PUBLISHED BY: Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER: Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
GRAPHIC DESIGNER: Jennifer Nelson jennifer@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com
SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE: Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2025 SmithPrint, Inc. PRINTED IN THE USA



John Shepherd, MD, President
Lyssa Ochoa, MD, Vice President
Jennifer R. Rushton, MD, President-Elect
Lubna Naeem, MD, Treasurer
Lauren Tarbox, MD, Secretary
Ezequiel “Zeke” Silva, III, MD, Immediate Past President
Woodson “Scott” Jones, Member
John Lim, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Saqib Z. Syed, MD, Member
Nancy Vacca, MD, Member
Col Joseph J. Hudak, MD, MMAS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School Representative
Cynthia Cantu, DO, UT Health Medical School Representative
Lori Kels, MD, UIW Medical School Representative
Ronald Rodriguez, MD, UT Health Medical School Representative
Alice Gong, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
BCMS SENIOR STAFF
Melody Newsom, CEO/Executive Director
Yvonne Nino, Controller
Al Ortiz, Chief Information Officer
Brissa Vela, Chief Membership and Development Officer
Jacob Hernandez, Advocacy and Public Health
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Jennifer C. Seger MD, Chair
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. Jyothula, MD, Member
George-Thomas Martin Pugh, MD, Member
Adam Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Amith Skandhan, MD, Member
Francis Vu Tran, MD, Member
Subhashini Valavalkar, MD, Member
Louis Doucette, Consultant
Brissa Vela, Staff Liaison
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Ayomide Akinsooto, Student
Elizabeth Allen, Volunteer
Rita Espinoza, DrPH, Volunteer
David Schulz, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer

By John Shepherd, MD, President, Bexar County Medical Society
One of the things I really love about traveling is randomly wandering the streets of a new place, discovering what it has to offer. Durian fruit in the markets of Vietnam — rated zero stars — do not recommend. A beer made from the Calafate berries in South America — five stars — highly recommend. Giant bugs on a stick in Bangkok — can’t give you a recommendation because I just couldn’t do it. Then there are the people, the children, the performers. Have you ever seen the guy on the street corner with the tip jar along with a harmonica, drums, symbols and an accordion or guitar? He starts on one instrument, adds a little vocal lyric, attempts to blow the harmonica around his neck while using his foot to activate a pedal to bang the drum. It’s impressive, isn’t it, for all the things he tries to make work on his own … that one-man band.
As physicians we often pride ourselves on our individual skills and achievement, and rightly so. We’ve all dedicated years to education, training and honing our expertise to provide the best care possible. However, while being a “one-man band” may seem admirable, it also has its limitations. No matter how skilled a physician is in their specialty or how committed they are to advocacy, no single practitioner can address the multitude of needs within the practice of medicine. Just as the performance of a one-man band pales in comparison to the richness of a symphony, a single physician is far less effective advocating for the needs of our profession than the collective strength of the medical community, particularly when united through organizations like the Bexar County Medical Society and the Texas Medical Association.
For many of us, the simple practice of medicine isn’t quite as simple as it used to be. We now grapple with pre-authorization hassles, narrow insurance networks and a landscape of increasing regulations coupled with declining reimbursement rates. There are the constant challenges to scope of practice with everyone wanting to do what physicians do but without the education, training and certifications we have. Not to mention, attacks on established science and fundamental public health principles. It’s no surprise that these pressures add stress for all of us and contribute to high levels of physician burnout with close to 400 physicians choosing to take their lives each year … a rate significantly higher than the general population. How do we combat this? Together … We do it together.
As physicians, we hold the doctor-patient relationship sacred, working hard to maintain it, protecting it at all costs. To protect this and other facets of medicine, we need to worry about another relationship … the legislative relationship. Our elected officials control so much about medicine: Medicaid and Medicare reimbursement rates; graduate medical education funding; and maintaining boundaries on the scope of practice. It’s essential that we develop the type of relationships with them so that WE become the trusted voice when they have questions about how to best serve Texas patients and how to best serve

Texas medicine. Make no mistake about it, there are other groups in their offices telling them their truths and wants: independent practice and prescribing without physician oversight for nurse practitioners; direct access for physical therapists without any examination by an orthopedist or other physician; and test and treat for pharmacies. If they are not hearing OUR voices, they are listening to someone else’s.
I ask you to join me in amplifying medicine’s voice at the Capitol. Serve on the legislative committee, attend a fundraiser, volunteer for a campaign, thank a legislator for doing something in your community, and show up at First Tuesdays. Seeing the white coat invasion at the Capitol is a sight that makes you proud to be part of Texas Medicine. If you don’t do anything else, let your checkbook do the work by becoming a TEXPAC member. Electing candidates who have open ears and open minds to the needs of medicine is half the battle.
When I look at our membership, I see so many community leaders, physicians, Alliance members, medical students and mentors — each of you choosing to be engaged with the Bexar County Medical Society because you support organized medicine. I believe you want what I want … the best not only for physicians but the best for our patients and communities we serve. Our diverse specialties and perspectives strengthen us, creating a robust organization, but we have the potential to become even stronger and more influential. By inviting someone you know to join the Society or the Alliance, you amplify our impact. It may sound cliche, but there is undeniable truth in saying “strength in numbers.” A strong Society enables us to protect the integrity of the practice of medicine. A strong Alliance allows us to expand our reach as they put outreach programs in our community and work to make strong bonds with state, county and local leaders in the name of medicine. Think about it. How will you help us grow? Who will you ask to enhance our collective voice?
To all of you, thank you for being a member of the Bexar County Medical Society or the Alliance. I know you have a choice about where to spend your time, your efforts and your finances. I thank you for choosing medicine and I thank you for trusting in me to lead Bexar County medicine forward this year as your president.
John Shepherd, MD, 2025 President of the Bexar County Medical Society, has been an active lobbyist for the Family of Medicine at the Texas State Capital and has held several “Party of Medicine” events, introducing physicians on how to get involved with legislation that affects medical issues. He has been Chief of Surgery at Christus Santa Rosa Children’s Hospital, a past member of the Board of Directors of Tejas Anesthesia, and currently serves on the BCMS Legislative Committee. Dr. Shepherd served as Secretary on the BCMS Board of Directors for 2023.

Our Alliance welcomes members to an amazing opportunity to celebrate our special bond of medical family friendship, and highlight the value of our social and professional connections. We strike a balance between purposeful, mission-driven community service like our award-winning Period Poverty Project; legislative advocacy like our support of First Tuesdays at the State Capital; and fun, membership bonding events like our Pink Out! Fall Luncheon. Join us and BE THE FAMILY OF MEDICINE!
Victoria Kohler-Webb BCMSA Immediate Past President
Bexar County Medical Society Alliance 2025 Steering Committee
JENNY SHEPHERD Acting President
VICTORIA KOHLER-WEBB Immediate Past President
DANIELLE HENKES
KATRINA THEIS
NEHA SHAH
MARTHA VIJJESWARAPU

While the world, and medicine, may both look a bit different from our inception 108 years ago when we knitted, sewed, and made bandages for the WWI soldiers … we are still the same at heart. We are advocates, innovators, fundraisers, community ambassadors, relationship builders, support systems. We are difference makers.
Jenny
Shepherd
BCMSA Acting President, and TMAA President

For information on the Bexar County Medical Society Alliance, scan the code.



By Susan C. Mengden, PhD, CEDS-C, with Noel Ales, DO
Eating disorders are a group of mental illnesses resulting in significant medical comorbidities. The type of foods and how they are consumed by patients leads to physical consequences directly correlating with the patient’s mental health. The interdependency of physical and mental manifestations of these disorders has led to the American Psychiatric Association guidelines for a multidisciplinary treatment team. This mandated team includes physicians, dieticians and mental health specialists: both psychiatrists and eating disorder certified therapists.
Eating disorders are difficult to detect both medically and psychologically. Cultural norms, personal bias and lack of eating disorder training have led to these disorders being overlooked or misdiagnosed. The four main diagnoses for eating disorders are anorexia nervosa with subtypes - restricting type or binge-eating/purging type, bulimia nervosa, binge-eating disorder (BED), and avoidant restrictive food intake disorder (ARFID). Atypical anorexia is a person in a larger body who has the thoughts and behaviors of anorexia even though their body doesn’t represent emaciation. Clinically, these disorders overlap. They
each include restrictive intake behaviors, or excessive or obsessive movement or avoidance of movement. An eating disorder cannot be diagnosed based on appearance. Any of the eating disorders may present with any body size. It is important to note that these diagnoses are based on behaviors, not BMI or weight.
The prevalence of eating disorders has increased over the past decade and particularly during the COVID-19 quarantine. Diets, exercise, weight-loss regimes and medications became daily social media, wellness and healthcare discussions. The diet industry and messages to diet for “health” or “wellness” have normalized restrictive eating behaviors. “Eating in balance” is no longer recommended in health classes or physician offices. Society correlates a person’s weight status with their health status. Weight loss medications are often overprescribed or misused by patients with undisclosed eating disorders. Up to 30 percent of patients seeking weight loss medications have an underlying eating disorder. The recent overwhelming influx of new and more effective weight loss medications is resulting in the exacerbation of eating disorders.
Physicians are often primary in the diagnosis of an eating disorder. It is imperative that all providers have a heightened awareness of the nuances of eating disorders to make a timely diagnosis. Open lines of communication between mental health providers and a patient’s primary care physician should become routine. This would enhance clinical outcomes in all patients with psychological and medical diagnoses as both providers could collaborate care and information leading to a unified diagnosis. In addition to the multitude of medical complications from eating disorders such as cardiac insufficiency, liver, kidney and bone disease, the mental health consequences of eating disorders are the most impactful and devastating. Common co-occurring disorders include obsessive-compulsive disorder, major depressive disorder, substance use disorder, post-traumatic stress disorder and borderline personality disorder. Anorexic and bulimic patients are 7-18 times more likely to COMPLETE suicide. All eating disorder patients are 33 percent more likely to have suicidality. These patients are deeply suffering.
Each eating disorder has specific characteristics. Anorexic patients typically have underlying thoughts and emotions based on the irritational fear about becoming fat or unhealthy. In bulimia, the underlying thoughts and emotions are about maintaining one’s current body size with restricting behaviors, then bingeing followed by compensatory behaviors of purging. The person believes that purging behaviors maintain their body size. The abrupt cessation of purging without treatment results in undereating to avoid feeling full. Fullness is the trigger for purging behaviors. In BED, the underlying thoughts and emotions are striving for weight loss with restrictive behaviors. The consequential physical hunger leads to overconsumption and intense anxiety over what was ingested. They cope with this anxiety by binge-eating. ARFID patients have underlying thoughts and emotions about the textures, smells or taste of foods. They may present with a sudden onset of traumatic weight loss, often secondary to a choking experience or heightened anxiety from traumatic experiences such as a death or accident.
Physicians should note that the thoughts and emotions underlying eating disordered behaviors are illogical, reactive and impulsive. Eating disorders are progressive and the thoughts that might have been rational initially such as: “I want to get in shape” or “lower my cholesterol” often worsen and lead to physically unhealthy behaviors of eating and movement. Before telling the thin patient that they look “healthy,” complimenting their new exercise plan for 2025, or remarking that another’s hypertension would improve with weight loss, take a moment to ask everyone about their eating patterns. Most eating disorder patients are secretive or ashamed. They are not likely to disclose their eating disordered behaviors. They will take your advice and walk out the door to binge, purge, restrict and overeat until the only thing they think about is food and their reactions to it.
The thoughts and obsessions of an eating disorder are all consuming for these patients. They may present to the primary care clinic making comments about the scale “being off,” wanting to lose weight to “be healthy,” or concerned about being “too thin” in the case of the patient with ARFID. It is important to hear their cues and ask the right questions. Ask your patients how they are eating rather than assuming what their diet consists of based on their weight. Never suggest that someone restrict whole food groups for weight loss. Patients of all body types often present with their eating disorder stating that they have been informed by a physician to lose weight without further guidance. A clinical interview assessing the thoughts and emotions behind the food, eating and exercise habits is what is recommended. When interviewing patients, listen for eating disorder clues: are they making weight and diet comments? Is there a family history (eating disorders are highly heritable)? Is there early osteoporosis in their mother, grandmother and great aunts? Don’t forget a social history. An eating disorder brings control to a chaotic or traumatic life.
Changing one’s eating behaviors is NOT about willpower or intellectual ability. An eating disorder is NOT an addiction. An eating disorder is complex and all aspects must be addressed for a patient to recover. In addition to the multidisciplinary approach, the specific, third wave of Cognitive Behavioral Therapies (CBT) have been researched to be effective for eating disorders. These evidence-based CBT therapies are techniques to move eating disordered thoughts from being ego-syntonic to ego-dystonic. These therapies are used in conjunction with specific nutritional guidelines and therapies under the medical guidance of a physician to bring complete healing and recovery to this special population of patients. Treatment is successful when a person learns to use new coping skills and coping behaviors for emotions and thoughts that are more effective than coping with food and movement behaviors.

Susan C. Mengden, PhD, Certified Eating Disorder Specialistiaedp Approved Consultant, and the Founder and Executive Director of Esperanza Eating Disorders Center, has over 35 years of clinical experience specializing in eating disorder treatment.
By Chasley Fortune-Pittman, MDS, RD, LD, and Sara Hamilton, PsyD
Studies show that 28.8 million Americans will have an eating disorder in their lifetime.1 Eating disorders are a complex set of behaviors, cognitions, emotions and physical conditions affecting people of all sizes, ages, genders and ethnicities. They can develop from a combination of factors including genetics, access to food, physiological conditions, mental health conditions, physical attributes, malnutrition, eating patterns/behaviors, cultural norms, stressors and interpersonal relationships. Due to this complexity, it is necessary to incorporate a variety of health professionals to best treat eating disorders.
Diagnosing Eating Disorders
Due to their complexity, it can require multiple assessments and observations over time for a healthcare team to identify and diagnose eating disorders. Many assume that eating disorders are easy to identify based on weight or size, but only around 6 percent of people with an eating disorder are medically underweight.2 Many adolescents and adults at normal body weight engage in disordered eating. Contrary to stereotypes, many of those at low body weight binge eat and many of those at a high body weight undereat.
Medical providers and mental health professionals can diagnose eating disorders. Eating disorders generally involve distress and/or significant negative consequences related to the types, amounts, qualities or impact of food consumed. They can involve overeating, undereating, and/or eating only limited types of foods. Some eating disorders involve concerns about body weight, shape and/or size, but not all.
There is no definitive answer to how long it may take to treat eating disorders. Treatment of eating disorders should be individualized based on the status of health, nutrition, mental health, behaviors of concern and the specific cultural needs of the patient. Settings for eating disorder treatment include (in descending order of structure): inpatient, residential, partial hospitalization, intensive outpatient and outpatient levels of care. Treatment of eating disorders focuses on medical stabilization, psychotherapy (individual, group and/or family), nutritional stabilization and education. When medically stable, treatment focuses on helping the individual and their family to build up skills and routines to treat the disordered
thoughts and behaviors, address the factors contributing to the disordered behaviors, and to help reduce risk of relapse.
Communication and teamwork ensure both the safety and effectiveness of treatment. Below are some examples of how various health professionals collaborate in the treatment of eating disorders.
The multiple evaluations done by physicians are crucial in determining the appropriate treatment for those with eating disorders; those with more physiological consequences stemming from their behaviors will need higher levels of care. Eating disorders affect many of the body’s systems and patients may not be insightful into nor forthcoming about their habits and their effects. It is important to conduct a comprehensive review of medical history, observe changes to weight or growth charts, order laboratory and diagnostic testing, and complete a thorough physical examination.3 Though questions related to dietary status and behaviors may not be as in-depth as from a registered dietitian, physicians may also review overall eating habits, food intake frequency and compensatory behaviors such as laxative and diuretic use, medication abuse or misuse, questionable supplement use, excessive exercise or purging behaviors. Substance abuse can correlate with those who have eating disorders and should also be properly assessed.









Physicians may struggle to identify eating disorders in those who appear to be following their recommended plans or whose symptoms overlap with other medical conditions. They may unintentionally further someone’s restriction and overexercising by encouraging them to lose more weight or mistake purging behaviors as food sensitivities or a consequence of severe reflux. Physicians can screen for disordered eating using the following validated screening tools listed below under references.
Laboratory testing is helpful for determining a proper diagnosis, level of risk and priorities for effective treatment plans. Testing should involve an evaluation of blood sugar levels, electrolyte levels, a comprehensive metabolic panel to gauge liver and kidney function as well as nutritional and immunity status, urinalysis for hydration and signs of food restriction, and electrocardiogram to determine irregularities and risks to the heart.
Physicians should use their evaluations to ensure both medical stability and make proper recommendations for level of care. Early detection helps prevent chronic, severe disease as well as promote faster recoveries.
Registered Dietitians:
Registered Dietitians focus on the nutritional status of the individual. To do this they must look at related health findings (labs, weight history, medications, etc.), assess calorie and macronutrient intake, vitamin/mineral supplementation, inspect eating patterns, and observe attitudes and behaviors around food. In addition, dietitians also take care to assess dieting history and probe to find more about compensatory behaviors, such as abuse or use of weight loss medications, extreme diets, fasting, induced vomiting, over-exercising or food restriction. Due to the nature of chaotic eating patterns or even the patient’s choice to not be forthcoming with information, dietitians must ask multiple questions in order to get an idea of the “big picture” of the client’s nutritional health and habits.
Dietitians are also a key component in the creation of interventions and the monitoring and evaluation of the patient’s treatment. The interventions created involve decreasing pathological behaviors, restoring patient to a healthy weight, encourage adherence to medical recommendations, and improve nutritional intake. Dietary education as well as motivational interviewing and counseling are essential to not only encourage the patient’s adherence to recommendations but also build habit changes to sustain results and prevent relapse.
Psychotherapy for eating disorders typically includes the patient and their families to best address the multitude of factors that contribute to the development of an eating disorder and to support the patient in their recovery. Treatment of eating disorders often focuses on helping clients to improve their ability to identify, manage, and communicate their emotions, to improve their functioning in their relationships, and to change thought patterns that are contributing to their distress related to eating. By addressing these factors, clients are better able to manage their distress related to eating and can then implement the needed dietary interventions more effectively.
There are multiple therapists that can play roles in the treatment of eating disorders. Speech therapists address chewing and swallowing issues that can cause fear of eating, particularly after a choking incident. Occupational therapists help strengthen abilities to do daily activities. Physical therapists help encourage safe movement that takes into account the patient’s barriers.
Nurses:
Nurses play a pivotal role in the gathering of information used for diagnosing and therefore deciding on effective treatment. They also monitor improvement in symptoms and provide valuable coaching to
clients on how to understand the ways in which their behaviors are impacting their physical health. Nurses often obtain clients’ weight information, which can be a very stressful part of treatment for many clients; compassionate nursing care helps many to tolerate this part of treatment more effectively.
Psychiatrists:
Eating disorders are often co-occurring with other mental health issues like anxiety and mood disorders, substance use disorders and a history of trauma. Psychiatrists can play a crucial role in helping to address symptoms of other disorders that can present barriers to effective engagement in eating disorder treatment. Improving mood and reducing anxiety can also make people less likely to turn to disordered eating behaviors to regulate mood. Some medications also facilitate reduction of eating disorder symptoms in addition to mood and anxiety symptoms. Psychiatrists may also be more likely to identify disordered eating thoughts and behaviors in their interactions with their patients than other healthcare providers due to their training. Among mental health professionals, they can order necessary lab tests and initiate medical interventions that others cannot.
Administrative Staff:
It may take a significant amount of time for someone to seek and/or receive diagnosis and treatment for an eating disorder. Treatment for eating disorders may be long and uncomfortable, and patients are at risk of prematurely terminating treatment as a result. Administrative staff are often the main communicators in many facilities and often some of the first voices these patients hear as they get help. Treatment cannot work unless patients are willing to start and continue treatment. In addition to helping coordinate treatment and keeping patients coming to their appointments, administrators are also another point to gather important information about barriers to treatment, mental status, behavioral patterns or environmental clues.
The treatment of eating disorders can often be intimidating due to the lack of training most professions receive in how to best identify and help people struggling with these conditions. Collaborating with a multidisciplinary team can improve symptom identification and help clients to address the impact of their behaviors more quickly and effectively. Those who specialize in treating eating disorders can be a resource to those less familiar who suspect a patient or loved one may be suffering from an eating disorder. Local and national resources are available for patients and providers alike to better understand eating disorders and to take steps forward toward happiness and healing.
Citations:
1. Deloitte Access Economics. The Social and Economic Cost of Eating Disorders in the United States of America: A Report for the Strategic Training Initiative for the Prevention of Eating Disorders and the Academy for Eating Disorders. June 2020
2. Flament, M. F., Henderson, K., Buchholz, A., Obeid, N., Nguyen, H. N., Birmingham, M., & Goldfield, G. (2015). Weight Status and DSM-5 Diagnoses of Eating Disorders in Adolescents from the Community. Journal of the American Academy of Child and Adolescent Psychiatry, 54(5), 403–411.e2. https://doi. org/10.1016/j.jaac.2015.01.020
3. Joy, E. A., Wilson, C., & Varechok, S. (2003). The multidisciplinary team approach to the outpatient treatment of disordered eating. Current sports medicine reports, 2(6), 331–336. https:// doi.org/10.1249/00149619-200312000-00009
References:
1. Eating disorder examination questionnaire (EDE-Q). CORC Child Outcomes Research Consortium. (n.d.). https://www. corc.uk.net/outcome-experience-measures/eating-disorder-examination-questionnaire-ede-q/
2. Home. EAT. (2025, January 9). https://www.eat-26.com/
3. Neda. National Eating Disorders Association. (2025, January 8). https://www.nationaleatingdisorders.org/
4. Strickland, K. (2025, January 9). How long does eating disorder recovery take? Walden Eating Disorders. https://www.waldeneatingdisorders.com/blog/how-long-does-eating-disorder-recovery-take/

Sara Hamilton, PsyD, is a licensed clinical psychologist and the clinical director of the Bariatric Counseling Center.

Chasley Fortune-Pittman, MDS, RD, LD, is a registered dietitian and the dietary director at the Bariatric Counseling Center.
They share the belief that successful health interventions focus on helping people to make changes that are meaningful to them and are sustainable long-term. At the Bariatric Counseling Center, they lead a multidisciplinary team of providers that treat eating disorders, particularly those involving binge-eating behaviors, at the intensive outpatient level of care.

By Camille Irene Hulipas, Lydia Beera and Ramaswamy Sharma, MS, PhD
Eating disorders (EDs), such as anorexia nervosa (AN), bulimia nervosa, binge-eating disorder and others, are complex mental and behavioral conditions that arise from distorted beliefs regarding body image, lead to abnormal eating, and result in deterioration of physical, mental and social functions. While obesity is not considered to be a mental disorder, it is associated with binge-eating disorder and schizophrenia, and is a known risk factor for bulimia nervosa and depressive disorders. Given that (1) EDs rank second among psychiatric disorders with the highest mortality rates, next only to opiate addiction, (2) their prevalence in children and adults is increasing worldwide, and (3) estimated economic and well-being costs in 2024 were approximately $327 billion, it is important to identify and break their barriers to treatment. Stigmatization associated with EDs is one such critical barrier.
Stigma can involve a cognitive component when it is based on shared beliefs about a group of people and thereby leads to stereotyping — an emotional component manifested as prejudice towards such groups — and a behavioral component that results in discrimination and therefore, disadvantages to that group. Most commonly, EDs are
thought to be self-inflicted lifestyle choices caused by lack of self-discipline that could be overcome easily by assuming personal responsibility; it is also perceived that reasoning and communication with such individuals is challenging (cognitive components). Such perceptions may result in irritation, anger, pity or disgust (emotional component), with society tending to keep distance from such individuals (behavioral component). Each type of ED has its own specific stigma associated with it. For example, anorexia nervosa was considered a disease of affluence, and stereotyped as affecting “skinny, white, affluent girls” (SWAG). However, it is important to note that less than 6 percent of people with an ED are medically underweight. Individuals with a history of obesity have a more severe ED experience than those who have never been obese; weight stigma involving negative beliefs as well as discrimination against large-bodied individuals is also a known risk factor for disordered eating. Weight stigma correlates partially with stigma associated with EDs in terms of their surrounding attitudes, the populations they affect and biopsychosocial factors; the overtly negative stigma towards obesity can contribute to the onset, perpetuation and masking of EDs.
Race, culture and socioeconomic status also play into EDs-related stigmas. People of color are half as likely to be diagnosed with EDs as their Caucasian counterparts; when combined with other factors such as cultural stigma towards mental health, community mistrust of healthcare providers and weight stigma, people of color are severely disadvantaged in terms of diagnosis and positive health outcomes of ED treatment. African Americans and Hispanics are more reluctant to seek help for mental disorders as compared to Caucasians.
Stigma surrounding EDs has negative effects on an individual’s psychological well-being and contributes to self-stigmatization, low self-esteem, non-pursuit of life goals, social withdrawal and poor quality of life. Stigmatization is associated with barriers to disclosure, reluctance to seek treatment, and adherence to treatment protocols. For example, patients with AN wait for an average of eight to nine months before seeking medical consultation.
Nurses and clinicians are not immune to stigmatizing EDs. Some healthcare providers hold strong negative attitudes and stereotypes about people with ED. Inexperienced clinicians and trainees, such as medical students and first-year residents, exhibit cognitive (negative beliefs), emotional (frustration, anger, feelings of helplessness and hopelessness, lack of motivation to care for these patients), and discriminatory (social distancing) components of stigma, stemming from patient resistance to change as well as perceived lack of competency in diagnosing and treating EDs. Only about 20 percent of ED-associated patients are correctly diagnosed and treated as compared to patients suffering from other mental health illnesses. Experienced clinicians find treating ED patients difficult because of the lack of systemic resources.
From a healthcare provider’s perspective, lack of knowledge and implicit bias borne from a broader public stigma may negatively impact the time to treatment and, worse, overtly trigger or cause relapse of an ED. The average times from ED onset and treatment ranges from 10-15 years as compared to only 8.2 years for those with other psychiatric conditions such as mood or anxiety disorders. The absence of a timely and accurate diagnosis can potentially exacerbate, prolong, and complicate their illness, worsening the severity of the ED and leading to decreased treatment adherence, mistrust and poorer overall health outcomes. Providers may fail to recognize or even overlook disordered eating behaviors in overweight individuals. This is a worrisome practice as women who were classified as “obese” per body-mass-index (BMI) were significantly more likely to exhibit body image concerns, restrictive food practices, bulimic episodes and other alarming practices when compared to smaller-bodied women. Larger-bodied individuals, despite having the same clinical profile as someone with AN are diagnosed with atypical anorexia nervosa (AAN), which is perceived as less severe than AN, preventing access to adequate treatment. Although AAN appears more frequently, fewer patients with AAN are referred to and admitted for ED-specific care. Diagnostic standards for other specified food and eating disorders (OSFED), under which AAN is categorized, fail to capture the complexity and full clinical picture of a patient and may result in suboptimal treatment. Instead of helping a struggling patient, the stigma associated with EDs may reinforce and even worsen harmful behaviors. Therefore, how should healthcare providers address and screen for EDs in ways that minimize harm and prevent health disparities by including vul-
nerable populations? Destigmatizing EDs by increasing their public awareness is an important first step towards reducing barriers. However, it is critical to design well-thought-out interventions as studies show that using ED stereotypes in public service announcements may lead to increased contempt. Possible improvements could also include continuous enhancement of guidelines as we progress in our learning of EDs, and providing increased training for students, residents and clinicians to better recognize ED symptoms and help them understand that their attitude towards EDs is tantamount to the success of treatment and long-term outcomes.
References:
1. Brelet, L., Flaudias, V., Désert, M., Guillaume, S., Llorca, P. M., & Boirie, Y. (2021). Stigmatization toward People with Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder: A Scoping Review. Nutrients, 13(8), 2834. https://doi.org/10.3390/ nu13082834
2. Camacho-Barcia, L., Giel, K. E., Jiménez-Murcia, S., Álvarez Pitti, J., Micali, N., Lucas, I., Miranda-Olivos, R., Munguia, L., Tena-Sempere, M., Zipfel, S., & Fernández-Aranda, F. (2024). Eating disorders and obesity: bridging clinical, neurobiological, and therapeutic perspectives. Trends Mol. Med., 30(4), 361–379. https://doi.org/10.1016/j.molmed.2024.02.007
3. Cardel, M. I., Newsome, F. A., Pearl, R. L., Ross, K. M., Dillard, J. R., Miller, D. R., Hayes, J. F., Wilfley, D., Keel, P. K., Dhurandhar, E. J., & Balantekin, K. N. (2022). Patient-Centered Care for Obesity: How Health Care Providers Can Treat Obesity While Actively Addressing Weight Stigma and Eating Disorder Risk. J. Acad.Nutr.Diet., 122(6), 1089–1098. https://doi.org/10.1016/j. jand.2022.01.004
4. Chen, C., & Gonzales, L. (2022). Understanding weight stigma in eating disorder treatment: Development and initial validation of a treatment-based stigma scale. J.Hlth.Psych, 27(13), 3028–3045. https://doi.org/10.1177/13591053221079177
5. Coffino, J. A., Udo, T., & Grilo, C. M. (2019). Rates of Help-Seeking in US Adults With Lifetime DSM-5 Eating Disorders: Prevalence Across Diagnoses and Differences by Sex and Ethnicity/Race. Mayo Clinic proceedings, 94(8), 1415–1426. https://doi.org/10.1016/j.mayocp.2019.02.030
6. Daugelat, M. C., Pruccoli, J., Schag, K., & Giel, K. E. (2023). Barriers and facilitators affecting treatment uptake behaviours for patients with eating disorders: A systematic review synthesising patient, caregiver and clinician perspectives. Euop.Eat.Disord. Rev., 31(6), 752–768. https://doi.org/10.1002/erv.2999
7. Field, A. E., Ziobrowski, H. N., Eddy, K. T., Sonneville, K. R., & Richmond, T. K. (2024). Who gets treated for an eating disorder? Implications for inference based on clinical populations. BMC Pub.Hlth., 24(1), 1758. https://doi.org/10.1186/ s12889-024-19283-2
8. Flament, M. F., Henderson, K., Buchholz, A., Obeid, N., Nguyen, H. N., Birmingham, M., & Goldfield, G. (2015). Weight Status and DSM-5 Diagnoses of Eating Disorders in Adolescents From the Community. J.Amer.Acad.Child &Adol.Psych. 54(5), 403–411.e2. https://doi.org/10.1016/j.jaac.2015.01.020
9. Griffiths, S., Mond, J. M., Murray, S. B., & Touyz, S. (2015). The prevalence and adverse associations of stigmatization in people with eating disorders. Int.J.Eat.Disord., 48(6), 767–774. https:// doi.org/10.1002/eat.22353
10. Harrop, E. N., Mensinger, J. L., Moore, M., & Lindhorst, T. (2021). Restrictive eating disorders in higher weight persons: A systematic review of atypical anorexia nervosa prevalence and consecutive admission literature. Int.J.Eat.Disord., 54(8), 1328–1357. https://doi.org/10.1002/eat.23519
11. Huryk, K. M., Drury, C. R., & Loeb, K. L. (2021). Diseases of affluence? A systematic review of the literature on socioeconomic diversity in eating disorders. Eat.Behav., 43, 101548. https://doi. org/10.1016/j.eatbeh.2021.101548
12. Innes, N. T., Clough, B. A., & Casey, L. M. (2017). Assessing treatment barriers in eating disorders: A systematic review. Eat. Disord., 25(1), 1–21. https://doi.org/10.1080/10640266.2016. 1207455
13. Krug, I., Dang, A. B., & Hughes, E. K. (2024). There is nothing as inconsistent as the OSFED diagnostic criteria. Trends Mol.Med., 30(4), 403–415. https://doi.org/10.1016/j. molmed.2024.01.006
14. McEntee, M. L., Philip, S. R., & Phelan, S. M. (2023). Dismantling weight stigma in eating disorder treatment: Next steps for the field. Front.Psych., 14, 1157594. https://doi.org/10.3389/ fpsyt.2023.1157594
15. Mishra, K., & Harrop, E. (2023). Teaching How to Avoid Overreliance on BMI in Diagnosing and Caring for Patients With Eating Disorders. AMA J.Ethics, 25(7), E507–E513. https://doi. org/10.1001/amajethics.2023.507
16. Nawaz, F. A., Kurdak, H., Dakanalis, A., Argyrides, M., & Kashyap, R. (2024). Editorial: Break the mental health stigma: eating disorders. Front.Psych., 15, 1416250. https://doi.org/10.3389/ fpsyt.2024.1416250
17. National Institute of Mental Health. (2024, January). Eating Disorders. U.S. Department of Health and Human Services, National Institutes of Health. Retrieved December 13, 2024, from https://www.nimh.nih.gov/health/topics/eating-disorders
18. Penwell, T. E., Bedard, S. P., Eyre, R., & Levinson, C. A. (2024). Eating Disorder Treatment Access in the United States: Perceived Inequities Among Treatment Seekers. Psychiatr.Serv. (Washington, D.C.), 75(10), 944–952. https://doi.org/10.1176/appi. ps.20230193
19. Phelan, S. M., Burgess, D. J., Yeazel, M. W., Hellerstedt, W. L., Griffin, J. M., & van Ryn, M. (2015). Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Rev., 16(4), 319–326. https://doi.org/10.1111/ obr.12266
20. Sonneville, K. R., & Lipson, S. K. (2018). Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. Int.J.Eat.Disord., 51(6), 518–526. https://doi. org/10.1002/eat.22846
21. Thompson-Brenner H, Satir DA, Franko DL, Herzog DB. Clinician reactions to patients with eating disorders: a review of the literature. Psychiatr. Serv. 2012 Jan;63(1):73-8. doi: 10.1176/ appi.ps.201100050. PMID: 22227763


Camille Irene Hulipas is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027.
Lydia Beera is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027.
Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma is a member of the BCMS Publications Committee.


By Ramon S. Cancino, MD, MBA, MS, FAAFP, and Richard M. Peterson, MD, MPH, FACS, FASMBS, DABS-FPMBS
The American Medical Association declared obesity a disease in 2013, and its prevalence remains well above the Healthy People 2030 goal of 36.0 percent. In the United States, the obesity rate among adults is 40.3 percent, which means two in five adults are obese (Body Mass Index [BMI] 30 kg/m2 or greater).1
In Texas, the current rate of the disease of obesity is at 35 percent. Bexar County alone fares even worse with overweight (BMI 25-30 kg/ m2) and obesity rates as high as 72 percent, which is much higher than the national average.
Obesity has many health consequences affecting every organ system of the body. In South Texas, we see a disproportionately high number of individuals with type 2 diabetes mellitus (T2DM), which goes hand-in-hand with this ubiquitous disease.
The health consequences of obesity do not stop with T2DM. Other comorbidities that are commonly associated with this disease are hypertension, stroke, obstructive sleep apnea, hyperlipidemia, fatty liver disease (now identified as metabolic associated steatohepatitis — MASH), and gastroesophageal reflux disease.2 Each of these listed comorbidities can come with dire consequences to individuals. Considered one of the most inflammatory diseases, obesity exacerbates all these comorbidities and more. In fact, obesity has been linked to several common cancers and also increases the risk of dying from cancer.3
The first step in understanding prevention and treatment is disease recognition. One of the easiest ways to help understand this disease is to think of the cancer treatment model. Cancer treatments can include medical and surgical options and, often, both. Most people perceive cancer as a process that affects the individual and do not necessarily assign fault to the individual for the disease. Unfortunately, obesity is
often seen as the fault of the individual, who may consume too many calories or live a sedentary lifestyle. This is far from the truth. While diet and exercise are a part of what an individual can often control with respect to their environmental exposure of their disease, an individual cannot control their genetics or their underlying metabolic state that leads to this disease. In addition, an individual may have little control over their environment or social status. Implicit weight bias can have detrimental effects on patients and, therefore, how we communicate can impact how we connect with patients about its treatments.4,5
Once we recognize obesity as a disease, we are then able to talk to our patients about treatment options. Both medical and surgical treatments are available and effective in the treatment of obesity. Obesity is a chronic disease and like cancer, can remain in remission for a lifetime after treatment, or may unfortunately recur, requiring further therapy.
Several FDA-approved medications have demonstrated efficacy in promoting weight loss when used in conjunction with lifestyle modifications. The most effective options include GLP-1 receptor agonists, such as semaglutide and liraglutide, which can lead to significant weight reductions of 10-20 percent of body weight. Tirzepatide, a dual GIP and GLP-1 receptor agonist, has shown even greater weight loss potential in clinical trials. Other options include combination therapies like phentermine-topiramate and naltrexone-bupropion, as well as orlistat, which work through different mechanisms to support weight management. Because these medications are more effective with lifestyle modification, patients should work closely with their primary care physicians or other medical specialists, like endocrinologists, before starting any medications. This will ensure a holistic plan is in place that includes recognition of patient goals, other medical
comorbidities, social and financial factors, and the appropriate medical team members, such as behavioral health practitioners or registered dietitians.
Today there are several surgical options that individuals with obesity can consider, and the type of surgery is tailored to the individual based on their level of obesity and the comorbidities from which they also may suffer. The American Society for Metabolic and Bariatric Surgery (ASMBS) endorses the following procedures for the treatment of obesity: adjustable gastric banding, sleeve gastrectomy, rouxen-y gastric bypass (RNYGP), biliopancreatic diversion/duodenal switch (BPD/DS), single anastomosis duodeno-ileostomy with sleeve (SADI-S), one-anastomosis gastric bypass (OAGB), intragastric balloons and reoperative procedures.
The first surgeries for obesity began in 1966 under the pioneer, Dr. Edward Mason. There have been many novel operations since that time, but the roux-en-y gastric bypass still stands as one of the gold standards of the surgical treatment of obesity. For over 50 years, surgery has remained the most effective and durable option in the fight of the disease of obesity. Today, surgery has the longest followed outcomes in the treatment of this disease. Over the last 20 years, the dedication of surgery to quality outcomes, led by the ASMBS and in partnership with the American College of Surgeons (ACS), formed the Metabolic Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP) to track quality data in this area. With over one million patients being followed and 947 nationally accredited programs (90 of which are in Texas), improvements in care quality have been tracked. Improvements in surgery and technique with metabolic and bariatric surgery (MBS) are such that, today, an individual undergoing an MBS procedure, is safer than having their gallbladder or appendix removed.
In the United States, only 1 percent of eligible patients receive metabolic and bariatric surgery. The sleeve gastrectomy remains the most common operation performed with approximately 60 to 70 percent of the individual’s excess weight being lost after this treatment. The roux-en-y gastric bypass is the second most common surgery performed with 70 to 80 percent of excess weight loss. As mentioned earlier, these surgeries have been proven to be some of the safest surgeries performed, with death rates noted to be less than 0.05 percent. The efficacy of surgery is also seen in the comorbidity resolution with T2DM noting a resolution/remission rate of greater than 80 percent, hypertension improvement/resolution of 70 percent and obstructive sleep apnea resolution greater than 75 percent. In addition, cancer risk reduction of 60 percent is seen with MBS.
In 2022, the ASMBS and the International Federation for the Surgery of Obesity (IFSO) released and updated the 1991 NIH Consensus Statement on bariatric surgery. The current guidelines6 recommend MBS:
• For individuals with a body mass index (BMI) ≥ 35 kg/m2, regardless of presence, absence or severity of comorbidities.
• MBS should be considered for individuals with metabolic disease and BMI of 30-34.9 kg/m2.
• BMI thresholds should be adjusted in the Asian population such that a BMI ≥ 25 kg/m2 suggests clinical obesity, and individuals with BMI ≥ 27.5 kg/m2 should be offered MBS.
• Appropriately selected children and adolescents should be considered for MBS.
The recognition of obesity as a complex, multifaceted disease is critical for improving patient outcomes and advancing treatment approaches. Physicians play a pivotal role in reframing the narrative around obesity, emphasizing its biological, environmental and social determinants rather than perpetuating stigma. By adopting evidence-based medical and surgical treatments, alongside lifestyle and behavioral interventions, we can offer patients effective and sustainable options for weight management and comorbidity resolution. Collaboration across specialties, combined with advancements in pharmacological and surgical therapies, has the potential to transform the landscape of obesity care. Ultimately, it is our collective responsibility as physicians to advocate for our patients, challenge implicit biases, and implement comprehensive care models that address this pervasive and life-altering disease.
References:
1. Emmerich, S., Fryar, C., Stierman, B., Ogden, C. Obesity and Severe Obesity Prevalence in Adults: United States, August 2021–August 2023. National Center for Health Statistics (U.S.); 2024. doi:10.15620/cdc/159281
2. Health Risks of Overweight & Obesity - NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed January 16, 2025. https://www.niddk.nih.gov/ health-information/weight-management/adult-overweight-obesity/health-risks
3. Pati, S., Irfan, W., Jameel, A., Ahmed, S., Shahid, R. K. Obesity and Cancer: A Current Overview of Epidemiology, Pathogenesis, Outcomes, and Management. Cancers. 2023;15(2):485. doi:10.3390/cancers15020485
4. Abbott, S., Shuttlewood, E., Flint, S. W., Chesworth, P., Parretti, H. M. “Is it time to throw out the weighing scales?” Implicit weight bias among healthcare professionals working in bariatric surgery services and their attitude towards non-weight focused approaches. eClinicalMedicine. 2023;55. doi:10.1016/j. eclinm.2022.101770
5. Puhl, R., Suh, Y. Health Consequences of Weight Stigma: Implications for Obesity Prevention and Treatment. Curr Obes Rep. 2015;4(2):182-190. doi:10.1007/s13679-015-0153-z
6. Eisenberg, D., Shikora, S. A., Aarts, E., Aminian, A., Angrisani, L., Cohen, R. V., De Luca, M., Faria, S. L., Goodpaster, K. P. S., Haddad, A., Himpens, J. M., Kow, L., Kurian, M., Loi, K., Mahawar, K., Nimeri, A., O’Kane, M., Papasavas, P. K., Ponce, J., Pratt, J. S. A., Rogers, A. M., Steele, K. E., Suter, M., Kothari, S. N. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for Metabolic and Bariatric Surgery. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2022;18(12):1345-1356. doi:10.1016/j.soard.2022.08.013

Ramon S. Cancino, MD, MBA, MS, FAAFP, is Executive Director of the UT Health San Antonio Primary Care Center and co-Chair of the Joint UT Health San Antonio/MD Anderson Mays Cancer Center Cancer Prevention and Steering Committee. Dr. Cancino is a member of the Bexar County Medical Society.

Richard M. Peterson, MD, MPH, FACS, FASMBS, DABSFPMBS, is Professor and Chief of Metabolic and Bariatric Surgery at the UT Health San Antonio. He is a past president of the Texas State Chapter of the ASMBS and current PresidentElect of the ASMBS.

By Alison Bartak and Ramaswamy Sharma, MS, PhD
Feeding and eating disorders, characterized by severe and persistent disturbances in eating that negatively affect physical, psychological and social functions, include anorexia nervosa, bulimia nervosa, binge-eating disorder, pica, avoidant/restrictive food intake disorders (ARFID) and ruminant disorder. Around 29 million (9 percent) U.S. adults suffer from these disorders, with a mortality rate of 10,200 deaths per year. Among these, the mortality rate of young individuals with anorexia is 12 times higher as compared to similar-aged individuals without anorexia. Therefore, it is important to diagnose this potentially fatal disorder as early as possible.
The Diagnostic and Statistical Manual of Mental Disorders (DSM5-TR; 2022) lists three important features for diagnosis: decreased energy intake relative to the body’s requirements in the context of age, developmental stage and sex, extreme fear of weight-gain or becoming fat even if underweight, and either excessive consideration of body weight and/or shape when evaluating oneself or inability to
understand the consequences of their low body weight, termed anosognosia. Patients with anorexia nervosa may have decreased levels of neurotransmitters such as dopamine and serotonin, differences in activation of the corticolimbic system, and decreased executive functions mediated by the frontostriatal circuits, resulting in multiple behavioral changes and psychiatric disorders such as obsessive-compulsive disorder. Prolonged exercise, restrictive eating or starving as well as excessive purging behaviors via vomiting, use of laxatives or enemas can lead to serious medical consequences. Seriously underweight individuals may show signs of depression.
Body mass index (BMI) has been used over many years to diagnose anorexia. Adults with a BMI less than or equal to 17, 16-16.99, 15-15.99, or less than 15 kg/m2 are considered to be suffering from mild, moderate, severe or extreme anorexia respectively; children and adolescents below the 5th percentile when evaluated using an appropriate age-based BMI calculator (www.cdc.gov/healthyweight/bmi/
calculator.html) are significantly underweight. However, BMI is no longer used as a diagnostic tool and its use has been restricted for assessing disease severity.
Other nuanced physical signs of anorexia nervosa can be found in the beginning stages (one to three months), intermediate stages (three to six months) and in more advanced stages (more than six months); identifying these changes could potentially lead to early diagnosis and treatment before irreversible damage occurs.
Within the first one to three months, an individual with anorexia nervosa may experience thermoregulatory changes as well as hair, skin and nail changes. Decreased thermoregulation occurs as a consequence of reduction in weight, which includes loss of insulating subcutaneous fat, decreased metabolism for conservation of energy, and vasoconstriction of peripheral capillaries for conserve core body temperature. Malnutrition can also lead to dysfunction of the hypothalamus, which acts as the body’s thermostat. The overall decrease in heat production results in the patient experiencing cold sensitivity and cold extremities. To compensate for the heat loss and protect the body, lanugo hair, which is thin, downy, pigmented hair that appears on the back, abdomen, forearms, along the spine, sometimes the sides of the face, and on the neck and legs, may develop. Malnutrition, specifically protein and micronutrient deficiency, also affects skin and nails. Protein deficiency and dehydration impair skin cell turnover as well as its barrier function, leading to pale, dry, paper-like skin that bruises easily and repairs poorly. Micronutrient deficiencies, especially deficiencies in Zinc and Vitamin B, impact nail matrix formation, manifested as brittle nails.
As the disease progresses, within a three-to-six-month period, the body begins to experience systematic changes that include changes in reproductive, cardiovascular and gastrointestinal functions. Endocrinopathies associated with disruptions in the hypothalamic-pituitary-gonadal axis, hypothalamic-pituitary-thyroid axis, hypothalamic-pituitary-adrenal axis, altered growth hormone secretion and activity, and decreased leptin and increased ghrelin levels begin to manifest. Decreased gonadotropin releasing hormone from the pituitary lowers estrogen levels and ultimately results in secondary amenorrhea in adult females; menarche is delayed in prepubertal females. Decreased sperm count and quality is observed in males. Hypothyroidism reduces metabolic rates and is associated with dry skin, hypothermia, hypotension and bradycardia, observed as dizziness when standing and syncope. Within the GI tract, digestive processes begin to slow due to reduced nutritional intake. Patients can experience delayed gastric emptying, decreased intestinal mobility, reduced enzyme production, and altered gut microbiome composition. This could be reflected physically in the individual as constipation and abdominal pain.
While most of these symptoms are reversible, long term and potentially irreversible consequences may occur. In addition to the physical symptoms previously described, loss of bone density, muscle wasting and increased consequences to electrolyte imbalance become apparent. More than 90 percent of women with anorexia exhibit reduced bone density, 38 percent of whom are diagnosed with osteoporosis and hence, an increased risk for fractures. Females with binging and then purging subtype of anorexia nervosa have a higher risk for developing osteoporosis as compared to the restricting subtype. Reduced estrogen, calcium and Vitamin D levels ultimately contribute to impaired bone formation, while elevations in stress-induced catecholamine and cor-
tisol increase bone resorption. To balance its energy needs, protein is catabolized for gluconeogenesis, protein synthesis required for muscle maintenance is decreased and exercise capacity is reduced, leading to disuse atrophy and muscle-wasting. Continued electrolyte imbalances involving sodium, potassium, calcium, magnesium and phosphate can lead to impacts on membrane potential and cellular function and induce muscle weakness, confusions/altered mental state, seizures, tetany, numbness and tingling, and in some severe cases, heart and respiratory failure. Other long-term complications include infertility, short stature, dilated cardiomyopathy, arrhythmias, mitral valve prolapse, brain atrophy, pre-renal renal failure and others.
The tell-tale signs of anorexia nervosa are often classified at much later stages. Understanding the potential warning signs is crucial for early identification and treatment/management before the onset of irreversible damage.
References:
1. Aldridge, D. (2023, November 20). Lanugo: Anorexia hair growth explained. Eating Recovery Center. https://www.eatingrecoverycenter.com/resources/lanugo-anorexia#how-is-lanugo
2. American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders: DSM-5-TR. American Psychiatric Association Publishing. https://doi.org/10.1176/appi. books.9780890425787
3. Bunnell, D. (2024, April 30). Eating Disorder Statistics. National Eating Disorders Association. https://www.nationaleatingdisorders.org/statistics/
4. Guarda, A. (2023) What are Eating Disorders? American Psychiatric Association. https://www.psychiatry.org/patients-families/ eating-disorders/what-are-eating-disorders
5. Ramaswamy, N., & Ramaswamy, N. (2023). Overreliance on BMI and delayed care for patients with higher BMI and disordered eating. The AMA Journal of Ethic, 25(7), E540-544. https://doi.org/10.1001/amajethics.2023.540
6. Moore, C. A., & Bokor, B. R. (2023, August 28). Anorexia nervosa. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih. gov/books/NBK459148/
7. Pike, E. Eating Disorder Statistics 2024 | Anorexia, bulimia, Binge Eating & ARFID. (2024, February 14). Eating Recovery Center. https://www.eatingrecoverycenter.com/resources/eating-disorder-statistics
8. The Alliance for Eating Disorders Awareness. (2024, August 16). Eating Disorder Statistics: An updated view for 2024. National Alliance for Eating Disorders. https://www.allianceforeatingdisorders.com/eating-disorder-statistics-an-updated-view-for-2024/
9. Usdan, L.S., Khaodhiar, L., & Apovian, C.M. (2008). The endocrinopathies of anorexia nervosa. Endocrine Practice, 14(8), 1055–1063. https://doi.org/10.4158/ep.14.8.1055

Alison Bartak is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. Her current interests include Preventative Medicine and Surgery.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma is a member of the BCMS Publications Committee.

By Victoria (Tori) Vargas
Social media has become a cornerstone of modern society, shaping how we connect, communicate, and share our lives. Popular platforms like Twitter, Instagram and TikTok spread trends and promote lifestyles tailored to each user. While these platforms offer a sense of connection and entertainment, they also present distorted views of health, fitness and beauty, often promoting inaccurate or misleading habits. Together, these factors can significantly impact users’ mental and physical well-being, contributing to the development of eating disorders such as anorexia, bulimia and binge-eating disorder.
Social media’s effectiveness in spreading information lies in its vast reach, algorithm-driven content delivery and diverse user base. Platforms like Instagram and TikTok cater to millions worldwide, offering personalized content based on user interests and behaviors. Once a user searches for specific topics, their feed becomes filled with related content. This tailored approach makes social media an incredibly powerful tool for sharing trends, advice and lifestyle tips. However, the sources of this information vary widely — from certified health professionals to influencers with little expertise. Misinformation is
prevalent on these platforms, and the algorithm helps spread content at an alarming rate, often regardless of the quality of the information.
Although people of all ages engage with social media, teenagers and young adults make up the largest group of users and are especially vulnerable to its influence. In 2023, 78 percent of U.S. Gen Z (born between 1997 and 2013) used TikTok, making them particularly impressionable. This demographic tends to internalize advice and adopt behaviors without questioning the credibility of the source. Social media’s combination of engaging visuals, relatable creators and peer validation is effective in shaping perceptions and habits — whether those habits are beneficial or harmful. Adolescence and young adulthood are critical periods for habit formation, making this age group particularly susceptible to adopting unhealthy behaviors.
While social media platforms were initially designed for communication and entertainment, they have evolved into sources of education, particularly in health and fitness. Many influencers, often showcasing desirable physiques, create content that others seek to emulate. As people turn to influencers for advice on nutrition, workouts and wellness,
they may adopt unsustainable or unhealthy behaviors. Many influencers, who are not qualified health professionals, promote diets, supplements and exercise regimens that lack scientific support or medical safety.
For example, diet trends like extreme calorie restriction or intermittent fasting are often popularized by influencers claiming dramatic health benefits. While these approaches may yield short-term results, they are typically unsustainable and can encourage harmful eating behaviors. Influencers may also label certain foods or food groups as “bad,” complicating people’s relationship with food and nutrition. As a result, users relying on social media for fitness advice may unknowingly adopt habits that increase their risk of developing an eating disorder.
At the heart of many eating disorders lies dissatisfaction with one’s body image, often fueled by external influences. Social media exacerbates this issue by portraying unrealistic standards of beauty and fitness. Platforms encourage sharing personal photos, many of which reflect an idealized physique. Instagram and TikTok are filled with influencers showcasing “perfect” bodies — slim, toned and symmetrical — often achieved through intense workouts and extreme dieting. While these photos may not appear deceptive, they often overlook factors such as genetics, lighting and the use of filters or editing software that alter appearances.
Some fitness influencers promote healthy methods and share unedited, authentic photos, but their approach to promoting fitness varies. For some, the primary goal is engagement or sponsorship, rather than authenticity or education. These influencers may use tactics that prioritize hooking viewers or gaining interactions, sometimes at the expense of providing accurate or responsible advice. The constant exposure to such “perfection” can lead to body dissatisfaction, and individuals may adopt extreme dieting, over-exercising, or purging in an attempt to conform to these idealized physiques.
While social media may not directly cause eating disorders, its influence is undeniable. Research shows that increased time spent on these platforms is linked to greater body dissatisfaction and a higher likelihood of adopting unhealthy eating habits. Social media fosters an environment of constant comparison, fueling insecurities. Furthermore, the flood of advice shared online is often inaccurate, failing to consider an individual’s unique health needs or goals. Both the images and the information encountered on social media should be approached critically, with users conducting their own research to verify what they see.
The focus on physical appearance in online spaces also leaves little room for discussions about mental health, self-care or body positivity. As eating disorders are often stigmatized and difficult to discuss, this lack of representation can further isolate individuals who are struggling, making it harder for them to seek help or even recognize their behaviors as problematic.
While the potential harms of social media on eating behaviors are clear, there are ways to mitigate its negative effects. Promoting body positivity, encouraging diverse representations of beauty and health, and teaching realistic portrayals of fitness and nutrition are steps in combating the rise of eating disorders. Some users have already begun challenging these trends by posting both edited and unedited versions of their fitness pictures, showing how lighting, posing and editing create the “perfect” form.
Education may be the most important step. Empowering individuals to critically engage with the content they encounter online — understanding that not everything they see reflects reality — can help reduce the likelihood of adopting unhealthy behaviors. Encouraging users to follow qualified professionals in nutrition and fitness, rather than unverified influencers, can provide more accurate and helpful information. It is important to recognize that short videos cannot properly guide a person’s health, and patient health should be discussed with healthcare professionals. While many physicians may not directly engage with media to counter misinformation, initiating conversations during appointments and providing proper education is key to combating the spread of misleading content.
Social media undoubtedly plays a significant role in shaping modern culture, particularly in health and fitness. However, its role in perpetuating unrealistic body ideals and promoting harmful behaviors cannot be ignored. By recognizing its potential harms, especially among vulnerable users, we can better understand patients with eating disorders. This approach will help create a more supportive online environment, combat the prevalence of eating disorders, and encourage healthier physical and mental well-being.
References:
1. Fardouly, J., & Vartanian, L. R. (2020). Social media and body image concerns: Current research and future directions. Children and Youth Services Review, 113, 104949. https://doi. org/10.1016/j.childyouth.2020.104949
2. 2. Hunter, A., Stiles, C. E., & Fullwood, C. (2022). Social media and eating disorders: A rapid review of the evidence and applications for prevention and treatment. PLOS Global Public Health, 2(11), e0001091. https://doi.org/10.1371/journal. pgph.0001091
3. 3. Ritchie, H., & Roser, M. (2023). Eating disorders prevalence by age. Our World in Data. Retrieved from https://ourworldindata.org/grapher/eating-disorders-prevalence-by-age
4. 4. Sharif, S. P., Waseem, M., Rana, S., & Razak, N. A. (2021). Social media addiction and psychological wellbeing: A systematic literature review. Journal of Medical Internet Research, 23(1), e17187. https://doi.org/10.2196/17187
5. 5. Sprout Social. (2023). Social media demographics to inform your brand’s strategy in 2023. Retrieved from https://sproutsocial.com/insights/new-social-media-demographics/#instagram

Victoria (Tori) Vargas is a medical student at the Long School of Medicine, Class of 2026.

By Rosa I. Vizcarra, MD, FAAFP
The aging population in the United States has changed significantly over time. Average life expectancy increased from 47 years in 1900 to about 79 years in 2014. By 2030, individuals over the age of 65 will exceed 20 percent of the U.S. population; by 2050, they will constitute over 20 percent of the world’s population. Aging is characterized by weakened homeostasis and diminished organ system reserves. Data in older adults hospitalized for acute medical conditions stated that up to 71 percent of them are at nutritional risk or malnourished, which is associated with higher mortality risk. More people are surviving to an older age and eating well is vital for everyone.
Aging is associated with common physiological changes like decrease in bone mass, lean mass and water content. However, fat mass mainly increases to expand intra-abdominal fat storage. These changes prompt a reduction in basal metabolic rate for the elderly, meaning a standardized nutrition requirement for younger or middle-aged adults cannot be generalized to elderly adults.
Daily food choices are extremely important as they directly impact energy levels on many diseases such as cardiovascular (coronary artery disease, myocardial infarct), neurological (stroke) and endocrinological (diabetes) conditions. Elderly nutritional needs are dictated by
multiple variables including organ compromise, activity levels, food accessibility, ability to prepare and ingest food, as well as personal food preferences.
Older adults should be encouraged to adopt a healthy lifestyle as this lowers their risk of developing a disability. In one cohort of 65 years and older without disability at baseline and followed for 12 years, the risk of developing moderate to severe disability was greater for individuals who had only low or intermediate levels of physical activity, ate less than one serving of fruit or vegetable daily, or were current or recent smokers.
Guidelines from The Food and Nutrition Board of the Institute of Medicine of the National Academies recommend a diet including 20 to 35 percent of energy as fat, with reduced intake of cholesterol, saturated fatty acids and trans fatty acids. They also suggest 45 to 65 percent of energy as carbohydrates, preferably complex carbohydrates in the form of fiber. Daily fiber intake for a 60-year-old consists of 30 grams for males and 21 grams for females. Protein intake is recommended as 10 to 35 percent of total energy.
Recommended dietary allowance (RDA) is the average daily micronutrient intake level estimated to meet the requirement of nearly all (97 to 98 percent) healthy individuals.
of
Selenium
Sodium 2,300 mg (1 teaspoon)* 2,300 mg (1 teaspoon)*
*Sodium if HTN 1,500 mg per day (⅔ teaspoon)
Nutritional status in this population can be influenced by several other factors. It is important to keep these in mind as many can be modifiable.
Risk Factors for Poor Nutritional Status
Alcohol or substance abuse
Cognitive deficiencies
Decreased physical activity
Depression-Mood disorders
Functional limitations
Financial hazard
Limited education
Limited mobility-transportation
Chronic disease process
Poor dentition
Medications
Restricted diet-poor dietary habits
Social Isolation
Obesity is most prevalent in older adults in their 60s and 70s. Excess body weight and modest weight gain (>5kg) in middle age can be associated with medical comorbidities later in life, including hypertension, diabetes mellitus, obstructive sleep apnea and osteoarthritis. Data has also shown that higher BMI in older populations may have a protective effect against mortality rates, with the lowest rates for those with BMI between 27 and 29. The theory is that fat mass stores energy that can be used during negative energy balance states like acute illness. BMI gain or loss was associated with increased mortality whereas BMI stability was not.
It is easier to prevent undernutrition than to treat malnutrition. One recommendation to enhance food intake is to cater to food preferences as much as possible. Patients should receive appropriate hand and mouth care when preparing for meals and be in a comfortable position; assistance should also be provided to those who need help. Increased sociability increases food intake. Food should be of appropriate consistency with attention to color, texture, temperature and arrangement; the use of herbs, spices and temperature could compensate for loss of taste and smell. Hard to open packages are not recommended and adequate time should be given for leisurely meals. Although supplementing protein produces a small but consistent weight gain in older adults, evidence does not support routine supplementation for older adults who are well nourished.
Nutrition is a definite concern for older adults, as there are various factors that have to be accounted for, including significant age-related changes, metabolic diseases, medication interactions and side effects, as well as social and functional components. It is essential to continue to address these factors to ensure the health of the aging population. A healthy diet leads to healthy aging!
References:
1. United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2013
2. Nutritional status of adult patients admitted to internal medicine departments in public hospitals in Castilla y Leon Spain- A multicenter study. De Luis, D., Lopez Guzman A., Nutrition Group of Society of Castilla-Leon (Endocrinology. Diabetes and Nutrition). Eur J Intern Med. 2006; 17(8):556
3. Involuntary weight loss in older outpatients: Incidence and clinical significance. Wallace, J.I., Schwartz, R.S., LaCroix, A.Z., Uhlmann, R.F., Pearlman, R.A. J Am Geriatrics Soc. 1995;43(4):329
4. Geriatric review Syllabus (9th revised edition) by the American Geriatrics Society. Chapter: Nutrition and Weight
5. Unhealthy behaviors and disability in older adults: three city Dijon Cohort Study. BMJ. 2013; 347:f4240 Epub 2013Jul23
6. Institute of Medicine of the National Academies, Food and Nutrition Board. Dietary references intakes. www.iom.edu/Global/Topics/Food-Nutrition.aspx
7. Winter, J.E., Maclnnis, R.J., Wattanapeanpainboon, N., & Nowson, C.A. (2014, April). BMI and all-cause mortality in older adults: AA meta-analysis. The American Journal of Clinical Nutrition,99(4), 875-890
8. Dahl, A.K., Fauth, E.B., Ernst-Bravell, M., Hassings, L.B., Ram, N., & Gerstof, D. (2013, April) Body mass Index, change in body mass index, and survival in old and very old persons. Journal of the American Geriatrics Society, 61(4), 512-518
9. National Institutes of Health State-of-the-Science Panel. (2007, January). National Institute of Health State-of-the Science Conference Statement: Multivitamin/mineral supplements and chronic disease prevention. The American Journal of Clinical Nutrition, 85(1) 257S-264S
10. nia.nih.gov Key vitamins and minerals for people over age 51accessed January 15, 2025

Rosa I. Vizcarra, MD, FAAFP, attended medical school at the Universidad Autonoma of Coahuila in Torreon, Coahuila, Mexico, completing her medical training in Philadelphia, Pennsylvania. A residency in Family Medicine at Drexel University was followed by a fellowship in geriatrics at Thomas Jefferson University. Dr. Vizcarra currently practices primary and preventative care at MacGregor Medical Center, with a passion for geriatrics and addressing health disparities. Dr. Vizcarra is a member of the Bexar County Medical Society

By Laura M. Cascella, MA, CPHRM, courtesy of MedPro Group
Issues related to informed consent are a persistent area of concern in healthcare, and a source of liability exposure. MedPro malpractice claims data show that more than one-fourth of all communication-related malpractice cases involve allegations associated with informed consent.1 Many of these allegations are related to inadequate consent processes and failure to manage patient expectations.
Because of these risks and the important role that informed consent plays in patient-centered care and shared decision-making, healthcare providers and organizations should assess their consent policies and protocols to identify improvement opportunities and monitor for adherence. An initial task during the assessment should focus on reviewing policies related to accountability for the consent process, including responsibility for having the consent discussion with the patient, responding to follow-up questions, and completing appropriate documentation.
MedPro maintains that the informed consent process is a nondelegable duty. This position has been upheld in case law, including a notable court ruling in Pennsylvania. That case, Shinal v. Toms,2 involved a patient who was undergoing surgery to remove a brain tumor. The patient was referred to a neurosurgeon who met with her to discuss surgery options and risks.
A few days after the consultation, the patient called the medical center with several follow-up questions related to scarring, the need
for radiation therapy, and timing of the procedure. The neurosurgeon’s physician assistant (PA) answered the patient’s questions, and later the PA provided the patient with additional information about the surgery and obtained her signature on the informed consent form.
After suffering severe injuries during the procedure, including brain injury and partial blindness, the patient filed a lawsuit alleging inadequate informed consent.3 In a 4-3 ruling in favor of the plaintiff, the Pennsylvania Supreme Court held that:
Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.4
Although this ruling was controversial, it raised a warning flag and gave healthcare providers and organizations a reason to carefully consider their consent policies and who is involved in the informed consent process.
Over the years, MedPro has consistently advised policyholders that the healthcare provider who is performing the surgery, procedure or
treatment must conduct informed consent discussions with the patient — or in certain cases, the patient’s guardian or authorized representative.
Qualified staff members may also participate in the informed consent process by providing general educational information and reinforcing specific information that the treating healthcare provider has communicated to the patient. However, if a patient has questions or is wavering about a decision, staff should refer the patient back to the treating practitioner.
Although these examples of staff involvement are generally accepted practices in many healthcare settings, providers should stay alert to state laws, evolving professional guidance and other potential cases that might establish case law related to informed consent.
Further, healthcare providers should avoid the common misperception that a signed consent form, by itself, demonstrates consent. The form merely documents one phase of the informed consent process. For patients to be truly “informed,” they must understand the information that they have received from their healthcare providers. Thus, as part of the consent process, providers should consider:
• Each patient’s understanding of their condition and the proposed treatment plan
• Each patient’s overall capacity to understand
• Cultural considerations and personal values that might affect each patient’s decision-making
• Any communication barriers that could impede the consent process
Additionally, patients should have ample time during appointments to ask questions, voice concerns, and clarify information with the treating provider.
For more information about the framework for informed consent and legal/professional considerations, see MedPro’s guideline titled Risk Management Strategies for Informed Consent. For curated resources on this topic, see MedPro’s Risk Resources: Informed Consent.
1. MedPro Group communication-related cases, closed 2012-2023
2. Shinal v. Toms, 162 A. 3d 429 (Pa: Supreme Court 2017); Justia, Shinal v. Toms M.D. (majority). Retrieved from https://law.justia.com/cases/pennsylvania/supreme-court/2017/31-map-2016. html
3. Crane, M. (2017, November 30). Legal risks of delegating informed consent to an NP or PA. Medscape. Retrieved from www.medscape.com/viewarticle/887074
4. Shinal v. Toms, 162 A. 3d 429 (2017)
MedPro Group is a Silver Member of the BCMS Circle of Friends Program.
The Texas Legislature meets every odd-numbered year for 140 consecutive days and will convene again January 14, 2025. Legislators need to hear from you — their physician, medical student and alliance constituents — during the session to understand how proposed legislation can potentially impact the practice of medicine in Texas.
Mark your calendar for 2025 First Tuesdays at the Capitol.
• February 4
• March 4 (TMA Alliance and Young Physician Month)
• April 1 (TMA Medical Student and Resident Month)
• May 6
Dr. John J. Nava, Sr., passed away on December 23, 2024. He was a cherished physician, colleague and friend. We are profoundly grateful for his decades of active involvement with the Bexar County Medical Society (BCMS), particularly during his tenure as the 2023 BCMS President.
Dr. Nava joined BCMS in 1979 and served as a respected leader in various roles. His committee participation was extensive, including the Public Health and Patient Advocacy Committee (2002-2024), Emergency Preparedness Committee (2009-2024), Delegation to the TMA (2003-2024), and Legislative and Socioeconomics Committee (2004-2024). He held numerous roles on the BCMS Executive Committee and was Chair of the COVID-19 Task Force. Most recently, he established and served as the Chair of the ad-hoc committee on Physician Wellness.
A native of San Antonio, Dr. Nava completed his residency in family medicine in 1988 and dedicated 39 years to serving his hometown as a Family Medicine physician. His passion for public health and patient health and safety was evident throughout his career. Dr. Nava served the City of San Antonio in various capacities at the Metropolitan Health District from 1998-2013. He was always one of the first to volunteer to represent BCMS at public health fairs and community events. His commitment to organized medicine made a lasting impact on his fellow physicians and patients alike.
Bexar County Medical Society extends its deepest condolences to the Nava family and those who were fortunate enough to know Dr. Nava. He is greatly missed, and the medical society and community will forever cherish his memory.






Happy Doctors’ Day! Today, we celebrate you — physicians, healers and leaders — who dedicate your lives to the care and well-being of others. Your expertise, compassion and commitment in service of others shapes the health and future of our communities. As we honor your contributions, we must also address an essential truth: you deserve the same level of compassion and support that you provide to others.
That is why, on behalf of the BCMS Physician Wellness Committee, we invite you to join us for our next Wellness & Leadership Masterclass, led by Nora Vasquez MD, Certified High-Performance Coach for Medical Professionals, Leaders and Executives. Dr. Vasquez is Chair of the Physician Wellness Committee for the Bexar County Medical Society and serves on the Texas Medical Association’s Council for Member Experience.
If you’d like to explore evidence-based strategies that enhance your leadership development and well-being, attend our next 2025 Masterclasses via zoom at 7:00 p.m. CST on:
Tuesday, February 25
Sunday, March 23
Tuesday, April 15
Sunday, May 18
The Bexar County Medical Society hosted its first 1853 Club luncheon of 2025, a gathering dedicated to bringing together retired member physicians. These luncheons, held on a quarterly basis, serve as an opportunity for retired members to reconnect with colleagues and friends while becoming informed on various topics presented by guest speakers.
At the January 14 luncheon, presenter Zachary Clark, CFP, Vice President and Financial Advisor at Aspect Wealth Management, spoke on “Smart Home; Smartphone to Enhance Senior Living.”
2025 Luncheon Dates and Topics:
• April 8: Healthy Diet, Healthy Living
• July 8: Keeping Your Mind Sharp
• October 7: Dr Aureliano Urrutia Story – Anna Elise Urrutia
If you are a retired or life BCMS member and are interested in joining the 1853 Club, please reach out to membership@bcms.org or 210-301-4391.
Bexar County Medical Society understands the importance of creating ample opportunity for our members to connect in person and to continue hosting the 1853 Club luncheons to ensure everyone can enjoy its benefits and endeavors. As such, we are requesting that all participants make a small donation of $50 each year to help offset the costs of the luncheons. This annual donation covers all four scheduled luncheons and is lower than the rate set by other neighboring medical societies with similar programs. Spouses will be allowed to attend the luncheons free of charge.
To make your donation by check, please mail to: BCMS, 4334 N Loop 1604 W, Ste 200, San Antonio, TX 78249.
We thank you for your support and are looking forward to our future luncheons.





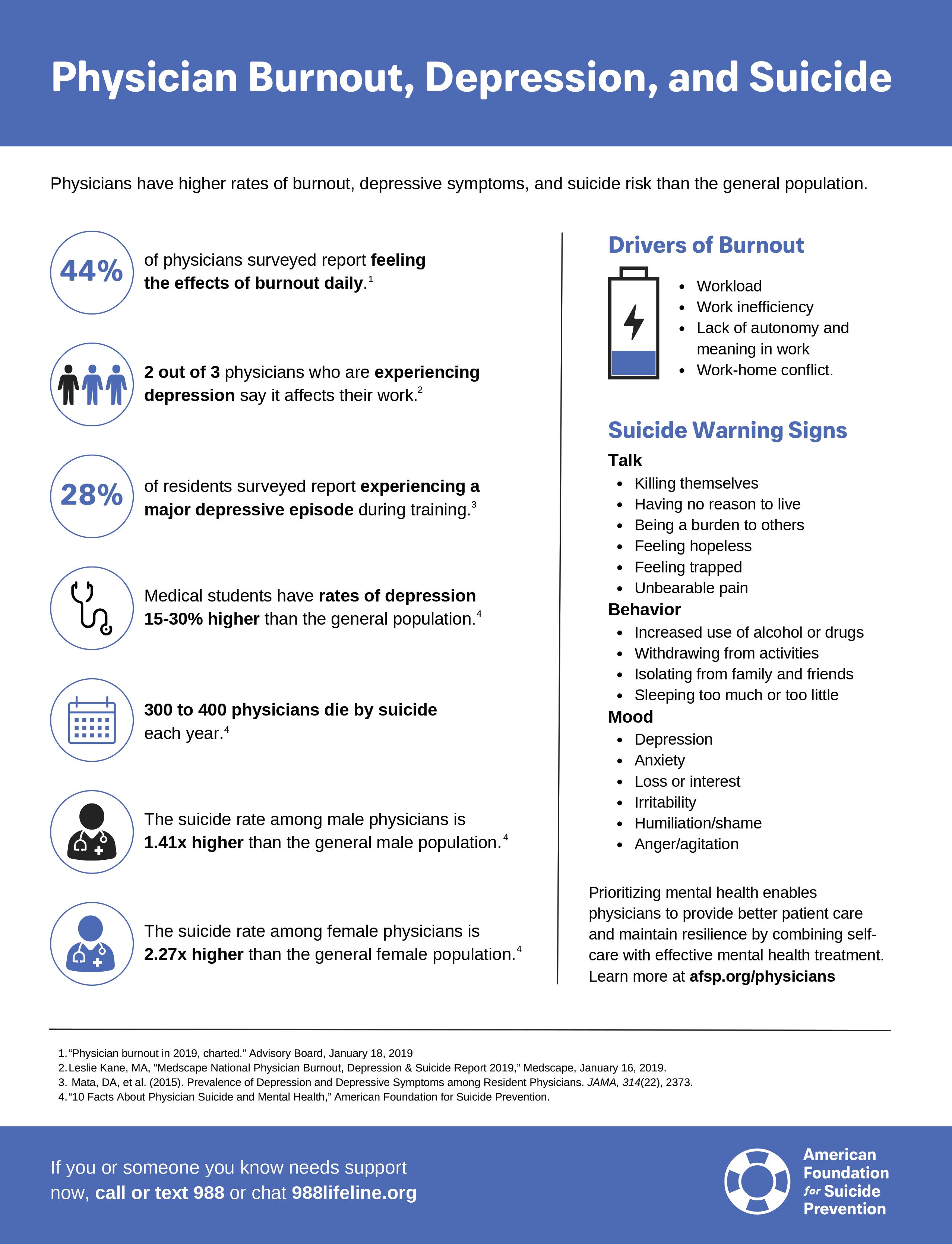
The 2025 BCMS Joint Installation of Officers was held on Saturday, January 25, at TSAOG Orthopaedics.
Dr. John M. Shepherd was sworn in as the 2025 BCMS President.
Dr. David N. Henkes was awarded the Golden Aesculapius Lifetime Service Award, and Drs. Adam V. Ratner and Abe Rodriguez received Distinguished Service Awards.



By Gabriella Bradberry
The Bexar County Medical Society recognized three of its most distinguished and long-serving members during the 2025 Installation Ceremony on January 25. The honorees were Dr. David N. Henkes who received the Golden Aesculapius Lifetime Service Award; and Drs. Adam V. Ratner and Abe Rodriguez who both received the 2025 Distinguished Service Award.
David N. Henkes, MD - 2025 Golden Aesculapius Honoree
Dr. David N. Henkes was inspired to pursue a career in medicine as a young boy. Growing up, he had a childhood friend whose father worked as a representative of a pharmaceutical company that made plastic models of various organs. Young David Henkes was gifted some of these models and immediately became enthralled with the world of medicine. He promptly told his parents he was going to become a doctor and even put a sign on his bedroom door that read, “David Henkes, MD.”
This childhood passion developed into the accomplished medical career Dr. Henkes has today. He shared that a mentor once told him, “Being a professional is not what you can get from your profession, but what you can contribute back to advance your profession.” This mindset has led Dr. Henkes to find his greatest sense of work accomplishment in being recognized by his peers and profession as being a physician and patient advocate. Recognition highlights include Past President of BCMS, 2025 BCMS Golden Aesculapius Honoree, recipient of the George T Caldwell Award for Distinguished Service from the Texas Society of Pathologists, and being elected as Chair of the Texas Medical Association Delegation to the AMA.
A career in the medical field prompts the great challenge of balancing work and personal life. Dr. Henkes credits the support of his wife and children for allowing him to find balance between the two. He also shared that there is joy in both of these worlds coming together, such as when he had the opportunity to hood his daughter on her graduation from medical school.
His Bexar County Medical Society Presidency in 2005 was highlighted by both challenges and accomplishments. Dr. Henkes’ term coincided with hurricanes Katrina and Rita. This led Dr. Henkes to tour the Brooks City Base facility where many evacuees were staying; there, he witnessed firsthand the devastation and impact it had on their lives. BCMS was challenged with coordinating the physician volunteers to ensure the facility had sufficient coverage. While difficult, Dr. Henkes is proud of how so many members helped triage and care for patients.

David N. Henkes, MD
Unprecedented events such as the devastation of the hurricanes can alter plans at a moment’s notice. Going into his presidency, Dr. Henkes thought he would be spending more time on physician and patient advocacy issues. Several other past presidents who had similarly large events develop and change the focus of their presidencies have shared the same sentiment. Dr. Henkes shares this advice to all future BCMS Presidents, “Be flexible, and be ready for the unexpected.”
Working as a physician, and specifically as a pathologist, serves as a reminder to Dr. Henkes that our lives are God’s gifts, and we should live life to the fullest each day. Dr. Henkes fulfills this reminder by taking time after work to be outside, gardening and enjoying his lake house with his family. The Bexar County Medical Society congratulates Dr. David N. Henkes, on his dedication to the field of medicine and recognizes him as our 2025 Golden Aesculapius Honoree.
Adam V. Ratner, MD - 2025 Distinguished Service Honoree
Dr. Adam V. Ratner credits a familial calling to medicine as his inspiration to become a doctor. He refers to medicine as “a genetic disorder in my family.” Since Dr. Ratner was a young boy, he was eager to make rounds with his father, a pediatric surgeon.
One of Dr. Ratner’s proudest accomplishments was achieved when he was only a medical student and had the unlikely chance to author a chapter in a textbook. During his studies, he researched a brand-new field of cardiac magnetic resonance imaging and was asked to share his findings in Braunwald’s Textbook of Cardiology. This feat was only the beginning of the prosperous career we admire today. As a physician, Dr. Ratner would go on to work in private practice of radiology for nearly 20 years, co-found and serve as chair for the nonprofit, The Patient Institute, and teach at both UIW School of Osteopathic Medicine and UT Health San Antonio.
Having served as the Bexar County Medical Society President in 2019, Dr. Ratner was inspired by his daughter, then a medical student and now a Geriatric Psychiatrist, to establish the first BCMS Physician Wellness Program. The program remains active today and provides physicians with confidential mental wellness resources, support lines, webinars and events. Dr. Ratner also remains actively involved in the medical society and continues to offer support and advice to current BCMS Presidents and fellow physicians.
A lifelong career as a physician is not without challenges. Dr. Ratner frequently witnessed personal suffering firsthand throughout his career.
When asked what originally inspired him to pursue what would become a life-long career in medicine, Dr. Abe Rodriguez would tell you his interest in the field began in high school. While there were several physicians in his family before him, he attributes his career choice to a natural inclination rather than due to outside influence. Dr. Rodriguez felt intrinsically drawn to the field of medicine from a young age and never wavered from that goal.
This calling has ultimately rewarded Dr. Rodriguez with a successful career in family medicine that has lasted 52 years and counting. Finding his footing in the profession has not gone without its challenges. Dr. Rodriguez began his pursuit of solo practice in 1977, and his early career was met with navigating practice upkeep, hospital medical affairs, insurance regulations, and witnessing the evolution of the practice of medicine firsthand. Overcoming such challenges has allowed Dr. Rodriguez to build relationships with his patients that have lasted throughout the years. He highlights caring for his patients as the utmost rewarding part of his career.
Membership in the Bexar County Medical Society has also been a fruitful pursuit in Dr. Rodriguez’s career. He has been an active member of the medical society since 1977 and throughout his membership has served as BCMS Vice President and Chairman of the Legislative Committee. One accomplishment he is especially proud to have been a part of is in 2001 when the medical society was able to assist in the fight to cap the malpractice award for noneconomic damages resulting in Tort Reform legislation. Overall, Dr. Rodriguez cherishes his involvement with Bexar County Medical Society and is happy to see younger physicians join and take up the challenges organized medicine faces every day.

He shared that such experiences have shaped him as a person and remind him of the great importance of caring for and healing a patient.
In addition to being a devoted physician, Dr. Ratner is a commercially rated pilot. In his free time, he may be found flying his airplane, playing with electronics and computers, and sharing quality time with family and friends. The Bexar County Medical Society congratulates Dr. Adam V. Ratner on his contributions to the field of medicine and awarded him as our 2025 Distinguished Service Honoree.
Dr. Rodriguez’s experiences as both a practicing physician and advocate for organized medicine have shaped him not only as a professional, but in his personal life as well. He considers it a blessing that being a physician allows him to recognize the challenges others experience. This has shaped his worldview, granting him the ability to be more empathetic, nonjudgemental, and truly recognize the importance of each individual he encounters.
In his free time, you will find Dr. Rodriguez gardening, reading, exercising and, most importantly, enjoying time with his family. Overall, Dr. Abe Rodriguez shares his great spirit with others both inside and outside of the clinic, leading Bexar County Medical Society to award him as our 2025 Distinguished Service Honoree.
We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 CDavis@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President
210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@broadway.bank www.broadwaybank.com
“We’re here for good.”

Texas Partners Banks (HHH Gold Sponsor)
Our private banking team specializes in healthcare banking and will work with you to craft and seamlessly integrate financial solutions for you and your practice, including practice loans, lines
of credit and custom local lockbox solutions headquartered in San Antonio. Maria Breen 210-807-5562
Maria.Breen@texaspartners.bank www.texaspartners.bank

Lone Star National Bank (HHH Gold Sponsor)
Established in 1983, Lone Star National Bank has provided banking services to communities in South Texas for the past 41 years. LSNB is an independent and locally owned bank subsidiary of Lone Star National Bancshares-Texas, Inc with consolidated assets of $3 billion (12/31/23) and 36 full-service banking centers throughout Starr, Hidalgo, Cameron and Bexar counties. Aside from personal and business banking, LSNB offers investments, wealth management & trust along with property and casualty insurance, health insurance and supplemental coverage.
Ivan Corona Molina Assistant VP 210-479-4713
MolinaI@lonestarnationalbank.com www.lonestarnationalbank.com
“We do what the Little Banks can’t, and the Big Banks won’t!”
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison 210-503-0003
Yulia@genicslabs.com
Kevin Setanyan Managing Partner 210-503-0003
Kevin@genicslabs.com
Artyom Vardapetyan Managing Partner 210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease and Genetics.
Robert Castaneda CEO 210-316-1792
Robert@livingstonmedlab.com www.livingstonmedlab.com/home
“Trusted Innovative, Accurate and STAT Medical Diagnostics”

American Health Imaging (HHH Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina.

US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora
Jaime.Zamora@usradiology.com
Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com
www.americanhealthimaging.com (main site)
www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor 210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Hancock Whitney (HHH Gold Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Larry Anthis Corporate Banking, Relationship Manager 210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez
San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington
Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com www.hancockwhitney.com

UT Health San Antonio
MD Anderson Cancer Center
(HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
(H Bronze Sponsor)
We were founded to meet a need: helping business owners succeed by giving them simple, quality, affordable U.S.-based contact solutions. In only a few years, our focus on nurturing client relations and building trust not only helped our customers grow their businesses, but helped us stake our claim in the highly competitive TAS industry as one of the most well-regarded and referred. Our 50 years of collective experience are the driving force behind our clients’ satisfaction.
Rachel Caero Managing Partner 844-554-3473
Rachel@dialops.net
(HH Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Fran Yacovone
Business Performance Advisor 210-558-2507
Fran.Yacovone@insperity.com
Dayton Parker Business Performance Advisor 210-558-2517
Dayton.Parker@insperity.com www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”

TMA Insurance Trust
(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service
insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits
512-370-1746
Wendell.England@tmait.org 800-880-8181 www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com

LASO Health Telemedicine and Rx App (HHH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care.
LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

(HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer 210-632-3411
DrJohn@parvussuites.com www.parvussuites.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol Field Sales Consultant
210-413-8079
Tom.Rosol@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Darby Rodriguez Regional Client Executive 281-753-3565
D.Rodriguez@eleosvhs.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President 210-308-7907 (Direct) KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising. Jeannine Ruffner President info4@samgma.org www.samgma.org

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
San Antonio Office 210-301-4362
www.favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”


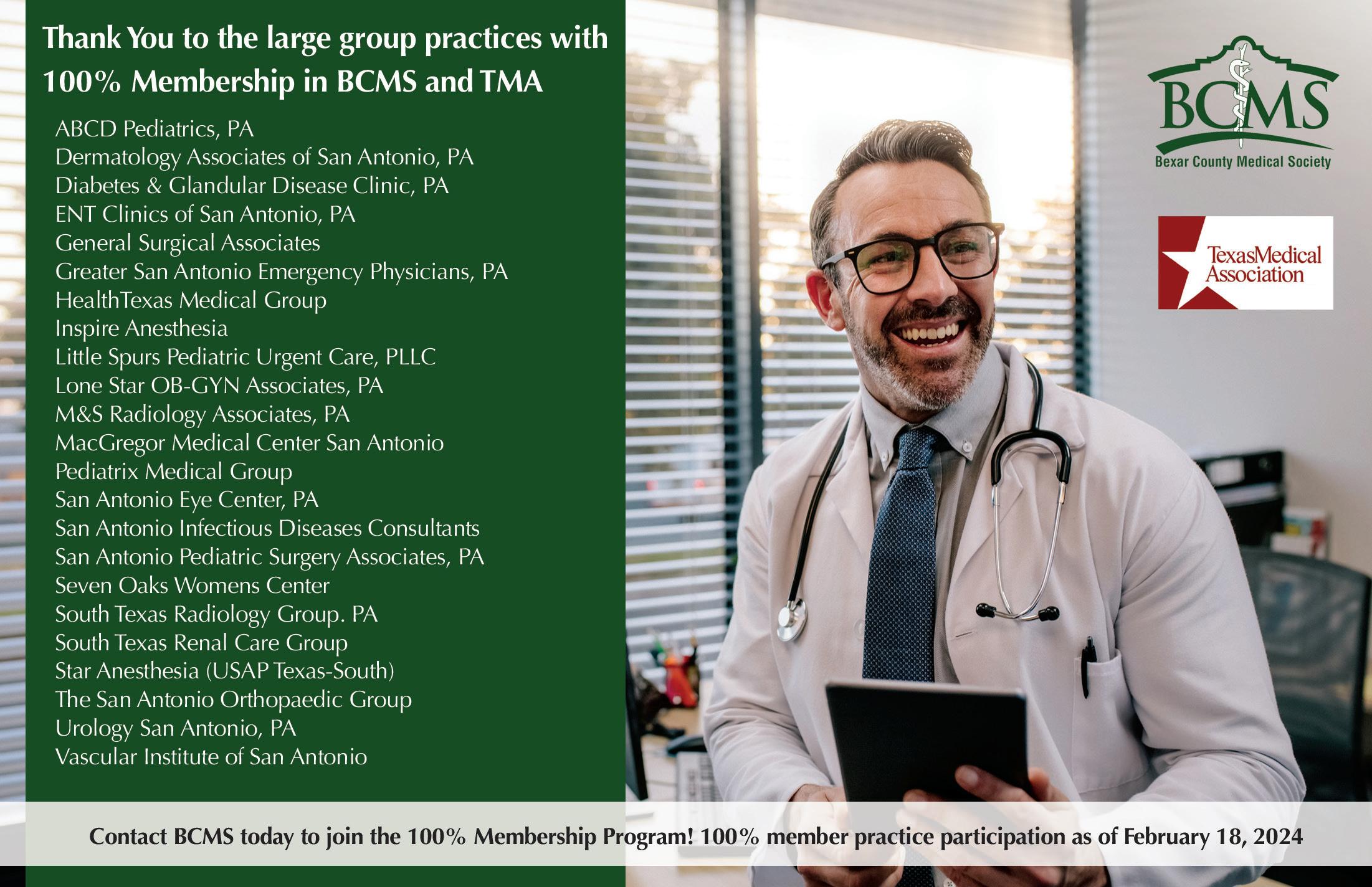

By Stephen Schutz, MD
In an automotive landscape increasingly homogenized by boring BEVs and crossovers, the 2024 Subaru WRX remains a defiantly analog vehicle, closely connected to its rally-bred DNA. Yet, beneath its rugged roots, the latest WRX reveals surprising sophistication. It’s as if the engineers at Subaru decided to take their street fighter and send it off to finishing school.
Design-wise, the 2024 WRX does not attempt to blend into the crowd. Angular creases carve out a purposeful stance, while black cladding along the wheel arches signals rugged intent. And the “look at me” hood scoop — a nod to its potent turbocharged engine — separates the WRX from its more civilized contemporaries.
While other manufacturers obsess over sleek aerodynamics, particularly with their BEVs, the WRX has been and will always be a no-nonsense tool for spirited driving, and I applaud Subaru for it. Bring on the creases and plastic cladding.
Step inside, and the WRX’s interior reflects an interesting dichotomy. It’s no Audi rival — don’t expect soft-touch leather covering every surface — but it’s definitely an improvement for Subaru, which generally prioritizes function over fashion. The materials are rugged, durable and well-assembled, qualities that owners doubtless appreciate over time, but they’re also noticeably nicer than they were in the last WRX I tested about four years ago.
A prominent 11.6-inch infotainment touchscreen dominates the center stack, offering Apple CarPlay, Android Auto and more. The user interface is intuitive, though occasionally sluggish, and while some (like me) may bemoan the reliance on touch controls for functions once governed by satisfying physical buttons and knobs, it works.
Seating remains a WRX strong suit, with deeply bolstered sports seats that hug you through the tightest of turns. Rear passenger space is pretty generous, thanks to clever packaging; I’m 6’2” and I was OK back there.


At the heart of the WRX lies a new turbocharged 2.4-liter flat-four engine delivering 271 horsepower and 258 lb-ft of torque. Those aren’t headline-grabbing numbers in today’s horsepower arms race, but they translate into a driving experience that’s refreshingly quick. The powerband is broad, delivering thrust that feels eager yet linear, and there’s minimal turbo lag.
It should be noted that the new WRX engine is quite different from the last one. While the new motor’s linearity is unquestionably nice, I miss the previous one’s “all on or all off” vibe. With the old engine, you’d sit and wait until the tach hit 4500RPM, and then, Bam, Big Power. Obviously, smooth predictability is “better,” but it’s also less fun. I described the old engine as, “a John McEnroe in a world of Roger Federers,” which means that the new WRX’s engine is now a Roger Federer. Sigh. Having said that, the WRX is still more fun than just about any other reasonably priced car for sale today.
The six-speed manual gearbox remains the weapon of choice for enthusiasts. It’s not the slickest shifter on the market, but the mechanical engagement is satisfying and way better than any automatic. For those opting for convenience, Subaru’s continuously variable automatic transmission (CVT) offers simulated gear steps and rapid response, though it lacks the tactile joy of its manual sibling.
On the road, Subaru’s renowned Symmetrical All-Wheel Drive system provides near-unflappable grip, whether you’re hooning over canyon roads or carefully navigating a curvy highway during a downpour (which I did). The suspension, equipped with adaptive dampers if you choose the GT trim, works well. Body roll is minimal, and the steering is precise, if a touch numb — a small blemish in an otherwise excellent package.
The WRX thrives in conditions where lesser cars falter. Uneven roads, rain, snow or even gravel? Bring it on. It’s a reminder that Subaru builds vehicles for those of us who see driving as more than just a commute.
Is now a good time to mention that Subaru just passed Toyota and Lexus to claim the title of, “Most Reliable Car Brand” from Consumer Reports? It’s true.
WRXs start at just under $37,000 and go up to $47,000 or so, if you check all the boxes. Fuel economy is an uninspiring 19MPG City and 26MPG Highway.
The 2024 Subaru WRX is a paradoxical gem: old-school charm wrapped in modern sensibilities. It provides accessible performance for those of us who value driving as an art form, and while it may lack the polish of some rivals such as the Volkswagen Golf R, the WRX’s attraction lies in its imperfections, raw edges and unapologetic character.
If you’re seeking a (small) car that can do it all — commute, carve, and conquer the elements, plus provide a manual transmission option — the Subaru WRX is an excellent choice. Get it while you can.

Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.





Auto Group
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Auto Group
Northside Honda
9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Auto Group
Lamborghini San Antonio 27605 IH 10 West Boerne, TX
Douglas Cox 210-600-5770
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600 9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945

Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000