APRIL2023,`50
STRATEGY
Overcoming uncertainties in regulatorystatus of digital health in India

HR
Emerging career pathways for allied healthcare professionals

VOL.16 NO 3 PAGES 44





























Chairman of the Board
ViveckGoenka
Sr.Vice President-BPD
Neil Viegas
Vice President-BPD
Harit Mohanty
Editor
Viveka Roychowdhury*
Editorial Team
Lakshmipriya Nair
Kalyani Sharma
DESIGN
Art Director
Pravin Temble
Senior Designer
Rekha Bisht
Senior Artist
Rakesh Sharma
Marketing Team
Rajesh Bhatkal
Ashish Rampure
Debnarayan Dutta


Production Co-ordinator
DhananjayNidre
Scheduling & Coordination
Pushkar Waralikar
CIRCULATION
Mohan Varadkar
HEALTHCARE IT
MEDTECH
12
THE FUTURE OF REMOTE PATIENT MONITORING IN POST-PANDEMIC WORLD
13 THE FUTURE OF CHRONIC DISEASE MANAGEMENT WITH IOMT
21 ANEWERA OFINDIAN HEALTHCARE SECTOR
CONTENTS
ITin radiology: Setting the stage for better care

Investment and collaborative efforts from all stakeholders can further strengthen ITenabled radiology sector in India and bring positive change | P-14
PUBLIC HEALTH
22 IS ERADICATING SICKLE CELL DISEASE A POSSIBILITY?
STRATEGY
23 OVERCOMING UNCERTAINTIES IN REGULATORY STATUS OFDIGITAL HEALTH IN INDIA

HEALTHCARE TRENDS
24 TRANSASIA BIO-MEDICALS LAUNCHES ‘MADE IN INDIA’CLINICAL CHEMISTRY REAGENTS
HR
25 EMERGING CAREER PATHWAYS FOR ALLIED HEALTHCARE PROFESSIONALS
Express Healthcare® Regd.With RNI No.MAHENG/2007/22045.Postal Regd.No.MCS/162/2022 - 24.Printed and Published byVaidehi Thakar on behalf of The Indian Express (P) Limited and Printed at The Indian Express Press,Plot No.EL-208,TTC Industrial Area,Mahape,Navi Mumbai-400710 and Published at Mafatlal Centre,7th floor,Ramnath Goenka Marg,Nariman Point,Mumbai 400021.
Editor: Viveka Roychowdhury.* (Editorial & Administrative Offices: Mafatlal Centre,7th floor,Ramnath Goenka Marg,Nariman Point,Mumbai 400021)
* Responsible for selection of news under the PRB Act.Copyright © 2017.The Indian Express (P) Ltd.All rights reserved throughout the world. Reproduction in anymanner,electronic or otherwise,in whole or in part,without prior written permission is prohibited.
April 2023 EXPRESS HEALTHCARE 9
Is Rajasthan's RTH Bill the right template for India?
The signing of an MoU between the Rajasthan government, Indian Medical Association- Rajasthan, Private Hospital and Nursing Home Society (PHNHS) and United Private Clinics and Hospitals of Rajasthan (UPCHAR) takes the state one step closer to launching a Right to Health (RTH) Bill.
Or does it?
Once the eight-point MoU is applied, only 47 out of the state's 4100 private health facilities remain part of the Bill. Eleven of these 47 health facilities are private medical colleges, while 36 got land at concessional rates, two of the inclusion criteria of the MoU.
So, will citizens in Rajasthan be able to actually exercise their right to healthcare, if such a large proportion of private health facilities are not covered by the Act? Is the state confident that public health facilities will meet the demand and aspirations of their citizens for good quality healthcare?
And will this become the template RTH Bill and modus operandi followed by other state governments and hospital/ doctor associations? If yes, is Universal Healthcare (UHC) in Indian destined to remain a distant, or worse, a dysfunctional dream in India?
Doctors in the state from the private sector had launched protests after the Bill was introduced on March 21, hampering access to healthcare. Most, but not all, are expected to resume duty after the MoU. For now, the MoU resolves the stalemate and leaves the door open for more consultation between the government and representatives of the private healthcare sector, to find common ground.
What's the legal status so far? The RTH Bill was introduced and passed by both the houses of Rajasthan legislature unanimously. It is only after the Governor gives assent that the "Bill" will become an "Act". The governor has not given assent to this Bill.
Thus, it remains to be seen if these recommendations will be incorporated at the Bill stage, rather than as amendments after it becomes an Act. The former process will reduce chances of these amendments being challenged and overruled during the implementation process.
There is no doubt that Rajasthan's RTH Bill is a step in the right direction, even though the motivation and application appear to be flawed. With other state governments (especially those due for elections this year) in a wait-and-watch mode, it is imperative that all stakeholders re-examine the issues carefully and resolve them, in the true spirit of giving citizens a right to healthcare and building the infrastructure for a sustainable and equitable UHC system.

Legal experts are of the opinion that Rajasthan's RTH Bill, in its original form, was harsh on doctors, in the sense that they will not only have to admit and take care of an emergency patient without any payment but may also have to incur the additional cost of transporting the patient to another hospital. The Bill stated that this cost will be reimbursed, but there is no clarity on the amounts and timeline to reimbursement. There have been numerous well reported accounts of the frustrating experience of doctors and hospitals in other states, where similar schemes are in force (not as a right to health).
Post the MoU, the legal experts surmise that the main issue seems to have been resolved, as smaller hospitals who were at the forefront in opposing this Bill, have now been exempted from the provisions of this Bill. This would seem a logical exclusion, as most smaller hospitals and standalone clinics may not have the clinical specialists and hospital infrastructure to deal with all emer gencies. Neither do they have the financial reserves to wait for reimbursements from the government for treatment administered under such schemes.
Associations representing hospitals from the private sector, the Association of Healthcare Providers (India) (AHPI) and NATHEALTH, as well as private practitioners belonging to the Alliance of Doctors for Ethical Healthcare (ADEH), were wary of the many grey areas. While Dr Girdhar Gyani, Director General, AHPI welcomes the agreement, he points out thatthe hospitals which come under points 3.c and 3.d in the MoU (3.c refers to hospitals built on land acquired free or at concessional rates from the government, whereas 3.d refers to hospitals run by trusts) which remain covered by the Bill, will have to bear the full patient load as they provide the bulk of tertiary care and critical patients will find their way to such hospitals.
These hospitals contend that there is no clarity about the mode of payment and more importantly, about the rate at which reimbursement will be made for critical care procedures. AHPI's statement emphasises that this has been a perennial problem, even with present government schemes like Rajasthan's Chiranjeevi scheme, the difference being that participation in such schemes is optional but once the RTH Bill comes into play, it will become mandatory.
Stressing that AHPI also supports the concept of RTH, as long as it takes care of the financial sustainability of hospitals, the statement warns that financial sustainability will be a serious issue, impacting the survivability (of the hospitals) in the long run. The statement indicates that AHPI and IMA will work together to take up these issues with the government under the 8-point agreement.
If hospitals are worried about the financial implications of the RTH Bill, then doctors are concerned about being the target of violence by patients and their caregivers, as well as being sued for malpractice. While the ADEH welcomed the spirit in which the Rajasthan Government has brought the RTH Bill, it appealed (in a pre-MoU statement) to authorities to address the core issues which are nurturing the "deep unrest amongst private healthcare practitioners." On the financial side, ADEH hoped the state will also make the necessary budgetary allotment and back the bill with robust political will.
The ADEH had recommended that the Bill should also specify the nature of primary emergency treatment and requested that the clause which reserves the right of the government to add more emergencies as and when needed; should be nuanced by the addition of the phrase – ‘after consulting doctors’ organisations. Lastly, the ADEH had suggested a robust accountability mechanism in the rules whereby along with doctors, the government officials would also be made accountable, as a robust grievance redressal system for both patients and doctors is necessary for success.
The NATHEALTH statement before the MoU was signed, points out that UHC has never been achieved anywhere in the world "where the private sector fears that public good will be delivered at private cost".Dr. Ashutosh Raghuvanshi, President, NATHEALTHhad therefore requested the Rajasthan Government to put this Bill on abeyance till a consensus is achieved and an operational framework is established.
While a perfect RTH Bill/Act might be a Utopia, Rajasthan's experience has many learnings. The reactions and recommendations from associations show that any RTH regulation needs to balance the interests of healthcare users (patients) and providers (hospitals, both private and government). And it will need a consultative, transparent approach, a meeting of minds or at least finding common ground, to start the process and put a framework in place.
viveka.roy3@gmail.com
EDITOR’S NOTE EXPRESS HEALTHCARE April 2023 10
VIVEKA ROYCHOWDHURY Editor viveka.r@expressindia.com
While a perfect RTH/UHC Bill might be a Utopia,all stakeholders should learn from Rajasthan's experience

HEALTHCARE IT
The future of remote patient monitoring in post-pandemic world

Management Services
The COVID-19 pandemic elevated the healthcare sector to a high-priority, front-line industry, creating an urgent need to boost productivity and efficiency while adapting to the new needs of a worldwide health crisis. Subsequently, the acceleration of digital transformation emerged as a key trend, with the shift from contact-based to virtual care necessitating the growth of telemedicine and remote patient monitoring. However, telehealth and RPM are not just pandemic trends but are predicted to grow and evolve in the post-pandemic world.
Post-pandemic shifts in healthcare
The pandemic turned out to be a reality check for the healthcare sector, especially regarding overall readiness. We realised that while we had contingency systems in place for times of crisis, they would need to be made more resilient to pressure. As a result, the post-pandemic healthcare ecosystem has witnessed a significant pivot, with a high emphasis on preventive healthcare, remote care and digital transformation.
Concerning telehealth, a perception shift is visible across the board. Today, it has been incorporated into the mainstream healthcare value chain as a tool to consult for common and chronic conditions. This has dramatically helped address capacity and infrastructure challenges in remote monitoring and patient management, especially in long-term care. In addition, the emergence of processes like smartphone-enabled monitoring of adherence to care recommendations has greatly helped improve the quality of care and the overall patient experience.
The pandemic forced almost every sector to embrace remote working, and the healthcare sector was no exception. Telenursing emerged as a key trend, with tech-driven remote services and virtual nurses quickly gaining popularity. In addition, phone services and video conferencing are increasingly being adopted as tools to check up on patients from afar.
The pandemic also resulted in an increased emphasis on the importance of improving disease surveillance and prediction models. Big data, predictive analysis and artificial intelligence are key drivers for ensuring the sector's preparedness for future healthcare crises. AI-enabled predictive capabilities also enable providers to identify patients at the highest risk, take proactive
steps to mitigate risk and ensure the best preventive quality of care. In addition, machine learning tools enable healthcare providers to convert data into actionable insights in realtime, automate manual tasks and streamline processes.
The evolution of RPM RPM, a subset of telehealth, involves utilising digital tools to track and document a range of health parameters, analyse the data, and transfer the same to healthcare providers for accurate assessment and decision making. This reduces hospitalisation, improving the patient's quality of life while lowering capacity challenges for providers.
Although RPM is not a new concept, the emergence of digital technologies has undoubtedly given it a new form. The earliest forms of RPM involved landline phones, telephone calls and telecommunicated examinations. In the era of digital medicine, this has evolved into sophisticated and easily accessible systems and devices to track various parameters and chronic health conditions, such as glucose monitoring, cardiac monitoring, pain levels and management, pill tracking, mental health and many others. Mobile RPM (or mRPM) has emerged as a key trend, with apps prompting patients to input essential details and providers receiving alerts if key parameters deteriorate. Use cases of RPM have also involved the discharge of patients into 'virtual wards', enabling post-discharge monitoring and quick identification of the need for re-hospitalisation.
The future of RPM
The pandemic greatly accelerates the uptake of RPM in healthcare - a trend that is sure to witness an upward
trajectory in the post-pandemic world. The global RPM market has been predicted to reach 117.1 billion by 2025, with a quintuple increase since 2020. Automation is tailoring the future of work across sectors, and technologies like AI and ML also drive this shift in the healthcare sector. With the rise in adoption, the data from telehealth systems would also have to be integrated into patient health records for a seamless patient-provider engagement.
The future of RPM is likely to involve using predictive and prescriptive tools to deliver accurate and high-quality care to patients and empower them with the tools for proactive and preventive healthcare management. Today, we are also grappling with a healthcare access gap in rural and difficultto-reach areas, and RPM holds the potential to bridge this gap as well.
As digital technologies become more accessible and mainstream, the adoption of RPM will only increase. This will reduce challenges such as administrative costs, staffing shortages and disease communicability for providers while improving ease of access, convenience and quality of patient care. We are also seeing increasing acceptance of RPM among patients, with a survey by MSI International revealing that four in five consumers favour remote patient monitoring, especially for managing chronic conditions.
Overall, we are seeing a shift from a reactive to a proactive and predictive care system, driven by the intelligent use of digital tools to enhance care and improve the sector's resilience. RPM will abide to grow and evolve in line with the same.
EXPRESS HEALTHCARE April 2023 12
Priyank Chandra,Vice President-Strategic Solutions,Omega Healthcare
stresses that telehealth and Remote Patient Monitoring (RPM) are not just pandemic trends but are predicted to grow and evolve in the post-pandemic world
The pandemic forced almost every sector to embrace remote working,and the healthcare sector was no exception. Telenursing emerged as a key trend,with tech-driven remote services and virtual nurses quickly gaining popularity.In addition, phone services and video conferencing are increasingly being adopted as tools to check up on patients from afar
The future of chronic disease management with IoMT
Chronic diseases are a growing concern in India, with an estimated 61 per cent of all deaths being attributed to them. The management of chronic diseases can be complex and expensive, which is why healthcare providers in India are constantly exploring new technologies to make the process more efficient and effective. One of the most promising of these technologies is the Internet of Medical Things (IoMT).
Before we go ahead, let’s delve deeper on the topic of chronic diseases. Chronic diseases are long-term conditions that typically progress slowly over time and these conditions can affect various parts of the body and can cause a range of symptoms and complications that can significantly impact a person’s quality of life.
Some common examples of chronic diseases include diabetes, heart disease, arthritis, Chronic Obstructive Pulmonary Disease (COPD) and cancer. These conditions can develop due to a range of factors, including genetics, lifestyle choices, and environmental factors.
Chronic diseases can often be managed with a combination of supplementation, lifestyle changes, and ongoing medical care. Regular medical care is also important for managing chronic diseases, as healthcare providers can monitor symptoms and adjust treatment plans as needed.
Overall, managing chronic diseases requires a holistic approach that addresses the physical, emotional, and social aspects of the condition. With ongoing care and support, many people with chronic diseases are able to lead fulfilling and healthy lives.
What is IoMT?
IoMT refers to the network of medical devices, sensors, and software that can connect to the internet and transmit data in
real-time. These devices are designed to collect data on patients’ vital signs, health behaviours, and medication adherence, among other things. IoMT devices can be integrated with electronic health records (EHRs) and other clinical systems to enable providers to access real-time data on patients’ health.
Examples of IoMTdevices
There are several types of IoMT devices that are being used for chronic disease management in India. Some of these include:
◆ Continuous Glucose Monitoring (CGM) systems: CGM systems are IoMT-enabled devices that are used by people with diabetes to continuously monitor their blood glucose levels. These devices provide realtime data on glucose levels, allowing patients to make informed decisions about their diet, exercise, and medication use. Some CGM systems can also transmit data directly to healthcare providers, allowing for more efficient management of the condition.
◆ Remote monitoring systems for cardiac patients: These systems use IoMT devices to re-
motely monitor patients with heart disease and other cardiac conditions. Patients can wear devices that monitor their heart rate, rhythm, and other important metrics, and healthcare providers can use this data to identify potential complications and adjust treatment plans as needed.
◆ Smart pill dispensers: These devices can be used to manage medications for people with chronic diseases, such as dementia and Parkinson’s disease. The devices can remind patients to take their medications at the appropriate times and can alert healthcare providers if medications are not taken as prescribed.
◆ Mobile apps for asthma management: There are a variety of IoMT-enabled mobile apps that can be used to manage asthma symptoms. These apps can track medication use, monitor symptoms, and provide personalized feedback and recommendations for patients.
◆ Remote patient monitoring: IoMT devices can be used for remote patient monitoring to keep track of patients with chronic diseases who live in remote areas or who have limited access to healthcare services.
◆ Population health management: IoMT devices can be used for population health management to identify patients with chronic diseases who are at higher risk of complications and intervene with preventative measures. For example, a healthcare provider may use a remote monitoring system to track patients with heart disease and intervene if their blood pressure readings become too high. By using IoMT devices to monitor patients’ health status and provide preventative interventions, healthcare providers can help reduce the overall cost of care and improve patient outcomes.
◆ Clinical trials: IoMT devices can be used in clinical trials for chronic diseases to collect realtime data on patients’ health status and medication adherence. For example, a researcher may use a smart pill dispenser to track patients’ medication adherence in a clinical trial for a new treatment for Parkinson’s disease. By using IoMT devices to collect data in clinical trials, researchers can gain a better understanding of how different interventions affect patients with chronic diseases and identify potential new treatments.
◆ Workplace wellness programs: Employers can use IoMT devices as part of workplace wellness programs to help employees manage chronic diseases and improve their overall health. For example, an employer may offer employees with diabetes a CGM system to help them better manage their condition. By providing IoMT devices as part of a wellness program, employers can help reduce absenteeism and improve productivity in the workplace.
◆ Smart rings: Smart rings are wearable devices that can track a range of health metrics, including heart rate, sleep patterns, and physical activity levels. Some smart rings, such as the Bonatra ring, have been shown to be

effective in monitoring symptoms of chronic diseases, such as heart disease and diabetes.
Overall, IoMT devices can be powerful tools for managing chronic diseases in a variety of B2B scenarios. By providing real-time data on health metrics, these devices can help healthcare providers, researchers, and employers make informed decisions about patient care and employee health
Benefits for healthcare providers
IoMT devices have several benefits for healthcare providers in India. Firstly, they provide healthcare providers with real-time data on patients’ health, allowing them to intervene early and prevent complications. Secondly, IoMT devices can reduce the number of hospitalisations and emergency room visits, which can help reduce healthcare costs. Finally, IoMT devices can improve patient outcomes by providing healthcare providers with a more complete picture of the patient’s health.
Conclusion
The use of IoMT devices for chronic disease management is a promising development in healthcare in India. By enabling healthcare providers to monitor patients remotely and intervene, when necessary, IoMT devices have the potential to improve patient outcomes and reduce healthcare costs. However, there are also challenges associated with the adoption of IoMT, such as data security and privacy concerns and the need for healthcare providers to be trained on how to use and interpret the data generated by IoMT. Nevertheless, as the technology continues to evolve, we can expect to see more widespread adoption and integration of IoMT into healthcare delivery systems in India, ultimately transforming the way we manage chronic diseases in the country.
April 2023 EXPRESS HEALTHCARE 13
Rahul Kishore Singh,CEO and Co-Founder,Bonatra emphasises that the management of chronic diseases can be complex and expensive,which is why healthcare providers in India are constantly exploring new technologies to make the process more efficient and effective.One of the most promising of these technologies is the IoMT
Investment and collaborative efforts from all stakeholders can further strengthen IT enabled radiology sector in India and bring positive change






 ByKalyani Sharma
ByKalyani Sharma
EXPRESS HEALTHCARE April 2023 14
)
cover

April 2023 EXPRESS HEALTHCARE 15
Information Technology (IT) has the potential to revolutionise healthcare delivery in India, especially in the field of radiology. It is a crucial diagnostic tool in modern healthcare, and the use of IT can improve the accuracy and efficiency of radiology procedures.
Overall, the use of IT in radiology can help improve the quality and accessibility of healthcare in India, especially in remote or underserved areas. By adopting these technologies, healthcare providers can improve patient outcomes, reduce costs, and improve overall healthcare delivery in India.
Emphasising on the role IT in radiology, Peeyush Kaushik, VP and Head, Healthcare Innovation Centre, Philips said, “As patients become increasingly interested in actively monitoring and managing their health, and healthcare organisations focus on providing new services to facilitate this process, the role of the radiologist is being revolutionised. Medical imaging is now used not only for diagnosis, but also for treatment and communication, and radiologists must utilise information technology to manage workflow, image collections, processing, treatment, and communication across multiple stakeholders, including patients, surgeons, and hospital staff. With the increasing workload, IT utilisation can help radiologists optimise workflow, simplify procedures, and monitor work processes.”
DrSunitaDube, Founder, MedscapeIndia comments, “IT and radiology go hand-in-hand. Since the emergence of IT within radiology, new imaging techniques are dependent on computers to generate images of one’s internal structures organs for a prompt diagnosis and treatment and it is commonly termed as digital images. Although both IT and radiology tend to appear as one entity at the beginning, they are actually two different within healthcare that have been combined together to meet the increasing demands of the healthcare sector. As such, IT within radiology includes x-rays, Ultrasound,
With the increasing workload,ITutilisation can help radiologists optimise workflow,simplify procedures,and monitor work processes
Peeyush Kaushik VPand Head, Healthcare Innovation Centre, Philips

Teleradiology has grown in demand globally given that it provides a rapid reliable response to medical crisis situations amid pandemic-induced constraints and emergencies
Dr Arjun Kalyanpur Chief Radiologist & Founder CEO, Teleradiology Solutions

Although both ITand radiology tend to appear as one entity at the beginning, they are actually two different within healthcare that have been combined together to meet the increasing demands of the healthcare sector
Dr Sunita Dube Founder, MedscapeIndia

Digital transformation has helped many industries and healthcare is not untouched with this,but there is a lot of opportunity to do more to take benefits of automation,artificial intelligence and improved process and regulatory compliances
Rajaneesh Kini SVP& Chief Technology Officer, Cyient

Computerised Tomography, Magnetic Resonance Imaging, Positron Emission Tomography, SPECT scans, Bone Density, and even Interventional Radiology among others. But we still need advancements in healthcare with the help of technology.”
Market size
According to a report by MarketsandMarkets, the Indian healthcare IT market is expected to grow from USD 1.45 billion in 2018 to USD 2.39 billion by 2023, at a compound annual growth rate (CAGR) of 10.4 per cent. The report further highlights the significant role of IT in radiology, such as Picture Archiving and Communication Systems (PACS) and Radiology Information Systems (RIS), in improving patient care and operational efficiency.
Another report by Research and Markets estimates that the Indian PACS market is expected to reach USD 79.4 million by 2024, growing at a CAGR of 6.4 per cent from 2019 to 2024. The report suggests that the growing adoption of digital imaging systems and the increasing demand for better healthcare infrastructure are driving the growth of the PACS market in India.
Overall, the market for IT in radiology in India is expected to grow at a significant pace in the coming years, driven by factors such as increasing demand for healthcare services, advancements in technology, and government initiatives to improve healthcare infrastructure.
Emphasising on the teleradiology market, Dr Arjun Kalyanpur, Chief Radiologist & Founder CEO, Teleradiology Solutions said, “Teleradiology has grown in demand globally given that it provides a rapid reliable response to medical crisis situations amid pandemic-induced constraints and emergencies. Currently, the global market stands at an estimated US$3.5 billion with the US holding around US$1.2 billion while EU/LATAM & Africa together account for US$1.8 billion, and APAC around US$0.5 billion. In India, the market has rapidly expanded due to joint X-Ray and
EXPRESS HEALTHCARE April 2023 16
cover )
PPP projects proposed by NHM-State governments for various high-end modalities. Industry experts predict that pure-play teleradiology services will account for Rs 300-500 crore in the next five years. Several states and regions are acknowledging the need for telereporting capabilities including parts of Northeast, Jharkhand, West Bengal, and Rajasthan for including the underserved segments.”
“These positive market projections are also owing to inherent challenges. India has seen a spurt in multi-speciality medical and diagnostics centres. However, there is a shortage of qualified staff with the right interpretative coverage and speciality expertise. Currently, India with an estimated 1.4 billion people has only 20,000 or so radiologists whereas the US has a much smaller population but has at least 100,000 radiologists. Experts recognise the urgent need to increase training spots to fill this skills gap and meet the spiralling need for timely diagnostic information”, he added.
Current trends
Over the past century, Radiology has evolved from a purely diagnostic tool to an interventional technology that actively participates in patient treatment. The adoption of digital imaging, PACS, cloud-based solutions, AI-enabled diagnosis, and EHRs has improved the quality, speed, and accuracy of medical imaging, making it more accessible to patients across the country.
Radiology is a crucial diagnostic tool in modern healthcare, and the use of IT can improve the accuracy and efficiency of radiology procedures.
Here are some ways in which IT can set the stage for better care in radiology in India:
◆ Electronic Medical Records (EMRs): EMRs can be used to store and access patient data, including radiology reports, images, and other relevant information. This can help healthcare providers make more informed decisions, reduce errors, and improve patient outcomes.
◆ Digital imaging: The shift
from analog to digital imaging has greatly improved the quality, speed, and accuracy of medical imaging. Digital imaging allows
for easy storage, retrieval, and sharing of images between healthcare providers, reducing the need for physical film and

increasing efficiency.
◆ PACS: It is a system used to store, retrieve, distribute, and display medical images. This
system can be used to streamline radiology procedures, improve the accuracy of diagnoses, and reduce waiting
April 2023 EXPRESS HEALTHCARE 17
times for patients.
◆ RIS: RIS is a software system that manages radiology workflow, including patient scheduling, image acquisition, and reporting. RIS enables healthcare providers to manage patient information, track appointments, and generate reports quickly and accurately.
Rajaneesh Kini, SVP & Chief Technology Officer, Cyient expresses that digital transformation has helped many industries and healthcare is not untouched with this, but there is a lot of opportunity to do more to take benefits of automation, Artificial Intelligence (AI) and improved process and regulatory compliances. He added, “As industry 4.0 has helped industries to get benefitted due to connectivity, aggregation of all data on a single platform and then driving business value and bring efficiencies in the system, similarly connected healthcare can bring the data and aggregate on a single platform by integrating various components of Healthcare Information System (HIS) such as patient health recordEHR, RIS, PACS, and Laboratory Information Management System and (LIMS).”
With support coming from different IT tools, modern-day systems allow access to images and reports via email, thirdparty standalone systems, or systems linked to the facility's archive/storage. Most are cloud or web-based and easily accessible from anywhere.
Giving an overview of the PACS, RIS and HIS, Dr Gaurav Malhotra, Sr. Consultant- Radiology, Sri Balaji Action Medical Institute, New Delhi added, “HIS and RIS have revolutionised the field by increasing productivity and efficiency. The HIS and RIS are networked software systems that manage medical imagery and related data, including tracking radiology imaging orders and billing details. PACS is yet another tool from IT which is used widely now. In conjunction with PACS, HIS and RIS manage image archives, record-keeping, and billing. PACS provides electronic storage, retrieval, distribution, and presentation of
PACS has brought a revolutionary transformation in the handling of digital radiology images,allowing clinicians in different locations and settings to easily access and view them,thus improving operational efficiency
Dr Gaurav Malhotra Sr.Consultant- Radiology, Sri Balaji Action Medical Institute
With technological advancements driving its growth in India,radiology is a rapidly evolving field.In recent years,AI and MI have profoundly found their way into many sectors of healthcare including radiology
Dr Aakaar Kapoor Medical Advisor and Chief Radiologist, City Xray & Scan Clinic



AI has begun transforming the way radiology is practiced today.AI algorithms can help radiologists interpret medical images more accurately and efficiently,improving diagnostic accuracy and reducing diagnostic errors as well amplifying the productivity of radiologists and clinicians in turn improving access
Amit Gandhi Chief Business Officer, Deeptek
images. Modern day digital imaging and communications in medicine (DICOM) is a data interchange protocol, digital image format and file structure for biomedical images and images related information. DICOM alongwith PACS increase productivity, save time compared to analog readings, reduce errors, and cut costs.”
“With digitisation in imaging,
the flow of data is seamless and wireless. For example, diagnostic imaging can now be reported wirelessly, without the discomfort of cords. With the webbased applications, there is no requirements for any kind setup/exe in any of the end user desktop / laptop which eliminates system configuration dependency. With latest PACS there is zero footprint viewing
and easy end user viewer interface. PACS has brought a revolutionary transformation in the handling of digital radiology images, allowing clinicians in different locations and settings to easily access and view them, thus improving operational efficiency. These digital DICOM images offer improved dynamic range and contrast, with exclusive 3D software, enabling
accurate diagnosis. The latest PACS systems are stable and provide high degree of security/privacy”, he added.
In terms of economic viability, the PACS is a definite solution for smooth workflow of any medical facility along with DICOM, HIS and RIS.
Dr Dube believes that PACS still needs improvement. She said that while using PACS, it is traditionally an X-ray tech consisting of advanced training in order to handle and maintain the server on a daily basis. But, doing so can invite issues with the IT department. When dealing with the IT department and the radiology department, both departments will consider each other as competition when it comes to who is able to handle the monitoring and tracking of information through the PACS server.
◆ Telemedicine and teleradiology: The use of telemedicine and teleradiology has seen tremendous growth as they have made it easier for radiologists to access medical images and reports remotely. This has been particularly beneficial for rural areas, where access to radiologists is limited. Telemedicine and teleradiology have enabled radiologists to provide expert consultations to patients and healthcare providers in remote locations, facilitating more timely and accurate diagnoses.
Highlighting the benefits of teleradiology, Dr Kalyanpur said, “Teleradiology applications in consultation, monitoring, and diagnostics enable radiologists in their daily tasks through online solutions and real-time analyses accessible via global cloud networks, such as TeleradTech’s Radspa workflow. These services can have a huge impact on India’s population which is largely rural with l imited access to accurate, quality healthcare and diagnostic services.”
“A case in point is the joint efforts for early diagnosis and better healthcare outcomes in rural parts of northeast Indian regions. We partnered with 26 Community Healthcare Centres, District, and Sub-district
EXPRESS HEALTHCARE April 2023 18
cover )
hospitals in Tripura to facilitate sharing of digital imaging and communications in medicinebased radiographs of patients of all ages/study groups from their sites via a cloud-based Radiology Information System and Picture Archiving and Communication System (RIS-PACS). Expert radiologists at a Teleradiology reporting hub in Bangalore could access these for interpretation at shorter turnaround times. Between 2018-2-12, 78622 studies were interpreted via Teleradiology. As a result, patients could consult their physician with their test reports on the same day and could benefit from optimal care during the same visit. Besides these improvements, Teleradiology leads to numerous other benefits such as reduced cost, and faster diagnosis while reducing the burden of limited staff and addressing the shortage of proficient radiologists. Turnaround times (total time elapsed from ordering imaging exam to) report interpretation) are critical in today’s scenario, and these are efficiently addressed by Teleradiology.”
◆ AI: It can be used to analyse radiology images and assist healthcare providers in making more accurate diagnoses. AI can also be used to identify patterns in patient data and predict outcomes, which can help improve treatment planning and patient care.
Explaining the role of AI in radiology, Dr Aakaar Kapoor, Medical Advisor and Chief Radiologist, City Xray & Scan Clinic said, “With technological advancements driving its growth in India, radiology is a rapidly evolving field. In recent years, AI and MI have profoundly found their way into many sectors of healthcare including radiology. With the exponential increase in data generated by medical imaging, these technologies have been instrumental in facilitating more efficient and accurate analysis of medical images. AI can empower radiology in numerous ways such as image quality improvement and monitoring, scan reading and image interpretation. Additionally, AI
and ML algorithms have helped immensely in automating tasks, such as image segmentation, lesion detection, and feature extraction, that were previously performed manually. This has significantly reduced the workload of radiologists and allowed them to focus on more complex cases.”
AmitGandhi, Chief Business Officer, Deeptek also believes, “AI has begun transforming the way radiology is practiced today. AI algorithms can help radiologists interpret medical images more accurately and efficiently, improving diagnostic accuracy and reducing diagnostic errors as well amplifying the productivity of radiologists and clinicians in turn improving access. For instance, AI can be used to identify early-stage cancers that may be missed by human eyes. Additionally, AI can also assist in the triage of patients by prioritising imaging studies based on the severity of their condition. The deployment of AI in radiology has also resulted in significant cost savings and improved patient outcomes.”
Overall, the use of IT in radiology can help improve the quality and accessibility of healthcare in India, especially in remote or underserved areas. By adopting these technologies, healthcare providers can improve patient outcomes, reduce costs, and improve overall healthcare delivery in India.
Kaushik says that while many new technologies have emerged, AI has made significant strides in the past 5-6 years and is essential for addressing the challenges that radiologists face, including overload, fewer resources, and complexity involved in multi-disciplinary treatments. AI will not replace radiologists but will complement them to do their job more effectively and efficiently based on new demands, such as minimal invasive treatments, time optimisation, low radiology dose to patients, and cost reduction.
Areas that still needs to be explored in this segment
Experts believes that automated
workflow, connectivity and interoperability supported by cloudbased operations and more focus on enhancing the role of AI will help physicians in delivering better patient care.
Kini suggests that we may look at each segment and suggest how to use latest technologies to improve the efficiency and efficacy of the sub system. This is achieved by improving modules and operation at various stages. Some of the options are as below-
❑ Patient record: Automated patient record from extracting the summary of patient and doctor communication, reading the data from imaging obtained from scanners and pathology slides, and then merging with existing patient records.
❑ Scheduling: Automated patient scheduling, and appointment booking based on the queue of patient at each stage of the workflow, will improve the efficiency and patient’s user experience of the services.
❑ Acquisition: Efficiency and efficacy is improved using automated execution, dose reduction, scan time reduction on the imaging instrument.
❑ Processing: AI based algorithms are helping in improving the post processing, and registration processes, thanks to high performance computing platforms supported by high processing Graphical Processing Units (GPUs). Algorithms improve the efficiencies in segmentation, detection of various conditions and also quantification. This improves overall clinical decision making and reach to more accurate inference.
❑ Reporting and reliable communication: Reporting generation and documentation in custom format and template and Result communication and storage of patient information in secure way is achieved using secure by design, implementing security from end to end, device to storage.
According to Gandhi AI is poised to play a significant role in improving productivity by taking on non-clinical work and reducing the burden of interactions with clinicians. He thinks
that this will be particularly important in addressing the shortage of radiologists, a problem that is unlikely to be solved by traditional means. By automating low-end work and enhancing decision-making at the high end, AI will enable physicians to focus on delivering better patient care. However, the widespread use of AI also raises important ethical and responsible practice considerations. AI is a complex technology that can introduce errors, unintended biases, and discrimination in its results. To address these concerns, governments and organisations are developing universal sets of principles to guide the ethical and societal implications of emerging AI technologies.
ITadaption in radiology: Gaps and challenges
While there are many potential benefits to using IT in radiology in India, there are also several challenges that need to be addressed like interoperability which in radiology is important because medical images and data need to be shared between different healthcare providers. However, many IT systems used in radiology are not interoperable, which can lead to delays, errors, and inefficiencies.
Data security is another major challenge. Medical images and patient data are sensitive and need to be secured to protect patient privacy. However, there are concerns about the security of medical images and data stored in the cloud, which can be vulnerable to cyber-attacks and data breaches.
On this, Dr Dube mentions that, “IT and radiology are not always perfect and can fail to give the desired results. Hence, computerisation includes the loss of confidentiality and illicit disclosure of information due to unofficial access by medical personnel. The regulations are formed to protect medical records and other individually identifiable health information even communicated electronically, orally, or on paper. But sometimes it is easy to gather information about any patient violating privacy. IT and Radiology
must also implement additional safety mechanisms to protect all information transmitted within the Radiology department.”
Standardisation is also important in radiology because it enables healthcare providers to compare and interpret medical images and data consistently. However, there are still no universal standards for image and data formatting in radiology, which can lead to inconsistencies and errors.
Access to IT infrastructure is still a challenge especially in rural and underserved areas. Healthcare providers in these areas may not have access to the IT infrastructure necessary to support digital imaging, PACS, and other IT systems used in radiology.
It is important for the future radiology workforce to expand and strengthen their skills in line with the need and upgradation of the technology in this sector.
Commenting on this, Dr Kapoor says, “Interventions of IT in radiology have significantly changed the functioning of radiologists, particularly AI has reshaped the way radiologists work. However, lack of adequate training and a systematic flow of information always pose challenges for radiologists while adapting to IT and its advances, reforming the traditional working environment. It is crucial to provide intense training before putting radiologists to use new technologies. There should be a proper demonstration of new technologies being implemented so that radiologists have indepth knowledge about them. Another challenge that radiologists face during the process of adapting to IT is that they find it difficult to entirely rely on technology such as AI for results interpretation. In that matter, such technologies should be introduced first as a pilot to radiologists so that they become familiar with the technologies and are able to identify which part of the technology is producing false outcomes.”
Kaushik stresses that, “IT can help radiologists communicate findings more effectively through integrated imaging and
April 2023 EXPRESS HEALTHCARE 19
latest software tools to present patient data in a simple, pictorial, structured, multimedia, and personalised report. As the healthcare industry moves towards a patient-centric model of care, real-time data will be critical for both clinical and patient needs, but technical training will play a crucial role in bridging the gap between traditional hospital settings and the adoption of new technologies. Proper training is necessary to equip radiologists with the latest technological tools and their usage."
According to Gandhi, trust and relevance in terms of using AI in radiology are also a challenge. He explains that, one
major challenge is trust, which refers to the ability of clinicians, radiologists, and the medical community to hold AI accountable for its outcomes while using it in its complete form. As AI is not easily explainable to the medical community, it can be difficult to trust its accuracy and fairness. AI is often perceived as a ‘black box’ wherein the workings and decision-making processes of a model remain hidden, and, therefore, untrustworthy. However, this does not need to be the case. Transparency in AI allows us to describe, analyse, and communicate the ins and outs of a model in a way that is comprehensible to the public.
In the healthcare sector, the implications of not having responsible AI frameworks are heightened, particularly in terms of user safety and security. AI systems should undergo proper risk assessments at each stage of development to minimise potential negative impacts along the way and ultimately provide reliable results.
Unforeseen conditions and problems should be considered such that a model is able to safely deal with the consequences and adapt to new settings without negatively impacting its users. Furthermore, data and models can behave differently based on ethnicity and can have biases in their training,
which can affect their trustworthiness. These issues make it challenging for the medical community to accept AI and its outcomes.
“The other major challenge is relevance. Creating an AI model takes a lot of effort, from regulation processes to building data processes and algorithms. While many AI models are available in the market for different pathologies and modalities, clinicians need multiple AI models in their workflow to make it relevant. One AI model alone cannot change their workflow. Thus, there is a need for a seamless integration of multiple AI models to make them
more relevant in decisionmaking processes”, he added.
Wayforward
IT in partnership with radiology is already bringing a positive change in the healthcare sector. As advancements in the field of radiology continue, both IT and radiologists will both find themselves changing roles, tasks, and duties, and they will need to keep up to date with such changes. It is the need of the hour that both IT and radiology come together and function as one entity for outcomes when it comes to the healthcare sector.
Kalyani.sharma@expressindia.com journokalyani@gmail.com

EXPRESS HEALTHCARE April 2023 20 cover )
Anewera of Indian healthcare sector
Himanshu Baid,Managing Director,Poly Medicure Ltd stresses that with increase in technological advancements and growing importance of data,medtech companies should consider partnering with consumer-focused technology and specialised digital health companies to stay up to date

The global medical devices market is projected to grow from $495 billion in 2022 to $718.92 billion by 2029 at a CAGR of 5.5 per cent. India is the 4th largest market of medical devices in Asia. During the COVID-19 pandemic, the Indian medical devices sector’s contribution became more visible with the production of medical devices and diagnostic equipment such as ventilators, RT-PCR kits, IR thermometers, PPE kits, and N-95 masks.
Enabling policies like PLI, export incentives, R&D support are some measures taken by the Indian Government to boost the medical device industry.The government is planning to further boost India’s strengths of skilled manpower, and ease of business through its industry-friendly rules. According to the government’s draft policy, import dependence on medical devices will be halved in the next 10 years.
Through the government’s flagship Make in India initiative, the medical devices industry is getting support in terms of investment, innovation, skill, and infrastructure under the new manufacturing policy that seeks to boost the contribution of manufacturing to the GDP from 16 per cent in 2013 to 25 per cent in 2025.
The future of healthcare sector will be shaped by technology. Better telecom connectivity, easy availability of home diagnostic devices, increasing comfort with teleconsultation will pivot primary care towards a digital mode. eSanjeevani, a national tele-medicine service, clocked around 80 million tele-consultations till December 2022. In less than 3 years, it has become the world’s largest
government-owned tele-medicine platform. India’s Digital Health Mission will enhance adoption of electronic health records and enable availability of vital data in digitised form which will assist doctors access patient records and help in early as well as accurate diagnosis.
With the increasing focus on preventive health after the pandemic, there has been an emergence of disruptive models from health-tech start-ups.
The Internet of Things (IoT), in conjunction with tele-medicine, has created a new Internet of Medical Things (IoMT), which will play a critical role in monitoring and preventing illnesses. AI-driven analytics, tools and machines can help healthcare providers find the right approach for each patient with more efficient, precise, and impactful interventions.
In the next few years, the healthcare space is also likely
to be impacted by 5G, which has already been rolled out in some parts of India. 5G can minimise the time, cost and effort involved in R&D trials by ensuring the seamless flow of information from the patient to the provider and then on to research labs.
With this increase in technological advancements and growing importance of data, medtech companies should consider partnering with consumer-focused technology
and specialised digital health companies to stay up to date. These companies have advanced capabilities, including the ability to collect, store, and analyse vast amounts of health data generated by medical devices, as well as deep insights on what motivates and engages consumers.
The health-tech sector in India can prove to be a big opportunity for investors in the future. Indian healthcare sector is on the cusp of an exciting new era powered by technologies that will imp rove patient outcomes. Technology is a strong enabler, but it needs to be backed by the right regulatory frameworks, infrastructure, and a wider talent pool to bring the promise of quality, accessible, affordable healthcare beyond cities, to the remote rural areas.
April 2023 EXPRESS HEALTHCARE 21
MEDTECH
The Internet of Things (IoT),in conjunction with tele-medicine,has created a new Internet of Medical Things (IoMT),which will play a critical role in monitoring and preventing illnesses
PUBLIC HEALTH
Is eradicating sickle cell disease a possibility?
The finance minister’s February 1 budget announcement launching a drive to eradicate Sickle Cell Anemia by 2047, the 100th anniversary of Indian Independence, is a welcome step toward eliminating a littleknown killer. But to get there, India must learn from Nigeria.

Sickle cell anemia, more commonly known as Sickle Cell Disease (SCD), is a genetic blood disorder that affects millions of people worldwide with its largest prevalence in sub-Saharan Africa and a significant portion of the population in India. The disease is characterised by the abnormal formation of haemoglobin in red blood cells, which results in misshapen and sickleshaped cells that can clog blood vessels and restrict the flow of oxygen to various vital organs and tissues in the body, making it a painful and incapacitating condition for sufferers.
In India, SCD is particularly prevalent in certain communities, such as the tribal populations in central and eastern India, and it is estimated that more than 10 million Indians are affected by the disease[1]. However, despite its high prevalence, SCD remains largely underdiagnosed and undertreated in India, which has contributed to significant health problems for affected individuals and families.
One of the biggest problems India faces in addressing SCD is a lack of awareness and education about the disease. Despite the high incidence of the disease in the country, many people are still unaware of the condition and its consequences. As a result, many individuals do not seek medical help until the disease has affected vital organs.
Another issue is the shortage of medical facilities and trained personnel equipped to diagnose and treat SCD and the lack of access to affordable and effective treatments. While there are some treatments available for the disease, including blood exchange/transfusions, bone
marrow transplants, gene therapy, and hydroxyurea therapy, these treatments are often costly, not widely available, and complicated in many parts of the country. In rural areas, access to medical care is limited, and many people are forced to rely on traditional healers who are not equipped to provide the specialized care required for this condition. Furthermore, the cost of treatment is often prohibitively high, making it difficult for individuals from low to middle -income backgrounds to access the care they need. As a result, many people with sickle cell disease are unable to access the care they need to manage their condition and maintain quality health.
To address these challenges, India must take a multi-pronged approach that includes increasing awareness, improving access to medical care, and investing in research and development of treatments for SCD. Screening 70 million individuals from the age of 0-40 years, as announced by the Finance Minister, is one of the most important initiatives highlighted. But, it will not be able to combat the problem alone.
India can learn from the efforts of Sub-Saharan countries, especially Nigeria, in addressing
sickle cell disease. Nigeria has the highest disease burden[2]of SCD globally and has made significant progress in improving awareness and access to medical care for individuals with sickle cell. For example, the country and citizen-sponsored NGOs have established a network of sickle cell clinics and have trained medical personnel to provide specialised care for individuals with the condition. This is a vital step in improving the lives of patients and creates an opportunity to standardize care for patient health improvement.
Another way India can learn from the efforts of Sub-Saharan countries is by investing in public health campaigns aimed at educating individuals about the importance of early diagnosis and treatment for sickle cell disease.
In Nigeria, SCD has been identified to be more prevalent in less literate communities where fewer people are aware the disease can pass invisibly from parent to child. Community sensitisation campaigns have turned to pop stars, local celebrities, and trusted leaders to help get the word out.
Aside from sensitisation and advocacy campaigns, Nigeria has adopted early new-born screening to properly identify, treat and
create routine treatment options that can improve life expectancy and reduce prospects of longterm disability. By focusing on early diagnosis and treatment, India can help to prevent the development of serious health problems in people with sickle cell anemia and provide opportunities to educate parents on future reproductive choices.
Another lesson from Nigeria’s experience with sickle cell anemia is the importance of building support networks for people with sickle cell disease including peer support groups and communitybased organisations, which have helped to increase awareness about the disease and provide affected individuals with the support they need to manage their condition. By taking a similar approach in India, local governments and healthcare providers can help to build a supportive network for people with sickle cell anemia, which can help to improve their health outcomes and quality of life.
Beyond these steps, the government’s new financial commitment to sickle cell disease must be part of a broader effort against the disease. Taking bold steps to increase young people’s awareness levels can be achieved by standardizing the education
materials and curricula for schools and youth focus groups.
One can argue that providing financial assistance to individuals from low-income backgrounds to help them access routine medical care and improving medical services and professional knowledge would provide a simple solution to the patient health accessibility dilemma. Currently, there is no cure for this condition, and the treatments available are limited with often serious side effects including hemolysis, priapism, organ damage, and addiction. India is strategically positioned to do much more by taking advantage of its robust pharmaceutical and research capacity to produce more effective treatments with fewer cost implications and more availability. This can revolutionise patient treatment on a local level and open a promising opportunity for India’s global medicinal exports.
References:
[1] https://tribal.nic.in/sickle-cell-disease-piramalswasthya.aspx#:~:text=Sickle%20Cel l%20Disease%20(SCD)%2C,births%2 0among%20STs%20have%20SCD
[2] https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC9120745/
EXPRESS HEALTHCARE April 2023 22
Dr Shuchin Bajaj,Director,Ujala Cygnus Group of Hospitals and Elmer Aluge,President of the Sickle Cell Aid Foundation in Nigeria highlights that one of the biggest problems India faces in addressing Sickle Cell Disease (SCD) is a lack of awareness and education about the disease
Dr Shuchin BajajElmer Aluge
STRATEGY
Overcoming uncertainties in regulatory status of digital health in India



Technology today has pervaded almost all aspects of human life. Health sector is also not untouched by the evolution of technology. Today, with the incoming of several digital technologies, healthcare delivery has become personalised and precise, and the direct intervention of a healthcare professional is limited.
The term ‘Digital Health’ is all encompassing and includes all applications resulting from the intersection of healthcare and technology. As per the World Health Organization, digital health is a broad umbrella term encompassing eHealth (which includes mHealth), as well as emerging areas, such as advanced computing sciences in 'big data', genomics, and artificial intelligence.
As per Ministry of Health and Family Welfare (MoHFW), eHealth or Digital Health is using of information and communication technology in the direction of reaching services to citizens and citizens empowerment through information dissemination.
Digital health includes the use of information and communication technologies in order to resolve the health problems and issues faced by people.
These technologies include both hardware and software solutions. It can cover everything from wearable gadgets to ingestible sensors, from mobile health apps to artificial intelligence, from robotic carriers to electronic records and from web-based analysis to remote monitoring sensors. It is basically about applying digital transformation, through disruptive technolo-
gies and cultural dynamics, to the healthcare sector and services.
Post COVID-19 pandemic, there has been a great rise in the rate of adoption of the digital technology in healthcare sector. As per an estimate, 60 per cent of patients and 65 per cent of physicians now favor digital platforms over in person consultations.
With such increased acceptance of technology and growing opportunities in the healthcare industry, there is a need for regulatory intervention to ensure correct and effective usage of the technology. Due to the regular exchange of personal data, the protection of the personal data thus generated has become a matter of concern. Today, everyone is freely using smartphones with pulse trackers, smartwatches that monitor people's heart rate even during sleep, and menstruation trackers, without being aware of the amount of data generated and stored.
In India, legal framework pertaining to e-health protection is broadly governed by the following provisions:
◆ IT Act, 2000, read with, the IT (SPDI) Rules, 2011,
Intermediary Guideline Rules 2011, which provide protection to the collection, disclosure and transfer of sensitive personal data, covering medical records and history.
◆ Drugs and Cosmetics Act,1940 (D&C Act): This is the principal legislation governing manufacture, sell, and distribution of drugs, cosmeticsand Medical Devices in India.
◆ The Clinical Establishment Act, 2010: It mandates the “maintenance and provision of Electronic Medical Record for every patient” for the registration and continuation of every clinical establishment.
◆ Telemedicine Guidelines 2020: It allows medical practitioner to perform telemedicine from anywhere in the country and provides direction on the type of care that can be provided and how that care should be delivered.
Although the aforesaid provisions provide legal and regulatory framework to digital health but there exist certain uncertainties which can be overcome with effective implementation of the aforesaid provisions and by introducing fresh set of legal and regulatory framework. Some
of areas of concerns are discussed below.
◆ Liability concerns: There are serious concerns regarding liability while accessing digital health enabled by technologies like Artificial Intelligence (AI). For instance, if a medical device, diagnosis or treatment is powered by AI, in such cases, the concerns arise that who is liable towards the same i.e., software developer, the manufacturer, service provider or the physician.
◆ Categorisation of “Software” as drugs: On 11 February 2020, MoHFW released two notifications concerning medical devices in India. The effect of the aforesaid notifications is that medical devices, including digital healthcare systems, will now fall within the definition of "Drugs" under the D&C Act. Some examples like - blood sugar monitor, diabetes tracker, pulse and sleep monitor applications are currently regulated as drugs. As per notification, the ambit of the term “medical devices” has been expanded to include all things that assist a human body in diagnosis, prevention, monitoring and supporting life. This can have far-reaching implications. The drugs
regulators are required to be equipped with the technology to regulate the intangible nature of software and other evolving technology in the healthcare sector.
◆ IPR related issues: A flurry of innovations are expected in digital health sector. Most of these inn ovations are going to be related to method or systems implemented on a computer. Under Section 3(k) of the Patent Act, 1970, a mathematical method or a computer program per se or algorithms are not patentable. For example, a typical digital health system might involve machine learning for diagnostic analysis which will involve computer program and mathematical methods and thus careful consideration regarding their patentability is required.
In light of the above, certain measures are required to be undertaken by the government to overcome the uncertainties in legal and regulatory status of Digital health. For instance, data generated by digital healthcare needs to be protected under the specific regulatory regime. A clear categorisation is required to be put in place to ascertain which products and services fall within the healthcare sector and which fall under other categories. The Digital Information Security in Healthcare Act 2018 (‘DISHA’) provides security, standardisation, privacy, and confidentiality standards for electronic health data and the same is required to be enacted soon. Digital health is an evolving sector with huge potential therefore introduction of a unified legal and regulatory framework is need of the hour.
April 2023 EXPRESS HEALTHCARE 23
Rajdutt S Singh-Partner, Aayush Sharma-Sr.Principal Associate,and Aditya Pratap SinghAssociate at S&ALaw Offices talks about the ways to overcome uncertainties in legal and regulatory status of digital health in India
Rajdutt S Singh
Aayush Sharma
Aditya Pratap Singh
HEALTHCARE TREND
Transasia Bio-Medicals launches ‘Made in India’Clinical Chemistryreagents
Launched on the sidelines of Andhra Pradesh Global Investors Summit 2023,the Erba CRPand
Erba HbA1c test kits will allow clinical laboratories to benefit from dedicated high quality reagents
Transasia Bio-Medicals
Ltd., the leader in In vitro Diagnostics segment in India has announced the launch of ‘Made in India’ clinical chemistry test kits, Erba CRP and Erba HbA1c, by Minister for Road Transport & Highways in the Government of India, Nitin Gadkari at its manufacturing facility located in Andhra Pradesh MedTech Zone Ltd, Visakhapatnam.
The launch occasion was graced by Dr Jitendra Sharma, MD & CEO, AMTZ and other government officials. These reliable and affordable test kits are aimed at enhancing patient care through 50000+ laboratories serving 150+ crore tests every year.
Suresh Vazirani, Founder Chairman, Transasia Erba Group said, “Transasia’s main goal is to create awareness that testing, in general, is the best measure for preventing or treating serious conditions.
The Erba CRP and Erba HbA1c test kits will allow healthcare professionals to test for different ranges of C-Reactive Protein (CRP) and glycated hemoglobin using patient samples, with precise results obtained in minutes. We are proud to be helping advance medical technology by Making in India for the world.”
The CRP test is a blood test to measure the levels of C-reactive protein (CRP), and can reveal whether a person has a condition that causes chronic inflammation.
In the case of HbA1C testing, results are used to monitor blood sugar control over time.
Aravind Viswanathan, CEO, Transasia Bio-Medicals Ltd said, "Transasia Bio-Medicals has a long history of providing quality reagents and test kits for Clinical Chemistry testing, and currently provides over 70

crore tests per year in this field.”
"To serve more than 50,000 Laboratories across India having Semi-Automatic biochemistry analyzers, Transasia has
recently launched Hba1c kit in Liquixx range to perform HbA1c test on any SAA. Liquixx HbA1c boasts of a linearity up to 16 per cent, and excellent correlation with Gold
Standard HPLC.”
The manufacturing facility at AMTZ, which was set up during the COVID-19 pandemic, is the largest in Asia for COVID19 testing solutions. It com-
prises a fully-equipped reagent and instrument manufacturing unit, with a roll-out capacity of 7 million ELISA-based antibody detection tests per month, in addition to 20 million RT-PCR tests and 2 million Rapid tests per month. The facility also produces 200 fully automated clinical chemistry analyzers every month, to meet the growing demand for a wide range of biochemistry tests for laboratories across the country.

EXPRESS HEALTHCARE April 2023 24
These reliable and affordable test kits are aimed at enhancing patient care through 50000+ laboratories serving 150+ crore tests every year
Emerging career pathways for allied healthcare professionals
Dr
G Arun Maiya,Professor & Dean,MCHP,MAHE

COVID-19 pandemic has truly redefined the pharma and healthcare industries in India, expanding the fortitude of opportunities for professionals across these industries. In 2022, employment across these sectors saw a significant surge. In fact, according the staffing industry sources, while 92 per cent of employers in India’s Healthcare & Pharmaceuticals were keen to hire, the projection for Q4 indicates a further 6 per cent increase in this pool.
Allied Health or health care professions has emerged as a strong domain within the healthcare paradigm. However, this segment has been facing a demand-supply gap which needs immediate attention.
FICCI and KMPG’s study reiterate that India’s current capacity of allied healthcare professionals stands at 57.5-58 lakh and need to increase by 8X by 2047 to enable the country’s vision to become a hub for health tourism and international medical treatment.
In 2022, the most promising opportunities for allied healthcare professionals included include audiology and speech-language therapy, physiotherapy, health information management, clinical nutrition, medical laboratory technology, emergency medical technology, perfusion technology, cardiovascular technology, respiratory therapy, optometry, occupational therapy, medical imaging technology, Psychology, physician assistants, renal replacement and dialysis, Sports and exercise science, nuclear medicine technology, medical radiation physics, operation theatre technologists, among others. In 2023, some of the key allied health profiles that will remain in vogue are:
◆ Psychologists: Psychologist plays an important role in
Manipal shares the top ten job profiles in
and food issues.
◆ Anaesthesia and Operational Theatre Technologists: They are skilled professionals involved in performing recovery, surgery, and administrating anaesthesia.
◆ Emergency Medical Technologists: They are qualified professionals for quicker response at emergency sites.
◆ Prosthetists and Orthotists: Patients who have had to have limbs or legs amputated can use prosthetics to replace them. Practitioners who specialise in orthotics treat skeletal and neuromuscular disorders.
◆ Medical Imaging Technologists: These professionals produce images of serious wounds and a range of illnesses, such as breast cancer screening and ultrasound. Cancer is treated by therapeutic radiologists either surgically or chemically.
◆ Speech and Language Therapists (SLTs): SLTs help adults and young children who have significant speech or language impairments.
◆ Physician Assistants: A Physician Assistant is a medical professional who can offer medical services to patients under the supervision of a doctor or a physician. Physician Assistants (PA) are responsible for implementing the physician directives and assessing the health of the patients by interviewing or examining them and studying their medical history.
currently changing from paper to electronic health records. As a result, new career specialisations are emerging in a variety of areas related to health information
◆ A cardiovascular technologist works in a cardiac cath lab and performs very complex procedures, including stent implants, cardiac pacemakers and defibrillators and other tests to diagnose heart disease. They take emergency calls and participate in saving the lives of those who are having a heart attack
◆ Medical Laboratory Technologists: contribute to the prevention of disease, and the diagnosis, treatment, and prognosis of pathophysiological conditions in humans. Medical laboratory personnel are responsible for assuring reliable and accurate laboratory test results
◆ Nuclear Medicine Technologists: The practice of nuclear medicine technology includes the use of sealed and unsealed radioactive materials, as well as pharmaceuticals, adjunctive medications and imaging modalities with or without contrast as part of diagnostic evaluation and therapy
studying the mental health of a person and helping them to cope with issues related to mental wellbeing.
◆ Occupational Therapists: Occupational therapists, also known as OTs, work in a variety of volunteer and independent sectors of society, helping patients with their mental, physical, and social problems.
◆ Physiotherapists: The use
of physical approaches to help cure Musculoskeletal, neuromuscular and such conditions are Physiotherapists.
◆ Chiropodists or Podiatrists: Chiropodists who focus on foot and ankle related pathologies.
◆ Clinical Nutritionists: Qualified professionals who are permitted to assess, identify, and treat patients’ nutrition
◆ Sports and Exercise Science Professionals: A broad range of fields that include physiology,psychology, and biomechanics, and their relationship to sports performance, health and wellbeing are covered in Sports Science.
◆ Health Information Management Professionals: Emerging specialisations where health organisations are
Currently, 60 per cent of all healthcare positions are in the allied healthcare sector, with the remaining 40 per cent being split between medical, nursing, and pharmacy. The need for AHPs has increased over the last few years, and is expected to continue with the continuous advancement in diagnostic and treatment approaches. Given the significant part that AHPs play in the delivery of healthcare solutions, maintaining suitable standards for their education and training is critical and academic institutions are also structuring their courses to prepare candidates for the future work roles.
April 2023 EXPRESS HEALTHCARE 25 HR
demand in 2023
Allied Health or health care professions has emerged as a strong domain within the healthcare paradigm.However, this segment has been facing a demand-supply gap which needs immediate attention

BUSINESS AVENUES EXPRESS HEALTHCARE April 2023 EXPRESS HEALTHCARE 26 To Advertise in Business Avenues Email: rajesh.bhatkal@expressindia.com rbhatkal@gmail.com



























BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE April 2023 27



BUSINESS AVENUES EXPRESS HEALTHCARE April 2023 EXPRESS HEALTHCARE 28

BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE April 2023 29

BUSINESS AVENUES EXPRESS HEALTHCARE April 2023 EXPRESS HEALTHCARE 30

BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE April 2023 31
HEALTHCARE TRACKER
Ultrasound: Critical differentiator in diagnosing and treating musculoskeletal ailments
The LOGIQ™ ultrasound system powered by Shear Wave Elastography has advanced features that are easy to use,quicker to grasp,with better image clarity,seamless for the imaging technician to use which help diagnose deep tissue changes across all body morphologies.
Dr Nidhi Bhatnagar,Associate Director-Radiology,Max Multispecialty Centre, Panchsheel,New Delhi shares her experience on the machine’s use in musculoskeletal imaging

Diagnostics and treatment changed with the intervention of superior imaging techniques and has continuously improved since then. This has not just directly impacted the understanding of diseases and ailments but has thrown new light on how pathology progresses and where quick intervention can stop and in certain cases reverse significant degeneration and tissue loss. AI and sharper imaging techniques have made machines efficient especially for musculoskeletal ailments and other diseases that get progressively worse over years.
With complex pathology has risen the need for better prognosis and advanced imaging techniques which traditional imaging falls short of. The USP of ultrasonography is its ability to catch tissue breakdown progress non-invasively, and making quick diagnostic decisions with precision and purpose.
The LOGIQ™ ultrasound system powered by Shear Wave Elastography has advanced features that are easy to use, quicker to grasp, with better image clarity, seamless for the imaging technician to use which help diagnose deep tissue changes across all body morphologies.
How has your experience been with the LOGIQ™ Ultrasound system in diagnosing soft tissue
pathologies in complex ailments?
I have been working with this machine for a while now and find it to be extremely strong and sound unit, primarily because of 2D imaging which has got very high contrast and fast processing. This helps in dealing with sensitive pathologies. It also gives me diagnostic confidence and I enjoy working on it.
The incorporation of UGAP into the LOGIQ™ Ultrasound system is extremely exciting. For gastroenterology, this gives a strong wholesome study. I am able to access the whole abdominal ultrasonography, with fibrosis index through 2D Shear Wave and then UGAP for fat qualification.
With the variety of probes in the LOGIQ™ machines, what challenges are they helping you solve and how?
The ML6-15-D probe has helped me to improve my functionality to see for newer structures which was a challenge earlier on. The compact autistic probe is also giving me a great added advantage. Latest technological innovations have been incorporated into the machine such as cSound technology which along with the new generation of XDclear™ probes, especially L2-9-D is of great help when I’m doing various imaging and small details.
How exactly is the LOGIQ™ ultrasound system helping you handle musculoskeletal
imaging?
The Radiantflow™ and color doppler imaging of this machine has a very stark contrast to the other machines I’ve been using. The Shear Wave elastography incorporated into this with kPa values and elasticity for fibrosis which I’ve been using extensively in musculoskeletal applications, brings the machine up to international standards.
As an imaging technician having worked with various other machines, how are the ergonomics and accessibility of the LOGIQ™ technology and its AI framework?
The AI incorporation in the LOGIQ™ machine is very exciting. The knobs on the panel are sensitively placed, making me more productive and improved in my work because I’m not constantly searching for them. The touchscreen panel has annotations that help in putting together a comparison graph for 2D elastography which is good learning for young radiologists.
For renal artery flows and gradient flows, the entire color doppler imaging helped me to shorten my work time, from 20 mins to 15 mins. I was able to deliver results quickly and accurately. This is a great unit with great functionality, and you’re not spending energies focused on optimising images, because its right there optimized for you.
EXPRESS HEALTHCARE April 2023 32
INTERVIEW
I have been working with this machine for a while now and find it to be extremely strong and sound unit,primarily because of 2D imaging which has got very high contrast and fast processing
Preventing future global shortages of iodinated contrast media requires industryaction

Kevin O’Neill,President & CEO,GE HealthCare Pharmaceutical Diagnostics highlights that iodinated contrast media is a pharmaceutical that’s injected into patients before an X-ray examination or CTscan to better visualise patients’organs,blood vessels,and tissues,playing a key role in diagnosis across major disease pathways,including cancer and heart disease
The key role of iodinated contrast media, used daily around the world in X-ray and Computed Tomography (CT) imaging was brought into sharp focus during the 2022 supply shortage following a COVID-19 lockdown in Shanghai.
Iodinated contrast media is a pharmaceutical that’s injected into patients before an X-ray examination or CT scan to better visualise patients’ organs, blood vessels, and tissues, playing a key role in diagnosis across major disease pathways, including cancer and heart disease. GE HealthCare’s contrast media are used worldwide to support three patient procedures every second.
Supply is now returning to normal, but the situation was unprecedented and challenging and required an industrywide response. Our global footprint helped ensure we could react with speed. Actions we took to mitigate the impact included increasing production from our other global plants, using air freight where we could instead of transporting our products by sea, and focusing on fewer product variations to cater to more patients. Still, the result was a shock to the healthcare system, with the sudden scarcity of an injectable pharmaceutical that had been readily available for decades and with healthcare providers having to prioritise patient procedures and adjust some of their normal protocols as a result.
Our learnings from the shortage shine a light on the need for long-term availability of these essential imaging agents and there is a bigger issue at play.
We expect global demand for iodinated contrast media —
the diagnostic pharmaceuticals impacted by the Shanghai lockdown to double in the next 10 years as the growing global prevalence of chronic disorders drives significant growth in CT procedures. CT has transformed diagnostic imaging since its inception in the late 1960s. In the U.S. alone, more than 80 million CT scans are now performed annually, com-
support this increasing global demand for CT scans. Yet demand for contrast media outstrips supply, and the gap between the two is set to widen further.
Unless manufacturers, providers and the whole industry work together, the impact of contrast media shortages could be far greater and wider ranging than anything we’ve seen with the 2022 supply shortage.
So, what can be done? First, contrast media suppliers need to step up and expand capacity to deliver more doses year after year. At GE HealthCare, we understand our responsibility. We’ve already invested almost $400 million in the past 10 years to increase capacity across our global manufacturing network. In just few months, we opened a new $30 million production line in our Cork, Ireland, facility to grow capacity there by 50 per cent, announced an $80 million expansion1 of our active pharmaceutical ingredient (API) site in Lindesnes, Norway and signed a multi-year agreement with a leading iodine supplier to secure increasing volumes of iodine raw material. 2 All of this will enable us to produce 30 million more patient doses annually by 2025.
for reuse.
Healthcare providers are also taking action. During the height of the contrast media shortage, many shared best practices for using less dose per patient, making every vial of contrast media count and reducing leftovers as much as possible. Increasingly, clinicians are adopting new protocols in areas like AI, weightbased dosing, and multi-dose packaging to help optimise contrast usage.
In India, radiology infrastructure has grown rapidly in last 2-3 years. This has increased our responsibility as market leader to secure the supply for the resulting increased demand for contrast media. The GE HealthCare team in India is focused on enhancing efficiencies in high volume radiology centers through the use of multi-dose contrast media vials to reduce unused leftover contrast media.
pared with just 3 million in 1980.
While CT technology has evolved over time, enabling less contrast dose injected per patient, the increase in CT scans and enhanced procedures has seen the contrast media market increase by 250 per cent from 2010 to 2018. The continued availability of iodinated contrast media is crucial to
But it’s not just about capacity. We’re investing across the whole of the contrast media life cycle, from what we call “extraction to injection” — from securing reliable supplies of more iodine raw material to investing in our manufacturing plants, and right through to offering services and innovations at the point of injection to help reduce the contrast dose delivered to each patient, reduce volumes of unused leftovers, and even recycle iodine from leftover contrast media
As it revolutionised healthcare, CT also vastly increased demand for contrast media. The 2022 shortage was unprecedented — but it has accelerated a necessary shift in thinking about how we protect and conserve contrast media. We need to work together to develop industry-wide approaches if we are to grow, secure and protect the future supply of these essential imaging agents.
References
1. https://www.gehealthcare.com/ about/newsroom/press-releases/gehealthcare-announces-80-million-investment-to-expand-contrast-mediaproduction
2. https://www.gehealthcare.com/ about/newsroom/press-releases/gehealthcare-announces-multi-yearagreement-with-sqm-to-secure-iodine-supply-for
April 2023 EXPRESS HEALTHCARE 33
While CTtechnology has evolved over time,enabling less contrast dose injected per patient,the increase in CTscans and enhanced procedures has seen the contrast media market increase by 250 per cent from 2010 to 2018
Sample integrityplays a vital role on the quality of results in hemostasis testing
Srinivas Naidu,Senior Product Manager- Coagulation Marketing,Sysmex talks about company’s CN-series which takes the reliability and performance of Sysmex CS-series and takes it up to a whole new level

In haemostasis, test results can point out major clinical issues, some of which may be life-threatening if not dealt with swiftly and accurately. For instance, Cardiovascular Disease (CVD) is one of the leading causes of death and disability in the world. And this is not likely to change any time soon, considering the demographics and lifestyle we see today. Like all patients, people with CVD have the best chance of survival when their illness is detected early.
Labs offering haemostasis testing can really support clinicians with patient diagnosis. Since confidence in the subsequent clinical decision-making is essential, you need equipment that performs reliably and produces results of consistent, high quality at all times. You need to meet TAT demands and help patients as soon as possible, so the tests have to be performed fast –even with complex samples that require precise pre-analytical treatment. And as the industry evolves, the spectrum of test requests is increasing too. It’s a challenging situation.
Unlike other areas of testing the sample integrity plays a vital role on the quality of results in hemostasis testing. So, if an analyzer is able to identify erroneous samples, then that would be an ideal analyzer for a respective laboratory.
Sysmex, a leading global player in hemostasis Instrumentation and Reagents addresses these concerns with their latest analyzer, Sysmex CN- Series.
Sysmex CN-series, takes the reliability and performance of Sysmex CS-series and takes

it up to a whole new level.
Sysmex was the first company worldwide to incorporate pre analytical sample testing and Platelet aggregometry testing in a hemostasis analyzer and our commitment remains the same with the CN-Series also which provides

all these and much more.
Sysmex CN-Series comes with a higher throughput thereby lessening the turnaround time and even with the higher throughput the space requirement is very low.
The dead volumes of samples are very low so that means there are more analyses from lesser volumes.
Sysmex CN-Series identifies sub-optimal samples by employing HIL (Hemolysed, Icteric and Lipemic) testing and Sample volume check, clot waveform analysis to assess comprehensive hemostasis functions. CN-Series Inhibitor testing more convenient with the Cross-mixing functions.
EXPRESS HEALTHCARE April 2023 34 HEALTHCARE TRACKER
HEALTHCARE TRACKER
IIHMR University: Adopting newtechnologies and academic models for student-centric education
Prof.(Dr) P.R.Sodani,President,IIHMR University,Jaipur had significantly contributed to creating an organisational culture for the growth and development of the university

Prof. (Dr.) P.R. Sodani is the President of IIHMR University, Jaipur. He is a well-known Health Economist and Public Health Professor for more than two decades and mentored faculty, students, and research scholars. Professor Sodani earned Ph.D. in health economics and a Master of Public Health from the University of North Carolina at Chapel Hill, USA. He has been associated with the Department of International Health, Johns Hopkins Bloomberg School of Public Health, USA for teaching the MPH program jointly offered by Johns Hopkins Bloomberg School of Public Health and IIHMR University.
He is the Associate Editor of the Journal of Health Management, an international peer-reviewed, Scopus-indexed journal published by SAGE Publications. He is also associated with various journals of repute in the capacity of the reviewer. He is the Secretary-General of the South-East Asia Public Health Education Institutions Network (SEAPHEIN). He has published papers in indexed journals of national and international repute. He frequently writes blogs on emerging issues in the health sector.
He has organised several national and international programs for health professionals on promoting Leadership, Strategic Management, Health Policy and Management, Health Economics, Health Financing, and Hospital Management. Professor Sodani is also a CoFounder of the IIHMR Foundation for promoting start-ups. Professor Sodani has been at various levels of leadership positions and had been responsible for leading and managing academics, research, training, fundraising, and networking with national and international organisations.
The Chief Minister of Rajasthan has nominated Dr P.R.Sodani as a member of the Rajasthan State Health Mission.He is also a member of the Technical Expert Group for Institutionalisation of State Health Accounts in Rajasthan
The Chief Minister of Rajasthan has nominated Dr P.R. Sodani as a member of the Rajasthan State Health Mission. He is also a member of the Technical Expert Group for Institutionalisation of State Health Accounts in Rajasthan. In addition to this, Professor Sodani is on board with various prestigious organisations/committees for supporting academic excellence and research for policy formula-
culture for the growth and development of IIHMR University, Jaipur.
IIHMR University has been established and incorporated as a postgraduate research university by the Government of Rajasthan. IIHMR University is UGC-recognised and NAAC - accredited. IIHMR University has a unique organisational culture that enshrines core values and ethos of autonomy, accountability, openness, and transparency. The multi-disciplinary teams of faculty representing public health, management, economics, statistics, demography, and social and behavioral sciences, constitute an enabling environment for learning and professional growth and development.
rashtra Emergency Medical Services, Jhpiego; American Society for Quality; for academics, training, capacity building, student exchange, faculty exchange, and joint research programs.
tion. Professor P.R. Sodani is a proud recipient of many prestigious awards including the Education Excellence Award 2021 for Outstanding work in the field of Education, by the Governor of Rajasthan Kalraj Mishra.
Professor Sodani demonstrated academic leadership, visioning, policy planning, and strategic implementation. He had significantly contributed to creating an organisational
IIHMR University offers postgraduate and research programs including MBA (Hospital and Health Management), MBA (Pharmaceutical Management), MBA (Development Management), Master of Public Health, Master of Public Health (Implementation Science) supported by WHO-TDR, Executive MPH, Executive MHA, and Ph.D. programs. Professor Sodani strongly believes in collaborations and partnerships for promoting academic excellence and research. IIHMR University has a strong collaboration with Johns Hopkins University, USA for academic and research, offering a joint degree MPH program, and implementing a number of multi-country research programs for improving health systems outcomes.
Apart from Johns Hopkins University, IIHMR University has collaborations with Chester University, UK; University of Montreal, Canada; Curtin University, Australia; Kandahar University, Afghanistan; Management and Science University (MSU) Malaysia, Rajasthan University of Health Sciences; NHA, NHSRC, NHM Odisha, Maha-
Under the able leadership of Professor P.R. Sodani, IIHMR University, Jaipur has been recognised as a Scientific and Industrial Research Organisation by the Department of Scientific and Industrial Research, Government of India. The university is also recognised as a Host Institute (HI) by the Ministry of Micro, Small and Medium Enterprises (MSME), Government of India, for implementing the incubation component under the MSME innovative scheme. As a Host Institute, IIHMR University is eligible to submit new innovative ideas for getting financial support under the new MSME innovative scheme. He has led significant developments and major transformations in achieving an excellent ranking of the university, IIHMR University, Jaipur has been Ranked 2nd at the All-India level and 1st at the State level – Rajasthan by Education World Ranking 202223, IIHMR University, Jaipur has been Ranked in 201-300 band among all world universities ranking and 18th rank among Indian universities by Time Higher Education Impact Ranking 2022.
Prof. P.R. Sodani believes in adopting new technologies and academic models for studentcentric education to better serve the industry and society. Prof. Sodani has successfully reinforced the University's status as a world-class research university with his strong leadership and vision leading to achieving its vision and mission, by taking various new and innovative initiatives, he also established the domain of Executive Education for working professionals at IIHMR University, Jaipur.
April 2023 EXPRESS HEALTHCARE 35
HEALTHCARE TRACKER
Nexage: India’s first trendy& stylish medical wear brand gets overwhelming response from the medical fraternity
Nexage by Medikabazaar is a game-changer in the medical apparel industry.It provides healthcare professionals with a wide variety of options in terms of fabric,color,and style.The scrubs are not only comfortable and functional but also reflect the personality of the wearer
In recent years, there has been a growing demand for medical scrubs that not only provide comfort and functionality but also reflect the wearer's personality. To meet this demand, MEDIKABAZAAR launched Nexage last year.
Since its launch, Nexage has received a positive response from doctors and hospitals for its fabric, comfort, and colour options. The quality of the scrubs is unparalleled, and they are available in a range of colours and fabrics, including Orange, Maroon, Mauve, Teal Blue, Denim, Doctor Blue, Sky Grey, Leaf Green, Hot Pink, Candy Green, Purple, Cotton, Woven Poly-Cotton, Poly-Cotton, Knit, Denim, and Stretch. This wide variety of options ensures that healthcare professionals can choose a scrub that is not only comfortable but also reflects their personality.
What sets Nexage apart from
What sets Nexage
from other medical scrubs
other medical scrubs on the market is its attention to detail. The company understands that healthcare professionals require apparel that is not only comfortable but also functional. As a result, Nexage provides a perfect balance between performance, safety, and personality. The scrubs are curated by ace fashion designers who provide a mix of elegance and comfort to healthcare workers.
Another unique feature of Nexage is its flexibility in terms of customisation. The company offers personalisation options for
CONTRIBUTOR’S CHECKLIST
● Express Healthcare accepts editorial material for the regular columns and from pre-approved contributors/columnists.
● Express Healthcare has a strict non-tolerance policy towards plagiarism and will blacklist all authors found to have used/referred to previously published material in any form, without giving due credit in the industryaccepted format.
● As per our organisation’s guidelines,we need to keep on record a signed and dated declaration from the author that the article is authored by him/her/them,that it is his/her/their original work,and that all references have been quoted in full where necessary or due acknowledgement has been given.The declaration also needs to state that the article has not been published before and there exist no impediment to our publication.Without this declaration we cannot proceed.

● If the article/column is not an original piece of work,the author/s will bear the onus of taking permission for re-publishing in Express Healthcare.The final decision to carry such republished articles rests with the Editor.
● Express Healthcare’s prime audience is senior
individuals and flexible bulk purchase options for hospitals. This means that hospitals can customise scrubs according to their preferences in terms of fabric, colour, size, and style. This can transform the look of the hospital workforce, boosting their confidence and enhancing patients' perspective of the hospital's service quality.
Vivek Tiwari CEO & Founder, Medikabazaar said, "We are thrilled with the positive response we have received from healthcare professionals around the world for Nexage. Our goal is
to provide healthcare professionals with scrubs that not only meet their functional needs but also their fashion needs. We are delighted that Nexage has been able to accomplish that."
Nexage is not just limited to India, but it has also received a positive response from healthcare personnel in Japan, China, the Middle East, and other countries. This is a testament to the fact that Medikabazaar with Nexage has succeeded in its mission to transform medical wear by introducing trendy, aspirational, comfortable, safe, and
management and professionals in the hospital industry.Editorial material addressing this audience would be given preference.
● The articles should cover technology and policy trends and business related discussions.
● Articles by columnists should talk about concepts or trends without being too company or product specific.
● Article length for regular columns: Between 1300 - 1500 words.These should be accompanied by diagrams,illustrations,tables and photographs,wherever relevant.
● We welcome information on new products and services introduced by your organisation for our Products sections.Related photographs and brochures must accompany the information.
● Besides the regular columns,each issue will have a special focus on a specific topic of relevance to the Indian market.You may write to the Editor for more details of the schedule.
● In e-mail communications,avoid large document attachments (above 1MB) as far as possible.
● Articles may be edited for brevity,style, relevance.
● Do specify name,designation,company name,
supremely functional worldclass apparel for medical professionals.
Nexage by Medikabazaar is a game-changer in the medical apparel industry. It provides healthcare professionals with a wide variety of options in terms of fabric, color, and style. The scrubs are not only comfortable and functional but also reflect the personality of the wearer. With its attention to detail, customization options, and global appeal, Nexage is set to revolutionize the medical wear industry.
Be Bold, Be Confident, Be Stylish, Be Nexage
Nexage: Approved by the Doctors, For the Doctors
Nexage, India’s first trendy & stylish medical wear brand gets overwhelming response from the medical fraternity.
department and e-mail address for feedback,in the article.
● We encourage authors to send a short profile of professional achievements and a recent photograph,preferably in colour,high resolution with a good contrast.
Email your contribution to:
viveka.r@expressindia.com
viveka.roy3@gmail.com
Editor, Express Healthcare
EXPRESS HEALTHCARE April 2023 36
apart
on the market is its attention to detail.The company understands that healthcare professionals require apparel that is not only comfortable but also functional

REGD.WITH RNI NO.MAHENG/2007/22045,POSTAL REGD.NO.MCS/162/2022 – 24,PUBLISHED ON 8TH EVERY MONTH, POSTED ON 14TH,15TH,16TH EVERY MONTH,POSTED AT MUMBAI PATRIKA CHANNEL SORTING OFFICE,MUMBAI – 400001











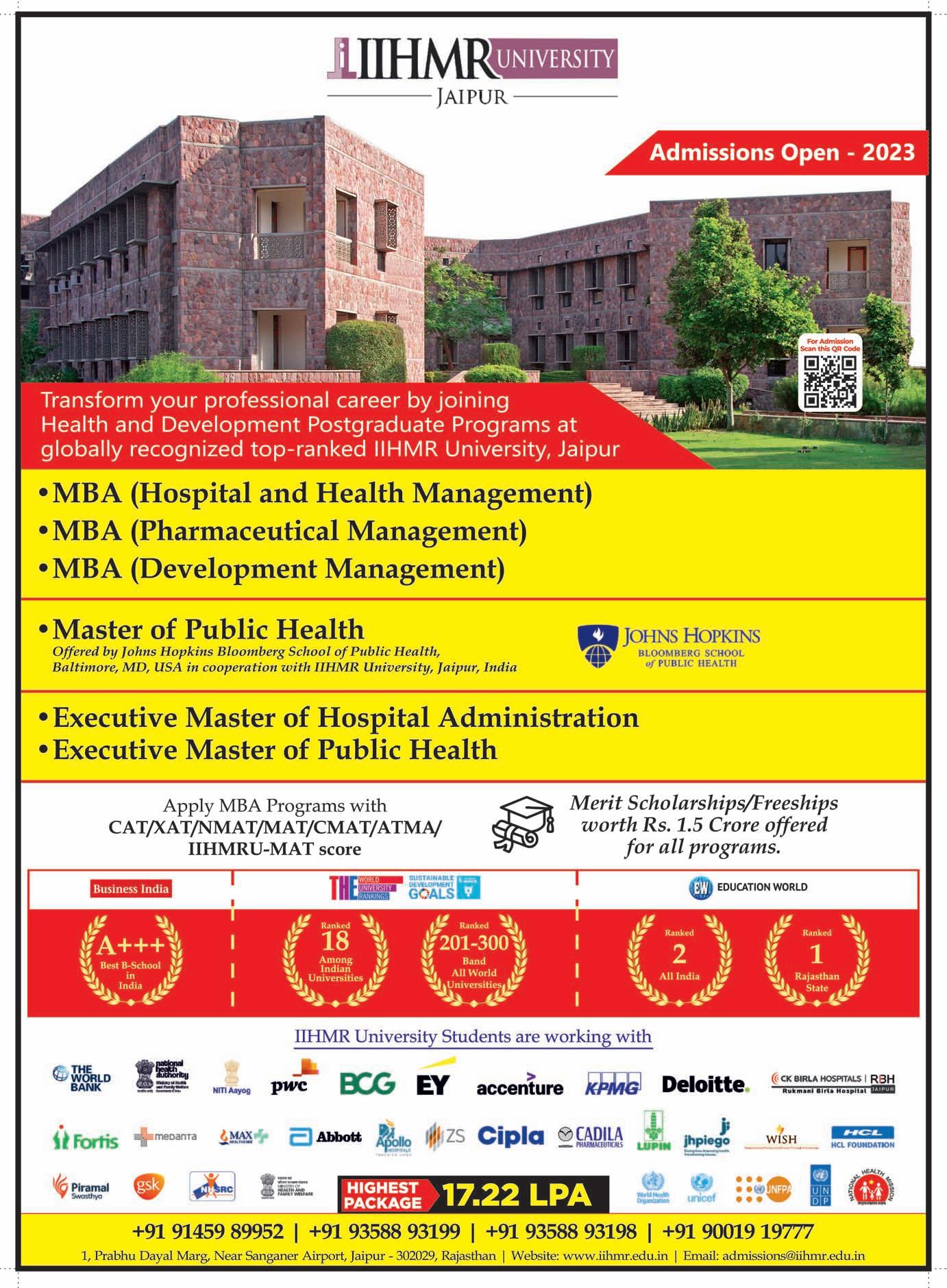
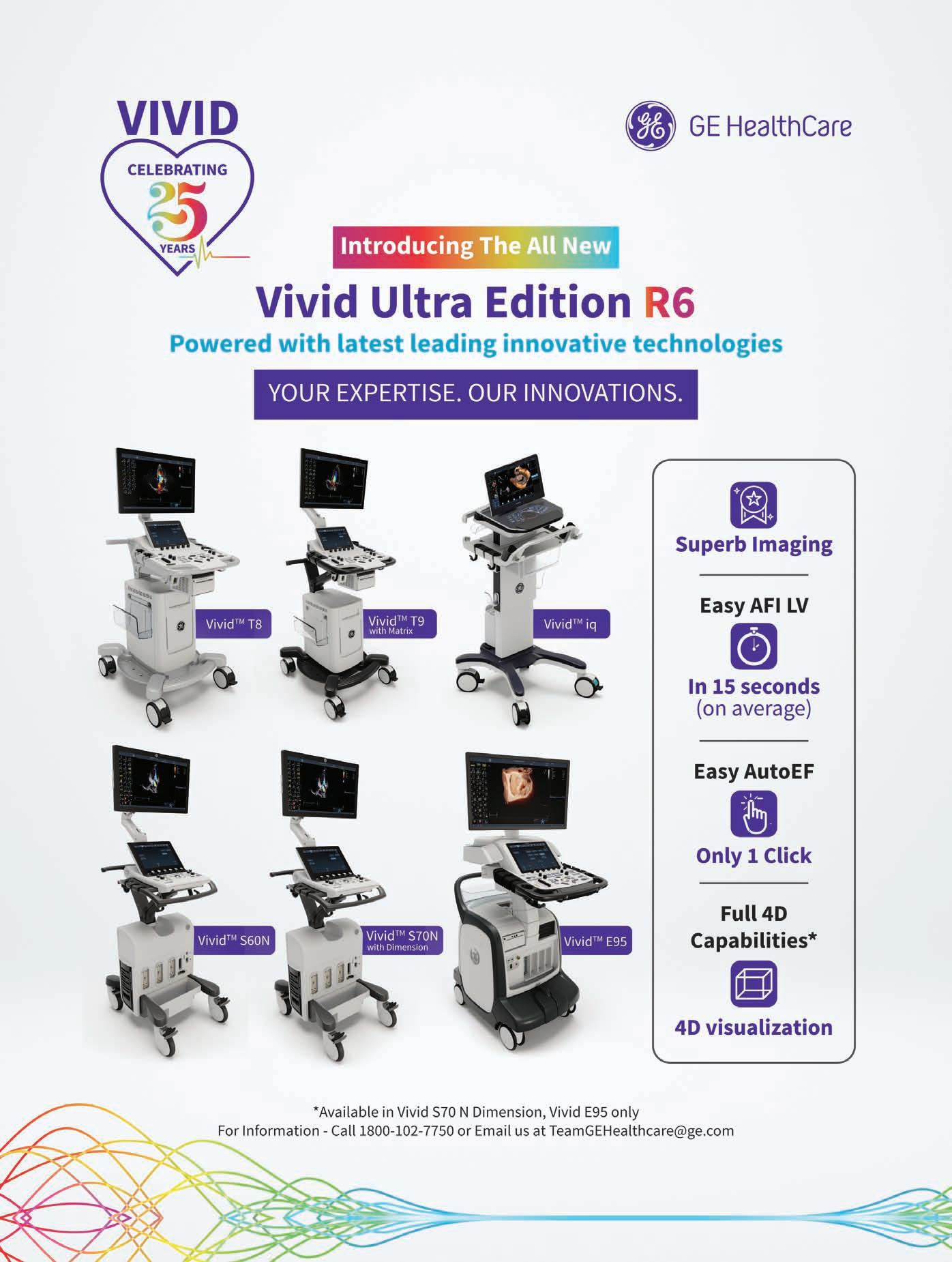













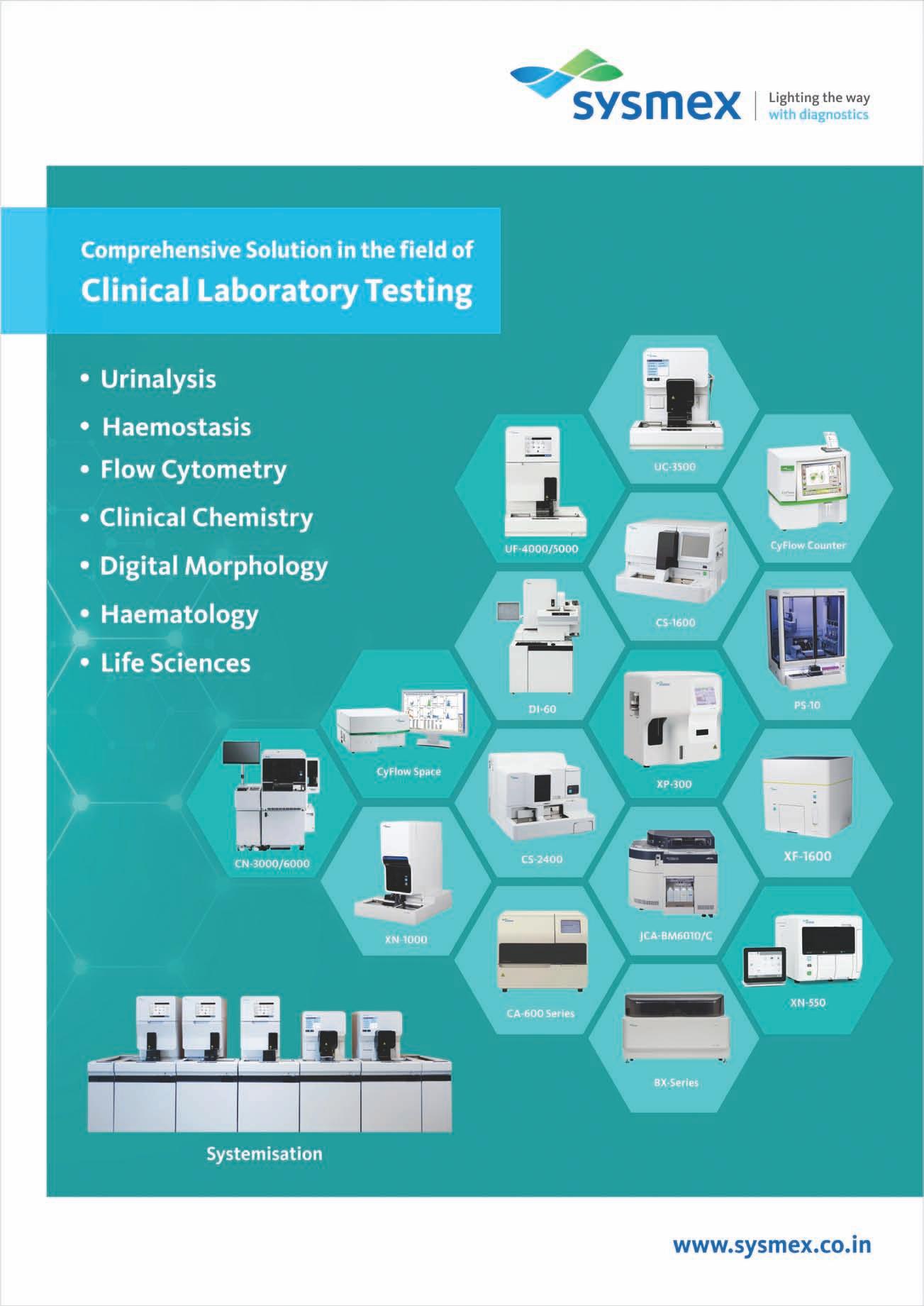















 ByKalyani Sharma
ByKalyani Sharma