3 minute read
Examining How Dynamic Hydrogels Affect Vascularity in New Tissue
By Amy Weldon INBT researchers hope to discover more about how tissue vasculature forms and adapt in a changing environment. The stiffness of the extracellular matrix (ECM) has long been the topic of regenerative tissue research, especially in the case of cancer cell migration. Sharon Gerecht, the INBT’s director, and her team have taken the vessel less traveled, by looking instead at the ECM’s responses to “stress relaxation.”
Using a brick wall as a metaphor for tissue formation, endothelial cells, or bricks, send out signaling proteins to interact with the ECM, or mortar, to form the tissue’s structure, or wall. As a result of this signaling, vacuoles, or void spaces, are created between and inside of cells, forming the vessel lumen, or the tubes through which blood flows. The faster blood can flow through newly formed or transplanted tissue, the more successful and stable the tissue will be in its new environment. This is a good thing in the case of transplanted organs or skin grafts, but for patients with cancerous tumors, it’s bad news. The nascent, or newly formed, vessels are constantly sprouting and branching through the tissues. Gerecht and her team sought to study the effects of the stress or strain of a living, moving environment on the formation of these networks.
Advertisement

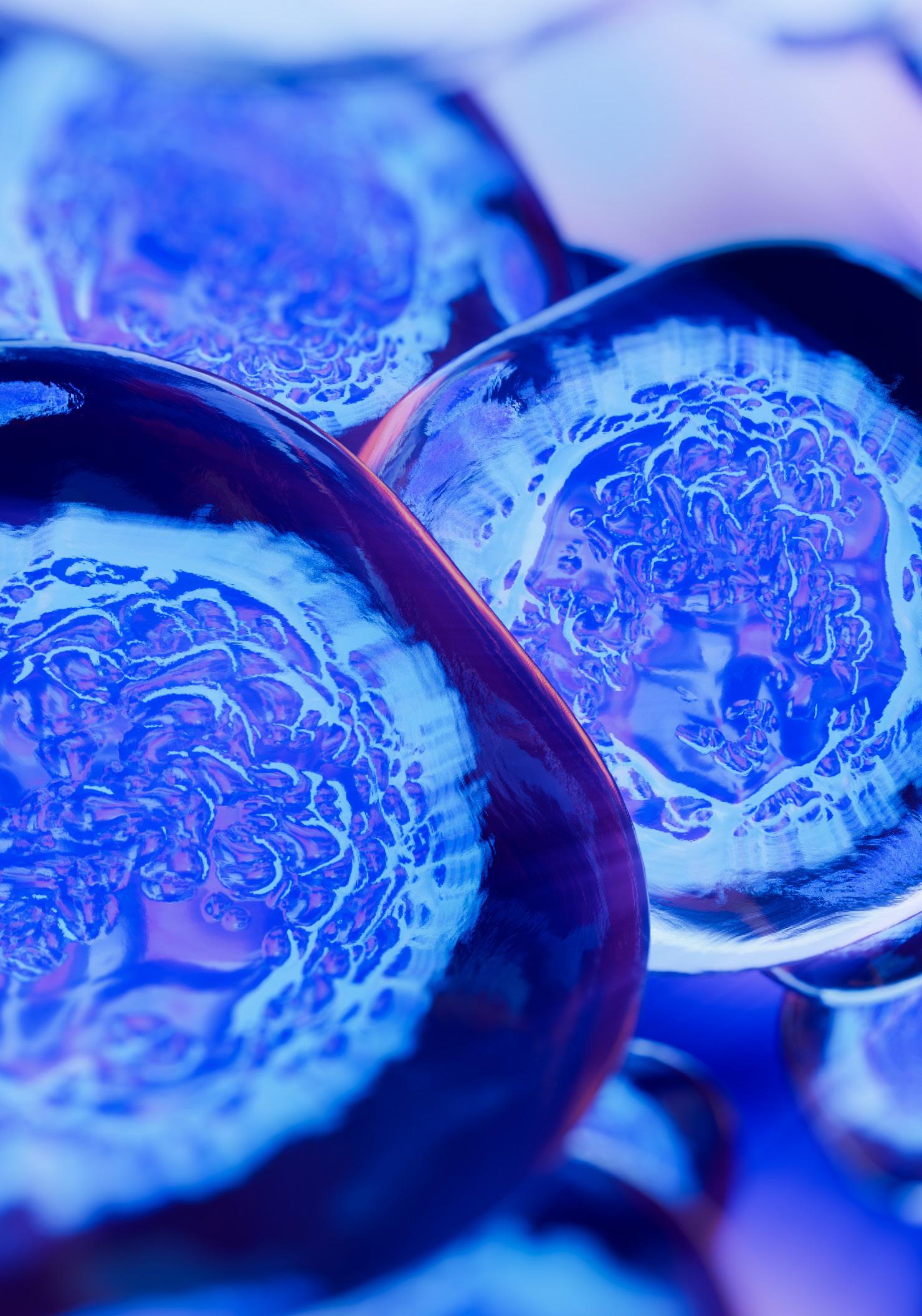
Blood vessels growing into the viscoelastic dynamic hydrogel.
While brick walls are thought to be sturdy, immovable structures, Gerecht’s team was interested in how the wall might form in an environment that more closely represents the conditions in a living body. This environment is neither rigid nor fluid but viscoelastic like Jell-O or Silly Putty. At first, Silly Putty responds to stress (being squished or pulled apart) by losing firmness and taking a new shape, but after a period of time, the putty relaxes into the new shape and regain firmness. To develop this viscoelastic ECM, or dynamic hydrogel, the team’s tissue engineers developed a new hydrogel scaffold materials platform that mimics aspects of three-dimensional physiological tissue microenvironments and is capa-
ble of stress relaxation. Researchers reasoned that the dynamic hydrogel’s ability to respond to the stress of deformation or remodeling can
impact how endothelial cells make vasculature. Stiffer, more static hydrogel, commonly used in studies involving tissue regeneration, does not yield the same downstream signaling between cells and speedy vasculature formation. The new vasculature forms more quickly within this dynamic or stress relaxing hydrogel and can pass fluid through and grow larger than in non-dynamic hydrogels. The faster formation of a network in the ECM can occur, the more efficient the integration process for the new tissue into the new environment. This characteristic could also prove to be essential to treatment developments for slowing down vascular growth in tumors and slowing the spread of cancer through the body.
“If you want effective tissue remodeling and vascularization, the tissue has to have a high stress relaxation property, it has to be dynamic,” explained postdoctoral fellow Rahel Schnellmann, “otherwise, all of your processes are extremely slowed down.” Faster cell signaling and vascularity formation would benefit research on a variety of topics from wound healing, faster integration of transplanted organs, how cancer spreads throughout the body, and more.

Further Highlights
Sharon Gerecht was appointed to the Edward J. Schaefer Professor in Engineering. The Schaefer Professorship was endowed through the generosity of Mrs. Hildegarde H. and Mr. Edward J. Schaefer ’23 to support outstanding Whiting School faculty members. She was also named a fellow of the American Association for the Advancement of Science—a lifetime distinction that recognizes outstanding contributions to science and technology, and a fellow to the National Academy of Inventors—which recognizes and honors academic inventors who have created or facilitated outstanding inventions that have had an impact on society. With an award from the Translational Research Institute for Space Health at Baylor College of Medicine, a partner to the NASA Human Research Program, Sharon Gerecht will lead a team that will study the effects of space radiation on vascular, cardiac, and neurovascular tissues. They will use applicable tissue and organ models, and develop potential countermeasures to offset the negative effects of space radiation on these tissues.