
Official Publication of SDCMS SEPTEMBER 2022 A New Epidemic Hepatitis C











Saturday October 8th 5-9 p.m. Veloce Motors The Vault 9340 Dowdy Drive #102 San Diego, CA 92126 roller dreams to support Champions for Health www.cfhcasinonight.org • gabriela.stichler@championsfh.org • 858.300.2789 Bring your high Hea h… Hea h Dress as your favorite James Bond character Strike a pose next to luxury autos www.cfhcasinonight.org • Saturday October 8th 5-9 p.m. . . . Veloce Motors The Vau 9340 Dowdy Drive #102 San Diego, CA 92126 Presented By Stony Anderson Maria Carriedo
Editor: James Santiago Grisolia, MD
Editorial Board: James Santiago Grisolia, MD; David E.J. Bazzo, MD; Robert E. Peters, MD, PhD; William T-C Tseng, MD
Marketing & Production Manager: Jennifer Rohr
Art Director: Lisa Williams
Copy Editor: Adam Elder
OFFICERS
President: Sergio R. Flores, MD
President–Elect: Toluwalase (Lase) A. Ajayi, MD
Secretary: Nicholas (Dr. Nick) J. Yphantides, MD, MPH
Immediate Past President: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
GEOGRAPHIC DIRECTORS
East County #1: Catherine A. Uchino, MD
East County #2: Rakesh R. Patel, MD
Hillcrest #1: Kyle P. Edmonds, MD
Hillcrest #2: Steve H. Koh, MD (Board Representative to the Executive Committee)
Kearny Mesa #1: Anthony E. Magit, MD, MPH
Kearny Mesa #2: Alexander K. Quick, MD
La Jolla #1: Preeti S. Mehta, MD (Board Representative to the Executive Committee)
La Jolla #2: David E.J. Bazzo, MD, FAAFP
La Jolla #3: Sonia L. Ramamoorthy, MD, FACS, FASCRS
North County #1: Arlene J. Morales, MD
North County #2: Christopher M. Bergeron, MD, FACS

North County #3: Nina Chaya, MD
South Bay #1: Paul J. Manos, DO
South Bay #2: Maria T. Carriedo-Ceniceros, MD
AT–LARGE DIRECTORS
#1: Thomas J. Savides, MD
#2: Kelly C. Motadel, MD, MPH
#3: Irineo (Reno) D. Tiangco, MD
#4: Miranda R. Sonneborn, MD
#5: Stephen R. Hayden, MD (Delegation Chair)
#6: Marcella (Marci) M. Wilson, MD
#7: Karl E. Steinberg, MD, FAAFP
#8: Alejandra Postlethwaite, MD
ADDITIONAL VOTING DIRECTORS
Medical Student: Jimmy Yu
Resident: Nicole L. Herrick, MD
Young Physician: Brian J. Rebolledo, MD
Retired Physician: Mitsuo Tomita, MD
CMA OFFICERS AND TRUSTEES
Robert E. Wailes, MD
William T–C Tseng, MD, MPH
Sergio R. Flores, MD
Timothy Murphy, MD
AMA DELEGATES AND ALTERNATE DELEGATES
District I: Mihir Y. Parikh, MD
District I Alternate: William T–C Tseng, MD, MPH
At–Large: Albert Ray, MD
At–Large: Robert E. Hertzka, MD
At–Large: Theodore M. Mazer, MD
At–Large: Kyle P. Edmonds, MD
At–Large: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
At–Large: David E.J. Bazzo, MD, FAAFP
At–Large: Sergio R. Flores, MD
At–Large Alternate: Bing Pao, MD
CMA DELEGATES
District I: Karrar H. Ali, DO, MPH
District I: Steven L.W. Chen, MD, FACS, MBA
District I: Franklin M. Martin, MD, FACS
District I: Vimal I. Nanavati, MD, FACC, FSCAI
District I: Peter O. Raudaskoski, MD
District I: Kosala Samarasinghe, MD
District I: James H. Schultz, MD, MBA, FAAFP, FAWM, DiMM
District I: Mark W. Sornson, MD
District I: Wynnshang (Wayne) C. Sun, MD
District I: Patrick A. Tellez, MD, MHSA, MPH
RFS: Rachel Buehler Van Hollebeke, MD
Opinions expressed by authors are their own and not necessarily those of San Diego Physician or SDCMS. San Diego Physician reserves the right to edit all contributions for clarity and length as well as to reject any material submitted. Not responsible for unsolicited manuscripts. Advertising rates and information sent upon request.
Acceptance of advertising in San Diego Physician in no way constitutes approval or endorsement by SDCMS of products or services advertised. San Diego Physician and SDCMS reserve the right to reject any advertising. Address all editorial communications to Editor@SDCMS.org. All advertising inquiries can be sent to DPebdani@SDCMS.org.
San Diego Physician is published monthly on the first of the month. Subscription rates are $35.00 per year. For subscriptions, email Editor@SDCMS.org. [San Diego County Medical Society (SDCMS) Printed in the U.S.A.]
Features
By Robert G. Gish, MD
16
Active Treatment for Extremely Preterm Babies on the Rise
By Amanda D’Ambroisio
Charles D. Lee, MD, JD, MBA
CDC: Paralytic Polio an Ongoing Risk for the Unvaccinated By Ingrid Hein
Local Doctor Richard Brown Releases Second Medical Thriller
Charity
SDCMS Staff
By Adama Dyoniziak
Helane Fronek, MD, FACP, FASVLM, FAMWA
David L. Feldman, MD,
SANDIEGOPHYSICIAN.ORG 1
Contents SEPTEMBER VOLUME 109, NUMBER 7
17
18
Novel to Benefit
By
19 It’s My Calling
20 Ignorance and Arrogance: A Dangerous Combination By
21 Classifieds
6 A New Epidemic: Hepatitis C
12 The Unknown Specialty! By
Departments 2 Briefly Noted: Public Health • Infectious Diseases • SDCMS Leadership 4 SDCMS’s First Physician Social Networking Mixer in 3 Years Is a Huge Success! 14 As Telemedicine Best Practices Emerge, Assess Your Practice By
MBA, FACS
BRIEFLY NOTED
PUBLIC HEALTH
Gov. Newsom Proclaims State of Emergency to Support State’s Monkeypox Response
AS PART OF THE STATE’S ONGOING response to the orthopoxvirus (monkeypox) outbreak, on Aug. 1 Governor Gavin Newsom declared a State of Emergency to bolster the state’s response to the monkeypox outbreak. The proclamation supports the work under way by the California Department of Public Health and others to coordinate a whole-ofgovernment response to monkeypox, bolster vaccination efforts, and expand outreach and education to inform Californians about mon keypox and ways to limit its spread.
As of Aug. 9, the state had distributed more than 62,000 vaccine doses, allocating vac cines to local health departments based on a number of factors, including the number of reported monkeypox cases in an area and esti mate of at-risk populations. (The state provides weekly updates on Tuesday on the vaccine allocation by local health department. For the most up to date figures, see the CDPH monkey pox vaccine page.)
To expand vaccination efforts, the proclama tion also enables emergency medical services (EMS) personnel to administer monkeypox vaccines that are approved by the FDA, similar to the statutory authorization recently enacted for pharmacists to administer vaccines. The state’s public health laboratory leaders have also been working with local public health, academic, and commercial laboratories to ensure testing capacity is increasingly avail able and coordinated with the public health response.
INFECTIOUS DISEASES
DHCS Advises Physicians to Hold Medi-Cal Claims for Monkeypox Tests

THE CALIFORNIA DEPARTMENT OF Health Care Services (DHCS) released guid ance regarding a new CPT code created to streamline the reporting of orthopoxvirus (e.g., monkeypox) testing (87593). As soon as DHCS has updated its systems, physicians will be able to bill CPT code 87593 as a Medi-Cal benefit. Until then, physicians are advised to administer the test as needed, but to hold the claim for submission.
Additionally, the American Medical Associa tion has also created two new CPT codes for monkeypox vaccines. The new monkeypox CPT codes are:
• 87593: Infectious agent detection by nucle ic acid [DNA or RNA]; orthopoxvirus [e.g., monkeypox virus, cowpox virus, vaccinia virus], amplified probe technique, each
• 90622: Vaccinia (smallpox) virus vaccine, live, lyophilized, 0.3 mL dosage, for percu taneous use
• 90611: Smallpox and monkeypox vaccine, attenuated vaccinia virus, live, non-rep licating, preservative free, 0.5 mL dosage, suspension, for subcutaneous use
For additional information on monkeypox symptoms, testing, treatment and vaccina tion, view the California Department of Public Health and the Centers for Disease Control and Prevention websites.
2 SEPTEMBER 2022
San Diego County Board of Supervisors Honors Dr. Ajayi

SDCMS’S NEW PRESIDENT, TOLUWALASE (LASE) AJAYI, MD, IS OFF TO a strong start. After being elected the first San Diegan to ever sit on the American Medical Association board, Dr. Ajayi recently received a special recognition from the San Diego County Board of Supervisors. Led by chair Nathan Fletcher, the board commended Dr. Ajayi for “outstanding service, leadership, and commit ment to the citizens of San Diego County” and declared June 28 as “Dr. Toluwalase Ajayi Day” throughout the county!
The county’s formal proclamation read in part:

WHEREAS, Dr. Ajayi is a hospitalist and pediatric palliative medicine physi cian at Rady Children’s Hospital San Diego; serves as the Director of Diversity Initiatives and a Senior Staff Scientist in Digital Medicine at the Scripps Research Translational Institute; and is the co–medical director of adult palliative medi cine at Scripps Mercy Hospital San Diego; and
WHEREAS, Dr. Ajayi’s research focuses on opportunities at the intersection of novel digital medicine technologies and unmet needs in maternal fetal health as well as pain and palliative medicine and she is a member of the Pediatric Opera tions Task Force and on the Digital Health Technologies committee of the All of Us Research Program with the National Institutes of Health as well as the Palliative Care Research Cooperative; and
WHEREAS, Dr. Ajayi is SDCMS’ 152nd President, its 9th female President, and the first Black woman to hold the position in the organization’s long history and during her Presidency, Dr. Ajayi plans to prioritize physician wellness as she works with the medical community to address the impact of systemic racism and bias on the most vulnerable and least served patients
Congratulations to Dr. Ajayi on this latest honor.
by
SDCMS CEO Paul Hegyi; former SDCMS president Holly B. Yang, MD; Supervisor Nathan Fletcher, chair of the San Diego County Board of Supervisors; SDCMS President Toluwalase Ajayi, MD; SDCMS Director Kyle P. Edmonds, MD, who is also Dr. Ajayi’s spouse; SDCMS President-elect Nicholas (Dr. Nick) Yphantides, MD, MPH; and SDCMS Secretary Steve Sang-Hyun Koh, MD, MPH, MBA were present at the presentation of the proclamation honoring Dr. Ajayi.
SANDIEGOPHYSICIAN.ORG 3
(858) 569-0300 www.soundoffcomputing.com TRUST A COMMON SENSE APPROACH TO INFORMATION TECHNOLOGY Trust us to be your Technology Business Advisor HARDWARE SOFTWARE NETWORKS EMR IMPLEMENTATION SECURITY SUPPORT MAINTENANCE Endorsed
SDCMS LEADERSHIP
SDCMS’s First Physician Social Networking Mixer in 3 Years Is a Huge Success!







Our physician networking mixer in July at Stone Brewing World Bistro & Gardens in Liberty Station was a wonderful success, with more than 75 physicians and their guests attending. As our first mixer since the pandemic, it had special meaning to see so many familiar faces and so many new ones come together to mingle, socialize, and network. We hope you’ll be able to join us at our next mixer later in the year!

4 SEPTEMBER 2022







SANDIEGOPHYSICIAN.ORG 5
A New Epidemic: Hepatitis C
San Diego County Implements a Plan to Eliminate Hepatitis C by 2030 BY ROBERT G. GISH, MD

THE LEADERSHIP OF THE Public Health Services (PHS) department in the County of San Diego Health and Human Services (HHSA) saw the opportunity to use the playbook from the Getting to Zero Initiative to develop a similar strategy for hepatitis C (HCV). “Working with community partners is how public health goals are achieved,” said Wilma Wooten, MD, MPH, County Public Health Officer. “This initiative is one of three elimination initiatives currently being implemented by the local public health department, in collaboration with many community partners. It is yet another example of how collective impact can be achieved when the County of San Diego Health and Human Services collaborates
with community partners, including the healthcare sector and others.”
The planning process to develop the Eliminate Hepatitis C San Diego County Initiative started in November of 2018 after the County of San Diego Board of Supervisors authorized HHSA’s PHS staff to develop the initiative with community stakeholders. This effort resulted in the board approving the recommendations in March of 2020 and approving an imple mentation plan in July 2021. HHSA con tracted with the Liver Coalition of San Diego County to serve as the convener of the partnership. The primary outcome of the Eliminate Hepatitis C San Diego County Initiative is to achieve an 80% de crease of incidence of chronic HCV and a 65% reduction in HCV mortality by 2030.
The plan has nine overarching recom mendations (www.endhepcsd.org):
1. Promote awareness of HCV as a major public health concern.
2. Implement prevention strategies in alignment with current best practices.
3. Screen for HCV in line with the rec ommendations of the U.S. Preventive Services Task Force (USPSTF), Cen ters for Disease Control and Preven tion (CDC), and best practices.
4. Ensure all individuals with HCV are linked to care and treatment.
5. Build capacity within the existing workforce to treat patients in diverse health care environments.
6. Ensure individuals with HCV have access to direct-acting antivirals (DAAs).
6 SEPTEMBER 2022
7. Ensure adequate surveillance, evalu ation, and monitoring.

8. Pursue policies in alignment with the World Health Organization (WHO)/ CDC that will help achieve elimina tion.
9. Support HCV research, implementa tion science, and operation research.
Treatment for HCV Has Advanced Greatly and a Cure Exists
First described as “non-A, non-B” hepa titis in the 1980s, the hepatitis C virus is a blood-borne pathogen transmitted through contaminated blood transfu sions, non-sterile medical procedures, tattoos, organ transplantation, intrave nous drug use (IVDU), and rarely through sexual contact or sharing of personal
care implements such as razors or tooth brushes. The CDC estimates that before the implementation of screening of the blood supply and the wave of universal precautions after the HIV epidemic, there were >300,000 incident cases per year in the U.S. Population-based surveys have shown that baby boomers (those born between 1945 and 1965) have an HCV seroprevalence that is three- to five-fold higher than the general population. Hence the CDC’s recommendation in 2020 to offer all adults a one-time screen ing for HCV without prior acquisition of risk. [1] This was followed by California State Law (AB 789), signed in October 2021, that mandates offering HCV testing to all adults.
Since 2000 in San Diego County more than 2,500 cases per year of chronic HCV have been reported, and an estimated 55,000 individuals with a history of HCV infection are currently living in San Diego County. [2] From 2015 to 2020, HCV was listed as an underlying cause of an average of 60 deaths per year in San Diego County.
In recent years, fueled by the opioid epidemic, >80% of new infections occur in people who inject drugs (PWID). The result is a very different looking epidem ic: a bimodal age distribution with one peak in the 20- to 30-year-old range, and another in baby boomers, currently aged 54–74 years. Parallel to the increase in HCV infection in women of child-bearing age is the recent increase in number of newborns who acquire the infection from their mothers. [3] It is believed that only 50% of the estimated 3 million prev alent infections have been diagnosed. [4] Through the lens of a cascade of care, the large drop from those suspected of having HCV to those diagnosed indicates we will not reach our elimination efforts by 2030. This cascade of care concept ap plies to children and adolescents as well as to adults; all infants born to high-risk mothers should be screened for HCV, given that about 5% of infected mothers transmit to their offspring. [5] Despite the great advances in HCV therapies, with cure rates of over 98%, if patients are not identified and linked into care and treatment, then they cannot benefit from the cure, no matter how simple, safe, and
effective the treatment. The time to act is now for all primary care providers to become involved with HCV testing and linkage to care. Pharmacists are also a cornerstone of HCV testing and linkage.
Historically, HCV treatment relied on interferon and ribavirin, and in 2010 the addition of a protease inhibitor, a course that typically lasted a year, came with many potentially severe side effects requiring careful patient selection and intensive monitoring, and with cure rates of only 50–70%. Because of the intensity of side effects and necessary patient support, typically only those with advanced liver fibrosis were offered therapy, and only highly specialized centers were able to handle the complexi ties of triaging, prescribing, and manag ing these therapies. [6] This meant that a basic component of treatment evalua tion was a liver biopsy — an expensive, invasive, specialized procedure that many patients declined. It is no surprise that estimates of the HCV care cascade showed only 16% of people with HCV infection received treatment and only 9% were cured as of 2014. [4] Liver biopsies are rarely performed today as fibrosis stage can easily be evaluated with imag ing and blood tests such as the aspartate aminotransferase to platelet ratio index (APRI) and fibrosis-4 (FIB4) index from liver enzymes and platelet counts, as well as proprietary testing such as the enhanced liver fibrosis (ELF) test and FibroSure/Fibrotest.
A Changing Diagnostic and Therapeutic Landscape
Enter two profound innovations that have dramatically changed the clini cal and treatment landscape and made HCV treatment primed for adaptation to primary care: noninvasive fibrosis assessment via liver elastography, and short-course DAA treatment regimens.
Liver elastography is a technology similar to ultrasound that allows a clini cian to assess liver damage at the bedside with a noninvasive, rapid, painless pro cedure that takes less than 10 minutes. The technology was developed and wide ly used in Europe more than a decade ago and has been available in the U.S. since 2012. DAA therapies were first used
SANDIEGOPHYSICIAN.ORG 7
McAlister Institute’s Medical Director, Dr. James Dunford, pictured with HR Operations Director Embrie Tapia (center) and Executive Director Marsa Varond (right).

Organized for Success
The Eliminate Hepatitis C San Diego County Initiative uses a collective impact model. The initiative has six committees: Steering Com mittee, Task Force Committee, Awareness and Prevention Committee, Linkage and Testing Committee, Surveillance Committee, and the Treatment Committee.
Join the Treatment Committee
The Treatment Committee, co-chaired by Christian Ramers, MD and Richard Dun ford, MD, is largely composed of clinicians, pharmacists, and other direct service staff who work with agencies that offer HCV treatment. Of the nine overarching recom mendations in the Implementation Plan, this committee focuses on two of the recom mendations: (5) Build capacity within exist ing workforce to treat patients in diverse healthcare environments; and (6) Ensure individuals with HCV have access to directacting antivirals. The full Implementation Plan is available at Eliminate-Hepatitis-CInitiative-Implementation-Plan-Board-ofSupervisors-7.13.21.pdf (livercoalition.org).
The Treatment Committee meets monthly; visit www.endhepsd.org for more information.

This initiative is currently funded by the County of San Diego, Health and Human Services Agency. Additional funding is provided by unrestricted educational grants/support to the Liver Coalition of San Diego — the convening agency — by AbbVie, Inc. and Gilead Sciences.
in 2013 in combination with interferon and ribavirin, but in the last 5 years have evolved into all-oral, highly effective, 8- to 12-week regimens with cure rates >98% in most cases, and safety profiles that often do not even require on-treatment monitoring. [7] They have rapidly become the standard of care and have enabled treatment to occur in primary care and other settings. These agents are approved for all, including those in the pediatric age group (3 years and older). [8] There are rare drug-drug interactions, and the dosing is eight–12 weeks with three tablets or one tablet per day.
These innovations coupled with steep drops in drug pricing and elimination of payer restrictions in California have al lowed HCV to be safely and easily treated in the primary care setting. California’s Department of Health Care Services ini tially had a policy restricting HCV thera pies in the Medi-Cal program on the basis of liver fibrosis, provider specialty, as well as the presence of concomitant drug and alcohol abuse. The most recent iteration of this policy has entirely removed these restrictions [9] and allows HCV treatment to be started on the same day as diagnosis in many cases using HCV antibody test ing and HCV RNA quantitative poly merase chain reaction (PCR). The need for genotype testing is now gone.
New and Emerging Models of Care In response to this new epidemic and with new diagnostic and therapeutic tools at hand, the need for a new ap proach to screening and linkage to care, treatment algorithm simplification, and integration with other services was self-evident. Although electronic-healthrecord-based HCV testing prompts have proven largely successful for the older baby boomer cohort — the Veterans Administration (VA) health system has screened >85% of their age cohort — there has been less success in screening and diagnosis in the younger, more recently infected PWID. Many reasons may help explain this difficulty: the long clinically latent period, the often asymptomatic nature of this disease, their low rates of interaction with the medical care system, and other competing priorities such as homelessness, poverty, addiction, and mental health challenges.
Traditional models of care wherein
8 SEPTEMBER 2022
patients may be screened in primary care settings and referred to gastroenterology, infectious disease, or hepatology offices have significant limitations, particularly for the younger patients with HCV who have new infections. Several models have emerged in response to these new needs. Co-location of services at a primary care clinic is one model that allows patients to see a specialist in their patient-centered medical home and still benefit from an important array of integrated services. Another model, known as the “Project ECHO” model, uses telehealth to link a multidisciplinary academic subspecialty team to rural and underserved primary care clinics in weekly didactic and case conference sessions. The ECHO model supports primary care providers with on going subspecialty consultation to help identify patients that require in-person specialty consultation. In an evaluation of ECHO, patients treated in primary care clinics in rural New Mexico had statisti cally equivalent cure rates compared with those treated in specialty settings.
[10] We need the full involvement of pri mary care providers now in HCV care.
A growing body of scientific literature has documented successful programs in real-world primary care settings with high HCV cure rates. Recent recom mendations from a consensus meeting endorse this approach of shifting HCV treatment to the primary care setting. Furthermore, the National Strategy for the Elimination of Hepatitis B and C notes in one of its key recommendations: AASLD [American Association for the Study of Liver Disease] and IDSA [Infec tious Disease Society of America] should partner with primary care providers and their professional organizations to build capacity to treat hepatitis B and C in primary care. Pharmacists have taken a major role in medical care settings such as the VA. [11]
Experiences of Local Primary Care Providers
Jim Dunford, MD, is the medical direc tor of McAlister Institute, a regional
substance treatment provider; emeritus professor of emergency medicine at UC San Diego; former medical director of the City of San Diego EMS system; and previous chair of the City of San Diego Clean Syringe Exchange Program. Dr. Dunford notes, “A recent longitudinal cohort study demonstrated the value of oral DAA on liver disease and mortality in a traditionally very difficult-to-reach population with HCV. [12] From 2006 to 2019, investigators followed 1,323 PWID (34% HIV-positive) in Baltimore as DAA became progressively more available. The HCV RNA positivity rate fell from 100% to 48%, and cirrhosis (based on serial elastography) decreased from 19% (2015) to 8% (2019). Undetectable HCV RNA was associated with an adjusted hazard ratio of 0.54 for all-cause mortal ity and 0.28 for cirrhosis. Remarkably, although the study did not provide treat ment, 39% of the participants self-report ed receiving HCV treatment by 2019. This study should cause all physicians who care for PWID to rethink their beliefs
Yet another of California’s medical liability insurers has transitioned from focusing on doctors to focusing on Wall Street. This leaves you with an important question to ask: Do you want an insurer that’s driven by investors? Or do you want an insurer that’s driven to serve you— one that’s already paid $140 million in awards to its members when they retire from the practice of medicine?
Join us and discover why delivering the best imaginable service and unrivaled rewards is at the core of who we are.
SANDIEGOPHYSICIAN.ORG 9
WHOSE INTERESTS does your malpractice insurer have at heart? Exclusively endorsed by
regarding the feasibility of significantly improving the health of even the most complex patients with HCV.”
Treatment in the primary care setting is likely to keep patients closer to other complementary services that may not be offered in specialty offices, such as addiction and mental health treatment and harm reduction services. The U.S. National Strategy for the Elimination of Hepatitis B and C further recommends: The most effective way to prevent hepa titis C among people who inject drugs is to combine strategies that improve the safety of injection with those that treat underlying addiction. The strategy docu ment further states: States and federal agencies should expand access to syringe exchange and opioid antagonist therapy in accessible venues [11].
Dr. Adla Tessier, a family practice physician who practices at the La Maestra Health Centers of San Diego, in City Heights, treats HCV infection in her primary care practice. Dr. Tessier describes her experience this way: “It is very gratifying to be able to treat and cure hepatitis C in the primary care setting. Working closely with Dr. Robert Gish as a consultant as well as a mentor has expanded our knowledge to provide in-house specialty care and thereby im prove timely access and linkage to care. Our Liver Clinic team works closely with our other departments, such as our ad diction program and outreach programs, in facilitating much needed care for our vulnerable population. Having the ability to cure these patients and the feedback provided by our patients and family makes this a very rewarding experience.”
Primary and Specialty Care: Finding the Balance
The ECHO model is one specific way to define the relationship between primary care and specialty care, but the principles of collaboration need not be limited to one specific program. [13] At La Maestra, where I’m the medical director, we now have several providers offering treat ment at multiple locations and can get patients in for an initial appointment within a week throughout the U.S. We can treat most patients immediately — from no fibrosis to compensated cirrhosis, but advanced liver disease and certain comorbidities definitely benefit from
liver specialist care, especially if liver transplant or liver cancer is part of the care spectrum. There are some innovative telemedicine opportunities that can help those patients that are in remote areas where specialty care is out of reach.

Dr. Kathleen Schwarz is a pediatric hepatologist on the staff of UCSD/Rady Children’s Hospital. She has played a na tional leadership role in developing treat ments for children and adolescents with HCV. She is currently treating pediatric patients at the Rady Pediatric Liver Center but is happy to work with primary care physicians to provide advice regarding treatment in the primary care setting.
There are not enough liver specialists in the country to care for all the people who need HCV testing and the patients with HCV that need treatment. Given the safety and ease of HCV treatment in the DAA era, it makes sense for patients to be treated by their primary care physi cians and pharmacists with whom they have had a long-term relationship. Shifting some of the burden of HCV treatment to primary care physicians and pharmacists will also allow patients with more advanced disease to access specialty hepatology care where proce
dural and transplant expertise is really needed. We continue to educate patients and providers that liver function test (LFT) terminology has been updated. Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are not LFTs; these are liver enzymes the denote inflammation but not function. Albumin bilirubin and international normalized ratio (INR) are the key LFTs. Staging liver disease to start liver cancer surveillance is also key and diagnosing metabolicassociated liver disease (MAFLD, also known as non-alcoholic fatty liver dis ease [NAFLD] or non-alcoholic steatohep atitis [NASH]) is also essential alongside alcohol use disorder and substance use disorder for the more complete care of the liver patient.
References
1. Centers for Disease Control and Prevention. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR. 2012;61: 1-32.
2. Wynn A, Tweeten S, McDonald E, Wooten W, Lucas K, Cyr CL, et al. The estimated hepatitis C seroprevalence and key population sizes in San Diego
10 SEPTEMBER 2022
in 2018. PLOS ONE 2021;16(6):e0251635.
3. Epstein RL, Espinosa C. Hepatitis C virus in neonates and infants. Clin Perinatol. 2021;48(2):343-357. doi: 10.1016/j.clp.2021.03.007
4. Yehia BR, Schranz AJ, Umscheid CA, Lo Re V. The treatment cascade for chronic hepatitis C virus infection in the United States: a systematic review and meta-analysis. PLoS One 2014;9(7):e101554. doi: 10.1371/journal. pone.0101554
5. Rogers ME, Balistreri WF. Cascade of care for children and adolescents with chronic hepatitis C. World J Gastroenterol. 2021;27(12):1117-1131. doi: 10.3748/wjg.v27.i12.1117

6. Drenth JPH. HCV treatment—no more room for interferonologists? N Engl J Med . 2013;368:1931-1932.
7. American Association for the Study of Liver Diseases and Infectious Diseases Society of America. HCV guidance: recommendations for test ing, managing, and treating hepatitis
C. Published September 21, 2017. Accessed February 4, 2019. https:// www.hcvguidelines.org/evaluate/ when-whom
8. Schwarz KB, Rosenthal P, Murray KF, Honegger JR, Hardikar W, Hague R, et al. Ledipasvir-sofosbuvir for 12 weeks in children 3 to <6 years old with chronic hepatitis C. Hepatol ogy. 2020;71(2):422-430. doi: 10.1002/ hep.30830
9. California Department of Health Care Services. Treatment policy for the management of hepatitis C. Updated December 9, 2021. Accessed August 2, 2022. https://www.dhcs.ca.gov/pages/ hepatitisc.aspx
National Strategy for the Elimination of Hepatitis B and C. Washington DC: The National Academies Press.
12. Cepeda JA, Thomas DL, Astemborski J, Rudolph JE, Gicquelais R, Kirk GD, et al. Impact of hepatitis C treatment uptake on cirrhosis and mortality in persons who inject drugs: A longitudi nal, community-based cohort study. Ann Intern Med. Published online July 12, 2022. doi: 10.7326/M21-3846

13. Ramers CB. Sharing the task at hand: San Diego frontline physicians an swer the call for hepatitis C elimina tion. San Diego Physician . 2019; 6-10.
10. Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med . 2011;364(23): 2199-2207.



11. National Academies of Sciences, Engineering, and Medicine. (2017). A

Vista Community Clinic has outstanding opportunities for Full-Time and Part-Time Physicians. We are looking for dedicated, motivated and enthusiastic team players who want to make a difference in the community.


Vista Community Clinic is a federally qualified, not-for-profit healthcare clinic with more than 800 employees and nine state-ofthe-art clinics treating more than 69,000 patients every year. We provide healthcare throughout the Southern California regions of North San Diego, Orange and Riverside Counties.

Our compensation and benefits program includes: Competitive compensation, sign-on bonus, relocation bonus, health, dental, vision, company-paid life, longterm disability, flexible spending accounts , 403(b) retirement plan, malpractice coverage, NHSC loan repayment eligible organization, CME allowance, and no oncall hours


For more information visit www.vcc.org or email hr@vcc.org EEO
SANDIEGOPHYSICIAN.ORG 11 PLACE YOUR AD HERE Celebrating 150 Y Artificial Intelligenceand Medicine THE DEBATE Celebrating 150 How to BUILD DIABETES Reversing the Risks DEMENTIA Reducing the Burden GUN SAFETY Engaging Patients BREAST CANCER Preventing Deaths PREVENTION Contact Jennifer Rohr 858.437.3476 • Jennifer.Rohr@SDCMS.org Dr. Gish teaches at UC San Diego Skaggs School of Pharmacy and Pharmaceuti cal Sciences, University of Nevada, and is a medical director of the Hepatitis B Foundation and Asia Pacific Health Foun dation. He is an adviser for the National Viral Hepatitis Roundtable that has a key role in changing HCV policies in the U.S.
Join a team that’s been helping to redefine what it means to be a community clinic for 50 years.
The Unknown Specialty!
BY CHARLES D. LEE, MD, JD, MBA
WE ALL KNOW OF THE various medical special ties and subspecialities we heard about in medi cal school. In fact, we rotated through the primary ones: surgery, medicine, pediatrics, radiology, pathology, and a few electives. Naturally, students can not be exposed to all options, especially unusual subspecialities (think aerospace medicine as one example). This is un fortunate because we tend to make our career choices based upon the one’s own experience.
Today I want to talk to you about a new specialty that I doubt you have ever con sidered. For the past 50 years, correction al medicine has grown from a backwater corner to an upfront option that can be considered by physicians at all stages in
their careers. In fact, the Accreditation Council for Graduate Medical Education (ACGME) is proposing it to be listed in its directory as a recognized specialty.
Correctional physicians see all types of medical, surgical, dental, and mental patients. No, they don’t need expertise in all of these disciplines, but must know how to manage them. Correctional medi cine resembles emergency medicine — another specialty with broad purview that existed for many years before it achieved recognition as a true specialty, deserving of its own accredited educa tional programs. Older physicians will remember when they rotated through emergency room settings without any special training.
We who work in jails and prisons are tremendously pleased with the ACGME
proposal; after it is approved, medical schools and major medical centers will develop accredited programs, benefit ting our patients and creating respect for those of us who work with the most needy group of citizens.
I am aware of only one residency train ing program for correctional medicine currently in existence. Medical schools (and training programs for physician assistants and advanced practice nurses) are beginning to expose students with rotations inside correctional settings. Those medical students I have met and mentored were surprised and enthusi astic with what they saw. Correctional medicine is an area whose time has come. How is this area unique and what is it? Most correctional docs are
12 SEPTEMBER 2022
CORRECTIONAL MEDICINE
primary care physicians and psychia trists, though other specialties are also represented. Patients in jails and prisons present with every illness seen in juve niles and adults, often without having re ceived adequate treatment in the outside community, if in fact any treatment at all was provided. Each new patient walking into an examination space can present with anything at all.
At the time an inmate is brought into a correctional setting, trained person nel, usually licensed nurses, develop an immediate sense of the patient’s current needs and past medical history. This fa cilitates immediate provision of care that is necessary. Correctional patients are unique in the United States inasmuch as

they have a constitutionally protected right to receive reasonable care neces sary to manage their serious medical conditions. Intake and point-of-entry screening begin the process of delivering this care.

Correctional patients demonstrate the same type of needs as do community pa tients and need a process to access care, to make their needs known. In some set tings this is accomplished through the use of digital kiosks, other times through written requests, and in others through conversation during routine nursing
consider third-party payers or fear that their patient may be lost to follow-up.
In correctional settings emergency services must be available 24/7. Depend ing upon the size and type of the facility, this is typically provided through a mix of on-site and local hospital services, sometimes including the local EMS sys tem. Hospitalization, when necessitated by a patient’s needs, is available.
Most patients in jails and prisons come from disadvantaged backgrounds. Whether due to race or ethnicity, lack of knowledge, or low socioeconomic status, they have neglected their health. Like all physicians, those working in correc tional medicine need to remember that every patient should be approached with respect, and that every patient is doing the best that they can. We clinicians also need to remember that upward of 90% of those experiencing incarceration will return to society, where they will, hope fully, become contributing members.
rounds. Typically nursing personnel triage the requests, responding within specified timeframes with interventions guided by the nursing process and treat ment protocols. This may include timely referral to on-site services or even to local hospital emergency departments. Inmates experience a higher preva lence of chronic diseases than are seen in community patients. When amenable to treatment, these patients are seen on schedules developed in accordance with various national guidelines promul gated by national organizations. Care for chronic diseases inside correctional settings tends to exceed the quality of care in the community, if only because the correctional clinicians do not need to
Those of us in correctional medicine are privileged. We went into medicine because we wanted to take care of pa tients. In this area of medicine, we can be dedicated to providing care as needed and experience the satisfaction of watch ing our patients’ conditions improve, and never have to submit bills or fight with insurance companies. We work as team members, with other dedicated profes sionals — registered and licensed nurses, dentists, physical therapists, and so on. And because most of our patients will re turn to life outside correctional facilities, the work we do is critical both inside and outside of our jails and prisons.
More information about correctional medicine can be found on the Ameri can College of Correctional Physicians (ACCP) website (www.accpmed.org).
Dr. Lee is the president of the American College of Correctional Physicians. He is a retired physician who practiced radiology in San Diego from 1980 to 1999 and served as the co-chair of the Medical-Legal Com mittee for SDCMS. Dr. Lee began working in corrections in 2001 and was medical director at the Salinas Valley state prison in Monterey County for 10 years. He now audits correctional facilities all around the country.
SANDIEGOPHYSICIAN.ORG 13
As Telemedicine Best Practices Emerge, Assess Your Practice
 BY DAVID L. FELDMAN, MD, MBA, FACS
BY DAVID L. FELDMAN, MD, MBA, FACS
EARLY IN THE PANDEMIC,
I heard an obstetrician say that a medical setting was the last place many patients were willing to go. As a result, he was checking on prenatal patients using telemedicine. With questions about standard of care in mind, I gathered obstetric leaders into a meeting group where providers discussed ways to safely utilize phone and video modalities to continue prenatal care be yond the pandemic. Would this modality, necessary in a time of crisis, be continued in the “new normal”?
Many specialties, facing the pandemic’s imperative to improvise, formed similar discussion groups, which are now dissem inating their findings via peer-reviewed medical journals or formulating best practices with their medical professional
societies. Fortunately, each specialty’s findings have connotations for patients in a variety of settings. With 2020’s spike in telemedicine visits followed by 2021’s con tinued record-breaking increases, we now know a surprising amount about how to safely provide telemedicine care.
As practices and hospitals work to inte grate their telemedicine platforms more smoothly into their workflows, this mo ment calls for us to reconsider how we are using telemedicine relative to care access, quality, safety, and the core principles of patient-centered care.
Specialty Example: Obstetrics
Obstetricians monitor risk indicators like blood pressure and blood glucose, which help them intervene early in cases of preeclampsia and/or gestational
diabetes. With the increasing availability of at-home monitors for blood pressure and blood glucose, the option to collect at-home metrics (which, admittedly, some patients do more reliably than others) shows how remote care can sometimes be safer and/or more accessible care.
Surprisingly, I’ve heard obstetricians say they value telemedicine most with their high-risk patients, simply because it facilitates more frequent conversa tions. This finding also turns up in other specialties.
Specialty Example: Otolaryngology
As in obstetrics, the physical exam needs of otolaryngology might seem impervious to many telemedicine advancements. Yet the author of a 2020 JAMA article argued to his colleagues, “We must rediscover
14 SEPTEMBER 2022
RISK TIP
the nuances of palpation and noninvasive inspection. Substantial portions of this examination can be completed without instrumentation or prior experience.” The person without prior experience is the patient: “The clinician can provide instructions to the patient for sequen tial elements of the examination and then verify correct performance of each maneuver.”
This collaborative spirit (which the author frames in terms of what Eric Topol, MD, of Scripps, has called the “activated patient”) aligns with the core principles of patient-centered care: “Patients are partners with their healthcare provid ers.” This partnership — facilitated by the practitioner while considering the patient’s emotional, social, and financial perspectives — is more than a remote-
care convenience: “The activated patient is empowered to participate in their care in a manner hitherto unappreciated, and in so doing, they may well enjoy greater engagement and satisfaction.”
Specialty Example: Surgery
Surgical specialties present an unex pected number of opportunities for remote care, from consultative conversa tions all the way through postoperative evaluations. For instance, many post-op evaluations can relocate to the telemedi cine space, where questions like how the wound looks and drain output can be evaluated.
Such uses of telemedicine, when ap propriate, improve the patient experience, and sometimes patient safety. After all, post-op patients don’t want to leave home, and sometimes safety is an issue. I know I’m not the only one who has ever made a house call during icy weather. If we use good clinical judgment, we can offer a version of the post-op house call to some patients with arguably comparable or improved patient safety.
Reducing Medical Malpractice Risks
Some of the state-to-state restrictions lift ed early in the pandemic have resumed, so check with the relevant state medical licensing boards. It remains important to know where your patients are: Practicing medicine without a license is still illegal, and your medical malpractice insurer cannot cover you if you were doing some thing criminal, even inadvertently.
We still see few medical malpractice lawsuits related to telemedicine, but those we do see mostly connect to diagnostic errors. Of course, the physical exam still matters: Even with workarounds and patient-assisted maneuvers, sometimes we need to lay hands on the patient. More over, since diagnostic errors often derive from communication gaps, we must remain mindful of the ways in which telemedicine amplifies communication challenges.
That said, some methods of mitigat ing diagnostic error risks are contained within our challenge to embed tele medicine within workflows. Systems that require the physician to fulfill the role of a tech support professional and/or medical
assistant increase cognitive load. Such distractions increase the chances that a significant symptom will be overlooked. Further, systems that make it difficult to track referrals or test results amplify diag nostic risks.
Therefore, better integrating telemedi cine appointments into workflow serves both provider sanity and patient safety by optimizing patient-provider commu nication. You can engage experts like my colleagues at Medical Advantage to help your practice with this process.
Telemedicine for PatientCentered Care

A recent survey found that 62% of re sponding organizations are expanding their telehealth programs, versus being in maintenance mode. This is the perfect time to rethink both what we need to do in person and how frequently we need to do it (e.g., ultrasounds during pregnancy), while accounting for the increasing availability of at-home gadgets, such as otoscopes and ultrasound solutions.
Gadgets are one of the many aspects of telemedicine that raise questions about patient access to care. Patient safety researchers extol the virtues of programs that reduce device costs for patients in need, and they also promote reimburse ment for providers who offer the substan tial technology education and orienta tion some patients need to function as activated patients within the telemedi cine landscape. Integrating translation services into virtual visits will also have an impact.
The access question is two-sided, because for every patient who could not access a telemedicine visit for lack of bandwidth or because they live in crowded conditions without privacy, there is a patient who could access their visit only because remote care comes without the price tag of childcare, trans portation, or a missed shift. Despite its difficulties, telemedicine is a net gain to our armamentarium for providing patient-centered care.
Dr. Feldman is chief medical officer of The Doctors Company and TDC Group, and senior vice president of Healthcare Risk Advisors.
SANDIEGOPHYSICIAN.ORG 15
Active Treatment for Extremely Preterm Babies on the Rise
Yet Researchers Find Racial and Ethnic Disparities in Treatment Initiation BY AMANDA D’AMBROISIO
BABIES BORN EXTREMELY preterm were more likely to receive active treatment in recent years, but there were gaps in treatment among different racial and ethnic groups, according to a crosssectional study.
From 2014 to 2020, the proportion of extremely preterm infants who received active treatment rose nearly 4% each year (45.7% to 58.8%), increasing in all racial and ethnic groups, reported Kartik K. Venkatesh, MD, PhD, of the Ohio State University College of Medicine in Colum bus, and colleagues.
The frequency of active treatment increased in all gestational age groups, and most rapidly among babies born in week 22 of pregnancy, at an average in crease of 14.4% per year in the study time period (from 14.0% to 29.7%), they stated in JAMA
However, babies born to white individu als were more likely to undergo treatment compared to those born to Asian or Pacific Islander, Black, or Hispanic people. The authors stated that in “2019, 66% of perivi able neonates were born to a mother who identified as either non-Hispanic Black or Hispanic,” and said “one possible explana tion for variations in active treatment in the periviable period by race and ethnic ity may be differing decisions of clinicians and families when faced with the high likelihood of morbidity and mortality and predictive uncertainty.”
In an accompanying editorial, Henry Lee, MD, and Deirdre Lyell, MD, both of the Stanford University School of Medi
cine in California, noted that more data are needed about treatment efficacy and prognosis. They added a lack of data de scribing an infant’s individual morbidity and mortality risk after active treatment creates barriers to effective counseling, as the definition of active treatment is un clear and dependent on the region where a patient receives care, the level of care at a hospital, and the individual family.
“Unlike other interventions that may be considered appropriate or optimal for a broad population, it is challenging to characterize active treatment and its components for the extremely prema ture population as always the ‘right’ treatment, given the uncertainties in the likelihood of survival and survival without morbidity,” they stated. “Qual ity care in this context should be viewed not as a simple matter of pursuing active treatment but rather as the optimal alignment of treatment, prognosis, and the values of the mother and family.”
The serial cross-sectional study obtained data on live births between 2014 and 2020 with data from the U.S. National Vital Statistics System Natality Files. Venkatesh’s group collected data from all live births, defining periviable births as infants born between 22 weeks and 25 weeks and 6 days’ gestation. The researchers excluded infants who were not U.S. residents and those with clinical anomalies.
They analyzed the proportion of neonates who received active treatment, which included interventions such as surfactant therapy, immediate assisted
ventilation at birth, assisted ventilation for more than six hours, and antibiotic therapy during neonatal ICU admission. They adjusted for covariates including maternal education, insurance status, year of delivery, age, parity, prepreg nancy BMI, preterm birth, gestational diabetes, infant birthweight, and sex, among others.
Of nearly 27 million live births in the U.S., approximately 62,000 extremely preterm neonates were included in the final analysis. The median maternal age was 28, and 54% of births were covered by Medicaid.
Around 5% of the infants in the study were Asian or Pacific Islander, 37% were Black, 24% were Hispanic, and 34% were white.
Of all periviable births, just over half received active treatment. Approxi mately 45% who received active treat ment underwent surfactant therapy, 96% immediate assisted ventilation at birth, 60% assisted ventilation for more than six hours, and 47% antibiotic therapy.
Compared to infants born to white in dividuals, those born to Asian or Pacific Islander (adjusted risk ratio [aRR] 0.82, 95% CI 0.79–0.86), Black (aRR 0.90, 95% CI 0.89–0.92), or Hispanic (aRR 0.83, 95% CI 0.81–0.85) individuals were less likely to receive active treatment. Infants born to people of color who were also delivered at 23, 24, and 25 weeks’ gestation were all significantly less likely to receive active treatment.
Study limitations included the lack of assessment of neonatal morbidity and mortality. Also, the researchers did not include stillbirths in the analysis, which raises the possibility for selection bias regarding the coding of deliveries as live births or stillbirths. And previous stud ies have had varying definitions of active treatment, the authors pointed out.
Amanda D’Ambroisio is a reporter for MedPage Today, where this article first appeared, and is on its enterprise and investigative team. She covers obstetricsgynecology and other clinical news, and writes features about the U.S. healthcare system.
16 SEPTEMBER 2022
PEDIATRICS
CDC: Paralytic Polio an Ongoing Risk for the Unvaccinated
No Additional Cases Identified, but Wastewater Testing Continues to Detect the Virus BY INGRID HEIN
NO ADDITIONAL U.S. CASES of poliomyelitis have been identified, according to a new CDC report detailing the nation’s first case in nearly a decade, but wastewater specimens in multiple New York counties indicate community trans mission and ongoing risk for paralysis in the unvaccinated.
Following stool sample testing, poliovirus was confirmed in June in an unvaccinated young adult from Rockland County, New York, representing just the second case of local transmission in the U.S. since 1979.

The patient had initially experienced fever, neck stiffness, gastrointestinal symptoms, and weakness in the limbs, and was hospitalized for possible acute flaccid myelitis (AFM), reported Ruth Link-Gelles, PhD, of the CDC’s Domestic Poliovirus Emergency Response Team and colleagues in the Morbidity and Mor tality Weekly Report
As part of national AFM surveillance, the New York State Department of Health reported the case to the CDC in July.
The patient was possibly exposed eight
days before symptoms started while attending a large gathering. The patient first experienced limb weakness on day three, and on day five, the patient was admitted to the hospital. Poliovirus type 2 was detected in the patient’s stool on days 11 and 12, and on day 16, the patient was discharged to rehabilitation.
As of this month, 260 wastewater samples from treatment plants in Rockland and Orange counties were tested for poliovirus, including samples that had been collected to test for SARS-CoV-2. Of these samples, 21 yielded positive results for poliovirus using RT-PCR and partial genome sequencing, including 13 from Rockland County and eight from Orange County.
Among wastewater samples col lected during May, June, and July, 20 specimens were genetically linked to poliovirus from the patient’s stool samples. Furthermore, one sample from April in Orange County was sequenced as poliovirus type 2, but the sequence was incomplete, which prevented the researchers from genetically linking the sample to the patient.
Further tests of wastewater collected 41 days after onset of the patient’s symp toms continued to detect the virus.
“The occurrence of this case, combined with the identification of poliovirus in wastewater in neighboring Orange County, underscores the importance of maintaining high vaccination coverage to prevent paralytic polio in persons of all ages,” Link-Gelles and colleagues wrote.
Three additional individuals have been classified as persons under investiga tion; however, available specimens have yielded negative results.
“Unvaccinated persons in the United States remain at risk for paralytic polio myelitis if they are exposed to either wild or vaccine-derived poliovirus; all persons in the United States should stay up to date on recommended poliovirus vaccina tion,” they noted.
According to the New York State Immu nization Information System, coverage with the three-dose polio vaccine among infants and children younger than 2 years living in Rockland County was 67% in July 2020, which decreased to 60.3% by this month. Zip-code-specific vaccina tion coverage was “as low as 37.3%,” noted Link-Gelles and coauthors.
Despite a brief increase in polio vaccination following an attempt by the Rockland County Department of Health to catch up the local population, “the number of doses administered at temporary and established clinics was not sufficient to meaningfully increase population [inactivated polio vaccine] coverage levels,” they added.
The origin of the virus found in the patient’s stool sample and in wastewater is unknown. However, “the patient’s stool samples indicates a chain of transmis sion within the United States originating with a person who received a type 2-con taining oral polio vaccine (OPV) abroad.”
Since the infected patient had not traveled internationally within the virus incubation timeframe, and the oral polio vaccine has not been part of routine im munization schedules in the U.S. since 2000, the origin of the virus is difficult to track.
Ingrid Hein is a staff writer for MedPage Today, where this article first appeared.
PUBLIC HEALTH
SANDIEGOPHYSICIAN.ORG 17
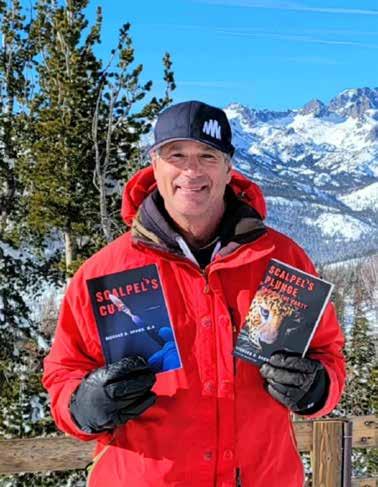
Local Doctor Richard Brown Releases Second Medical Thriller Novel to Benefit Charity
Scalpel’s Plunge: End of the Party Follows Success of His Debut Book BY SDCMS STAFF
 DEL MAR PHYSICIAN DR. RICHARD
DEL MAR PHYSICIAN DR. RICHARD
Brown wanted to write a novel for most of his adult life, but it wasn’t until his three children were grown that he fi nally decided to sacrifice his love of watching sports to spend time on fulfilling his long-held dream.
Dr. Brown’s first book, Scalpel’s Cut , was a medical thriller that focused on a massive financial fraud conspiracy inside a hospital but central to it was the day-to-day reality of being a physician. Dr. Brown self-published both novels and dedicated all pro ceeds from the first book to benefit Doctors Without Borders, the well-respected organization that provides medical services to those who need it most, from war zones to the poor est areas on the planet. His fundraising goal was $20,000 ini tially but he more than doubled it to $44,000 through both book sales and donations by enthusiasts for his literary endeavor.
The orthopedic hand surgeon relied on word of mouth and giving away copies of the book to family, friends, and colleagues to publicize his book. Dr. Brown’s latest novel is also benefitting Doctors Without Borders, and he’s determined to raise even more this time for the nonprofit group. The latest book is avail able on Amazon in both paperback and digital formats, and will be released as an audiobook.
The new book, Scalpel’s Plunge: End of the Party is an actionpacked thrill ride that puts the medical elements in the back ground as its author focused on giving the reader an exciting and fast-paced entertainment experience, one that doesn’t take itself too seriously. Dr. Brown hopes readers will enjoy it as a fun beach read.
“There’s a lot more action in this book,” he says. The book hops around the globe, from the Sierra foothills to Boston to South Africa.
The book’s plot involves such disparate elements as the international drug trade, the Russian mafia, and a lifesaving treatment for the Ebola virus. The book’s pro tagonist, also an orthopedic surgeon, is named Erick “VJ” Brio, and is ensnared by a global crime syndicate.
Dr. Brown also brings in the experiences and knowl edge of his patients into his novels. In this one there is a critical rock climbing scene which the doctor, not a rock climber himself, relied on descriptions and experiences of patients
who are veterans of the sport. He also had visited South Africa but relied on interviews with South Afri can patients to help capture life in Cape Town, one of his novel’s key locations. “Basi cally, I used my patients as resources, which is fun,” Dr. Brown says.
Dr. Brown is now work ing on a third novel and writing treatments for his first two books as possible TV series on a streaming service such as Netflix. Brown balances that with his full-time career in or thopedic medicine, where he practices in both Del Mar and Mammoth Lakes.
Dr. Brown has no desire to switch careers, though. “I love being a doctor,” he says. “I enjoy writing, but I don’t want to do it full-time.” Brown and his wife, Ellen, also like to leave time for their love of the outdoors, whether it’s skiing or hiking with their dogs.
18 SEPTEMBER 2022
SAN DIEGO DOCTORS OF INTEREST
It’s My Calling
BY ADAMA DYONIZIAK
HOPE FOR THE BEST; PREPARE FOR THE worst. This is the best way to live your life, especially in medicine. Tackle the problem together and overcome it.” This is a favorite quote of Dr. Hung Nguyen, a urologist with Genesis Urology and a volunteer with Project Access San Diego since 2019. Dr. Nguyen continues, “The best thing about being a doctor is the instant connection and trust with a patient. This relation ship is very important and special because it starts the process to improve the patient’s quality of life.”
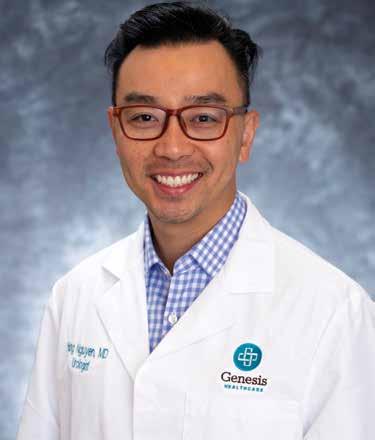
A first-generation Vietnamese immigrant, he emigrated to the US with his family. His parents instilled in him and his sister the importance of picking a meaningful career to improve the quality of life for other people. His family was from a poor, disadvantaged background, so he knows firsthand about lack of healthcare. His older sister was his role model, becoming an internal medicine physician. “As I was going through college, I was inspired by medicine. I didn’t lose interest or get bored — I was excited to learn about it every day. Now, it’s not
just my job, it’s my calling,” Dr. Nguyen says.
He originally pursued internal medicine to be a pulmonary critical care physician in the emergen cy room. During his surgery rotation, Dr. Nguyen found being in an operating room and working with his hands changed his life. He joined Genesis Urology to provide individualized urologic care to patients of North County San Diego. “Urology has a diversity of surgeries, which is exciting,” continues Dr Nguyen. He specializes in minimally invasive surgery and robotic surgery for treat ment of benign and malignant urologic disease. In addition, he has expertise in stone disease, male sexual dysfunction, and female urology.
As a Project Access volunteer, Dr. Nguyen meets patients who face language and resource barriers.
“My parents gave me the opportunity to learn in the U.S. and gain a comfortable lifestyle. As doc tors, we are more fortunate than other people. It is gratifying for me to make a difference through my work. If I don’t do it, who will?”
Magdalena M, a patient in her 30s with two chil dren, was so grateful to Dr. Nguyen for his time and for removing the kidney stones that caused her agonizing pain. Magdalena has returned to her regular schedule with her children and enjoys spending time with them. She gifted Dr. Nguyen and her Project Access care manager, Evelyn Pen aloza, with customized planters.
Dr. Nguyen is an avid traveler with his wife, Christine, whom he considers his good luck charm. When he isn’t globetrotting, he stays active by hiking, golfing, and playing with his French bulldogs, Gary and Peanut. He also dabbles in the culinary arts and loves to cook and barbecue. His current hobby is being an avid gardener of tropical fruit trees — cheri moya and calamondin — so he can have a slice of Vietnam in his backyard.

Since 2008, Project Access has facilitated $24 million in care for 7,500-plus uninsured patients by provid ing free consultations and surgeries — all thanks to the dedication, time, and talent of our volunteer specialty physicians. Offer your unique skill set to transform a life — volunteer your expertise by contacting us at adama.dyoniziak@championsfh. org or (858) 300-2780.
Adama Dyoniziak is executive director of Champions for Health.
CHAMPIONS FOR HEALTH SANDIEGOPHYSICIAN.ORG 19 “
Ignorance and Arrogance: A Dangerous Combination
BY HELANE FRONEK, MD, FACP, FASVLM, FAMWA
reassurance, as we tend to underesti mate the knowledge and intuition we gain from experience, often to our detri ment and risk.
Confirming this belief, we found our selves following a barge piloted by Joe, an older man with no boating experience who was accompanied by his wife and her parents — an even older man and a blind woman. It quickly became evident that Joe wasn’t up to the task. His barge whipsawed across the canal, occasion ally ending up perpendicular to and completely blocking the canal. Seeing his limited skills, members of our group repeatedly held his lines in the locks and offered suggestions to make his piloting more successful. He ignored our sugges tions and expressed no appreciation.
Near the end of our trip, we were sad dened to discover the dire consequences of his ignorance and refusal to accept guidance: Following Joe’s command to jump onto shore before it was safe to do so, his wife broke her leg and needed sur gery. Surgery is never ideal — certainly less so in a foreign country — and we were sorry this had happened.
THE CANAL DU MIDI, A 241 KM long canal through southern France, was built in the 17th century to transport goods between the Mediterranean Sea and the Atlantic Ocean. Now, it serves as a beauti ful route for vacationers to leisurely visit the charming towns in the area. Distinct from other luxurious barge trips in which your meals are cooked, the boat is piloted, and you are driven to wineries and other destinations, most barges on the Canal du Midi are staffed by vacation
ers themselves, as we recently did.
We enjoyed learning to negotiate the locks that allow the boats to travel along varied elevations; steering the boat through hairpin turns, bridges, and tunnels; and rectifying the unexpected problems that occurred along the way.
Fortunately, our “crew” included six able-bodied people, including two expe rienced boat captains. While the barge company stated that “no prior experience is necessary” to manage this voyage, I’ve learned to be suspect of such dismissive
The combination of ignorance and ar rogance is a dangerous one, and some thing we can easily fall prey to. Becoming a physician involves managing situa tions we initially feel unprepared to deal with, and we can easily come to believe we can do almost anything. This shows up in many ill-fated situations — from the internist who overestimates his abil ity to diagnose melanoma to the surgeon who refuses to call for help when she encounters complications in the operat ing room. By maintaining an awareness of our own limitations as well as the cu riosity to ask questions and willingness to request assistance or simply another opinion, we can learn and grow while avoiding many calamities and complica tions along the way. We left our vacation with many beautiful memories and a renewed belief in humility, all of which we will treasure in the years to come.
Dr. Fronek is an assistant clinical profes sor of medicine at UC San Diego School of Medicine and a Certified Physician Development Coach, CPCC, PCC.
20 SEPTEMBER 2022
PERSONAL AND PROFESSIONAL DEVELOPMENT
CLASSIFIEDS
VOLUNTEER OPPORTUNITIES
PHYSICIANS: HELP US HELP IMPROVE THE HEALTH LIT ERACY OF OUR SAN DIEGO COUNTY COMMUNITIES by giving a brief presentation (30–45 minutes) to area children, adults, seniors, or employees on a topic that impassions you. Be a part of Champions for Health’s Live Well San Diego Speak ers Bureau and help improve the health literacy of those with limited access to care. For further details on how you can get involved, please email Andrew.Gonzalez@ChampionsFH.org.
CHAMPIONS FOR HEALTH PROJECT ACCESS: Volunteer physicians are needed for the following specialties: endocrinol ogy, ENT or head and neck, general surgery, GI, gynecol ogy, neurology, ophthalmology, orthopedics, pulmonology, rheumatology, and urology. We are seeking these specialists throughout all regions of San Diego to support those that are uninsured and not eligible for Medi-Cal receive short term specialty care. Commitment can vary by practice. The mission of the Champions for Health’s Project Access is to improve community health, access to care for all, and wellness for pa tients and physicians through engaged volunteerism. Will you be a health CHAMPION today? For more information, contact Andrew Gonzalez at (858) 300-2787 or at Andrew.Gonzalez@ ChampionsFH.org, or visit www.ChampionsforHealth.org.
PHYSICIAN OPPORTUNITIES
INTERNAL MEDICINE PHYSICIAN: Healthcare Medical Group of La Mesa located at 7339 El Cajon Blvd is looking for a caring, compassionate, and competent physician for providing primary care services. We require well–organized and detail–oriented with excellent written and oral communication skills, and excellent interpersonal skills to provide high–quality care to our patients. We provide a competitive salary, paid time off, Health insurance, 401K benefits, etc. We provide plenty of opportunities to refine your clinical competency. Our CEO Dr. Venu Prabaker who has 30 years of teaching experience as a faculty at multiple universities Including Stanford, UCSD, USC, Midwestern, Western, Samuel Merritt, Mayo, etc. — will be providing teaching rounds once a week. You will also get plenty of opportunities to attend other clinical lectures at many of the 4–to–5–star restaurants in San Diego. We also have once a week– one–hour meeting for all the staff for team building and to create a “family atmosphere” to improve productivity and thereby create a win–win situation for all. Visit us at caremd.us.
ASSISTANT, ASSOCIATE OR FULL PROFESSOR (HS CLIN, CLIN X, ADJUNCT, IN-RESIDENCE) MED-GASTRO
ENTEROLOGY: Faculty Position in Gastroenterology. The Department of Medicine at University of California, San Diego, Department of Medicine (http://med.ucsd.edu/) is committed to academic excellence and diversity within the faculty, staff, and student body and is actively recruiting faculty with an interest in academia in the Division of Gastroenterology. Clinical and teaching responsibilities will include general gastroenterology. The appropriate series and appointment at the Assistant, Associate or Full Professor level will be based on the candidate’s qualifications and experience. Salary is com mensurate with qualifications and based on the University of California pay scales. In-Residence appointments may require candidates to be self-funded. For more information: https:// apol-recruit.ucsd.edu/JPF03179 For help contact: klsantos@ health.ucsd.edu
CARDIOLOGIST POSITION AVAILABLE: Cardiology office in San Marcos seeking part-time cardiologist. Please send resume to albertochaviramd@yahoo.com.
DERMATOLOGIST NEEDED: Premier dermatology practice in La Jolla seeking a part-time BC or BE dermatologist to join our team. Busy practice with significant opportunity for a motivated, entrepreneurial physician. Work with three energetic dermatologists and a highly trained staff in a posi tive work environment. We care about our patients and treat our staff like family. Opportunity to do medical/surgical and cosmetic dermatology in an updated medical office with state-of-the art tools and instruments. Incentive plan will be a percentage based on production. If you are interested in finding out more information, please forward your C.V. to jmaas12@hotmail.com.
RADY CHILDREN’S HOSPITAL PEDIATRICIAN POSI TIONS: Rady Children’s Hospital of San Diego is seeking board-certified/eligible pediatricians or family practice physicians to join the Division of Emergency Medicine in the
Department of Urgent Care (UC). Candidate will work at any of our six UC sites in San Diego and Riverside Counties. The position can be any amount of FTE (full-time equivalent) equal to or above 0.51 FTE. Must have an MD/DO or equivalent and must be board certified/eligible, have a California medical license or equivalent, PALS certification, and have a current DEA license. Contact Dr. Langley glangley@rchsd.org and Dr. Mishra smishra@rchsd.org.
PER DIEM OBGYN LABORIST POSITION AVAILABLE: IGO Medical Group is seeking a per diem laborist to cover Labor and Delivery and emergency calls at Scripps Memorial Hospital in La Jolla. 70 deliveries/month. 24-hour shifts preferred but negotiable. Please send inquiries by email to IGO@IGOMED.com.
MEDICAL CONSULTANT – SAN DIEGO COUNTY: The County of San Diego, Health and Human Services Agency’s Public Health Services is looking for a Board Certified Family Practice or Internal Medicine physician for the Epidemiology and Communicable Disease Division. Under general direction, incumbents perform a variety of duties necessary for the iden tification, diagnosis, and control of communicable diseases within the population. This position works closely with the medical and laboratory community, institutional settings, or hospital control practitioners. Learn more here: https://www. governmentjobs.com/careers/sdcounty?keywords=21416207
KAISER PERMANENTE SAN DIEGO - PER DIEM PHYSIAT
RIST: Southern California Permanente Medical Group is an organization with strong values, which provides our physicians with the resources and support systems to ensure they can focus on practicing medicine, connecting with one another, and providing the best possible care to their patients. For consideration or to apply, visit https://scpmgphysiciancareers. com/specialty/physical-medicine-rehabilitation. For questions or additional information, please contact Michelle Johnson at 866-503-1860 or Michelle.S1.Johnson@kp.org. We are an AAP/EEO employer.
PRIMARY CARE PHYSICIAN POSITION: San Diego Family Care is seeking a Primary Care Physician (MD/DO) at its Linda Vista location to provide direct outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care, and participation in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@sdfamilycare.org or call us at (858) 810- 8700.
FAMILY MEDICINE OR INTERNAL MEDICINE PHYSI CIAN: TrueCare is more than just a place to work; it feels like home. Sound like a fit? We’d love to hear from you! Visit our website at www.truecare.org. Under the direction of the Chief Medical Officer and the Lead Physician, ensure the provision of effective quality medical service to the patients of the Health center. The physician is responsible for assuring clini cal procedures are continually and systematically followed, patient flow is enhanced, and customer service is extended to all patients at all times.
PUBLIC HEALTH LABORATORY DIRECTOR: The County of San Diego is seeking a dynamic leader with a passion for building healthy communities. This is a unique opportunity for a qualified individual to work for a Level 3 Public Health Laboratory. The Public Health Services department, part of the County’s Health and Human Services Agency, is a local health department nationally accredited by the Public Health Accreditation Board and first of the urban health depart ments to be accredited. Public Health Laboratory Director21226701UPH.
NEIGHBORHOOD HEALTHCARE MD, FAMILY PRACTICE AND INTERNISTS/HOSPITALISTS: Physicians wanted, beautiful Riverside County and San Diego County. High-quality family practice for a private-nonprofit outpatient clinic serving the communities of Riverside County and San Diego County. Work full-time schedule and receive paid family medical benefits. Malpractice coverage provided. Be part of a dynamic team voted ‘San Diego Top Docs’ by their peers. Please click the link to be directed to our website to learn more about our organization and view our careers page at www.Nhcare.org.
PHYSICIAN WANTED: Samahan Health Centers is seeking a physician for their federally qualified community health centers that emerged over forty years ago. The agency serves low-income families and individuals in the County of San Diego in two (2) strategic areas with a high-density population of Filipinos/Asian and other low-income, uninsured individuals — National City (Southern San Diego County) and Mira Mesa (North Central San Diego). The physician will report to the Medical Director and provide the full scope of primary care services, including but not limited to diagnosis, treatment, coordination of care, preventive care and health maintenance to patients. For more information and to apply, please contact Clara Rubio at (844) 200-2426 EXT 1046 or at crubio@ samahanhealth.org.
PRACTICE FOR SALE
OTOLARYNGOLOGY HEAD & NECK SURGERY SOLO PRACTICE FOR SALE: Otolaryngology Head & Neck Surgery solo practice located in the Ximed building on the Scripps Memorial Hospital La Jolla campus is for sale. The office is approximately 3,000 SF with 1 or 2 Physician Offices. It has 4 fully equipped exam rooms, an audio room, one procedure room, one conference room, one office manager room as well as in-house billing section, staff room and a bathroom. There is ample parking for staff and patients with close access to radiology and laboratory facilities. For further information, please contact Christine Van Such at (858) 354-1895 or email: mahdavim3@gmail.com.
OFFICE SPACE / REAL ESTATE AVAILABLE
CHULA VISTA MEDICAL OFFICE: Ready with 8 patient rooms, 2,000 sf, excellent parking ratios, Lease $4000/mo. No need to spend a penny. Call Dr. Vin, 619-405-6307 vsnnk@ yahoo.com.
OFFICE SPACE AVAILABLE – BANKERS HILL: Approxi mately 500 sq foot suite available to lease, includes private bathroom. Located at beautiful Bankers Hill. For more details, please call Claudia at (619) 501-4758.
OFFICE AVAILABLE IN MISSION HILLS, UPTOWN SAN DI EGO: Close to Scripps Mercy and UCSD Hillcrest. Comfortable Arts and Crafts style home in upscale Mission Hills neighbor hood. Converted and in use as medical/surgical office. Good for 1-2 practitioners with large waiting and reception area. 3 examination rooms, 2 physician offices and a small kitchen area. 1700 sq. ft. Available for full occupancy in March 2022. Contact by Dr. Balourdas at greg@thehanddoctor.com.
OFFICE SPACE IN EL CENTRO, CA TO SHARE: Office in El Centro in excellent location, close to El Centro Regional Medi cal Centre Hospital is seeking doctors of any specialty to share the office space. The office is fully furnished. It consists of 8 exam rooms, nurse station, Dr. office, conference room, kitch enette and beautiful reception. If you are interested or need more information, please contact Katia at (760) 427-3328 or email at Feminacareo@gmail.com.
SUBLEASE AVAILABLE IN DEL MAR OFF 5 FREEWAY. Share rent. 2100 sq ft office in professional building. Utilities included. Great opportunity in a very desirable area. 858-342-3104
OFFICE SPACE / REAL ESTATE WANTED
MEDICAL OFFICE SPACE WANTED IN HILLCREST/ BANKERS HILL AREA: Mercy Physicians Medical Group (MPMG) specialist is looking for office space near Scripps Mercy Hospital. Open to lease or share office space, full time needed. Please respond to rjvallonedpm@sbcglobal.net or (858) 945-0903.
NON-PHYSICIAN POSITIONS AVAILABLE
ASSISTANT PUBLIC HEALTH LAB DIRECTOR: The County of San Diego is currently accepting applications for Assistant Public Health Lab Director. The future incumbent for Assistant Public Health Lab Director will assist in managing public health laboratory personnel who perform laboratory activities for the purpose of identifying, controlling, and preventing disease in the community, as well as assist with the development and implementation of policy and procedures relating to the con trol and prevention of disease and other health threats. Please visit the County of San Diego website for more information and to apply online.
SANDIEGOPHYSICIAN.ORG 21
San Diego County Medical Society
8690 Aero Drive, Suite 115-220 San Diego, CA 92123
Celebrating Independent Physicians
At the Cooperative of American Physicians (CAP), we celebrate you—the independent and solo practitioner who keeps healthcare personal. We are here to support you with exceptional medical malpractice coverage supplemented by a host of outstanding risk management and practice management services, so you can stay focused on what’s important— patient care.
For over 40 years, CAP has delivered financially secure medical malpractice coverage options and practice solutions to help California physicians realize professional and personal success.
Scan the QR code to see how much you can save on your medical malpractice coverage

Find out what makes CAP different.
CAPphysicians.com 800-356-5672
MD@CAPphysicians.com
Medical professional liability coverage is provided to CAP members by the Mutual Protection Trust (MPT), an unincorporated interindemnity arrangement organized under Section 1280.7 of the California Insurance Code.
 More than
California physicians rely on CAP to protect their practices every day.
More than
California physicians rely on CAP to protect their practices every day.
[ Return Service Requested ] $5.95 | www.SanDiegoPhysician.org PRSRT STD U.S. POSTAGE PAID DENVER, CO PERMIT NO. 5377
12,500
