





The magazine of the Royal College of Paediatrics and Child Health INSIDE AUTUMN 2023 Supporting trans kids: a paediatrician and parent’s view Page 12 Using social prescribing for young people Page 20 Top tips for sub-specialty applications Page 18 How to bring more kindness to your work Page 28
PARTNERS IN PAEDIATRICS
Editor ’s pick 28
This Autumn edition of Milestones comes with its own milestone as we bid a fond farewell to the wonderful Aisling Beecher. Queen of cat-herders, funny, incredibly organised and patient; the whole editorial team cannot thank her enough for raising Milestones through the challenging early years. Everyone who has contributed since our first edition in Winter 2019 will have been boosted from the positivity that Aisling exudes. We wish you all the best for your next adventure – you will be missed!

As a parting gift, Aisling has teed up another bumper issue of membership matters that matter. There’s something for everyone; acing your GRID application, the one-of-a-kind Bob Klaber, our allied health partners in care, the fascinating insight into the world of a parent-paediatrician of a transgender child and so much more.
Please get in touch if you'd like to get involved – milestones@rcpch.ac.uk –we’d love to hear from you!
#RCPCHMilestones
Dr Seb Gray

General Paediatric Consultant
Salisbury NHS Foundation Trust
THIS ISSUE
12 A paediatrician and parent's view
Supporting a transgender child
14 Partners in paediatrics
Six advanced practitioners explain their roles

18 How to ace your subspecialty application
Top tips for success and how to start preparing early
19 The best paediatric diabetes team!
How Dr Anu Sharma's team helped her improve her own wellbeing
20 Social prescribing for children and young people

A new way of offering support
21 London's childhood asthma programme
All about the #AskAboutAsthma campaign
EVERY ISSUE
4 Update
The latest from the President, news, opportunities and more
11 RCPCH &Us
How RCPCH &Us is making a difference every day
22 Members
News and views from members
28 Wellbeing
Dr Bob Klaber reflects on kindness in the workplace
30 A day in the life
Dr Natasha Sauven on why she loves working with teenagers
KEEP IN TOUCH Milestones AUTUMN 2023 3 Contents Autumn 2023 Copyright of the Royal College of Paediatrics and Child Health. All rights reserved; no part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means – electronic, mechanical, photocopying, recording, or otherwise – without prior permission of the publishers. The views, opinions and policies expressed in Milestones do not necessarily reflect those of the College. While all reasonable efforts have been made to ensure the accuracy of the contents of this publication, no responsibility can be accepted for any error, inconsistency or omission. Products and services advertised in Milestones are also not recommended or endorsed by the College. Readers should exercise their own discretion and, where necessary, obtain appropriate independent advice about their suitability. Royal College of Paediatrics and Child Health is a registered charity in England and Wales (1057744) and in Scotland (SC038299). Registered address: 5-11 Theobalds Road, Holborn, London WC1X 8SH. Design Manager: Christina Richmond Senior Editor: Lizzie Hufton Publisher: James Houston. Milestones is published four times per year on behalf of the Royal College of Paediatrics and Child Health by James Pembroke Media, 90 Walcot Street, Bath, BA1 5BG. T: 01225 337777. Advertising: Alex Brown, Head of Corporate Partnerships advertising@rcpch.ac.uk @RCPCHTweets @RCPCH @RCPCH milestones@rcpch.ac.uk EDITORIAL Managing editor: Aisling Beecher @AislingBeecher Editorial board: Dr Seb Gray @SebJGray Dr Hannah Baynes @HLB27 Dr James Dearden @drjamesdearden Dr Dita Aswani @DrDita Dr Maddy Fogarty Hover @I_am_spottacus Contact We’d love to hear from you – get in touch at milestones@ rcpch.ac.uk
19 11
The Milestones team: (L-R) Seb Gray, Hannah Baynes, Dita Aswani, Maddy Fogarty Hover, Aisling Beecher and James Dearden
The latest news and views PRESIDENT’S UPDATE
WELCOME TO OUR AUTUMN EDITION OF MILESTONES!
I am so thrilled with how this members’ magazine is now embedded in the rhythm of the year, and I continue to be in awe of how our editorial team manages to find the creative energy for each edition such that each one brings fresh surprises and inspiration. As ever, I record my grateful thanks to the hours given to this endeavour by our members who so faithfully give their time and energies.
I hope you have all had a chance to take a break over the summer. Stepping away from the frontline and switching off the emails is crucial. None of us are indispensable and genuinely taking a break, disconnecting from social media, spending time with family and friends, reading a book, waking up without the alarm clock… these are all the ingredients I believe we need if we want
to give ourselves any chance of thriving, not just surviving. It is so easy to fall into the trap of ‘just keeping going’… but all batteries need recharging, and I so hope you managed some good quality downtime over the last few months.
Our conference was a few months ago. However, I am still feeling the warm glow of seeing so many of you in Glasgow and celebrating so much success – the prizes, the Honorary Fellowships, the PAFTAs. It’s great to be surrounded by colleagues who are being recognised for their amazing contributions to our specialty and to enjoy being together to learn, socialise and share ideas. Our 2024 conference is March 25 – 27 in Birmingham, with the call for abstracts now open. Keep an eye on the College website as our 2024 conference will not disappoint!

As the temperatures fall in the Northern Hemisphere, we all know that work gets busier. Let’s look out for each other – and ourselves, over the next months. With my very best wishes to you all,
Camilla
Awards 2023
JAMES SPENCE MEDAL
Professor David Edwards
HONORARY FELLOWS
Professor Viv Bennett
Professor Nick Bishop
Dr San San Oo
Dr Carol Roberts




Dr Arvind Shah
Professor Lisine Tuyisenge
MEMBERS’ AWARD
Professor Ian Sinha
Dr Elizabeth Whittaker
Team Soft Landing: Dr Nadia Baasher and Dr Habab Easa
We’d love to hear from you, get in touch through our channels
Twitter @RCPCHTweets

Facebook @RCPCH
Instagram @RCPCH
milestones@rcpch.ac.uk

THE TRAINEE RESEARCH SURVEY
Dr Eva Wooding Academic Clinical Fellow

 Royal Devon University Hospital
RCPCH Chair of the Trainee Research Network @paedsdr
Royal Devon University Hospital
RCPCH Chair of the Trainee Research Network @paedsdr
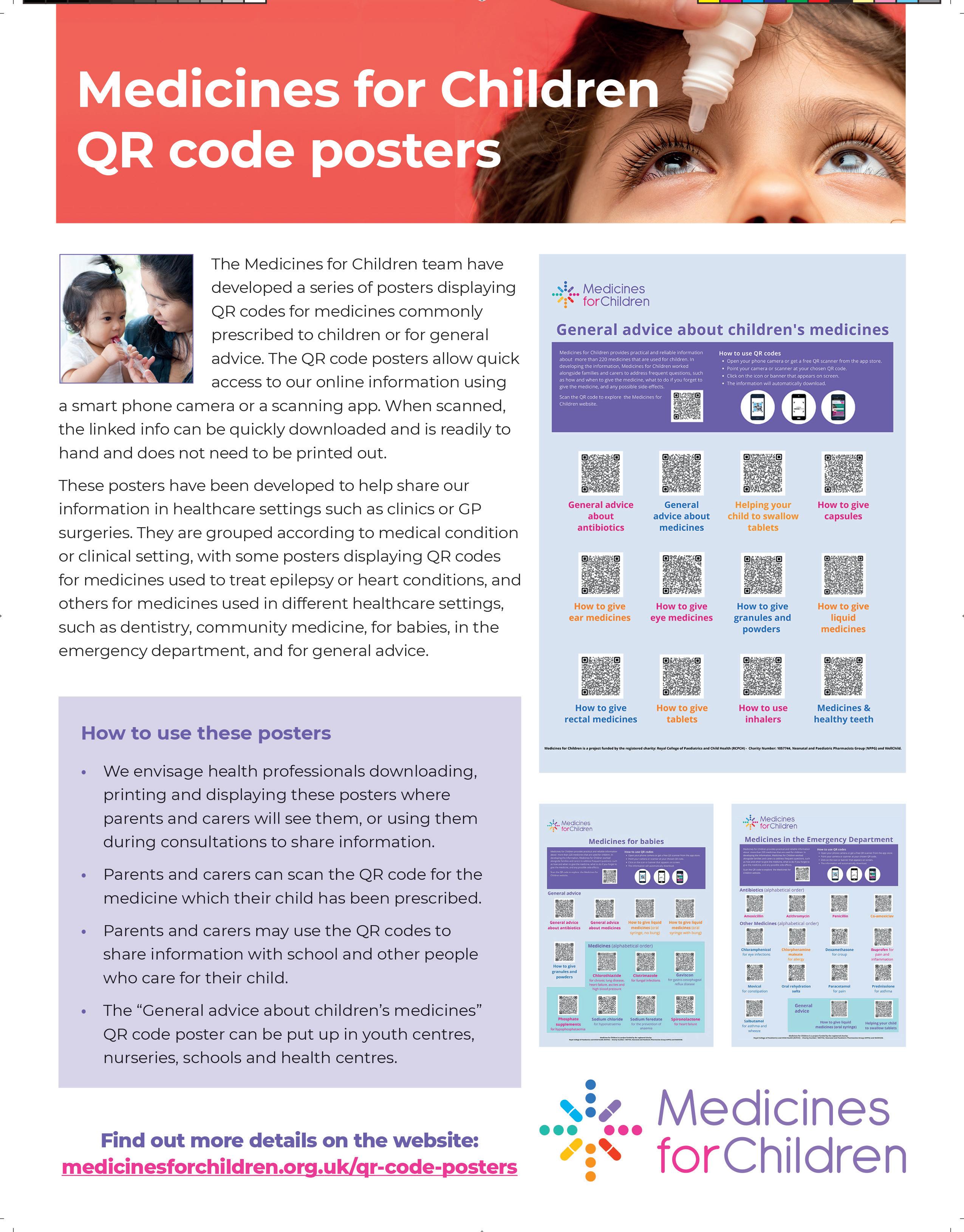
THE UK LAGS behind our European neighbours in child health research and outcomes, despite progress over the last 10 years since the College published ‘Turning the Tide’. Low funding for child health research and fewer academic paediatricians than two decades ago remain issues. In a hope to upskill trainees as the academic paediatric consultants of the future, the Trainee Research Network (TRN) was launched through the College in 2021 led by trainees. Shortly afterwards the College and TRN launched a survey which aimed to identify opportunities and barriers for trainees doing research.
588 trainees responded (16% response rate) of which 62% were UK graduates and 18% were international medical graduates. 9% were in an academic post with regional variation favouring larger centres. Many research active trainees were carrying out research activity in their own time; 7% committed >18hrs per month outside work.
Over half respondents agreed that research involvement enhanced their leadership, management, and academic skills. On our thematic analysis, a key motivator for researching was a desire to advance science and clinical care. Major barriers included priority for service provision, paucity of training, short rotations, lack of protected time and reluctance to extend training with out of programmes for research (OOPRs).
The survey identified a group of trainees who did not want to participate in research in training, likely to be underrepresented in our results due to non-response. Trainee viewpoints need incorporating into conversations about supporting trainee research in the Progress+ era.
Visit: www.rcpch.ac.uk/traineeresearch-network
04 AUTUMN 2023 Milestones KEEP IN TOUCH
Dr Camilla Kingdon RCPCH President @CamillaKingdon
Professor David Edwards being awarded the James Spence Medal at this year’s RCPCH Conference
The role of the BPSU in rare diseases
 Dr Peter Davis Consultant Paediatric Intensivist Bristol Royal Hospital for Children Chair of BPSU Committee @BPSUtweet
Dr Peter Davis Consultant Paediatric Intensivist Bristol Royal Hospital for Children Chair of BPSU Committee @BPSUtweet


IT’S BEEN A BUSY TIME at the British Paediatric Surveillance Unit (BPSU): we have had a symposium for World Rare Disease Day in February and a workshop at the RCPCH Conference in May.
The symposium had some excellent speakers, including a parent taking us through a feeling that there was something not quite right with her son, to the discovery that he had Barth syndrome, and how they had coped with this diagnosis with the help of the UK specialist Barth Team based in Bristol. Amongst others, we also had a presentation on the only specific SWAN (Syndrome Without A Name) clinic in the UK, set up in Cardiff, plus sessions on both the rapid exome sequencing for critically
ill children, and the Genomics Education Programme in England.
It was a pleasure to attend the RCPCH Conference and discuss the role of the BPSU in rare diseases. The idea of ‘rare diseases’ as a larger entity is a relatively recent one from the 1980s. The BPSU was set up around the same time, and it was salutary to review the effect that our work has had over the years in terms of public health legislation to reorganisations of services in the NHS for rare conditions.
We will have more webinars for completed BPSU studies to share their findings, plus we look forward to receiving applications for the Sir Peter Tizard Bursary to run a study through our surveillance system. Closing date for applications is 16 October. Finally, to any consultants reading this, please continue to complete your monthly online ‘Orange Card’.
Visit: www.rcpch.ac.uk/bpsu
A new starters’ guide to paediatric training
Felicity Beal
A GROUP OF enthusiastic paediatricians worked with the College on an exciting initiative to support newly recruited ST1s. We subsequently created Paediatric training at ST1 – here’s all you need to know!
Many of us can relate to that feeling of starting a new job, with feelings of excitement, uncertainty and questions about what the new job or training might entail.
We discussed our own experiences and questions we had prior to starting training, then arranged focus groups with current ST1 and ST2 paediatric trainees who were also extremely motivated in supporting the new ST1s. They highlighted three key themes that new paediatric trainees wanted to
Visit: www.rcpch.ac.uk/st1-guide
2023

1,143 IN-PERSON DELEGATES
543

VIRTUAL DELEGATES
39
NUMBER OF COUNTRIES DELEGATES TRAVELLED FROM
know about:
Your RCPCH ePortfolio: How to use ePortfolio, what should be logged and how to create a personal development plan. Neonatal exposure and skills: Explaining what a neonatal job would involve, dispelling myths and providing a jargon buster surrounding terms that are heard on the neonatal unit.
Wellbeing: Advice including how to seek support, who you can talk to and the role of debriefs in difficult cases.
This guide provides practical advice for on-the-job learning, ePortfolio tips and useful resources to use both professionally and personally to support paediatric doctors and their wellbeing. Most importantly this beginners’ guide welcomes our new generation of paediatric doctors, breaks down barriers to learning and aims to reassure and re-enforce the team spirit that lies at the heart of paediatrics!
377 SPEAKERS SHARED THEIR INSIGHTS AND RESEARCH
71 SESSIONS
345 POSTERS ONSITE
553 EPOSTERS
31
PRIZES WERE AWARDED AT PLENARY SESSIONS
UPDATE Milestones AUTUMN 2023 05 RCPCH FACTS RCPCH CONFERENCE
Dr
ST6 Paediatric Nephrology Birmingham Children’s Hospital RCPCH Recruitment and Lifelong Careers Board Member
RCPCH &US VOICE CHAMPION OF THE YEAR
IN
MY ROLE AS
TEAM
LEADER
The new Purple Book goes digital
Jill Conium Clinical Nurse Specialist - Children’s Epilepsy East and North Hertfordshire NHS Trust




for the children’s epilepsy nursing team, I ensure the epilepsy service provides an effective, wellcoordinated and responsive level of care for all CYP and their families. My colleagues and I manage a caseload of more than 550 young people. I am also the specialist nurse working with the Epilepsy 12 Youth Advocates with RCPCH &Us. This group of epilepsyexperienced or interested young people volunteer to improve care for epilepsy patients and their families.
This role has taught me that driving quality improvement with CYP at the heart of change is fundamental. This group of young people want to learn and work with professionals to express their views and become part of offering their ideas whilst shaping change in child health services of the future. They demonstrate how engagement can be a tool to ensure paediatric services reflect their needs and ultimately improves child health outcomes.
Winning the RCPCH &Us Voice Champion Award 2023 was a total surprise, and an honour both for me as a specialist nurse but also for the young people who are so passionate about wanting to shape change. I am blessed to have opportunities to be involved in a variety of different meetings and events all over the country involving individuals from various backgrounds. It enables me to listen, hear and share ideas, whilst promoting the work of each group. I will continue to work with our advocates on the projects they have identified to improve epilepsy care for our patients in the future and to amplify the CYP voice in healthcare. If I had four words to explain what is important to me it’s educate, collaborate, engage and change!
Dr Emilia Wawrzkowicz Consultant Paediatrician North
THE RECENT PUBLICATION of the Independent Inquiry into Child Sexual Abuse, coupled with high profile child abuse cases reported in the media, mean child sexual abuse is firmly in the public’s consciousness. The challenges that this field of work presents make it vital to give professionals the appropriate resources to help them to protect CYP and their families. The Physical Signs of Child Sexual Abuse (aka The Purple Book) was first published by RCPCH in 2008. This field has evolved significantly since then and the guidance needs to reflect current
NHS Foundation Trust
research and evidence. I am therefore delighted to announce the publication of the third edition of this key resource to support clinical decision making. A huge evidence review has been led by the Child Protection Subcommittee CSA co-leads, Jo Gifford and Michelle Cutland, supported by experts in the field and our trainees. The new edition builds on the evidence base established in the 2015 second edition. Collaborative contributions from experts in America, Australia and Asia have provided valued international endorsement. This latest version will be available in a digital format through the RCPCH portal and available to all members, with specialist access only to images for Named and Designated Safeguarding Doctors.
Visit: childprotection.rcpch. ac.uk

Paediatric Mental Health Champion roll out

 Dr Karen Street Consultant Paediatrician Devon Partnership Trust Chair Eating Disorder Workstream MHLDN Provider Collaborative RCPCH Officer for Mental Health
Dr Karen Street Consultant Paediatrician Devon Partnership Trust Chair Eating Disorder Workstream MHLDN Provider Collaborative RCPCH Officer for Mental Health
RCPCH HAS LONG ADVOCATED for a paediatric mental health lead to be embedded in paediatric departments, alongside the aspirations and commitments of the NHSE Framework: Supporting Children and Young People with mental health needs in acute paediatric settings. NHS England now provides funding for a Mental Health Champion in every provider that admits children. This is for 1PA of senior clinician time.
Key functions of the role are to:
Build confidence and knowledge of the wider paediatric team and department
Encourage uptake of training
Facilitate joint working, promoting parity of esteem for mental health, establishing closer links with mental health teams, and developing appropriate pathways
Provide leadership and advocate for children and young people’s mental health within paediatric departments and wider ICB structures.
See the RCPCH website for more details including on how these roles might develop, the support available from RCPCH, and bringing the Champions together to create a national network. The money has gone to regional systems so please approach them for distribution in your area. We hope for a similar commitment in the devolved nations.
UPDATE 06 AUTUMN 2023 Milestones
West Anglia
LISTENING TO OUR COLLECTIVE EXPERIENCES
Dr Jess Morgan Dinwoodie Clinical Fellow RCPCH

WE’RE IN HANDOVER. Once again, that sinking feeling that we don’t have enough doctors, a workload that feels insurmountable. We race through the patient list, aware of the time pressures and the need to get on with it. A long ward round, frustrated families, relentless admissions, food grabbed on the run, no time for teaching...
There is no denying the unbelievable pressure that paediatricians are under right now and the ramifications that this has on wellbeing and retention. With rising rates of burnout and increasing numbers of doctors leaving the NHS, if there was ever a time to address this, it’s now. Our working lives cannot just be about survival. We need to be supported to thrive in our careers as paediatricians, to feel a sense of purpose and fulfilment. This is why Thrive Paediatrics exists, because WE MATTER, and our working lives and wellbeing are fundamental
to the delivery of high-quality care for children and young people.
Extensive research by Professor Michael West outlines three core needs that we have as health professionals. These are featured in the figure below.
Every day however, we experience the multi-layered, interconnected challenges that make it difficult for these needs to be met, be it workload, rotas, job plans, difficulties accessing professional development, career advice and management opportunities. We know the impact of culture, leadership and communication on

wellbeing… Thrive Paediatrics is about listening to our collective experiences, learning from each other and engaging individuals, leaders and organisations to activate change. Every positive action we take, no matter how big or small, has the potential to improve someone’s working day.
Over the next few months, we will be running events, engaging communities and inviting individuals and organisations to collaborate with us. Please look out for upcoming information and find our contact details at www.rcpch.ac.uk/thrive
(source: The King’s Fund)
Staff Spotlight
I JOINED THE COLLEGE in November 2021 as a divisional coordinator for the Membership, Policy & External Affairs and Research & Quality Improvement divisions. My role is extremely varied as I support three directors in delivering their divisional strategy, as well as supporting the work and functioning of the wider divisions. I feel very lucky that my role allows me to work with so many amazing and passionate people across the College.
A lot of my time is focused on providing committee support and coordinating the completion of various reporting structures including the monthly CEO report. Servicing committees allows me the privilege of
working with such hard working, dedicated paediatricians.
In addition to my job, I volunteer as a communications officer for our Women’s Network, managing internal communication and engagement channels to promote its work. I also work as a core member of RCPCH’s Green Team, on our project to achieve net zero by 2040. We are currently organising the next RCPCH Green Week, which will commence in September this year!
I have a very active social life and spend a lot of time exploring different pubs and restaurants in East London. To stay active, I enjoy swimming and playing football with my local team Goals Aloud.

UPDATE Milestones AUTUMN 2023 07
Poppy Downes Divisional Coordinator
New standards for GMC CESR applicants
Dr Neha Sharma Consultant Neonatologist University Hospitals Plymouth NHS Trust RCPCH CESR Assessor @DrNehaSharma16

PROGRESS+ WILL EMPHASISE quality work experience in a more trainee-friendly programme for paediatric trainees, which means good news for Certificate of Eligibility for Specialist Registration (CESR) aspirants too!
CESR is for doctors who wish to join the GMC Specialist Register, whose specialist training, qualifications or experience are partly or completely acquired outside of an approved CCT (Certificate of Completion of Training) programme.
The GMC is collaborating with RCPCH to change the framework for CESR assessments to support doctors seeking entry to the Specialist Register.
With the changing model, CESR candidates will no longer have to show they have fulfilled the full detail of the CCT curriculum. This means that the paediatrics curriculum will not be too complex for CESR candidates to meet. The new standards will change from ‘equivalence to the curriculum’ to ‘knowledge, skills and experience’ (KSE) for consultant practice in the UK. The framework for assessing KSE will reflect the high-level learning outcomes (HLLOs) in paediatrics to provide a more tailored, inclusive approach to all CESR candidates.
The GMC plans to change the legislation by October 2023 and to apply the standards of KSE for future applications. The GMC has a page on its website explaining the changes and will offer further guidance on social media to help candidates understand the upcoming changes.
The RCPCH CESR Committee is drafting the new HLLOs, assessing issues of suitability of evidence, incorporation of accessibility, timelines of evidence, impact on patient safety, and so on. There is an emphasis on making CESR assessment more open and flexible while ensuring that applicants have the right knowledge, skills and experience.
This is a huge task, so we encourage paediatric consultants or recently passed CESR candidates to join the GMC and RCPCH CESR team to help improve this framework. If you’re interested, check the GMC and the RCPCH volunteering webpages for assessor roles on the CESR Committee.
Visit: www.rcpch.ac.uk/cesr
JOURNAL: ADC UPDATE
THERE’S A LOT of information in the ‘Editor in Chief’ brochure, but one area that’s not routinely mentioned is the sociological angle. Why mention this now, you (rightly) ask! What brought it to mind are the changes, the patterns of research, writing, torque and potential influence of work submitted around the pandemic.
Editor-in-Chief
Stage 1: The deluge. The steady flow from the pre-2019 days became a monsoon early in 2020. It reflected efforts to ‘learn’ this new illness (previously unreported symptoms fast-track published) and the extra time now largely out-of-hours housebound paediatricians had to revisit old work. Simultaneously, funding ran dry, RCTs failed to launch or were halted mid flow, deemed untenable in the face of restrictions.
Stage 2: The plateau. A year of less frenzied work, but nonetheless an active period. Objectively, little new on the corona front, though that didn’t deter some heated policy debate.
Stage 3: The global slump. Normal clinical work resumed; all old data had been addressed and the readjustment so draining that, for many, new research was near unthinkable. Submission rates went down dramatically, gems became conspicuous by their rarity.
Stage 4: Renaissance. We’re now firmly into recovery territory, trials back in full swing, hypothesis generation and hunger to probe back to 10, maybe even 11.
Check out the journal. It’s been wavy, but we haven’t been treading water.
JOURNAL: BMJ PAEDIATRICS OPEN UPDATE
Imti Choonara

 Editor-inChief
Editor-inChief
VIOLENCE TOWARDS CHILDREN unfortunately is a global problem. This can be physical, psychological or sexual. All children are at risk of violence, but disadvantaged children are at greatest risk. Research on violence against children is crucial, but clearly randomised trials are not possible. Observational studies and retrospective analysis of databases and hospital attendances are some of the methods used.
BMJ Paediatrics Open considers all types of studies, but all papers undergo full peer review, to ensure only robust data are published. Education of the public and health professionals is important. In many countries, violence towards children is tolerated and condoned by the public, health professionals and even children themselves (England, unlike Wales and Scotland, allows violence towards children). BMJ Paediatrics Open is publishing several articles highlighting the prevalence of physical and sexual violence towards children. It is hoped that the articles will highlight the need for changes in society’s attitudes towards children.
UPDATE 08 AUTUMN 2023 Milestones
Nick Brown Archives of Disease in Childhood
@ADC_BMJ
BMJ Paediatrics Open
@BMJ_PO
CONSULTANT JOB PLANNING TOOLKIT
CONSULTANT JOB PLANNING
Dr Kay Tyerman Consultant Paediatric Nephrologist Leeds Children’s Hospital


RCPCH
Officer for Workforce Planning
@kay_tyerman
, as we know it, was formalised as part of the consultant’s contract in 2003. The aim being to describe the quantum of clinical care delivered by a consultant alongside scheduled time for supporting professional activities that allow for continued professional development throughout their career.
Job planning should not feel like a ‘paper exercise’ – complicated sums that simply make work done ‘fit’ into an allocated number of professional activities (PAs). When done well, a consultant’s appraisal objectives and team discussions should feed into an individualised job plan accurately reflecting the time required to deliver direct clinical care and supporting professional activities (SPA). SPA
should include allocated time for quality improvement/audit, research, training as well as time to develop expertise in leadership and/or education. The process should also consider a consultant’s seniority and value the expertise that they bring to local, regional and national roles including voluntary activities.
When it comes to job planning, however, local guidance varies, particularly in relation to time allocated for SPA including research and recognition of time to deliver teaching and supervision. We recognise that this variation may impact on our ability, as a profession, to meet the targets set out in Facing the Future –standards for paediatric care.
The RCPCH Consultant Job Planning Toolkit has been developed to provide clear guidance and support for paediatricians in their local job planning discussions.
Whether we are working in acute general paediatrics, a subspecialty in the hospital or community setting and/or have a designated
role, we all need time in our job plans to deliver a high standard of care that improves outcomes and with adequate time allocated for all forms of SPA.

With the new Progress+ curriculum and shortened training time, it is more vital than ever that delivery of training, including time for both educational and clinical supervision, is factored into our daily working lives.
Many of us will be working well beyond reaching our sixth decade and job planning needs to account for this, particularly in the delivery of out-of-hours work. This guidance can be used in conjunction with the RCPCH Thrive Paediatrics Roadmap for Transforming Working Lives of Paediatricians.
We would encourage you to see job planning as an opportunity to both improve your ability to deliver care to our children and young people and to ensure you thrive throughout your consultant career.
Visit: www.rcpch.ac.uk/consultant-job-planning
GMC matters and RCPCH
 Professor Steve Turner Consultant Paediatrician
Professor Steve Turner Consultant Paediatrician
 Royal Aberdeen Children’s Hospital
Royal Aberdeen Children’s Hospital
THE GMC IS THE REGULATOR for over 350,000 doctors. Its role, set out in the Medical Act 1983, is to “protect patients and improve medical education and practice across the UK”.
Practitioners Tribunal Service (MPTS), less than 3% of all referred cases. The MPTS can make recommendations which include warning, suspension and erasure from the GMC register. Around 150 doctors are erased from the register annually, very few due to clinical issues.
RCPCH
Registrar
@SteveTurnerABDN
Each year approximately 9,000 doctors are referred to the GMC. Of these cases, more than 80% are closed without action. There is a provisional enquiry in many remaining cases, and about 80% of these are closed. Approximately 300 cases are investigated by the Medical
The MPTS is meant to be independent from the GMC. But currently the GMC can appeal a decision made by the MPTS. The GMC has challenged 24 MPTS decisions in the last five years.
Our 2018 AGM approved the motion ‘This College considers the criminal prosecution of dedicated doctors for gross negligence manslaughter, following systemic errors, impairs the advancement of safe healthcare for patients.’ A 2018 review of GMC processes, after it challenged the MPTS
decision for our member, Dr BawaGarba leading to her prosecution, recommended the GMC should no longer be able to appeal MPTS decisions, and the Government agreed to bring forward legislation to make the change. RCPCH and other organisations are concerned that this commitment has not been carried out, so we have written a joint letter to the Government urging them to change the law.
The GMC is there to protect patients. But it is also present to protect doctors by saying what we should do when caring for our patients (Good Clinical Practice). Please can I ask members to consider becoming expert witnesses to help paediatricians being investigated by the MPTS.
UPDATE Milestones AUTUMN 2023 09
Team spirit
Dr Anu Sharma describes how a team event helped her improve her own wellbeing

Diary Dates
Listed below are some of the up and coming courses and events, which are online unless otherwise stated. We will add to this list over the coming months, so keep an eye on our website.
Read more Find more dates at www.rcpch.ac.uk/ courses www.rcpch.ac.uk/ events
PODCASTS
Wellbeing as paediatricians –creating environments where we can thrive at work
Conversations with policy makers – with Dame Andrea Leadsom MP
How to build a paediatrician Stories of impact – on healthcare, outcomes and the quality of life for children and young people with diabetes Child health inequalities –interviews with two quality improvement projects
See the College’s podcasts www.rcpch.ac.uk/podcasts
UPDATE 10 AUTUMN 2023 Milestones
p19
Statement & report writing – England/ Wales (Level 3)
Paediatric
Effective
Supervision
Sustainable
Epilepsy12
Conference (London
Common Dermatological Problems
Paediatric Services (London)
Child Protection Study Day
Effective Educational Supervision
Paediatric
Training
10
Statement
Ireland
10
15-16
Effective
Supervision
FASD in
Paediatric Services
Statement
writing - England/ Wales
Effective Educational Supervision
Statement
Paediatric
Training
to RCPCH
you
7 September How to Manage:
Sickle Cell 13 September
Educational
21 September
Child Health 21 September
and OPEN UK National
and online) 27 September How to Manage:
2 October How to Manage: FASD in Community
5 October
– Scotland 5 October
3 November How to Manage:
Allergy
(PAT 1)
November
& report writing – Northern
(Level 3)
November Expert witness in child protection (Level 3+, 4 and 5)
November
Educational
6 December How to Manage:
Community
11 January
and report
(Level 3) 17 January
13 February
and report writing - England/ Wales (Level 3 6 March How to Manage:
Allergy
(PAT 2) 21 March See more Listen
Podcasts wherever
get your podcasts
Making a difference
RCPCH &Us member Shreya shares her experiences of contributing to our understanding of living with long-term health conditions
IWAS DIAGNOSED WITH ASTHMA AT A VERY YOUNG age so I never knew what a life without asthma was like. At the age of seven, I noticed that nearly all of the leaflets were aimed at carers or people over 16. I wanted a leaflet for me, that was catered to me in words that I could understand. I often wondered how much could be improved if children and young people could share their experiences and change things. I then realised that this existed as RCPCH &Us.
For the last three and a half years, I‘ve been a podcaster, an Asthma Ambassador, an interviewer, a leaflet designer, a plenary speaker, a member of an amazing team and most importantly, a child voice.
Being a part of RCPCH &Us is more than making a difference, it’s learning about yourself and others. I have gained so much understanding about healthcare, our healthcare professionals’ skill, and other conditions. All children and young people should have the opportunity to make a difference to something that matters to them and become remarkable young people willing to make a change and able to take
care of their health conditions.
For most young people, health conditions have defined our entire lives. We were the kids with flags by our names in the register, who teachers kept their eyes on during class, the ones who couldn’t run on sports day, but we are more than patients, we are young people. We should be able to grow up to be empowered adults

RCPCH &Us: The Children and Young People’s Engagement Team delivers projects and programmes across the UK to support patients, siblings, families and under 25s, and gives them a voice in shaping services, health policy and practice. RCPCH &Us is a network of young voices who work with the College, providing information and advice on children’s rights and engagement.

@RCPCH_and_Us
@rcpch_and_us

who are capable of achieving their dreams while successfully managing their conditions. We should be able to live with a health condition rather than a health condition be our life.
I earlier mentioned that RCPCH &Us is more than making a difference. It is making a difference – and you see it every time you walk into a hospital.
@RCPCHandUs and_us@rcpch.ac.uk
KEEP IN TOUCH RCPCH &US
ABOUT Milestones AUTUMN 2023 11
Shreya, age 14 RCPCH &Us volunteer
RCPCH &Us helps children to live life to the full
My thoughts as a paediatrician and parent of a transgender child
Paediatricians play a key role in supporting children and young people who are transgender or gender non-conforming. A College member tells their story as both a parent and a paediatrician

When my kid was six years old they said to me, “How do people know if they are a boy or a girl? Because I think I’m a boy.” When we met a transgender person in a shop and I explained about respecting people’s chosen name and pronouns, they happily exclaimed, “That’s like me, I’m a girl on the outside and a boy on the inside.”
We had been attempting to raise our children in a feminist, gender-neutral way. Brightly coloured clothes. Tea sets and train sets. Books about strong willed girls breaking down the patriarchy. My kid loved playing with soft toys, putting them to bed and tucking them in. They had fierce concentration in karate class. They liked to play ninjas with their brother. They had a group of little girl friends. At the same time, they had long expressed a feeling of being different to other people, feeling like their little girl friends didn’t really like them, expressing feelings of sadness that seemed out of proportion to their generally joyful and resilient manner. Could what they were saying relate to misogyny, feeling that girls weren’t allowed to do certain things? Was it a way of expressing feelings of being different? Or were they telling us that they were transgender?
Despite nearly ten years of paediatric training, I really knew nothing about what it meant to be transgender and certainly nothing of any use to decide how to respond to my child. I remembered one lecture that noted a high level of mental health difficulties and suicidal ideation among transgender teens. I was filled with fear at what the future might hold, and also confusion as to whether at this age I should push back against the assertion that they were really a boy, exploring more about how being a girl doesn’t have to limit you, that you can be a girl with typically masculine interests and appearance, that you can be a girl and want to marry a girl in the future.
Things came to a head when I asked my child if they wanted to have a haircut.
Their eyes shone as they looked up and said excitedly, “Can I have it cut like X [their brother]? And when I have my haircut, can you call me he?” The hair was cut but we didn’t immediately change pronouns. We went into overdrive trying to educate ourselves – joining social media groups for parents of gender non-conforming kids, lots of reading and listening (healthtalk.org has an excellent in-depth set of interviews with trans young people, and parents), buying books for my kid like Red: a crayon’s story by Michael Hall, It feels good to be yourself by Theresa Thorn and Jamie is Jamie by Afsaneh Moradian, finding affirmative cartoon series featuring characters with a range of different LGBTQ identities (The Owl House, Dead End). We wanted to show our child that they are not the first to challenge
FEATURE
12 AUTUMN 2023 Milestones
Anonymous A paediatrician and parent
“We had been attempting to raise our child in a gender-neutral way”
society’s expectations of gender expression, and to give them some more language to explore their feelings, without immediately assuming that they were indeed transgender. Switching pronouns seemed like an enormous deal and how could we be sure, and were they really sure?
Gradually over the next few months we saw the gender euphoria that my child experienced taking steps into ‘masculinity’ – wearing boxer shorts for example. Their language became clearer in expressing their gender identity and dysphoria. We realised that trying out different pronouns didn’t have to be a big deal, and that it could help people to understand what felt right for them. I realised that even if I hadn’t told my child they were wrong about themselves, by ignoring their request to change pronouns I was sending the message that this wasn’t what I wanted, that this would be the wrong choice in my eyes. It was also clear to me that many trans people were aware of their gender identity from a very young age.
So we made the switch to he/him pronouns. He cycled through a few names before settling on one that we all liked. It was interesting how quickly we got used to things, how quickly our brains re-wired and how strange his birth name started to seem when others used it unknowingly or by mistake. All of our close family were supportive, even those who found the idea odd. The few who didn’t approve kept their reactions away from our child. His classmates were slightly confused for about a day and then almost just got on with it. When
one kid teased him, his friends defended him in outrage. Teachers and family members say they feel he is more joyful, more liberated. It’s been nine months and he remains totally sure that he is not a girl.
My overall realisation was that my child was learning that his little version of society trusted him, respected how he saw himself, loved him for who he is rather than who they thought he was. And regardless of where his gender journey ends up, what an incredible and joyful thing that is to learn when you’re seven years old. His social transition has not been a panacea – he still expresses low self-esteem. But he’s also extremely proud of being trans (a label that we were careful not to apply to him but which he chose to apply to himself). Where so many trans people’s childhoods have been steeped in fear of rejection, shame and internal conflict, my child has experienced affirmation, love and pride. There isn’t room here to talk about the evidence base around social transition (changing name, pronouns, appearance in line with your gender identity), or how gender identity evolves for gender non-conforming kids. Have a look at the suggested reading list for some papers looking at the positive mental health outcomes associated with affirmation and social transition, and identity trajectories.
As paediatricians we will all be seeing a lot more trans kids in the future. Recent census data showed that 1% of people aged 16 to 24 years identify as transgender. The Cass Review encourages paediatricians to take on emerging roles as coordinators of care within regional paediatric transgender services, and paediatric endocrinologists will in particular have a key role in management of puberty blockers and affirmative hormones for those who may need them. But you are also going to see kids like mine coming with totally unrelated medical problems –gastroenteritis, diabetes, asthma. We need to move beyond the sometimes vitriolic public discourse and really listen to trans kids and those who love them. I hope this article has inspired you to be a better doctor to kids like mine.
Useful resources:
Non-academic
This child of ours by Sadie Pearce
All the things they said we couldn’t have by Tash Oakes-Monger HealthTalk series of interviews: healthtalk.org/Experiences-of-transand-gender-diverse-young-people RCPCH principle statement supporting LGBTQ+ CYP: www. rcpch.ac.uk/supporting-lgbtq-cyp
Academic:
1. de Castro et al. 2022. High persistence in Spanish transgender minors: 18 years of experience of the Gender Identity Unit of Catalonia. Revista de Psiquiatría y Salud Mental. https://doi.org/10.1016/J. RPSM.2022.02.001

2. Durwood et al. 2017. Mental Health and Self-Worth in Socially Transitioned Transgender Youth. Journal of the American Academy of Child & Adolescent Psychiatry, 56(2), 116-123.e2.
doi.org/10.1016/j.jaac.2016.10.016
3. Horton. 2022. “Euphoria”: Trans children and experiences of prepubertal social transition. Family Relations. doi.org/10.1111/fare.12764
4. Olson et al. 2022. Gender Identity 5 Years After Social Transition. Pediatrics, 150(2). doi.org/10.1542/ PEDS.2021-056082
5. Russell et al. 2018. Chosen Name Use Is Linked to Reduced Depressive Symptoms, Suicidal Ideation, and Suicidal Behavior Among Transgender Youth. Journal of Adolescent Health, 63(4), 503–505. doi.org/10.1016/j. jadohealth.2018.02.003
6. Tollit et al. 2021. The clinical profile of patients attending a large, Australian pediatric gender service: a 10-year review. International Journal of Transgender Health doi.org/10.1080/26895269.2021.1939 221/SUPPL_FILE/WIJT_A_1939221_ SM0274.DOCX
FEATURE Milestones AUTUMN 2023 13
PARTNERS IN PAEDIATRICS
We are lucky in paediatrics to work as part of a diverse team with a wide skill base. Advanced practitioners provide continuity in their departments, and with their hybrid training and experience have a unique perspective into the needs of their colleagues and patients. Milestones is proud in this edition to showcase some of these fantastic advanced practitioners. We hope you enjoy their stories!

FEATURE 14 AUTUMN 2023
Milestones
Elizabeth Young Physician Associate Torbay and South Devon NHS Foundation Trust
PHYSICIAN ASSOCIATE
I HAVE BEEN A QUALIFIED PHYSICIAN ASSOCIATE (PA) for over four years and have worked in the paediatric team of a DGH for the majority of that time. I sit within the Tier 1 on-call rota and feel that out-of-hours work has provided me with invaluable exposure to the core aspects of what paediatric care entails and this has helped advance my skills and knowledge. I am able to carry out the basic skills required – venepuncture, cannulation
and lumbar puncture of neonates and paediatric patients – and attend deliveries independently after gaining NLS and APLS qualifications. Whilst it is frustrating that I am unable to prescribe, the whole team is very understanding and accommodating and we all hope that this will become an option in the future.
Additionally, I contribute to the induction process of our rotating Tier 1 doctors; teaching the skills and knowledge that help them during their time with us, as well as providing them with an understanding of their day-to-day responsibilities and expectations. I am there to support them through their rotation and help build their confidence in paediatrics.
I (alongside all PAs) am looking forward
to the long-awaited completion of the regulation process and eager to learn how that will change the future of PA development. Whilst I am not certain how my exact role will develop over the years, there is no doubt that paediatrics provides endless opportunities for personal and professional growth to support the team and our patients.
Donna Wilkinson PICU Advanced Clinical Practitioner Leeds Children’s Hospital



PICU ADVANCED CLINICAL PRACTITIONER
I QUALIFIED IN 2001 as a children’s nurse from Leeds University and I have pretty much worked on the unit since. I was a Band 6 Sister on PICU for six years before I decided to make the leap into advanced practice.
Whilst there are many career paths for nurses to choose from, I was keen to stay in a role which had significant patient contact. Advanced practice was being discussed for PICU and after chatting to the consultants about how they envisaged the role, I felt this ticked all the boxes I was looking for.
My typical work week is very variable. Whilst the ACPs sit and fill slots on the medical rota, we don’t follow the shift pattern – this is split between the whole
ACP team. Some weeks are clinically heavy and others have more non-clinical time. Clinical shifts can vary depending on the time of year (seasonal variations and timings around rotating medics’ arrival –it is always more intense whilst everyone settles onto the unit and figures out how things run and start to feel comfortable with the patient and workload) but nonclinical work is consistent. I enjoy the variety – there’s never a dull day on PICU.
The ACPs carry out ward reviews and offer clinical advice, attend crash calls within the trust and admit patients to the unit. We are responsible for the care of patients whilst on the unit including carrying out any clinically skilled interventions (intubating, inserting all types of lines and supporting the extended team during interventions that require bedside anaesthesia). We work days, nights and weekends alongside the medics and consultants and at times we can have ACPonly shifts. I help the consultants manage
the medics and ACP rota, I try to be approachable, informative, and fair to all. I have had some amazing feedback over the last few years whilst doing this and whilst rota management isn’t everyone’s cup of tea, I love solving problems that arise.
I find saying no challenging when something needs to be done, be it clinical or non-clinical. I can often take on too much and have had to make a conscious effort not to do this in recent months. Teams meetings and teachings are great but we all need to strike the right work/life balance. Also when I see how busy the nurses are –whilst we help out where we can, our own workload is also high, it’s a multi-team approach to caring for a patient on PICU and we all have to support each other. The change over the last 20 years has altered and we have all had to alter alongside it.
The one thing I’d change is night shifts! Whilst working independently is great and you’re able to really get stuck in as there are just two of us on shift, my increasing need for caffeine and chocolate to get me through is a worry. I look more and more like a zombie come morning handover and I hate to think what random nonsense I sometimes say. It’s a good job everyone knows what I’m really like.
FEATURE Milestones AUTUMN 2023 15
“I help the consultants manage the medics and ACP rota, I try to be approachable, informative, and fair to all. I have had some amazing feedback over the last few years whilst doing this”
“I am there to support them through their rotation and help build their confidence in paediatrics”
Sam Pearce Advanced Clinical Practitioner (Trainee) CAMHS Cornwall Partnership NHS Foundation Trust
@SamPearce30
CAMHS ADVANCED CLINICAL PRACTITIONER

I HAVE BEEN a qualified paediatric nurse for (ahem) over 20 years and that career has taken me from children’s intensive care in Leicester to special school nursing and then into CAMHS, where I am completing training for my ACP role, mental health pathway.
The ACP accreditation is well established in physical health, but new in mental health,
so there is still lots of learning about how an ACP fits in with traditional roles of psychiatry and psychology. The ACP route affords the possibility to pursue a clinical career, study at master’s level and to gain recognised accreditation.
Training has been a bit of an emotional rollercoaster. It only feels now, a year in, that I understand my role, what the training calls for and have become comfortable with having imposter syndrome! I have been fortunate to have some great consultant psychiatrists and psychologists as supervisors who have been willing to take a journey into the unknown with me, pick me up when I felt despondent and support my learning with opportunities and feedback that felt nurturing, not critical.
I am fortunate to be able to explore any learning opportunities or placements where I feel I needed experience. This has led me to my current placement in children’s and young people’s eating disorders, which it turns out feels like just my cup of tea, combining and growing my paediatric and mental health skills set.
Fiona Holter Advanced Paediatric Nurse Practitioner East Sussex Healthcare NHS Trust



ADVANCED PAEDIATRIC NURSE PRACTITIONER

ADVANCED PRACTITIONERS ALIGN to the four pillars of advanced practice, which encompasses clinical practice, education, leadership, and research. One of my passions is teaching. I enjoy demystifying paediatrics for the adult nurses, allied health professionals and medics whom I work with in my clinical setting. I offer teaching sessions, placements and shadowing opportunities and one new area I am currently developing is providing restorative supervision for staff after difficult situations.
When considering training opportunities with colleagues who are new or unfamiliar with paediatrics, I have found the following things helpful: try to understand the audience where they work, what their experiences of paediatrics might be, what might be something they see often or something they are afraid of seeing.



This helps me then to think about the aspects of anatomy and physiology that will be helpful for them to know about, framing it
in a simple but relatable way and not making assumptions about what they know. As an example, explain about babies being nasal breathers, suddenly the penny drops and the tiny baby with bronchiolitis that isn’t feeding and is struggling to breathe, makes sense to them.
I try and use processes or systems that are familiar to them, such as the A-E assessment; this way they are building on old knowledge and hopefully feel less overwhelmed. As well as signposting them to the good educational resources and guidelines that will help them in practice.
My other role is to work for Sussex health and social care. This is a system role within the integrated care system as the advanced practice network lead. I work within the non-medical education team, who are a mixture of nurses, allied health professionals and a healthcare scientist. This work puts me in contact with senior nurses, midwives and allied health professions from the various acute and community trusts, primary care, hospice,
and social care settings. This means that I am looking at advanced practice across the whole age spectrum and across a variety of specialty areas. I also work with universities, national advanced practice groups and the southeast advanced practice faculty at HEE. My role is to discuss various topics of concern or areas for growth in the advanced practice workforce, focusing on supervision, looking at training requirements and opportunities, career progression, funding, and organisational governance for the role as well as recruitment, and retention challenges.
Although this work isn’t exclusively CYP focused, it gives me a great platform to advocate for them amongst a mostly adult-centred workforce. One example is the current expansion of advanced practice roles in mental health, learning disability and autism services. Having the ability to turn the conversation to include CYP is exciting for me.
This role enabled me to network with other colleagues who have a passion for paediatrics and share knowledge and experience. Strategic work is often seen as far removed from patients, but I believe it is the marrying of clinical knowledge with system leadership that ensures the patient, and their voice, is always present.
FEATURE 16 AUTUMN 2023 Milestones
“There is still lots of learning about how an ACP fits in with traditional roles of psychiatry and psychology”
“It gives me a great platform to advocate for them amongst a mostly adult-centred workforce”
Kate Brown Advanced Neonatal Nurse Practitioner Hull University Teaching Hospitals NHS Trust


ADVANCED NEONATAL NURSE PRACTITIONER
PRIOR TO STARTING my Advanced Neonatal Nurse Practitioner (ANNP) training, I had worked in neonates for eight years, going from a newly qualified staff nurse and then over the years progressing to senior staff nurse. Part of my role as a neonatal nurse in a tertiary unit required me to care for critically sick and preterm babies in intensive care and also High Dependency Units (HDU) and Special Care
Baby Units (SCBU), as well as providing support, leadership, knowledge and teaching clinical skills to the nursing team. I have always had a passion to develop and learn more in neonates and enjoy the clinical aspects of the job, rather than progressing into a management role, so I felt the move to trainee ANNP was the right career path.
The training required me to complete a three-year Masters course at the University of Sheffield which involved completing an e-portfolio, lectures/presentations, simulation scenarios, essays, biosciences exams, nonmedical prescribing and a dissertation. This was alongside working supernumerary learning a brand-new role, essentially going from an expert nurse to novice.
Since qualifying last year, I started working on the Tier 1 medical rota. A typical week in the role can vary depending on which part of the unit I am covering, alongside the registrar and consultant. Intensive care days involve caring for the sickest babies potentially needing lots of procedures, such as intubation, Umbilical Venous Catheter (UVC)/Umbilical Arterial Catheter (UAC)/long line insertion, chest drains, cannulas and blood gases. Working in special care and the postnatal wards involves carrying the bleep where I attend all high-risk deliveries and review babies of concern, as well as carrying out the SCBU ward round and the postnatal ward babies.
The ANNP role is by far the best career pathway in neonates. It is an integral part of the neonatal team and is described as the ‘professional bridging gap between medical and nursing teams’. ANNPs provide a consistent and permanent level of expertise and I feel very privileged to be a part of the amazing ANNP team in Hull.
Deirdre Kindregan Trainee Advanced Clinical Practitioner in Community Paediatrics & Paediatric Neurology Barts Health NHS Trust


COMMUNITY ADVANCED CLINICAL PRACTITIONER

I TRAINED AS a physiotherapist and completed a PhD at Trinity College, Dublin. During the PhD I was keen to work clinically throughout so I worked in a children’s hospice at weekends. This meant working seven days a week to do both clinical and research jobs. I moved to London in 2018 and decided to work clinically full-time in paediatric neurodisability. Advanced Clinical Practitioner (ACP) roles appealed as a way to combine my clinical and research experience in one role, but also as a chance to work at the top of my licence and get
more involved in the diagnostic side of neurodisability. I’ve been really lucky to be embraced by both the community paediatricians and the paediatric neurology team at Mile End and the Royal London Hospitals.
Becoming an ACP has opened up a new world for me, particularly with the incredible developments in genetic testing. I have been involved in finding diagnoses for children who previously only had a description of their problems. My role allows me to be a truly holistic practitioner, looking at all aspects of a
child’s development and linking this with their health, as well as collaborating with the wider team, across medical and therapies teams. I hope that my experience as a physiotherapist and my newly acquired skills in advanced assessment, diagnostics and prescribing, make me an ideal practitioner to assess, investigate and treat children with difficulties with gross motor development. I am currently completing my dissertation for the MSc in ACP and am very excited to gain experience as a fully-fledged ACP.

FEATURE Milestones AUTUMN 2023 17
“Working in special care and the postnatal wards involves carrying the bleep where I attend all highrisk deliveries and review babies of concern, as well as carrying out the SCBU ward round and the postnatal ward babies”
“My role allows me to be a truly holistic practitioner, looking at all aspects of a child’s development and linking this with their health, as well as collaborating with the wider team, across medical and therapies teams”
How to ace your subspecialty application
Dr Niall Durrant gives his top tips on the sub-specialty application process and how you can start preparing to make a successful application


ON A COLD WINTER’S NIGHT in 2021
I spent hours hanging fairy lights, only for them to fuse at the last moment. On stomping inside, I received an email announcing my sub-specialty application had abruptly ended with rejection prior to interview. A little over a year later, I was deliberating between two separate sub-specialty offers. How?

The basics


With Progress+ you can apply to subspecialty training from ST4. You need to have your clinicals by the time of interview and a satisfactory ARCP. You can apply as many times as you want, if there’s enough time to complete before CCT. It’s also worth considering SPIN – this isn’t available in every sub-specialty, but does keep you in your current region, and isn’t as competitive.
Be smart, start now
On the RCPCH website, find your specialty scoring criteria and assess yourself. Make SMART goals to improve low scoring areas. Pay attention to timelines – a smaller completed project may score better than a bigger, more impressive one. Before saying yes to anything, ask yourself if it fits your criteria – and say no to those that don’t. Submit everything, including previous work, for presentation or publication – some conferences even publish poster abstracts, as a bonus.
Start writing your application early too, making sure to link experiences or cases directly to specific personal development.
The room where it happens
Contact relevant organisations, such as PERUKI, and ask to join. They’re often surprisingly welcoming, and a trainee voice can bring genuine added value. These spaces provide insight into management, governance and research often invisible to trainees. Once in the room, say yes to things! This is also a good way to make contact with those who went through the sub-specialty recruitment process before you.
Find your tribe
As they say, it’s dangerous to go alone. Contact colleagues in your specialty already and ask them to review answers or practice for interview with you – Twitter is a great place to start. I had incredible support from mentors and friends who gave honest, critical advice.
Nail the interview
Prepare answers, use structures such as CAMP (but be sure not to rely solely on pre-prepared answers and make sure you answer the question asked each time), think of examples of conflict, mistakes etc. Relate every answer back to specialty and demonstrate
awareness of real-world specifics.
Practise. I cannot emphasise this enough. Practise multiple times, with different people. Create as much pressure as possible – on video, under timed conditions. Consider a ‘dress rehearsal’ – in the location you’ll do the interview, in the same outfit, ideally at the same time of day, to make sure lighting, connections and sound all work.
On the day
Be ready early. Optimise your space, minimise distractions and interruptions. Dress the part – including from the waist down! Have a glass of water handy – taking a sip helps to pace answers and prevent you rushing into a response. Don’t forget multi-part questions are a possibility. Assessors are always instructed to let candidates know if a question will have a second part in advance but on the off-chance they do forget or go off script, don’t worry –the panel lead and observers are there to keep things fair and on track.
Prepare to fail
As hard as rejection is, no advice I can give will be as useful as actual experience. There’s no penalty for applying multiple times, so I strongly urge you to take a crack. You can gain time for extra attempts by taking an OOP – these don’t have to be directly in your specialty of choice, either. Taking a teaching fellowship gave time and an open remit for projects of my choice, putting me in a much stronger position for the second attempt. (Don’t say that’s why you want an OOP though!)
Find me on Twitter for any questions, and good luck!
Find out more:
www.rcpch.ac.uk/apply-sub-specialty
FEATURE
18 AUTUMN 2023 Milestones
Make sure any projects you take on fit your criteria
Dr Niall Durrant PEM Sub-specialty Trainee ST6 St Helier Hospital @DurrantNiall
The best paediatric diabetes team!
Dr Anu Sharma shares how her team has had a motivational impact on her personal health and wellbeing




ISN’T IT GREAT if you work with a group of people who leave a lasting positive impact on you? I have a bunch of enthusiastic paediatric diabetes specialist nurses (PDSN) and dieticians in my team, who are always involved in some outdoor activities like Parkruns, marathons, half marathons and rugby. I learnt that they were running the Newport 10K in April. Although I liked the team spirit, I did not believe that I could also possibly do it. So, I kept quiet. One fine day, as I was sitting in the clinic, one of the PDSNs named Bel (who I think is always in a top gear) said to me that none of the doctors from the team were running the 10K. I replied that I would have liked to do it, but I feel so tired. I have a young family and so on. Bel replied in an instant that “with this attitude Anu, you can’t do anything!”

And that was it! Even though I left it till the last minute thinking that nobody will remember it, I still registered for the 10K. But I was the first one to reach the venue! Inside me was a pounding heart that was constantly reminding me that I could return any time. Emily, our dietician, had arranged for the team T-shirts. Suzanne and Viv came in the morning of the race,
only to support us. The running team also had Claire, Laura and Jonny. I was feeling very nervous and a bit embarrassed within myself. I had barely managed up to 5K on the treadmill and regularly walked my dog for the last few weeks. That was all that my endurance and strength training was about. I also promised myself a pair of new trainers if I managed to finish this race. I thought that bribing might help and keep me motivated.
I started my first 10K. Within no time, I felt a cramp in my leg. I eased off a bit and started to walk. There were moments when I felt that I could step out and return. But there were so many volunteers including children who were watching. I thought that I would be more embarrassed if I backed
out. I vaguely remember that a volunteer was offering Haribo sweets on the way and that one Haribo was enough to recharge me. I decided not to have water from the water station on the way. But just like a tortoise, slow and steady, I finished the race! I was so proud of myself. I couldn’t thank the team enough. No wonder, I believe that I work with the best team ever!
It did not stop there! I have a significant family history of Type 2 diabetes. Knowing that, my team offered me to try a continuous glucose monitor. This was really an eye-opening experience. I could understand the unfriendly relationship between my blood sugars and the food that I ate. I could appreciate the difficulties of my patients with Type 1 diabetes, who have to constantly keep a tab on their sugars, in a much better way.
To this day, I continue to do regular walks and my food choices have improved for good. No matter if it is just a workplace, we can still try to support each other in good things which can help some of us, like me, a long way! Thank you, team, and well done!
My message to everyone is to reach out to others if you can. Make a difference with little gestures, like sending birthday wishes. You never know if somebody is living away from their loved ones and being lonely in the cold! Hold team events and stay connected. You never know when and on whom you can have a lasting positive impact!
FEATURE Milestones AUTUMN 2023 19
Dr Anu Sharma
ST8 Paediatric Registrar
The Grange University Hospital, Cwmbran @anusharma777
Anu with Bel, Laura and Claire at the 10K run
Social prescribing for children and young people
From offering practical support to setting goals, Luana Baptista outlines how she has been empowering children and young people


IWORK
WITH YOUNG PEOPLE FROM THE AGES OF 11 TO 18. The two cohorts include young people with sickle cell or thalassemia and young people that present with medically unexplained symptoms.
My referrals come from clinical teams at Royal London Hospital including consultants, clinical nurse specialists, clinical psychologists and psychiatrists. I have four to six sessions with a young person. These could be in their home, the hospital, a local youth/community centre or in a coffee shop. Normally for the first session we meet in the hospital, so that the young person can meet me and build that initial rapport and trust. Young people are encouraged to come independently unless they would like their parents to be there too. In the first session, we complete the Youth Star Scales by Triangle which means the young people rate themselves on six different sections of their life including interests and activities, hopes and dreams, health and wellbeing, education and work, communicating and choices and behaviour. The Youth Star scales rate 1 as stuck, 2 as considering, 3 as having a go, 4 as working on it and 5 as achieving. Each section has a sentence describing the scale which really helps young people decide and have a real example rather than just a “agree, disagree” or 1-5 rating.
In every session we complete a HEEADSSS assessment. The assessment stands for home, education, eating,
activities, drugs and alcohol, safety, suicide/depression, sleep, social media and sexuality and allows a very open and holistic conversation. Although there is a structure and I discuss every section of HEEADSSS, I allow the conversation to flow and guide it accordingly. For example, if the young person has a restricted diet due to a health condition such as IBD, we will discuss eating and I may ask about how their restrictive diet affects their mood/how much they do with friends. This would then link into the suicide/depression section, as well as activities.
From the information gathered from the initial session, we figure out goals that the young person would like to achieve. These could range from finding table tennis sessions, to shaping up their CV to apply for
jobs because they want to save up for a new phone. Typically, I aim for three goals on the first session. This gives me three different areas I can research to find services to fulfil the goals of the young person. We also try to have a couple of goals for the young person to take away, such as thinking about what course they would like to do at college or if they can think of another social activity they would like to participate in. I then collect the information and either actively signpost or refer the young person to the service. I also offer practical support. For example, I may go with a young person for their first boxing session at a youth centre, as this can be super overwhelming initially. I can also go with a young person to the library to get a library card and find out what activities they’re running. Every session is goal led, always focusing on empowering young people and ensuring what we do is sustainable once the intervention is over.
Feedback I have received from young people has been very positive. A 16 year old young person said: “Hi there, I’m doing great. Hope you’re doing well. Since I have finished the sessions I have been fine, I am currently looking for jobs at the moment but I should be able to find some now that I have my CV sorted. I didn’t really have a favourite part of the sessions, I’d say that I enjoyed it as a whole. I think that the sessions were incredibly useful and there is nothing else that would’ve wanted from the session, it was great!” We have also had interest from other teams in the hospital including trauma, haemophilia, A&E and the adults haematology team.
It has been incredible to be part of such an innovative and young person-focused project, especially in secondary care.
FEATURE
20 AUTUMN 2023 Milestones
Luana Baptista Children and Young People’s Social Prescribing Link Worker (CYP SPLW) Royal London Hospital
London’s childhood asthma programme

With London experiencing high levels of asthma admissions, the #AskAboutAsthma campaign aims to improve asthma care and services
IN 2014-15, LONDON WAS EXPERIENCING HIGH LEVELS OF ASTHMA ADMISSIONS, excessive deaths plus fragmentation and variation in care. Resources were limited for children and young people who did not feature within the NHS Five Year Forward View. Responding to this concerning trend, London health leaders, including me – at the time, Deputy Director for the Children and Young People’s Programme at Healthy London Partnership – worked to develop a social movement to increase awareness of asthma care and promote improvement in services across the capital.

The London asthma programme began in 2016 and asthma ambitions standards and an asthma toolkit were developed to raise the profile of childhood asthma. Whole system standards brought together national and international standards of care and have since influenced the development of the national asthma bundle of care (England, 2021).
Children and young people’s asthma now forms part of the NHS England – London Babies, Children and Young People’s Transformation programme and our team works collaboratively across the whole asthma system to produce new tools and resources and give training and networking opportunities for clinical professionals.
Seven years on, however, asthma is still often seen as a minor health condition –despite its prevalence and the potentially fatal consequences of poor management. To address this, our team has launched campaigns including the ‘Right Inhaler Image Campaign’, which aimed to improve the quality of media portrayal of inhaler devices, and an annual awareness campaign in London, #AskAboutAsthma, which centres around simple changes that can help children and young people and their families to manage their asthma effectively.
In 2022, #AskAboutAsthma reached its largest audience yet with support from the Mayor of London, NHS organisations across England and national asthma charity, Asthma + Lung UK, amongst others. This year’s campaign week takes place from 11-17 September, just ahead of the annual spike in hospital admissions for asthma following the start of the autumn term. This year’s theme is ‘Widening our view’, highlighting the wider factors of children and young people’s asthma care such as housing, mould and vaping. By highlighting these everyday factors and their impact on lung health, we hope to encourage professionals and teams outside of
healthcare – for instance education, housing and environment – to consider lung health when planning and delivering long-term improvement policies across London.
The theme also invites us all to reach out to everyone who has asthma, their friends, families and the system that cares for them, and help them learn about the four measures that can help manage the condition:
1. An asthma action plan A written asthma action plan drawn up between a clinician and patient means people are four times less likely to have to go to hospital for their asthma.
2. Effective use of inhalers Less than threequarters of children and young people have any form of instruction in how to use their inhaler. Poor technique means patients don’t get the full benefit of their medication.
3. Asthma reviews An asthma review by a clinician after every attack helps to work out what went wrong. An annual review ensures effective management of the condition.
4. Knowing the impact of air pollution Every asthma conversation should consider the impact of outdoor and indoor air pollution on children and young people’s asthma.
The campaign week includes themed webinars, a virtual one-day conference and daily podcasts, videos and blogs shared by young people and families and experts in pharmacy, nursing and primary care.
FEATURE
Sara Nelson
Joint-Head of Babies, Children and Young People’s Transformation Programme
Milestones AUTUMN 2023 21 Visit: www.transformationpartnersinhealthandcare.nhs.uk/ask-aboutasthma-2023 Get in touch if you’d like more information about becoming an #AskAboutAsthma ambassador around the UK: england.cyptransformationldn@nhs.net
NHS EnglandLondon @BCYP_NHSLDN
KEEP IN TOUCH
We’d love to hear from you, get in touch through our channels
Twitter @RCPCHTweets
Facebook @RCPCH
The latest member news and views
Celebrating 50 years of the Welsh Paediatric Society
JUST BEFORE THE SUMMER
SOLSTICE, the Welsh Paediatric Society (WPS)
 Dr David Tuthill Consultant Paediatrician Cardiff & Vale University Health Board
Dr David Tuthill Consultant Paediatrician Cardiff & Vale University Health Board
celebrated its 50th anniversary at the beautiful Lake Vyrnwy Hotel. The WPS was founded in 1973 to provide a political and social network for Welsh paediatricians, promoting good practice and research. Its meetings have provided enduring friendships for members and much encouragement to trainees.


Paediatricians from across Wales and neighbouring areas have had the opportunity to share knowledge, undertake and present research; all aiming to provide the best possible child health service. Since 1989 we have had the Welsh Paediatric Journal published and in 1992 set up the Welsh Paediatric Surveillance Unit which has completed over 40 successful studies.
We have an active membership of over 200 and have two meetings each year; traditionally the spring
one is held in North Wales and the autumn gathering in the south. This year, we had a single one-and-a-half days celebration. It focused on the commemoration of good practice of paediatrics and what had spread out from Wales to the wider community. The bar was set high by the first speaker on the use of the SAIL database for research and the strides made in paediatric diabetes. Subsequent guest speakers and presenters maintained this excellent start all the way through to the closing presentation on paediatric training, covering palliative care and genomics screening amongst others on the way. The presence of the Irish Paediatric Association’s and the Scottish Paediatric Society’s Presidents represented our wider Celtic devolved nations’ areas. The first day was rounded off by a celebratory meal, a twmpath (a Welsh barn dance) and fireworks across the valley, followed by group singing. This provided a fitting celebration to the first 50 years; roll on the next 50!
Instagram @RCPCH
milestones@rcpch.ac.uk
HISTORY TAKING: A MOTTO FOR PAEDIATRICIANS
I HAVE ALWAYS BEEN PROUD of the ‘child health’ aspect of RCPCH. I’ve drunk the Kool-Aid and love the work done to improve the lot of children, as well as paediatricians. Where does the focus on health and not just sickness come from?
James Spence (of medal fame) was born in Northumberland in 1892 and trained in Newcastle. He served in WWI, receiving the Military Cross for conspicuous gallantry.
After returning to the Northeast in 1924, he became the physician to a nursery, which evolved into Newcastle Babies’ Hospital, and the medical officer of a child welfare clinic. Here, Spence realised the benefit to patients of holistic care involving the families, but noted that “many preferred professional convenience to the logic of biology”.
In 1932, the city asked him to investigate the relationship between health and nutrition in young children – the first time that social and clinical factors were linked. Social paediatrics was born and Spence developed child epidemiology as an academic pursuit, with a 1,000-family birth cohort study.
Dr Richard Daniels Paediatric Registrar (OOP)







He advocated for paediatrics becoming a significant part of the undergraduate curriculum and went on to hold numerous roles, sharing best practice across the world. He assisted the founding of the NHS and the British Paediatric Association (BPA), the forerunner of RCPCH. Yet, amidst this patientfacing success, the most resonant thing is something he wrote about his leadership role.
“The first aim of my dept is comradeship not achievement”.
By supporting each other, we create an environment where there is space for many to improve child health. Something to think on.
Radish @DrRDaniels
22 AUTUMN 2023 Milestones
David with Dr Michael O’Grady, President of the Irish Paediatric Association and Prof Steve Turner, President of the Scottish Paediatric Society
IMMS UP TO DATE?
ASKING ABOUT IMMUNISATIONS is ingrained into us from the minute we start paediatric training and is often a cursory question with ‘up to date’ scribbled in the clerking. Sometimes, the answer might be more complicated – maybe they’ve been delayed, or parents are opting out of some or all the routine vaccinations. How do we address this?
All too often the answer is to put the conversation off – because the child is acutely unwell, the parents seem defensive or the healthcare professional doesn’t really know what to say. The conversation is more complicated when it comes to vaccines not included on the routine schedule, such as the varicella zoster vaccine. It becomes not only a case of answering concerns about side effects and complications but also understanding the barriers that may prevent many families from accessing it.
This year, I’ve had the chance to gain a much better understanding about the work that goes on behind the scenes looking at vaccine hesitancy and education. Working with experts in the field of vaccine hesitancy, we’ve created a survey to look at paediatricians’ attitudes towards the varicella zoster vaccine, with the aim of understanding current practice and looking for gaps in knowledge and training. This project has been an incredible insight into the impact of vaccine hesitancy on childhood disease, and the health inequity gap that is widened by vaccines not being on the routine schedule. Open until 16 September, the survey is available via QR code, or by visiting chicken-pox.org where you can find participant information and a link to the survey – it takes 10-15 minutes, and the results will help to inform policy and educate trainees.



INGREDIENTS

100g hazelnuts
I LOVE MERINGUE! If you asked me what dessert to make for a dinner party, I would generally recommend a pavlova. A perfect way to use up any fruit, which also complements the sweetness of the meringue beautifully. Plus who doesn’t love a bit of whipped cream? They can be tricky to handle without cracking so baking the meringue in tins is much easier. This meringue cake is nuttier and has the look of a Victoria sponge, but is way more exciting and naughtier to eat (also gluten free!). The gold standard method to consume a meringue bake – grab a spoon and dig in! Be warned though, it won’t last long so be primed to fight your guests for every bite!
cake
Sunflower oil for greasing
150g caster sugar and an extra
2 tablespoons


3 large egg whites
Pinch of salt
½ teaspoon white wine vinegar
170ml oat cream
½ teaspoon vanilla extract
170g Greek-style natural yoghurt
400g strawberries, sliced
Instructions
1. Preheat the oven to 180˚C. Roast the hazelnuts on a baking tray for eight minutes until golden and set aside to cool.
2. Grease two loose-bottomed 18cm sandwich cake tins with sunflower oil and line them with baking parchment.
3. Using a food processor, pulse the cooled hazelnuts with one tablespoon of caster sugar until finely ground.
4. Using an electric whisk or mixer, whisk the egg whites with a pinch of salt until they form stiff peaks. Continue whisking whilst adding in the 150g caster sugar one spoonful at a
time until combined to form meringue.
5. Fold the ground hazelnuts and white wine vinegar into the meringue. Divide between the two tins, smoothing the tops. Bake in the oven for 30 minutes then allow to cool completely.
6. Whisk the cream with the remaining one tablespoon of sugar and vanilla extract until the mixture forms soft peaks. Stir in the yoghurt.
7. Remove the meringue cakes from their tins. Start with a layer of meringue and top with a layer of cream and then strawberries. Repeat the process forming a second layer. Voila – serve at once!


MEMBERS
Strawberry and hazelnut meringue
Milestones AUTUMN 2023 23
Dr Ashish Patel ST8 Paediatric Nephrology & Sim Fellow Birmingham Children’s Hospital @DrKidneyAsh
Dr Lizzie O’Mahony Paediatric ST3 Royal Brompton Hospital @Lizzie_Omahony
A medical student prize winner

AS ONE OF THE WINNERS of the RCPCH medical student prize, I had the opportunity to attend this year's RCPCH Conference in Glasgow. I am excited to share my experience so you can consider applying next year!
The RCPCH medical student prize offers you the chance to have your interest in paediatrics recognised and furthered. It provides an opportunity to connect with likeminded individuals at RCPCH and explore what a career in paediatrics looks like for you!

The experience began with a prize-giving reception hosted by the wonderful RCPCH Choose Paediatrics team! I met the other students and talked with senior clinicians, including RCPCH Officers, VicePresidents, and the President.
Whilst attending my first national paediatrics conference seemed
daunting at first, I quickly realised that everyone was incredibly enthusiastic about meeting medical students who share their passion for paediatrics! I thoroughly enjoyed the diverse line up of talks and subspecialty workshops.
The highlight of the conference was meeting the other prize winners. Whether it was planning which workshops to attend over breakfast, reflecting on the keynote speeches during coffee breaks, or exploring Glasgow in the evenings, we had a wonderful time together!
To apply for the RCPCH medical student prize, you'll need to submit an application to your Head of Paediatrics, who will nominate a winner. Reach out to them during the autumn term for details and the internal deadline for your medical school. Best of luck!
Being relatable to patients as a medical student
A COMMON DILEMMA for medical students is learning how to balance being relatable to patients whilst maintaining professional boundaries. In some situations, the student may not be much older than the patient. It is easy to see how being more ‘relaxed’ around adolescents, using common interests, can help build rapport but this can blur boundaries. Often, the adolescent is not trying to be inappropriate, but they feel comfortable to open up to the medical student as someone they see as being relatable.
Osasere Osayimwen Final Year Medical Student University of Southampton





Whilst being relatable can contribute to a positive experience, we must do this safely by adopting clear boundaries. Students should reflect on what topics would not breach professional boundaries and, if they are unsure, seek advice. If these boundaries are crossed, students should gently redirect the conversation. It can be effective to be honest with your patient; this is a display of respect which can strengthen the relationship with a patient, who sees they are regarded as mature enough to handle such feedback. Trust your own judgement and shift conversations that don’t feel right – you’re doing an amazing job for your patients even if you don’t share everything!
AN ASPIRING PAEDIATRICIAN AT RCPCH CONFERENCE
Dr Jerin Rahman Foundation Year 1 Doctor Scunthorpe General Hospital
I DECIDED TO get a ticket for the RCPCH Conference as I was interested in learning more about the paediatric career pathway and making connections with like-minded people. I was a bit nervous before attending as I didn’t know anyone before going but from hearing patient stories to making new friends and important reflections on exploring links between social inequity and health outcomes, I’ve gained so much.
My favourite talk explored the use of patient stories
for medical education. The patient story was so moving and allowed me to reflect on how much impact we have on our patients as healthcare providers. Hearing this story will impact the way I approach patient interactions in the future. Of course, the conference dinner was also a major highlight packed with dancing, tasty food and great conversation, I even got a chance to try ceilidh dancing! I would recommend the conference to any budding paediatricians interested in learning more about the field and exploring new ideas.
MEMBERS
Shivani
Ganesh
4th Year Medical Student
Barts and the London School of Medicine and Dentistry @shivani_g22
24 AUTUMN 2023 Milestones
FOR IMGS BY IMGS: ACHIEVING SUCCESS IN THE MRCPCH CLINICAL EXAMS
A career in paediatric allergy
 Dr Josephine
A. Quaynor ST3 Paediatric Trainee
Dr Josephine
A. Quaynor ST3 Paediatric Trainee
Birmingham Children’s Hospital
THE DECISION TO relocate to the UK from my home country Ghana was not an easy one, but it was all with the dream of becoming a paediatrician. After clearing the hurdles of getting into paediatric training, I faced the arduous task of passing the MRCPCH exams.
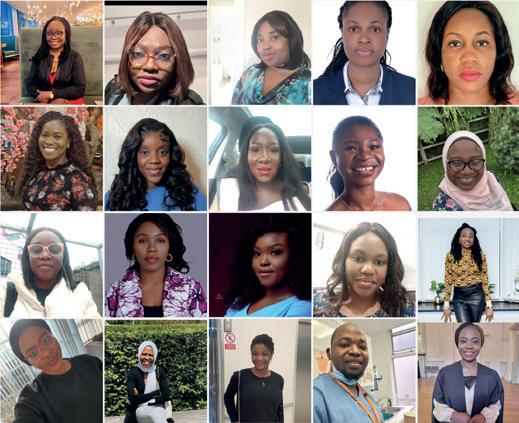

ALLERGY IS A TRULY exciting area of medicine to work in right now! Cutting-edge research is driving changes to worldwide clinical practice, with new approaches to preventing and treating allergies, which dramatically impact on our patients’ quality of life.
I am aware of some challenges faced by international medical graduates (IMGs) with limited experience in the UK and the issues surrounding differential attainment, so I knew I had to put in the effort to pass the clinical exams. I have always believed in the power of group studying so I got together with other IMGs online to study for the clinical exams. We would meet online after work and practise for two hours. Most of us had never sat the clinicals before so we sought advice from senior trainees.
@MRCPCH_Pearls
After we had passed the clinical exams, we wanted to support and empower other IMGs through a similar platform to achieve higher success rates. This led to the formation of Clinical Pearls, a platform where candidates can prep for the clinical exams through safe spaces and constructive feedback. The faculty is now made up of over 20 enthusiastic and committed paediatric doctors and we have close to 60 candidates who have gone through the programme in the past year and a half.
The Clinical Pearls group is now a second family to me, and we support each other outside the sessions. You don’t want to see us banter about Ghana and Nigerian Jollof! It is always so exciting. The Clinical Pearls group aims to continue to play a key role in improving success outcomes for IMGs sitting the clinical exams. If you’d like to get involved, please get in touch at mrcpchclinicalpearls@gmail.com
I didn’t start my medical training thinking I would become a paediatric allergist, or even knowing it was a thing, but here I am a few years later, with a brilliant portfolio career. My job keeps me challenged with a mixture of clinical medicine, service development, education and research. All of this, with the flexibility to work around family commitments, and no nights or on-calls. If this sounds attractive then it is definitely worth considering as a career!
I am currently working as a consultant in paediatric allergy at Southampton Children’s Hospital, a large specialist tertiary allergy centre. I completed my training in paediatric allergy, immunology and infectious diseases and studied for an MSc Allergy at the University of Southampton at the same time. I am faculty and module leader on the MSc Allergy, which has gained international recognition and is an excellent way to learn about it.
Paediatric allergy is an outpatient-based, multidisciplinary specialty involving doctors, nurse
specialists, dietitians and psychologists. Day to day clinical work focuses on the diagnosis and management of allergic disease including food allergy, eczema, asthma, allergic rhinitis, chronic urticaria and drug allergy. On our day ward we perform food challenges and drug provocation tests and many centres now offer food desensitisation. Allergen immunotherapy is a busy part of the service, treating patients with pollen, dust-mite and venom allergies. Paediatric allergists work closely alongside general paediatric teams and other specialties including dermatology, respiratory, gastroenterology, ENT and ophthalmology. There is plenty of opportunity for collaborative working with joint clinics, as well as shared care with teams in local and regional centres. There are many opportunities to become involved with clinical research at local, national and international levels.
Paediatric allergy is a small sub-specialty but with increasing demand. As a result, I have a close network of colleagues (and now friends) up and down the country, and across the world. There are opportunities to become involved with regional and national committees, including our friendly and active British Society of Allergy and Clinical Immunology (BSACI), and European Academy of Allergy & Clinical Immunology (EAACI). To find out more about training in paediatric allergy, either sub-specialty or SPIN (specialist interest), then contact the Training Team at RCPCH CSAC.
www.rcpch.ac.uk/paiid-csac
MEMBERS Milestones AUTUMN 2023 25
Dr Stephanie Cross Consultant in Paediatric Allergy Southampton Children’s Hospital
Members of Clinical Pearls
BOOK REVIEW: SOMETIMES PEOPLE DIE
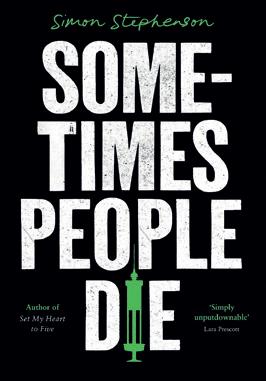 by Simon Stephenson
by Simon Stephenson
I’M ALWAYS ON the lookout for a good audiobook, and recently on a long drive back to the continent I found the perfect one – for anyone who’s ever been a junior doctor and for anyone who likes a thriller. Sometimes People Die, by Simon Stephenson, is a whodunnit set in a hospital in 1999, where patients are dying at an alarming rate. You’ll recognise the atmosphere, and the characters, and it’s oh so believable. The book is punctuated by fascinating little snippets of history about healthcare-related murderers.
My teenager sat next to me as the French sun fell over the autoroute and the kilometres ticked by, listening intently, not even playing on their phone (a never event), and worryingly is now making noises about being interested in medicine (having previously declared that “no offence, medicine is a dumb job”). Should I be worried? …Probably. (As should you.)
Anyway, I won’t tell you any more of the plot. I don’t want to ruin the joy of discovery. Borrow it from your local library (and did you know that many libraries have apps to borrow e-books or audiobooks?) or buy it – you’ll soon be passing it to your medic friends!
BOOK REVIEW: PSYCHOANALYTIC WORK WITH CHILDREN IN HOSPITAL
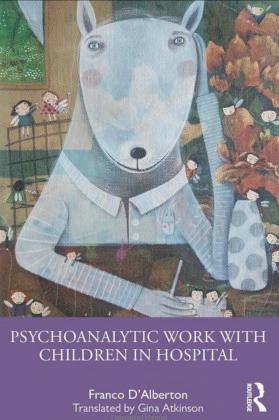 by Franco D’Alberton
Dr Gautam Kulkarni Consultant Paediatrician Circle Health London @geekulkarni
by Franco D’Alberton
Dr Gautam Kulkarni Consultant Paediatrician Circle Health London @geekulkarni
 Consultant Clinical Psychologist
Consultant Clinical Psychologist





“EVERY TIME FREUD is right, a psychologist dies”. Not elegant, but this T-shirt slogan flags my resistance, expecting environment or endeavour alien to UK paediatrics. After my usual cringe at the power imbalance between the unknowing patient and the interpreting psych, came the recognisable complex interplay of psychological and physical presentation, insights, and co-working. D’Alberton introduces identity, what you have vs what you are, upholds intellectual curiosity, centres societal and family context, and gives us the psycho-dynamics of interprofessional organisational systems. Chapters of well written wisdom are organised by theoretical fundamentals and clinical concerns, e.g. neonates, pain and memory; parent-child consultations; functional disturbances, and chapters on group work with staff. The work is modern, relevant, enjoyable and helpful. It reminds us that our wideranging medical and psychological practice is interpersonal and intrapersonal, and mind/body severance is futile.
Recent Advances in Paediatrics
RECENT ADVANCES IN
PAEDIATRICS was my favourite publication during my paediatric training. So, I was thrilled when I was asked to take responsibility for the latest edition. Featuring a collection of articles relevant to paediatricians across the world, it reflects the changing landscape in paediatrics, with a significant emphasis on adolescent health.
As paediatricians, it is vital we are involved in the care of children undergoing surgery. There is an emphasis on improving the safety of the children we look after by introducing safety checklists and
having clear pathways of escalation for sick children as well as hub and spoke models. Implementing safety checklists universally could mean doctors and nurses moving across hospitals (or even continents) can provide the same high standards of care.
The book is also relevant for medical students as it covers aspects of paediatrics often not covered in conventional textbooks. Some aspects of this book including the sections on adolescent health, technology and improving safety will be relevant to parents whose expertise in their own children is always one of our most
valuable resources!
We have referenced conversational AI and Chat GPT which leads me to reflect on whether, in future, healthcare may move to a point where parents are indeed experts in their children's health and paediatricians help facilitate this by requesting investigations and treatment plans in conjunction.
I feel current healthcare systems have caused frustration amongst clinicians by burdening them with administrative tasks. This could change with AI facilitating tertiary referrals, discharge letters and ongoing patient support, leaving us with clinical work!
MEMBERS 26 AUTUMN 2023 Milestones
Dr Julie Alderson
University Hospitals Bristol and Weston NHS Foundation Trust
Milestones Editor @I_am_spottacus
Dr Maddy Fogarty Hover ST6 Paediatrics Leeds Children’s Hospital
We put 10 questions to a consultant paediatrician and her paediatric trainee



Dr Linda Whiteford
 Paediatric Consultant, Somerset NHS Foundation Trust
Paediatric Consultant, Somerset NHS Foundation Trust











1) Describe your job in three words. Challenging, rewarding, teamwork.
2) After a hard day at work, what is your guilty pleasure?
Watching a good murder mystery and trying to work out who did it.
3) What two things do you find particularly challenging?
Dealing with teenagers (at work and at home) and ‘management speak.’
4) What is the best part of your working day? The start – there is still so much time to do all the things I need to do!
5) What is the one piece of advice you wish you could impart to yourself as a junior trainee?
Don’t stress about the future – it all worked out in the end, and you have a great job now.
6) Who is the best fictional character of all time, and why?
The Doctor – intelligent, witty, repeatedly saves the world and has more than one lifetime of stories to tell.
7) What three medications would you like with you if you were marooned on a desert island filled with paediatric patients?




Co-amoxiclav, paracetamol and salbutamol.
8) If you were bitten by a radioactive gerbil, what would you like your superpower to be, and why?
X-ray vision – I never have to try and organise a GA MRI scan again.
9) What is the single, most encouraging thing that one of your colleagues can do to make your day?
Make me a cup of tea… and if it comes with a chocolate bar, even better!
10) How can you and your colleagues inspire the next generation of paediatricians?
Leading by example – sharing our passion and enthusiasm with others.
Dr Claire Hope

 Paediatric Registrar, Somerset NHS Foundation Trust @babydrclaire
Paediatric Registrar, Somerset NHS Foundation Trust @babydrclaire


1) Describe your job in three words. Teamwork, rewarding, tiring.
2) After a hard day at work, what is your guilty pleasure? Being childlike silly with my toddler... then a big grown-up glass of wine.
3) What two things do you find particularly challenging? As a trainee never knowing where you’ll be working or how your life will look in the next six months/year. In work when you’re firefighting and pulled in so many directions on a busy shift you don’t feel you give your ‘best self ’ to any patient.
4) What is the best part of your working day? The team around you and the little moments, reassuring parents their child is OK.
5) What is the best advice you have received as a trainee?
“This too shall pass” is something my parents have always said. It applies to the worst shifts or most tricky periods of training.
6) Who is the best fictional character of all time, and why?
I’m reading Zog and the Flying Doctors a lot and love Princess Pearl. She’s fiesty, kind and stands up for herself. A fantastic role model for my little girl and uses EBM to solve problems!
7) What three medications would you like with you if you were marooned on a desert island filled with paediatric patients? I love adrenaline… IM/IV/nebulised. Maybe some Dex. And salbutamol. Can you tell it's been a wheezy week?!
8) If you were bitten by a radioactive gerbil, what would you like your superpower to be, and why?
I’d like to borrow a time-turner so I could do all the things I need to do AND find time to read, play sport, tackle the garden and spend time with my loved ones.







9) What is the single, most encouraging thing that one of your colleagues can do to make your day?













Give positive feedback. We can be too busy to do it sometimes or focus on the negatives, but a bit of praise or encouragement goes a long way.
10) How do you think you and your colleagues can inspire the next generation of paediatricians? Keep doing our jobs well! Paediatricians are kind, enthusiastic, passionate doctors and I honestly feel it rubs off when you get an interested trainee.
praise and and
MEMBERS Milestones AUTUMN 2023 27
STARTER FOR TEN KEEP IN TOUCH
@RCPCHTweets @RCPCH @RCPCH milestones@rcpch.ac.uk
s
Wellbeing Starting with kindness
With increasing pressures placed on us all, Dr Bob Klaber explores how kindness can move from being a passive concept to something that is actively demonstrated and at the heart of the workplace





ANUMBER OF FRIENDS
of mine who don’t work in healthcare have expressed disbelief that an industry that is focused on the delivery of care is, at times, so deeply unkind, harsh and uncaring.
Yet for all of us working in healthcare in the NHS, and indeed in healthcare systems across the globe, our working lives can feel incredibly challenging at the moment. The stresses and pressures on everyone seem to be growing all the time, and it’s hard to stay hopeful about the future with the background of a 24/7 newsreel that is unrelentingly negative. But my feeling is that a key responsibility of being a doctor, and in that a leader, is to find ways to generate hope and excitement about a better future for the people and communities we serve. At the heart of outstanding care is kindness.
Not kindness as a soft and frivolous thing, nor as a state of being that belongs only to optimists, but as actions and decisions we choose to make every single day. In my mind, there is nothing more important than this, and if we get this right pretty much everything else can follow.
And so it’s been amazing to be part of a growing community of health and care workers across the globe coming together, with a determination to make healthcare a much kinder place. For everyone involved in this work it has been a real thrill to see our Royal College place this agenda of kindness front and central to its main annual scientific conference. And having had the privilege of the opportunity to present a plenary session at the conference in May, I have been bowled over by the response from so many people, stretching from students still contemplating a career in paediatrics to others long since retired. A small part of this response has been one of thanks, for recognising and describing this issue and the opportunities around it, but at its heart the response from people has been one of action, one that says “count me in”.
And it is this focus on action –recognising that kind behaviours are both a choice and an action – that needs to say central. After all, as I touch on in my talk, the evidence base for action on kindness is really strong. The likes of Len Berry have beautifully demonstrated that kinder care leads to better outcomes in patients with cancer; Michael West has spent a career demonstrating empirical evidence of the importance of compassionate leadership in building and nurturing teams; and the likes of Amy Edmondson, and Google’s Project Aristotle, have shown that psychological safety is the most important condition we can create as leaders for a team to be high performing. I have found no better
28 AUTUMN 2023 Milestones WELLBEING
Dr Bob Klaber Consultant Paediatrician & Director of Strategy, Research & Innovation Imperial College Healthcare NHS Trust @BobKlaber
Kindness helps colleagues to perform their roles better
tool in creating that condition than a strong focus on kindness.
So if you have got to the bottom of this article, I think there are three things to spend a moment reflecting on:
1. Are there actions and behaviours that I can do more of, or practise getting better at, that might help to create better conditions for more inclusive, higher performing, equitable health and care teams, organisations and systems where I work?
One of these behaviours I am thinking about a lot at the moment is listening. How can I learn to be better at truly listening, what Nancy Kline would call ‘listening with fascination’? It feels like something that if we all got a little better at could lead to a very big change.
2. When I see unkind behaviours, what am I prepared to walk past and ignore?
This feels really tough and difficult, but unless we are really
active bystanders to the things that are going on around us, my worry is that very little will change. My experience of challenging behaviours is that the two-pronged intervention of (a) “that is not acceptable” and (b) “what is going on behind the scenes?” reveals that there is always something happening in the background for the person who is behaving in an unkind way. It might be self-esteem issues, it might be worries at home, or difficulties at work, or something else… but these are things that can be addressed with help and support, provided there is some insight and an acknowledgement of the impact of their behaviour.
3. What am I going to do to increase the focus on kindness and to reconnect myself and my colleagues with the real mission in healthcare?
The final action is one around leadership, and our role in reminding ourselves and the people around us what healthcare is really about. It doesn’t matter how early or how late you are in your career, or however junior or senior you may feel, all of us as people have a key influence every minute of every day on how the people around us feel. How we behave and act matters more than anything, so if you do one thing, make kindness your starting point and you will find that everything else will follow.
Find out more:
Kindness in healthcare
kindnessinhealthcare.world
A recording of Bob’s plenary session on Kindness in Healthcare at this year’s RCPCH Conference
www.youtube.com/ watch?v=LCth_684mjM

Milestones AUTUMN 2023 29 WELLBEING
Bob speaking at the RCPCH Conference in Glasgow this year
“There is always something happening in the background for the person who is behaving in an unkind way”
Dr Natasha Sauven Consultant Community Paediatrician and Paediatric Eating Disorders Lead Royal Cornwall Hospitals NHS Trust @NSauven
I became a paediatrician because for some reason I had always wanted to be one. My father was a surgeon and I was always desperate to work in the hospital. I remember loving occasionally accompanying my father to work in the hospital when he was doing a Christmas Day ward round and enjoying the excitement of it all. In hindsight, we were just fed lots of chocolates…! I always thought getting to ‘entertain’ kids for a living would be a great idea too! The decision stuck and I have not regretted it. I’ve been lucky to work with some amazing paediatricians through training who have kept me inspired.

My typical day starts with either a short bike or drive to work. One of the advantages of living in Cornwall is that the bike commute is enjoyable and a good way to unwind at the end of a day. I’m cheating somewhat these days with an e-bike though to make it quicker! I usually start with emails and coffee. My job plan is somewhat different as I work one day a week with community paediatrics doing child protection and working with unaccompanied asylum seekers and then for two days a week, I work with the eating disorders team within our local hospital and community team. Within eating disorders, we’ve managed to get much more integrated with CAMHS in the last few years, so my clinics are usually myself, a dietitian, and a specialist nurse but we’re trialling joint psychiatric clinics and joint clinics with the therapy team too. I’m also responsible for any ward patients with eating disorders so will liaise with the wards and review them.
If I’m on for community then it’s either seeing young people who have fled their home countries for health assessments and liaising within social care and education or being on call for child protection cases coming into the community.
A DAY IN THE LIFE
Alongside this I’m involved with YPHSIG (Young People’s Health Special Interest Group) and the Southwest Paediatric Mental Health Network (SWPMHN) and have recently taken on the mental health paediatric lead for our trust.

The most difficult part of my job is changing other professionals’ attitudes to my patient cohort and trying to advocate that my patients get the same attention as other children. Working with teenagers may not be every paediatrician’s dream but they deserve attention and respect and so often they fall through gaps.
The best part of the job is the eclecticness of it. I did my last year of paediatric training in Vancouver and did a fellowship in adolescent medicine, so it was my aim to advocate for young people’s health as a consultant. I love working with teenagers, they can be so funny and heartwarming, and I like the variety that I get in my job.
My most memorable time is spending a year working in a rural hospital in Makeni, Sierra Leone on a global health fellowship with RCPCH, something I had always wanted to do. I went with my fiancé (now husband) and it was one of the hardest years of our lives and the most fulfilling –certainly working with your partner 24/7 is memorable! I think working abroad, especially in resource-poor settings, gives you such a different picture of healthcare. It inspired me to do a master’s in public health and changed my outlook, hopefully for the better.
like to be a taxi driver for my three children aged 10, eight and five years! And when I’m not doing that, I’m usually trying to be in or by the sea, making the most of where we live in Cornwall!


KEEP IN TOUCH
30 AUTUMN 2023 Milestones @RCPCHTweets @RCPCH @RCPCH milestones@rcpch.ac.uk
When I finish work, I
Natasha loves living near the sea
“I love working with teenagers”
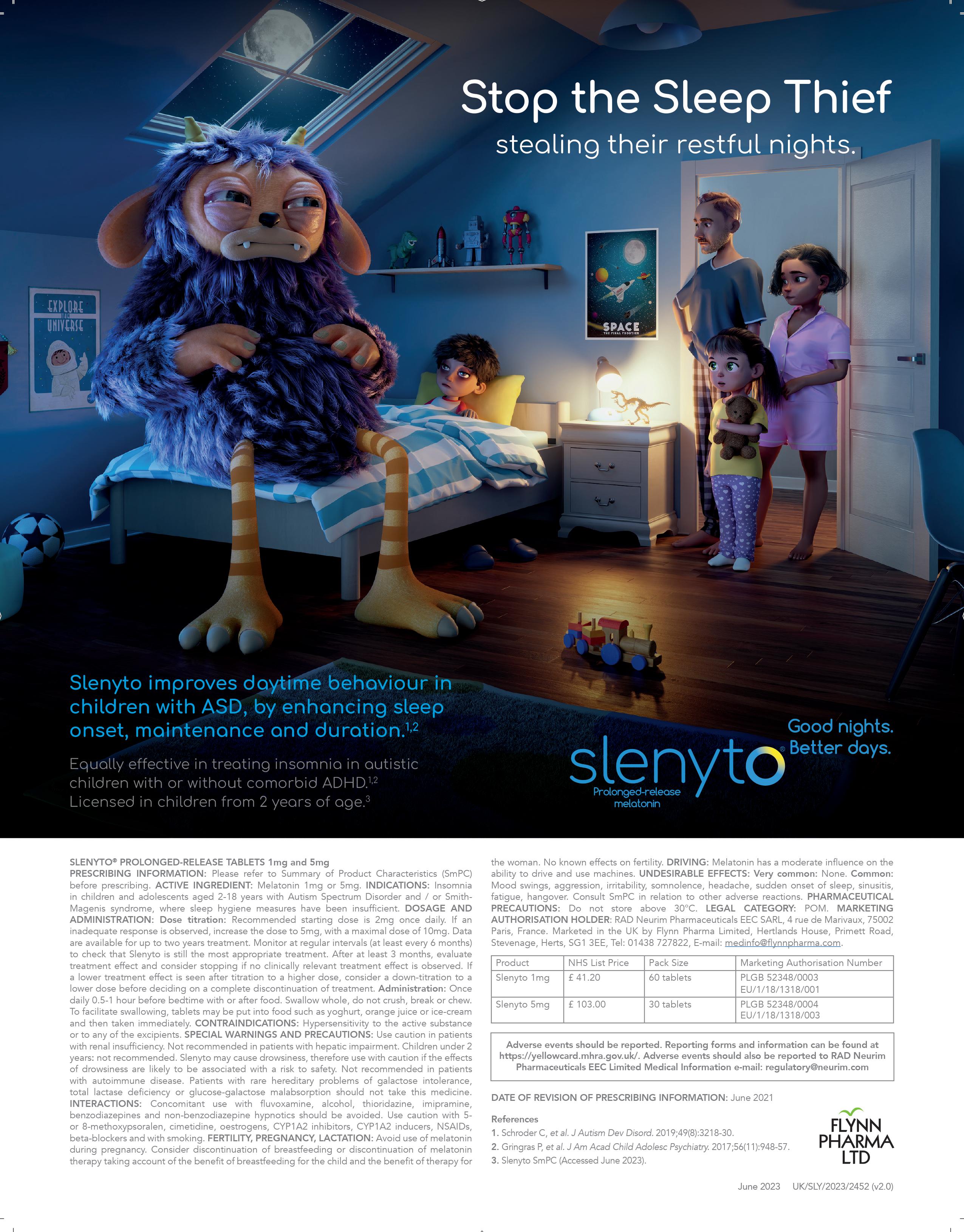






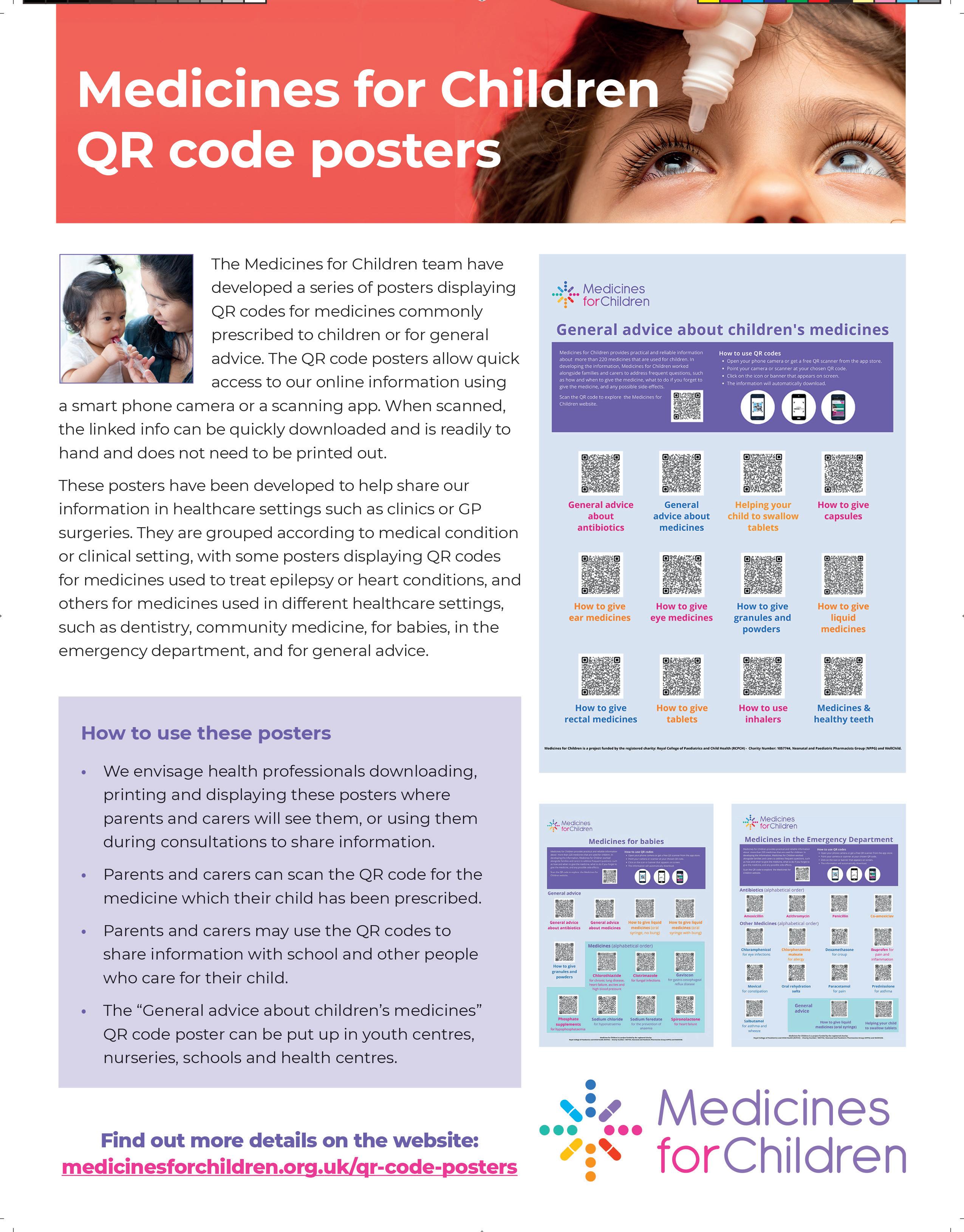













 Royal Devon University Hospital
RCPCH Chair of the Trainee Research Network @paedsdr
Royal Devon University Hospital
RCPCH Chair of the Trainee Research Network @paedsdr
 Dr Peter Davis Consultant Paediatric Intensivist Bristol Royal Hospital for Children Chair of BPSU Committee @BPSUtweet
Dr Peter Davis Consultant Paediatric Intensivist Bristol Royal Hospital for Children Chair of BPSU Committee @BPSUtweet










 Dr Karen Street Consultant Paediatrician Devon Partnership Trust Chair Eating Disorder Workstream MHLDN Provider Collaborative RCPCH Officer for Mental Health
Dr Karen Street Consultant Paediatrician Devon Partnership Trust Chair Eating Disorder Workstream MHLDN Provider Collaborative RCPCH Officer for Mental Health





 Editor-inChief
Editor-inChief



 Professor Steve Turner Consultant Paediatrician
Professor Steve Turner Consultant Paediatrician
 Royal Aberdeen Children’s Hospital
Royal Aberdeen Children’s Hospital






































 Dr David Tuthill Consultant Paediatrician Cardiff & Vale University Health Board
Dr David Tuthill Consultant Paediatrician Cardiff & Vale University Health Board
























 Dr Josephine
A. Quaynor ST3 Paediatric Trainee
Dr Josephine
A. Quaynor ST3 Paediatric Trainee

 by Simon Stephenson
by Simon Stephenson
 by Franco D’Alberton
Dr Gautam Kulkarni Consultant Paediatrician Circle Health London @geekulkarni
by Franco D’Alberton
Dr Gautam Kulkarni Consultant Paediatrician Circle Health London @geekulkarni
 Consultant Clinical Psychologist
Consultant Clinical Psychologist








 Paediatric Consultant, Somerset NHS Foundation Trust
Paediatric Consultant, Somerset NHS Foundation Trust















 Paediatric Registrar, Somerset NHS Foundation Trust @babydrclaire
Paediatric Registrar, Somerset NHS Foundation Trust @babydrclaire