Cancer Care










 Blumenthal
Blumenthal



Ostensibly, it’s a clinical trial of an immunotherapy for blood cancer patients with specific kinds of leukemia or lymphoma, for whom other treatments have not been successful. A good result could mean the difference between life and death for these patients and the importance of this trial for them cannot be overstated, as Owen Snider will attest.


Mr. Snider was one of the first patients to enrol in the trial. At the time, his lymphoma had returned, for the third time in 10 years. His doctors had given him maybe six months to live. Then he was told about the Canadian-Led Immunotherapies in Cancer (CLIC-01) clinical trial, funded in part by BioCanRx. Today, 18 months later, Mr. Snider remains cancer-free and, as he's said publicly several times, he appreciates each and every day.

Mr. Snider is one of an eventual 60 patients who will participate in the trial, about half of whom have been enrolled so far. And with each patient who receives treatment, lead investigator Dr. Natasha Kekre of The Ottawa Hospital gets a little more excited.

“We're now seeing success, and that’s been huge for us,” she says.


But, she adds, the importance of this trial goes much further. It's the fi rst trial that uses Canadian-made CAR T cells and, if successful, it


means that further research innovations will be available to Canadian patients.

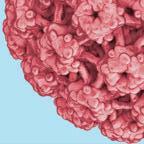
CAR T cells, or chimeric antigen receptor modified T cells, aren't simple, off-the-shelf products. They are, says Dr. Kekre, much more complex than drugs. They work by enhancing the body’s own immune system to better attack cancer.

treatments. To date, two CAR T cell therapies are on the market, targeting certain types of B-cell lymphoma and acute lymphoblastic leukemia, but this came years after clinical trials were completed elsewhere. Without the ability to manufacture CAR T cells in Canada, patients in Canada would continue to wait for approvals like this, putting them at the end of the line for these therapies.
“We want to build up the research infrastructure,” says Dr. Kekre. “Canadian cancer patients shouldn’t have to wait for the research to be done elsewhere, but be able to participate in innovative clinical trials here at home.”




Support from BioCanRx helped develop that manufacturing capacity here in Canada, the CLIC-01 trial is the first to use these home-grown CAR T cells. But, says Dr. Kekre, it won’t be the last. She's looking forward to a future of “more trials, more cancers, more patients.”



The cells are made from patients’ own T cells, a type of immune system cell. The T cells are extracted from their blood, genetically modified in the lab to be more active, and then re-administered to the patients. These “souped-up” immune cells are then better able to attack and kill cancer cells.
CAR T cells have shown tremendous promise in treating cancers that haven’t responded to other

CLIC-01 is critically important for the patients involved. But it's also being watched closely for its impact on future research that will be carried out, here in Canada and for the benefit of Canadian patients. A giant step in cancer treatment, indeed. Additional funding was provided by BC Cancer, OICR, The Ottawa Hospital Foundation and the Leukemia & Lymphoma Society of Canada.
Full of powerful personal stories, practical tools, video tutorials and uplifting content for women and teens facing cancer, their caregivers and supporters, the Look Good Feel Better magazine has something for everyone. Head over to lgfb.ca.








Cancer doesn’t define who I am.
It's the first trial that uses Canadian-made CAR T cells and, if successful, it means that further research innovations will be available to Canadian patients.
Peggy Pickett, 57, was leading a full and active life — working full-time at a job she loved, travelling, volunteering, knitting, playing guitar, and enjoying her family.
In early 2012, she started feeling a strange pain on her upper right side. Being a diabetic, she checked in regularly with her family doctor and would frequently mention it to him. “He basically dismissed it as a pulled muscle and nothing that proper diet and exercise couldn’t fi x,” says Peggy.
A long two years until a diagnosis After repeated attempts to describe her condition to her physician with no outcome, Peggy decided to stop talking to her doctor about it. But the pain persisted, and in September 2013, her husband Jack watched her suffer an excruciating episode. Something needed to be done immediately.
In January 2014, surgery confirmed a diagnosis of advanced high-grade serous ovarian cancer. There were 11 tumour sites and multiple clusters of tumours, including a few on her liver. The pain on her upper right side turned out to be from the tumours on her diaphragm. “They would twist with exercise or breathing, and I’d been living with that for two years,” she says. One month later, on her 50th birthday, Peggy started her fi rst chemotherapy treatment.
Awareness of early signs is imperative for women
Typical symptoms of ovarian cancer are bloating, difficulty eating, pain, and changes in bladder habits — but these non-specific symptoms can easily be confused with other benign conditions. A woman may also experience other symptoms, as Peggy did, that don’t seem related to ovarian cancer. “The pain I had on my right side wasn’t a classic ovarian cancer symptom,” she says.
From patient to self-advocate and advocate for other women Peggy has come to terms with her anger about her complaints being dismissed. “I had stopped being a self-advocate and I realize now that doctors can’t diagnose what you don’t tell them. If they don’t suspect it, they won’t detect it and if they don’t detect it, they can’t treat it,” she says.
Then something changed after her second round of chemo. “I felt the need to know more about what was happening so I could make informed decisions,” says Peggy.

She contacted Ovarian Cancer Canada to request a free copy of their resource book, which she received in the mail, along with a follow-up call. “This was a pivotal moment when I went from being a patient to a self-advocate,” she says.


Rather than waiting for her treatment to end and then pick up her life again, Peggy made a choice to live as much as the day could hold, find good sources of information, and share the power of her experience rather than give that power away. “I set out to become the world’s leading expert on Peggy and, as such, have become a valuable member of my medical team,” she says.
Ovarian cancer is a form of cancer that occurs due to the abnormal and uncontrolled growth of cells from the ovaries, fallopian tubes, or peritoneum.
Her family doctor ordered an ultrasound, which she received in December. That same evening, her doctor called to report that the results showed something suspicious. Peggy was immediately referred to a cancer centre, where she had more tests. Six days later a gynecologic oncologist told her she had two tumours — one the size of a cantaloupe on her right ovary and another the size of an orange or small grapefruit on the left one.
While Peggy went through three recurrences, two more rounds of chemotherapy, and two rounds of radiation, her take-charge self-advocacy approach ensures she has access to the latest and most effective treatments for her needs. She’s now a peer volunteer with Ovarian Cancer Canada, and constantly looks for opportunities to improve the outcomes for women living with the disease. “Becoming educated in my disease and the medical system and becoming an advocate for myself and other women has been my road away from powerlessness,” says Peggy.
Her advice to other women: “Become the world’s leading expert on you. Know yourself, know your body, and know your options,” she says.
Ovarian cancer can start from three common cell types: epithelium, germ cells and stromal cells.
The most common type of ovarian cancer is epithelial, which accounts for 90% of all cases of ovarian cancer.
An estimated 3,100 Canadian women were diagnosed with ovarian cancer in 2020. An estimated 1,950 have died from the diseaseiv
Ovarian cancer is the 8th most common cancer in women and is the most fatal gynecological cancer in Canadaiv
Epithelial ovarian cancer is the most common type of ovariancanceri 5-year survival rate according to Canadian Cancer Statistics 2019 report for 2012-2014 period is 45% iv
About 75% of women with ovarian cancer are diagnosed at later stages (Stage III/IV)v
It’s not clear what causes ovarian cancer, but risk factors include:i,ii
• family history of ovarian or breast cancer
• deleterious gene mutations including the BRCA gene
• previously having endometriosis
• increasing age
• infertility
• smoking
Nearly 75% of women diagnosed with advanced ovarian cancer will experience relapse
Raising awareness around ovarian cancer, including the signs and symptoms, is critically important. Well informed, Canadian women have a better chance of discovering the disease early and having a positive outcome.
With the patients’ voice at the heart of our mission, at GSK we are committed to fulfilling unmet patients’ needs by developing innovative medicines that help improve the quality of life and outcomes for Canadian women living with the disease.”
• lynch syndrome (genetic disorder)
Many women with early ovarian cancer have no signs or symptoms and when present, they are similar to other, more common and benign conditions. This can make for a challenging and late diagnosis.
Some early symptoms are:i,ii
• abdominal pain,
• swelling & bloating
• changes in bowel movements
• pelvic & lower back pain
• fatigue
• frequent or urgent need to urinate
To help diagnose ovarian cancer, exams and tests may be used, such as:ii
• Biopsy
• Physical evaluation and pelvic exam
• Ultrasound and other imaging tests
• Blood tests
In general, treatment for ovarian cancer may include a combination of the following: i,ii

• Surgery
• Targeted therapy
• Chemotherapy
Becoming educated in my disease and the medical system and becoming an advocate for myself and other women has been my road away from powerlessness.Marni Freeman Medical Director, GSK Canada
There’s arguably nothing more devastating than hearing that you or a loved one has cancer. Two in five Canadians are expected to be diagnosed with cancer in their lifetime and it’s the leading cause of death in Canada, but cancer’s prevalence does nothing to soften the blow of a diagnosis.
The impact of cancer cannot be underestimated. Every day, hundreds of thousands of Canadians face challenging treatment protocols, care for loved ones undergoing treatment, and pray for a cure. What may be the most distressing, however, is that promising breakthrough treatments exist and are starting to make a real difference in cancer care — but that many Canadians cannot get timely access to them.
Bringing new hope — but not to all Recent medical advancements have led to a greater understanding of cancer and to new breakthrough treatments targeting cancer at the cellular or genetic level, most notably for melanoma, multiple myeloma, breast cancer, lung cancer, and prostate cancer tumours. These new treatments are extending patients’ lives and bringing new hope.
However, although Canada does well regarding the time it takes to approve breakthrough treatments for use, complex price-payment negotiations have made the process slow and difficult to complete. As a result, many patients face access delays.




These gaps in patient access have led to lost economic value and lost tomorrows for Canadians facing cancer and their loved ones. To explore the impact of delayed access, the Conference Board of Canada — Canada’s leading independent research organization — undertook a research initiative supported by Innovative Medicines Canada, which represents Canada’s pharmaceutical industry.
The resulting study, “Tomorrow Can’t Wait: The Value of Breakthrough Cancer Treatments for Canadians,” highlighted just how dramatic that impact is.
“When we developed this report, our focus was to estimate the potential life years gained and the subsequent economic value to Canadians and the Canadian economy if all eligible Canadians had access to breakthrough cancer treatments for the five tumour types,” says Chad Leaver, Director of Health at the Conference Board of Canada.
The report found that 226,445 life years could’ve been gained, along with $5.9 billion in economic value, over the past decade. “This is about patients being able to maintain or resume employment on their cancer journey and to contribute to society and their community,” says Leaver.
“And what this means for patients and families is more tomorrows — another laugh, another smile, another talk, another hug. These priceless outcomes may not be quantified in our study, and yet they’re undoubtedly the most meaningful.”
Better access also represents the hope that more time will allow patients to access the next treatment that may come along and potentially cure them, stabilize them, or put them into remission, says Eva Villalba, Executive Director of the Quebec Cancer Coalition. “Modern medicine has been moving so quickly that we see incredible progress,” she notes.

Access to scientific breakthroughs is also an important reminder of hope and empowerment for every Canadian, Leaver adds. “It’s important that Canadians know these treatments are available and are encouraged to learn more,” he says.

We could all use a little more hope these days. Patients facing cancer

today do so under the compounding stress of the pandemic. “People with cancer and their families have to deal with not only the tremendous shock of diagnosis, but also the uncertainty and anxiety of navigating the health care system,” says Villalba. “They also have to manage the impacts on their personal and professional life as well as on their finances. All of this is difficult enough under normal circumstances, and now with the pandemic it’s even worse. Access to cancer care and services has been impacted, and people with cancer also have an increased risk of complications from getting COVID19, so every moment counts.”
The importance of timely access Today more than ever, it’s essential for Canada to accelerate and provide equitable access to breakthrough cancer treatments. The Conference Board of Canada recommended four system-level reforms to increase timely patient access, including improving the current regulatory and price negotiation processes, changing the way therapies are funded, funding access to diagnostic services, and expanding and integrating systems that collect and share data. The solution is within reach, and we must do everything we can to improve access — because as those who have faced a cancer diagnosis know, tomorrow can’t wait.
To learn more, visit mybreast screening.ca . It provides current, evidence-based information to empower women to make informed decisions for their health. This article was sponsored by mybreast screening.ca


Get mammograms starting at 40
The evidence is clear: annual mammograms starting at age 40 save the most lives. Seventeen percent of breast cancers occur to women in their 40s, and those cancers are more aggressive. Minority women are more likely to be diagnosed in the 40s. Women in Ontario can’t self-refer for mammograms in their 40s. They need a requisition from their health care provider. Canadian guidelines state that women can choose to have a mammogram in their 40s. Your body. Your decision. If you’re unjustly denied, visit a walk-in or fi nd out what to say to your provider at mybreastscreening.ca
Learn about the importance of knowing your breast density

About half a million women in Ontario are at increased risk of breast cancer because they have dense breasts. They haven't been told. Breast density is only determined after a mammogram. Dense breasts are normal, but increase both the risk of breast cancer and the risk cancer will be hidden on a mammogram. Your health care provider knows your density category. After your mammogram, just ask.
Women are routinely denied access to screening ultrasound in Ontario. Mammograms aren’t enough for women with dense breasts because both cancer and dense tissue appear white on the X-ray, creating a masking effect. Ultrasound fi nds additional cancers missed in dense breasts. Insist on additional screening and fi nd out how to advocate for an ultrasound at mybreastscreening.ca

Cancer screening has been disrupted in Canada due to the COVID-19 pandemic. According to Ontario Health, during the first wave there was a significant decrease in screening in Ontario compared to the same period in 2019: A 97 percent decrease in screening for mammograms through the Ontario Breast Screening Program has been reported.1
In addition, approximately 40 percent of the population has dense breasts,2 which can increase a woman’s chance of developing breast cancer by 4 to 6 times for women with category D density.3 In fact, 71 percent of breast cancers are found in dense breasts.4 This makes early detection especially important, as it can increase treatment options and improves a woman’s chance of survival.5
While having dense breasts is normal, it makes it harder to detect cancer. Breast tissue is made up of milk glands, milk ducts, dense breast tissue and fatty tissue. Women with dense breasts have more dense tissue than fatty tissue. Normal dense breast tissue looks white on a mammogram, and so do tumours, making it hard to distinguish normal breast tissue from a tumour.
An effective strategy is needed to minimize potential harm to people who missed their screening, with a personalized focus on breast density.
But how do you know if you have dense breasts?
According to Dense Breasts Canada, policies to ensure that women with dense breasts are informed of their density differs province-to-province. In Ontario, you'll be informed by mail if your density is over 75 percent (Category D) and you'll be asked to return annually for a mammogram and your health care provider will also be told. However, dense breasts refer to breasts with 50 percent and over dense tissue. Women in the 50-75 percent category (Category C) are currently not told they have dense breasts. 500,000 women in Ontario are not told that they have dense breasts or the implications. A clear mammogram may not be clear. All
health care providers are now informed of your breast density category (A,B, C, D).2
Toronto Centre for Medical Imaging (TCFMI) is providing women with innovative screening aids to deliver personalized care for patients with dense breasts. Dr. Alnashir Ismail, a Diagnostic Radiologist and Owner of TCFMI, is using Automated Breast Ultrasound (ABUS) to help detect breast cancer in women with dense breasts. Dr. Ismail has adopted an ABUS system in his clinic that provides a rapid, reliable screening tool to detect many of the cancers that mammography may miss in this patient population.
“With all of the information on dense breasts and cancers being missed, I knew that for women with dense breasts, mammography was not enough. Without an ultrasound, a patient with a normal mammogram can have cancer that is missed. With ABUS, we finally have something that can help women with dense breasts,” says Dr. Ismail.
Early detection can save lives ABUS with its non-invasive and patientfriendly technology is moving Breast Care from reactive to proactive. When used as a supplement to mammography, studies have shown that ABUS increases cancer detection in dense breasts by 55 percent and the additional mammography occult cancers found with ABUS were predominantly invasive and node negative.7 Detecting cancer at this early stage has important prognostic implications and can reduce the total cost of care.8 When breast cancers are found at Stage 1 and 2, 70 percent of patients may avoid chemotherapy.9
TCFMI gives women the opportunity to get imaged from an experienced radiologist that specializes in this space. Using

software, Dr. Ismail can review the images that show layers of dense tissue from different perspectives, which can help them find breast cancers that may have been missed on a mammogram.


Advances in technology allow for more personalized medicine Dr. Ismail explains that performing an automated breast ultrasound in addition to a mammogram on a woman with increased breast density, improves cancer detection. “Every year, mothers, sisters, women in their 40’s are dying from breast cancer. What is important to note is that whatever number of people dying from breast cancer, it should be dramatically less.”
Since 40 percent of the population has dense breasts, 2 Dr. Ismail is happy the technology exists to provide women with more options. This means a patient and physician can consider a woman’s individual risk factors and tailor her screening accordingly. One size does not fit all.
You Can’t Treat What You Can’t See.





















Cervical cancer kills hundreds of Canadian women every year. With the right screening, immunization, treatment, and support, we could bring that number down to virtually zero. Almost all cervical cancers are caused by HPV, the most common sexually transmitted infection in Canada. And HPV is both vaccine-preventable and treatable.
“Cervical cancer is preventable,” emphasizes Dr. Kathleen Decker, a Scientist with the Research Institute in Oncology and Hematology at CancerCare Manitoba. “There are three key strategies used to prevent cervical cancer: immunization using the HPV vaccine, screening, and treating women who have an abnormal screening test.”
Better screening means earlier diagnosis



Modern cervical cancer screening is more robust than the pap smear most people are familiar with. Advances in screening technology have made it possible to test for high-risk HPV strains directly. “HPV testing and HPV immunization have been valuable innovations in the prevention, early detec-





tion, and management of the precursors of cervical cancers,” says Dr. Nathan Roth of the Department of Obstetrics and Gynecology at University of Toronto.“The results of HPV testing help determine what steps should be taken and what treatments to give to prevent cervical cancer from occurring.”
These advances are particularly important because detecting cervical cancer or precancer at the earliest stages is one of the biggest predictors of survival. “Earlier detection has had a major impact on the cervical cancer death rate in Canada and other countries with widespread cervical cancer screening programs,” says Dr. Leah Smith, Senior Manager of Surveillance at the Canadian Cancer Society. “In Canada, the cervical cancer death rate has dropped at least 70 percent since the 1970s. This is primarily due to the success of widespread screening.”
A literal vaccine against cancer
If we continue to build upon this success, cervical cancer could potentially go the way of polio and smallpox. “We stand on the edge of a historic achievement, the elimination of cervical cancer. It's a global commitment,
achieve within a single generation, thanks to all the groundwork laid over the past many years,” says Dr. Jennifer Blake, CEO of the Society of Obstetricians and Gynaecologists of Canada. “It will take vaccination, which we know is safe and effective, organized screening with HPV testing, and early treatment at the pre-cancerous stage. Today.”
The most important thing you can do to protect yourself against preventable cancer is to talk to your health care provider. Ensure that you're immunized and ask if there's more complete screening available than what you currently receive. It could save your life.





Bladder cancer patients across Canada welcome the news of a new strain of Bacillus Calmette-Guerin (BCG) on the Canadian market.





BCG is the most common type of immunotherapy inserted directly into the bladder for treating early-stage bladder cancer. It’s used to help stop the cancer from growing and preventing it from coming back. Originally developed as a vaccine for tuberculosis, BCG is a weakened form of the tuberculosis bacterium, which stimulates immune responses within the bladder to destroy the cancer cells.
Fortunately, 75 percent of bladder cancer diagnoses are identified as non-muscle invasive which means that BCG is an effective treatment to preserve the patient’s bladder and their quality of life.
However, in 2019, the bladder cancer community was informed of an anticipated BCG shortage due to increased global demand. Merck Canada, who has provided

BCG OncoTICE® to bladder cancer patients in Canada for over a decade, increased production by more than 100 percent to enable it to be produced at the full extent of their manufacturing capacity.



Since the number of bladder cancer diagnoses continues to increase each year (12,500 Canadians will be diagnosed in 2022) and the disease has a recurrence rate of 65 to 70 percent, the demand for BCG continues to rise.

In late 2021, Verity Pharmaceuticals joined the Canadian market with a new strain of BCG for patients diagnosed with papillary (a type of cancer) nonmuscle invasive bladder cancer (TA or T1), without evidence of carcinoma in situ (cancer that has not spread beyond the cells where it started).


For bladder cancer patient Jonathan, who has undergone 18 rounds of BCG in North Bay, Ontario, it's reassuring to him that an additional strain of BCG is now available. Says Jonathan, “No patient dealing with a bladder cancer diagnosis should also have to worry that their BCG treatments will be delayed or if they are only receiving a partial dose due to limited quantities in Canada.”
While many hospitals and doctors continue to use Merck as their primary source of BCG, it’s important for bladder cancer patients to ask their health care team if Verity BCG™ is an option for them, particularly if they meet the criteria and are currently experiencing delays to their BCG treatments or partial dosing.


No patient dealing with a bladder cancer diagnosis should also have to worry that their BCG treatments will be delayed or if they are only receiving a partial dose due to limited quantities in Canada.
If you haven’t heard of an isotope called Actinium-225, it’s for good reason. Even with an army of nuclear scientists at your disposal, you’d be hard pressed to fi nd more than just a trace of Actinium-225 on the planet. An alpha-emitting isotope with a short half-life, Actinium-225 is so rare that the annual global production is less than a grain of sand. Given this scarcity, it should come as no surprise that the isotope has been dubbed ‘the rarest drug on Earth.’
Today, the unique properties of Actinium-225 have also made it one of the most sought-after isotopes in the world by the medical community. The material made headlines in 2016 when a German patient suffering from terminal cancer was treated with a novel new therapy enabled by this rare isotope. Eight months later, the tumours had largely disappeared, the patient was still alive, and international researchers were clamouring for more Actinium-225, in order to explore the potential of this radioisotope.
“Given the extraordinary results, it is clear why this case captured the world’s attention, and further studies have shown just as much promise,” explains Joe McBrearty, President and Chief Executive Officer at CNL. “Unfortunately, the limited supply of the isotope has really hampered the world’s ability to advance research on targeted alpha therapy, which is the treatment that uses Actinium-225. There is not a lot of the material to make use of, and it is also quite difficult to produce.”


Enter Canadian Nuclear Laboratories (CNL). CNL operates the Chalk River Laboratories north of Ottawa, which is owned by the federal government's nuclear crown corporation, Atomic Energy of Canada Limited (AECL).
Chalk River once produced more than half the world’s supply of molybdenum-99, a key isotope used for cancer diagnostic procedures, among others.
CNL estimates that isotopes produced in Chalk River have been used in over one billion medical procedures.
With the closure of the National Research Universal reactor in 2018, CNL ceased producing molybdenum-99, but the company still fulfills a vital role as a national research laboratory, with con-
siderable strengths in health sciences and the development and testing of medical isotopes and radiopharmaceuticals. With the growing interest in Actinium-225, CNL quickly recognized that it was one of a handful of companies in the world that could not only produce research quantities of the rare material, but study it as well.
“CNL has not only all of the health science laboratories, equipment and expertise to conduct research programs based on Actinium-225, but we also have the nuclear materials needed to produce more of this rare isotope,” explains Dr. Jeff Griffin, Vice-President of Science and Technology at CNL. “Over the past three years, we've developed a smallscale generator which produces enough Actinium-225 for our own research, but also meaningful quantities that we can share with strategic partners in industry and academia to advance treatment safety and efficacy.”
How do those treatments work, exactly? Actinium-225 is attached to what's known as a targeting molecule, such as an antibody, that is designed to seek out and bind with cancer cells. As the isotope decays, it emits high-energy alpha particles that effectively kill cancer cells, leaving nearby healthy cells virtually unharmed in the process. With a favourable half-life of 10 days, Actinium-225 lasts long enough to do its job in fighting cancer and doesn't harmfully linger in the body. Due to its many unique attributes it's seen as a ‘goldilocks’ isotope in nuclear medicine.
This treatment is collectively known as targeted alpha therapy (TAT), and CNL is positioning itself to be an international hub for this type of research into the future. In addition to radioisotope production, CNL also maintains capabilities to conduct biological research at its Biological Research Facility, a unique facility that holds the necessary capabilities to perform TAT-related research and development for universities and innovative companies, and which is on its way to obtain Good Laboratory Practice (GLP) recognition.
But even bigger plans are in the works. CNL sees a clear opportunity to build on its legacy in isotope production and processing and is exploring the construction of new facilities on its main campus
that would establish a stable, commercial supply chain for Actinium-225. In pursuit of that goal, CNL recently signed a Memorandum of Understanding with ITM Isotope Technologies Munich, a leading radiopharmaceutical biotech company based out of Germany.

It’s all very exciting for the many researchers who are quietly advancing nuclear science and technology at the Chalk River Laboratories, a Canadian science institution that once transformed the way the world fights cancer and diagnose many life threatening diseases, and which gave hope to millions of people all over the world. With Actinium-225, they’re about to do it again.
The world’s first Cobalt-60 cancer treatment was delivered in Saskatoon, Saskatchewan.

The


CNL contributes to pre-clinical and toxicology studies for the use of next generation isotopes.













Dr. Jeff Griffin Vice-President, Science & Technology, Canadian Nuclear Laboratories
CNL has not only all of the health science laboratories, equipment and expertise to conduct research programs based on Actinium-225, but we also have the nuclear materials needed to produce more of this rare isotope.


The COVID-19 pandemic spurred unprecedented changes to how people access cancer care in Canada. Over just four days in March 2020, virtual care at Princess Margaret Hospital — Canada’s largest cancer centre — rose from two percent to 71 percent of visits. This dramatic pivot in health care delivery wasn't unique or short-lived.
Two years later, virtual appointments remain an important aspect of care for people living with cancer. A survey conducted by the Canadian Cancer Society (CCS) in January 2022 indicated that 79 percent of patients continue to meet with health care providers virtually.

This surge in virtual care has provided clear evidence of the promise this model of care holds. Using technology to facilitate medical appointments has been shown to increase access to care by making it more convenient, less costly, and less time-consuming than in-person visits.
But more needs to be done to improve and optimize virtual care equitably in Canada. Nearly half of the respondents to CCS’s 2022 survey reported that the quality of their virtual appointments was lower than in-person appointments.
This is unsurprising given how quickly virtual care shifted from an emerging area of exploration to an urgent and immediate need. Canada’s health care system — and cancer care system specifically — was simply not prepared to meet the unexpected demand. To better support people living with and beyond cancer in a post-pandemic world, we must invest in more research to advance our knowledge of the tools and resources needed to deliver effective, high quality virtual care.
Building a body of knowledge large enough to bring about meaningful changes in health care practices and systems can take a long time. Fortunately, initiatives like CCS’s new Centre for Cancer Prevention and Support (CCPS) — which brings together


researchers, clinicians and patients from across the country to share discoveries and implement learnings — can accelerate this process.
As a national hub of research and innovation, CCPS represents a new opportunity to translate research on virtual care into practice faster. That’s why, with the support of our donors and partners, the Centre is embarking on a journey to investigate and evaluate approaches to virtual care so that going forward, we can optimize the delivery of care and improve the patient experience.
While virtual care will never fully replace in-person care for people facing cancer, it can reduce the burden of medical appointments and ultimately enhance a person’s experience with cancer care. In a world where virtual care is becoming standard practice, we have a duty to invest in research to ensure this type of care meets the needs of those who will rely on it. Applying these research findings is the path forward for enhancing the future of cancer care delivery in Canada.











Kidney cancer can be a silent disease. Often there are no symptoms until it’s advanced and found incidentally by ultrasound or scan. When diagnosed at a more advanced stage, the options for treatment can be challenging.

Suggested causes of kidney cancer are smoking, obesity or family history. Symptoms can be flank or back pain, a lump or a thickening, and blood in the urine.
The diagnosis of a kidney mass doesn’t automatically mean that it’s kidney cancer. It’s possible that it’s a benign growth and doing a biopsy, or having it surgically removed, would determine the pathology and the type, stage, and grade of the mass and subsequently the next steps required. If the tumour is relatively small and localized (early stage), active surveillance with close monitoring and regular diagnostic tests, or surgery to completely remove the tumour are the most common treatments. There are options of surgery methods, depending on the size, position, and complexity of the
tumour and is performed by a urologist or uro-oncologist.
When the cancer is advanced, treatment opportunities are different and immunotherapy drugs offer excellent options for cancer that has spread. Systemic treatment would be prescribed and monitored by an oncologist and could be used in conjunction with surgery or radiation therapy.
Kidney cancer is a unique disease. There’s no cure, but there are many patients living and thriving. How the disease and treatment affect one patient can be completely different for another. It’s vital for Canadians diagnosed with or caring for someone with kidney cancer to educate themselves about the disease and treatment options so they can make the best pos-
sible decisions with their doctor for their individual situation.
Kidney Cancer Canada can help! We are a national community of patients, caregivers, and health professionals who work together to provide every Canadian touched by kidney cancer with support, information, education, and advocacy for treatment options. Programs and services are bilingual. Our website has a wealth of information, including our Video Knowledge Library presented by kidney cancer specialists from across Canada.
Resources are available on nutrition, exercise, mindfulness, and stress management and one-to-one peer support and our Coffee Chats offer a safe environment for patients and caregivers to talk, share experiences, and discuss all topics.









It’s vital for Canadians diagnosed with or caring for someone with kidney cancer to educate themselves about the disease and treatment options so they can make the best possible decisions with their doctor for their individual situation.