




















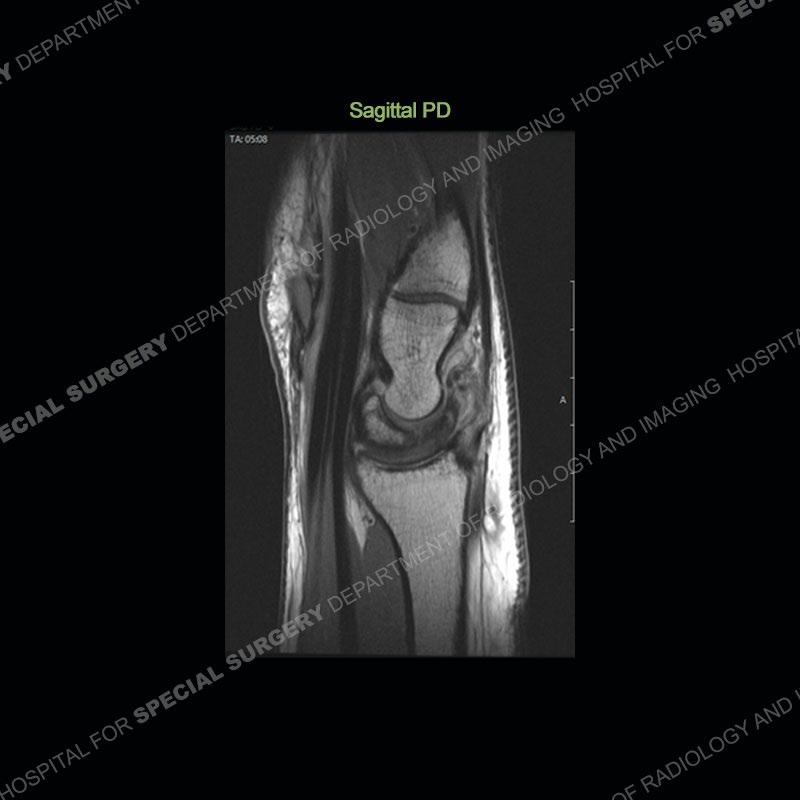























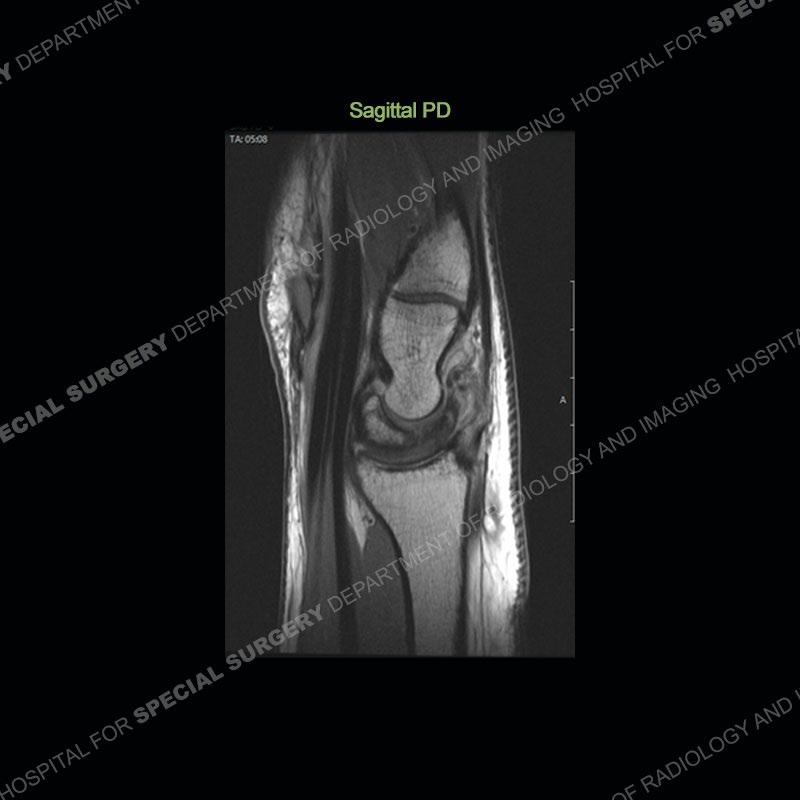

Both cases demonstrate similar findings to slightly less and more conspicuous degrees. The radiographs show sclerosis and fragmentation/collapse of the lunate. The CT images for case one just further clarify the architecture of the lunate. The MRI images show a slightly greater degree of variability but with overall persistent areas of low signal of the lunate on all pulse sequences and with a loss of the geometry of the lunate indicating collapse and fragmentation.






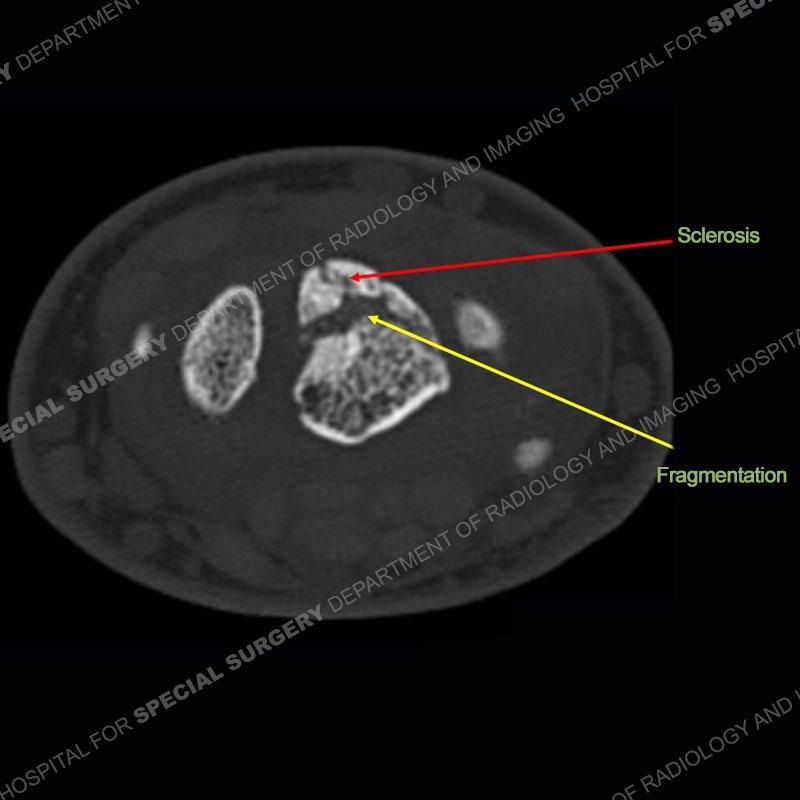


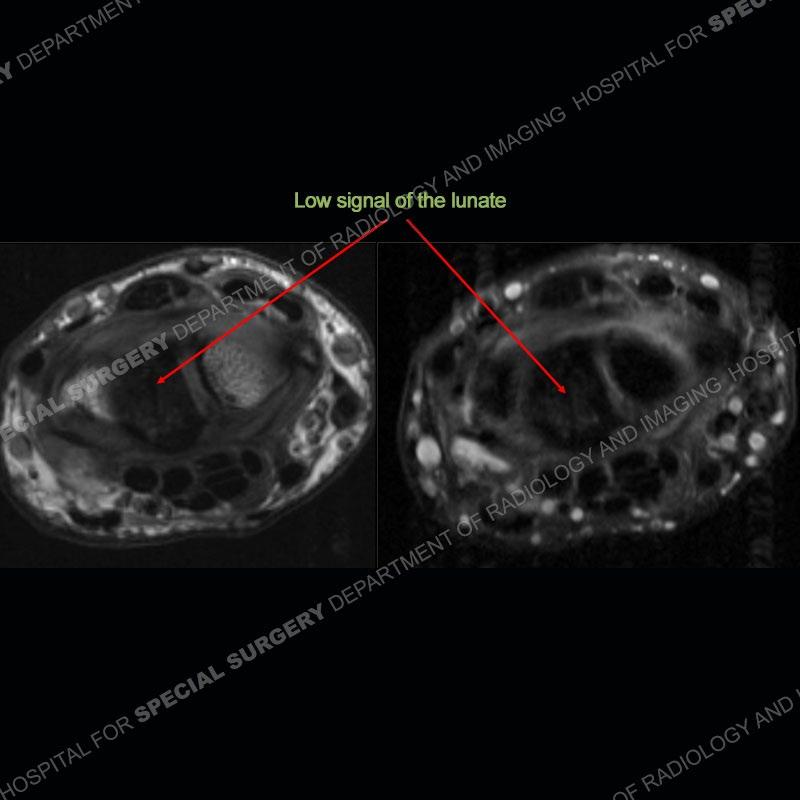




A well recognized but still poorly understood entity with necrosis and collapse representing the end stage of the pathology. The reasons for the necrosis are likely multifactorial and relate to the anatomy of the wrist inclusive of ulnar variance and the anatomy of the vasculature to the lunate. Other inflammatory, biological processes and overuse/trauma also likely play a role in the development of the necrosis. The disease manifests by sclerosis of the lunate followed by collapse and fragmentation. This is then followed by abnormal orientation of the scaphoid in a palmar flexed position and then adjacent arthritis. These latter processes were not the focus of this case presentation. The MRI will show areas of low signal on all pulse sequences indicating the areas of devitalized bone. The foci of slightly increased signal are in keeping with areas of maintained perfusion and highlight the variable architecture and findings of Kienbock’s. The fragmentation and collapse of the bone are seen well on both CT and MRI.

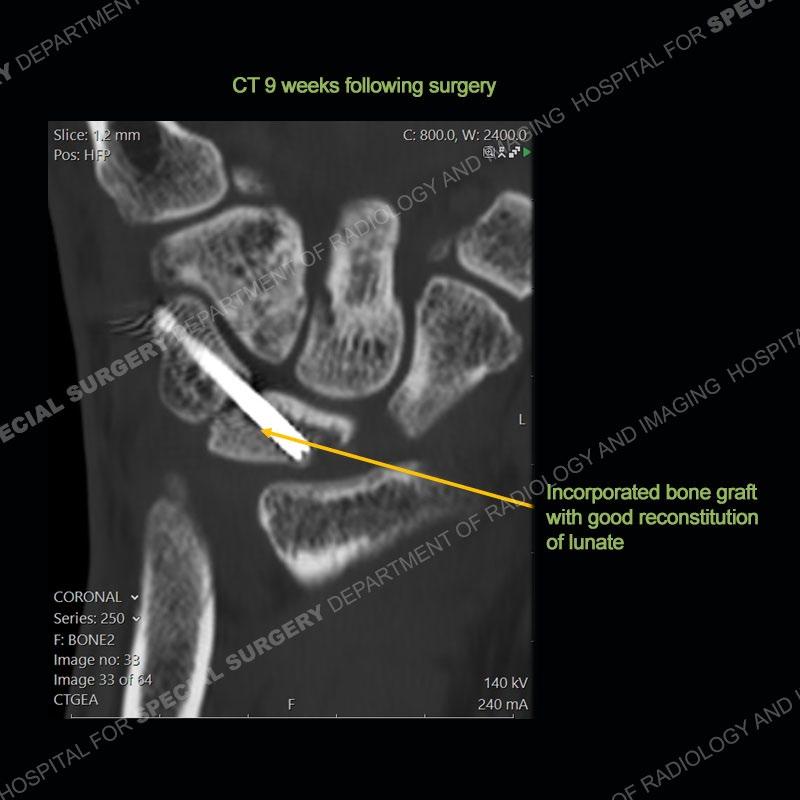
The treatment as the underlying cause of Kienbock’s remains somewhat elusive. Prior to collapse, osteotomies to decrease load or shearing forces to the lunate may be helpful. Once collapse and arthritis have been engendered, fusion and carpectomy have been performed. Now, the role for vascularized bone grafting is being investigated with long term results still being somewhat lacking. Given the young age of the second patient and lack of adjacent, advanced cartilage wear, a vascularized bone graft was performed. The area of necrotic bone was excised, a vascularized bone graft from the distal femur was harvested, and then using microsurgical technique it was grafted to the lunate. A temporary fixation was performed and once the graft was incorporated, the fixation hardware was removed. Although still early in the postoperative period, the patient is doing well.









Kienböck's disease in 2021. Emmanuel J Camus, Luc Van Overstraeten. Traumatol Surg Res. 2022 Feb;108(1S):103161. doi: 10.1016/j.otsr.2021.103161. Epub 2021 Nov 30.
The Lichtman classification for Kienböck's disease: An assessment of reliability. harles A. Goldfarb, MD, James Hsu, MD, Richard H. Gelberman, MD, Martin I. Boyer, MD DOI:https://doi.org/10.1053/jhsu.2003.50035.
VOLUME 28, ISSUE 1, P74-80, JANUARY 01, 2003
Kienböck's Disease. Nader Paksima DO, MPH and Angelo Canedo BA Journal of Hand Surgery, 2009-12-01, Volume 34, Issue 10, Pages 18861889, Copyright © 2009.
Kienbock's disease. F Schuind, S Eslami, P Ledoux. J Bone Joint Surg Br. 2008 Feb;90(2):133-9. doi: 10.1302/0301-620X.90B2.20112.