Diabetes in America
June 2024 | www.futureofpersonalhealth.com
“Recent technology has enabled the development of several exciting options to help people with diabetes optimize their health.”
Jane K. Dickinson, RN, Ph.D., CDCES, 2024 President, ADCES Page 02
An independent supplement by Mediaplanet to USA Today
“Whether you’re newly diagnosed, have had diabetes for a while, or are a caregiver, you can thrive with diabetes — and we have the steps to help you get there.” American Diabetes Association
Page 06

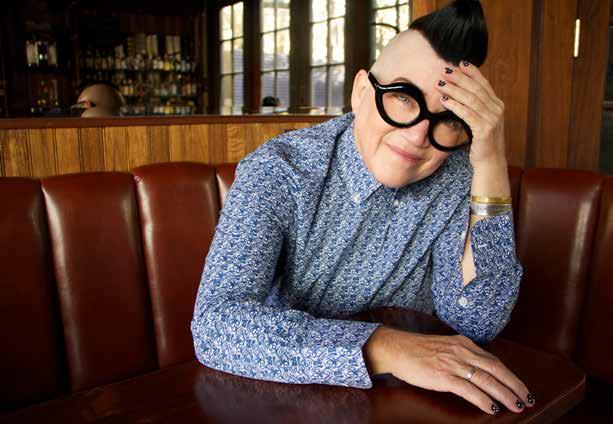
The comedian and
“Orange Is the New Black” star talks about the lifestyle changes she made to get her type 2 diabetes under control
Read more on Page 04
LEA DELARIA
The Keys to Treating Diabetes in Patients With Obesity
In the world of healthcare, the disease of obesity emerges as a particularly intricate challenge.
The relationship between obesity and diabetes often forms a cycle in which each condition worsens the other. Treating diabetes in patients with obesity requires a comprehensive treatment plan that encompasses a variety of psychological, physical, and lifestyle factors.
At the core of diabetes and obesity lies a strong interplay of genetic, environmental, and lifestyle factors. Treating both conditions requires that all these factors be considered.
Genetic predispositions play a significant role in both conditions, influencing susceptibility to obesity and insulin resistance. Recognizing these genetic factors can inform personalized treatment strategies, guiding clinicians to decide the most appropriate modifications for each patient.
Lifestyle interventions are the most essential part of treatment. Emphasizing nutrition modifications and increased physical activity can help patients achieve weight loss and improve metabolic health.
While every patient is different, nutritional strategies often focus on reducing calorie intake, limiting refined sugars and saturated fats, and emphasizing nutrient-dense foods, such as fruits, vegetables, whole grains, and lean proteins.
As we continue to unravel the complexities of these two conditions, ongoing research, innovation, and collaboration can help in advancing our understanding and refining our approaches to diabetes care in the context of obesity.
Written by Angela Fitch, M.D., FACP, FOMA, Founder and Chief Medical Officer, knownwell; Immediate Past President, Obesity Medicine Association
Using New Diabetes Technologies to Optimize Self-Care
Diabetes care has come a long way in recent years, with technological advancements playing a significant role in improving the lives of people with diabetes. From continuous glucose monitoring to automated insulin delivery, recent technology, including AI, has enabled the development of several exciting options to help people with diabetes optimize their health.
Some of the most popular devices that are currently available to individuals with diabetes include:
Continuous glucose monitors (CGMs):
A device that measures glucose levels in real-time using a sensor under the skin. It helps people with diabetes track their glucose levels, and identify trends and proactively respond to them.
Smart insulin pens:
A connected insulin pen that can track insulin doses and send reminders to take insulin. It syncs this information with a smartphone app to make trend identification easier.
Insulin pumps and automated insulin delivery (AID) systems: Insulin pumps have been around for a while, and new AID technology combines a pump and CGM with a mathematical algorithm to automatically deliver insulin. This system is designed to help regulate glucose levels by delivering insulin when needed, based on real-time glucose readings from the CGM.
Life-changing solutions
These technologies can be truly life-changing for many people living with diabetes. As with any new technology, however, there’s a learning curve. People are often challenged with using these devices effectively,

troubleshooting, and interpreting the data to make treatment decisions. This is not always easy, though it can become more manageable with the help of a diabetes care and education specialist.
Diabetes care and education specialists are healthcare professionals dedicated to helping people with diabetes become experts in their own care, make informed choices, and get the most out of their treatment options, including using these new technologies. They are especially helpful when it comes to device initiation or start-up, overall education and support, and follow-up to make any adjustments the person needs.
Ask your primary care professional or endocrinologist for a referral to a diabetes self-management education and support program in your area, or visit www.adces.org/ diabetes-education-dsmes to find an accredited program near you.

02 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM @futureofpersonalhealth Contact information: US.editorial@mediaplanet.com @MediaplanetUSA Please recycle
Managing Director Gretchen
Production Manager Dustin Brennan Creative Director Kylie
Cover Photo by
All photos are credited to Getty Images unless otherwise specified. This section was created by Mediaplanet and did not involve USA Today.
Publisher Bryan Espinosa
Pancak
Armishaw
Tina Turnbow
WRITTEN BY Jane K. Dickinson, RN, Ph.D., CDCES 2024 President, Association of Diabetes Care & Education Specialists












































































































































How Comedian Lea DeLaria Is Taking Diabetes 1 Day at a Time
Known for her role as Big Boo on Netflix’s “Orange Is the New Black,” actress and comedian Lea DeLaria was diagnosed with type 2 diabetes early in the show’s run. We talked with her about how she’s managed the condition through lifestyle changes and daily medication, and has become an advocate for other diabetics.
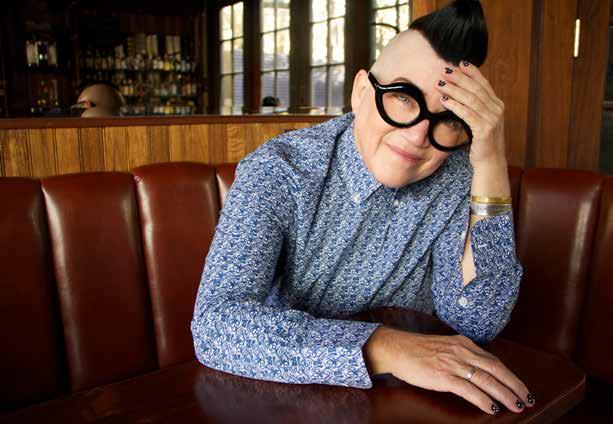
What went through your mind when you were first diagnosed with type 2 diabetes?
My mom was diagnosed with diabetes in her 30s and just a few months before I got the diagnosis, I had visited my family and my brother was diagnosed. We’re a very sarcastic family, so I was laughing at him like, “Yeah, I’m fat, but at least I don’t have diabetes.” And then three months later when I went for a physical, the doctor told me I had diabetes. I was like, “Oh my god.” And then of course my brother and I just proceeded to text each other.
My blood sugar was over 400 and my A1C was over 11, and the normal level is 7. There are a lot of things that one looks for or is aware of, like frequent urination, exhaustion, weight loss, and at the time I was perimenopausal, so I was going through the change hormonally and I didn’t even think about diabetes until
they told me. The whole thing took me by a bit of a surprise. You think you know your health until this happens.
The whole thing took me by a bit of a surprise. You think you know your health until this happens.
Also, I did not have health insurance, so I wasn’t getting a physical very often. So, when I was cast in “Orange is the New Black” and I had health insurance through my union, that was when I was able to get a physical and found out I had diabetes. So, it’s hard for most people without insurance to get screened and
most are living undiagnosed, which can be dangerous.
Why did you decide to go public with your diagnosis and how did you handle the media attention?
When the show premiered, it blew up and was crazy popular, and I was diagnosed about a year after the first season hit the airways. So, I was doing a lot of press and walking red carpets, and I had lost a lot of weight because I was changing my habits in relation to the disease.
Everybody was like, “how did you lose weight?” And I said, “Well, first you contract diabetes,” and I was being funny about it, but once I did start becoming vocal about it, I noticed there were a lot of other people who were vocal about it and decided this should be something that we discuss.
I started talking about lifestyle changes that you have to make,
like changing your habits. For example, the first thing I do is take my medication — I never mess around with that. I have to take medication every day and I take it on schedule. I also go to the gym, and it becomes this routine of making sure you take your medication, are eating on time, and that’s it.
Is there any advice you can give to other people who have been recently diagnosed with and are currently managing type 2 diabetes?
It’s a process. Eventually you will get used to this process, and you’re going to make mistakes. Just give yourself some grace, correct, and move on. Find alternatives for your favorites, like keto, and compensate. We’re all freaking human — give yourself a break.
I messed up yesterday, today is another day, and I’m handling my diabetes one day at a time.
04 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM
Photo Credit: Lea DeLaria
Photo by Tina Turnbow
Patients Living With Diabetes Deserve Specialized Hospital Care
Of the 37 million people in the United States who are living with diabetes and hyperglycemia, 12 million are admitted to the hospital each year. Inpatients diagnosed with type 1 diabetes account for an estimated 600,000 of those admissions.
People living with diabetes represent up to one-third of hospitalized patients. And while all patients face serious risk of harm from preventable medical errors, injuries, and infections, people living with diabetes are even more vulnerable. Inequity makes those risks even greater for some patients. For instance, Black and Indigenous people with diabetes are 30% more likely than white people with diabetes to undergo amputation.
There are established and tested best practices for hospitals to safely care for inpatients living with type 1 and type 2 diabetes, and some hospitals excel in this area. That’s why the Leapfrog Group, a national watchdog organization of employers and other purchasers focused on healthcare safety and quality, joined with the American Diabetes Association (ADA) to launch a new program that honors hospitals going the distance for this vulnerable
population: Recognized Leaders in Caring for People Living with Diabetes.
Going the extra mile
The aim of the program is to galvanize hospitals to take the appropriate actions to protect patients living with diabetes. Recognized hospitals do the following, among other things:
• Provide safe, high-quality care for people living with diabetes
• Implement blood glucose (blood sugar) testing and hypoglycemia protocols
• Engage in specialized preparation for inpatient surgery
• Plan meals and insulin regimen
• Offer robust discharge planning for high-risk patients with diabetes
Patients living with diabetes who may need hospital care should ask their hospitals about protocols and practices they have in place to protect them
from preventable harm. This program aims to encourage more hospitals to put patients first and prioritize the specialized needs of patients living with diabetes.
In March, Leapfrog and the ADA annouced the first hospitals to receive national designation as Recognized Leaders in Caring for People Living with Diabetes. The designation reflects a strong commitment to the safety and well-being of hospitalized people living with diabetes.
We are proud to honor these hospitals and encourage others across the country to apply for this annual recognition. Applications for 2025 Recognized Leaders in Caring for People Living with Diabetes open July 1, 2024, and close November 30. Winners will be announced in spring 2025. A full list of the 2024 Recognized Leaders can be found at bit.ly/recognizedleaders


05 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM
WRITTEN BY
Leah Binder
President and CEO, The Leapfrog Group
5 Ways to Thrive With Diabetes
The numbers are staggering. Over 38 million Americans have diabetes and nearly 98 million live with prediabetes. But there are steps you can take to not only survive, but thrive with the condition.
 Sponsored
Sponsored
Finally, An Affordable Oral Treatment for Type 2 Diabetes
Type 2 diabetes affects 1 in 10 adults in the United States, and proper treatment is key to preventing complications and improving quality of life.
However, adhering to treatment can be challenging. Thirty-five percent (35%) of patients with type 2 diabetes struggle to stick to their blood sugar-lowering medication, according to research in the journal Clinical Therapeutics.1
Poor adherence is often linked to financial burden. A study in the journal Diabetes Care found that approximately 18% of individuals with diabetes reported cost as a factor in their inability to take their medications.2
That means that affordable and accessible medicines can significantly improve the overall health of people with diabetes. A treatment called BRENZAVVY® (bexagliflozin) aims to meet this
need at a much lower price compared to other heavily advertised treatments in the same class.
“I’m encouraged by the evolution of the supporting data for BRENZAVVY,” said Brian Connelly, CEO of TheracosBio, “and believe that [the Diabetes Care] study confirms that BRENZAVVY can serve as a cost-effective treatment option for millions of patients with type 2 diabetes mellitus. We do not think patients should have to compromise on efficacy or safety when they receive a more affordable option.”
BRENZAVVY is FDA-approved to help manage blood sugar levels in people with type 2 diabetes when used with diet and exercise modifications. BRENZAVVY
belongs to the drug class oral sodium-glucose transporter 2 (SGLT2) inhibitors and is not approved for use in people with type 1 diabetes. The adverse reactions across clinical trials are typical for this drug class. The most common reactions (incidence >5%) are female genital mycotic infections, urinary tract infection, and increased urination.
BRENZAVVY is available at local independent and online pharmacies, which can be convenient for both patients and providers.
Written by Melinda Carter
REFERENCES
1 Yang et al., 2009; Clinical Therapeutics 31(10) 2178-2188
2 Taha et al., 2022; Diabetes Care 45(3) 594-603
We do not think patients should have to compromise on efficacy or safety when they receive a more affordable option.
To learn more and for the full Prescribing Information, visit brenzavvy.com


06 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM
Although receiving a diabetes diagnosis can be scary, there’s hope. Small lifestyle changes can make a big impact on your health. With a few swaps and additions to your routine, you or your loved one can live a long and healthy life.
Whether you’re newly diagnosed, have had diabetes for a while, or are a caregiver, thriving with diabetes is possible — and we have the steps you can take to get there.
1. Get moving
Regular physical activity is an important part of managing diabetes. Walking is a great place to start and a great daily activity to work into your life. Walk with a loved one, your dog, or by yourself while listening to an audio book or your favorite tunes. If you’re feeling overwhelmed
by the idea of starting a more active life, take heart. Every change, no matter how small, makes a difference in your ability to manage diabetes.
2. Have an eating plan
Eating well with diabetes doesn’t mean giving up your favorite foods — it’s about finding the balance between keeping the flavors you love and including the nutrients you need to manage diabetes.
Try using the Diabetes Plate — a visual guide that makes creating healthy meals simple. Fill half of a 9-inch plate with non-starchy vegetables, one-quarter with lean protein foods, and one-quarter with quality carbohydrates.
3. Simplify your routine
Find ways to make life easier by simplifying your daily routine. If you use specific diabetes
Splenda® to Donate $2,500 to 25 Families Impacted by Diabetes
Splenda® is awarding $2,500 to 25 families in honor of its 25th birthday to support families impacted by diabetes.
Splenda, America’s No. 1 sweetener brand, proudly announces the launch of “25 Families for 25 Years” as a part of the brand’s 25th birthday celebrations.
For more than two decades, Splenda has been at the forefront of empowering individuals to lead happier, healthier, and longer lives by making it easier to reduce sugar. In alignment with its mission and 25th birthday, Splenda is donating $2,500 to 25 families living with diabetes to offset costs toward medical expenses, educational pursuits, or other essential needs.
What started as a little yellow packet to help people reduce sugar in their coffee & tea has transformed
supplies every day, sign up for auto-delivery so you won’t forget to get more when you’re running out. Or try setting up virtual routine medical appointments to avoid travel cost and time.
4. Consult your healthcare team
Take charge of your health with guidance from the trusted experts on your healthcare team. They will support your goals for managing diabetes and reducing your risk of diabetes-related complications. The more information you give them when setting up your treatment plan, the more individualized it will be.
Be sure to write down all your questions and concerns and ask them at your appointments. And remember, the most important member of your healthcare team is YOU!
Sponsored
into a global brand with a mission to help people achieve their health goals. Today, Splenda offers an entire portfolio of products, including sweeteners, diabetes care shakes, and more, to help people successfully reduce sugar. Splenda invites individuals and families affected by diabetes to participate in the “25 Families for 25 Years” campaign by sharing their stories of resilience and determination.
Written by Splenda

5. Prioritize your mental health
Tracking blood glucose (blood sugar) levels, medications, planning meals, staying active — it’s a lot to think about. It can leave you feeling run down, emotionally drained, and completely overwhelmed.
That’s called diabetes burnout. And that’s why it’s important to stay in touch with your emotions as you manage your diabetes. What are you feeling? Stressed out? Angry? Sad? Scared? Take time to take stock of your emotions and reach out to those around you to talk honestly and openly about how you feel. Better yet, find a mental health professional to guide you through the emotional terrain around your disease.
Written by American Diabetes Association

07 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM
visit splenda.com/ 25-families
To participate, please

We accept over 500 insurance plans and nation-wide Medicare. Let US MED handle the billing for you! Discover the convenience of accessing Continuous Glucose Monitors with complete 90-day supplies, backed by Medicare Parts B & D. Choose US MED® for cutting-edge diabetes care technology and service. Join over 1,000,000 happy members and enjoy top-tier support and supplies delivered promptly to your doorstep. US MED®: Modern diabetes care, made easy for Medicare Visit us in booth #447 at ACDES24 for insights into our services and to meet the people behind your care. Get started at: www.usmed.com/usat or give us a call! 1-888-710-0454

















 Sponsored
Sponsored

