MC

THIS THE REAL LIFE? Is this just fantasy?
How cool is Cosplay?


THIS THE REAL LIFE? Is this just fantasy?
How cool is Cosplay?
Dominic dresses up for more than fun – it’s changed his


MC Magazine team:





We ask when does a fear become a phobia? And what can you do about it?
As the festive season approaches we ask experts – is a low carb diet the gift that keeps on giving?
Managing Editor: Steve Murphy. Editor: Jackie Rankin.
Contributors: Diane Cooke, Jo Henwood.
Cover shot: ©BBC Page 18
AND
Photography: Joel Goodman, Dupe Creative Freepik.com, Steve Murphy, pixabay.com.
Design: Jo Hadfield.
Illustrations: Ella Byworth.
You can contact us at: communications@merseycare.nhs.uk


Data Protection Regulation (GDPR), is a European-wide law, which governs how organisations can collect, use and transfer personal data. It came into force on 25 May 2018 alongside the new Data Protection Act 2018. As a Foundation Trust, Mersey Care has a statutory requirement to develop and maintain a membership and it is necessary for us to process our members’ personal data to perform this task. Our members are drawn from the public, people who use our services or care for people who use our services and staff. We request and securely hold data on our members, which they provide when joining our membership. The data we hold on our members enables us to show that we are representative of the community we provide services for, to keep members updated through our quarterly MC Magazine via email or post and to invite all members to the Annual General Meeting. We also engage with all members advising when the election for governors will be taking place, giving members the opportunity to nominate themselves to become a governor and to vote in elections for the council of governors. Should you no longer wish to be a member of Mersey Care please email: membership@merseycare.nhs.uk with your details or call 0151 471 2303 asking that your details be removed.

We’ve been discussing how we mentally prepare for the ‘dark nights’ – some of us can’t wait to draw the curtains and put the fire on, others mourn outdoor living. We all spend a day or so talking about the ‘real‘ time and that we need to just forget the clock change and accept that the time is now.
How that time is spent can make a difference to our wellbeing as we move into autumn. Brisk walks are always a good option as is food cooked over fire pits, and movie nights. But this issue also shows how being creative is as good for you as a dose of vitamin D.
We belly laughed at the Acting Up drama group. And we admired a group of unlikely ballet dancers.
Cosplay – dressing up as comic characters – is pure unadulterated fun – we hear from a psychologist about how it can boost confidence.
As we head for the party season how do you keep your healthy eating on track? Experts talk about the new thinking on carbs.


Do soaps really portray dementia as it is? We talk those who think not – and find out why getting support early can make a difference.
A couple whose lives were turned upside down by a brain injury talk frankly about life and love in difficult times.
Forget the clock and make the most of your time this autumn.
The MC editorial team.
A psychologist tells us how cosplay can boost confidence. How time is spent can make a difference to our wellbeing...




My psychosis has given me an insight that simply wouldn’t be there had I not have gone through this experience.

When actor David Harewood shared his experiences of psychosis on Twitter 30 years after he was sectioned, more than 35,000 people told of their own battles.
He was just 23 when he was sectioned after a friend found him with a corkscrew punctured copy of a Shakespeare script. He has since made a BBC film to help him understand what happened back then and debunk myths about a condition that affects one per cent of 14 to 25 year olds in the UK.
Ronnie Parker is one of them. He told his story to MC Magazine (see page 6) in the hope that young people and their families will get help and have hope.
David Harewood’s psychosis began as a 23 year old acting student in his final year at RADA “The final days at drama school brought the real world in – I was being offered jobs but I didn’t feel in control, I was totally alone and unhappy. I can remember deciding that it was best not to look at reviews as I would begin to question and also doubt myself. That’s not the time to start smoking weed and drinking but that’s what I did and that’s when the breakdown started.”
26 year old Ronnie tells a similar story. He was in his last year of university when he became unwell after using cannabis as a form of escapism and stress relief.
“I spent a lot of time alone and began thinking people were talking about me. I felt threatened – that was the starting point, the trigger.”
Both men were aware that something was wrong. David Harewood recalled in the programme: “My sleep pattern wasn’t what it should be, I was wandering the streets, I’d black out and come round miles from home. I knew I wasn’t well but I felt if I could control what I was feeling I could manage it. But I was mistaken and I ended up in a pretty dangerous place.
A combination of isolation and cannabis also kick started the psychosis that led to Ronnie spending time in Clock View Hospital.
Consultant psychologist Dr John Stevens says this is typical of someone experiencing a psychotic episode.
“Psychosis often begins in response to being under high stress, and we can be more vulnerable based on difficult experiences we have been through earlier in life. Psychosis can creep up at these times, with people starting to question the reality of what’s going on around them, often making them feel more paranoid. It can take over and affect how easy it is to engage with the important aspects of life.“
Both men say they’re stronger for the experience.
David Harewood says: “My psychosis has given me an insight that simply wouldn’t be there had I not have gone through this experience so whilst I’m not exactly glad it happened I’m grateful for what it has given me.”
Ronnie Parker says his experience has made him more confident. If you go through something like this you’re no longer easily fazed, you develop the strength to face whatever comes.”
Dr Stevens says telling someone and gaining support is essential for recovery.
“Getting help early with psychosis really helps with recovery. Your GP can arrange an assessment with the Early Intervention in Psychosis Team, who will work with you to put a plan in place. Specialist practitioners and psychologists will offer support to help you make sense of the situation and advise on medications to reduce symptoms. As these stories show, with the right support people can move on with their lives after psychosis.
• Hallucinations
• Seeing, hearing, tasting or smelling things others don’t
• Confused beliefs, for example that you’re in danger, that you’re someone very important
• Feeling others can access your thoughts
• Finding it hard to concentrate or keep a train of thought
• More snappy and argumentative with family and friends
• Not socialising, avoiding college or work
• Thinking things are linked where there is no evidence.
• Talk to friends and family about what is happening
• Get regular sleep
• Do things you enjoy and relax you
• Cut out substances that might impact eg. drugs, caffeine, alcohol
• Get help with the things that are stressful
• Seek support from your local Early Intervention in Psychosis team.
• Don’t panic
• Go at their pace
• Encourage the person to be open
• But don’t get frustrated when they withdraw or are confrontational
• Talk about it… talk about it more.
RESOURCES
voicecollective.co.uk hearing-voices.org mind.org.uk rethink.org
David Harewood starred in the BBC drama ‘The Night Manager.’ He is currently appearing in the American sci-fi series ‘Supergirl’. 5

I was in the final year of a physics degree at Sussex University when my psychosis began. It was drug induced.
I’d smoked cannabis for a while – it helped with stress but I did it mainly because I enjoyed the feeling of escape. I spent a lot of time alone and began thinking people were talking about me. There was an incident on a bus with a group of lads while I was high. I felt threatened – that was the starting point, the trigger.
I became delusional, seeing everyone as a potential threat. I didn’t feel safe and went back home, but things got much worse.
I believed I had an insight into what the world was really like, another layer of existence that held danger for my family. If I heard something on TV I’d be convinced they were speaking directly to me. It would feel like thoughts would pop up out of no where that I didn’t particularly like or agree with. I was terrified my family would die, that if I died they’d be safer.
One day I ran out of the house over garden fences and climbed into a car. The driver called an ambulance and I was admitted to hospital.
Each day you’re a little bit more like how you were before the psychosis.
The medication and meditation helped, but the anxiety of having to be with people was overwhelming. I’d have pins and needles throughout my body. Then I went along to the early intervention in psychosis support group. The facilitators helped me put things in perspective when my thoughts became irrational. They’d explain why I was thinking like that. I’m still friends with people from the group.
As time went by the thoughts became less frequent and bothered me less – you realise that each day you’re a little bit more like how you were before the psychosis.
One of the things I found most helpful was writing down my thoughts. It can be anything, any epiphanies you have, any observation or anything interesting that happened that day. Once it’s written down it doesn’t play on your mind. It helps you move forward with your thoughts.
At the height of my illness it helped to think that every day you wake up is like a reset button. I’ve come off medication and lost the weight I gained while I was on it.
I was determined to do the final year of my degree. I was offered a transfer but I’d re-sat an A level to get there so I wanted to finish where I’d started. I was excited – but the anxiety isn’t there any more. I passed and am about to move to start a dream job working in the aerospace industry.
If anything my experience has helped me understand, and made me more confident. If you go through something like this you’re no longer easily fazed, you develop the strength to face whatever comes.”

Frank spent a lifetime on drugs. Now he is a dancer. MC magazine looks at how creative therapy changes people’s lives.
By Jo Henwood

Paul is on a journey of recovery. He first drank alcohol when he was eight, smoked a joint at 13, almost died at 30 and last spring he met the Queen.
Aborn entertainer who would ‘get into fights’ at school, Paul Bayes Kitcher’s life changed when, aged 11, he secured a place at the Royal Ballet School.
Travelling from his native Yorkshire to train in Surrey alongside former Strictly Come Dancing judge Darcey Bussell and the real-life Billy Elliot (the Royal Ballet’s Philip Mosley), Paul knew his life would never be the same again.
But while his dance career blossomed, his relationship with drink and drugs was having the opposite effect.
Nevertheless, Paul secured a position as soloist with the Birmingham Royal Ballet.
“I worked hard and I played hard,” he said. “Looking back, I don’t know how I did it.
“By 30, when I retired as a performer, my diet was basically crack and vodka. I had no structure and I was spiralling downwards.”
Paul’s mum stepped in and convinced him to try rehab, but at the end of the first programme he started to use heroine.
He recalls:“My veins collapsed, I weighed 8½ stone, I didn’t wash for weeks, I was a tramp. I was dying before I realised I had to stop.”
Through further rehab and recovery groups Paul started exploring his own journey and realised his dance and choreography skills could help others.
Fallen Angels Dance Theatre, founded in 2011, now has recovery groups working regularly in Liverpool, Chester and Leigh and they recently embarked on a project with residents at HMP Berwyn in Wrexham.

Paul has given TED Talks, worked with internationally renowned choreographers and featured in a BBC documentary. Last May, his ‘angels’ were invited to perform for Her Majesty the Queen and The Duchess of Sussex at the opening of Storyhouse in Chester.
Reflecting on the success of his dance therapy, Paul said:“One of the new members of the group was recently told by doctors that she would never get better. This week, she chose to come to Fallen Angels rather than attend a prescribed therapy session. She says her head is clearer, she has had no mood swings and it just makes her feel better. How does that happen?”
• To find out more about Fallen Angels Dance Theatre email: claire@fallenangelsdancetheatre.co.uk Twitter: @FallenAngelsDT

I THOUGHT ‘YOU’RE NOT GETTING ME IN A LEOTARD...’
He had spent a lifetime on drugs and in and out of institutions because of his mental health.
“Ketamine, amphetamines, MDMA, marijuana, LSD, cocaine, magic mushrooms in the rainforests of Australia – you name it, I have taken it,” said Frank.
Now he considers himself a dancer and describes Fallen Angels Dance Theatre as his salvation.
“I know so many people who have died because of drug use. This man (Paul) saved my life. When I met him he stopped the clock.”
Obviously well-educated and informed, Frank talks proudly of his almost perfect pass rate for a foundation course in art
before beginning a bachelors degree at what is now Middlesex University London. He tells me he has exhibited in the capital and danced at the Tate Gallery in Liverpool, with Mondrian and Lowry as his backdrop.
It was this love of art that first brought him to Fallen Angels.
“I had no plans to dance,” said Frank. “I thought: ‘You’re not getting me in a leotard mate,’” he laughs, looking at Paul.
“So I sat at the side and drew the dancers.
“Then someone suggested I tear my drawings off the pad and give them to each of the dancers. I did and the next thing I knew I had my shoes off and I was dancing.”
Three years ago, Frank needed a support worker to go anywhere.
Last year Frank performed in front of The Queen and Meghan Markle when Her Majesty opened Storyhouse theatre, cinema and library complex in Chester.
He said: “Paul has taken me out of nowhere and put me in a place of recognition and respectability. I have been discharged from all psychiatric services and I am resolved to stay off drugs.
“Fallen Angels has turned some drug addict from a madhouse situation, in some ghetto, into a theatre dancer, a film actor and performer. It has been a huge part of my recovery.”



Editor Jackie Rankin takes a seat at a show where art mimics life – and your cheeks ache from laughing.
The stage is set. The scene is a party. The ‘cast’ has only seconds to come up with a character. You feel nervous for them.
Slightly the worse for wear, Dolores claims infatuation with the chap next to her – he seems fine with it. The DJ and his security sidekick are concerned there’ll be trouble and start planning their next move. Angry Angela has just seen her son in law with his best friend’s wife. She’s not best pleased.

It’s all an act – this is improvisation at its best. But we’re in stitches, and so are the cast members. One man is laughing so much he’s almost crying. They interact so seamlessly it’s hard to believe this group met for the first time only a month earlier –and that they’re not real actors.
This is the last session of a four week drama course at Bootle Life Rooms. The curtain
This is improvisation at its best... One man is laughing so much he’s almost crying.
must fall, there’s a sense of final night sadness, but facilitator Mark Bell reminds the cast that there are more times like this ahead and to stay in touch.
Bell, himself a trained actor and now recovery learning facilitator for Mersey Care’s Life Rooms, devised the Acting Up course with volunteers.
“It takes you back to being a kid, when you had no inhibitions and you were at your most confident. There’s no getting it wrong here.”
He’s vital to the group, always there, ready to prompt and step in to help. There’s a mutual respect.
I’m invited to the debriefing. Mark encourages people to give themselves a pat on the back, it’s a soothing technique often used with people who have mental health issues – today it’s a true ‘well done.’
People share their thoughts on what the course has given them. June used to feel the need to apologise constantly.“My life has been so serious from childhood but you can let that go here, I’ve learned a lot I can use in my everyday life, in the way I react. That you don’t always have to say sorry.”
Carol had already experienced a creative writing group and came to learn how to develop characters.“If people want to open up in a scene they can…and they do. Mark is brilliant; he draws out ideas, gives you the hook and lets you explore it. It’s like food for thought, you don’t need the ideas to already be there, he brings them out, teases out lines.”
• on Life Rooms go to merseycare.nhs.uk
It takes you back to being a kid, when you had no inhibitions and you were at your most confident. There’s no getting it wrong here.

What’s life like after a diagnosis of dementia? Plans put on hold, fear for the future? Or, as Jill Pendleton suggests, a support network that is bringing untold new experiences and friendships.
Dementia lead for Mersey Care’s service in Liverpool Jill doesn’t underestimate the devastating impact of finding out that memory loss is much more than simple ageing.
“People have usually suspected but it’s still a bolt from the blue. It’s the thing most
people are frightened of. We don’t pretend nothing will change, that everything is going to be fine, but we do try to offer a future that can be hopeful rather than despair.“
Psychologist Dr Sarah Butchard says outlook can prevent the low mood that comes with a diagnosis becoming depression.
People have usually suspected but it’s still a bolt from the blue. It’s the thing most people are frightened of.
“There are links between dementia and mood. Dementia causes biological changes to your body but it also changes how you see the world. It’s natural to feel low when things change, but it’s not inevitable that it turns into depression.

Dr Sarah Butchard

How you deal with the news can also make a difference. You could stop going out, maybe start to feel you don’t have a role, a bit worthless –or you can say ‘things may happen while I’m out but I’m going anyway’.
“Families can help too. It’s natural to want to keep your loved one safe but restricting someone can make them feel worse. Take a Dementia Friends awareness course, ask us for a card which the person can carry with them explaining the situation.”
Jill Pendleton says it’s often to do with public perception and embarrassment at faltering before friends and family.
“Television may try to give an insight but it’s far from reality. Soaps have tried to present the issue sensitively but because the timescale is condensed, the characters with dementia appear to change rapidly, like falling off a cliff! People think that will happen to them and they get scared.
“It is a progressive condition but the changes are often very slow – a person may have many years of full and active life ahead of them – we don’t want
If you’ve been diagnosed with dementia, remember you’re still you, even though you have problems with memory, concentration and planning. Everyone experiences dementia differently, focusing on the things you can still do and enjoy will help you to stay positive
Find out about dementia-specific services near you from Alzheimer’s Society online directory Dementia Connect. Age UK provide a range of services and local support.
people waiting for the next symptom or things to go wrong when they could be having some good times as well.
Getting this early help will let you see there is life after dementia.
“Evidence suggests that having structure to your week helps,” says Jill.“You may have to adapt over time but use any support that’s offered to find out more. Our support groups offer so much and no-one judges you, they’ve been there, they know how it feels, you can come as you are.
In Liverpool staff raise funds to take groups on coach trips and days out.
“It can be reassuring knowing you’re with people who know how difficult it can be but uplifting to have some normality… and fun,” says Jill.
“People don’t want to be constantly talking about their condition, but may appreciate having professionals on hand who can answer questions and talk things through. Everyone who joins our post diagnostic support groups knows pretty soon that we’ll be with them long term.
Join an online forum, such as Alzheimer’s Society Talking Point. Online forums are a good way to share your experiences of living with dementia and advice on how to continue living independently.
Keeping in touch with people and engaging in social activities is good for your confidence and mental wellbeing. If you have someone who helps care for you, an active social life is good for them, too.
Many communities are now dementiafriendly. Join a local dementia-friendly
Peer support really makes a difference, says Jill.“There’s such a lot of informal support and real friendships. The group meets every Saturday at Sainsbury’s for breakfast and members have their own What’s app group.
That’s how it’s meant to be. People are giving of themselves – it’s their life. Friends they have had all their lives may fall away but these new friendships are so strong.
Jill says getting post diagnostic support is the best thing someone newly diagnosed can do.
“Your worst fear has just been confirmed, your world has been turned upside down. The two things you need most are good information and being around people who have been in your position and truly know what it feels like.
“We never lose sight of how challenging it can be and we can’t map out a path for you but getting this early help will let you see there is life after dementia.”
We do try to offer a future that can be hope rather than despair.
group, perhaps at a memory café or community centre.
Mersey Care services include specialist assessment, medication, post diagnostic support, peer support groups, courses for carers, and therapies, including those recommended by the National Institute for Health and Care Excellence. FIND OUT MORE Dementia UK - dementiauk.org NHS UK - nhs.uk
Sources: dementiauk/nhsuk
- healthwatch.co.uk Alzheimers UK - alzheimers.org.uk
An ex nurse, Roy Foden loved fell walking and had an active social life. But after his dementia diagnosis friends began slowly drifting away.

Not today – Roy (above right) says any one of 50 people from his local dementia support group would come to his aid if he called.
He plays an active role – when MC Magazine spoke to him, he and fellow member and close friend Stan Limbert had been to visit a dementia friendly care home. They give regular talks to GPs and medical students.
The pair also talk to people at post diagnostic groups run at Mossley Hill hospital for people who have recently been diagnosed with the condition.
Stan, 75, has early onset dementia. He agrees with Roy, “We tell people we’re all still ourselves and we’re here to show them there’s still plenty of life to be had.”
The duo run a coffee afternoon in a church hall. Old Liverpool films are followed by Roy’s famous nostalgia quiz, a picture or a music quiz. People enjoy answering questions about the films – it’s memory evoking,” says Roy.
“It’s an isolating disease but I don’t ever want to sit around looking at a wall or popping pills. I want to do all I can help remove stigma, to make things better for the next generation and their families.”
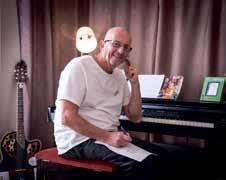
Although he was initially in shock after his dementia diagnosis four years ago Paul, 67, decided he was enjoying what he calls his ‘bohemian’ lifestyle to devote too much time to his condition.
It’s that mind set that gives him the drive to play his instruments – he was a regular on the Liverpool music scene in the 70 and 80s –and enjoy family life and his beloved garden.
“I’ve got so much going on that I hardly think about it. I have dark days and sometimes consider my own mortality – but don’t we all?
Paul can remember every line of every Beatles song – but he can’t recall where he’s put his car keys. Not that it bothers him.
He does take some practical steps to stay well. “I did some research on diet – now I don’t eat meat during the week, and I try to stay away from conflict and negativity.”
We
have some good times together.
Paul is a regular at the Mossley Hill support group and has just completed his Dementia Friends trainer course. “We have some good times together, we go into the city centre and listen to bands – we can be singing all afternoon!”
And the dementia? “It’s just another part of me – one of those things in life you have to deal with. It is devastating but what follows depends on which path you take. I think the people who go downhill quickly do that because they let that part of their life take over their whole life. If you organise yourself, go right away and get help from a support group you’ll get back to normal.”
Paul’s latest gig is the launch of a new dementia hub in Liverpool later this year. He’s looking forward to performing again. “As the song goes” he says, ‘It’s coming back to life…’”

If you organise yourself, go right away and get help from a support group you’ll get back to normal.
Heather’s had to put up with a lot. The brain injury has changed me.

How do you cope after a life changing injury? Andy and Heather Davies draw on their shared emotional bonds, tenacity…and poetry.
ANDY:
Iwas a mental health nurse but I haven’t worked, or even gone out much since my brain injury. I’d have been sectioned without Heather. She’s had to put up with a lot. The brain injury has changed me.
When we met everything was going well. I’d overcome depression and trauma from things that happened in my childhood. I left my job as a support worker to become a nurse. My life was fulfilled.
Heather and I met through work – I always say she chased me! We got married at Liverpool Football Club, life was good.
No-one knew at first that the accident I had at work had caused a brain injury; we were told it was concussion. I started hearing voices, I wouldn’t tell anyone but Heather knew something was wrong.

I put on four stone and found there was a tumour on my pituitary gland.
I became depressed. I pushed her out, accused her of having affairs, but she knew it wasn’t me talking.

The
I write down my thoughts – they come out as poetry. I’ve no idea why but it stops me ruminating. Heather can tell when it’s happening, she tells me to work on some poetry. It’s because of her and the clinical team that I’m where I am – I work hard to get better for them.
My poetry and the book take away the ball of knots in my stomach. I used to say to my patients ‘write down your problems it really helps.’ I didn’t know if it was really true, but I do now.
It’s been a hard journey but Heather and I are closer than ever. The rapport we have is incredible; she’s my best friend, my soul mate. The brain injury has robbed everything but I still have her and my poetry…
We’re very close, so I knew something was wrong with Andy after the accident. For a long time no-one knew the full story but me, not many people know even now. He was scared to admit he was psychotic. He’s a nurse, so he knew how bad things could become. He was hearing voices that told him he was rubbish. He thought people could tell just by looking at him. In the first year he was suicidal. I took six months off to get his medications right –I didn’t want to leave him. Even now going out is a challenge. We’ve just been on a family camping trip. That was a massive achievement. I’m proud of him.
In the early days he used to get upset and apologise. He’d tell me to find someone else – I’d just say I didn’t want anyone else.
His writing has been so good for his recovery. And it’s good you know! I can see the difference in him when he writes; I have to convince him that it’s good.
We’re both tenacious – we don’t give up. People thought he’d only be as good as he was at the beginning. We’re proving them wrong.
His writing has been so good for his recovery.



Costume play – or Cosplay as it’s known – is a combination of costume and play. It’s becoming more and more popular with conventions like Comic Con dedicated to the art.
But alongside the fun of creating imaginative outfits and dressing up there are significant benefits to wellbeing. Diane Cooke finds out more.
When Dominic Bassnett wears the dark robes of Games of Thrones’ hero Jon Snow or the gargoyle-esque make-up of Batman’s nemesis, The Joker, he’s no longer someone crippled by anxiety.
Likewise when Dominic, 32, lead singer of Liverpool indie band The Jackobins, dresses and performs as one of his musical heroes, he forgets himself and lives in the moment.
“I spend hours on the internet sourcing costumes. I like to get them absolutely right. So if I’m dressing as one of The Beatles, I have to get the right style of wig, cut of jacket, shades, or it doesn’t feel authentic. It’s a kind of escapism. I feel less vulnerable and negative when I become that character.”
The early 90s saw the rise of Cosplay into popular culture, although it probably originated initially in Japan. It is the practice of portraying a fictional character and, at times, completely identifying as that character while in costume.


By Diane Cooke
Programmes like Dr Who appeal to our inner superhero. Costumes are cool personified. We talk to people who take it a step further. It’s a kind of escapism. I feel less vulnerable and negative when I become that character.

It seems there are many motivations for donning Lycra or a cape. It could be love of a character, enjoying the attention of being in an elaborate costume, or the appreciation from peers of creating something complex and unique.
Dominic has suffered from panic attacks while performing on stage. He also struggled for years with his sexuality – he’s bisexual. Cosplaying Freddie Mercury helped him cope with that period of his life.“I put a lot of my problems down to repressed sexuality, but being Freddie allowed me to be more camp and flamboyant. It helped a lot.”
Fans view Cosplay as a unique form of performance art. Conventions are regularly held at venues around the world. This massive subculture has made it cool to be geek.
For 19 year old student Alice it’s being at a gathering that’s full of fun, colour and friendly people.
“It’s not hiding in plain sight; it’s becoming a character for a day and enjoying the empowerment that comes from being that person.”
And the geek label?“Science fiction and fantasy fans have got over the old judgement that they are nerds. Being nerdy or geeky is fine. It’s neither a help nor a hindrance. Cosplay is a welcoming world.”
Obsession and happy infatuation vary from Smurfettes making a point about on screen equality representation or Stormtroopers making… well no point at all really, save perhaps about plans for the Battle of Yavin.
Being nerdy or geeky is fine. It’s neither a help nor a hindrance. Cosplay is a welcoming world.
“It’s extremely levelling” says Alice. “The quietest, shyest, most introspective of individuals will mix with the most outgoing, demonstrative and flamboyant characters.”

When they dress up as their superheroes and put on a cape or a tutu, they become super-confident and it helps them to express themselves.
Mersey Care consultant general adult psychiatrist Dr Tomos Williams can easily see why people are attracted to it.
“Superheroes have strong characters that we like to identify with, but they also have complex back stories that someone may resonate with personally.
“If you think about Batman, who is an orphan, and X-Men characters, who have met with a lot of hostility because of their mutant powers, you understand why they are relatable.
“The Joker is a complex character, an anti-hero, but he has a lot of traits people identify with. He’s naughty, but he’s playful and humorous – maybe that provides relief from a society that expects us to always conform.
“There’s something to be said for identifying with a flawed relatable character who can overcome adversity and rise to a position of power or get more control so they can defend themselves and others in unfortunate positions.”
There can be negatives – say if someone identifies too closely with the character and spends more time in costume than as themselves. Girls have been known to develop body image problems in order to emulate the almost impossible body shapes.
“When people see it as an artistic medium and are able to express their creativity that’s a positive aspect and therapeutic.” Says Dr Williams.“It’s the same feeling children get when they


dress up as their superheroes and put on a cape or a tutu. They become super confident and it helps them to express themselves.”
Dressing up it seems, isn’t just for the kids...


Superheroes have strong characters that we like to identify with, but they also have complex back stories that someone may resonate with personally.

Who
12 is on its way and will be returning to BBC One in early 2020
You know the feeling – your head hurts, throat’s sore, limbs ache. Is this ever going to go away – do you need an antibiotic?
It’s easy to blame health professionals as cost cutting when they suggest pain relief and sitting it out. It’s also a worry – how long do you leave an illness to run its course?
Yet research proves that antibiotics are not only ineffective for most common illnesses, they can do us harm and leave us vulnerable when we most need them.
The Royal College of GPs has urged parents to trust their health professional if they advise that antibiotics are not needed for common respiratory tract infections such as coughs, colds or sore throats. Researchers looking at 250,000 pre-school children found that even two antibiotic courses a year made further courses 30 per cent more likely to fail.
Pharmacist Emma Wilson leads a programme within Mersey Care making sure prescribers and patients are aware of the effects of inappropriate antibiotic use.
“Antimicrobial resistance as it’s known, can cause serious problems. If someone develops an infection after surgery, or during chemotherapy, we need to be sure their antibiotics will work.
A routine operation may even be cancelled if we do not have an effective antibiotic available. Not completing a prescribed course may not kill the infection entirely, so it returns and they need more antibiotics, putting them at even more risk.”
But how do we tell the difference? Especially since we’re being asked to look for symptoms of sepsis?
Emma’s advice:“Most common symptoms such as a headache, sore throat, aching, a fever in children, are linked to viral infections. It can be difficult to distinguish early on as viruses can have quite nasty symptoms. But the worst is usually over in a few days and although some symptoms can linger for a couple of weeks you should start to improve. Bacterial infections tend to have additional symptoms and your healthcare professional will examine you for these.
“Rest, painkillers and plenty of fluids is the best care for a virus. I’d say listen and watch over a few days. If you’re worried seek help from a health professional and be ready to take their advice.”
Antimicrobial resistance as it’s known, can cause serious problems.


If the sight of a cobweb makes you shiver you’re not alone. But when does a fear become a phobia? And can it be cured?
We talk to a cognitive behavioural therapist and hear about a phobia that’s more common than you’d think.
Phobias of dogs, insects, flying, even vomiting are very common but few people seek treatment.
“People generally manage their phobias on their own by just avoiding the triggers, but sometimes this can make life quite difficult” says Cognitive Behavioural Therapist Lee-Anne Widnall.

“If someone fears their situation so much their threat system goes into fight or flight mode.” says Lee-Anne.“In the days when we had to fend off wild animals it was essential to stay alive. In the modern world our brains have to deal with so much more, coping with complex social situations, being

concerned we have enough money or even that we’re wearing the right clothes.
“People ask ‘why do I feel so anxious”? We explain that our threat system is the most primitive part of our brain. When we experience a perceived danger our brain sends adrenaline pumping round the body to prepare for fight or flight. This diverts oxygen from your head to your legs so they’re ready to run – that’s why you feel dizzy. Your heart beats faster and so that you are lighter to run away your bladder and bowel muscles relax.
“The good news is your threat system can’t stay like that forever. If you’re gradually exposed to the situation your brain will learn that the danger isn’t real. With spiders we might begin with photographs and work up to a dead spider and finally a live one.”
Exposure isn’t the whole answer with some phobias, for example misophonia – a phobia of unnecessary sounds in which people can become so badly affected they can react angrily – the fight or flight mode.



“We wouldn’t usually encourage avoidance to treat a phobia, but with misophonia the treatment has to be more individualised as there is currently a lack of evidence that the threat system can be turned off, in other words we don’t know yet if people can habituate to all the varied noises that life throws up. What often works is a combination of exposure, mindfulness and noise blocking.”(See Rob’s story on page 24.)
HOW CAN COGNITIVE BEHAVIOURAL THERAPY HELP?
“This sort of therapy teaches people to be their own therapists. To reassure them that they’re in control.“We would never make someone do anything they don’t want to –we know what works and we’ll advise you, but it’s led by you. It is anxiety provoking but in a managed way to help your brain adjust and realise the danger isn’t real.”
CONTINUED OVER.
Talk Liverpool is a free NHS talking therapy service.
You can refer yourself online by visiting talkliverpool.nhs.uk or calling 0151 228 2300, alternatively you can be referred by your GP or another health professional.
Last year hearing a ticking clock would make Rob Johnson’s heart race and his palms sweat. Someone sniffing, chewing, or even breathing heavily all sent the 36 year old IT worker into a state of panic.
He’s not alone. The Misophonia support group Facebook page has almost 20,000 members. Translated literally “hatred of sound,” negative emotions, thoughts, and physical reactions are triggered by specific sounds.
It caused problems at work, where he’d have to leave his desk and sit in the toilet cubicle until he calmed down. At home his marriage was coming under pressure from his inability to tolerate noises his wife made when she chewed food, and clicking noises as she slept.
“It made me very down – I knew it was affecting our relationship and that it was my problem. You can’t complain to someone about something they do in their sleep, but I’d tried so many ear plugs and none worked.”
Rob, a gently spoken man, says he didn’t become aggressive with people but he would slam doors out of frustration.
A phobia is an overwhelming and debilitating fear of an object, place, situation, feeling or animal. Phobias are more pronounced than fears. They develop when a person has an exaggerated or unrealistic sense of danger about a situation or object.
Symptoms may include:
• unsteadiness, dizziness and light headedness
• nausea
• sweating
• increased heart rate or palpitations
• shortness of breath
“Work was hard. Even someone clicking a pen would make my heart race and my palms sweaty – I’d have to ask them to stop but I wondered what they thought of me. One colleague had long nails which she’d use to type – that was a massive trigger.”
Rob can recall incidents as far back as his school days.“A boy who sat next to me would breathe heavily. It made me very anxious but I couldn’t get up and leave the classroom, nor could I tell people the reason for my panic. I kept it to myself for years before getting help.”
Rob was referred for talking therapies by his GP. “I had a lot of confidence in Lee-Anne from the first session. It felt good to have someone to talk openly with, to say how I felt without judgement. She reassured me that the fight or flight feeling would plateau, that I could stay in the situation, the threat would go away. We worked on developing mindfulness and meditation techniques to help me tolerate the noise and stay with it. It takes a lot of practice; I still have triggers and it is unpleasant, but thanks to the therapy the phobia no longer stops me doing things and going places.”
• trembling or shaking
• an upset stomach.
Almost all phobias can be successfully treated and cured.
Ask a GP for help if you have a phobia. They may refer you to a specialist with expertise in behavioural therapy, such as a psychologist.
Find out more at nhs.uk/conditions/phobias


The summer before your child goes off to university is ridden with tension.
Revision, exams, waiting for results, conditional offers going through clearing, packing…and then the journey to their new home But the weeks and months after you drop off your child at a university campus is perhaps the toughest time of all. Of course, you’re proud of their achievements and you want them to be independent – but it’s tough letting go.
Glynis Kelly, child protection officer at Cornwall College likens the feeling of loss many parents feel to grieving. There’s also ‘unfamiliar tensions as family members learn new ways of interacting with each other.’ she told the Independent.
It can start as soon as you know they’re leaving, or when you say goodbye at halls, says Celia Dodd, author of The Empty Nest: How to Survive and Stay Close to Your Adult Child.“For some, it’s later still – perhaps when they see a mum with her child in the supermarket or they walk past a primary school.”
The charity Family Lives has dedicated advice pages for what it describes as a stressful time. But Kelly suggests focusing on the positive – no more waiting up into the early hours – and the house stays tidy!



• Be the one who stays in contact
• Visit them. But be flexible and accept that things may change
• Ask them how they are
• Give them space
• Offer practical help
• Remember that studying can feel like a job – they may be under pressure
• Find other things to fill your time. familylives.org.uk

Changes in seasons can put people more at risk of asthma related conditions. Specialist nurse practitioner Tanya Downes gives advice on how to stay well and where to get help:

If you feel that your symptoms are not controlled or that the inhalers are not effective, it may be that the technique being used isn’t correct.
You should always take your inhalers and tablets as directed by the person who prescribed them for you.
Asthma UK have step by step instructions on how to take the different types of inhalers, dry powder and pressurised inhalers, with or without a spacer device.
Give it time – you may have to use your inhaler continually for up to three weeks before you see an improvement. Do always attend your review appointment.
If you’ve used the correct technique but your symptoms are not controlled, contact your GP practice and ask for a medication or asthma review. It could be that you need a change in medication or a second inhaler. Your practice nurse and GP have your full history and can provide the best management.
If you are using your inhaler more but your symptoms get worse and your GP practice is not open seek medical help from NHS111 or a walk in centre. If you or your child are having difficulty in breathing or cannot speak in full sentences you should call 999.
Asthma UK: asthma.org.uk

By Diane Cooke
As we go headlong into the party season food and drink overload is a temptation. How do we get through to January unscathed? Could low carbs be our saviour? We ask two experts.
When it comes to losing weight and keeping well, low carb seems to be the new diet on the block.
From bodybuilders to celebrities like Halle Berry and Kim Kardashian, #keto – short for ketogenic – is the buzz word.
Keto is a low-carb, high-fat diet.
Endless studies are showing how it helps improve your weight and your health. Research suggests it
may also have benefits against diabetes, cancer, epilepsy and Alzheimer’s disease.
It involves drastically reducing carbohydrate intake (in some cases as little as 20g a day, although a more moderate version is 50g a day) and replacing it with fat.
The reduction in carbs puts your body into a metabolic state called ketosis. When this happens, your
Low carb diets have become particularly relevant to brain health.

body becomes efficient at burning fat for energy. It also turns fat into ketones in the liver, which can supply energy for the brain.
Ketogenic diets can cause massive reductions in blood sugar and insulin requirements. This, along with the increased ketones, has numerous health benefits.
Warrington GP, Dr Joanne McCormack, who writes the blog fatismyfriend. co.uk, is an advocate of low carb diets, particularly for people with diabetes. She says: “As medical students we were taught that a balanced diet was all anyone could do to be in good health. I’ve since learned about a new, different way of eating which involves eating real, nutrient dense, unprocessed food.
“I was very sceptical at first, I gave up all sugary foods, but I still ate toast, pasta, rice and had milk in my coffee. As I got stricter I lost weight and felt amazing. I realised that it’s much more complicated than calories in and out. We need to eat healthy fat such as mackerel, salmon, olives, avocados, nuts, eggs.”
What’s more, she says some psychiatrists are recommending this way of eating to their clients.
“Clinicians now consider it a good idea to get a client’s diet right before they go on medication, if they get the diet right they may get much better results than with just medication and psychotherapy,” she says.


Low carb diets have become particularly relevant to brain health. Dr McCormack cites neurologist Dr David Perlmutter whose books and papers talk about how diet affects brain function.
“Your brain needs fat to function as well as glucose. And the glucose it needs can come from the body rather than from food. Sugary foods do nothing for the brain function of people with mental health issues. They can cause blood sugar spikes and crashes even in someone who’s not diabetic and that does nothing for mental wellness. And if people eat less sugar, they need less insulin and medication for diabetes.
Dr McCormack has seen impressive results in patients who have followed her suggestion of following a ketogenic diet.
“One of my patients has controlled his blood sugars as he would if he wasn’t diabetic. For two years now he’s followed the diet, exercised and maintained a normal weight – his blood sugars are within normal range. I also have patients who have come off insulin and other diabetic medication. 10 years ago I wouldn’t have known that was possible with just diet. It’s amazing.”
Carbohydrates are one of the nutrients that form a large part of our diet – the others being fat and protein. There are three different types of carbohydrates: sugar, starch and fibre.
Sugars added to food or drinks, and sugars found naturally in honey, syrups, and unsweetened fruit and vegetable juices, smoothies and purées – should not make up more than for 5 per cent of the energy (calories) you get from food and drink each day. Sugar found naturally in milk, fruit and vegetables does not count.
Starch is found in foods that come from plants. Starchy foods, such as bread, rice, potatoes and pasta, provide a slow and steady release of energy throughout the day.
Fibre is the name given to the diverse range of compounds found in the cell walls of foods that come from plants. Good sources of fibre include vegetables with skins on, wholegrain bread, whole wheat pasta, and pulses (beans and lentils).
You can find out more about these at nhs.uk
Dr McCormack runs regular low-carb eating support groups in her local area. For more information go to www.fatismyfriend.co.uk



Dave
LOW CARB FOODS
• Lean meats, such as sirloin, chicken breast, or pork
• Fish
• Eggs
• Leafy green vegetables
• Cauliflower and broccoli
• Nuts and seeds, including nut butter
• Oils, such as coconut oil, olive oil, and rapeseed oil
• Some fruit, such as apples, blueberries, and strawberries
• Unsweetened dairy products including plain whole milk and plain Greek yogurt, butter, cheese.
Abram is a specialist diabetes dietitan. He takes a more moderate approach based on the individual.
“As dietitians, we always deal with the person in front of us, supporting what they want to do, and what they feel they can realistically do. We don’t want to ban foods because it makes people feel deprived, but we do focus on portion control and how much is too much.”
“A low to moderate carbohydrate intake (130 to 170g a day) does allow people to include carbs they like in smaller portions, making it more achievable and sustainable. So someone who has been eating a high carb intake, say 450g a day, reduces to 200g, they’ll reduce both calorie intake and glucose load on the body which is better for their diabetes control but also something they may be able to keep up.
“We work with the person to develop a plan to ‘eat better’. So if someone wants to eat rice for
example, we’d help them learn about portion sizes – we’d explain that 30 to 50g or about a handful of cooked preferably whole grain rice is generally ok.
“Similarly, steak and fries are fine if the fries are a quarter of the plate and vegetables and salad are the biggest part – about half.”
He gives tips on how to combine carbs and other foods to make them healthier.“For instance a baguette is a fast-acting carb and will quickly raise your sugar levels, but adding chicken, olive oil dressing and some mixed leaves, will slow down the absorption rate. Changing the baguette to two slices of wholegrain bread would be an even better choice, as it would reduce the amount of carbs by about half and have a slower absorption. Overall we want someone’s diet to include food from all food groups, but in the right amount, so it’s balanced in nutrition, calories and carbohydrate.”


Serves 4
INGREDIENTS:
Curry paste 100g 280 kcal 7g carbs
Chopped tomatoes (1 tin) 100 kcal 16g carbs
Peppers x3 120 kcal 18g carbs
Mushrooms (200g) 16 kcal 1g carbs
Courgette (150g) 30 kcal 3g carbs
Onion 40 kcal 8g carbs
Cauliflower rice (400g) 80 kcal 16g carbs
Quorn (200g) 200 kcal 3g carbs
Spinach (150g) 45 kcal 2g carbs
Olive oil (2 tbs) 270 kcal 0g carbs
This delicious curry cuts down on the carbs but not the flavour says dietitian Dave Abram.
Replacing normal rice with cauliflower rice reduces both carbs and calories*.
METHOD:
1. Soften the onions and peppers in the oil.
2. Add courgette, mushroom, curry paste, 100ml water, tin of chopped tomatoes.
3. When simmering, add the quorn, cook for 12 mins, add the spinach, mix through.
4. While the curry is cooking remove outer leaves from the cauliflower, cut into chunks and blend for 30 seconds (or alternatively grate coarsely). If fresh, microwave in a heatproof bowl, covered with cling film, for three minutes, or if frozen for four minutes, mixing the ‘rice’ half way through cooking.
5. Serve with cauliflower rice.

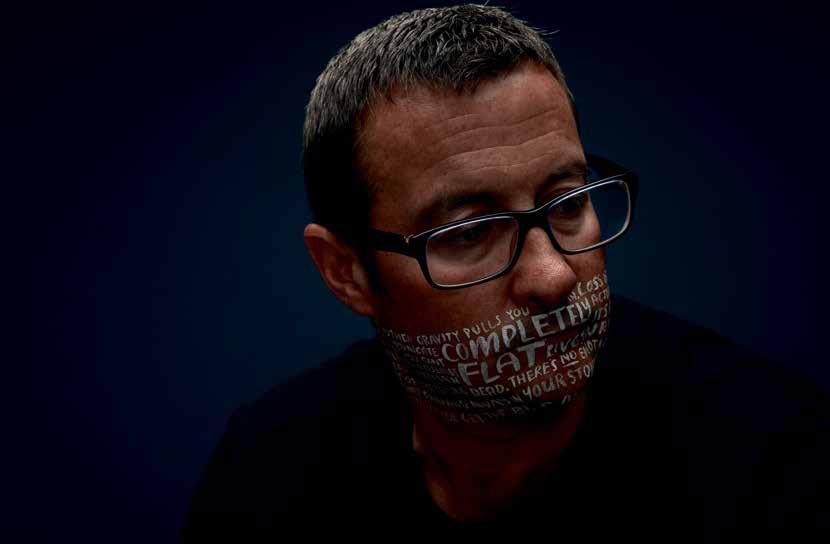
Charlie Clift opened up to his parents when he became depressed as a student. They supported him as he recovered. They bought him a camera as therapy.


Charlie became an acclaimed professional photographer and now he’s using his experiences and his skills to help others open up and share their thoughts and feelings.
Ihad to drop out of my studies because I just lost all motivation and drive. I ended up moving back in with my parents and taking a year off. They were amazing and really supportive. Thankfully, I could open up and talk to them – that really helped me a lot,” he told arts blog mymodernmet.
Still occasionally haunted by depression he began thinking about how he could use his work to stimulate conversation and contribute to the growing movement to wipe out mental health stigma.
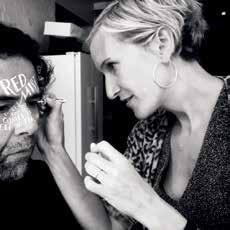
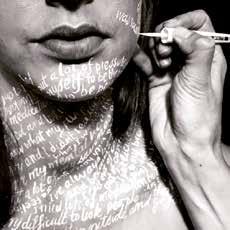
“I had wanted to talk about mental health in my work for a while, but couldn’t find the right way to show what was happening inside someone’s head in a photograph,” he told blogger Jessica Stewart: “I was joking about putting graffiti on someone’s face and it struck me that this would be a great way to show someone’s thoughts in a photograph.”
Charlie linked up with lettering artist Kate Forrester. He’d seen Kate’s work and knew she was the right person for what would be a hugely challenging experience for everyone
involved, not least the portrait subjects.
Through their powerful new portrait series Let’s Talk, Charlie aims to spark a conversation about mental health.
Let’s Talk asks ordinary people who have suffered from mental health issues to open themselves up and share what goes on inside their minds. Their words are then transformed into artistic hand lettering across their skin by Kate, allowing their inner thoughts to come out in Charlie’s moving portraits.
“I launched a social media campaign and was overwhelmed by the amount of people who got in touch wanting to take part. It made me realise that there are many people willing to open up and talk about their mental health.
“The process was quite a long one and the whole way through I made sure people felt comfortable and knew exactly what they were getting into – I didn’t want there to be any surprises for the participants. I also made sure that I didn’t judge anyone.”
CONTINUED OVER.


Art has a unique power to encourage conversation.

CONTINUED FROM PAGE 31
His photographs and the lettering throw bare the often hidden facets of someone with a mental health issue. The contrast between facial expressions and the words and phrases on people’s faces are a stark reminder of how our thoughts belie our public persona. And that everyone is different with their own story to tell.
Charlie recalls the bravery shown by people who had been through ‘incredibly tough times’.
”I was asking them tough questions but needed to get them to express in their own words how it feels inside their head. I recorded this conversation so that later on Kate and I could pick out the most poignant words and phrases to write on their face.
“Seeing how much they achieved despite their mental health difficulties was really inspiring for me… this campaign has been very public and I admire them hugely
for opening up and encouraging others to do the same in the process.
“I also found that it helped me understand my own mental health difficulties a lot more — during the interviews I often found myself thinking ‘I’ve felt like that’ or ‘that’s happened to me’.
“I have had people write to me saying that Let’s Talk has helped them talk to their partner or child when they couldn’t before. They’ve used it to spark a conversation. I believe that art has a unique power to encourage conversation. The more each of us is open about our difficulties with others, the easier it will be for them to seek help when they need it.”
See how Let’s Talk was made at vimeo.com/292276387
For more information visit: letstalkcampaign.com
@charlieclift @forrester_kate

MC: What is HPV?
NW: It’s the name given to a group of viruses. HPV infections can be spread by any skin-to-skin contact and are usually found on the fingers, hands, mouth and genitals. This means the virus can be spread during any kind of intimate contact including touching with another person who may already carry the virus. Not all HPV viruses cause cancer but some can. It’s a hidden virus and you may never know that you carry or have it.
MC: Why were girls vaccinated first?
NW: 99.7 per cent of cervical cancers and 70 per cent of vaginal and vulvar cancers are caused by infection with a high-risk type of HPV so it’s vital to protect young women before they become sexually active.
MC: Why are boys only being offered the jab now?
NW: We’ve since learned that HPV infection causes 90 per cent of anal cancers and 60 per cent of penile cancers. It can also cause head and neck cancer. We needed to ensure boys were protected too.
MC: How does it work?
NW: The vaccine stimulates your immune system to produce antibodies. They lay dormant in your body ready to protect you if you come into contact with the virus.
MC: Is it for people who have lots of partners?
NW: Not at all – you might have one long term partner who happens to be a carrier and they can unknowingly pass it on, condoms do not protect against HPV viruses.
MC: When is the vaccination given?
NW: The national programme offers it in school at Year 8.
MC: How do you explain it to boys?
NW: We discuss the vaccination in school assemblies and explain that it’s to protect them into adult life. We explain that the vaccination is like making soldiers (antibodies) to create an army ready to fight off the virus should they be exposed when they’re older. It’s estimated the programme will prevent more than 4,000 cervical cancers and almost 50,000 non-cervical cancers by 2058.
The HPV vaccine has been offered to school aged girls for over ten years now; from September 2019 the vaccine will also be offered to year 8 boys. This is because the evidence is clear that the HPV vaccine helps protect both boys and girls from HPV related cancers. Nikki Wilinski who co-ordinates the HPV vaccine programme in Liverpool tells us more...

MC: Is the vaccination safe?
NW: Yes. There’s been a lot of research and more than 80 million vaccinations have been given worldwide. Authorities around the world, including the World Health Organization (WHO) have monitored the use of the HPV vaccine very closely for many years. You can ask your school or immunisation nurse if you have concerns.
Because the programme to vaccinate teenage girls, and reduce cervical cancers, has proved very successful.
There has been a reduction in HPV infections, genital warts and pre-cancerous growths in teenage girls and young women since the vaccine was introduced.
Other groups, like teenage boys, have seen benefits too because the virus is not being passed on to them.
Source: bbc.co.uk/news/health
What always strikes me when I’m on a ward is just how different everyone is and how we can improve their care just by finding ways to understand them, support them and involve them in the planning. My own sister has a learning disability and bipolar disorder, so I know first hand how important it is to consider everyone in their own right, and respect people’s differences.
Today I’ve been with staff from our medium secure unit talking about how we’ll do things in our new state of the art hospital. How we’ll discuss people’s treatment with them and their families and carers; let them lead the way, develop genuine relationships, involving them in every decision – almost like an invisible golden thread running through everything we do for them and with them.
I met a chap today on one of our low secure wards who has autism and mental health issues. When I last saw him he was sad and unmotivated. We’d asked then if there was anything else we could do for him – he told us that was the first time anyone had asked him that. It was so powerful – we now ask it as routine. People get tired of having things done to them. To get the best outcome we need to hear their story and help them tell it.
My early career was as a TV make up artist, but I felt people were often treated unequally – it didn’t fit with my values. I questioned my purpose and left to work in a nursing home. My passion for quality derived from ensuring people are heard and treated equally, I’m always analysing and working out how to make things better. I looked to my own family and chose to pursue learning disability nursing – although they say you don’t choose that area of nursing – it chooses you.
I saw a lady today who had been self injuring. It was felt taking her out of the ward would help, but through working with her, we realised it traumatised her more. We now nurse her on the ward. She told
me today it’s the best ward she’s ever been on – she was simply misunderstood, but it’s an example of how we should be doing only the things that add value and make a difference to people.
People get tired of having things done to them. To get the best outcome we need to hear their story.


Dean Hegarty community mental health support worker and staff governor.
Itravel around 150 miles a week on my bike, visiting people in their homes. I always try to help them to get out and about, sometimes we go for a bike ride. It can make a big difference to someone’s mood if they see the world outside. They’re on their own journey to recovery but we travel together.
Actually that’s not always true! My aim is to help them become truly independent so if they prefer to go by bus I’ll sometimes travel behind them. That way they feel empowered but they’ll know I’m always right behind them.
The cyclists have started meeting up as a group, I’m really pleased they have their own social circle outside of the service.
I love working with people, helping them achieve their full potential. We do everything at their pace, step by step.
I’m also a carers’ champion – carers are so valuable to everyone else involved in someone’s care – we should listen to them and direct them to places where they can feel safe too.
The governor role is new to me. If I’m honest I really didn’t expect to get the votes

needed. I put myself forward because I wanted to put the viewpoints of staff to the people making decisions, but I thought I’d get no more than a few votes from colleagues!
I feel privileged to be able to look out for the people who work at Mersey Care. I’ve got a lot to learn but I’ll just be myself and take it from there, step by step...”
Our next members’ event will take place at Holiday Inn Liverpool City Centre, Lime Street, Liverpool L1 1NQ on Tuesday 15 October 2019 from 12.30pm to 3.30pm. RSVP to membership@merseycare.nhs.uk or call 0151 471 2303
Find out more about our membership and governors at: Website: merseycare.nhs.uk. Phone: 0151 471 2303 or 0151 473 2778 Email: membership@merseycare.nhs.uk Write to: Alison Bacon, Mersey Care NHS Foundation Trust, V7 Building, Kings Business Park, Prescot, Liverpool L34 1PJ.

