Hearing Health Summer 2022
A Publication of Hearing Health Foundation
hhf.org
The Family Voices Issue Parents and children living well with hearing or balance conditions
h e a ri n g h e alt h fo u n dation
Catch every word, every call You don’t want to miss a single detail. Trust CapTel® for accurate word-for-word captions of everything your caller says. CapTel keeps you connected to the important people in your life, confident you’ll catch every word.
CapTel 2400i
www.CapTel.com 1-800-233-9130 FEDERAL LAW PROHIBITS ANYONE BUT REGISTERED USERS WITH HEARING LOSS FROM USING INTERNET PROTOCOL (IP) CAPTIONED TELEPHONES WITH THE CAPTIONS TURNED ON. IP Captioned Telephone Service may use a live operator. The operator generates captions of what the other party to the call says. These captions are then sent to your phone. There is a cost for each minute of captions generated, paid from a federally administered fund. No cost is passed on to the CapTel user for using the service. CapTel captioning service is intended exclusively for individuals with hearing loss. CapTel® is a registered trademark of Ultratec, Inc. The Bluetooth® word mark and logos are registered trademarks owned by Bluetooth SIG, Inc. and any use of such marks by Ultratec, Inc. is under license. (v2.6 10-19)
2
hearing health
hhf.org
The mission of Hearing Health Foundation (HHF) is to prevent and cure hearing loss and tinnitus through groundbreaking research and to promote hearing health. HHF is the largest nonprofit funder of hearing and balance research in the U.S. and a leader in driving new innovations and treatments for people with hearing loss, tinnitus, and other hearing and balance conditions. As part of our outreach, we provide this quarterly magazine for free to our vibrant community of readers and supporters, as well as to the dedicated professionals who work with them. Please subscribe at hhf.org/subscribe and make a donation at hhf.org/donate.
Summer 2022: The Family Voices Issue Hearing and balance conditions affect everyone in the family, sparking opportunities to cope successfully, together.
Timothy Higdon President and CEO Hearing Health Foundation
a publication of hearing health foundation
summer 2022
3
Hearing Health The Family Voices Issue
Summer 2022, Volume 38, Number 3
Publisher Timothy Higdon, President and CEO, HHF
Features
Editor Yishane
08 Family Voices We Believe “CI Kids” Can Do Anything. Hiroko Endo 12 Managing Hearing Loss How We Got Our Dad to Say Yes to Hearing Aids. Rohima Badri, Ph.D. 14 Living With Hearing Loss From “Bionic” Kid to Giving-Back Dad. Mark J. Miller 16 Family Voices On Monsters and Music. Cristina Duarte
Family Voices Let’s Let More 19 People Learn About Hearing Loss. Asher Bunkin 20 Managing Hearing Loss Travel Gets Easier for Telecoil Users. Stephen O. Frazier
usic Family Dynamics, 22 M Polsfuss-Style. Sue Baker
24 Media Leaning Into Tinnitus. Morenike Oyenusi 26 Media Unheard No More. Janine McGoldrick 28 L iving With Hearing Loss From Dark Days to a Bright Future. Sahar Reiazi 30 Research Recent Research by Hearing Health Foundation Scientists, Explained.
42 Managing Hearing Loss Explanations for Cochlear Implant Hesitancy—and What Hearing Care Professionals Can Do About It. Nancy M. Williams
Departments
Sponsored
06 In Memoriam 46 Meet the Researcher James W. Dias, Ph.D. Meringoff Family Foundation
44 Advertisement Tech Solutions. 45 Marketplace
Hearing Health Foundation (HHF) and Hearing Health magazine do not endorse any product or service shown as paid advertisements. While HHF makes every effort to publish accurate information, it is not responsible for the accuracy of information therein. See hhf.org/ad-policy.
Cover Takashi Endo with his oldest daughter Sakura (right) and his middle daughter An (left). Photo by Hiroko Endo.
Scan to subscribe or visit hhf.org/subscribe to receive a FREE subscription to this magazine. 4
hearing health
hhf.org
Lee
Art Director Robin Senior Editor
Kidder
Amy Gross
Staff Writers Pat
Dobbs, Shari Eberts, Stephen O. Frazier, Kathi Mestayer
Advertising GLM: 212.929.1300
hello@glmcommunications.com Editorial Committee
Judy R. Dubno, Ph.D. Christopher Geissler, Ph.D. Lisa Goodrich, Ph.D. Anil K. Lalwani, M.D. Rebecca M. Lewis, Au.D., Ph.D., CCC-A Joscelyn R.K. Martin, Au.D. Board of Directors
Chair: Col. John T. Dillard (U.S. Army, Ret.) Sophia Boccard Robert Boucai Judy R. Dubno, Ph.D. Jason Frank, J.D. Jay Grushkin, J.D. Roger M. Harris Elizabeth Keithley, Ph.D. Cary Kopczynski Sharon Kujawa, Ph.D. Anil K. Lalwani, M.D. Michael C. Nolan Paul E. Orlin Robert V. Shannon, Ph.D. Nancy Young, M.D. Hearing Health Foundation 575 Eighth Avenue #1201, New York, NY 10018 Phone: 212.257.6140 TTY: 888.435.6104 Email: info@hhf.org Web: hhf.org Hearing Health Foundation is a tax-exempt, charitable organization and is eligible to receive tax-deductible contributions under the IRS Code 501(c)(3). Federal Tax ID: 13-1882107 Hearing Health magazine (ISSN 2691-9044, print; ISSN 2691-9052, online) is published four times annually by Hearing Health Foundation. Copyright 2022, Hearing Health Foundation. All rights reserved. Articles may not be reproduced without written permission from Hearing Health Foundation. USPS/Automatable Poly To learn more or to subscribe or unsubscribe, call 212.257.6140 (TTY: 888.435.6104) or email info@hhf.org.
"When I first discovered the InnoCaption app, I was blown away by its potential to completely change my life and the lives of many other deaf and hard of hearing individuals." Joe Duarte Co-CEO and daily user of InnoCaption
Who We Are InnoCaption is owned and led by two Co-CEOs whose partnership and collaboration led to the launch of the first mobile-focused real-time call captioning service. We are a passionate, purpose-driven team on a mission to provide an empowering accessibility solution for the deaf and hard of hearing community. The InnoCaption Difference Our mission and mindset make our service unique. We focus solely on smartphone technology while our industry mainly offers landline phone solutions. We utilize live stenographers (CART) to provide faster and more accurate captioning despite the higher cost it entails. We are the only captioned phone service provider to offer users the choice between automated speech recognition technology or live assisted captioning on every call. All because we care about our users and put their needs first.
Dr. Olsen (Ringing) (Connected) Family Hearing Services, how can we help you today? You’d like to schedule an appointment with your audiologist? Sure, we can help you with that! What is your name? Thank you, Dr. Olsen can see you this Thursday at 9am. Does that work for you? Okay, great, we will see you on Thursday then! Please don’t forget to bring your ID with you and fill out the patient questionnaire online before arriving. We look forward to seeing you. Have a great day!
Hearing Healthcare Professionals Download our app and register for a demo account if you would like to test our service before recommending it to patients. If you have any questions regarding our service or require assistance, please contact us at healthcare@innocaption.com.
Disclaimer: InnoCaption is ONLY available in the United States. FEDERAL LAW PROHIBITS ANYONE BUT REGISTERED USERS WITH HEARING LOSS FROM USING INTERNET PROTOCOL (IP) CAPTIONED TELEPHONES WITH THE CAPTIONS TURNED ON. IP captioned telephone service may use a live operator. The operator generates captions of what the other party to the call says. These captions are then sent to your phone. There is a cost for each minute of captions generated, paid from a federally administered fund. No cost is passed along to the InnoCaption User for using the service. *911 Calling Advisory: Calling 911 from a landline remains the most reliable method of reaching emergency response personnel.
in memoriam
h ear i ng health foundation
In Memoriam: Bryan Pollard of Hyperacusis Research By the Board of Hyperacusis Research We, the board of Hyperacusis Research, are devastated to report that Bryan Pollard, our founder and shining star, has died at age 57. We are taking this opportunity in the pages of our partner Hearing Health Foundation’s magazine to remember Bryan and his contributions to the field of hyperacusis research. Bryan single-handedly created an entirely new diagnosis in the field of otology—pain hyperacusis—and worked tirelessly on behalf of those who suffered from it. Bryan himself had a noise injury, with symptoms appearing after exposure to a wood chipper removing a tree in his yard. Like many with this kind of noise injury, Bryan was unable to get answers from the doctors he saw. Unlike many, he took action, starting the nonprofit Hyperacusis Research in 2011 and becoming the first non-researcher to present at the Association for Research in Otolaryngology conference, prompting researchers to take seriously the condition of being unable to tolerate everyday noise levels without discomfort or pain. “Bryan was a force of nature,” says Michael Maholchic, who has assumed the presidency of Hyperacusis Research and will carry on the work with the help of the board. This includes our partnership with Hearing Health Foundation and its Emerging Research Grants program. Bryan not only created a new diagnosis, he had to reverse years of the clinical community’s misunderstanding about hyperacusis. Especially important was his influence on changing the harmful myth that quiet was bad for patients with hyperacusis, and his emphasis on the importance of avoiding setbacks, which result from additional noise exposure. He was always responsive to those who sought his counsel and advice. He was all too aware that pain—a key component of this kind of noise-induced injury—was barely mentioned. This is why he used “noise-induced pain,” modeled on the term “noise-induced hearing loss,” in order to make the concept of hyperacusis more understandable to everyone in the fields of audiology and otology. He was also aware that 6
hearing health
hhf.org
Bryan Pollard, second from right, with (from left) Betsy Maholchic, Leslie Liberman, Charlie Liberman, Ph.D., and Michael Maholchic, at a Mass Eye and Ear event in 2017. Liberman is head of an otology research lab at Harvard Med School and Mass Eye and Ear, and Michael Maholchic has assumed the presidency of Hyperacusis Research.
the conventional wisdom passed around to people with hyperacusis—that there was no need to protect against noise—was harmful to many. Patients wanted substantive research into their condition, and Bryan was instrumental in making that happen. He wrote several pieces for professional journals, articles that sufferers found incredibly helpful as they faced a skeptical medical community. In his article “Unraveling the Mystery of Hyperacusis With Pain,” published in ENT & Audiology News in 2019, he noted that the pain component had previously been completely overlooked as part of hyperacusis. The mission was not just to propel a nascent field forward. Bryan had to turn it around first, and he did so with grace and patience. He emphasized the individual and heterogeneous nature of the condition, with the same noise dose having no effect on some people but causing life-
in memoriam
Bryan single-handedly created an entirely new diagnosis in the field of otology—pain hyperacusis—and worked tirelessly on behalf of those who suffered from it. He would become the most prominent patient-activist and the driving force for promoting research nationally focused on this condition. ruining injuries for others. Bryan preferred to make his points by asking questions rather than spouting information. For example, people would sometimes say they improved because they stopped wearing ear protection. In fact, they stopped wearing ear protection because they improved. “Which is the cause and which is the effect?” he often asked. His influence on the field was transformational. “Both audiologists—such as myself—and physicians share responsibility for not knowing more about hyperacusis,” says David Eddins, Ph.D., CCC-A, an audiologist and professor at the University of South Florida. “In my 40-year career, I know of no patient-activist who has influenced the academic and clinical auditory research community in pursuit of knowledge leading to treatment and resolution of his condition as did Bryan,” says Craig Formby, Ph.D., a professor emeritus at the University of Alabama. He adds, “Bryan was a truly unique man from a very humble background. Somehow, while working full-time as an engineer, he would become the most prominent patient-activist and the driving force for promoting research nationally focused on his condition, namely, pain hyperacusis.” Bryan also influenced the careers of several young researchers who are now focused on this new field. “He had the ability to think broadly about how science and medicine should be integrated to advance treatment,” says Paul Fuchs, Ph.D., a professor at Johns Hopkins University School of Medicine. “Our own basic research benefited directly from his insight and interest.” Daniel Fink, M.D., credits Bryan for influencing his decision to become a noise activist. He contacted Bryan after seeing him quoted in The New York Times. “For a non-M.D., non-researcher to somehow influence a surgical subspecialty and get its members to do research on a condition, one which he unfortunately suffered from, is truly remarkable,” says Fink, who developed tinnitus and mild hyperacusis after exposure to loud music at a
restaurant on New Year’s Eve. “Most of the time it takes thousands of people with a condition or symptom or complaint years or even decades to get it recognized as a real medical condition,” Fink adds. “For a relatively rare condition like hyperacusis, what Bryan did was just remarkable.” An engineer and a scientist, Bryan made a huge difference in the lives of people with hyperacusis and noise injuries. His passing is such a blow to so many, personally and professionally. His insight gave hyperacusis real validity when faced with a slow-moving and conservative medical community that had been relying on outdated and scientifically unfounded information, and that was as a result unaware of the true nature of the condition. To honor Bryan’s memory, we urge people to donate their ears to science by signing up for the temporal bone registry at Mass Eye and Ear, so that scientists can further their knowledge of hearing disorders. And, of course, we always welcome donations to continue our research and to spread the word about the reality of hyperacusis. From the board of Hyperacusis Research, we are forever in Bryan’s debt. We love you, Bryan. Rest in peace and silence. HHF is very grateful to Bryan Pollard for his work bringing attention to hyperacusis, and to Hyperacusis Research for their ongoing support of our Emerging Research Grants program in the area of hyperacusis. For the National Temporal Bone, Hearing, and Balance Pathology Resource Registry, see masseyeandear.org/tbregistry. For more, see hyperacusisresearch.org and hhf.org/erg.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
7
family voices
We Believe ‘CI Kids’ Can Do Anything Two daughters with hearing loss due to Usher syndrome inspire a family in Japan to open their hearts to the world. By Hiroko Endo I am the mother of three beautiful daughters: Sakura, age 12, An, age 8, and Riri, age 4. When Sakura was born I didn’t know anything about hearing loss. But after An was born I learned a lot about hearing loss. An and Riri both have profound hearing loss due to Usher syndrome type 1 that means they will also begin to develop vision difficulties around the age of 10. They say that necessity is the mother of innovation and that is very true in my case. After our daughters were diagnosed, I found myself feeling helpless and desperate to find solutions for them. I didn’t have a moment of peace because I was stressed all the time. Seeing my distress, my husband Takashi gave me some words of wisdom, 8
hearing health
hhf.org
family voices
Hiroko Endo with her husband Takashi and their daughters (from left) An, Riri, and Sakura. Opposite page: The family lives in Osaka, Japan, and traveled to Australia to learn auditory verbal language skills.
saying, “It’s not right for you to base your happiness on our daughters’ health situation. It’s debilitating.” So the question became: What can we do with what we have? We decided to use our special circumstances as a stepping stone, and that our goal would be to raise our daughters as global people of the future. To figure out how to give our children the best chance for success, I wrote many emails and letters. I made countless phone calls. I visited institutions and centers around Japan to meet with teachers and doctors who know how to best educate children with hearing loss. Finally I met a university professor in Japan who was very helpful. He told me about an innovative way of thinking and educating kids who wear cochlear implants in Australia. I did not know what a cochlear implant was. Now when people in Japan ask me, “What is the meaning of CI?,” I can explain how it stands for cochlear implant, a device implanted into the cochlea, or inner ear, to help children as young as age 6 months hear sounds and acquire speech.
Inspired by the Possibilities
We traveled to Australia as a family, where we learned so much and met so many wonderful people. Our daughters were enrolled in auditory verbal therapy sessions. Their teacher was so inspiring. She believed not only in the abilities of “CI kids” but also in the possibilities they will have in the future. She was such a strong teacher determined to bring out the best abilities of children with hearing loss. I learned that 90 percent of children with hearing loss in Australia attend mainstream schools, thanks to speech and language therapy. I spoke to so many parents who had developed their children’s speech successfully. I then realized that these children are not disabled. The handicaps are not the hearing loss or cochlear implants but rather the low awareness of the parents and caregivers around them about their chances for success.
People in Japan often ask me, “What is the meaning of CI?” And I explain how it stands for cochlear implant, a device implanted into the cochlea, or inner ear, to help children as young as age 6 months hear sounds and acquire speech.
a publication of hearing health foundation
summer 2022
9
family voices
h e aring health foundation
Opposite page: An (near right) wears cochlear implants, as does her younger sister Riri.
To figure out how to give our children the best chance for success, I wrote many emails and letters. I made countless phone calls. I visited institutions and centers around Japan to meet with teachers and doctors who know how to best educate children with hearing loss. Finally I met a university professor in Japan who was very helpful. He told me about an innovative way of thinking for kids who wear cochlear implants and their education system in Australia. Children with hearing loss are a minority in every country, and those who wear CIs are even more of a minority. So it’s understandable that parents worry about their CI kids fitting in and being able to adapt and succeed in school. I realized adversity is an opportunity and with this in mind, I launched Anfini. It is an online school that teaches English to children around the world who wear cochlear implants. It is the first international school of its kind. I believe strongly that CI kids are the key to opening doors for themselves and others in the future. As the saying goes, “The best way to predict the future is to invent it.” These students provide hope and inspiration for future generations. They do not “need to be saved” but rather will be the ones helping others, becoming future leaders in a diverse, international society. We have 18 countries represented already! Our current curriculum includes teaching English to students, teaching auditory verbal techniques to parents, and training parents to be coaches. We provide training through videos and written text, even games, and in English and Japanese. In parts of the world, cochlear implantation is a fairly new technology so many parents are not familiar with auditory verbal techniques to enhance learning outcomes. We are taking a parent-coach approach in hopes that parents can teach English and the child’s native language in countries where CI kids do not have access to government-subsidized rehabilitation programs. We have so far conducted trial courses for several sets of Japanese 10
hearing health
hhf.org
parents and received positive feedback about the group activities, the group counseling sessions, and the parentchild English lessons. We’ve also already had many opportunities to meet with other countries through a virtual summer school, international online Meetups, and an online summit. For our inaugural summer program in 2021, CI kids from 15 countries participated. We shared two interviews, one with a ballerina from South Africa and another with a pianist from the Philippines. Both cochlear implant wearers, they talked about their challenges and how they overcame them. I think these inspirational interviews were especially beneficial for the parents because they are positive role models for their CI kids. This January during a global Meetup, representative CI kids from each country introduced themselves in English. We also shared information about the different types of government support and rehabilitation, and the common challenges that we face.
Friends Forever
I would like to introduce a member of Anfini who has quickly become my best friend. Sometimes I think it was a miracle that we met each other. Sahar and I both gave birth to children with hearing loss in our respective countries. I am Japanese and Sahar is an IranianAustralian who was then living in Iran. We both decided that our children needed cochlear
implants. We both chose a center in Australia called Royal Institute for Deaf and Blind Children (now known as Nextsense) to get speech therapy for our children. The center has over 20 branches in Australia and our children happened to have the same teacher. But that’s not even how we met! Sahar moved back to Iran and I moved back to Japan. Sahar wrote and illustrated a children’s book called “My Cochlear Implants” and sent it out to parents of children with cochlear implants she found on Instagram. She would ask parents if they were willing to translate her book so more children with hearing loss could benefit from her book. She reached out to me and I gladly translated her book to Japanese and that’s how we became friends. As we started to exchange more information about each other we realized that we had so many things in common. We are now best friends, and we work together at Anfini and share the same goals and ideas. Children with hearing loss are a minority in every country, and CI kids are even more of a minority. So it’s understandable that parents would worry about their CI kids fitting in, adapting, and learning in their communities. There are also other issues to think about such as making friends, being bullied, and education. We want these families to expand their horizons from their home country to the world. We want CI kids to become a global community and create lasting friendships like Sahar and I did.
Talking With the World
At first I thought I would have to learn English to make friends in other countries—but I was wrong. The way I see it now, I try harder to learn English once I have made friends outside of my country and am eager to build friendships with them. I haven’t started to teach English to my daughters just yet, but Riri clearly said “watermelon” when a CI kid from Senegal said the word while showing her the fruit. She spoke something in English for the first time!
Hiroko Endo lives in Osaka, Japan. For more, see anfini-global.com or find Anfini on Instagram @anfini_global.
Share your story: Tell us your family’s hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
11
managing hearing loss
hearing health foundat i o n
Opposite page: Take a cue from Aristotle (shown in this statue in Germany) and appeal to your reluctant loved one’s ethical, logical, and emotional senses in order to encourage them to try hearing aids.
How We Got Our Dad to Say Yes to Hearing Aids… …With some help from Aristotle. By Rohima Badri, Ph.D. My dad, without a doubt, is the most challenging hearing aid patient I’ve ever had! And he jokingly says that it was his payback for all my childhood mischief. This is the story of how my family used Aristotle’s three appeals—ethos, logos, and pathos—to encourage my dad to take action on his hearing loss—that is, to try hearing aids! To be honest, we had no idea that our method had its roots in the ancient form of persuasion at the time, but what’s important is that it worked. Hearing loss affects and challenges everyone in the family, not just the person who suffers from it. And one thing we quickly realized was that convincing your loved one to seek help is a marathon that requires a lot of patience, resilience, and empathy. Some of the early signs of hearing loss we noticed in Dad were asking us to speak up, turning up the TV volume, and saying “what?” a lot. Any subtle references to his hearing ability were frequently met with Dad firmly declaring that everything is fine and that the entire world has begun to mumble and speak in fashionably low voices. Often, denial of hearing loss is the first and toughest barrier for the family to crack in the process of getting help for their loved one. If they can accept they have a hearing loss and get a hearing test, that is half the battle won! This is where Aristotle’s three appeals—ethos, logos, and pathos—helped us get our dad into an audiologist’s office. Ethos (appeal to someone’s ethical sense): Establish your credibility by standing by your family member with a hearing loss and gaining their trust. Even though I have a doctorate in hearing sciences and training and experience as an audiologist, I still had to work to earn my dad’s trust that I would be empathetic, supportive, dependable, and 12
hearing health
hhf.org
honest throughout the process. Our family wanted our dad to take action on his hearing loss, but it was important for him to know that when we suggested hearing tests and, eventually, hearing aids, we were keeping his interests, challenges, and needs in mind. As a result, even before we began educating him about hearing loss, we first listened to his stories and challenges, empathized with him, and understood his reluctance without passing judgment. Logos (appeal to their logical senses): Establish your knowledge on the subject and use logical reasoning and sound ideas to educate your family member with a hearing loss. I researched studies and curated articles that would resonate with him. I presented statistics, expert opinions, and testimonials, as well as video clips, illustrating how untreated hearing loss affects overall quality of life. Also, I highlighted the far-reaching effects of untreated hearing loss—isolation, depression, and a decline in cognitive abilities—and the importance of timely intervention. Most importantly, we made sure not to exaggerate or overwhelm but instead let the facts speak for themselves. We gave him time and space to understand and process the information. Pathos (appeal to their emotional sense): Pathos, which means emotion in Latin, is the quickest and most powerful appeal you can make to your loved ones. Connect with your loved one’s emotions without jeopardizing the trust and credibility you’ve built. In other words, we needed to convey the facts to my dad in a way that resonated with him without alarming him as well. Remember, he needed to say yes for himself, not for us, so he wouldn’t become resentful of the entire process.
managing hearing loss
ETHOS Ethics/Credibility Trustworthiness or authority Tone/style
illustration credit: kpu press books, photo credit: flickr/maha-online
PATHOS Emotion Emotional impact Personal connection
We explained the risks of missing important information—sirens, fire alarms, or a cry for help from Mom. We discussed how his hearing loss affected not only him but his entire family. In a caring and non-accusatory manner, we pointed out how his enjoyable conversations and contributions to family time were dwindling, as well as how his tendency to be loud about everything made family gatherings and conversations challenging. He was surprised to learn how much his hearing loss had affected his family members. Last but not least, we explained how his grandchildren were unable to carry on conversations with him and how they were missing out on opportunities to get to know their fun grandpa and build a beautiful relationship. (I believe this one really hit home.)
Taking the Next Steps
“Bah, what’s there to lose?” my dad said loudly a few days later. “Let’s get started on that hearing test you’ve been talking about!” he said in his usual semi-gruff voice. But something changed when he was left standing with a piece of paper that read, “Bilateral mild to severe steeply sloping high-frequency sensorineural hearing loss.” He now had tangible proof that not all is well with his hearing. That, I believe, helped to put things in perspective. Now he was the one who had a lot of questions: “What does it mean? Can it be corrected? Do I have to wear hearing aids now?” We told him to take a deep breath and that he didn’t have to make any decisions just yet, at least not until the next step, the hearing aid evaluation. I explained to him that the hearing aid evaluation allows him to experience what it’s like to wear a hearing aid, ask questions, and
LOGOS Logic/Reason Facts and statistics Scientific evidence
discuss the best course of action. At the hearing aid evaluation, my dad purchased a pair the same day! We were overjoyed as a family. However, buying hearing aids is one thing, making a habit of wearing them consistently is quite another. This is another adventure worthy of its own chapter. My dad now recalls how patient, empathic, and honest his family was throughout the process, even though we’d been waiting for him to say yes to hearing aids from day one. So, if you are wondering about how to encourage your loved ones to take action on their hearing loss, take a cue from Aristotle and appeal to their ethical, logical, and emotional senses with honesty, empathy, and patience. Don’t just convince; connect and converse as well.
Rohima Badri, Ph.D., lives in New Jersey. She is a hearing healthcare adviser for HHF’s Keep Listening prevention campaign. For more, see hhf.org/keeplistening.
Share your story: Have you helped convince a loved one to treat their hearing loss? Tell us at editor@hhf.org.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
13
living with hearing loss
hearing health foundati o n
From ‘Bionic’ Kid to Giving-Back Dad A “hearing teacher” who grew up with a hearing loss helps deaf and hard of hearing students navigate school and life. By Mark J. Miller TV’s “The Six Million Dollar Man” was a bit of a savior to me back when I was a kid in the ’70s. The show followed a former astronaut who, after an errant test flight, gets rebuilt with “bionics” that make him extra strong and extra fast. He, of course, becomes a secret agent, and viewers often got to see the electronics embedded in his skin. Meanwhile, I was walking around with a massive Zenith hearing aid under my shirt and a wire popping out of my collar and up to my ear. It helped to be able to tell other kids I was like the Bionic Man. I’d pretend to be able to hear conversations two rooms over through my before-its-time wearable tech. The ruse only worked for so long, but at least we got a few laughs out of it. I was born with a bilateral, mild-to-profound sensorineural loss due to BOR Syndrome, a rare syndrome that can affect your hearing and kidneys; my audiogram looks like a double-black-diamond ski slope. For some unknown reason, I only wore one hearing aid for most of my childhood, but eventually graduated to two behindthe-ear aids and then in-the-canal outfits once I graduated from college and had a little dough (stress on “little”). One of my sisters is also hard of hearing, but we didn’t compare notes too often about our predicament. Other than her, I had never met anyone else who was hard of hearing until my senior year of high school when a girl noticed my hearing aid and told me she had one, too. I was 14
hearing health
hhf.org
completely stunned into silence, not knowing what to say. I still feel bad about it. As an adult, I spent 25 years in the world of magazine and website publishing and absolutely loved it, but a strange thing happened. A good friend who is a teacher kept encouraging me to become a teacher, too, after seeing how much I enjoyed coaching the soccer team our young daughters played on together. While I liked the idea, I also didn’t want to take on a classroom, where it would be hard to hear students in the back. Truth be told, I didn’t want to deal with actually managing the emotional roller coaster of 30 kids, either. Plus, I loved what I did. Every day as a writer was a new adventure with new stories to tell. Then I got a phone call from my pal. “A woman came into my classroom today who is something called a hearing teacher. Have you heard of such a thing?” Well, no, I hadn’t. And so we talked about what hearing teachers do, which is meeting with deaf and hard of hearing (DHH) students and helping them with any social, emotional, academic, and straight-up technical issues related to their hearing. As hearing teachers, we are advocates for our students, teaching instructors, administrators, and even parents how to work with each child’s hearing loss. Then we teach the students to advocate for themselves. The potential impact
living with hearing loss
Opposite page: Coaching his daughter’s soccer team led Mark Miller to recognize how much he enjoys teaching. He became a hearing teacher for students with hearing loss, an adult advocate he wishes he had as a kid growing up (far left).
One of my favorite moments when I meet a new student is when I take out my hearing aids and show them that we have something in common; oftentimes I’m the first fellow hard of hearing person they’ve ever met. I never had a hearing teacher, but I wish I’d had someone who could have helped guide me through the social pitfalls and taught me how to be a better self-advocate. we can have when working one-to-one or in small groups attracted me. It sounded interesting, and also appealed as a way I could give back. One of my favorite moments when I meet a new student is when I take out my hearing aids and show them that we have something in common; oftentimes I’m the first fellow hard of hearing person they’ve ever met. I never had a hearing teacher, but I wish I’d had someone who could have helped guide me through the social pitfalls and taught me how to be a better self-advocate. Instead, I just nodded and smiled before figuring out on my own that there was a better way to go through life. I loved journalism, but I love being a hearing teacher, too. Like my past life, each day brings new characters, new adventures, and new stories. It is an honor to try and help these kids try to figure out where they fit in and how to be sure they can hear to the best of their abilities. Perhaps my work now is a way to make up for leaving my classmate with a hearing loss hanging all those years ago. So now I get to hear the stresses of today’s young kids with hearing loss and relate them back to my own concerns. The world of hearing devices has obviously changed with digital, Bluetooth, and even accessories for hearing aids that make them look like tiny basketballs. When I found myself in the hearing-teacher world, I realized I was reading a ton of hearing-related articles that were extremely helpful, whether it was to show students examples of the cool jobs done by hard of hearing adults, keep up on the tech and political changes happening in the DHH world, or discover all the different forms advocacy could take. I figured my colleagues could use this
same info so I created a little in-house newsletter, which evolved into the Hear Ye website. It’s pretty rudimentary, but the basic idea is to provide a central point for news about hearing issues so people can find it in one place. I try to update it a few times during the course of the week. Some weeks I’m more successful with that than others. While the audience is very specialized, it feels good to know that I’m helping someone out there find the information. Being hard of hearing has certainly shaped who I am. One of the most important lessons I share with my students is discerning the difference between hearing and listening. In the end, we discover that just because we don’t have great hearing doesn’t mean we can’t be great listeners. Most people, hearing or not, aren’t good listeners, but I believe it’s crucial that we all work on this dying art (even if we can’t exactly make out what’s being said two rooms away).
Mark J. Miller is a teacher in the New York City school system. For more, see sites.google.com/view/hear-ye.
Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
15
family voices
Cristina Duarte with her husband and parents.
On Monsters and Music My life as a real-life “CODA,” child of deaf adults, was both like and unlike that portrayed in this year’s winner of the Academy Award for Best Picture. By Cristina Duarte I cannot tell you how many times in my 32 years people have asked me, “What is it like to have parents who are deaf?” My answer has always been the same, regardless of who is asking or how old I am: “What is it like to have hearing parents?” My parents were both born with profound hearing loss to hearing families. Since they were born into hearing families, they were not raised signing—in fact they both only learned to sign in their 20s when they joined (and met through) Self Help for the Hard of Hearing (SHHH) which has since become the Hearing Loss Association of America (HLAA). As a result of their experiences and upbringing, my parents are both strong lip readers (speech readers), communicate orally, and sign in exact English (SEE)— even my dad, who grew up in Portugal. My mom tells us that neither I nor my siblings really went through the “terrible twos” because we could sign before we could speak, and because of this, we were able to communicate our needs from a young age. 16
hearing health
hhf.org
From what I hear, I was a pretty good signer up until the time I went to kindergarten and saw that none of the other kids signed. Apparently, I came home and confidently informed my parents I would not be signing anymore (what a terrible kid, I know!). Today, as an adult who works in the deaf and hard of hearing community, I sign again. I was beyond excited when I saw the trailer for the film “CODA” (child of deaf adults) for the first time. Even just from watching the clip, I could tell it was going to be good, and probably a little emotional. Once I finally got to watch it, it did not disappoint. I thought the entire cast did a wonderful job, and there were so many points in the movie where I found myself reminiscing about my childhood. It was so wonderful the film won the 2022 Academy Award for Best Picture!
I Can Relate
There were many parts of the movie where I found myself smiling because I felt like I could relate. However, the primary mode of communication in my house growing up
family voices
From what I hear, I was a pretty good signer up until the time I went to kindergarten and saw that none of the other kids signed. Apparently, I came home and confidently informed my parents I would not be signing anymore (what a terrible kid, I know!). Today, as an adult who works in the deaf and hard of hearing community, I sign again. was spoken English. We had communication rules in the house: Always be facing Mom and Dad when speaking to them; don’t cover your mouth while talking; enunciate your words and speak clearly, among other things. I remember my dad used to get frustrated with me all the time because as a teenager I would speak “like a machine gun on fire.” I would get constant reminders that I needed to speak up and slow down. In contrast, in “CODA,” Ruby’s family relies on American Sign Language, which is a very different experience. In my house growing up, my parents had flashers— we called the assistive device a “baby crier.” When the phone rang or the doorbell went off, one of us started screaming, and the lights would flash. My parents used this technology at night to wake them up when a baby was crying. When I was about 6, I went through a phase where I would wake up in the middle of the night and want to go to sleep with my parents. I am sure a lot of kids go through that, but I was also scared of getting out of bed because the “monsters” could get me, and I needed my dad to come get me. Every night—for probably too long—I would wake up and just scream in my bed to cause the lights in my parents’ room to start flashing. Like clockwork, I would see my dad come out of his room and go to the nursery to check on my baby brother. Once my dad realized it was not the baby crying, he would come to my room and see me gesturing to be picked up and carried back to my parents’ room. One night, and I remember it like it was yesterday, I started screaming per usual and watched my dad go to the baby’s room. However, this time when he came out, instead of picking me up, he looked at me, unplugged the baby crier, and went back to his room. To say I was distraught is an understatement. In hindsight I laugh because I could have easily gotten
out of bed and walked myself to their room, but I didn’t. And ultimately it worked—I didn’t wake them up anymore and slept through the night. At the time, I couldn’t believe my father would leave me to the monsters, but that is my most vivid memory associated with being a CODA. My parents always encouraged us to pursue music. My dad, like the dad in the movie, loved music with heavy bass. Now, he didn’t listen to rap, but there was a lot of classic rock and especially in the car, it was always very loud. My mom would get mad at him all the time because we would borrow his car, turn it on, and immediately jump out of our seats because he’d left the music all the way up where he could feel it. I would always laugh, and I loved riding with my dad with the music blasting and windows down. I was obsessed with “The Sound of Music” when I was a kid; I can’t even count the number of times we watched it as a family, and my parents would put it on the loudspeaker as my siblings and I danced around singing. We have multiple home videos of us belting the songs in at home “performances.” I remember when we were singing for our dad back when he had hearing aids, he would place his hand lightly on the side of our throats to feel the vibrations of us singing—also like the father in the movie. I was actually surprised when I saw the father in the movie do that because I had thought it was just something my dad did!
Communication Help
I attribute my communication skills and empathy to my experiences growing up. I think observing my parents’ struggles with lack of accessibility—and specifically seeing so many hearing individuals make it clear that communication with my parents was burdensome—shaped me into the person I am today. I watched my parents gracefully advocate not only for themselves but for others, and I feel like I followed their example. a publication of hearing health foundation
summer 2022
17
family voices
h e aring health foundation
Cristina’s parents, Meg and Joe, in August 1984. They met in 1982 and started dating in July 1983.
The lack of accessibility portrayed in the movie was very real and hit close to home even though my parents’ accessibility needs weren’t the same. While there were many things I noticed, the primary one was the issues with telecommunications accessibility. For as long as I can remember, I would answer the landline phone in the family home. I had everything very well-rehearsed: “Duarte residence, Cristina speaking. How can I help you?” I loved getting to answer the phone and relaying the messages for my parents. Some other CODAs have shared with me that they always felt burdened by the responsibility, but I can’t relate to that because it is something I always enjoyed. I would either take messages down for my parents or listen on the phone and mouth to them what the caller was saying. This was back before captioned telephones and other relay services were available. As I got older, telecommunications relay services started becoming available, but due to delays with the technologies I got to keep my job as the answerer of the phones! When I was at school and had to call my parents from the nurse’s office—which admittedly was frequently because I loved staying home from school—it was a struggle to communicate what was going on. Luckily, I was such a frequent visitor of the nurse’s office that she developed a “yes/no” system with my mom. My mom would ask questions and the school nurse would answer yes or no very clearly. This resulted in me being sent back to class probably 75 percent of the time. When my parents got the InnoCaption app on their cellphones it was the first time I was ever able to reach my parents like my hearing peers. It was incredibly special and to this day I don’t take having that ability to connect 18
hearing health
hhf.org
with them for granted. The InnoCaption technology and the doors it opened for my parents is actually why I specialized in communications law—specifically telecommunication relay services. I can tell you I love my family and how close we are. I know a lot of people say this, but I feel like I have the best parents in the world and I am incredibly grateful to have been born to them. I love being able to sign and where my connection to the community has led me in life. I am grateful for the values my parents instilled in me, which were probably largely due to their experiences growing up hard of hearing. Occasionally I get asked whether I would have preferred to have hearing parents—and while I can say I have no idea what that would have been like, I can also honestly say that I am happy with my family and have never wished that it was different.
Cristina Duarte is the senior director of regulatory affairs at InnoCaption, a mobile app that provides call captioning for the deaf and hard of hearing, where she works with her father. InnoCaption is a promotional partner for Keep Listening, HHF’s hearing loss prevention campaign. “CODA” is available to stream on Apple TV+.
Share your story: Are you a CODA? Tell us at editor@hhf.org.
Support our research: hhf.org/donate.
family voices Wearing hearing aids gives Asher Bunkin, shown at near left with his family, an opportunity to teach others about hearing loss.
Let’s Let More People Learn About Hearing Loss By Asher Bunkin My name is Asher and I will start middle school in the fall. I have bilateral, mild-moderate sensorineural hearing loss. When I was around 4 ½ years old I had an ear infection and had a lot of trouble hearing. My mom took me to an ENT (ear, nose, and throat) doctor who treated the ear infection and suggested seeing an audiologist to test my hearing. The audiologist confirmed I had an underlying hearing loss, and then I got my first pair of hearing aids. Even though we have some family history of hearing loss, no one realized I had hearing loss before that ear infection.
It’s important that you don’t let people bring you down for wearing hearing aids. Take the opportunity to explain about hearing loss and using hearing aids. Let them know more about it! After I was diagnosed, I was fitted with hearing aids. They help me hear. If I miss things during conversations, I sometimes change the topic so I can continue to participate in a group discussion. I need to focus on the big picture of a conversation to make sense of what is going on in case I miss words here and there. I also try to read lips and stay close to the person who is speaking. I have trouble hearing people when they are whispering or if I am too far away from the person speaking. I rely on friends to help me if I need something repeated. When
people are talking quickly or wearing masks it is not easy to hear. For example, when I am swimming I can’t wear my hearing aids and as a result cannot hear what is going on around me. Sometimes I run into trouble if my hearing aids shut off during the day—when the rechargeable batteries die. Otherwise, my hearing loss doesn’t stop me from doing anything at all. I would tell someone with a new diagnosis to persevere, know that you can get used to it, and think about the positives and not the negatives. It’s important that you don’t let people bring you down for wearing hearing aids. Take the opportunity to explain about hearing loss and using hearing aids. Let them know more about it! I heard about Hearing Health Foundation from my mother because I was in school with the younger daughter of HHF’s former CEO, Nadine Dehgan. Now my mother works for SoundPrint, the decibel measuring app, which is how we reconnected with HHF. Our family thinks it is important to educate as many people as possible about the research HHF does for hearing health and encourage them to protect their hearing.
Asher Bunkin lives in New York City with his family, including mom Sharon Bunkin, the director of marketing at SoundPrint. SoundPrint is a promotional partner for Keep Listening, HHF’s hearing loss prevention campaign. For more, see hhf.org/keeplistening/partners. Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
19
managing hearing loss
hearing health foundat i o n
Travel Gets Easier for Telecoil Users In the past couple of years there’s been an explosion of what could be industry-altering hearing loop news in the field of transportation, ready to go for us for when we’re all fully back on the road. By Stephen O. Frazier Hearing loops have been available in the U.K. for years, in airports, train stations, the Underground, and even London taxicabs. They’re now becoming more plentiful in transportation systems here in the U.S. Recent announcements of new hearing loop installations and major plans for their future use in the field of transportation have pushed this time-tested technology to the forefront in efforts to accommodate the special needs of travelers with hearing loss. A hearing loop is a wire that surrounds a defined area and is connected to an electronic sound source such as a public address system. It emits a silent electromagnetic signal that carries the sound from its electronic source to receivers called telecoils (T-coils) in hearing aids or cochlear implant (CI) processors. The majority of hearing aid models currently on the market have (or can be fitted with) telecoils. CI processors also generally come fitted with telecoils, varying by manufacturer. My hearing aids and their telecoils are already optimized to match my audiogram and provide an extra boost to those frequencies I have the most difficulty hearing. Turning them on is simple: In a looped setting I just touch a button on my hearing aid and I’m instantly connected to the loop and its signal. Any number of telecoil users in a room can access the signal from the loop, something that is not possible with Bluetooth, which is basically a 1-to-1 system. Here are some highlights: » The list of airports offering one or more forms of hearing loop technology in their terminals in the U.S. grew from 12 to 20 in just the past year or so. Among those added to the list were the major hubs of LaGuardia Airport in New York City and Los Angeles International Airport. Memphis International is looping the departure gates in a new concourse now under construction, and, thanks to a grant from the Federal Aviation Administration, the Billings, Montana, airport will be including hearing loops in upgrades to their two terminals. In addition, the airports in Minneapolis and Phoenix, both major hubs that already offered the technology, are expanding its presence at a variety of locations within their terminals. » New York’s Metropolitan Transit Authority (MTA) is testing looped city buses. A Hearing Loss Association of America NYC chapter member who volunteered to test says, “We were able to hear announcements from both the bus driver (live) and from outside 20
hearing health
hhf.org
My hearing aids and their telecoils are already optimized to match my audiogram and provide an extra boost to those frequencies I have the most difficulty hearing. Turning them on is simple: In a looped setting I just touch a button on my hearing aid and I’m instantly connected to the loop and its signal. Any number of telecoil users in a room can access the signal from the loop, something that is not possible with Bluetooth, which is basically a 1-to-1 system.
managing hearing loss
Adventures in Looping, Near and Far Since the advent of COVID I’ve not strayed much outside of Albuquerque’s Rio Grande Valley but previously, en route to Paris via Madrid, I listened to Plácido Domingo through my personal (don’t leave home without it) neckloop instead of the offered earbuds on an Iberia Airlines flight. In Paris I used a neckloop for a self-conducted tour of the catacombs under Notre Dame. There was a counter loop at the tourist office in tiny Les Eyzies in rural France, and upon my departure I experienced the loop in a waiting area at Charles De Gaulle Airport. Across the Channel, I used my neckloop in place of the offered earphones with the receiver they provided to hear the prerecorded messages at each of the monolithic stones at Stonehenge in the English countryside. I’ve also been able to talk with agents at subway information/fare booths and at Penn Station in New York City. A theater-provided neckloop let me hear and understand the dialogue in the award-winning “Kinky Boots” musical on Broadway. I regularly attend Hearing Loss Association of America conventions and, of course, all of the meeting rooms are looped so even if I sit in the back row it’s as though I have a front row seat. And at home in Albuquerque there’s a plethora of opportunities to use my telecoils. —S.O.F.
» » »
»
»
(recorded). The sound quality varied between the two sources, but both were pretty good.” The MTA board has approved the funding for over 500 new subway cars dubbed the R262 model that will be fitted with hearing loops. The MTA has also tested the installation of a hearing loop at the busy Bowling Green subway station in lower Manhattan. In July 2021 Amtrak signed a $7.3 billion contract for 83 new train sets (expected to be six cars each) to be built by the German company Siemens in their California plant. They will be fitted with hearing loops and used on the line’s heavily traveled Northeast Corridor routes. The Port Authority of New York and New Jersey announced a set of new accessibility requirements for all transportation terminals it operates. The requirements mandate the inclusion of hearing loops at departure gates and information booths at all new or significantly upgraded airports and at the information counters at rail, bus, and ferry terminals as well. Also recently San Francisco’s Bay Area Rapid Transit System (BART) took delivery of a fleet of hearing loop– equipped rail cars and completed the installation of hearing loops at all 50 of the system’s stations.
Prior to these recent developments, hearing loops had already found their way into other travel-related facilities such as New York’s Penn and Grand Central stations, the Intermodal station in Milwaukee that serves short and long distance train and bus passengers, and even New
York City taxicabs. The Rail Vehicles Access Advisory Committee had made a recommendation to the U.S. Access Board to encourage the appropriate federal agency to require that all future rail cars be equipped with hearing loops. All of this points to a future where travel will be just a little bit easier for people who have the little copper telecoils in their hearing aids or cochlear implant processor.
Trained by the Hearing Loss Association of America as a hearing loss support specialist, staff writer and New Mexico resident Stephen O. Frazier has served HLAA and others at the local, state, and national levels as a volunteer in their efforts to improve communication access for people with hearing loss. Contact him at hlaanm@juno.com. For more, see sofnabq.com and loopnm.com. For references, see hhf.org/summer2022-references.
Share your story: Tell us where you use hearing loops at editor@hhf.org.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
21
Family Dynamics, Polsfuss-Style Each in their own way, Les Paul’s parents nurtured their son to change the music industry. By Sue Baker
Above, from left: George and Evelyn Polsfuss, Les Paul’s parents. Lester Polsfuss, who became Les Paul, with his mom Evelyn, circa 1924. Les and Evelyn. Les and his brother Ralph. Opposite page, top: Les and Evelyn at her 100th birthday party.
22
hearing health
Lester Polsfuss—later known as Les Paul—was the second child of George and Evelyn Polsfuss. They divorced when Les was quite young but they each, in their own ways, helped Les. In his memoir “Les Paul in His Own Words,” Les wrote that his father was “a good man, a great rascal and storyteller.” One could say that also describes Les. George gave Les the nickname “Red” because of his red hair. Les relayed how his father would bring home an assortment of strange gambling winnings. “He was something else, a real trip,” Les wrote. In the 1920s, when teenage Les wanted to build a cutting lathe to record his music, he went to his dad’s auto dealership where George’s mechanic helped Les build his first lathe. After George and Evelyn divorced, Les said his father settled down. It was George, along with Ralph, who invited Les and Mary Ford to perform at the opening of their jointly owned Club 400. Les said Ralph was handsome and outgoing, and the brothers were fond of each other, hhf.org
despite the age difference and their very different personalities. Evelyn Stutz Polsfuss loved both of her sons. Even when Les was a preschooler, she recognized his talent. She would arrange for her young son to perform for local fraternal organizations. Les was so tiny that they placed him on top of a table where he would sing, dance, and tell funny stories. “I did a lot of crazy, stupid things when I was a kid,” Les wrote in his book. “But rather than scold me, she always took pride in the fact that I was thinking creatively and had the initiative to do something.” While Les was still young, his mom gave him his first stage name, Red Hot Red. Les shared, “She always said, don’t look at the negative, look at the positive, and you can do it. And she shoved me out on stage the same way. ‘Go out and get ’em, Lester. Go out and get ’em.’” Les’s ferocious curiosity meant Evelyn was always answering questions. When she did not know an answer, she would take Les to
music
“I did a lot of crazy, stupid things when I was a kid,” Les wrote in his book. “But rather than scold me, [Mom] always took pride in the fact that I was thinking creatively and had the initiative to do something.” While Les was still young, his mom gave him his first stage name, Red Hot Red. Les shared, “She always said, don’t look at the negative, look at the positive, and you can do it. And she shoved me out on stage the same way. ‘Go out and get ’em, Lester. Go out and get ’em.’ ”
the library or to a local teacher. She was determined to help her son be his best. When Les’s favorite musicians came to town, Evelyn found ways to get her son to see the performances. She even took Les to Nashville to see country and blues star DeFord Bailey. When 13-year-old Les wanted to amplify his voice while performing, Evelyn allowed him to use her telephone and radio. Around the same time, Evelyn arranged for Les to perform on a Milwaukee radio station—and from there he never stopped. Even when Les was an adult, Evelyn continually encouraged him to stretch to his full potential. When he was playing his electric guitar professionally, she urged him to sound different from other guitar players. That impetus drove Les to spend two years building his multifaceted sound and a new, solid-body guitar that set the music world upside down. “She was the biggest single influence of my life,” Les said about his mom, “and we were close in a way that never diminished till the day she died at the age of 101 and a half.”
Sue Baker is the program director at the Les Paul Foundation. We are grateful to the Les Paul Foundation for its ongoing support of tinnitus research through HHF’s Emerging Research Grants program.
Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
23
media
h e ar i n g h e alth foundation
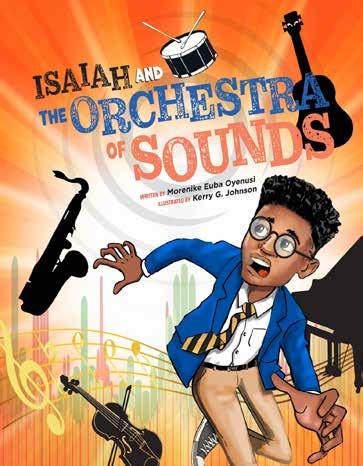
Morenike Euba Oyenusi wanted to create an approachable way to educate young people about tinnitus and how tinnitus can be caused by exposure to loud sounds.
Leaning Into Tinnitus What if the cacophony of tinnitus sounded like an orchestra? By Morenike Euba Oyenusi
My struggle with tinnitus started on Monday, November 25, 2019. I remember that day distinctly because it was my daughter Oyinade’s 19th birthday. I had begun to experience extreme dizziness the day before, so much so that I could not walk initially, and by Monday morning, the dizziness was accompanied by horrible nausea and stomach pain. I urgently implored Tunji, my late husband, to drive me to the nearest emergency room, where I was diagnosed with vertigo. Later that day, the tinnitus symptoms started, and they have been continuous since then. Two weeks later—by which time the other symptoms had thankfully disappeared—I was diagnosed with a partial hearing loss and tinnitus. The tinnitus was a traumatic ordeal for me. I found myself just writing down my thoughts to cope with the terror. This evolved into a poem, which continued to get longer and longer. I became decidedly fascinated by the sounds in my ear—each individual and distinguishable, but with all the 24
hearing health
hhf.org
noises working together to make a complex, incredible sound, just like instruments in an orchestra. There is no other way to describe it. That began the notion of writing about tinnitus as an orchestral performance. My first thought was to have my epistle published as a poem in a literary journal. I sent it to an academic journal, but I had no response. The rejection (or failure to reply) was a marvelous blessing because, several months later, God gave me the idea of turning the poem into a short graphic novel for preteens, teenagers, and young adults. The idea was to create an approachable way to educate these age groups about tinnitus and how tinnitus can be caused by loud noise and hearing loss. (The doctors speculate that, in my case, infection rather than loud noise was more likely the cause of tinnitus and hearing loss.) I was captivated by this vision and looked for an illustrator to help me implement it while working on turning the very long poem into a story. The result is “Isaiah and the Orchestra of Sounds,” with illustrations by Kerry G. Johnson. Our hero, 15-year-old Isaiah, starts
media
I became decidedly fascinated by the sounds in my ear—each individual and distinguishable, but with all the noises working together to make a complex, incredible sound, just like instruments in an orchestra. There is no other way to describe it. That began the notion of writing about tinnitus as an orchestral performance.
to hear terrifying and strange noises in his right ear on a normal, regular day in Baltimore. The story follows his battle with tinnitus. Even though Isaiah is not dealing with musical tinnitus (and I learned only later that there is such a thing), he expresses his experience as that of an alien orchestra performing in his ear. I use the musical performance theme and musical references throughout the book, and I am quite pleased with how all that turned out. I also include resources to help people with tinnitus and advice for noise avoidance. My hope is to have the book in doctors’ offices, schools, and libraries to help teach that loud noise is a very real threat to hearing health and well-being. This is an acute concern given the prevalence of headphone use and loud concerts, and how little cognizance there is of the dangers. The irony is that music is beautiful and pleasant to listen to, but if you listen to it too loudly, you can experience a ghastly orchestra, as Isaiah does, and one that may never stop playing.
Morenike Euba Oyenusi is a NigerianAmerican lawyer, author, and minister who lives in Maryland. Her first book, “Chasing Butterflies in the Sunlight,” was a finalist in the 2021 Next Generation Indie Books Awards. For more, see paradiserestoredpublishing.com.
Share your story: How do you cope with tinnitus? Tell us at editor@hhf.org.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
25
media
h e ar i n g h e alth foundation
Unheard No More An entertainment executive’s search for support sparks the idea to capture Ménière’s disease in a documentary. By Janine McGoldrick It has been nine years since I was diagnosed with Ménière’s disease. “A disease? Am I going to die?” I asked my doctor. He explained Ménière’s wouldn’t kill me but, unfortunately, it is a chronic condition with no cure. I’d have to learn to manage the symptoms and, well, just live with it. Easier said than done. Ménière’s symptoms can include horrible bouts of vertigo and nausea, drastic hearing loss, roaring tinnitus (ringing in the ear), painful ear pressure, extreme fatigue, and severe imbalance—just to name a few. Ménière’s is an “invisible” illness, not widely known and difficult to explain. Google and WebMD became my best friends but are no substitutes for personal empathy and understanding—two things desperately needed by people with an enduring health condition. Unfortunately, hearing a list of symptoms can’t give someone a full picture of what Ménière’s does to you. I have spent nearly a decade struggling to describe my condition to my family, friends, employers, and even strangers on the subway who think I’m drunk because I have difficulty walking straight. Now, I admit I love me some Guinness, but when I explain, “It’s not the alcohol, it’s the Ménière’s,” I’m met with blank stares. Complicating things further is the fact that a Ménière’s “attack” can happen anywhere, at any time, with little warning. One moment you’re fine, working at your desk or 26
hearing health
hhf.org
making dinner. Then, with the flick of a switch, pressure begins to build in your head, you are thrown off balance, and everything around you starts to spin so violently you collapse and can’t move. This can last for a few minutes or a few weeks. As it all takes place inside your head, and happens while you “look healthy,” others—including doctors—are skeptical it’s even occurring, leaving you feeling anxious, depressed, and isolated. Jobs are lost, social engagements are canceled, relationships end. Hearing issues weren’t new to my family as my dad suffered severe hearing loss due to years working with airplane engines and large electrical machinery. But none of us had ever heard of Ménière’s or were prepared for the life changes that would ensue. My mother witnessed several of my Ménière’s attacks— helping me to the bed, scrambling to get my rescue meds, and cleaning up my vomit. Now she is constantly worried about the greater harm that may happen if I have an attack when I am alone or traveling. My brother Michael told me it can be difficult to know exactly how to help family members who have medical ailments, but it’s harder when they suffer from a disease as mysterious as Ménière’s. As much as my loved ones wanted to grasp how much my world has changed they couldn’t. When I found a community of Ménière’s support groups on social media, I heard similar repeated refrains: “No one realizes what I go through”; “My family doesn’t get it”; “I’m alone on this journey.” So I wanted to find a way to give my family,
media Janine McGoldrick (second from right) and her family hadn’t heard of Ménière’s disease before she was diagnosed, and none were prepared for the life changes that come with the condition.
One moment you’re fine, working at your desk or making dinner. Then, with the flick of a switch, pressure begins to build in your head, you are thrown off balance, and everything around you starts to spin so violently you collapse and can’t move. This can last for a few minutes or a few weeks. and many others, a better understanding of the monster called Ménière’s. As a veteran entertainment industry executive, I am acutely aware of the power that film and television have to enlighten, so I decided to develop “Unheard: The Ears of Ménière’s,” a documentary that will shine a light on this debilitating disease which has remained unheard of for far too long. The film will create a visceral viewing experience for audiences so they directly experience the effects of the condition. Through creative camera movements and innovative sound design, it will simulate Ménière’s symptoms so viewers not only learn but also feel. When I mentioned my film idea to my brother he was so excited. He said having visual and auditory examples of the Ménière’s experience would be an invaluable tool for people like him who need to know more about this debilitating illness. Another goal of the documentary is to elevate Ménière’s in the public consciousness and attract funding for more research to find better treatments and hopefully a cure. Research for Ménière’s disease, like many vestibular disorders, is vastly underfunded. In order for people to have a better quality of life, this needs to change. I’m grateful to Hearing Health Foundation (HHF) for supporting our film through recommending medical experts as well as patients of the condition who have shared their stories with HHF. My hope is that Ménière’s
becomes as recognizable as Parkinson’s, diabetes, and multiple sclerosis. So, the next time I need to call out sick, cancel plans, or ask for help in public after stating, “I am having a Ménière’s episode,” I am met with recognition and not incomprehension from family and strangers alike.
Janine McGoldrick is an entertainment strategist and producer. She can be reached via email at janine@2ndchapterproductions.com and on Twitter and Instagram at @2ndChapterProd. “Unheard: The Ears of Ménière’s” welcomes corporate sponsorships and other funding toward production. To learn more, see 2ndchapterproductions.com.
Share your story: Tell us your Ménière’s disease journey at editor@hhf.org.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
27
living with hearing loss
hearing health foundati o n
From Dark Days to a Bright Future Networking among mothers of cochlear implanted children around the world leads to a solution for a young girl. By Sahar Reiazi Samin lives in Iran. A family friend, Soheila (above, center), accompanied her on the day her replacement cochlear implant processor was switched on. Through a network of cochlear implant families, Samin was able to receive a processor donated from Australia that was used and older—but just like the one she lost.
28
hearing health
hhf.org
Samin was born in a small village in the province of Mashhad in northeast Iran. She is the only person in her family who has a hearing loss. Doctors suggested cochlear implants, and even though her father did not have the money they opted to get the surgery. Her father borrowed the money he needed and Samin was unilaterally implanted in Iran when she was 7 years old. Teachers in her school were impressed as Samin proved herself a fast learner and a bright child. Samin turned 9 and her speech was progressing well. One day when she was riding the bus with her parents Samin dozed off. When they got off the bus, her parents realized the cochlear implant processor wasn’t on her ear. They were devastated. They searched and searched, contacted the bus company, and even filed a statement with the police saying her cochlear implant device had been lost. But the processor was gone. For the first time in two years, Samin had to experience silence. Her family was distraught. Samin cried every day for a month, until she just went silent and communicated with her family through lipreading (speechreading). Her elder brother by two years was upset for his sister, and asked their mother why Samin wouldn’t talk anymore. “I was so distressed that I would lay down all day depressed and hopeless,” Samin’s mom says. “I couldn’t muster up the energy to get up and cook for my own children.” Samin’s mom refers to that time as “the dark days.” They were still paying installments on Samin’s last device and could not afford to buy a new one. Though they appealed to different organizations, all said that due to the long waitlist it could be years until Samin was eligible for a new device—a device the family could not afford to begin with.
living with hearing loss
They searched and searched, contacted the bus company, and even filed a statement with the police saying her cochlear implant device had been lost. But the processor was gone. For the first time in two years, Samin had to experience silence.
I heard about Samin’s story through a mutual friend. I told her I would help raise funds for Samin no matter what. Something inside me woke up, a little flame that would not be put out until I saw Samin with a new device. I started making calls and sending out emails. My mind was working nonstop to find someone I could reach out to. Every day counted, because I would wake up thinking how Samin could not hear, and how that wasn’t fair. So many emails and messages from people across the globe came in, reassuring me that they would do anything within their power to find a device for Samin. One person I contacted was my friend Hiroko in Japan. She was sympathetic because she had two daughters who wear cochlear implants and she could understand Samin’s situation well. After just 48 hours, I received a call from Hiroko. When I picked up and said hello, she said excitedly, “Hi, Sahar. A device has been found for Samin from Australia! It will be donated to her, please contact….” I was crying tears of joy; Hiroko was crying tears of joy. It was one of the best moments of my life. Australia has excellent medical care for their citizens. The country supplies the newest hearing devices and latest technologies for free as part of a government organization called Medicare. That is why people often donate their older devices. The device donated to Samin was an older model—but exactly the same as what she had before. I offered to pay for postage fees to the kind donor, but she insisted that she would pay for it herself. The device was sent out to Soheila Naderi, the friend who had introduced Samin to me. She lived close to Samin’s village and had better access to her than me. Soheila also has a son with cochlear implants. She is a dear soul who helps
and informs families of children with hearing loss on her social media page. The device arrived! Samin’s mom was informed, and Soheila took Samin and her mother to their local audiologist. The audiologist asked, “Samin, can you hear me?” and she replied “Yes.” Soheila recorded it all using her phone and sent the videos to me. We were all overcome by emotion. I still keep in touch with Samin’s mom to ask how Samin is doing. Samin is attending rehabilitation classes and mainstream school and her future looks bright. I aspire to create an organization in Iran which focuses on donating used hearing devices—such as hearing aids and cochlear implant speech processors, and spare parts such as batteries—to families who need them. Who knows, maybe we’ll call it “The Samin Foundation.” Samin is an Arabic word that means “precious,” and not only is everyone in this story precious to me, but so is being able to fully hear.
Sahar Reiazi (near left) appeared on the cover of the Spring 2021 issue, at hhf.org/magazine. Hiroko’s story is the cover story of this issue.
Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
29
research
Recent Research by Hearing Health Foundation Scientists, Explained Increasing Our Understanding of Avian Hair Cell Regeneration The hearing organ in mammals is the cochlea. In birds, it is the basilar papilla that, in sharp contrast to the cochlea, can regenerate its sensory hair cells and as a result recover from hearing loss within weeks. The mechanisms that trigger, sustain, and terminate the regenerative response in live animals (in vivo) are largely unknown. Prior research has shown that the mobilization of immune cells or activation of immune genes is essential for aspects of regeneration promoting cell proliferation and wound healing. But while both the avian basilar papilla and the mammalian cochlea invoke an immune response after hair cell damage, one happens in the context of regeneration and the other does not. For this study, we set out to build on our previous work that created a surgical model for the local infusion of the ototoxic drug sisomicin in the chicken ear in vivo. This eliminates the hair cells “all at once,” allowing for not only greater efficiency but also better leveraging of single-cell RNA-sequencing technology. Our prior research showed, intriguingly, that damaged chick hair cells communicate with supporting cells before dying themselves, sending signals that may promote the regenerative process. Using single-cell analysis we set out to find out how these signals affect the surrounding non-hair cells, also called supporting cells. In addition, we were able to leverage our recently created, comprehensive inventory of tens of thousands of genes activated and deactivated throughout the first 24 hours of hair cell death. This baseline single cell data of the avian basilar papilla is in effect a “roadmap” for detecting changes in gene expression occurring after ototoxic insult. We used the same strategy to investigate the regenerative process at 30, 38, and 96 hours after hair cell death at a single cell resolution. As published in the journal Development in May 2022, we found that among avian supporting cells at 30 and 38 hours, the most prominent change in gene expression was the upregulation, or activation, of immune-related genes, linked to a common signaling pathway that is known as JAK/STAT. We also showed that the upregulated 30
hearing health
hhf.org
genes within the supporting cell layer are linked to JAK activation, and that inhibition of JAK/STAT signaling abolishes the upregulation of these genes. We provide evidence that in the regenerating basilar papilla, the expression of immune-related genes is tightly controlled, such that four days after damage, they are no longer expressed in newly regenerated hair cells. This is important because the JAK/STAT signaling pathway is highly potent, leading to inflammation, cytokine storms, and fibrosis. Our next steps are to identify the signals that lead to upregulation of immune-related genes in supporting cells and to determine whether these signals are essential for the process of hair cell regeneration. Building on research from fellow members of the Hearing Restoration Project, this paper contributes mechanistic knowledge about avian hair cell regeneration, finding that newly regenerated avian hair cells display unique combinations of genes that differ from naturally generated hair cells. This unveils differences between avian hair cell development/homeostasis and avian hair cell regeneration. Our collection of gene expression changes during avian hair cell regeneration provides a valuable resource with respect to devising strategies for hair cell regeneration in mammals. The process of how we utilize data analysis methods to order gene activation during hair cell regeneration along a temporal axis is a major technical advance that was possible through the support from the Hearing Restoration Project. Each study will bring us a step closer toward unraveling possible strategies for novel therapies. —Amanda Janesick, Ph.D., and Stefan Heller, Ph.D.
Amanda Janesick, Ph.D., is a former postdoctoral fellow in the laboratory of Stefan Heller, Ph.D., who is a 2001–2002 Emerging Research Grants (ERG) scientist, a member of HHF’s Hearing Restoration Project (HRP), and a professor of otolaryngology–head & neck surgery at Stanford University.
research
A schematic of the mouse cochlea (A) and the mouse brain (B) regions used for the enrichment analysis, in the American Journal of Human Genetics paper. Abbreviations: Amg, amygdala; Cbx, cerebellum; Ctx, cerebral cortex; Hi, hippocampus; Hy, hypothalamus; IHC, inner hair cells; Mb, midbrain; My, medulla; OB, olfactory bulb; OC, organ of Corti; OHC, outer hair cells; P, pons; Sc, spinal cord; SGN, spiral ganglion neurons; Str, striatum; Sv, stria vascularis; Th, thalamus.
Hope for Treatments Against Hearing Loss as 10 New Genes Identified Researchers led by King’s College London, Karolinska Institute, and Erasmus University have identified 10 new genes linked with hearing loss and have located the part of the ear affected. The findings, published in the American Journal of Human Genetics in June 2022, cast doubt on the understanding that age-related hearing impairment originates mainly from sensory hair cells. Researchers argue that the stria vascularis, a part of the cochlea in the ear, is a new target for treatments to help people with hearing loss. Many people gradually lose some of their hearing ability as they get older, and an estimated 2.4 billion individuals will have some form of hearing loss by 2050. Age-related hearing impairment is a top contributor to years lived with disability and is also an important risk factor for dementia. The team studied genetic analyses previously carried out in centers around the world using samples from 723,266 people from 17 studies with clinically diagnosed or self-reported hearing impairment. This meta-analysis is one of the largest conducted in hearing genetics to date. The researchers identified 48 genes linked to hearing loss, including 10 new variants newly linked to hearing. Further analysis looking at mouse genetics indicated
that age-related hearing loss is due to changes in the stria vascularis, which is necessary for hearing. The results provide targets for the basis of future research that could improve therapies against hearing loss. “Our findings identify 10 genes newly linked with hearing loss,” says co-main author Frances Williams, Ph.D., a professor at King’s College London. “This study points to genes we could target for screening purposes, drug development, and even gene therapy in the future. This study provides a solid foundation for ultimately improving therapies against hearing loss.” Co-main author Christopher R. Cederroth, Ph.D., an associate professor at the Karolinska Institute, adds, “It was hypothesized since the 1970s that the stria vascularis may play a role in hearing loss in humans, but the molecular evidence for this was missing until today.”
This press release originally appeared on EurekAlert. The paper’s coauthors also include 2009–2010 ERG scientist and HRP member Ronna Hertzano, M.D., Ph.D. (pictured), who is a professor in the department of otorhinolaryngology–head & neck surgery at the University of Maryland School of Medicine; Cynthia Morton, Ph.D., a member of HHF’s Council of Scientific Trustees; and 2002–2004 ERG scientist Anna Giersch, Ph.D.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
31
research
From the American Journal of Cancer Research paper, confocal images (A-D) of the middle turns of the mouse cochlea (Segment 3, frequency range: 19.1-36.5 kHz) immuno-stained with Myosin 7A, show hair cell loss after HNK and/or cisplatin treatment. Severe outer hair cell loss was induced by the treatment of cisplatin at 15 mg/kg (C), which is largely reduced by pre-treatment of HNK 20 mg/kg (D). Scale bar: 100 µm. Data represents mean ± SEM.
Honokiol Presents a Potential Paradigm Shift for Reducing Cisplatin Ototoxicity Platinum-based chemotherapeutic drugs are used in about 40 percent of cancer treatments. As potent as they are, severe side effects, such as damage to the brain, liver, kidney, etc., may occur. As a major side effect during chemotherapy, cisplatin ototoxicity (damage to the inner ear) affects an estimated 100,000 to 300,000 cancer patients annually in the U.S. The symptoms include severe hearing loss, tinnitus, and dizziness. Cisplatin ototoxicity (CO) is related to the accumulation of reactive oxygen species (ROS), causing the loss of the outer hair cells (OHC), one of the two sensory hair cell types for hearing function in the inner ear. To date, no effective Food and Drug Administration– approved treatment is available to protect against CO. The major concern of the candidate treatments is the interference of the therapeutic effects either by deactivating cisplatin or protecting tumor cells. Recent work by our team—my lab and that of ClausPeter Richter, M.D., Ph.D.—shows for the first time that honokiol, a multifunctional small molecule extracted from herbal medicine (genus Magnolia), prevents cisplatininduced hearing loss both in vitro, in cultured cells derived from the inner ear, and in vivo, in mice. Furthermore, this hearing protective effect of honokiol has also been verified on a transgenic tumor-bearing mouse model in chemotherapy regimen mimicking standard clinical treatments. Treatments were given in three cycles; in each cycle, 4 mg/kg/day (milligrams/ kilogram/day) of cisplatin was given for four days through injection, followed by a 10-day recovery interval. After the three-cycle treatments, cisplatin induces a severe hearing loss and OHC loss in the high frequency 32
hearing health
hhf.org
region (over 16 kilohertz), which is significantly reduced by parallel honokiol treatments (10 mg/kg/day, injected one hour before cisplatin). Meanwhile, the tumor growth is significantly slower, and animal survival rate is higher in the honokiol and cisplatin group than in the cisplatinonly group. These results indicate that honokiol is synergistic with cisplatin in tumor suppression, which is consistent with previous publications. Further studies show that the mechanism is related to the upregulation of sirtuin 3, a critical enzyme in mitochondria essential for ROS detoxification. The sirtuin 3 expression level is upregulated in the hair cells after honokiol treatment. Our study indicates that honokiol is a promising candidate for hearing protection against cisplatin ototoxicity. Honokiol is approved by the European Food Safety Authority as a food supplement and has been tested for its anti-asthma and anti-anxiety activities in preclinical trials. As a result, we expect a paradigm shift in cisplatin chemotherapy based on the current study and future clinical trials, where honokiol is applied to reduce side effects including hearing loss. This paper, published in the American Journal of Cancer Research in December 2020, formed the basis for my National Institutes of Health R01 project titled “Hearing Protection in Cisplatin Chemotherapy,” which was funded in February 2022. —Xiaodong Tan, Ph.D. A 2017 ERG scientist, Xiaodong Tan, Ph.D., is a research assistant professor in the department of otolaryngology at Northwestern University’s Feinberg School of Medicine.
research
Clues to How the Auditory Cortex Controls Subcortical Circuits Undergraduate textbooks typically paint the central auditory system as a linear, hierarchical structure: Sound information enters the brain via the 8th nerve, and electrical signals ascend through subcortical auditory circuits in a “bucket brigade” fashion. Sound is processed along each step of the pathway, and the auditory information reaches the auditory cortex, which supports higher-order perception and behavior. However, this textbook model is somewhat simplistic: Decades of research shows that the auditory cortex originates descending projections that operate in parallel with the ascending auditory system: Neurons in the deep layers of auditory cortex send excitatory nerve fibers back down to the majority of subcortical regions, like the thalamus, inferior colliculus, and cochlear nucleus. These “corticofugal” projections likely play a major role in hearing, as they provide an avenue for higher-order signals from the auditory cortex to shape how the early auditory system interprets incoming sounds from the ear. This cortical input conveys “top-down” information, which may provide contextual information to local processing in subcortical regions. Despite the existence of corticofugal pathways being well-established, little is known regarding the cellular and biophysical mechanisms that enable the auditory cortex to transmit top-down signals. In addition, we don’t understand how descending cortical signals are integrated with ascending information. In our eLife paper published in January 2022, we addressed this knowledge gap by studying the descending projection from the auditory cortex to the inferior colliculus (IC), a midbrain hub important for sound localization and speech perception. We combined optogenetic approaches with in vivo and in vitro patch-clamp electrophysiology in mice to study how the auditory cortex transmits messages to the IC. Our results revealed surprising biophysical properties of auditory cortex -> IC synapses that allow descending cortical signals to quickly amplify how individual IC neurons respond to ascending sound information. Interestingly, descending cortical pathways are not unique to the auditory system, but are also a feature of the brain’s visual, tactile, and olfactory pathways. Thus, our results may provide broadly generalizable insight into how the mammalian brain dynamically processes incoming sensory information. —Hannah Oberle and Pierre Apostolides, Ph.D.
This image from eLife shows an example micrograph of an injection site in the left auditory cortex in the mouse model. Dashed lines denote approximate borders of auditory cortical areas.
A 2019 ERG scientist, Pierre Apostolides, Ph.D., is an assistant professor of otolaryngology-head and neck surgery and an assistant professor of molecular and integrative physiology, both at the University of Michigan Medical School.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
33
research
Vestibular end organ whole mounts from the mouse model imaged with 25× objective, as shown in Bio-Protocol. The utricular macula, anterior canal crista, and horizontal canal crista can be dissected out of the temporal bone in one piece. Calretinin (magenta) is expressed in Type I hair cells. Single nerve fibers are labeled with green fluorescent protein.
Protocols for Preparing Mouse Balance Organs for Research The vestibular (balance) sensory apparatus contained in the inner ear is a marvelous evolutionary adaptation for sensing movement in three dimensions and is essential for an animal’s sense of orientation in space, head movement, and balance. Damage to these systems through injury or disease can lead to vertigo, Ménière’s disease, and other disorders that are profoundly debilitating. One challenge in studying vestibular organs is their location within the bony inner ear and their small size, especially in mice, which has become an advantageous mammalian model. This protocol, published in Bio-Protocol in May 2022, describes the dissection procedure of the five vestibular organs from the inner ear of adult mice. Immunohistochemical labeling can be used to identify specific hair cell types, such as calretinin-expressing Type I hair cells, or to localize proteins involved in mechanotransduction, cell structure, or vestibular disorders. We then describe the process of immunolabeling of a whole mount preparation using antibodies to label endogenous proteins or to amplify genetically expressed fluorescent proteins for confocal microscopic imaging. Using typical lab equipment and reagents, a patient technician, student, or postdoc can learn to dissect and immunolabel mouse vestibular organs to investigate their structure in health and disease. This is adapted from a paper published by Timothy Balmer, Ph.D. (far left), and Laurence Trussell, Ph.D. (near left), in Bio-Protocol in May 2022. A 2017 and 2022 ERG scientist, Balmer is an assistant professor in the School of Life Sciences at Arizona State University. His 2017 grant was generously funded by the Les Paul Foundation. A 1991 ERG scientist, Trussell is a professor of otolaryngology– head and neck surgery at Oregon Health & Sciences University. Balmer and Trussell used this procedure in their April 2019 eLife study, “Selective Targeting of Unipolar Brush Cell Subtypes by Cerebellar Mossy Fibers.” 34
hearing health
hhf.org
research
Clues About the Development and Regeneration of Chick Hair Cells The auditory system of the chicken has been extensively used in comparative studies of the evolution and development of hearing. The auditory systems of both humans and chickens are at comparable stages at birth, partially but not fully developed. Also, both species start to hear in the second-third of the gestation period, making the chick cochlea an attractive model system to study the developmental mechanisms of hair cells. In addition, avian species can regenerate hearing, an ability lost in mammals. The avian equivalent of the mammalian organ of Corti is the basilar papilla. The two hair cell types found in the chicken basilar papilla are tall and short hair cells, with tall hair cells similar to mammalian inner hair cells, and short hair cells similar to mammalian outer hair cells. Calcium ions are fundamental to the most important roles in sensory processing mechanisms in vertebrate hair cells, including avian and mammalian, such as mechanotransduction, synaptic release, and frequency selectivity. Moreover, it is well established that calcium ions are instrumental to hair cell development, for instance, by supporting the ability to produce spontaneous electrical activity (spontaneous action potentials), one of the hallmarks of development. This developmentally regulated spontaneous electrical activity also reappears in regenerating chick hair cells, suggesting that the process of regeneration may partly mimic developmental processes. This is an important implication to keep in mind when trying to regenerate the sensory epithelium in mammals. Auditory hair cells fire spontaneous action potentials before the onset of hearing, which may be a major determinant of synaptic formation and ensuing establishment of proper tonotopic maps along auditory axes during development. Once synapses are established between hair cells and spiral ganglia neurons, the spontaneous action potentials cease, highlighting the importance of spontaneous action potentials to the development of the auditory inner ear. Specific ion currents have been identified as major players supporting this electrical activity in developing and regenerating chick hair cells. This research by
The avian equivalent of the mammalian organ of Corti is the basilar papilla. The two hair cell types found in the chicken basilar papilla are tall and short hair cells, with tall hair cells similar to mammalian inner hair cells, and short hair cells similar to mammalian outer hair cells. Snezana Levic, Ph.D., published in Frontiers in Cell Neuroscience in January 2022, details the role of smallconductance, calcium-ion-activated potassium channels (SK) in developing and regenerating chick hair cells. Analysis of the functional expression of SK current showed that most dramatic changes occurred between embryonic day 8 and embryonic day 16. Further, the SK current is present in developing tall hair cells and contributes to the patterning of spontaneous electrical activity, and the SK current reappears in regenerating hair cells. This study provides direct evidence that the functional expression of SK current may contribute to the patterning of spontaneous action potentials in developing and regenerating chick tall hair cells.
This is adapted from a paper in Frontiers in Cell Neuroscience by Snezana Levic, Ph.D. A 2008 ERG scientist, Levic is a lecturer in physiology at Brighton and Sussex Medical School in the U.K.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
35
research
Why Children With Autism May Experience Auditory Sensory Overload The successful navigation of complex everyday environments with multiple sensory inputs—such as restaurants, busy streets, and other social settings— relies on the brain’s ability to organize the barrage of information into discrete perceptual objects on which cognitive processes, such as selective attention, can act. Failure of this scene-segregation process, where one sound source stands out as the foreground “figure” and the remaining stimuli form the “background,” can result in an overwhelming sensory experience that makes it difficult to focus attention selectively on one source of interest while suppressing the others. The experience of sensory overload and difficulty with being able to selectively listen to a foreground sound source of interest are ubiquitous in autism spectrum disorders (ASD). To group sound elements scattered across different frequencies correctly into individual sources (e.g., components of a speaker’s voice vs. components of background traffic noise in a busy street), the brain must carefully analyze the temporal coherence across the different sound elements in a mixture. A leading hypothesis about sensory processing abnormalities in ASD is that this kind of temporal “synthesis” of sensory information is atypical. This hypothesis stems from behavioral data indicating that individuals with ASD often show impaired processing of analogous dynamic stimuli in the visual domain, such as the coherent motion of visual dots. Although behavioral evidence in ASD is consistent with the impaired-temporalsynthesis hypothesis, direct neural correlates have not been identified. In our study published in PLOS Biology in February 2022, we investigated whether auditory temporal coherence processing is in ASD by employing a novel auditory paradigm. By manipulating temporal coherence in the scene with synthetic sounds, the paradigm was designed such that the acoustic features of the stimulus
36
hearing health
hhf.org
perceptually bind together into auditory objects with different levels of salience, with the salience of the foreground “figure” object parametrically increasing with increasing temporal coherence. As hypothesized, we found that children with ASD had significantly reduced evoked responses to the pop-out of the foreground figure, alongside a lower magnitude of induced gamma band activity. Importantly, the cortical measures were not correlated with the behaviorally assessed ability to suppress attention to distractors, suggesting that lower-level auditory processes contribute to the observed abnormalities. The cortical measures did, instead, correlate with both ASD severity and abnormality of auditory sensory processing, thus predicting how children within the ASD group would stratify behaviorally. These results suggest that neural processing of the temporal coherence of the acoustic constituents of an auditory stimulus is atypical in ASD. Given the importance of temporal coherence as a binding and scene segregation cue in natural sounds, the atypical processing of temporal coherence in ASD could contribute to poorer object binding, as has indeed been suggested, and demonstrated indirectly in the visual domain in ASD. In scenes with multiple sound sources, the reduced growth of the response with temporal coherence could lead to foreground sounds “standing out” less saliently and a reduced ability to filter out extraneous sounds, contributing to a feeling of sensory overload. This would inevitably also impact speech and language processing, which are highly temporally sensitive, especially in environments with multiple sound sources. Indeed, speech perception impairments in noisy environments in particular have been documented in ASD. One key advantage of our novel stimuli and the passive design is that the paradigm is translatable to patient populations where behavioral assessments cannot easily be performed (such as infants and toddlers). The paradigm
research
Responses evoked by overall stimulus onset, as shown in PLOS Biology. (A) Averaged left hemisphere evoked responses relative to stimulus onset, in source space, based on individually identified regions of interest (inset), for each group. (B) Same as (A), for the right hemisphere. Shaded areas show standard error per group. Abbreviations: ASD, autism spectrum disorder; L, left; R, right; TD, typically developing.
is also applicable to animal models of ASD and other neurodevelopmental disorders. In sum, our observations of reduced growth of neural responses with increasing temporal coherence of auditory stimuli in ASD provide new insights into the mechanisms that may ultimately contribute to the sensory processing deficits and socialcommunication challenges that are characteristic of ASD. If borne out in larger-scale studies, our findings also raise the possibility that audiological interventions (such as remote microphones in classroom settings) that help those with central auditory processing challenges may also be beneficial for children with ASD. —Hari Bharadwaj, Ph.D.
A 2015 ERG scientist generously funded by Royal Arch Research Assistance, Hari Bharadwaj, Ph.D., is an assistant professor at Purdue University with a joint appointment in speech, language, and hearing sciences, and biomedical engineering.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
37
research
Pinpointing How Older Adults Can Better Hear Speech in Noise In real-world listening situations, we always listen to speech in the presence of other sources of masking, or competing sounds. One of the major sources of masking in such situations is the speech signal that the listener is not paying attention to. The process of understanding the target speech in the presence of a masking speech involves separating the acoustic information of the target speech and tuning out masker speech. Young, typical-hearing individuals can function in moderate amounts of speech distortions with a minimal reduction in speech understanding, while older individuals with and without hearing loss are much more susceptible to the distortions of the speech signal and often experience increased difficulties in understanding speech in noisy environments. The process of understanding target speech in the presence of masking speech partially involves separating out and attending to the acoustic information of the target speech while ignoring the acoustic information of the masking speech. Target speech and masking speech can be segregated based on factors such as the locations of the target and maskers in the environment, differences in fundamental frequencies between the target and maskers, interaural (between the two ears) time differences, interaural level differences, or differences in contextual information between the target and maskers. Spatial release from masking (SRM) is the reduction in target identification thresholds when the maskers are physically distanced from the target. Results from recent speech masking studies confirmed that an individual’s ability to obtain a better identification threshold when the target and maskers are spatially separated is driven by a combination of better-ear listening, binaural (using both ears) unmasking, and perceived location of the target and the maskers. Better-ear listening is an auditory phenomenon created by the head shadow effect wherein the listener uses the interaural level differences between the two ears to better understand speech. Binaural unmasking is the increased ability of the listener to better understand speech in
38
hearing health
hhf.org
the presence of noise when there is an interaural time difference between the signals reaching the two ears. An individual’s temporal acuity is typically described using the gap detection threshold, which is the smallest silent interval in the stimulus detected by the listener. While many studies have concluded that older individuals have broader difficulties in temporal and spatial processing tasks, very few studies are available in the literature that contain multiple temporal and spatial processing measurements from the same individual. We sought to measure the temporal and spatial processing capabilities of older individuals with hearing loss and to use statistical models to identify the individual contributions of gap detection thresholds and localization acuity to SRM. Twenty-five older listeners with varying degrees of hearing loss participated in this experiment, the results of which were published in the International Journal of Audiology in November 2021. We found that spatially separating target and masker sources helps to better identify speech in speech-on-speech masking scenarios, and that difficulties in spatial and temporal processing co-occur in older individuals and individuals with reduced hearing acuity. However, reduced temporal and spatial processing due to aging, independent from reduced hearing acuity, was not observed. Multiple regression models predicting SRM using gap detection thresholds and localization acuity indicated that the ability of the listeners to use interaural time differences between the signals arriving at the two ears is responsible for obtaining better identification thresholds in spatially separated conditions. —Nirmal Kumar Srinivasan, Ph.D. A 2016 ERG scientist generously funded by Royal Arch Research Assistance, Nirmal Kumar Srinivasan, Ph.D., is an assistant professor in the audiology program in the speech-language pathology and audiology department at Towson University in Maryland.
research
This is an illustration of cochlear implantation via the modiolus approach used in the rat model for this study in Measurement and Control. Abbreviations: HC: hair cell; SGC: spiral ganglion cell; CN: cochlear nucleus.
Using Algorithms to Measure Response Times to Auditory Nerve Stimulation Neural information travels among multiple areas in the brain, which has been of great interest in the field of neurocomputation, and several computational methodologies have been developed and applied to measure the neural information flow. Measurement of the information flow along the ascending auditory pathway from the periphery to the auditory cortex (AC) has been given much attention in neurocomputation. While the neurophysiological mechanisms of the auditory pathway have been well studied, the temporal resolution and relationships among the auditory centers are still under investigation, especially when suffering from acoustic trauma that results in peripheral deficits and signal changes in the auditory system. In our study published in the journal Measurement and Control in April 2022, by chronically implanting the electrodes in the auditory nerve (modiolus approach) and auditory cortex, we measured rat auditory cortex (AC) neurons and auditory nerve (AN) signals in a digital format by using two new algorithms to calculate the neural response time of the AC neurons to electrical stimulation of the AN and quantify the neural information flow in the temporal domain. The proposed algorithms could provide a clue on the signal response and its shifts in the AC during the development of hyperactivity, a neural mechanism of tinnitus, and lead to an in-depth understanding of the information flow inside the auditory pathway. This will help us to better understand the mechanisms of tinnitus. One algorithm compared the time differences of neural spikes directly, which was based on the conventional idea of the spike train in neurocomputation. The other employed a modified cross-correlation algorithm. To test the effectiveness of the proposed method, the time difference of the AC to AN was calculated by both algorithms with raw neural signals collected.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
39
research
The animals had measurements before and after noise trauma, and one of the animals received intra-modiolus electrical stimulation to stimulate the AN. As a proof-of-concept study, the consistent results from using these two algorithms support quantifying AC time delays to AN stimulation, which could interpret temporal information processing along the auditory pathway. For future work, a larger sample size of animals will be used and multichannel neural signals will be simultaneously collected in the AC and other areas of the brain, allowing us to develop a more complete measurement system to analyze the temporal relations along the auditory pathways. Together, the temporal relation and correlation would provide a clearer view of the neural information flow that will better our understanding of the mechanism of tinnitus-related neural activities in auditory brain structures. —Hao Luo, M.D., Ph.D. A 2019 ERG scientist generously funded by Royal Arch Research Assistance, Hao Luo, M.D., Ph.D., is an instructor at Henry Ford Health System in Detroit.
40
hearing health
hhf.org
Perceptual Decision-Making for Speech Recognition in Noise Speech recognition in noise is typically poorer for older adults than younger adults, which can reflect a combination of sensory and cognitive-perceptual declines. Considerable variability, with some older adults performing nearly as well as younger adults, may be explained by differences in listening effort or cognitive resources to facilitate speech recognition. Neuroimaging evidence suggests that a set of frontal cortex regions are engaged with increasing listening difficulty, but it is unclear how this might facilitate speech recognition. Speech recognition in noise task performance has been linked to activity in cingulo-opercular regions of the frontal cortex, in what appears to be a performance monitoring role. More extensive frontal cortex activity during challenging listening tasks has been shown for older compared to younger adults, which could reflect task difficulty. Our study, published in the journal NeuroImage in June 2022, examined neural mechanisms that may support speech understanding in noise and other difficult recognition tasks. In relatively quiet acoustic conditions, speech recognition often occurs very rapidly, mapping sensory input (sound) onto stored mental representations. However, when speech information is distorted or limited by background noise, recognition often becomes slow and effortful. Recognition based on incomplete sensory information (e.g., noisy conditions) is theorized to involve perceptual decision-making processes that collect evidence until a recognition criterion is met. A perceptual decisionmaking theoretical framework has been used to account for the speed-accuracy tradeoff: fast responses associated with low accuracy, and slow responses associated with high accuracy.
research
A figure from the NeuroImage paper shows the word recognition task significantly increased activity throughout superior temporal regions and cinguloopercular regions of cortex.
We used an fMRI (functional magnetic resonance imaging) experiment with middle-aged and older participants to examine perceptual decision-making activity, particularly in cingulo-opercular regions across the frontal cortex. Participants were instructed to listen to a word presented in a multi-talker babble environment (e.g., cafeteria noise), and repeat the word aloud. A sparse design with long, quiet gaps between scans (6.5 seconds) allowed speech to be presented without scanner acquisition noise and minimized speech-related head movement during image collection. We found that word recognition was significantly less accurate with increasing age and in the poorer signal-tonoise ratio condition. A computational model fitted to task response latencies showed that evidence was collected more slowly and decision criteria were lower in the poorer of two signal-to-noise ratio conditions. Our fMRI results replicated an association between higher, pre-stimulus BOLD contrast (i.e., prior to each presentation) measured in a cingulo-opercular network in the frontal cortex and subsequent correct word recognition in noise. Consistent with neuroimaging studies that linked cingulo-opercular regions in the frontal cortex with decision criteria, our results also suggested that decision criteria were higher and more cautious on trials with elevated activity. The takeaway is that perceptual decisionmaking accounted for changes in recognition speed and was linked to frontal cortex activation that is commonly observed in difficult listening tasks. In summary, our study indicates that 1) perceptual decision-making is engaged for difficult word recognition conditions, and 2) frontal cortex activity may adjust how
much information is collected to benefit word recognition task performance. These findings potentially connect neuroscientific research on perceptual decision-making, often focused on visual object recognition, with our research on agerelated listening difficulties and (nonauditory) frontal cortex function in these tasks. Similar neural mechanisms may help guide how a person drives a car in heavy fog or listens to a friend speaking in a crowded restaurant. In either of these cases, a related set of brain networks may collect evidence until recognition occurs. Additional studies will characterize how evidence collection and decision criteria relate to hearing loss and older age. —Kenneth Vaden, Ph.D.
A 2015 ERG scientist generously funded by Royal Arch Research Assistance, Kenneth Vaden, Ph.D., is an assistant professor in the department of otolaryngology–head and neck surgery at the Medical University of South Carolina, where HHF board member Judy R. Dubno, Ph.D., one of the paper’s coauthors, is a professor. For references, see hhf.org/summer2022-references.
Support our research: hhf.org/donate. a publication of hearing health foundation
summer 2022
41
managing hearing loss
hearing health foundat i o n
Explanations for Cochlear Implant Hesitancy—and What Hearing Care Professionals Can Do About It By Nancy M. Williams
Cochlear implants are often recommended to patients with severe to profound hearing loss who no longer benefit from hearing aids. According to the World Health Organization, a person with severe hearing loss is unable to hear a raised voice three feet away, while a person with profound hearing loss cannot hear a shouted voice in the ear. Despite the benefits of cochlear implantation, adoption is low. Current cochlear implant (CI) usage among adults who are indicated for them is about 5 percent. To investigate barriers to adult CI adoption, I partnered with Erin Schafer, Ph.D., a professor and audiologist at the University of North Texas. We curated, analyzed, and synthesized several recent publications in peer-reviewed hearing health literature to determine why patient demand and adoption lags. We reached three important conclusions: » Uncertainty surrounding the outcome of cochlear implantation drives top patient concerns expressed in the studies. » Of the top five patient concerns, three center around whether a CI would improve communication ability and music appreciation better than hearing aids. » Variability in patient experience with the CI healthcare system and public perceptions about surgical risks exacerbate patient concerns about uncertain outcomes.
Top Benefits
When CI candidates evaluate implantation, they often solicit advice from family members, close friends, and even coworkers. Taken together, the people in candidates’ circles make up the general public. In a survey of over 600 people in the U.S. general public, the perceived risks of cochlear implantation in most cases outweigh the benefits, according to a March 2022 Otology & Neurotology study. To participate in this study, respondents did not need to have or even know someone with hearing loss. The top benefits selected by survey participants (shown in the graphic at right) center around enhanced 42
hearing health
hhf.org
communication. Respondents assigned the highest priority to a person’s ability to converse with a stranger. We believe that the public demonstrates a good understanding of a key challenge faced by people with hearing loss: the difficulty of recognizing and understanding an unfamiliar voice in a noisy environment.
Wide Range in Outcomes That said, an important foundation to understanding adult patient barriers to CI adoption is the wide range in outcomes. Patients’ 12-month postoperative speech perception ranges from 0 to 100 percent, according to a January 2022 Laryngoscope study that mined a multi-institutional outcomes database. (Dr. Schafer is a coauthor of this paper.) Patients experience significant uncertainty in the face of this wide range of outcomes. Generally patients who register higher speech recognition during their CI evaluation realize the best outcomes, a fact some clinicians may communicate during patients’ decision making process. Nonetheless, patients may still struggle when determining whether to proceed with cochlear implant surgery. They may want to understand, for example, how their personal hearing loss history could impact
managing hearing loss
their predicted outcome. Patients’ willingness and ability to undergo rehabilitation could also play a sizable role. As a result of these factors, patients lack a process for predicting their outcomes with cochlear implantation.
Original Medicare does not cover hearing aids, but it does cover cochlear implantation, with most private payers following Medicare’s lead. (The exception is Medicare Advantage’s limited copays and allowances for hearing aids.)
Top Concern
Opportunities for Change
In an Otology & Neurotology paper published in December 2021, patients indicated their primary concern with implantation is that a CI would not improve their ability to communicate. This study surveyed 52 patients from a single center and included roughly equal numbers of CI recipients and people who were candidates but did not opt to pursue a CI. We believe the uncertainty surrounding outcomes for cochlear implantation is the primary driver of this top patient concern. Concerns about postoperative recovery, including waiting for CI activation and rehabilitation, is a secondtier barrier, as is the surgery itself. Patients expressed concern about the surgical risks of cochlear implant surgery, a concern which echoes public perceptions. Importantly, a subgroup of respondents who had “personal knowledge of someone with a CI” found all risks acceptable. Familiarity with a patient reversed the public’s risk-benefit calculation to support for implantation. The implication is that peer meetings for CI candidates are crucial, even at the center level. A 2018 Trends in Hearing report supports the finding that meeting someone who had a good outcome with a CI is an important motivator for getting the surgery.
infographic credit: auditory insight
Additional Patient Uncertainty
Expanding to the third tier in the Otology & Neurotology study reveals two additional patient concerns: losing music appreciation, and that a CI is unnecessary because hearing aids suffice. Fears surrounding loss of music appreciation originate in mixed postoperative outcomes. Some CI recipients report adequate music appreciation while others report that their ability to play or listen to music is destroyed. Clearly limitations in CI technology impact music perception post-surgery. Given the uncertainty of CI surgical outcomes, many patients are no doubt motivated to limp along with their hearing aids for as long as possible. This behavior is reflected in the research, showing the typical patient waits until their hearing loss reaches a profound level before proceeding with a CI, according to the Laryngoscope research and the Trends in Hearing study. However, it is notable that insurance coverage of cochlear implants is far broader than for hearing aids.
While the industry moves toward developing standards and clinical guidelines for adult CIs, we see three important opportunities for CI centers: » Develop center-level data to summarize patient outcomes and time requirements » Help patients chart personalized risk/benefit analyses » Create a center-level advocacy team of parents and patients. Our conclusion is that the primary causative barrier to CI adoption is outcome uncertainty, exacerbated by process variability (such as the lack of an institutionalized screening program for adults like that for newborns) and reinforced by public opinion. The programs of the three CI manufacturers—Advanced Bionics, Cochlear, and MED-EL—to provide CI candidates with access to peers who are satisfied CI wearers is an important step in the right direction. The industry faces exciting opportunities to continue to address patient needs and increase CI adoption, providing more adults with better hearing.
A former board member of Hearing Health Foundation, as well as a strategic adviser and thought leader on transforming hearing healthcare, Nancy M. Williams is the founder and president of Auditory Insight. She partners with senior executives to create successful market development strategies in hearing healthcare, and also advises investment firms on the hearing sector. For more, see auditoryinsight.com. For her experiences as a pianist with a hearing loss, see grandpianopassion.com. For references, see hhf.org/summer2022-references.
Share your story: Have you considered cochlear implants? Tell us at editor@hhf.org.
Support our research: hhf.org/donate.
a publication of hearing health foundation
summer 2022
43
advertisement
This sponsored page shows current trends in technology.
Tech Solutions
Simple Yet Powerful Hearing Amplifier
CapTel® Captioned Telephone
Never Miss a Word With Olelo Captioned Calls
Developed in Israel for people with mild to severe hearing problems, BeHear® SMARTO provides up to 70 dB of customizable hearing boost. It is hand-held or body-worn, easy to use, Bluetooth®-enabled, and rechargeable. SMARTO integrates award-winning technologies reducing background noise to clarify speech in live conversations, cell phone and video calls, and TV programs. It features a masking noise generator for tinnitus relief, and an emergency call button. Visit alango-behear.com.
Enjoy the phone again with confidence! Ideal for people with hearing loss, the CapTel® Captioned Telephone shows captions of every word the caller says over the phone. You can listen to the caller, and read the written captions in the CapTel® display screen. Only CapTel® gives you several models to choose from, including contemporary touch-screen options and traditional telephone styles. All CapTel® phones include a large display screen, adjustable font sizes and colors, and a builtin answering machine that shows captions of your messages. CapTel® gives you the confidence to reconnect over the phone, knowing you won’t miss a word! Visit CapTel.com.
Powered by advanced speech recognition, Olelo is a next-generation captioned phone service designed for maximum accuracy and privacy in an easy-to-use mobile app. Captions each spoken word in real time. Fully automated captioning protects your privacy. Voicemail, saved transcripts, Bluetooth, and more. It’s free! Olelo is an FCC-certified service paid for by a federally administered fund. Try Olelo today! Install takes just minutes! Visit getolelo.com.
• • • •
These featured products are paid advertisements. To advertise in Hearing Health magazine, email hello@glmcommunications.com or call 212.929.1300.
44
hearing health
hhf.org
marketplace
Supporters of Hearing Health Captioned Telephone
Everything that you need and nothing that you don’t. Cellular service on the nation’s most dependable network. Free flip phone or smartphone, free activation, free shipping. Start saving on your cell phone service today!
Hand-held or body-worn, Bluetoothenabled, and rechargeable, BeHear SMARTO provides up to 70 dB of customizable hearing boost. It reduces background noise, provides tinnitus relief through a masking sound generator, and has an emergency call button.
affinitycellular.com
alango-behear.com
captel.com 800.233.9130
page 48
page 44
pages 2, 44
InnoCaption is the only mobile app that offers real-time captioning of phone calls through live stenographers and automated speech recognition software—the choice is yours. Our technology makes phone calls easy and accessible!
The Les Paul Foundation inspires innovative and creative thinking by sharing the legacy of Les Paul through support of music education, recording, innovation, and medical research related to hearing.
Olelo Captioned Calls is an easyto-use app that produces accurate captioning in less than a second, keeps conversations private by using automated speech recognition, and can be used anywhere service or WiFi is available.
CapTel captioned telephone shows word-for-word captions of everything a caller says over the phone. Like captions on TV—for your phone. Helps people with hearing loss enjoy phone conversations, confident they’ll catch every word.
innocaption.com
les-paul.com 212.687.2929
olelophone.com
page 5
pages 22–23, 34
page 44
Picture Your Company Logo Here Hearing Health Foundation’s Emerging Research Grants (ERG) fund innovative approaches toward understanding, preventing, and treating hearing and balance conditions.
Hearing Health Foundation’s Hearing Restoration Project is the first international research consortium investigating how to regenerate inner ear sensory hair cells in humans to eventually restore hearing.
All Hearing Health advertisers and other partners are featured on this Marketplace page at no additional charge. Please join our community of supporters.
hhf.org/erg
hhf.org/hrp
212.929.1300
pages 32–41, 46
pages 30–31 a publication of hearing health foundation
summer 2022
45
meet the researcher
hearing health foundation
Emerging Research Grants (ERG) As one of the leading funding sources available for innovative research, HHF’s ERG program is critical. Without our support, scientists would not have the needed resources for cutting-edge approaches toward understanding, preventing, and treating hearing and balance disorders.
Meet the Researcher James W. Dias, Ph.D.
The Medical University of South Carolina
Dias received his doctorate in psychology from the University of California, Riverside. He completed postdoctoral training in the department of otolaryngology-head and neck surgery at the Medical University of South Carolina, where he is now an assistant professor. Dias is a 2022 Emerging Research Grants recipient generously funded by the Meringoff Family Foundation. older adults, including my grandparents, typically have difficulty understanding speech, especially in noisy or echoey listening environments, and may use their sight to compensate. My research project was developed to determine how age-related changes across the nervous system can explain how older adults are better able to use what they see to understand what they hear. I hope that understanding the underlying neurophysiology for cross-sensory compensation will provide new avenues for rehabilitation, helping people communicate effectively throughout their lifespan. when i was a kid, I wanted to be an astrophysicist and to build the USS Enterprise! By college, my goal was to be a veterinarian. So I have always loved science, but it was not until I started working in the lab at California State University, Fresno, during my master’s that I became passionate about multisensory processing. Our experiments in audiovisual speech perception fueled my interest in how the brain takes information from across the senses to understand the world around us. I was first in my family to receive a Ph.D. I trained at the Medical University of South Carolina, developing my skills to include aging research and neuroimaging.
i hold a black belt in American Kenpo. Martial arts are themselves multisensory, incorporating what you hear and see with physical motion and proprioception. Likewise, cooking—I am a big foodie—is also multisensory. What you hear, smell, and feel can all affect what you taste and how you enjoy the experience. I love trying out new restaurants and wine-tasting. I like to challenge myself to learn new cooking skills and techniques. My family and friends have certainly reaped the benefits of this hobby. my longer-term goal is a vibrant, independently funded research program with trainees concerned with understanding the neurophysiology that facilitates audiovisual speech processing across the lifespan. Or, if this whole science thing doesn’t work out, I’ll open a bed and breakfast with my partner!
James W. Dias, Ph.D., is generously funded by the Meringoff Family Foundation. HHF sincerely thanks them for their commitment to research on age-related hearing loss.
We need your help funding the exciting work of hearing and balance scientists. Please consider donating today to Hearing Health Foundation to support groundbreaking research. Visit hhf.org/how-to-help. 46
hearing health
hhf.org
YOU CAN MAKE A DIFFERENCE NOW announcing a planned giving matching challenge
Ann Pruitt has named HHF in her estate plans.
Planned giving, also called estate or legacy giving, means a gift that your favorite charity receives upon your passing. It is a gift for the future. A generous, anonymous donor has launched a challenge that will match your planned gift now. This enables Hearing Health Foundation to continue funding the life-changing science that benefits the millions of people who live with hearing and balance challenges. Your planned gift will be matched when you make a bequest to HHF or name us as a partial beneficiary of a retirement fund or life insurance policy.
Here’s how the matching challenge works: » » »
For any planned gift of up to $10,000, HHF receives a match of $1,000. For any planned gift of $10,000 or more, HHF receives a match of $10,000. For larger planned gifts, HHF receives a match of $100,000.
Please email Harriet Hessam at hhessam@hhf.org to let us know about your planned gift or for more information.
You can make a difference NOW as well as in the FUTURE.
Please scan this QR code to learn more about Hearing Health Foundation’s extraordinary planned giving matching challenge.
Don’t have a will? Create one for free with our partner FreeWill at freewill.com/hhf.
h e a ri n g h e alt h fo u n dation
48
hearing health
hhf.org