
46 minute read
Outpatient antibiotic stewardship spreads its wings
Part 1 of a 2-part series
ABx Stewardship Spreads Its Wings
Antimicrobial stewardship programs are on the rise. What started as an effort to improve antibiotic prescribing and reduce antibiotic resistance in inpatient settings has been gradually expanding to ambulatory care, emergency departments (EDs), and even some settings outside of traditional health systems.
“We’ve seen, in the last 10 years, tremendous growth in antimicrobial stewardship programs,” said Anna Legreid Dopp, PharmD, the senior director of clinical guidelines and quality improvement at ASHP. In a 2018 ASHP survey, about 45% of responding hospitals said they had antimicrobial stewardship programs, she noted. That number today is over 90%. In addition, the survey suggests there are opportunities for antimicrobial stewardship practices to extend beyond hospitals, into ambulatory settings. This includes 90% of responding larger hospitals with more than 600 beds, and 30% of smaller hospitals.
“We know that close to 30% of antibiotics used in outpatient settings are prescribed unnecessarily, so there’s definitely a huge need for it,” Dopp said.
Stewardship is being evaluated in many areas, said Susan Davis, PharmD, the president-elect of the Society of Infectious Diseases Pharmacists and a professor of pharmacy practice at Wayne State University, in Detroit. Pharmacists are recognizing that although the broad-spectrum antibiotics might be used in hospitalized patients, the bulk of antibiotics are used outside of the hospital. “That means inpatient stewardship experts are having to learn practice models they haven’t previously been involved in, so partnering with pharmacists in community and ambulatory care settings is really essential,” Davis said.
One ongoing project at her health system involves working with primary care and urgent care clinics to offer symptom relief gift bags to patients 218 The number of interventions clinical pharmacists made on daily rounds to optimize antimicrobials. 26
The number of recommendations made to optimize anticoagulation. 20
Patients educated at discharge about their high-risk medications. 100%
Of interdisciplinary clinicians strongly agreed that a pharmacist should continue on the
ABx stewardship care team.


presenting with common respiratory illnesses—such as sinusitis, bronchitis or sore throat—who don’t need antibiotics.
Borrowing an idea posted on Choosing Wisely by Mayo Regional Hospital in Maine, the Detroit pharmacists developed a symptom relief guide for patients, naming over-the-counter products to address their symptoms. They also put together bags containing items such as saline nasal spray, tissues, lip balm and sugar-free cough drops, as well as a card referring them to an outpatient pharmacy within the health system, where pharmacists help patients choose products that may provide relief.
“It’s really hard to send someone home and say, ‘Sorry, we can’t do anything for you,’” she said. “That’s the last thing a clinician wants to do.”
Davis and her colleagues tracked results during the first year of the program and got “some great uptake,” especially in downtown hospitals. Some 500 gift bags were distributed in five walk-in clinics in 2018, with half of pharmacy vouchers redeemed for over-the-counter products. From there, the team received a grant from the Michigan Pharmacists Foundation to provide 650 bags in nine clinics in 2019. “It’s something that our pharmacists feel excited to do,” she said.
At Duke, EDs a New Focus
Outpatient, urgent care and EDs are another area of growth for antimicrobial stewardship programs. Rebekah Wrenn, PharmD, an infectious diseases clinical pharmacist at Duke University Hospital, in Durham, N.C., and her colleagues have been tackling antibiotic prescribing for urinary tract infections (UTIs) in the ED.
About 13.7 million antibiotic prescriptions are written by emergency physicians nationally, and about half of outpatient antibiotic prescriptions are expected to be inappropriate, said Wrenn, citing 2017 CDC data (bit.ly/ 30DNbBG) Her team is focusing on socalled “treat-and-release” patients who present to the ED but are not admitted.
“Patients are seen briefly, and clinicians don’t have a lot of data when making antibiotic decisions,” she said. “We felt clinicians really needed tools to help treat patients appropriately that fit into the workflow of the ED, which is quite different than inpatient treatment.”
In a pilot project at three hospitals in the Duke University Health System (DUHS), Wrenn and her colleagues created a UTI antibiogram based on outcomes from treat-and-release patients at the institutions, as well as current treatment guidelines. They also conducted in-person education sessions
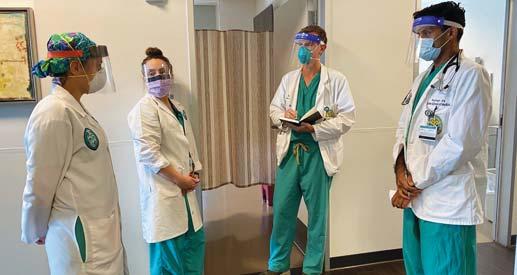
At Duke University Hospital, in Durham, N.C., the antimicrobial stewardship and evaluation team (aset) created pocket cards (left) on appropriate antibiotic prescribing and placed the cards at workstations. The cards are part of Duke CustomID, a decision support tool intended to provide clinicians with institution-specific, accessible, easily customizable information about the diagnosis and treatment of infectious diseases.





for resident physicians on appropriate prescribing and made recordings of those sessions available for attending providers. A pocket card on appropriate antibiotic prescribing was placed at workstations and added to a centralized tool, Duke CustomID. The team has provided feedback on how the ED providers are doing with guidelines concordance on a monthly basis; that is being expanded to look at individual provider performance.
A poster about the work, presented at IDWeek (No. 45), showed that these interventions improved DUHS’s guidelines concordance in the first six months of the project, from 31% to 39% at one hospital, from 48% to 49% at a second hospital, and from 48% to 60% at the third hospital. Further studies will tease out how to continue these improvements.
The goal is not to get to 100% guidelines concordance, Wrenn noted. For example, there will be cases in which patients have prior cultures indicating they need a different antibiotic or have adverse reactions to the guidelines-recommended treatment. Wrenn’s team also is sampling some cases in which providers didn’t follow the guidance and doing a deep chart review to identify why.
PeaceHealth Southwest Keeps Stewardship in the Family
UTIs also were the focus of a pharmacist-led ambulatory antimicrobial stewardship program in a family medicine clinic at PeaceHealth Southwest Medical Center, in Vancouver, Wash. There, a combination of in-person education for clinicians, a guidelines-based antibiotic treatment summary made available in the electronic health record (EHR), and treatment defaults in the electronic order sets nearly doubled guidelines-based treatment adherence for uncomplicated cystitis and pyelonephritis (J Clin Pharm Ther 2020 Jul 24. [Epub ahead of print]. doi: 10.1111/jcpt.13210). In 2018, before the intervention, 37% of patients were given the proper antibiotics at the appropriate dose and duration; that increased to 71.6% after the intervention (P<0.001).
Although it can be helpful to have stewardship teams in the background making changes to the EHR, the work gains traction in the live education and training of residents and clinicians, noted study co-author and clinical pharmacist Luke Vander Weide, PharmD. Clinics that have resident physicians who turn over annually can benefit from periodic reeducation about proper antibiotic selection, added study co-author and clinical pharmacist Julia McCormick, PharmD.
Johns Hopkins Bayview Reaches Into Underserved Departments
Pharmacists also can make a difference extending stewardship to previously untapped areas of the hospital. Johns Hopkins Bayview Medical Center, in Baltimore, did not have a clinical pharmacist dedicated to general and orthopedic surgery. Because pharmacy staff received a lot of clinical questions from this area, they wanted to see what would happen if a pharmacist was assigned to the units, said Farrah Tavakoli, PharmD, formerly with the medical center and now a formulary management pharmacist with the University of Maryland Medical System. In just a two-week period, the clinical pharmacist attended daily multidisciplinary rounds and made 218 interventions, including 38 recommendations to optimize antimicrobials, 26 recommendations to optimize anticoagulation, and provided education for 20 patients who were discharged on high-risk medications (J Pharm Pract 2020 Jul 21. doi. org/10.1177/0897190020938196). In an anonymous survey of multidisciplinary staff on these floors, 100% of respondents strongly agreed that a clinical pharmacist should be part of the team.

The hospital is in the process of working toward a full-time clinical pharmacist dedicated to that area, but meanwhile has central antimicrobial stewardship clinical pharmacist support to consult on and review key decisions, said study co-author Stacy Dalpoas, PharmD, the assistant director for decentralized and clinical pharmacy services for the hospital.
Beyond the Hospital Walls
Some antimicrobial stewardship efforts are moving outside of hospitals. Wrenn’s group at Duke, for example, is providing basic stewardship education this fall to dentists with the UNC 10% of all antibiotics in the U.S. [J Am Dent Assoc 2017;148(12):878-886] and often don’t have the support of an ID pharmacist there to help guide them in agent selection, duration and antibiotic allergies,” Wrenn said.
Long-term care facilities also have unique challenges for antimicrobial stewardship, said Kerry LaPlante, PharmD, with the VA Providence Healthcare System, in Rhode Island, and a professor of pharmacy at the University of Rhode Island, in Kingston. “What we typically see in long-term care is an older adult population with more vulnerability, increased UTIs, and more pneumonias and respiratory tract infections,” LaPlante said. “It’s much more challenging to discern if they have an active infection or not.”
Wanting to do no harm, physicians tend to give residents antibiotics, she said. “But it’s important that if there is a status change, that the providers and nurses in long-term care facilities evaluate the whole patient to determine if there is an environmental change, social changes, new medications or dehydration contributing to that status change. We really need to do a better job ruling out all other causes and not just think it’s a UTI and give an antibiotic.”
Telehealth for Smaller Hospitals
Some smaller and rural hospitals that don’t have their own stewardship teams are getting centralized telehealth help from pharmacists at a larger center, Davis said. Through these arrangements, a centralized stewardship team can track data on antibiotic use and resistance and review any challenging cases with a local physician or pharmacist, who can then talk to patients in person. She said Allegheny Health Network in western Pennsylvania and New York has such a system, and demonstrated that telehealth stewardship reduced the use of broad-spectrum antibiotics by 24% in a six-month period (Clin Infect Dis 2020;71[3]:539-545).
During COVID-19, ID pharmacists have helped with stewardship efforts in managing patients facing the novel infection, Dopp and Wrenn said.
Moving forward, there could be a role for antimicrobial stewardship in specialty clinics that see other conditions in which these drugs are frequently used, such as gastroenterology, oncology, urology, obstetrics and otolaryngology, Dopp said. Outpatient parenteral antimicrobial therapy, in which patients are discharged home or referred to an outpatient clinic with an IV antibiotic, also is an area for needed stewardship principles, she said. Dialysis clinics and substance use disorder programs present still more opportunities to expand, Davis said.
“Pharmacists can take a real prominent role in antimicrobial stewardship programs,” Dopp said. “They’ve demonstrated it in hospital settings and in emergency departments, so they should be considered as partners as some of these new locations are being considered.”
The sources reported no relevant fi nancial relationships.

School of Dentistry. “Dentists prescribe
—Karen Blum
Supporting Pharmacy Efficiency with a Growing Product Formulary

Liquid Unit Dose

from American Health Packaging
American Health Packaging delivers unit-dose products supporting patient safety and pharmacy efficiency initiatives. Products come in multiple pack sizes to provide flexibility in managing local inventory. Liquid Unit Dose cups are available through partner wholesalers and GPOs. Pull-tab labels promote ease of opening and product administration
Thick-gauge cups with excellent label seal integrity aid in avoiding costly damage and clean up

Legible labels aid in selecting correct products from the pharmacy shelf Cups and storage trays are designed to optimize limited storage space
ABC 8-digit # Cardinal Item # McKesson Item #

Morris & Dickson # Product Description Unit Strength
Cup Delivery Cup Strength
Pack Size NDC 10237650 5660352 1557057 906891 Amantadine HCl Sol 100mg/10mL 100mg/10mL 10mL 100mg/10mL 100ct 10211921 5517206 3795689 584466 Fluoxetine Oral Solution, USP 20mg/5mL 5mL 20mg/5mL 40ct 10188404 5465380 3917226 363275 Fluoxetine Oral Solution, USP 20mg/5mL 5mL 20mg/5mL 50ct 10228115 5552237 3968229 752410 Hydrocodone Bitartrate & APAP Oral Solution CII 7.25mg/325mg/15mL 15mL 7.25mg/325mg/15mL 50ct 10211783 5517214 3901766 584557 Levetiracetam Oral Solution, USP 100mg/mL 5mL 500mg/5mL 40ct 10183100 5430343 3775822 238550 Levetiracetam Oral Solution, USP 100mg/mL 5mL 500mg/5mL 50ct 10210354 5512413 3777034 568063 Ondansetron Oral Solution, USP 4mg/5mL 5mL 4mg/5mL 30ct 10219153 5528518 3949997 603993 Oxycodone HCl Oral Solution CII, USP 5mg/5mL 5mL 5mg/5mL 40ct 10219154 5528526 3950037 604306 Oxycodone HCl Oral Solution CII, USP 5mg/5mL 5mL 5mg/5mL 50ct At Duke University Hospital, in Durham, N.C., the antimicrobial stewardship and 10231522 5587894 2549509 822841 Phenobarbital Elixir CIV, USP* 20mg/5mL 5mL 20mg/5mL 50ct evaluation team (aset) created pocket cards (left) on appropriate antibiotic 10209414 5508114 3751294 560649 Phenytoin Oral Suspension, USP 125mg/5mL 4mL 100mg/4mL 50ct prescribing and placed the cards at workstations. The cards are part of Duke CustomID, a decision support tool intended to provide clinicians with 10211558 5515705 3935129 575878 Potassium Chloride Oral Solution, USP 10% 20mEq/15mL 15mL 20mEq/15mL 30ct institution-specific, accessible, easily customizable information 10212031 5520416 3909884 584904 Potassium Chloride Oral Solution, USP 10% 20mEq/15mL 15mL 20mEq/15mL 40ct about the diagnosis and treatment of infectious diseases. 10191061 5486220 3263035 321570 Potassium Chloride Oral Solution, USP 10% 20mEq/15mL 15mL 20mEq/15mL 50ct 10211557 5515713 3935137 575894 Potassium Chloride Oral Solution, USP 10% 20mEq/15mL 15mL 20mEq/15mL 80ct 10212749 5521521 3937786 591016 Potassium Chloride Oral Solution, USP 10% 20mEq/15mL 30mL 40mEq/30mL 40ct 10191066 5487574 3266467 465344 Potassium Chloride Oral Solution, USP 10% 20mEq/15mL 30mL 40mEq/30mL 50ct 10236851 5655030 1552645 881052 Siladryl Allergy (Diphenhydramine Hydrochloride) Antihistamine Liquid 25mg per 10mL 25mg/10mL 10mL 25mg/10mL 100ct 10182920 5427497 3772373 231159 Theophylline Oral Solution, USP 80mg/15mL 15mL 80mg/15mL 50ct 10231260 5583273 2080927 793638 Valproic Acid Oral Solution, USP 500mg/10mL 10mL 500mg/10mL 100ct *Product contains 10% alcohol. 60687-0239-56 60687-0244-77 60687-0244-67 60687-0417-71 60687-0249-77 60687-0249-67 60687-0252-86 60687-0406-77 60687-0406-67 60687-0448-67 60687-0275-66 60687-0341-58 60687-0341-64 60687-0341-71 60687-0341-07 60687-0341-14 60687-0341-72 60687-0267-56 60687-0258-71 60687-0262-56
Planning for 2021 reimbursement:
A Holiday of Opportunities and Responsibilities
As we’re entering the holiday season, let’s pause for a moment to see that we’re on track for all those important changes that will affect pharmacy reimbursement in 2021, in addition to the ones in the proposed 2021 Outpatient Prospective Payment System rules published previously (bit.ly/3jr7DwS). Not all are in “pharmacy-specific” rule sets or decisions, which makes bursting out of that silo and exploring other opportunities or recognizing implications of payment changes ever more important.
Use this to your competitive advantage! Each U.S. hospipital is required ed to provide clear, ar, accessible pricricing information mation online about the items he items and services they provide hey provide in two ways: 1) a compre1) a comprehensive machine-readable file ine-readable file with all items and services, and services, and 2) a display of shoplay of shoppable services in a conin a consumer-friendly format. y format.
What role has your has your pharmacy played in showcaslayed in showcasing the drug component of the shoppable services chosen by your facility? Still fuzzy on what’s required? Do you need more information to quickly move to being compliant? Check out these resources from the Centers for Medicare & Medicaid Services (CMS): • Hospital Price Transparency FAQs: go.cms.gov/30sFH4d • 8 Steps to a Machine-Readable File of All Items & Services: go.cms. gov/30sO14c • Quick Reference Checklists: go.cms. gov/33niOkz • 10 Steps to Making Public Standard
Charges for Shoppable Services –
This document contains a wealth of information, including how to make a consumer-friendly display to aid pricing transparency: go.cms. gov/2EYxb5I • For an overview of the pricing transparency requirements, check out the final rule in the Federal Register at bit.ly/33plnD2.
NTAPs for FY 2021
The new technology add-on payment (NTAP) program is a payment system designed by Congress to encourage the uptake of new and costly medical technologies in the hospital setting under the Hospital Inpatient Prospective Payment System (IPPS) in Medicare Part A. (FY 2021 IPPS Final Rule; bit.ly/ 3nuTem2). NTAPs provide separate payment outside of the diagnosis-related group (DRG) payment for new technology for a defined period of time when the products are used in the inpatient setting. This policy is applied in a similar manner to pass-through drugs, which provide separate payment in an outpatient setting. The Table summarizes those medications losing NTAP status and those with continuing status through fiscal year (FY) 2021.

There also are important new payment changes under NTAPs addressing chimeric antigen receptor (CAR) T-cell therapy products and certain antimicrobials:
CAR T-Cell Therapy
Payments for CAR T-cell therapy fall under CMS’s Medicare Severity (MS)DRG 018 for CAR T-cell treatment stays, with differential reimbursement based on whether the product was provided as part of a clinical trial. MS-DRG 018 includes several important additional
Table. Table T bl FY 2021 NTAPs FY2021NTAPs FY 2021 NTA AP



Product (NEW) ICD-10-PCS Code
IMFINZI® (durvalumab) and TECENTRIQ® (atezolizumab) XW03336 or XW04336 (IMFINZI) & XW033D6 or XW034D6 (TECENTRIQ)
Max NTAP FY 2021
$6,875.90
Soliris (eculizumab)®
NUZYRA® (omadacycline) for Injection XW033C6 or XW043C6 $21,199.75
XW033B6 or XW043B6 $1,552.50
RECARBRIO™ (imipenem, cilastatin, and relebactam) XW033U5 or XW043U5 $3,532.78
XENLETA™ (lefamulin) XW03366 or XW04366 or XW0DX66 $1,275.75
ZERBAXA® (ceftolozane and tazobactam) XW03396 or XW04396 $1,836.98
Andexxa™ (coagulation factor Xa (recombinant), inactivated-zhzo) XW03372 or XW04372 $18,281.25
AZEDRA® (iobenguane Iodine-131) Solution XW033S5 and XW043S5 $98,150.00
CABLIVI® (caplacizumab-yhdp) XW013W5, XW033W5, and XW043W5 $33,215.00
ELZONRIS™ (tagraxofusp-erzs) XW033Q5 and XW043Q5 $125,448.05
Balversa™ (erdafitinib) XW0DXL5 $3,563.23
SPRAVATO™ (esketamine) XW097M5 $1,014.79
XOSPATA® (gilteritinib) XW0DXV5 $7,312.50
“Reimbursement Matters” is a tool for maintaining your health system’s fiscal health. Please email the author at bonniekirschenbaum@ gmail.com with suggestions on reimbursement issues that you would like to see covered. Bonnie Kirschenbaum, MS, FASHP, FCSHP
features and reimbursement codes to keep in mind: • Payment rate of $239,928.79, assuming a wage index adjustment of <1, not including adjustments • Relative weight for the CAR T-cell
MS-DRG (37.290) is the highest under the IPPS • Maps the following ICD-10-PCS (Procedure Coding System) codes to the new MS-DRG (both used to report administration of tisagenlecleucel [Kymriah, Novartis] and axicabtagene [Yescarta, Kite Pharma]): - XW033C3: introduction of engineered autologous chimeric antigen receptor t-cell immunotherapy into central vein, percutaneous approach, new technology group 3 - XW043C3: introduction of engineered autologous chimeric antigen receptor t-cell immunotherapy into central vein, percutaneous approach, new technology group 3) • New ICD-10-PCS codes for brexucabtagene autoleucel (Tecartus, Kite
Pharma) and lisocabtagene maraleucel (liso-cel, Bristol-Myers Squibb) to MS-DRG 018. (Note that lisocabtagene maraleucel is an investigational
CAR T-cell therapy in development for the treatment of adult patients with relapsed or refractory large
B-cell lymphoma; it has not yet been approved by the FDA.)
There are two additional CAR T-cell therapy reimbursement wrinkles to consider:
1. Cost-to-charge ratios (CCRs).
“There is nothing that precludes hospitals from setting their drug charges consistent with their CCRs,” CMS noted in the NTAP section of the IPPS final rule (bit.ly/30JttnY). CMS added that tumor-infiltrating lymphocyte therapy and engineered T-cell receptor therapy are on the horizon; the agency thus plans to engage stakeholders to ensure prompt patient access. 2. Discontinued coverage. It’s critical to note that NTAPs for tisagenlecleucel and axicabtagene have been discontinued for FY 2021 due to time limits. The cost criterion threshold for the new MS-DRG
018 is set at $1,237,393. Unfortunately, NTAP applications for brexucabtagene autoleucel and liso-cel didn’t meet the July 1 deadline for FDA approval and aren’t eligible for the FY 2021 NTAP.
Antibiotic Therapy
CMS established an alternative NTAP policy for certain antimicrobial products:
FY 2020: Products with the FDA’s qualified infectious disease product (QIDP) designation are considered new and not substantially similar to an existing technology for purposes of NTAP. As such, they don’t need to meet the “substantial clinical improvement” criterion but only the cost criterion.
FY 2022: CMS expands the alternative NTAP pathway for QIDPs to include products approved through the FDA’s limited population pathway for antibacterial and antifungal drugs (LPAD pathway). There aren’t any products approved under the LPAD pathway to date.
FY 2022 and subsequent years: If an antimicrobial product is approved through the FDA’s LPAD pathway, it will be considered new and not substantially similar to an existing technology for purposes of an NTAP, and does not need to meet the “substantial clinical improvement” criterion but only the cost criterion.
For QIDPs that do not receive FDA approval by July 1, and products that do not receive approval through the FDA’s LPAD pathway by July 1 but otherwise meet the applicable addon payment criteria, CMS will provide conditional NTAP approval to enable certain antimicrobial products to receive an NTAP sooner, effective for discharges the quarter after the date of FDA approval.
Recurring Denials And Incomplete Claims!
Do whatever you need to do to stop this. Why continue to waste time and resources appealing denied claims over and over again. Get to the root cause of the problem, and change your problematic standard operating procedures to which an analysis of patterns of denials point. Is it prior authorizations? Other payor requirements? Billing unit conversion errors? Healthcare Common Procedural Coding System (HCPCS) errors/miscoding? Poor/ incomplete documentation? Outdated charge description masters? Inappropriate scrubbing or hard stops? Missing national drug codes? Unidentified/incorrect payor info? Randomly pick 10 denied outpatient charges and follow each step along the way, from the computerized prescriber order entry order to actual payment or denial to find the missteps. You cannot afford to be complicit in this recurring problematic cycle—especially at a time when your facility is in desperate need of revenue.
Reporting Bevacizumab For Ophthalmologic Use
Local coverage article A53121 Information Regarding Uses, Including OffLabel Uses, of Anti-Vascular Endothelial Growth Factor (anti-VEGF), for The Treatment of Ophthalmological Diseases on 2.13.2020 has been revised to clarify billing instructions. Physicians providing bevacizumab for ophthalmologic use should report HCPCS code J7999 (compounded drug, not otherwise classified). Each 1.25-mg dose administered is considered one unit. The total dosage administered should be noted in the “remarks” section of the claim.
A Shout-out to APhA!
Recognizing that many pharmacists and technicians need more background on reimbursement, the American Pharmacists Association (APhA) began a helpful series, “Learn the Lingo.” The latest is “Learn the Lingo—Bundled Payment Models,” which APhA members may access at bit.ly/2GHS2dVZ.
New Patient Assistance Resource
MLN Connects, the official CMS news from the Medicare Learning Network, announced a new section dedicated to information in assisting you in working with your patients. The inaugural piece is “Making Insulin More Affordable for Medicare Patients Beginning January 1,” which can be accessed on CMS’s Fact Sheet: Part D Senior Savings Model at go.cms.gov/2SC3afb. ■
Amid COVID-19, the Challenge of DIY 503B Continues
In retrospect, Vanderbilt University Medical Center hit “pause” on creating its own in-house 503B compounding facility at just the right time. As 2019 drew to a close, the medical center’s Department of Pharmaceutical Services determined that, before moving forward, it would take the time to put key products through the enhanced stability testing required for meeting the extended beyond-use dating (BUD) ‘In these critical [pandemic] situations, I cannot underscore enough the importance of having these [outsourcing] relationships, and even multiple relationships for redundancy.’
—Deidra Dickerson, PharmD
standards that are part of the FDA’s current good manufacturing practice requirements for 503B compounding outsourcing facilities.
“We wanted to send all of our products through that level of testing just as a measure of preparedness for the future,” Deidra Dickerson, PharmD, the manager of sterile and nonsterile compounding at the Nashville, Tenn., institution, told Pharmacy Practice News. “So at the end
NUZYRA® (omadacycline) injection for intravenous use NUZYRA® (omadacycline) tablets, for oral use
BRIEF SUMMARY OF FULL PRESCRIBING INFORMATION
For complete details, please see Full Prescribing Information.
INDICATIONS AND USAGE Community-Acquired Bacterial Pneumonia (CABP)
NUZYRA is indicated for the treatment of adult patients with communityacquired bacterial pneumonia (CABP) caused by the following susceptible microorganisms: Streptococcus pneumoniae, Staphylococcus aureus (methicillin-susceptible isolates), Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, Legionella pneumophila, Mycoplasma pneumoniae, and Chlamydophila pneumoniae.
Acute Bacterial Skin and Skin Structure Infections (ABSSSI)
NUZYRA is indicated for the treatment of adult patients with acute bacterial skin and skin structure infections (ABSSSI) caused by the following susceptible microorganisms: Staphylococcus aureus (methicillinsusceptible and -resistant isolates), Staphylococcus lugdunensis, Streptococcus pyogenes, Streptococcus anginosus grp. (includes S. anginosus, S. intermedius, and S. constellatus), Enterococcus faecalis, Enterobacter cloacae, and Klebsiella pneumoniae. USAGE: To reduce the development of drug-resistant bacteria and maintain the effectiveness of NUZYRA and other antibacterial drugs, NUZYRA should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy. CONTRAINDICATIONS: NUZYRA is contraindicated in patients with known hypersensitivity to omadacycline or tetracycline-class antibacterial drugs, or to any of the excipients.
WARNINGS AND PRECAUTIONS Mortality Imbalance in Patients with Community-Acquired Bacterial
Pneumonia-Mortality imbalance was observed in the CABP clinical trial with eight deaths (2%) occurring in patients treated with NUZYRA compared to four deaths (1%) in patients treated with moxifloxacin. The cause of the mortality imbalance has not been established. All deaths, in both treatment arms, occurred in patients >65 years of age; most patients had multiple comorbidities. The causes of death varied and included worsening and/or complications of infection and underlying conditions. Closely monitor clinical response to therapy in CABP patients, particularly in those at higher risk for mortality. Tooth Discoloration and Enamel Hypoplasia-The use of NUZYRA during tooth development (last half of pregnancy, infancy, and childhood up to the age of 8 years) may cause permanent discoloration of the teeth (yellow-gray-brown). This adverse reaction is more common during long- term use of the tetracycline-class drugs, but it has been observed following repeated short-term courses. Enamel hypoplasia has also been reported with tetracycline-class drugs. Advise the patient of the potential risk to the fetus if NUZYRA is used during the second or third trimester of pregnancy. Inhibition of Bone Growth-The use of NUZYRA during the second and third trimester of pregnancy, infancy and childhood up to the age of 8 years may cause reversible inhibition of bone growth. All tetracyclines form a stable calcium complex in any bone-forming tissue. A decrease in fibula growth rate has been observed in premature infants given oral tetracycline in doses of 25 mg/kg every 6 hours. This reaction was shown to be reversible when the drug was discontinued. Advise the patient of the potential risk to the fetus if NUZYRA is used during the second or third trimester of pregnancy. Hypersensitivity Reactions-Hypersensitivity reactions have been reported with NUZYRA. Life-threatening hypersensitivity (anaphylactic) reactions have been reported with other tetracycline-class antibacterial drugs. NUZYRA is structurally similar to other tetracycline-class antibacterial drugs and is contraindicated in patients with known hypersensitivity to tetracycline-class antibacterial drugs. Discontinue NUZYRA if an allergic reaction occurs. Clostridium difficile-Associated Diarrhea-Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile. C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents. If CDAD is suspected or confirmed, ongoing antibacterial drug use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial drug treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated. Tetracycline-Class Effects-NUZYRA is structurally similar to tetracycline- class of antibacterial drugs and may have similar adverse reactions. Adverse reactions including photosensitivity, pseudotumor cerebri, and anti-anabolic action (which has led to increased BUN, azotemia, acidosis, hyperphosphatemia, pancreatitis, and abnormal liver function tests), have been reported for other tetracycline-class antibacterial drugs, and may occur with NUZYRA. Discontinue NUZYRA if any of these adverse reactions are suspected. Development of Drug-Resistant Bacteria: Prescribing NUZYRA in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria. ADVERSE REACTIONS: The following clinically significant adverse reactions are described in greater detail in the Warnings and Precautions section of the labeling: • Mortality Imbalance in • Inhibition of Bone Growth Patients with CommunityAcquired Bacterial Pneumonia • Hypersensitivity Reactions • Tooth Development and • Tetracycline-Class Effects Enamel Hypoplasia
Clinical Trials Experience-Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. Overview of the Safety Evaluation of NUZYRA: NUZYRA was evaluated in three Phase 3 clinical trials (Trial 1, Trial 2 and Trial 3). These trials included a single Phase 3 trial in CABP patients (Trial 1) and two Phase 3 trials in ABSSSI patients (Trial 2 and Trial 3). Across all Phase 3 trials, a total of 1073 patients were treated with NUZYRA (382 patients in Trial 1 and 691 in Trials 2 and 3) of which 368 patients were treated with only oral NUZYRA. Imbalance in Mortality: In Trial 1, eight deaths (2%) occurred in 382 patients treated with NUZYRA as compared to four deaths (1%) in 388 patients treated with moxifloxacin. All deaths, in both treatment arms, occurred in patients >65 years of age. The causes of death varied and included worsening and/or complications of infection and underlying conditions. The cause of the mortality imbalance has not been established [see Warnings and Precautions (5.1)]. Serious Adverse Reactions and Adverse Reactions Leading to Discontinuation: In Trial 1, a total of 23/382 (6.0%) patients treated with NUZYRA and 26/388 (6.7%) patients treated with moxifloxacin experienced serious adverse reactions. Discontinuation of treatment due to any adverse reactions occurred in 21/382 (5.5%) patients treated with NUZYRA and 27/388 (7.0%) patients treated with moxifloxacin. Most Common Adverse Reactions: Table 4 lists the most common adverse reactions occurring in ≥2% of patients receiving NUZYRA in Trial 1. Table 4: Adverse Reactions Occurring in ≥2% of Patients Receiving
NUZYRA in Trial 1
Adverse Reaction NUZYRA (N = 382) Moxifloxacin (N = 388)
Alanine aminotransferase increased 3.7 4.6
Hypertension 3.4 2.8
Gamma-glutamyl transferase increased 2.6 2.1
Insomnia 2.6 2.1
Vomiting 2.6 1.5
Constipation 2.4 1.5
Nausea 2.4 5.4

—Eric Kastango, MBA, BSPharm
of 2019, we made the decision to start using a 503B outsourcing facility while pulling back from our own internal program, planning to ramp back up later once the results started trickling in.”
After meeting with several outsourcing facilities, Vanderbilt settled on QuVa, which has compounding facilities in Sugar Land, Texas, and Bloomsbury, N.J., serving more than 2,200 hospital customers with over 280 product SKUs. “We placed our
NUZYRA® (omadacycline) injection for intravenous use NUZYRA® (omadacycline) tablets, for oral use
Serious Adverse Reactions and Adverse Reactions Leading to Discontinuation: In the pooled ABSSSI trials, serious adverse reactions occurred in 16/691 (2.3%) of patients treated with NUZYRA and 13/689 (1.9%) of patients treated with comparator. Discontinuation of treatment due to adverse events occurred in 12 (1.7%) NUZYRA treated patients, and 10 (1.5%) comparator treated patients. There was 1 death (0.1%) reported in NUZYRA treated patients and 3 deaths (0.4%) reported in linezolid patients in ABSSSI trials. Most Common Adverse Reactions: Table 5 includes the most common adverse reactions occurring in ≥2% of patients receiving NUZYRA in Trials 2 and 3. Table 5: Adverse Reactions Occurring in ≥2% of Patients Receiving
NUZYRA in Pooled Trials 2 and 3
Adverse Reaction NUZYRA (N = 691) Linezolid (N = 689)
Nausea* 21.9 8.7
Vomiting 11.4 3.9
Infusion site reactions** 5.2 3.6
Alanine aminotransferase increased 4.1 3.6
Aspartate aminotransferase increased 3.6 3.5
Headache 3.3 3.0
Diarrhea 3.2 2.9
*In Trial 2, which included IV to oral dosing of NUZYRA, 40 (12%) patients experienced nausea and 17 (5%) patients experienced vomiting in
NUZYRA treatment group as compared to 32 (10%) patients experienced nausea and 16 (5%) patients experienced vomiting in the comparator group. One patient (0.3%) in the NUZYRA group discontinued treatment due to nausea and vomiting. *In Trial 3, which included the oral loading dose of NUZYRA, 111 (30%) patients experienced nausea and 62 (17%) patients experienced vomiting in NUZYRA treatment group as compared to 28 (8%) patients experienced nausea and 11 (3%) patients experienced vomiting in the linezolid group. One patient (0.3%) in the NUZYRA group discontinued treatment due to nausea and vomiting. **Infusion site extravasation, pain, erythema, swelling, inflammation, irritation, peripheral swelling and skin induration. Selected Adverse Reactions Occurring in Less Than 2% of Patients Receiving NUZYRA in Trials 1, 2 and 3: The following selected adverse reactions were reported in NUZYRA-treated patients at a rate of less than 2% in Trials 1, 2 and 3. Cardiovascular System Disorders: tachycardia, atrial fibrillation; Blood and Lymphatic System Disorders: anemia, thrombocytosis; Ear and Labyrinth Disorders: vertigo; Gastrointestinal Disorders: abdominal pain, dyspepsia; General Disorders and Administration Site Conditions: fatigue; Immune System Disorders: hypersensitivity; Infections and Infestations: oral candidiasis, vulvovaginal mycotic infection; Investigations: creatinine phosphokinase increased, bilirubin increased, lipase increased, alkaline phosphatase increased; Nervous System Disorders: dysgeusia, lethargy; Respiratory, Thoracic, and Mediastinal disorders: oropharyngeal pain; Skin and Subcutaneous Tissue Disorders: pruritus, erythema, hyperhidrosis, urticaria.
DRUG INTERACTIONS
Anticoagulant Drugs-Because tetracyclines have been shown to depress plasma prothrombin activity, patients who are on anticoagulant therapy may require downward adjustment of their anticoagulant dosage while also taking NUZYRA. Antacids and Iron Preparations-Absorption of oral tetracyclines, including NUZYRA, is impaired by antacids containing aluminum, calcium, or magnesium, bismuth subsalicylate, and iron containing preparations.
USE IN SPECIFIC POPULATIONS
Pregnancy: Risk Summary—NUZYRA, like other tetracycline-class antibacterial drugs, may cause discoloration of deciduous teeth and reversible inhibition of bone growth when administered during the second and third trimester of pregnancy. The limited available data of NUZYRA use in pregnant women is insufficient to inform drug associated risk of major birth defects and miscarriages. Animal studies indicate that administration of omadacycline during the period of organogenesis resulted in fetal loss and/or congenital malformations in pregnant rats and rabbits at 7 times and 3 times the mean AUC exposure, respectively, of the clinical intravenous dose of 100 mg and the oral dose of 300 mg. Reductions in fetal weight occurred in rats at all administered doses (see Data). In a fertility study, administration to rats during mating and early pregnancy resulted in embryo loss at 20 mg/kg/day; systemic exposure based on AUC was approximately equal to the clinical exposure level. Results of studies in rats with omadacycline have shown tooth discoloration. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15-20%. Results of animal studies indicate that tetracyclines cross the placenta, are found in fetal tissues, and can have toxic effects on the developing fetus (often related to retardation of skeletal development). Evidence of embryotoxicity also has been noted in animals treated early in pregnancy. Lactation: Risk Summary—There is no information on the presence of omadacycline in human milk, the effects on the breastfed infant or the effects on milk production. Tetracyclines are excreted in human milk; however, the extent of absorption of tetracyclines, including omadacycline, by the breastfed infant is not known. Because there are other antibacterial drug options available to treat CABP and ABSSSI in lactating women and because of the potential for serious adverse reactions, including tooth discoloration and inhibition of bone growth, advise patients that breastfeeding is not recommended during treatment with NUZYRA and for 4 days (based on half-life) after the last dose.
Females and Males of Reproductive Potential
Contraception Females: NUZYRA may produce embryonic or fetal harm. Advise patients to use an acceptable form of contraception while taking NUZYRA. Infertility Males: In rat studies, injury to the testis and reduced sperm counts and motility occurred in male rats after treatment with omadacycline. Females: In rat studies, omadacycline affected fertility parameters in female rats, resulting in reduced ovulation and increased embryonic loss at intended human exposures. Pediatric Use-Safety and effectiveness of NUZYRA in pediatric patients below the age of 18 years have not been established. Due to the adverse effects of the tetracycline-class of drugs, including NUZYRA on tooth development and bone growth, use of NUZYRA in pediatric patients less than 8 years of age is not recommended. Geriatric Use-Of the total number of patients who received NUZYRA in the Phase 3 clinical trials (n=1073), 200 patients were ≥65 years of age, including 92 patients who were ≥75 years of age. In Trial 1, numerically lower clinical success rates at early clinical response (ECR) timepoint for NUZYRA-treated and moxifloxacin-treated patients (75.5% and 78.7%, respectively) were observed in CABP patients ≥65 years of age as compared to patients <65 years of age (85.2% and 86.3%, respectively). Additionally, all deaths in the CABP trial occurred in patients >65 years of age. No significant difference in NUZYRA exposure was observed between healthy elderly subjects and younger subjects following a single 100 mg IV dose of NUZYRA. Hepatic Impairment-No dose adjustment of NUZYRA is warranted in patients with mild, moderate, or severe hepatic insufficiency (Child-Pugh classes A, B, or C). Renal Impairment-No dose adjustment of NUZYRA is warranted in patients with mild, moderate, or severe renal impairment, including patients with end stage renal disease who are receiving hemodialysis. OVERDOSAGE No specific information is available on the treatment of overdosage with NUZYRA. Following a 100 mg single dose intravenous administration of omadacycline, 8.9% of dose is recovered in the dialysate.
To report SUSPECTED ADVERSE REACTIONS, contact Paratek Pharmaceuticals, Inc. at 1-833-727-2835 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
Distributed by: Paratek Pharmaceuticals, Inc. Boston, MA, USA PARATEK® and the hexagon logo are registered trademarks of Paratek Pharmaceuticals, Inc. NUZYRA® and its design logo are registered trademarks of Paratek Pharmaceuticals, Inc. For patent information: www.paratekpharma.com/products/patent. © 2019 Paratek Pharmaceuticals, Inc. All rights reserved. first order with QuVa in January, right before the pandemic hit the United States,” Dickerson said. “By March and April, they were experiencing such demand that they were no longer able to bring on new customers because of the need to properly serve existing customers.”
Vanderbilt initially outsourced only a handful of products to QuVa, including ephedrine, epinephrine and phenylephrine syringes, and phenylephrine and midazolam IV bags. But as the pandemic continued, more were added. “Fentanyl was an item that became challenging early on, and we were having difficulties procuring any of the vials for infusion we typically get from our standard wholesaler,” Dickerson said. “QuVa was able to step in then, which took a stressor off of us during that time frame.”
Funds Dry Up During Pandemic
Before the pandemic, many hospitals and health systems, like Vanderbilt, were putting significant investments into pharmacy as one of their profit centers. However, with COVID-19 decimating the bottom line for many institutions, the availability of capital for major new investments, such as a 503B compounding facility, has dried up. “Of the CEOs and chief pharmacy officers I’ve spoken with, most of them say that prospectively trying to get into 503Bs probably isn’t in the works for at least another couple of years, financially speaking,” said Michael Souza, the CEO of New England Life Care (NELC), whose Advanced Compounding Solutions (ACS) 503B outsourcing facility is jointly owned by its 50-plus member hospitals (most in the Northeast).
“We are experiencing an uptick in interest based on our model, so much so that we’ve created a joint venture with another system-owned 503B facility in Minnesota, and we are combining our efforts both to market to a broader base and provide more capacity for the increased demand we’re seeing,” said Keith Thomasset, PharmD, ACS’ vice president of clinical solutions and chief pharmacy officer. “I would say that this is at least partially attributable to pressures from the pandemic, especially for those hospitals that were considering developing their own 503Bs. But even pre-pandemic, the capital investment
503B CHALLENGE
continued from page 35 [Outsourcers] can have a portfolio of 50 items or more, but for














and operating expenses associated with smaller [in-house 503B] operations like ours, it doesn’t make sense opening a 503B can get pretty scary if you’re going it alone.” to have all those products, especially if only one or two of our sites
Fagron Sterile Services US, anoth- use them or the volumes are really low. There’s a place for both.’er leading 503B outsourcing company, found early in the pandemic that it had —Kristina Bryowsky, PharmDto modify its production planning. “We had a significant increase, approximately of existing products for needs such as sup- Fagron Sterile Services US. “They needed within their facilities to provide the dos20%, in demand from our customers, porting high numbers of patients going high quantities of narcotics like fentanyl age forms and volumes they needed. with hospitals requiring new and differ- on ventilators,” said Jason McGuire, who and hydromorphone to sedate patients, Every day, there was something new that ent products or much greater quantities oversees operational and quality areas of and they just didn’t have the support would pop up from health systems, and some of these products, quite frankly, we didn’t have immediately available,” McGuire said. “But we [were] still able to respond fairly quickly with something
Read Pharmacy Practice News that would work and yet maintain a high level of quality.”
Anywhere, Anytime! A Pioneer Partners Up
The midwestern hospital system SSM Health, which operates more than two dozen hospitals and health centers in Wisconsin, Illinois, Oklahoma and Missouri, was the first health system to register as a 503B sterile compounder in 2014, and remains one of only a handful of such systems in the country. SSM Health currently produces about nine products in-house. Because operating rooms closed to elective surgeries during the height of the pandemic, SSM Health pharmacy director Kristina Bryowsky, PharmD, said her facility shifted production toward bags for the ICU and away from OR syringes. “We saw a reduction in volume overall because of the ORs, so we shifted the days we would have produced other products to make sure we stocked up heavily on IV products for the ICUs, so we never had a shortage of those bags. That was a big relief for our ICU team,” said Bryowsky, a Pharmacy Practice News editorial advisory board member. In December 2019, SSM Health had started its first round of testing to add fentanyl to its list of compounded products, but after the pandemic began, the system was unable to access active pharmaceutical ingredients (API) to complete the next two rounds of testing. Bryowsky said they will complete that testing before the end of the year, but in the meantime, to accommodate the high volume of fentanyl needed at the system’s larger hospitals, they use either an outsourcer or compound in-house under 503A’s internal <797> seven-day BUD limits. “Some of our bigger centers had allocations with larger outsourcers, but if you didn’t have that already, you weren’t going to get it during COVID-19,” Bryowsky said. “Because our ORs were closed and care had shifted to patients who were incredibly acute, the volume wasn’t as high. So we were able to spend the extra www.pharmacypracticenews.com time to make internal batches of 300 bags with 2- or 5-mL vials, which is not
Flexibility From the FDA

During the COVID-19 pandemic, the FDA provided some flexibility for both 503B outsourcing facilities that produce large batches of product with or without prescriptions while adhering to current good manufacturing practices (CGMPs), as well as 503A entities, which are traditional compounding pharmacies that compound in accordance with patient-specific prescriptions and comply with U.S. Pharmacopeia (USP) standards.
In April, the agency issued two guidance documents establishing temporary policies regarding the compounding of certain drugs. For 503Bs, the FDA said that under the current state of supply disruption, it would not take action against an outsourcing facility for compounding a drug that is considered essentially a copy of an approved drug, or for using bulk substances not on the FDA’s approved Bulks List if those drug products are used to treat COVID19 for hospitalized patients. The agency also would not pursue enforcement against 503Bs for not meeting CGMP requirements for product stability testing and establishment of an expiration date, provided the outsourcer used shorter default beyond-use dates (BUD)s as specified by the FDA. Furthermore, in an unprecedented move, 503As would be temporarily permitted to compound drugs in short supply for hospital patients with COVID-19 without a patient prescription.
“They’ve flexed pharmacy,” said Eric Kastango, BSPharm, the vice president and managing partner at Kastango Consulting Group. “The 503Bs have capacity limits: There are only so many doses they can make and they only have so much ability to ramp up production to meet demand. With the COVID crisis and the number of patients who needed emergency medications, they could not keep up. So, the agency published a guidance of when a 503A can do compounding that is typically limited to a 503B, identifying half a dozen mostly critical care, anesthesia and pain management agents.”
Still unknown: the question of when and how the FDA will ultimately implement its draft “one mile” rule, which allows 503A compounding hospital pharmacies to distribute compounded drugs to health care facilities owned and controlled by the same entity as the pharmacy, as long as they are located within a one-mile radius of the pharmacy. The rule, first released in draft form as part of the agency’s 2016 compounding guidance, is based on the reasoning that a central pharmacy sending compounded drugs beyond the one-mile limit would be operating like a 503B pharmacy but not regulated like one.
In its April 2020 guidance, the agency made it clear that the rule was still in draft and would not be enforced at present. “The FDA has been saying for well over a year now that the new version is coming, and that they are considering all of the comments they’ve received,” said Mike Koch, the senior vice president of professional services for Central Admixture Pharmacy Services, a national network of outsourcing pharmacies. “They have also previously hinted that they may alter the one-mile radius either by making it time dependent, in terms of beyond-use dating, or by extending the radius. But it’s all just rumors right now, and I wouldn’t begin to hazard a guess on what they will ultimately say or their timing.” —G.S.
something an outsourcer will do anyway.” Because of the shutdown of elective surgeries in both hospital ORs and ambulatory surgery centers, compounders such as Fagron also were able to free up some of their capacity and shift it to meet hospitals’ ICU needs. “It was still a bit of a challenge, especially as it relates to narcotics—you have to go to the Drug Enforcement Administration [DEA] and request access for more than your original quote,” McGuire said. “Fortunately, the DEA was very responsive and helpful, as was the FDA. For example, if there was a product that we had never created before within our facility, we might not have performed the full stability testing or validation around it. So we were permitted to leverage our partner laboratories’ data available via R&D or the published literature, and then using FDA guidance, get something out there, even though it might have more limited dating. They were really trying to find ways for outsourcing facilities to be flexible during this extraordinary time, to meet patient needs while still maintaining our responsibility for the high quality of the products we produce.”
The February closure of PharMedium, AmerisourceBergen’s compounding business, was a double whammy for hospitals in the Northeast, noted Stuart Hinchen, the co-founder and chief executive officer of QuVa. “The initial wave of COVID hit the Northeast particularly hard, and that was also an area where PharMedium had been very strong,” Hinchen said. “So a lot of hospitals were really cut short, and we were getting four times the regular demand for certain products, particularly in critical care. We had to give preferential treatment to COVID-related products wherever we could. We looked at other inventory we had on the shelves, and where we had adequate reserves, slots that would have gone to that inventory were reallocated to COVID-related products. Throughout March and April, every day was a major production effort and there really was no playbook.”
As changes in the pandemic have rippled throughout the country, along with reopenings of elective procedures, outsourcers have worked to keep up with shifting demand. “COVID-19 became less frantic in May, but then elective surgeries started to open up in June, so we went through an oscillation as the health networks were extremely keen to get those going again,” Hinchen said. “Then in the summer, COVID-19 cases spiked in the Sun Belt and we had dual pressures of both COVID-19 and elective surgeries.”
QuVa, NELC/ACS and Fagron all have increased capacity to meet the changing demand. QuVa has added more than 100 people to its labor force this year, with more staffing planned in the immediate future. “We put on a third shift in our Sugar Land site, which handles the bulk of our compounding work, and five days a week we are running 24/7 with stopgap work over the weekend,” Hinchen said. The company’s 75,000-square-foot facility in New Jersey will double in size over the next 12 months, and a lease on a new facility in Sugar Land also will double the company’s current 75,000-square-foot footprint in Texas. Similarly, NELC/ACS has added weekend shifts and filled all its hoods on the weekday second shift.

A Need to Pivot Quickly
Although NELC/ACS, like its non-hospital-owned competitors, experienced an early increase in demand for some supplies at the height of the pandemic, particularly products for patients on mechanical ventilation, Thomasset said there was never significant concern that they would not be able to meet demand. “We tend to keep at least three to four months’ worth of API on our shelves, so API shortages that affected some hospitals were not affecting us. The FDA had also provided guidance that we could compound sterile preparations from sterile API with a small extension beyond the current USP <797> BUD without requiring studies. That gave us upwards of about a month’s worth of expiration.” (See sidebar.)
McGuire said the biggest lesson for 503B compounders from the COVID-19 pandemic has been understanding how to pivot very quickly. “You need to have a culture in your business where people are willing to do whatever it takes to meet patients’ needs,” he said. “It was amazing to see how folks rallied around each other and made sure we did everything possible to get medicine out the door to wherever the needs were.”
Vanderbilt is still in discussions about creating its own 503B facility—a conversation that Dickerson said will likely take several years—and does plenty of its own 503A compounding, with only about 10 products outsourced. But regardless of what happens with those plans, the medical center still will continue relationships with 503B compounding outsourcers. “Even aside from the pandemic, we know there are still some products that it doesn’t make financial sense for us to make in-house,” she said. “Some institutions still have fears associated with 503Bs, and frustrations with them because the consistency of product availability may not always be what people would hope. But in these critical situations, I cannot underscore enough the importance of having these [outsourcing] relationships, and even multiple relationships for redundancy.”
Bryowsky agreed. “We still have outsourcing partnerships and always will. [Outsourcers] can have a portfolio of 50 items or more, but for smaller [in-house 503B] operations like ours, it doesn’t make sense to have all those products, especially if only one or two of our sites use them or the volumes are really low. There’s a place for both.”
Eric Kastango, MBA, BSPharm, the vice president and managing partner at Kastango Consulting Group, cited cost as perhaps the biggest barrier to taking a DIY approach to 503B compounding. “[It] costs, by conservative estimates, $5 [million] to $15 million and three years to open your doors,” he said. “It’s not a quick fix, not just <797> on steroids.
“Most of the people I have spoken with are going to multiple sources and have created relationships with more than one 503B,” Kastango added. “Most people can’t get by using just one 503B vendor, because they don’t all make the same products, or they are looking for supply redundancy. This pandemic has given us a new appreciation for just how important this unsexy part of pharmacy—compounding and distribution—really is.”
—Gina Shaw





