

Human Mobility












PUBLISHED
Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER: Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
GRAPHIC DESIGNER: Jennifer Nelson jennifer@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com
SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the ofcial publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE: Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006
www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily refect the opinion of BCMS, its members, or its staf. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our ofce to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and ofer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2025 SmithPrint, Inc. PRINTED IN THE USA

John Shepherd, MD, President
Lyssa Ochoa, MD, Vice President
Jennifer R. Rushton, MD, President-Elect
Lubna Naeem, MD, Treasurer
Lauren Tarbox, MD, Secretary
Ezequiel “Zeke” Silva, III, MD, Immediate Past President
Woodson “Scott” Jones, Member
John Lim, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Saqib Z. Syed, MD, Member
Nancy Vacca, MD, Member
Col Joseph J. Hudak, MD, MMAS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School Representative
Cynthia Cantu, DO, UT Health Medical School Representative
Lori Kels, MD, UIW Medical School Representative
Ronald Rodriguez, MD, UT Health Medical School Representative
Alice Gong, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Yvonne Nino, Controller
Al Ortiz, Chief Information Ofcer
Brissa Vela, Chief Membership and Development Ofcer
Jacob Hernandez, Advocacy and Public Health
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Jennifer C. Seger MD, Chair
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. Jyothula, MD, Member
George-Thomas Martin Pugh, MD, Member
Adam Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Amith Skandhan, MD, Member
Francis Vu Tran, MD, Member
Subhashini Valavalkar, MD, Member
Louis Doucette, Consultant
Brissa Vela, Staf Liaison
Gabriella Bradberry, Staf Liaison
Trisha Doucette, Editor
Ayomide Akinsooto, Student
Elizabeth Allen, Volunteer
Rita Espinoza, DrPH, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer


By John Shepherd, MD, President, Bexar County Medical Society
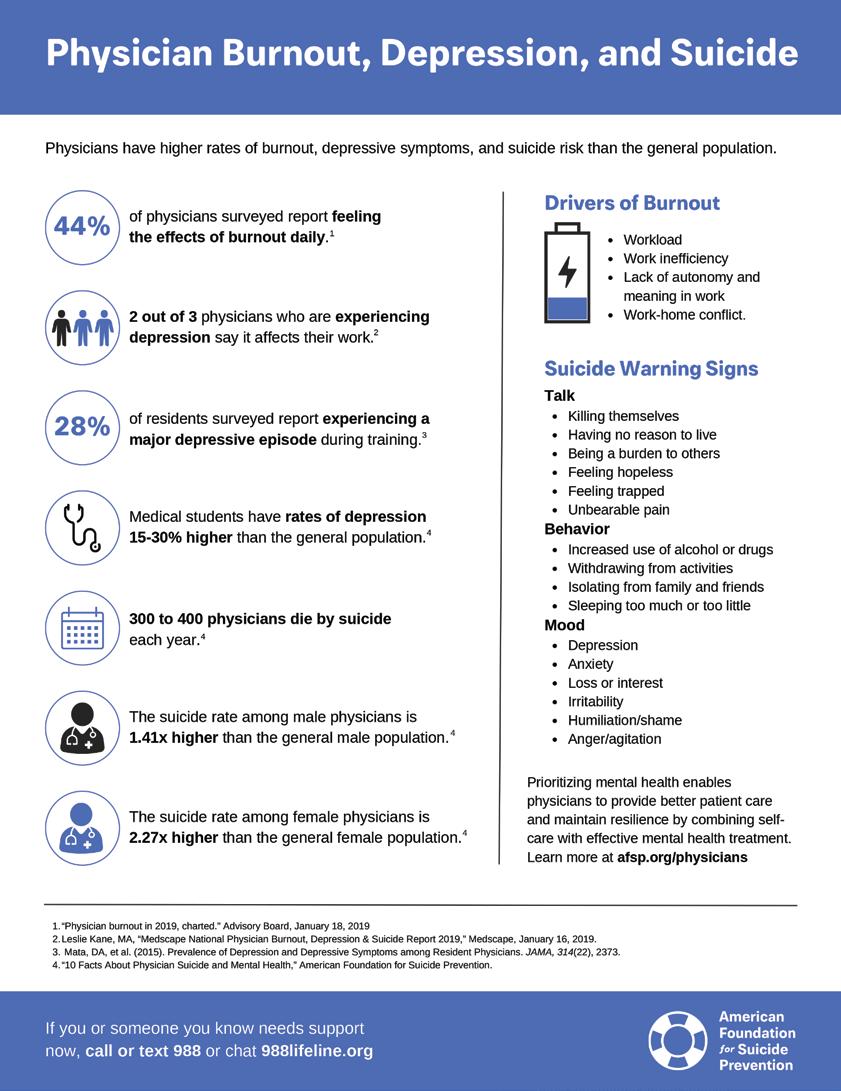
Today, somewhere, a physician took their own life. It happened the day before, too. And the day before that.
Physicians, o!en hailed as the healers of society, are tasked with the monumental responsibility of caretaking for others, yet their own well-being is frequently overlooked. Studies show that nearly 50 percent of physicians experience some form of burnout during their careers. More alarming, between 300 to 400 physicians choose to take their own lives annually — a rate double that of the general population. "e constant stress, long hours and emotional demands of the profession can lead to a state of physical, emotional and mental exhaustion, which contributes signi#cantly to this pervasive issue.
What can we, as physicians, do to stop the devastating trend of burnout and suicide within our profession? "e answer is not simple, nor is there a singular solution. "is complex issue demands a multifaceted approach that works to address the problem at individual, organizational and systemic levels.
One of the most signi#cant contributors to physician burnout is the overwhelming administrative burden that detracts from valuable time spent with patients. Physicians are increasingly #nding themselves bogged down by excessive paperwork, electronic health record management and bureaucratic requirements that take away from their core missions of providing patient care. "is administrative load not only increases stress levels but also erodes job satisfaction and contributes to feelings of ine$cacy. Additionally, reimbursement rates make it increasingly di$cult to sustain a practice, as physicians struggle to balance the #nancial pressure of running a practice with the need to provide adequate care for their patients. By engaging in advocacy, physicians can work collectively to in uence policy changes that address the root causes of administrative overload and improve the healthcare system as a whole. Programs like First Tuesdays empower physicians to take back control of how medicine is practiced, ensuring that the focus remains on patient care rather than stress-inducing bureaucratic hurdles.
Addressing the overwhelming administrative burdens is just one aspect of tackling physician burnout. Equally important are the organizational changes that prioritize physician mental health. Implementing policies that promote work-life balance, such as exible scheduling, can signi#cantly alleviate pressure on physicians. Additionally, creating supportive environments through peer mentorships, mental health resources and regular check-ins with leadership fosters a culture of openness and support. By prioritizing these things, healthcare organizations would #nd that they not only enhance physician well-being but also enhance job satisfaction, patient care and retention rates.
Dr. Jayesh Shah, TMA President-Elect, reminds us of the need for self-care, saying, “Burnout is a common struggle among physicians, but we must prioritize our own well-being to care for others e&ectively. Just like the airline safety instructions remind us to put on our own oxygen

mask #rst, we must do the same in medicine. A physician who prioritizes their own wellness is not only more productive but also fosters a healthier, more resilient community of patients.”
It’s important to ask ourselves if we are doing enough to recognize the signs and symptoms of stress and burnout. When was the last time you asked a colleague how they were doing or if they were okay when something with a patient didn’t go as expected? It’s crucial that we destigmatize conversations surrounding mental health, leaving physicians feeling able to seek help without fear of judgement. By normalizing these conversations, we encourage more people to access mental health services when needed, leading to early intervention and improved outcomes. "is culture shi! not only supports those struggling but also promotes overall well-being in the community.
It’s not just about formal healthcare; the support we receive from friends, family and colleagues can help bu&er stress, reduce anxiety, and combat feelings of isolation. When individuals have a safe space to share their struggles, especially without fear of judgment, it can make a signi#cant di&erence in their mental health. Consider inviting colleagues to join you for dinner or a walk on the San Antonio Greenway — it’s a great way to nurture those connections. Even better, include signi#cant others in these activities to further strengthen those bonds and help everyone feel more supported. It’s all about creating an environment where people can relax, recharge, and know they’re not alone in facing challenges.
"ere is still work to be done advocating for systemic change, fostering conversations about mental health, and building environments that prioritize well-being. Despite that, the Bexar County Family of Medicine is a place of compassion and understanding. Our goal is to ensure that every physician and their family feels valued and supported.
We all face di$cult times — some days, weeks or even years are harder than others. But remember, don’t let yourself or your colleague become just another statistic. Reach out for support when you need it and o&er it to others when you can. We all need it at times.
Every physician who has ever apologetically asked for a medical favor, help or advice for their self or their family has heard me tell them not to worry or feel apologetic. And then I say the same thing to each of them, “We help each other so that we can help those who need us.”
John Shepherd, MD, 2025 President of the Bexar County Medical Society, has been an active advocate for the Family of Medicine at the Texas State Capitol and has held several “Party of Medicine” events, introducing physicians on how to get involved with legislation that a ects medical issues. He has been Chief of Surgery at Christus Santa Rosa Children’s Hospital, a past member of the Board of Directors of Tejas Anesthesia, and currently serves on the BCMS Legislative Committee and the Bexar Delegation to TMA.


By Neha Shah, PT, CLT
People who are undergoing treatments such as chemotherapy, radiation and/or surgery for cancer can face limitations in physical and mental health along with side e&ects like nausea, weight loss, body pain and lack of energy. It would be a normal human tendency to rest and limit their activity while experiencing such symptoms. With improvements in treatments to manage certain side e&ects, some people tend to gain weight. However, the American Cancer Society recommends people to eat healthy and stay active during treatment. Today, there is enough research to back up the bene#ts of exercise at all stages of the cancer continuum: prevention, diagnosis, treatment, survivorship and palliative care.
How can regular exercise help you before, during and a!er cancer treatment? It can help your body and brain work better; reduce feeling tired (fatigue); help lessen depression and anxiety; help you sleep better; keep or improve your physical ability to get things done; improve your muscle strength, bone health and range of motion; strengthen your immune system; increase your appetite; help you get to and maintain a healthy weight; help with breast cancer-related lymphedema (and does not increase risk); decrease the chance that some types of cancer will come back; improve your quality of life; and reduce treatment side e&ects. (https://www.cancer.org)
Cancer rehabilitation (rehab) can help people to regain strength, physical function and the independence they may have lost due to cancer or its treatment. A multidisciplinary team comprising physicians, physical therapists, occupational therapists, speech pathologists, dieticians and psychologists can help address the side e&ects from cancer surgery and its treatment.
A!er a thorough evaluation from one of the therapists, a safe and individualized treatment plan is tailored to a patient’s needs. "erapists can address common side e&ects such as joint aches; neck or back pain; decreased range of motion; spinal cord injury; numbness or tingling; loss of strength; post-surgical pain; radiation #brosis; lymphedema; muscle spasms; cramps or achiness; bowel and bladder disorders; di$culty speaking or swallowing; fatigue and weakness; balance and walking di$culties; and brain fog, i.e. di$culty with memory and concentration. "e goal of all therapists is to enhance function and restore or maintain quality of life.
"e American Cancer Society has a Nutrition and Physical Activity Guideline for Cancer Survivors. "ese guidelines call for cancer survivors to: avoid inactivity and return to normal daily activities as soon as possible a!er diagnosis and treatment; take part in regular physical activity; start slowly and build up the amount of physical activity over time; build up to 150 minutes of moderate (or 75 minutes of vigorous intensity) activity each week; exercise several times a week for at least 10 minutes at a time; include resistance training exercise at least two days per week; and perform stretching exercises at least two days each week. "ese are general guidelines. You can #nd more information, including how much to exercise for speci#c cancer-related side e&ects, on the American College of Sports Medicine Moving through Cancer website. (https://www.exerciseismedicine.org/)
Neha Shah, PT, CLT, is a lymphedema specialist and a cancer-rehab therapist, longstanding member of the BCMS Alliance, and serves on the 2025 BCMS Alliance Steering Committee.





By Ravi Patel; Ian Dorsa; and Ramaswamy Sharma, MS, PhD
Mobility — broadly de#ned as the ability to move independently or with the assistance of devices — is essential for maintaining optimal quality of life. Key components of mobility include gait, walking speed and balance, all of which depend on e$cient musculoskeletal function. Preventing impairment of mobility is one of the most signi#cant challenges associated with aging. Mobility limitations in older adults are o!en associated with an age-related decline in muscle strength and muscle mass, collectively known as sarcopenia. Muscle strength begins to decline around the age of 30, with the rate of decline accelerating to approximately 12 to 15 percent per decade a!er the age of 50, becoming even more pronounced a!er the age of 60. Studies have shown that muscle strength decreases at an annual rate of about 2.5 percent at the knee joint and 1.5 percent at the elbow joint above age 60. Additionally, bone density begins to decrease from the second decade of life; in females, lower estrogen levels a!er menopause accelerates bone loss. Loss of muscle and bone mass together increase the risk of fractures a!er falls, frailty and disability. E&ective strategies for maintaining mobility with aging rely on adopting healthy lifestyle behaviors such as regular physical activity and high-quality diets.
Numerous studies have highlighted a dose-response relationship between physical activity and mobility; the bene#ts of structured physical activity in maintaining muscle strength, gait speed, balance and overall function for continuing daily activities is well-established. Adults aged 65 years and older who consistently engage in moderate-intensity physical activity for at least 30 minutes per day — or who maintain high to very high levels of physical activity — signi#cantly reduce their risk of fall-related injuries and bone fractures. A variety of interventions have been shown to improve mobility in older adults; these include progressive resistance training, multicomponent exercise, dual-task training, active video gaming, tai chi, yoga and dance. Such activities not only enhance physical function but also provide cognitive and social bene#ts, making them particularly valuable for older adults.
"e World Health Organization (WHO) and the American College of Sports Medicine advise that adults aged 65 and older should engage in either 75 minutes of high-intensity exercise (at 76 to 96 percent of their maximum heart rate), 150 minutes of moderate-intensity exercise (at 64 to 76 percent of maximum heart rate), or a combination of both per week. For example, brisk walking is considered moderate-intensity activity, while running or jogging is considered vigorous. However, most older adults rarely reach moderate-to-vigorous intensity daily, and light-intensity activities such as walking o!en make up most of their physical activity. Encouraging older individuals to begin with light-intensity activities and gradually increase their activity level can yield signi#cant bene#ts. Studies show that individuals with sarcopenia who begin with gait speeds less than 0.8 m/s increase their life expectancy by an average of 0.4 years with each improvement of 0.1 m/s in gait speed.
Importantly, skeletal muscle remains responsive to exercise throughout life, even in individuals aged 90 and older. Weight-bearing exercises, such as resistance training and jump training, are particularly effective for enhancing bone health and muscle strength,
especially for older adults at higher risk of fractures. High-intensity resistance training and low-load blood flow-restricted training have been shown to improve muscle size, strength and physical performance in older adults with mobility limitations. For optimal results, resistance training should be performed at least twice per week, with 7–9 repetitions per set and 2–3 sets per exercise at an intensity of 70 to 79 percent of one-repetition maximum (1RM), which refers to the maximum weight an individual can lift for a single repetition of a given exercise. Progressive resistance training (PRT), which involves gradual increase in the number of repetitions and sets along with an increase in the weight lifted, is even better as it increases lean body mass. This approach not only maximizes muscle strength but also improves muscle cross-sectional area and overall mobility, making it a key strategy for maintaining physical function in older adults.
In addition to regular physical activity, proper nutrition and diet play a vital role in preserving muscle mass and in counteracting the decline in physical performance associated with aging. Age-related loss of skeletal muscle is closely associated with decreased muscle mass and is attributed to an imbalance between muscle protein synthesis (MPS) and breakdown, resulting in negative protein balance. "is is further exacerbated by a phenomenon called “anabolic resistance,” which is pronounced in the elderly; elderly muscles require more of a stimulus to begin MPS, perhaps due to decreased levels of hormones such as testosterone, as well as due to reduced mobility with aging. Experts recommend two primary nutritional targets for older adults: (1) a daily energy intake of 25 to 30 kcal per kilogram of body weight (adjusted for ideal weight when necessary), and (2) a daily protein intake of at least 1.0 to 1.3 grams per kilogram of body weight, preferably divided equally between daily meals and a!er resistance workouts. Vitamin D levels should also be monitored regularly, with supplementation recommended if levels fall below 30 ng/mL.
A high-protein diet or protein supplementation is particularly e&ective in enhancing the bene#ts of resistance training for older adults, even in the presence of anabolic resistance, especially when combined with physical activity. "e quality of protein intake is also important, as branched chain amino acids, such as leucine, play an important role in stimulating MPS. A variety of healthy protein sources — including animal-based options such as whey, casein, skim milk, plain Greek yogurt, lean chicken, salmon and beef, as well as plantbased options such as cooked beans, soy, peas, and rice — can help meet daily protein needs at varying doses. Adequate protein intake stimulates MPS, thereby promoting muscle growth and repair, especially when combined with physical activity. Whey protein has been shown to be the most e&ective for increasing muscle mass, followed by milk protein, meat, soy protein and casein. Protein supplementation is very important for those individuals su&ering from the “anorexia of aging,” wherein there is a gradual aging-related loss of appetite and nutrient intake, governed by several factors such as dysregulation of appetite-regulating neurohormones. Intentional supplementation with high-quality protein sources is likely to be highly e&ective in modifying risk from both anabolic resistance and the anorexia of aging in age-related sarcopenia.
Preserving mobility in aging populations requires a comprehensive understanding of the biological processes underlying functional decline. While age-related deterioration of muscle strength, balance and overall mobility is inevitable, targeted interventions can slow its progression and mitigate its impact. Key physiological pathways involved in aging can be in uenced by dietary and lifestyle modi#cations, highlighting the potential for proactive measures to extend health span. A holistic approach that combines structured exercise, tailored nutrition, and supportive social and environmental factors o&ers the most e&ective strategy for maintaining mobility and independence in older adults. Decline in these interrelated factors with aging is “normal,” but it is far from inevitable!
9. Li, Y., Liu, M., Zhou, K., et al. "e comparison between e&ects of Taichi and conventional exercise on functional mobility and balance in healthy older adults: a systematic literature review and meta-analysis. Front Public Health. 2023;11:1281144. Published 2023 Dec 18 doi:10.3389/fpubh.2023.1281144
10. Liao, C.D., Huang, S.W., Chen, H.C., Huang, M.H., Liou, T.H., Lin, C.L. Comparative E$cacy of Di&erent Protein Supplements on Muscle Mass, Strength, and Physical Indices of Sarcopenia among Community-Dwelling, Hospitalized or Institutionalized Older Adults Undergoing Resistance Training: A Network Meta-Analysis of Randomized Controlled Trials. Nutrients. 2024;16(7):941. Published 2024 Mar 25. doi:10.3390/ nu16070941
References:
1. Billot, M., Calvani, R., Urtamo, A., et al. Preserving Mobility in Older Adults with Physical Frailty and Sarcopenia: Opportunities, Challenges, and Recommendations for Physical Activity Interventions. Clin Interv Aging. 2020;15:1675-1690. Published 2020 Sep 16. doi:10.2147/CIA.S253535
2. Blomstrand, E., Eliasson, J., Karlsson, H.K., Köhnke, R. Branched-chain amino acids activate key enzymes in protein synthesis a!er physical exercise. J Nutr. 2006 Jan;136(1 Suppl):269S-73S. doi: 10.1093/jn/136.1.269S
3. Brahms, C.M., Hortobágyi, T., Kressig, R.W., Granacher, U. "e Interaction between Mobility Status and Exercise Speci#city in Older Adults. Exerc Sport Sci Rev. 2021;49(1):15-22. doi:10.1249/JES.0000000000000237
4. Cuthbertson, D., Smith, K., Babraj, J., Leese, G., Waddell, T., Atherton, P., Wackerhage, H., Taylor, P.M., Rennie, M.J. Anabolic signaling de#cits underlie amino acid resistance of wasting, aging muscle. FASEB J. 2005 Mar;19(3):422-4. doi: 10.1096/ (.04-2640(e. Epub 2004 Dec 13.
5. Dipietro, L., Campbell, W.W., Buchner, D.M., et al. Physical Activity, Injurious Falls, and Physical Function in Aging: An Umbrella Review. Med Sci Sports Exerc. 2019;51(6):1303-1313. doi:10.1249/MSS.0000000000001942
6. Harvard Health. Preserve your muscle mass. (2016, February 19). https://www.health.harvard.edu/staying-healthy/preserve-yourmuscle-mass
7. Helms, E.R., Zinn, C., Rowlands, D.S., Brown, S.R. A systematic review of dietary protein during caloric restriction in resistance trained lean athletes: a case for higher intakes. Int J Sport Nutr Exerc Metab. 2014 Apr;24(2):127-38. doi: 10.1123/ ijsnem.2013-0054. Epub 2013 Oct 2. PMID: 24092765
8. Kassis, A., Fichot, M.C., Horcajada, M.N., et al. Nutritional and lifestyle management of the aging journey: A narrative review. Front Nutr. 2023;9:1087505. Published 2023 Jan 24. doi:10.3389/fnut.2022.1087505
11. Martone, A.M., Onder, G., Vetrano, D.L., Ortolani, E., Tosato, M., Marzetti, E., Landi, F. Anorexia of aging: a modi#able risk factor for frailty. Nutrients. 2013 Oct 14;5(10):4126-33. doi: 10.3390/nu5104126
12. Measuring Sarcopenia Severity in Older Adults and the Value of E&ective Interventions. J.Nutr, Hlth & Aging 2018: 22 (10): 1253-58.doi: 10.1007/s12603-018-1104-7
13. Pennings, B., Boirie, Y., Senden, J.M., Gijsen, A.P., Kuipers, H., van Loon, L.J. Whey protein stimulates postprandial muscle protein accretion more e&ectively than do casein and casein hydrolysate in older men. Am J Clin Nutr. 2011 May;93(5):997-1005. doi: 10.3945/ajcn.110.008102. Epub 2011 Mar 2
14. Sadaqa, M., Németh, Z., Makai, A., Prémusz, V., Hock, M. (2023) E&ectiveness of exercise interventions on fall prevention in ambulatory community-dwelling older adults: a systematic review with narrative synthesis. Front. Public Health 11:1209319. doi: 10.3389/fpubh.2023.1209319

Ravi Patel is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. He is interested in Emergency Medicine and in the application of arti cial intelligence in improving multiple clinical aspects of medicine.

Ian Dorsa is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. An army veteran, his interests include Family Medicine and improving access to care in San Antonio.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma serves on the BCMS Publications Committee.
During the first full week of April each year, the American Public Health Association (APHA) brings together communities across the United States to observe National Public Health Week (NPHW). NPHW recognizes the contributions of public health, and highlights issues that are important to improving our nation's health.
Join us April 7-13, 2025, for the 30th anniversary of National Public Health Week! APHA serves as the organizer of NPHW. The City of San Antonio Metropolitan Health District (Metro Health) will have events during the week along with other partners to display the impact of public health on our community.
This year's theme is “It Starts Here!”
Public health starts with each of us making a di erence in our homes and communities here in San Antonio. It’s about how the places we live, work and play shape our well-being. It’s the strength we gain by coming together to build a healthier, more resilient community through collaborations in our community and advocating for the health of our neighborhoods. Join us for the 30th anniversary of National Public Health Week as we reflect on our successes, confront challenges ahead unified, and work toward a healthy San Antonio for all.
Join Metro Health in the Celebration!
Metro Health invites San Antonio healthcare providers to engage in meaningful discussions and community events designed to strengthen our city’s public health infrastructure.
Key Events:
Public Health Fest
April 10, 2025, | 3:00 p.m. to 6:00 p.m.
Rosedale Park
A community celebration with interactive health exhibits, resources and vaccinations.
City of San Antonio’s Proclamation of NPHW
April 10, 2025
San Antonio City Council A-Session
A formal recognition of NPHW and public health e orts.
Metro Health encourages healthcare providers to participate in NPHW 2025 to help shape the future of public health in our community. For details, visit SA.gov/NPHW


By Claire Kowalick, UT Health San Antonio
About one in 10 Texans is living with Type 2 diabetes — one of the highest rates of the disease in the United States. In San Antonio, the rate is one in six people and another third of the population is prediabetic, according to the American Diabetes Association.
Type 2 diabetes is a chronic condition in which the body cannot produce enough insulin or use insulin properly and, if le! uncontrolled, can lead to high blood sugar, heart disease and kidney failure. Chronically elevated blood glucose, common among diabetics, can damage the nerves of the hands, feet and legs. "is damage, called neuropathy, puts people at risk for foot ulcers, infection and potential limb amputation.
Neuropathy can feel like burning or prickling sensations in their hand and feet, pain, cramping, numbness or tingling. For some people, neuropathy feels like bugs crawling on them and others perceive that their feet are freezing cold when they are warm to the touch. Some people feel like they’re wearing thick socks and cannot feel the ground even when they’re barefoot. About half of patients with diabetes will develop neuropathy that is severe enough to cause sensory loss in the feet.
Because neuropathy causes reduced or absent feeling in the feet, people may not sense a minor cut, blister or callus. A small sore can turn into an open wound and lead to the breakdown of surrounding tissue called an ulcer. Having diabetes also causes the body to heal more slowly, adding to an increased risk of long-term open wounds and infection.
Structural foot deformities like hammer toes, bunions or limited joint motion are also precursors to potential foot ulcers. "ese factors can contribute to pressure sites that turn into ulcers.
A recent study) from "e University of Texas Health Science Center at San Antonio (UT Health San Antonio) on complications from diabetic foot infections found that nearly half of patients with an infection were likely to experience reinfection, even a!er successful treatment. Patients with unhealed wounds for three months or longer and patients who had bone infections were most at risk of reinfection. Understanding these risk factors can guide provider care and produce better patient outcomes.
“It’s not related to people not having e&ective treatment of the #rst infection. It’s wound healing. When your wound fails to heal or you develop another wound, the clock starts ticking,” said Lawrence A.
Lavery, DPM, MPH, diabetic foot complications specialist and professor of orthopaedics at UT Health San Antonio, Joe R. and Teresa Lozano Long School of Medicine’s Division of Podiatry.
Along with a higher risk of reinfection, patients with unhealed wounds can experience longer healing time, more foot-related hospital readmission and longer hospital stays. Calling awareness to these risk factors could help stem a cycle of infection, reinfection, amputation, re-amputation, repeat hospitalizations and even early death. "ese diabetic complications can be emotionally and #nancially draining for patients and their families.
“You come into the hospital and you’re dealing with a limb-threatening, life-threatening infection and it gets resolved. Maybe you don’t have surgery, maybe you lose part of your foot. You think you’re out of the woods and then you get another event,” Lavery said.
Men are twice as likely to experience a diabetic-related amputation, many of whom are working age with families. Lavery said individuals o!en face the di$cult decision of staying home to heal properly or returning to work to provide for their loved ones, risking a longer recovery and a higher chance of reinfection.
Lavery said a priority in diabetic care today is developing tools, strategies and treatments to accelerate wound healing. If a wound heals before it becomes an ulcer, it substantially lowers the risk of infection.
“It’s about closing the loop faster. If patients don’t develop an ulcer, then the event is over. But once someone has an ulceration, they are at risk of having another ulcer or amputation in the next year. With no preventive treatment, about 60 percent of these patients will have another ulcer,” said Lavery.
While some may think diabetes and related complications only happen in older adults, Lavery’s study shows otherwise. He found that among diabetic patients experiencing chronic foot infections, the average age was 53. In recent years, diabetic complications have risen sharply among younger adults — a trend that shows no signs of stopping as people are developing obesity, high blood pressure and other comorbidities at earlier ages. With the rising incidence of Type 2 diabetes among younger people, youth doesn’t guarantee fewer or less severe diabetic complications.
“It’s not as much the chronological age as the physiological age caused by the burden of disease that is making them ‘older.’ We are getting more and more 30-year-olds in the hospital with foot infections. Usually, people don’t get neuropathy until they’ve had diabetes for a decade. People are getting diabetes younger, and it is increasing the number of people facing limb-threatening infections,” Lavery said.
To help prevent diabetic foot infections and related complications, UT Health San Antonio has developed a comprehensive program
that incorporates education, preventive care and addressing potential healthcare barriers in specialized prevention clinics. UT Health San Antonio podiatrists hosted a free foot screening clinic in February where they conducted quick, painless exams and provided information.
“Once we get people healed, we really need to spend time and resources on preventive strategies like therapeutics use, insoles education and talking to people about their diet and activity. "is is a holistic approach to prevention,” Lavery said.
"e UT Health San Antonio podiatry team has six recommendations to help avoid foot-related diabetic complications:
1. Maintain blood sugar and avoid smoking: Managing blood sugar helps keep neuropathy at bay and smoking can increase circulation problems, increasing risks.
2. Inspect feet daily: Check for blisters, cuts or calluses to catch problems early. An annual visit with a podiatrist is recommended for people with diabetes.
3. Choose the right footwear and socks: Supportive shoes are recommended, such as athletic shoes with arch support, heel counters and adequate toe box. Cushioned, moisture-wicking socks help reduce friction and prevent blisters.
4. Trim toe nails regularly: Cutting nails straight across helps avoid ingrown toe nails and infection.
5. Moisturize skin: Diabetes can cause skin to be drier than normal and dry skin can lead to cracks and cuts. Apply a dermatologist-recommended moisturizer to the skin but avoid applying between the toes to avoid potential fungal infections.
6. Always wear shoes: Wearing protective footwear, even in the house, decreases the risk of foot injuries.
Reference:
1. https://news.uthscsa.edu/ut-health-san-antonio-study-uncovers-key-risk-factors-for-diabetic-foot-infection-recurrence

Claire Kowalick is a science writer and senior public relations specialist with e University of Texas Health Science Center at San Antonio. She is a graduate of the University of North Texas. As a science writer, she combines her passion for writing with a deep appreciation of biomedical science to tell people about the groundbreaking research and novel discoveries happening at South Texas’ largest academic research institution.
By Andrew J. Marks, MD, FRCSC; and Juan C. Prieto, MD
In recent years, robotic surgery has transformed the #eld of pediatric urology, providing signi#cant advancements in the way urological conditions in children are treated surgically. Traditionally, certain complex pediatric urologic procedures o!en required large incisions and longer recovery periods, leading to delays in recovery, prolonged hospital stays, need for narcotic pain medications, and even potential long-term disability. Today, thanks to the integration of robotic-assisted technologies and minimally invasive techniques, many of these procedures have become less invasive, using increasingly sophisticated and precise tools, all of which contribute to improved patient mobility a!er surgery. "e use and innovation of robotic and other minimally invasive surgical techniques continue to help us maximize mobility and improve recovery in our young patients, enabling them to return to their active lives more quickly and comfortably while preserving excellent clinical outcomes.
Historically, pediatric urological surgeries, such as those for urinary tract reconstruction or obstructive conditions, were performed through large, open incisions. While these procedures were e&ective in addressing urologic disease, performing these complex surgeries using an open technique came with a range of challenges. Long hospital stays, signi#cant post-operative pain and slower recovery times were common drawbacks for young patients.
"e advent of minimally invasive techniques, including robotic-assisted surgery, has dramatically changed this landscape. Robotic surgery uses small, precise incisions and sophisticated tools that enable surgeons to operate with enhanced accuracy. With robotic systems like the da Vinci Surgical System, surgeons have access to high-de#nition 3D imaging, #ne motor control, and the ability to make smaller, more precise movements during procedures. Newer technology has even allowed for real time haptic feedback, one of the earlier limitations of robotic surgery. " is breakthrough technology has had a profound impact on the recovery trajectory of pediatric patients, allowing them to regain mobility much faster than with conventional methods.1,2
One of the most signi # cant advantages of robotic surgery in pediatric urology is the ability to perform procedures with minimal invasiveness. In the past, many pediatric urologic surgeries, such as pyeloplasty (the repair of an obstructed ureter at the uretero-pelvic junction), vesicoureteral re ux surgery and bladder reconstruction, required large incisions that could take weeks to heal. In contrast, robotic-assisted surgeries use much smaller incisions, and in turn faster healing times.3
For pediatric patients this is especially important. Children’s bodies are resilient, but they are also more sensitive to the stress of surgery and the recovery process. With robotic-assisted procedures, young patients can experience less pain post-surgery, and thus quicker recovery to full mobility. Studies have shown that pediatric patients undergoing robotic surgery o!en have shorter hospital stays, reduced need for narcotic pain medications and less overall post-operative discomfort. As a result, they can return to their normal activities — such as playing, attending school, and engaging in physical exercises — sooner than if they had undergone traditional surgery.4
In addition to these physical bene#ts, the psychological e&ects of robotic surgery should not be underestimated. "e reduction in post-operative pain and faster recovery times have been shown to decrease anxiety in pediatric patients, by decreasing pain and enabling them to recover in a less stressful environment at home. Children who are not limited by prolonged hospital stays or recovery times are more likely to experience better emotional and social outcomes as well, contributing to an overall improved quality of life.5

Precision is one of the cornerstones of robotic-assisted pediatric urologic surgery. Robotic systems provide surgeons with high-de#nition, 3D visualization of the surgical #eld, allowing them to identify and navigate delicate anatomical structures with incredible accuracy. For instance, during a robotic-assisted pyeloplasty, the surgeon can have a clear view of the kidney and surrounding structures by taking advantage of the expanded view of the peritoneal cavity, minimizing the risk of unintentional damage to nearby structures.) "e ability to perform intricate surgeries with minimal disruption to the surrounding tissues leads to a more seamless recovery process. A key factor here is the reduced need for postoperative interventions such as physical therapy or extended bed rest. "ese early recovery milestones help children regain their independence, build strength, and avoid the prolonged inactivity that can sometimes result from traditional open surgery. +
Numerous studies have demonstrated the bene#ts of robotic-assisted pediatric urological surgery. Studies have shown that robotic surgical approaches for conditions such as obstructive uropathy, bladder dysfunction or renal anomalies experience complication rates and success rates comparable with open surgery. However, given the minimally invasive nature of these procedures, there can be a quicker return to functional mobility.,
As technology continues to evolve, the role of robotic surgery in pediatric urology will only expand. With the development of even more advanced robotic systems and techniques, surgeons will be able to address a broader range of pediatric urological conditions with increased precision and e$cacy. Future innovations, such as augmented reality and arti#cial intelligence, may further enhance a surgeon’s ability to perform highly specialized procedures with even less risk and faster recovery times.)
In addition, the growing accessibility of robotic surgery in hospitals and clinics across various regions is expected to make these advanced procedures available to more children. As robotic systems become more commonplace, it is likely that more pediatric patients will bene#t from minimally invasive surgical approaches, allowing them to recover without some of the limitations traditionally associated with more invasive urological techniques.+
Robotic-assisted pediatric urologic procedures have rede#ned how we approach the treatment of urological conditions in children. By minimizing the invasiveness of surgery, reducing post-operative pain, and enhancing the precision of surgical interventions, these procedures enable young patients to recover more quickly and regain their mobility sooner. As we look to the future, the role of robotic surgery in pediatric urology promises even greater advancements in patient care, ultimately helping children with urologic conditions that require surgical care lead healthier, more active lives.

1. Zerphey, M., & McKenna, M. (2021). Advances in Robotic Pediatric Urology: Improving Outcomes and Reducing Recovery Time. Pediatric Urology Journal, 33(4), 1125-1131
2. Hyams, E.S., & Sutherland, A.M. (2020). "e Impact of Robotic-Assisted Surgery on Pediatric Urology: A Systematic Review. Journal of Pediatric Surgery, 55(6), 1200-1207
3. Beasley, S.W., & Smith, R.L. (2019). Minimally Invasive Surgery in Pediatric Urology: Bene#ts Beyond the Incision. Pediatric Surgery International, 35(1), 23-29
4. Adam, M., & Brenner, R. (2018). Robotic Pyeloplasty in Children: A Comprehensive Review. Urology Annals, 10(3), 235-240
5. O’Reilly, A.S., & Watson, W. (2022). Enhanced Recovery A!er Surgery in Pediatric Robotic Urology: A Path to -uicker Mobilization. Pediatric Surgery Today, 38(2), 101-107

Andrew J. Marks, MD, completed his Urology Residency at the University of British Columbia in Vancouver, and his Pediatric Urology Fellowship at Children’s Memorial Hospital in Chicago. His areas of interest and expertise include minimally invasive and robotic surgery, reconstructive urology, urologic oncology and pediatric stone disease. Dr. Marks is board certi ed in urology and subspecialty board certi ed in pediatric urology by the American Board of Urology. He is also a fellow of the Royal College of Surgeons of Canada. Dr. Marks is a member of the Bexar County Medical Society.

Juan C. Prieto, MD, completed his Urology Residency at the Universidad Nacional de Colombia in Bogotá. Then, he completed two Pediatric Urology Fellowship programs at Miami Children’s Hospital and Children’s Medical Center of Dallas. His areas of interest and expertise include reconstructive pediatric urology and urogynecology, neurogenic bladder management, and minimally invasive and robotic surgery. Dr. Prieto served as the Section Chief of Pediatric Urology at Children’s Hospital of San Antonio &om 2014 to 2020, and as the President of the Iberoamerican Society for Pediatric Urology &om 2018 to 2020. Dr. Prieto is a member of the Bexar County Medical Society.

By Antonio Webb, MD
As an orthopedic spine surgeon, I have dedicated my career to restoring mobility and reducing pain for patients su&ering from degenerative spinal conditions. One of the most transformative advancements in spine surgery is Arti # cial Disc Replacement (ADR) — a motion-preserving alternative to spinal fusion. During my fellowship training at the Texas Back Institute, I had the privilege of learning under the pioneers of arti#cial disc replacement: Dr. Richard Guyer, Dr. Scott Blumenthal and Dr. Jack Zigler. "eir groundbreaking work in this #eld has helped shape the future of spine surgery, providing patients with better long-term
outcomes. "e #rst arti#cial disc replacement in the United States was performed by Dr. Scott Blumenthal at the Texas Back Institute in 2000. His work helped pave the way for motion-preserving spine surgery as an alternative to spinal fusion.
Artificial disc replacement is a surgical procedure that involves removing a degenerated intervertebral disc and replacing it with a mechanical prosthesis designed to maintain normal spinal motion. Unlike spinal fusion, which permanently fuses two vertebrae
together, ADR allows for continued movement at the treated level, reducing stress on adjacent segments. The procedure is commonly performed in the cervical and lumbar spine for patients suffering from disc degeneration, herniation or spinal stenosis. This is very similar to knee (TKA) and hip replacements (THA) in that both procedures aim to restore motion and reduce pain by replacing a degenerated joint with a prosthetic implant. Just like knee and hip replacements preserve mobility and improve function, artificial disc replacement maintains spinal motion, preventing the stiffness associated with fusion surgery. These advancements help patients regain an active lifestyle while reducing long-term stress on surrounding structures.
1. Motion Preservation: One of the key advantages of ADR is that it maintains the spine’s natural movement. Fusion eliminates motion at the a & ected level, which can lead to sti & ness and restricted mobility. ADR, however, mimics the function of a healthy disc, allowing for exion, extension, rotation and lateral bending.
2. Reduced Risk of Adjacent Segment Disease (ASD): Spinal fusion alters the natural biomechanics of the spine, increasing stress on the discs above and below the fused segment. Over time, this can accelerate degeneration in adjacent levels, o!en requiring additional surgeries. ADR reduces this risk by preserving motion, distributing loads more naturally, and decreasing stress on neighboring vertebrae.
3. Faster Recovery and Less Postoperative Pain: Patients undergoing ADR o!en experience shorter hospital stays, faster recovery times and less postoperative discomfort compared to those who undergo spinal fusion. Because the procedure does not require bone gra!ing or fusion hardware, there is typically less surgical trauma and reduced postoperative complications.
4. Improved Long-Term Outcomes: Clinical studies have shown that ADR patients can report higher satisfaction rates, reduced reliance on pain medications and improved function compared to fusion patients. "e ability to maintain spinal mobility also contributes to a higher quality of life post-surgery.
Not all patients qualify for arti#cial disc replacement. Ideal candidates are those who:
• Have single-level or two-level disc degeneration with no spinal instability
• Do not have signi#cant osteoporosis, infections or spinal deformities
• Have failed conservative treatments such as physical therapy, medications and injections
• Are seeking to preserve mobility and avoid the limitations of spinal fusion
As advancements in spine surgery continue to evolve, arti#cial disc replacement is becoming an increasingly preferred option for eligible patients. At South Texas Spinal Clinic, I am committed to helping patients explore the latest surgical innovations that o&er the best possible outcomes. If you’ve been told you need a spinal fusion, I encourage you to seek a second opinion — ADR may be the better solution for your long-term mobility and quality of life.

Antonio Webb, MD, is a fellowship trained and board-certi ed orthopedic spine surgeon with South Texas Spinal Clinic. He has special interest in minimally invasive spine surgery (MIS), robotics/computer navigation and arti cial disc replacement. Dr. Webb is a member of the Bexar County Medical Society.

By Jamie Lynch, MD

San Antonio, we love our sports! We hear the loud smack of a pickleball or the hard thud of a volleyball slamming the court, and we are exhilarated. But with every thrilling spike, pivot and jump, there is a risk — a risk to those crucial joints: knees and shoulders. As part of TruOrtho, an orthopaedic surgery practice, and a specialist in shoulder and knee surgery and sports medicine, I understand the passion that drives your athletic ambitions.
No one likes to be out of commission. Whether you are a professional athlete, a t-ball star or a weekend warrior, you need to protect those joints. Although we cannot prevent all injuries, we can certainly try to reduce their frequency.
Knees
"e knee and the shoulder are two of the most complex and important joints of the human body. "ey enable us to do amazing things, but they are also prone to injury. Consider the knee: a marvel of ligaments, tendons and cartilage, designed to absorb shock and provide stability. However, those same important structures can be compromised by sudden twists, overextension or repetitive strain, particularly common in sports like basketball, soccer and CrossFit.
Take the shoulder, an extremely mobile joint, which gives it capacity to do so many things, however, and likely secondary to its mobility, it is not immune to risks. Rotator cu& tears, SLAP tears and dislocations a&ect even the most active individuals. "e shoulder is under a lot of pressure, with the popularity of overhead sports like volleyball and the dynamic movements in pickleball. Kilic et al.), o&ers very useful information on the incidence, causes and prevention of musculoskeletal injuries in volleyball. "is study also shows that the shoulder is one of the most common joints a&ected due to repetitive overhead motion.
Preventing injuries is more than just a quick stretch prior to going into the court. It is a holistic approach that includes strength training, exibility, correct technique and even nutrition.
• Strength Training: Having strong muscles around the knees and shoulders gives the athlete support and stability. Target the quadriceps, hamstrings and glutes for knee health and the rotator cu& and scapular stabilizers for shoulder health.
• Flexibility and Mobility: It is a well-known fact that tight muscles and decreased joint motion can lead to an increase in the risk of injury. Include dynamic stretching before activity and static stretching a!erwards. Yoga and Pilates can also be used as cross-training.
• Technique is Everything: Improper form is a common cause of many injuries. Consult coaches or trainers to make sure you employ the proper techniques for your sport. We understand the importance of a proper jump landing technique and recognize it has resulted in decreased knee injuries.)
• Listen to Your Body : Pain is an indicator; it is a message that something may be wrong. I recommend not to try and bear the pain. Practice thoughtful active rest, specifically remaining mobile and concomitantly reducing stress, apply ice and if the symptoms persist, consult a professional. CrossFitters can reduce injury with a focus on good form, a gradual increase in load and appropriate rest. Research indicates that most injuries are due to incorrect posture and exhaustion. +
• Nutrition and Hydration: A balanced diet, which includes protein, collagen, vitamins and minerals, helps in the healing of the tissues and general health. Consider an adequate intake of water an essential for overall health and wellness. Additionally, it can help in the prevention of muscle fatigue and strains.
Many sports injuries do not just occur suddenly — they can be related to other existing health issues. For instance, hormonal imbalances, nutritional de#ciencies and even stress can lead to fatigue, decreased bone density and muscle weakness that may lead to injury.
At TruOrtho, every athlete of any age or gender has a set of health concerns. We educate patients on how to use nutrition and exercise to enhance bone density and improve muscle strength, and we express the importance of managing systemic conditions to reduce the likelihood of injury.
Despite our best e&orts, injuries do occur. If physical therapy, Airrosti, activity modi#cation and thoughtful rest do not improve the issue, then surgical treatment may be required. As a specialist in shoulder and knee surgery, I am committed to providing the most advanced and e&ective surgical options, including minimally invasive techniques that minimize scarring and optimize your return to play.
1. e Prehab Routine: It should no longer be a novelty to warm up, prehab. Incorporate exercises that strengthen the muscles around your vulnerable joints in preparation for desired activity. For shoulders, think resistance band rotations and exercise to stabilize the shoulder blade. For knees, try squats with bands around your thighs.
2. e Listen and Learn Approach: Record your workouts and any discomfort you experience. "is may help you identify possible troubled joints or muscles before they become major issues.
3. e Hydration Hustle: Always carry a reusable water bottle with you, put salt in your water or an electrolyte packet, especially when you are engaging in intense exercise.
4. e Sleep Sanctuary: Get enough sleep. Aim for seven to nine hours of quality sleep each night., "is is when your body repairs and regenerates.
5. e Mindful Movement: It is advisable to practice mindfulness during your workouts. Pay attention to the patterns of your movement, your body position and the way it feels. "is enhances body awareness and helps you avoid overexertion and injury. Proper breathing while exercising is also crucial.
1. e Equipment Check Routine: It is important to check that your gear is appropriate for your size and is in good condition. " is applies to shoes, to protective gear and to sports-speci # c equipment.
Real-Life Example: I have seen many knee injuries in pickleball players due to worn out court shoes. If the shoe does not grip appropriately, then slips and subsequent twists occur. In the same way, a helmet that is too loose for a young cyclist will not give the

best protection. Before each season, or even each game, take a moment to check — Are your shoes providing good traction? Is your helmet snug? Are your pads secure? "is simple check can prevent serious injuries.
2. e Cross-Training Balance: Cross-train to avoid overuse injuries by engaging in a variety of physical activity. "is will reduce stress on any particular joint or part of the body.
Real-Life Example: A common issue I see with runners is knee pain from imbalanced muscles. Instead of constantly running, they should include swimming, cycling and weight training in their weekly schedule. "is o&ers the cardiovascular bene#ts without the impact on the knees. A soccer player should consider yoga to enhance exibility and core strength. Adjustments to a routine give overused muscles a rest and strengthens supporting muscles. Review the current literature examining integrative training strategies to decrease the risk of injury and enhance the performance of youth athletes..
3. e Recovery and Rest Strategy: Include rest and recovery in your training plan. "is means not only sleeping enough but also using foam rolls and other active recovery strategies. Hopefully you see the theme in this discussion.
Real-Life Example: I can recall a young basketball player who consistently pushed through fatigue, leading to a stress fracture. She was overtraining and not allowing her body to recover. I advocate for recovery days. When you have a tiring game or workout, instead of lying on the sofa and remaining completely inactive, try to stretch and use a foam roller to relieve muscle pressure. And most importantly, get those essential hours of sleep. A good night’s rest is when your body does its best healing.
Embracing a Holistic Approach
At TruOrtho, we o&er an approach to sports medicine that considers the whole patient. We collaborate with physical therapists, athletic trainers and other healthcare professionals to deliver optimum care for patients 9 years and up. We also concentrate on patient education so that you can become an active participant in your healthcare and get you back to sports.
References:
1. Kilic, O., Maas, M., Verhagen, E., Zwerver, J., Gouttebarge, V. Incidence, aetiology and prevention of musculoskeletal injuries in volleyball: A systematic review of the literature. Eur J Sport Sci. 2017 Jul;17(6):765-793. doi: 10.1080/17461391.2017.1306114. Epub 2017 Apr 9. PMID: 28391750
2. Shim, S.S., Con#no, J.E., Vance, D.D. Common Orthopaedic Injuries in CrossFit Athletes. J Am Acad Orthop Surg. 2023 Jun 1;31(11):557564. doi: 10.5435/JAAOS-D-22-01219. PMID: 37155727
3. Watson, N.F., et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015 Jun 1;38(6):843-4. doi: 10.5665/sleep.4716. PMID: 26039963; PMCID: PMC4434546
4. Myer, G.D., Faigenbaum, A.D., Ford, K.R., Best, T.M., Hewett, T.E. Integrative training strategies to reduce injury and improve performance in youth sports. Br J Sports Med. 2021;55(13):714-722
American Academy of Orthopaedic Surgeons (AAOS): www.aaos.org
National Institutes of Health (NIH): www.nih.gov
Sports Medicine Resources from Mayo Clinic: www.mayoclinic.org

Jamie Lynch, MD, is a board-certified fellowship-trained orthopaedic surgeon with over a decade of experience in treating orthopaedic disorders and sports medicine injuries of both the upper and lower extremities. As a member of the AAOS, ASES, AOSSM and AANA, Dr. Lynch speaks nationally sharing her techniques and expertise in shoulder surgery. She sits on the board of the Texas Medical Liability Trust and is an active member of the Forum. She is co-founder of TruOrtho, a supra-subspecialized all women orthopaedic practice in San Antonio, Texas and she is a wife and devoted mother of four young girls.

By Demetrios Macris, MD
Losing a leg is not the end of the book. Rather, it’s another chapter of life — a chapter #lled with challenges and opportunities for growth and resilience. For many patients, the journey begins long before amputation, o!en marked by weeks, months or even years of struggling with a lower extremity wound that is painful and hinders their ability to move freely. "e healthcare team that has worked to prevent amputation, must pivot their focus to executing a well-planned surgical procedure followed by a comprehensive rehabilitation program during the healing process. Once the decision for amputation is made, a prosthetist will be essential to help the patient regain mobility. "is relationship between the amputee and the prosthetist o!en endures longer than most other healthcare provider relationships, becoming a vital part of the recovery narrative.
This new chapter, however, is not without its bewildering moments and challenges. Amputees encounter a range of difficulties that can be physical, emotional and social in nature.
Adapting to lost mobility often requires learning new ways to move, including the use of prosthetics or mobility aids. Patients may experience significant pain, such as phantom limb sensations or discomfort from their prosthetics. Furthermore, the loss of a limb can impact overall strength and endurance, necessitating rehabilitation and training to regain fitness.
The psychological impact of limb loss can be profound. Patients may struggle with grief as they mourn the life they once had, often experiencing heightened levels of depression and anxiety. The loss can also lead to identity struggles, as individuals navigate changes in self-image and the way they perceive themselves in the eyes of others.
Amputees often face societal stigma and misunderstanding about their condition, leading to feelings of isolation. Mobility limitations can hinder their ability to maintain social connections or participate in activities they once enjoyed, and they may encounter workplace challenges when adapting to environments that are not accommodating.
The financial implications of limb loss can also be burdensome. The costs associated with prosthetics, rehabilitation and potential loss of income can create significant financial strain. Additionally, practical accessibility issues in homes, public spaces and transportation can further complicate their daily lives.
The risk of further health complications, such as obesity and cardiovascular disease, can increase due to reduced mobility and physical activity.
Addressing these multifaceted challenges requires a multidisciplinary approach. A robust support system — including medical professionals, psychological counselors, physical therapists and community resources — is essential to help individuals adapt and thrive after limb loss.
Society often exhibits discomfort towards amputees, as demonstrated by the temporary shutdown of The Prosthetic Foundation’s website due to the perceived inappropriateness of an image depicting an amputated stump. It is imperative for the healthcare team to break through this prejudice and approach the process of obtaining a prosthesis as an opportunity for renewed life rather than a symbol of defeat. This transition offers a chance to move beyond pain, frequent dressing changes, multiple doctor visits, surgeries and healthcare bills.
Limb salvage requires coordination, communication and expertise; similarly, amputation, recovery and prosthesis fitting are crucial to a patient’s well-being and demand the same level of effort. In Bexar County, a wealth of resources is available for amputees, but a positive outcome hinges on the compassion and guidance provided by a dedicated and informed healthcare team. By restoring mobility to an amputee, we enhance the individual’s quality of life and create immeasurable benefits for their families and communities.
Most patients who undergo amputation have little knowledge or experience of the postoperative expectations. If they receive some optimal care, they do not realize it. Navigating on their own requires a Herculean effort at a time when they are least able. A dedicated healthcare team can minimize unnecessary pain, poor healing, poorly fitting prostheses and financial roadblocks from this chapter in their lives. Providing a wheelchair provides comfort, but providing mobility provides empowerment.

Demetrios Macris, MD, has provided expert vascular care in San Antonio since 1992, specializing in aortic surgery, complex revascularization and limb salvage for diabetic patients. Trained at e University of Chicago, Emory University, and the University of Tennessee, he is board certi ed in Vascular Surgery and a Fellow of the American College of Surgeons. Dr. Macris has led advancements in vascular care, including Texas’s rst ICAVL-accredited vascular lab, and co-founded e Prosthetics Foundation to support amputees. Dr. Macris is a member of the Bexar County Medical Society.
Texas Biomedical Research Institute has been advancing the discovery and development of diagnostics, vaccines and therapies for more than 80 years.
Since its founding in 1941 by businessman, inventor, engineer, philanthropist and adventurer, Tom Slick, Texas Biomed has gained worldwide recognition in scienti#c and academic communities for the quality of its research. "e results of the Institute’s work have
Texas Biomed Professor Deepak Kaushal, PhD, has developed a vaccine candidate to combat tuberculosis (TB), one of the world’s deadliest infectious diseases. "e live-attenuated vaccine, which is in preclinical testing at Texas Biomed, aims to o&er broad, long-term protection to millions of people exposed to the pathogen worldwide each year. Currently, the only licensed vaccine for TB is the Bacille Calmette-Guérin (BCG) vaccine, which was developed more than 100 years ago and is based o& the bovine strain of TB. BCG does not completely protect against pulmonary TB, including reactivation and reinfection, highlighting the critical need for more e&ective replacement candidates.
Dr. Kaushal’s vaccine candidate is based on a weakened form of Mycobacterium tuberculosis, the bacterium that causes TB in humans. Notably, he knocks out a gene required to make a protein called Sigma H, which the bacterium needs to manage oxidative stress properly and survive in the lungs. "e vaccine candidate completely protects nonhuman primates from an otherwise lethal dose of TB, prompting a superior immune response that e$ciently eliminates the bacteria, while minimizing excessive in ammation.
Texas Biomed Professor Marie-Claire Gauduin, PhD, is focused on HIV prevention with an innovative vaccine candidate that targets the basal cells in the mucosal epithelium of the vagina and rectum, where HIV is most likely to breach the body’s defenses. Dr. Gauduin’s candidate is engineered to engage the epithelium’s basal cells, establishing an ongoing barrier against HIV entry as the vaccine is passed on to new cells as old cells die o&. Live-attenuated vaccines have previously failed in HIV because the virus mutated enough over decades to regain its potency. Dr. Gauduin’s patented, live-attenuated, replication defective, “single-cycle” vaccine virus gets around this issue by removing the virus’s ability to replicate and spread.
Dr. Gauduin’s vaccine exhibited promising results in early trials involving nonhuman primates, and her next studies will demonstrate the vaccine’s safety and e$cacy before it moves into human clinical trials. Currently, the vaccine is delivered directly to the mucosal lining by liquid drops. Dr. Gauduin will explore other delivery methods that may prove more e$cient, which will be critical for making it practical for mass immunization in developing countries.
included advancing the #rst COVID-19 vaccine, the #rst Ebola treatment, the #rst Hepatitis-C therapy, as well as many more developments and technologies.
Texas Biomed is dedicated to the advancement of human health through research into the prevention and eradication of infectious disease. Here are four of the top innovations currently underway at Texas Biomed:


“Unbreakable” Lassa vaccine candidate shows 100% effcacy against virus
Texas Biomed Professor Luis Martinez-Sobrido, PhD, and Scripps Research Institute Professor Juan Carlos de la Torre, PhD, have been working on a vaccine candidate for Lassa virus for the past decade. Lassa virus, an acute viral hemorrhagic illness, has no approved vaccine and no cure, and infects between 100,000 and 300,000 individuals each year, according to the Centers for Disease Control and Prevention (CDC). "e virus, which can cause fever, severe bleeding and organ failure, is passed from infected rodents to people through contaminated food or surfaces.
In a paper published in npj vaccines, the researchers demonstrated that their vaccine candidate against Lassa virus completely protected guinea pigs exposed to an otherwise lethal dose of the virus. Dr. Martinez-Sobrido and Dr. de la Torre combined their distinct approaches to attenuate the Lassa virus by tweaking both sections of its genome, which consists of a small segment and large segment. Dr. Martinez-Sobrido and his team used codon deoptimization to edit the RNA in the small segment to turn down production of a key protein responsible for binding the virus to infected cells. Dr. de la Torre and his team replaced part of the large segment RNA with the corresponding part from the small segment. "eir attenuated virus demonstrated a robust safety pro#le, reduced replication and did not evolve to regain virulence. "e study was completed in collaboration with NIAID’s Integrated Research Facility at Fort Detrick.
Repurposing a cancer drug to treat drug-resistant tuberculosis
Physician-scientist, President and CEO at Texas Biomedical Research Institute, Larry Schlesinger, MD, and his team led by Dr. Eusondia Arnett are working to repurpose a cancer drug to treat drug-resistant tuberculosis (TB). TB is currently the leading cause of death worldwide from a single infectious agent, accounting for 1.25 million deaths annually. More than 25 percent of these deaths occur due to antimicrobial resistance. Drs. Schlesinger and Arnett are investigating proteins BCL-2 and MCL-1 as a promising approach for TB host-directed therapy. "ese inhibitors are currently FDA approved for use in the treatment of blood cancers, including certain lymphomas and acute myeloid leukemia. "ey target proteins that promote cell survival and can induce apoptosis, or programmed cell death.
In a paper published in Biomedicine and Pharmacotherapy, Dr. Arnett as lead author demonstrated that MCL-1 and BCL-2 are promising targets for host-directed therapies to control both drug-susceptible and drug-resistant TB. "is therapeutic approach is expected to provide a treatment option that the pathogen is unlikely to develop resistance to, shortening treatment duration, boosting the immune response and reducing the chance of severe disease developing. If preclinical trials are successful, Dr. Schlesinger believes this new drug has the potential to be an important tool in the #ght against infectious diseases like TB.

By Grace Denise Huizar; Arunabh Bhattacharya, PhD; and Ramaswamy Sharma, MS, PhD
How o!en do we wake up with neck pain in the morning? While we can use various methods for obtaining relief from this aggravating condition, such as pain medication, topical creams and stretching exercises, what if there was another avenue to easily help alleviate this pain?
Osteopathic Medicine, founded by Dr. Andrew Taylor Still in 1874, originated from his newly coined word, osteopathy, which means "bone su&ering.") It is based on the philosophy that the body's structures (bones, muscles, organs) work together to create a harmonious and well-balanced system capable of self-healing and recovery.+ Before establishing the principles of osteopathy, Dr. Still practiced medicine on a Shawnee Indian reservation and witnessed medical practices as he fought against slavery during the American Civil War. His experiences practicing allopathic medicine, alongside the loss of three of his children to spinal meningitis, made him question the e$cacy, safety and patient-centered care of medicine during the nineteenth century. He was concerned about using toxic substances such as calomel for remedies and believed that they were doing more harm to the patients than good.) Determined to improve the practice of medicine, he dedicated himself to the pursuit of drugless, spiritual and holistic medicine based on anatomy and physiology, ultimately establishing a set of principles that has changed the practice of medicine. Upheld by the American Osteopathic Association, the Tenets of Osteopathic Medicine are: “(1) "e body is a unit; the person is a unit of body, mind, and spirit. (2) " e body is capable of self-regulation, self-healing, and health maintenance. (3) Structure and function are reciprocally interrelated, and (4) Rational treatment is based upon an understanding of the basic principles of body unity, self-regulation, and the interrelationship of structure and function.”,
Dr. Still strongly emphasized the concept of “holism,” in which all aspects of the human body (physical, emotional, mental, spiritual and environmental) depend on one another and work together to make up the totality of a human being. He rationalized that our body systems were self-regulated to maintain a healthy state, and the osteopathic physician must facilitate and encourage the body's natural ability to self-heal. Since our body systems collaborate to sustain our health, a change in one system can offset the function of another system. For example, lower back pain can be associated with a stomachache. By viewing the patient through these principles, treatment plans can be more tailored to every aspect of the patient’s life. .
To address neck pain, headaches, back pain, kidney stones and a variety of disorders, Dr. Still established a new skillset called Osteopathic Manipulative Treatment (OMT) in addition to establishing a guideline of osteopathic principles. OMT is a non-invasive, low-cost

and highly e&ective hands-on treatment that promotes the body’s self-healing mechanisms.5 "e modality of touch is the basis for both diagnosis and treatment during OMT./ During treatment, the simple act of laying hands on a patient signi#es trust between the patient and their physician. "is humanizing act of treatment welcomes compassion and encourages an emotional connection, regardless of language or cultural di&erences.0 "ese attributes of empathy and compassion are essential when providing an osteopathic touch and connecting with patients from every background, culture and lifestyle. Dr. Still continued to develop OMT for ameliorating various modalities addressing a wide range of issues that are now taught in osteopathic medical schools.
Osteopathic medicine recognizes that lifestyle medicine is an essential part of patient-centered care, with the ultimate goal of promoting whole-body wellness. For example, a patient with acid
reflux (gastroesophageal reflux) can receive OMT as well as lifestyle recommendations. Instead of immediately prescribing medication, DO providers take the time to discuss which foods to avoid, practical exercise routines and good sleep habits. 1 According to a survey, patients felt listened to and involved in their treatment when receiving osteopathic patient-centered care. 2 The patients appreciated the thorough assessment covering quality of life, mental health state and consideration of comorbidities. Assessing and treating patients from a holistic perspective customizes patient care and encourages patients to establish a strong relationship with their physician.
"e #rst American School of Osteopathy began on October 3, 1892 with less than 20 students ranging from ages 16 to 68.) Today, the number of osteopathic physicians in the United States is close to 149,000 and there are approximately 38,000 students enrolled in 41 osteopathic medical schools.10 "ese students receive over 200 hours of OMT practice to expand their clinical reasoning and improve their OMT skills across various ailments. Free Osteopathic Manipulative Medicine (OMM) clinics established by these Colleges of Osteopathic Medicine allow the students to provide free OMT to the local underserved population regardless of insurance status or ability to pay.11 Osteopathic medicine not only provides accessible, patient-centered care through OMM for the community, but it also utilizes OMM as a tool to connect with patients across di&erent cultures and language barriers.0
Dr. Still initially established osteopathic medicine to address the inadequacies of medicine at the time. He presented a new way of thinking, a new set of principles that considered the mind, body and spirit as a united system. Today, these principles act as the foundation for osteopathic medicine's patient-centered, holistic care.

References:
1. Lewis, John Robert. (2012). A.T. Still : From the Dry Bone to the Living Man. Blaenau Ffestiniog : Dry Bone Press. http://archive. org/details/atstillfromdrybo0000lewi
2. Se$nger, M.A., Hruby, R.J., Rogers, F.J., Willard, F.H., Licciardone, J., Jones III, J.M., and King, H.H. (2018). Foundations of Osteopathic Medicine: Philosophy, Science, Clinical Applications, and Research. 4th edition. Wolters Kluwer Health
3. American Osteopathic Association. (2024). Tenets of Osteopathic Medicine. https://osteopathic.org/about/leadership/aoa-governance-documents/tenets-of- osteopathic-medicine/
4. Hruby, R.J. (2014, March 1). Osteopathic Philosophy: Andrew Taylor Still, M.D. https://www.westernu.edu/osteopathic/about/ osteopathic-philosophy/#accordion-1- button.
5. Roberts, A., Harris, K., Outen, B., Bukvic, A., Smith, B., Schultz, A., Bergman, S., & Mondal, D. (2022). Osteopathic Manipulative Medicine: A Brief Review of the Hands-On Treatment Approaches and "eir "erapeutic Uses. Medicines (Basel, Switzerland), 9(5), 33. https://doi.org/10.3390/medicines9050033
6. Baroni, F., Ru$ni, N., D’Alessandro, G., Consorti, G., & Lunghi, C. (2021). "e role of touch in osteopathic practice: A narrative review and integrative hypothesis. Complementary therapies in clinical practice, 42, 101277. https://doi.org/10.1016/j.ctcp.2020.101277
7. "e DO Sta&. (2024, June 28). Conquering Language Barriers with the ‘ART’ of OMM. "e DO. https://thedo.osteopathic.org/ columns/conquering-language-barriers-with-the-art-of- omm/.
8. Drozek, D. (2016). Lifestyle Medicine: A New Paradigm Embedded in Osteopathic Principles. Journal of Osteopathic Medicine, 116(8), 500–501. https://doi.org/10.7556/jaoa.2016.101
9. Orrock, P. J. (2016). "e patient experience of osteopathic healthcare. Manual "erapy, 22, 131–137. https://doi. org/10.1016/j.math.2015.11.003
10. "e DO Sta&. (2023, September 7). Number of DOs and DO students has quadrupled in the past 3 decades, latest OMP Report reveals. "e DO. https://thedo.osteopathic. org/2023/09/number-of-dos-and-do-students-has-quadrupledin-the-past-3-decades-latest-omp-report-reveals/
11. "e DO Sta&. (2024, March 29). How to Create a Free OMM Clinic at Your COM. "e DO. https://thedo.osteopathic.org/ columns/how-to-create-a-free-omm-clinic-at-your-com/



Grace Denise Huizar is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2026. She is passionate about serving her community and interested in pursuing obstetrics and gynecology or pediatrics.
Arunabh Bhattacharya, PhD, is an Associate Professor at the University of the Incarnate Word School of Osteopathic Medicine. He is passionate about researching factors that in uence healthy aging.
Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma serves on the BCMS Publications Committee.

By Rita Espinoza, DrPH, MPH; Casey Perez, MS; and Anita K. Kurian, MBBS, MPH, DrPH
Many impacts have been realized and occurred since the pandemic from COVID-19, some positive (data modernization, addressing health disparities, etc.) and others not so great (increase in vaccine hesitancy). "ere has always been controversy whether children should receive their vaccinations. Some parents say yes, others are skeptical, and others refuse for various reasons. "e issue of refusing to vaccinate has been highlighted even more due to the COVID-19 pandemic and response. "ere is a large debate about vaccines and whether there should be requirements for the vaccines or should it be le! up to personal choice.
All 50 states allow exemptions from vaccinations due to medical reasons./ "irty states and Washington D.C. allow exemptions for people who have religious objections to immunizations. "irteen states allow exemptions for either religious or personal reasons (including Texas). Two states, Louisiana and Minnesota, do not specify whether
the non-medical exemption must be for religious or personal reasons. Five states do not allow any type of non-medical exemption.
Vaccine-preventable diseases (VPDs) have been around for many years. Prior to routine vaccinations, thousands of cases a&ected our community. Most have been controlled through successful vaccination campaigns reaching vaccination coverage levels of 95 percent or higher in the community. Due to the high vaccination coverage levels, most VPDs have been reduced drastically in the U.S. and in Texas, and here locally in San Antonio. Unvaccinated individuals are not the only concern. Travel is another potential source for cases from countries where these diseases are still prevalent. Unfortunately, diseases do not know boundaries and can be introduced by everyday travel.
A few individuals, unvaccinated, spanned across a large geographic area, may not make a big impact on the overall vaccination coverage level and community protection. However, when the number of indi-
viduals not vaccinated occur in a close community, then the risk for contracting these diseases increases. VPDs can occur from exposure to someone that has traveled to a country where disease is still prevalent or from a traveler visiting from these countries. "ough the important note is that once the individual becomes ill, then those around them that have not been vaccinated, for whatever reason, are at-risk. "is has been highlighted even more with the current outbreak of measles that is occurring in West Texas.) "is outbreak has expanded to 259 cases as of March 14, 2025, including 34 hospitalizations and one fatality in a school-aged child. "is outbreak has now spread to two other states, New Mexico and Oklahoma.
Vaccine hesitancy has been an issue for several years and has become an even bigger challenge. In 2012, the World Health Organization’s (WHO) Strategic Advisory Group of Experts (SAGE) on Immunizations developed a working group to address vaccine hesitancy due to the growing concerns of its e&ects on vaccine uptake. "e SAGE working group de#nes vaccine hesitancy as a ‘‘delay in acceptance or refusal of vaccines despite availability of vaccination services.’’1 "e internet is a powerful tool, which can be used to share factual information and misinformation on vaccinations.
What are some effective approaches for dealing with vaccine hesitancy?
According to Lafnizegger and Gaviria-Agudelo,, there are multiple factors that in uence whether a parent vaccinates their child. "ere is not a one-size #t to address vaccine hesitancy. Instead, the method must be tailored to the concerns of the individual/community, which means you must listen to the individuals, hear their concerns and address them.
Role of healthcare providers:
Healthcare providers remain the most trusted source about vaccines., Providers can provide unbiased, evidence-based information to parents. Printed educational handouts or videos can increase attitudes toward vaccines, but ultimately are not enough to incite change. Establishing trust and partnership with parents is key. Parents’ opinions about
vaccines are in uenced by a multitude of individual and contextual factors that need to be acknowledged and understood by providers.
Use presumptive language vs. participatory:
Using presumptive language, such as, “Baby has some shots today,” is an approach that presumes parental consent. In contrast, using a participatory approach such as, “What do you think about baby’s shots today?” shows that decision-making is shared. Researchers found that providers who elicited a participatory language had a larger proportion of parents resist vaccine recommendations than those who used a presumptive language.0 Also, the study showed that parents who initially were resistant to vaccines became more compliant when the provider continued to give recommendations. "e participatory approach is becoming more expected amongst parents. Parents are now seeking to be more active in their child’s care and decision-making.
Vaccine information provided should include the safety, e$cacy, and the range of side e&ects from mild to severe. Acknowledging concerns with empathy and regarding the parents’ questions about vaccinations will help build trust. Using scare tactics were not found to be helpful and worsened attitudes towards vaccines. It’s also important to debunk misinformation and to present the facts simply since it may be easier to accept the simple information than the myth. If, however, the parent and the provider #nd themselves in an argumentative encounter, motivational interviewing may help.,
Use motivational interviewing:
Motivational interviewing is an e&ective communication tool that can be used to address vaccine hesitancy among parents. "is interviewing technique seeks to understand existing motivations and concerns about vaccination to bring out a change “by using a supportive and nonconfrontational approach.”, Motivational interviewing is based on #ve key principles: open questioning, a$rming, re ecting, summarizing, and informing and advising.2 "is style of communication uses an empathetic approach to explore a person’s existing motivations and concerns about a behavior (like vaccination) to elicit behavior change.. "e intent is to empower the parent to accept vaccination by using a supportive and nonconfrontational approach.+

Summary
Unfortunately, no single solution to the issue of vaccine hesitancy exists and interventions that are multimodal and tailored to speci#c populations are likely to be most successful. "e starting point is establishing a strong foundation of trust and respect between the providers and their patients and families. "is will allow providers to create a safe space for parents to discuss their concerns and openly ask questions about vaccinations and, subsequently, follow their guidance. Providers should not underestimate the power of their knowledge and recommendations when addressing vaccine-hesitant parents. Below are some useful resources to get information on vaccinations and the diseases that they prevent.
Resources:
• San Antonio Metropolitan Health District Immunization Program – Local public health department that can provide information on becoming a Texas Vaccines for Children Provider (TVFC), provider education, and outreach to the community. www.SA.Gov/Directory/Departments/SAMHD/Health-Services/Immunizations
• Immunize.org - An award-winning 501(c)(3) nonpro#t organization, headquartered in Saint Paul, Minnesota. "ey work to ensure that healthcare professionals and the public are up to date on all aspects of vaccination and advocate for policies that remove barriers to vaccination.
• Centers for Disease Control and Prevention – Has information about the vaccine-preventable diseases, how to prevent and control them. www.CDC.gov
• Texas Department of State Health Services – www.DSHS.Texas. gov/Immunizations
References:
1. Texas Department of State Health Services (DSHS). https:// www.dshs.texas.gov/news-alerts/measles-outbreak-2025. Accessed on 3/14/25
2. Gagneur, A. Motivational interviewing: A powerful tool to address vaccine hesitancy. Can Commun Dis Rep 2020;46(4):93–7
3. Lafnitzegger, A., Gaviria-Agudelo, C. Vaccine Hesitancy in Pediatrics. Advances in Pediatrics 2022; 69:163–176
4. Leask, J., Kinnersley, P., Jackson, C., et al. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatr 2012; 12:154
5. McClure, C.C., Cataldi, J.R., & O’Leary, S.T. Vaccine hesitancy: where we are and where we are going. Clinical therapeutics, 2017;39(8), 1550-1562
6. National Conference of State Legislatures (2025). State Non-Medical Exemptions from School Immunization Requirements. https://www.ncsl.org/health/state-non-medical-exemptions-from-school-immunization-requirements accessed on 3/10/25
7. Opel, D.J., Taylor, J.A., Zhou, C., et al. "e relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatr. 2013; 167:1065–1071
8. SAGE Working. Report of the SAGE working group on vaccine hesitancy. Geneva: World Health Organization; 2014
9. Tuckerman, J., Kaufman, J., Danchin, M. E&ective Approaches to Combat Vaccine Hesitancy. "e Pediatric Infectious Disease Journal 2022; 41(5) e243-e245
10. WHO. Vaccine hesitancy: A growing challenge for immunization programs. https://www.who.int/news/item/18-08-2015-vaccine-hesitancy-a-growing-challenge-for-immunization-programmes. Accessed on 3/12/25

Rita Espinoza, DrPH, MPH, has served as the Chief of Epidemiology for the San Antonio Metropolitan Health District since April 2015. With over 20 years of experience in Infectious Disease Epidemiology, she has led numerous disease investigations and has responded to statewide and local public health events, such as hurricanes and disease outbreaks. She is now co-leading the O(ce of Epi Analytics & Informatics. Dr. Espinoza obtained her master’s degree of public health in epidemiology &om Tulane University and her doctoral degree in public health leadership &om the University of Illinois. She serves on the BCMS Publications Committee.

Casey Perez, MS, is an Epidemiologist at the City of San Antonio Metropolitan Health District in the O(ce of Epi Analytics & Informatics. She received a bachelor’s degree in Biology &om Texas Tech University and a master’s degree in Health and Kinesiology &om the University of Texas at San Antonio. Her work focuses on syndromic surveillance, creating public-facing data dashboards, and program evaluation.

Anita K. Kurian, MBBS, MPH, DrPH, is the Assistant Director at the San Antonio Metropolitan Health District and leads the activities of the Communicable Diseases Division, including Epidemiology, Immunizations program, STD/HIV clinic, Tuberculosis clinic and laboratory services. She has over 18 years of public health experience and previously served as the Associate Director at Tarrant County Public Health and the Chief Epidemiologist for Tarrant County where she led infectious disease outbreak investigations. She has a medical degree &om India, an MPH in Epidemiology &om Emory University and a doctoral degree in Clinical Research &om UNTHSC.
The Texas Legislature meets every odd-numbered year for 140 consecutive days and will convene again January 14, 2025. Legislators need to hear from you — their physician, medical student and alliance constituents — during the session to understand how proposed legislation can potentially impact the practice of medicine in Texas. Mark your calendar for 2025 First Tuesdays at the Capitol.
• April 1 (TMA Medical Student and Resident Month)
• May 6



Co-Authored By Eric Kala CPWA©, CIMA©, CFP©, CBEC©, AEP©, RMA©, CLU©, ChFC©, CRPS© & Dan Reinke, MBA, CIMA©, CFP©, CBEC©, ChFC©, CRPS© of Avid Wealth Partners
Are you making the most of strategies designed to lower your tax burden while building long-term wealth? Many physicians and physician practice owners overlook key opportunities that could signi#cantly reduce their taxable income. "e good news? "ere’s still time to apply two powerful strategies for the 2024 tax season — and set yourself up for success in 2025 and beyond.
If you own commercial real estate, medical o$ce buildings or rental properties, a Cost Segregation Study (CSS) can provide substantial tax deductions by accelerating depreciation. Instead of waiting decades to claim depreciation, you can front-load deductions to o&set taxable income in high-earning years.
Real estate is typically depreciated over 39 years for commercial properties and 27.5 years for residential rental properties. A Cost Segregation Study reclassi#es certain building components — such as electrical systems, ooring, cabinetry and specialized equipment — into shorter depreciation schedules of 5, 7 or 15 years instead of 27.5 or 39 years. "e result? A signi#cant upfront tax deduction that can be used to lower your taxable income immediately.
"is strategy is particularly useful if you’ve had a large income event, such as selling a practice or receiving a signi#cant bonus. Even if you’ve owned your property for years, a study can be conducted retroactively to unlock deductions from past tax years. Timing a Cost Segregation Study correctly can signi#cantly increase your tax savings.
For physician practice owners seeking aggressive tax deferral and long-term wealth accumulation, Cash Balance Plans o&er a compelling solution. "ese plans allow contributions well beyond standard 401(k) limits, reducing taxable income while rapidly growing retirement assets.
Unlike traditional retirement plans, a Cash Balance Plan allows for much higher pre-tax contributions, sometimes in the hundreds of thousands of dollars per year. Contributions are tax-deductible, signi#cantly lowering adjusted gross income (AGI), and funds grow tax-deferred, helping build substantial wealth over time.
This strategy is especially beneficial for physicians earning $400,000+ per year who have already maxed out their 401(k) and profit-sharing contributions. Cash Balance Plans must be set up alongside a 401(k) plan but can still be implemented for 2024, as long as they are established before the #nal business tax #ling deadline in 2025.
For example, a 55-year-old physician earning $900,000 annually, has already contributed the maximum $76,500 to their 401(k) and pro#t-sharing plan. By implementing a Cash Balance Plan, they could contribute a maximum additional $248,000 pre-tax, reducing their taxable income for the year. With an estimated 35 percent tax savings, this strategy provides $86,800 in tax relief annually — or $868,000 over 10 years. More importantly, it allows them to accumulate over $2.5 million in tax-deferred retirement assets, strengthening their long-term #nancial outlook.
Both Cost Segregation Studies and Cash Balance Plans provide immediate and long-term tax advantages. Cost Segregation allows for accelerated depreciation, reducing taxable income in high-earning years. Cash Balance Plans enable large pre-tax contributions, lowering AGI while growing retirement savings. "ese strategies are highly e&ective but require proper planning and execution.
If you’re interested in optimizing your tax strategy and maximizing your wealth building opportunities, reach out to Avid Wealth Partners.
Avid Wealth Partners is a Gold Member of the BCMS Circle of Friends Program. AvidForPhysicians.com
DISCLOSURE: The information in this article is for educational purposes only and should not be considered tax, legal or fnancial advice. Physicians and business owners should consult their professional advisors before making fnancial or tax decisions. Avid Wealth Partners, LLC is a Registered Investment Advisor. Advisory services are only offered to clients or prospective clients where Avid Wealth Partners and its representatives are properly licensed or exempt from licensure. Individual tax situations vary, and past performance is not indicative of future results.
With heavy hearts, we share the news of Dr. James Hadnott’s passing on January 20, 2025. He was a cherished physician, veteran, advocate, colleague and friend. We are grateful for his dedicated service with the Bexar County Medical Society throughout his career.
Dr. Hadnott became a member of the Bexar County Medical Society in 1967. "roughout his membership, he served on various committees, including the Service Bureau Board of Directors, Nominating/Constitution Bylaws Committee, Legislative and Socioeconomic Committee, and Finance Committee. He also served as Chair for the Board of Censors and Director of the BCMS Management Holding Company.
Following in the footsteps of his two physician brothers, Dr. Hadnott earned a Doctor of Medicine degree in an accelerated, three-year honors program in 1962. He then completed his residency in Obstetrics and Gynecology at the University of Texas Health Science Center at San Antonio while serving as a Major in the Texas Army Reserve. He would later serve as a full-time faculty member at UTHSCSA, and went into private practice as an OBGYN for 40 years. As a recognized leader in his profession, he served in various other roles such as Director of the City of San Antonio Health Facilities Development Corporation, President of the San Antonio Obstetrics and Gynecology Society, Treasurer of the Texas Medical Association, and more.
Bexar County Medical Society extends its deepest condolences to the Hadnott family and friends. Dr. James Hadnott leaves behind a lasting impact on both his community and colleagues. We are thankful for his lifelong commitment to exemplary medical leadership and community service.

By Jacob Hernandez
" is month’s First Tuesdays at the Capitol event saw record turnout TMA-wide for a March First Tuesdays, and Bexar County’s delegation was no exception! Many thanks to the following participants: John M. Shepherd, MD, BCMS President; Jenny Shepherd, TMAA President; Ezequiel “Zeke” Silva, MD, BCMS Immediate Past President; Jayesh Shah, MD, TMA President-Elect; Neha Shah; Sanjiv Kumar, MD; Carmen Garza, MD; Amita Kumar, MD; Lubna Naeem, MD; Antonia Helbling, MD; Gerardo Ortega, MD; Catherine Ortega; Ethan McGonagle (UTHSCSA); and Emma Tao (UTHSCSA).
Our group discussed TMA’s 2025 legislative priorities with legislators and sta& from each of the Bexar County legislative o$ces. Legislation supported by TMA includes SB 547, which would build on the framework of the 2021 Gold Card Law for helping physicians earn exemptions from onerous prior authorization requirements by adding greater transparency and accountability for insurers; SB 815 & HB 2922, which would prohibit insurers from using fully autonomous systems (i.e., augmented intelligence) to make coverage determinations; SB 922 & HB 1699, which would require that patients must receive serious and sensitive test results directly from their physician, rather than through a portal; and a provision in SB 1, the state budget for 2026-2027, that would give physicians a 10 percent increase across-theboard in Medicaid payments.
Conversely, legislation that TMA opposes includes SB 911 & HB 1756, which would allow Advanced Practice Registered Nurses (APRNs) to practice independently without oversight by a physician, thus destroying the physician-led team framework that is at the heart of medical care; SB 1102, which would allow professional midwives to administer dangerous medications during labor without any supervision; HB 845, which would allow pharmacists to test and treat for illnesses such as u or Covid, despite not having training in the practice of medicine; and SB 818 & HB 1906, which would establish a cost analysis program that would give health plans an advantage by using data supplied by health insurance companies, thus undercut physician and patient protections.


With all of this very di&erent legislation owing through o$ces and committees, we’re grateful to TMA’s Division of Public A&airs for their constant work in helping legislators and their teams understand the e&ects these bills would have on physicians and patients across the state, and glad to be able to help out once a month at First Tuesdays.
If you haven’t made it to First Tuesdays yet this year, there’s still time to get involved! You can register at https://www.texmed.org/ #rsttuesdays/ to attend the events on May 6. If you choose to travel up on May 5 and stay overnight in Austin, there is a special room rate of $259 (cuto& April 14) at the DoubleTree Suites by Hilton Hotel at 303 W. 15th St, right next door to TMA’s o$ces.
More information is available at the TMA Web page linked above, but if you have any speci#c questions, please feel free to reach out to Jacob Hernandez, BCMS Advocacy & Public Health Specialist, at jacob.hernandez@bcms.org.

























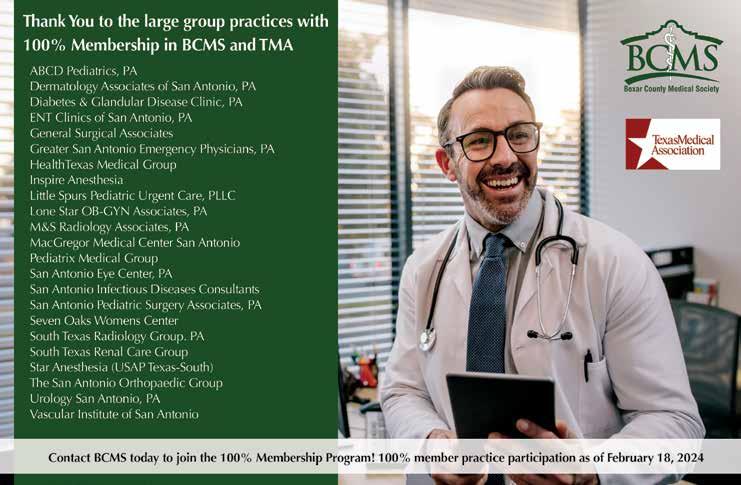

Introducing the Acura ADX, an all-new premium compact SUV that will welcome buyers to the performance brand with an engaging driving experience, a feature-rich interior and top-class cabin and cargo space that supports their active lifestyles. "e turbocharged 2025 Acura ADX brings a new gateway model to the Acura lineup, building on the incredible success of the Integra and expanding the appeal of Acura as a destination brand for a new generation of buyers. "e new ADX will begin arriving at Acura dealers in early 2025 with a price range starting in the mid-$30,000s.
• All-New 2025 Acura ADX!
• First-ever ADX, an all-new premium compact SUV, boasts youthful design, engaging driving experience and turbocharged performance to attract a new generation of buyers.
• ADX features an upscale, tech-rich interior including a 10.2-inch Acura Precision Cockpit™, 9-inch touchscreen interface with wireless Apple CarPlay and Android Auto compatibility, wireless charging pad – all standard.
• Available premium features include panoramic moonroof, ventilated front seats and 15-speaker Bang & Olufsen premium sound system.
“ "e all-new Acura ADX is an exciting new model for the Acura brand, expanding our performance SUV lineup to four exceptional models in the most popular segments,” said Mike Langel, Assistant Vice President, Acura National Sales. “ADX will hit the heart of the premium compact SUV segment, which has grown signi#cantly over the past few years.”
ADX will be o&ered in three well-equipped trims, including A-Spec and A-Spec with Advance Package, which are for buyers who desire an even sportier appearance with LED fog lamps, gloss black lower exterior trim, Gun Metallic skid garnishes front and rear, larger 19-inch wheels and A-Spec badges. Both A-Spec trims also include a panoramic moonroof and ventilated front seats. At the top of the lineup, ADX A-Spec with Advance Package receives gloss black mirrors, Berlina Black 19-inch wheels and a class-leading abundance of
premium features that include Google built in, heated steering wheel, surround-view camera system, and a powerful Bang & Olufsen premium sound system.
Acura is a leading automotive brand committed to delivering expressive styling, innovative engineering, and high-performance, all built on the brand’s Precision Cra!ed Performance DNA. "e Acura lineup consists of two sport sedans, the Integra and TLX, and three sport-utility vehicles, the RDX, MDX and all-electric ZDX. A line of high-performance Type S variants further demonstrates the virtues of Acura Precision Cra!ed Performance. All Acura vehicles sold in America are made in the U.S., using domestic and globally sourced parts.
Gunn Acura invites you to experience the Precision-Crafted Performance of the all-new 2025 Acura ADX frsthand.
Visit our location at 11911 IH-10 West, San Antonio, today! Gunn Acura is a Member of the BCMS Auto Program. GunnAcura.com | Acura.com









11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Northside Honda
9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Auto Group
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Auto Group
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson
877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
Auto Group
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
Auto Group
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200


