REFERRAL the power of a HEART FAILURE


the stigma of
MENTAL ILLNESS
"words" really are
PAINFUL


REFERRAL the power of a HEART FAILURE


the stigma of
MENTAL ILLNESS
"words" really are
PAINFUL













As an IBERIABANK Private Client, personalized service from an experienced and knowledgeable team of professionals is our priority. Your rela�onship team will work to carefully assess your financial and investment needs. Whether you prefer a high personal touch or innova�ve electronic channels, our goal is to provide you with flexible and hassle-free banking. We are a fiduciary – simultaneously managing risk while always serving in your best interest. With the resources and exper�se of a large firm and the a�en�ve service of a bou�que, we provide personalized strategies to help you grow, protect and transfer wealth to the next genera�on.






To reach our readers, whether through editorial contribution or advertising, please contact Kelly Reese at
The information and opinions contained in this publication constitute general medical information only and should not be construed as medical advice. Before making important medical decisions, readers should consult with a physician or trained medical provider of their choice and have their needs and concerns assessed in a clinical setting appropriate for their problem.
S alpy
Kimberly Waldrop,
Elisa Brooks
Larry Parker, MD
Kari Kingsley, MSN, CRNP
Rachel Sullivan, MFTA
Victor Chin, MD
Ben Macklin

Michael Potter
Michael Beuoy, PT, Cert. MDT
Brian Baer
C urt Freudenberger, MD
Patti Hutchison
SALES & MARKETING
Kelly Reese, Founder
Lisa Layton, VP Sales/Marketing
CHIEF EDITORIAL WRITER
Kimberly Waldrop, MA
GRAPHIC
Leigha Parker PUBLISHERS
Blake Bentley, President
It’s a great time to grab a recent copy of Inside Medicine, and relax while you read.
Our hope and prayer with this publication is to always reflect God’s love. We work hard to try and give you stories that are uplifting, informative, and even sometimes spiritual. In this edition of Inside Medicine, we hope you find something you can use or share with others.
I am so excited to share Patti Hutchison’s story. It is all about her journey. From chronic hip pain to surgery, to preparing for and then climbing Mt. Kilimanjaro, you will enjoy every ounce of her article. She has generously shared her experience and I’m sure you will find it inspiring! She has a positive and thankful spin on her adventures, as well as the doctor who helped get her there.

Huntsville once again is leading our state in the innovative spine procedures. Spine surgeon Larry Parker, MD brought Huntsville the first lumbar spine procedure in 2003. Newest generation procedures are quickly impacting our medical landscape. Featured articles with the activL and special highlights with Q&A’s will give you informative insight on how these procedures keep us at the forefront of medicine.
Also in this edition, you can read about mental health, TMJ pain, and even the best versions of insect repellants. You can also find good information regarding health referrals and the process behind it.
Did you know researchers are starting to use over the counter pain medications to help with physical as well as emotional pain?
As always, we hope you enjoy our magazine and will share it with others. If you ever have any questions or concerns, ideas for stories, or want to be a contributor, please let us know!
YOU ARE



"Quietly I heard a whisper to my own heart, Elisa, you are My workmanship."
There’s a lot out there on social media, blogs, and various forms of communication about self-love. The idea that perhaps we inherently don’t love ourselves and need to practice the art of loving yourself. I’m guessing that perhaps you have seen these thoughts and ideas out there as well, in the form of writings, memes, and who knows what else. And then, something that happened in my own daily life, made this whole idea come full circle for me.
I teach a variety of fitness classes, and though I’m not currently doing personal training, I’ve been a certified personal trainer for a number of years. I was going about my normal daily routine, and was teaching an hour class at the gym. In the first few minutes of class, two other instructors slid in the doors to take the class. Normally, that does not affect me much. However, these two just have never happened to have taken any of my classes because our schedules don’t cross, and something about them walking in made me nervous. Would they think I did the right safety cues? Do they think I’m great instructor? And so forth. As I’m literally coaching class, these thoughts and more are spiraling through the back of my mind.
About halfway through the class, I made a mistake that to me botched up a significant few minutes. I’ll attribute it to the fact that 1) I’m not perfect; and 2) I was nervous, knew I was nervous, and I allowed that to get the best of me. I got myself back on track, but was SO frustrated with myself for that mistake! Driving home all I could think of was what their perception of me might be … they probably thought I was ridiculous! Maybe they were sorry they ever walked in those doors tonight.





And on and on and on. Mind you, I would NEVER let my husband, my mom, my kids, my friends, anyone I know berate themselves with such negative talk if I could help it! But I was laying it on thick to my own self at that moment.
Quietly I heard a whisper to my own heart, Elisa, you are My workmanship.

I don’t know what point you are at in your life, whether or not you believe in God, whether or not you believe in a God that speaks to you. But I do. I believe that the Creator of the entire world is a loving God who cares for me and speaks to me. In that moment He quickly set things straight. What He spoke to me lines right up with a verse in Ephesians 2:10 which says, “For we are his (God’s) workmanship, created in Christ Jesus for good works, which God prepared beforehand that we should walk in them.” Another translation puts it this way, “For we are God’s masterpiece.”
What God calls His workmanship and His masterpiece is definitely not a mistake, a failure, or ridiculous. He made me. He made you. And in the Bible when the story of creation is concluding, God says that what He made is good. That includes us. We’re made in His image. Because of that, you and I have worth. We’re not worthless, like some people might say, like sometimes you or I might have felt at times in our lives. A masterpiece is priceless. We’re the masterpiece of God.
How does this tie in to self-love? I think we are missing the point. This is not about self-love. You can try and love yourself to pieces, but it won’t solve any of your problems. You’ll still make mistakes. So will I. You might look in the mirror and still be frustrated with the reflection. So will I at times. I don’t need to practice self-love. I need to know and believe down in the deepest places of my soul that I have worth. Not because I can necessarily produce anything worthwhile, but because the One who made me says I have worth. That I was created with purpose and destiny written in my heart. Because I am HIS masterpiece, HIS workmanship, and what He makes is good! I have inherent value because I was created by the Creator!
When moments come like the mistake in the class? The times when I wish I wouldn’t have said something I said? When I look back and am disappointed with myself? That’s when I need to remember, when you need to remember that we have worth. That we were not a mistake. That a good God has good plans for our life (Jeremiah 29:11). When I settle into that heart attitude and that trust in God that He loves me no matter what, I can lose the negative self-talk. I can move forward from mistakes and they don’t hang on me like a weighted backpack that I can’t seem to get rid of.
You might be facing tough circumstances at home, at work, in life, in health, etc. And if you aren’t right now, you will be at some point. That’s life. It has ups and downs. I believe it is no accident that at this very moment God is planting the truth in your heart that you have worth. When life feels rough, it can be so hard to hang on to that truth! But begin to settle it now. Ask Him how He sees you. Let Him tell you about the masterpiece that He created you to be. Look in the mirror and remember that you are the workmanship of God. And though ups and downs, that foundation of Whose you are will carry you through.

A generation of people is regarded as all of the people born and living at about the same time, regarded collectively. But there is so much more to it! Each generation has its own culture… its own fashion, music, and vernacular lingo.
There are currently six generations still alive in America today. The oldest of which is the GI generation: those born from 1901-1926 to children of World War I who went on to live through World War II. They remember living through the Great Depression and have generally been regarded as community-minded, strong individuals with deep loyalties. The Mature (or Silent) Generation were those born between 1927-1945 growing up in a world of conformity and structure but later embracing postwar peace. This generation is known for their strong morality and near-absolute standards of right and wrong. Baby Boomers arrived on the scene between 1946 through 1964 and embraced peace, love, and happiness with optimistic and opened minded personalities. Generation X was born from 1965 to 1980. History will remember them as entrepreneurial and very individualistic.
Enter Millennials. Those born between 19812000. Born in 1983, I guess that makes me a millennial, although, truth be told, I have never identified as such. From birth, we have been told we are special and we expect the world to treat us that way. Each generation wonders whether or not the generation before them was the best. I contemplate frequently about my parent’s generation. Baby boomers…. hippies and freelove seem to speak to the soul. My parents idolize their World War II parents, calling them “the greatest generation” ever to live. America is also a melting pot, with immigrants reshaping our cultural and generational landscape for the better.
To hear the word millennial nowadays is almost associated with a bad connotation. But what if these millennials were evolving into quite possibly one of the best generations to come? Meet Generation Z. Look out millennials… we may be in for a run for our money. Generation Z-ers have grown up with computers and web-based learning. Five-year-olds now know more about cellphones and laptops than we did finishing college. As each generation contemplates the impact they will leave on society and the world,
it helps to see those working so hard to make a difference.
One such young man is Nalin Dang. Nalin is a senior at Randolph High School with aspirations of helping to reshape not just our community but quite possibly the world. Nalin became inspired by his grandmother’s journey to find, not just adequate, but exemplary memory care for dementia. As his family pulled together to find effective treatment, particularly at home for an affordable price, Nalin, at 17-years-old, realized the Tennessee Valley did not yet have such a program in place. Most teenagers would have acknowledged this and moved on. Struggles of homework and teenage responsibilities are enough to keep any high school student busy, right? But Nalin decided to build his own in-home memory care program when his grandfather was later diagnosed. Nalin’s grandfather thrived with the program. The family was thrilled with the results, so Nalin then made the choice to dedicate more time and energy into creating a program to offer memory care assistance to others in need, free-of-charge.
In 2017 Nalin launched We Can Remember HSV. We Can Remember is a non-profit organization created to help those in need to maintain or improve their memory function over time. Memory loss affects the majority of our society’s elders. These members of society are some of our greatest national resources. They hold stories and information that educate us on our history, helping us understand just why we are the way we are. Nalin sees them as national treasures and works tirelessly to ensure their mental capacities and strengths are optimized. He appreciates that some of our greatest lessons can be learned from these older generations. We Can Remember is an eight-week program offering specialized memory care exercises based on the severity of impairment. Nalin’s goal throughout the program is to help the individual recall more of their memory. Ongoing in-person memory exercises will continue to minimize forgetfulness and aid in maintaining function. Nalin and his team of volunteers strive to complete the program in four weeks, but work as long as it takes to achieve improvement in their patients. Each patient session has various memory exercises. A volunteer from We Can Remember is sent to the elder’s house to work on improving memory skills through specific games and activities, making the lesson both helpful and enjoyable for the participant.
I made the (wrong) assumption that Nalin had created We Can Remember as part of a school project or extra-credit assignment. That will teach me to assume. Nalin dedicates countless hours of his free time to work for those with memory impairment. He is a family oriented young man with hobbies not unlike those of other
teenagers. He enjoys hanging out with his friends and several extra-curricular activities. His role models are his parents, Paul and Neeta Dang, both local physicians. He is quick to say he is not exactly sure what direction his college ambitions will take him, but that he is intrigued by neuro-science and hopes one day this passion will manifest into a career. He is also inspired by Stephen Hawkins and both his physical and intellectual journey through life. Nalin finds it admirable that he never let his physical impairments, with all the struggles and doubts they entail, derail him from studying the origins of the universe. Nalin is also greatly inspired by his older siblings, Rajan, Sumeet, and Sabina: a physician completing his ENT residence at Washington University in St. Louis, a Harvard law graduate, and a medical student at Vanderbilt respectively. Nalin tutors piano in his spare time. He has also volunteered at Clearview Cancer Institute and Manna House. Clearview later brought him on as a medical assistant to help in a research study involving Multiple Myeloma.

George Santayana once said, “Those who do not learn history are doomed to repeat it”. After getting to know Nalin Dang, I think he not only embraces this concept, but is actively making strides to ensure that our generations with the most knowledge of our history are able to access the great gift they bestow. In this age of coming into our own and creating makeshift confidence, it’s refreshing to see a young man use not only his intellectuality, but also his free time to make the world a better place. Nalin Dang and the Generation Z he represents is serving up some pretty stiff competition for the rest of us.
For more information on We Can Remember please visit www.wecanremember.com.







 by Brian Baer
by Brian Baer
Vector-borne diseases are diseases that are transmitted to humans by living organisms. Mosquitoes are the best known disease vector. Others include ticks, flies and fleas. These diseases are very serious and can be fatal. In the United States, vector-borne disease cases are increasing and include West Nile and Zika viruses, Lyme disease and spotted fever.

Vector-borne diseases are caused by parasites, viruses and bacteria that are transmitted by these insects. Every year there are more than 700,000 deaths from mosquito-transmitted diseases.
Prevention is the key against contracting these diseases and using insect repellents is the best weapon. In the current repellent market, the majority of people believe that products containing DEET are the most effective. However, they also know that DEET is an oily, smelly chemical, not safe for children or pregnant women and has serious, potential health impacts. Most consumers just don’t know there is anything else they can use.
Some repellents offer different chemistries such as IR3535, Oil of Lemon Eucalyptus and natural and essential oils. Although products with these ingredients are DEET-free, they still do not offer the effectiveness or skin-friendly feel consumers are asking for. Fortunately, there is a truly safe, highly effective and healthy alternative to DEET and other chemistries called Picaridin. Picaridin is an EPA approved repellent that is synthetically derived from the pepper plant (piperine family). It is non-oily, not greasy, has no odor and is safe for adults, children and pregnant women. Products containing Picaridin are being introduced to consumers and leading the way is Zone® Insect Repellents.
The EPA has recognized Picaridin as a highly effective repellent and the CDC (Centers for Disease Control) and the World Health Organization (WHO) have endorsed Picaridin as the preferred repellent chemistry in the world.
Zone Insect Repellents are made with 20% Picaridin, gentle skin moisturizers and have a light, clean scent that smells nothing like other repellents. Zone Insect Repellents are EPA registered and proven effective worldwide for 12hour protection against mosquitoes, ticks, flies, fleas, chiggers, gnats and no-seeums. They are safe and are simply the best repellent products on the market today.
Zone Repellents are currently in Home Depot, Amazon and on the website at www.zonerepellents.com.Do you feel clicking, popping or grinding when you are eating? Do you limit how wide you open your mouth because of pain in the jaw? Do you feel like your teeth don’t quite fit together right? These can all be symptoms of temporomandibular dysfunction or TMD. Headaches, ear pain and even neck pain can also be symptoms of TMD as well.

The temporomandibular joint (TMJ) is where the lower jaw attaches to the head. This hinging joint allows the lower jaw to move up and down so that we can talk, eat, and yawn. Like any other joint in the body, if it is not moving correctly it can be painful. Symptoms may be intermittent, or they may be persistent. Often, we will accommodate to the pain by altering our movement, chewing on the other side or limiting how wide we open our mouth.

Overactive muscles that control the movement of the jaw are often a major source of the pain associated with TMD. Muscles that stay contracted all the time become painful. Clinching of the jaw is a problem that many people with TMD have and may not even realize it. Some people clinch or grind their teeth while sleeping. Your partner will usually let you know if you are grinding because the sound will wake them at night. But many people are clinching during the day and have no idea. Your top teeth and bottom teeth are not supposed to be in contact with each other at rest. This is a form of clinching and it keeps the muscles that control the jaw in a constant state of contraction. If you find that your teeth are in contact with each other on a regular basis, try to allow the lower jaw to relax. Make a note
to gently move your jaw up and down as well as side to side for a few seconds throughout the day. The movement may help to allow the muscles to relax and limit the contact of your teeth. Popping and clicking may also be noted with TMD. Reasons for this could be related to the disc that is in the joint or possible changes to the surface of the joint. The disc plays an important role in the function of the joint and when displaced can be a source of pain as well.
Headaches and neck pain are often associated with TMD due to the hyperactivity of the muscles. High stress levels and poor posturing can create further tension in the muscles of the jaw, neck, shoulder and head.


Treatment for TMD comes in several forms. Your dentist may be able to make a splint that helps to position the jaw and relax the muscles. Some people may require orthodontic intervention for correction of the bite. Worst case scenarios may even require surgery, though that should always be the last option.
As a physical therapist, I treat pain related to joint disorders throughout the body. The TMJ is no different. A course of physical therapy treatment for TMD pain includes a thorough evaluation to determine the best course of action. Treatment by a physical therapist for this pain should include education for posture, foods that place less stress on the jaw, and avoidance of activities that are keeping the muscles hyperactive. Manual treatments are used to help the muscles to relax and exercises are performed to normalize movement of the joint as much as possible. Modalities such as heat or ice may also be beneficial to decrease pain. The cervical spine needs to be addressed to look for abnormal movements as well. If you suffer from symptoms like this, ask your doctor, dentist or physical therapist if a course of physical therapy treatment is right for you.










For nearly a decade Dr. Curt Freudenberger has utilized the Medtronic Prestige LPTM cervical disc system, an advanced technology indicated in skeletally mature patients for reconstruction of the disc from C3-C7 following discectomy at one or two contiguous levels. According to a Medtronic representative, Dr. Freudenberger implants the largest number of Prestige LPTM cervical disc systems in the southeast region. Building on his vast experience in cervical disc replacement, Dr. Freudenberger brought Alabama its first case utelizing the 3rd generation lumbar disc ActivL for treatment of chronic low back pain.

Living in a high-tech community, driven by innovation; it’s no surprise that our medical providers demenstrate advancements in their daily practice. On June 6, 2019 – Huntsville surgeon, Kurt Fruedenberger, MD performed a lumbar disc replacement using a 3rd generation activeL. This newly introduced implant will be a game changer for our area spine surgeons. In fact, it once again puts Huntsville on the map as the first city in Alabama to offer the latest generation Aesculap artificial lumbar disc, a disc designed to address chronic low back pain caused by degenerative disc disease. In contrast with other treatments such as spinal fusion, the activL Artificial Disc is designed to more closely mirror the natural movement of the healthy human spine following surgery.
surgery. In clinical studies, patients who received a lumbar artificial disc were three times less likely to have adjacent level problems five years after their procedure than patients who received a fusion. “Not every patient is going to be a candidate for this procedure and that’s OK,” said Dr. Freudenberger. “Fusion isn’t a bad procedure, if it is indicated. Still it’s important that patients have access to providers and facilities that will consider the best option for each patient’s anatomical needs.”

Aesculap Implant Systems, LLC, a B. Braun company, is part of a 175-year-old global organization focused on meeting the needs of the changing healthcare environment. Through close collaboration with its customers, Aesculap Implant Systems develops advanced spine and orthopaedic implant technologies to treat complex disorders of the spine, hip and knee. Aesculap Implant Systems strives to deliver products and services that improve the quality of patients’ lives. For more information, call 800-234-9179 or visit aesculapimplantsystems.com.
450,000 Americans will have spine surgery each year because of chronic low back pain. “Lost work time due to chronic back pain is something that many of my patients are significantly concerned with and for good reason,” said Dr. Freudenberger. By the time that chronic back pain patients seek out surgical options for their chronic pain, studies have shown that 30% are narcotic dependent and out of work.
“For me, the evidence for motion preserving surgery like this one made sense. I saw that there were benefits to the procedure that would help some of my more active patients,” said Dr. Freudenberger. Fusions have been associated with causing patients with low back pain to start experiencing pain at levels adjacent to their initial fusion several years after their
The literature supports that within six-months of lumbar artificial disc surgery more than 86% of back pain patients will go back to full-time employment without restrictions and because of their decreased pain and increased function will be able to stay off narcotics. “The activL trial found that 98.5% of lumbar disc patients are still narcotic free more than five years after surgery,” said Dr. Freudenberger.
“The benefits of artificial lumbar disc replacement have been equal to my experience with cervical disc replacement. My patient was up and waking the same day of surgery with her old pain completely gone,” he said. “In addition to addressing painful symptoms caused by degenerative disc disease, minimizing recovery time, preserving disc space between the vertebrae, maintaining range of motion in the spine, and reducing the possibility for future surgeries are all key factors when thinking about surgical options for patients. Artificial disc replacement accomplishes these goals and allows patients to get back to the activities they enjoy.”









 BY MICHAEL T POTTER
BY MICHAEL T POTTER
Shortly before Christmas 2018, I was recovering very well from a lumbar procedure done in mid-October. But the day after New Year’s 2019, I began to have discomfort in my lower spine. Within two days, I was back to using a cane.
By the 4th day, I had digressed to needing a walker. Our son-in-law (Justin Tarr), who works for Dr. Freudenberger at SportsMed, scheduled me an appointment for Monday the 7th of January. As we got ready to go that morning, I collapsed on our bathroom floor - my legs lost their strength. Thankfully, Patricia (my wife) had alerted several neighbors to be on standby in case we needed help. So, within minutes, she had two big guys helping me out the door and into the car. We gave Justin a heads up to meet us with a wheel chair.
The fifth lesson is to take the time to see the big picture and wake each day with a sense of purpose. Centenarians in the “Blue Zones” still have daily goals and ways they still contribute to their communities.
Lesson 6: Downshift
Lesson number six is to take the time to relieve stress. Each of the “Blue Zone” communities has daily or weekly rituals which allow them to disconnect from being busy. They slow the mind. They relax with family and friends.
Lesson seven is to participate in a spiritual community. All of the “Blue Zone” centenarians have deep faith and belong to active religious communities. The Sardinians and Nicoyans are Catholic. The Okinawans have a blended religion. Ikarians are Greek Orthodox, and most people in Loma Linda are Seventh-day Adventists.
Lesson 8: Loved Ones First
functions. Less than 3 months post-op, I am walking without the need of a brace, nor do I need a cane all the time. I feel that I am more than 85% back to normal.
The day after my 2nd surgery, I redeveloped some cardiac rhythm issues that extended my stay in Crestwood a total of 11 days! Hence, we experienced the care of both the orthopedic and cardiac staffs at Crestwood. In addition to the skills of my surgeon & his team, I, and my family, cannot adequately express our heartfelt gratitude to the hospital staff. The nurses and tech crew, the cardiac and hospitalist doctors were all customer-focused and professional. Even the facilities maintenance folks were attentive. Department managers would frequently stop by to see if we needed anything. The hospital system Crestwood has created is simply better than anything we have experienced anywhere. While I was glad to finally get out of the hospital, my wife and I truly missed the people we met and befriended. We often talk about them and how caring they were to us.
Lesson number eight is to make family a priority. In the “Blue Zone” communities, centenarians have a strong sense of duty when it comes to family. They live close together and have established family rituals or traditions. Shared meals and activities play an important part of their everyday lives.
We arrived at SportsMed around 9:30 AM and after a brief consult, Justin did his SportsMed “magic” and I had an MRI in record time. As soon as Dr. Freudenberger saw it, he came in and told us that he suspected an intrathecal disc herniation, but would not know for sure until he operated on me. The initial plan was to do a fusion of my affected vertebrae and remove the disc material - I was admitted to Crestwood by noon. We were not aware that this type disc herniation was both rare and serious.

From our experience in October, we had trust in Dr. Freudenberger’s skills and his intelligence – the man is a logical thinker and a brilliant surgeon. We knew his deductive reasoning would always focus on the best outcome for me as a patient.
The last lesson is to surround yourself with people that share “Blue Zone” values. These people are your tribe. “Blue Zone” communities have close social circles that they count on in difficult times and with whom they create strong bonds of friendship.
Tuesday morning’s surgery did indeed affirm that I had an intrathecal herniation and there was material inside the thecal sack. However, after completing the T-LIF fusion, Dr. Freundenberger suspected I had additional disc matter still inside my spinal cord that was not visible. He judged, however, it was not worth the risk of continuing the operation with exploratory surgery.
If you have any interest in living long and living well, I encourage you to pick up a copy of this book. It’s full of valuable information and inspiring stories. After you read it, share your ideas of “Blue Zone” communities with others.

Now, I am recovering as well as one could hope. Looking back on this experience is a constant reminder of how truly blessed we are. Every aspect of this “adventure” could not have been better scripted in our favor.
Drs. Freudenberger and Dixit operated as a team to perform the spine surgery.
Dr. Freudenberger is an orthopaedic spine surgeon specializing in degenerative spine, spine trauma, disk herniation, complex spine situations and minimally invasive surgeries.
Dr. Dixit is a board certified neurosurgeon specializing in the treatment of both brain and spine disorders with an emphasis on minimally invasive therapies.
For more information visit Traci’s blog at tracimccormickmd.com
To satisfy his suspicion, an MRI was ordered for Wednesday morning and more disc material was indeed discovered. Neither Dr. Freudenberger, nor any of the surgeons he knew, had operated on this type herniation. But he was confident he could do the surgery and assemble the right team to make it happen. After discussing all the options available to us, we decided to have a second surgery on Thursday afternoon.
It was then that the severity of my situation hit our family - potential paralysis, loss of bladder and bowel functions were all real possibilities. It would be impossible to enumerate the fear-provoking scenarios that ran through our minds. My wife and I had experienced her father becoming a paraplegic and living with that condition for 28 years. We didn’t have to work very hard to envision the negatives of being paralyzed.
old 100 years
Our pastor happened to be paying us a visit at the moment we found out the MRI results. I’m not an emotionally religious man, but I know that at some point one must realize we are not in control of every outcome. We must lay that worry at the feet of our Maker and trust in God, as well as the medical professionals we had on our side. We had done all we could and had the best medical support for which one could hope. I’ll never be able to express the calm I felt once I simply trusted in my faith.
Thankfully, the Thursday surgery was a success! I had no paralysis and full control of my bladder and bowel
we had trust in Dr. Freudenberger’s skills and his intelligence – the man is a logical thinker and a brilliant surgeon.

There is no question that exercise is good for just about every body system. When we work out, oxygenated blood showers our brain cells, stimulating the release of “feel good” endorphins which provides euphoria and calming effects while improving connections between neurons. Exercise allows our hearts to pump more forcefully and efficiently, increasing perfusion to vital tissue and organs. Perhaps the real reason Dorothy’s buddies, Tin Man and Scarecrow, received their respective heart and brain was the cross-country trek across Oz. Maybe the Wizard was a metaphor for exercise?? Probably best to not over analyze… Long term effects of exercise on our skeletal system includes increased bone density which helps to ward off osteoporosis while also making us more flexible and less susceptible to injury.
To say I am not athletic is an understatement. In high school, I was the slowest person on the track team. The walk-on track team. I actually never finished a race. Full disclosure, I wanted my picture in the yearbook wearing a track shirt. Who knew you couldn’t show up to your first track meet without practicing and not go home with a gold medal?! Movies make it look so easy!
My love-hate (mostly hate) relationship with exercise only deteriorated from there. I finished a 5K in 48 minutes once. I would begin a walking regimen each morning only to start slapping “snooze” on my alarm a few days in. I was your stereotypical New Year’s Resolutionist. Quit drinking soda. Check. Take my multi-vitamin. Check. Go to the Gym. Well… I would… but my neighbor’s friend’s cat might need a bath… so I better be available.
My aversion to sweat and athletic pain would change in 2013 after a girlfriend dragged me (nearly kicking and screaming) to a new form of group exercise. Friendly agile instructors guided me through a 50-minute class utilizing the ballet barre to pinpoint specific muscle groups using small isometric movements to lift, tone, and burn not only my physique but my attitude about exercise as well. During the first class I felt like a baby walrus trying to dance her way through a pool of Jell-O. But with each class the movements became easier and I became stronger. The instructor’s gentle guiding voices coached not only my muscles and core but my mental health as well.
Owners of Pure Barre Huntsville, Angelica Lee and Susanna Chesser, share a passion and enthusiasm for helping their clients achieve total body workouts fueling both physical fitness and self-esteem. Angelica explains that “Pure Barre is a total body workout that uses the ballet barre to perform small isometric movements which burns fat, sculpt muscles, and creates long, lean physiques. It is the fastest, most effective, yet safest way to change your body in just a 50-minute workout.” But to Angelica, Pure Barre represents so much more. It is a sense of community, a sense of belonging, and a sense of self-awareness. Pure Barre provides a positive environment where her clients can come to class, work on their well-being and lift each other up mentally. “The technique strengthens your body and also your mind” Angelica emphasizes. “You can do anything you put your mind to. To me, the hardest part about Pure Barre is walking through the doors, showing up and allowing yourself to push through each class.” Angelica took her first Pure Barre class and was blown away with how difficult and challenging it was. She didn’t come back for six months. She remembers thinking, "who wants to do that?"... But months later after her regular work out had plateaued, she decided to give Pure Barre another chance. “I came back for my second class and was hooked. I attended 5-6 classes every week for 6 months and then became an instructor. I have been teaching Pure Barre since May 2012 and then pursued ownership of Pure Barre Huntsville with my best friend, Susanna Chesser, in October 2018.” She recommends her clients “show up ready to work and with the mindset that you will definitely see results...not just physically, but mentally. Don't ever give up on yourself!”
Owners of Pure Barre Huntsville, Angelica Lee and Susanna Chesser, share a passion and enthusiasm for helping their clients achieve total body workouts fueling both physical fitness and self-esteem. For more information, please visit them on the web at www.purebarre.com/ al-huntsville/ or call (256) 655-1544.
Susanna Chesser grew up as, what she would consider, a very athletic, healthy person. However, after college, the challenges of becoming an adult had turned her into the unhealthiest version of herself - both physically and mentally. “When I walked through the doors of Pure Barre Huntsville in 2013, I was greeted with a positive energy, welcoming faces, and a workout that totally and utterly kicked my tail. What an eye opener! It was this humbling experience along with the sense of community that brought me back for the next class. I was determined to find the strength that I had once known. Within just a few classes I began to feel like myself again. After 6 months I had lost 25 pounds and genuinely felt I had found my tribe.” Five years later, the same passion for Pure Barre that led her through the double doors, led her to purchase the franchise with her best friend Angelica. “For me, working out is not just about the physical benefits; it is about relieving stress, focusing on a goal, surrounding myself with a community of friends, and creating ALL those endorphins. We strive to create an environment where anyone can walk through the door and feel welcomed and walk out the door feeling like the very best version of themselves.”

Many of us rely on taking a pill for any medical ailments that comes along. If ever there was a “magic pill” for youth and vitality, staying physically fit would be it. The phrase raising the bar encourages us to set tougher goals and increase standards. Pure Barre encourages us to raise the standards of quality and exceptionalism in our personal journey to physical and mental health.



We all learn this rhyme in our youth. It implies a distinction between pain arising from a physical attack and pain associated with language. We are challenged to remain stoic in the face of insulting words; to not allow language to crush us. For centuries we have believed the physical and the mental are separate spheres of our existence. Brain research in the past 15 years, however, has started to reveal both physical stimuli and language affect the brain in similar ways. Language can touch our deepest neuronal reality.
Functional magnetic resonance imaging (fMRI) is a scanning technique that detects brain blood flow changes associated with increased neuronal activity. Functional MRI has been used to reveal regions of the brain activated by a painful stimulus, areas that have been collectively termed the “pain matrix.” Imaging studies [1] have revealed the pain matrix is stimulated not only by painful physical events, such as laceration with a knife, but also by words describing pain such as “excruciating,” “grueling,” and “paralyzing.”
In another experiment [2], these same pain words versus neutral words were shown to people before an electric shock was applied. Increased pain ratings were reported following an electric shock if the participant was primed with a pain word as opposed to a neutral word such as “cubic.” These results confirm the popular intuition that a pre-existing negative attitude can tinge our perception and experience of an event. In colloquial terms, everything in the world is darker if you perpetually wear sunglasses.
Chronic back pain is one of the most common conditions seen in a pain management clinic. A research study [3] revealed chronic back pain patients have
an increased response in the brain pain matrix on fMRI to pain words compared to normal people without back pain. Those tortured by chronic pain are more vulnerable to piercing words than those without the affliction. There is a vicious circle regarding physical pain and pain language. Both stimulate the brain pain matrix. Pain words preceding physical pain can increase the intensity of pain. Chronic physical pain can amplify the reaction to pain words. The pen and the sword; each alone can cause suffering and together they can perpetuate it. As a pain management physician, I wonder how can we interrupt the cycle and release the patient from the vortex of suffering?
Cognitive behavioral therapy (CBT) is a psychological technique that draws upon the ancient philosophy of Stoicism. Epictetus, a famous stoic philosopher, once said “Men are disturbed not by things, but by the views which they take of them.” CBT aims to shift the locus of control to the patient herself; to empower her to recognize and change distorted and destructive thoughts in the here and now that affect her behavior and pain response. CBT can help a patient reframe her chronic pain and relationship with it. An imaging study [4] using fMRI indicated that CBT can change the brain pain matrix and decrease pain. So we return to the last part of the above childhood rhyme: “…but words can never hurt me.” Perhaps with the aid of CBT and Stoic philosophy we can change how language affects pain. The following quote is attributed to the Nazi concentration camp survivor Dr. Viktor Frankl:
References
1. Richter M, Eck J, Straube T, et al. Do words hurt? Brain activation during the processing of pain-related words. Pain. 2010 Feb;148(2):198-205. doi: 10.1016/j.pain.2009.08.009. Epub 2009 Oct 28.
2. Richter M, Schroeter C, Puensch T, et al. Pain-related and negative semantic priming enhances perceived pain intensity. Pain Res Manag. 2014;19(2):69–74. doi:10.1155/2014/425321
3. Ritter A, Franz M, Puta C, Dietrich C, Miltner WH, Weiss T. Enhanced Brain Responses to Pain-Related Words in Chronic Back Pain Patients and Their Modulation by Current Pain. Healthcare (Basel). 2016;4(3):54. Published 2016 Aug 10. doi:10.3390/healthcare4030054
4. Shpaner M, Kelly C, Lieberman G, et al. Unlearning chronic pain: A randomized controlled trial to investigate changes in intrinsic brain connectivity following Cognitive Behavioral Therapy. Neuroimage Clin. 2014;5:365–376. Published 2014 Jul 23. doi:10.1016/j.nicl.2014.07.008
“Between stimulus and response, there is a space. In that space is our power to choose our response. In our response lies our growth and our freedom.”
 by Salpy Pamboukian, MD Director, Mechanical Circulatory Support Device
Program and Women’s Heart Health Clinic
The University of Alabama at Birmingham
by Salpy Pamboukian, MD Director, Mechanical Circulatory Support Device
Program and Women’s Heart Health Clinic
The University of Alabama at Birmingham
Option 4: Even your options have options! Try a combination of the three. Many people elect to have a small nasal procedure combined with quitting Afrin, or using short-term oral steroids and/or switching to non-addictive medications like nasal steroid sprays as well as safer herbal remedies like Xylitol sprays.
Be sure to discuss your treatment options as well as alternative medications with your primary care doctor or ENT. Patient expectation is CRUCIAL. When using intranasal steroid and antihistamine sprays, a butter knife is not going to cut like a machete! But how do you eat an elephant? One bite at a time!
With approximately 10,000 practicing physicians in the state of Alabama, there is a vast community of doctors dedicated to providing superior care and striving to improve outcomes to an estimated 5 million Alabamans.1At times, health conditions may arise that require a patient to be referred to a medical specialist outside of their community, such as a cardiologist.

“Kari Kingsley, MSN, CRNP is an otolaryngology nurse practitioner with over 8 years of ENT experience who currently works at Huntsville ENT (256-882-0165). She is a medical writing consultant for Inside Medicine and enjoys writing articles on pertinent material to keep the residents of North Alabama up to date on the forefront of medicine.”
Given the close and trusting nature of physicianpatient relationships, it can be a difficult but necessary decision to refer a patient to a colleague for treatment of more advanced or complex conditions. It’s important to recognize that referring a patient is not a negative reflection on the referring physician, instead quite the opposite: understanding that a patient might need more integrated or specialized care. Quite simply, a referral can help a patient not only get a second opinion, but an additional assessment could also offer highly specialized treatment options that could be the difference between life and death.
According to a report in the Annals of Family Medicine, every year 45% of physicians receive new patients through referrals. In my role as a cardiologist at The University of Alabama at Birmingham, I work with a team who sees patients daily with advanced stage heart failure and were referred by other physicians. Frequently, these patients need treatment options or interventions that go beyond what can be provided by their primary care physician or general cardiologist. Unfortunately, heart failure is prevalent in Alabama, with heart disease being the leading cause of death throughout the state.2The good news is that many new treatment options have emerged in the last decade that can positively impact on both survival and quality of life. Consultation with a specialized advanced heart failure cardiologist like myself can determine which treatments are right for a particular patient. It is important to remember we are not taking the place of the local physician. We partner with referring doctors to make sure patients are receiving the most up to date treatments.

Advanced heart failure patients may experience shortness of breath, fatigue and other symptoms, usually with activity, but sometimes even at rest. Of the approximately 6 million American adults living with heart failure, about 10% have an advanced form of the disease where their hearts are not strong enough to adequately pump blood through the body.3

Heart failure is often diagnosed only when it begins to have serious health consequences. In a worst-case scenario, the disease goes unrecognized and advances to the point where a referral to a specialist is too late. This is because heart failure is largely misunderstood (even within the medical community) and often the risk factors are not identified or treated early enough. Patients in an advanced stage of the disease can require significant interventions to extend their life expectancy – but often require a patient be healthy enough to complete and recover from the Options for Advanced Heart Failure Patients
As a specialist, I depend on referrals to ensure I’m seeing heart failure patients early and often, as this allows for comprehensive care and medical intervention options that can offer the best possible patient outcomes. When advanced heart failure patients visit me, my primary focus is to provide the patient with a treatment plan that can potentially extend the patient’s life and improve the quality of that life.
Heart failure progressively becomes more difficult to treat, meaning treatments that had been used in the past often no longer work. At this point in the treatment journey, intravenous medications may be an option, as well as implanted devices and heart transplants.4 While a heart transplant may seem like an ideal option to get a “new” heart, it’s important to acknowledge that it’s not an immediate or appropriate option for all patients. Some patients may be too ill to qualify for or survive the transplant surgery, and the transplant list is long with a limited amount of donor hearts. Consider this: despite the prevalence of heart failure, in 2018, only 3,400 heart transplant procedures were done in the United States.5
A mechanical heart pump can be a life-saving option for the thousands of patients currently waiting for a heart transplant (known as “bridge to transplant” patients), or for those who are not candidates for heart transplant surgery (“destination therapy”). A mechanical heart pump, such as the Abbott HeartMate 3TM (www.heartmate.com), can help restore blood flow throughout the body. This option, as well as other available life-saving techniques, can help improve a patient’s length and quality of life, but requires commitment from the patient, as well as their support network and other physicians, to ensure a safe recovery and longterm survival.

As physicians, it is our duty to provide patients with the education necessary to understand various risk factors and diagnoses, and to ensure we have an awareness of the available physician network, including the myriad of specialties that can diagnose and treat complex, advanced or rare conditions.
We can improve the likelihood of a referral if we are educated about the diagnosis and treatment options that a specialist may present to our patient, as we help prepare and educate the patient about the potential path forward. Ultimately, we want to help patients feel empowered to make informed decisions about their health. Additionally, patients need to take an active role in their own health care and communicate with their doctor if they feel the time has come to seek a second opinion or specialized care. It is also critical that a referral comes when the patient is stable and not experiencing a medical emergency as this allows the doctor and the patient to make the most informed decision possible.
As a physician community comprised of various specialties, it’s our collective responsibility to embrace the old adage that two minds are better than one, and sometimes an outside opinion or expertise is necessary to ensure quality patient outcomes. Strong relationships connecting the physician community can further help improve interdisciplinary care for patients. It’s important to remember that the right referral at the right time can dramatically change the course of a patient’s treatment, as I’ve witnessed numerous times with my heart failure patients.
1 Association of American Medical Colleges. Alabama Physician Workforce Profile. Retrieved from: https://www.aamc.org/download/484510/data/alabamaprofile.pdf
2 Alabama Public Health. Cardiovascular Diseases. Retrieved from: https://www.alabamapublichealth.gov/healthrankings/cardiovascular.html
3 American Heart Association. Living With Heart Failure and Managing Advanced Heart Failure. Retrieved from: https://www.heart.org/en/health-topics/heart-failure/living-with-heart-failure-and-managing-advanced-hf
4 WebMD. Treatment Options for End-Stage Heart Failure. Retrieved from: https://www.webmd.com/heart-disease/heart-failure/end-stage-heart-failure-treatments#1
5 United Network for Organ Sharing. Transplant Trends. Retrieved from: https://unos.org/data/transplant-trends/
-an estimated 27 million people are considered slaves with the average victim being between 12 and 14 years of age.



There’s no time like the start of a new year to work on a new you! TherapySouth can help you heal, move better and overcome the challenges of your physical life. If you haven’t tried physical therapy for the things that keep you from moving without pain—we’re here for you! We can help you get back to the things you love.

TherapySouth is an outpatient physical therapy practice with a fun, family-oriented environment. Our experienced physical therapists know our patients by name and strive to help you achieve your physical goals. You don’t need a doctor’s referral to see a PT, so give us a call today! Huntsville 6485 University Drive, Suite C | 256.513.8280 www.therapysouth.com

and function of the Attune total knee improve the daily life of my patients vs total knee implants I have used in the past. My patients gain early post-op exion, greater overall range of motion and stability. Many patients insist they ”forget” they even have a total knee implanted. -Jack Moore, MD











Patients implanted with the ATTUNE® Knee have reported improvements in the following outcomes: stability, function, range of motion, and reduced pain.1 The ATTUNE Knee can help you get back to your life and pursuing your passions


1. Hamilton WG, Brenkel, I, Clatworthy M,, Dwyer K, Gibbon A, Kantor S, Lesko J, Himden, S. Early Outcomes with a New primary TKA system vs. contemporary TKA: interim results of two worldwide, multi-center prospective studies. American Academy of Orthopaedic Surgeons (AAOS), San Diego, California. March 14-18, 2017; Poster #106. Other implants tested: SIGMA Knee (DePuy), NexGen® (Zimmer), Triathlon® (Stryker).
2. Etter K, Lerner J, Kalsekar I, de Moor C, Yoo A, Swank M. Comparative Analysis of Hospital Length of Stay and Discharge Status of Two Contemporary Primary Total Knee Systems. J Knee Surg. 2017. 1(212): 1-10. DOI https://doi.org/10.1055/s-0037-1604442.
3. Clatworthy, M. (2015). An Early Outcome Study of the ATTUNE® Knee System vs. the SIGMA® CR150 Knee System. DePuy Synthes Companies White Paper. DSUS/JRC/0814/0418. In an IRB approved early outcomes study, physiotherapists collected data on 40 patients implanted with ATTUNE® Knees and 40 patients with SIGMA® CR150 knees. The results demonstrated that patients implanted with the ATTUNE Knee had statistically significant improvements in some early outcomes, other outcomes demonstrated a trend favoring the ATTUNE Knee, and some outcomes were equivalent.
sooner vs. other knee brands.2,3
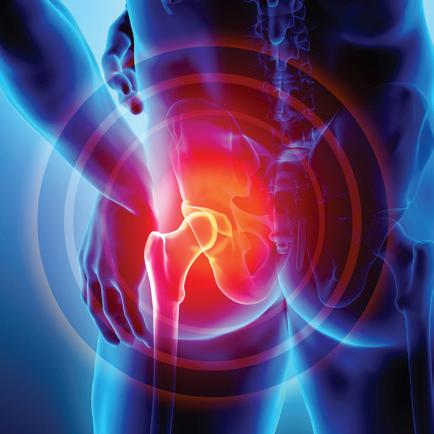
One hip. I should say… one good hip and one bad one. That had been my entire life. Almost 48 years and counting. I was born with a deformed right hip joint. I was put in traction as a baby, then in a cast for 8 weeks. And though I could walk and do all the activities of daily life including exercise, I had always been in some sort of pain or discomfort.

This wasn’t going to be a routine procedure, even for someone as experienced as Dr. Clayton.
My husband, Kevin, and I love to travel. We love to take the children to places like New Orleans, DC, and Chicago. But that means lots and lots of walking. With each trip, it was getting harder and harder to spend the day walking. Advil wasn’t cutting it anymore. My favorite exercise is cross country cycling and even that wasn’t as easy as it used to be. I finally said enough is enough. I cannot continue living like this. I have too many things to do. That’s how I came to know Dr. Matthew Clayton.
Dr. Clayton, my husband, and I talked about the options available. We knew surger y would be an eventuality, but we exhausted everything else first. We did stretching, therapy, and regular cortisone injections. The injections would work for 6-8 weeks at first, but as time went on, they grew less and less effective. It was time to talk seriously about a total hip replacement. This wasn’t going to be a routine procedure, even for someone as experienced as Dr. Clayton. With a deformed hip joint, he wasn’t going to be able to know his exact procedure until I was actually on the operating table. So, we prepared ourselves for any one of three procedures. To further complicate things, it was going to be a posterior procedure. I had been told to be prepared for less flexibility and perhaps even less mobility due to the risk of a dislocation post-surgery. (Dr. Clayton did assure me that I’d be able to return to cycling without any issues.)
Tuesday morning, November 28th, 2017, was the day of surgery. Kevin and I had made all the preparations for
surgery. We had arranged the house to make room for the walker I knew I would be using for the next several weeks. My work knew I would be out for at least 2 months. (I stand for hours at my job.) We were ready to rebuild my hip. The staff at Crestwood are awesome. Dr. Clayton’s team, second to none. As for Dr. Clayton, I’ll let the rest of this speak for his skill as a surgeon.
Dr. Clayton had a primary plan for my total hip replacement. But he also had two contingency plans, but as it would turn out, he didn’t need them. They tell me it took less than two hours to complete the operation. No complications during surgery except for needing just one screw to hold the hip joint cup in place. By the evening I was up walking. Not just short trips to the bathroom, but around the halls of the hospital. We weren’t setting any speed records of course, but I was moving. It took a little bit, but I began to notice something. I didn’t have any hip pain. Sure, I could feel the pain from the incision, but the pain deep in my hip was gone. 48 years of pain was gone in an instant. When Dr. Clayton came in the next morning, I asked when I could go home. After he saw how much I had been walking, he told me I could go home that day. I was ecstatic. So, 33 hours after I arrived at the hospital, I was going home.
But my rapid recovery doesn’t end there. By Saturday, I was moving about the house without my walker. Still moving very slow and being very, very cautious, but sans the walker. By two weeks post-surger y, we were attending a Trans
It took a little bit, but I began to notice something. I didn’t have any hip pain. Sure, I could feel the pain from the incision, but the pain deep in my hip was gone. 48 years of pain was gone in an instant.

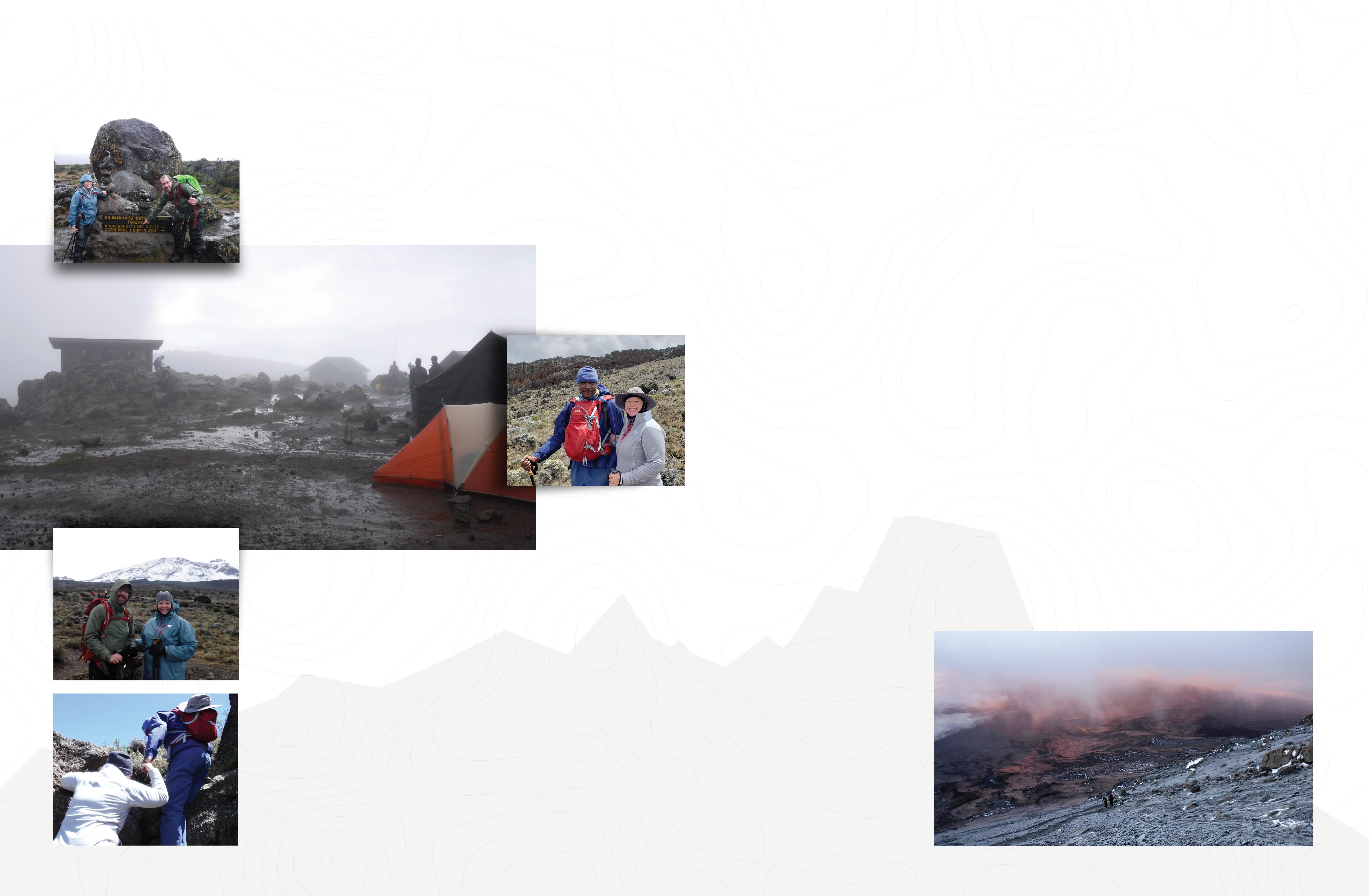
Siberia Orchestra concert where I had to walk up several flights of stairs. (To be transparent, that did hurt a little bit.) By Christmas, there was still a little limp from the incision site, but overall, I couldn’t have asked for better results. I knew that my life was going to be so much better. And more importantly, my husband and I would be able to continue our adventures. And in mid-January (just 6 weeks after surgery), that’s when my husband popped the question. Why don’t we go to Africa and climb Mt. Kilimanjaro?
My husband had wanted to climb Kilimanjaro for years but wouldn’t do it without me. But being the eternal optimist he is, and seeing how well my recovery was going, he knew it was now a doable adventure. My first response was “I can’t climb a mountain.” But as the days went by, and I started to feel better, I was intrigued. So, I did some research. It’s a 9-day, 53-mile trek around the mountain that summits at 19,341 ft. where the oxygen is half of what it is at sea level. Though it isn’t technical, that doesn’t mean it’s easy. It is very hard for everyone who attempts to summit it. Some places are very, very steep. And there are some areas where

you have to scramble over rocks. Altitude sickness is a very real possibility. People do die attempting to summit. But as I read about it, I started to think that maybe I could do this. It took a little more prodding from my husband (along with promising a safari) to convince me to give it a try. And we’d have 11 months to build my strength up. In fact, we would spend my 49th birthday on the mountain.
By late February I was able to begin the process of training for this grand adventure. We started off easy by doing simple hikes. We weren’t going to risk injury or over train. Slowly, methodically, we began to increase the mileage and elevation. And as spring arrived, we added our cycling back in. It felt so good to be able to do all these things without pain. Yeah, my glute was still an issue (I have a 9-inch incision through the muscle). But with every step or pedal stroke I was getting stronger. By May we were either doing 3-hour hikes or riding 20 miles on our bikes. By early June our cycling was up to 35 miles. The strength was back. And I could ride every day without that nagging pain from my hip. On June 30th, we rode 51 miles! And so, it continued for the summer. Except my husband was adding more and more hills for us to ride up. It was at my 6-month post-surgery visit with Dr. Clayton where we told him what we were going to do. He was so excited, we thought he was going to jump out of his shoes.
In August we had a setback. Not from my hip, but my back. A disc had bulged. It was bad. So right after Labor Day, I had my L4-L5 fused by Dr. Curt Freudenberger. This pretty much brought our cycling to a stop for the year. Kilimanjaro was now a question mark. We would have to make a decision by mid-October. I rested my back. I let the fused discs recover.
Mid-October came and I started to get back into hiking. Fortunately, everything felt good. Thankfully, my leg
strength was still good, and we could quickly get our hiking miles back up.
My husband is a physicist and plans out every single detail to the nth degree. He spent every day of the 11 months planning our African trip. So generally, I just have him tell us what we need to plan for, or train towards. But I must say, that as November arrived, my anticipation for what we were about to attempt began to fill my thoughts throughout every day. What would it be like to go to Africa? What would it be like to camp in a tent for 8 consecutive nights? What would the food be like? Could I really climb the highest free-standing mountain in the world?
Finally, the 10th of January 2019 arrived. It had been 408 days since my surgery. Time to fly to Africa. No turning back now. In 4 days, we would begin the climb.
Tanzania is a beautiful country. Yes, it’s a 3rd world country. The average person earns less than $5 a day. But the people are thankful for what they have. They are a very genuine people and are happy to see tourists. They are giving of themselves. They know tourism is an important part of their economy and every person we encountered along our journey went above and beyond anything we could ask. From keeping the restaurant open late our first night so that we could have a good meal upon arriving, to giving us guided tours of the shops and markets simply because we asked to see them. We both made a very concerted effort to learn and use their language, Swahili, and that was worth more than money to the Tanzanian people.
A climb such as Kilimanjaro cannot be accomplished without guides and porters. There were 15 climbers in our group and to support us, we had 2 lead guides, 5 assistant guides, and 47 porters. All the tents, food, and supplies
It’s a 9-day, 53-mile trek around the mountain that summits at 19,341 ft. where the oxygen is half of what it is at sea level.


are carried by the porters. We were only required to carry small backpacks with our water, snacks, and rain gear. And I’m glad that’s all we carried. When leaving the main gate to begin the climb, there is no simple, easy beginning to kind of warm your legs up. Instead, from the first step you climb a series of “steps” cut into the ground that rises at over a 20% incline. For a person who likes a few miles to warm up when cycling, this was a shock to the system. I must admit, that I was questioning my ability to make the climb within the first hour. But with the encouragement of my husband, our
guides (who became our good friends), and my fellow climbers, I trudged on. It certainly didn’t hurt to hear my husband and one our assistant guides singing traditional Kilimanjaro songs in Swahili. Day one is the shortest day. Only about 3 miles through the rainforest. But it ascends just over 2000 ft. Night one was spent at 9500 ft. (You could already tell there was less oxygen.)
Day Two is very similar to Day One. A little longer, but another 2000 ft. in elevation gained. At this time, I’m still questioning my sanity. (And my husband’s!)
Day two starts in the rainforest, but by

the end of the day, you emerge out of it into a more open area known as Moorland. Here is where you get your first view of the mountain. The beautiful snows of Kilimanjaro. Except it was cloud covered until right at dinner time when the clouds cleared, and you had an unobstructed view of this majestic mountain. Seeing what you’re about to ascend is beyond breathtaking. And very motivating.
Day Three is a generally a very easy day. Except for us it was raining the entire way. Only 1000 feet of elevation gain. Of course, this takes you to 12,500 ft. That’s really high!
have learned to live without constant access to your phone or TV and you feel liberated. You have become a part of
Day Four is a unique day. You climb to nearly 14,500 feet then descend back down to 13,500 feet. This is done to help acclimate yourself and keep the dreaded, and potentially lethal, altitude sickness away. It’s also on this day that you begin to think that you’re going to get a chance to summit this mountain.
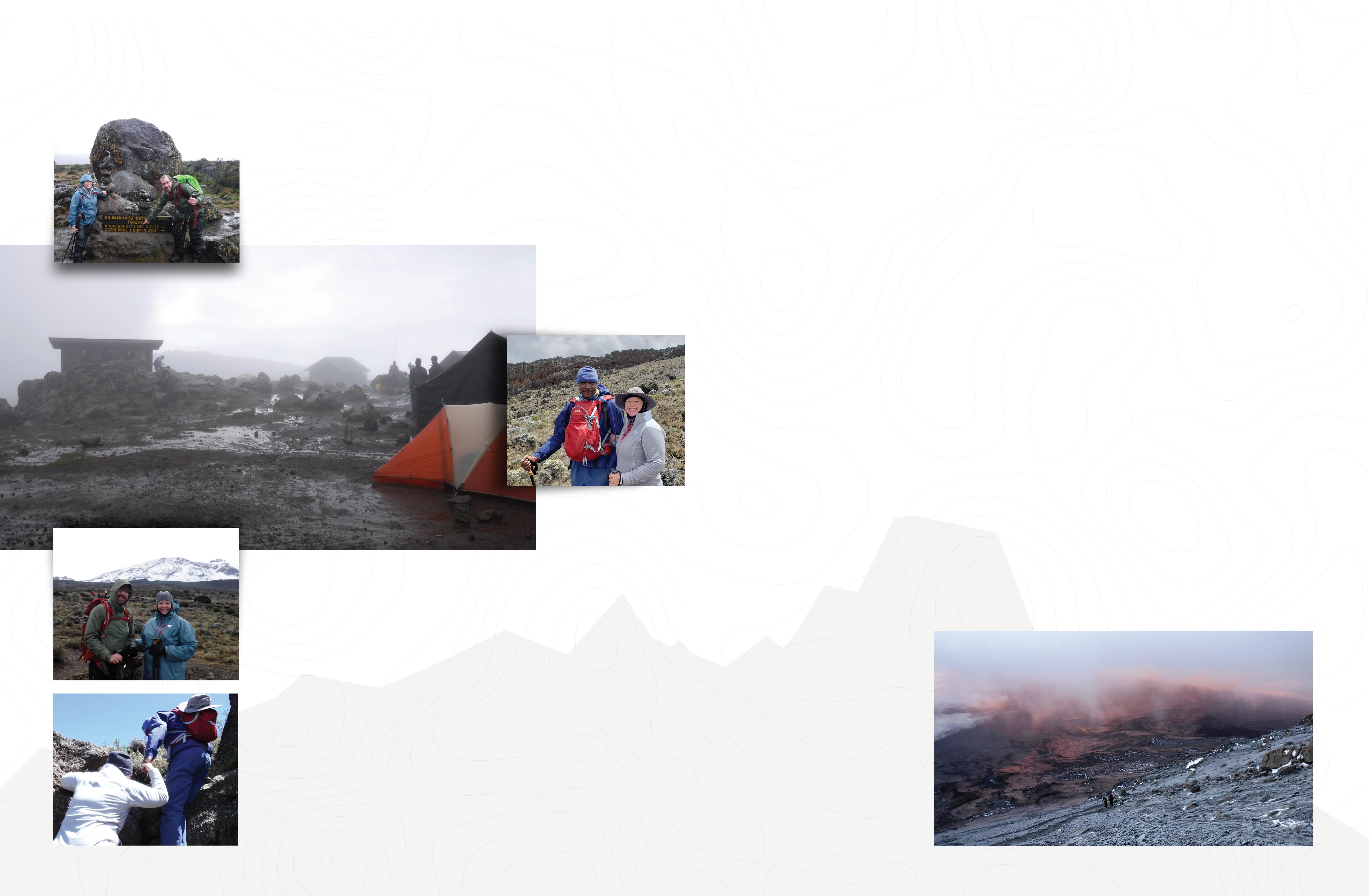
Day Five is the day you spend scrambling over large rocks. It’s the day I needed the most help from our guides. It’s also the day that they assigned our biggest and strongest guide, Mboyi, to my group. They all knew I had an artificial hip and would need to take extra precautions getting up (and down) over these rocky areas. At times Mboyi literally picked me up so that I wouldn’t bend my hip joint too far.
Day Six is the easiest day. A slight descent over a short 5-mile hike around to the north side of the mountain. The mountain begins to loom heavily on you at this point. The apprehension of what summit night will be like. It seems like you could just reach out and touch it, but you knew the hardest was still to come. Tomorrow things would change.
We woke to beautiful weather on Day Seven. After descending the past two days, today begins the continuous uphill journey to summit base camp. We started our day at 12,500 feet and would climb to 15,400 feet. Today is simply about reaching base camp. There are no rocks to scramble over. Nothing to do but place one foot in front of anoth-
[ You
Kilimanjaro.
er. Kilimanjaro is a unique mountain. It makes its own weather. Though only 200 miles south of the equator, it snows yearround. It has glaciers across its summit. It also has 5 distinct ecological zones. Today we would pass through three of them.
By the seventh day, you’re tired. Excited, but tired. The long hours spent walking give you ample time to reflect on life. You think about yourself and how this journey has already changed you. You appreciate life differently. You have learned to live without constant access to your phone or TV and you feel liberated. You have become a part of Kilimanjaro. You are part of the soul of the mountain. And it is part of you. Each step that takes you higher into the rarified air has meaning now. As we passed 14,700 feet we saw firsthand, the snow that had fallen on the mountain on day three. I can’t express how it felt to reach down and feel the cold of the beautiful white snow. Knowing that tomorrow we would hopefully be standing on the summit of this glorious mountain motivates you in ways that we never experience at home. It would be another two hours before we would make base camp, but the mountain had another gift for us. Snow! We walked into camp under a light snowfall. However, that wouldn’t be our last snowfall.
Base Camp sits at 15,400 feet. Anything that requires effort becomes hard. There simply isn’t enough oxygen to make any kind of major exertion. Even changing clothes is harder. Walking up the few rocks to get to the upper part of camp is hard. And it only takes a couple steps to realize that. So, the best thing to do is rest. Because you will need it. Summit day doesn’t begin the next morning. It begins that night!
You have to be prepared for summit night. It will be the hardest thing you’ve ever done. Our guides try to prepare us for this. They tell us what to expect. How to dress for the freezing temperatures. What to eat. (The cooks are amazing.) And finally, what to pack in
our backpack. I was able to take a short nap that afternoon with the hope of getting another short nap after dinner. Our guides told us we would be leaving camp at 10:30 that night to begin our summit attempt. The hope is to reach the summit or at least the crater rim (Kilimanjaro is a dormant volcano) by sunrise around 6:30 in the morning.
O ur final preparation meeting began at 5:00 that afternoon. Dinner followed at 6:15. And we were finally able to get to our tents around 7:30. We would be up in 2 hours. Well, my husband would be. I couldn’t get to sleep. I knew I needed the sleep but thought I would be ok. The plan was to leave at 10:30. Summit by 7:30-8:00, then descend to our new camp by 1:00 the next afternoon. I could stay up 24 hours. I’d done it before. But that’s now how things would play out.
9:30 came and we began to get dressed and pack up our gear. Nighttime at over 15,000 ft is cold. Freezing cold. The temps had dropped from the upper 30s to the upper 20s. At the summit they could be well below zero. So, we dressed in layers. Thermal underwear. 2 pairs of socks. Followed by a pair of hiking pants and long sleeve shirt. Followed by fleece hiking pants and another long sleeve shirt. Then add on a pair of rain pants. Your upper body is topped off by your fleece jacket and down jacket. Your rain
jacket goes into your backpack. Heavy gloves, balaclava, and fleece beanie finish out your clothing. When that’s done, you head to the mess tent to eat. Even though we had a carbohydrate loaded meal at 6:00, the cooks still prepare another light meal before we begin our summit attempt. We would learn quickly though, that this wasn’t enough.
W ith our headlamps on, we leave camp at 10:45 p.m. It’s cold, but fortunately there isn’t much wind. Like Day One, the beginning of summit night has no “warm-up” area. Immediately leaving camp, you begin the uphill journey. The crater rim sits at 18,700 ft. That makes for 3,300 ft. of elevation and a 4-mile hike to reach it. The steepness of the climb doesn’t allow you to just take one step after another endlessly. You must take one step, slight pause, another step, and so on. And this process slows as you ascend. The path up consists of continuous switchbacks. It’s basically an 18-inchwide dirt path that thousands of people have cut out of the rocks on each side. Although we left at 10:45, most teams leave around midnight. It’s very surreal to look back toward base camp and see all the tiny lights in the distance. In fact, as you go higher and higher and it becomes steeper, you have the feeling that if you slipped and fell, you would slide all the way back to camp.
Our first extended rest stop came around 17,500 ft. at Hans Meyer Cave. Hans Meyer was the first person to summit Kilimanjaro in 1889. It’s a great place to sit down and reflect on hard it must have been to summit at a time when the mountain was covered in ice. I was still feeling strong at this point of the climb, but that was about to change.
The energy expenditure required to climb in the cold, at extreme elevations, and at ascent angles of over 40% at times, is immense. Upwards of 1000 calories an hour. Your hope is that you’ve eaten enough to have the glycogen stored nicely away and to eat enough as you’re climbing to prevent the dreaded “bonk”. I’d like to say that happened for us, but I can’t. It is that way for almost everyone. Even our guides. It’s this section from Hans Meyer Cave to the summit rim at Gilman Point where people begin to give up and turn around. Even one of our group had to abandon her climb. But we trudged on. Step by step. At 18,000 feet you can look up and see what looks like the crater rim. It’s your first moment of hope among the misery of total exhaustion that has laid waste to your body. In reality it’s an illusion. The curvature of that area hides the rim from your view. You will walk for 30 minutes and look up and see what looks exactly the same. And on it goes. 30 minutes becomes an hour, then two. Our pace had become so slow that we could walk no more than 50-100 feet at a time without leaning all our body weight on our trekking poles. We had hoped to be to the crater rim by sunrise, but that time had come and gone. It was approaching 8:00 in the morning, over 9 hours after we had left camp when we finally caught a glimpse of the rim. This is where you shed your first tears. You know you’ll at least make it to the crater rim. It would be 8:30 when we finally stood at Gilman Point. But the work is far from done. This is only 18,700 feet. We still have to navigate the crater rim past Stella Point and then onto Uhuru Point, the summit of Kilimanjaro.
The hike from Gilman Point to the summit isn’t steep. Only an additional 700 feet up, except that those 700 feet will take you above 19,000 feet high. It is however a very long walk. For most people this will take about 2 hours. We were already way behind our planned schedule, so we had to move. It would take an hour and a half to reach Stella Point, halfway to the top of Africa. It was 10:00 and we hadn’t summited. We didn’t know if our guide would let us summit at this point. We could barely walk. We had absolutely no energy in our bodies. I will say that I have never been so exhausted in my entire life and I don’t believe I ever will be again. But I wanted to summit. My husband and I had come so far. This had been his dream. It had become mine. It’s amazing how the Kilimanjaro guides will

people to the summit. Even knowing that a 6-hour descent awaited, our guide Ezekiel was going to push us to the summit. He alleviated out doubts by doing an oximeter test on us to prove we still had it in us. 50% he said and we could still summit. We were at 70%! And then the snows came.
As we departed Stella Point, a snowstorm moved in. Not just any snowstorm. 30-40 mile an hour winds. Snow blowing sideways across the mountain. But we were not going to be denied. My husband kept saying “With each step, a success.” And that’s what we did. And at 11:30 a.m. on January 21st, 2019, in a blinding snowstorm, my husband and I embraced each other at the top of Africa, with tears flowing down our cheeks. It was the greatest thing I’ve ever done or will ever do. I’m so proud of my accomplishment. Of our accomplishment. But I wouldn’t have been there without the dream of my husband and the skilled hands of Dr. Clayton.
Dr. Clayton had a flag made for me to carry to the summit. Unfortunately, the wind was too strong to get a good picture

at the summit but were able to get a picture at Stella Point once we returned from the summit. But it made it there with me.
Our story isn’t quite over there though. We were still in the middle of the snowstorm as we began the journey to our new camp. As thrilled as we were with summiting, we still had the long, arduous descent before us. Descending Kilimanjaro isn’t like ascending. There aren’t a series of switchbacks. It’s basically a straight shot down the mountain. But whereas we started our night at 15,400 ft. and summited at 19,341 ft., we now had to find our way down to 11,000 feet. Most people think that descending is easy. It’s not. Your legs have no energy to support you. The rocks are slippery and tend to roll out from under you. (I feel a couple times.) I got to the point where Ezekiel had to literally grab me by the arm and hold me up as we hiked down the mountain. How he did this for hours is beyond me. Finally, at 7:30 p.m., in the dark, we entered camp. We had been on the mountain for nearly 21 hours!
When you reach this level of exhaustion, you only have one thing you can do
When you reach this level of exhaustion, you only have one thing you can do and that’s to cry. Cry for the agony of the day. Cry for the accomplishment.
and that’s to cry. Cry for the agony of the day. Cry for the accomplishment. It’s been five months now and I still cry when I think about what we did. Something that two short years ago wasn’t a possibility. But now and for the rest of my life, I can say I conquered Mt. Kilimanjaro. No one can ever take that away from me.
I need to say thanks to my husband for his vision and planning. To our guides for motivating us and their friendship. And to Dr. Clayton and staff. I have a new hip that made a dream come true.




What exactly is an artificial disc?
An artificial disc replacement, also known as arthroplasty, is the replacement of a damaged spinal disc with an artificial (manufactured) disc.
When did you perform your first lumbar artificial disc replacement?
“In the year 2003. I have performed many since then for both the cervical and lumbar spine.”
What “levels/area/region” of the spine can this surgery be performed?
“In my opinion typically the Cervical C3-C7 and Lumbar L4-L5 or L5-S1.”
Who are good candidates for lumbar total disk replacement (LTDR) surgery?
•Patients who have failed conservative management
•Patients who have disc disease at 1 level in the lumbar spine.
•Patients who lack sciatica (pain radiating down the leg related to compression of a nerve root).
Who are good candidates for cervical total disk replacement (CTDR) surgery?
Newest-generation cervical artificial discs are designed to restore physiologic motion to the spine and are indicated as an alternative to cervical fusion. An artificial cervical disc preserves motion by restoring biomechanical function at the treated level
after native disc removal and potentially reduces subsequent degeneration of adjacent vertebral segments.
What are the benefits of a cervical disc replacement compared to the traditional ACDF procedure?
Artificial disc replacement may preserve motion and may decrease adjacent level degenerative disc disease as compared to traditional ACDF procedure
What are the benefits of lumbar total disk replacement (LTDR) compared to the traditional lumbar fusion procedure?
• Traditional lumbar fusion restricts motion between the bones in the lumbar spine to eliminate pain at the diseased segment. This changes the stress points in the lumbar spine and may lead to adjacent level disk degeneration above and below the lumbar fusion requiring future repeat surgery.
• Recovery from lumbar arthroplasty may be quicker than traditional fusion.
Dr. Parker, in your 20 year experience of performing total disc replacements, how has the technology improved and changed over the years?
“Like most technologies, newer generation artificial discs for the cervical and lumbar spine continue to improve as technology evolves.”


the Earth’s crust. These electrons will then satisfy the need required by the free radicals so that they do not produce any further damage. This concept is called “Earthing” or “grounding”. While it may not be widely accepted by everyone, no one can dispute the pleasure one feels from standing on warm sand or a cool, grassy patch of dirt.
If this is indeed true, we will spend hours or even days while at the beach with a direct connection to the ocean water or wet sand. This extended time may give a boost to our overall health that presents with a quick improvement in our sense of well-being.
While a vacation may be “just what the doctor ordered”, it may not be practical or possible to just relocate to your favorite beach. Good news, however, you don’t have to move to enjoy some of these same benefits. Getting regular sun exposure will produce the same effects. Studies show that 10-15 fifteen minutes of sunlight on exposed arms and legs can produce 10,000 IUs in fair skin.
Walking barefooted on grass or dirt can give you the same effect for grounding that the beach gives you. One caveat is to be aware of any chemical treatments applied to the grass. One recommendation stated 45 minutes a day of barefoot exposure to the ground. Concrete can also provide a direct link as well. This may not be practical, but getting regular exposure may make you feel better. Staying indoors and wearing shoes outside insulate us from that connection. I still encourage you, however, to regularly consume plenty of fresh fruits and vegetables to supply your body with antioxidants as well as other vital nutrients.
Seth Godin is quoted as saying, “Instead of wondering when your next vacation is, maybe you should set up a life you don’t need to escape from.” Again, it may not be practical to just up and permanently leave our lives, but I think we can all find ways to either reduce stress or find better ways to cope with them. As for today, you can start by simply going outside to get some fresh air and sunshine.
Reference
Ratner, K. G., Kaczmarek, A. R., & Hong, Y. (2017). Can Over-the-Counter Pain Medications Influence Our Thoughts and Emotinos? Policy Insights From the Behavioral and Brain Sciences, 5(1), 82-89. http://doi.org/10.1177/2372732217748965
https://journals.sagepub.com/doi/pdf/10.1177/2372732217748965



Get all the tantalizing smells, tastes and textures of your Newk’s favorites, delivered wherever you need them. Our catering specialists will deliver, set up and everything in between. All you have to do is relax and enjoy the food!
 by, Rachel Sullivan, MFTA
by, Rachel Sullivan, MFTA
What if we talked about mental health as openly as physical health? Imagine what our communities would look like if individuals affected by a mental illness were able to gain support from their family and neighbors for their depression, the same as when they are post-op from a heart surgery. There is such a stigma surrounding mental health. A stigma is defined as “a mark of disgrace associated with a particular circumstance, quality, or person.” Layer that over mental health, and specifically mental illness and now the definition reads “a mark of disgrace associated with mental illness.” Ouch. It breaks my heart that mental illness continues to carry a mark of disgrace with it, especially with the high prevalence in our communities.
Did you know that an estimated 1 in 5 adults struggle with a mental illness? When we include youth and children in this estimate, the percentage rises. With such significant numbers, the fact that mental health is still discussed minimally, if at all, is discouraging. We know that individuals with a mental health diagnosis are at a greater risk for social isolation, have greater difficulty developing fulfilling relationships, and that there is a correlation between untreated mental illness and suicide risk. Despite the known complications, as well as the known benefits of treatment, conversations about mental illness continue to happen below the threshold necessary to encourage change.
Wouldn’t it be wonderful if we talked about mental health as openly as physical health? It would be so helpful if individuals affected by a mental illness were able to gain support from their family and neighbors for their struggles, the same as when they are discharged from the hospital after a procedure. Consider what the recovery process for mental illness would look like if when someone disclosed their struggle and their journey to wellness they were accepted and encouraged! Do you think that kind of support would affect whether people with mental illnesses reach out for help? I think so, and I believe this kind of change is possible, with some shifts in how society thinks about mental health.
How do we begin to unravel the stigma? I believe the first step is to get educated! Almost without exception, when I have a judgment about a topic, it is due to a lack of information about that subject. Mental health is no different. In my opinion one issue that prevents people from being educated about mental health includes the lack of open discussions regarding the prevalence and impact of mental illness. Due in large part to stigma, many individuals who struggle with mental illness feel unable to talk as openly as someone who is battling cancer – and yet mental illness can be just as detrimental. When we hear personal testimonies about how mental illness affects people, we can connect our hearts with the importance of the cause. As I see it when we become educated, through real people accounts, our understanding and compassion provides the catalyst for reducing the stigma and normalizing mental health care. To begin changing the conversations surrounding mental health I have unpacked some points I believe are important.
1. Understand mental illness is not a choice. Depression, Anxiety, Bi-Polar Disorder, PTSD, Anorexia, Oppositional Defiant Disorder. These diagnoses, like so many others, involve a reaction in the brain that the afflicted individual has difficulty controlling without outside assistance. The behaviors, thoughts, reactions, and effects are not something the person would choose for themselves. Unfortunately, because of a lack of information, society sometimes paints a picture that people who are mentally ill choose to live this way. The truth is that even if they felt comfortable doing so, many people do not know where to turn to for help, or even that something is “wrong”. Mental illness tells lies like “You are the only one that feels this way”, it is from this isolating place that the person struggling keeps their battles tucked away, lest they seem “crazy”.

2. Mental illness can be treated.
The field of psychiatry and therapy has grown tremendously over the past few decades. What we now know about the brain allows clinicians and physicians more opportunities to assist individuals diagnosed with mental illnesses. Previously, a schizophrenia diagnosis would almost certainly mean hospitalization. Fortunately, the advances in medicine and psychiatry have allowed a more comprehensive approach, providing platforms for many individuals with schizophrenia to live full, independent lives. These advances have positively impacted the field of mental health in many ways. Understanding the possibility of treatment can encourage those struggling to get help, which means more people on the road to wellness.
3. People with mental illness are not their diagnosis. Mental illness does NOT define an individual. We do not say “That bi-polar woman”, but rather “the woman with bi-polar disorder”, because the diagnosis does not define the person. It is a struggle they are walking through, not a definition of their being. Can you imagine calling the mom battling breast cancer “the cancer lady”? Absolutely not, and yet society has normalized the labeling of people struggling with mental illness by their diagnosis. In my opinion, this reinforces the stigma, rather than creating space for safe, open conversation about the struggle. Realizing that mental illness is something that affects the individual, rather than who they are, is key in updating how we view mental illness.
4. People with mental health diagnoses are capable. Individuals with a mental health diagnosis are just as capable of living abundant lives, raising families, and working fulfilling jobs as people who do not struggle with mental illness. It is true that some diagnoses will require more intense, or even long-term care for symptom management, but this does not prohibit productivity or decrease the value of the individual. Some of the most resilient people I know have battled mental illness and come out with more grit, tenacity, and compassion for others than individuals who have never dealt with mental health issues.
So, what do we do with all of this? The reality is mental illness is not going away, a fact we cannot change. What we can change is the way we perceive mental health as well as the individuals who struggle with mental illness. We can set into motion a snowball effect of acceptance, and thus facilitate dialogue for healing. I believe when we do so the stigma decreases, and the topic of mental health care becomes a more normal conversation. People who are struggling feel more safe reaching out for help, and a shift begins. I am ready to be a part of the change, are you?






You’ve worked hard to create security and freedom through sound financial decisions. Partner with Progress to take your accounts to the next level. Our private banking services give you the features found at big banks, but with the personal, connected service only found at a local bank.
As a full-service community hospital, Crestwood offers a wide range of services. It is our mission to serve by providing exceptional patient care and service for patients and their families who choose Crestwood. Thank you for your support of Crestwood.

• Bariatric Surgery Center
• Cardiology
• Emergency Department
• Gastroenterology
• Maternity Center & Women’s Services
• Neonatal Intensive Care Unit
• Outpatient Diagnostic Imaging
• Outpatient/Inpatient Surgery
• Pediatrics
• Robotic-Assisted Surgery
• Sleep Center
• Spine & Neuro Surgery
• Therapy Services
• Total Hip & Knee Center
• Vascular Lab
• Vein Center
• Women’s Center with 3D Mammography
• Wound Care
• 180 Private Patient Rooms