

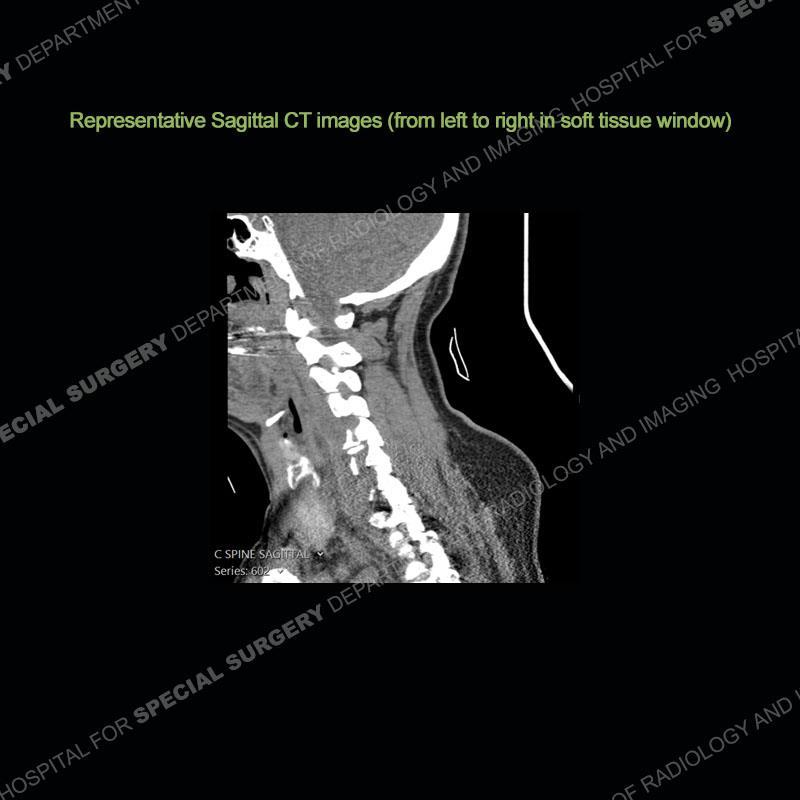








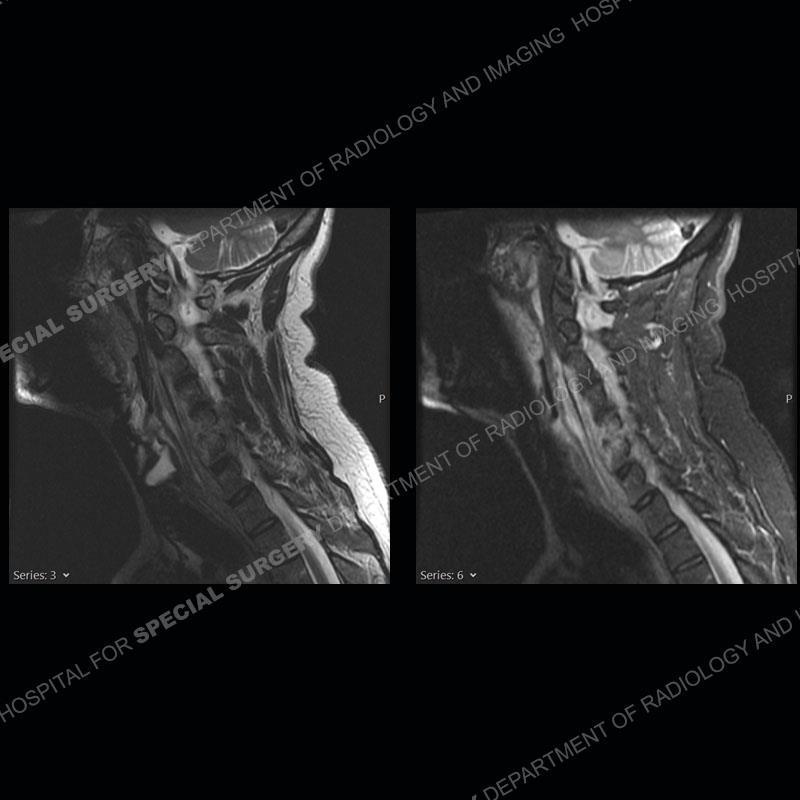


































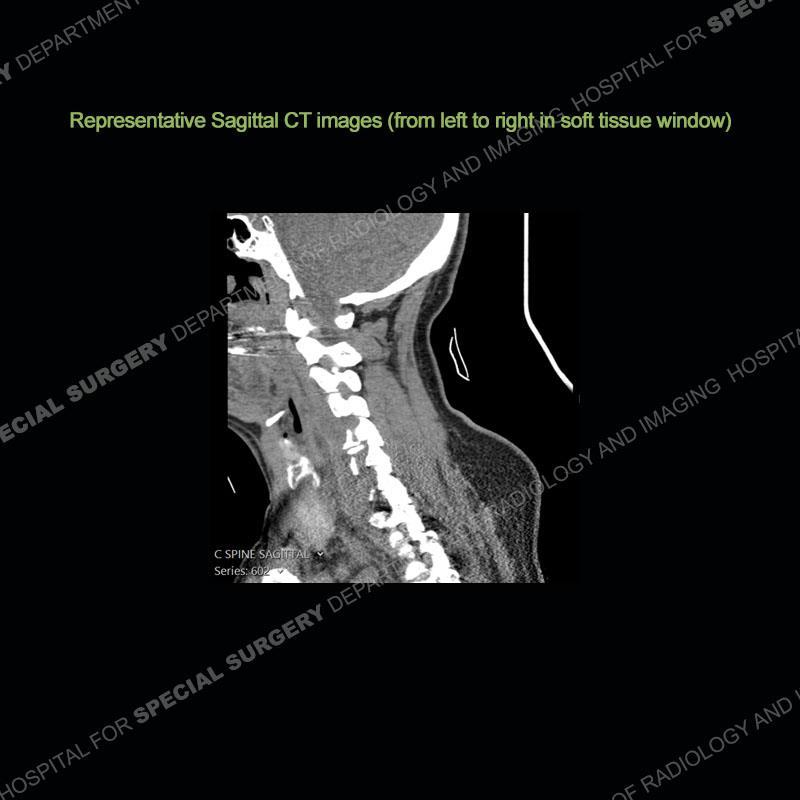








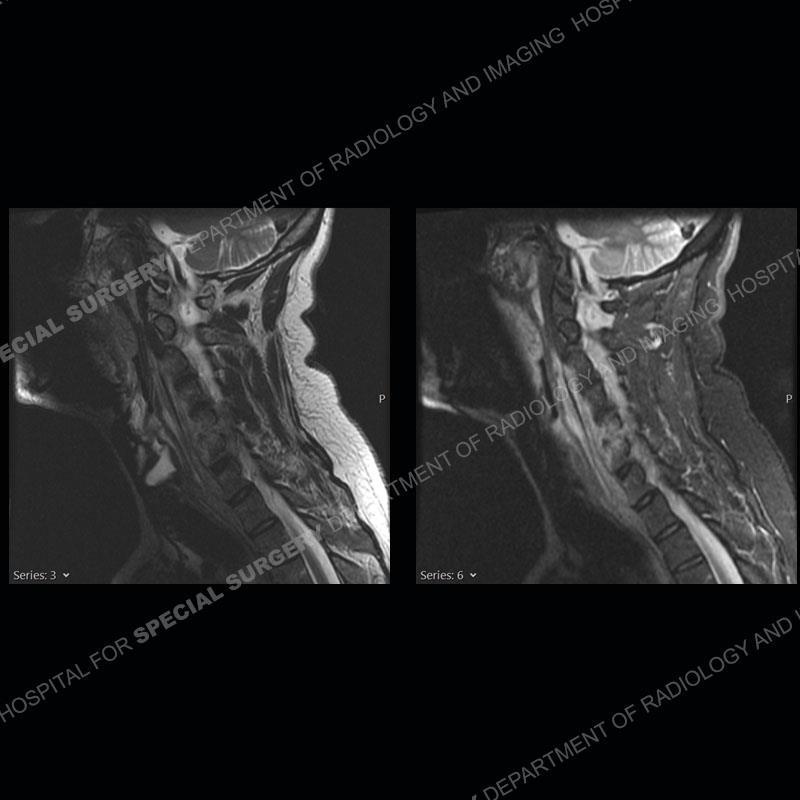































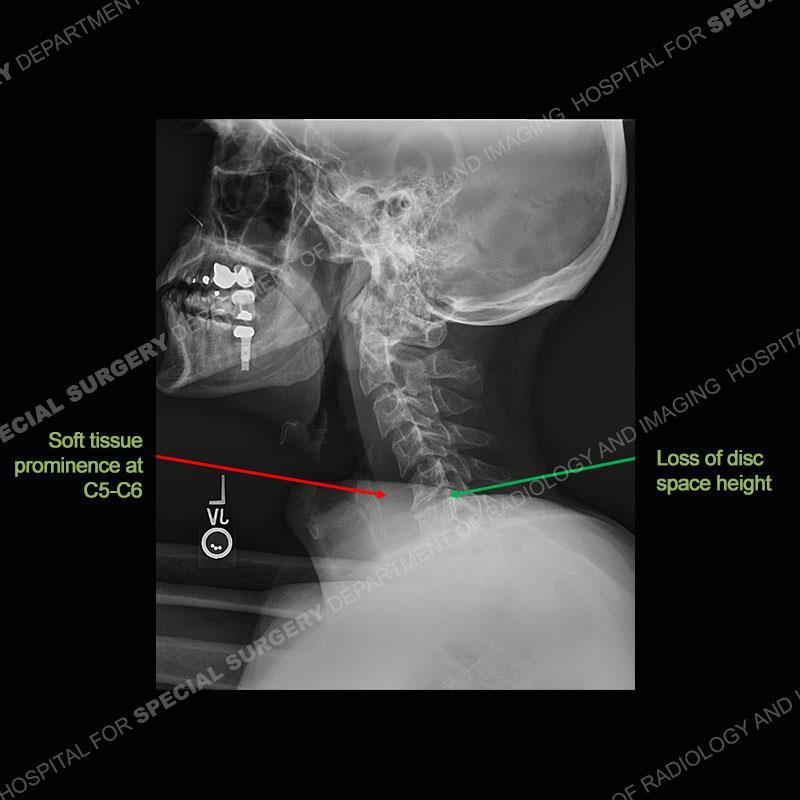
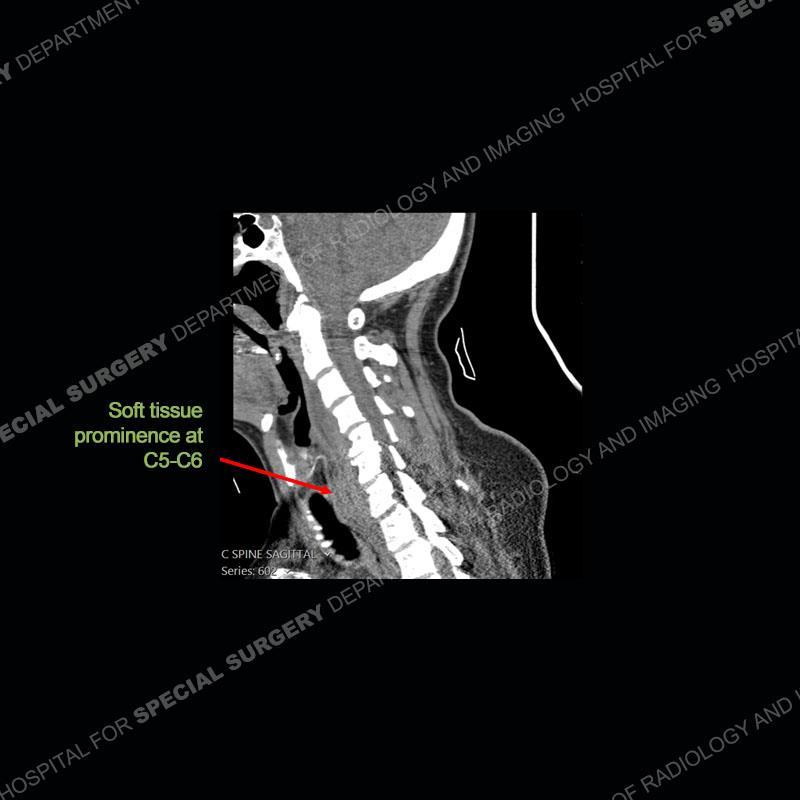
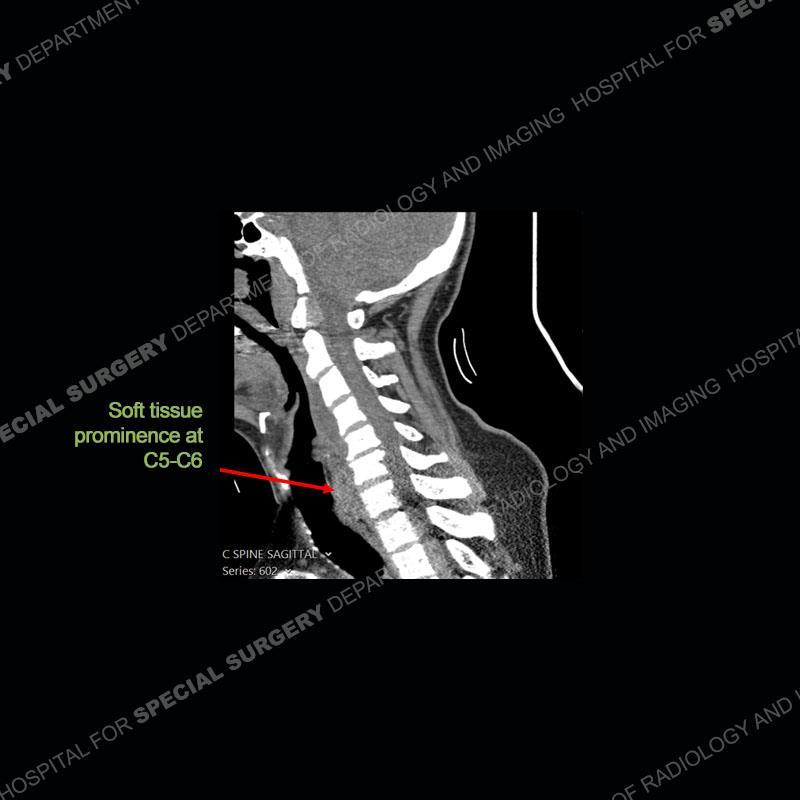
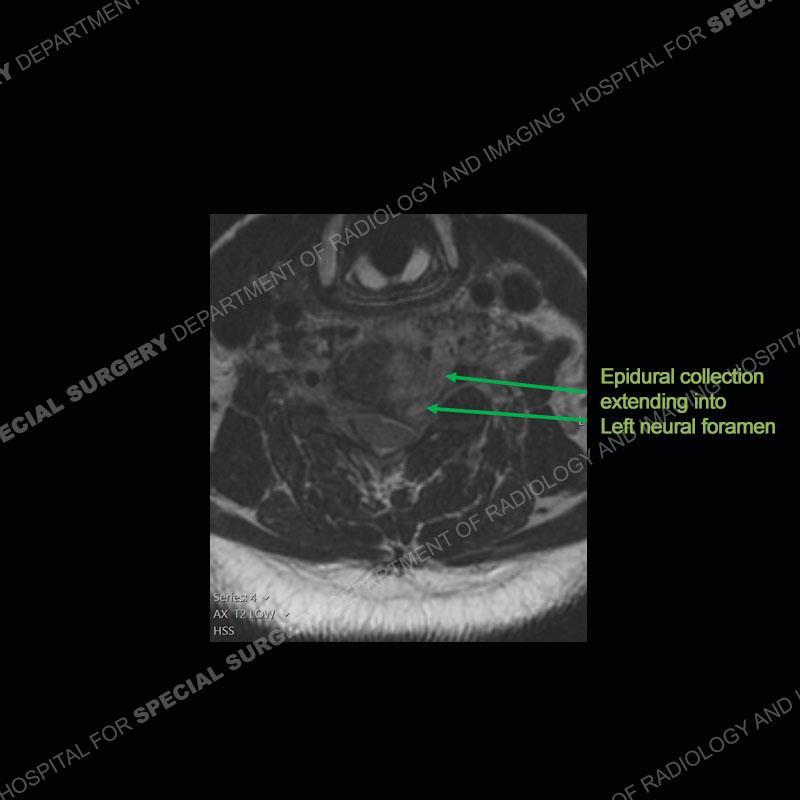
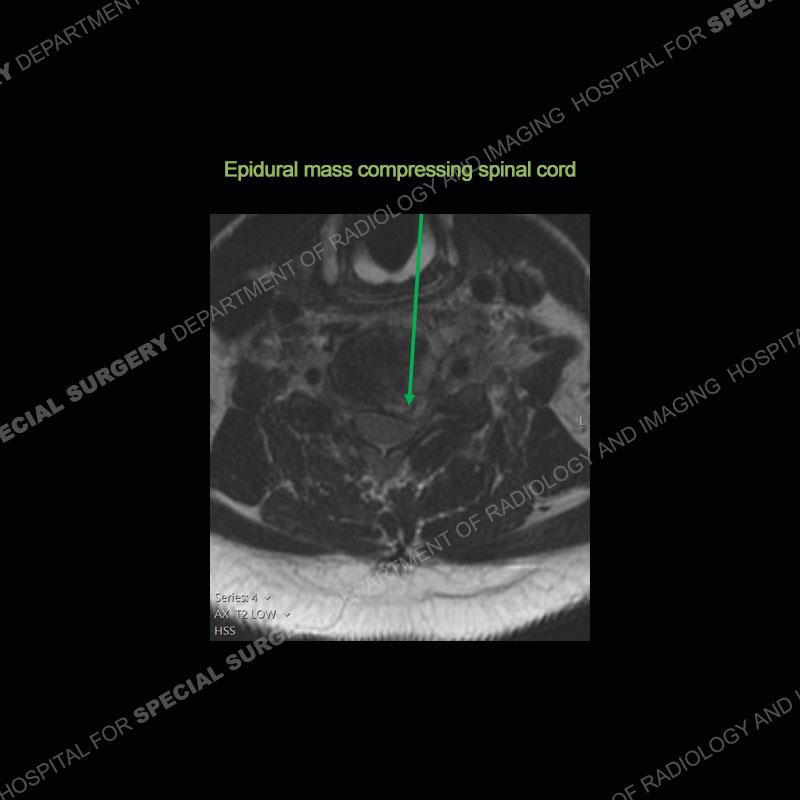
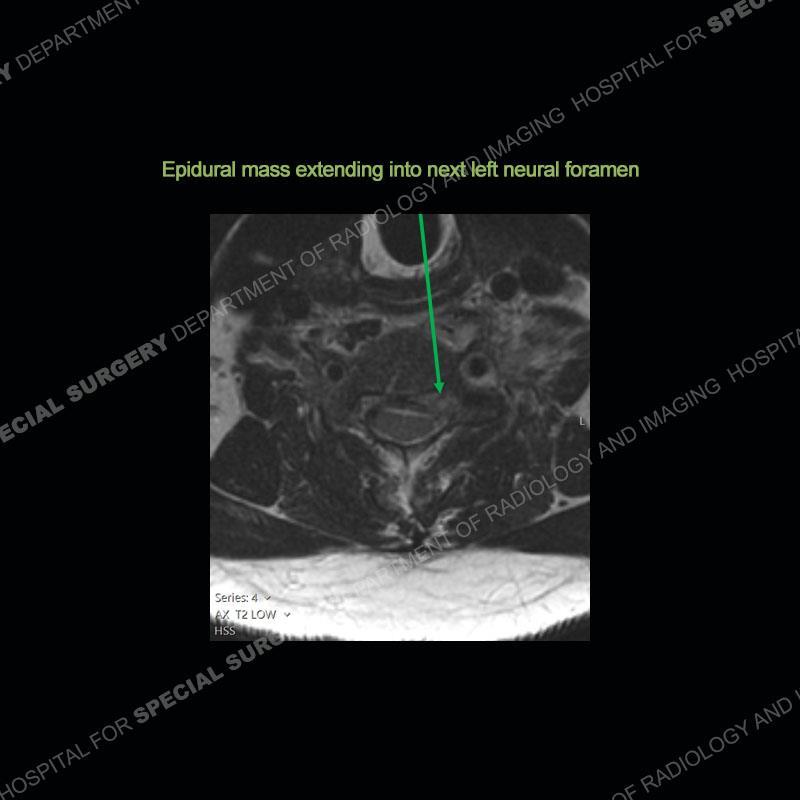
The radiographs demonstrate a prevertebral soft tissue fullness centered at C5-C6 that persists even on extension. There is a slight loss of disc height at C5-C6. The CT more readily shows the prevertebral soft tissue swelling at C5C6 where there is a punctate focus of gas. On the MRI, there is a marked amount of edema and a heterogeneous collection in the prevertebral soft tissue at C5-C6. Edema is present of the C5 and C6 vertebral bodies with a loss of the normal architecture about the disc space. A heterogeneous epidural collection has formed that causes compression of the spinal cord asymmetric to the left side and also precipitates severe left sided neural foraminal stenosis.














Spontaneous RPA in the non-immunocompromised, adult population is an extremely rare occurrence. RPA most frequently occurs in young children and most typically after a URI. It may be associated with torticollis in Grisel syndrome. In the adult population, the pathomechanism is not well understood with some suggesting a hematogenous spread or perhaps a seeding from the adjacent aerodigestive tract. The abscess as in this case can extend to involve the vertebral column and then the neural elements. At times, this process can be treated with antibiotic therapy alone but when there are neurologic symptoms and especially progression of neurologic symptoms, surgical intervention is warranted. In this case, given the extent of the process and the patient’s clinical situation, a corpectomy with fusion was performed in addition to antibiotics.



Spontaneous, Non-Traumatic Retropharyngeal Abscess Complicated by Spinal Osteomyelitis and Epidural Abscess in Immunocompetent Adult: Management and Proposal Pathophysiological Mechanism. Giorgos Sideris ,Thomas Nikolopoulos, Nikolaos Papadimitriou. Cureus. 2020 Jul; 12(7): e9028. Independent predictors of failure of nonoperative management of spinal epidural abscesses. Sang Do Kim, Rojeh Melikian, Kevin L Ju, David Zurakowski, Kirkham B Wood, Christopher M Bono, Mitchel B Harris. Spine J. 2014 Aug 1;14(8):1673-9. doi: 10.1016/j.spinee.2013.10.011. Epub 2013 Oct 30.
Retropharyngeal abscess with secondary osteomyelitis and epidural abscess: proposed pathophysiological mechanism of an underrecognized complication of unstable craniocervical injuries: case report. Carlos R Goulart, Tobias A Mattei, Mariano E Fiore, William J Thoma, Ehud Mendel. J Neurosurg Spine. 2016 Jan;24(1):197-205. doi: 10.3171/2015.4.SPINE14952.
Surgical treatment of spondylodiscitis in the cervical spine: a minimum 2-year follow-up. Christoph E Heyde , Heinrich Boehm, Hesham E Saghir, Sven K Tschöke, Ralph Kayser. Eur Spine J. 2006 Sep;15(9):1380-7. doi: 10.1007/s00586-006-0191-z. Epub 2006 Jul 26.