“Defibrillators


Cardiovascular Health www.healthawareness.co.uk Q3 2023 | A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content “AI can detect heart issues with 40% greater precision, revolutionising diagnosis.”
British Heart Foundation Page 02
Professor Sir Nilesh Samani, Medical Director,
must be placed in areas of highest need, where there is a high incidence of cardiac arrest and low defibrillator provision.”
07
Professor
Andy Lockey MBE, President at Resuscitation Council UK Page
Cardiac rehab provides the personalised support people need to manage health after a cardiac event.

Surprisingly, just 50% of eligible patients take advantage of cardiovascular prevention and rehabilitation programmes across the UK. These are free NHS programmes, delivered by healthcare professionals to BACPR (British Association for Cardiovascular Prevention and Rehabilitation) standards. They aim to empower people who have experienced a cardiac event to manage their condition through better knowledge and exercise.
Support through cardiac rehab
Karen Molloy has had two heart attacks, the first of which was at age 40. “It was a total shock and a life-altering experience, physically and mentally. I was not in a particularly high-risk group.” Leading a busy life as a working mother, Molloy benefited from access to cardiac rehab. “Everybody has different experiences after cardiac events, but rehab gives you the opportunity to rebalance and use the support from experienced professionals to gain the knowledge you require.”

What the programme offers Programmes include an educational component where patients are given information about how best to change behaviours to adopt healthier lifestyles. They also include advice on risk factors and medicines, along with supervised or home exercise sessions. Patients who attend rehab are less likely to experience a recurrence or drift away from using medication. Molloy benefited from learning about approaches to making small changes, such as in diet and exercise — including supervised exercise sessions. She also learnt about the medical side, including the imperative to keep taking medicines. “Above all, I benefited from the emotional support of talking to experts because, as you get back to normal life after a heart scare, you are worried about the future. The process helped me to recalibrate and rebalance.”
Cardiac support from professionals
Molloy urges people who have had cardiac incidents — particularly, women who may not feel they have time in their busy lives — to access cardiac rehab. “Everyone needs a reset after a cardiac incident. If you start researching things on your own, you will get confused and worried. Cardiac rehab assimilates advice through professionals who direct you where to go.”
How AI is improving heart health diagnosis
Artificial intelligence is making its way from labs to hospitals, thanks to new research. Our funding is driving the development of AI that can improve diagnosis, treatment and care for heart patients in the UK and around the world.
MRI scans are crucial tools to help doctors diagnose, monitor, and treat heart disease. However, analysing scans by hand is timeconsuming, taking on average 13 minutes or longer - valuable time that doctors could be spending with their patients.
AI to fast-track diagnosis
A new AI scanning technology, developed by scientists at University College London with funding from the British Heart Foundation, is being introduced into hospitals in the UK and around the globe. The AI tool can analyse scans and spot issues such as early signs of heart disease in just 20 seconds - while the patient is still in the scanner.

The researchers trained the AI using heart scans from over 1,900 people. It measures the size of the left ventricle — the main pumping chamber of the heart — and how well it pumps blood around the body. They found that it was able to detect changes to the heart’s structure and function with 40% greater precision and could draw out information from scans that the human eye can’t detect.
The researchers estimate that their AI tool could save around 3,000 clinician days every year. By helping to fast-track diagnosis, it can also help heart patients get the treatment and care they need much sooner.
Improving women’s heart attack care
Women who have a heart attack are 50% more likely than men to receive the wrong initial diagnosis. Clinical trials are testing an AI tool that could help to narrow the heart attack gender gap.

University of Edinburgh researchers, funded by the British Heart Foundation, are also developing an AI tool to diagnose heart attacks faster and more accurately. Trained on data from over 10,000 people, including 48% women, the AI combines patient information with blood test results to detect troponin, a protein released during a heart attack.
The team found the tool could rule out a heart attack with 99.5% certainty, confirming patients were safe to go home. It also identified those who would benefit from staying in hospital for further tests and was able to diagnose heart attacks with greater accuracy than current tests, especially in women.
New technologies funded by BHF donations could save thousands of lives worldwide. We need your support to power research and drive forward new diagnostic tools and treatments for heart and circulatory diseases. This September, we’re shining a spotlight on these conditions and amplifying the voices of those affected. Please share your stories, time, donations or money to help us beat heartbreak forever.
02 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK @HealthawarenessUK
Why cardiac rehab is a positive step to take after a heart attack
@MediaplanetUK Please recycle
WRITTEN BY Professor Sir Nilesh Samani Medical Director, British Heart Foundation
Project Manager: Millie Thompson millie.thompson@mediaplanet.com Business Development Manager: Josie Mason Managing Director: Alex Williams Country Manager UK: Ellie McGregor | Head of Print & Design: Thomas Kent Designer: Aimee Rayment Content Editor: Angelica Hackett O’Toole | Head of Digital Operations: Harvey O’Donnell Paid Media Strategist: Jonni Asfaha Social & Web Editor: Henry Phillips Digital Assistant: Carolina Galbraith Duarte | All images supplied by Gettyimages, unless otherwise specified | Contact information: uk.info@mediaplanet.com or +44 (0) 203 642 0737 Paid for by BACPR Find out more at bacpr.org
INTERVIEW WITH Karen Molloy Patient
WRITTEN BY James Martin
Why more needs to be done to prevent cardiovascular disease
For many years, HEART UK have referred to cholesterol as the Cinderella of cardiovascular disease (CVD) conditions, due to a serious and sustained lack of cholesterol testing across the UK.

While some positive steps have been taken prior to and since the pandemic, such as the inclusion of cholesterol as a focus within the NHS Long Term Plan and in CVDPrevent, there is much still to do.
Cholesterol is not given the attention it should be A recent review by HEART UK of all integrated care system (ICS) strategies showed that CVD featured in 39 of 42 strategies. However, cholesterol, as a condition, was called out in fewer than half.
Meanwhile, the NHS Long Term Plan (LTP), published in 2019, included targets of preventing 150,000 heart attacks and strokes over the next 10 years and increasing the identification of familial hypercholesterolaemia (FH) (inherited form of high cholesterol) from 7% to 25% by 2024. To date, though, progress has been glacial and both targets look unlikely to be met.
The Government is also working on publishing a major conditions strategy and have announced this will focus on both primary (before the disease has developed) and secondary (reduce the impact of a disease) prevention. This is all good news and very welcome, but, so far, there is little detail on what this looks like - and of course whether cholesterol will be included.
Primary prevention in the community needs more support More also needs to be done to move the conversation on from secondary prevention to include primary prevention in the community, including within GP practices. This is critical because managing people’s CVD risk early and keeping it as low as possible will help to avoid events happening in the first place. Not only does this save the NHS money, but it also keeps families from being torn apart by an event. A key piece of the puzzle will be formalising the role of pharmacists, who are well placed to lead the charge on cholesterol testing, by building this into their contracts.
The time is now for Government to act; only by doing so can we turn the tide on the threat that cholesterol represents. HEART UK would also encourage all adults to get to know and understand their cholesterol and other blood fat numbers and empower people to be taking appropriate action. A simple blood test is all it takes.
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 03 MEDIAPLANET Find out more at heartuk.org.uk/
WRITTEN BY Jules Payne Chief Executive, HEART UK – The Cholesterol Charity
The time is now for Government to act; only by doing so can we turn the tide on the threat that cholesterol represents.
More also needs to be done to move the conversation on from secondary prevention to include primary prevention in the community.
WRITTEN BY Tony Greenway
How a ‘one and done’
treatment could revolutionise heart disease care
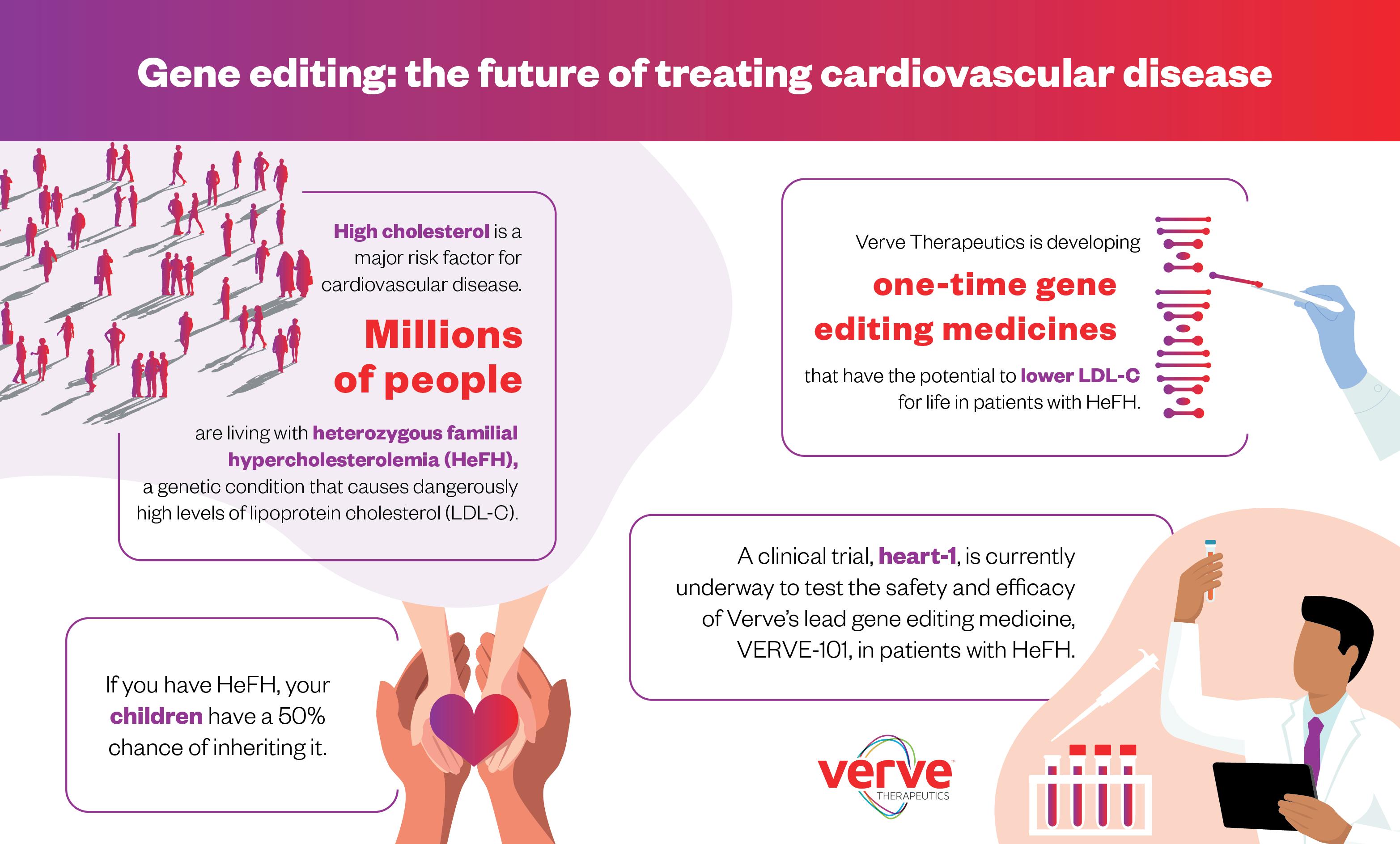
People with high cholesterol need daily medication to lower their risk of heart disease. A ‘one and done’ treatment that could lower cholesterol permanently is in development.
High cholesterol can be a killer. Worryingly, while cholesterol-lowering medications are readily available, many people who need these drugs are not taking them properly — this can be due to a variety of reasons including high costs of medication, side effects, issues with access or poor adherence. Consequently, these individuals are at increased risk of developing potentially fatal atherosclerotic cardiovascular disease (ASCVD).
Why cholesterol can be dangerous to health
It’s important to put cholesterol in context, however. This lipid, or fat, which is produced in the liver, gets bad press — but not all cholesterol is harmful. Indeed, a certain amount of it is important for our metabolism, hormone production and tissue repair.
However, a potentially life-threatening problem occurs when high levels of lowdensity lipoprotein cholesterol (LDL-C) — so-called ‘bad cholesterol’ — cause fatty deposits to build up in the arteries over time.
“As we age, this can result in atherosclerotic cardiovascular disease, which is the leading cause of death worldwide,” explains Dr. Sekar Kathiresan, Co-Founder and Chief Executive Officer of genetic medicines company, Verve Therapeutics. “If the arteries become clogged or blocked due to LDL-C, blood flow can be restricted or cut off. The outcome can be a stroke or heart attack.”

Keeping ‘bad cholesterol’ low for as long as possible
Fortunately, the solution to this global health problem is well-understood. To prevent ASCVD, it’s necessary to keep LDL-C as low as possible, for as long as possible. The challenge is that, while this is straightforward in theory, it’s not so easy to do in practice.
“Cholesterol-lowering medications can be delivered via daily pills or intermittent injections,” says Dr. Kathiresan. “Yet, there is still a large unmet need because the majority of patients who should have this type of treatment are not receiving it. Take those with ASCVD who have already had a heart attack. Only 50% of them are taking any sort of
medication to lower their cholesterol. That’s an unbelievably low figure.”
Genetic disease causing high cholesterol
Then, there are the approximately 3 million patients in the U.S. and Europe who have heterozygous familial hypercholesterolemia (HeFH) — a genetic condition that causes extremely high cholesterol levels from birth. More than 95% of these patients have not achieved their LDL-C goal.
Why not? It can be a challenge to reduce LDL-C to guideline-recommended levels in HeFH patients because of the current model of care for chronic disease, acknowledges Dr. Kathiresan. A new treatment approach could be beneficial to reduce the global burden of HeFH.
Why the current care model to treat chronic disease is broken
There is a fundamental reason why many people with high levels of LDL-C remain untreated, Dr. Kathiresan explains: the chronic care model for disease is broken. “That’s because patients have to be motivated to take a daily pill, or be given a regular injection, for several decades,” says Dr. Kathiresan. “They have to choose to do it — and they have to remember to do it. They also need regular access to the healthcare infrastructure. This puts a heavy burden on patients, providers and the healthcare system as a whole.”
Certainly, the statistics regarding patient adherence to cholesterol-lowering drugs are alarming. Statins are the standard of care for patients who are at increased risk of ASCVD. Taken daily, they remain one of the most commonly used and effective drugs for reducing LDL-C. Even so, studies show that long-term statin use is extremely low; less than 25% of people who are prescribed the medication are still taking it five years later.
Fortunately, gene editing technology could change the treatment paradigm of cardiovascular disease by offering a more convenient — and, crucially, permanent — cholesterol-lowering solution.
04 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
INTERVIEW WITH Sekar Kathiresan, M.D. Co-Founder and Chief Executive Officer, Verve Therapeutics
Paid for by Verve Therapeutics
The chronic care model for disease is broken.
A revolutionary concept that turns off a cholesterol-raising gene Verve has been pioneering a pipeline of genetic medicines for patients who have or are at risk of developing ASCVD.
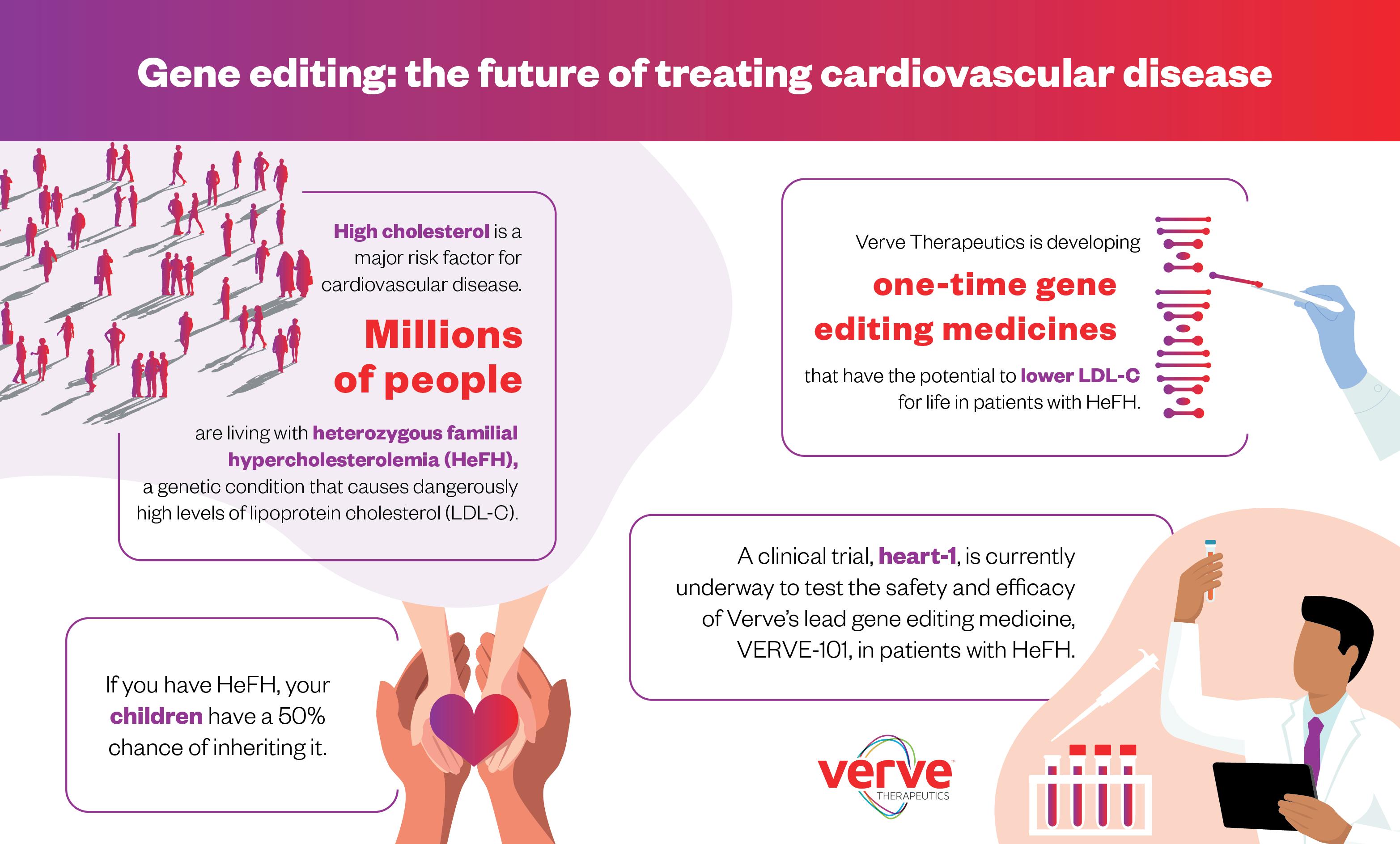
The company’s first medicine being studied in clinical trials, VERVE-101, can be delivered in just one or two hours by intravenous infusion and has the potential to dramatically lower LDL-C levels. The key point here, though, is that it is designed to be a ‘one and done’ single treatment, explains Dr. Kathiresan.
“Once a patient receives the treatment, there’s a potential that their LDL-C will be lowered for life. A one and done treatment could improve the way patients with ASCVD are treated,” he says.
Dr. Kathiresan and the Verve team began to develop the treatment when researchers discovered a group of people who lacked a cholesterolraising gene called PCSK9. “We realised they had hit the jackpot,” he says. “They lacked the gene but were fit and healthy and had very low levels of LDL-C in their blood, and this lifelong low blood cholesterol naturally protected them from the risk of heart attacks. Our idea was to develop a medicine that could mimic the natural protection they experienced by turning off the PCSK9 gene in high-risk people.”
Studying the safety and efficacy of treatment in clinical trials
Verve is pursuing this with a next-generation gene editing technology called base editing. While first-generation gene editing technology cuts the DNA in the gene in a specific location, base editing offers an even more targeted approach — making just a single spelling change in the DNA sequence of the PCSK9 gene turns off PCSK9 protein production by the liver, ultimately lowering LDL-C levels in the blood. Dr. Kathiresan likens it to correcting a spelling mistake with a pencil, erasing and rewriting a specific letter in the gene.
Verve is currently studying the safety and efficacy of the
treatment in clinical trials in both the UK and New Zealand, and initial data is expected later this year. “This is the first time this kind of medicine has ever been tested in patients,” says Dr. Kathiresan. “It’s a remarkable concept — like molecular surgery. Our first two investigational medicines are designed to target PCSK9 safely and effectively, an approach that has been validated by human genetics and pharmacology.”
Value of developing additional treatment options for patients
Understanding the vast unmet medical need in ASCVD, Verve is working as expeditiously as possible to provide patients with an additional treatment option that could be a longer-term solution. “We began this journey in 2018,” Dr. Kathiresan says. “On average, it takes 10 to 12 years for drugs to go through the development and trials process and then receive approval from the UK regulator — the MHRA (The Medicines and Healthcare products Regulatory Agency) — and the US regulator — the FDA (Food and Drug Administration).” If approved by the MHRA in the UK, Dr. Kathiresan hopes that it will be made available through the National Health Service (NHS).
Dr. Kathiresan’s research and founding of the company stems from his family’s connection to ASCVD. “There is a history of high cholesterol in my family,” he reveals. “My brother passed away when he was just 42 after a heart attack. One of the motivations behind Verve was the realisation that we need to do more to avert such tragedies.” This isn’t about replacing conventional therapies, notes Dr. Kathiresan. The company’s aim has always been to develop additional treatment options that could benefit patients and their healthcare providers. “We think a ‘one and done’ medication could add real value,” he says. “It’s new, it’s exciting and, if approved, it could offer a single treatment alternative for those who need to lower their cholesterol.”
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 05 MEDIAPLANET
Once a patient receives the treatment, there’s a potential that their LDL-C will be lowered for life.
Take fainting to heart — there is no such thing as a simple faint
Fainting (syncope) affects one in two people at least once during their lifetime. This unexplained loss of consciousness is a common yet overlooked symptom of an underlying, potentially fatal, heart rhythm disorder.
Many people may faint due to low blood pressure, dehydration or heat-related syncope. However, for others, something more serious can be causing the sudden loss of consciousness.

Fainting can be a sign of underlying heart condition
Any unexplained loss of consciousness or fainting should be investigated, and an electrocardiogram (ECG) should be undertaken and analysed by a heart rhythm specialist (electrophysiologist). Fainting should never be ignored as it can be a sign of an underlying, potentially fatal, heart rhythm condition. If you experience syncope that occurs without warning or is preceded by a racing heart rate, consult your GP urgently.
There is no such thing as a simple faint Fainting is sometimes the only symptom before sudden cardiac death. While many arrhythmias (heart rhythm disorders) are nothing to worry about (after all, we all experience palpitations sometimes), others can prove fatal. Long QT and Brugada are arrhythmia syndromes that can present as ‘simple faints’ leading to sudden death. Sadly, cases could have been easily identified and prevented with a simple ECG and treatment. Both conditions are genetic, so close family members should also be investigated for a history of fainting. Not everyone with Long QT or Brugada experiences fainting episodes — some have no symptoms and die suddenly.
Support for syncope
STARS (Syncope Trust And Reflex anoxic Seizures) is the only organisation providing information and support to people affected by unexplained loss of consciousness. They have a checklist you can download and share with your GP.
During initial assessment, your GP will take a history of your condition and conduct a physical examination, including a blood pressure reading and standard ECG. The Blackouts Checklist, developed under the guidance of STARS’ expert Medical Advisory Committee, will help you prepare for your appointments and equip you with the right questions.
Taking charge of your diagnosis

Unexplained loss of consciousness is traumatic; however, there are ways to manage your condition. Consult your doctor for self-care measures to help manage vasovagal syncope and postural tachycardia syndrome (PoTS), such as isometric counterpressure exercises, compression garments and trigger avoidance. Additionally, you can join patient-to-patient support groups to learn more about your condition and meet other affected individuals. Get the knowledge to support you throughout your care pathway. If you experience ‘simple faints,’ don’t delay — get checked straight away.
Download the Blackout Checklist on stars.org.uk to share with your GP for initial assessment. For 30 years, STARS has supported patients affected by an unexplained loss of consciousness to receive the correct diagnosis and appropriate treatment.
06 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
Unexplained loss of consciousness is traumatic; however, there are ways to manage your condition.
Trudie Lobban MBE FRCP Founder STARS (Syncope Trust And Reflex anoxic Seizures)
New atrial fibrillation treatment with emerging benefits for patients and healthcare
Pioneering treatment for atrial fibrillation at London specialist heart hospital could significantly help to cut NHS wait times.
Royal Brompton and Harefield Hospitals, world leaders in cardiology innovation, are testing a new energy technique for the treatment of atrial fibrillation (AF), which is already receiving positive feedback from patients. The innovation, called Pulsed Field Ablation (PFA), is a potential game-changer for the condition.
Disturbances of atrial fibrillation
Heart rhythm disturbances, such as AF, are diagnosed via an electrocardiogram (ECG) recording or a heart monitor. AF occurs when the electrical activation between the upper chambers of the heart falls out of sync with the normal heartbeat. It is a common condition, particularly affecting people as they age. It can leave people feeling unwell with palpitation and breathlessness.
While AF can be controlled with medication, it is treated most effectively with ablation.
Royal Brompton and Harefield consultant cardiologist and electrophysiologist Dr Zhong Chen notes that if AF is left untreated, the condition can worsen and pose an increased risk of stroke.
Advantages of pulse field ablation
Traditional catheter ablation, which takes one to two hours under general anaesthetic, sees a soft wire guided through a vein into the heart to deliver radio frequency (RF) electrical current that generates heat to treat the area of the heart responsible for the irregular electrical activity.
Now, Royal Brompton and Harefield hospitals are offering PFA, which uses a different energy delivery approach and has advantages over conventional catheter ablation. Dr Chen explains: “The energy is designed specifically to target cardiac tissues, meaning lower chances of injuring nerves, blood vessels and other muscle tissues near the heart.

Reduced risk and quick treatment
The complete ablation process to treat the AF takes only 15–30 minutes. This means the overall procedure takes significantly less time than existing ablation techniques. This is better for patient recovery, with many going home on the same day. “Another bonus is that patients notice little chest discomfort after PFA treatment,” says Dr Chen, who specialises in heart rhythm disturbances in adult cardiac patients. As an early adopter of PFA, Royal Brompton and Harefield Hospitals have treated over 100 patients since the end of last year with positive outcomes.
Improving processes in healthcare
Dr Chen says PFA is a ‘game-changer,’ with shorter treatment times and reduced hospital stays. “If offered to more patients, it will change the way we treat AF,” he adds. “Previously, we could do two ablation cases a day; with PFA, we can fit in five. That improves catheter lab efficiencies. Patients can go home earlier, which is good for the NHS and private care, with implications in reducing waiting lists.”
Defibrillators are designed for public use: how to ensure they’re within reach
A cardiac arrest is the ultimate medical emergency. Early cardiopulmonary resuscitation (CPR) and defibrillation within three to five minutes of collapse can significantly increase a person’s chances of survival.
This year, for our Restart A Heart campaign, we’re highlighting the importance of defibrillators. This piece of equipment is easy to use and doesn’t require training, but it could make the difference between life and death, so it’s important to find and use a defibrillator in an emergency.
Normalising defibrillator use
WRITTEN BY Professor Andy Lockey MBE President, Resuscitation Council UK

A survey of over 4,000 people revealed that 61% were not confident enough to use a defibrillator. We want to change this and let everyone know that early CPR along with defibrillation within three to five minutes of collapse can significantly increase the chances of survival.
Don’t be scared, it’s simple
Publicly available defibrillators are designed to be used by the public — that’s why they are also called ‘public access defibrillators.’ When you switch the defibrillator on, it will provide clear instructions and talk you through what you need to do.
Expanding community access
The Government has recently announced a £1 million pot for community organisations to bid for funding for a defibrillator in their area. The funding will provide an estimated 1,000 new defibrillators in community spaces across England, which is great news.
Distributing defibrillators to the right areas
Now, we need to ensure that community groups place their defibrillator in a location where they can benefit as many people as possible. Defibrillators must be placed in areas of highest need, where there is a high incidence of cardiac arrest and low defibrillator provision.
Research tells us that these are more likely to be in the most deprived communities, so these areas must be prioritised. Currently, defibrillators are disproportionately placed in more affluent areas. At Resuscitation Council UK (RCUK), our ambition is to address this imbalance so everyone, everywhere has their best chance of surviving cardiac arrest.
Locate nearest defibrillator and learn CPR
It’s also vital that guardians of defibrillators register their device on ‘The Circuit.’ This is a network that ensures ambulance services can immediately direct people to their nearest defibrillator, saving valuable time.
Last year, we launched our ‘CPQR code.’ You can scan it and learn CPR in two minutes. More than 14,000 people have scanned the code. This year, let’s ensure we combine CPR with defibrillation wherever possible, so we can increase survival rates of cardiac arrest.

A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 07 MEDIAPLANET
INTERVIEW WITH Dr Zhong Chen, Consultant Cardiologist and Electrophysiologist, based at Harefield Hospital, part of Guy’s and St Thomas’ Specialist Care
Find out more at rbhh-specialist care.co.uk
WRITTEN BY Mark Nicholls
Paid for by Royal Brompton and Harefield
Visit resus.org.uk or scan the QR code to Access lifesaving skills
WRITTEN BY Daniel José Piñeiro President of the World Heart Federation and Professor of Medicine, The University of Buenos Aires, Argentina

Within our grasp: better heart health for all
The global death toll of cardiovascular disease (CVD) in 2021 exceeded 20 million, nearly doubling in 30 years. Often premature and preventable, awareness and access to care involves us all.
On World Heart Day, 29 September, we urge everyone to join the movement to make access to cardiovascular care everyone’s right. It must be a priority in policy and investment. When we know more about our hearts, we can make careful choices.
Prevalence of cardiovascular conditions
Four in five CVD deaths occur in low and middle-income countries (LMICs). Learning about our cardiovascular health for ourselves and those around us — and encouraging others to do the same — will increase awareness and promote the human connection that contributes to heart health.
Cardiovascular conditions can be caused by lifestyle or a genetic predisposition. In addition, neglected CVDs such as rheumatic heart disease and Chagas disease occur in some of the most vulnerable communities, affecting nearly 50 million people combined.

Improving knowledge, investment, equity
With in-depth analysis of CVD risk and mortality data worldwide and trends across gender and regions, the World Heart Report offers insight into approaches and policies to reverse the trend. One priority is Universal Health Coverage for interventions to prevent, manage and
treat cardiovascular conditions and reduce the suffering they cause.
Healthcare investment as a percentage of gross domestic product (GDP) and lower death rates are correlated. CVD death rates are higher in countries where people pay more out-of-pocket for healthcare. Countries must invest at least 5% of GDP in cardiovascular health — a practice currently seen in 97% of high-income countries.
Building on breakthroughs
The signs are encouraging. Today, 91% of countries have policies or programmes targeting tobacco’s harmful impacts while 86% have established guidelines for managing CVD. The digital health landscape is another potential gateway to access by all.
The WHO Essential Medicines List now includes polypills that combine medicinal agents. Polypills offer hope for strengthening access and affordability of care and enhancing patients’ adherence to taking their medication.
Breakthroughs and positive developments often result from pooling resources and committing to change. Together, we can confront cardiovascular disease and give every person and all societies the best chance to flourish.
#UseHeart #KnowHeart
08 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK