01/2025
JANUARY-FEBRUARY 2025

New hospital sets standards for future clinical design
Budget special report — the impact on health infrastructure
Winners of the National Care Awards and HealthInvestor Power List are revealed





01/2025
JANUARY-FEBRUARY 2025

New hospital sets standards for future clinical design
Budget special report — the impact on health infrastructure
Winners of the National Care Awards and HealthInvestor Power List are revealed




Since the last edition of Healthcare Property, the new Labour government has made a number of announcements based on its pre-election manifesto, many of which follow through on key promises about the future delivery of healthcare services.
Notable among these was Chancellor, Rachel Reeve’s, Budget speech in November, which awarded the NHS an additional £22.6bn for routine spending, spread over this financial year and next, and a further £3.1bn in capital spending for extra beds and improvements to buildings.
But just how far will this cash go when waiting lists remain at an all-time high, the cost of delivering care and purchasing muchneeded equipment is rising, and the Government is pledging staff pay increases and increases to the national minimum wage and living wage?

their views on the promises and what needs to be done to ensure the viability of the sector moving forward.
Elsewhere in this edition we showcase some of the latest health and care developments which are setting a benchmark for the future (p28), including the new Midland Metropolitan University Hospital and Wombwell Hall Care Home in Gravesend, Kent.
And we name the winners of the 2024 HealthInvestor Power List and the National Care Awards (p46), as well as review the recent Healthcare Property Forum, a new event organised by Healthcare Property publisher, Nexus Media Group (p40).
For health and care estates and facilities managers, times will undoubtedly continue to be tough, with pressure on the Government to find a new public/private capital model to replace the now-defunct PFI approach to delivering modern, fit-for-purpose infrastructure.
But, for investors and financiers, while the market may be waiting for the dust to settle following the election and the subsequent Budget, there is a reported uptick in interest in both health and care facilities, particularly in the later-living, private healthcare, and primary care sub sectors.
You can read more about these opportunities in our Budget special report (p12) where industry insiders give
Since its launch in January 2024, Healthcare Property has led the way in bringing the latest news and developments within the sector to readers, and this will continue through 2025.
As well as the latest property and finance news, we will explore best practice in design and construction and offer support and guidance to the estates and facilities managers in charge of health and care estates.
In the next edition we will be looking at Modern Methods of Construction (MMC), fire safety, and infection prevention and control.
If you can help with any of these articles, or wish to get in touch with editor, Jo Makosinski, please email joanne.makosinski@nexusgroup.co.uk
Jo Makosinski
Editor, Healthcare Property
About Jo: Jo is the editor of Healthcare Property, having joined Nexus Media in November 2023.
She has been specialising in design and construction best practice for the past 16 years, working on the Building Better Healthcare Awards and editing both
Building Better Healthcare and Healthcare Design & Management magazines.
She has a special interest in the design of public buildings, including schools, nurseries, colleges, hospitals, health centres, and libraries.


Chief executive officer
Alex Dampier
Chief operating officer
Sarah Hyman
Chief marketing officer
Julia Payne
Editor
Joanne Makosinski
joanne.makosinski@nexusgroup.co.uk
Reporter and subeditor
Charles Wheeldon
Advertising & event sales director
Caroline Bowern
Business development executive
Kirsty Parks
Publisher Harry Hyman

We round up the latest big stories, including the selection of Ramboll as lead consultant for the design of the children’s cancer centre at Evelina London Children’s Hospital and the announcement of the five architectural firms in the running to design The Fleming Centre at St Mary’s Hospital; and we profile

A new report from Christie Finance takes a focused look at the financial markets that support the care sector, while Broadwood Capital secures backing for a dedicated sustainable later-living credit fund, and we list the latest property deals

Investor Publishing Ltd, 3rd Floor, 10 Rose & Crown Yard, King Street, London, SW1Y 6RE
Tel: 020 7104 2000
Website: www.healthcare-property.com
Healthcare Property is published six times a year by Investor Publishing Ltd.
ISSN 3029-0627
© Investor Publishing Limited 2025
The views expressed in Healthcare Property are not necessarily those of the editor or publishers.
@HCprop

linkedin.com/company/healthcare-property/

Exploring best practice in the delivery of dementia-inclusive environments; plus case studies on the new Midland Metropolitan University Hospital and Wombwell Hall Care Home

How technology is helping hospitals to locate vital equipment, and discussing the evolution of vending technologies in health settings
An overview of the firstHealthcare Property held in London
We announce the winners of the 2024 National Care Awards and HealthInvestor Power List 50 People
The movers and shakers in the health and social care sector
Global engineering, design, and sustainability consultancy, Ramboll, has been appointed as lead consultant for the design of the new Children’s Cancer Principal Treatment Centre at Evelina London Children’s Hospital.
Appointed by Guy’s and St Thomas’ NHS Foundation Trust, Ramboll will provide a full range of multi-disciplinary advisory and design services, with subconsultants providing further specialist support. This includes collaboration with ADP Architecture for architectural and lead designer services, with further specialist services from GL Hearn, Art in Site, Thornton Tomasetti, and Safer Sphere.
In line with the trust’s ambitions, the project will involve a multi-phased approach to ward decants and department remodelling across three separate buildings at the hospital.
Design solutions will align with the trust’s Sustainability Strategy net zero requirements covering plant selection, renewable energy, water management, air quality, and material use.
There are currently 13 children’s cancer Principal Treatment Centres (PTC) in England which provide specialist care for children aged 15 and under with cancer.

Following an NHS England led decisionmaking process, Evelina London Children’s Hospital, part of Guy’s and St Thomas’ NHS Foundation Trust, has been chosen as the future PTC location for south London and much of South East England.
Evelina London is now working closely with patients, families, its own staff, and staff from the existing service delivered by The Royal Marsden and St George’s Hospital, to plan for the safe transfer of specialist cancer services to Evelina London Children’s Hospital. The service is not expected to move before October 2026.
James O’Brien, the children’s cancer Principal Treatment Centre operational delivery director, said: “The appointment of the team from Ramboll and ADP Architecture, with their specialist subconsultants, is a significant step in our journey to bring specialist cancer services to Evelina London Children’s Hospital.
“We are grateful to the patient representatives who got involved in the decision-making process and to colleagues from the existing service who have already
done so much to contribute and to share their expertise and views with us.
“Their voices are essential to developing these vital services for children and young people from south London and much of South East England, and we are looking forward to involving them at every stage of the programme.”
He added: “In all of Evelina London’s developments, we pride ourselves on working closely with children, families, and staff to ensure we are well placed to deliver excellent care in a child-friendly and welcoming environment.
“As with our award-winning Children’s Day Treatment Centre, which was designed by ADP Architecture, we will involve children, families, and staff in all elements of the design and planning of our cancer service.”
Commenting on the appointment, Kevin Smith, head of healthcare UK at Ramboll, said: “We are delighted to have been selected to provide multi-disciplinary design services on this complex project.
“With 500 dedicated healthcare experts
globally, and an extensive international and UK healthcare portfolio, notably Cambridge Children’s Hospital, we look forward to working with the trust to provide a smooth, timely, and affordable service transfer of the Principal Treatment Centre from the Royal Marsden Hospital and St George’s Hospital to Evelina London Children’s Hospital.
“Our experience with hospital projects gives us a holistic perspective that prioritises patients and it is our goal to ensure that children with cancer have access to safe and timely care with compassionate support and good outcomes.”
Environmental sustainability will be integral to the development and delivery of this project, which will contribute to the trust’s ambition to reduce its absolute scopes 1 and 2 emissions by 47% by December 2029 and achieve net zero carbon by 2045.
Focusing on projects that are both sustainable and patient-focused, Ramboll’s design solutions are crafted to minimise environmental impact while having maximum effect on wellbeing.
The Royal Institute of British Architects (RIBA) has announced a shortlist of five architects who will progress to the next phase of design for The Fleming Centre at St Mary’s Hospital, following a RIBA design competition launched in collaboration with Imperial College Healthcare NHS Trust in July.
The Fleming Centre will be at the heart of the global Fleming Initiative, an innovative and collaborative approach led by the trust and Imperial College London, with HRH Prince of Wales as its Patron, to tackle antimicrobial resistance (AMR).
The centre will be part of a global network of facilities in strategic locations around the world, aiming to catalyse worldwide action.
Professor the Lord Darzi of Denham, executive chair of the Fleming Initiative, recently announced it had raised an initial £100m, supported by three new partners, LifeArc, Cepheid, and Optum, alongside founding partner, GSK, and other philanthropists.
The centre is due to open at St Mary’s Hospital in 2028, helping to mark the centenary of the discovery of penicillin at the

hospital by Sir Alexander Fleming. It will be the first new building to open on the St Mary’s site as part of a planned full redevelopment of the estate.
The evaluation panel has selected the following practices to proceed to the next phase of the competition:
• AHMM
• Allies and Morrison
• Grimshaw
• Stanton Williams
• Wilkinson Eyre and White Arkitekter
The teams will now enter the next phase of the process, with a final decision expected to be announced later this month.
The Fleming Centre will be a key part of the trust’s Paddington Life Sciences development
which is creating a thriving ecosystem for life sciences research and innovation, with St Mary’s as its hub.
In turn, Paddington Life Sciences is an integral part of the Imperial WestTech Corridor, a globally-significant concentration of technology and innovation stretching across west London and acting as a catalyst for investment, employment, and inclusive growth.
St Mary’s Hospital — along with the trust’s two other main sites, Charing Cross and Hammersmith hospitals — are part of the Government’s New Hospital Programme.
Professor Tim Orchard, chief executive of Imperial College Healthcare NHS Trust, said:
NHS England’s newly-published Insightful Board guidance aims to provide support for trusts and integrated health boards (ICBs) when handling and acting on the information they receive, including references to the estate.
The guidance considers the leadership behaviours and culture of the board and how these can affect the information it receives and the actions it takes, as well as metrics that can support the board to better understand an organisation’s overall performance.
A spokesman said: “It is important for boards to continually review and understand their trust’s performance against guidance and good practice.
“‘Active’ governance means issues are considered by the most-appropriate people, relevant information is reviewed in the mostuseful format and at the right time, and the level of scrutiny produces rigorous challenge and an effective response.
“Findings with a material importance for the organisation should be identified and reported promptly to the board and analysed through a thematic lens.”
The guidance makes several references to estates functions, including the collection of The Estates Return Information Collection (ERIC) data, which contains information relating to the costs of providing, maintaining, and servicing the NHS estate.
“We are excited by the prospect of plans for the Fleming Centre that incorporate creative ways to honour the legacy of Sir Alexander Fleming.
“We will be engaging with staff, patients, and local communities to ensure the Fleming Centre brings real impact, locally and globally, as a visionary space for collaboration, groundbreaking science, and engagement to drive change.”
Lord Darzi added: “Science alone will not solve the global threat of antimicrobial resistance, we have to change human behaviour.
“The Fleming Centre is an embodiment of our commitment to making public engagement and behavioural science the cornerstones of the innovative solutions we need.
“I look forward to reviewing plans for the Fleming Centre that will make this vision a reality."
The trust is proposing to build the Fleming Centre on the site currently occupied by The Bays buildings on the west of the hospital site.
These former industrial warehouses were built around 1850 for transport and distribution networks and were incorporated into the hospital in 1983, primarily for office use.
It also looks at estate risks and the Premises Assurance Model Self-Assessment, which supports boards, directors of finance, and estates and clinical leaders to make more-informed decisions about the development of their estates and facilities services and provides assurances that the estate is safe, efficient, effective, and of high quality.
And it calls for benchmarking of estates functions against other organisations and analysis of achievable efficiencies.
NHS Estates and Facilities will be following up the release with a template to support estates and facilities leads to report up to their organisation’s board.

Flexible workspace operator, Spacemade, in partnership with The Howard de Walden Estate, has announced plans to open Hale House — the UK’s flagship HealthTech space — at Portland Place in the heart of London’s Marylebone.
Opening in March, this innovative workspace is set to become the UK’s mostcollaborative ecosystem for HealthTech and innovation stakeholders, fostering the next generation of advancements in health and wellbeing.
Hale House occupies several buildings within the Harley Street Health District, a globally-renowned centre for excellence in healthcare, managed by The Howard de Walden Estate.
Harley Street Health District encompasses a wide network of specialist hospitals, modern outpatient clinics, rehabilitation centres, and state-of-the-art healthcare facilities.
And Hale House perfectly aligns with the district’s mission to become the world’s leading destination for whole health and innovation, creating the most-connected health community globally.
At the heart of the Hale House ecosystem, 76-78 Portland Place will serve as the flagship location for HealthTech startups, investors, and venture capital firms, while ancillary services such as legal, data compliance, and recruitment firms will be based across two additional townhouses at 42 and 19 Portland Place, further supporting the dynamic needs
of this growing sector.
Together, these spaces will create a unique collaborative environment designed to foster innovation, attract investment, and enable transformative developments in healthcare.
“This launch represents a new chapter for HealthTech in the UK,” said Jonny Rosenblatt, co-founder of Spacemade.
“Hale House will serve as the epicentre of HealthTech innovation in the UK; a place where the brightest minds in HealthTech can come together to collaborate, innovate, and drive the future of healthcare forward.
“By uniting start-ups, investors, and essential professional services in one space, we’re building a community that is poised to transform the future of healthcare.”
Mark Kildea, chief executive of The Howard de Walden Estate, added: “Hale House is integral to our whole health strategy for the Harley Street Health District, where we are working to create the best-connected health community in the world.
“This partnership with Spacemade is more than flexible workspace; it’s about nurturing collaboration and innovation.
“Our mission is to support the development of pioneering healthcare technologies that will define the future of health and wellbeing.”
Once open, Hale House will welcome UCLPartners as its anchor tenant, occupying the first floor of 76-78 Portland Place.
As a leading academic health science partnership, UCLPartners is at the forefront of transforming healthcare through cuttingedge research, collaboration, and patientfocused innovations.
• A collaborative ecosystem: A thriving hub where start-ups grow, investors unlock new opportunities, and professional services support the development of pioneering healthcare technologies
• Prime location: Situated within the prestigious Harley Street Health District, Hale House offers access to one of the world’s leading medical communities
• State-of-the-art facilities: Flexible, highquality workspaces designed to inspire innovation, including a dry lab for computerbased modelling and simulations
• Media production facilities: Flexible content creation areas, including a screening room and podcast studio to support members’ media and communication needs
• Wellness amenities: A wellness room and gym/yoga studio to support physical and mental wellbeing
• Onsite café: Operated by Humdingers, providing high-quality food and drinks for the HealthTech community
• Versatile event space: A large, multifunctional event space for up to 90 people, ideal for networking, workshops, and product launches
The mayor of Basingstoke and Deane, Councillor Dan Putty, and local MP, Luke Murphy, were guests of honour at the official opening of the town’s new state-ofthe art neurological rehabilitation centre.
Cllr Putty and Murphy cut the ribbon to officially open Hamberley Neurocare Basingstoke, a care service for local people with complex neurological conditions.
The contemporary 28-bedroom building features therapy and medical consulting rooms and a therapy gym fitted with state-ofthe-art rehabilitation equipment.
Cllr Putty said: “I was amazed to see such large rooms for the rehabilitation of the residents. They are five star in the making.
“The gym room was very impressive and will aid many to regain fitness.
“And the décor was stunning, giving a homely feeling and will offer comfort to all.”
Home manager, Gill Irish, added: “Hamberley Neurocare Basingstoke will be a hub of clinical expertise, compassion, and genuine kindness – a place where individuals receive truly-tailored care that supports their recovery and resilience.
“Our dedication to exceptional care and individualised attention will shine through in every part of our service, and our launch celebration truly marked that ambition.”
Hamberley Neurocare Basingstoke will




provide rehabilitation, long-term, respite, and palliative care for people with brain injuries and neurodegenerative conditions such as Parkinson’s disease and Huntington’s disease.
The building was designed by RDT

The project team also included Hamberley Development, Lancer Scott Construction, Fed3 Project Managers, Harniss Engineers, Ward Associates, and Park Grove Interiors.
Contractor, Tilbury Douglas, has handed over Yeovil Hospital’s new breast cancer unit on behalf of Somerset NHS Foundation Trust.
The completion of the £2.5m Maple Unit, procured via the Procure Partnerships Framework, follows a five-year fundraising campaign run by the trust’s official charity, which saw members of the community, the Tilbury Douglas team, former patients, and colleagues at the hospital take part in hundreds of moneyspinning events.
The 500sq m facility, based across two floors, is the hospital’s first stand-alone, purpose-built breast cancer unit.
With social value at the heart of the scheme, the Tilbury Douglas


team achieved a 48% social value return on investment, triple what was initially targeted.
Designed with lots of art and natural light, The Maple Unit also offers a dedicated area for difficult conversations and a comfortable waiting area away from other busy outpatient areas and treatment rooms.
Caroline Osborne, a consultant breast surgeon at the hospital, said: “This is amazing news and I’m over the moon that it’s finally opening.
“It has been such a long time in the making, from when we first came up with the idea 10 years ago, and the incredible fundraising campaign that followed, to seeing the unit getting built before our very eyes.”
A new Optegra ophthalmic clinic has opened in Leicester dedicated to providing NHS cataract surgery for patients across Leicestershire and the East Midlands.
Newly-elected MP for Mid Leicestershire, Peter Bedford, visited the Meridian Business Park clinic to meet the local team, tour the new facility, and cut the ribbon to officially open the unit.
He said: “The investment that Optegra has made in Leicestershire will help local people access this sight-saving surgery more quickly, and at great convenience.
“From touring the clinic today, I can see that patients who are referred here will be experiencing the highest-quality facilities with excellent patient care and impressive outcomes.”
The purpose-built facility was designed by CSM Architects and was built by DD Porter Construction.
It is part of Optegra Eye Health Care, a network of specialist eye hospitals and clinics across the UK and Europe that provide cataract and vision-correction procedures.
Richard Armitage, NHS director for Optegra Eye Health Care, said: “Over the past couple of years we have been expanding our NHS cataract treatments by opening a series of

“Leicester now joins Nottingham as one of our key locations in the East Midlands and we are delighted to be supporting existing ophthalmic services in the area and working with the NHS to substantially reduce waiting

Work has completed on Knowl Park House, a state-of-theart dementia daycare centre and centre of excellence for Kirklees Council.
Delivered through the Crown Commercial Service (CCS) Construction Works Framework, the project has transformed the site to offer vital care services and innovative training resources to the community.
The project recently won the Constructing Excellence Award for Delivering Value, recognising the significant social impact created during the construction.

Contractor, Tilbury Douglas’ commitment to community engagement and social value was pivotal in achieving this accolade.
The new, single-storey daycare centre provides 25 places and meets the University of Stirling’s
arts and crafts, and a garden zone — ensuring a stimulating and supportive environment for service users.
The facility also includes staff welfare areas, dining and kitchen spaces, and hygiene rooms.
Alongside the daycare centre, the centre of excellence offers cutting-edge training
hands-on learning.
And community involvement was central to the project’s success.
Social value initiatives included participation in Build UK’s Open Doors programme, educational outreach through guest lectures and site visits, and fundraising for Reach Academy’s
Bloom in rejuvenating Hopton New Road Bridge.
Paul Ellenor, regional director for Yorkshire and North East at Tilbury Douglas, said: “We are incredibly proud to have delivered a facility that not only meets the highest standards in dementia care, but will also have a lasting positive impact on the local community.”




Here, we look at the key points of the new Government’s Autumn Budget and how this will impact the sector
The NHS won a record rise in funding in Chancellor, Rachel Reeves’ first Budget, but experts are warning that patients are ‘unlikely to notice’ as the cash is swallowed up by urgent building repairs, staff pay rises, and continuing service inefficiencies.
In her first speech as Labour’s new Chancellor, Reeves awarded the NHS an additional £22.6bn for routine spending, spread over this financial year and next, and a further £3.1bn in capital spending for extra beds and improvements to buildings, describing it as ‘the largest real-terms
growth in day-to-day NHS spending outside of COVID since 2010’.
But leading health think tanks warned the money will merely ‘help sustain services’ rather than bring any lasting improvements for patients.

Siva Anandaciva, chief analyst at The King’s Fund, said: “This Budget has been delivered among a backdrop of dire NHS performance and extremely-tight public finances.
“The Chancellor has said that ‘change must
be felt’, but the health spending announced is unlikely to be enough for patients to see a real improvement in the care they receive.”
Key points announced in the Budget included:
• A £22bn increase in total health and social care revenue and capital funding as part of a two-phased Spending Review
• NHS England’s ring-fenced revenue budget will increase by 4.7% this year to £181.4bn and then by another 3.3% next year to £192bn. The overall health and care budget, from which NHS England may be given further money to take forward activity such as bringing down elective waiting lists, will increase by a smaller 3.8% and 3% respectively
The Chancellor has said that ‘change must be felt’, but the health spending announced is unlikely to be enough for patients to see a real improvement in the care they receive
• £1.5bn to fund new surgical hubs which will help build capacity for over 30,000 additional procedures, and more than 1.25 million additional diagnostic tests, which use CT or MRI scanners
• £70m to invest in new radiotherapy machines to improve cancer treatment
• Over £2bn for NHS technology and digital improvements to increase productivity and save staff time
• Over £600m increase in local government spending to support social care services
• £26m to open new mental health crisis centres
Key for the healthcare property sector was the announcement that the health and social care capital budget will increase by 9.8% and 12.1% (or £3.1bn overall) this year and next.
The commitment to improving the estate comes after a recent report by Lord Ara Darzi found the NHS had been ‘starved of capital’ funding during the 2010s — a £37bn shortfall — and that this has prevented hospitals from being productive.
Reeves said Phase 1 of the Spending Review provides record levels of capital investment for health, with an increase of £3.1bn in 2025 26 compared to the 2023-24 outturn, rising to £13.6bn, a two-year average real-terms growth rate of 10.9%.
This will, she said, begin to reverse the trend of capital underfunding, with over £1bn to tackle dangerous reinforced autoclaved aerated concrete (RAAC) and make inroads into the existing backlog of critical maintenance, repairs, and upgrades across the NHS estate — protecting staff and patients and boosting NHS productivity.
She also pledged to establish a dedicated fund to deliver around 200 upgrades to GP surgeries across England, supporting improved use of existing buildings and space, boosting productivity, and enabling practices to deliver more patient appointments.
And it will enable continued delivery of the Government’s beleaguered New
Hospital Programme (NHP) on a moresustainable and deliverable footing, moving swiftly to rebuild hospitals wholly or primarily built with RAAC or which are currently being built.
Remaining schemes will be delivered through a rolling programme of major investment as part of the Government’s commitment to providing hospital infrastructure investment.
Further details regarding the programme review and next steps will be set out by the Department of Health and Social Care ‘in due course’, a spokesman said.
Commenting on the implications of the speech, Anandaciva, said the cash would not be felt on the ground as much of it would be eaten up by new staff pay deals and the rising costs of delivering care.
He added: “The 3.8% real-terms uplift over two years to the Department of Health and Social Care budget will help sustain services, but is unlikely to drastically improve care over the rest of this year, and certainly not overnight. That’s because the £22bn for two years allocated for day-today spending will also need to cover existing commitments for new staff pay deals and rising costs of delivering care.”

towards hospitals, eyes will turn to the Spending Review to secure money needed for transformation.”

Commenting on the increased capital funding, Michael Woodford, director of the London studio at White Arkitekter, said: “The UK’s healthcare system has been suffering from inefficient funding for too long, so we’re pleased to hear about the budget allocation towards healthcare buildings and equipment.
“While this is a step towards reducing the scale of the backlog, there is a pressing need for capital investment in the context of the climate crisis.
“This means upgrading and transforming our hospitals to create high-quality healthcare environments with a sustainable design that stimulate the circular economy.
“We will be looking attentively at how the funding for the next financial year will be distributed, strongly encouraging the Government to account for renovation and planning policies that will enable us to deliver modern, healthy hospitals for its patients, people, and employees.”

Richard Coe, project director at Kajima Europe, added: “The £31bn increase in the capital budget is a positive step towards revitalising the NHS and addressing the immediate challenges faced by the healthcare system.
“However, the industry needs a pipeline
The Nuffield Trust’s director of research and policy, Becks Fisher, added: “The funding will meet the health service’s immediate day-to-day needs, but will not stretch far towards the Government’s ambitions to rebuild an ailing NHS.
“The increase in the overall Department of Health and Social Care budget is sufficient to meet the urgent £4.8bn funding gap facing the NHS in England. However, it is less clear how non-NHS health spending, such as for public health, will fare once those unavoidable immediate pressures in the NHS have been addressed.
“The Government is right to want to shift care from hospital to community, but with most funding seemingly targeted
The Government is right to want to shift care from hospital to community, but with most funding seemingly targeted towards hospitals, eyes will turn to the Spending Review to secure money needed for transformation
of projects to ensure a steady flow of investment in health infrastructure.
“Projects take a long time; we need to do better in delivering key elements of health infrastructure.
“We hope to see a clear pipeline addressed in the 10-year plan for the UK’s health system in the spring, which will attract investment, reduce the costs associated with delivery, and encourage economic growth.”
And Anandaciva described the increase in capital spending as ‘a modest downpayment’, adding: “This will go some way towards reducing the waiting list in coming years, by increasing the number of hospital beds and surgical hubs in the NHS.
“However, the existing backlog of NHS maintenance issues with buildings and equipment is a staggering £13.8bn and the extra funding will only be a modest downpayment on what is needed to tackle unsafe and outdated NHS facilities.”
To truly meet the need for more-modern, fit-for-purpose buildings, there have been calls for a new approach to using private finance following the cancellation of PFI.

Following Reeves’ speech, Peter Jackson, senior associate at UK and Ireland law firm, Browne Jacobson, said: “PFI was cancelled in 2018 after receiving criticism for issues including perceived poor value for the taxpayer and windfalls for investors that refinanced debt at lower rates following the riskier construction phase.
“The Government must identify a new private finance model that learns from the mistakes of PFI to ensure the public purse receives better value and control, while remaining attractive to the private sector.”
John Hutton, a former cabinet minister who now chairs the Association of Infrastructure Investors in Public Private Partnerships, added: “The Chancellor’s commitment to public investment in new
infrastructure is to be welcomed. However, it will be impossible to get the scale of investment needed to get Britain building again without private financing.
“The UK is one of the only countries in the developed world that doesn’t use public private partnerships to build new hospitals, schools, and transport.
“We need a modern partnership between the private and public sectors that addresses the issues of the past if we’re avoid another lost decade of British infrastructure.”
The private sector will also be crucial in delivering the additional services outlined in the Budget, experts said.
Carly Caton, a partner at Browne Jacobson, told Healthcare Property: “Any new funding that helps to add capacity will, of course, be welcomed within the NHS.
“But, to prevent this just being a sticking plaster, we must also identify new avenues to generate additional revenue for trusts and their NHS patients.
“The Government should actively encourage trusts, backed by funded support programmes, to develop a commercial mindset and explore how to maximise their available resources, while simultaneously improving healthcare services for the general public.
“Increasing private patient activity within NHS hospitals is one of the easiest routes to achieving this.
“Most trusts already do this to some extent with private patient units, but these tend to be relatively small, meaning they provide untapped potential in terms of raising additional income to plough back in to NHS services.
“There are numerous way of expanding these units and it doesn’t necessarily require significant capital investment if a trust is willing to partner with a private provider.
“Partnership structures can extend from commercial agreements to developing some form of physical expansion to estates, and all while creating new income streams for
It is disappointing that the Budget does little to stabilise the beleaguered social care sector in the immediate term, and that the supporting rhetoric made no mention at all of the future reform it so desperately needs
NHS patients at no cost to the taxpayer.
“Many of our decision-makers are all too keen to shout from the rooftops about the NHS being broken, but this isn’t necessarily the case — it boasts world-leading assets and expertise that, if harnessed correctly, can provide ample opportunities for healthcare to help drive economic growth as opposed to hampering it.”
The announcement of a £600m boost for social care, while widely welcomed, was also deemed inadequate to fix a ‘broken system’ and will mean some providers having to make tough decisions, the experts warn.
Anandaciva said: “It is substantially less than what has been allocated to the NHS — and many social care leaders will look on with envy at the funding their health service colleagues have received.
“Care providers will also have to shoulder extra employer costs from national insurance changes and minimum wage increases, exacerbating the difficult financial position they are in.”
Fisher adds: “Increases in local authority budgets are welcome, but they face hugelydifficult decisions on where to spend to meet myriad local needs.
“The £600m social care grant announced for next year will be insufficient to enable councils to keep pace with demand.
“While changes to the carers’ allowance are a positive development and the national minimum wage and living wage increases will benefit much-valued care staff, they will put buckling council and provider budgets under pressure.
“On top of this, higher national insurance rates will pile still more costs onto organisations which provide care, many of which are already struggling.
“With no specific support to cover these costs, care providers are likely to face financial collapse, or difficult choices to pass higher costs on to people who pay for their own care.
“It is disappointing that the Budget does little to stabilise the beleaguered social care sector in the immediate term, and that the supporting rhetoric made no mention at all of the future reform it so desperately needs.”
Anandaciva concludes: “On the whole, this Budget has been a starting point for the investment and reform that is needed to begin to stabilise the trajectory of NHS performance, but it is not enough for the system to deliver the wholesale shift needed for a health and care system fit for the future.
“To achieve that, more funding will be needed in next year’s Comprehensive Spending review.” n





Browne Jacobson and the NHS Transformation Unit explore provider group models in new report
Group working between NHS healthcare providers presents opportunities to improve organisational resilience and patient outcomes, according to a new report.
UK and Ireland law firm, Browne Jacobson, and the NHS Transformation Unit published the Collaborative Care: Creating Value from Scale guide to
coincide with NHS Providers’ annual conference in November.
It summarises common challenges and opportunities associated with group working — shared by NHS hospital group leaders during two roundtable events in October facilitated by Sir David Dalton, former NHS Providers chief executive — and offers guidance on how trusts can
develop group models that help them to balance responsibility ‘at-scale and at-site’.
The report outlines how establishing a single legal governance structure can enable strong decision-making, while retaining a flexible model that facilitates a bespoke response to local healthcare needs.
For a multi-trust group, governance structures are centred around joint leadership and a formal joint committee; for a single merged organisation, this will be a unitary board.

Christian Dingwall, partner in Browne Jacobson’s health and life sciences team, said: “There have been significant changes to the provider landscape in England over the last 20 years.
“All providers are now working within a provider collaborative in some form

to understand their model and how it operates.
Having a single organisational mind to direct strategies across partner organisations helps to develop a clear narrative that articulates the value proposition of the group model.
and many are also going further by closely collaborating in other ways, such as adopting a form of shared leadership.
“During our discussions with NHS hospital group leaders, we found there is a benefit in not having a fixed model imposed on groups, which means they can be tailored to the local circumstances they aim to address.
“While there is no single blueprint for the mechanics of a group model — which range across a wide spectrum from informal collaboration arrangements to a single merged provider approach — there is an emerging commonality in the core legal governance structures within the group.
“Having a single organisational mind to direct strategies across partner organisations helps to develop a clear narrative that articulates the value proposition of the group model. In turn, this can tackle some of the obstacles to effective collaboration, such as historic differences between providers, a sense of tribalism and a lack of trust.
“Ultimately, successful collaboration can support providers in their quest to drive positive change that delivers safe, effective, and sustainable services to the populations they serve.”
Examples of the recommended governance structures are explored in the report.
A unitary group board is the model adopted by single trust groups such as the Royal Free, Barts Healthcare, and Mid and South Essex trusts.
A joint committee group board is the model adopted by multi-trust groups such as Liverpool University Hospitals, University Hospitals Tees, and Royal Wolverhampton and Walsall trusts.
Developing a sound understanding among staff, stakeholders, regulators, and non-executive directors is therefore key to success, the report says.

Janet Budd, director of the NHS Transformation Unit, said:
“Structural change by itself is not the route to improvement — there must be a clear purpose for making the change to a group model, aligned to addressing the challenges and issues which are not capable of being resolved by
“In the absence of a ‘group blueprint’, providers are faced with a range of delivery options when considering how best to collaborate.
The report identifies a key benefit of the multi-trust model of taking time to roadtest working as a single organisation, allowing NHS hospital groups to undertake important groundwork for how a merged organisation might operate in future.
Developing a clear risk-led governance and escalation framework is key to this, enabling group leaders to adopt an assurance focused and strategic approach to leadership.
Another challenge noted by existing provider groups is transparency and clarity of governance, supported by effective communications, to help regulators such as the Care Quality Commission
“This means leaders need to make informed choices as they design and develop a tailored model which aligns to their needs and strategic aims and this involves careful consideration of both the benefits of scale, across multiple hospitals, and the retention of strong site/ hospital leadership.
“Developing a shared view and ambition can help trusts considering collaboration to plan for a solution which best addresses the issues they have jointly identified.
“Our recent roundtable events — and the associated report — provided a great mechanism to explore these matters with inputs from colleagues from across the country.”
To read the full report, visit the NHS Transformation Unit website. n

New report reveals the lasting impact of the NHS Local Improvement Finance Trust (LIFT) approach to health infrastructure delivery
Anew report exploring the value of the NHS Local Improvement Finance Trust (LIFT) portfolio reveals that the public/private estates delivery model has delivered a host of qualitative and quantitative benefits.
The LIFT Programme is a partnership of the public and private sectors which supports, improves, and delivers lasting transformation of the NHS primary care and community health estate.
Since its inception in 2000 it has delivered more than 340 schemes and £2.5bn of capital investment.
PwC’s independent analysis is presented in its report entitled The NHS Local Improvement Finance Trust (LIFT): Occupancy Cost Assessment, which highlights the benefits and advantages of the buildings to local communities and health systems, as well as comparing the relative cost of the LIFT estate to broader NHS and commercial infrastructure.
And it finds that the LIFT estate has delivered a host of qualitative and quantitative benefits, including:
• The LIFT estate has improved the quality and accessibility of services for patients and communities by providing modern, fit-forpurpose and integrated facilities that are flexible and adaptable
• LIFT provides long-term cost certainty to NHS tenants via comprehensive lease agreements. Lease payments for tenants are fixed at lease agreement and increase in line with retail price inflation (RPI) only
• By comparison commercial rents have increased by 25% in the last seven years.
In addition, while the rental payment
Increasing utilisation of the LIFT buildings as core health assets will enable the NHS to deliver the Government’s mission, drive up NHS productivity, and transform care delivery, while achieving greater value


LIFT estate presents value for money and other significant benefits to the NHS, its patients, and staff.
“Increasing utilisation of the LIFT buildings as core health assets will enable the NHS to deliver the Government’s mission, drive up NHS productivity, and transform care delivery, while achieving greater value.
“The LIFT buildings are modern, well-maintained facilities in community settings and through our ability to repurpose and adapt these at pace, we can support the NHS with estate solutions that enable the shift of services into local communities, drive up productivity, and unlock value from the current physical infrastructure.”
the wider estate.
“The analysis we performed using the ERIC data and the LIFT structure reemphasised that value for money in estates needs to be a balanced assessment.
“Headline costs can be misleading and value for money needs to consider wider factors, including maintenance behaviours.
“Managing the estates portfolio will be a continuing challenge and the evolution of ICB estates strategies should allow for more-joined-up masterplanning.
“Our work with CHP re-emphasises that value for money is a broader measure than a headline occupancy price and, aligned to the Darzi findings, ignoring the true cost of a properly-maintained estate is a false economy.” n
Managing the estates portfolio will be a continuing challenge and the evolution of ICB estates strategies should allow for more-joinedup masterplanning

The NHS LIFT Programme (Local Improvement Finance Trust) is a partnership of the public and private sectors which supports, improves, and delivers lasting transformation of the NHS primary care and community health estate.
Community Health Partnerships (CHP) delivers this programme through 49 individual LIFT companies, which have delivered more than 340 schemes and £2.5bn of capital investment.
CHP is wholly owned by the Department of Health and Social Care, which established the programme in 2000 to support the transformation of primary care and increase community access to services
LIFT companies are Public Private Partnerships (PPPs) with 40% public and 60% private ownership.
CHP is the 40% shareholder on all but seven LIFT companies where 10 local authorities — Manchester, Salford, Trafford, Leeds, Newcastle, North Tyneside, Nottingham, Barnsley, Doncaster, and Newham — are also shareholders.
LIFT has brought about the largest and most-concentrated investment by the NHS and the private sector in the primary health care and community estate.
And it was purposefully designed to support better patient outcomes, make services more accessible for those in greatest need, and provide modern, purpose-built environments for staff using off-government debt-funded solutions.
LIFT also delivers strategic estate planning and development capability, which ensures maximum return from health investment.
The programme has also brought a plethora of health and care services together under one roof.
The co-location of a range of service providers in one building has enabled better service integration, and, in turn, facilitated improved joint working as well as better integration of primary and secondary care, community health, and local authority services.
Forty-four of the LIFT buildings are integrated joint service centres with local authorities, including 24 with community libraries. There are also eight purpose-built health, fitness, and wellbeing centres with swimming facilities.


FJimmy Johns, director of corporate debt advisory for the healthcare sector at Christie Finance, takes a focused look at the financial markets that support the care sector, considering the current funding landscape and sentiment in the market
or the last two years, writing any kind of blog or opinion on the care sector and its supporting financial markets has been somewhat of a challenge.
It is a rapidly-changing landscape, with political, economic, regulatory, and global issues all influencing the facets within the day-to-day operations of a care business.
The sector, which delivers frontline services and care to people who can be at their most vulnerable, constitutes a vital part of the healthcare provision in the UK.
And it has been well documented that the UK has an ageing population, with higher needs and earlier diagnoses of conditions.
Alongside subsequent referrals, there is an increase in demand on providers.
Christie & Co data suggests that by 2034, 21% of the population could be over 65, equating to 16 million people.
When exploring funding, any operator or new entrant has to consider the noise that is in the sector, whether it is regulatory, economic, or political.
Established operators will see opportunities in potential homes to improve them, or
When exploring funding, any operator or new entrant has to consider the noise that is in the sector, whether it is regulatory, economic, or political

increase their value.
If this is to be the case, due diligence must be done.
In most instances clear financial forecasts and operational strategy will be essential for a successful lend.
And, more so than ever, existing operators need to be prepared to act on a potential acquisition.
Although, in general terms, lenders will not provide a ‘blank cheque’, from our experience we are supporting clients with an assessment of their current business alongside any potential target, providing confidence to agents and sellers that offers are deliverable.
According to Christie & Co’s market analysis, supply and demand is increasing, especially for the small-to-medium groups.
63% of completions of care homes in the first half of 2024 were between 20-59 beds, subsequently being sold to 30% independent and 32% smallto-medium groups.
The supply of homes into the market between 20-59 bedrooms has remained consistent. However, the demand from operators to acquire has increased by
Lenders will seek confidence in how well a new entrant can operate their first acquisition, what their career history is, and what direct experience they can bring
11% year on year, from 38% in 2023 to 43% in 2024.
Typically, these operators will be wanting to acquire the larger homes of 35-plus beds, potentially a better quality than their existing assets.
This strategy of acquisition and demand is further supported by Christie & Co data through 2023, and H1 of 2024, remaining at its highest since 2021.
This demand has caused values to remain solid and multiple bids on targets.
When seeking to expand portfolios, operators will need to be well prepared with funding strategy.
And this is an area where Christie Finance has supported multiple clients, making sure they are financially fit to acquire.
For new entrants, the key areas to focus on will be the quality of experience or management team.
Lenders will seek confidence in how well a new entrant can operate their first acquisition, what their career history is, and what direct experience they can bring.
The next focus should be on the target acquisition.
What is the quality of the current service provision? What is the regulatory rating? What is the financial performance? Is the current management and senior management remaining?
The funding market is still challenging to navigate for first-time buyers. However, we have supported many to acquire their first home.
Preparation is key to a successful funding application and a lot of our process is to fully understand a clients’ plans with any potential target.


Overall, the sentiment and transactional analysis from Christie & Co’s Care Market Review suggest the market remains buoyant.
However, there is an increasing supply pressure for potential buyers.
There has been a decrease in first-time buyers, which could be due to the decrease in homes below 20 beds and lack of medium providers being able to acquire or upgrade their portfolios, thus disposing of their smaller assets.
The finance market has continued its cyclical nature, with funders changing policies, exiting, and returning.
This makes acquiring debt a challenge, before even getting into the detail of operation, structure, affordability, regulatory, and quality of the asset.
Over the past 12 months we have seen the Bank of England Base rate continue to fall, alongside contracting debt margins.
Appetite remains strong to support the sector, but heightened due diligence and lack of understanding by lenders can sometimes frustrate and protract credit decisions.
The ability to make yourself fit to buy by fully understanding, not only the sector, but structure of debt, the available funders, and the terms that could be available to you, will enable you to act quickly when
Appetite remains strong to support the sector, but heightened due diligence and lack of understanding by lenders can sometimes frustrate and protract credit decisions
offering on target.
Christie & Co released its 2024 Care Market Review in October, analysing a range of topics relating to the UK healthcare business market, including capital markets, land, and development, the transaction market, shifts in local authority fee rates, operator sentiment, and featuring a Q&A with Matt Lowe, chief executive of LNT Care Developments.

Alternative lender, Broadwood Capital, has secured backing from asset manager, Aviva Investors, for a dedicated sustainable later-living credit fund.
The Broadwood Later Living Sustainable Construction Finance Fund will provide funding for the development of new care homes and later-living residential properties which meet selected environmental and sustainability criteria.
The debt fund will provide developers with loans of up to 90% of the total cost and 75% of the value to support the ground-up construction of new-build property.
Developers will need to demonstrate that completed properties meet, or exceed, energy use targets and that the development promotes environmentallysustainable construction.
The discretionary fund has initial capacity for £100m of gross lending, with the seed investment being provided by Aviva Investors Climate Transition Real Assets Long Term Asset Fund (LTAF).
The intention is to grow the fund with further third-party investment in the first half of this year, providing investors with access to a credit strategy focusing on delivering assets that meet the demands of the ageing demographic.
As part of the agreement, Ben Sanderson,
managing director of real estate at Aviva Investors, will join the board of the fund’s investment management company; while Luke Layfield, portfolio manager of the Aviva Investors Climate Transition Real Assets LTAF, will sit on the fund’s credit committee.
Dan Smith, chief executive of Broadwood Capital, said: “There is an indisputable demographic shift taking place in the UK.
“We have a rapidly-ageing population and do not currently have the infrastructure to support it.
“With future later-living accommodation requirements unlikely to be delivered via the public purse or from traditional lenders, we need to look at more-creative ways of providing essential capital to developers.
“The fund does exactly this and not only offers investors access to a credit strategy delivering attractive risk adjusted returns, but also to a strategy which is promoting the climate and social agendas.
“This is a very-challenging environment in which to raise capital, and we are incredibly privileged to have the support of Aviva Investors and are looking forward to working with Ben, Luke, and the wider Aviva Investors team, as we grow the fund over the coming years.”
Layfield added: “Later living is an
There is an indisputable demographic shift taking place in the UK. We have a rapidlyageing population and do not currently have the infrastructure to support it
important part of the UK housing market and one where there is a fundamental need to support supply of new homes.
“As an investor aiming to deliver longterm investment outcomes for retirement savers, while also deploying capital where it has the potential to make a positive contribution within communities, we are very pleased to partner with Broadwood Capital, a best-in-class credit manager, in providing funding to deliver additional later-living facilities.”
The Broadwood Later Living Sustainable Construction Finance Fund is operated and administered by Khepri, an FCA-regulated alternative investment fund manager and fund administrator.
Taylor Wessing was legal advisor for Broadwood Capita on structuring the fund. n
A Qualia Care home — the 73-bedroom St Mary’s Nursing Home in Moston, Manchester — has been sold to Vriddhi Investments, which is backed by Agha Group, on behalf of the administrator, Griffins.
This is the first of the care group’s 14 homes which were initially funded through a Ponzi scheme to be sold following a landmark High Court ruling in September.
Qualia Care Properties and Qualia Care Developments took contributions from individual investors of between £50-70,000 to purchase a long-term lease on a care home room in order to sublet the room back to the other Qualia companies.
In total the scheme received £57m from individual investors between February 2016 and September 2020.
There were 14 homes funded under the Qualia Care brand before both entities were liquidated in the summer of 2022 and Qualia Care went into administration in October of that year.
While some of the care homes have since closed, nine, including St Mary’s, are still in operation.
In September a team from Gateley Legal secured an order from the High Court which enabled the sale of the home with ‘fractional ownership’ leaseholders surrendering their leases.
Colliers’ healthcare team was appointed to sell the homes and St Mary’s nursing home received more than 50 expressions of interest.
Administrator, Stephen Hunt, said: “By securing the legal ruling we have been able to unlock the sales process of these assets, which will enable investors and creditors to recover some of their funds.
“We have managed to secure a strong outcome for those involved in St Mary’s and anticipate a similar level of interest in the other operational assets within the portfolio.
“This will be a landmark case, which we hope will now be able to proceed at pace.”
The acquisition marks Agha Group’s inaugural investment in the healthcare sector.
The home will be operated by Serene HC UK, a group of healthcare professionals.
Agha Sameer Anwar, chief executive of Agha Group, said: “St Mary’s Nursing Home was carefully selected as it is ideally placed to benefit from our operating company Serene HC’s particular skill set; working closely with the community to ensure that the most vulnerable are given the dignity and highest

level of focused care they deserve.
“Our plans to invest significantly in the fabric of the property will support this commitment to provide leading care for our customers.
“We’re looking forward to working with the staff and providing reassurance to them and the residents who have been through a significant period of uncertainty.”
Vriddhi Investments was advised by commercial estate agent, Fisher German’s investment team, with legal advice provided by Browne Jacobson’s healthcare team.
Commercial real estate firm, Colliers, in association with chartered surveyor Peter
Fenwick & Co, facilitated the sale.
Ali Willoughby from Colliers’ healthcare team said: “There was a real swell of interest in St Mary’s due to the size and quality of the home.
“This has of course been a concerning time for residents and staff, who I’m sure are pleased that there will be stability going forward following completion of the sale of the operational asset.
“There is continuing interest in the wider Qualia Care portfolio, and we’re hopeful that the ongoing sales will result in the individual investors being able to recoup a good proportion of their funds.”

Elevation Advisors LLP has announced that its Elevation Healthcare Properties real estate fund has completed the sale and leaseback of a care home in St Neots, Cambridgeshire.
Henbrook House is let to Connaught Care on a long-term lease with RPI-linked escalator with cap and collar.
Connaught is an operator of four high-quality prime care homes in the East and South East of England, comprising 281 beds and with an active pipeline of seven development sites providing residential and residential dementia care in purpose-built environments.
Henbrook House, which opened in May 2024, has 69 ensuite wetroom bedrooms designed for the comfort and safety of relatives and staff.
Other amenities include a bistro, cinema room, private dining room, and health spa. In line with EHP’s ambitious ESG strategy, Henbrook House has a high build quality with a design emphasis on environmental performance.

New Construction rating of ‘Good’ and is expected to achieve a BREEAM In-Use rating of ‘Very Good’ with the potential for ‘Excellent’.
In addition to all-electric kitchen and laundry equipment, minimising gas use, the home incorporates water-efficient fittings throughout.
To encourage sustainable travel, there are also EV charging points and cycle storage, in addition to the home’s proximity to local public transport hubs.
The home also offers ample green space to residents, in excess of 30% of the site’s area, to support wellbeing and local biodiversity.
to continue its ambitious growth plans and realise its pipeline of development opportunities that will see us bringing 11 highend homes to the elderly care market in the
James Giles, investment director at Elevation, adds: “We carefully select operating partners who have an excellent record in care and are excited to begin a new partnership with Connaught, adding this high-calibre care home into the portfolio as we continue deployment in EHP.
“This is the 22nd asset addition by EHP this year, bringing the portfolio to a total of 45 UK elderly care home assets with over 3,000 beds and a strong pipeline of further acquisitions and pre-let forwardfunded transactions.
The home already has an EPC A rating, with further plans to install solar panels to improve energy efficiency at the home in the near-term.
The home has also achieved a BREEAM
Andrew Winstanley, chief executive of Connaught Care, said: “We are delighted to have partnered with EHP for the sale and leaseback of Henbrook House.
“This partnership will enable Connaught
“Henbrook House has strong environmental credentials in line with EHP’s ESG strategy and we are delighted to fulfil the market need for care homes which are built for longevity and benefit the lives of residents, staff, families, and the local community.”
Elevation was advised by Bevan Brittan, Grant Thornton, Carterwood Analytics, Pinders, and Envision.
Connaught was advised by Freeths LLP.
Specialist business property adviser, Christie & Co, has been instructed to sell a turnkey healthcare development in Denbighshire, North Wales, on behalf of Star Units Limited.
Star Units acquired full planning permission through Denbighshire County Council in November 2021 for the ‘erection of a 198-bed Registered Care Home (Use Class C2), landscaping, parking facilities, and associated works’.
The 4.54-acre site is situated north of the St Asaph Business Park and is equidistant between the settlements of St Asaph and Bodelwyddan, strategically positioned in a gateway location at Junction 26 of the A55: North Wales Expressway.
Under the consent, accommodation will be arranged in three blocks to potentially cater for a range of resident needs including reablement care, dementia care, palliative care, and general care.
It also includes a suite of communal amenities including a café, a hair salon, a selection of lounge and dining spaces, a GP office, and a family room.
Externally, provision has been made for a landscaped communal courtyard garden, external landscaping, and 100 car parking spaces.
And there is flexibility in the consented scheme which could allow for different configurations and a wide spectrum of operating models across the healthcare and later-living sub sectors.
Potential uses could include a private hospital, elderly care home, specialist care models including ABI or rehabilitation, extra care apartments, an integrated retirement community, retirement housing,

or supported later-living accommodation.
There may also be other uses subject to discussion with the developer. Jordan Rundle, director of healthcare investment and development at Christie & Co, who is handling the sale, said: “Our Wales Healthcare Market Insight report, published in May 2024, highlighted the increasing undersupply of market-standard care beds in Wales, with a greater need in North Wales, and that only four newly-constructed elderly care homes have been opened in three years, none of which are located in the North Wales region and only serve to underpin the material requirement for market-standard beds in the region.
“The Ty Seren project can provide an immediately-deliverable solution.”
Bupa Health Services has announced the acquisition of The Dermatology Partnership consisting of seven specialist dermatology clinics across the UK.
The clinics are based in London’s Harley Street, Wimbledon, Oxford, Canterbury, Cheltenham, Cheadle, and Shrewsbury.
The acquisition enables Bupa’s UK Insurance customers to have faster access to the dermatology care they need, alleviating pressure on services.
Sarah Melia, general manager for Bupa Health Services, said: “We’re delighted to acquire The Dermatology Partnership and expand our specialist services into dermatology.
“This new partnership will enable us to create a seamless pathway for customers to have their concerns addressed.
“Our long-term strategy is to provide more Bupa services directly to customers, which is further cemented with the acquisition of The Dermatology Partnership.”
The acquisition follows Bupa Health Services’ successful acquisitions of London Medical and Blackberry Clinics.
Christie & Co has announced the sale of Stirling Dental Care in Stirling, central Scotland.
Stirling Dental Care is a three-surgery, mixed-income dental practice with around 4,500 registered patients, located in Dunbarton Road in the city of Stirling.
The practice was previously owned by Jane Lang, who decided to sell to exit from practice ownership.
Following a confidential sales process with Joel Mannix at Christie & Co, it has been purchased by Christopher Black & Hamish Brown of Black & Brown Dental, which also owns Oakley Dental Practice in Dunfermline.
Lang said: “I set the practice up in 2006 with a strong ethos of patient-centred, highquality dental care.
“Over the years, the practice has grown from a single-handed practice to three dentists and a hygienist.
“The private aspect of treatments has grown considerably, not least as the dentists have all upskilled in advanced restorative treatments.
“The practice was relocated to provide a modern purpose-built facility with an additional surgery and storage space and I elected to sell as I was finding practice ownership had become very onerous, particularly following the huge impact of COVID and the practice relocation.
“However, I knew I was not ready to retire as I still very much enjoy clinical dentistry. I

sincerely hoped the practice would continue as an independent practice, upholding the same values of patient-centred care and quality dentistry, with a fresh look at some aspects of the business from a younger enthusiastic owner.”
Black adds: “Stirling Dental Care offered us the opportunity to purchase a modern, forward-thinking dental practice and this was the logical next step to expand the group.
“It is a well-established practice with a strong reputation within the community for providing patient-focused quality dental care and there is space within the current practice to expand the provision of dental care, and we intend to increase NHS registrations and provide all aspects of general dentistry within the practice.”
Stirling Dental Care was sold for an undisclosed price.
A later-living development site in the Essex town of Maldon, which has the benefit of outline planning consent for up to 82 apartments over 1.47-acres, has been brought to market.
This is the latest neighbourhood centre scheme being brought forward by Charterpoint Group alongside Charterpoint Senior Living, an experienced specialist senior living developer.
The site is situated in a high-profile position in the new Neighbourhood Centre in its Westcombe Park garden suburb development, which comprises a care home, medical centre, convenience food retail, nursery, and ancillary retail uses.
Through the pre-application process, Maldon accepted there is a need for a range of new purpose-built retirement accommodation within its district.
A key part of this is the provision for older people who enjoy the mental health and social benefits of being in a like-minded community, but do not need a care package.
Maldon would be receptive to a planning application for either C2 or C3 later-living scheme.
The scheme benefits from an existing outline consent and offers the opportunity for an operator to incorporate its own bespoke specification and layout requirements at a reserved matters stage of the planning process.
Construction of an adjacent 66-bedroom care home is anticipated to begin early next year.

The wider residential elements of the masterplan are currently being delivered by Countryside Homes, Bellway, and Crest Nicholson.
Jordan Rundle, director of healthcare development and investment at Christie & Co, who is handling the sale, said: “We are pleased to be offering this exciting later-living development opportunity in Maldon’s new Westcombe Park garden suburb.
“The demographic support for a new retirement or assisted living accommodation in the catchment is excellent, with 25,000 people over the age of 65, along with elevated affluence levels.
Deer Park Care Home in Holsworthy, Devon, has been sold to Camelot Care.
Situated in Rydon Road, the former care home, which traded for many years, offered care for the elderly with a CQC registration for up to 56 residents. It has now been purchased by Camelot Care, a familyrun business with 25 years of experience, which is looking to refurbish the site to provide highquality dementia care services.
Eve Apperley, business agent at Christie & Co, who handled the sale, said: “We received
“The neighbourhood centre will be the focal point for over 1,000 new homes currently coming forward on the masterplan and is close to a range of desirable local amenities including retail, eateries, sports clubs, and green spaces, including ancient woodland to be managed by the Lands Trust.”
Giles Nursey, managing director of Charterpoint, adds: “Westcombe Park offers a high-quality environment featuring a pleasant landscaped setting and has good access to public transport, amenities, and local services that are ideal for multi-generational living.
“We are pleased to be able to work with Countryside to deliver this exciting senior


Inside issue 04, July-August 2024
• Advocating a simpler approach to the healthcare planning process
• The implications of a new accountancy treatment on NHS leases
• Designing mental health facilities closer to home Scan to read now

Inside issue 05, September-October 2024
• Contractor appointed to build £15m community health centre
• Keyworker housing model supports recruitment and retention of staff
• Investors and property developers remain interested in health and care sector
Scan to read now

Inside issue 06, November-December 2024
• Why we need to rethink our approach to healthcare design and delivery
• How private capital can bring long-term solutions for the health estate
• RAAC hospitals to be rebuilt despite Labour's spending review
After a decade of planning and construction, the new Midland Metropolitan University Hospital has been completed
Photos: Paul Raftery

The long-awaited Midland Metropolitan University Hospital (MMUH) has been completed, providing a new, state-of-theart acute hospital for Sandwell and West Birmingham NHS Trust.
Designed by HKS, Cagni Williams, and Sonnemann Toon Architects, the handover of the building comes after a decade of close collaboration with clients and co-consultants.
The flagship project, part of the Government’s New Hospital Programme (NHP), sets a new standard for clinical healthcare design and is one of the mostadvanced medical centres in Europe, as well as a community regeneration catalyst in an area with high levels of deprivation.
Bringing acute and emergency care from two separate hospitals into one centralised hub, MMUH is designed to support operational efficiency and technological innovation, while enhancing the patient and staff experience.
Featuring surrounding green space, a central Winter Garden, and accessible roof terrace, it delivers a new model of care that encourages patient mobility, independence, and wellbeing.

The 11-storey hospital spans 84,000sq m and provides both a purpose-built emergency department with imaging and diagnostic services and a dedicated children’s emergency department and assessment unit.
It also has 13 operating theatres for
emergency, planned, and maternity surgery. Additional facilities include a midwifeled birthing unit and delivery suite, two maternity wards and antenatal services, a neonatal unit, same-day emergency care for adults, and a regional sickle cell and thalassaemia centre.


The hospital’s efficient spatial layout centres around the ‘hot block’ clinical facilities, arranged around six internal courtyards.
Less-heavily-serviced ward accommodation is arranged above the ‘hot block’, with two levels of car parking below.
And MMUH’s Winter Garden covers five floors across the east-facing side of the building.
The garden’s ETFE roof offers a highlytransparent, lightweight, and sustainable façade, bringing natural light into the heart of the building, while offering impressive views back out over the immediate neighbouring communities, Birmingham, and the surrounding countryside.
It provides a peaceful and therapeutic space to promote healing, relaxation, and reflection and delivers a bright and modern arrival point to the hospital, with transparent lift cores, stairwells, and walkways further enhancing daylight, connectivity, and wayfinding across each floor.
The Winter Garden gives way to an outdoor roof terrace, accessible for patients, visitors, and staff and also features an expansive art gallery space, overnight visitor facilities, and a multi-faith prayer room.
Individual patient rooms and wards are designed to optimise natural daylight and views, creating a calm and uplifting environment to support patient recuperation.
The hospital provides over 700 new beds and 50% of inpatients will be cared for in single rooms with ensuite bathrooms.
Individual patient rooms and bays have been designed to promote patient safety and ease of visibility for staff, and single-






occupancy rooms allow for easy adjustment to accommodate additional levels of isolation if required.
Logistics, wayfinding, and patient flow are also central to the design.
The interior has a clear design language, centred around easy-to-navigate orange cores, and separate circulation routes are in place for patients, staff, and visitors, to enhance privacy, navigation, and safety.
The paediatric department incorporates a more-colourful palette, along with play areas and spaces for children’s artwork to go on display.
To optimise flexibility, the hospital design is based on a single structural grid. This accommodates a wide range of clinical and functional spaces that can be easily adapted for future expansion, and to support the delivery of new service models and working practices, as medical technology and acute healthcare needs evolve.
The building’s external envelope facade materials are organised by vertical elements to break up the building mass and reflect the rhythm of the structural grid.
Alongside ETFE pillows, the palette
includes terracotta, concrete, painted metal cores, and metal louvres.
Sustainability is at the heart of the design approach.
The Winter Garden is south facing and passively ventilated, and the hospital also incorporates intelligent lighting, solar PV panels, and water conservation measures.
The building design includes a unitised façade system and components including the Winter Garden roof and bridge links have been prefabricated offsite, making it an exemplar in the use of Modern Methods of Construction (MMC).
MMUH will have a range of transport options, including dedicated public transport service routes, electric vehicle charging points, and secure cycle storage facilities.
Green spaces surrounding the hospital include a circular, cricket pitch-sized green; a series of landscaped beds; and a community garden, as well as pedestrian and cycle routes alongside the canal, helping to transform this post-industrial site.

The new hospital represents a landmark development and a vehicle for growth for this designated regeneration zone between Birmingham and Sandwell.
The wider masterplan includes The Midland Metropolitan Learning Campus, a new education and employment building under construction, plus additional plots for development, earmarking it as an emerging destination for the West Midlands.
Jane Ho, regional practice director for health at HKS, said: “HKS is thrilled to see Midland Metropolitan University Hospital open its doors to patients after collaborating closely with the Sandwell & West Birmingham NHS Trust and the wider project team throughout the last 10 years, building a trusted partnership to create a world-class hospital.
“The design responds to the challenges faced by trusts, workforces, and patient environments today and will be the catalyst for improving the patient experience, staff environment, and outcomes for the region.
“The successful delivery of this project is a testament to the unwavering resilience



The design responds to the challenges faced by trusts, workforces, and patient environments today and will be the catalyst for improving the patient experience, staff environment, and outcomes for the region
and dedication of the trust project team, without whom this wouldn’t have been possible.”
Edward Williams, founding director of Cagni Williams, adds: “From the very beginning we were determined to design a ground-breaking hospital together with the wider project team.
“From the earliest sketches and models, the idea of the Winter Garden was always to create a central heart for the hospital — a welcoming, unique, and vibrant space for patients, staff, visitors, and the local community.
“It’s been a rewarding journey, working

closely with specialist contractors to bring the vision to life, while preserving the integrity of the original design.
“Good ideas take time and dedication, and the result is a testament to 10 years of constant collaboration and hard work.”
And Cressida Toon, founding partner of Sonnemann Toon Architects, said: “We are privileged to have played a role in this transformative project, witnessing years of dedicated planning come to fruition.
“The final outcome exemplifies the principles of efficient clinical design, established with care from the outset and safeguarded by stakeholders throughout the
From the earliest sketches and models, the idea of the Winter Garden was always to create a central heart for the hospital — a welcoming, unique, and vibrant space for patients, staff, visitors, and the local community
collaboration and it is deeply gratifying to see these concepts realised so successfully.
“This project is a testament to teamwork, considered design, and a shared commitment to improving healthcare environments and we are proud to have contributed to a development that will positively impact all who use it and are confident this facility will not only transform healthcare delivery for the local community, but will also serve as a catalyst for Sandwell’s future growth and prosperity.”


This article provides an overview of Belmont Healthcare Group’s new £5.5m dementia care development in Gravesend, Kent, which marks a significant milestone in supportive design for people living with dementia
Belmont Healthcare Group recently announced the completion of the first phase of an ambitious £5.5m development project aimed at providing dedicated dementia care at Wombwell Hall Care Home in Gravesend, Kent.
This scheme, christened ‘Copperfield’, honours the area’s rich connection to Charles Dickens and marks a significant milestone in dementia care in the region.
The Copperfield phase introduces 22 ensuite rooms and four suites, providing an additional level of luxury, with a TV seating area and private access to patio garden areas.
The emphasis was on creating a thriving environment for those living with dementia, with amenities including a bistro, beauty salon, private dining areas, and a 24-hour manned reception, designed not only for comfort and convenience, but also to promote a high quality of life.
Central to the design ethos is the balance between independent living and a safe, secure environment.
Two general-use kitchens, quiet lounges, family rooms, and private patio areas provide residents with spaces to engage in everyday activities, socialise, and relax with
their family and friends.
Developed in collaboration with specialist dementia care design studio, ADG Architects, the approach ensures that every aspect — from the choice of furniture to the selection of wallpaper — supports safety and wayfinding and reduces confusion.
Local historian and historical advisor to Swanscombe & Greenhithe Town Council,
Christoph Bull, played a crucial role in integrating the rich history of Gravesham into the home.
And the Copperfield phase celebrates not only Charles Dickens, but also pays homage to other local historical figures and landmarks, such as the real-life princess, Pocahontas, who is buried at St. George’s Church, and the now-demolished grand stately mansion of Wombwell Hall itself.

These historical references are thoughtfully woven into the design, creating a familiar and comforting atmosphere that encourages residents to reminisce and feel at home while still being connected to the local community.
Adam Hutchison, managing director of Belmont Healthcare, said: “Completing the first phase of our development is a significant achievement for Wombwell Hall Care Home.
“Our goal has always been to create an environment where people living with dementia can thrive, feel safe, and enjoy a high quality of life.
“By integrating the latest in care facilities with a deep respect for the rich history of Gravesham, we’ve created a truly-unique space that both residents, their families, and our care teams can cherish.”
Following the successful completion of the Copperfield phase, Belmont Healthcare is moving onto the second phase of development, named ‘Pickwick’.
This building will offer comprehensive dementia nursing care, further enhancing the care home’s capacity to support the community.
Hutchison said: “Wombwell Hall Care Home's groundbreaking development sets a new standard for dementia care facilities.
“By combining luxurious surroundings with the latest in care innovations, the home is poised to become a beacon of excellence in the region, ensuring that residents living with dementia receive the highest standard of care in an environment designed to support their independence and wellbeing.”
When all phases are fully completed, the home will offer 102 rooms including 60 ensuite bedrooms and larger suites.
Speaking to Healthcare Property, John Bell, architect and director of ADG Architects, explained: “This is a working care home and the original site featured four single-storey properties all identical to each other and each with 30 bedrooms with a central core.
“However, they had no en-suite bathrooms or wetrooms and they wanted to address this.
“Working with a live site, we looked to break down the project, developing the scheme zone by zone.”
The first decision was to reduce the number of rooms in each block, from 30 to 22, a bold decision for any operator, but essential to provide the ensuite facilities and to enable a household model to be created which would provide a more-supportive and lessinstitutional environment.




“This approach allowed us to create two ‘households’ within Copperfield — one with 10 rooms and one with 12 rooms, designed around a central hub area,” explains Bell.
“The intention for the central hub was for it to be multi-use, and when we do Pickwick we will be using the same approach, but maybe the hub area can be used for different activities. That way all four buildings will have a unique element and it will encourage movement between them and that feeling of a community.”
The design team visited the worldrenowed Hogeweyk dementia care village in The Netherlands to get inspiration for the build.
And they are hoping to replicate some of the external spaces within that flagship development on the Wombwell scheme.
“Outdoor space is very important and currently there is a carpark at Wombwell,” said Bell.
“We are looking to landscape this in the final phase and hopefully maximise external space so that residents can move about in a safe environment.”
He added: “Our whole approach has been about making spaces homely and recognisable and, by reducing number of beds, it means we haven’t got 30 residents all trying to live in the same space.
“Instead they have more choice, with communal and quiet lounges, seating areas, and spaces where people can make a cup of tea.
“The design is also all about destination, which is important for people living with dementia.”
Carolyn Mace, senior architectural designer at ADG Architects, was responsible for the interiors at Copperfield.
She said: “We took a sensitive approach, creating an environment that is friendly and homely, rather than clinical, with neutral colour palettes based around warm tones

The idea is to encourage residents to come out of their bedrooms and have social interaction, which is important for people in care homes and extra important for people with dementia
with pops of colour and tactile materials.
“These colours and textures are inspired by the natural environment and use imagery which is familiar to people and not too overpowering for those with dementia who may suffer from confusion or visual impairment.
“The idea is to encourage residents to come out of their bedrooms and have social interaction, which is important for people in care homes and extra important for people with dementia.
“The entrances spaces and central hub, in particular, feature lots of daylight and are very accessible, with limited furniture to reduce the risk of trips and falls.
“Bedrooms also have lots of natural light and scope for residents to personalise their environment — maybe put an armchair in from home, or picture frames on the chest of drawers.”
Wayfinding was also key, with all spaces clearly labelled and vision panels enabling residents to see what is going on inside the rooms.
“All of day spaces have different colour scheme, so residents can make the association and in corridors there are no dead ends and a lot of natural light and views out to the gardens, which helps with orientation,” Mace adds.
In addition, the project was designed to be energy efficient and sustainable.
Bell said: “The refurbishment enabled
us to invest heavily in the energy efficiency of the building.
“It wasn’t too bad before, but there were energy efficiency technologies which were installed, but never well used, such as solar panels, which we have recommissioned and which should provide around 80-90% of electricity supply for the development.”
Copperfield was refurbished in just four months and work on Pickwick is expected to take 4-6 months.
Bell said: “This project is an opportunity to create a global masterplan for the Wombwell site.
“We are taking an existing home and repurposing it in a different way for residents with complex care needs.
“Dementia comes in different forms and people deal with it in different ways — some are very quiet, but very mobile, while others can be aggressive and quite insular.
“Having different units doing different things means they can support residents with a range of needs.
“The scheme is evolving as we continue, with lessons learned from Copperfield being put into the design of Pickwick.”
Claire Skinner, manager at Wombwell Hall Care Home, concludes: “We feel tremendously lucky to be bestowed with this bespoke facility and are excited to move forward with the next phase of our project, continuing our commitment to providing exceptional care and support to our community.” n

How a challenging art installation was key to the construction of the new hospital
Ten years ago, Tony and Karen van de Bospoort of Hospital Art Studio collaborated with Judith Martin, then a specialist nurse for organ donation at Sandwell Hospital in Birmingham, to create a temporary sunflower artwork.
The sunflower was chosen as a symbol of renewal and hope, a meaningful tribute to the gift of organ donation.
And, with plans already in motion for the new Midland Metropolitan University Hospital, Martin envisioned a larger, permanent installation to carry this message forward.
Years later, Martin reconnected with Hospital Art Studio to discuss bringing this vision to life.
From there, the design team explored multiple concepts, producing numerous drawings and 3D renders for each.
Harry van de Bospoort led this creative process and each iteration brought new ideas, refinements, and options to consider as the team experimented with different shapes, compositions, and lighting techniques, carefully weighing each option to find the right balance.

Shackleton co-ordinated with skilled metalworkers and an electrician to bring the design to life, making necessary adjustments along the way to ensure easy maintenance and long-term durability.
Before installation, Richard Molloy, the construction project director for the new hospital, arranged several site visits to assess the space and discuss the specifics.
During these visits, he co-ordinated the removal of lighting fixtures that were initially planned for the area where the sunflower would be placed.
And Molloy arranged for his team to drill an aperture in the ceiling tiles, fit the custom-made fixing plate, and ensure a power connection was in place with a hatch by the sculpture.
John Simpson of Onsite Print Installations Ltd also carried out a recce within ImageCo’s studio, where the team fitted all the petals and then removed them again to figure out the optimal method for installation.
This dedication to fine tuning each aspect of the sunflower ensured the sculpture would not only be visually striking, but would also carry the intended symbolism of life and renewal through organ donation.
As the new hospital was built, Hospital Art Studio was fortunate to work closely with Cagni Williams, the architectural firm overseeing the entrance area.
Together, they fine tuned details such as the ideal hanging height, the placement of the accompanying plaque and wall text, and how the sculpture would integrate with the lighting in the space.
Laura Carrara Cagni, director of Cagni Williams, said: “It was a wonderful design collaboration.
“We feel the artwork integrates beautifully and complements the space, which was our shared goal from the beginning.”
From there, Hospital Art Studio partnered with David Shackleton of ImageCo Ltd and Matty Bullough of Three D Visions to delve into the specifics of fabrication and installation.
Bullough provided detailed CAD drawings down to every nut and bolt, along with structural calculations for wind load and potential pressure, guaranteeing that the sculpture would be fully compliant with health and safety standards for this hightraffic hospital entrance.
This process was crucial for determining how best to access the fixing points to securely bolt the petals into place.
The installation itself was tricky, requiring one person inside the sunflower and another outside to ensure the petals were fixed properly.
The installation was completed over two days in the summer, just before the hospital’s opening.
First, the team mounted the lettering and installed the plaque. Then, the sunflower structure was carefully lifted into place, with the electrical line discreetly routed through the ceiling.
Once suspended, each of the 38 brassfinish petals was secured, followed by the light panel with its Fibonacci pattern and the bespoke ‘sunflower seed’ luminaires.
Harry van de Bospoort, director of Hospital Art Studio, said: “This collaborative journey, supported by the Organ Donor Committee, reflects the spirit of community and generosity at the heart of this project.
“We extend our heartfelt thanks to everyone involved, and most importantly to Birmingham’s organ donors and their families.
“This artwork is dedicated to honouring their selfless gift of life and spreading awareness within the community.” n

Dementia experts from Stirling University have produced fresh guidance on creating truly-supportive environments
The world-renowned Dementia Services Development Centre (DSDC) at Stirling University has issued design guidance for creating supportive environments in care homes for people living with dementia.
It states that: “A well-designed environment can help feelings of comfort and security by promoting independence, personal identity, enhancing confidence and self-esteem, while allowing required care tasks to take place in a dignified way.

feelings which bring back bad memories.
For those who are not able to move around, it is important to provide a room with a view, something absorbing to look at such as a busy streetscape or garden.
And there should also be a choice of spaces available within the home, such as an activity room, a quiet room, and outdoor space.
“This might sound like an overwhelming list, but it is easily achievable.”
To start with, DSDC recommends avoiding creating often-favoured ‘dementia wings’ or ‘households’, stating: “It’s likely that many residents who arrive without dementia will develop it during their stay.
“You want to avoid moving rooms for people with a dementia; they should ideally retain one bedroom throughout their residency.
“A dementia-inclusive design is best to be incorporated throughout the building: this will cater for residents who may not have dementia, but have impairments of ageing such as sight and hearing or mobility issues.”
Instead, the guidance favours creating spaces which ‘draw on a sense of homeliness and familiarity’.
While this can be a balancing act, avoiding clinical environments is best, the experts said, as they can be distressing or evoke negative
“Allowing residents to bring their own furniture and meaningful items will aid familiarity and helps them to settle in,” they state.
Designers should reinforce personal identity through personal objects and familiar fixtures and fittings. For example, focusing on personalisation of the bedroom entrance to differentiate from a corridor of similar doorways and aid wayfinding.
And, when it comes to fitting out bedrooms, the obvious place to start is: does the room look comfortable?
The guidance states: “It needs to be welcoming in addition to the other wellthought-out elements.
“For instance, it’s worth thinking about the flooring in wetrooms. Stippled safety floors in wet rooms can be very uncomfortable underfoot for the thinning skin of an older person.
“What about acoustic comfort? The right flooring, ceilings, wall panels, artwork, and soft furnishings help absorb reverberation, avoid auditory overstimulation, and aid conversation.”
“Residents need to be able to continue to take part in hobbies and interests as well as daily living activities,” it states.
“This could be anything from a baking or gardening group through to being able to hang up the washing.”
To support this, care home designers and operators need to ensure they reduce physical and perceived barriers to allow free movement and access throughout the care home.
“Residents shouldn’t have to be escorted through a restricted access point into a lift to go down a level to enjoy some outdoor space,” it adds.
It concludes: “Dementia design does not need to cost any more to achieve practical levels of finishes. Plus, what is good design for an ageing population is good design for everyone.
“It’s worth remembering that while creating a space that is inclusive for people living with a dementia, you also need to have staff who are appropriately trained in dementia and the building, too.
“Only then, when you have an inclusive space and well-trained staff, will they work in harmony to provide residents with true comfort and care while retaining all of the required practicalities.” n

This article looks at the role of technology in helping healthcare estates and facilities managers to track vital equipment
Each year, hospitals lose approximately 13.5 million working hours due to misplaced equipment, significantly reducing the time staff can devote to patients, and impacting the overall quality of care.
However, it is not only patients that are affected by this; staff and facilities are also impacted as the permanent loss of critical equipment results in significant financial strain as hospitals are forced to replace essential, and often expensive, assets.

To address this, Living Map, a leader in digital wayfinding, has recently launched an asset visualisation and location product which offers a powerful digital solution that enables hospitals to efficiently locate and assign vital assets in real-time including equipment, wheelchairs, and stretchers.
The solution streamlines healthcare operations, enhances response times, and ensures critical assets are always directed to where they are needed most based on their proximity.
In an interview with Healthcare Property,
Peter Asman, chief revenue officer at Living Map, explains: “If you think about hospitals, they are vast buildings with a tremendous amount of high-value, high-tech equipment, so critical items can get lost relatively quickly within the complex space.
“One hospital we are working with has an incredibly-expensive piece of equipment which moves round and they lose it all the time. In fact, they have had to replace it three times already as they couldn’t find it.
“Our asset visualisation platform, Live Locator, ensures that vital resources are always available when needed, improving care for patients and supporting staff in their efforts.”
The system works by attaching an off-theshelf sensor to each piece of equipment the hospital wants to track.
The sensor then sends an X-Y co-ordinate
If you think about hospitals, they are vast buildings with a tremendous amount of high-value, hightech equipment, so critical items can get lost relatively quickly within the complex space
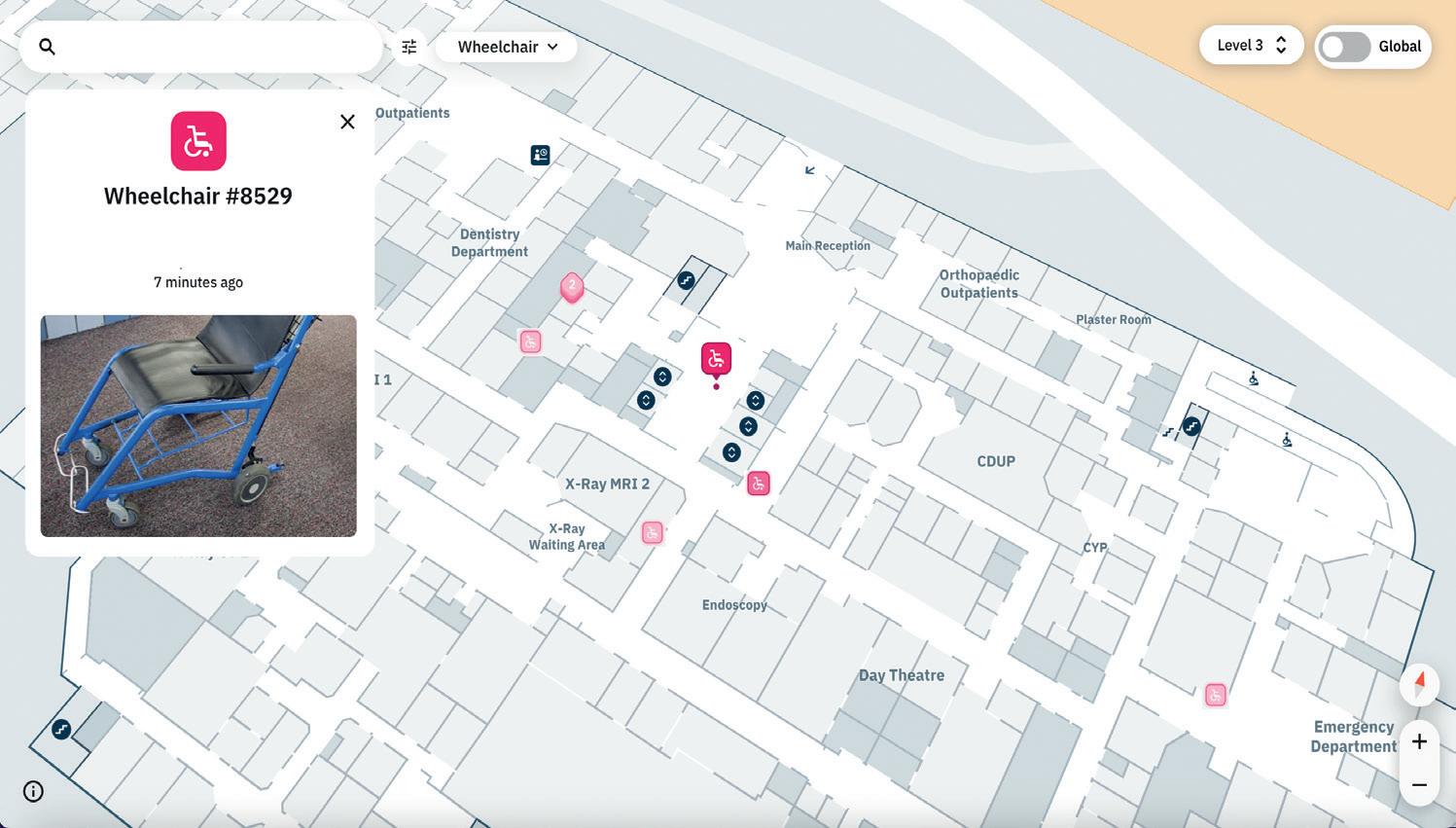

to a transport mechanism which provides an exact location of that asset on an interactive map.
Asman explains: “If you look at wheelchairs, for example, they are ridiculously expensive, and no one can ever find them in the hospital.
“We fix a sensor on each wheelchair and that sends a X-Y co-ordinate, whether it is inside or outside the hospital.
“That co-ordinate can be sent every second, minute, or few minutes, however the hospital decides to do it, and the location is then shown on a map.
“If a porter walking around needs to find a wheelchair, they can go to the system, and it will show there are four in one location and three somewhere else and the nearest one is 100m away.”
What differentiates Living Map from other similar asset tracking systems, and makes it increasingly appealing to the healthcare sector, is that no additional infrastructure is needed so it can be retrofitted to existing hospitals at a low cost.
Asman said: “Similar to how a shop till might work, or a printer or scanner, this technology uses existing systems already in place within hospitals.
“All hospitals have a WiFi network, or Bluetooth, and these scan around constantly. While in many hospitals the WiFi signal is shocking, there will be a tiny connection coming off these different systems and the senor can pick up on that.
“This gives you the X-Y co-ordinate, which is put across the transport mechanism and gives you a location.
“It doesn’t need any new infrastructure at all. We are looking to use and embrace what is already there.
“This means that, for hospitals, it can be easily retrofitted and that is really important as you are not closing a room so you can install lots of wires.
“To this day we have not built new infrastructure for any client. If it’s there, we will utilise it.”
The technology is an evolution of Living Map’s digital wayfinding solution which is helping hospitals across the UK to enhance the patient experience and cut the number of missed appointments and associated costs.
Asman said: “It’s basically providing satnav, but for indoor environments.
“If someone is coming to see an oncologist for an appointment, for example, they are incredibly stressed and once they get into the hospital it is a vast building where there might be multiple reception areas.
“There is always going to be some map on a wall somewhere or a volunteer trying to help.
“If your appointment letter tells you that you are seeing Mr Smith in Room 17 on the sixth floor, in wing six, you have to try and find your way there.
“When you get there, the room might have changed, or it is in a different part of the building.
It’s basically providing sat-nav, but for indoor environments

“The reality is that about 30% of appointments don’t get met and 70-80% are because people get lost in the buildings or can’t find where their appointment is.
“Our map management system allows facilities to create QR codes which visitors can scan from their appointment letter.
“When the QR code is scanned using a mobile device, users follow the loaded route on the hospital map to help them get to their appointment quickly.
“Some hospitals, like South Warwickshire Hospital, also have a big interactive kiosk on the wall which links to your phone and provides the same information.
“The patient is none the wiser that the room has changed, they are just sent to the relevant place.”
The system also marks out key areas such as toilets and cafes and can be programmed to find the quickest route or one which is stair free.
“Because of GDPR rules, we can help people to move around, but we cannot track them. However, we can do this for assets in hospitals and other complex environments with our asset visualisation technology.
“You can put a sensor on almost anything — even an individual pillow — so you know where everything is.
“In the future it could help hospitals further by recognising where empty beds are, thus helping to speed up admissions from A&E to the wards.” n
hospital operations more intelligent.
Locate critical equipment in real-time, to complete more tasks on time.
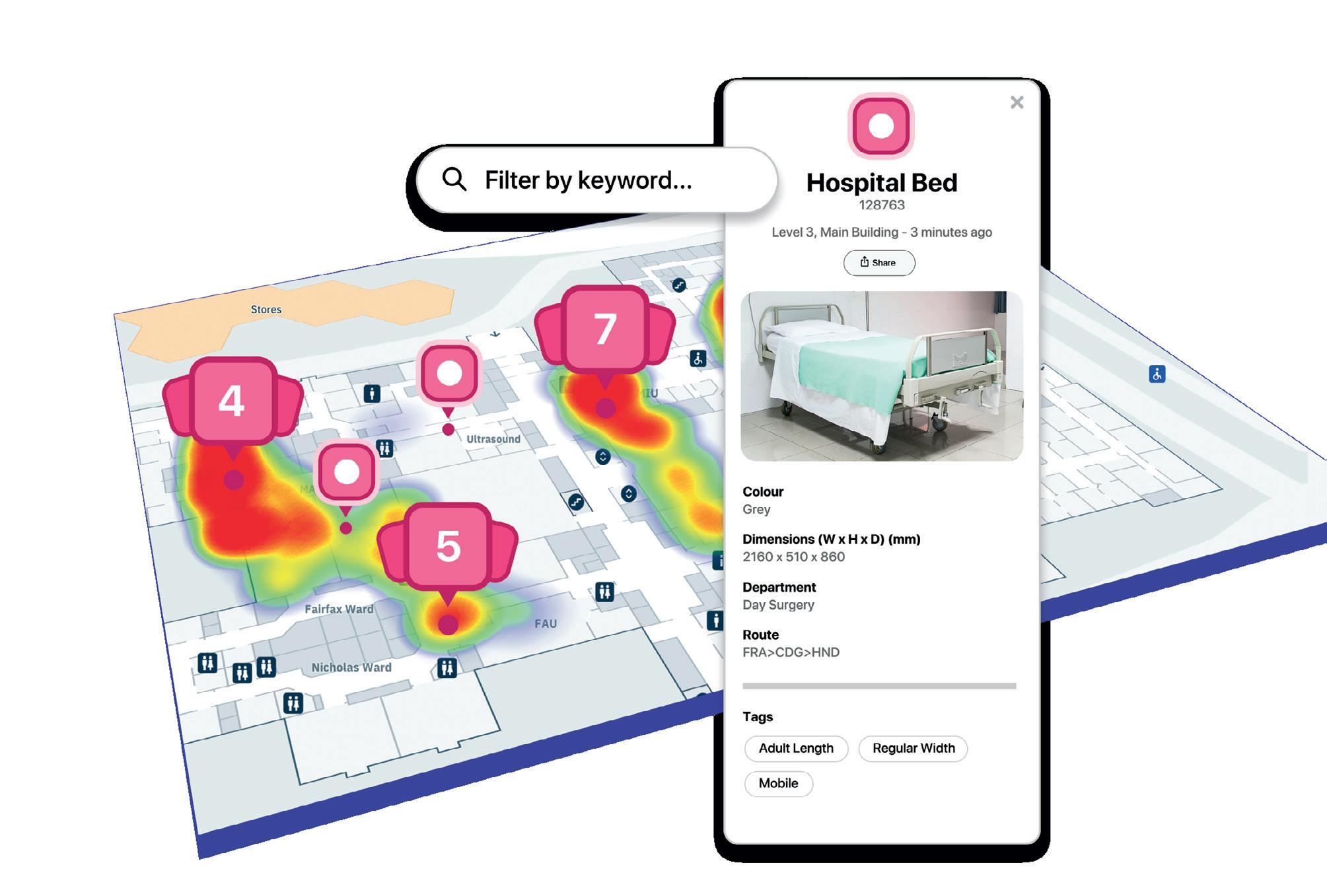






WDavid Llewellyn, chief executive of the Vending & Automated Retail Association (AVA), discusses how vending has evolved to enable healthcare facilities managers to offer access to healthy and tasty food and drinks all hours of the day
hen was the last time you used a vending machine? For many people visiting or staying in hospital — whether briefly or for an extended period — a vending machine often becomes the go-to solution for a quick snack.
And that’s not necessarily a bad thing.
Modern vending machines feature advanced technology and a wide range of food and drink options, catering to diverse diets and lifestyles.
And, in healthcare facilities, these machines are essential, not only for visitors and patients, but also for the healthcare estates and facilities managers responsible for their operation.
The combination of enhanced service quality, diverse product offerings, and
improved storage capabilities, enables vending machines to provide a wider selection of fresh food and drinks.
Modern technology has revolutionised hospital nutrition.
With advancements in vending machine technology, smart maintenance that streamlines the work of healthcare estate managers, and efficient waste management, on-the-go food options in hospitals have never been more appealing.
New technology has significantly advanced the capabilities of vending machines to align with evolving customer expectations for accessible food and drink options.
These upgrades have rendered the
machines safe, secure, and versatile.
And, as the shift from cash to contactless payments becomes more prevalent, machines now efficiently manage transactions with minimal manual intervention.
According to a recent AVA census, 85% of vending machines are now equipped with cashless payment systems, reflecting a decade-long trend.
This integration has also facilitated telemetry and data collection as standard practices, enabling better-informed decisions regarding stocking, service, and maintenance based on customer purchasing habits.
Telemetry and smart technology allow facility managers (FMs) to integrate vending machines into their predictive maintenance schedules for other estate components, such as HVAC systems or essential healthcare equipment.
As such, vending continues to play an influential role in healthcare estates nationwide.
The AVA census indicates a 4% increase in the machine base within healthcare settings since 2014, with such environments now constituting 8% of the entire UK machine base.
This growth underscores the rising impact of improved vending options and convenience for healthcare.
Vending operators provide a diverse array of nutritious options in response to increased consumer demand for healthier foods and adapting to new regulations such as the Sugar Tax and nutritional guidelines set by entities like the FSA in Northern Ireland.
The data recorded in our most-recent AVA census supports this notion:
• 81% of pre-packaged cold drinks now contain less than 5% added sugar per 100ml
• 78% of confectionery and sweets contain 250 calories, or fewer, per item
• 36% of savoury snacks are less than, or equal to, 30g, offering healthier portion sizes
These figures indicate that vending services are adapting to contemporary health trends.
For instance, 49% of consumers reported eating healthier foods this year, and 32% felt healthier than the previous year.
This focus on health-enhancing food is anticipated to continue growing, and vending is keeping up with the trend.
While traditional vending machines are now very advanced, a new trend is emerging in healthcare environments: the adoption of micro markets and Smart Markets.
These modern retail solutions, offering both attendant-operated and self-service options, blend the convenience of vending machines with the richer variety of a small store layout.
According to the AVA census, micro markets are proving increasingly appealing in several sectors, with a 37% year-onyear growth in the UK and 660 active installations nationwide.
Micro markets align perfectly with the round-the-clock operations of hospitals.
They provide a broader selection of products than traditional vending machines, including fresh food selections, which is crucial in healthcare settings where many people come throughout the day.
They serve these fresh items during staffed hours and more-traditional vending products during off-hours, adding invaluable flexibility for hospital staff and visitors who require 24/7 access to food and drinks.
On the technological front, micro markets use sophisticated point-of-sale (POS) systems compatible with various
For healthcare estate managers, micro markets bring reduced labour costs and offer real-time data on sales and inventory, facilitating waste reduction and ensuring the availability of popular products
payment methods, simplifying and speeding up transactions for users.
For healthcare estate managers, micro markets bring reduced labour costs and offer real-time data on sales and inventory, facilitating waste reduction and ensuring the availability of popular products.
This capability will likely drive further innovations in micro markets and vending machines, enabling the tracking of consumer behaviour to guide inventory choices and product pricing.
Facilities managers will be able to develop optimal stocking strategies that align with their occupancy data, ensuring occupants consistently have access to necessary products while minimising revenue loss and reducing food waste.
Vending machines have also reached new levels of efficiency due to advancements in vending management software.
This innovative technology, leveraging AI and automation, optimises stock levels, schedules refills, and plans efficient operator routes.
It ensures that operators visit machines only when necessary, enhancing operational efficiency, reducing unnecessary trips and overall waste and allowing healthcare estate managers to adapt offerings based on visitor and staff patterns.
Additionally, maintaining vending machines in well-stocked and fullyfunctional condition is crucial to customer satisfaction.
Connected machines make this much easier by sending notifications when supplies are low, or maintenance issues arise.
This allows vending operators and maintenance teams to respond quickly, ensuring machines stay operational and deliver great products to customers with ease.
Sustainability is a top priority for consumers, with many now seeking reusable cups and eco-
friendly waste management solutions.
This is something the vending industry has been actively collaborating with the UK Government and Defra on to address these demands.
As a result, Defra’s Extended Producer Responsibility (EPR) scheme aims to transfer the cost of packaging waste management from the taxpayer to the producers, encouraging reduced packaging use and a greater focus on recyclable materials.
Although concerns about potential cost increases have delayed its implementation, many see the benefits of such a scheme, which could foster closer collaboration between facilities managers and vending operators, enhancing waste management at healthcare and other facilities.
Another relevant method is the Deposit Return Scheme (DRS), which encourages recycling through a refundable deposit system on drink containers.
With billions of plastic bottles and cans consumed annually in the UK, DRS could significantly reduce waste, supported by ‘reverse vending machines’ that facilitate easy recycling at workplaces.
As the UK progresses towards carbon neutrality, adopting schemes like EPR and DRS will be crucial for FMs in the vending sector to help achieve sustainability and meet environmental goals.
In recent years, the vending industry has gone from strength to strength by adapting to contemporary work environments and aligning with health and lifestyle trends.
Healthcare estates managers are encouraged to embrace modern vending solutions that offer flexibility for patients and staff while ensuring a range of healthy and accessible snack options.
By investing in these new technologies, estates managers can enhance patient and staff wellbeing while maintaining the highest-quality offerings from their vending machines. n


An overview of the first-ever Healthcare Property Forum held in London
The challenges and opportunities within the medical real estate market were brought to the fore as Nexus Media Group, owner of Healthcare Property magazine, launched its first Healthcare Property Forum
Held in London, the event provided a day of quality content, discussion, and high-level networking for key players in the healthcare property sector.
It offered suppliers the chance to meet with investors and operators in a number of pre-arranged sessions, and a conference stream provided industry insight into key issues facing the market.
This included an overview of the property market for adult social care, primary and acute care, and the private health sector.
Commenting on the social care sector, Gary Reed, director of property at HC-One, told delegates that the company was embarking on the single biggest refurbishment programme in local authority care homes that the country has ever seen, with £93m being spent across its portfolio over a seven-year period.
This focus on refurbishment, he said, was common among providers struggling to meet the rising capital costs of new-build facilities and with a shortage of suitable developments sites in areas of need.
He said: “Typically our care homes are 30-40 years old and we are looking for opportunities to make the buildings flow better.
“And our biggest challenge is carrying out these improvements while our homes are occupied.”
As well as improving the layout of buildings and the interior design, the company is also focusing on enhancing the energy efficiency of its estate through the installation of solar PV panels, removal of gas tumble driers, and through



can create 650 bedrooms in our existing homes by reconfiguring things like storage spaces and day spaces which have not been used for years.
“That’s the equivalent of 10 care homes we have ready to open.”
Also speaking on the social care property sector at the forum was Mandip Bhogal, a partner in the healthcare property development consultancy at Knight Frank. He revealed some key statistics from within the sector, including that care home occupancy levels were up from 86% in 2023 to 89% in 2024, fee rates were increasing across the board, and staff costs were reducing, creating an improved market for the coming year.


And he revealed that 29% of current social care bed provision did not conform to market standards and that there would be an estimated shortfall in beds of 86,000 by 2028.
He agreed that refurbishment and the creation of extensions at existing homes was the focus of much activity.
ESG, he added, was also a key consideration.
“The subdued residential market is allowing care operators to be more competitive,” he said.
“There are strong funds out there with an appetite for more care developments.”
Speakers in the primary and acute care property session were Sarah Livingstone, executive director of healthcare at CBRE; Nicola Theron, director of estates in North Central London ICS; and Madeline Ball and Lisa Geary, property leads at DAC Beachcroft.
Geary said the primary care property model was shifting away from buildings owned by the GP partners to one where properties are purchased by developers and leased back to medical providers.
And all speakers expected private

capital to play a role in the improvements needed to improve the existing estate and create new buildings in both primary and acute care sectors.
The forum also explored the buoyant private medical market, which is being bolstered by the NHS’s waiting list crisis.
Speakers in the session were Nick West of Northwest Healthcare Properties REIT; Paul Fegan of Mansfield Advisors; and Jon Webb of Assura Plc.
They revealed that the NHS is entering a period of ‘hyper demand’, with a record 7.6m procedures on the waiting list. And it will need to rely on independent providers to reduce this and satisfy the growing
demand for elective procedures.
In particular, private providers are looking to build satellite units which can carry out elective procedures such as joint replacements and ophthalmology.
Fegan said: “The UK has one of the smallest private acute hospital sectors in Europe, but within the context of an overstretched NHS, it is a critical component part of the overall health system.
“NHS engagement with the private sector has its origins in the last Labour Government — and there’s every sign that engagement will continue.”
Webb revealed the private care property market was entering a period of ‘hyper demand’.

One of the more-heated debates of the day was around the current planning system, which is currently being reviewed by the new Labour government, amid plans to simplify the process.
This was an approach welcomed by speaker, Khosro Bashi of Tooley Foster Architects, who described the current system as ‘ridiculous’.
He said: “There is a huge list of documents you have to provide to make a planning application.
“There is the pre application, which is very detailed and often involves a lengthy wait; then the planning application; then conditions discharge and detailed design; and then amendments or reapplication.
“It is ridiculousness and madness to expect someone with no commitment from the council for the development to put something like that together.
“And then, if you need to make a change when you get to stage four, they will not send you back to stage three, but all the way back to the beginning.
“Some applications take years.”
He also hit out at the duplication in the current process, which sees planning authorities made responsible for issues already covered by Building Regulations or Natural England.
Instead, he proposed a watereddown planning process which involved submitting an ‘application in principle’ followed by a concept design and detailed design phase.
“The current process in dead and buried.
“My proposed system would be a step in the right direction if what the Government wants to do to simplify it,” he said.
But fellow speakers, Anna Gillings of Gillings Planning and Sally Stroman of Aitchison Raffety Group, disagreed that the current system was completely inefficient, despite some concerns over the number of applications refused by council committees against the recommendations of qualified



planning officers.
Gillings said: “Planning permission does get granted and schemes do get through, so it does work.
“Planners are just doing their job and they have a system to work through, so trying to give as much information as possible helps get the application through.”
Stroman added: “It’s about how can national planning policy better support local authorities and promote healthy communities.”
Other sessions during the forum looked at the role of heat pumps in achieving the NHS’s net-zero emissions target; the shift towards care villages as a one-stop shop for older-age living; and how the arts can help to create more-supportive healing environments.
Speakers included Louisa Williams from Art In Site, Jenny Buterchi from PRP Architects, Clare Connell from Connell Consulting, Nick Sanderson from Audley Care Villages, Gary Broadbent from Pure Thermal, Tim Rook from Clade Engineering, and Tim Steer from Hospital Rooms.
And Sarah Waller from the University

of Worcester’s Association for Dementia Studies; Fiona Walsh from DDS Architects; and Harry van de Bospoort and Naomi Roxby Wardle of Hospital Art Studio provided an insight into the importance of wayfinding in creating dementia-inclusive health and care environments.
Walsh said: “Spatial disorientation and declining wayfinding are among the first early symptoms of dementia.
“Every physical environment has a cognitive load and this must be decoded — and for someone with cognitive impairment this becomes a challenge.
“We need to design environments that limit cognitive overload through interventions such as lighting, colour, signage, and furniture.
“Everything needs to be visible to reduce decision making and we need to reduce cognitive overload in all stages of design."
Commenting on the event, Stroman said: “In addition to the insightful presentations, the event offered a fantastic opportunity to exhibit and participate in speed networking with the attending companies.
“This was a great opportunity for us to broaden our connections and showcase our integrated services.”
Following the success of the event, Nexus Media Group will be running three forums in 2025 on 6 March in Sutton Coldfield, 8 July in London, and 18 September in Newport.
For more information, or to book, go to www.nexusmedigroup.co.uk/events/ n



at a recent ceremony in London. Now in its 25th year, the annual competition is organised by Healthcare Property publisher, Nexus Media Group. Hosted by TV host and personality, Alex Jones, this year there were 30 trophies up for grabs.













Care Activities Co-ordinator/ Facilitator of the Year
SPONSORED BY TLC CARE


Winner: Emma Mayne, The Chestnuts (Mysa Care)
The Sara Berrio Care Champion Award
Winner: Kate Buckle (BM Care)
Care Chef of the Year
SPONSORED BY BIDFOOD
Winner: Katie Smith, Magna Care Centre (Aria Care)
Care Home Group (Small)
SPONSORED BY MOONRISE
Winner: Nightingale Hammerson
Care Home Group (Medium)
SPONSORED BY VIRGIN MONEY
Winner: Hallmark Luxury Care Homes
Care Home Group (Large)
SPONSORED BY ONTEX
Winner: Care UK
Care Home of the Year
SPONSORED BY ONTEX
Winner: Bartley Green Lodge (Sanctuary Care)



SPONSORED BY DOMUS RECRUITMENT
Winner: Amie Merret (Appletree Support)
Care Newcomer of the Year
SPONSORED BY NEUVEN
Winner: Norman McGlashan (Sanctuary Care)
Care Operations/Area Manager of the Year
Winner: Mirko Ridolfo (Majesticare)
Carer of the Year
Winner: Tilu Ngwira, Castlecroft Care Home (Sanctuary Care)
Care Registered Nurse of the Year
SPONSORED BY CARE UK
Winner: Michelle French, Cedars Place Care Home (Stow Healthcare Group)
Care Team of the Year
SPONSORED BY IMPACT FUTURES
Winner: Sabrina Community Team (HC-One)
Dementia Care
Manager of the Year
SPONSORED BY ARIA
Winner: Shona Bradbury, Appleby House (Care UK)

Deputy Manager of the Year
SPONSORED BY COUNTRYWIDE HEALTHCARE
Winner: Sabrina Brown, Autism Care (Lifeways Group)
The Dignity & Respect Care Home of the Year
Winner: Atfield House (Barchester Healthcare)
Care Housekeeper of the Year
SPONSORED BY P&G PROFESSIONAL
Winner: Edwina Coleman, Wisteria Lodge
Lifetime Achievement in Care
SPONSORED BY RADAR HEALTHCARE
Winner: Mike Parsons
Care Home
Manager of the Year
SPONSORED BY WE CARE GROUP
Winner: Daisy Slavkova, Loveday Kensington
Care Personality of the Year
SPONSORED BY WIGHTMAN & PARRISH
Winner: James Tugendhat
Domiciliary Carer of the Year
Winner: Lynne-Marie Worgan (Neighbourhood Care)
Domiciliary Care
Provider of the Year
Winner: BelleVie Care
Specialist Carer of the Year
Winner: Marion Hanna, Kinly Care Homes (Optima Care)
Specialist Care Provider of the Year
Winner: Jane Percy House (Brainkind)
Supplier of the Year — Services
Winner: Procurement For Care
Supplier of the Year — Staffing Winner: Florence
Supplier of the Year — Supplies Winner: Blueleaf Care
Supplier of the Year — Tech and Learning
Winner: FaultFixers
Tech Innovation of the Year
SPONSORED BY SANCTUARY CARE
Winner: PredicAire
Training & Development of the Year
SPONSORED BY CONNECT2CARE
Winner: Southern Healthcare (Wessex) Ltd


The winners of the 2024 HealthInvestor Power List 2024 have been announced. The name change this year from HealthInvestor Power 50 to HealthInvestor Power List reflects a commitment to inclusivity and broader recognition within the industry, showcasing a diverse and comprehensive range of leaders and innovators.
Organised by Nexus Media Group, parent company of Healthcare Property, this year’s competition includes new categories and has been independently judged by a panel of industry experts,
better acknowledging the dynamic and evolving landscape of the industry and celebrating excellence in a way that is both inclusive and representative of current health investment.




This year there were 14 trophies up for grabs, with the winners announced at a ceremony at The Marriott
London









Consultant
Hannah Farrar, CF (Carnall Farrar)
Corporate Financier
Anthony Ball, KPMG LLP
Debt Provider
Steve Fergus, Barclays
Equity Investor
SPONSORED BY ASHFORDS
Mark Gross, Downing



The winners are…
ESG & Impact
Jacob Hurtley, Elevation
Healthcare Innovator
Dr Ben Maruthappu, Cera
Property Investor/Developer
Andrea Auteri, Elevation Advisers
Property Consultant
Julian Evans, Knight Frank LLP

Legal Advisor
Sarah Skuse, Bevan Brittan
Private Healthcare Leader
Jim Easton, Practice Plus Group
Residential Care Leader
Dr Pete Calveley, Barchester Healthcare
Specialist and Complex Care Leader
Johann van Zyl, Care-Exec
One to Watch –Healthcare Executive
(e.g. upcoming CEOs, CFOs. COOs etc)
Hannah Morgan, CareBrain
One to Watch –Investors & Advisors
Jordan Rundle, Christie & Co
KPMG International has announced a new round of global sector head appointments as it strengthens support for clients across industry.
Three new appointments have been made across the organisation’s life sciences, industrial manufacturing, and asset management sectors to support client growth and drive forward innovation.


Anthony Harnden has been appointed as the new chairman of the Medicine and Healthcare products Regulatory Agency (MHRA).
Harnden is a Professor of Primary Care at the University of Oxford, and until the end of December 2024, a registrant council member of the General Medical Council and chairman
He worked for the NHS for 40 years and notably will bring 33 years experience of working directly with patients during his time as a GP in Wheatley, Oxfordshire.
Health Minister, Karin Smyth, said: “I am delighted to welcome Anthony, who brings a wealth of regulatory and healthcare experience, including 33 years as a GP.
“The MHRA plays a vital role in ensuring the safe use of medicines, medical devices, and blood transfusions across the UK and I look forward to working with Anthony as we reform our health service and make it fit for the future.”
Dr June Raine, MHRA chief executive, added: “We are delighted to welcome Professor Anthony Harnden as our new chairman.
Liz Claydon has been appointed global sector head of life sciences, alongside two roles she will continue to serve – head of global deal advisory and vice chair within KPMG in the UK.
Claydon has extensive experience in deal advisory, consumer, and life sciences, having supported some of the world’sleading brands and businesses.
She said: “I’m delighted and proud to lead our strong global life sciences business, working with our talented colleagues across the world to deliver value to our clients in this critical purpose-led sector.
“My immediate priorities are to focus on spending time with our global leaders across the sector; refresh our strategic ambition, and in doing so, refine our investments to achieve the growth opportunity ahead of us.”
The appointments also included Jonathon Gill as global sector head of industrial manufacturing; and Jim Suglia as global sector head of asset management.
Regina Mayor, global head of clients and markets at KPMG International, said: “As we reach an inflexion point in business where attention shifts from cost cutting to growth, business leaders across the globe are seeking pro-active, agile, and innovation solutions to support their future growth plans.
“Our three new global sector heads bring decades of industry experience and are equipped with the insight required to deliver a service offering aligned to these evolving client needs.
“With their direction and experience, I’m confident KPMG firms will help companies across all sectors return to long-term, sustainable growth.”
He was also previously deputy chairman of the Joint Committee on Vaccination and Immunisation (JCVI) and played a key role in ensuring public trust and patient safety during the distribution of the COVID vaccine.
He succeeds former MHRA chairman, Stephen Lightfoot, who served from September 2020 and stepped down in 2023.
In his new role he will play a key role in driving forward the strategic direction of MHRA to maintain the UK as a global centre of excellence in life sciences, in the best interests of patients and the public.
“Anthony brings with him a wealth of experience from across the healthcare sector and academia that will be invaluable when advising on the strategic direction of the agency to protect and promote public health.”
Harnden said of his new role: “It is a great honour and privilege to be appointed by ministers to be the next MHRA chairman.
“I am looking forward to making a contribution to the future successes of the organisation.
“I will use my experience in healthcare and regulation to help the MHRA deliver its strategic priorities — keeping patients safe and enabling timely access to new medicines and technologies.”

Alan Milburn has been appointed lead nonexecutive member to the board of the Department of Health and Social Care (DHSC).
Milburn is one of a number of experts that the Government is bringing in to help develop policy, alongside the survey it has launched to enable NHS staff and patients to share their experience and ideas for change.
Members of the department board provide independent advice and expertise to inform the department’s strategy, performance, and governance and the lead non-executive member provides additional support to the Secretary of State for Health and Social Care in his role as chair of the board.
As a former Secretary of State, Milburn brings experience at the highest levels of helping transform the health and care system.
Health and Social Care Secretary, Wes Streeting, said: “As Secretary of State, Alan made the reforms which helped deliver the
shortest waiting times and highest patient satisfaction in the history of the NHS.
“This Government has inherited a broken health service with some of the longest waiting times and lowest patient satisfaction in history.
“I am delighted to welcome Alan to the department board, where he will offer advice on turning the NHS around once again.
“His unique expertise and experience will be invaluable and he has an outstanding track record of delivering better care for patients.”
Milburn adds: “Having spent three decades working in health policy, I have never seen the NHS in a worse state. Big reforms will be needed to make it fit for the future.
“I am confident this Government has the right plans in place to transform the health service and the health of the nation and I’m looking forward to working with them to achieve that mission.”
Milburn was Labour MP for Darlington from 1992-2010 and was a health minister from 1997-1998. He became the Secretary of State for Health between 1999-2003.







