
36 minute read
An urban medical center tackles the opioid crisis
How One Urban Med Center Tackled the Opioid Crisis
In 2016, Kevin Horbowicz, PharmD, BCPS, was tired. Every day, he came to work at Boston Medical Center (BMC), the large urban hospital in the historic South End neighborhood, which has been hit hard by the opioid crisis. As the associate director of inpatient clinical pharmacy services, Horbowicz saw the signs of suffering all around—crime, homelessness and addiction. He and other stakeholders believed they could do better to confront this crisis.
So they decided to tackle the problem in the only way they could: by changing the way BMC doctors prescribe opioids and treat addiction. It was a comco plex process, which included expanding nding the presence of pharmacists on sursurgery floors, and overhauling the electronic health record (EHR) to modify default prescription settings. But it was all worth it, said Horbowicz; in fiscal year (FY) 2018, BMC providers dispensed 74,000 fewer opioid pills than the year before.
“I’m very proud of the collaborative multidisciplinary work that we did,” Horbowicz said.
A Local Issue
Massachusetts is one of the top 10 states with the highest rates of opioid-related overdose deaths. To help combat the crisis, in 2017, BMC received a $25 million grant from Eilene and John Grayken. Executive leadership and other stakeholders—from surgery, nursing, emergency medicine, information technology and, of course, pharmacy—were all committed to making a difference in prescribing habits. The first place they tackled was inpatient utilization. They started by expanding the presence of pharmacists on acute care surgery floors, so pharmacists could suggest opioid alternatives, such as acetaminophen, ketorolac and other nonopioid pain medications, for appropriate patients. The strategy “gave pharmacists a seat at the table to help them contribute to those daily decisions that were made by the surgical team,” Horbowicz said. Indeed, this change alone reduced the use of opioids among acute care surgery inpatients by 12%, according to data that Horbowicz presented at the ASHP 2019 Midyear Clinical Meeting, in Las Vegas.
In the emergency department, the pharmacy team worked with nurses and doctors to administer buprenorphine-naloxone (Suboxone, Indivior) or methadone earlier, connect more patients to treatment, and increase access to intranasal naloxone (Narcan, Adapt Pharma). And for patients who want to seek treatment for opioid use disorder, the emergency department now hands out free two-day buprenorphine-naloxone kits, a “bridge
BMC Successes:
Reduced the use of opioids among acute care surgery inpatients by 12% Dispensed nearly 74,000 fewer opioid pills in FY 2018 than in FY 2017
Source: Kevin Horbowicz, PharmD, BCPS
therapy,” until they can th attend their appointment a with providers, he said. Perhaps the most effective change was e modifying the EHR to alter pain scale range orders and the 55 postoperative order sets used by more than two dozen surgical specialties at BMC. “Those two IT changes were the most important,” Horbowicz said, adding that in the past, surgical patients who reported pain scores of 1 to 3 (out of 10) were given 5 mg of oxycodone every four hours as needed— which was “just too much.” So stakeholders agreed on a new set of standard doses for pain scales, in which patients do not receive an opioid unless their pain is at 4 or higher. If patients had additional pain, prescribers had the option to prescribe more opioids as needed.
As noted, BMC dispensed nearly 74,000 fewer opioid pills in FY 2018 than in FY 2017; between 2016 and 2019, the inpatient use of opioids among surgical patients fell by 41%.
Horbowicz acknowledged that smaller facilities may not have the same resources as BMC, given the size of the grant that fueled many of his team’s opioidreduction initiatives. Still, “many of these changes—such as changing order panels to omit opioids for mild pain—are possible anywhere,” he said. “It just requires some persistence, focus and courage.”
Christine McLellan, PharmD, MHA, the pharmacy clinical coordinator at Emerson Hospital, in Concord, Mass., agreed that many of BMC’s opioid-related interventions are possible elsewhere, and said many health systems are taking similar approaches. “The way BMC has done it with a multipronged [strategy] is the right way,” McLellan told Pharmacy Practice News. “It’s not just one solution that solves the problem.”
Move Away From Opioids
For instance, she said, many other organizations have moved away from giving opioids to patients with only mild pain. “Some of this can be done without a grant, but you definitely need the support of administration, and you need physician champions to support those efforts,” she said. Seeing the success of a large center such as BMC helps make the case that well-designed and executed opioid management strategies will be worth it, added McLellan, who moderated the session at the ASHP Midyear Clinical Meeting. “It helps other hospitals recognize they can do this, too.”
To McLellan, giving pharmacists an integral role is the most crucial step at any facility to reducing opioid use. Pharmacists can help with everything, she said: revising order sets, being on the surgical floor to recommend nonopioid therapies, and suggesting intranasal naloxone for high-risk patients at discharge. “The pharmacist is primed for opportunities like this to be able to combat the opioid crisis,” she said. “I think the pharmacist is the key to a lot of it.” —Alison McCook
The sources reported no relevant fi nancial relationships.
Helping you deliver better medicine to more people.
Leiters is an FDA registered and inspected 503B outsourcing provider of high-quality compounded sterile preparations and services including:
Pre-filled syringes, IV bags and vials Opioid-free surgical pain services medications ON-Q* Pain Relief System fill services Ophthalmology medications including FDA-compliant repackaged Avastin®
Thinking Outside the Ideal Body Weight
The Pharmacist’s Role in Management of Bariatric Surgery Patients
Madeline Lutz, PharmD
Clinical Pharmacist
Elizabeth Powell, PharmD, BCACP
Clinical Pharmacist
AdventHealth Celebration Celebration, Florida
Bariatric surgery brings many different changes to a patient, from the physical altering of the gastrointestinal tract to the psychological changes that come after a life-altering surgery. As we know, patients who undergo bariatric surgery can experience rapid weight loss. With this weight loss comes inevitable changes to medications used to control disease states. Pharmacists can play an integral role in a patient’s bariatric surgery journey by providing patient-specific consultations and making recommendations to adjust medication therapy both before and after surgery.
Table. Criteria to Identify Risk Factors For Readmissiona
BMI >50 kg/m2
Chronic obstructive pulmonary disease
Complication or extended surgery
Length of hospital stay >4 d
Deep vein thrombosis
Medicare and Medicaid insurance
Metabolic syndrome
Surgical site infection
Urinary tract infection
Other risk factors identified during the initial surgical consultation
Based on references 2 and 3. a After bariatric surgery; based on the Decreasing Readmission through Opportunities Provided Initiative.
At our pharmacist-run ambulatory care clinic within a large medical group, pharmacists work closely with a bariatric surgeon’s office to provide optimal care to patients who are undergoing bariatric surgery and have complex medical conditions managed by numerous medications. A small retrospective, single-center study done at our practice site in 2015 to 2016 assessed 30-day all-cause readmissions. Of the 113 patients included, 63 patients met with a pharmacist for a 2-week postoperative follow up. Of these, 4 patients (6.3%) who met with a pharmacist were readmitted within 30 days compared with 5 patients (10%) in the
control group (P=0.48). (The estimated national average 30-day readmission rate after bariatric surgery is 5%.1) Although our institution saw a smaller percentage of patients readmitted within 30 days if a pharmacist was involved at a 2-week postoperative appointment, the results were not statistically significant. Since the conclusion of this study, our clinic services have expanded to include optional preoperative disease state optimization, a preoperative visit, and additional postoperative follow-up visits as detailed below.
Patients typically are referred to our service by the bariatric surgeons’ offices during initial surgical consultations. These patients may benefit from medication management services based on certain criteria set forth by bariatric providers. Suggested criteria include patients taking 5 or more maintenance medications, high-risk medications (eg, anticoagulants), or diabetes medications, as well as patients on dialysis and patients who may be at high risk for readmission as described in the DROP (Decreasing Readmission through Opportunities Provided) initiative (Table).2,3 The criteria are not set in stone, and it is up to the provider’s discretion to refer patients to this service.
After referral, patients are seen in our clinic before surgery. The focus of the visit includes a medication reconciliation and recommendations (eg, smoking cessation) to optimize management of diseases such as diabetes and hypertension before surgery. A preoperative visit typically is scheduled 2 to 4 weeks before surgery to review medications, provide medication holding instructions before surgery, and provide counseling on medications typically prescribed immediately after surgery. This visit usually coincides with the patient’s preoperative clearance and lab review visit with the bariatric surgeon.

After the visit, the pharmacist documents an up-to-date and accurate medication history and consultation note in the inpatient and outpatient electronic health records. This update is completed before admission to the hospital for surgery.
After surgery, patients are scheduled for appointments at 2 and 6 weeks, 3 and 6 months, and 1 year to coincide with their follow-up visits at the bariatric surgeon’s office. Again, at each visit, a medication reconciliation occurs; this is especially important because medication therapy is very dynamic during this time. The workflow for postoperative visits is shown in the Figure.
During these visits, we assess the patient’s entire medication regimen and make recommendations to the bariatric surgeon or prescribing doctor to adjust medications. We assess perioperative medications for appropriate use and duration of therapy, considering most recent lab results and giving special attention to medications that have a narrow therapeutic index, vitamin levels, and kidney and liver function. Adherence to a bariatric vitamin regimen is crucial for these patients to prevent malnutrition and/or vitamin deficiency. As pharmacists, we can help these patients identify specific formulations of vitamins and/or supplements that will best fit their needs. We review blood glucose and blood pressure logs to make recommendations for diabetic and hypertension-controlling medications. We also counsel on ways to avoid dumping syndrome, bloating, and constipation; the importance of diet and exercise; avoidance of alcohol; appropriate contraception (if applicable); and any other issues specific to the patient’s needs. At all of these visits, the patient’s medications are screened for potentially inappropriate ones used after bariatric surgery. These agents may include extended-release formulations and medications with high risk for gastrointestinal irritation.
Bariatric surgery is a lifelong journey and patients are offered optional follow-up after the 1-year postoperative visit. We assess patient-specific needs for additional follow-up appointments, scheduling them routinely or on an asneeded basis, whichever is most appropriate for each patient.
Our services are billed at each visit by charging a facility fee.
Each patient has a unique journey while undergoing bariatric surgery. Pharmacists are formally trained medication experts who serve as an integral part of a patient’s interdisciplinary team. We aim to bridge the gap between different providers by performing medication reconciliation and providing recommendations to providers to help patients achieve optimal medication management of their disease states during their bariatric surgery journeys.
References
1. Abraham CR, Werter CR, Ata A, et al. Predictors of hospital readmission after bariatric surgery. J Am Coll Surg. 2015;221(1):220-227. 2. Morton J. The first metabolic and bariatric surgery accreditation and quality improvement program quality initiative: decreasing readmissions through opportunities provided.
Surg Obes Relat Dis. 2014;10(3):377-378. 3. Morton J, Brethauer S, Fraker T, et al.
Decreasing readmissions through opportunities provided (DROP): The First National
Quality Improvement Collaborative from the
Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). Surg Obes Relat Dis. 2016;12(7 suppl ): S1-S2. https://www.soard.org/article/
S1550-7289(16)30209-X/fulltext.
Remdesivir for COVID-19: Where Does It Stand?
Preliminary positive findings led remdesivir to become a staple in the armamentarium to treat hospitalized patients with COVID-19, but the latest data from two large wo large studies by the National Institutes nstitutes of Health and the World Health Health Organization (WHO) indicate cate the drug provides no mortality ity benefit.
Despite this finding, on Oct. 22, , the FDA approved remdesivir (Veklury, Gilead) as the first t treatment indicated for COVID-19 9 (bit.ly/2TyC6h7).
The NIH COVID-19 treatment ment guidelines also continue to recommend mmend the drug for patients with severe severe COVID-19 (bit.ly/2G00tkL), while while stating that health care providers should prioritize its use in “hospitalized patients with COVID-19 who require supplemental oxygen but who do not require oxygen delivery through a highflow device, noninvasive ventilation, invasive mechanical ventilation, or extracorporeal membrane oxygenation” (bit.ly/3dWapsc). The antiviral portion of the guidelines indicated that the section on remdesivir “would be updated soon.” At press time, the update was still pending.
A WHO panel is working on its own guidelines on remdesivir, looking at “the totality of the evidence,” said Janet Diaz, MD, the head of the clinical unit in the WHO’s emergency programm, at a press conference on Oct. 23. She said they expect the guidelines to be published in three to four weeks.
Underscoring the importance of these guidelines, Michael Ryan, MD, the executive director of the emergency programme, said it is the role of the regulatory process to guide “what can go on the shelf,” but it is the guidelines that help clinicians determine how “to use what’s on the shelf.”
SOLIDARITY Trial Disappoints
Evaluated as part of the WHO-sponsored SOLIDARITY trial, rem desivir did not improve the outcomes of mor tality, initiation of ventilation and duration of hospitalization, ac cording to findings released in a preprint in MedRxiv on Oct. 15 (bit.ly/3mq4Cy5). The ongoing multina tional, open-label, randomized SOLIDARITY trial conducted at 405 hospitals in 30 countries was designed to evalu ate four antiviral agents—rem des i vir, hydroxychloroquine, lopi navir/ ritonavir (Kaletra, AbbVie), and interferon-β1a in adults hospitalized with COVID-19. After results from the United Kingdom’s Recovery trial, released in June, showed that hydroxychloroquine and lopinavir/ritonavir did not increase survival (www.recoverytrial.net/results),
Interpretation of the SOLIDARITY findings should reflect
the confidence interval (0.79-1.05),
which ‘absolutely excludes the suggestion that
remdesivir can prevent a substantial
fraction of all deaths.’


Source: WHO Solidarity Trial Consortium (bit.ly/3mq4Cy5).
the SOLIDARITY the SOL investigators halted those investigators hal study arms. The interferon arm was halted on Oct. 16.
The results reported in the preprint show none of the study drugs, including remdesivir, “had any definite effect on mortality, either overall … or in any subgroup defined by age or ventilation at entry (or other entry characteristics, or geographic region, or corticosteroid use).”
More specifically, the investigators found that the rate ratio (RR) for death with remdesivir (200 mg on day 0, and 100 mg on days 1 through 9 or until death or discharge) was 0.95 (95% CI, 0.81-1.11; P=0.50; 301/2,743 vs. 303/2,708).
No Mortality Benefit in NIH Trial
Final results from the remdesivir versus placebo stage of the NIH’s Adaptive COVID-19 Treatment Trial-1 (ACTT1), published Oct. 8 (bit.ly/2J20zti), also showed no mortality benefit for remdesivir, but the drug reduced hospital length of stay and helped reduce the risk for death in some patients with COVID-19 who were receiving oxygen. Median recovery time was 10 days (95% CI, 9-11 days) in remdesivir-treated patients versus 15 days (95% CI, 13-18 days) in the placebo group (RR for recovery, 1.29; 95% CI, 1.12-1.49; P<0.001 by log rank test). Mortality varied considerably between groups according to baseline severity, with the greatest benefit seen among patients with a baseline ordinal score of 5 (hospitalized and requiring any supplemental oxygen, but not high-flow oxygen or noninvasive or invasive ventilation) (hazard ratio [HR], 0.30; 95% CI, 0.14-0.64).
Considering the ACTT-1 mortality findings along with those from their own trial as well as two smaller studies, the SOLIDARITY investigators underscored that their trial provides “more than three-quarters” of the evidence related to remdesivir. Using the combined results of the four trials— SOLIDARITY (604 deaths among approximately 5,000 patients), ACTT1 (136 deaths among approximately 1,062 patients) and 41 deaths in two smaller trials—they calculated the remdesivir RR for death to be 0.91 (95% CI, 0.79-1.05).
However, they stressed that in ter preta tion of these findings “should chiefly reflect not the P-value (P=0.21) or point estimate (RR=0.91) but the confidence interval (0.79-1.05), which ... absolutely excludes the suggestion that remdesivir can prevent a substantial fraction of all deaths. The confidence interval is comfortably compatible with prevention of a small fraction of all deaths, but is also comfortably compatible with prevention of no deaths.”
Commenting on the study, Jeffrey R. Aeschlimann, PharmD, an associate professor at the University of Connecticut School of Pharmacy, in Storrs, and adjunct associate professor at UConn School of Medicine’s Division of Infectious Diseases, in Farmington, said the “SOLIDARITY results align with the ACTT-1 trial results,” which indicate that “remdesivir therapy does not appear to significantly reduce overall mortality from COVID-19 infection in patients who are sick enough to warrant inpatient hospital care.”
Benefit for Other Outcomes
Despite the lack of mortality benefit, Aeschlimann said there is “a strong argument for granting FDA approval to a drug that can shorten the duration of symptoms and/or allow patients to get discharged from inpatient hospital care quicker—especially if that disease is causing a pandemic that is stressing health care systems worldwide.”
In a FAQ sheet about remdesivir on its website, the FDA noted: “While both the SOLIDARITY trial and the ACTT-1 trial contribute to our understanding of interventions to help treat COVID-19, the two clinical trials had different ... designs and primary goals. The design of ACTT-1 (i.e., randomized, placebocontrolled, double-blinded) was better suited to rigorously assess a time to recovery end point compared to a trial with an open-label design, such as the SOLIDARITY trial. Based on the findings of the ACTT-1 trial, benefit to patients for [remdesivir] was demonstrated, including a shorter time to recovery and better odds of clinical improvement. The SOLIDARITY results do not refute these findings of benefit to patients” (www. fda.gov/media/137574/download).
In addition to being a different type of trial from ACTT-1 with a different focus and primary end point, SOLIDARITY did not include “enough detailed data collection about day-to-day symptom severity” to allow comparisons with ACTT-1 trial results on those measures, Aeschlimann told Pharmacy Practice News. “Also, the data on hospital length of stay should be interpreted with caution,” he said, “because the trial design did not really permit a scientifically rigorous assessment of impact of therapy on duration of hospitalization.”
Although he recognized the need for the FDA to consider outcomes other than mortality in its approval process, Aeschlimann said he was “disappointed that the FDA approval language wasn’t more specific in its guidance for why [remdesivir] should be used, and which types of COVID-19-infected patients it seems to benefit most—patients who have not progressed to needing invasive mechanical ventilation.”
The bottom line, Aeschlimann said, is the “SOLIDARITY trial results reinforce the current scientific opinions of most clinician researchers about the drug: It is an anti-COVID-19 therapy that can provide some modest overall therapeutic benefits when started in the right patients. It is not a drug that will help us to significantly lower the risks of death in patients with severe COVID-19 infections.”
—Sarah Tilyou
Mind and Body: The Untapped Health Resource
‘The key to a healthy life is having a healthy mind.’ —Richard Davidson
We hear so much concern about burnout in health care workers. Many professional societies are focusing on this important practice issue, including sessions at several recent ASHP meetings.
We are all aware that stress is not good for our health, but being a pharmacy leader is particularly challenging. How are you responding to these pressures? It’s important to remember that although you cannot control the majority of the circumstances that cause stress in your life or work, you can control howyou respond to those stressors. The stakes are high for success: A recent study found that a pessimistic outlook proved to be deadlier than congestive heart failure or smoking 50 or more packs
“Leadership in Action” is authored by Ernest R. Anderson Jr., MS, RPh, FASHP, FMSHP, of Brockton, Mass. Mr. Anderson welcomes your input on leadership issues, at ernestanderson1130 @gmail.com.
Ernest R. Anderson Jr., MS, RPh, FASHP, FMSHP


Innovation in Secure Drug Delivery Prep-Lock™Tamper Evident Caps for IV Syringes are an active deterrent to potential tampering or misuse. They help ensure syringe integrity is maintained from the time it leaves the sterile hood until it is administered by an authorized clinician. IMI has been creating American-made products for the compounding pharmacist for over “Simple, Innovative Solutions to Enhancing Drug Security Programs. half a century. Our quality, reliability and exceptional customer care have made Prep-Lock Tamper Evident Caps an industry standard for guarding IV
Syringes. of cigarettes every year (Circulation 2000;102[15]:1773-1779). Wow! Let’s dig deeper to understand the interconnection between the mind and body.

Our Perceptions Affect Our Health
A positive person views a problem as an opportunity for a solution that advances the situation. Pharmacists face this decision constantly throughout the day: Are you positive or negative in your thinking? These mindsets affect our health, not just our leadership.
As medical professionals, we are well aware of the placebo effect. If patients feel positive about a treatment because they think they’re getting the active drug, they do better—regardless of whether they actually are in the active treatment group. What more evidence of positive thinking do you need?
Well, consider this: researchers have found that people with a family history of heart disease who had a positive outlook were one-third less likely to have a heart attack or other cardiovascular event within five to 25 years than those with a more negative outlook (bit.ly/2RhMFDL).
Of course, the converse also is true: A study of 5,888 Americans over the age of 65 years at Johns Hopkins University found that a poor image of one’s health roughly doubled the risk for death within five years, regardless of other health risk factors (Circulation 2000;102[15]:1773-1779).
Kindness also has been tied to clinical outcomes. In a 2014 study, the authors explored various psychosocial risk factors in cardiovascular disease. They found that anxiety, depression, chronic stress, isolation and low sense of purpose all increased people’s risk for experiencing heart failure (Circulation: Heart Failure 2014;7:385-387). Conversely, the same study showed that higher rates of optimism, compassion and kindness reduced stress, strengthened our immune systems, and helped reduce anger, anxiety and depression. Patients who exhibited those positive attitudes and qualities were at a lower risk for heart failure.
But here’s the challenge: Acts of kindness begin in our minds; there needs to be an intention to be kind before acts of kindness manifest. Fortunately, the payoff is worth it: Being kind benefits our interpersonal relationships —and, as noted in these clinical studies—benefits our health as well.
Neuroscience Holds the Key
Neuroscience partly explains how this mind–body connection plays out. Studies have shown that negative thoughts and stress increase our heart rate, respiratory rate and cortisol levels (the fight-or-flight hormone) and decrease immunity. Conversely, positive thoughts lower heart rate and respiratory rate and release endorphins, enkephalins, serotonin and dopamine (the feel-good hormones). This in turn reduces pain, increases our mood and sense of calm, and allows us to look at challenges realistically. Therefore, how we view life’s hardships and challenges matters. Do we view these as opportunities to grow or do we stress out?
I’ve often asked in these columns, given two equally qualified people, would you hire the pessimist or optimist? This should stimulate your mind to develop questions to go after this answer during the interview.
You may have heard it said that we become our thoughts. This is true, partly because repetitive thoughts build dendrites and neurons in the brain, which help facilitate the formation of
short-term memory, and when repeated enough, then become part of our longterm memory. Our view of the world and what we say and do come out of these cerebral processes. This is why it is so important to take in positive thoughts and stimuli and not negative, toxic thoughts. You become what you think about. So, it may be time to think more about your thinking!
Perhaps you should put a reminder in your daily schedules to check your thinking periodically. My recommendation: If you feel out of control or are thinking negatively, take a break; take some deep, long belly breaths and slow down your mind. Being an adrenaline junkie is not a healthy state. Instead, think kind thoughts and put others first.
Effect on Health Care
If all this positive thinking is physiologically good for you, perhaps we should teach it to our patients, because they need to do more than eat right, exercise and reduce stress; they need a healthy mindset as well. The idea is to teach our patients, and ourselves, to reframe circumstances in our lives before they, or we, let our emotions get the best of us⎯sometimes referred to as “an amygdala hijack” ⎯and we act out of control without thinking, in essense enslaved by the baser impulses that reside in our prefrontal cortex. We need to teach people to ask questions to determine the “why” behind a situation, and ask whether it is true and the degree to which we may think it is a crisis. Then we can reframe, de-escalate and decide our next steps. Remember, we are in control of our response to our circumstances.
Choosing What We Will Think
Yes, we will become our thoughts unless we examine negative thoughts and replace them with positive ones. For example, the two universal issues that all people face are fear and selfdoubt. If you ruminate on these two negative “loops” in your mind, they will become part of your thinking and memory. However, if you challenge the veracity of that fear and self-doubt and overcome it with more positive affirmations of your self-worth, you will become the victor.
Eleanor Roosevelt said: “You gain strength, courage and confidence by every experience in which you really stop to look fear in the face. You are able to say to yourself, ‘I have lived through this horror. I can take the next thing that comes along.’ You must do the thing you think you cannot do.” Even she realized the power of the mind, without benefit of modern-day brain scan technology.
So, What Do We Do?
We are largely a set of memorized, learned behaviors, reactions, skills, beliefs, perceptions and attitudes in our short- and long-term memory learned by about 35 years of age. So, what if we are operating out of the wrong paradigm for some items and need to change? Are we hopeless? No, we can train ourselves to think differently. Positive attitudes and habits can be cultivated and learned, giving us another way to think, which will improve our relationships and our health. It is widely accepted that it takes 21 days to develop a habit, and it takes three cycles to make it automatic. So, fear not: You can change your thinking paradigm, with resilience and new thinking being the invaluable results. ■










Read Specialty Pharmacy Continuum Anywhere, Anytime!
Next Column:

Lion’sLead: The Magic Bullet For Pharmacy Leaders
Most pharmacy leaders have taken a myriad of leadership tests, but are they really assessing leadership? No, most tests assess personality, not leadership. LionsLead is a true leadership test, measuring learned behavior that influences outcomes, not personality profiles of a person’s tendencies. Don’t miss it!


From swab and serology y testing to monitoring g patients’ oxygen saturation level, ambulatory y pharmacists have ample opportunities to demonstrate their value beyond medication dispensing and counseling during the COVID-19 pandemic. The extent to which
TEMPERATURE INTELLIGENCE®
Monitoring solutions for central pharmacy operations
Protect the stability of your temperature sensitive medication – onsite and in transit
Getting medication and vaccines to your various sites within the right temperature range is critical to quality patient care. From single-use temperature indicators to reusable wireless dataloggers to facility monitoring — Temptime offers solutions to meet the needs of every central pharmacy, no matter the size or reach. Learn more about how Temptime can help you improve efficiency and reduce costs while protecting your medication inventory from start to finish: temptimecorp.com/pharmacy

they contribute now will have benefits beyond this crisis, experts believe.
HHS Recognizes Profession’s Value
As Tom Kraus, JD, the vice president of government affairs at ASHP, noted, pharmacists have already been called upon to help in important ways, such as expanding COVID-19 testing availability. He pointed to authorization by the Department of Health and Human Services (HHS) for pharmacists to order and provide serology testing (bit.ly/3lo3FFX).
“We’ve also seen a number of governors do the same thing through executive orders,” Kraus said, noting these state-level emergency orders temporarily waive enforcement of some limits in scope of practice laws.
Although expanded testing is a critical step in mitigating the spread of COVID-19, initiatives by pharmacists could include administration of a vaccine and antiviral medications, should they be found, he said.
“If an effective antiviral emerges, pharmacists would be in a good position to initiate therapy if it can be provided in an ambulatory setting, since they are already testing,” Kraus said. “That would be particularly true if the antiviral’s administration was time-sensitive, like oseltamivir [Tamiflu, Roche], which needs to be given within 48 hours of influenza infection to be effective.”
Yale New Haven Leverages Telehealth
Elsewhere, ambulatory pharmacists are taking on other innovative roles during the pandemic. At Yale New Haven Health (YNHH) in Connecticut, for example, recent growth in telehealth has opened up opportunities for outpatient and ambulatory care pharmacists to help reduce the burden on their provider and nurse colleagues, said LeeAnn Miller, MS, PharmD, the vice president and chief pharmacy officer at YNHH.
“Our pharmacists have been able to provide virtual care for patients in the community—primarily those with chronic hypertension as well as patients on anticoagulation therapy— and help reduce the patient load for the health system’s physicians and nurses,” Miller said.
Pharmacists here also have helped manage shortages of hydroxychloroquine, which has been touted as a potential COVID-19 treatment, she said.
When prescribing of hydroxychloroquine ramped up, YNHH pharmacists “quickly put together guidance for
Compliance Q&A With Contec Healthcare
Are operating room mopping products acceptable for cleaning the USP <797> pharmacy cleanrooms?
It is not uncommon to see cotton mops or relaundered microfiber products in operating rooms. According to strict USP guidelines, these products are not allowed into the pharmacy. Mopping systems and buckets should be dedicated to the pharmacy cleanroom and should not be used in other areas. Contec Healthcare offers many non-shedding mops for ISO (International Organization for Standardization) class 7 and 8 rooms. pharmacy market, by definition, are “lint free,” “non-shedding” and “low lint.” These terms are expected to be defined in a pending Recommended Practice of the Institute of Environmental Sciences and Technology (www.iest.org).
Are there training modules or representatives that can help me implement bestpractice protocols at my facility?
Yes; we invite you to work with our specialists to improve your critical care cleaning process. We will assist you in selecting the Contec Healthcare wipes, mops and solutions that best fit your application. More importantly, we will help you design correct procedures that will improve your processes. To arrange a trial, or to learn more about Contec Healthcare and our products, please contact a sales representative or visit our Education & Training page.
Can PeridoxRTU® be used for hazardous drug decontamination?
Yes; when used according to Contec Healthcare procedures, PeridoxRTU® has been shown, via third-party testing, to be effective for hazardous drug decontamination
Are Contec Healthcare disinfectants found on Environmental Protection Agency (EPA) List N for effectiveness against SARSCoV-2 (COVID-19)?
Yes; please check the official EPA List N for an updated list of disinfectants that are effective against COVID-19. Please note that some items may be under a master registration EPA number listing. If you have questions, please call your local Contec Healthcare representative for support. For all other COVID-19 information, please visit our Contec COVID-19 resource page at bit.ly/2HOaYIB.
Is the Klean Max™ pad disposable?
Yes; designed for maximum mechanical removal of contaminants and even distribution of a disinfectant on walls and floors during a terminal clean, the Klean Max™ pad is the perfect product in this environment. It is used once per room and then discarded.

Which disinfectant is best to use in a cleanroom pharmacy setting: ready-to-use or concentrated?
Ready-to-use disinfectant products are ideal for pharmacies where there is no mixing station. They ensure repeatability of process and eliminate the need for creating operating procedures for mixing, including water purity verification. Readyto-use products also ensure that the correct amount of active ingredient is present, and often have a longer shelf life versus diluted solutions. Concentrated disinfectant products often are not encouraged by state boards, as well. Concentrated products are often ideal for large facilities with adequate space for mixing stations, storage, and large and frequent cleaning demands.
What if my customer needs to kill a pathogen that is not listed on the Contec disinfectant label? How can I verify that Contec disinfectants will kill that pathogen?
If you have a specific organism that is not on the product label that your customer’s facility wants to address, please contact your Contec Healthcare sales representative. Contec Healthcare will work with you to determine the best path forward for your product efficacy requirements.
Are Contec Healthcare’s wipes and mops lint free or non-shedding?
Our wipes and mops for the compounding on stainless steel surfaces. Contact your Contec Healthcare sales representative to learn more.
Is it OK to use sterile lint-free gauze?
According to the USP <797> Sterile Preparations guide,1 “sterile 70% IPA wetted gauze pads or other particle-generating material shall not be used to disinfect the sterile entry points of packages and devices.” Suggested operating procedures should state that nonessential objects that shed particles shall not be brought into the buffer area, including pencils, cardboard cartons, paper towels and cotton items (e.g., gauze pads).
1. 2012 USP–NF General Chapter <797> Pharmaceutical Compounding — Sterile Preparations.
AMBULATORY
continued from page 26
ambulatory care providers, both within our health system and in the community, explaining that there is no evidence that hydroxychloroquine is effective for COVID-19 prophylaxis,” Miller said.
Instead, they identified the most effective treatments for COVID-19, noting that these efforts minimized inappropriate prescribing of hydroxychloroquine and ensured the medication is available for patients who need it, such as those with rheumatoid arthritis.
Such an approach with hydroxychloroquine is supported by recent data. In a randomized trial testing the drug as postexposure prophylaxis for COVID-19, the incidence of a new illness compatible with COVID-19 did not differ significantly between participants receiving hydroxychloroquine (49 of 414 [11.8%]) and those receiving placebo (58 of 407 [14.3%]) (N Engl J Med 2020;383:517-525).
Pulse Oximetry Option
An innovative role that Miller’s team is trying to carve out for YNHH ambulatory pharmacists is the capability to dispense pulse oximetry devices to nonhospitalized COVID-19–positive patients, she said. “We’ve seen COVID-19 patients with low oxygen saturation who are still speaking, where they’d typically be gasping for air or clearly struggling to breathe with that level of oxygenation. Because of this unusual presentation, some very sick patients are waiting too long to go to the hospital.”

Innovation in Secure Drug Delivery

Prep- Fill™ Guarded Luer Connectors provide pharmacy compounding operations with simple, high-quality connectors to enhance pharmacy productivity and effi ciency. Prep-Fill Guarded Luer Connectors feature select enhancements that make them the premier choice for Pharmacies. • Expanded Wings Reduce Touch
Contamination • Open Wing Permits First Air • Built-in Drip Tray Captures Stray
Droplets • Made in the USA
Distributing pulse oximeters in the community could help identify emergency cases based on their oxygen saturation levels, Miller said, and her team is collaborating with physicians to determine how they can help provide the device to patients who are prescribed one by a physician.

Lack of Reimbursement Impedes Access
Like Kraus, Miller believes COVID-19 testing and vaccination are a natural fit for ambulatory and community pharmacists, as well as pharmacy technicians. However, a lack of direct mechanisms for reimbursement hinders widespread rollout of testing and possible vaccination by pharmacists, she said. “Adequate reimbursement would make it easier to justify the added resources required to support these services.”
Pharmacists at YNHH have collaborative practice agreements in place, providing them a channel through which to offer financially sustainable direct patient care for chronic conditions as well as potentially COVID-19 services. However, many pharmacists across the country would rely on Medicare Part B reimbursement for testing and vaccination, ASHP’s Kraus said.
At the moment, he noted, reimbursement through Medicare Part B is only available through “complex administrative mechanisms,” such as incidentto billing. Although the HHS guidance authorizes that pharmacists can order and administer tests, it does not address the question of reimbursement, according to Kraus.
“If we’re not able to get Medicare to reimburse pharmacists in a straightforward manner, at least with regard to testing during the emergency, that’s going to be a potential barrier to access,” Kraus said. ASHP has urged federal lawmakers to create some type of Medicare reimbursement mechanism for COVID-19–related services that pharmacists are authorized to provide, but he said Congress has yet to act on these recommendations.
Meanwhile, reimbursement by commercial insurers and Medicaid depends on state rules, most notably laws affecting scope of practice, and these differ by state, Kraus said. “We’ve put out a series of recommendations to state lawmakers laying out both the scope-of-practice authorities and payment avenues that need to be in place in order to ensure access to care by pharmacists.”
A Channel in Medicare Part B
Daniel Nam, RPh, Esq, an associate principal in pharmacy policy at Avalere Health, a health policy consulting and analytics firm in Washington, D.C., is optimistic that pharmacists will see a direct Medicare Part B reimbursement mechanism for testing and vaccination for COVID-19, particularly given the “tremendous value pharmacists provided in rolling out vaccinations during the H1N1 pandemic.
“We also have the mass immunizer roster billing process, through which pharmacists can administer influenza and pneumococcal vaccines under Medicare Part B,” Nam added. The mass immunizer roster billing process is a payment mechanism for providers and nonproviders of population-level vaccinations as defined by the Centers for Medicare & Medicaid Services. Although COVID-19 vaccinations are not yet included under the mass immunizer program, Nam said, “it could be expanded to cover those vaccinations.”
A Boost for Provider Status
Demonstrating pharmacists’ value during “tough situations like the COVID-19 pandemic” could boost the
case for provider status, Nam believes. However, “to really move the conversation forward, pharmacists need to continue to quantify the outcomes and provide evidence that their interventions are indeed having an impact,” he said. “I also think that although it’s typically been an all-or-nothing process in terms of getting provider status legislation, there is a parallel approach in which pharmacists can inch toward provider status by incrementally taking on broad Medicare reimbursement for additional services, which are ‘If we’re not able to get Medicare to reimburse pharmacists in a straightforward manner, at least with regard to testing during the pandemic], that’s going to be a potential barrier to access.’
—Tom Kraus, JD
already temporarily available to them to provide during the pandemic, like point-of-care testing.”
Kraus agreed with that assessment, saying that novel ways to “more fully utilize the skills of pharmacists will certainly inform future provider status discussions.
“One could imagine that some of the authorities [that] pharmacists are given during the pandemic could be left in place afterward if there’s a recognition that they provide a lot of value in their services to their communities,” Kraus said. “I think we’ll see a push long after the pandemic to access those points of care, which would feed into the provider status argument.” —David Wild
The sources reported no relevant fi nancial relationships.
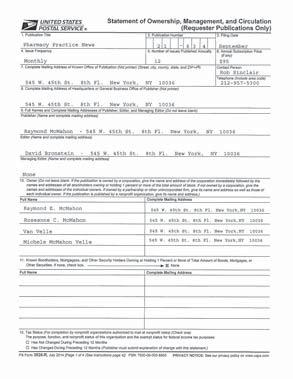
Statement of Ownership




THE PEAK OF PREPARATION.


You need to be prepared at all times. No one understands this more than CAPS®— we’ve got you covered with three FDA-registered 503B outsourcing facilities and the largest network of state-licensed 503A pharmacies in the country.



Same day. Next day. Every day. For almost 30 years, we’ve made sure you have the Compounded Sterile Preparations (CSPs) you need, when you need them.
Count on CAPS to keep you at peak performance.

CAPS is part of the B. Braun Group of Companies in the U.S.





