
Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER: Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
GRAPHIC DESIGNER: Jennifer Nelson jennifer@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE:
Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2025 SmithPrint, Inc. PRINTED IN THE USA


Most people would answer: It’s priceless. As a physician, no doubt you agree. Every life is precious.
But there is also a practical answer to this question that we all must consider. With life insurance, it’s not about the value of your life, it’s about making sure your family can carry on if you are not there to provide for them. That’s what life insurance is for, to make sure they can live every day to the fullest, so their potential is reached and the dreams you have for them are realized.
Life insurance helps ensure that your loved ones will lead their best possible lives. Every milestone they achieve will remind them of your love, and they’ll cherish your gift for a lifetime.

Their lives are too precious not to be fulfilled. Have a conversation about protecting your family’s future with one of our advisors. They can be reached by calling 800-880-8181, Monday through Friday, 8:00 AM to 5:00 PM, or scanning the QR code. You can also visit us online at tmait.org. It will be our privilege to help protect what’s priceless to you. SCAN TO CALL

John Shepherd, MD, President
Lyssa Ochoa, MD, Vice President
Jennifer R. Rushton, MD, President-Elect
Lubna Naeem, MD, Treasurer
Lauren Tarbox, MD, Secretary
Ezequiel “Zeke” Silva, III, MD, Immediate Past President
Woodson “Scott” Jones, Member
John Lim, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Saqib Z. Syed, MD, Member
Nancy Vacca, MD, Member
Col Joseph J. Hudak, MD, MMAS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School Representative
Cynthia Cantu, DO, UT Health Medical School Representative
Lori Kels, MD, UIW Medical School Representative
Ronald Rodriguez, MD, UT Health Medical School Representative
Alice Gong, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Yvonne Nino, Controller
Al Ortiz, Chief Information Officer
Brissa Vela, Chief Membership and Development Officer
Jacob Hernandez, Advocacy and Public Health
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Jennifer C. Seger MD, Chair
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. Jyothula, MD, Member
George-Thomas Martin Pugh, MD, Member
Adam Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Amith Skandhan, MD, Member
Francis Vu Tran, MD, Member
Subhashini Valavalkar, MD, Member
Louis Doucette, Consultant
Brissa Vela, Staff Liaison
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Ayomide Akinsooto, Student
Elizabeth Allen, Volunteer
Rita Espinoza, DrPH, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer


By John Shepherd, MD, President, Bexar County Medical Society
The Texas legislature’s 89th session is in full swing and in today’s political landscape, your voice is more important than ever. When it comes to shaping policies that affect our medical community and your ability to practice medicine, advocacy plays a pivotal role in the legislative process. Fortunately, advocacy isn’t reserved for experts or those in positions of power — it’s something each of us can contribute to, regardless of background or experience.
We don’t do it alone and have valuable partners in the TMA Council on Legislation (COL) and the TMA Division of Advocacy. Led by Bexar County Medical Society Immediate Past President Zeke Silva, MD, the COL, which is made up of physicians from across the state in all practice specialties, sets legislative priorities for Texas medicine, informed by input from 19 TMA councils covering various health topics. Clayton Stewart oversees the Division of Advocacy, directing the association’s legislative and political efforts, including finding bill sponsors, obtaining support for bills to be enacted or working toward the defeat of others. TEXPAC, medicine’s largest statewide political action committee, is led by TMA newcomer and PAC Director Brianna Menard who works tirelessly to elect and support medicine-friendly candidates.
During this legislative session, the top 10 priorities for medicine are grouped into three main categories: access to care, practice viability and physician autonomy.
In each session, there are providers who wish to do what physicians do without having gone to medical school. Pharmacists who wish to test and treat, advanced practice nurses who wish to practice and prescribe independently and other mid-level specialists who wish to expand what they do without physician oversight are all currently asking the legislature for expanded scope of practice. We are working


to stop that expansion and find ways to address healthcare workforce shortages in ways that ensure patients have access to physician-led care regardless of living in a metro area or in more rural parts of the state.
Fighting for increases in Medicaid reimbursement at the state level and standing against potential Medicare cuts on the federal level both aid to advance coverage for Texans. Medicare cuts and stagnant Medicaid rates continue to put financial strain on medical practices, especially in underserved or rural regions. Higher rates would support the sustainability of practices and improve the overall system by enhancing access to care for some of our most vulnerable populations.
Covid changed the way many things operate, including the use of technology to administer healthcare. Using telemedicine as a method of delivering healthcare is no longer a short-term pandemic solution but a long-term answer to expanding access to care in rural or underserved areas. Payment parity for telemedicine services is crucial to ensure that physicians are compensated at the same rates as for in-person visits. Our time and expertise should be worth the same regardless of the format.
Routine child and adult immunizations have been proven safe and effective against disease. It is imperative that we resist any efforts to roll back standards and that we defend Texas’ vaccine laws to protect public health. It is up to us to communicate the importance of basic public health principles while ensuring continued access to immunizations.
Medical liability protections are essential for attracting and retaining physicians in the state of Texas. With each new legislative session, it is necessary to fight to preserve our landmark medical liability reforms of 2003 as well as prevent any new liability risks that threaten access to care and workforce growth as well as increased litigation with unsustainable verdicts.
Prior authorization and other similar health insurance practices not only take away from direct patient care but contribute to rising healthcare costs and add to physician stress. Comprehensive prior authorization reform is needed to reduce delays in patient care and reduce overall administrative burdens on physicians.
While technology offers numerous benefits, it also carries potential drawbacks. Given the rapid advancement of artificial intelligence (AI), it is crucial that new medical technologies undergo thorough vetting by qualified physicians. The regulation of AI in healthcare should strike a balance: it should enhance and support physicians’ practices while ensuring that it does not supplant their medical expertise. Additionally, just as we have protections in place to protect patient privacy in our current practices, we must ensure that any use of AI does the same.
Addressing non-compete laws in medical practices is needed to strike a balance between the needs of the employed physician and the physician employer. It is valid that the physician acting as employer is able to protect their business interest while the employed physician may desire a change in practice.
Ensure that non-medical entities do not alter the practice methods of physicians. It is important for physicians to practice medicine with autonomy, according to their training and in a manner that best serves patients in Texas.
The physician-patient relationship is crucial, especially regarding criminalization. Texas physicians need clarity on exceptions to the state’s laws on abortion to safely treat pregnant women in crisis. This isn’t about pro-life or pro-choice; it’s about providing the best care for women in difficult, potentially life-threatening situations.
Which of these priorities for medicine resonates with you? Which one would make a real difference in your life? What story do you have to share with your legislator? Join the Bexar County family of medicine as we head to Austin for First Tuesdays at the Capitol on March 4, April 1 and May 6, 2025. Speak up about the issues that matter to you — your voice is what ensures that every Texan receives the highest standard of care, and that our profession remains strong and independent.
John Shepherd, MD, 2025 President of the Bexar County Medical Society, has been an active lobbyist for the Family of Medicine at the Texas State Capitol and has held several “Party of Medicine” events, introducing physicians on how to get involved with legislation that affects medical issues. He has been Chief of Surgery at Christus Santa Rosa Children’s Hospital, a past member of the Board of Directors of Tejas Anesthesia, and currently serves on the BCMS Legislative Committee. Dr. Shepherd served as Secretary on the BCMS Board of Directors for 2023.

& PRIVATE BANKING
As a physician you have unique needs ranging from personal to business financial services. We can seamlessly address both, providing a comprehensive banking experience that feels custom tailored to you. Our team is comprised of highly credentialed, best-in-industry experts with decades of experience. We will work with you to clear your path to any account, loan, investment or solution you require for yourself, your family and your business.
• Healthcare-Focused Expertise
• Flexible and Specialized Healthcare Financing Options
• Comprehensive Financial Services
• Personalized Solutions broadway.bank/health • (210) 764-0166

Feb. 28
Connect Over Coffee* | 10 am | Coffee + Culture
May 2
Past Presidents Lunch* | noon | TBD
May 8-10
ALLMED Conference | JW Marriott SA
October - November
Physician Family Day* | 11 am | Shepherd Ranch
December 7
Holiday Party* | evening | TBD
Advocacy
First Tuesdays at the Capitol | Austin March 4, April 1, May 6
Outreach
Hard Hats for Little Heads
Walk with a Doc weekly | 2 groups
BookShare Program
Period Project
Bimonthly
Empty Nesters - Feb, April, June, Aug, Oct, Dec Book Club - Jan, March, May, July, Sept, Nov
Pop-Up
Lunch with Littles, Sips & Dips, Supper Club, Medicine & Mahjong, Game Night
*general membership meeting
Please join the BCMS Alliance for fun and fellowship in 2025!

Earn free online Continuing Medical Education (CME) credits developed by the Texas Department of State Health Services and physician experts on Alzheimer’s disease and related dementias. These courses will keep you up to date on the latest validated assessment and screening tools, help you direct patients to community resources, and reinforce your role in helping patients and their families manage symptoms throughout the disease process.
Learn more at dshs.texas.gov/alzheimers-disease/provider
Supporting a physician spouse can be both a rewarding and challenging journey. From offering emotional support during tough times to celebrating their achievements, spouses play a crucial role in maintaining a balanced and fulfilling life for their partners, who face demanding schedules and high-stress environments.
We asked a few Bexar County Medical Society Alliance members to share their personal stories with us and discovered that while everyone’s medical journey may lead them down different paths, spouses provide a stable foundation for their family that helps physicians thrive both personally and professionally.
By Danielle Henkes
When our daughter Nichole was 7, she declared she was going to be a doctor, just like her daddy. It wasn’t an unusual declaration — what medical family hasn’t had a kid donning their parent’s white coat and listening to hearts with the stethoscope or peering at slides under the microscope (the pathologist version).
A mixed media artist, we thought Nichole may opt for artistic pursuits, but in high school it became apparent she was serious about medicine. David was delighted, but eager that she fully grasp the long road, intensity and sacrifice that would be required. He hatched a “great plan” — have her shadow friends who were in a specialty she was sure to find the unappealing — gastroenterology. The result? She loved it. The gastroenterologists were top of their fields and encouraging mentors, and the experience resulted in years of published research, continued close relationships and a lasting fascination with gastroenterology.
At Baylor University, Nichole thrived, and met the love of her life, Alex. After graduation, she interviewed at medical schools statewide, ultimately deciding that UT Health Long School of Medicine in SA would give her the family support she needed to fully give her all to medical school. After a whirlwind of college graduation, moving, adoption of a kitten and a white coat ceremony with dad, Nichole’s official medical journey began. We learned to be flexible, available and have no expectations of spending time with her. Both David and I felt such support from our BCMS/BCMSA and TMA/TMAA friends during this time, whether it was commiserating as parents of kids pursuing medicine, physicians suggesting program possibilities, young physician families providing insight into the new application process or realtors helping us purchase and sell our student condo.
Newly engaged to Alex, with interviews at top residency programs nationwide, we sensed that “our baby” would be headed out of state.
Our hearts hurt a little at the idea of her moving far away from us even as we joined her in feeling great pride in her acceptance to the internal medicine program at Mayo Clinic Florida. As medical school wound down for Nichole, we helped plan her wedding, David “hooded” her at graduation and we loaded up two condos into a huge U-Haul and drove them to Jacksonville.

Now, as Nichole and Alex face another crossroads together — choosing a gastroenterology fellowship program — they know that we, as well as Nichole’s brother, Daniel, and his wife, Malinda, are here to support them in any way they need. As long as it doesn’t involve a U-Haul …
Danielle Henkes is a Past President of the BCMS Alliance and currently serves on the 2025 Steering Committee. David Henkes, MD, a practicing pathologist, is a Past President of BCMS, past chair of the TMA Board of Trustees and 2025 recipient of the BCMS Golden Aesculapius award. Dr. Nichole Henkes-Pathos is an internal medicine resident with Mayo Clinic Florida.
By Taylor Frantz, RDN, LD
I met Garrett when he had just started his second year of medical school. Within weeks he was starting to prepare for Step One, which meant nonstop studying — not the best time to start a new romance. He soon started using my townhouse as his quiet study location, which morphed into him living there.
When dating someone in medical school and residency, the demands on their time are immense, with long hours of studying, clinical rotations and exams, leaving very little room for personal life. When you do get time together, it often feels like you’re trying to squeeze in quality moments during tiny windows of free time. These moments might not always be spontaneous dates or weekend getaways, but instead short, meaningful conversations between study sessions or a quick dinner before diving back into studying. Years later, we still have a deep appreciation for even the smallest stolen moments together.
Residency brought us our first grand adventure with a move from downtown Phoenix to small town central Texas. As I look back on residency with rose-colored glasses, it was a time of growth, both individually and as a couple. I enjoyed joining the medical alliance and being a part of a community of medical transplants in the same stage of life. After residency, we took off on another adventure, this time to a bigger city. Having such a positive experience with the medical alliance during residency, I immediately sought out the Bexar County Medical
Society Alliance where I was able to gain friendships and support.

I view being married to medicine as a team sport. Emergency medicine schedules can be brutal with switching from days to nights, shift schedule inflexibility, and sometimes emotional tolls that can linger longer than we’d all like to admit. As a family, we have learned to adjust and adapt to a lifestyle that often looks and feels different than our neighbors. That said, I am so incredibly proud of my husband and I couldn’t imagine a life different than the one I have from being married to medicine.
Taylor Frantz, RDN, LD, is a registered dietitian and served as President, Membership VP and Events VP for the BCMS Alliance. Garrett Frantz, MD, practices emergency medicine.
By Virginia Profenna
I remember the night we were sitting at the dinner table with my husband and 1-year-old son in Brugnera, Italy. It was March 1999 and we had been stationed at Aviano Air Base for a year and a half. My husband, Len, was working as an internal medicine physician.
That night, there was a persistent rumble throughout dinner. Scores of U.S. and NATO countries’ aircraft had been staging for weeks at Aviano, and although we couldn’t see anything, we could tell something was up. President Clinton’s deadline to Slobodan Milosevic had passed, and he had refused to negotiate, prompting NATO to pursue military action in defense of Kosovo.
The next night, we drove to the base and parked in front of the flight line to watch the fighter jets and stealth aircraft take off. This was the night that Len knew he needed to stay in the military. He asked
me what I thought. I wasn’t sure what that would mean for us or for our family, but after lots of conversations, we were aligned. He would switch to aerospace medicine, which opened our lives to a continuous cycle of moving, deployments and putting service above self.
He was deployed to Kuwait when I was four-and-a-half months pregnant, with a 2-year-old and no family to support me. I quickly learned to lean on the support of the military community and bond with women in the same circumstances — and, of course, my mother got a lot of frequent flyer miles! We had another child in Boston, moving when I was seven months pregnant, and the kids grew up in Germany and Italy.
Through 22 years in the military, I always knew he was making a difference — helping to make the world a better place, preventing illness and “stomping out disease” one patient at a time. And back at home, I was the one who was making his world a better place, raising our children and holding down our fort. Maybe I wasn’t saving as many lives as him, but my strength and support helped him accomplish his mission as a military physician.

Virginia Profenna served as Treasurer, Programs VP and Membership VP for the BCMS Alliance. Colonel (Ret.) Leonardo Profenna, MD, practices hyperbaric medicine.
By Victoria Kohler-Webb, BBA, MS
How did we become part of the family of medicine? We are grateful to say it has been an exciting road and the opportunity of a lifetime. Ben and I are both Aggies and after four years studying Biology and as a member of the Corps of Cadets, Ben began those medical school interviews that everyone remembers so well. We agreed on UT Houston! I finished graduate school in marketing and statistics at A&M and landed my job in Houston, which meant I could both financially support Ben and I through medical school and also continue to climb the career ladder.
We both loved the medical school experience! It was a chance to keep that college kid feeling and we really enjoyed getting together with the other students and residents. Attending physicians were tough but mostly kind and took us all out to dinners and parties at their houses.
Then ENT Residency! The surgical subspecialties work some serious hours, and many times I left dinner plated in the refrigerator. I knew he came home at some point only because the plate was empty. However, Ben always knew that every day he was making a difference and was one day closer to achieving his dream.
Fast forward to San Antonio and joining his practice, Alamo ENT, along with his partners that we feel blessed to know as friends. I found my home at the Bexar County Medical Society Alliance and have never looked back. The Society and Alliance have provided us close family friendships, meaningful professional networking opportunities, and actively works to protect our livelihood as a physician fam-
By Neha Shah, MPT
After marrying Jayesh (Jay) in May 1993 in India, he was set to begin his first year of residency in New York in June, while I was preparing for my physical therapy board exam. I was fortunate to secure a full-time PT job at the same hospital where Jay was doing his residency. As newlyweds, I hoped to spend more time together, but his demanding schedule meant we only saw each other occasionally during lunch or dinner and on weekends when he was not on call. I knew he was working tirelessly, adapting to a new medical system and culture.
In 1996, after three years of residency, we moved to Uvalde, Texas, to start Jay's first internal medicine private practice. I became the office manager and, together, we learned the ins and outs of coding, billing and practice management. We attended TrailBlazer (Medicare) workshops and sought guidance from local doctors to ensure our practice’s success.
In 1999, we relocated to San Antonio with our two young children. As Jay’s wound care practice grew, I attended practice management workshops and webinars offered by the Medical Office Managers Association (SAMM) and Texas Medical Association (TMA), and most of these meetings were held locally at the Bexar County Medical Society (BCMS) office. The BCMS Alliance has always been a great resource for physicians and their spouses, helping us understand and navigate the challenges of balancing work, family and personal life.
With Jay working long hours from 7 a.m. to 7 p.m., I managed our home, children and office duties. Our shared trust and goals allowed
ily through their work advocating for doctors at the State Capitol. Now we have our own future doctor to educate. Our son, Luke, shadows Ben in the OR and cannot wait to join the ranks of medical students who choose this path.

Our Alliance is a blessing to our lives and I am so proud to be a member and continue to serve and learn from such dynamic leaders.
Victoria Kohler-Webb, BBA, MS Marketing Statistics, is a BCMSA Past President. She and Ben, an ENT/Head & Neck Surgeon, are proud Aggies and parents to Luke, 15, and four rescue dogs.

Jay to focus on his patients and his extensive involvement in his specialty as well as in organized medicine, knowing I had everything else in hand. I am grateful to God for placing me alongside Jay, as his dedication inspires me to live purposefully.
Becoming a physician is a monumental journey, and I am incredibly proud of our daughter, who is following her father’s footsteps. Despite the challenges, she has our unwavering support as she works toward success in her own medical career.
Neha Shah, MPT, is a lymphedema and cancer rehab therapist, longstanding member of the BCMS Alliance, and serves on the 2025 BCMS Alliance Steering Committee. Jayesh B. Shah, MD, is an internist and wound care specialist, Past President of BCMS and TMA President-Elect.
By Jenny Shepherd
My mother told me not to marry a doctor because as a nurse with a 50-year career, she knew from a different perspective what we all know … medicine is a uniquely demanding profession and as physician spouses, there are equally unique demands placed on us. Despite that, there is no better place to be than in the family of medicine.
John and I met in a stuck elevator on his first day of internship at William Beaumont Army Medical Center in El Paso, Texas — a place that seemed foreign to two Midwesterners. I exited the elevator having not shared a word with him and began my first day by proclaiming, “I just met the man I’m going to marry; he just doesn’t know it yet.” And so began a 37-year love affair with medicine and the man who practices it.
As 20-somethings, we couldn’t possibly imagine how medicine would shape our lives. From the beginning as a Special Operations Aviation flight surgeon and a Department of Defense audiologist, we found ways to weave our love of service to others together. This commitment to service didn’t end with the military; it evolved into a lifelong dedication to medicine and public health.
Despite the complexities of a medical career and family life, we have always remained focused on the impact we could make — whether through patient care, community outreach or advocacy at the Capitol. Thankfully, together we forged a path that not only strengthened our bond but also allowed us to contribute meaningfully to medicine, reinforcing our belief that true fulfillment comes from lifting others up and serving with purpose.
So, here’s to my mother, who once advised me not to marry a doctor — you were right; it hasn’t always been easy. On the other hand, this journey has led me to a life far richer and more fulfilling than I could ever have imagined and has left me feeling so grateful to celebrate Doctors’ Day.

Jenny Shepherd is the TMA Alliance President and First Tuesdays at the Capitol Chair, while her husband, Dr. John Shepherd, University Hospital pediatric anesthesiologist, is the BCMS President and the TEXPAC Candidate Evaluation Chair. They currently serve together on both the BCMS Legislative Council and the TEXPAC Executive Board.

By Izza Imran
As a first-year medical student at the University of the Incarnate Word, I often find myself reflecting on the immense legacy I am privileged to carry forward. Medicine is more than a career in my family — it’s a calling that has been passed down for four generations, each contributing uniquely to the tapestry of our shared history in healthcare.
The story begins with my paternal great-grandfather, Abdul Ghani, who practiced medicine in rural Punjab at the end of the 19th century. With no formal medical school training, he practiced a traditional form of medicine in Pakistan known as hikmat, relying on natural remedies to treat ailments like malaria, typhoid and dysentery. His work was deeply rooted in the needs of his community, a legacy of care that has endured through the generations.
My paternal grandfather, Dr. Mohammad Bashir, took this legacy further by pursuing formal training in England, specializing in neonatology. He was at the forefront of an era when incubators were just beginning to revolutionize the care of premature infants. After years of practice in England, he returned to Pakistan, dedicating 25 years to saving the lives of the tiniest and most vulnerable patients.

My parents, Dr. Naser Imran and Dr. Lubna Imran, continued this tradition of excellence. Both graduates of Dow Medical College in Karachi, Pakistan, they embarked on a remarkable journey together. After medical school, they moved to Ireland, where my mother chose to set aside her career as a gynecologist to raise my siblings and me. My father pursued further training in the United States and is now a practicing cardiac electrophysiologist. Among his siblings, the love for medicine remains strong, with his sister specializing in endocrinology and his brother practicing internal medicine in the UK. Medicine, quite literally, runs in our blood.
Growing up surrounded by physicians was both inspiring and, at times, daunting. Dinner table conversations often involved discussions of complex cases or medical breakthroughs. I absorbed not only
their knowledge but also their passion and commitment to healing. Yet, the weight of living up to such a storied legacy was undeniable. As I navigate my first year of medical school, I am deeply aware that I am standing on the shoulders of giants. Each generation has faced its unique challenges and opportunities — my great-grandfather’s reliance on traditional remedies, my grandfather’s adoption of emerging technology, and my parents’ international journey to advance their careers. These stories inspire me to embrace the complexities of modern medicine with the same courage and adaptability they demonstrated.

Being a fourth-generation physician is both an honor and a responsibility. It’s a reminder of where I come from and a motivation to contribute to this legacy of healing in my own way. As I learn the art and science of medicine, I carry with me not only the knowledge and values imparted by my family but also the determination to make my own mark in this noble profession.

11 days after appendectomy, tests for acute abdominal pain revealed a
left inside the patient.
Surgical miscounts are considered never events because they are usually preventable by following established procedures.
ProAssurance offers risk assessments designed to help practices minimize errors by establishing and evaluating safety procedures and communication protocols.
With reliable procedures in place, our insureds are more likely to reduce errors in their medical practice, avoid claims, and make claims more defensible if they do occur.


By Trisha Doucette
Meet two talented physician artists with distinct styles and preferences:
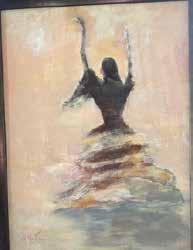
Dr. Rodolfo “Rudy” Molina is primarily a portrait artist who has worked in pencil and pastels but prefers the immediacy and vibrancy of acrylics. He excels in capturing the essence of his subjects with bold strokes and dynamic colors. His current series includes expressive and spontaneous works that convey a sense of movement.
On the other hand, Dr. Miguel A. Vazquez works with multiple mediums, where each project is a labor of love that takes hours to complete. He enjoys the intricate process of creating rich, textured pieces that tell a story. The time invested in each artwork allows for deep exploration and experimentation, resulting in captivating creations.
As a young boy, Dr. Rodolfo “Rudy” Molina had a natural talent for drawing — and a passion that stemmed from the excitement he felt when he would not just see, but study paintings he would find in books and magazines. “As a child, I drew with my pencil. We didn’t have the means to buy artist paints or canvases; however, on occasion I would use the school’s crayons,” recalled Dr. Molina.
“I must have been 8-years-old when I informed my father that I was going to pursue a career in art ‘when I grew up.’ He gave me a stern look and then said in a compassionate way that I should pursue a career in something where I would not have a boss — where I could be my own boss. I hadn’t a clue of what that could be until much later; but my father was, and in memory continues to be, my hero. And with that piece of advice, I pushed out the thought of ever becoming a professional artist,” he shared.
Fast forward to his first day of 10th-grade biology class when Dr. Molina remembers overhearing two students telling each other their ambitions of becoming medical doctors like their fathers. “I thought to myself, ‘yes, of course they will become doctors just like their fathers.’ Mr. Koepke, our instructor, sat us in alphabetical order, and then stated that everyone would be changing seats after each test. The student with the best score would sit in the front row chair designated as number one and the student with the worst score would be seated in the back far-left corner chair. After the first test, I found myself sitting in the first chair and, as I looked back at the two students who I felt sure would become doctors, well, they were in the middle of the class. It was an epiphany for me. I was smart and I could become a doctor. I’ve never regretted that choice. It is, in my opinion, the most noble of all professions. Oh, I remained in the first chair throughout the school year.”
A childhood interest in geology grew into a passion for paleontology as an adult, and Dr. Molina spent more than a decade doing weekend digs around the U.S. and Mexico. But art remained a priority as both an avid art collector and an artist. His says his collection spans from impressionism, both early and modern, to abstract expressionism, and he is inspired by them all.
His personal paintings have ranged in subject matter from landscapes to portraits, often painting his patients. “By far, I have done more portraits. For me, people are much more interesting. Whereas a landscape may, and often does, capture the beauty of nature, capturing the complexities of people is much more challenging and rewarding when it is done. I am currently trying to push a style of art that portrays movement,” explained Dr. Molina. “I love painting with acrylics
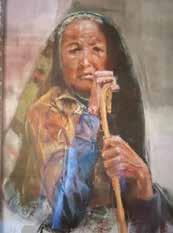
because they dry quickly and suit my style. However, I must admit that my good friend Ramon Kelly, a professional artist from Denver, prefers my pastels. When he reviewed my work, he particularly liked my pastel of a Native American holding a cane.”
As a Rheumatology Specialist with more than 49 years of experience, Dr. Molina’s career, talent and dedication to his art are inspiring. “I have many interests and hobbies: painting, paleontology, writing (yes, I finally published my first novel — The Society of Angels: A Nephilim Conspiracy — and I am working on my third book on the same subject, to be a trilogy), traveling, and having a good conversation. If you have a passion for something, you will find a way to pursue it. Motivation is fueled by passion.”
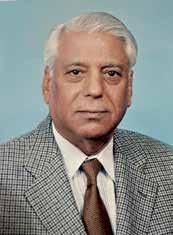
Rodolfo (Rudy) Molina, MD, FACP, MACR, was the recipient of a U.S. Air Force Scholarship, and during active duty, he was Chief and Program Director for rheumatology in a pilot program with Walter Reed Army Medical Center. Dr. Molina is retired from Arthritis Associates in San Antonio, a former member of the Bexar County Socioeconomic and Legislative Committee and PastPresident of the Bexar County Medical Society.

With a career in Family Medicine spanning 45 years, Dr. Miguel Vazquez said, “Being an artist is not what I imagined I would be doing at this juncture in life.” However, he eloquently added, “I will say that any doctor would make a good artist. To be described as a ‘good doctor’ means one should have a healthy dose of empathy, which leads to a good understanding or connection with the patient. Artists, too, seek to make an emotional connection with their work. I appreciate it when someone tells me they like my art, but I am very grateful when they say nothing at all and become emotional with the work.”
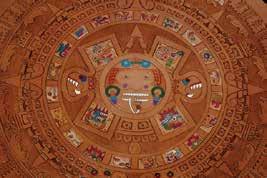
Art did not factor in his childhood, occupied by sports and academics. Medical school, residency, a medical practice and raising a family followed. “As each of the kids ventured from the nest, this gave me a little time to explore. I dusted off some leather tools and completed my first piece … the Aztec calendar. I like detailed graphics, so 30 hours later this worked out for me,” he shared.
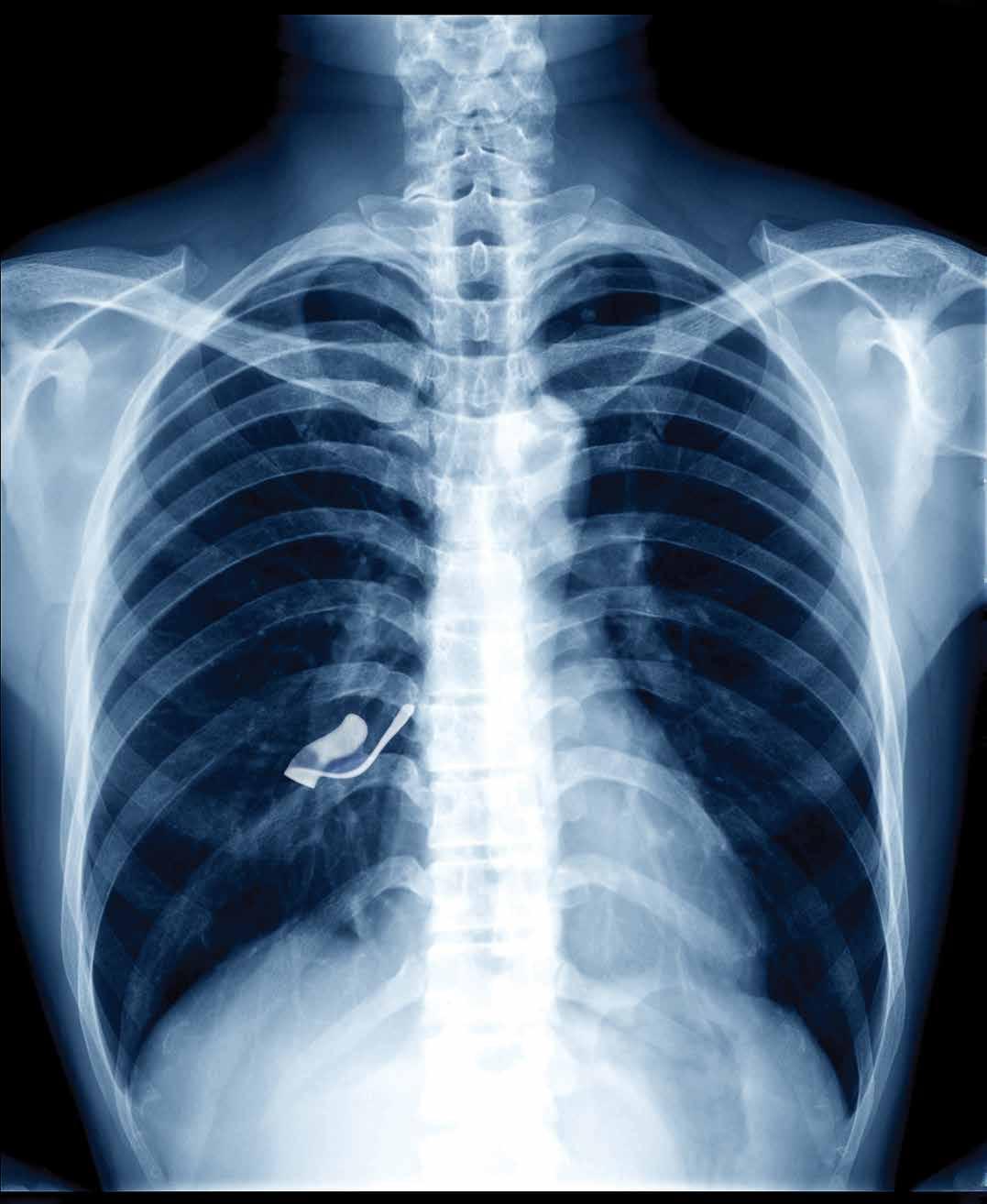
But ultimately, Dr. Vazquez’s interests lie in realism and anatomy, being quick to point out: “There is plenty of art all around us in the medical field. Radiology tends to lead the field in this respect with its various images in X-ray, CT, MRIs and ultrasounds. The hidden world under the microscope reveals imageries that appear whimsical, imaginary, yet beautiful.” His artistic themes gradually evolved into “fanciful anatomically correct hearts, lungs and kidneys. I was pleasantly surprised many people liked this type of art as it relates to them personally through a past experience with their own or a family member’s illness.”
Creative experimentation and various art workshops led to work in other mediums. “I then went to drawing, which included charcoal, pastel and colored pencil. There was a smooth transition from leather carving to linocut relief printing. Printing then led me to painting, mostly in acrylics. Each medium requires a learning curve, and I am still very much on that arc. I am in a painting phase presently, but my favorite medium remains the leather carving.”
Perhaps the most dramatic medium in his creative trajectory can be found in his Swarovski crystal-embellished skulls and skeletons, all striking and whimsical pieces. Drawing inspiration from cultural remembrance celebrations, Dr. Vazquez credits the intricately beaded art of the Huichol, as well as the funerary customs of other indigenous peoples of Mexico. While his initial muse remains, his life-sized and crystalized human skeleton, affectionately named Starletta, dazzles. “It took 420 hours to encrust more than 50,000 crystals, one by one, onto the skeleton. I then created a toddler for Starletta and her name is Celeste. One or both have been on view at the UT Health Science Center Library and the UTMB Medical Museum. I’d like to see these two travel to other medical schools/venues as well.”
Carving out more than 400 hours in addition to a work schedule can seem daunting. Dr. Vazquez explains that time is a resource that can be limiting, but medical professionals are adept at managing it as part of their learning process. The key question becomes how one uses the time, as we constantly make choices.
Dr. Vazquez also advises that while some may feel they lack creativity, everyone has an innate sense of what they like or dislike when they see an image or art piece. Remember, as he said, if one has empathy, one has the capability of being artistic.
“There is the practice of medicine and the art of medicine. I’m happy to have dipped my toes in both warm bowls.”
Miguel A. Vazquez, MD, began his practice in family medicine with obstetrics in 1984, had a private solo practice for 20 years, and then worked in various group practices. Dr. Vazquez has served as medical director for several local companies, and most recently as medical director for BCBS in their medical fraud unit. Dr. Vazquez is a member of the Bexar County Medical Society. His art can be viewed at IStudio393.com.


By Alvin Marx, MD, MBA, Inventor
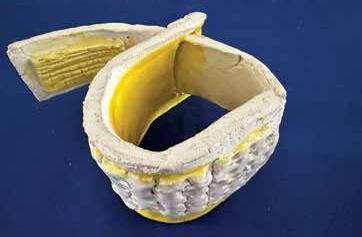
Inventing has been in my blood ever since experimenting with a chemistry set in the basement of my home as a youngster. Allin-all, I have received 22 U.S. Patents for my inventions. The big breakthrough as an inventor came with the Ace Tennis Elbow Brace. After personally suffering from a chronic case of tennis elbow, with little relief from available treatment modalities, I explored existing overthe-counter remedies, especially the brace. In general, the braces were either too soft or too rigid. Why not develop a brace that was both — i.e. a semi-rigid elbow brace? After several iterations, a new tennis elbow brace was created. Initially, Johnson & Johnson (J&J) licensed and marketed it as their elbow brace. Unfortunately, they closed their sport medical division. Becton Dickinson (BD) subsequently bought and licensed the brace. The Ace Elbow Brace sold over 1,200,000 units, worldwide.

Hypertension is a leading cause of morbidity and mortality, particularly of poorly controlled or undiagnosed high blood pressure. Recently I came up with the idea of partially blocking inspiration to lower blood pressure. I came across a controlled study in a complimentary medical journal concluding that pulmonary function can be improved by partially blocking inhalation for a few minutes, twice daily. A second study in the American Heart Journal concluded that partially restricting inhalation lowers blood pressure in males. More broadly, I thought this method could also help lower blood pressure in a safe, economical way, as a primary treatment in mild, often intermittent cases, as well as an adjunct for medically treated hypertensive patients. For further clarification, I explored ChatGPT with about 80 questions and it basically confirmed my ideas: partially blocking inhalation lowers intrathoracic pressure. This in turn lowers venous pressure resulting in lower arterial blood pressure. This information prompted a bright idea: I asked a prototype model-maker I have worked with on previous projects to build the Mini Inhaler-set of tubes, with progressive increase in partial resistance openings, to be inhaled through. When personally inhaling through these partially-inspiration-resisting tubes, I have lowered my baseline blood pressure to below 120 over 70. This patent pending device may be instrumental in improving blood pressure control in treated as well as currently undiagnosed cases of hypertension. It can take multiple attempts to bring an invention to market. While I am currently engaged with a particular medical equipment company, trying to license or sell this device, I welcome any suggestions for other connections to make this product available for use.

The elbow brace project grew out of my earlier concept for a vital sign measuring device that automatically measures blood pressure, respiratory rate and pulse. The blood pressure cuff of the vital sign device had a semi-rigid backing so that it would be easy for patient application.
My cousin and her engineer husband agreed to make the original elbow brace prototypes. I approached both BD and J&J to license the elbow brace. Both companies wanted it. J&J licensed it first and six months later gave it back to me. BD said they were still interested. BD subsequently licensed it for 20 years. An idea for a new wrist brace followed. A friend’s daughter, a high-school gymnast, thought the wrist brace was amazingly effective in preventing her gymnastic wrist sprains. When BD did not want to license the wrist brace, I licensed it to a smaller company. They never produced it, unfortunately.
I patented an IV fluid regulator that calculated the volume of drops by calculating three-dimensional measurements of the drop. After several discussions, a company in Chicago asked me to come visit them in a snowstorm, only to tell me they weren’t interested.
The iDropper™, an electromechanical eyedrop delivery system, is a more recent invention, developed to an almost pre-production stage. My wife thinks it’s the next best thing to sliced bread. I had this bright idea when watching an elderly family member try unsuccessfully to mechanically administer eye drops for his glaucoma. He always deferred to a younger person to do the job. This device blocks the automatic and interfering eye-blink reflex, occurring when administering eyedrops. It does this by spreading and holding the lids open. It also introduces an easily operated lid spreader and electronic drop release button. For patients with fine motor coordination issues, eye-drop administration is often unsuccessful and results in poor compliance. This product was granted a National Institutes of Health (NIH) grant, which was used to further develop this product. A national medical equipment company was initially interested, but didn’t follow through with a license or sale agreement.

Recent developments include a topical preparation with high dose magnesium sulfate that helps reduce arthritis pain. A cousin, who has a torn ACL and resultant knee osteoarthritis, used it with considerable pain relief for years. It was patented and I was unable to license it. Two other topical preparations I developed include a higher dose zinc ointment, and an ointment with high dose lactic acid. I have found both of these preparations effective for relief of joint pain. For now, I have put a hold on further development of these topical preparations.
Most recently, in this nutraceutical era, I learned of the healing properties of lemon juice. A wound registered nurse told me lemons will help in weight loss as well as wound healing. I began drinking Stevia-sweetened lemonade amounting to the juice of two small lemons daily. With this regimen, I have lost 20 pounds, and my fasting blood sugar is down to 85 and total cholesterol to 177. Food patents are difficult to obtain, so I decided not to patent my recipe. If I were younger, I may have further developed it.
Besides the challenges and expenses of being an inventor, there are fringe benefits. Inventions facilitated obtaining pathology and medical community positions I desired and enjoyed. It also led to a part time job as an officer in an auto-crash dummy development company. I was President of the Rochester (NY) Pathology Club. In retirement, I became President of Alamo Inventors, the San Antonio inventors’ organization.
In conclusion, invention is a form of imagination. It can bring the world, including patient healthcare, to a better place. While challenging and at times discouraging, invention can be a driving force in bringing our civilization forward. To quote Albert Einstein: “Imagination is more important than knowledge. For while knowledge defines all we currently know and understand, imagination points to all we might yet discover and create.”
Alvin J. Marx, MD, MBA, is a retired, board-certified pathologist with 39 years of experience. Initially, he served as a hospital pathologist, doing both anatomical and clinical lab work. For the last 23 years, he served as director of several community hospital labs, the last seven years of which were done in Bexar County. Dr. Marx has been a member of the Bexar County Medical Society since 1992.

By Gabriella Bradberry
Since the dawn of time, mankind has foraged for new innovations to improve quality of life. The pursuit of discovery has brought forth medical advancements from hand washing, medications, vaccinations and beyond, all to help provide patients live longer, healthier lives. Here are a few medical innovations that were developed in our very own city of San Antonio, Texas.
Albert P. Shepherd Jr., PhD, inventor, entrepreneur and late professor at the University of Texas Health and Science Center at San Antonio physiology department, founded A-Vox Systems, Inc in 1976. He later invented and dispersed the AVOXimeter 1000E and the AVOXimeter 4000, microcomputer-based oximeters designed to outperform and overcome limitations of earlier whole-blood oximeters.
The AVOXimeter 1000E is the most widely used oximeter, used in cardiac catheterization laboratories across hospitals in the United States. This AVOXimeter measures both total hemoglobin concentration and oxyhemoglobin fraction, then automatically computes the oxygen concentration.
The AVOXimeter 4000 is the first and only co-oximeter that measured the four species of hemoglobin without rupturing the red blood cells. The battery-operated desktop whole blood oximeter automatically calculates the oxygen content, percent saturation and oxygen carrying capacity of the blood samples.
Jean X. Jiang, PhD, with UT Health San Antonio, has pioneered research for potential cancer and spinal cord injury therapeutics via antibodies. The initial discovery is based on Jiang’s research on proteins known as “connexins,” the “hemichannels” they form, and their roles in the pathological processes in neuronal and skeletal tissues. This research led to the possibility of creating custom antibodies to impact the activity of connexin hemichannels.
In 2017, UT Health San Antonio entered a licensing agreement with the life sciences company, AlaMab Therapeutics Inc., to develop first-in-class antibody drugs using custom antibodies created by the Jiang laboratory. One of the “...antibody therapeutics targets neuro-inflammatory injuries such as spinal cord injury,” while the other is for “... treatment of breast cancer metastasis and osteosarcoma…,” a bone cancer. A clinical trial for these antibodies has been ongoing as of 2022, and Dr. Jiang’s team is working to develop new therapeutics.
Jean X. Jiang, PhD, was inducted into the National Academy of Inventors in 2023 for her research and antibody therapeutics and demonstrating the spirit of innovation.
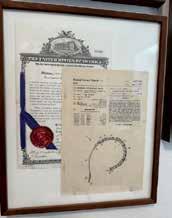
Another San Antonio innovator inducted into the National Academy of Inventors is Julio C. Palmaz, MD, who was honored for his invention of the Palmaz Stent, patented in 1988. The Palmaz Stent is the first vascular stent and “...changed the worldwide standard of care in cardiology and peripheral vascular medicine.”
The Palmaz Stent is a stainless-steel mesh tube that is “...placed into a narrowed pulmonary artery and expanded to widen it”, permanently staying in the blood vessel to reduce how hard the blood works to move blood to the lungs.
Dr. Palmez’s creation has brought relief to over a million people who suffered from chest pain and heart attacks. His work is commemorated as one of the “Ten Patents that Changed the World,” and his early stents are on display at the Smithsonian.
Another medical advancement created in San Antonio is a growth-sparing spine deformity treatment, known as the Vertical Expandable Prosthetic Titanium Rib (VEPTR). The titanium rib was invented by Robert M. Campbell Jr., MD, of University of Texas Health Science Center and the Thoracic Institute at CHRISTUS Santa Rosa Children’s Hospital, a physician who originally began his upper education as an engineering student. Dr. Campbell’s work in spine deformity treatment would save the lives of hundreds of infants and children.
Campbell’s road to innovation began in 1987, where staff physician at the Thoracic Institute and professor at the Health Science Center, Melvin D. Smith, MD, approached Dr. Campbell with X-rays of an infant born without a chest wall. Together, the doctors were able to create an artificial chest wall, and two years later, Dr. Campbell developed the titanium rib for the same child.
The titanium rib is made of a lightweight titanium that does not interfere with MRIs and curves like a ribcage. It has holes to allow surgeons to expand the device every six months in outpatient surgery.3 It can be implanted as young as 6 months of age and in teenagers until they meet skeletal maturity, and can be left in after maturity if they continue to successfully function.
After the success of this development and approval from the FDA, Drs. Campbell and Smith continued to develop new operations utilizing the titanium rib and traveled the world to share their techniques.

Gabriella Bradberry is the Admin/Communications Specialist for the Bexar County Medical Society.

By Trisha Doucette
In addition to their clinical responsibilities, physicians are passionate educators, many committed to shaping the next generation of medical professionals by integrating real-world clinical experiences into their teaching. We asked Charles W. Randall, MD, CEO and Founder of Gastroenterology Research of America as well as a Clinical Professor of Medicine at the University of Texas Health Science Center San Antonio, to share his perspective on how playing a dual role as a practitioner and educator allows medical students to bridge the gap between theory and practice, ensuring that students receive a well-rounded and practical medical education.
Following the completion of his fellowship training, Dr. Randall returned to his hometown of San Antonio. He has since enjoyed what he refers to as a hybrid practice, balancing his roles as a partner in the Gastroenterology Clinic of San Antonio and as a clinical professor of medicine at the University of Texas San Antonio.
Dr. Randall teaches medical students, residents and gastroenterology fellows in both clinical G.I. medicine and clinical G.I. research. His curriculum covers the fundamentals of conducting clinical trials and writing scientific papers. The clinic boasts one of the 10 largest inflammatory bowel disease research centers in the United States, with five residents and three students currently working at the facility.
With approximately 30 years of experience, Dr. Randall dedicates about 60 percent of his time to clinical medicine and 40 percent to academic pursuits, including teaching, research and invited lectures. He finds teaching fulfilling, saying, “I have always felt it is a duty for physicians to pass on their knowledge of how to care for patients, teaching them the art of medicine in addition to the science of medicine as well, and how to pursue an idea and develop it into a clinical trial to hopefully find a solution that will help those inflicted with certain conditions.” Despite being on the clinical faculty and not the full-time faculty, Dr. Randall is not compensated by the university for his teaching efforts.
Dr. Randall’s education was rooted in traditional academic programs, where many physicians pursued full-time academic careers. This background has shaped his approach to practice, which mirrors that of an academic physician. As a tertiary referral center for inflammatory
bowel disease, functional disorders and esophageal diseases, Dr. Randall maintains an academic practice style while seeing patients daily. He emphasizes the importance of developing close, positive relationships with patients, sharing, “One of my phrases that I tell students and trainees is that we cannot cure everyone, but we can certainly do our best to heal everyone.”
Over the years, Dr. Randall has observed significant changes in medical education, with less intense curricula and increased government and industry influence. He notes that recent graduates face fewer opportunities to establish their own practices, and academic medicine now places more revenue-generating burdens on faculty, reducing time for teaching and research. Despite these challenges, Dr. Randall believes he holds the best possible position.
He finds that teaching students and young doctors today is challenging due to the limited time full-time faculty can dedicate to teaching the true art of medicine. Managed care and industry pressures have increased the focus on volume over patient interaction. Dr. Randall strives to teach his students and trainees the importance of taking their time with patients, despite these obstacles. “The reward of this approach is opening up the minds and spirits of my students and trainees and watching them grow and mature as new physicians. To see them care for people in the right way is the best reward of all. From the research side, I enjoy watching their eager minds work to solve problems and the smiles on their faces when a paper they have written is accepted for publication and/or presentation,” he said.
In closing, Dr. Randall advises new graduates that despite the stresses and pressure, to approach patients with kindness and ample time, follow their dreams, and never let anyone deter them from their professional goals. “You do have choices in careers and never feel as though you have to back into something that does not conform to how you see yourself professionally.”

Trisha Doucette is the editor of San Antonio Medicine magazine, Cordillera Ranch Living magazine and Rio magazine.
Embarking on the journey to become a medical professional is both an exciting and challenging adventure. From the first day of medical school to the moment grads don their white coats, medical students are stepping into a world where science meets compassion, and where every day brings new oppor -
Bachelor of Arts in Psychology, University of Texas at San Antonio The University of the Incarnate Word School of Osteopathic Medicine, Class of 2027

From a young age, I knew I wanted a career that would allow me to make a meaningful impact on people’s lives. Osteopathic medicine became my calling because it not only allows me to treat disease but also emphasizes prevention and encourages healthier lifestyles. I want to be the kind of physician my patients can turn to in times of uncertainty — someone who alleviates fears, instills confidence, and empowers them with the knowledge to take charge of their own health.
My journey into medicine was not entirely traditional. I earned a Bachelor of Arts in Psychology with a minor in Biology at the University of Texas at San Antonio, but my true passion for patient care was solidified through hands-on experiences. Throughout my undergraduate career and after college, I worked in various medical settings — first as a patient care technician and later as a medical assistant — gaining invaluable clinical exposure. These roles allowed me to connect with patients, assist in their care, and witness firsthand the profound impact a physician can have on someone’s life. These experiences reinforced my decision to pursue medicine, confirming that it was not just a career choice but a lifelong commitment to making a meaningful difference in my patients’ lives.
Like many aspiring physicians, I’ve faced obstacles along the way. Balancing rigorous academics with personal challenges required resilience and determination. Coming from a family without doctors or the advantage of connections or mentors, I had to seek out opportunities and navigate the complex path to medical school on my own. There were times when I felt lost in a system that often seemed easier to navigate for those with established guidance and support.
For anyone considering medical school, my greatest advice is to never let doubt — whether from others or yourself — stand in your way. If becoming a physician is truly your passion and you can’t see yourself doing anything else, you will find a way to make it happen. The path is demanding, but the opportunity to care for others, provide comfort in times of uncertainty, and inspire healthier lives makes every challenge worth it. Keep pushing forward and never give up.
tunities to grow and make a difference in people’s lives. Medical students shared their journeys, from the moments they encountered triumph to moments of doubt, and the reasons they chose to become healers, researchers, advocates and leaders in the field of medicine.
Bachelor of Science and Arts in Biology, University of Texas at Austin Master of Biomedical Science, University of North Texas Health Science Center
UT Health Long School of Medicine, Class of 2026
Every morning, I put on my scrubs — a symbol of both responsibility and privilege. As a third-year medical student, I am constantly reminded of the unique position I hold. I am not yet a doctor, but I am invited into spaces where few are allowed. I have witnessed some of the most vulnerable moments in a person’s life, moments that, if the roles were reversed, I might not want a medical student to overhear. Yet, patients allow me to listen, to learn, and to stand beside them. That is a privilege.

I have counseled individuals from all walks of life — young, old, healthy and critically ill. I have shared in both joy and sorrow, delivering good news that brings relief and bad news that reshapes lives. I have prayed for my patients, and in turn, they have prayed for me. I have stood beside those who believed they did not deserve care and advocated for them, because everyone is deserving of dignity and compassion.
This year has tested me in ways I never expected. I have endured sleepless nights, skipped meals, and shed tears in quiet moments between patient encounters. I have made sacrifices — of time, of comfort, of personal ease — all in pursuit of becoming the physician I have long aspired to be. And yet, despite the exhaustion, despite the challenges, I recognize the immense privilege of being here.
I have grown, not just in knowledge, but in empathy. The privilege of this journey is not only in what I am allowed to witness, but in who I am becoming because of it. The light at the end of the tunnel is no longer a distant flicker; it is brighter than I ever imagined. And as I continue forward, not yet a doctor but ever closer, I carry the weight of this privilege with gratitude and purpose.
Bachelor of Science in Kinesiology Applied Exercise Physiology, Texas A&M at College Station
UT Health Long School of Medicine, Class of 2026
My story isn’t anything wild or dramatic. I loved health and fitness, and I considered professions that would allow me to connect more deeply with my passion — medicine, physical therapy, personal training and dietetics. I thought about all of these options, but at the end of the day, I realized I wanted as much knowledge as possible to advise someone on their health. For me, that meant pursuing medicine, and so I set my sights on medical school.

I majored in Kinesiology with a focus on Applied Exercise Physiology. I thought I was more interested in physical therapy or being a personal trainer. I was obsessed with sports, specifically powerlifting and soccer, and I couldn’t imagine a life that didn’t involve them. I trained 10 hours a week in powerlifting, competed in multiple meets every year, and even made it to Collegiate Nationals in my senior year. On the side, I practiced with my intramural soccer team weekly and traveled to compete against other schools. Everything I did revolved around being active.
Even after deciding on medical school, I constantly worried about how difficult it would be to maintain my hobbies. I questioned whether I should consider a different career path because staying connected to what I love was essential. These concerns became very real during my MCAT studying. It took time away from my hobbies due to how challenging it was for me. The constant reminders from others that medical school would only get tougher didn’t help, and I initially thought it was not going to be a good fit. However, I found that while medical school is harder, it’s challenging in a way that I can manage. If the MCAT feels rough, don’t be surprised. It forced me to remind myself daily why I wanted to pursue medicine.
My advice is to make a mental list of what matters most to you. This is crucial when deciding if medical school is right for you and it will continue to guide you as you choose your path within medicine. For me, school was just as important as the things I loved outside of it. While this mindset might steer some people away from medicine, I approached it knowing my priorities and surrounded myself with like-minded peers — people who had goals and passions outside of school, which they prioritized.
Now, I am in my third year at the Long School of Medicine. I still lift, play soccer, and have even picked up new hobbies like running, baking, painting and reading. As I make final decisions about my specialty, I continue to refine my mental list on what matters most to me. Throughout school, there were times when my studies had to take precedence, but I never lost my life outside. It’s a challenging path but being able to balance my passions while helping others is more than I could ever ask for.
Bachelor of Arts in Psychology, University of California, Riverside
The University of the Incarnate Word School of Osteopathic Medicine, Class of 2027
Master of Public Health Candidate, UIWSOM, Class of 2027
Growing up in a low-income community, I witnessed firsthand the profound impact that limited access to healthcare and preventive resources had on individuals and families. Many in my community relied on emergency services as their primary source of care, often due to financial constraints or logistical barriers. These early experiences shaped my understanding of healthcare disparities and motivated me to pursue a career where I could make a meaningful difference.
As an EMT, I encountered these challenges on a daily basis. Patients frequently sought emergency care for conditions that could have been managed or even prevented with proper access to primary care services. The recurring cycle of poverty, delayed medical attention, and worsening health outcomes reinforced my commitment to addressing these systemic issues.
Similarly, my time working in a cancer center during the COVID-19 pandemic further deepened my perspective on public health. Treating immunocompromised patients during such a critical time underscored the importance of infection control measures, patient education and systemic protections for vulnerable populations. Beyond my professional responsibilities, I carried a personal concern — I feared exposing not only my patients but also my own family, as my father and sister are both immunocompromised. This experience reinforced my belief that medicine extends beyond direct patient care; it requires a broader understanding of public health principles to implement effective disease prevention and healthcare policies.
Recognizing the intersection between clinical medicine and public health, I chose to pursue a dual degree in medicine and public health. Currently, I am a second-year medical student and first-year MPH candidate at UIW, with plans to graduate in 2027 with a DO/MPH degree. This program is equipping me with the knowledge and skills to address healthcare disparities at both the individual and systemic levels. By integrating public health principles into my medical practice, I aim to advocate for underserved populations, develop evidence-based interventions, and implement policies that enhance healthcare accessibility and outcomes.
Currently, I am exploring specialties such as Plastic Surgery, Hematology Oncology and OB/GYN. Whether through reconstructive surgery, advancements in cancer treatment, or improving maternal health outcomes, I aspire to be a physician who makes a lasting impact both in the clinic and at the community level.
The path to becoming a physician is both rigorous and deeply fulfilling. As I continue my medical and public health training, I am committed to developing a comprehensive approach to patient care — one that not only treats disease but also prevents it through education, advocacy and systemic change.
Bachelor of Science and Arts in Biology, University of Texas at Austin
Texas Tech University Health Sciences Center School of Medicine
UT Health San Antonio, Internal Medicine, PGY2
Bachelor of Science in Emergency Medical Services, University of New Mexico
Master of Science in Physician Assistant Studies, University of St Francis

My first real experience with medicine was in my high school anatomy class. I was never one of those kids that grew up knowing they would become a doctor, who played with miniature stethoscopes or pretended their stuffed teddy bear was a sickly patient. I had joined the anatomy class with the expectation that it would be difficult but interesting, but even more importantly, my best friend and I would be in it together! I spent hours in that classroom watching videos of ophthalmology surgeries (tough … I had to look away multiple times) and documentaries about processes like bone formation, and even more time at the back benches completing intricate dissections on frogs, mice, and even cats. Although the work was hard, I felt motivated to study for that class over my other ones and genuinely enjoyed the challenges it brought.
I decided to pursue a biology degree in college with the goal of eventually entering a healthcare career. I initially considered optometry as I personally enjoyed visiting my optometrist (not as scary as visiting the dentist or doctor). However, I quickly realized that I needed a bit more excitement in my daily work life after spending one of my early college summers shadowing a local optometrist. After a lot of self-reflection, speaking with loved ones, and doing my own research, I decided to pursue a career in medicine as I loved the variety of specialties available in the field. As a doctor, I would be challenged to grow every day, be my own leader, and collaborate with a variety of other healthcare specialists as a team.
When I finally got accepted to medical school and graduated college, I felt that I had climbed a Mount Everest of sorts (it really did feel next to impossible). During my first year in medical school, I initially felt drawn to emergency medicine. However, by the time residency application season arrived, I had decided on internal medicine. Internal medicine offered me the greatest chance to encounter as many medical subspecialties as possible via the variety of patients and conditions I would encounter. I also valued the ability to follow up on patients daily to see if my care had made a difference in the inpatient setting. As a second-year resident, I know now that I have made the right choice for me!
My advice for first-year medical students is to focus on the journey itself. Take the time to make memories here and now, whether it is by celebrating after each exam with your new medical school friends, traveling home often to stay in touch with your hometown friends and your family, getting your first ever pet, or even finding a new hobby that will keep you sane throughout your studies and residency. Another thing I would recommend is to stay flexible … life happens, your specialty interests may change, personal relationships begin and end, or you may temporarily find yourself in places less than ideal. You will be surprised what you will take away from these seemingly adverse experiences if you remain unrelentingly open-minded.
The University of the Incarnate Word School of Osteopathic Medicine, Class of 2027

My introduction to medicine was through a volunteer fire station. I was pursuing a degree in civil engineering and an instructor encouraged me to volunteer somewhere. I chose a fire station and learned that fire stations spend more time on medical calls than fighting fires. If you volunteered, they paid for you to get an Emergency Medical Technicians license. One night I was sitting a shift alone when the station was toned out for a medical call. I arrived on scene and saw a man lying on the pavement.
He was not able to communicate, but his eyes were open, and he seemed to know that I was there. I talked to him while I was taking his vitals and though he could not respond verbally, I looked up to see that a tear had fallen from his eye. I sensed that he was grateful that someone was there to help. It had a powerful effect on me.
I switched my degree plan to a Bachelor of Emergency Medicine and made plans to be a paramedic firefighter. I became a paramedic and finished my degree, but my girlfriend had made a commitment to the Air Force, and I knew that it would not be possible to pursue a career as a firefighter. I added extra classes to my degree plan, which allowed me to apply to Physician Assistant (PA) school. For several years I worked as a PA in the Emergency Department. A continuing desire for more tools, and the encouragement of colleagues who were doctors, pushed me to apply to medical school.
I am in my second year of medical school. At this moment I am strongly considering residency in OB/GYN. While in PA school, I had the opportunity to help deliver quite a few babies. There was a lot of joy in those miracles. However, it’s not all happiness. I’ve had challenging conversations with patients, which I consider a privilege and can be more meaningful than moments of joy.
I took a crooked path to medical school, but I am happy about where my journey has led me. That is affirmed each time I am able to be of service to someone, whether that is putting together a wheelchair for a child that a parent literally brings in out of poverty to the wheelchair clinic, volunteering at a medical clinic held for those who are homeless, or attending a patient in the ER. If I had a word of advice for those considering a life of service through medicine, it would be to listen to that voice in your head, volunteer somewhere where you can get practical experience, and study hard.
Megan C. Pranger, DO
Bachelor of Science in Biochemistry, Lindenwood University
Alabama College of Osteopathic Medicine
Captain U.S. Air Force
San Antonio Uniformed Serviced Health Education Consortium; Internal Medicine Residency, PGY3
“How did you decide to become a doctor?” An inquiry I would investigate with all my preceptors during medical school, whether to make conversation or out of genuine curiosity. Now that I reflect on this, I have memorable experiences that brought me where I am today.

When I was 15, I nannied for a family; every time I took care of the kids, they had me read a book about a child’s experience getting diagnosed with type 1 diabetes. After we finished reading, they inevitably asked me to “play doctor.” Each took their turn pretending to be the child in the book. With my newfound knowledge, I held an office visit about diabetes, demonstrating how to check blood sugar, administer insulin, and eat properly to control blood sugar. It was probably more entertaining for me than it was for them.
Fast forward. I’m 21 with college graduation right around the corner. I was a biochemistry major and, having forgotten the experiences of my youth as a fabricated children’s doctor, I figured I would soon end up working in a lab, isolated. My mom called me one morning while I was at school. My dad was having chest pain and went to the hospital; he needed a stent placed for what I know now to be an NSTEMI. I remember how scared we were at the possibility of a heart attack, as that was the cause of my grandfather’s death just years prior. In our fearful, vulnerable state, the internal medicine doctor taking care of him calmed our uncertainties. He flawlessly communicated with the cardiology team, ensured all our questions were answered, and confirmed my dad had everything he needed. I admired how he facilitated collaboration of care among specialties; he instantly became a role model that made a difference in my dad’s life. I decided then that my own life had something in store for me other than a lab bench.
Deciding to join the military was easy; after years of athletics, I wanted a career with camaraderie, and I knew the military would offer that. Besides, what better way to serve your country than healing those who had sacrificed so much? Medical school is intimidating, but the best advice given to me as a first-year medical student was, “Stay in your lane.” It’s hard not to compare yourself to others, what they know, how they’re studying, what resources they use. It’s important to find how you learn and what best suits you. While you shouldn’t compare yourself to others, I encourage a study partner to discuss concepts you don’t understand, and you can test each other to ensure the information is taking root. That person may also turn into a lifelong friend. Becoming a doctor has challenges. Emotionally, physically and mentally, the road hasn’t been easy, and there are more trials that lay ahead, but I would do it all over again.
Disclaimer: The views expressed in this article are those of the author and do not necessarily reflect the official policy or position of the Defense Health Agency, the Department of Defense, nor any agencies under the U.S. Government.
Bachelor of Arts in Biology, Taylor University
Loma Linda University School of Medicine
Captain U.S. Air Force
San Antonio Uniformed Serviced Health Education Consortium; Internal Medicine Residency, PGY1

I have always had an interest in medicine and science, and I knew early on that I wanted to become a physician. Growing up in a small town in Wyoming, experiencing the disparities that affect those in rural areas, and having the opportunity to travel and experience the richness of various cultures, shaped my foundation for the type of physician that I am becoming. While I was in my final undergraduate year at Taylor University, my mentor brought up the military HPSP program, which serves as a pipeline for those wanting to become military physicians. Military service is an important part of my family legacy and serving my country has always been important to me. I jumped at this opportunity to pursue my dream of working as a physician while also serving the individuals and their families who sacrifice to protect our freedom. I attended Loma Linda University School of Medicine where I had numerous mentors who pushed me to become a well-rounded physician, a strong leader and an Air Force officer dedicated to serving my patients and my country. I chose Internal Medicine as my specialty and matched at Brooke Army Medical Center in San Antonio.
I found the perfect combination of being challenged to think critically about a broad range of diseases while also having the ability to develop rapport with patients while I care for them longitudinally. The interplay of complex problems that need solving is exhilarating and I am surrounded by a team of doctors that foster excellence and encourage me in my pursuit of being a lifelong learner. In the military, there is a unique dynamic that is founded in teamwork, dedication and selflessness while welcoming diversity of ideas in pursuit of providing the highest quality of care for all patients. I am currently considering a fellowship in Critical Care or Cardiology, though I know that I will have numerous experiences in the various subspecialties that may change my trajectory. I will continue to build on my background experiences with underserved, rural populations, addressing the community aspects of healthcare, learning to tackle complex cases with the adaptability to take on patient care in a multitude of settings both domestic and abroad, and to become a respected Air Force officer, leader and educator.
Disclaimer: The views expressed in this article are those of the author and do not necessarily reflect the official policy or position of the Defense Health Agency, the Department of Defense, nor any agencies under the U.S. Government.

By Fatima Ali, BS; M. Nicole Bartel, JD, BA; and Jenessa Short, BS, MBS
Medicine is challenging. The journey to medicine and working in medicine varies greatly for each individual, but one thing has remained common among all aspiring, practicing and retired physicians: the mental and emotional grind. Despite these challenges, the U.S. needs physicians to choose and stay in medicine. The AAMC reports that there will be a shortage of over 80,000 physicians by 2036. 1 The WeLEAP Program offered by The Patient Institute aims to build connections within San Antonio’s medical community to support the wellbeing of current and future healthcare providers, helping them navigate the demands of the profession while building sustainable and fulfilling careers in medicine.
The WeLEAP Mentorship Program was founded in 2020 by Dr. Codie Kurka (UIWSOM), with co-founders Jenessa Short (UIWSOM), Fatima Ali (UIWSOM) and Dr. Madi Krimbill (LSOM). Inspired by her own journey to medical school, Dr. Kurka partnered with The Patient Institute to address the gap between San Antonio pre-med students and medical students.
The program quickly gained momentum with the goal of bridging that gap. WeLEAP takes pride in matching mentees with mentors who share similar backgrounds and experiences. Whether pre-med students are first-generation, from military families,
interested in primary care, of a particular religious background, or even uncertain about pursuing medicine, WeLEAP pairs them with medical student mentors who have faced similar challenges. This tailored approach fosters connection and guidance, helping mentees navigate their path to medical school. Since the origin of the Pre-Medical Mentorship Program, over 100 mentor-mentee matches have been made.
Mentoring sessions are held once a month in-person or virtually, depending on student preference and scheduling. Mentors are medical students at The University of the Incarnate Word School of Osteopathic Medicine and The University of Texas Health Science Center San Antonio Long School of Medicine. Past mentees have included students from The University of Texas at San Antonio, The University of the Incarnate Word and St. Mary’s University. WeLEAP is expanding to other undergraduate institutions as the program grows.
Pre-medical students also benefit from WeLEAP’s other programs including the Pre-Medical Student Educational Series, which provides engaging lectures on topics not traditionally discussed in college curricula, and the Pre-Med Library, which provides free MCAT books and flashcards donated by medical students to premed students who may have financial barriers to purchasing exam prep materials.
WeLEAP’s newest initiatives, the Medical Student Mentorship Program and the Medical Student Educational Series, are set to launch in 2025. Led by Dr. Amita Kumar, with support from Jenessa Short and a dedicated committee from The Patient Institute team, these programs aim to prepare young physicians to navigate the challenges of a demanding medical career.
The Medical Student Mentorship Program will connect San Antonio medical students with physician mentors, offering valuable networking opportunities and personalized guidance. The Medical Student Educational Series will feature sessions on WeLEAP topics: wellness, leadership, ethics, applied economics and professionalism.
Together, these programs are designed to equip medical students with practical skills, promote sustainable habits, and provide the support and encouragement needed to build rewarding, lifelong careers in medicine.
WeLEAP programs are only a selection of the many initiatives offered by The Patient Institute. The Patient Institute empowers patients and caregivers to more effectively navigate the healthcare system and offers mentorship and educational programs under WeLEAP to provide patients with caring, knowledgeable healthcare providers. To cultivate professionalism and leadership in physician trainees, The Patient Institute presents the Physician-in-Training Professionalism and Leadership Awards each year to nominated medical students and residents. It is through these programs that The Patient Institute gives back to the community and promotes better healthcare in San Antonio.
For more information or to get involved, please contact info@ patientinstitute.org.
The authors would like to thank the following individuals for their hard work and invaluable contributions:
Codie Kurka, DO, a PGY-1 Emergency Medicine resident, partnered with The Patient Institute during medical school at UIWSOM to lead the formation of the WeLEAP Mentorship Program. Inspired by her non-traditional background as a first-generation medical student, Dr. Kurka believed that having a mentor on her side was paramount to her admission and success in medical school.
Madison Krimbill, MD, Vice President of Education and a PGY-3 Psychiatryresident,wasoneoftheco-foundersofthePre-MedicalStudent Mentorship & Educational Series Programs.
Amita Kumar, MD, is the Vice President of Development for The PatientInstituteandiscurrentlydevelopingtheMedicalStudentMentorship and Educational Series with Jenessa Short.
Randy Surratt is the Past President of The Patient Institute. His leadership was instrumental in guiding the organization through significant milestones and growth.
Adam Ratner, MD, Chairman of The Patient Institute, established The Patient Institute in honor of his late father, Dr. Irving Ratner. Dr. Adam Ratner’s vision and Dr. Irving Ratner’s legacy have been foundational to the organization’s mission and success.
References:
1. Association of American Medical Colleges. “New AAMC Report Shows Continuing Projected Physician Shortage.” June 11, 2023. Accessed December 31, 2024. https://www.aamc.org/ news/press-releases/new-aamc-report-shows-continuing-projected-physician-shortage

Fatima Ali, BS, is Co-President of The Patient Institute and a medical student at The University of the Incarnate Word School of Osteopathic Medicine, Class of 2026. She was one of the co-founders of the Pre-Medical Student Mentorship & Educational Series Programs and was instrumental in the formation of the Pre-Med Library.

M. Nicole Bartel, JD, BA, is Co-President of The Patient Institute and a medical student at The University of Texas Health Science Center San Antonio Long School of Medicine, Class of 2027. She is a non-traditional medical student with prior career experience, and attributes much of her professional and academic success to a few fantastic mentors.

Jenessa Short, BS, MBS, is Executive Vice President of The Patient Institute and a medical student at The University of the Incarnate Word School of Osteopathic Medicine, Class of 2025. She was one of the co-founders of the Pre-Medical Student Mentorship & Educational Series Programs and is currently developing the Medical Student Mentorship and Educational Series with Dr. Amita Kumar.

By Nora Vasquez MD, Certified High-Performance Coach for Medical Professionals, Leaders and Executives
Happy Doctors’ Day! Today, we celebrate you — physicians, healers and leaders — who dedicate your lives to the care and well-being of others. Your expertise, compassion and commitment in service of others shapes the health and future of our communities. As we honor your contributions, we must also address an essential truth: you deserve the same level of compassion and support that you provide to others.
We understand that the medical profession is demanding. Long hours, emotional intensity, administrative burdens and the unrealistic expectation to always be resilient can take a toll. According to studies, 63 percent of U.S. physicians report experiencing burnout at least once a week, affecting not only their personal health but also the quality of patient care and access.
Literature shows that fostering physician well-being requires a combination of both organizational interventions — such as improving workplace efficiency and reducing administrative burdens — and individual strategies that support self-care and professional development. Dr. Tait Shanafelt’s research has shown that professional coaching decreases emotional exhaustion and burnout while improving the quality of life and resilience of physicians.
As physicians, we must seek support — whether through coaching, mentorship or mental health services. We ALL need guidance and a new perspective from time to time. This is NOT a sign of weakness; rather it is a sign of strength, personal growth and greater self-awareness. Prioritizing your well-being is not just about preventing burnout — it’s foundational to ensuring that your career is sustainable, fulfilling, and filled with purpose and joy.
Physicians often navigate their careers independently, but seeking support is an essential professional skill, not a personal failing. Understanding there are multiple kinds of supportive services you can utilize during times of change can make all the difference.
• Coaching: If you are looking to optimize your performance, leadership skills, navigate career transitions or achieve better work-life harmony, a certified physician coach can help guide you to develop strategies for a thriving career. For example, transitioning from residency to fellowship comes with increased responsibilities, and coaching can help you develop a growth mindset and skills that increase confidence in your role as you lead your team.
• Mentorship: If you need advice, seeking a mentor — someone who has walked a similar path — can provide insights and encouragement. A seasoned attending physician mentoring a resident is an example of this.
• Counseling: If you are facing workplace stress, relationship struggles or psychological challenges, counseling can help you develop strategies to improve your mental wellness and relationships.
• Mental Health Services: If you are experiencing persistent anxiety, depression or other mental health challenges, seeking therapy or psychiatric care is a proactive step toward treatment and healing.
Each form of support serves a unique purpose and often utilized together can be synergistic to your overall well-being. Asking for help is a sign of self-awareness, not inadequacy.
The Importance of Prioritizing Well-Being for a Sustainable Career
Medical training and career transitions — moving from medical school to residency, then fellowship, and ultimately becoming an attending — bring increasing levels of responsibility, patient loads and leadership expectations. Having structured support during these transitions can turn stress and self-doubt into opportunities for growth and success. A physician coach who understands the nuances of medicine can help navigate these career shifts effectively, ensuring a more empowered, fulfilling and sustainable practice. Physicians who prioritize their well-being provide better patient care, experience greater job satisfaction, and enjoy longer, more fulfilling careers.
1. Prioritize Rest and Recovery: Sleep is not a luxury — it’s essential for better decision-making, emotional regulation and overall well-being. Set boundaries around rest to maintain long-term resilience and health.
2. Set Healthy Boundaries: Saying “no” to unnecessary commitments and learning to lead your team skillfully, manage your time effectively and delegate tasks can prevent overwhelm and burnout in your personal and professional life.
3. Engage in Mindfulness and Reflection: Mindfulness practices, whether through meditation, prayer, journaling or simple deep-breathing exercises, can reduce stress and improve clarity, leading to better communication, patient interactions and leadership.
4. Cultivate Supportive Relationships: You are not designed to go through life alone. It’s important to seek mentorship, coaching and peer support groups as you navigate challenges. We must be intentional and build strong professional relationships and personal connections. That is why we invite you and your family to join us every Saturday morning at 8:30am CST for the BCMS Weekly Walking Group led by Dr. Fernando Karst. We meet in the parking lot of the Olmos Soccer Fields off Devine Road.
5. Take Care of Your Emotional and Physical Health: Discovering the power of emotional intelligence and managing your mind around challenges improves your ability to better understand and care for yourself and others. Regular physical activity, a balanced diet and mental health check-ins contribute to sustained energy and emotional stability.
6. Develop Leadership Skills and Seek Professional Growth: Great physicians are also great leaders. Engaging in coaching and leadership development programs can enhance your career satisfaction and impact. It is important to seek opportunities for personal development to support your goals.
7. Join a Community of Growth-Minded Physicians: Connecting with other physicians who share similar experiences and struggles reduces isolation and builds a supportive network.
Join Our Online Community and Leadership & Wellness Events
This Doctors’ Day, we invite you to invest in your personal growth. Join our online community where you can access a library of wellness and leadership resources, attend monthly Leadership & Wellness Masterclasses, and connect with like-minded professionals who understand your journey.
You deserve to thrive, not just survive! Let’s work together to build a culture where physician well-being is the norm, not the exception.
Happy Doctors’ Day — and remember, your well-being matters! If you’d like to explore evidence-based strategies that enhance your leadership development and well-being, attend our next 2025 Masterclasses via zoom at 7:00 p.m. CST on:
• Tuesday, February 25
• Sunday, March 23
• Tuesday, April 15
• Sunday, May 18
Visit www.renewyourmindmd.com/renewed for all the details. Spaces are limited, so secure yours today!
References:
1. Changes in Burnout and Satisfaction with Work-Life Integration in Physicians During the First 2 Years of the COVID-19 Pandemic. Shanafelt, Tait D. et al. Mayo Clinic Proceedings, Volume 97, Issue 12, 2248 – 2258
2. Dyrbye, L. N., Shanafelt, T. D., Gill, P. R., Satele, D. V., West, C. P. Effect of a Professional Coaching Intervention on the Well-being and Distress of Physicians: A Pilot Randomized Clinical Trial. JAMA Intern Med. 2019;179(10):1406–1414. doi:10.1001/jamainternmed.2019.2425
3. Shanafelt, T., Goh, J., Sinsky, C. The Business Case for Investing in Physician Well-being. JAMA Intern Med. 2017;177(12):1826–1832. doi:10.1001/jamainternmed.2017.4340
4. Maike van Niekerk, Kali Tileston, Maryse Bouchard, Alfred Atanda, Rachel Goldstein, George Gantsoudes, Cordelia Carter, Melissa A. Christino, System-Level Interventions for Addressing Burnout and Improving Professional Wellness for Orthopaedic Surgeons,Journal of the Pediatric Orthopaedic Society of North America, Volume 5, Issue 1, 2023, 620, ISSN 2768-2765, https:// doi.org/10.55275/JPOSNA-2023-620
5. The new physician burnout research builds on landmark studies conducted at regular intervals between 2011 and 2021 by researchers from the AMA, Mayo Clinic and Stanford Medicine. Together, these studies found the overall prevalence of burnout among U.S. physicians was 62.8% in 2021 compared with 38.2% in 2020, 43.9% in 2017, 54.4% in 2014, and 45.5% in 2011. Each study consistently demonstrated that the overall prevalence of occupational burnout among physicians were higher relative to the U.S. workforce.
6. Since 2012, the AMA has led the national conversation on solving the physician burnout crisis and advocated for new thinking and solutions that acknowledge physicians need support, system reforms, and burden reduction. The COVID-19 pandemic exacerbated many of the drivers of physician burnout. Research has shown that due to COVID-related stress, 1 in 5 physicians intend to leave their current practice within 2 years. https://www. ama-assn.org/press-center/press-releases/physician-burnout-ratespikes-new-height

Nora Vasquez, MD, CHPC, is a triple Certified HighPerformance Coach for Physicians, APPs and Executives. Dr. Vasquez is a board-certified Internist with over a decade of experience. Dr. Vasquez is the Co-Chair of the Physician Wellness Committee for the Bexar County Medical Society and serves on the Texas Medical Association’s Council for Member Experience. She developed the Physician Coaching and Wellness Masterclass Series for BCMS physician members to empower healthcare professionals with evidence-based coaching strategies to mitigate burnout and enhance their well-being. You can learn more about Dr. Nora Vasquez at www.renewyourmindmd.com/renewed or email her at renewyourmindmd@gmail.com.
By Lucas J. Stevens and Ramaswamy Sharma, MS, PhD
Dr. Pat Ireland (P. I.) Nixon, President of the Bexar County Medical Association almost a century ago, stands as a towering figure in the evolution of San Antonio’s healthcare and public health systems. His lifelong commitment to medicine and civic service profoundly shaped the city’s medical community.
P. I. Nixon was born in Old Nixon, Texas, on November 29, 1883, to Robert Thomas Nixon and Frances Amanda (Andrews) Nixon. Within a few years of Texas joining the union as the 28th state, Nixon’s family settled in Luling, an area of Texas just outside San Antonio, brought by the community’s values: tradition and hope.1 These ideals and the close-knit family structure galvanized Nixon’s love for the state and his desire to improve the community.
After graduating from Luling High School as salutatorian in 1900, Nixon graduated maxima cum laude from the Bingham School in Asheville, North Carolina in 1902. He returned to Texas, thereafter, graduating with a Bachelor of Science degree from the University of Texas in 1905. At UTSA, he met his future wife, Olive Gray Read, whom he married in 1912 and had four sons: Pat Ireland Nixon Jr (1913), Robert (1914), and twins: Benjamin and Thomas (1921). Nixon continued his education in Baltimore, obtaining his medical degree from John Hopkins University School of Medicine in 1909. He remained in the Baltimore area for two years, interning at Baltimore-area hospitals and specializing in Gynecology.2
While his education and experience on the East Coast were invaluable, Nixon knew that his true calling was back in the state where he grew up. Nixon moved back to Texas, opening his medical practice in San Antonio on October 1, 1911. His first patient was seen the next day, and was charged $15 for the visit.3 His caring for San Antonio citizens would continue for more than 50 years. A true pioneer at the time, Nixon was a jack-of-all-trades in the medical field, serving as a general practitioner, as an OB-Gyn who delivered babies, and as a surgeon. Nixon practiced at Baptist Memorial, Santa Rosa and the historic Nix Memorial throughout his career. His role in the medical community was appreciated by his election as President of the Bexar County Medical Association in 1926 and by the Texas Surgical Society in 1956.4
At a time when medical technology was still in its infancy, Nixon was lauded for his expertise in the field. His emphasis on the doctor-patient relationship instantly built his rapport with the community, a reminder today of the importance of the medical interview. It was said that he could diagnose most people he saw on the street, just by looking at and speaking to them.5 Nixon brought the people what his father was searching for all those years ago: hope.
To better serve the community he loved, Nixon understood it was necessary to be more vocal about the condition of San Antonio’s public health. When Nixon was practicing medicine, San Antonio had the highest tuberculosis mortality rate of any city, a fact that appalled Nixon.3 Though initially indifferent to politics, Nixon became a relent-
less advocate for public health, fiercely challenging the city’s deplorable sanitary conditions and championing the needs of its most vulnerable residents. He vociferously attacked the current health department for their lack of action, not relenting until real change was made. Other areas that deeply concerned Nixon were the spread of polio, syphilis and infant diarrhea. From 1928 to 1949, Nixon tirelessly served on several key health boards, fighting political resistance to improve San Antonio’s public health.3
Forever the lifelong learner, Dr. Nixon was an excellent physician and an esteemed historian, writer and researcher. He continued to be a trailblazer in all his endeavors, becoming one of the first physicians to document the history of Texas medicine in three books, including: A Century of Medicine in San Antonio, The Medical Story of Early Texas, 1528–1853, and The History of the Texas Medical Association, 1853–1953, published in 1936, 1946 and 1953 respectively.2 His achievements did not just apply to his physician career, as Nixon received the Summerfield G. Roberts and Clement E. Trout literary honors in 1957. His importance to several organizations is exemplified by his election to the highest posts in those establishments-he was the President of the San Antonio Historical Association in 1941, the Philosophical Society of Texas in 1946, and the Texas Historical Association from 1946 to 1949.2
Perhaps the most notable contribution of Dr. Nixon that continues to be a gift to San Antonians today is his vast collection of medical and Texana books. His passionate love of literature and knowledge made him seek many rare books to add to his collection. He understood the importance of having diverse materials to study when he founded the Bexar County Medical Library Association in 1919, serving as Chair.4 Through his dedicated work, the medical library greatly expanded its collection, allowing future physicians the resources they needed to be successful. Even indirectly, Nixon was still performing the same task he had always strived to do: helping the people of San Antonio.
Dr. Pat Ireland Nixon passed away on November 18, 1965. Serving the community up until his death, he donated his collection of Texana books to Trinity University in 1964. In 1970, the Bexar County Medical Society donated most of the oldest books held by the Bexar County Medical Library Association to UT Health San Antonio to create the P.I. Nixon Medical Historical Library. The collection was named after Dr. Nixon in honor of his tireless efforts to build it, and is housed in the Briscoe Library. Strengths of the Nixon collection are in the areas of ophthalmology, surgery and anatomy and the superb core collection of over 6,000 volumes includes original works by Andreas Vesalius (De HumaniCorporisFabrica – 1543), Bernhard Siegfried Albinus (Tables oftheSkeletonandMusclesoftheHumanBody – 1749), Aulus Cornelius Celsus (De Medicina – 1481), Avicenna (Ibn Sina) (The Canon of Medicine – 1486), Robert Burton (Anatomy of Melancholy – 1632), and Robert Hooke (The Micrographia – 1667). One extremely rare book that was included in the donated collection was an original The OriginofSpecies by Charles Darwin. The library regularly features a historical book of the month on the Treasures of the P.I. Nixon Historical Blog at https://library.uthscsa.edu/category/treasures/.
As a physician, public health advocate and historian, Dr. Nixon provided direct medical care and spearheaded critical reforms addressing public health crises. His efforts to combat diseases and reform
health policies, and his extensive contributions as a historian reflect his enduring impact. His legacy continues to inspire advancements in healthcare and serves as an excellent example for current and future physicians of San Antonio.
References:
1. Nixon, P. I. (1956). The Early Nixons of Texas: With Genealogies by Dr. and Mrs. Pat Ireland Nixon, Jr.
2. Burns, C. R. (1995, May 1). Nixon, Pat Ireland. Texas State Historical Association. https://www.tshaonline.org/handbook/ entries/nixon-pat-ireland
3. Nixon, P. I., & Lang, Herbert H. (1979). Pat Nixon of Texas: autobiography of a doctor (1st ed.). College Station: Texas A & M University Press.
4. P. I. (Pat Ireland) Nixon, 1883-1965 - UT Health Science Center Library. (2021, August 25). UT Health Science Center Library. https://library.uthscsa.edu/resources/pi-nixon-library/pat-ireland-nixon/
5. Nixon, Jr., Dr. P. I. (2004, October 7). Interview with Dr. P. I. Nixon, Jr. (P. Borchers, Interviewer). https://library.uthscsa.edu/ wp-content/uploads/2021/04/Narrative-transcript.pdf

Lucas J. Stevens is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. His interests include new scientific and technological advancements that will improve patient care, and he is interested in pursuing a career in the fast-paced environment of emergency medicine.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma is a member of the BCMS Publications Committee.

The Texas Legislature meets every odd-numbered year for 140 consecutive days and convened again on January 14, 2025. Legislators need to hear from you — their physician, medical student and alliance constituents — during the session to understand how proposed legislation can potentially impact the practice of medicine in Texas. Mark your calendar for 2025 First Tuesdays at the Capitol.
• March 4 (TMA Alliance and Young Physician Month)
• April 1 (TMA Medical Student and Resident Month)
• May 6

By John D. Rodriguez, MD
Gone are the days of the private practice physician. This is very evident in the study found in the PAI-Avalere Health Report showing that in 2023 nearly four of five physicians (77.6 percent) of physicians are now employees of hospitals/health systems and other corporate entities.
To add to the above trend is the ever-present primary care shortage, which is projected to be between 17,800 – 48,000 physicians by the year 2034, the independent and autonomous private practitioner will essentially cease to exist.
The days of “Marcus Welby” medicine began to wane with the inception of managed healthcare insurance in the 1970s. The goal of managed healthcare insurance was to help control the cost of healthcare, but this “cost containment” approach has affected primary care providers the hardest. The fact is that primary care providers rely solely on evaluation and management coding, which reimburses substantially less than procedural CPT coding. Couple this with the fact that Medicare reimbursements have not kept up with the cost of running a practice. According to the AMA, Medi -
care reimbursement has declined 29 percent from 2001 to 2024 when adjusted for inflation, and most commercial payor contracts are based on a percentage of Medicare. So, it is not difficult to understand why independent solo/small group practices are going out of business.
One would applaud the rescue by large hospital systems as the solution to this crisis, but even these hospitals take a loss on each primary care provider hired as displayed in the graph on the following page.
One solution to this primary care dilemma is a healthcare delivery model known as the micro-practice. The definition is listed as “a streamlined medical care model with minimal overhead.” Simply put, a micro-practice provider works out of one room with few to no employees and manages most of the day-to-day running of a practice. With a good EHR and its tools as well as the institution of AI in the documentation/coding process, a provider can efficiently run his/her practice while providing quality healthcare. Most providers state that, despite doing more of the administrative work and sometimes even custodial work, this tradeoff is well worth it.
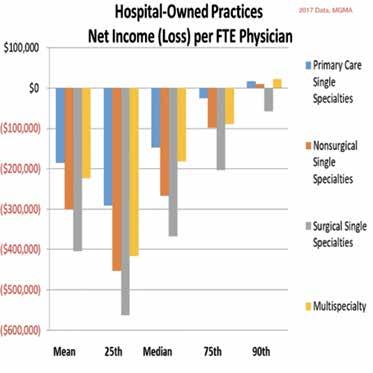
The downside to a small practice is that one is not capable of seeing 25 patients a day, which is necessary to cover high overhead. This high-volume model only leads to unhappy patients and can affect the delivery of quality medicine. But one now has autonomy and can practice the way he/she wants without being told when to work and how many patients to see.
One of the concerns raised about this model is that one cannot make enough money because the physician is not able to see a large volume of patients in a day. An overhead that runs 70 to 80 percent of collections in the old delivery model now is lowered to 10 to 15 percent in a micro-practice. Though despite seeing fewer patients, the profit margins are much better.
Because overhead is much smaller, one can see as little as 10 to 12 patients per day and still do just as well as an employed provider. While in a traditional practice, the first 12 to 15 patients of the day go to overhead, only 2 to 3 patients per day meet the overhead needs in a micro-practice. Thus, it is easy to see that, with a well-run and efficient practice, one can do very well financially while giving patients the attention they need.
This healthcare delivery approach is catching on with numerous providers here in Texas. Dr. Osvaldo Villareal, who started Abrazos Optimum Health in Boerne, Texas, is happy that he took the plunge into a micro-practice. “I was disgruntled with the system and forced to leave because of my vaccine status.” He came across this micro-practice idea and after doing his due diligence, opened up his pediatric clinic in a small office about two years ago. He has no employees and manages the day-to-day but states, “I can spend more time with my patients and honor their parental rights.” He states he is now doing better financially than in his previous position and would never go back to being employed.
The start-up and maintenance costs are the secret to a successful micro-practice. While a start-up loan can run over $100,000 in a traditional practice, in a micro-practice only a fraction is needed. The ability to moonlight can help offset the costs as the physician ramps up a practice, and with the shortage of primary care in Texas, this ramp-up period is very short.
Dr. Caleigh Rodriguez, who started her primary care clinic in New Braunfels out of one room through Parvus Medical Suites, grew very quickly and in only one year is near capacity. She works two-and-onehalf days per week yet makes almost twice what a full-time employed physician makes. She is a full-time mom and part-time physician. “Because of my low overhead, I am able to run a successful practice and be a mom to my children.” She is also able to help uninsured patients by offering them a low-cost monthly membership that gives them a medical home.
When questioned what it is like working out of one room, she stated, “I find utilizing a one room/office is a breath of fresh air. Not only do I get extra work done between patients, I find that patients actually love the personalized office aspect of it.”
Dr. Won Park, who recently started River City Internal Medicine out of one room through Parvus Medical Suites in San Antonio, was looking to simplify his life. He is a busy hospitalist, looking for a way to make a change, and came across a micro-practice approach. “I wanted more control and autonomy back in my life and not to be told how many patients to see.” He works one week as a hospitalist and the other week building his practice. He will soon be able to step away from hospitalist medicine and dedicate his time to his own private practice. “I appreciate this low-cost option of starting a practice and can now spend more time with my patients.”
One of the challenges in a micro-practice is locating space small enough where the rent is affordable and looks professional. Most medical office space available is too large and expensive with long-term leases that are risky. Some providers are able to rent one room from a busy specialist practice but this could create Stark Law violations if one is not careful. But persistence will find one a place that fits one’s budget and offers a professional atmosphere.
In follow up, micro-practice medicine may seem on the surface to not be a viable option because of poor cash flow and the menial work being beneath most physicians. But providers are proving this wrong and now have the independence and financial reward they have been looking for while providing quality healthcare that patients love and value.
Medical Suites is a Platinum Member of the BCMS Circle of Friends program

John D. Rodriguez, MD, is board certified in Internal Medicine and has a passion for primary care. He is the owner of Parvus Medical Suites and Chief Medical Officer and Co-founder of Healthcare2u LLC. Dr. Rodriguez is a member of the Bexar County Medical Society.
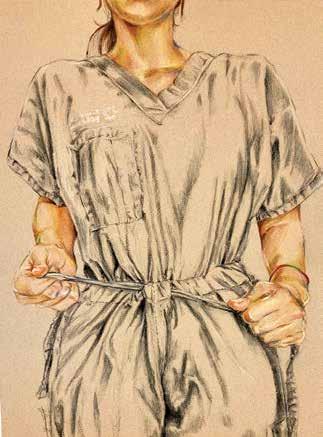
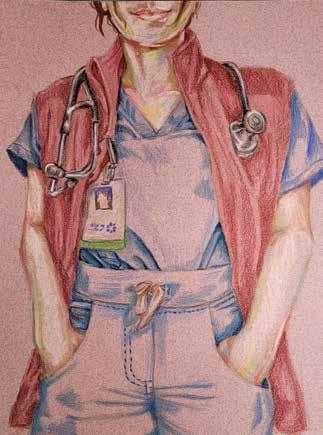
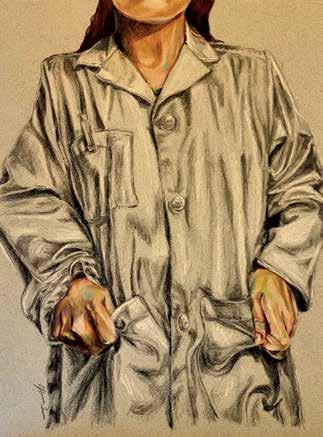
Artist’s Note: “Perfect Fit” is a series of self-portraits documenting my journey through medical education, outlining my experiences coming into new identities as a medical student and soon-to-be-doctor, and the excitement and trepidation of growing into the clothes I wear; growing into the expectations and responsibilities of becoming a physician; and growing comfortable in my own skin.

UT Health San Antonio
Long School of Medicine
Medical Class of 2025
With heavy hearts, we share the news of Dr. Donald Gordon’s passing on January 15, 2025. He was a cherished physician, veteran, educator, colleague and friend. We are grateful for his dedicated service to the Bexar County Medical Society throughout his membership and as our 2010 BCMS President.
Dr. Gordon became a member of the Bexar County Medical Society in 1980. Throughout his membership, he served on various committees, including the Board of Directors, Board of Ethics, Emergency Preparedness Committee, Nominating/Constitution Bylaws Committee, Board of Censors, Public Health and Patient Advocacy, and Membership Committee, etc.
After serving 20 years in the United States Army, Dr. Gordon completed his residency at Brooke Army Medical Center, which led him to plant roots in San Antonio. In addition to being a BCMS member, he was the Medical Director for San Antonio and Bexar County’s EMS for 22 years, President of the American Red Cross in San Antonio, and a member of the Northwest Rotary Club and the West San Antonio Chamber of Commerce.
Bexar County Medical Society extends its deepest condolences to the Gordon family and friends. Dr. Donald Gordon left behind a lasting impact on his community, and we are thankful for his lifelong commitment to improving emergency medical care.



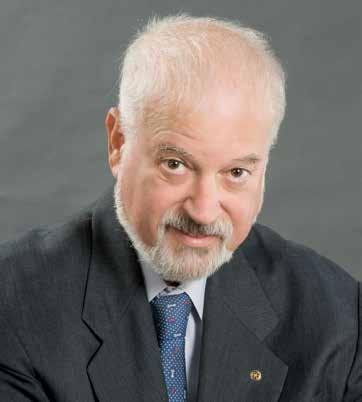


By Jacob Hernandez
We were so excited to kick off the 89th Legislative Session at the Texas Capitol on February 4 with an enthusiastic delegation of physicians, medical students and TMA Alliance members from Bexar County for the inaugural First Tuesdays at the Capitol event of 2025! Much gratitude to the following participants: John M. Shepherd, MD, BCMS President; Jenny Shepherd, TMAA President; Ezequiel “Zeke” Silva, MD, BCMS Immediate Past President; Jennifer Rushton, MD, BCMS President-Elect; Jayesh “Jay” Shah, MD, TMA President-Elect; Daniel Deane, MD; Sanjiv Kumar, MD; Kenneth Maverick, MD; Alex McKinlay, MD; Gerardo Ortega, MD; Catherine Ortega; John Michael Austin (UTHSCSA); Ruba Krichati (UIWSOM); and Tirzah Polk (UIWSOM).
Our group met with legislators and staff from each of the Bexar County legislative offices, who graciously made time to discuss important issues and bills that inform access to care, practice viability and physician autonomy in San Antonio and across the state. Paramount among these are opposition to SB 911 and HB 1756, which would remove physicians from the healthcare team by giving APRNs full independent diagnostic and prescriptive authority; support of SB 922 and HB 1699, which require patients to be given the results of sensitive diagnostic tests directly from a physician rather than through a portal; clarifying exceptions to Texas’ abortion ban in cases where the life of a pregnant patient is at stake and removing criminal and civil litigation incentives that can deter doctors from providing the standard of care to women and girls in danger; and support of SB 547, which would strengthen the implementation of Texas’ Gold Card Law and cut down on unnecessary, even predatory use of prior authorizations to deny healthcare access to patients. These issues and many more are at the forefront of the efforts made every day by TMA’s stellar Division of Public Affairs, and we’re glad to have the opportunity to bolster their efforts each month.


If you haven’t made it to First Tuesdays yet this year, there’s still time to get involved! You can register at www.texmed.org/firsttuesdays/ to attend the events on April 1 (with a special highlight on medical students and residents, though all levels of participants will be present) and May 6. Legislators need to hear from you as the session churns on, in order to continuously develop an understanding of how proposed legislation will actually affect the practice of medicine for you, your community and all Texans. Please come! More information is available at the TMA web page linked above, but if you have any specific questions, please feel free to reach out to Jacob Hernandez, BCMS Advocacy & Public Health Specialist, at jacob.hernandez@bcms.org.

During the February 4 meeting with staff from Rep. Ray Lopez’s office, Jayesh Shah, MD (right), reflects on scope-of-practice challenges while Legislative Director Christopher Ludiker listens. Looking on at left are Gerardo Ortega, MD; Catherine Ortega; and Alisa Pierce, TMA staff; with Tirzah Polk, UIWSOM medical student, in the foreground.






We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 CDavis@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark
President
210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank
(HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@broadway.bank www.broadwaybank.com
“We’re here for good.”

Texas Partners Banks (HHH Gold Sponsor)
Our private banking team specializes in healthcare banking and will work with you to craft and seamlessly integrate financial solutions for you and your practice, including practice loans, lines of credit and custom local lockbox solutions headquartered in San Antonio.
Maria Breen
210-807-5562
Maria.Breen@texaspartners.bank www.texaspartners.bank

Lone Star National Bank (HHH Gold Sponsor)
Established in 1983, Lone Star National Bank has provided banking services to communities in South Texas for the past 41 years. LSNB is an independent and locally owned bank subsidiary of Lone Star National Bancshares-Texas, Inc with consolidated assets of $3 billion (12/31/23) and 36 full-service banking centers throughout Starr, Hidalgo, Cameron and Bexar counties.
Aside from personal and business banking, LSNB offers investments, wealth management & trust along with property and casualty insurance, health insurance and supplemental coverage.
Ivan Corona Molina
Assistant VP 210-479-4713
MolinaI@lonestarnationalbank.com www.lonestarnationalbank.com
“We do what the Little Banks can’t, and the Big Banks won’t!”
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org
www.synergyfcu.org
“Once a member, always a member. Join today!”

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison 210-503-0003
Yulia@genicslabs.com
Kevin Setanyan Managing Partner 210-503-0003
Kevin@genicslabs.com
Artyom Vardapetyan Managing Partner 210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease and Genetics.
Robert Castaneda CEO 210-316-1792
Robert@livingstonmedlab.com www.livingstonmedlab.com/home “Trusted Innovative, Accurate and STAT Medical Diagnostics”

American Health Imaging (HHH Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina. US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com

Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora
Jaime.Zamora@usradiology.com
Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com www.americanhealthimaging.com (main site)
www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations
210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”

Avid Wealth Partners (*** Gold Sponsor)
For over 15 years, Avid Wealth Partners has been the trusted financial partner for local physician specialists and practice owners. We specialize in physician-focused financial advising, offering proactive tax planning, customized investment strategies, and comprehensive risk management solutions. Our approach addresses every aspect of your financial life, protecting your hardearned assets and building lasting wealth. With a team of credentialed specialists, we simplify complexity so you can focus on what you do best— caring for patients
MDWealth@avidwp.com www.avidforphysicians.com 210-864-3333
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor 210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”
Hancock Whitney (HH Silver Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Serina Perez
San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com

UT Health San Antonio
MD Anderson Cancer Center
(HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at
locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager
210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229

Equality Health
(HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
(H Bronze Sponsor)
We were founded to meet a need: helping business owners succeed by giving them simple, quality, affordable U.S.-based contact solutions. In only a few years, our focus on nurturing client relations and building trust not only helped our customers grow their businesses, but helped us stake our claim in the highly competitive TAS industry as one of the most well-regarded and referred. Our 50 years of collective experience are the driving force behind our clients’ satisfaction.
Rachel Caero Managing Partner
844-554-3473
Rachel@dialops.net

(HHHH 10K Platinum Sponsor)
TMA
of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits
512-370-1746
Wendell.England@tmait.org
800-880-8181 www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust
(HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann
Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group
(HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
LASO Health Telemedicine and Rx App (HH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care.
LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

Parvus Medical Suites (HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer 210-632-3411
DrJohn@parvussuites.com www.parvussuites.com
Trust is a full-service
agency offering a full line
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com
Continued on page 42
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
Field Sales Consultant
210-413-8079
Tom.Rosol@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Darby Rodriguez Regional Client Executive 281-753-3565
D.Rodriguez@eleosvhs.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care”
Methodist Physician Practices (**Silver Sponsor)
Methodist Physician Practices is committed to providing exceptional care for patients in greater San Antonio and South Texas. As part of Methodist Healthcare, we are dedicated to raising the standards of performance excellence while advancing the health and well-being of the communities we serve. Our extensive network of highly-skilled primary care physicians, specialists and surgical care providers ensures patients receive comprehensive, coordinated and compassionate care. As part of the Methodist Healthcare System, our physicians are committed to delivering personalized, high-quality services that meet the diverse needs of our patients. At Methodist Physician Practices, we go beyond healthcare — providing hope, healing and unwavering support for each individual we serve.
Erin Fitzgerald
Methodist Healthcare I Methodist Physician Practices
M:281-673-7350
methodistphysicianpractices.com
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery
President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber
President 210-308-7907 (Direct) KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA)
(HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner
President info4@samgma.org www.samgma.org

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
San Antonio Office 210-301-4362
www.favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”


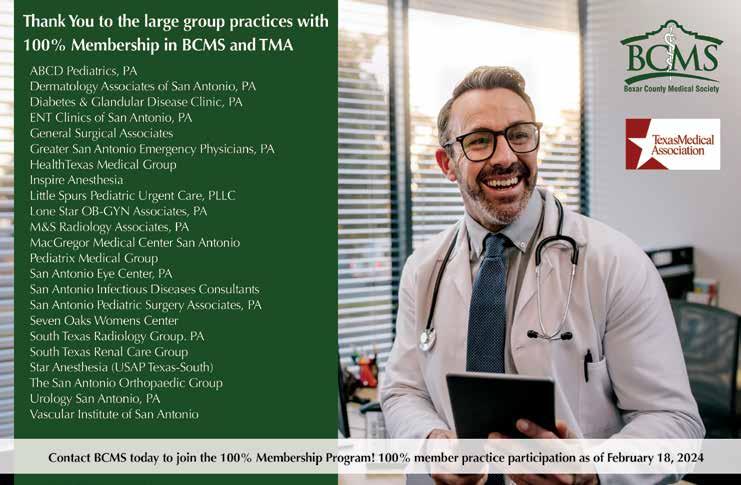

By Stephen Schutz, MD
The Infiniti QX80 was freshened in 2024 in an effort to strengthen Infiniti’s presence in the luxury full-size SUV segment. Good thing, because the previous QX80 needed significant improvements to challenge the class-leading Cadillac Escalade, Mercedes-Benz GLS and BMW X7.
Just one glance shows that Infiniti was serious with its latest update of their flagship model. Gone are the round and bulbous proportions of the old QX80, replaced with angular design elements, thin headlights and an imposing grille. From the side, strong lines and crisp creases lend it a more muscular look, while the floating roofline and full-width rear LED lights add modern touches.
The outgoing QX80 also suffered from a cabin that felt a generation (or two) behind its rivals. That’s no longer the case as Infiniti has completely reimagined the interior with large high-tech horizontal screens, nice leather accents and open-pore wood.

Two 14.3-inch curved displays dominate the dashboard: the one in front of the driver is for the digital instrument cluster, while the central one is for infotainment. Meanwhile an additional 9-inch touchscreen sits below the middle screen and handles climate controls. It’s a clean, high-tech layout, and it brings the 2025 QX80 closer to its competitors.
The seats are comfortable but not groundbreaking. Plush, beautifully stitched leather is a welcome touch, and the massage functions for both the driver and front passenger are nice. The second row is spacious but doesn’t quite match the size of the Escalade’s.
Naturally, given its size, the 2025 QX80 comes with a third row of seats. As usual, the “way back” is best for children, although they’re OK for adults if it’s a short trip.
Infiniti has partnered with Klipsch Audio to develop a 24-speaker premium sound system for the QX80, which is excellent. Lexus’ Mark


Levinson system is the gold standard in this class, and Infiniti’s set-up is close to that in audio quality.
Perhaps the biggest change in the new QX80 is its powertrain.
Gone is the 5.6-liter naturally aspirated V8, replaced by a 3.5-liter twin-turbocharged V6 producing 450 horsepower and 516 lb-ft of torque. That’s a significant increase in power, and the potent engine is aided by a new 9-speed automatic transmission that replaces the old 7-speed unit.
Despite all of that turbocharged V6 progress, please allow me a moment of sadness for the loss of the old V8 soundtrack. Sigh.
Fuel economy for the 4WD QX80 is 15MPG City and 19MPG Highway. Not good, but it’s better than the old V8, and hashtag welcome to the luxury full-size SUV fuel economy neighborhood.
By the way, switching from V8 to V6 engines has become the norm with luxury full-size SUVs. The latest Lexus LX is now V6 only, and most BMW X7 and Mercedes GLS models sold come with turbo V6s. Will the popular GMC Yukon Denali and Cadillac Escalade ever surrender to the emissions and fuel economy gods and make the switch to turbo V6s? I’d say yes, but probably not for 5-10 years.
Acceleration for the new turbo V6 QX80 is excellent, with a 0-60 mph time of around 5.5 seconds.
The exhaust note is nicely subdued, and towing capacity remains 8,500lbs, meaning the QX80 is one of the most capable haulers in the segment. That matters to buyers who have to tow a boat to the lake or horses to a show.
With a curb weight of around 6,000lbs, the QX80 was never going to feel nimble, but Infiniti has taken steps to improve its driv-


ing dynamics. An (optional) air suspension delivers a smoother ride, particularly over rough pavement, and even in “normal” suspension mode, the QX80 drives fine. As I’ve noted previously in reviews of larger SUVs, even those from upscale brands, these are people/gear/ stuff haulers and trailer pullers so don’t expect sports car driving dynamics.
Infiniti’s ProPilot Assist 2.1 active driver assistance system adds hands-free highway driving abilities, putting it on par with Cadillac’s Super Cruise and Ford/Lincoln’s BlueCruise. The system works very well on the interstate, though it requires occasional driver intervention (that’s ok, it makes long drives much better than they would be without it). In other situations, I don’t have complete trust yet.
Pricing for the 2025 QX80 ranges from $85,000-ish for a base model to just over $112,000 fully loaded. Compared with all of the other competitors mentioned above, the Infiniti will probably be cheaper (and more discounted), which will increase its appeal.
The 2025 Infiniti QX80 has been upgraded in its design, interior and powertrain, which will make it more competitive in the luxury full-size SUV market. Infiniti has historically struggled to compete in this arena, but the myriad of improvements Infiniti made for 2025 make it worthy of a look for any potential buyer in this market segment.

Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.



11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Northside Honda
9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Kahlig Auto Group Kahlig Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Lamborghini San Antonio 27605 IH 10 West Boerne, TX
Douglas Cox 210-600-5770
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
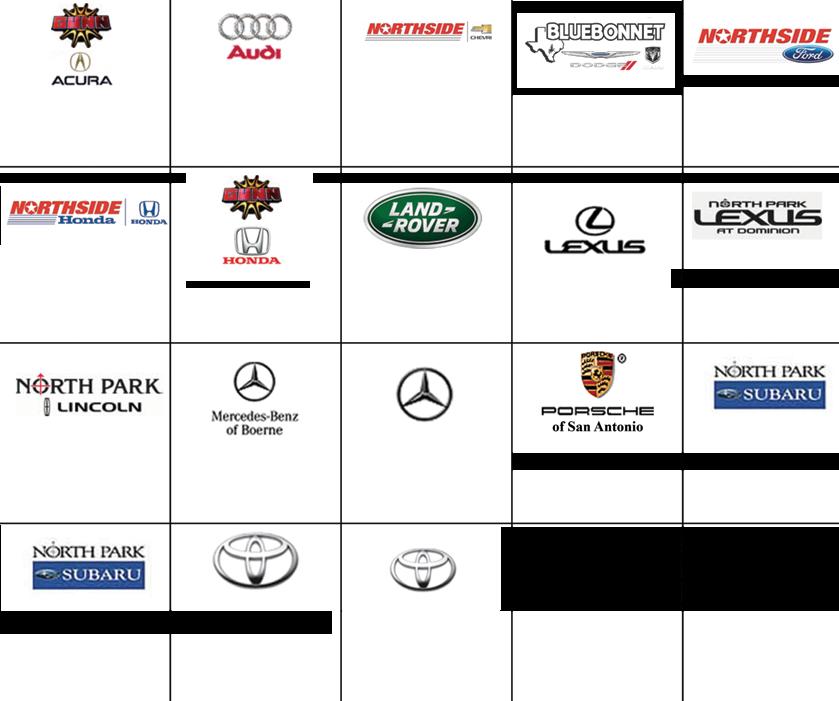
North Park Subaru
9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
Auto Group Kahlig Auto Group Kahlig Auto Group
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Auto Group Kahlig Auto Group
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945