The magazine from Kidney Research UK

New living kidney donor buddy service
Page 3
Hope for people with diabetic kidney disease
Page 12


New living kidney donor buddy service
Page 3
Hope for people with diabetic kidney disease
Page 12

I’m excited to share with you the latest news from Kidney Research UK. Thanks to your amazing support, we’ve been able to take some big steps towards improving the lives of people with kidney disease.
One of the impacts of dialysis treatment is an increased chance of memory problems and cognitive impairment. On page 19, you can read about how your support is helping Professor Susan Francis use MRI scans to find out why.
Improving transplant success
Many kidney patients need blood
Contact the editorial team Kidney Research UK, Stuart House, City Road, Peterborough PE1 1QF 0300 303 1100 pressoffice@kidneyresearchuk.org
Website: www.kidneyresearchuk.org
Designed by www.adeptdesign.co.uk
Registered charity no. 252892. Scottish charity no. SC039245.
transfusions, but the treatment can trigger their immune systems to produce antibodies. These antibodies may impact the chances of a successful kidney transplant. On page 20, discover how you’re helping Dr Katrina Spensley find ways to reduce the development of antibodies.
Choosing to donate a kidney to someone is an amazing act of generosity, but it can be a daunting journey. On page 3, find out about the new service we’ve helped to launch to support kidney donors by pairing them up with someone who has already been through the experience.
Together we’re there for kidney patients at every stage of their journey. Thank you for everything you do for the kidney community. We really appreciate it.
Sandra Currie OBE, chief executive
Cover photo Kidney donor John Burns took part in our awareness-raising installation this winter. See page 3 for more news about our work on living donation.

The UK Living Kidney Donation Buddy Support Service was launched in December. Offering a secure and safe place for people considering donating a kidney to chat with someone who has first-hand experience of the living donation journey, it is run by the Robert Dangoor Partnership for Living Kidney Donation.
Support is essential for kidney donors and those around them, both before and after donating. This new service offers a place for potential donors, as well as their friends and family, to chat with someone who has first-hand experience and understands what’s involved in donating a kidney.
The service is provided through an online platform where buddies and users can set up a profile and manage appointments themselves. Potential donors and their loved ones then select a buddy based on age, location, ethnicity, gender and religious beliefs, depending on their own circumstances.
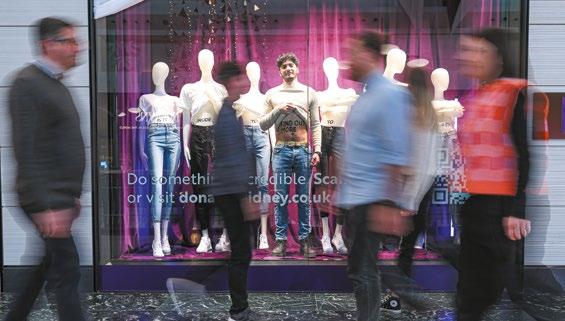
A thought-provoking window display was installed at Bluewater Shopping Centre this January by the partnership to encourage visitors to think about living kidney donation.
The Robert Dangoor Partnership was launched by Kidney Research UK and Give a Kidney – a charity devoted to living kidney donation –to raise awareness of living kidney donation, as well as support and guide potential donors through their donation journey.
People who have already donated a kidney and are interested in becoming a buddy can visit the website to find out how to get involved. Living donors’ loved ones can apply too.
By donating a kidney you are going to transform their life. You’ll be able to see the good you can do.
Prafula Shah

To learn more about the service and how to apply, visit the partnership’s website www.donateakidney.co.uk kidney disease ends here.
Play your part in supporting the kidney cause this World Kidney Day on Thursday 13 March and help raise awareness of kidney disease and kidney health.
Detecting kidney disease early is the most effective way of stopping it in its tracks, so lifestyle changes or specific medications can be introduced.
But awareness is low, 80% of people don’t even know what the kidneys do, so ensuring people know what symptoms to look for is vital. This year, our ‘Take a wee look’ campaign is designed to help people look for warning signs in their wee.
We have created posters and leaflets that explain how blood or protein in the urine can be a sign of kidney problems, and encourage people to take our online kidney health check.

We’ll be raising awareness ourselves, and we’re also asking you, our brilliant supporters, to help spread the word even further. Can you find new places to display and share our posters and leaflets – perhaps in your workplace, local café, church, mosque or temple?
“Our supporters will know how devastating kidney disease can be and we’re doing everything we can to stop people reaching kidney failure.
A simple poster has the power to encourage people to think about their kidney health. Together, we can save lives by spreading the word.”
Lucy Sreeves Executive director Kidney Research UK
Want to help?
Urine good company. To download or order our ‘Take a wee look’ materials, visit: www.kidneyresearchuk.org/ weelook
In November, we unveiled a new action plan making a series of recommendations to improve the diagnosis and treatment of chronic kidney disease in Scotland.
The action plan includes proposed measures to improve the monitoring of people with diabetes and heart disease who are at most risk of CKD, support GPs and other primary care staff to lead on diagnosis and management, and ensure patients can access specialist emotional, practical and digital support.
The plan was launched at an event attended by MSPs, patients and clinicians who discussed the urgent need for the Scottish Government to implement the action plan and prioritise the health of more than 600,000 Scots thought to be living with CKD, including 240,000 currently undiagnosed.
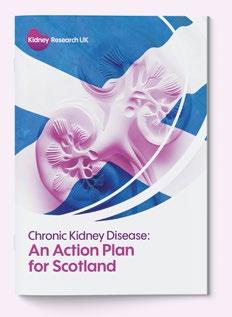
The plan was developed by a group of academics, clinicians and patients led by our former chair of trustees, Professor Jeremy Hughes, professor of experimental nephrology at the

University of Edinburgh. The group carried out extensive consultation with a wide range of stakeholders before publication.
Jeremy said: “It is possible to build a better future for people with CKD and this action plan shows the Scottish Government how this can be achieved. This investment is vital to avoid the looming nightmare of thousands more people requiring exhausting, expensive dialysis, as predictions based on existing data show. Embedding and prioritising CKD in Scottish government and public health policy is the only way forward.”
Scotland’s Minister for Public Health and Women’s Health, Jenni Minto attended the launch, and welcomed the plan, saying that the Scottish Government would consider its recommendations. kidney disease ends here.
The start of 2025 held special significance for Kidney Research UK, as our chief executive Sandra Currie was named as the recipient of an OBE.
Sandra has been named as an Officer of the Order of the British Empire (OBE) in recognition of Services to People Affected by Kidney Disease, in the King’s 2025 New Year Honours list.

Having been CEO for more than 12 years, Sandra has overseen significant growth in the charity’s activities and research funding, with more than £71 million invested in research in the last decade, alongside raising awareness of the disease and championing the needs of kidney patients and their loved ones amongst government, NHS, policy makers and industry.
Around 7.2 million people in the UK are already living with kidney
disease, a number that is predicted to grow partly due to the increase in risk factors such as diabetes, heart disease and high blood pressure.
“For patients, their families and anyone working in the field, the devastation that kidney disease causes to people’s lives is well known,” said Sandra. “Yet, despite it affecting around ten per cent of the UK population, there is still a long way to go to make recognising, preventing and treating kidney disease a real priority.
“Every day in the UK, around 23 people need to start ongoing and challenging treatment because their kidneys have failed.
This award not only recognises the significance of kidney disease, but also the commitment of the charity and our partners in responding to the challenge.”
Sandra Currie Chief executive Kidney Research UK
A study we helped to fund has revealed that blood tests can predict the severity of Covid-19 infection in kidney transplant patients and could lead to individualised approaches to vaccination.
The Mass Evaluation of Lateral Flow Immunoassays for the Detection of SARS-CoV-2 Antibody in Immunosuppressed People (MELODY) study was led by Dr Michelle Willicombe from Imperial College London and was published in The Lancet. Involving over 28,000 patients it investigated whether people on immunosuppressants developed antibodies against the virus that causes Covid-19, following a minimum of three vaccinations.
Antibodies to Covid-19 were found in 76% of kidney transplant patients, with health records showing a reduced number of infections and hospital admission following infection in this group compared to those without antibodies.

Dr
Michelle said: “MELODY has shown it is possible to individually assess vaccine response and the risk of severe outcomes following Covid-19 infection in this group. This information has the
potential to support personalised approaches to Covid-19 prevention for at-risk patients, such as individualised vaccination schedules or treatments.”
Factors found to be related to higher rates of infection across all participants groups included on-going shielding and living in a household with children.
Michelle commented: “Vaccination has improved the outcomes of Covid-19 infection considerably for most patients, but we know that we will face outbreaks of viruses in the future. MELODY has provided valuable information on how best to protect at-risk populations both in terms of behavioural changes such as shielding, and vaccinating, based on personal circumstances. This knowledge can be applied to inform ongoing Covid-19 risk and also outbreaks of other viruses, should they occur.”
Michelle Willicombe kidney disease ends here.
Without knowledgeable, skilled researchers working on the big questions in kidney disease there will be no research breakthroughs for our community.
Alongside supporting new researchers to investigate key areas of interest for patients with kidney disease, and supporting skills development, we are also committed to helping those whose research careers have paused, to return to research. Donate to
Our joint fellowships with the Daphne Jackson Trust support researchers wishing to return to kidney research, following a career break for family, caring or health reasons, enabling them to contribute much-needed scientific progress in kidney disease. We caught up with University of Plymouth based researcher Dr Jane Carré, who was awarded this fellowship in 2019, about her experience with it and what it has meant for her career.
Jane’s work involves looking at mitochondria (specialised parts of the cells in our body that convert fuel from food into energy) and the role that they play in the muscle weakness experienced by those living with chronic kidney disease. This research will also help doctors to identify the patients most at risk of early muscle loss and predict more effectively when different people could respond best to nutrients, exercise, or new treatments.
“During my maternity break I had a conversation with a previous recipient of a Daphne Jackson Fellowship. I told them I was interested in using my longstanding research interest to understand the loss of muscle function in chronic kidney disease (CKD) and they explained what a wonderful opportunity the fellowship had been for them. Coincidently, the advert had just come out, so I applied. I am so grateful that I was given one of the few opportunities to have a second chance at a research career, allowing me to continue my work supporting better outcomes for kidney patients.
“The fellowship also offered a fantastic training element. After being out of research for a while, it was really important for me to build my confidence and develop new skills.
“The fellowship has allowed me to build a long-term career in kidney research. Without it, I probably
would have pursued a teaching route because I could not see how balancing a young family with a research career was possible and being out of the lab for a while also affects your confidence.
“Overall, my Daphne Jackson Fellowship has given me a sense of pride and ownership of my research project. I cannot sing praises of the Daphne Jackson Trust and Kidney Research UK enough for the support that they have given.”
Jane now leads a research group at the University of Plymouth looking at muscle loss and has recently taken on a PhD student to help her take this work further.

Dr Jane Carré
Thank you to our supporters, thanks to whom we can invest in our researchers and build research capacity so that together we can make a difference to patients.
kidney disease ends here.
Researchers at the University of Manchester are striving to prevent childhood kidney disease by building on a previous project in urofacial syndrome, (UFS) a disease which causes urinary problems and impedes a patient’s ability to smile.
We have already shown that gene therapy can be successful in laboratory models of certain inherited bladder disorders that cause kidney failure. The latest funding from Kidney Research UK will allow us to take the next steps to bring gene therapy closer to patients by identifying how best to use these treatments in human tissue, while also looking at whether this approach can work in other related disorders.”
Dr Neil Roberts

Dr Neil Roberts received a fellowship from us in 2015 and, together with his colleagues, showed how gene therapy could potentially be used to treat the cause of UFS.
In this syndrome the nerves and muscles in the bladder do not work together well, which can lead to multiple severe urine infections, followed by kidney damage. UFS also impacts facial control, particularly in relation to smiling. Dr Neil Roberts

Gene therapy is a technique where a faulty gene is replaced or altered to treat or prevent disease. Conditions that result from changes to a single gene are particularly good candidates for gene therapy. Gene therapy offers hope of new and effective treatments for certain inherited medical conditions that are not currently curable. By targeting the cause of disease, and preventing the symptoms from ever developing, this approach has the potential to offer substantial quality of life benefits by removing the need for ongoing medical interventions such as surgery.
Neil and his colleagues had found that, in UFS, changes (or mutations) in a gene called HPSE2 meant that muscles that control bladder emptying are unable to properly stimulate the bladder muscle. They were able to show that by putting a non-mutated gene back into the bladder nerves, they could restore near-normal bladder function in laboratory-based models. Having been awarded a studentship grant of £84,000 last year, Neil is now working with his PhD student to build on these learnings and take the next steps on the long road towards a treatment for patients with different kinds of bladder disease.
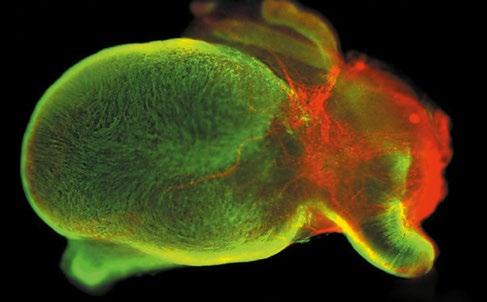
In collaboration with Professor David Long from University College London and Professor Adrian Woolf from the University of Manchester, the team will investigate how best to deliver gene therapy to human tissue samples. In addition, they aim to develop a long-term strategy to enable this approach in other inherited urinary tract and kidney conditions. Together with patient groups, they aim to understand current treatments, unmet needs and attitudes towards new therapies. This exciting research could have a massive impact on families like mine. Since birth my daughter, Izzy, has faced multiple interventions and procedures which you wouldn’t wish on an adult, let alone a child. To think that interventions such as catheterisation could be eliminated or only be a temporary measure in the future would greatly improve this emotionally draining part of living with kidney disease.”
Emma Headings
kidney disease ends here.
An international team led by researchers from the University of Bristol, has identified key molecules and pathways involved in the development of diabetic kidney disease, which could lead to future treatments. The research, directed by Dr Abigail Lay and Professor Richard Coward, was funded by Kidney Research UK and recently published in the journal Nature Communications.

Professor Richard Coward
Diabetic kidney disease is a leading cause of kidney failure in the UK. Despite this, our understanding of the mechanisms leading to kidney damage in patients with diabetes is incomplete and new approaches to protecting the kidneys of individuals living with diabetes are needed. Greater knowledge of the pathways and changes that lead to reduced kidney function is crucial for developing new treatments and diagnostics.
Richard applied to Kidney Research
UK for a grant to investigate how kidney cells react to the changes in the body that happen when a person has diabetes. By comparing different types of kidney cells from patients with and without a key feature of diabetes, known as insulin resistance, Richard and colleagues were able to identify several unknown changes in genes, cell communication pathways and protein production that are linked with diabetic kidney disease.
“We know that insulin resistance is important for the development of kidney problems in diabetic patients, and this study has allowed us to identify some of the changes to cells that happen during this disorder,” Richard said. “Importantly, we have pinpointed several alterations that occur in the same way in many key cell types within the kidney; this provides us with important new treatment targets that could protect different elements of kidney function.
“By better understanding the changes that occur, this work may also support new ways of detecting kidney damage earlier, and monitoring kidney health, in individuals living with diabetes.”
Identifying the precise changes that happen in the kidneys of patients living with diabetes is key to understanding the underlying mechanisms of the disease and providing new treatment targets.
Richard said: “This is a great first step towards new treatments for diabetic kidney disease, but more work is needed.”
We are determined to find ways to tackle diabetic kidney disease. By providing detailed information on genes and pathways involved in diabetic kidney disease, Professor Coward’s work takes us one step closer to a more complete understanding of this condition, but also towards discovering new targeted agents to prevent it.”
Dr Aisling McMahon Executive director of research Kidney Research UK
Having access to expert information, tips and resources is vital in making decisions about your kidney health and navigating the challenges of kidney disease.
In this section, you will learn more about holidaying when you are in kidney failure, and about the online platform Kidney Beam.
Going on holiday and leaving everyday cares behind is one of life’s joys. However, if you’re living with severe kidney disease, planning a trip away can come with many additional considerations.
For dialysis patients, the need to be connected to a machine for treatment multiple times each week makes taking a holiday more challenging.
Paul Cookson, a dialysis patient from Cambridge, says: “Like anyone, kidney patients deserve a break, whether that’s abroad or in the UK.
A holiday for me isn’t a break from dialysis, but it is a change from my day-to-day routine which is important. There is a lot of extra planning involved but I’ve been fortunate to have support from a holiday coordinator on my dialysis unit and a specialist company, who have helped me arrange dialysis abroad.
“This does not always have to be difficult or expensive, particularly in the European Union and countries with a reciprocal healthcare agreement with the UK. You just need to plan with your care team in advance, obtain travel insurance and book your holiday accommodation and activities around your dialysis sessions.”
Waiting on the transplant list can be an uncertain time. That call could come at any time and patients need to be able to travel to hospital when it does. But do you have to put your life on hold?
Miranda Wilkinson, transplant coordinator at James Paget University Hospital in Norfolk says: “It is possible for someone on the renal transplant waiting list to go on holiday, but they need to inform their transplant coordinator and would usually be suspended from the waiting list for the time they are away, unless they stay locally.
“Once the patient returns home, they would need to advise their transport coordinator so they can be re-activated straight back on to the waiting list, provided they remain in good enough health.”
Miranda also advises ensuring you have travel insurance in case you receive your transplant just before your holiday and need to cancel to recuperate.
Travelling abroad is not advised for at least six months after receiving a transplant, but if all is well after this time, a new kidney certainly offers more freedom.

Post-transplant patients must still take steps to protect their health though, particularly as they are at increased risk of skin cancer because of the immunosuppressive medication that helps to protect their transplanted kidney.
Nephrologist Professor Claire Sharpe, says: “Taking care in the sun is extremely important for transplant patients to reduce their risk of skin cancer. Sunburn or a tan is a sign of skin damage and there are ways to prevent this. Using sunscreen with SPF 50+ and at least 4-star UVA protection is recommended, reapplying every two hours, or immediately after swimming. No sunscreen provides 100% protection, so wearing sun-protective clothing and hats can also help keep people safe. Sunbathing should be avoided, and people should stay out of the sun to find shade, especially between 11am and 3pm, to limit risk.”
For more information and tips, visit www.kidneyresearchuk.org/ holidays
kidney disease ends here.
.
The new year enthusiasm for looking after ourselves and doing more exercise may be subsiding, but help is on hand for kidney patients through the online platform, Kidney Beam.
Kidney Beam offers live and on-demand exercise classes led by professional physiotherapists, tailored specifically to people with kidney disease. You can dip into classes that are organised by fitness/ wellness level, or follow an exercise, nutrition and wellbeing programme, all from the comfort of your home.
It was launched in 2020 by renal physiotherapist Professor Sharlene Greenwood in conjunction with the developers at Beam, as a way of reaching patients denied access to renal rehabilitation clinics due to the Covid-19 pandemic. It has become an enormous success and the team’s ambitions have expanded.
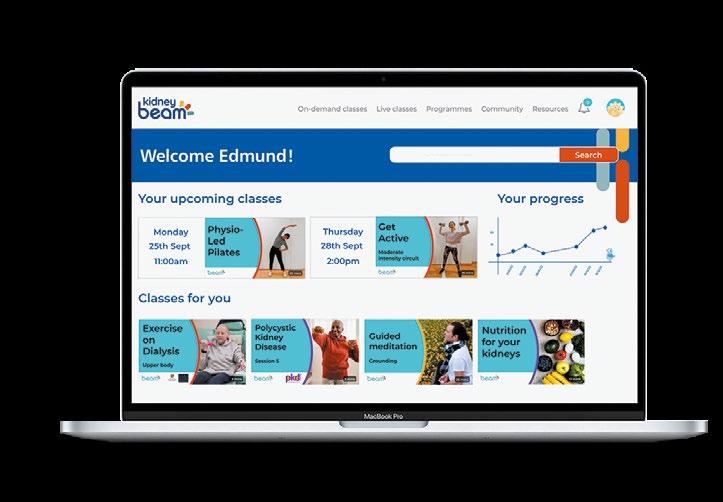
Thousands now use the platform, appreciating the sense of community it provides.
Prior to Kidney Beam, access to rehabilitation services for people living with kidney disease was not routinely offered by the NHS, with very few kidney-specific physiotherapists in the UK. We hope to have the potential to reach any kidney patient living in the UK.”
Professor Sharlene Greenwood
Living with a chronic condition can be a very lonely place. You don’t really know what’s around the corner. When I log on to Beam to do my exercises, I’m met with so many lovely people who are all passionate about improving their lives and their company is something that helps me get through it.”
Edmund England kidney patient
When Kidney Beam was first conceived, we knew how important it was to approach it academically and show whether it would work for patients, as renal rehabilitation had always been delivered in a physical setting and there was little precedent for delivering it online. So we awarded the Beam team a research grant. With support from King’s College Hospital NHS Trust, they ran a clinical trial, which has confirmed that people using the platform see improvements in their mental health, their physical function, their energy levels and their ability to selfmanage their condition.
Since these positive outcomes, we’ve made an investment into the platform to help ensure the service continues to be available to patients.
My dad’s definitely changed as a result of using Kidney Beam. The classes have helped him come out of his shell and it’s given him a more positive outlook on everything. He’s enjoying exercise – I’m really pleased he’s got Kidney Beam in his life.”
Corinne, daughter of kidney patient Edmund
What’s on offer – all resources are tailored to different levels of fitness:
Live and on-demand classes including:
• Mobility and flexibility
• Strengthening exercises
• Nutrition
• Meditation
• High intensity interval training
• Dance
• Yoga Programmes – a series of classes with set objectives –including:
• Exercise on dialysis to keep you moving through a long session in the dialysis chair
• Yoga for balance and harmony
• Kidney strong to increase whole body strength and endurance
• Intermediate cardio
• Menopause pilates
Kidney Beam is now more accessible to UK kidney patients. Visit: www.kidneybeam.com
Thanks to you, our supporters, we’ve pledged to fund a number of new projects in the last few months. Here’s just a selection, with thoughts from some of our readers about the difference they will make.
Professor Susan Francis and colleagues from the University of Nottingham have received a start-up grant of £40,000 to look at how salt and water levels change in the brains of patients undergoing haemodialysis.
Patients receiving haemodialysis are three times more likely to develop problems with memory and other thought-related processes (known as cognitive impairment, or CI). The reasons for development of CI in these individuals is unclear. Using special types of magnetic resonance imaging (MRI) scans, the team will look at salt and water levels in different parts of the brain tissue, which could indicate brain tissue health. These levels will be measured in patients before and after haemodialysis and compared to participants who are not on haemodialysis. Participants will also complete problem-solving tasks and a memory test.
This work will help us to understand how haemodialysis patients are impacted by CI. Having a clearer


understanding of how haemodialysis impacts the brain could help identify new ways to support these patients and inform future research to develop ways of preventing CI.
Dialysis is a vital, life-sustaining treatment but its impact on brain functions like memory can affect patients’ everyday lives. Understanding the stress on the brain during dialysis could help us to improve treatments in the future.”
Professor Susan Francis
As a haemodialysis patient, this is very interesting. My memory, especially for words and names of things is shocking, I’ve put this down to toxins in my system but to now hear it could be down to haemodialysis makes me want to know more! I look forward to reading the outcome.”
Angela
Riley, in-centre haemodialysis patient
Dr Katrina Spensley from Imperial College London has received a training fellowship of £290,000 to look at improving blood transfusion methods to prevent later risk of kidney rejection and ensure the greatest number of potential donor matches.
Doctors must seek the closest possible match for kidney transplantation, but the same does not happen routinely for blood transfusion recipients. This may lead to the development of antibodies.


The presence of antibodies can reduce the likelihood of finding a compatible donor kidney and also impact the long-term health of transplanted kidneys. In this project, Katrina will look at which kidney transplant patients develop harmful antibodies following blood transfusion and then develop a computer programme to select the best unit of blood for an individual.
We need to understand more about how the immune system responds to blood transfusions. This project aims to improve access to kidney transplants and increase success rates by reducing the development of antibodies in patients who need a transfusion.”
Dr Katrina Spensley
I suffered with anaemia like many kidney patients and blood transfusions helped greatly during that period. But they are a balancing act as antibodies can make finding a kidney transplant harder and put those transplanted at risk of rejection, so this project is one I am particularly pleased to hear about.” Carla Thompson, kidney patient
Mr James Bennett from the University of Liverpool has received a Kidney Research UK Allied Health Professional Fellowship award of £140,000 to look at developing a special filter to remove a substance toxic to the kidneys released by red blood cells during some types of surgery. This will build on previous Kidney Research UK-Stoneygate funded work.
Over 60% of patients who have surgery to repair the thoracoabdominal aorta (a large artery) get acute kidney injury (AKI). During surgery, blood flow to the section of artery needing repair is stopped and may be redirected through a machine and returned to the patient. This can damage red blood cells, releasing their contents into the blood, including a protein called haemoglobin which can be broken down into compounds harmful to the kidneys.
James will pass blood from surgical patients through a filter that binds to haemoglobin to remove it from the blood and will then add this to kidney cells to observe their response and survival.

Thoracoabdominal surgery can prevent a potentially fatal aneurysm rupture in patients at risk. Understanding the kidneys’ response to essential blood processing during surgery could inform interventions to reduce the risk of AKI for these patients in the future.”
Mr James Bennett
Reading that so many things can go wrong before and after surgery is scary, but it is nice having the faith that some risks can be potentially removed because of research like this.”
Simon Elmore, a patient soon to undergo surgery
Thank you to all our Team Kidney heroes for your help in our mission to end kidney disease. We can’t do it without you!
On Sunday 27 April, more than 50 fantastic people are running for us in the TCS London Marathon.

Liam Ward, 31, from Gloucester, says: “My kidney disease has had a huge impact on my life, preventing me from pursuing my dream job in the army. Before my transplant I would be out of breath walking to the end of my street. Now I’m training to run the London Marathon!
“Giving back to Kidney Research UK is important to me, as I want to support a charity that has helped give me a better life, by making research possible.”
Good luck to everyone who is training hard for the big day!

Thank you to everyone who has registered for our virtual and in-person March March events this year.
Supporters are invited to join the fight against kidney disease at our five-mile Peterborough March March on Sunday 29 March. Becca Moore is bringing a group of family and friends.
Becca says: “Kidney disease turned my life upside down. Walking the Peterborough March March will help raise awareness and fund research which will change the future for people like me, who live with kidney disease.”
Meanwhile, supporters across the UK will unite for the virtual March March, walking 10,000 steps a day, across the month of March.
Stephanie Roche, from Kettering, completed the challenge in 2024: “I loved going on new walks throughout the month. I’m so proud we raised so much money to make a big difference to the lives of people living with kidney disease.”
Sign up here: www.kidneyresearchuk.org/ support/events
kidney disease ends here.
A special thank you to Vidur Dindayal, who is funding a kidney research project in memory of his late wife Sabita.
Vidur and Sabita met in Guyana in 1953 and were married for 60 years before she died with kidney disease in 2019.
Vidur says: “I was lucky to be married to Sabita and miss her a great deal. She had all the best qualities in a human
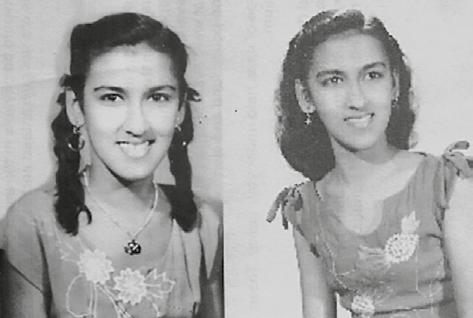

being. She was incredibly caring and was always there for her family and people in the local community.
“We knew Sabita was coming to the end of her life, but she was always determined to enjoy her time and look after others.
“It’s important to me to leave a gift and keep Sabita’s name alive. We should all strive to make other people’s lives better and happier. I hope Sabita’s research project will achieve that for kidney patients and their families.”


Patients are an integral part of our research funding rounds. Colette McLaughlin joined our lay advisory group in March and has played a vital role in ensuring the patient voice is represented at our grants committee panel meetings.
Colette reads through applications from researchers and attends meetings to present feedback on these, to explain what patients feel about the proposed projects.
Mae Law, public and patient manager says: “This is such an important step in decision making, to ensure we are funding projects that are important to patients and people like Colette make sure that patient voice is heard.”
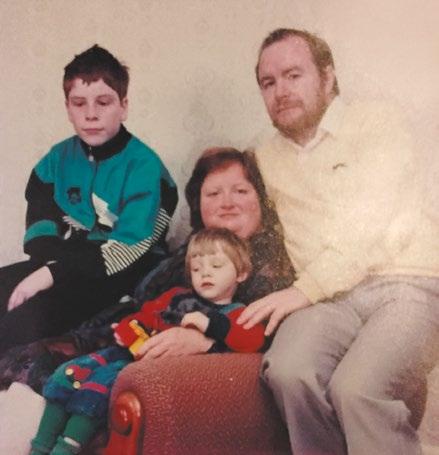
John Walker from Stockport is leaving a gift to kidney research in his will, in memory of his wife, Elaine, who died aged 49, following her 30-year battle with kidney disease. John, aged 74, says: “I knew quickly that Elaine was the one for me and we were married for 27 years. She was bright and determined, but kidney disease significantly affected our lives and took her away far too young.
“It’s hard to see people going through the same things. That’s why I send regular donations and am leaving a gift in my will, to prevent more families being devastated by kidney disease.”
kidney disease ends here.
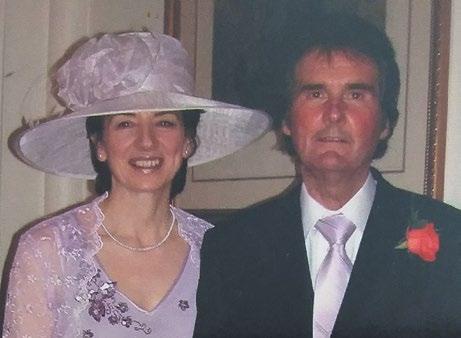
We’re very grateful to Evelyn Notman, from Cowdenbeath, for raising funds in a tribute to her husband Martin, who had been one of the longest-surviving kidney transplant recipients. He died in May 2024, having lived with his transplanted kidney for over 52 years.
Evelyn says: “We met at 18 years old and were

about to celebrate 55 years of marriage before he died.
“Martin needed dialysis at 23 years old, and I was told he wouldn’t survive. Thankfully he had his successful transplant in 1971.
“Supporting research in his memory is important to me. I don’t want other families to have to go through what we did.”
A huge thank you to our volunteers, who continue to do amazing work to raise awareness of kidney disease.
Lady Rukhsar helps at her former dialysis unit and displays leaflets in GP surgeries in Birmingham. She says: “It’s important to me to give people the knowledge to feel less alone in navigating treatment.”

Thank you to our supporters who raised more than £17,000 by walking 120km in our BIG Purple Dog Walk, including Winnie, a four-year-old black labrador. Owner Danielle Smith said: “Winnie is always there for us and was the perfect dog to join in because of her energy levels!”


Make a note of these key dates and visit our website to register your interest in our events.
Virtual March March
March 2025
World Kidney Day
Thursday 13 March 2025
Peterborough
March March Saturday 29 March 2025
London Marathon Sunday 27 April 2025
The Big Garden Party Saturday 24 – Monday 26 May 2025
Newcastle Bridges Walk Sunday 8 June 2025
Andy Cole Golf Day Wednesday 18 June
London Bridges Walk Sunday 6 July
Glasgow Bridges Walk
Sunday 31 August 2025
Great North Run
Sunday 7 September 2025
Liverpool Bridges Walk
Sunday 14 September 2025
kidney disease ends here.
