Infectious Diseases

“Floods are just one of the troubling synergies between antibiotic resistance and climate change.”
“Where can you find more antimicrobialresistant bacteria? Look in low-income ZIP codes.”
There simply aren’t enough antibiotics to treat bacteria that cause serious disease and death, and antibiotics’ effectiveness is diminished the more they are used.
Read more on Page 02
Haley A. Pritchard, M.D., M.S. Assistant Professor of Clinical Medicine, Indiana University Health
The Society for Healthcare Epidemiology of America
Page
(SHEA)
06
Henry
Ph.D., M.Jur., CEO, AMR Action Fund Page
Skinner,
04
September 2023 | futureofpersonalhealth.com An independent supplement by Mediaplanet to USA Today
How the PASTEUR Act Can Solve America’s Superbug Crisis
Antibiotics transformed modern medicine, offering lifesaving treatment and preventing widespread outbreaks of infections. Many common but dangerous infections are now largely resistant to the drugs traditionally used to treat them, risking the lives of the entire population. Legislation has been proposed to ensure continued access to antibiotics that work — but Congress must act fast.
The Centers for Disease Control and Prevention estimates that antimicrobial resistance already causes at least 3 million illnesses and 35,000 deaths in the United States each year — averaging nearly 100 people each day. Infections are one of the most common complications for patients with cancer, causing or contributing to half of all cancer deaths as resistance makes these infections increasingly harder to treat.
Drug-resistant bacteria pose a particularly severe threat to women’s health, as they can lead to cases of urinary tract infections, sepsis, and sexually transmitted infections that are incredibly difficult or impossible to treat.


More than 92% of bacteria that cause UTIs are resistant to at least one common medication, and almost 80% are resistant to at least two. Sepsis is already a leading cause of maternal mortality, a problem made worse by antimicrobial resistance, which increases the danger and challenge of treating it. This year, experts sounded the alarm as cases of gonorrhea, the second most common STI in the United States, emerged with increased resistance to every kind of antibiotic available to treat them.
Historically marginalized populations are at disproportionate risk for certain antimicrobial-resistant infections. The rates of community-associated antibiotic-resistant MRSA are higher among Black populations, and American Indian and Alaska Native communities have substantially higher rates of Group A Streptococcus.
The PASTEUR Act
Doctors need a robust antibiotic pipeline to protect patients and resources for antibiotic stewardship programs in healthcare facilities, which guide appropriate antibiotic use to improve patient outcomes and preserve antibiotics’ effectiveness. There simply aren’t enough antibiotics to treat bacteria that cause serious disease and death, and antibiotics’ effectiveness is diminished the more they are used.
Proposed bipartisan legislation, called the PASTEUR Act (which stands for Pioneering Antimicrobial Subscriptions to End Upsurging Resistance), calls for a change in the way the government funds the development of new antibiotics.
The PASTEUR Act would strengthen the antimicrobial pipeline by transitioning to a subscription-style program, providing reliable federal contracts for critically needed antimicrobials. This would give drugmakers — typically very small companies — a predictable return on investment that aligns with the need to limit the prescription of antibiotics to maintain their efficacy.
In essence, Congress would support the development of much needed antibiotics that we don’t want a lot of people to use — or overuse. PASTEUR would also provide hospitals and long-term care facilities with resources to support appropriate antibiotic use.
Lawmakers must pass the PASTEUR Act to ensure doctors and their patients can access lifesaving antimicrobial treatments that work — before it’s too late.
 WRITTEN BY Haley A. Pritchard, M.D., M.S. Assistant Professor of Clinical Medicine, Indiana University Health
WRITTEN BY Haley A. Pritchard, M.D., M.S. Assistant Professor of Clinical Medicine, Indiana University Health

02 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM
are
Publisher
Shannon Ruggiero Managing Director Julia Colavecchia Production Manager Taylor Daniels Lead Editor Dustin Brennan All photos
credited
to Getty Images
unless
otherwise specified. This section was created by Mediaplanet and did not involve USA Today.
Learn more at idsociety.quorum.us/ campaign/47463/ READ MORE ONLINE Addressing Gaps in Infection Control Knowledge and Practice
Sepsis and Antimicrobial Resistance: A Complicated, Dangerous Relationship
The Future of Global Infectious Disease: A Roundtable Discussion World AMR Congress 2023 Speakers Philadelphia, PA @futureofpersonalhealth Contact information: US.editorial@mediaplanet.com @MediaplanetUSA Please recycle
Amy Kolwaite, Ph.D., RN, ARNP Nurse Epidemiologist, CDC
Alexandria
Sadorf Colvin Director of Marketing and Communications, Sepsis Alliance
For more than three decades, Gilead has been dedicated to developing innovative treatments and therapies for HIV. But medicine alone is not enough. It takes the collective power of all of us. It’s only by collaborating and partnering with community organizations and individuals that we can achieve our collective goal of bringing the HIV epidemic to an end for everyone, everywhere.






































Get inspired by Arianna’s story at GileadHIV.com Harnessing the power of many working as one. Together we ignite change.
Learn more at GileadHIV.com @ @gileadhivus @GileadHIVUS GILEAD, the GILEAD Logo, and the & Design are trademarks of Gilead Sciences, Inc. All other marks referenced herein are the property of their respective owners. US-UNBC-1764 09/23
AriannaInurritegui-Lint ExecutiveDirector,Arianna’sCenter GileadGrantRecipient
WRITTEN BY Henry Skinner, Ph.D., M.Jur. CEO, AMR Action Fund


Floods, Superbugs, and Lessons From Texas
All this flooding portends something nasty for public health.
Winter delivered a series of atmospheric rivers that soaked California and submerged towns from the Central Valley to the Santa Cruz Mountains. Spring saw destructive downpours that dumped more than 2 feet of rain in half a day on parts of South Florida. Summer storms put large parts of New England underwater.
Strong storms and floods have long been known to spread pathogens and inflict illness. Now emerging research shows they may be supercharging the spread of drug-resistant bacteria and fungi, posing near- and longterm health challenges that claim lives and strain hospital systems. Just look at Texas.
The heart of Texas
When Hurricane Harvey stalled over Houston in 2017, the acute
devastation was heartbreaking — more than 100 people died, an estimated 300,000 buildings and homes were damaged or destroyed, and several wastewater treatment facilities failed, sending rivers of bacterialoaded sewage into the streets and people’s homes. As the flood waters receded and clean-up efforts commenced, teams of scientists began studying how the flooding affected the microbes in the surrounding environment. The findings, which are still trickling out, are concerning and should serve as a warning to residents, healthcare professionals, and policymakers in flood-prone regions.
Rising temperatures
Floods are just one of the troubling synergies between antibiotic resistance and climate change. Several studies show
that extreme heat — another hallmark of global warming — can accelerate the rate at which microbes grow, spread, and adapt to live at body temperature.
In the face of such evidence, the world needs to better prepare for the likelihood that extreme weather events will drive outbreaks of drug-resistant infections. Policymakers who are designing and implementing climate resiliency plans would do well to consider the multifaceted dynamics of antibiotic resistance, from wastewater management and agricultural practices, to public health surveillance systems and the paucity of new antibiotics in development.
With fall torrents on the horizon, more floods are sure to come. There’s nothing we can do to stop the rain, but we can prepare for it — and the germs it spreads.
Paving the Way to Better Gram-Negative Antimicrobial Discovery
WRITTEN BY Bruce Blough Senior Research Chemist, RTI; Principal Investigator, CC4CARB
The pharmaceutical industry has divested from antibiotic research, drastically reducing funds for early discovery. Large screening efforts failed. A natural tendency to question novelty reduces enthusiasm for new ideas.
Consequently, obtaining and maintaining funds for discovery or to develop novel scaffolds is difficult. Emerging theories, such as the “eNTRy” model, suggest Gram-negative antimicrobial discovery efforts have been hampered by the lack of structural features enabling penetration. Features like primary amines, avoided in mammalian targeted drug discovery, facilitate penetration, and their absence may explain screening failures.
Seeding discovery
As a solution, the National Institute of Allergy and Infectious Diseases (NIAID) launched the Chemistry Center for Combating AntibioticResistant Bacteria (CC4CARB).

CC4CARB is an international collaboration aimed at seeding the discovery of antimicrobials by building a publicly available screening library of Gramnegative related chemical matter. Small, focused libraries based on community-solicited scaffolds are combined to form the screening library. Scaffolds can be in early discovery, hit-tolead, lead optimization, or can be AI-generated.
CC4CARB prefers traditional, small molecule discovery conducive for library synthesis, but can manage complex projects based on natural products, peptides,
or organometallics. CC4CARB projects include broad spectrum and selective antimicrobial discovery. Submitters will receive enough of each compound to seed their research.
The research community is invited to submit scaffold ideas. Proposals are reviewed by the CC4CARB team, a scientific advisory board, and then NIAID. Library design is a collaborative effort between the scaffold submitter and CC4CARB chemists, and will incorporate modern approaches to Gramnegative antibiotic discovery.
The program includes an 18-month disclosure embargo period to enable intellectual property development.
Compounds may be tested for antimicrobial activity, depending on available funding. CC4CARB also accepts compound donations.
04 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM
Novel Gram-negative antimicrobial scaffold discovery is one of the surest ways to avoid resistance, but efforts to find them remain challenging.
learn more, visit cc4carb-collection. org or request a teleconference by emailing CC4CARB@rti.org
Sponsored To
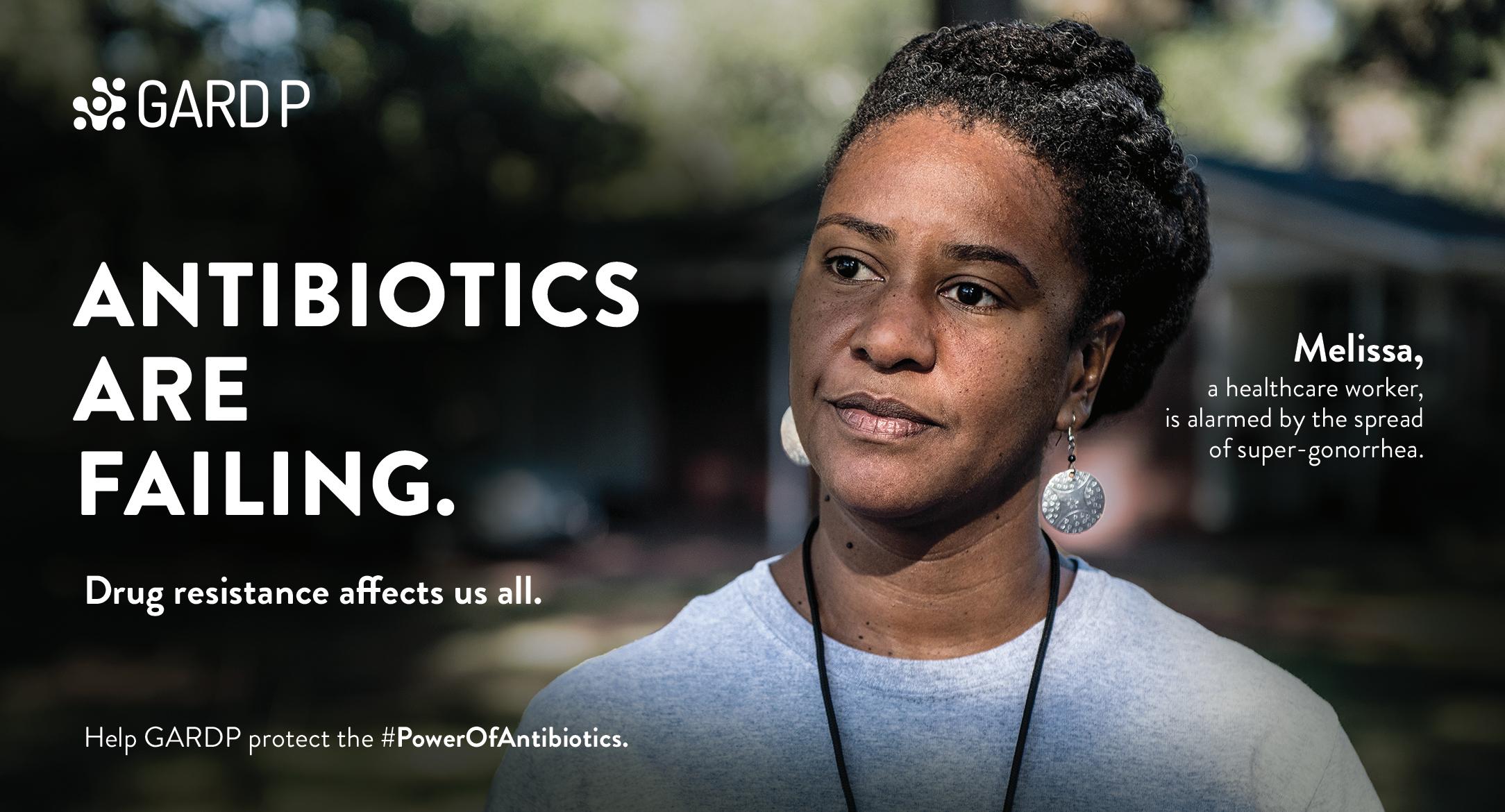
WRITTEN BY Dr. Manica Balasegaram Executive Director, Global Antibiotic Research &

Why Drug Resistance Needs Long-Term Global Solutions
It is often described as the silent pandemic, but there is nothing silent about antimicrobial resistance (AMR).
AMR currently kills at least 1.27 million people a year globally — more than HIV/ AIDS and malaria combined. And no matter who you are or where you live, we are all at risk.
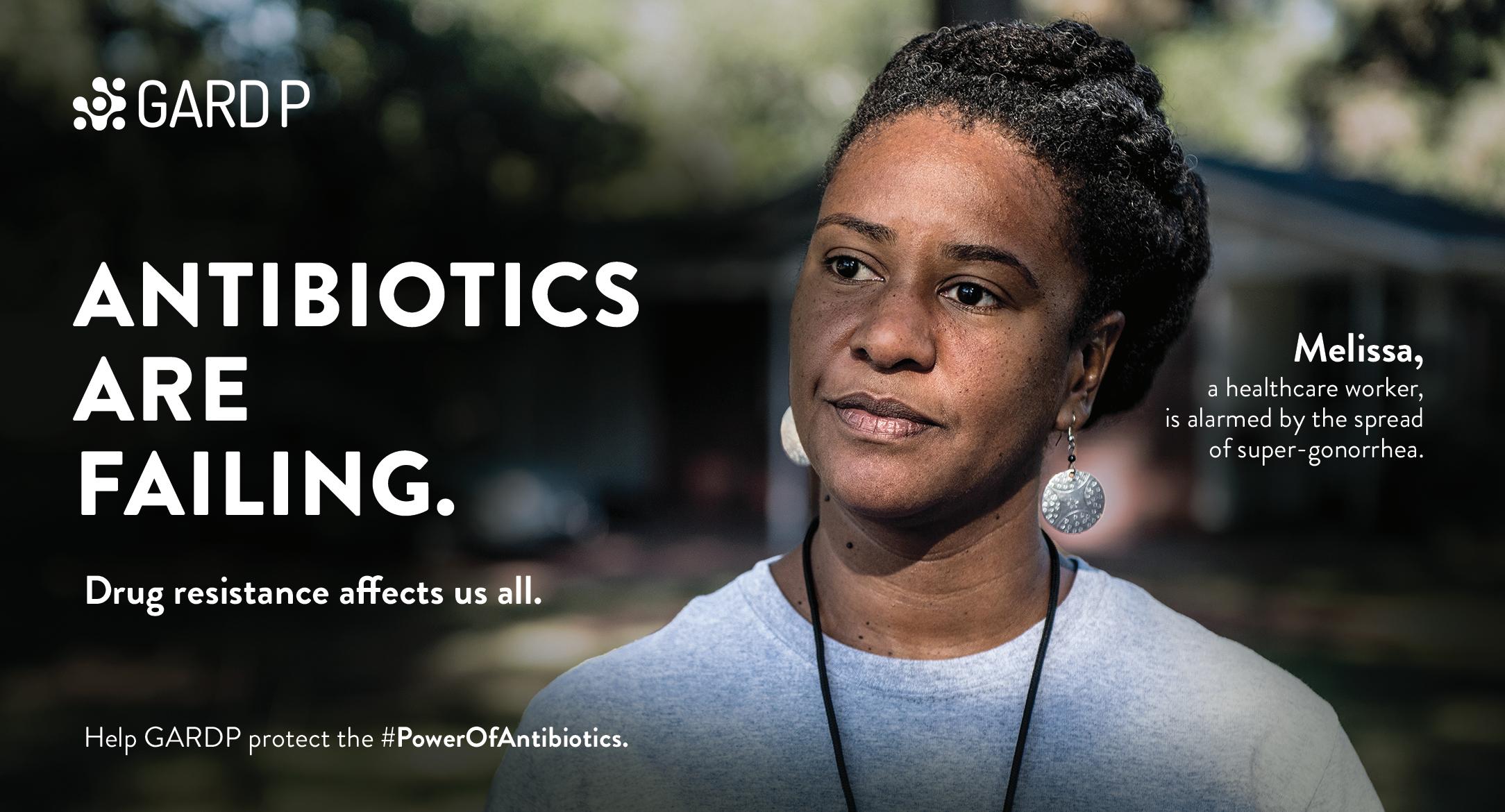
While many now recognize that we need new and effective antibiotics treatments to outpace the spread of drugresistant bacteria, the scale and breadth of the global response is still not reflecting the scale or scope of the problem — nor the level of urgency required.
Far from being some kind of looming threat that will happen suddenly — like a pandemic — AMR is a global
crisis that is already upon us. Gonorrhea is just one example; once highlytreatable, today we are seeing an alarming trend of outbreaks of “supergonorrhea,” which are resistant to all antibiotics, which means it could become one of the first diseases to once again become untreatable, unless new antibiotics are developed.
People over profit
My organization is working to prevent this scenario from happening, with the development of the first in a new class of antibiotics that could potentially treat drugresistant gonorrhoea. While there is a clear need for investment into the
development of new drugs like this, broader global solutions are needed to beat AMR — ones that not only solve the market failures that helped create this problem, but also the public health failures that have resulted from it. That is why in addition to helping develop new treatments against multidrugresistant bacteria that pose the greatest public health threat, it is important to ensure these treatments reach the people that need them most, and continue to do so. Our aim is to make this possible by helping to rebuild a global pipeline for antibiotics that is driven by public health need, rather than profit.
05 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM
Development Partnership (GARDP)
Understanding the Link Between Antimicrobial Resistance and Health Disparities
Where can you find more antimicrobial-resistant bacteria? Look in low-income ZIP codes.
WRITTEN BY
When a May 2023 study published in Infection Control and Hospital Epidemiology found that multidrug resistance is significantly and persistently more prevalent in samples taken from patients in lowincome versus high-income ZIP codes in North Carolina1, readers of the medical journal were likely not surprised.
Health inequities are persistent. Marginalized populations face barriers to healthcare access and experience worse health outcomes. Vulnerable communities, including those with lower socioeconomic status and limited access to quality healthcare, bear a disproportionate burden of infectious diseases.
To best address health inequity and combat antimicrobial resistance (AMR), antibiotic stewardship programs must focus their efforts on better understanding this relationship and implementing programs that address health disparities.
antibiotic stewardship is no different. Poor sanitation, overcrowding, and inadequate nutrition in underserved areas create environments conducive to the spread of resistant pathogens. Without properly resourced antimicrobial stewardship programs, patients may be at risk of developing adverse antibiotic effects, including allergic reactions, Clostridioides difficile infections, or bearing the burden of AMR infections later in life.
Steps to change
A critical step in addressing the health equity burden lies in acknowledging that these inequities exist. Inequitable access to healthcare and health insurance, poor health literacy, and other social determinants of health result in disparities in infections.
WRITTEN BY
Zanthia Wiley, M.D., FHM, FIDSA Associate Professor of Medicine, Emory School of Medicine; Education Committee Chair, SHEA


Inequality and AMR
The CDC defines antibiotic stewardship as, “the effort to measure and improve how antibiotics are prescribed by clinicians and used by patients.” This specialized, multidisciplinary effort addresses the threat of AMR by monitoring antibiotic use (and misuse) and implementing processes to support proper use.
Historically, antibiotic stewardship has focused on the antibiotics themselves and the diseases for which they’re prescribed to treat, but how do health inequalities in our medical system compound the effects of AMR? What can practitioners, policymakers, and patients do to help address health inequity and AMR?
Racial and ethnic disparities have been well documented in many healthcare settings, and
There is inequitable and biased antibiotic prescribing. We urge healthcare providers to be aware of their own biases and to use this awareness to inform equitable patient care practices. There is a need for more diverse healthcare providers.
Attaining equity will help build trust in healthcare, which is critical to our ability to respond to the next healthcare crisis. Additionally, we must design research that accurately quantifies and characterizes existing inequities in AMR. Race and ethnicity demographic data are often absent from studies, and we must continue to develop and implement practices to collect accurate data.
The mission of The Society for Healthcare Epidemiology (SHEA) has always been “Safe Healthcare for All.” As healthcare epidemiologists and antibiotic stewards, we are dedicated to strengthening antibiotic stewardship activities, and patient and public awareness of these issues to improve the overall quality and equity of care in our communities.
1Brown, D., Henderson, H., Ruegsegger, L., Moody, J., & Van Duin, D. (2023). Socioeconomic disparities in the prevalence of multidrug resistance in Enterobacterales. Infection Control & Hospital Epidemiology, 1-3. doi:10.1017/ ice.2023.116

06 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM Safe Healthcare for All shea-online.org
Rekha Murthy, M.D., FIDSA, FSHEA Professor of Medicine, CedarsSinai; DEI Committee Chair, SHEA
The Keys to Accessing Smart Medicines





Every week, my team works tirelessly to give hope to people suffering from life-threatening antibioticresistant infections. Who they are may surprise you.
Rather than the elderly or chronically ill, people of all ages, including children, are in peril because antibiotics, once our go-to cure, are losing their effectiveness. At TAIL Φ R LABS, a non-profit research center at Baylor College of Medicine, we are pioneering a promising alternative to traditional antibiotics — bacteriophages.
Why bacteriophage?

Bacteriophages, or phages, are viruses that kill bacteria. These viruses, like bacteria, exist ubiquitously, not only throughout Earth but within our bodies. They are so abundant they outnumber stars in the known universe, representing a boundless supply of potential antibiotics to combat bacterial infections.








The root of the antibiotic resistance crisis is change. The bacteria change, but our medicines do not. Classical antibiotics are chemically locked compounds. If we want to change them, it may take 10 years and up to $1 billion to bring to the market. But bacteria change fast; so fast that resistance can develop within months of an antibiotic’s introduction to the world.
Enter phage. Unlike antibiotics, a phage uses the same mechanisms bacteria do to change, and fast. Phages are smart medicines that can be harnessed to adapt to bacteria in ways that not only kill resistant bacteria, but possibly prevent resistance altogether.
Tactical deployment
Phages have been used for more than a century, but only recently has technology
and new knowledge emerged that permits scientists to harness their full bacterial busting power.



TAIL Φ R Labs was founded on the idea that phages, under the right conditions, can be customized as a personalized medicine to treat the most problematic of bacterial infections. However, this personalization limits treatment optimization, and we are only beginning to appreciate the intricate relationships between the phages, their bacterial targets, and the patients they treat.
Professor Anthony Maresso, co-founder of TAIL Φ R, refers to this as “addressing the natural history of infection.” Each phage, Maresso says, has a personality that must be appreciated; know the phage and its target, and you begin to appreciate how to use them.
Phiogen, a new biopharma start-up born of TAIL Φ R’s R&D efforts, will leverage new technologies to find the rarest of elite phages to address specific bacterial challenges.




The road ahead




















While phages hold immense promise, we need the same support systems developed for traditional antibiotics, such as rapid diagnostic tools, sensitivity assays, and robust manufacturing pipelines.
By discovering nature’s already wonderful solutions and enhancing their capabilities through technology, phage can become the next great generation of anti-infectives.




This article was paid for by Cellexus.







































07 MEDIAPLANET READ MORE AT FUTUREOFPERSONALHEALTH.COM Contact us: www.cellexus.com l enquiries@cellexus.com l +44 (0) 1382 666357
WRITTEN BY Dr. Austen Terwilliger Co-Founder, TAILΦ R LABS
Advertorial





 WRITTEN BY Haley A. Pritchard, M.D., M.S. Assistant Professor of Clinical Medicine, Indiana University Health
WRITTEN BY Haley A. Pritchard, M.D., M.S. Assistant Professor of Clinical Medicine, Indiana University Health