












Changing Patterns of Hospital Patient Care in 2024
By John J. Seidenfeld, MD, MSHA, FACP 12
Thinking Outside the Box Delivered Outcomes in Type 2 Diabetes
By William Trigoso, MD, FACE, and Tina Copple, DNP, FNP-BC, CDCES 14
The Impact of AI on Healthcare Costs
By Ronald Rodriguez, MD, PhD, with Parin Chanana 16
Omega-3 Fatty Acids: Nothing Fishy About the Benefits
By Philip Makedon, MEd, MLS(ASCP); Cooper Allenbrand, BS, BA; and Ramaswamy Sharma, MS, PhD 18
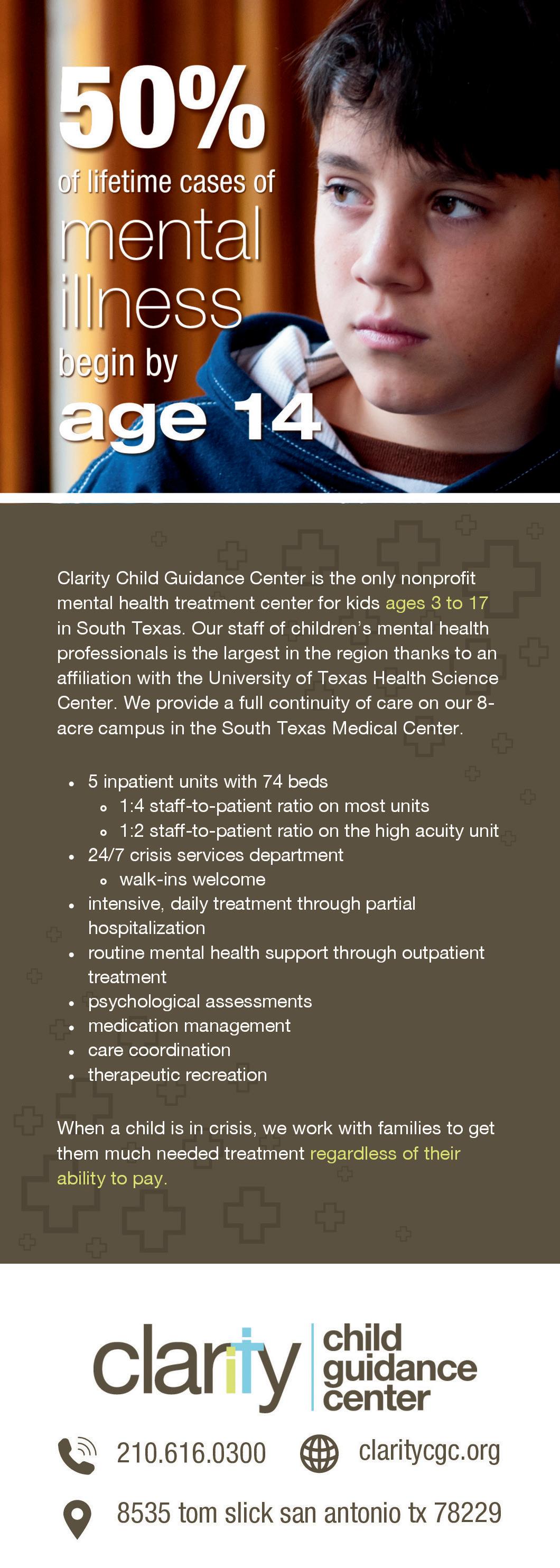
Suicide Prevention Resources: University Health’s Zero Suicide and CoSPLAY Programs
By Mercedes Ingram, PhD, LPC 20
When a Micro Discovery Leads to a Nobel Prize®
By Kreny Savaliya, Hunter Buescher and Ramaswamy Sharma, MS, PhD 22
High-Performance Goal Setting: 3 Steps to Make 2025 Your Best Year Yet!
By Nora Vasquez, MD, CHPC 24
Where
Breakthroughs
The State of Texas Association of Rheumatologists Establishes a $2 Million Fellowship Training Awards Endowment Fund for the Five Adult Programs in Texas By Rodolfo “Rudy” Molina, MD, FACP, MACR, and Brian R. Loggins, BS, BBA, MBA
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE: Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC. A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
Inc.
and operated San Antonio-based printing and publishing company
has
business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2024 SmithPrint, Inc. PRINTED IN THE USA


Ezequiel “Zeke” Silva, III, MD, President
Lyssa Ochoa, MD, Vice President
John Shepherd, MD, President-elect
Jennifer R. Rushton, MD, Treasurer
Lubna Naeem, MD, Secretary
John Joseph Nava, MD, Immediate Past President
Woodson “Scott” Jones, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Ana Rodriguez, MD, Member
Raul Santoscoy, DO, Member
Lauren Tarbox, MD, Member
Nancy Vacca, MD, Member
Col. Elisa D. O’Hern, MD, MC, FS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School
Representative
Cynthia Cantu, DO, Medical School Representative
Lori Kels, MD, Medical School Representative
Ronald Rodriguez, MD, Medical School Representative
Victoria Kohler-Webb, BCMS Alliance Representative
Carolina Arias, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
BCMS SENIOR STAFF
Melody Newsom, CEO/Executive Director
Yvonne Nino, Controller
Al Ortiz, Chief Information Officer
Brissa Vela, Chief Membership and Development Officer
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
PUBLICATIONS COMMITTEE
Monica Jacqueline Salas, MD, Co-chair
Jennifer C. Seger, MD, Co-chair
Lokesh Bathla, MD, Member
Elizabeth Clanton, MD, Member
Erika Gabriela Gonzalez-Reyes, MD, Member
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. K. Jyothula, MD, Member
Kristy Yvonne Kosub, MD, Member
Jaime Pankowsky, MD, Member
George-Thomas Martin Pugh, MD, Member
Rajam S. Ramamurthy, MD, Member
Adam V. Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Boulos Toursarkissian, MD, Member
Francis Vu Tran, MD, Member
Faraz Yousefian, DO, Member
Louis Doucette, Consultant
Brissa Vela, Consultant
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Deepthi S. Akella, Student
Moses Alfaro, Student
Victoria Ayodele, Student
Tue Felix Nguyen, Student
Andrew Ta, Student
Alixandria Fiore Pfeiffer, DO, Resident
Elizabeth Allen, Volunteer
Adelita G. Cantu, PhD, Volunteer
Rita Espinoza, DrPH, Volunteer
Natalie Reyna Nyren, PA-C, Volunteer
David Schulz, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer
By Ezequiel "Zeke" Silva III, President, Bexar County Medical Society (BCMS)
This is my final column as BCMS President for 2024.
In January, I outlined my aspirations for the year, which we have successfully met through the exceptional teamwork of BCMS leadership, members, staff and community partners. Here, I share examples of our success and the ongoing potential for future achievements.
Maximizing BCMS’ Value to Our Members:
In February, I emphasized our mission to understand and meet members’ needs, ensuring BCMS remains essential for their professional and personal growth.
Achievements:
• Membership has grown to over 6,000, surpassing 2023’s total.
• Readership of San Antonio Medicine, including online views, continues to rise.
• Our social media presence has expanded with an increasing number of impressions each month.
• We continue to serve as a center for physician wellness and professional development, offering numerous CME opportunities.
Enhancing Member Experience:
In February, I reaffirmed our commitment to adapting our services to meet members’ evolving needs and recognizing the importance of their contributions.
Achievements:
• Social events have returned to pre-pandemic levels, including the Women Leaders in Medicine and Spring and Fall Mixers.
• Our leadership includes community, hospital and practice leaders, enriching our board, committees and delegation to the Texas Medical Association (TMA).
• Outreach to medical students and residents has increased, with initiatives to promote advocacy and engagement from the earliest stages of their careers.
• Our club for retired physicians, the 1853 Club, has grown, offering valuable educational and social activities.
Increasing BCMS Representation:
In April, I discussed our active role in the TMA, and in September, the importance of strengthening community partnerships.
Achievements:
• Nearly 30 delegates represented us at TexMed 2024, aiding in the election of past BCMS President, Jayesh Shah, as TMA President-Elect.
• Our community partnerships, such as with the San Antonio Medical Foundation and STRAC, have significantly increased.

Conclusion:
In my opening January column, I wrote the following:
I firmly believe in the power of associations, echoing the words of President Theodore Roosevelt in 1908: “Every man owes part of his time to the business or industry to which he is engaged. No man has a moral right to withhold his support from an organization that is striving to improve conditions within his sphere.” Today, this statement is inclusive of every citizen.
My year as President has deepened my belief in the critical role of BCMS in supporting our profession and community. Through our collective effort, we enhance our practices, benefit our patients, and strengthen our community.
I am grateful for your trust and commitment, which have made this year’s achievements possible.
Thank you.
Ezequiel “Zeke” Silva III, MD, is the 2024 President of the Bexar County Medical Society. Dr. Silva is a radiologist with the South Texas Radiology Group, Adjunct Professor of Radiology at the UT Health, Long School of Medicine, and Vice-Chief of Staff at Methodist Hospital Texsan. He is Chair of the TMA Council on Legislation and is a TMA Delegate to the AMA. He serves on the AMA Council on Medical Service, and chairs the AMA RVS Update Committee (RUC).




By Victoria Kohler-Webb, BBA, MS
We serve our Members. We serve our Community. Service is the essence of the Bexar County Medical Society Alliance, and the friendships we build together in the process keep us all coming back year after year. For over 100 years, we have strengthened our physician families by providing a combination of relevant educational resources and exciting social offerings.
President-Elect, introduced and congratulated BCMSA scholarship winner Neriah Sosa. We offer heartfelt thanks to our hosts, TMAA President Jenny Shepherd and Dr. John Shepherd, President-Elect, BCMS, for hosting us in their lovely home.




Our Pink Out Fall Luncheon and General Meeting is a perfect example! Attired in pink, our members gathered to enjoy an elegant lunch buffet, signature cocktails and each other’s company. Keynote Speaker Dr. Stephanie Schaefer, FACOG, presented an in-depth, engaging and informative discussion about Breast Cancer Awareness. In addition, Dr. Schaefer highlighted the community need for the Alliance Period Poverty Project and underscored the importance of this Alliance initiative. Jenny Shepherd presented an update on TMAA programs and underscored specifically how TMA and TEXPAC serves all physicians and their livelihoods. As always, I was on hand to highlight our membership drive and to update our members about BCMSA programs and upcoming events. Brittany
What an exciting year for our Alliance! I have enjoyed every minute that I have spent as President and I extend a huge thank you to our 2024 Board. Past-Presidents Jenny Shepherd and Danielle Henkes continue to be such a blessing to my life both as friends and as the best Presidential Advisors you could ask for. I am so excited for President-Elect Brittany Garcia-Noche, and I know she will lead our Alliance in 2025 beautifully. Keep up with your Alliance on Facebook/Bexar County Medical Society Alliance and see everything we do!
Garcia,

Victoria Kohler-Webb, BBA, MS Marketing Statistics, is the 2024 Alliance President. She and Ben, an ENT/Head & Neck Surgeon, are proud Aggies and parents to Luke, 15, and four rescue dogs.


For information on the Bexar County Medical Society Alliance, scan the code.

By John J. Seidenfeld, MD, MSHA, FACP
The metaphor of “Frog warming in an increasingly hot bath” is applicable to the change in hospital care we have seen over the past twenty years. You do not realize the dramatic changes in hospital care in 2024 until you need to access it. Now, human-like robotic voices through either algorithmic or artificial intelligence (AI) phone instructions direct us to the emergency room for daytime, after hours and weekend care. Twenty years ago, we would contact our family doctor to be examined at the office, in the patient’s home, or at the emergency room. In the previous model, the patient and primary care physician, after a careful history and examination, would craft a strategy for diagnosis, consultation with specialists, and treatment once hospitalized. We now have a significantly different approach to care.1-5 Currently the ER physician, contracted often through a group, decides on initial care and admission, and then contacts a hospitalist contracted with the hospital. Allegiances are unclear; the patient, the group, the hospital, the contract and the corporation all have influence on the physician. The hospitalist plans (with or without the patient’s input) diagnosis, and consultation and treatment.6,7 Training of hospitalists varies, and they are mostly residency trained internists, family practitioners or pediatricians. Physician societies give certification or designation for these doctors, but these certificates are not available at the time of care and usually not communicated so the patient is unaware of a physician’s credentials. Critical medical histories often become the work of aides and AI instead of careful work by trained physicians, and histories derived from interview and exam are often abbreviated by specialists and focused in most cases. The result might be characterized by a critical practitioner or patient reviewer by the GIGO (garbage in garbage
out) adage whereby flawed, biased or poor-quality information or input produces a result or output of similar quality.8
Often the patient is left out of the initial care discussion, and consultants and diagnostic procedures begin in the ER and proceed throughout the hospitalization. A critical difference in these processes is that the choice of medical consultants and nurse practitioner specialists, diagnostic tests and treatment are no longer done by the patient and their primary care doctor. Often in this era of managed care, the caregivers may be out of network and procedures may not be authorized by the insurer. In this case, the patient ends up with out of network bills, which increase the cost of the hospitalization and add confusion to the already complicated process.
Overall, the pattern of medical care for hospitalized patients is constantly evolving, driven by factors such as technological advancements, changing demographics and healthcare policy shifts. Staying informed about these changes is crucial for healthcare providers to deliver high-quality, patient-centered care in the hospital setting. Patients are often unaware of the many changes that comprise their care. What are the changing patterns of medical care for hospitalized patients? Below are key trends and observations:
• Increased Complexity of Patient Cases: As baby boomers, an unusually large population group, require hospitalization, there is a rise in patients with multiple chronic conditions and comorbidities, leading to more complex medical needs and treatment plans. This trend necessitates a greater focus on careful history taking, care coordination and multidisciplinary teams. Are the changes noted above up to this challenge? Did COVID hospitalizations increase avoidable out-of-hospital deaths for those without COVID?
• Shorter Hospital Stays: Due to managed care and advancements in technology and treatment approaches, hospital stays are generally becoming shorter. This shift emphasizes the importance of effective discharge planning and transitional care to ensure patients receive appropriate support and follow-up after leaving the hospital. It is critical to have family and patient input in this decision-making process.
2
• Rise of Telemedicine and Remote Monitoring: The COVID-19 pandemic accelerated the adoption of telemedicine and remote patient monitoring technologies, which are now being integrated into routine hospital care. These tools enable virtual consultations, remote monitoring of vital signs, and improved communication between patients and healthcare providers. Many seniors miss out on this change due to being less tech savvy and lacking internet resources, particularly in rural areas.9
• Emphasis on Value-Based Care: The healthcare industry is moving towards a value-based care model, where reimbursement is tied to patient outcomes and the quality of care. This shift incentivizes hospitals to focus on reducing readmissions, preventing complications, and improving patient satisfaction. The data is unclear currently as to the achievement of these aspirational goals.10
• Growing Role of Hospitalists: Hospitalists, physicians who specialize in inpatient care, are becoming more prevalent in hospitals. They provide dedicated care to hospitalized patients, thus allowing primary care physicians to focus on outpatient care and continuity of care. Is the patient best served by this model where patients may see several hospitalists during their stay due to shift handoffs and rotations? We must ensure that doctors who choose this work are deeply devoted to patient care and work with specialists to tailor care to the patient’s needs. They cannot cede the care to the specialists and must constantly advocate for their patients as captain of the care team despite the pull of other allegiances.
• Focus on Patient-Centered Care: The concept of patient-centered care is gaining momentum, emphasizing patients’ preferences, values and needs in the decision-making process. This approach includes involving patients in their care plans, providing them with information and resources, and ensuring clear communication throughout the hospitalization. This approach is largely aspirational at this time in the San Antonio community. (personal communication)
Whatever our concerns are, we will not be going back anytime soon. We must do our best as physicians to make sure that hospitalized patients or their designated caregivers become partners in care and planning, and we must make sure that their improvement and return to wellness is topmost in our minds. To do this, we must put the interests of the patient above corporations that employ us, hospitals that give us privileges to practice in their institutions, managed care companies that we credential and contract with to care for their enrollees and pharmaceutical companies that reach into practice by employment (CVS model) and education. The complexity and power and priority differentials of this environment should be focused on the excellent care of our patients, and further research is needed in this area to complete the quality circle of Edward Deming. As Deming said, “In God we trust: all others bring data.”11
References:
1. Goodwin J.S., Li S., Zhou J., Kuo Y.F., Nattinger A. Variation among hospitals in the continuity of care for older hospitalized patients: a cross-sectional cohort study. BMC Health Serv Res. 2021 Jun 5;21(1):552. doi: 10.1186/s12913-021-06584-0. PMID: 34090431; PMCID: PMC8180074
2. Goodwin J.S., Li S., Kuo Y.F. Association of the Work Schedules of Hospitalists with Patient Outcomes of Hospitalization. JAMA Intern Med. 2020 Feb 1;180(2):215-222. doi: 10.1001/jamainternmed.2019.5193. PMID: 31764937; PMCID: PMC6902197
3. Farid M., Tsugawa Y., Jena A.B. Assessment of Care Handoffs Among Hospitalist Physicians and 30-Day Mortality in Hospitalized Medicare Beneficiaries. JAMA Netw Open. 2021 Mar 1;4(3):e213040. doi: 10.1001/jamanetworkopen.2021.3040. PMID: 33760093; PMCID: PMC7991971
4. Stommel M., Olomu A., Holmes-Rovner M., Corser W., Gardiner J.C. Changes in practice patterns affecting in-hospital and post-discharge survival among ACS patients. BMC Health Serv Res. 2006 Oct 24;6:140. doi: 10.1186/1472-6963-6-140. PMID: 17062154; PMCID: PMC1630429
5. König S., Hohenstein S., Pellissier V., Leiner J., Hindricks G., Nachtigall I., Kuhlen R., Bollmann A. Changing trends of patient characteristics and treatment pathways during the COVID-19 pandemic: A cross-sectional analysis of 72,459 inpatient cases from the German Helios database. Front Public Health. 2022 Nov 7;10:1028062. doi: 10.3389/fpubh.2022.1028062. PMID: 36420010; PMCID: PMC9678052
6. Rennke S., Yuan P., Monash B., Blankenburg R., Chua I., Harman S., Sakai D.S., Khan A., Hilton J.F., Shieh L., Satterfield J. The SDM 3 Circle Model: A Literature Synthesis and Adaptation for Shared Decision Making in the Hospital. J Hosp Med. 2017 Dec;12(12):1001-1008. doi: 10.12788/jhm.2865. Epub 2017 Oct 18. PMID: 29073314; PMCID: PMC5709161
7. O’Connor A.M., Bennett C.L., Stacey D., Barry M., Col N.F., Eden K.B., Entwistle V.A., Fiset V., Holmes-Rovner M., Khangura S., Llewellyn-Thomas H., Rovner D. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD001431. doi: 10.1002/14651858.CD001431.pub2. Update in: Cochrane Database Syst Rev. 2011 Oct 05;(10):CD001431. doi: 10.1002/14651858.CD001431.pub3. PMID: 19588325
8. Kulikowski C.A. Beginnings of Artificial Intelligence in Medicine (AIM): Computational Artifice Assisting Scientific Inquiry and Clinical Art - with Reflections on Present AIM Challenges. Yearb Med Inform. 2019 Aug;28(1):249-256. doi: 10.1055/s0039-1677895. Epub 2019 Apr 25. PMID: 31022744; PMCID: PMC6697545
9. Haleem A., Javaid M., Singh R.P., Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021;2:100117. doi: 10.1016/j.sintl.2021.100117. Epub 2021 Jul 24. PMID: 34806053; PMCID: PMC8590973
10. van Staalduinen D.J., van den Bekerom P., Groeneveld S., Kidanemariam M., Stiggelbout A.M., van den Akker-van Marle M.E. The implementation of value-based healthcare: a scoping review. BMC Health Serv Res. 2022 Mar 1;22(1):270. doi: 10.1186/s12913-022-07489-2. PMID: 35227279; PMCID: PMC8886826
11. The Essential Deming: Leadership Principles from the Father of Quality W. Edwards Deming, 2013 McGraw-Hill

John J. Seidenfeld, MD, MSHA, FACP, is an Associate Professor, CASE, at the University of the Incarnate Word School of Osteopathic Medicine. He is a member of the Bexar County Medical Society and serves on the Publications Committee.

By William Trigoso, MD, FACE, and Tina Copple, DNP, FNP-BC, CDCES
In the race against Type 2 diabetes complications, insulin has been the main protagonist.
Glucagon, or its related peptides, were a good explanation of the physiopathology of the disease but never considered part of the armamentarium to fight this disease.
With a limited understanding of the complex physiopathology of type 2 diabetes, during the 1970s and 1980s, we developed medications to potentiate the action of insulin within the body. Our main goal was to improve glycemia, with the hope of preventing complications, and hoping to improve the quality of life of the person. During the 1990s, metformin revolutionized the management of type 2 diabetes. It was a game changer that gave us the confidence that made us believe that we could match the results of the Diabetes Control and Complications Trial (DCCT)1 published a few years earlier. This study proved beyond a doubt that in people with type 1 diabetes, aggressive glycemic control led to the prevention of complications.
To our dismay, after eight years, the results of the United Kingdom Prospective Diabetes Study (UKPDS) showed barely positive outcomes in the prevention of microvascular complications and a non-significant trend in the improvement in cardiovascular complications.2
Our common sense kept telling us that the task of softening the blow of type 2 diabetes was achievable. In the coming years, we became more aware of the mechanisms of insulin resistance and ways to overcome it. The development of thiazolidinediones finally gave us straightforward evidence that we could significantly improve cardiovascular outcomes.3
It was only when we turned or eyes away from insulin, looking into different domains, that we were able to re-discover the action of glucagon-like peptide hormones and unveil their secrets, like the incretin effect, the regulation of hepatic glucose production and its effects in feeding behaviors and its repercussions in weight reduction. A new era had begun, and we started to see significant improvements in glycemia and weight reduction and a decrease in insulin use among the sufferers who also demonstrated greater patient satisfaction.
The long-awaited favorable outcomes begin pouring in one by one. Liraglutide showed a significant amount of improvement in cardiovascular death.4 Tirzepatide demonstrated reduction in the risk of heart failure,5 significant resolution of MASH6 and significant reduction of the apnea hypopnea index (AHI) in persons with moderate-to-severe obstructive sleep apnea and obesity.7 Semaglutide decreased the primary composite outcome of cardiovascular death, nonfatal myocardial
infarction or nonfatal stroke in patients with type 2 diabetes and cardiovascular disease,8 showed significant resolution of NASH,9 and also reduced the risk of clinically important kidney outcomes and death from cardiovascular causes among patients with type 2 diabetes and chronic kidney disease.10
All those results were obtained in significantly less time than the eight years of the duration of the UKPDs trials. More is coming with the addition of other novel agents like the SGLT2 inhibitors.
The early medications that remain in use today, in many instances, are still helpful. They have their own set of side effects that, over the years, we have learned how to meander around to deliver care for patients. In many situations, they optimize the effect of the newer ones. Our newer agents also are not free of side effects. We need to remain observant of when to start them, when to stop them and who would be the better candidates for them. We also need to educate the patients about the side effects of these medications so they will not let them escalate into significant decompensation, which in some circumstances have created controversy, especially these days, where the media easily grabs a fact and brews it into a superlative distortion of reality.
Burping, nausea and vomiting are some of the most common side effects of GLP-1 and GLP1-GIP agonists. It can range from mild to severe and is often accompanied by a persistent sensation of abdominal discomfort and bloating. These drugs have demonstrated kidney benefits in patients with type 2 diabetes, but in rare cases, kidney damage has also happened when using them, especially if nausea, vomiting or diarrhea leads to severe dehydration. To minimize chances of dehydration due to gastrointestinal causes, it is recommended to begin these agents at a low dose and gently adjust them to meet the patient’s needs. Patients are more likely to have nausea when they first start treatment or after increases in the dose. For most people, these side effects resolve uneventfully. Rapid escalation of the dose may lead to rapid escalation of symptoms and side effects. Constipation is less common than diarrhea and nausea, but it can still occur as a side effect of these medications. Adequate hydration ameliorates this in a significant manner. The presence of severe epigastric pain or severe abdominal discomfort, although infrequent, should raise the alert for the presence of pancreatitis. Patients should be made aware of this to seek immediate consultation with a physician.
Blurry vision or visual defects should also be communicated to the physician since progression of diabetic retinopathy or retinal vein occlusion, although infrequently, has been reported as a potential side effect.
Although only seen in rats, medullary-thyroid carcinoma has been added to the label warning and potentially may happen in association with multiple endocrine neoplasia syndrome type 2. In any case, a good examination of the thyroid is always warranted in every patient. These days, the big challenge is to make these medications available to the population at large. The main barrier is the prohibitive cost and economic toxicity of these medications. Large segments of the population, especially in the lower economic strata, are at substantial risk of developing metabolic diseases, which lead to becoming type 2 diabetics and suffering complications. This is even more pronounced among minorities with limited access to insurance or to third-party payers willing to cover this category of medications.
References:
1. Diabetes Control and Complications Trial (DCCT): Results of Feasibility Study. The DCCT Research Group. Diabetes Care 1 January 1987; 10 (1): 1–19
2. American Diabetes Association; Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care 1 January 2003; 26 (suppl_1): s28–s32
3. Pioglitazone and cardiovascular outcomes in patients with insulin resistance, pre-diabetes and type 2 diabetes: a systematic review and meta-analysis. Liao et al, bmjopen-2016-013927
4. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes, Marso et al, N Engl J Med 2016;375:311-322
5. A Study of Tirzepatide (LY3298176) in Participants With Heart Failure With Preserved Ejection Fraction (HFpEF) and Obesity: The SUMMIT Trial, ClinicalTrials.gov ID NCT04847557 2024-07-22 )
6. Tirzepatide for Metabolic Dysfunction–Associated Steatohepatitis with Liver Fibrosis Loomba et al. 2024 N Engl J Med 2024;391:299-310
7. Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity, Malhotra et al, 2024N Engl J Med 2024;391:1193-120
8. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes, Marso et al, N Engl J Med 2016;375:1834-1844
9. A Placebo-Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis, Newsome et al, N Engl J Med 2021;384:1113-1124
10. Effects of Semaglutide on Chronic Kidney Disease in Patients with Type 2 Diabetes, Perkovic et al, N Engl J Med 2024;391:109-121)

William Fernando Trigoso, MD, FACE, is a physician and surgeon who graduated from the Universidad Peruana Cayetano Heredia in Lima, Peru, trained in Internal Medicine at the Michael Reese Hospital in Chicago, IL., and earned his fellowship in Endocrinology and Metabolism at the University of Wisconsin Hospital. Dr. Trigoso is board certified in Internal Medicine, Endocrinology, Diabetes and Metabolism, Clinical Lipidology, and Clinical Bone Densitometry and Neck Ultrasound. He is a fellow of the American College of Endocrinology and member of the American Association of Clinical Endocrinologists, American Diabetes Association, National Lipid Association and International Society for Clinical Bone Densitometry. Dr Trigoso is the Vice-President of Diabetes and Glandular Disease Clinic in San Antonio, a 100% group member of BCMS and TMA.

Tina Copple, DNP, FNP-BC, CDCES, received her Doctorate of Nursing Practice at The University of Alabama at Tuscaloosa and Master of Science in Nursing, Family Nurse Practitioner at The University of Texas Health Science Center. She is a Certified Diabetes Care and Education Specialist, Certified Diabetes Educator Clinical Lipid Specialist and Certified Clinical Densitometrist (CCD).

By Ronald Rodriguez, MD, PhD, with Parin Chanana
U.S. healthcare spending is estimated to exceed $6 trillion by 2027,1 which translates to an average cost of more than $19,000 per person each year. With the advent of generative AI, the healthcare landscape is rapidly transforming, promising to revolutionize patient care, streamline operations, and potentially reduce costs.2,3 However, the financial implications of AI in healthcare are complex and multifaceted, presenting both opportunities for savings and potential challenges.
Tech giants and startups alike are pouring billions into healthcare AI. While many predict substantial healthcare savings from the use of AI, a McKinsey report identified many obstacles and real-world problems in the actual implementation of AI, which have not permitted realization of those savings.4 Microsoft invested $19.7 billion in OpenAI, the creators of ChatGPT, which has applications in medical chatbots and patient education. Google is pioneering AI-driven drug discovery through its subsidiary, DeepMind. Amazon acquired PillPack and launched Amazon Care, leveraging AI for prescription fulfillment and telehealth services. These investments are driven by the belief that AI can address some of healthcare’s most pressing challenges. AI offers several avenues for cost reduction in healthcare. It can automate administrative tasks like claims processing, prior authori-
zation and scheduling, freeing up staff and reducing administrative overhead. AI algorithms can analyze medical images and patient data to detect diseases like cancer and heart disease at earlier stages, when treatment is often less expensive. AI can help tailor treatments to individual patients based on their genetic makeup and lifestyle factors, potentially leading to better outcomes and lower long-term costs.
While AI offers significant potential for cost savings, there are also concerns that it could drive up healthcare expenditures. Developing and implementing AI systems can be expensive, requiring significant upfront investments in software, hardware and training. AI algorithms may identify patients who require additional testing or treatment, potentially leading to increased utilization of healthcare resources. Furthermore, ethical concerns about how insurance companies might use AI to identify at-risk populations and charge higher premiums or deny coverage based on predicted future health problems could lead to increased costs for patients and exacerbate existing health disparities.
The FDA considers AI software used in healthcare to be a medical device, subject to regulatory oversight and approval.5 This process can be costly and time-consuming, adding to the overall expense of implementing AI in healthcare. Currently, these costs are typically borne
by the developers of AI software, but they are ultimately passed on to healthcare providers and patients through software licensing fees and increased costs for medical services.
The Dragon Ambient eXperience (DAX) is an AI-powered tool developed by software giant Nuance, that automates clinical documentation. It uses voice recognition and natural language processing to transcribe patient encounters, summarize key findings, and generate portions of clinical notes. DAX is being adopted by practices to reduce administrative burden, improve documentation accuracy, and enhance patient interaction. However, the cost of DAX and similar AI tools is substantial though it can vary depending on the final vendor and the specific features included. These costs are typically incurred on a subscription basis or per-user basis, adding to the ongoing expenses of healthcare practices.
The costs of AI in healthcare are incurred incrementally. Each new AI tool or application adds to the overall expense of healthcare delivery. While individual tools may offer cost savings in specific areas, the cumulative effect of adopting multiple AI solutions could lead to increased healthcare costs in the short and long run. The profit motive behind developing AI tools means that healthcare providers are not the only entities looking to benefit from these technologies. Third-party payors, electronic medical record companies, hospitals, healthcare systems, nursing home administrators, home health organizations, durable medical device developers and commercial sales organizations like Amazon are all seeking ways to derive additional profit through the use of AI. Undoubtedly, they will find methods to extract more revenue with these tools. However, the expenses associated with these profit-driven initiatives are likely to be passed on to patients, increasing the overall cost of healthcare.
The future of healthcare has never been so exciting, as our current technologies are advancing at a rate never before seen in human history. The advent of AI has precipitated much of these rapid advances. AI has the potential to revolutionize healthcare and improve patient outcomes, but its impact on healthcare costs is complex and multifaceted. While there are opportunities for cost savings, there are also potential challenges and ethical concerns that must be addressed. As AI continues to evolve and become more integrated into healthcare, it will be crucial to carefully evaluate its costs and benefits to ensure that it is used in a way that is transparent, safe, effective and equitable.
References:
1. Staff M. U.S. Health Expenditure Expected to Reach $6.07 Trillion by 2027. Managed Healthcare Executive 2024; Available from: https://www.managedhealthcareexecutive.com/view/u-shealth-expenditure-expected-to-reach-6-07-trillion-by-2027
2. Kasyanau A., Council Post: Balancing The Cost Of AI In Healthcare: Future Savings Vs. Current Spending, in Forbes. 2024
3. Khanna N.N., et al., Economics of Artificial Intelligence in Healthcare: Diagnosis vs. Treatment. Healthcare (Basel), 2022. 10(12)
4. Company M. Reimagining healthcare industry service operations in the age of AI. Healthcare, Sept 19, 2024
5. FDA, Artificial intelligence and machine learning (AI/ML)-enabled medical devicesAI MedTech Insights: Empowering Decisions with AI in Healthcare & Wellness. 2021

Ronald Rodriguez, MD, PhD, is an Ashbel Smith Professor of Urologic Sciences, Professor of Medical Education and Urology, Assistant Dean for Undergraduate Medical Education and Program Director, MS in AI at UT Health San Antonio. Dr. Rodriguez is an experienced urologic oncologist, research scientist and medical educator. His research has varied substantially over time, and he has made significant contributions to the development of oncolytic adenoviral gene therapy, immunotherapy, targeted ablative therapy and surgical management of advanced kidney cancers. He also help establish the first Dual Degree program, MD/MS in AI, in the country and is an expert in medical education focusing on the use of AI. Dr. Rodriguez is a member of the Bexar County Medical Society.

Parin Chanana is a high school sophomore and a mentee of Dr. Ronald Rodriguez, with a strong interest in health economics. He is passionate about research, is working on publishing a finance book, and recently earned first place nationally in Business Professionals of America’s Health Insurance and Medical Billing competition. Parin plans to pursue a career in health economics to drive innovation in the healthcare field.


By Philip Makedon, MEd, MLS(ASCP); Cooper Allenbrand, BS, BA; and Ramaswamy Sharma, MS, PhD
You have certainly heard of a friend or family member taking fish oil supplements for their potential health benefits, and you may be wondering if you should take them, too. Do they benefit your body? How much should you take? Is there a limit beyond which it is not safe? How can you avoid that fishy smell when you burp?
Fish oil has been considered to be beneficial because it is rich in omega3 fatty acids such as alpha linoleic acid (ALA), docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), essential nutrients our bodies cannot produce.1 While ALA is often consumed as part of the Standard American Diet and can be converted to DHA and EPA, direct consumption of the more beneficial and potent DHA and EPA is recommended.2 Omega-3s are helpful in lowering inflammation in our bodies. Inflammation is a fire within our bodies caused by white blood cells to protect us from foreign material that enters our bodies.3 Normally, the fire is extinguished as soon as the foreign entity is disposed of and the body heals; however, in some of us, inflammation occurs continuously, damaging our own cells. Long-term inflammation is implicated in various health conditions including heart disease, depression, multiple sclerosis, several types of cancer, rheumatoid arthritis, psoriasis, migraine headaches, lupus, Crohn’s disease, ulcerative colitis and many others.4-6 Importantly, inflammation increases with aging. Nutrition researcher and omega-3 expert, Dr. William Harris, uses the following analogy to describe omega-3’s anti-inflammatory effects: “Fish oil is an oil, and you think about oil in your car and having enough oil in the engine to lubricate all the cylinders as they go up and down.” Omega-3s reduce the “friction” (inflammation) that can occur in our “engines,” and thereby improve our quality of life. Dietary supplementation with omega-3s has been shown to improve:7
• Brain Development and Function: Omega-3s are involved in the development and maintenance of the structure and function of nerve cells. Several studies have documented its benefits in enhancing cognition, reducing depression, aggression, stress, mood disorders, anorexia and other psychiatric disorders, preventing dementia, and in reducing the frequency of seizures in intractable epilepsy. Omega-3s consumed during pregnancy may also help in later cognitive development of children.
• Cardiovascular Health: Omega-3s can help regulate fat metabolism and maintain healthy cholesterol levels, lower triglyceride levels, and slow blood clot formation, thereby decreasing the risk for high blood pressure and heart attacks.
• Liver Health: Omega-3s lower fat synthesis in the liver, change metabolism such that triglyceride production is reduced, and enhance liver function in patients with non-alcoholic fatty liver disease (NAFLD), as shown by a decrease in several stress-related markers such as ALT, AST and GGT. Conversely, poor liver function has been associated with a decreased level of omega-3s.
• Lung Health: Omega-3s, especially DHA, has been shown to reduce inflammation in the lung, which is associated with chronic obstructive pulmonary disease (COPD), and improve lung function.
• Eye Health: Low levels of omega-3s as compared to omega-6 fatty acids are associated with an increased risk of age-related macular degeneration. High levels of omega-3s, especially EPA, are associated with lower risk for both dry and wet age-related macular degeneration.
• Cartilage, Bone and Muscle Health: Omega-3s reduce osteoarthritis and rheumatoid arthritis characterized by joint swelling, pain, morning stiffness and inflammation. Omega-3s also help improve muscle strength, decrease pain, and enhance recovery from delayed onset muscle soreness after high intensity interval training exercises in overweight/obese people.8-9 Foods that are rich in omega-3s include “SMASH,” an acronym for cold-water fish (Salmon, Mackerel, Anchovies, Sardines and Herring), walnuts, flaxseeds, microalgae oil and bioengineered plants. Lower fat content fish such as shrimp, lobster, tilapia, cod, perch, bass and many lake fish contain low amounts of omega-3 fatty acids. Below is a quick reference table:10-12
Obtaining adequate levels of omega-3s through diet alone can be challenging. Hence, supplementation with fish oil, krill oil or algae oil are great options. However, most supplements contain less than 1g of EPA and DHA, which vary from batch-to-batch, and may contain high levels of unhealthy saturated fatty acids as well as oxidized lipid products. Therefore, it would be best to use omega-3s prescribed by your physician as they are usually purest. Some studies have also shown that a higher concentration of EPA is more beneficial for cardiac health.13-14
There are varying guidelines for the recommended dietary intakes. The 2015-2020 Dietary Guidelines for Americans recommends eight ounces of varied seafood weekly, providing an average of 250mg of EPA and DHA daily.5 The American Academy of Nutrition and Dietetics suggests consuming two or more servings of fatty fish per week to provide at least 500mg of EPA and DHA per day.15 The American Heart Association recommends a consumption of “one to two seafood meals per week to reduce the risk of congestive heart failure, coronary heart disease, ischemic stroke, and sudden cardiac death” and up to 4g daily of omega-3s to reduce triglyceride levels.16 When used daily and as recommended, high-quality omega-3 containing (i.e. fish oil) supplements that contain no more than 5g of EPA and DHA are considered safe by the FDA.17 Some common side effects are typically mild and can include an unpleasant taste, “fishy” breath, nausea and gastrointestinal discomfort. Some of these side effects can be mitigated when taking fish oil appropriately, most often by taking the fish oil supplement during a meal. Importantly, fish oil also has the potential to interact with anticoagulant medications; therefore, it is recommended to consult your doctor before starting fish oil supplements.

Philip Makedon, MEd, MLS(ASCP), is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2026. He is passionate about healthy living and has a special interest in hematopathology and transfusion medicine.

Cooper Allenbrand, BS, BA, is a dedicated medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2026. Committed to health optimization and equity, he is particularly interested in physical medicine & rehabilitation and family medicine, aiming to make a significant impact in these fields.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life.
References:
1. Sears B. What are the real differences between EPA and DHA? Psychology Today. 2012, April 1. Retrieved from: https://www. hsph.harvard.edu/nutritionsource/omega-3-fats-and-seafood/
2. The Nutrition Source. Omega-3 Fatty Acids: An Essential Contribution. Harvard T.H. Chan School of Public Health. 2022. Retrieved from: https://nutritionsource.hsph.harvard.edu/whatshould-you-eat/fats-and-cholesterol/types-of-fat/omega-3-fats/
3. Tomlinson G.M., Bhattacharya A., and Sharma R. Inflammation: Dousing the fire within. San Antonio Medicine, 2024, July, 77
(7): 30. Retrieved from: http://www.bcms.org/SAM/2024/ SAMJul2024/mobile/index.html
4. Sokoła-Wysoczańska E., Wysoczański T., Wagner J., Czyż K., Bodkowski R., Lochyński S., Patkowska-Sokoła B. Polyunsaturated Fatty Acids and Their Potential Therapeutic Role in Cardiovascular System Disorders-A Review. Nutrients. 2018 Oct 21;10(10):1561. doi: 10.3390/nu10101561
5. Office of Dietary Supplements. Omega-3 Fatty Acids. National Institutes of Health. 2022. Retrieved from: https://ods. od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/#h2
6. Rimm E.B., Appel L.J., Chiuve S.E., Djoussé L., Engler M.B., Kris-Etherton P.M., Mozaffarian D., Siscovick D.S., Lichtenstein A.H. Seafood long-chain n-3 polyunsaturated fatty acids and cardiovascular disease: a science advisory from the American Heart Association. Circulation. 2018 Jul 3;138(1):e35-47
7. Natural Standard Research Collaboration. Omega-3 fatty acids, fish oil, alpha-linolenic acid. Medline Plus. 2005 Aug. Retrieved from http://web.archive.org/web/20060503222604/http:// www.nlm.nih.gov/medlineplus/print/druginfo/natural/patientfishoil.html
8. Makaje N., Ruangthai R., Sae-Tan S. Effects of Omega-3 Supplementation on the Delayed Onset Muscle Soreness after Cycling High Intensity Interval Training in Overweight or Obese Males. J Sports Sci Med. 2024 Jun 1;23(2):317-325. doi: 10.52082/ jssm.2024.317
9. Shawl M., Geetha T., Burnett D., Babu J.R. Omega-3 Supplementation and Its Effects on Osteoarthritis. Nutrients. 2024 May 28;16(11):1650. doi: 10.3390/nu16111650
10. U.S. Department of Agriculture, Agricultural Research Service. 2016. Retrieved from: https://ods.od.nih.gov/pubs/usdandb/ ALA-Food.pdf
11. U.S. Department of Agriculture, Agricultural Research Service. 2016. Retrieved from: https://ods.od.nih.gov/pubs/usdandb/ DHA-Food.pdf
12. U.S. Department of Agriculture, Agricultural Research Service. 2016. Retrieved from: https://ods.od.nih.gov/pubs/usdandb/ EPA-Food.pdf
13. Brinton E.A., Mason R.P. Prescription omega-3 fatty acid products containing highly purified eicosapentaenoic acid (EPA). Lipids Health Dis. 2017 Jan 31;16(1):23. doi: 10.1186/s12944017-0415-8
14. Sherratt S.C.R., Mason R.P., Libby P., Steg P.G., Bhatt D.L. Do patients benefit from omega-3 fatty acids? Cardiovasc Res. 2024 Feb 17;119(18):2884-2901. doi: 10.1093/cvr/cvad188
15. Williamson L. Are you getting enough omega-3 fatty acids? American Heart Association News on Heart.org. 2023 Jun 30. Retrieved from: https://www.heart.org/en/news/2023/06/30/ are-you-getting-enough-omega-3-fatty-acids
16. Klemm, S. What are omega-3 fatty acids? Academy of Nutrition and Dietetics. 2024, May 17. Retrieved from: https://www. eatright.org/health/essential-nutrients/fats/what-are-omega-3fatty-acids
17. U.S. Food and Drug Administration. Advice about eating fish. 2024, March 3. Retrieved from: https://www.fda.gov/food/consumers/advice-about-eating-fish

By Mercedes Ingram, PhD, LPC
Suicide is a leading cause of death in the United States, with a significant rise among young people in recent years. In 2021, it became the second leading cause of death for individuals aged 10-24. To combat this issue, University Health has proposed two innovative programs and received funding to connect individuals with resources and provide care for those at risk of suicidal ideation.
CoSPLAY
The latest initiative, CoSPLAY (Comprehensive Suicide Prevention Blueprint for Adults and Youth), was awarded a $3.6 million, four-year federal grant in late 2023, funded by the Centers for Disease Control and Prevention and the National Center for Injury Prevention and Control.
While CoSPLAY is a new program, it reflects University Health’s ongoing commitment to suicide prevention. It builds on the success of the Zero Suicide initiative, launched in July 2019 with support from the Substance Abuse and Mental Health Services Administration (SAMHSA).
Alyssa Martinez, a licensed clinical social worker with University Health’s Community Initiatives and Population Health team, has seen how the programs can help people. “The impact of both Zero Suicide and CoSPLAY have been truly life-saving,” Martinez said. “When we educate somebody about the crisis lines, help them create a safety plan, or even just be an open ear willing to listen to their story, we help them find hope to continue forward and live another day.”
University Health began implementing the Zero Suicide program in July 2019 as a comprehensive suicide prevention and intervention initiative. The program aims to reduce suicide attempts and fatalities, particularly among adults, veterans and individuals with serious mental illness. The Zero Suicide team has also worked to raise awareness about the impact of suicide in Bexar County and establish referral processes for individuals experiencing suicidal thoughts. Additionally, the program focuses on improving care and outcomes for patients at risk of suicide. Crucially, the program’s success in fostering a leadership-driven, safety-oriented culture within University Health ensures its sustainability and long-term effectiveness. Although funding from our federal partner, SAMHSA, ended on September 30, 2022, we continue to support the program.
In 2023, nearly 300,000 primary care appointments took place in clinics implementing Zero Suicide. During these visits, the Patient Health Questionnaire (PHQ-3), which screens for symptoms of depression, was administered in 201,210 appointments. This frequency of screening has accounted for 69 percent of all appointments. The PHQ-3 successfully identified suicide risk in patients, leading to further evaluation with the more detailed PHQ-9. This helped clinicians identify, diagnose, monitor and measure the severity of depression in 552 cases, representing 0.3 percent of those screened. So far in 2024, PHQ screenings have occurred for nearly 70 percent of appointments, with 0.3 percent of patients screened showing some degree of suicide risk. The top three types of mental health referrals in 2023 and 2024 were to 1) neurology, 2) psychiatry and 3) behavioral health. In total, there were 17,216 referrals made for these specialties in 2023 and 13,781 in 2024 to date. Specifically for behavioral health, there were 5,103 referrals in 2023 and 3,179 in 2024 thus far. Our five social workers dedicated to the Zero Suicide initiative have provided care to at least 498 patients since 2023. Two years after receiving funding, Zero Suicide has established and reinforced a workflow that effectively screens, detects and refers patients at risk for suicide, saving lives — one patient at a time.
While Zero Suicide has helped thousands of people screened through University Health care sites, CoSPLAY is expanding to
involve multiple partners in higher education and organizations serving teens and young adults, including the LGBTQ+ population that is at higher risk of suicidality. CoSPLAY aims to strengthen access and delivery of suicide care interventions, create protective environments, and identify and support persons at risk for suicide.
CoSPLAY partners include Our Lady of the Lake University, University of Texas at San Antonio, San Antonio College and organizations like Alamo Area Teen Suicide Prevention Coalition and Fiesta Youth.
The CoSPLAY program is designed to establish multiple pathways to support young people at risk. University Health is starting with its own clinics and will then expand to collaborate with community partners, training staff to recognize warning signs and connect individuals to resources and care. We are implementing healthcare-based interventions where patients will be screened for suicide risk. Those who screen positive will be connected to social workers trained in reducing access to lethal means. Additionally, the program will involve training teachers to equip them with coping and problem-solving techniques, enabling them to better identify and assist individuals at high risk for suicidal ideations. Just like Zero Suicide, the CoSPLAY team works to identify and engage patients at risk for suicide by increasing screening, comprehensive assessment and safety planning, and ensuring the continuity of care for youth.
In the past year, University Health has established referral pathways and trained staff to effectively support youth with, or at risk for, suicidal ideation. This year, we are shifting our focus to fostering interagency collaboration.
Program staff have an important goal: to de-stigmatize mental health issues and achieve a 10 percent reduction in suicides and suicide attempts. They plan to accomplish this through healthcare provider training, expanding access to mental health treatment and suicide prevention resources, and teaching coping and problem-solving skills through social-emotional learning programs.
CoSPLAY is funded by the Centers for Disease Control and Prevention and National Center for Injury Prevention and Control.
“Deaths due to suicide and homicide, often referred to collectively as violent deaths, have been a leading cause of premature death to people aged 10–24 in the United States. A previous version of this report with data through 2017 showed that suicide and homicide rates for people aged 10–24 were trending upward … The suicide rate among people aged 10–24 remained stable from 2001 through 2007 and then increased 62 percent from 2007 through 2021 (from 6.8 deaths per 100,000 to 11.0).” www.cdc.gov/nchs/data/databriefs/ db471.pdf

Mercedes Ingram, PhD, LPC, is the Senior Director of the Mental Wellness Initiative, Community Initiatives and Population Health at University Health.

By Kreny Savaliya, Hunter Buescher and Ramaswamy Sharma, MS, PhD
Sir Alfred Nobel, a Swedish chemist credited with inventing explosives such as dynamite, blasting gelatin and ballistite, bequeathed his vast estate for recognizing distinguished, paradigm-shifting achievements that benefit humans in the fields of physics, chemistry, physiology or medicine, economic sciences, literature and peace. These awards, known as Nobel Prizes, come with a diploma, a medal and a cash prize of 11 million Swedish kronor, and are presented by the King of Sweden. Victor Ambros, a professor of molecular medicine at the University of Massachusetts Chan Medical School, and Gary Ruvkun, a professor of genetics at Harvard Medical School, were selected this year to receive the Nobel Prize in Physiology and Medicine for their discovery of a new type of RNA that plays a major role in regulating gene expression. Their findings have led to the discovery of a thousand other microRNAs and a better understanding of the tight genetic control exerted in our cells.
Our bodies consist of trillions of cells with the same genetic makeup; yet, our neurons behave and function differently from our muscle cells. This is due to a process known as specialization, which involves gene regulation. Genes are made up of specific sequences of deoxyribonucleic acid (DNA); it was earlier thought that each gene is transcribed to form a specific sequence of ribonucleic acid (RNA), which, in turn, is translated to form a particular protein. Since all the cells in our body contain the same 22,300 protein-coding genes, only those genes that are relevant towards its formation and function will be active in a given cell type; the remaining genes are “silenced.” Thus, the genes that are active in a neuron will be different from those in a muscle cell, thereby making it function differently from a muscle cell. Prior to the seminal discovery of Ambros and Ruvkun, it was thought that certain proteins, called transcription factors, attach to DNA and either promote or inhibit formation of proteins, thereby deciding which genes were active and were translated to synthesize proteins.
During the 1980’s, Ambros and Ruvkun worked together as postdoctoral fellows in the laboratory of Robert Horvitz, who received the Nobel Prize in 2002 for his contribution towards the elucidation of programmed cell death during development. Interestingly, Ambros had previously been mentored by David Baltimore, another Nobel laureate, for his graduate research at the Massachusetts Institute of
Technology. The Horvitz laboratory used Ceanorhabditis elegans, a roundworm that is just a mm in length, as a model to determine how cells develop. Horvitz, John Sulston and Martin Chalfie (all Nobel laureates) had earlier characterized many heterochronic mutant C. elegans worms, so-called because their temporal pattern of cell development was disturbed by those mutations, when they worked in Sydney Brenner’s laboratory (also a Nobel laureate); one such heterochronic mutant was lin-4 (cell lineage abnormal-4) that was unable to lay eggs and displayed defects in cell lineage. Ambros and Ruvkun further analyzed these heterochronic mutants in Horvitz’s laboratory. Ambros discovered three more genes involved in heterochronicity – lin-14, lin-28 and lin-29. Both scientists continued working on these genes after they set up their own laboratories.
Ambros’s laboratory at Harvard University discovered that lin-4 inhibited lin-14 expression. Lin-14 expression is required for normal early-stage development but its reduced expression is associated with normal late-stage development. He cloned lin-4 and found that it generated an incredibly short RNA molecule that did not code for a protein. Meanwhile, Ruvkun’s laboratory at Massachusetts General Hospital determined that the lin-14 gene was transcribed to generate mRNA at the later stages of development but did not make protein, i.e., lin-14 inhibition was post-transcriptional. They also discovered a sequence in the 3’Untranslated Region (3’ UTR) of lin-14 RNA that was complementary to lin-4 RNA. Together, Ambros and Ruvkun established that the short RNA transcribed by the lin-4 gene bound to the lin-14 RNA and prevented its translation to protein. This was a groundbreaking discovery, as Ambros and Ruvkun were the first to demonstrate that short RNAs (called microRNA or miRNA) could regulate gene expression after DNA was transcribed to RNA. Their findings were published in 1993 in back-to-back articles in the journal Cell. However, it took seven more years and the identification of another microRNA, let7, for their discovery to be accepted by the scientific community. Many more microRNAs have been discovered since.
We now know that miRNAs are non-coding RNAs, typically around 22 nucleotides long, that mostly interact with the 3’ UTR of target mRNAs, resulting in their degradation and thereby, translational repression. Recent discoveries indicate that miRNAs not only reg -
ulate transcription but can also activate translation. We have a deeper understanding of the molecular mechanisms underlying this process. Given their vital roles in cell development and function, it is not surprising that they are evolutionarily conserved across a wide range of species. For instance, let-7, which is essential for larval development in C. elegans, is also found in humans.
Dysregulation of miRNAs is associated with many pathologies. Mutations in miRNA-coding genes have been associated with conditions such as congenital hearing loss and skeletal abnormalities. Therefore, miRNAs are being scrutinized as targets for drug development as well as therapeutic agents themselves. For example, inhibitors targeting miR-92a and miR-122 are under investigation for their potential benefits in treating cardiovascular diseases and hepatitis C, respectively. Additionally, several miRNA candidates are currently being tested for targeting cancer in clinical trials. Their role as biomarkers is particularly compelling as they show remarkable promise in identifying and tracking pathologies such as cancer, cardiovascular diseases and neurological disorders. Because miRNAs can be detected in liquid biopsies such as blood and urine, they represent a minimally invasive option for diagnosis, paving the way for easier patient monitoring.
The landscape of RNA-based medicine continues to evolve with the identification of other non-coding RNA classes, including long non-coding RNAs (IncRNAs), circular RNAs (circRNAs), and small interfering RNAs (siRNAs). A notable milestone in this domain was the FDA’s approval of Patisiran in 2018, the first siRNA-based drug for treating hereditary transthyretin-mediated amyloidosis. While challenges such as off-target effects and the development of efficient delivery systems remain critical hurdles, the potential for RNAbased diagnostics and treatments appears increasingly promising. No wonder the Nobel committee is recognizing the pivotal discovery of miRNA in medicine that has heralded a transformative shift in how we approach healthcare.
References:
1. “Alfred Nobel’s Will - Nobel Peace Prize.” Www.nobelpeaceprize. org, 30 Aug. 2021, www.nobelpeaceprize.org/nobel-peace-prize/ history/alfred-nobel-s-will
2. Almeida M.I., Reis R.M., Calin G.A. MicroRNA history: discovery, recent applications, and next frontiers. Mutat Res. 2011 Dec 1;717(1-2):1-8. doi: 10.1016/j.mrfmmm.2011.03.009
3. Ambros V., Horvitz H.R. The lin-14 locus of Caenorhabditis elegans controls the time of expression of specific postembryonic
developmental events. Genes Dev. 1987 Jun;1(4):398-414. doi: 10.1101/gad.1.4.398
4. Bhaskaran M., Mohan M. MicroRNAs: history, biogenesis, and their evolving role in animal development and disease. Vet Pathol. 2014 Jul;51(4):759-74. doi: 10.1177/0300985813502820
5. Lee R.C., Feinbaum R.L., Ambros V. “Nomination and Selection of Medicine Laureates.” NobelPrize.org, 2019. www.nobelprize. org/nomination/medicine/
6. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993 Dec 3;75(5):84354. doi: 10.1016/0092-8674(93)90529-y
7. O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front Endocrinol (Lausanne). 2018 Aug 3;9:402. doi: 10.3389/ fendo.2018.00402. https://doi.org/10.3389/fendo.2018.00402
8. “The Nobel Prize in Physiology or Medicine 2024.” NobelPrize. org, 7 Oct. 2024. www.nobelprize.org/prizes/medicine/2024/ press-release/
9. Wang D. and Farhana A. “Biochemistry, RNA Structure.” PubMed, StatPearls Publishing, 2020, www.ncbi.nlm.nih.gov/books/ NBK558999/
10. Wightman B., Ha I., Ruvkun G. Posttranscriptional regulation of the heterochronic gene lin-14 by lin-4 mediates temporal pattern formation in C. elegans. Cell. 1993 Dec 3;75(5):855-62. doi: 10.1016/0092-8674(93)90530-4

Kreny Savaliya is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. She is passionate about pursuing a career in pediatrics to positively impact children’s health. She is also dedicated to participating in mission trips to provide medical care to underserved communities and broaden her understanding of global health issues.

Hunter Buescher is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. His interests include preventative medicine and community health.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma serves on the BCMS Publications Committee.

By Nora Vasquez, MD, CHPC
As a Certified High-Performance Coach for Physicians, APPs and Executives, one of the most important exercises I coach my clients on is powerful goal-setting. It is the foundation to creating a life you love — in and outside of medicine. As the end of the year approaches, this is the perfect time to reflect on what you’ve achieved and recalibrate for the new year ahead.
High-performance goal setting isn’t about rigid targets; it’s about setting intentional goals that align with your values, creating space for exciting new possibilities, and empowering you to reach your highest potential! In this article, I’ll guide you through a three-step process to reflect, reassess, and reset your goals. To take this process even further, you are invited to join us on Tuesday, December 17, 2024 at 7:00 p.m. CST for an exclusive Goal-Setting Masterclass where we will dive deeper into each step, helping you begin the new year with more growth, clarity and purpose! Register for the webinar here: www.renewyourmindmd.com/renewed
Step 1. Reflect on Your Wins and Lessons Learned
Reflection is a powerful step in high-performance goal setting. Taking time to look back on the year helps you acknowledge your progress and identify lessons that can guide you forward. A balanced reflection allows you to appreciate achievements and acknowledge challenges, creating a well-rounded view of your journey.
Imagine, for example, Dr. Maria, who is a busy physician who set a goal to publish research on patient engagement by year-end. As the year progressed, she found her energy shifting toward mentoring her team and supporting new initiatives. While she hadn’t reached her original goal, she acknowledged her success in gathering valuable data and helping her team thrive.
3 Key Questions to Guide Your Reflection:
1. What were my significant achievements this year?
• Write down both big wins and smaller accomplishments. Like Dr. Maria, you might realize that valuable work happened even if you didn’t achieve every goal.
2. What challenges did I face, and what did I learn from them?
• Identify areas where you grew from difficulties. For example, Dr. Maria’s experience taught her how to balance team support with her own projects.
3. What motivated me and brought me joy?
• Reflecting on what energized you can clarify which goals align most with your core values and bring a sense of purpose.
Taking time to reflect on these questions helps you understand the core motivations behind your actions. This clarity is essential for creating goals that feel meaningful and aligned with your evolving vision of success.
Step 2. Reassess and Let Go of What No Longer Serves You
One of the keys to high-performance goal setting is knowing when to let go. Sometimes, the best way to make room for new opportunities is to release goals that no longer resonate with who you are or where you’re heading. High achievers often find themselves holding on to old goals out of habit, even when those goals feel more like burdens than motivators.
Dr. Maria, for example, realized that her original goal of publishing her research felt like pressure. Her true passion had shifted toward mentorship and practical, hands-on patient care. Rather than pushing through, she decided to redirect her efforts to create a workshop series on patient engagement strategies, which aligned better with her current values and priorities.
3 Questions to Help You Reassess Your Goals:
1. Which goals no longer resonate?
• If a goal feels draining rather than inspiring, it might be time to reassess. Like Dr. Maria, you may find that priorities have shifted over the year.
2. What am I holding onto out of habit and old expectations?
• Goals often lose their relevance over time. Be honest about whether you’re pursuing certain targets for continuity’s sake or genuine interest.
3. Where can I redirect my energy?
• Letting go of outdated goals allows you to refocus on areas that feel more authentic and aligned with who you are now.
Reassessing is about refining your path forward. By releasing goals that no longer serve you, you create room for new possibilities that better match your vision and bring a renewed sense of excitement for the year ahead.
Now that you’ve reflected on your wins and refined your priorities, it’s time to set intentional, high-performance goals for the new year. Unlike a long list of resolutions, these are goals that align with your core values and inspire sustainable growth. Dr. Maria’s decision to pivot her research project into a workshop series exemplifies this approach — she set a goal that aligned with her passion for mentorship, creating a purpose-driven plan for the year.
1. Prioritize with Clarity. Choose one to three impactful goals that will make the most meaningful difference in your life.
• For example, Dr. Maria identified mentorship as her primary area of impact, adjusting her goals accordingly.
2. Break Each Goal into Actionable Steps
• Define specific steps to create consistent progress. For Dr. Maria, this meant outlining “workshop development milestones” for each quarter.
3. Set a Timeline with Checkpoints
• Create a roadmap that includes quarterly check-ins to stay on track. These check-ins allow for adjustments and help you remain accountable to your goals.
1. Is this goal in alignment with my values?
• Goals that reflect your core values are more fulfilling and motivating.
2. How will I measure my progress?
• Clearly define success, whether it’s a milestone, a habit or a specific outcome.
3. What support or resources do I need?
• Identify the resources and support you’ll need to reach each goal. Dr. Maria, for instance, leaned on her team to help develop workshop content.
By setting purposeful goals that align with your values and breaking them down into actionable steps, you’re creating a plan that not only keeps you motivated but also brings a sense of fulfillment as you make progress.
When to Reassess Throughout the Year
High-performance goal setting is dynamic, not static. Schedule quarterly check-ins to review your progress and adjust as needed.
Life is unpredictable, and goals may need to evolve with your circumstances.
3 Signs It’s Time to Reassess:
1. You’re consistently avoiding tasks related to the goal.
2. External changes impact your priorities or resources.
3. The goal feels exhausting rather than inspiring.
Regularly reassessing allows you to stay agile, letting you course-correct in a way that keeps you connected to what matters most.
Moving Forward with Confidence
End-of-year goal setting is a powerful way to celebrate growth, release what no longer serves you, and step into the new year with clarity and purpose. When you approach goals with flexibility, alignment and compassion, you set yourself up for a year of meaningful progress and fulfillment.
Ready to Start? Join Our High-Performance Goal-Setting Masterclass!
Working with a professional coach can help fast track your success! That is why we invite you to take this process even further by joining us for an exclusive Masterclass entitled “High-Performance Goal Setting3 Steps to Make 2025 Your Best Year Yet!” on Tuesday, December 17, 2024 at 7:00 p.m. CST.
In this interactive Masterclass, we’ll dive deeper into each step, helping you:
1. Reflect on your wins and growth over the past year.
2. Reassess and let go of what no longer serves you.
3. Reset with clarity to make 2025 your best year yet.
You’ll leave with a step-by-step plan to set and achieve purposeful goals in 2025. Register today at:
www.renewyourmindmd.com/renewed or scan the QR Code for all the details — spaces are limited, so secure yours today! Make 2025 the year you realize your potential and thrive with purpose!


Nora Vasquez, MD, CHPC, is a triple Certified HighPerformance Coach for Physicians, APPs and Executives. Dr. Vasquez is a board-certified Internist with over a decade of experience. Dr. Vasquez is the Co-Chair of the Physician Wellness Committee for the Bexar County Medical Society and serves on the Texas Medical Association’s Council for Member Experience. She developed the Physician Coaching and Wellness Masterclass Series for BCMS physician members to empower healthcare professionals with evidence-based coaching strategies to mitigate burnout and enhance their well-being. You can learn more about Dr. Nora Vasquez at www.renewyourmindmd.com/renewed or email her at renewyourmindmd@gmail.com.

By UT Health San Antonio
As the golden sun peeks over the Hill Country skyline, UT Health San Antonio Multispecialty and Research Hospital begins to stir with the promise of a new day. A physician scientist steps purposefully through the sleek glass entrance into an atrium bathed in natural light. Their path leads to an expansive lab equipped with the latest in diagnostic technology, ready for breakthroughs to come.
During morning rounds, clinicians greet patients in spacious private rooms designed to feel more like serene suites than medical spaces, offering a sense of calm and comfort in every interaction. As the day winds down, a physician scientist pauses, reflecting on a fulfilling journey. Here at UT Health San Antonio Multispecialty and Research Hospital, this is more than a day’s work — this is where pioneering science and compassionate care unite to foster an environment of healing, discovery and hope.
“UT Health San Antonio Multispecialty and Research Hospital brings unparalleled, comprehensive patient care and cutting-edge clinical research directly to the heart of South Texas. Our goal is to not only advance the science of medicine but ensure our community has access to the latest breakthrough treatments close to home. We are setting a new standard for health outcomes in our region,” said UT Health San Antonio Multispecialty and Research Hospital Chief Executive Officer Jeff Flowers, MBA, FACHE.
From the beginning, the hospital’s planning team knew they wanted a place where deep commitment to patient care merged seamlessly with cutting-edge research and use of the latest technology. Every aspect of the facility was thoughtfully designed to foster clinical innovation while prioritizing patient well-being. Chief Operating Officer Jeremy Viles, DNP, said the hospital was specifically designed to support care teams in all their missions — clinical, educational and research. “We had a great



deal of faculty and provider participation in the planning process, in all the clinical and research areas, to really be able to augment the entire continuum of research that we offer at the university,” said Viles. Continuity of care during clinical trials
A top priority was providing continuity of care for patients involved in clinical trials, many of whom are highly immunocompromised or have other comorbidities. For example, working together with the Institute for Drug Development within the Mays Cancer Center at UT Health San Antonio, front-line clinical trials require frequent pharmacokinetic monitoring. This involves conducting numerous blood tests to identify medication levels over time in a patient’s system. At the new hospital, patients can have testing completed and processed immediately in one convenient location.
“Rather than stopping and starting in an outpatient clinic setting, this gives us the option to treat those patients consistently and timelier through their entire continuum of care. It offers a better experience to our patients, and it offers greater efficiency to the primary investigators for our clinical trials,” Viles said.
The hospital also provides a protective environment unit, meeting the highest safety requirements for an in-patient setting. Patients staying at the hospital for long periods of time such as those undergoing stem cell transplants, cellular therapy or other oncology services, can be continuously monitored and have immediate access to a higher level of care delivery required for their unique disease.
A first for UT Health San Antonio, this hospital will be able to support novel pharmacy research through fully United States Pharmacopeia (USP)-compliant non-sterile compounding, or food compounding, along with typical sterile compounding. Additionally, the hospital’s 22,000 square-foot laboratory is nearly double the capacity for hospitals this size, providing ample room for the unique blend of scientists, researchers and hospital personnel.
At the forefront of new technologies, treatments
Associate Vice President for Research Operations Kimberly Summers, PharmD, said researchers are gearing up to initiate clinical trials
as soon as the hospital achieves accreditation by The Joint Commission, which is anticipated in 2025. “UT Health San Antonio Multispecialty and Research Hospital will be at the forefront of adopting new technologies and providing leading treatments for our patients. As an academic-research hospital, we have the potential to significantly enhance patient care by delivering innovations and discoveries from our UT Health San Antonio investigators directly to the bedside, seamlessly integrating these advancements with the care of our patients,” said Summers.
In the 2024-2025 U.S. News & World Report’s Best Global Universities rankings, UT Health San Antonio ranked No. 51 among the world’s top 1,000 universities with clinical medicine research programs, and No. 32 among all U.S. healthcare institutions in the 2024 Nature Index for their research output. The hospital, as part of UT Health San Antonio, means it can integrate research and education into its operations, offering specialized services and treatments previously unavailable in this region. “The academic connection ensures that leading experts in various medical fields are deeply involved in both patient care and research delivering novel treatments and therapies to patients,” she said.
Current and future efforts will be significantly enhanced, particularly in areas that disproportionately impact the health of our South Texans. “This includes expanded research in complex diseases such as cancer, aging, brain health and neurosciences. These focused efforts will drive advancements in understanding and treating these critical health issues, ultimately benefiting our community,” Summers said.
Exceeding expectations in cancer care, research Patient care servi ces in oncology and research, in conjunction with the Mays Cancer Center, is expected to account for the majority of hospital services. Cancer research is an interdisciplinary effort, and this innovative multispecialty hospital elevates our research capabilities, said Lei Zheng, MD, PhD, executive director of Mays Cancer Center and vice president for oncology at UT Health San Antonio.
Some of the upcoming clinical trials made possible through the connection to the new hospital include novel CAR-T and TCR-T cell therapies and innovative surgical procedures that can only be conducted in a hospital setting. “We will make the hospital a national resource where personalized, culturally sensitive clinical care and scientific discovery are conducted, focusing on the unique population of San Antonio and South Texas,” Zheng said. Quoting Sir William Osler, the father of modern medicine, Zheng said the practice of medicine “is an art, not a trade; a calling, not a business.”
“Our academic connection makes UT Health San Antonio Multispecialty and Research Hospital a place where the best art of medicine is practiced for the benefit of our patients,” said Zheng.
Tomorrow’s treatments today
While cancer research is at the forefront for the hospital, it has the capability to accommodate many other types of research conducted by UT Health San Antonio. “Anything that is going on for research at our university, we can augment at the hospital,” Viles said. “These are tomorrow’s standard-of-care treatments, and we’re offering them today. Regardless of setting, whether it’s oncology or other specialties, these medications and treatments represent the most advanced treatment that we can provide.”
UT Health San Antonio Multispecialty and Research Hospital was created by the community, for the community as a hub of discovery where tomorrow’s medical breakthroughs take shape today. The hospital’s opening marks not the end of almost a decade of planning, but the beginning of an ongoing journey, continually evolving to meet the ever-changing needs of San Antonio and South Texas. “We are committed to continually assessing the healthcare needs of our community, and that’s the core purpose of our hospital,” Viles said.“
UT Health San Antonio, UTSA merger another achievement
In another monumental achievement, the UT System Board of Regents announced in August that UT Health San Antonio and The University of Texas at San Antonio will merge, pending approval in 2025 by the Southern Association of Colleges and Schools Commission on Colleges (SACSCOC). The merged university will be the third largest in Texas, uniting unique strengths to offer Texans unmatched opportunities in education and healthcare. This powerful alliance will enhance the university’s reach and accelerate the translation of innovative research into clinical practice, expanding its significant impact nationally and shaping a brighter, healthier future for all.
Find out more about the UT Health San Antonio and UTSA merger at https://utsanantoniotogether.org/.
Learn more about the new UT Health San Antonio Multispecialty and Research Hospital at https://uthealthsahospital.org/.





By Rodolfo
“Rudy” Molina, MD, FACP, MACR, and Brian R. Loggins, BS, BBA, MBA
The State of Texas Association of Rheumatologists (STAR) has created a $2 million endowment fund with the Rheumatology Research Foundation (RRF). This generous commitment establishes the State of Texas Association of Rheumatologists Fellowship Training Award Endowment, which provides financial salary support annually to one fellow at qualifying ACGME-accredited adult or pediatric rheumatology fellowship training programs in the state of Texas. This endowment is intended to help address the rheumatologist shortage in Texas and elsewhere.
The State of Texas Association of Rheumatologists, STAR, was founded by Rodolfo “Rudy” Molina, MD, FACP, MACR in 2015 with the assistance of his practice administrator and STAR CFO, Brian R. Loggins, BS, BBA, MBA. Dr. Rudy Molina is also a Past-President of the Bexar County Medical Society (2021). STAR’s current Board of Directors are: President, Prashanth Sunkureddi, MD; President-Elect, Naser Elkhalili, MD; Treasurer, Jane Ayala, MD; and Secretary, Reeti Joshi, MD. The Past-Presidents of STAR are Rudy Molina, MD; Alex Limanni, MD; Matthew Mosbacker, MD; and Fehmida Zahabi, MD.
STAR’s mission is to promote the highest quality, evidence-based, specialty care for patients with rheumatic disorders and to provide cutting-edge education to members and the healthcare community at large while promoting the advancement of the specialty of rheumatology in the great state of Texas.
“We are thrilled to make this commitment to bolster the rheumatology workforce in Texas,” said Dr. Molina. “Making this investment to support future rheumatology professionals in Texas was an easy decision. I’m delighted we could do it at this time due to the substantial growth STAR has seen in membership and sponsorship.”
At the annual American College of Rheumatology Conference in Washington, D.C. in November 2024, the Rheumatology Research Foundation honored Dr. Molina and Brian Loggins by inducting them into the Foundation’s Honorary Board of Advisors. According to the Foundation, “The Honorary Board of Advisors is reserved for individuals who have made a transformative contribution, either through monetary support and/or an act of leadership, which made an indelible mark on the Foundation’s future fundraising success.”
“This exceptional commitment demonstrates the collective impact groups like state societies can have by rallying around pertinent issues affecting their local communities,” said Foundation executive director Rachel Myslinski, MBA. “STAR’s commitment to supporting the workforce in Texas is unprecedented. We are grateful for their vision of philanthropic support and for the opportunity to partner with them to create an avenue to invest back in the rheumatology workforce in Texas.”
According to the CDC, by 2040, the number of United States adults diagnosed with arthritis is projected to increase by 49 percent to 78.4 million. The 2015 American College of Rheumatology (ACR) Workforce Study projected that by 2030 adult rheumatology providers (physicians, nurse practitioners and physician assistants) will decline by 25 percent in terms of full-time equivalents, resulting in demand exceeding the supply of rheumatology providers by 102 percent.
The State of Texas Association of Rheumatologists Fellowship Training Award Endowment is funded from the income generated from STAR’s members’ registration and sponsorship fees for their annual meetings. The intent is to rotate the awards between the five adult and or two pediatric rheumatology training programs in Texas based on qualified applications received each year.
Rodolfo Molina, MD, FACP, MACR, earned his Medical Degree and completed his Internship and Residency at the Baylor College of Medicine, and his Rheumatology Fellowship at the Johns Hopkins University School of Medicine. He was the recipient of an U.S. Air Force Scholarship, and during his nine years of active duty, he was Chief and Program Director for rheumatology in a pilot program with Walter Reed Army Medical Center. Dr. Molina is a Past-President and Founder of the State of Texas Association of Rheumatologists (STAR). He is retired from Arthritis Associates in San Antonio, a former member of the Bexar County Socioeconomic and Legislative Committee and Past-President of the Bexar County Medical Society.
Brian R. Loggins, BS, BBA, MBA, is the Practice Administrator at Arthritis Associates in San Antonio, Texas. He is a co-founder of the State of Texas Association of Rheumatologists (STAR) and is currently the CFO of STAR. He is a member of the National Organization of Rheumatology Managers, ARP of the American College of Rheumatology, San Antonio Medical Group Management Association, and the Development Advisory Council of the Rheumatology Research Foundation.
The Texas Legislature meets every odd-numbered year for 140 consecutive days and will convene again January 14, 2025. Legislators need to hear from you — their physician, medical student and alliance constituents — during the session to understand how proposed legislation can potentially impact the practice of medicine in Texas.
Mark your calendar for 2025 First Tuesdays at the Capitol.
▪ February 4
▪ March 4 (TMA Alliance and Young Physician Month)
▪ April 1 (TMA Medical Student and Resident Month)
▪ May 6

www.texmed.org/firsttuesdays

By John E. Green, III, MD
Several months ago, San Antonio Medicine magazine featured an article about the Court Appointed Special Advocate (CASA) program and its interaction with physicians in Bexar County. CASA volunteers play a critical role in advocating for children experiencing foster care, often becoming the only consistent support system these children have during a turbulent time.
CASA volunteers are appointed by a judge to independently advocate for a child who has been removed from their home due to abuse or neglect. Their advocacy spans medical, social, developmental and behavioral needs — ensuring that the child’s best interests are represented. For more details about the CASA program and the training involved, visit casa-satx.org.
My Journey as a CASA Advocate
When I retired from active clinical practice last year, I sought a meaningful way to give back to my community. A television ad for
CASA sparked my interest, and after investigating further, I decided this was the perfect opportunity to make a difference. After completing the initial training — two evenings a week for four weeks — I was sworn in at the Bexar County Courthouse. Three days later, I was assigned to my first case: a 2½-year-old girl with significant medical needs. Most of the children may not have the complexity of medical problems as my case but all have some medical issues.
This little girl had not seen a physician since her discharge from the newborn nursery. Despite being born with jaw and tongue deformities and failing her newborn hearing test, she had no follow-up care. Tragically, her case came to CPS due to parental drug use and domestic violence. Her placement in daycare highlighted the urgency of beginning her immunizations. As her advocate, I worked alongside foster parents and CPS to ensure she received the medical attention she desperately needed. We then moved to correct her dental and oral problems and she had surgery at the UT San Antonio Pediatric Dental Service.
CASA advocates do not arrange medical visits or provide care directly. Instead, we serve as the child’s voice, providing reports to the district court judge about the child’s physical, emotional and social needs. In cases like mine, a physician’s expertise can be invaluable for explaining medical or developmental concerns to foster families and helping navigate complex medical systems — all without entering a patient-provider relationship.
For medical professionals, spouses or family members seeking a way to use their skills outside the clinic, CASA advocacy offers a unique and rewarding opportunity. Physicians especially bring a unique skill set to CASA advocacy. Our ability to analyze and communicate complex information can make a significant impact on a child’s life. If you’re feeling burned out or seeking a non-medical way to contribute, CASA offers a fulfilling opportunity to help a vulnerable population while broadening your perspective beyond medicine.
This role also works well for couples — many advocates serve alongside their partners, strengthening bonds while supporting children in need.
As an advocate, you commit to spending a few hours a month with your assigned child(ren) for the duration of the court case. Throughout this time, you provide the one constant in a child’s life as they navigate the CPS system, which may involve multiple placements. CASA
advocates provide a steady, reliable presence in the lives of children who often feel invisible within the system.
You’ll be guided by experienced staff members who help you navigate the complexities of the foster care and legal systems. While challenging at times, the process is incredibly rewarding — you become the anchor for a child during their most vulnerable moments.
Advocating for a child is life-changing, not only for them but for you as well. You’re not just supporting a child through a difficult time — you’re helping them rediscover a sense of normalcy and hope for the future. For me, the experience has been profoundly rewarding, and I firmly believe it was divine intervention that brought me to the right child at the right time.
If you’re looking for a way to give back, especially as you transition out of or scale back from clinical practice, consider becoming a CASA advocate. Together, we can make a difference — one child at a time.
You may email me at docgreen3@aol.com, sign up for an information session about how to become a CASA Advocate at casa-satx.org, or share this article with a colleague.
John E. Green, III, MD, became a CASA Advocate in August 2023 after a 44-year career in family medicine. Dr. Green is a life member of Bexar County Medical Society.

October 17, 2024
The BCMS Auto Program recently hosted its 38th Annual Auto Show. Each year, our members are invited to view various vehicles from our many participating auto dealers, all while enjoying live music, dinner, and the company of friends and colleagues. Thank you to our sponsors: Mission Oncology Partners, Fogo De Chao, Ruth’s Chris Steak House, the Bariatric Counseling Center, Pappas Delivery and Spurs Club @ the Rock.


Learn more about our Auto Program by going to www.bcms.org/autoprogram.php or calling 210-301-4367.








On Saturday, November 2nd, BCMS participated for the second year in the American Foundation for Suicide Prevention’s Out of the Darkness Community Walk for San Antonio and South Texas. One of many such events held across the country, the Community Walks gather together organizations and ordinary people to walk and raise awareness of the many lives lost each year to suicide, and the steps that can be taken on an individual and broader social level to prevent suicide and engender better mental health. “Teams” consisting of civil society groups such as BCMS, as well as the family and friends of people who died by suicide, gathered at the Nelson Wolff Municipal Stadium



before dawn for a three-mile walk. Despite a rainy start to the morning, the walk saw hundreds of people turn out, including our own BCMS team, consisting of Dr. Fernando Karst; Dr. John Nava; Dr. Mrudula Rao; Paulina Johnson, BCMS Alliance member; and Jacob Hernandez, BCMS staff. Also present at the BCMS table was BCMS CEO/ Executive Director Melody Newsom. At the table, BCMS distributed pens and Band-aids to attendees and fielded medical questions. A special thanks to all of our team members who attended, and to WoodmenLife Chapter 4525 for a generous donation that allowed us to purchase T-shirts!







Artist’s Note: This photograph, taken in Algeria, in a small town called Sidi Oqba, captures the stark reality of climate change’s impact on vulnerable populations in the Global South. A farmer is seated with his assortment of wares on a tarp, surrounded by the remnants of plastic and waste on the sandy desert ground around him. There is a striking irony that lies in the fact that the very material he uses for a makeshift marketplace — the plastic tarp — is a symbol of one of the many causes of the environmental challenges that are disproportionately and deleteriously impacting marginalized communities like his around the world, a metaphor for the complex relationships between poverty, livelihoods and climate change. The uncertainty etched on his face takes on added poignancy as it tells of his tribulations and of the interconnectedness of environmental degradation and human well-being, both physical and mental. We must all beware of cultivating a desert of hope, of remaining passively hopeful about our planet’s future, lest our inaction become the arid landscape from whence our children’s future tills.

Class


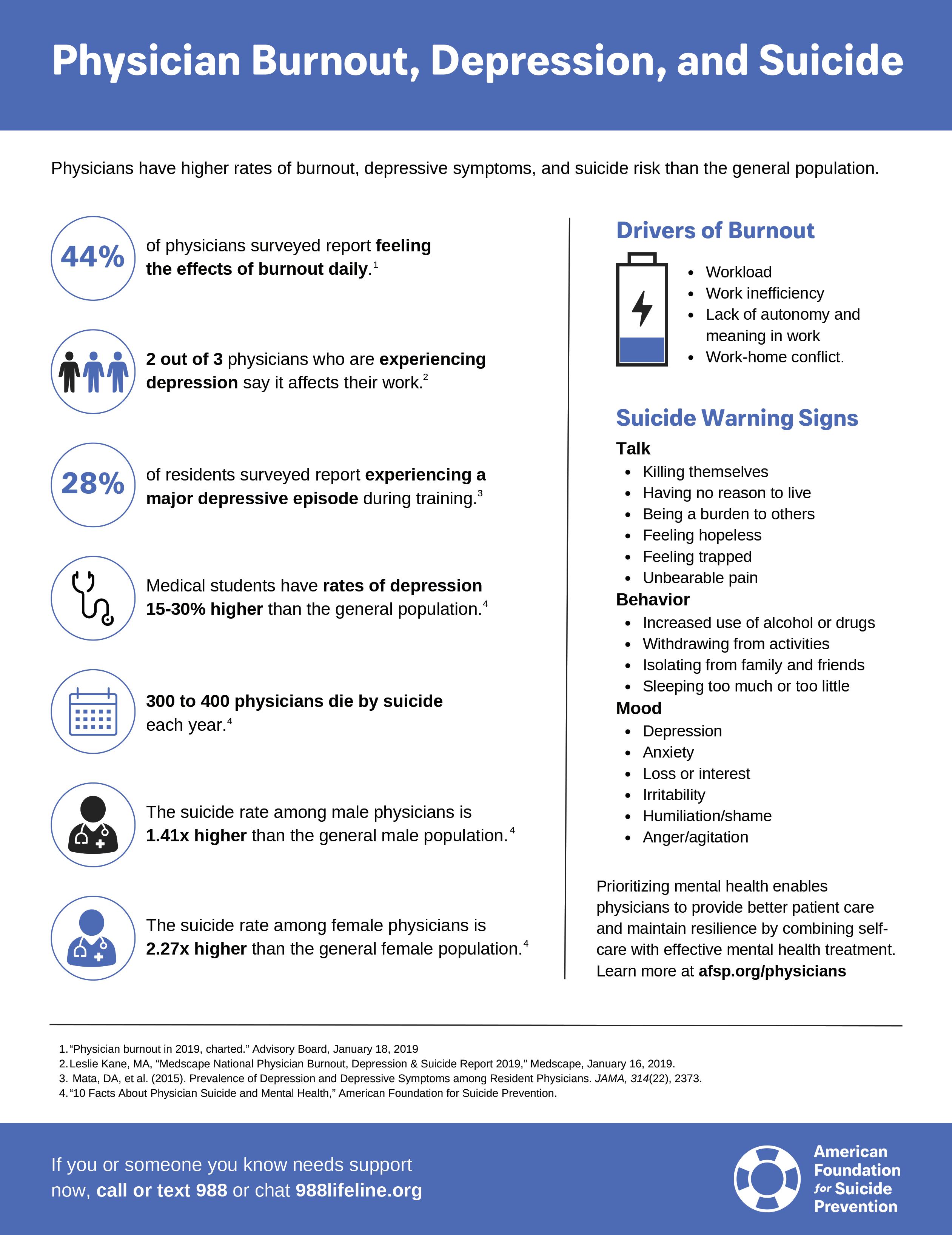
We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.

Sol Schwartz & Associates P.C.
(HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA
210-384-8000, ext. 118
CDavis@ssacpa.com
www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management
(HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark
President
210-268-1520
MClark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank
(HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead
210-283-6640
TDuran@broadway.bank
www.broadwaybank.com
“We’re here for good.”

Texas Partners Banks (HHH Gold Sponsor)
Our private banking team specializes in healthcare banking and will work with you to craft and seamlessly integrate financial solutions for you and your practice, including practice loans, lines
of credit and custom local lockbox solutions headquartered in San Antonio. Maria Breen
210-807-5562
Maria.Breen@texaspartners.bank www.texaspartners.bank

Lone Star National Bank (HHH Gold Sponsor)
Established in 1983, Lone Star National Bank has provided banking services to communities in South Texas for the past 41 years. LSNB is an independent and locally owned bank subsidiary of Lone Star National Bancshares-Texas, Inc with consolidated assets of $3 billion (12/31/23) and 36 full-service banking centers throughout Starr, Hidalgo, Cameron and Bexar counties.
Aside from personal and business banking, LSNB offers investments, wealth management & trust along with property and casualty insurance, health insurance and supplemental coverage.
Ivan Corona Molina
Assistant VP 210-479-4713
MolinaI@lonestarnationalbank.com www.lonestarnationalbank.com
“We do what the Little Banks can’t, and the Big Banks won’t!”
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.

Synergy FCU Member Services
210-750-8333
info@synergyfcu.org
www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison 210-503-0003
Yulia@genicslabs.com
Kevin Setanyan Managing Partner 210-503-0003
Kevin@genicslabs.com
Artyom Vardapetyan Managing Partner 210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease and Genetics.
Robert Castaneda CEO 210-316-1792
Robert@livingstonmedlab.com www.livingstonmedlab.com/home
“Trusted Innovative, Accurate and STAT Medical Diagnostics”

American Health Imaging (HHH Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina.
US Radiology Physician Number
210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists
210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora
Jaime.Zamora@usradiology.com
Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com
www.americanhealthimaging.com (main site)
www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)
ORGANIZATION

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney
Financial Advisor
210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Hancock Whitney (HHH Gold Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services. John Riquelme San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Larry Anthis Corporate Banking, Relationship Manager 210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez
San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington
Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com www.hancockwhitney.com

UT Health San Antonio
MD Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
Appointments: 210-450-1000
UT Health San Antonio
7979 Wurzbach Road San Antonio, TX 78229

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
DialOPS
(H Bronze Sponsor)
We were founded to meet a need: helping business owners succeed by giving them simple, quality, affordable U.S.-based contact solutions. In only a few years, our focus on nurturing client relations and building trust not only helped our customers grow their businesses, but helped us stake our claim in the highly competitive TAS industry as one of the most well-regarded and referred. Our 50 years of collective experience are the driving force behind our clients’ satisfaction.
Rachel Caero Managing Partner 844-554-3473
Rachel@dialops.net
Insperity
(HH Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Fran Yacovone
Business Performance Advisor 210-558-2507
Fran.Yacovone@insperity.com
Dayton Parker
Business Performance Advisor 210-558-2517
Dayton.Parker@insperity.com www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”

TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits
512-370-1746
Wendell.England@tmait.org 800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com

LASO Health Telemedicine and Rx App (HHH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care. LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com
SERVICES

Parvis Medical Suites
(HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer 210-632-3411
DrJohn@parvussuites.com
www.parvussuites.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
Field Sales Consultant
210-413-8079
Tom.Rosol@henryschein.com
www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout.
Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Darby Rodriguez
Regional Client Executive
281-753-3565
D.Rodriguez@eleosvhs.com
www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President
210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE
Vice President 210-912-0120
GMeyn@vestedbb.com
https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People”
Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber
President 210-308-7907 (Direct)
KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org www.samgma.org

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP® QKA
Senior Private Wealth Advisor 512-649-8113
Service@oakwellpwm.com www.oakwellpwm.com
“More Than Just Your Advisor, We’re Your Wealth Management Partner”

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle. San Antonio Office 210-301-4362
www.favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”



While driving the all-new 2024 Toyota Land Cruiser recently, I found myself thinking about brothers. My wife and I raised three boys, and it’s interesting how you’ll see an older brother in 11th grade who’s mature and six feet tall with a 7th grade younger bro who’s just short and young. You’re surprised that they’re even related. Then ten years later you’ve got 27- and 23-year-olds who are both adults and physically similar.
That’s the new Land Cruiser and 4Runner. Three years ago, the Land Cruiser was a full-size SUV that started at $80,000 and had a big V8, while the 4Runner was much smaller with a V6 and much smaller price tag. Now, after a two-year hiatus, the 2024 Land Cruiser returns riding on the same platform as the upcoming 2025 4Runner, uses the same drivetrain, and looks almost like the same truck, just slightly larger.
For the record, the newest “real” Land Cruiser — the 300 generation — is still available in many countries around the world, and can
“sort of” be purchased in the U.S., but in order to get it, you have to buy a Lexus LX 600.
As you might expect given all that, Toyota’s attempt to revive the Land Cruiser name for a smaller vehicle has met with mixed reviews, as the new version tries to balance nostalgia with a more compact, eco-friendly vehicle. Here’s a closer look at the, umm, Land Cruiser America?
The 2024 Land Cruiser’s design has a rugged look that draws heavily on the classic second generation FJ60’s (1970s) styling. I’d call it ruggedly modern, and the LED headlights and assertive front grille give it some upscale touches. While I think the newest Land Cruiser may be trying too hard to replicate the FJ60’s vibe, it’s undeniably handsome, and it’s worth noting that the boxy dimensions are good for passenger and luggage space.
The smaller size of the 2024 Land Cruiser makes it more maneuverable in tight spaces, which is good, but it loses some of

the commanding road presence that made the last generation so pleasing on the highway.
Acceleration isn’t great, but neither was it in the last version despite its V8 engine because of its prodigious curb weight. For the record, 0-60MPH for the 2024 Land Cruiser happens in just under eight seconds.
The four-wheel drive system and Toyota’s Multi-Terrain Select make the new Land Cruiser just as capable off-road as the last version. I didn’t take my press car off road, but many testers have, and no one has raised concerns about how the 2024 Land Cruiser does in the dirt.
Pricing is significantly lower than it was for larger 200-series models. Base 2024 Land Cruiser models go for around $58,000 with loaded versions maxing out at approximately $64,000.
While the last (200 series) Land Cruiser came with a thirsty V8, the new one has a turbocharged 2.4-liter four-cylinder assisted by two electric motors to make 326 horsepower. Its hybrid powertrain is rated at 22 MPG City and 25 MPG Highway, a big improvement over the 200 series but not particularly impressive.
Not surprisingly, the interior of the new Land Cruiser lacks some of the upscale feel that the last Land Cruiser had. To their credit, Toyota made sure everything you see and touch inside this year’s model looks tough and durable, even if subtracting some luxurious materials inevitably leaves the cabin feeling a bit spartan. And naturally, the new Land Cruiser’s smaller size means that rear passengers will find themselves with less room than before. Toyota decided not to include a third-row seat in the 2024 Land Cruiser, which reduces seating capacity to five.
Toyota has included many standard tech features, as you’d expect.
A 12.3-inch touchscreen comes standard, offering Toyota’s latest infotainment software, Apple CarPlay and Android Auto. Standard safety features like adaptive cruise control, lane departure warning and pre-collision braking are all there, too.
So, the newest Land Cruiser and its little brother, the 4Runner, have kind of merged, just like male siblings do when they’re all “growed up.” That’s a good thing with people, but it makes choosing between a 2024 Land Cruiser and the upcoming (slightly smaller) 4Runner a lot more difficult than it used to be. They’re both excellent SUVs to be sure, but they’re a lot more similar than they are different.

Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.






11911 IH 10 West San Antonio, TX 78230 Coby Allen 210-696-2232
Audi
21105 West IH 10 San Antonio, TX 78257
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198 14610 IH 10 West San Antonio, TX 78249 Tim Rivers 832-428-9507
Domingo
TX 78216
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463 Northside Ford 12300 San Pedro San Antonio, TX
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Chris Martinez 210-366-9600 9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945

