delays their treatment. For a patient who has already lost recovery time during their transport to the hospital, an ineffective triage causes them to wait fatal waiting periods before they can get medical attention.
Supporting Facts
there is no objective triage system in place for patients over the age of 5 years
patients are seen in time order rather than according to medical urgency
the large number of patients and lack of human resources lead to delays in recognising those who are medically unwell thorough assessment and treatment is not performed due to lack of equipment and restricted space patients are transferred to a ward without any treatment where they will wait for the sole nurse working on a ward of three patients per bed to attend to them
How is emergency triage carried out in Malawi?
Malawi has not had an effective triage system to sort patients over the age of 5 years (for patients under the age of 5 years the WHO Emergency Triage Assessment and Treatment system is in place). The South African Triage Group developed a scale adapting existing models for use in Africa. The scale uses the simple color coding system of red, orange, yellow and green to determine urgency.
How is it being addressed?
Currently extra beds are used if possible and if not, the patients are placed on the sidewalk due to the low capacity of the emergency ward at KCH and district hospitals
There is an emphasis that has been made to focus on teaching clinical officers and healthcare workers in Malawi an effective and efficient triage system.
In Rumphi District Hospital in the Northern Region of Malawi, 80 healthcare workers were trained on this triage system using lectures, discussion forums and simulation on a 1-day course over a 1-week period by two emergency medicine physicians from the UK.
52
University -
Thomas Jefferson
East Falls | Kamuzu Central Hospital
26 25 30 25 25 30 25, 30 25 25
The Issue of Emergency Triage System and Ward Overcrowding EMERGENCY & MASS CASUALTY
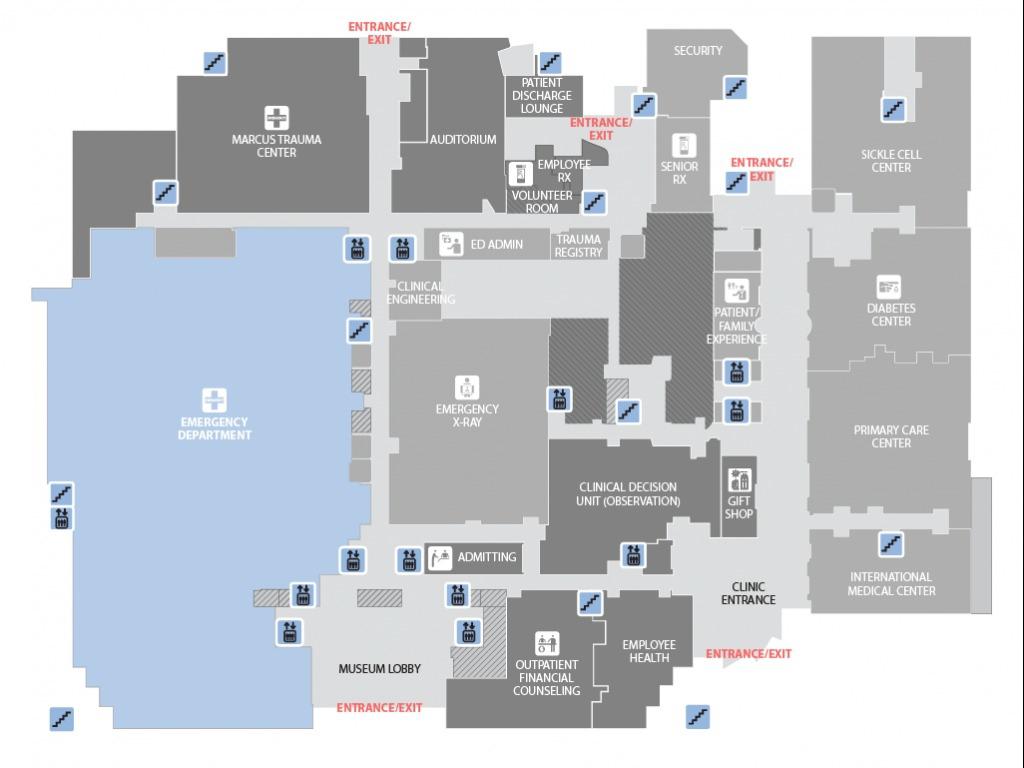
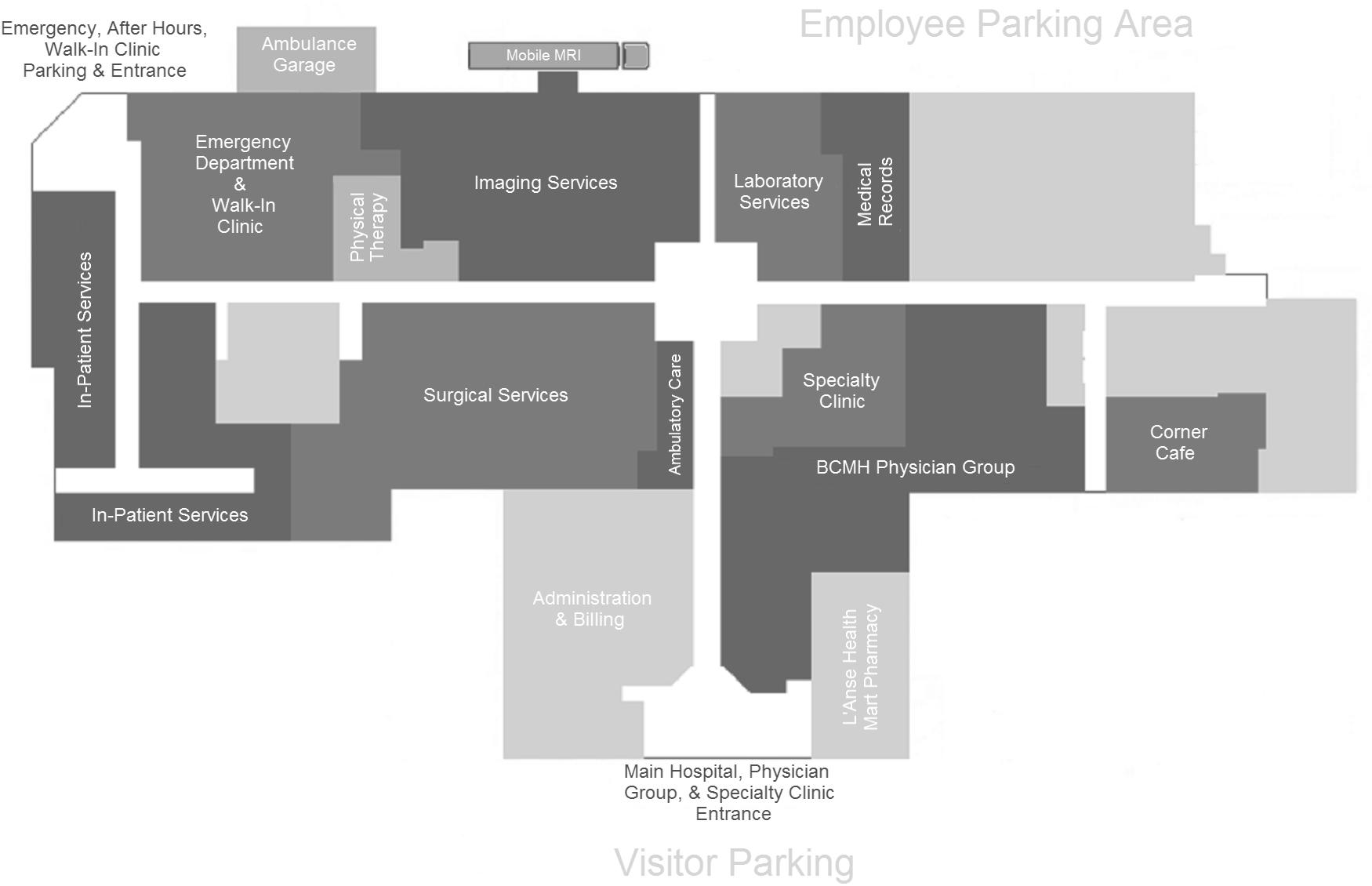
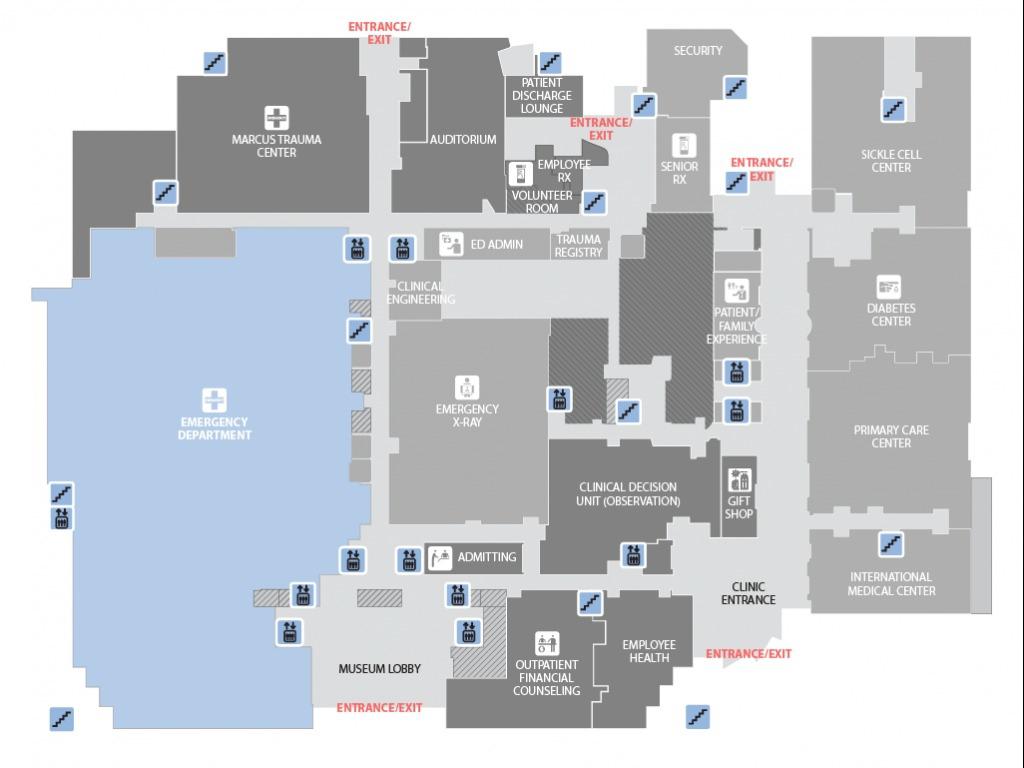
AN OPTION WHICH SHOWS THE NECESSARY PROGRAM ADJACENCIES
Baraga County Memorial Hospital, USA
RESEARCH
In these precedents onec an observe that the triage, surgery, emergency ward, ICU/HDU, imaging, and laboratory are located either adjacent along the same corridor or directly across from each other. There is an axis in the plan that connects all of these programs with a singular main circulation path for efficiency.
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
Grady Health System, USA
USA
53
TRIAGE ED WARD SURGERY X-RAY LAB TRIAGE ED WARD X-RAY PROGRAM ANALYSIS OF TWO HOSPITALS’ EMERGENCY WARDS
THE
IN
TRIAGE STEP 1 TRIAGE STEP 2 HDU/ICU SURGERY PHARMACY X-RAY/ RADIOLOGY ENTRANCE/SERVICE ENTRANCE > URGENCY/RISK EMERGENCY ENTRANCE ENTRANCE/SERVICE ENTRANCE > URGENCY/RISK EMERGENCY ENTRANCE
THE DEVELOPMENT OF A THESIS
THE PICO QUESTION:
I began my research by establishing the PICO question: Can faster emergency transportation and a more effective triage system decrease the mortality rate of road traffic incident victims?
METHODS:
My research on mass casualties and RTIs in Malawi was majorly literature review and it was conducted on the Jefferson Library databases. I plan on, in the future, conducting a systematic review on mass casualties in lower and middle income countries on PubMed. I also hope to get into contact with individuals and medical professionals to recieve feedback on the proposed solution.
THE CURRENT ISSUES:
The main issues in the current emergency healthcare system revolve around a few main categories: the patient, the facility, the transportation methods, and the emergency healthcare triage. Due to a lack of structured and well equipped emergency transport, large distances to adequate health facilities, and lack of immediate access to preliminary basic emergency care road traffic accident
victims present late. Once they do arrive at a healthcare facility such as KCH, they are met with chaos, overcrowding, or have not been able to reach the hospital in the time they should have. There is also an overwhelming lack of supplies and resources at these healthcare facilities whether it is a district hospital or a large central hospital which contributes to the facility’s inability to treat a large flux of mass casualty patients.
PROPOSAL:
The development of a highly efficient and easily replicated trauma center model could possibly aid in achieving the PICO goal. Along with the replicated architecture, having a plan established for ambulatory circulation (on main roads such as the N-S road) to provide road traffic incident victims better emergency care in transit within a shorter time frame could also aid in saving lives.
54
Thomas Jefferson University - East Falls | Kamuzu Central Hospital
SUPPORTING INFORMATION:
Malawi’s healthcare system is tiered which means that victims of mass casualty incidents such as road traffic incidents seek help at district hospitals initially and then from there, if needed, they are referred to the Central hospital. this means that the district hospitals are the first point of contact to the population. I focused on road traffic injuries because they’re the leading cause of adult injury-related deaths and Malawi has one of the world’s highest rates of traffic related fatalities.
THE DEVELOPMENT OF A THESIS
The emergency response system in Malawi for these types of road traffic incidents is quite unorganized and it leads to a high mortality. I identified two main issues: the issue of emergency transportation and travel distances and the issue of emergency Ward triage and overcrowding.
In terms of the issue of emergency transportation and travel distance, the basic issues are that there is a large population involved in these incidents, there’s a lack of ambulatory circulation along the roadways where these injuries are most common, the distance to the nearest health center is quite far, the roads are of poor quality and makes vehicular transportation difficult, and
there is a lack of emergency medical support. The current solution for this issue is that patients utilize motorboats, canoes, bicycles with trailers, tricycles with platforms, tractors with trailers, reconditioned vehicles, and ox carts as transport.
When it comes to the issue of emergency Ward triage and overcrowding the main problems are that when victims arrive at the healthcare facility, they are met with an inadequate triage system which cannot handle a flux as large as one that comes with a mass casualty. this ineffective triage system causes them to wait almost fatal waiting periods before they can get medical attention. Due to this triage system, overcrowding is also a big issue and due to the low capacity of the emergency Ward at KCH and other district hospitals patients are placed on the sidewalk.
In conclusion my proposal of building multiple efficient and easily replicated trauma centers between the district hospitals along the roadways where these mass casualties occur, would reduce travel time for victims and increase their response time and in turn their chance for survival. If these trauma centers also had an efficient triage system and possibly a flexible emergency ward space, they would be able to manage the large flux of patients as they arrive.
55 Thomas Jefferson University - East Falls | Kamuzu Central Hospital
BIBLIOGRAPHY
“Malawi” Countries and Their Cultures. Accessed August 22, 2018. http://www.everyculture.com/Ja-Ma/index.html.
Jenkins, David Thomas, and Laura Jane Veal. “Volunteering in Africa.” The BMJ. June 23, 2010. Accessed August 31, 2018. https://www.bmj.com/content/340/bmj.c3251.
“My Experience as a Healthcare Volunteer in Africa.” OneWorld365.org - Meaningful Travel, Gap Years, Volunteer, Teach, Work, Intern & Study Abroad. Accessed August 31, 2018. http://www. oneworld365.org/blog/my-experience-as-a-healthcare-volunteer-in-africa.
O’Hare, Bernadette, Ajib Phiri, Hans-Joerg Lang, Hanny Friesen, Neil Kennedy, Kondwani Kawaza, Collins E. Jana, George Chirambo, Wakisa Mulwafu, Geert T. Heikens, and Mwapatsa
Mipando. “Task Sharing within a Managed Clinical Network to Improve Child Health in Malawi.” Human Resources for Health13, no. 1 (2015)
Hongoro, Charles, Barbara Mcpake, and Peter Vickerman. “Measuring the Quality of Hospital Tuberculosis Services: A Prospective Study in Four Zimbabwe Hospitals.” International Journal for Quality in Health Care 17, no. 4 (2005): 287-92. doi:10.1093/intqhc/mzi040.
Mortier, Stéphane Du, and Monica Arpagaus. “Quality Improvement Programme on the Frontline: An International Committee of the Red Cross Experience in the Democratic Republic of Congo.” International Journal for Quality in Health Care 17, no. 4 (2005): 293-300. doi:10.1093/intqhc/mzi042.
Fekadu, S., and B. Getachewu. “Microbiological Assessment of Indoor Air of Teaching Hospital Wards: A Case of Jimma University Specialized Hospital.” Ethiopian Journal of Health Sciences 25, no. 2 (2015): 117. doi:10.4314/ejhs.v25i2.3.
Are hospitals prepared to support newborn survival? - An evaluation of eight first-referral level hospitals in Kenya
OO Bankole, JO Taiwo, “Quality of careat a pediatric dental clinic in Ibadan, Nigeria,” Niger J Clin Pract. 16, no. 1, (Jan-March 2013) 5-11.
C. Nord, “Patient sociality in hospital architectural space: a qualitative case study in Namibia,” World Hosp Health Serv. 41, no. 2 (2005): 17-20, 40, 42.
A Leonard, C Bonaconsa, L Ssenyonga, M Coetzee, “Graphic facilitation as a novel approach to practice development,” Nurs Child Young People 29, no. 8 (October 2017): 42-45.
AL Leonard, A Verster, M Coetzee, “Developing family-friendly signage in a South African paediatric healthcare setting,” Curationis 37, no. 2 (November 2014):1-7.
KD Bream, S Gennaro, U Kafulafula, E Mbweza, D Hehir, “Barriers to and facilitators for newborn resuscitation in Malawi, Africa,” J Midwifery Womens Health 50, no. 4 (July-August 2005): 329-34
PN Swift, “The hospital care of East African children. Levels of care and lines flow. Planning a paediatric centre: the paediatricians view,”J Trop Pediatr Environ Child Health 18, no. 1 (March 1972): 82-3.
C. Nord, “Patient sociality in hospital architectural space: a qualitative case study in Namibia,” World Hosp Health Serv. 41, no. 2 (2005): 17-20, 40, 42.
S Heymann, “The Transvaal Memorial Hospital for Children,” S.A. Medical Journal, (13 October 1973): 1827-1833.
KD Bream, S Gennaro, U Kafulafula, E Mbweza, D Hehir, “Barriers to and facilitators for newborn resuscitation in Malawi, Africa,” J Midwifery Womens Health 50, no. 4 (July-August 2005): 329-34.
C Opondo, S Ntoburi, “Are hospitals prepared to support newborn survival?,” Tropical Medicine and International Health 14, no. 10 (October 2009): 1165-1172.
C Herrler, A Bramesfeld, “A model for improving the quality of reproductive health care in rural Kenya,” Zeitschrift für Evidenz 109, no.9-10 (January 2015): 739-747.
L Cofie, C Barrington, “Integrating community outreach into a quality improvement,” Global Public Health, no. 9 (2014): 1184-1197.
M Thwaites, “Neonatal care in the tropics,” Journal of Tropical Pediatrics 19, no. 2 (June 1973): 98-100.
56 Thomas Jefferson University - East Falls | Kamuzu Central Hospital
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
PN Swift, “The hospital care of East African children. Levels of care and lines flow. Planning a paediatric centre: the paediatricians view,”J Trop Pediatr Environ Child Health 18, no. 1 (March 1972): 82-3.
Repoussis, Panagiotis P., Dimitris C. Paraskevopoulos, Alkiviadis Vazacopoulos, and Nathaniel Hupert. 2016. Optimizing emergency preparedness and resource utilization in mass-casualty incidents. European Journal of Operational Research 255 (2): 531-44.
Branas, C. C., E. J. MacKenzie, and C. S. ReVelle. 2000. A trauma resource allocation model for ambulances and hospitals. Health Services Research 35 (2): 489-507.
Harrison, Hooi-Ling, Nigel Raghunath, and Michele Twomey. 2012. Emergency triage, assessment and treatment at a district hospital in malawi. Emergency Medicine Journal : EMJ 29 (11): 924-5.
Haac, Bryce E., Jared R. Gallaher, Charles Mabedi, Andrew J. Geyer, and Anthony G. Charles. 2017. Task shifting: The use of laypersons for acquisition of vital signs data for clinical decision making in the emergency room following traumatic injury. World Journal of Surgery 41 (12): 3066-73.
“#Envision2030: 17 Goals to Transform the World for Persons with Disabilities Enable.” United Nations. Accessed November 28, 2018. http://www.un.org/development/desa/ disabilities/envision2030.html.
Samuel, J. C., E. L. P. Campbell, A. G. Charles, and B. A. Cairns. 2010. Burn epidemiology and burn care in malawi: Outlining prevention strategies. Injury Prevention 16 (Supplement 1): A61-.
https://www.who.int/bulletin/archives/80(11)900.pdf
Harrison, Hooi-Ling, Nigel Raghunath, and Michele Twomey. 2012. Emergency triage, assessment and treatment at a district hospital in malawi. Emergency Medicine Journal : EMJ 29 (11): 924-5.
Chokotho, Linda, Wakisa Mulwafu, Kathryn H. Jacobsen, Hemant Pandit, and Chris Lavy. 2014. The burden of trauma in four rural district hospitals in malawi: A retrospective review of medical records. Injury 45 (12): 2065-70.
Lynn, Mauricio. “Hospital Planning and Response to Sudden Mass Casualty Incidents.” Mass Casualty Incidents, 2016, 25-55. doi:10.1007/978-1-4939-3496-6_3.
Sion, Melanie, MD, and Anthony Charles, MD, MPH, FACS. Central Malawi District Hospital Surgical Capacity Assessment. Report. Department of Surgery, Thomas Jefferson University Hospital.
57 Thomas Jefferson University - East Falls | Kamuzu Central Hospital
BIBLIOGRAPHY
22 23 24 25 26 27 28 29 30 31 32 33