4 minute read
Increasing Awareness of Pressure Ulcers in Those with Physical Limitations Due to Disabilities
By Rebecca Wang and Christina Pierce
What are pressure ulcers?
Advertisement
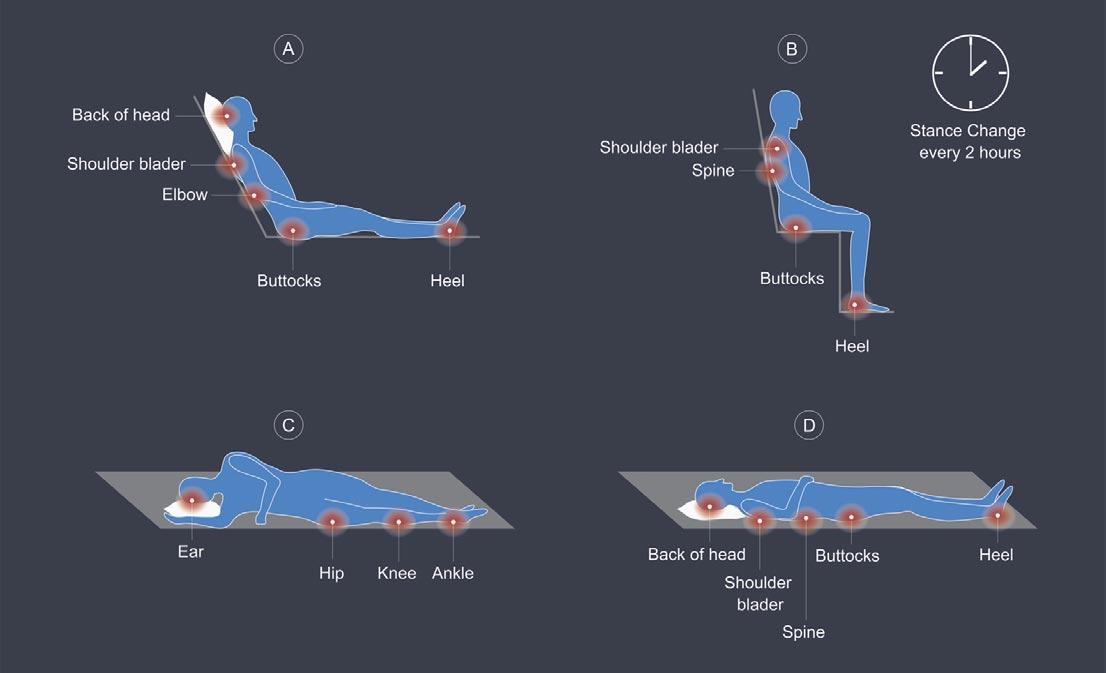
Decubitus ulcers, commonly referred to as pressure ulcers or “bed sores,” are injuries of the skin or soft tissue that occur due to lack of movement and remaining in the same position for prolonged periods of time.1 Continued pressure in a specific region of the body, such as the hips, tailbone, ankles, and heels, lead to damage and injury of the skin causing pressure ulcers to develop.2 Pressure ulcers can first appear as a scrape or blister with the area of skin being discolored in comparison to the surrounding healthy skin. In those unable to feel physical pain, pressure ulcers can progress rapidly before being detected. The development of pressure ulcers can lead to infection and physical deformities which can further exacerbate underlying health conditions.
Who is at risk of developing pressure ulcers?
Those with disabilities ranging from physical limitations, mental challenges, and psychological conditions that are unable to change positions without assistance and/or remain in bed for long periods of time are at risk of developing pressure ulcers. Specifically, patients with certain conditions that cause impaired consciousness, lack of sensation, or decreased mobility all increase the risk for developing pressure ulcers, such as patients with cardiovascular or neurologic disease, patients under prolonged anesthesia or surgery patients.1 In these patients, the lack of sensation of pain or discomfort causes them to be unaware of the developing ulcers and thus not change positions to relieve pressure from their bodies. Additionally, many of these patients are also physically incapable of moving their own bodies. Many internal factors can also increase the risk of developing pressure ulcers such as malnutrition, anemia and fever.1
Pressure ulcers are very common in elderly or debilitated populations. A study demonstrated that 83% of patients in one hospital who developed pressure ulcers did within five days of admission.1 Additionally, elderly patients are more at risk for developing sacral pressure ulcers with approximately two-thirds of ulcers occurring in patients 70 years and older. Another study determined that most of the patients who developed ulcers were ICU-level care patients.1 Almost 60,000 patients die each year due to complications from pressure ulcers.3
What are the complications of pressure ulcers?
A patient who remains in the same position for even two hours can create the basis of a pressure ulcer.1 With long-term pressure on blood vessels, capillary beds can become occluded and blood flow can decrease to the surrounding tissue.1 With time, the tissue can become ischemic and release toxic metabolites.1 Finally, the ulcer can develop and tissue necrosis can occur.1 External factors, such as moisture from the skin or urine in immobilized patients or friction between the skin and material, e.g., the bed or clothing can worsen the developing ulcer and lead to breakdown within the skin.1
Infection is the most common complication of pressure ulcers. Both aerobic and anaerobic bacteria can infect the open wound.1 With deeper wounds that expose bone, such as pressure ulcers on the ischium, trochanters, sacrum, or heels, severe infections such as osteomyelitis or septic arthritis can form.1 Osteomyelitis requires prolonged, high-dose antibiotics for treatment, and septic arthritis often requires surgical intervention. Additionally, in a patient population that is already debilitated, an infection can adversely affect patient recovery and be challenging to manage. Due to the catabolic nature of pressure ulcers, other complications that can develop include severe protein and fluid loss, leading to malnutrition and anemia.1
There are no clear studies documenting the exact prognosis of pressure ulcers. However, lifelong treatment of these ulcers and prevention are often required to manage debilitated patients who develop pressure ulcers.1 Pressure ulcers in the sacral region are also highly susceptible to recurrence.1 Additionally, patients with underlying chronic conditions, such as diabetes, malnutrition, hypoxia, or older age are all at increased risk of decreased wound healing.3
What is the prevention and treatment for pressure ulcers?
The most crucial treatment for pressure ulcers is prevention. The current standard of care is turning and repositioning the patient in twohour intervals to prevent prolonged pressure on any one body part.1 However, items such as pressure dispersion cushions or supportive mattresses can all be used to relieve pressure on specific body parts and prevent ulcers.1 Proper skin care and usage of urinary catheterization or rectal tubes for patients with incontinence can also prevent skin barrier damage and the development of ulcers.1 Additionally, patients at risk for developing pressure ulcers should not be bathed with harsh products such as soaps, hot water, or lotion with alcohol, as they can all dam- age the protective skin barrier.3 Daily skin examination is essential to identify any signs of pressure ulcers.
Once a pressure ulcer develops, antibiotic coverage is the standard of care to prevent sepsis.1 The depth of the ulcer measured by the National Pressure Ulcer Advisory Panel (NPIAP) must be determined, as deeper wounds, usually Stage II or IV, may require surgical treatment.1 The ulcer must be cleaned thoroughly to remove dead tissue and prevent infection. Hydrocolloid dressings are often used to provide a moist environment for proper wound healing.1 Proper nutrition must be maintained for the patient to promote proper wound healing, and the patient should ambulate with physical therapy as often as possible.3
The management of pressure ulcers requires a team - which includes primary care physicians, dermatologists, home and wound care nurses, rehabilitation professionals and surgeons. It is important to reduce or relieve pressure on the skin, debride the necrotic tissue, cleanse the wound, and maintain clean wound dressings that are changed periodically to manage the bacterial load and colonization of the wound.4 Therefore, it is important to prevent the development of pressure ulcers through education to prevent hospital admissions and their associated costs.
What can be done to increase awareness?
Patient education is an excellent way to increase awareness of pressure ulcers. By teaching patients about the prophylactic treatment and turning every two hours, patients can take charge of their own care. We encourage those with physical limitations to request help with moving if they have not been repositioned within two hours. Additionally, educating patients’ families about pressure ulcers and prevention can help arm the families with tools to take care of the patients once they have been discharged from the hospital.
Resources
1. Zaidi, S. R. H., & Sharma, S. (2021). Pressure Ulcer. In StatPearls [Internet]. StatPearls Publishing.
2. Bedsores (pressure ulcers). Mayo Clinic. (2022, April 19). Retrieved January 18, 2023, from https://www.mayoclinic.org/diseases-conditions/bed-sores/symptoms-causes/syc-20355893
3. Al Aboud, A. M., & Manna, B. (2018). Wound pressure injury management.
4. Bluestein, D., & Javaheri, A. (2008). Pressure ulcers: prevention, evaluation, and management. American family physician, 78(10), 1186-1194.









