Mona Amini, MD, shares how moving to concierge psychiatry helps her patients see positive results.
21 years
National Asset Protec tion
Legal prac tice in 2024
IK E DE VJI
Founde r and Managing At torney
PRO AS SE T PROTECTION
Of Counsel, Davis Miles McGuire Gardner
Of Counsel, Lodmell & Lodmell

202 4 marks 21 years of legal prac tice devoted exclusively to asse t protec tion , wealth preser vation and risk management planning Of ten at the referral of A rizona’s bes t law yers and advisors , we help protec t billions of dollars in personal asse ts for a national client base of thousands of successful clients including:
• Real Es tate Inves tors
• Business Owners and Entrepreneurs
• Physicians
We have a wide range of cut ting edge strategies available that include both well proven conventional domestic planning , of fshore strategies and plans that combine the best of both.
• C - level E xecs
• Family Business O wners
• And Some of Arizona’s Most Successful Law ye rs!


Editor-In-Chief
Desire’e Hardge, MBA
Managing Editor Edward Araujo
Creative Design
Randi Karabin, KarabinCreative.com
Cover & Featured Articles
Photography Jeff Noble, jeffnoblepictures.com
Advertising ads@arizonaphysician.com
Maricopa County Medical Society Board Members
President Jane Lyons, MD
Treasurer Vishal Verma, MD, MBA
Secretary Karyne Vinales, MD
Past President
Zaid Fadul, MD, FS, FAAFP
Directors
Kishlay Anand, MD, MS
Jay Arora, MD, MBA
Rahul S. Rishi, DO, FAAAAI, FACAAI
Ann Cheri Foxx-Leach, MD, D.ABA
Resident & Fellow Director Issa Ismail, DO
Medical Student Director
Samantha Matta, OMS-III

Hospice of the Valley’s leadership team discusses HOV’s growth, services & programs, and how their dementia care center is impacting valley communities.
Digital & Social Media
arizonaphysician.com
ArizonaPhysician
@AZPhysician

@AZ_Physician
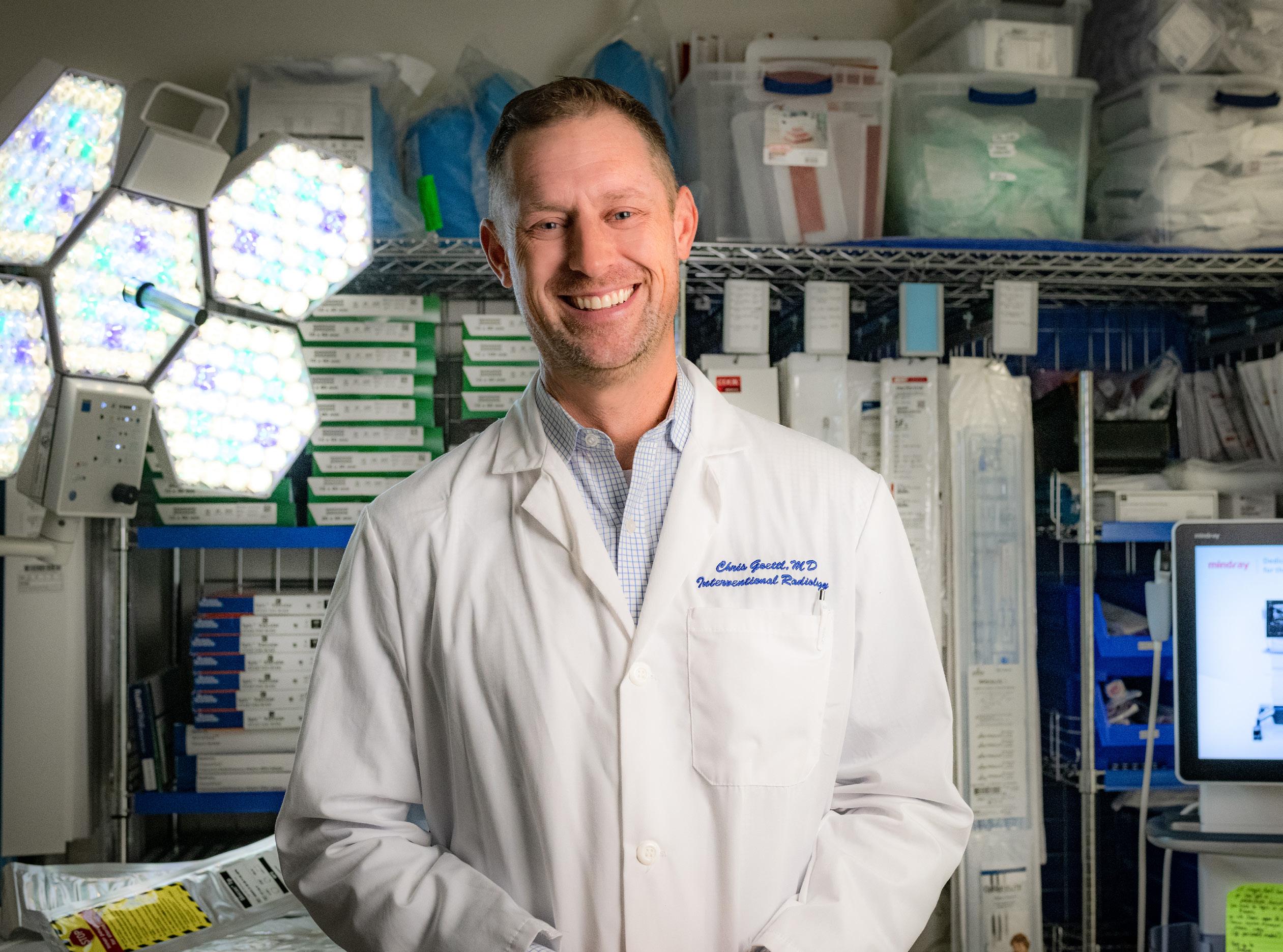
Chris Goettl, MD, MBA, of Vascular Interventional Partners shares how VIP operates and what its future holds.
more about MCMS member practices and how they help their patients.

Throughout a physician’s career we make connections at all stages of our medical journey. Some of a physician’s deepest connections start and get stronger throughout medical school, where the rigorous classroom learning and first experiences in clinical medicine leave students bonded closely to one another throughout those four years and beyond. Then the rigorous clinical training in residency also expands that bond. Yet, at times once we have our “real jobs,” we can become more separated and disconnected. This happens whether we are in small practices, or passing through the hallways of a hospital, signing out to the next shift worker, our connections just become more limited. Frustration with health care, busy family lives, and the never-ending requirements to continue to be a physician, can leave us feeling isolated.
My local medical society has been an important source of connection for me since I first began my medical career. Organizations such as the San Diego Medical Society where I started and The Maricopa County Medical Society where I currently lead a talented board of physician leaders, has help me build many types of connections. Connection to physicians of different specialties, connection to leaders in our community, connection to politicians who could help improve the laws that affect our profession, and connection so I can further my education.
At the Maricopa County Medical Society (MCMS) we are here to connect you with what you need to be the best physician you can be. As a publication of the medical society, Arizona Physician magazine connects you to other physicians making waves in healthcare and you can learn about some advances in medicine and technology that may help your practice or career.
Recently I was eating lunch at my hospital doctor’s lounge and was able to say hello to physician friends I met through MCMS, an adult internist and a palliative care physician, who in my pediatric office across the street, I would have never known otherwise. So, let MCMS and Arizona Physician keep you connected.
Jane Lyons, MD MCMS Board President

Dr. Jane Lyons is a Pediatrician, who provides care for patients in both the inpatient and outpatient setting. She works locally in Phoenix as well as providing rural locum hospital based care. Dr. Lyons completed her medical training in San Diego, CA, has two young children, and enjoys the outdoors, cooking, and spending time with family and friends.


CIVIC HEALTH CHECK-UP:
Voting is an important way to make your voice heard and influence government policies that impact your health.
As Maricopa County Medical Society (MCMS) commemorates 132 years, we reflect on a journey marked by innovation, dedication, and an unwavering commitment to the health and well-being of our physician community. This milestone is not just a celebration of longevity but a testament to the resilience and vision of the countless medical professionals who have contributed to our legacy.
Founded in 1892, our medical association was established at a time when the medical field was still in its infancy. The world of medicine has changed dramatically since then—from the advent of antibiotics and vaccines to the development of advanced surgical techniques and the emergence of digital health technologies. Through these changes, our association has been at the forefront, guiding the medical community through periods of discovery, challenge, transformation, and how information is delivered.
Our founders envisioned an organization that would not only advance the practice of medicine but also elevate the standards of care for all patients. Over the past 132 years, we have stayed true to this vision, championing medical education, advocating for patient and physician rights, and fostering a community of medical professionals committed to excellence.
CAN
In 1955, the Arizona Physician Magazine (formally known as Round-up) was born with the idea to inform and connect its membership base along with allied health professionals, health agency executives, public health officials, and hospital administrators. As we mark the 69th anniversary of our esteemed medical magazine, we take a moment to reflect on the journey that has brought us here—a journey defined by dedication to advancing medical knowledge, supporting healthcare professionals, and keeping readers at the forefront of medicine. For over half a century, our magazine has been a trusted
source of information, insight, and inspiration for the Arizona medical community.
When our magazine was first published 69 years ago, the landscape of medical journalism was vastly different. The world was on the cusp of major scientific breakthroughs, and the medical community needed a reliable source to disseminate new findings, discuss emerging trends, and provide a platform for professional dialogue. Our magazine was founded with a clear mission: to deliver accurate, timely, and relevant medical news and research to physicians across Arizona.
The past 69 years have seen incredible advancements in medicine, from the development of new vaccines and treatments to the rise of personalized medicine and digital health technologies. Through these changes, our magazine has remained adaptable, evolving to meet the needs of our readers in an everchanging world.
As digital media began to reshape the way information was consumed, we embraced these innovative technologies to expand our reach and impact. Our transition to digital formats allowed us to provide more interactive content, timely updates, and a more personalized reading experience. Whether through our website or social media channels, we have continued to innovate in how we deliver content, ensuring that our readers have access to the information they need, when they need it.
One of the most rewarding aspects of our 69-year history has been our role in spotlighting the incredible achievements of individual physicians in our medical community. We have had the privilege of featuring some of the most influential physicians in Arizona and important medical breakthroughs of the past half-century, from the first heart transplants to the sequencing of the human genome, and from the development of life-saving drugs to the rapid advancements in telemedicine.
Beyond reporting on medical news, our magazine has been a champion of education and medical professional development, along with our allied partners. We have published countless articles that delve into the complexities of medical practice, offering insights into new techniques, emerging specialties, legal health, and evolving standards of care. Our commitment to providing high-quality, evidence-based content has helped countless physician readers enhance their skills, knowledge, and network.
As we celebrate this 69-year milestone, we are also looking to the future with excitement and anticipation. The field of medicine continues to evolve at a rapid pace, and so does the role of Arizona Physician magazine. We are committed to staying at the forefront of this evolution, embracing modern technologies, and exploring innovative ways to deliver content that meets the needs of today’s medical professionals.
To our physician readers, we say thank you for allowing us to be a part of your professional journey. To our contributors—whether you are a writer, researcher, clinician, partner, or thought leader—thank you for sharing your expertise and insights with our audience.
Today Arizona Physician reaches over 14,000 physicians across Arizona.
With Gratitude,


Desire’e Hardge, MBA Arizona Physician Editor-in-Chief MCMS CEO & Executive Director

Transforming Arizona’s Healthcare Spaces with Cutting-Edge Design

In recognition of Hispanic Heritage month from September 15–October 15, we salute great physicians that have made great impact historically. Here are four Hispanic physicians you should know more about.

JOSE CELSO BARBOSA, MD (1857 – 1921) | Dr. Barbosa was a Puerto Rican physician born in 1857. Dr. Barbosa paved the way for many minorities to enter medicine during a time when it wasn’t allowed in many states. After much rejection, Dr. Barbosa became the first Puerto Rican to receive a medical degree in the United States from the University of Michigan in 1880. Interested in learning more about Dr. Barbosa, you can read The Quiet Rebels; Four Puerto Rican Leaders: Jose Celso Barbosa, Luiz Munoz Rivera, Jose De Diego, Luiz Munoz Marin.
NORA VOLKOW, MD (1956 – PRESENT) |
Dr. Volkow is currently the Director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health. She is one of the world’s leading psychiatrists born in Mexico and earning her medical degree from University of Mexico and completing her Residency at New York University. She has earned numerous awards and has published over a thousand peer-reviewed articles and written in over 113 books. Interested in learning more about Dr. Volkow’s work, you can read Neuroscience in the 21st Century, From Basic to Clinical, Third Edition.

SERENA MARIA AUNON-CHANCELLOR, MD (1976 – PRESENT) | Dr. Aunon-Chancellor is both a physician, engineer, and NASA astronaut. Dr. Aunon Chancellor earned her medical degree from University of Texas Health Science Center at Houston and completed her Residency at University of Texas Medical Branch (UTMB). Dr. Aunon-Chancellor, who is Cuban American, has spent close to 197 days in space as part of the ISS mission in 2018. Learn more about Dr. Aunon-Chancellor, read Serena Aunon-Chancellor by Annette M. Clayton.
BARUJ BENACERRAF, MD (1920 – 2011) |
Dr. Benacerraf was a Venezuelan American Immunologist who won the 1980 Nobel Prize in Physiology or Medicine for his discovery of major histocompatibility complex genes. Dr. Benacerraf earned his medical degree from the Medical College of Virginia and would go on to earn numerous awards, honorary degrees, and other accolades for his work and discovery. To learn more about Dr. Benacerraf, you can read From Caracas to Stockholm, A Life in Medical Science



Election day is right around the corner. Yet so is 2025. As we move into 2025 the Maricopa County Medical Society (MCMS) encourages you to have your voice heard at the state legislature, where policies are decided upon your behalf, the physician community, the patients you care for, and the overall healthcare landscape. From House Bills (HB) like HB2093 (health professionals; title use; prohibitions) that closes an insurance medical loophole of emergency services that was signed and
passed into law to HB2513 and Senate Bill (SB) SB1037 (AHCCS; preventative dental care) that is still ongoing, and all bills in between MCMS stands unified as a collective strong voice among its members, healthcare community, and allied medical associations.
These significant decisions and policies made by elected officials are often done without the much-needed voice of a physician. These laws once enacted can have a profound impact on the public and medical
professional community. Your voice as a physician can carry more weight due to your education, training, knowledge, and experience. Your voice can have a positive effect on legislative bills passed or opposed in committees or vetoed by the governor.
The Maricopa County Medical Society (MCMS) encourages you, all physicians across Arizona, to sign up for Request to Speak (RTS). This simple and easy platform allows you, as a constituent and medical professional, to have your voice heard on legislation that is being considered. RTS is a straightforward way to register your opinion and leave comments for committee members.
To register or for more information on RTS please visit, www.azleg.gov.









Hospice of the Valley is Arizona’s largest hospice & palliative care provider. They provide many programs and services across Arizona. We sat down with three of their leaders, CEO, Debbie Shumway, Executive Medical Director, Ned Stolzberg, MD, and Dementia Care Medical Director, Gillian Hamilton, MD, PhD, to discuss their career paths, their work at HOV, and how they help move forward HOV’s mission in the future.
We began our conversation with Debbie Shumway, CEO, who has now been at HOV for over 30 years. We discuss the programs/ services HOV provides, plus her incredible leadership at the helm of one of Arizona’s renowned non-profit organizations.
ARIZONA PHYSICIAN: Deb, please share with us your history at Hospice of the Valley? DEBBIE SHUMWAY: I am so honored to have just celebrated my 30th anniversary at Hospice of the Valley! I joined the agency as finance director in 1994. But my

appreciation for this wonderful organization began in the early ’80s, when I had the opportunity as a teenager to visit patients with my mother, who was a Hospice of the Valley volunteer. Over the years, I had the opportunity to work closely with our field staff and better understand the operations of HOV, and in 2016, I assumed the Executive Director role. There have been many changes over the last 30 years, but the dedication and commitment of our care teams to provide beautiful care has never wavered. We continue to create programs to meet the changing needs of our community while staying focused on our mission: Bringing comfort, dignity and compassionate care to our community.
AZP: Deb, there are many hospices in our community, but Hospice of the Valley is unique because it is a nonprofit. Tell us more about that.
DEBBIE SHUMWAY: Hospice of the Valley was the first hospice in Arizona, founded by a small group of volunteers 47 years ago—our visionary founders. Today, we are the only nonprofit hospice in Maricopa County—a responsibility we take seriously As a nonprofit, we provide care for all in need, regardless of someone’s financial resources. We can do this thanks to the support of our generous community. This last year, we provided more than $14 million in charity care and community services.
AZP: Hospice of the Valley also offers many other services and programs in addition to hospice care. Can you share a few that patients use most?
DEBBIE SHUMWAY: Many families come to us for compassionate Hospice Care. Our skilled interdisciplinary teams of physicians, nurse practitioners, nurses, social workers, nursing aides and chaplains are focused on personalizing care for each individual while supporting their family members. We can provide this important care through strong collaboration with community physicians and other healthcare partners.
All our programs are supported by a skilled after-hour clinical team that supports patients and provides in-home clinical visits 24 hours a day. The goal of each of our programs is to improve our patients’ quality of life, help them live safely at home and avoid unnecessary hospitalizations.
We have several programs tailored to individuals dealing with advanced illnesses. Some of them include:
Supportive Care for Dementia, a unique program where dementia educators visit caregivers in the home to provide resources, clinical and emotional support, and help navigate the challenges of caregiving.
Arizona Supportive Care is our program to manage the symptoms of chronic illnesses like heart and lung disease, along with cancer and other health challenges. We provide education, community resources, care coordination and after-hour support 24/7. Our experienced clinicians serve patients where they live, just as our hospice and dementia care programs do.
Serving home-limited patients who are not able to get to their primary care provider, our Geriatric Solutions program provides in-home primary care services. Our physicians and nurse practitioners make home visits providing primary care services like wellness exams, symptom management and care coordination with specialists.
AZP: How did HOV become the hospice provider for Banner Health? Share what that means for patients and families.
DEBBIE SHUMWAY: We were pleased to work with leaders at Banner Health as they transitioned their hospice operations in Phoenix and Tucson to Hospice of the Valley. This helped us expand our care for more families and strengthen nonprofit hospice care in Arizona. The transition was seamless for patients, thanks to a dedicated team of experienced hospice care professionals. Banner hospice employees joined Hospice of the Valley, providing patients

with continuity of care with their clinical teams. It has been our hope to expand services to Tucson and this integration allowed that to happen smoothly.
Over our 47 years, we have been fortunate to collaborate closely with all the regional hospital systems. Our admission nurses work seamlessly with hospital case managers to ensure a smooth transition from the hospital to the patient’s home, wherever that may be.
AZP: Where do you see Hospice of the Valley in 10 years?
DEBBIE SHUMWAY: Over the next 10 years, Hospice of the Valley will continue to expand programs and create new care models to support those dealing with advanced illnesses. Our ongoing focus will be to partner with community physicians and other health providers to provide excellent care and education, improve quality of life for those dealing with significant health challenges, and reduce unnecessary healthcare expenses. We are committed to growing a workforce that is dedicated and passionate about caring for our community and serving all in need. As we all age, we anticipate that care needs will continue to grow, and we are honored to help ensure that all of us have access to this critical care.
Ned Stolzberg, MD, serves as Executive Medical Director for Hospice of the Valley. We asked a few questions on why physicians come to work at HOV and what it takes as a physician to be successful working at hospice & palliative care organization.
AZP: Dr. Stolzberg, please share with us your history at Hospice of the Valley.
NED STOLZBERG: My interest in hospice began during my Family Medicine residency. Subsequently, both of my parents needed hospice, and I was able to experience the care Hospice of the Valley provides from the perspective of a family member. As a result, in 2007 I joined the agency part time as a team physician. I gradually transitioned away from private practice to work in hospice care full time, and along the way became board-certified in Palliative Medicine. I held multiple clinical positions with HOV prior to assuming my current role in 2015.
AZP: You oversee all physicians and nurse practitioners at HOV, what makes a physician a good fit at HOV? What are qualities you look for in a physician looking to work in non-profit and hospice & palliative care?
NED STOLZBERG: We look for physicians who are compassionate, good communicators and skilled at working in a team environment. They also must be comfortable working in gray areas. End-of-life care often defies what might be found in a textbook and hospice physicians need to be able to treat the patient and not the disease.
AZP: There are 45 physicians at HOV, are they all full time or part time?
NED STOLZBERG: Our physician team is a blend of doctors who have had formal training in Hospice and Palliative Medicine and those who have had experience in other fields (Internal Medicine, ER, anesthesia, etc) and were new to hospice when they started with us. There is a learning curve to hospice medicine, but the person is more important than their background. We also have a mix of people who work full-time and those that are part-time and still work in another area of medicine.
AZP: What can physicians expect working for a hospice & palliative care organization like yours instead of, say, working with geriatric patients in a hospital?
NED STOLZBERG: The bulk of hospice care is delivered in a patient’s home. You can get a much deeper understanding of what might work best for a patient in this environment. The care is also delivered by an interdisciplinary team (nurse, certified nursing assistant, social worker, chaplain, volunteer, etc.). This allows for very personalized care plans with the patient as the focus, not the disease. Sometimes my input is the key to achieving the patient’s goals, sometimes it’s another team member’s. It’s a great model of practice.
AZP: What’s your pitch to young or seasoned physicians interested or considering hospice & palliative care?
NED STOLZBERG: Most of our physicians “self-select.” That being said, hospice offers an opportunity to practice medicine in a manner free of many of the constraints and frustrations common in our medical system. You can use your skills to solve unique challenges creatively and make significant impacts every day for your patients and their families. I’ve not worked with a better group of colleagues or in a better culture. Hands down this has been the most fulfilling job I’ve had in medicine.

Being board certified in both internal medicine and geriatrics & palliative medicine, makes Gillian Hamilton, MD, PhD, a natural fit as leader of HOV’s Supportive Care for Dementia program. We discussed HOV’s new Dementia campus and how physicians can feel comfortable referring their patients to hospice & palliative care providers like HOV.
AZP: Dr. Hamilton please share with us your history at Hospice of the Valley
GILLIAN HAMILTON: When I was teaching Geriatrics at Good Samaritan Hospital (now Banner U.) 28 years ago, I attended an open house at Hospice of the Valley and the executive director at that time, Susan Goldwater (now Levine) admired a photo of my daughter just adopted from Peru. We had an immediate connection, and I started working at HOV a few hours a week—gradually increasing as more needs appeared. HOV is incredibly innovative and provided the opportunity for me to develop many new programs, including volunteer programs for teens and pet therapy teams, a pulmonary program, a dementia program (including an inpatient unit just for dementia), and then a program to support people living with early or mid-stage dementia called Supportive Care for Dementia. The most recent innovations have been a Dementia Care Fellowship (for all professions, including architects, hospital systems, improvisation actors, educators in under-served communities, etc.) and finally, our wonderful Dementia Care and Education Campus– a comprehensive resource for our whole community.
AZP: Tell us more about your dementia care campus and the services it provides for patients.
GILLIAN HAMILTON: The campus is an incredible gift to our community provided by our Board. It includes an Education Center providing many services at no charge, including events, support groups and educational programs on campus and virtually. Supportive Care for Dementia (SCD) also operates from the campus to support people with dementia living in their homes alone or with caregivers. That program has grown to a current census of over 750 and will expand further in July

because we have just been awarded a new 8-year CMS demonstration program, Guiding an Improved Dementia Experience Model (GUIDE), to improve care of persons with dementia and their families. In addition to the free programs, the campus includes an assisted living facility, an Adult Day Club with adjoining childcare and daily interaction, and a hospice inpatient unit. The Campus is a place to model superb dementia care for mild, moderate and advanced dementia for all learners: medical students and residents; students in nursing, social work, occupational and physical therapy; certified nursing assistants and home health aides; college undergraduates; as well as family caregivers. A full-time music therapist and occupational therapist serve the campus and our patients at home.
AZP: Do you feel there is any disconnect between primary care physicians and organizations such as yours when it comes to referring patients? If so, how do we change that?
GILLIAN HAMILTON: When primary care physicians and neurologists learn about our Supportive Care for Dementia program for those with mild cognitive impairment or any level of dementia, they are eager to refer. We can partner with home visits to find ways to provide support for patients and family

and coordinate with their providers. Our census has grown very rapidly as physicians learn about the program, and we are thrilled to help families, who often come to us with very little knowledge about dementia and how to help those they care for.
AZP: Your Dementia Care and Education Campus recently received a grant from MCPHD to educate PCPs and other primary care medical providers about dementia diagnosis and management. How did that go? Beyond the grant, how do you educate primary care physicians on dementia care for their patients?
GILLIAN HAMILTON: The grant-funded education we provided was extremely successful and showed the demand for dementia education in our community. During the 15 months of the grant, we educated over 6,000 professionals, focusing on medical students and physicians/NPs/PAs, but also many students in other health professions, from high school students getting nursing assistant certification to first responders across Maricopa and Pinal counties. We continue to provide education to healthcare professionals and caregivers in many venues throughout the Valley. We also look forward to serving primary care providers and specialists caring for people living with dementia in our new federal GUIDE program, which will provide free respite for caregivers, when eligible. ■

46 Physicians
18 Nurse Practitioners
Over 1,500 Total Employees
Other staff include:
Nurses, certified nursing assistants, social workers, chaplains, educators, and administrative.
Hospice care, palliative care, MediCaring, pulmonary care, grief support, family caregiver support, pediatric services, mindfulness, music therapy, and dementia care.
Connect with Hospice of the Valley (HOV) hov.org | 602-530-6900
Mental health is an integral aspect of a person’s health. For years either through stigma, lack of access, or even a focus on physical health has made mental health well-being overlooked. Today, mental health has become one of the top health concerns globally.
Mental health professionals like psychologists, counselors, social workers, and therapists form a cooperative community alongside physicians like psychiatrists in helping patients with their mental health. Yet, due to their education, training in therapy, medical interventions, and ability to prescribe medications, psychiatrists like Dr. Mona Amini are leading the way in helping patients achieve mental health and well-being.


Mona Amini, MD, MBA, is a board-certified psychiatrist who owns and operates her own practice in northern Scottsdale. Dr. Amini began her medical journey at St Matthew’s University in the British West Indies while also earning an MBA from Davenport University. Upon graduation, she completed her Residency at Banner Good Samaritan Medical Center in Phoenix (now Banner University Medical Center – Phoenix) in 2013. She has completed over a decade in clinical and administrative medicine with numerous executive and administrative roles.
Dr. Amini has always been future focused and goal oriented. She shares that very early in her career she grew a passion for brain health as one of several components in psychiatry. Psychotherapy, psychotherapeutic models, and psychoanalysis were enticing to her as she completed medical school. Yet, it was the idea that as a psychiatrist, she states, “you have the capability to help somebody change their mindset, which can then have a powerful effect on their physical health.” During residency she would spend a bit more time with psychiatric patients to learn more about them and their stories.
Dr. Amini has experienced her fair share of adversity while starting her medical career. She and her husband married young and while deciding on their respective futures in medicine they decided to attend the same medical school. To do that they decided to attend St. Matthew’s in the British West Indies. Yet, a category 5 hurricane in Grand Cayman forced a semi-permanent relocation to Maine for most of the remainder of basic sciences. During their clinical rotations, her focus on psychiatry led them to spend time in different states for a while. It wasn’t until residency that they felt ready to start a family and move forward with their careers and she is truly grateful for that opportunity.
Why has there been such a stigma about mental health? From media portrayals, stereotypes, personal beliefs, to self-stigma, psychiatry professionals like Dr. Amini work tirelessly to eliminate those barriers. She does so by forging genuine and deep-rooted personal connection with each one of her patients. She states, “When
“You have the capacity to help someone change their mindset, which can then have a powerful effect on their physical health.”
—Mona Amini, MD
you are somebody that can sit in front of a patient and show empathy and authenticity,” that forges better patient communication, care, and ultimately better outcomes.
How does a psychiatrist that is just beginning to learn more about their patients get them to a place where they can open up and discuss the issues that are affecting them? Dr. Amini shares that you can’t be fake, a good psychiatrist must build beyond the transactional relationship in which a patient may initially see when they come in.
Breaking away from traditional psychiatry norms is helping to break down psychiatry barriers. By moving away from typical psychiatric medical management through 10 to 15-minute visits, Dr. Amini is helping to redefine psychiatry. She hears from her patients how in many instances in their past, those types of psychiatry services have gotten them nowhere and they don’t feel better. So, she adds a more whole-person approach in which she really delves into what her patient’s day-today looks like, their hygiene, their sleep, relationships, and even goes back to ask about their childhood, adolescence, and adulthood. She’s never afraid of asking tough questions about their personal lives to better understand her patients and ensure she’s getting the right details to better help her patients reach their mental wellness when they see her.

After years of working at other companies and consulting, Dr. Amini decided to open her own practice in October of 2023. In earning her MBA, she could put to practice some of the business skills she had learned along the way. She also decided to be a sole practitioner and specifically, to be a concierge medical practitioner.
Concierge psychiatry differs from typical psychiatry in that patients do pay out-of-pocket, yet have more flexible access to their psychiatrist, spend more time with their psychiatrist during each visit, and there is a focus on personalized care for each patient. For psychiatrists like Dr. Amini it helps remove the burden of being told how many patients to see and eliminates the burdensome filing of insurance claims.
Dr. Amini has learned to thrive in this concierge environment. She makes her patients feel safe, is discrete, and has a confidential setting in which they only engage with her. High-end clients appreciate the departure from the typical psychiatrist’s office, instead being welcomed into a professional yet intimate setting where they feel comfortable sharing what’s on their mind. Her approach incorporates psychotherapy, guiding patients toward a deeper understanding of self-care, encouraging thought-provoking questions, and helping them explore new perspectives on important issues. Her patients get to see and feel an aesthetic and attention to detail, which speaks to her thought-provoking nature. She also is her practice’s best marketer, as she knows how to be its best spokesperson by speaking directly to her entire community.
Beyond her practice, Dr. Amini stays active as the Medical Director of other psychiatric practices, an advisor to companies, and a speaker, leading wellness seminars for physicians and medical professionals. Amid her busy schedule, she always prioritizes carving out high-quality time to spend with her husband and family.
Dr. Amini tells us, “The future of psychiatry has more digital health with a lot of innovation.” She sees a huge outpouring of venture capital
Concierge psychiatry differs from typical psychiatry in that patients do pay outof-pocket, yet have more flexible access to their psychiatrist, spend more time with their psychiatrist during each visit, and there is a focus on personalized care for each patient.
funding for mental health as an extension of COVID19 pandemic era investment into the industry. From neurofeedback headbands that help with sleep, devices patients will utilize at home in conjunction with their mental health professional, to even more sophisticated and advanced applications that make telehealth and virtual health models more and more common and useful to both patient and physician.
The future in psychiatry will involve a lot of screening as there’s going to be a lot more objective data and evidence to help back some of rationales for types of treatments. She also believes that there will be a lot more funding going towards psychedelics based on seeing how they have helped different populations when it comes to post-traumatic stress disorder (PTSD), depression, and anxiety.
Finally, Dr. Amini shares her excitement when it comes to the next generation of physicians turning to psychiatry because it is becoming ultra-competitive in residency matching, meaning those coming into the

profession are bright, looking to make change happen, leading psychiatry into a very different trajectory. This approach may lead many to offer concierge-level services, helping to prevent early burnout, allowing them to avoid a strict patient quota, and, most importantly giving them the time to sit down with their patients, truly get to know them, and provide more personalized care for better outcomes. ■

By Edward Araujo Managing Editor Arizona Physician earaujo@mcmsonline.com
Visit Mon'Vie Mind Wellness at monviemindwellness.com
Vascular & Interventional Partners is one of Phoenix’s most respected interventional radiology practices. They perform a variety of minimally invasive procedures for their patients.
Arizona Physician recently sat down with Chris Goettl, MD, MBA, to discuss interventional radiology, VIP, and what the future holds for his practice.
ARIZONA PHYSICIAN: Dr. Goettl, what is your history with Vascular & Interventional Partners (VIP).
DR. GOETTL: I have worked with this same group since graduating my fellowship in 2018. I am one of the five founding physicians when VIP transitioned on to private practice in 2022.
AZP: Dr. Goettl, most physicians that earn an MBA do so after they have established themselves as physicians. What led you to become a physician after obtaining your MBA?
DR. GOETTL: Starting in high school, I was fortunate to have a clear picture in my mind of how I wanted my career to look. My goal was to become an interventional radiologist, and to help run the business side of a group practice in addition to working as a physician. This led me to pursue a premed degree as an undergraduate and then complete an MBA. I then worked as a management consultant for 2 years before medical school and residency training. But my long-term goal was always to become an interventional radiologist.

AZP: Dr. Goettl, you are an interventional radiologist. Tell us more about this specialty and what makes it different from a typical radiologist.
DR. GOETTL: IR is a unique field and has transitioned from being a sub-specialty of Diagnostic Radiology to its own distinct primary specialty in medicine. In our practice we are full-time IR physicians, meaning we do not practice any traditional diagnostic radiology (although we are constantly reviewing images as part of our procedural care). Our day is more like surgical practice than diagnostic radiology, split between patient consultations and performing image-guided procedures.
“At VIP, we are wholly physician owned, without any large health system or private equity ownership. This allows us to focus on patients more than profit.”
AZP: You serve as both CEO and practicing physician within the group. Share with physicians how you can be successful in both of those vital positions.
DR. GOETTL: Balancing administrative and patient care duties can be challenging. The key for me to be successful is our outstanding IR partners and colleagues. We work as a team and everyone contributes unique strengths to the practice, which has allowed us to be collectively successful. We also have excellent techs, nurses, and administrative staff that allow us to provide the best care possible to our patients.
AZP: Can you share with us a brief history of Vascular and Interventional Partners (VIP).
DR. GOETTL: The VIP group was formed out of a group of hospital-employed IR physicians, with each of us practicing full-time IR or Neuro-IR. Our focus was not diagnostic radiology or combined IR/DR practice. We were initially 100% hospital-based, but we felt that we needed a highly clinical and accessible outpatient office to provide our patients with the best care. We opened our first procedural office in Scottsdale in 2022 and are now expanding to new hospitals and outpatient sites of service.

AZP: What services do you provide for patients? Which are the most popular?
DR. GOETTL: We provide the full spectrum of IR and Neuro-IR care in our practice. In the hospital, we treat high-complexity and high-acuity patients with procedures like stroke thrombectomy, trauma embolization, TIPS placement, and cerebral aneurysm coiling. In the outpatient setting, we perform elective procedures including chest port placement, uterine artery embolization, liver and kidney tumor ablation, or prostate artery embolization (PAE). PAE is becoming very popular in men seeking a less invasive way of treating their BPH.

AZP: What makes VIP stand out from its competitors in Arizona?
DR. GOETTL: Our group practices 100% IR, rather than the more traditional combined IR/DR private practice models. This allows us to focus entirely on procedural and consultative care, rather than spending a part of our day interpreting images. In addition, we are wholly physician owned, without any large health system or private equity ownership. This allows us to focus on patients more than profits, and to refer to whichever provider we think is best for the patient regardless of where they work.
AZP: Share with us what has changed in radiology / interventional radiology in the last 10 years.
DR. GOETTL: As I mentioned before, IR has emerged as its own primary medical specialty over the last several decades. Our field has shifted away from training “technicians” (taking a written order from another physician and performing requested procedure) toward training well-rounded “clinicians” (who perform clinical evaluation and management of patients before, during, and after an IR procedure). At the same time, we have witnessed exciting progress in the various procedural devices and imaging equipment that we use every day. This ongoing innovation allows us to help more patients in a minimally invasive way.

“I believe our future at VIP is very bright. We have developed a professionally rewarding IR group model that provides excellent patient care and appears to be economically sustainable.”
AZP: Are there new trends in radiology or new technology that VIP is taking advantage of to better help patients while also helping its bottom line?
DR. GOETTL: Yes. We are constantly looking at new and improved imaging equipment (ultrasound machines, angiography systems) which was previously only available in a large hospital department but is now commonly accessible to a physician’s office on your neighborhood corner. In addition, we are looking closely at new devices and products used in vascular procedures, including radiopharmaceuticals and liquid embolics that can be used for complex vascular cases.
AZP: Dr. Goettl, we see that VIP has six physicians, three nurse practitioners, and three physician assistants. How does that provider mix help your practice?
DR. GOETTL: Our nurse practitioners and PAs are a hugely important part of our practice. They help perform some of our most common procedures, provide high-level pre-procedure evaluation, and help us ensure great clinical follow up. Our physicians and APPs are constantly working together to make sure we provide the best procedural services and clinical support possible.
AZP: Do you see any opportunities that will allow your practice to get bigger?
DR. GOETTL: Definitely. We are seeing a surge in demand for quality IR medical services, not only in Maricopa County but across the country. Whether it is a large hospital, or a small independent physician practice, physicians and administrators genuinely appreciate the diverse value that we bring to patients. We believe in growing our model and thus expanding access to care for more patients across the southwest.
AZP: What do you see are the largest obstacles in running a group practice today?
DR. GOETTL: Obstructive behavior by private insurance companies is one of the largest challenges facing group practices today. We need significant policy reform to help change the way that insurance entities operate and impact healthcare. Second, ongoing cuts to CMS physician payments are not sustainable. We cannot continue to pay physicians less for the same work in an environment of cost inflation if we want to preserve quality outcomes and access to care.
AZP: Dr. Goettl, what does the future hold for VIP?
DR. GOETTL: I believe our future at VIP is very bright. We have developed a professionally rewarding IR group model that provides excellent patient care and appears to be economically sustainable. Increasingly young IR physicians are expressing interest in this model and reaching out to join the practice, so we feel that our best days are ahead of us. ■

Vascular & Interventional Radiology Procedures
Oncology, venous disease, neurovascular, men’s health, women’s health, spine, kidney disease & dialysis access, GI interventions, arterial disease, and joint pain
Conditions Treated
Compression fractures, portal hypertension, enlarged prostate (BPH), osteoarthritis, hemorrhoids, liver cancer, May-Thurner Syndrome, Spine Health & Pain Relief 2
and Phoenix

The heat doesn’t just burn; it sears, it oppresses. For those without shelter, it’s more than just uncomfortable— it’s deadly. Last summer’s brutal temperatures claimed 645 lives in Maricopa County alone, forcing us to confront a harsh reality: traditional healthcare methods were failing the most vulnerable among us. So, Circle the City did what we do best—we adapted, we innovated, and we took action. The solution came from the streets.
This summer, one of our street medicine teams broke new ground, becoming the first in Arizona to administer IV hydration directly on the streets. It was a simple concept with a radical impact: meet people where they are, before they end up in crisis. Dehydration and heat-related illnesses can escalate with terrifying speed, especially for those already struggling with chronic conditions. We couldn’t wait for them to come to us; we had to bring the care to them right then, right there.
And it worked. By stabilizing patients on the spot, we didn’t just treat symptoms—we prevented crises, avoided costly emergency room visits, and, most importantly, saved lives. This wasn’t just a win for our patients but for the entire healthcare system in Phoenix. With emergency departments already stretched thin, every crisis averted meant that critical resources could be preserved for those who needed them most.

the people it serves.
But this story is bigger than IV hydration. It’s about a team that refuses to let people fall through the cracks. Every day, our street medicine teams are out there, navigating the scorching heat, providing comprehensive care that addresses the full spectrum of health challenges—from managing chronic diseases to offering mental health support. This isn’t just about keeping people out of the hospital but giving them a fighting chance at health, stability, and dignity.
Our work hasn’t gone unnoticed. Media outlets from around the world have highlighted Circle the City’s efforts, with The New York Times describing us as “the most sophisticated model in healthcare for those facing homelessness.” It’s validation that what we’re doing matters, that it’s making a real difference, and that it’s setting a new standard for what’s possible in healthcare.
Looking ahead, we’re not content to rest on our laurels. The success of our IV
For the healthcare professionals in our community, this is more than just an update— it’s a call to action. There’s an opportunity here to partner with a team that’s not just easing the burden on emergency services but redefining what it means to provide care to those who need it most. We’re not just stopping symptoms in their tracks; we’re rewriting the script of how healthcare is delivered in our city.
As this relentless summer continues, Circle the City will be out there, pushing boundaries, breaking barriers, and finding new ways to serve. This isn’t just about surviving the heat—it’s about thriving despite it. And together, we can ensure that our community’s most vulnerable members aren’t just another statistic, but a testament to what can be achieved when healthcare is driven by compassion, innovation, and an unshakeable commitment to those we serve. ■

By William Ellert, MD Chief Medical Officer Circle the City wellert@circlethecity.org

In today’s rapidly evolving healthcare environment, connecting with patients is crucial, and digital marketing offers a powerful way to enhance that connection. From increasing patient engagement to improving retention, these five digital marketing techniques can help physicians meet and exceed their patient’s expectations.
Patients today expect a personalized experience similar to what they encounter in other areas of their lives, like retail and entertainment. Personalized digital marketing creates a stronger emotional connection with patients. To do this, you can leverage email newsletters, social media content, and patient portals to provide relevant, targeted information based on patient demographics, medical conditions, or treatment preferences.
For example, sending tailored reminders for annual checkups or screenings can keep your patients engaged.
Additionally, sharing content on chronic disease management, preventive care, or post-treatment tips based on individual profiles demonstrates a level of care and attention that strengthens the doctorpatient relationship.
Patients often turn to search engines to find healthcare providers, so having a robust online presence is essential. Search Engine Optimization (SEO) helps your practice appear at the top of search engine results when patients seek the services you provide. By optimizing your website with relevant keywords, location-based search terms, and high-quality expert content, you make it easier for potential patients to find you. For instance, if you’re a cardiologist in Phoenix, focusing on SEO strategies such as using keywords like “cardiologist in Phoenix” or “heart specialist near Phoenix” will improve visibility and attract patients.
Social media platforms like Facebook, Instagram, LinkedIn, and even TikTok offer you a unique opportunity to build a community of patients and establish yourself as a thought leader in the space. Through regular posts about health tips, patient testimonials, or behind-the-scenes videos of the practice, you can humanize your practice and foster trust with current and potential patients.
Beyond sharing content, actively engaging with patients by responding to comments, messages, and reviews creates a two-way conversation. This interaction can build a sense of community and reinforce patient loyalty. Social media also provides a platform to share updates, promote services, or inform patients of office hours and new treatments.
Word-of-mouth has long been a significant driver for patients choosing healthcare providers, but in the digital age, this has shifted online. Patients now rely heavily on online reviews to make informed decisions about their healthcare. And there are so many platforms to manage this, it can often seem overwhelming. You must prioritize managing your online reputation by encouraging satisfied patients to leave positive reviews on platforms like Google, Healthgrades, or Zocdoc. You can’t manage all the platforms, so determine the ones driving the most traffic, and prioritize those first so it has the most positive impact on your practice.
However, reviews aren’t only about promotion and can offer valuable feedback. Addressing positive and negative reviews with professionalism and care shows a commitment to patient satisfaction and continuous improvement. Managing online reviews can establish trust and credibility.
Video content is a powerful way to engage and educate patients. Whether it’s a quick message about seasonal healthcare tips, or an explanation of a complex procedure, video can add a personal touch to your patient interactions. YouTube, Facebook, TikTok, and Instagram are popular platforms for healthcare professionals to share video content. Videos that provide helpful, easy-to-understand medical insights can boost your patient engagement and position your practice as an authority. Video marketing also helps clarify common questions and alleviate patient concerns, leading to more informed, confident patients who feel more connected to you and your practice.
As healthcare becomes more digitized, it’s crucial for physicians to adapt to these changes to meet patient expectations and build lasting relationships. By leveraging digital marketing strategies, physicians can create a patient-centered experience that drives growth and improves patient outcomes and satisfaction.
Whether promoting convenient services or engaging patients through personalized communication and videos, digital marketing offers physicians the tools to stay competitive and relevant in a fast-changing healthcare landscape. The key is to remain adaptable and patient-focused to foster deeper connections with the patients who continue to trust you with their health. ■

By Elyse Flynn Meyer Owner & Founder Prism Global Marketing Solutions Elyse.meyer@prismglobalmarketing.com
In addition to protecting their personal assets, medical practice owners and leaders must also act proactively to protect their businesses from a wide variety of predictable risks.
GET AN INSURANCE CHECK UP
Liability insurance is a system not just a single policy and works best when implemented in layers that are designed to address specific threats. Please think beyond your medical malpractice policy and the general business liability insurance that covers non-medical liabilities on your property (like a slip and fall) both of which should be at seven figure limits.
All polices and carriers are not the same, so be an informed buyer when it comes to this vital first line of defense that can either save or cost you millions. I advise my clients to work with an independent, multi-line commercial insurance broker that has access to the entire market, not just one company, and the experience to guide you on both proper coverage limits and the differences between policies.
This is a list of the most basic commercial insurance coverage every medical practice should consider. It is by no means a complete list, nor can it address your specific facts. As with any legal topic addressed in this format, get personalized, professional help.
EPLI (Employment Practices Liability Insurance) for employment law issues.
Data Brach and Cyber Liability Insurance to cover HIPAA/ data breaches, ransom ware attacks, internet defamation claims etc.
Workers Comp to cover workplace injuries.
High limits of General Liability insurance.
RAC Audit Insurance to cover payer audits.
Director’s and Officer’s (D&O) Insurance to cover your business liability as a practice owner, executive or manager.
Disability Overhead Insurance to keep the lights on if you are sick or injured and can’t bill for services.
Key Person Disability Insurance in case a key member of your practice can’t perform their vital tasks.
Active Shooter Insurance to protect your staff, patients and practice from the growing threat of violence in healthcare settings.
Business Insurance to cover issues like fraud, theft, business interruption and other operational risks.
In 2022, the largest Arizona civil lawsuit verdict of the year (over $22 Million) involved four physicians, but it wasn’t a malpractice claim, it was an internal business dispute between partners.
Medical practices run into trouble and conflict when key business legal documents are missing or outdated. A missing or defective document often means the courts will decide how a conflict should be resolved, rather than the actual intent and agreement of the parties.
Here is a partial list the basic documents I routinely see cause a panic in crisis:
Corporate formation documents for your practice including corporate recording documents, operating agreements and buy-sell agreements.
Employment agreements, contracts and employment policy manuals.
Tax Records
Insurance Policies
Contracts with vendors and other third parties
Leases (real estate and equipment)
Employment law risks are serious and predictable exposures for medical practices. Physicians statistically face two malpractice claims during their career, but the average American business owner is five times more likely to face an employment lawsuit than any other reason. The average sexual harassment lawsuit, as one example, produces a verdict of over $500K and can easily cost six figures to litigate. Here is a three-step approach that I have seen produce great results.
First, leadership and a culture of respect and legal and ethical compliance. This means accountability and strictly enforced standards that correct or remove those that fail to meet your standards. This includes front office and admin staff, medical professionals and providers and partners in your practice who jeopardize your business when they do not comply with your policies and current standards and sensitivities.
Second, be insured with Workers Comp coverage and Employment Practices Liability Insurance (EPLI) that can cover both the costs of defense and potentially even judgment itself.
Third, have a professionally drafted, state specific employment manual that both outlines your workplace polices and standards and which provides employees a meaningful and specific way to report and addres any issues or conflicts before they become lawsuits. ■

By Ike Devji, JD Founder and Managing Attorney Arizona Wealth Law/Pro Asset Protection
ike@azwealthlaw.com
Adnan Saithna, MD, discusses his career in orthopedic surgery and what continues to motivate him as a physician.
Q: Share with Arizona Physician why you decided on orthopedic surgery as your specialty?
A: I was inspired to become an orthopedic surgeon by a fantastic mentor. While I was in medical school (Birmingham, UK), Professor Rob Grimer (an internationally recognized orthopedic oncologist) supervised one of my first ever clinical research studies. We conducted an international study that compared the outcomes of treatment of bone tumors in patients in Italy and the UK. We showed that patients in the UK had worse survivorship and that this was likely due to differences in chemotherapy protocols used between the two countries. Our work was the impetus for subsequent research that led to major changes in the chemotherapy protocols used in the UK, and likely significantly improved life expectancy and survivorship of patients.
I was so inspired that my work could save lives and impact patients and their families (and not just patients whose care I was directly involved with, but also those I would never meet) in such a profound way that I have been committed to clinical research ever since. Although I am no longer involved in managing patients with bone tumors, I remain very involved in clinical research in orthopedic sports medicine and my work has won several major awards and influenced global practice patterns.
I will always be grateful to Professor Grimer because without his mentorship I would never have been inspired to become an orthopedic surgeon, or undertake clinical research, and certainly not at a globally impactful level.
Q: What type of procedures do you perform? Which procedure is performed most on your patients and why?
A: I specialize in minimally invasive and arthroscopic knee and shoulder surgery.
The most common knee surgery I perform is ACL reconstruction (where a graft is used to reconstruct a torn anterior cruciate ligament). Injuries to the ACL are amongst the most common sports injuries and

approximately 300,000 ACL reconstructions are performed in the United States annually. However, one of the risks of surgery is failure of the graft (when the graft tears again). Although overall failure rates are low, certain groups are at high risk. One of the highest risk groups is the young female soccer athlete, with failure rates of up to 20-30% being frequently reported.
Much of my clinical research has been focused on reducing the risk of ACL graft failure. In 2017, I (along with my colleagues in the SANTI Study Group) received the Richard O’Connor award (the highest research award from the Arthroscopy Association of North America) for our work showing that adding a small additional procedure on the outside of the knee (an anterolateral ligament reconstruction) significantly reduces graft failure rates. At the time of this award, the topic was controversial, but over the last decade our extensive body of clinical research has resulted in major changes in global practice patterns and many surgeons are now performing these types of procedures worldwide.
In addition to ACL surgery, I also specialize in complex revision ACL reconstruction, the reconstruction of other knee ligaments (PCL, MCL, LCL, posterolateral corner, MPFL), tendon repair, patellar dislocation, osteoarthritis, meniscus and cartilage injuries, and also knee osteotomy surgery.
The most common shoulder procedure I perform is rotator cuff repair. The rotator cuff is a group of muscles and tendons in the shoulder that allow a wide range of movement while maintaining the stability of the joint. The rotator cuff can be injured during trauma to the shoulder (e.g. athletic injury, fall or motor vehicle collision) but degenerative tears (those that occur through overuse or ageing, without

any injury) are also very common. Symptoms of rotator cuff tear include shoulder pain (especially at night or during activity), restricted movement and weakness. Although rotator cuff surgery is very common in my practice, I also frequently perform other arthroscopic shoulder surgeries including for shoulder dislocations and separations, biceps tendonitis, SLAP tear, osteoarthritis, impingement, calcific tendonitis and frozen shoulder.
Q: Tell us more about arthroscopic surgery, what sets it apart from general orthopedic surgery?
A: Arthroscopic surgery involves the use of a camera placed into a joint (e.g. the knee or shoulder) through a tiny incision. The camera is used to visualize and treat pathology. The use of a camera allows excellent visualization of areas that may otherwise be difficult to access without extensive surgical approaches and large incisions. The avoidance of large incisions helps to achieve expedited recovery and reduces the risk of infection and the morbidity of surgery.
Q: As an orthopedic surgeon that specializes in sports medicine for over 20 years, what advice would give the next generation of orthopedic surgeons?
A: This is a great question and a complex one. The healthcare landscape is constantly changing and there are always new challenges. It is likely that the next generation will face challenges that are different to the ones I faced. But at the end of the day, the most important thing is our patients.
There are many different aspects that I could focus
on to answer this question, but I will pick just one that I think is particularly relevant for newer generations, and that’s the influence of industry marketing. Over the last few years, we have seen many trends in orthopedic sports medicine with new procedures and implants being much more readily adopted into clinical practice than previously. In my opinion this faster acceptance and uptake reflects the powerful influence of social media and industry marketing. We see many new innovative ideas hit the market with rapid sales growth and then dwindling usage as we gather more clinical data. I think it’s important to maintain our critical appraisal and research skills and not succumb to industry pressure and marketing hype. In a competitive market it’s logical to try to find a niche or a unique selling point to market our services to patients but in my opinion new procedures should be thoroughly evaluated in well-designed clinical research studies before widespread adoption. I think of myself as an innovator and early adopter of new technology, but at the same time my clinical practice is strongly evidence-based, and that’s essential for getting the best possible outcomes for my patients.
Q: What do you love about being a physician? What keeps you motivated?
A: I get a huge amount of satisfaction from seeing my patients recover from injury and get back to doing the things they love. The ultimate test of my work is seeing my professional athletes get back to the highest levels. It’s incredibly satisfying to be a small part of their success stories! However, I get equal satisfaction from seeing patients recover from an injury to return to recreational activity, or being able to pick up their grandchild again, or simply be able to perform activities of daily living without pain. There’s no better feeling for me than giving someone back the ability to enjoy life. That’s why I picked sports medicine instead of other specialties in medicine. With what I do I can see huge and immediate impact and that’s a major source of satisfaction and motivation. If you love what you do, it’s not work! ■

TOP SPECIALTY | SURGERY


OVERVIEW | Arizona Advanced Surgery (AAS) provides patients with the highest quality surgical care and the latest surgical techniques. Surgeons at AAS deliver expert surgical care while minimizing disruption to patients’ lives. They routinely perform minimally invasive procedures that dramatically reduce risks and recovery time.
SERVICES AND CONDITIONS TREATED | Bariatric surgery, colon & rectal surgery, general surgery, laparoscopic surgery procedures, plastic surgery, robotic surgery, surgical oncology, trauma surgery, and vascular surgery.
NUMBER OF PHYSICIANS | 45
LOCATIONS | 14 offices in Chandler, Gilbert, Glendale, Goodyear, Mesa, Peoria, Phoenix, Scottsdale, and Surprise
MAIN OFFICE | 2945 S Dobson Rd, Mesa, AZ 85202 480-969-4138
WEBSITE | arizonaadvancedsurgery.com

OVERVIEW | Pediatrix physicians and staff focus on the overall well-being of children. They believe each child is a special individual; thus, they consider the specific needs of the child at each visit. Likewise, Pediatrix address parents’ concerns to help families meet the needs of their children. In cases of children with special needs, Pediatrix coordinates referral care from specialists to ensure the process of care moves smoothly for parents. Children not only experience special attention at Pediatrix; they also receive the finest medical care.
SERVICES AND CONDITIONS TREATED | Care of premature infants, care for children with special needs, adolescent care, ADHD management, pediatric nutrition & obesity prevention.
NUMBER OF PHYSICIANS | 8
LOCATIONS | 2 offices in Phoenix (Black Canyon & Happy Valley)
MAIN OFFICE | 15650 N Black Canyon Hwy, STE 100, Phoenix, AZ 85053 | 602-866-0550
WEBSITE | pediatrixmd.com

OVERVIEW | As the foremost urogynecology practice in Phoenix, Arizona, Valley Urogynecology Associates offers exemplary care to patients with urinary and gynecologic issues. Valley Urogynecology Associates emphasizes a strong quality of life for every patient. The team offers a variety of treatment options, from conservative nonsurgical care, like lifestyle changes and medication, to advanced treatments, including minimally invasive vaginal surgery and robotic surgery.
SERVICES AND CONDITIONS TREATED | Hysterectomies, urinary incontinence, thermiVA, overactive bladders, fecal incontinence, pelvic organ prolapse, sacral nerve stimulation, bladder Botox, Vesicovaginal fistula, vaginal suspension, rectovaginal fistula, robotic surgery, laparoscopic surgery, and urethral bulking.
NUMBER OF PHYSICIANS | 4
LOCATIONS | 1 office in Phoenix
MAIN OFFICE | 1616 E Maryland Ave, Phoenix, AZ 85016 602-788-1521
WEBSITE | valleyurogynecology.com

OVERVIEW | The doctors at Vascular & Interventional Partners are renowned in the Phoenix area for their knowledge and specialized procedural skills. Our expertise comes from decades of combined experience treating some of the most complex medical conditions in Arizona. Our team’s commitment to improving the health and wellness of our patients has helped us become one of the most respected interventional radiology (IR) divisions in the state.
SERVICES AND CONDITIONS TREATED | Oncology, venous disease, neurovascular, men & women’s health, spine care, dialysis access, Gi interventions, arterial disease treatment, join pain treatment.
NUMBER OF PHYSICIANS | 7
LOCATIONS | 2 offices in Scottsdale and Glendale
MAIN OFFICE | 22455 N Miller Rd #B100, Scottsdale, AZ 85255 | 480-613-3445
WEBSITE | vipinternational.com
OVERVIEW | Valley ENT is a multi-practice physician group that specializes in otolaryngology, allergy, audiology, and facial plastics. No matter the ear, nose, and throat problem, the physicians and providers at Valley ENT can take care of the problem with expertise and care.
SERVICES AND CONDITIONS TREATED | Adult ENT services, allergies & asthma, facial/cosmetic surgery, snoring & sleep apnea, dizziness & balance, head & neck cancer, swallowing & speech issues, hearing loss & hearing aids, sinus conditions & nasal surgery, thyroid, parathyroid & salivary issues.
NUMBER OF PHYSICIANS | 39
LOCATIONS | 18 offices in Phoenix, Glendale, Chandler, Mesa, Scottsdale, Flagstaff, Green Valley, Sierra Vista, and Tucson
MAIN OFFICE | 9097 E Desert Cove, STE 250, Scottsdale, AZ 85260 | 480-614-0499
WEBSITE | azvent.com

OVERVIEW | DKA physicians are tireless advocates for Arizona patients vulnerable or already suffering from CKD and those experiencing end-stage renal disease (ESRD). Their mission is to meet the varied needs of each patient, provide value and excellence in their care, and work to improve every patient’s quality of life.
SERVICES AND CONDITIONS TREATED | Chronic kidney disease treatment, kidney transplant management, kidney stone management, kidney transplants, dialysis, diabetic neuropathy, hypertension treatment, hematuria.
NUMBER OF PHYSICIANS | 14
LOCATIONS | 16 offices in Phoenix, Avondale, Chandler, Mesa, Casa Grande, Florence, Gilbert, Globe, Lake Havasu, Maricopa, Prescott, San Tan Valley, Show Low, and Sun Lakes.
MAIN OFFICE | 612 W Baseline Rd, Mesa, AZ 85210 480-834-9039
WEBSITE | desertkidney.com

OVERVIEW | DISC is an orthopedic spine center of excellence practice serving spine patients in the greater Phoenix, Arizona area. DISC surgeons treat a wide array of spine conditions such as herniated disc, sciatica, spinal stenosis, and degenerative disc disease. DISC provides compassionate and customized patient care to those suffering in pain.
SERVICES AND CONDITIONS TREATED | Artificial disc replacement, endoscopic spine surgery, selective endoscopic discectomy, endoscopic visualized dorsal rhizotomy, and endoscopic foraminoplasty.
NUMBER OF PHYSICIANS | 5
LOCATIONS | 6 offices in Phoenix, Gilbert, Glendale, and Scottsdale
MAIN OFFICE | 1635 E Myrtle Ave, STE 400, Phoenix, AZ 85020 | 602-944-2900
WEBSITE | sciatica.com
TOP SPECIALTY | OTOLARYNGOLOGY

OVERVIEW | AOC provides multiple levels of comprehensive primary ENT care including the diagnosis and management of all diseases of the ears, nose, throat, and sinuses.
SERVICES AND CONDITIONS TREATED | Management of pediatric airway, cancer, skill base surgery, neuro-otology, advanced head & neck surgery, craniofacial surgery, ENT diseases, pediatric otolaryngology, laryngology, endoscopic sinus surgery, audiology & hearing aids, voice & swallowing disorders, thyroid & parathyroid.
NUMBER OF PHYSICIANS | 8
LOCATIONS | 3 offices in Phoenix, Glendale, and Mesa
MAIN OFFICE | 4530 E Shea Blvd, STE 180, AZ 85028 602-264-4834
WEBSITE | aocphysicians.com
TOP SPECIALTY | OPHTHALMOLOGY

OVERVIEW | Associated Retinal Consultants has an experienced team of Arizona eye specialists that diagnose and treat vision problems. Their focus is on the retina and macula (the back of the eye) and the vitreous humor (gel like tissue) in the eye.
SERVICES AND CONDITIONS TREATED | Retinal diseases, ocular oncology, inherited retinal disease, retina surgery, and clinical trials.
NUMBER OF PHYSICIANS | 10
LOCATIONS | 13 offices in Phoenix, Gilbert, Goodyear, Mesa, Scottsdale, Peoria, Prescott Valley, Prescott, Casa Grande, Cottonwood, Flagstaff, Payson, and Sedona.
MAIN OFFICE | 1750 E Glendale Ave, Phoenix, AZ 85020 602-242-4928
WEBSITE | associatedretinalconsultants.com

OVERVIEW | Radiation Oncologists of Central Arizona, LLP (ROCA) has been offering compassionate, cutting-edge cancer treatment to Valley residents for over 20 years at the premier hospital-based cancer centers in metro Phoenix. ROCA physicians are internationally recognized leaders in advanced radiotherapy technology and have introduced state-of-the-art therapies to the Valley. ROCA physicians have also provided Arizona’s cancer patients access to clinical trials through collaborative research organizations.
SERVICES AND CONDITIONS TREATED | Lung cancer, breast cancer, prostate cancer, brain cancer, trigeminal neuralgia, abdominal cancer, acoustic neuroma, and arteriovenous malformations (AVM).
NUMBER OF PHYSICIANS | 4
LOCATIONS | 1 office in Phoenix
MAIN OFFICE | 4611 E Shea Blvd, STE 120, Phoenix, AZ 85028 602-441-3845
WEBSITE | phoenixcyberknifecenter.com
TOP SPECIALTY | KIDNEY, LIVER, & PANCREAS SURGERY

OVERVIEW | Arizona Transplant Associates has continued to wage war on cancer for decades.
SERVICES AND CONDITIONS TREATED | Whipple procedures, liver resections, liver transplants, kidney transplants, kidneypancreas transplants, pancreas transplants, and other pancreas & bile duct resections.
NUMBER OF PHYSICIANS | 6
LOCATIONS | 1 office in Phoenix
MAIN OFFICE | 2218 N 3rd Street, Phoenix, AZ 85004
602-252-2543
WEBSITE | aztransplant.com
TOP SPECIALTY | OPHTHALMOLOGY

OVERVIEW | At Retinal Consultants of Arizona, they diagnose and find new innovative treatments for retinal conditions. Their goal is to provide patients the best possible outcomes for their unique retinal needs.
SERVICES AND CONDITIONS TREATED | Diabetic macular edema, diabetic retinopathy, flashes, floaters, macular degeneration, macular holes, macular pucker, posterior vitreous separation, retinal artery occlusions, retinal detachment, retinal tears, retinal vein occlusions, and uveitis
NUMBER OF PHYSICIANS | 7
LOCATIONS | 15 offices in Phoenix, Gilbert, Mesa, Peoria, Scottsdale, Bullhead City, Flagstaff, Kingman, Payson, Prescott, Yuma, and Yuma Foothills
MAIN OFFICE | 1101 E Missouri Ave, Phoenix, AZ 85014 602-222-2221
WEBSITE | retinalconsultantsaz.com

OVERVIEW | At Arizona Preferred Surgeons, their surgeons are skilled in complex decision making and diagnosis, as well as treatment and management.
SERVICES AND CONDITIONS TREATED | From anal fistula & fissures, appendectomies, breast surgery, colon cancer surgery, colonoscopies & upper endoscopies, Crohn’s & Ulcerative colitis, diverticulitis, fecal incontinence, gallbladder surgery, gastric resection, hernia surgery, hemorrhoids, and Nissen Fundoplication.
NUMBER OF PHYSICIANS | 3
LOCATIONS | 1 office in Glendale
MAIN OFFICE | 18699 N 67th Ave, Glendale, AZ 85308
602-995-0822
WEBSITE | azpreferredsurgeons.com

OVERVIEW | Cornea Consultants of Arizona has been serving patients of all ages for a wide variety of ophthalmic conditions of the cornea and anterior segment for the past 35 years. Each of their physicians are board certified and have completed over 13 years of training including medical school, internship, ophthalmology residency, and an additional fellowship year in cornea, external disease, and refractive surgery.
SERVICES AND CONDITIONS TREATED | Cornea transplant, dry eyes/external diseases, investigative trials, laser vision correction, and premium cataract surgery.
NUMBER OF PHYSICIANS | 3
LOCATIONS | 4 offices in Phoenix, Chandler, Peoria, and Prescott Valley
MAIN OFFICE | 3815 E Bell Rd, STE 2500, Phoenix, AZ 85032 602-258-4321
WEBSITE | corneaaz.com
TOP SPECIALTY | DERMATOLOGY

OVERVIEW | Arizona Dermatology is proud to be a leader in the skin care industry and they strive to provide the highestquality medical dermatology, skin cancer treatments, cosmetic procedures, and med spa aesthetic services in Arizona. They use advanced techniques, expertise, and state of the art technology that allow them to provide unparalleled skin care results.
SERVICES AND CONDITIONS TREATED | Medical Dermatology (wart removal, acne treatments, psoriasis treatments, rosacea treatments, vitiligo treatments, melasma treatments), skin cancer (skin cancer screening, Mohs therapy skin cancer treatment), Botox, facial fillers, and Medspa services (intense pulse light therapy (IPL), micro-needling, chemical peels, vascular laser, dermaplaning, and microdermabrasion).
NUMBER OF PHYSICIANS | 6
LOCATIONS | 5 offices in Phoenix, Paradise Valley, Apache Junction, Mesa, and Show Low
MAIN OFFICE | 4835 E Cactus Rd, STE 155, Scottsdale, AZ 85254 | 602-996-3050
WEBSITE | arizonaderm.com
TOP SPECIALTY | PEDIATRICS

OVERVIEW | Pleasant Pediatrics was founded in 2008 by a devoted husband-wife team with a vision of providing compassionate, family-centered care. The Pleasant Pediatrics logo of three joyful children (inspired by the founders’ triplets) represents their inspirations and commitment to nurturing every child’s wellbeing.
SERVICES AND CONDITIONS TREATED | Routine well child exams, sports physicals for school, immunizations, TB skin testing, hemoglobin, urinalysis, rapid strep treatment, flu testing, pregnancy testing, antibiotic injections, circumcision, ear lavage, frenectomy (tongue tie), umbilical granuloma, and nebulizer treatments.
NUMBER OF PHYSICIANS | 16
LOCATIONS | 8 offices in Peoria, Glendale, Ahwatukee, and Phoenix
MAIN OFFICE | 9059 W Lake Pleasant Pkwy, STE E540, Peoria, AZ 85382 | 623-322-3380
WEBSITE | pleasantpediatrics.com
Phoenix, AZ 85004
(602) 417-2303
information@arizonaphysician.com